P r o d u c t R a t i o n a l e S u r g i c a l T e c h n i q u e - Biomet
P r o d u c t R a t i o n a l e S u r g i c a l T e c h n i q u e - Biomet
P r o d u c t R a t i o n a l e S u r g i c a l T e c h n i q u e - Biomet
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
P r o d u c t<br />
S u r g i c a l<br />
R a t i o n a l e<br />
T e c h n i q u e<br />
ELASTIC STABLE<br />
INTRAMEDULLARY<br />
NAILING
The Nancy and ECMES Nails Philosophy<br />
Elastic Stable Intramedullary Nailing (ESIN) is an established philosophy for treatment of long bone<br />
fractures in children. Pioneered at the Hopital des Enfants in Nancy, France, ESIN relies on the<br />
flexibility of Titanium to provide a stable reduction and dynamisation of long bone fractures in<br />
children. ESIN uses Two Small Diameter Titanium Nails which are pre-bent and inserted in<br />
either a retrograde or antegrade fashion into the fractured bone.<br />
M/L Stability (Figure 1)<br />
The Bend in the nails causes the nails to act as springs which<br />
stabilise the two bone fragments in the medio-lateral plane.<br />
Axial and Rotational Stability (Figure 2)<br />
Figure 1<br />
The Sharp Flattened Extremities penetrate the distal or proximal<br />
cancellous bone to provide both axial and rotational stability to the<br />
bone fragments.<br />
Figure 2<br />
Minimally Invasive Approach (Figure 3)<br />
The Small Diameter of the nails (maximum 4 mm) allows for a<br />
minimally invasive approach (2 cm incision).<br />
Figure 3<br />
Continuous Dynamisation (Figure 4)<br />
Titanium provides flexibility to the nails, thus allowing continuous<br />
dynamic loading of the fracture site.<br />
The Results<br />
These design and biomechanical factors combine to benefit the<br />
child by enabling:<br />
• Early Weight Bearing<br />
• Rapid Return to Normal Activities<br />
Figure 4<br />
2
Clinical Results<br />
Case 1 Case 2 Case 3<br />
Femoral Spiral Comminuted Fracture<br />
Retrograde Nailing<br />
Femoral Transverse Fracture<br />
Antegrade Nailing<br />
Ulna and Radial Diaphyseal Fracture<br />
Bifocal Nailing<br />
Case 4 Case 5 Case 6<br />
Radial Head Fracture<br />
Retrograde Nailing<br />
Spiral Tibial Fracture<br />
Antegrade Nailing<br />
Proximal Humeral Fracture<br />
Retrograde Nailing<br />
3
Design<br />
ESIN can be achieved very effectively with either the Nancy<br />
or ECMES Nails. Both Nails present specific advantages<br />
(Table 1) and the selection of nail type is at the physician’s<br />
discretion.<br />
Indications<br />
The Nancy and ECMES Nails are indicated for the treatment<br />
of diaphyseal fractures of long bones where:<br />
• Minimal growth plate disturbance is paramount<br />
• Dynamisation is required<br />
• The medullary cavity is narrow<br />
Nancy Nail<br />
ECMES Nail<br />
5 diameters<br />
(2.0, 2.5, 3.0, 3.5 and 4.0 mm)<br />
Ti6Al4V Alloy<br />
Curved, Flattened Tip<br />
Atraumatic End<br />
5 diameters<br />
(2.0, 2.5, 3.0, 3.5 and 4.0 mm)<br />
Ti6Al4V Alloy<br />
Curved, Flattened Tip<br />
Atraumatic Cap<br />
Various Pre-cut Lengths Cut to Length Intra-operatively<br />
Table 1. The main features of the Nancy and ECMES nails.<br />
Both paediatric and adult indications are therefore included,<br />
although limited to:<br />
• Paediatric diaphyseal femoral fractures<br />
• Paediatric diaphyseal tibial fractures<br />
• Paediatric diaphyseal humeral fractures<br />
• Paediatric proximal humeral fractures<br />
• Paediatric and adult diaphyseal forearm fractures<br />
• Paediatric radial head fractures<br />
• Adult stable diaphyseal humeral fractures<br />
Contra-Indications<br />
The Nancy and ECMES Nails may not be used for the<br />
treatment of unstable fractures such as long oblique or long<br />
spiral fractures. Comminuted fractures should also be<br />
adequately reduced prior to inserting the nails.<br />
The Nancy and ECMES Nails are not indicated for the<br />
treatment of lower extremity fractures in the adult.<br />
4
Nail Selection<br />
Nail diameter and length are critical in achieving effective<br />
fracture stabilisation.<br />
Length<br />
The length of the nail is equal to the distance separating the<br />
proximal and distal growth plates (Figure 5).<br />
Always ensure that the length of the nail is such that it will<br />
protude one or two centimetres outside the entry portal area.<br />
Diameter<br />
The nail diameter can be chosen either by calculation<br />
Nail Length<br />
Calculation<br />
Nail Diameter = Minimum Canal Diameter x 0.4<br />
1 - 2 cm<br />
or by adopting a typical size as illustrated in Table 2.<br />
Always select the largest diameter nail possible.<br />
Figure 5.<br />
Typical Sizes<br />
Bone Age Nail Diameter<br />
Femur 6 -8 years 3.0 mm<br />
9 - 11 years 3.5 mm<br />
12 - 14 years 4.0 mm<br />
Tibia 8 - 14 years 2.5 to 4.0 mm<br />
Humerus 8 - 14 years 2.5 to 3.5 mm<br />
Forearm 8 - 14 years 2.0 to 2.5 mm<br />
Table 2.<br />
5
Pre-Bending the Nail<br />
Pre-bend each nail to an angle of 30˚, ensuring that<br />
the tip lies in the same plane as the plane formed by the<br />
bend. The pre-bend can be achieved by hand or by using the<br />
Cannulated T-Handle (M21897) as a lever arm.<br />
Caution 1<br />
Ensure that the apex of curvature lies at the level of the fracture site.<br />
✔ ✖ ✖ ✔<br />
Caution 2<br />
In order to achieve optimum reduction, stabilisation and alignment of the fracture, the curvature must be identical in both nails.<br />
6
Surgical Technique<br />
Femoral Fractures<br />
Paediatric femoral fractures are typically treated with two nails inserted in a retrograde<br />
fashion from medial and lateral entry portals located above the epiphysis. Very distal<br />
fractures should be treated with an antegrade approach.<br />
Positioning and Fracture Reduction<br />
The patient is positioned on an orthopaedic traction table (Figure 6). An image<br />
intensifier is positioned so that it can be rotated to obtain AP and lateral views. It<br />
should also be possible to visualise the whole femur from the knee to the hip joint.<br />
The entire thigh including the knee is prepared as an operative field. External<br />
manipulation is conducted until adequate reduction is obtained and confirmed by<br />
flouroscopy.<br />
Figure 6<br />
Approach<br />
Make a 2 cm skin incision distally to the required entry hole to provide access for the<br />
instruments, and to prevent any trauma to the skin (Figure 7). You may start either<br />
on the medial or the lateral side. An oblique drill hole is made 2 - 4 cm above the<br />
growth plate by applying a careful angulation movement of the drill bit until the<br />
entry hole is at an angle of at least 60˚ with the axis of the medullary canal (Figure 8).<br />
Make the the entry hole slightly larger than the diameter of the chosen nail.<br />
Figure 7<br />
Figure 8<br />
7
Figure 9 Figure 10 Figure 11<br />
Nail Insertion<br />
The nail is held in a Cannulated T-Handle Inserter (M21897). Align the horizontal<br />
bar of the T-Handle and the curved tip of the nail in the same plane. This will enable<br />
you to identify the position of the curved tip as it is passed along the medullary canal.<br />
Pass the nail through the entry hole with the curved tip pointing downwards.<br />
Once in the medullary canal rotate the curved tip so that it is pointing in the<br />
direction in which the nail is to be passed (Figure 9). Drive the nail up the<br />
canal by rotating the the T-Handle Inserter back and forth. Avoid using a<br />
mallet to force the passage of a nail which has become stuck as a secondary<br />
fracture may occur.<br />
Advance the nail to the fracture site (Figure 10). With a mallet, lightly<br />
tap the nail across the fracture taking care not to rotate the tip as this<br />
may cause the nail to slip behind or in front of the opposite<br />
fragment. Advance the nail towards the metaphysis and anchor it<br />
into the cancellous bone (Figure 11). Advance the second nail<br />
using the same backward and forward movements. Do not rotate<br />
the second nail through a full 360˚ as this may result in the<br />
second nail wrapping itself round the first nail. Again tap the<br />
nail across the fracture site and advance it towards the<br />
metaphysis and anchor it into the cancellous bone.<br />
8
Figure 12 Figure 13 Figure 14<br />
Final Impaction and Cutting<br />
It is at this stage of surgery that the Nancy and ECMES Nails<br />
must be differentiated. The Nancy Nail is already the<br />
correct length and should now be impacted in its final<br />
position. The ECMES Nail must be cut to length prior to<br />
being impacted in its final position.<br />
ECMES Nail<br />
Once the ECMES Nail is located in the cancellous bone,<br />
impact it in its final position by lightly tapping the<br />
Cannulated T-Handle. Remove the Cannulated T-Handle<br />
and cut the nail using the cutter (M21840), ensuring that<br />
1 to 2 cm of the nail remains outside the entry hole, as for<br />
the Nancy Nail, the tip of the nail can be moderately<br />
Nancy Nail<br />
curved using surgical forceps.<br />
The Impactor/Extractor (M21898) is used to impact the nail<br />
in its final position. By lightly tapping the hammer pad of<br />
the Impactor/Extractor with a mallet the tip of the nail<br />
inserted medially should finally rest against the cortex above<br />
Optional: In order to minimise the risks of soft tissue irritation<br />
caused by the cut tip of the nail, Polyethylene End Caps<br />
(M21941 to M21946) are provided to cover the tip.<br />
the medial femoral condyle (Figure 12).<br />
Post Operative Care<br />
Caution: Do not make unnecessary rotational movements whilst<br />
the Impactor/Extractor holds the nail as it may cause the rounded<br />
tip to snap off.<br />
No immobilisation is required. Once the patient can<br />
straighten the leg, partial weight bearing may commence. As<br />
soon as the patient feels ready, full weight bearing is allowed.<br />
Physiotherapy should reinforce the quadriceps muscle and the<br />
At this stage the atraumatic rounded tip of the nail can be<br />
moderately curved to facilitate its future retrieval (Figure 13).<br />
extension of the knee. Do not force the knee into flexion as<br />
the extremities of the nail may cause some discomfort.<br />
If distraction of the fracture is evident this may be overcome<br />
by exerting pressure on the knee. If the nail is too long, it<br />
may be shortened by using the Nail Cutter (M21840).<br />
Nail Retrieval<br />
The removal of the nails should be undertaken at around<br />
4 - 6 months depending upon the appearance of the X-rays.<br />
For the Nancy Nail, use the Impactor/Extractor (M21898).<br />
For the ECMES Nails, use the Extraction Clamp (M21900).<br />
9
Tibial Fractures<br />
Paediatric tibial fractures are typically treated with two nails inserted in an antegrade<br />
fashion from anteromedial and anterolateral entry portals below the physis. The<br />
recommended age for treating fractures is over 8 years in children or in younger<br />
patients when conservative treatment has failed.<br />
Positioning<br />
The patient is positioned supine on a standard table.<br />
Approach<br />
Make the skin incision proximally to the entry hole to provide better access for the<br />
instruments, and to prevent trauma to the skin. You may start either on the medial or<br />
lateral side. An oblique drill hole is prepared in the proximal metaphysis anteromedial<br />
and anterolateral faces. During the approach the tibialis anterior muscle is pushed<br />
backwards. The nails are passed as per the instructions for the femur. The nails<br />
should not be impacted into the cancellous bone of the distal tibia until any residual<br />
deformity has been corrected.<br />
Insertion and Impaction<br />
As per femoral technique.<br />
Post Operative Care<br />
A simple dressing is put in place for 48 hours after which walking is allowed using<br />
crutches. Plaster immobilisation is not required unless there is a persistent deformity<br />
that requires correction, in which case a below the knee cast should be worn for 3<br />
weeks. Weight bearing can commence between the 4 th and 6 th post operative week<br />
depending upon the appearance of X-rays.<br />
Nail Retrieval<br />
The removal of the nails should be undertaken at around 4-6 months, depending<br />
upon the appearance of the X-rays.<br />
10
Forearm Fractures<br />
Paediatric forearm fractures typically<br />
require only a single nail inserted in<br />
Positioning<br />
The patient is positioned supine with the affected arm on a radiolucent arm table.<br />
each bone, either in an antegrade or<br />
retrograde fashion depending on fracture<br />
location. The recommended age for<br />
treating forearm fractures is over 8 years<br />
in children and adolescents and when<br />
conservative treatment has failed.<br />
Approach and Insertion - Radius<br />
The entry hole is made at the distal metaphysis of the radius. The incision can be<br />
either a stab wound or a larger incision with blunt dissection to avoid the radial nerve<br />
and extensor tendons. An awl is used to make the entry hole which is enlarged by<br />
circular movements. The nail is passed up the medullary canal to the fracture site.<br />
Once the fracture has been reduced, the nail can be passed into the proximal<br />
fragment. Once into the proximal fragment, rotate the nail by 180˚ thus reducing the<br />
pronation of the curve of radius.<br />
Approach and Insertion - Ulna<br />
The entry hole is made on the medial surface of the proximal ulna through the<br />
muscle. Pass the nail as described above and secure it in the distal metaphysis.<br />
Note: The concavity of the two nails must face each other.<br />
Impaction<br />
As per the femoral technique.<br />
Post Operative Care<br />
Plaster immobilisation is unnecessary. Forearm movements can be started early. Skin<br />
irritation by the nail may occur but can be minimised if the patient is informed<br />
before hand.<br />
Nail Retrieval<br />
In some cases the fracture can be slow to reunite and some cases of recurrent fractures<br />
have been observed. It is therefore recommended that removal of the nail is<br />
undertaken at around 8 months.<br />
11
Humeral Fractures<br />
Paediatric humeral fractures are typically<br />
treated with 2 nails inserted in a<br />
retrograde fashion from a posterior entry<br />
portal. The recommended age for<br />
Positioning and Fracture Reduction<br />
The patient is positioned supine without a tourniquet, with the arm supported by a<br />
radiolucent arm table. An image intensifier is required and is positioned so that the<br />
long axis of the humerus is in view.<br />
treating humeral fractures is over 8 years<br />
in children and adolescents and when<br />
conservative treatment has failed.<br />
Approach<br />
A 3 cm skin incision is prepared on the lateral border of the humerus and distally to<br />
the entry hole in order to provide better access for the instruments and to prevent<br />
any trauma to the skin.<br />
Two retrograde oblique drill holes are created on the lateral supracondylar ridge, one<br />
above the other. Make the entry holes slightly larger than the diameter of the chosen<br />
nail.<br />
Insertion and Impaction<br />
The first nail is introduced through the inferior hole and passed upwards, towards<br />
and beyond the fracture site. Rotate the nail through 180˚ so that the curved tip is<br />
anchored in the medial metaphysis. The second nail is introduced through the<br />
superior hole and passed upwards, and anchored in the lateral metaphysis. Impaction<br />
is conducted as per the femoral technique.<br />
Post Operative Care<br />
A sling is used for 3 weeks at which time the patient can begin to mobilise their<br />
shoulder and elbow on their own.<br />
Nail Retrieval<br />
The removal of the nails should be undertaken at 3 months.<br />
12
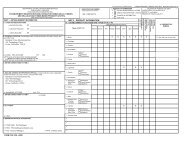
Ordering Details<br />
Nancy Nail<br />
Instruments<br />
Implants<br />
M21897<br />
Cannulated T-Handle Inserter<br />
M21850<br />
2.0 mm Diameter, 130 mm Length<br />
M21898<br />
Impactor-Extractor<br />
M21851<br />
2.0 mm Diameter, 150 mm Length<br />
M21899<br />
Sliding Hammer<br />
M21852<br />
2.0 mm Diameter, 170 mm Length<br />
M21853<br />
2.0 mm Diameter, 190 mm Length<br />
Delivery Systems<br />
M21860<br />
2.5 mm Diameter, 150 mm Length<br />
M21845<br />
Nancy Nail Tray<br />
M21861<br />
2.5 mm Diameter, 170 mm Length<br />
M21862<br />
M21863<br />
2.5 mm Diameter, 190 mm Length<br />
2.5 mm Diameter, 210 mm Length<br />
ECMES Nail<br />
Implants<br />
M21864<br />
2.5 mm Diameter, 230 mm Length<br />
M21922<br />
2.0 mm Diameter, 400 mm Length<br />
M21870<br />
3.0 mm Diameter, 210 mm Length<br />
M21925<br />
2.5 mm Diameter, 400 mm Length<br />
M21871<br />
3.0 mm Diameter, 230 mm Length<br />
M21930<br />
3.0 mm Diameter, 400 mm Length<br />
M21872<br />
3.0 mm Diameter, 250 mm Length<br />
M21935<br />
3.5 mm Diameter, 400 mm Length<br />
M21873<br />
3.0 mm Diameter, 270 mm Length<br />
M21937<br />
4.0 mm Diameter, 400 mm Length<br />
M21874<br />
3.0 mm Diameter, 290 mm Length<br />
M21880<br />
3.5 mm Diameter, 270 mm Length<br />
Polyethylene End Caps<br />
M21881<br />
3.5 mm Diameter, 290 mm Length<br />
4M21941<br />
2.0 mm Diameter<br />
M21882<br />
3.5 mm Diameter, 310 mm Length<br />
4M21943<br />
2.5 mm Diameter<br />
M21883<br />
3.5 mm Diameter, 330 mm Length<br />
4M21944<br />
3.0 mm Diameter<br />
M21884<br />
3.5 mm Diameter, 350 mm Length<br />
4M21945<br />
3.5 mm Diameter<br />
M21890<br />
4.0 mm Diameter, 330 mm Length<br />
4M21946<br />
4.0 mm Diameter<br />
M21891<br />
4.0 mm Diameter, 350 mm Length<br />
M21892<br />
4.0 mm Diameter, 370 mm Length<br />
Instruments<br />
M21893<br />
4.0 mm Diameter, 390 mm Length<br />
M21897<br />
Cannulated T-Handle Inserter<br />
M21894<br />
4.0 mm Diameter, 410 mm Length<br />
M21840<br />
Nail Cutter<br />
M21895<br />
4.0 mm Diameter, 430 mm Length<br />
M21900<br />
Extraction Clamp<br />
M21896<br />
4.0 mm Diameter, 450 mm Length<br />
13
This publication is not intended for distribution in the USA.<br />
Nancy Nail is a trademark of DePuy Orthopaedics, Inc.<br />
© 2011 DePuy International Limited. All rights reserved.<br />
Registered Office: St. Anthony’s Road, Leeds LS11 8DT, England.<br />
Registered in England No. 3319712<br />
Cat No: 9066-70-000 version 1<br />
DePuy International Ltd<br />
St. Anthony’s Road<br />
Leeds LS11 8DT<br />
England<br />
Tel: +44 (0)113 387 7800<br />
Fax: +44 (0)113 387 7890<br />
DePuy France<br />
24 rue Francis de Pressensé<br />
BP 2175<br />
F-69603 Villeurbanne Cedex<br />
France<br />
Telephone: +33 472 69 96 69<br />
Fax: +33 478 93 12 30<br />
0086<br />
Revised: 05/11