CONNECTIONS - Royal College of Nursing, Australia
CONNECTIONS - Royal College of Nursing, Australia
CONNECTIONS - Royal College of Nursing, Australia
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
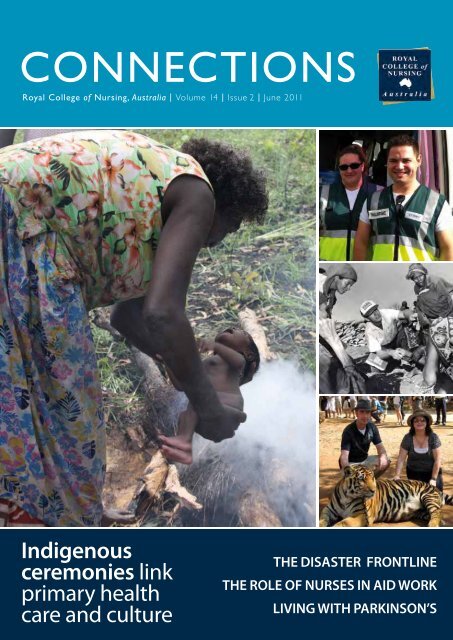
<strong>CONNECTIONS</strong><br />
<strong>Royal</strong> <strong>College</strong> <strong>of</strong> <strong>Nursing</strong>, <strong>Australia</strong> | Volume 14 | Issue 2 | June 2011<br />
Indigenous<br />
ceremonies link<br />
primary health<br />
care and culture<br />
the dIsaster frontlIne<br />
the role <strong>of</strong> nurses In aId work<br />
lIvIng wIth ParkInson’s
InspIrIng,<br />
progressIng and<br />
promotIng the<br />
pr<strong>of</strong>essIon <strong>of</strong><br />
nursIng.<br />
Become an RCNA member, and<br />
contribute to influencing health policy in <strong>Australia</strong><br />
access resources for nurses<br />
receive advice and support<br />
apply for RCNA grants and awards<br />
receive RCNA publications.<br />
Your RCNA membership entitles you to receive discounts on<br />
Guild Pr<strong>of</strong>essional liabilities Insurance.<br />
To find out more visit guildinsurance.com.au/nurses or freecall 1800 810 213<br />
Employment Status<br />
Limit <strong>of</strong><br />
Indemnity<br />
NSW<br />
VIC/WA/<br />
ACT/NT<br />
QLD SA TAS<br />
Employed/Part time $10M $232.76 $242.00 $232.10 $244.20 $235.84<br />
Employed/Full time $10M $384.06 $399.30 $382.96 $402.92 $389.13<br />
Self Employed/Part time $10M $465.52 $484.00 $464.20 $488.40 $471.68<br />
Self Employed/Full time $10M $698.28 $726.00 $696.30 $732.60 $707.52<br />
*Price variations are in accordance with Government and Stamp Duty Fees as applicable in each State.<br />
Part time – Less than 20 hours per week<br />
Full time – 20 hours or more per week<br />
Join today!<br />
www.rcna.org.au<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN<br />
RCNA does not provide advice on whether insurance selected is appropriate or suitable for an RCNA member. RCNA<br />
members should rely on their own enquiries as to whether the insurances are appropriate or suitable for their needs.
From the Chief Executive<br />
Debra Y Cerasa FRCNA<br />
1<br />
The past months have seen natural<br />
disaster devastate communities on the<br />
home front and abroad. As <strong>of</strong>ten<br />
happens, with the worst kind <strong>of</strong><br />
situation comes the best kind <strong>of</strong><br />
human behaviour. The special feature<br />
articles on the Queensland and<br />
Victorian floods in this issue <strong>of</strong><br />
Connections indicate that recent cases<br />
are no exception. These articles<br />
demonstrate the spirit <strong>of</strong> the nursing<br />
pr<strong>of</strong>ession, the team work which<br />
underlines nursing and the<br />
fundamental drive so many nurses<br />
have to care for people in need, <strong>of</strong>ten<br />
with great sacrifice to themselves. In<br />
light <strong>of</strong> these recent experiences <strong>of</strong><br />
nurses in disaster response, RCNA are<br />
developing an exciting new initiative<br />
with a key focus on disaster health.<br />
Keep your eye out for progress in the<br />
September edition <strong>of</strong> Connections!<br />
Another upcoming event is the RCNA<br />
Community and Primary Health Care<br />
<strong>Nursing</strong> Conference (CPHCNC)<br />
which will be held in Hobart from the<br />
19–21 October 2011. The focus <strong>of</strong> the<br />
conference is: Leading the way to local<br />
care and we are planning a<br />
comprehensive event that will provide<br />
CONNECtioNS<br />
<strong>Royal</strong> <strong>College</strong> <strong>of</strong> <strong>Nursing</strong>, <strong>Australia</strong><br />
VOL 14 | ISSUE 2 | June 2011<br />
Connections is distributed quarterly<br />
Editor Debra Cerasa/Jackie Poyser<br />
Editorial coordinator Kathryn Hind<br />
Editorial assistant Casey Hamilton and<br />
Phoebe Glover<br />
Design Nina Vesala<br />
Get published with Connections<br />
Send your submissions to<br />
publications@rcna.org.au<br />
Download submission guidelines and<br />
view our image specifications at<br />
www.rcna.org.au/publications/get_published<br />
Advertise with Connections<br />
Send your enquiries to:<br />
advertising@rcna.org.au or visit<br />
www.rcna.org.au/advertising<br />
a forum to discuss, plan and innovate<br />
ways forward for community and<br />
primary health care. It is such a huge<br />
topic to cover; community and<br />
primary health care affects everyone<br />
as they seek the best care for<br />
themselves and their families and it<br />
is also <strong>of</strong> great importance to a huge<br />
number <strong>of</strong> nurses, as they are the<br />
predominant health pr<strong>of</strong>essionals in<br />
the field. The role nurses play in<br />
community and primary health care is<br />
invaluable and they are working across<br />
<strong>Australia</strong>, including in rural and remote<br />
settings, to ensure it is everything it<br />
should be; accessible, reliable and with<br />
the health and wellbeing <strong>of</strong> patients at<br />
the centre <strong>of</strong> action. The CPHCNC is<br />
going to be the place to tackle issues,<br />
challenges and progressions <strong>of</strong> the<br />
nursing pr<strong>of</strong>ession in community and<br />
primary health care.<br />
On a final note I am thrilled to report<br />
that those <strong>of</strong> us from RCNA who<br />
attended the 2011 International<br />
Council <strong>of</strong> Nurses (ICN) Conference<br />
in Malta in May have returned<br />
invigorated after the opportunity<br />
to unite and engage with the<br />
international community <strong>of</strong> nurses.<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN<br />
Publisher <strong>Royal</strong> <strong>College</strong> <strong>of</strong> <strong>Nursing</strong>, <strong>Australia</strong><br />
1 Napier Close, Deakin ACT 2600<br />
Tel 02 6283 3400<br />
Email canberra@rcna.org.au<br />
ABN 69 004 271 103<br />
Printing Paragon Printers<br />
© <strong>Royal</strong> <strong>College</strong> <strong>of</strong> <strong>Nursing</strong>, <strong>Australia</strong> 2011<br />
The opinions expressed within are the authors’<br />
and not necessarily those <strong>of</strong> <strong>Royal</strong> <strong>College</strong> <strong>of</strong><br />
<strong>Nursing</strong>, <strong>Australia</strong> or the editors. Information is<br />
correct at time <strong>of</strong> print.<br />
All images marked ‘file photo’ or credited to<br />
iStockphoto are representative only and do not<br />
depict the actual subjects and events described in<br />
the articles.<br />
While at the conference, RCNA<br />
hosted a function to promote the<br />
next ICN 25th Quadrennial<br />
Conference to be held 18–25 <strong>of</strong> May<br />
in Melbourne. This conference will be<br />
a fantastic opportunity for <strong>Australia</strong>n<br />
nurses to get involved in the<br />
development <strong>of</strong> the nursing pr<strong>of</strong>ession<br />
on an international level. More on<br />
Malta next issue!<br />
Debra Y Cerasa FRCNA FCN<br />
Chief Executive<br />
Contents<br />
02 Special features<br />
02 Nurses volunteering on the disaster<br />
frontline<br />
04 Reflections on the water<br />
06 Faculties<br />
06 Rural <strong>Nursing</strong> and Midwifery Faculty<br />
10 movement Disorders and Parkinson’s<br />
Nurses Faculty<br />
14 New Generation <strong>of</strong> Nurses Faculty<br />
18 Community and Primary Health Care<br />
Faculty<br />
20 health and Wellbeing in Ageing Faculty<br />
22 national networks<br />
22 Acute Care NN<br />
24 Breast Care NN<br />
26 Ethics NN<br />
28 History NN<br />
30 Leadership NN<br />
32 Legal Issues NN<br />
34 Nurses in Business NN<br />
38 Nurse Practitioner NN<br />
40 Oral Health NN<br />
41 Pastoral <strong>Nursing</strong> Care NN<br />
43 Research NN<br />
46 Transcultural NN<br />
48 RCNA Chapter committees<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
2<br />
special feature<br />
Nurses volunteering<br />
on the diSASter frontline<br />
By James Bonello MRCNA, Emergency Nurse, Flinders Medical Centre<br />
In times <strong>of</strong> natural disasters and tragedy our communities rely upon the hard work and dedication<br />
<strong>of</strong> ordinary <strong>Australia</strong>ns who support our volunteer emergency services. Registered nurse James<br />
Bonello, Chair <strong>of</strong> the RCNA New Generation <strong>of</strong> Nurses Faculty, shares his experiences <strong>of</strong><br />
deployment as part <strong>of</strong> the Queensland Flood Relief effort with St John Ambulance <strong>Australia</strong>.<br />
Photo courtesy <strong>of</strong> M. Jenner<br />
James Bonello (far right) with colleagues from St John Ambulance <strong>Australia</strong><br />
Major flooding devastated extensive<br />
areas <strong>of</strong> Queensland from December<br />
2010 and throughout January 2011.<br />
Large areas were inundated and<br />
washed away, with property destroyed<br />
and lives tragically lost. All <strong>of</strong> <strong>Australia</strong><br />
watched on in disbelief as<br />
Queenslanders faced one <strong>of</strong> the most<br />
severe natural disasters in living<br />
memory.<br />
As a registered nurse and volunteer<br />
with St John Ambulance in South<br />
<strong>Australia</strong>, I was only too keen to put<br />
my hand up when the call for an<br />
emergency response clinical<br />
deployment was made. Fortunately, I<br />
had the support <strong>of</strong> my nurse managers<br />
at Flinders Medical Centre in South<br />
<strong>Australia</strong>.<br />
Feeling excited to be able to help and<br />
slightly apprehensive about the<br />
‘unknown’ elements <strong>of</strong> disaster<br />
response, I also felt as prepared as I<br />
could be; my pr<strong>of</strong>essional experiences<br />
working as a nurse within a major<br />
public hospital emergency department<br />
mean that I’m no stranger to assisting<br />
people in crisis along with their<br />
families. I had also been volunteering<br />
as a uniformed member with St John<br />
Ambulance for several years and<br />
worked part-time as an <strong>Australia</strong>n<br />
Army medic for almost five years. I had<br />
completed additional training in Mental<br />
Health First Aid and previously lived as<br />
a volunteer in rural northern Thailand<br />
for a year, where I spent time in<br />
refugee camps on the Thai-Burmese<br />
border. While all <strong>of</strong> these qualifications,<br />
skills and past experiences gave me<br />
some confidence to fulfil my role,<br />
I knew that the deployment would<br />
challenge me physically and mentally.<br />
The scene in flood affected Brisbane<br />
was shocking. Thigh-high, stinky,<br />
contaminated black mud layered over<br />
previously beautiful suburbs. Entire<br />
homes, warehouses, major bridges and<br />
whole suburbs had been submerged,<br />
showing stark evidence with muddy<br />
water marks and debris caught in<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
special feature 3<br />
I strongly believe that<br />
nurses are uniquely placed<br />
to assist when such large<br />
scale events occur.<br />
“<br />
”<br />
structures far above our heads. Local<br />
residents sat in groups talking s<strong>of</strong>tly, or<br />
wandering slowly down their streets<br />
as if in a trance, ‘shell-shocked’ by the<br />
surreal nature <strong>of</strong> their whole lives<br />
being changed so suddenly. I very<br />
quickly discovered that despite my<br />
previous experiences in emergency<br />
nursing or as an army medic, by far<br />
the most important skill needed was<br />
sincere human compassion and<br />
emotional maturity, as flood victims<br />
sought support and comfort in the<br />
immediate aftermath.<br />
Elderly people in particular would see<br />
our uniforms, see the word ‘nurse’<br />
written across my high-visibility tabard<br />
and converge towards us, or invite us<br />
graciously into what was left <strong>of</strong> their<br />
homes. As well as the medical or first<br />
aid needs, many just wanted some<br />
human contact and reassurance, to<br />
tell their story, to debrief and ask<br />
questions about what was happening<br />
in other areas. Our role within the<br />
community recovery process very<br />
quickly became determined by the<br />
needs <strong>of</strong> those in need.<br />
It was moving to see local residents,<br />
many <strong>of</strong> whom had lost their own<br />
homes and belongings, coming to<br />
volunteer their time and efforts to<br />
clean up public facilities. It was hard<br />
physical work at times, but I did not<br />
hear one person complaining – in fact<br />
morale was positive and resilient. In<br />
addition to this we found many more<br />
people and community groups willing<br />
to provide food and water to workers,<br />
stopping throughout the day to give a<br />
reassuring word <strong>of</strong> encouragement.<br />
On one particularly hot afternoon<br />
some young men arrived at a<br />
community work point with bags full<br />
<strong>of</strong> cold icy poles for the cleanup teams<br />
– a welcomed and much needed<br />
refreshment break. Another older<br />
gentleman told our team how he<br />
wanted to contribute so much that<br />
he’d caught two buses and walked<br />
blocks from his home to come and<br />
<strong>of</strong>fer assistance.<br />
While the vast majority <strong>of</strong> people<br />
banded together, there will always be a<br />
tiny minority who try to exploit others’<br />
misfortune. Local residents in one<br />
flood-affected area told me first-hand<br />
<strong>of</strong> looting and violence that had<br />
occurred during and following the<br />
floods. Residents had lost property<br />
to looters, lost money to con-artists<br />
running scam cleanup or building<br />
services and in some cases been<br />
physically attacked by home invaders<br />
in broad daylight. While the residents<br />
told me that police had acted<br />
promptly and appropriately with<br />
increased patrols, these horrific events<br />
only served to distress and undermine<br />
any sense <strong>of</strong> safety remaining for these<br />
already traumatised people and their<br />
families.<br />
My role in these situations was to<br />
administer first aid or basic medical<br />
care if required, but more importantly<br />
to listen, provide emotional support<br />
and reassurance, assess the person’s<br />
risks and needs holistically based on<br />
their personal situations, then to liaise<br />
with local Brisbane City Council<br />
<strong>of</strong>ficials and other agencies to refer<br />
individual cases for appropriate follow<br />
up. This important link to the<br />
community meant that St John<br />
Ambulance volunteers could help to<br />
ensure victims received ongoing care,<br />
including access to counselling and<br />
financial support.<br />
I strongly believe that nurses are<br />
uniquely placed to assist when such<br />
large scale events occur. We remain<br />
the largest single group <strong>of</strong> health care<br />
pr<strong>of</strong>essionals and with national<br />
registration in place the capacity<br />
to work across state borders is<br />
streamlined without unnecessary ‘red<br />
tape’. Furthermore, I believe that the<br />
unique nursing ethos that engages<br />
Photo courtesy <strong>of</strong> S. Bolton<br />
Incident Management Team command<br />
centre, St John Ambulance Queensland<br />
Photo courtesy <strong>of</strong> S. Bolton<br />
An oval in Queensland which became a<br />
‘temporary’ dumping zone<br />
both clinically and personally with all<br />
areas <strong>of</strong> human experience and need,<br />
along with a fundamental<br />
understanding <strong>of</strong> holistic health factors,<br />
means that nurses will remain a vital<br />
human asset for major disaster<br />
response and relief efforts.<br />
Overall I was encouraged to witness<br />
the incredibly resilient and selfless<br />
response <strong>of</strong> Queenslanders and their<br />
friends from every state and territory.<br />
I would like to acknowledge the<br />
incredible volunteers <strong>of</strong> St John<br />
Ambulance Queensland, many <strong>of</strong><br />
whom are nurses, who freely gave<br />
their time and expertise, working long<br />
hours in extreme heat, all unpaid, to<br />
serve their communities. I commend<br />
and thank you.<br />
If you would like more information<br />
about volunteering or contributing<br />
financially to the invaluable community<br />
work <strong>of</strong> St John Ambulance nationally,<br />
please visit the website:<br />
www.stjohn.org.au<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
4<br />
special feature<br />
Reflections on the water<br />
By Wendy Rogasch, Unit Manager, Acute Services, Rochester & Elmore District Health Service<br />
The old saying “Every dark cloud has a silver lining,” rings true many times during our lifetimes;<br />
and no truer than in recent events for Rochester & Elmore District Health (REDHS).<br />
Two years ago, the terrible events that<br />
unfolded, now known as Black Saturday,<br />
alerted every Victorian to the awesome<br />
and terrible power that mother nature<br />
is capable <strong>of</strong> unleashing on us mere<br />
mortals. Organisations and individuals<br />
across Victoria were suddenly aware<br />
that planning and systems must be put<br />
in place to deal with such situations.<br />
As a result <strong>of</strong> Black Saturday, REDHS<br />
had put into place a framework to deal<br />
with life threatening emergencies and<br />
the unlikely event <strong>of</strong> evacuation. This<br />
framework was tested to its utmost on<br />
Saturday, January 15 2011, when the<br />
unusually torrential rainfall in the upper<br />
catchments <strong>of</strong> the Campaspe, Loddon,<br />
Avoca and Murray River systems<br />
overloaded the river systems far<br />
beyond any previously documented<br />
levels, and the township <strong>of</strong> Rochester<br />
was caught by surprise, to the horror<br />
and amazement <strong>of</strong> all concerned.<br />
On that Saturday, I was enjoying a<br />
warm and pleasant day at Lake<br />
Eppalock, casually incredulous at the<br />
level <strong>of</strong> water, which had risen almost<br />
two metres above its high water mark.<br />
When I eventually checked my phone<br />
later in the morning, I found a number<br />
<strong>of</strong> messages from work asking me to<br />
make contact. I felt sick in the stomach.<br />
I knew there were flood waters on the<br />
way, but was flabbergasted to find that<br />
the staff who were on duty were in<br />
full flight, activating an emergency<br />
evacuation plan. The role given to me<br />
that morning was to stand by in<br />
Bendigo to assist in receiving patients<br />
and residents who were at that time<br />
being loaded onto buses, army vehicles,<br />
ambulances and helicopters to be sent<br />
to numerous locations in the region.<br />
After dashing home to stock up on<br />
clothing and personal items, and to give<br />
my family the news and inform them<br />
not to expect to see me for the rest <strong>of</strong><br />
the day, or even for the next few days, I<br />
arrived at the Mercy Health Bethlehem<br />
Aged Care facility in Bendigo. Moments<br />
later, a large bus arrived and <strong>of</strong>f stepped<br />
all the faces I was so familiar with seeing<br />
at Rochester, certainly not at Bendigo!<br />
Seven aged care residents were to call<br />
Wendy Rogasch<br />
Bethlehem home for an indefinite<br />
amount <strong>of</strong> time.<br />
As staff struggled to unload each<br />
one, slowly and carefully and with<br />
considerable difficulty, the faces <strong>of</strong> each<br />
resident were veiled in fear and<br />
confusion. The faces <strong>of</strong> the receiving<br />
staff glowed with such empathy for the<br />
emotions and pain these elderly frail<br />
folk were all going through. On the<br />
faces <strong>of</strong> the Rochester staff, all smiling as<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
special feature 5<br />
they gently encouraged and consoled<br />
each person, I also saw the underlying<br />
worry for the fate <strong>of</strong> their beloved<br />
residents, the effort that was required<br />
to evacuate each individual with as<br />
much respect and love as humanly<br />
possible, and the hidden fears that they<br />
were all trying not to think about –<br />
their own homes and families who they<br />
knew were battling rising flood waters<br />
<strong>of</strong> a level never before seen<br />
in the area.<br />
I spent the rest <strong>of</strong> that evening assisting<br />
the wonderful Bethlehem staff in<br />
settling in their new lodgers. There were<br />
many questions as they were keen to<br />
continue the care <strong>of</strong> each individual<br />
in a seamless and consistent way.<br />
Medications to be given, special diets to<br />
be arranged, worried residents to be<br />
consoled. Bethlehem staff took it all in<br />
their stride. The cavalry arrived later<br />
that evening, in the form <strong>of</strong> several<br />
Rochy staff members who pitched in<br />
and were also able to give detailed care<br />
requirements <strong>of</strong> each individual. During<br />
a quick ‘check-in’ phone call to our<br />
CEO, Glenis Beaumont, I was given a<br />
portfolio <strong>of</strong> three <strong>of</strong> the destination<br />
health services to act as Liaison Officer;<br />
Bethlehem, Castlemaine Health and<br />
Heathcote Health and so headed home<br />
to plan for the next day’s priorities.<br />
The next day and the following six days<br />
were an endless run <strong>of</strong> phone calls to<br />
check for any issues that may have<br />
arisen, problems that needed to be<br />
solved, visits to each site to touch base<br />
with the patients, residents and staff<br />
who had freely <strong>of</strong>fered to assist in<br />
direct care <strong>of</strong> the evacuees. There were<br />
twice daily phone meetings with the<br />
team, consisting <strong>of</strong> the executive, unit<br />
managers, facilities manager, and<br />
maintenance and support clerical staff.<br />
After each meeting, I was able to then<br />
convey a situation report to all facilities,<br />
staff and patients/residents. I remember<br />
the great pleasure that it was to finally<br />
give the residents the wonderful news<br />
that we were ready to bring all our<br />
people home.<br />
Shortly after we had overcome the<br />
problems arising from the mass<br />
evacuation, we were focusing<br />
on and planning for the return to full<br />
functional service and bringing ‘our<br />
people’ home. The logistics <strong>of</strong> the<br />
return trip turned out to be almost as<br />
challenging as our hurried departure.<br />
To the staff <strong>of</strong> REDHS, I salute you; to<br />
the patients and residents who were<br />
evacuated, your bravery and stoicism<br />
during that week was truly<br />
commendable and to all <strong>of</strong> the staff<br />
from the facilities who so willingly and<br />
graciously welcomed our evacuees, I<br />
cannot thank you enough for your<br />
patience and generosity.<br />
Register<br />
today!<br />
Conference fast facts<br />
Dates: Wednesday 19 – Friday 21 October 2011<br />
Venue: Novotel Sydney Brighton Beach,<br />
New South Wales, <strong>Australia</strong><br />
Expecting in excess <strong>of</strong> 300 delegates from<br />
<strong>Australia</strong>, New Zealand, Asia Pacific region,<br />
Europe and USA<br />
19 July 2011 Early bird registration closes<br />
19 September 2011 Standard registration closes<br />
To register now, visit<br />
www.accypn2011.eventplanners.com.au<br />
The conference theme is Navigating New Directions in<br />
Children and Young People’s Health Care.<br />
Key program themes will include leading and learning:<br />
in practice in global issues<br />
through diversity in leadership<br />
in education in safety and quality.<br />
Keynote speakers<br />
Pr<strong>of</strong>essor<br />
Philip<br />
Darbyshire<br />
Dame<br />
Elizabeth<br />
Fradd<br />
We look forward<br />
to welcoming you<br />
to Sydney in<br />
October 2011!<br />
Associate<br />
Pr<strong>of</strong>essor<br />
Kari Bugge<br />
Ms Molly<br />
Carlile<br />
ACCYPN 2011 Conference Managers T: +61 7 3858 5529 F: +61 7 3858 5499<br />
c/- MCI (formerly Event Planners <strong>Australia</strong>) E: accypn11@eventplanners.com.au<br />
PO Box 1517 Eagle Farm QLD 4009<strong>CONNECTIONS</strong> W: www.accypn2011.eventplanners.com.au<br />
| VOL 14 | ISSUE 2 | june
6<br />
RURAL NURSING AND MIDWIFERY FACULTY<br />
A Cultural Rite – The Smoking Ceremony<br />
Putting culture at the centre <strong>of</strong> health for Aboriginal<br />
mothers and babies<br />
By Margaret Stewart, Lecturer, School <strong>of</strong> <strong>Nursing</strong>, Midwifery and Nutrition, James Cook University<br />
When the songs are not sung, the dances left undone, and the ceremonies no longer remembered,<br />
then the community begins to disintegrate: the old lose heart and the young lose the direction and<br />
the certainty that have so long sustained Aboriginal people (Stewart, 2000).<br />
At the interface between two worlds,<br />
Aboriginal women’s cultural choices<br />
concerned with where a woman<br />
chooses to give birth and the demands<br />
<strong>of</strong> Western medicine have become<br />
problematic, in that the right to exercise<br />
choice has largely disappeared. Women<br />
are at their most powerful yet most<br />
vulnerable when they give birth. This is a<br />
disarming paradox. Therefore, decisions<br />
about birthing must be built around<br />
knowledge, empowerment and social<br />
justice. The long term practice <strong>of</strong><br />
transferring women from their<br />
community to birth elsewhere may be<br />
seen as ‘normal’ practice for some,<br />
however this practice <strong>of</strong>ten has long<br />
term health and cultural implications.<br />
Whilst all efforts are made to provide<br />
the best possible care to Aboriginal<br />
mothers when they are transferred to<br />
a regional centre to birth, in many<br />
instances no one has asked the young<br />
Aboriginal woman if this is her<br />
preference, based on her traditional and<br />
cultural values and her capabilities as a<br />
mother and a woman.<br />
The ‘smoking ceremony’ for many<br />
Aboriginal women may be seen as a way<br />
forward toward compensating for the<br />
loss <strong>of</strong> connection to culture and birth<br />
place as a result <strong>of</strong> having to birth<br />
elsewhere. While the smoking ceremony<br />
after a birth is not common practice for<br />
some Aboriginal communities, it is a<br />
powerful cultural rite and one that has<br />
been practiced for thousands <strong>of</strong> years in<br />
a number <strong>of</strong> remote communities. Many<br />
Aboriginal women hold the view that the<br />
secret to better health and<br />
empowerment lies in this cultural rite<br />
and practice. My experience as a remote<br />
area nurse/midwife, in a number <strong>of</strong><br />
remote communities, has lead me to<br />
believe that it is not only the younger<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
7<br />
women <strong>of</strong> the community who are<br />
disempowered as a consequence <strong>of</strong> an<br />
inability to exercise a right to choose,<br />
but their mothers and grandmothers<br />
are similarly affected by a lack <strong>of</strong><br />
involvement in birthing and child<br />
rearing practices.<br />
The women <strong>of</strong> Milingimbi Community<br />
in the East Arnhem <strong>of</strong> the Northern<br />
Territory demonstrate how the<br />
strength <strong>of</strong> Aboriginal culture, through<br />
the smoking ceremony, rejuvenates the<br />
community. They demonstrate fidelity<br />
to this traditional practice when new<br />
mums and babies present back to the<br />
community. The smoking ceremony can<br />
be performed at any stage <strong>of</strong> a persons’<br />
life but is best performed in the first<br />
instance around the time <strong>of</strong> the birth.<br />
This sets the foundation <strong>of</strong> good health<br />
and wellbeing. The ceremonies for the<br />
land, the kinship relationships and a<br />
sense <strong>of</strong> self worth are sustained.<br />
Further, the importance <strong>of</strong> culture, law<br />
and tradition in maintaining a strong<br />
community continues.<br />
The women speak <strong>of</strong> the smoke as<br />
being a healing and cleansing force.<br />
This force empowers the individual and<br />
ensures the wellbeing <strong>of</strong> the child.<br />
A senior woman <strong>of</strong> the Milingimbi<br />
community says “We put this little one<br />
through the smoke and we know that<br />
this little one will always be strong and<br />
know where he/she comes from.” The<br />
material that is used in the ceremony,<br />
the paper bark, the swamp grass and<br />
the place itself – the edge <strong>of</strong> a paper<br />
bark swamp – all speak strongly <strong>of</strong> an<br />
unbroken and unchanging connection<br />
to the land which is central to good<br />
health.<br />
My experience with the smoking<br />
ceremonies has reinforced for me the<br />
centrality <strong>of</strong> culture and tradition in<br />
creating an authentic primary health<br />
care framework which is respectful<br />
<strong>of</strong> and responsive to the distinctive<br />
environment in which health care<br />
services are delivered. The ceremonies<br />
in the context <strong>of</strong> a paper bark forest,<br />
where women are able to demonstrate<br />
a sense <strong>of</strong> connection to culture and<br />
place, stand in sharp contrast to the<br />
sterility <strong>of</strong> a clinical environment which<br />
may serve to disempower and alienate.<br />
Even the most detached <strong>of</strong> health<br />
pr<strong>of</strong>essionals would have to reflect<br />
on the positive health aspects <strong>of</strong> this<br />
participation in culture and tradition.<br />
While the women may not have read<br />
the texts on primary health care, their<br />
lived experience is one <strong>of</strong><br />
comprehensive primary health care<br />
practice and one from which all health<br />
pr<strong>of</strong>essionals could learn a great deal.<br />
I consider it a great privilege to have<br />
been invited to be a part <strong>of</strong> such a rich<br />
and powerful ceremony. It took me<br />
back to my time in the Kimberley<br />
17 years ago when as an expectant<br />
mother I was passed through the<br />
smoke and upon my return to the<br />
community, my new born child was<br />
passed through the smoke and<br />
welcomed to the land.<br />
References<br />
Stewart, M. (2000). Ngalangangpum Jarrakpu<br />
Purrurn: Mother and Child. The Women <strong>of</strong><br />
Warmun as told to Margaret Stewart. Broome,<br />
WA: Magabala Books.<br />
Left page: From left: Ruth Nalmakarra,<br />
Laurie Milindidj 2, Margaret Stewart, Daisy<br />
Namanatj 2 and Lena Walunydjunalil<br />
Right top: The new mothers Elizabeth<br />
Galangarr and Esther Warrngayu (bottom<br />
centre) look at their babies Natasha and<br />
Antonia after the smoking ceremony, while<br />
their grandmothers Daisy Namanatj 2,<br />
(bottom far right) and Ruth Nalmakarra<br />
(bottom far left) take the lead supporting<br />
role. Extended traditional grandmothers and<br />
mothers (top from left) Laurie Milindidj 2,<br />
Lena Walunydjunalil, Nikisha Gulngura,<br />
Rhonda Gungurinya and Sandra<br />
Mulanyawuy-Dhumy were all a part <strong>of</strong> the<br />
preparation and practice <strong>of</strong> the smoking<br />
ceremony for the new mothers and their<br />
babies<br />
Right middle: Ruth Nalmakarra passing her<br />
grandchild over the smoke<br />
Right bottom: The healing hands <strong>of</strong> Daisy<br />
Namantj, over the fire, as she prepares the<br />
fire and smoke<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
8<br />
RURAL NURSING AND MIDWIFERY FACULTY<br />
A passion for Indigenous health<br />
By Kanya Nanayakkara, Remote Area Health Corps<br />
Alan Wilson<br />
Alan Wilson, a registered nurse from<br />
Sydney, has worked with Remote Area<br />
Health Corps (RAHC) since 2009.<br />
Alan is one <strong>of</strong> a growing example <strong>of</strong><br />
dedicated RAHC health pr<strong>of</strong>essionals<br />
taking up regular repeat placements<br />
in the same remote Indigenous<br />
community. In April 2011 Alan will<br />
complete his seventh RAHC placement<br />
for the Anyinginy Regional Remote<br />
Health Service in communities across<br />
the Barkly region in Central <strong>Australia</strong>.<br />
Alan’s commitment to assisting people<br />
in the Barkly region has helped him<br />
forge a special relationship with the<br />
local Indigenous communities, based<br />
on mutual trust and friendship. Alan’s<br />
repeat placements to the Barkly region<br />
have allowed him to develop a deep<br />
understanding <strong>of</strong> the communities<br />
in the area, their health needs and<br />
priorities and the value placed on<br />
being an honest communicator.<br />
Alan is committed to providing remote<br />
area nursing services and finds the<br />
RAHC model suits his pr<strong>of</strong>essional<br />
and personal circumstances. These<br />
placements enable Alan to have<br />
extended periods in communities<br />
across Barkly combined with regular<br />
return trips back home to Sydney<br />
to see his family and friends.<br />
For success in remote environments,<br />
Alan suggests, “The individual should<br />
be flexible, resilient and have an<br />
appreciation and respect for cultural<br />
differences.” Another trait Alan believes<br />
is vital when working in remote<br />
Indigenous communities is the ability<br />
to speak “straight”, be direct and<br />
compassionate with patients and<br />
ensure they understand what is<br />
being relayed to them.<br />
Be part <strong>of</strong> the effort to improve<br />
Indigenous health<br />
Get involved.<br />
Call 1300 MYRAHC<br />
or apply online<br />
at rahc.com.au<br />
Funded by the <strong>Australia</strong>n Government
9<br />
One story Alan shares is his new<br />
found friendship with not just the local<br />
people but the local animals. While<br />
on placement in 2010, Alan’s partner<br />
Christina came to Tennant Creek to<br />
visit him and found three small stray<br />
pups on the train tracks. When she<br />
tried to remove them, one particular<br />
puppy was quite stubborn and would<br />
not leave. However when Christina<br />
walked away, she turned around to see<br />
that puppy barking and following her.<br />
She took it back to Alan and convinced<br />
him to keep the dog, now named<br />
Jackie. Every night for six weeks Alan<br />
washed the dog in borax, peroxide and<br />
mild shampoo and to his disbelief, black<br />
hair began to grow. When Alan<br />
returned home to Sydney he brought<br />
Jackie with him and before long she<br />
had the family wrapped around her<br />
paw.<br />
Jackie is now a loving dog with black fur<br />
and a single white blaze on her chest.<br />
Alan says, “I have gained a wonderful<br />
friend and mate who keeps me on my<br />
toes, gives me something to do, makes<br />
sure I exercise regularly and likes the<br />
same food as I do. She loves being in<br />
the bush as much as I do; which is<br />
every spare minute.”<br />
Alan believes the work he and other<br />
RAHC health pr<strong>of</strong>essionals are doing<br />
on placements is benefiting<br />
communities as it provides them with<br />
additional access to health care. Alan<br />
Alan’s dog, Jackie<br />
relishes his time at Tennant Creek<br />
and in late 2010 his contribution<br />
was recognised by the Tennant Creek<br />
community when he received a<br />
Certificate <strong>of</strong> Appreciation from the<br />
Anyinginyi Health Centre.<br />
Over the back fence<br />
Pam Brinsmead FRCNA, Pr<strong>of</strong>essional Development Coordinator, Mental Health/Drug and Alcohol,<br />
NSW Health<br />
Pam Brinsmead is a member <strong>of</strong> the Rural <strong>Nursing</strong> and Midwifery Faculty and is one <strong>of</strong> our new<br />
Faculty Advisory Committee (FAC) members. For many years Pam has been a vocal and passionate<br />
advocate for nurses living and working in rural communities. RCNA is thrilled to have Pam’s<br />
expertise on the FAC.<br />
After 19 years <strong>of</strong><br />
working as a nurse<br />
educator, I am still<br />
enthusiastic about<br />
my role and know<br />
there is always<br />
Pam Brinsmead<br />
much more to<br />
learn. Variety continues to fuel the<br />
passion I have for my job. I like the fact<br />
that there are both big picture projects<br />
that challenge me and give me a chance<br />
to have an influence on the culture <strong>of</strong> a<br />
workplace, as well as working on some<br />
really detailed smaller picture issues.<br />
At the end <strong>of</strong> the day, my job is focused<br />
on ensuring that client outcomes, within<br />
our rural mental health and drug and<br />
alcohol services, are the best they<br />
can be.<br />
My earliest memory… Making mud<br />
pies in the red volcanic soil under our<br />
old house in northern New South<br />
Wales.<br />
At school I… won a prize for reading<br />
the entire primary school library by end<br />
<strong>of</strong> grade five. I loved reading then and<br />
still do.<br />
I wish I’d… found out sooner how<br />
much fun it was to have longer hair.<br />
Having a pet… My two long-haired<br />
Dachshunds (Cammie and Menkee) are<br />
my family and the three <strong>of</strong> us just love<br />
snuggling up together on the lounge<br />
chair watching TV on cold winter nights.<br />
The last meal I cooked was… a lovely<br />
grilled porterhouse steak with mashed<br />
potatoes and broccolini.<br />
Kids should be… given every<br />
opportunity to explore and grow as<br />
individuals.<br />
The book that changed my life…<br />
Cherry Ames: Student Nurse by Helen<br />
Wells. As a child I used to play being a<br />
nurse. One day, whilst shaking a glass<br />
thermometer in the hallway, I<br />
accidentally broke it. I clearly remember<br />
chasing the silver mercury balls across<br />
the floor as I didn’t want to have to tell<br />
Mum what I had done. However, she did<br />
find out, as she was highly allergic to<br />
mercury and came out in a dreadful<br />
rash when she next went to wash the<br />
floor on her hands and knees.<br />
My favourite moment is… having that<br />
first taste <strong>of</strong> c<strong>of</strong>fee in the morning.<br />
Relaxing involves… sitting down in my<br />
craft room to make cards. I use a<br />
variety <strong>of</strong> scrapbooking and other<br />
innovative craft techniques to design<br />
and create hand-made cards for friends<br />
and family.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
10<br />
Movement Disorders AND Parkinson’s Nurses Faculty<br />
Peter has Parkinson’s – a partner’s account<br />
By Gillian Adams<br />
“Peter has Parkinson’s.” Well those few words say so much and<br />
yet say so little. Parkinson’s is such a daunting prognosis –<br />
overwhelming, frightening and even the thought <strong>of</strong> writing about<br />
it brings tears to my eyes. My response to Peter’s condition is<br />
reflective <strong>of</strong> the way I perceive the world. It will not be the same<br />
for all who have a person with Parkinson’s (PWP) in their life.<br />
So first <strong>of</strong> all a bit about me… I am an<br />
achiever, in that I perform in ways that<br />
will garner praise and positive attention.<br />
My underlying fear is that the world is<br />
a scary place and that it needs to be<br />
controlled – and who better to do it<br />
but me! Get on with it or just get out<br />
<strong>of</strong> my way! So you can see that Peter’s<br />
condition is a personal challenge to me.<br />
It is something uncertain, something<br />
that I cannot control or ‘fix’ and<br />
something that pushes a lot <strong>of</strong> my<br />
buttons (and not all the good ones).<br />
My first reaction was to get some facts<br />
about Parkinson’s – what it is, what<br />
causes it, what is the progression and<br />
what treatments are available. I learnt<br />
it is a degenerative neural disease,<br />
no-one knows why, it is highly variable<br />
in progression and treatments (but<br />
within a range <strong>of</strong> expected symptoms<br />
and drugs). I also joined an email list for<br />
carers <strong>of</strong> PWP and watched the email<br />
traffic go by. I then promptly ignored<br />
everything I learnt and read as it was<br />
‘all too scary’. With his diagnosis, the<br />
rational part <strong>of</strong> my brain found it easier<br />
to tolerate some <strong>of</strong> his foibles – leaving<br />
the bathroom light on, eating slowly,<br />
procrastinating and mumbling. The<br />
emotional side saw everything he did<br />
and said “it’ll get worse”. My fears<br />
about it being out <strong>of</strong> control became<br />
worse. Our lives, our futures, our plans<br />
and dreams were all vanishing in front<br />
<strong>of</strong> my very tightly closed eyes – or<br />
rather in my imagination. However, the<br />
day to day realities were that not much<br />
changed at all and Peter’s medication<br />
helped him regain control over his<br />
movements and activities.<br />
Nevertheless I was angry, very angry!<br />
At night in my dreams I endlessly<br />
fought with Peter – he would make<br />
changes to our lives without telling me,<br />
I would punch and hit him and yell and<br />
nothing would change, it was all out <strong>of</strong><br />
my control. By day I was calm, a bit<br />
more remote than usual, suffering from<br />
some increased signs <strong>of</strong> stress but<br />
nothing really drastic. It took me six<br />
months or more to realise just how<br />
angry I was. At the same time I realised<br />
that I was actually angry with him.<br />
I then realised that it was not him that<br />
I should focus my anger on (if I had to<br />
focus it on anything or anyone), rather<br />
it was the disease.<br />
Well time has gone by, some <strong>of</strong> Peter’s<br />
symptoms have become worse, while<br />
others have changed very little or even<br />
improved. I worry when he becomes<br />
stressed because his symptoms get<br />
worse and take quite a long time to<br />
recover. I try to let things go and take<br />
life a bit slower – it doesn’t really<br />
matter if we are late or if most things<br />
take a bit longer or even if they don’t<br />
get done at all! When I <strong>of</strong>fer to help<br />
Peter do things it is now no longer out<br />
<strong>of</strong> a desire to ‘just get it done’ rather it<br />
is to help him if he wants the help. Of<br />
course I still get annoyed but I try to<br />
make the most <strong>of</strong> our time together<br />
and when I need a break I take one –<br />
it reduces my irritation with whatever<br />
is (or is not) happening and is an<br />
acknowledgement that I do not have<br />
all the answers and that going with<br />
the flow is acceptable. There is time<br />
enough in the future for whatever<br />
comes and we, and our relationship, is<br />
more important than being in control.<br />
As one <strong>of</strong> the wise women on the<br />
email list said “these moments are<br />
nuggets <strong>of</strong> gold”.<br />
“<br />
I try to let things go and take life a bit slower – it doesn’t<br />
really matter if we are late or if most things take a bit longer<br />
or even if they don’t get done at all!<br />
”<br />
A brief post script… The lesson about<br />
valuing what we have regardless <strong>of</strong> the<br />
progression <strong>of</strong> the disease came home<br />
to me in a very real manner just the<br />
other day. On the email list there was<br />
a posting from a fairly new member <strong>of</strong><br />
the list who asked to be removed from<br />
the list. Her husband, who had been<br />
diagnosed just a few years ago and<br />
who was not yet experiencing the<br />
problems <strong>of</strong>ten discussed on the list,<br />
had recently been killed in an accident.<br />
He had been riding his recumbent<br />
tricycle in a bike lane and was struck by<br />
a driver who had suddenly swerved<br />
out <strong>of</strong> her own lane. She was grateful<br />
that our support group existed and<br />
regretted that her husband did not live<br />
long enough for her to need the kind<br />
<strong>of</strong> help it provides.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
11<br />
I have Parkinson’s – a personal account<br />
By Peter Swarbrick, Psychologist<br />
This is my personal account <strong>of</strong> my Parkinson’s diagnosis. My current situation is that I’m still broadly<br />
functional, still working reduced hours and trying to maintain and prolong my efficacy. There are some<br />
things that just don’t work very well any more (my attempts at dancing frighten small children) and<br />
others which require my full concentration (putting on underwear and doing up shoes).<br />
Peter and Gillian<br />
Today, I’m feeling quite well, probably<br />
because I made myself get enough sleep<br />
last night, but on some days even<br />
breathing seems to absorb all my<br />
attention. I can do most things ‘at my<br />
own pace’, but my pace is <strong>of</strong>ten out<br />
<strong>of</strong> step with those around me. The<br />
challenge for me is to remain positive,<br />
constructive and creative in how I<br />
incorporate this condition in the other<br />
plans I have for the future. None <strong>of</strong> us<br />
really know how long we will be around<br />
for and apart from the occasional days<br />
when I could scream with frustration<br />
that my recalcitrant limbs won’t do what<br />
they’re told, I have a very good life and<br />
can think <strong>of</strong> no one I would change<br />
places with.<br />
My story<br />
Four years ago, I was walking to a baker<br />
for a low-fat apricot scroll (and a<br />
high-fat sausage roll). I had just bought a<br />
new belt clip for my mobile phone and<br />
as I walked my right arm brushed<br />
against it. I stopped and moved the clip<br />
further around. For a day or so that was<br />
sufficient then I noticed my arm<br />
touching it again when I walked. I moved<br />
it further to the back but was curious<br />
about why my arm, which had<br />
previously swung quite happily, even<br />
rakishly when I strode about, now<br />
seemed less enthusiastic. My left arm still<br />
kept the proper rhythm, so I proceeded<br />
in a somewhat lopsided fashion. Perhaps<br />
being a typical male and certainly being<br />
a procrastinator <strong>of</strong> long-standing, I did<br />
nothing about it.<br />
Three months later, my right forearm<br />
and shoulder began to ache and my grip<br />
lessened noticeably. I was training at a<br />
gym at the time, so reasoned that I had<br />
simply strained a muscle or jarred a joint<br />
and continued to work my arm in the<br />
hope that it would come good with<br />
exercise. It didn’t. The pain continued<br />
and despite massage and exercise I<br />
found that my elbow developed a bend<br />
– even when I was standing still, my right<br />
arm would not hang straight unless I<br />
made it.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
12<br />
Movement Disorders AND Parkinson’s Nurses Faculty<br />
You might have thought I would get this<br />
checked out, but no. I had secretly (it<br />
probably wasn’t a secret to those who<br />
knew me) prided myself on being<br />
physically able and fit – or at least able<br />
to be so with a minimal amount <strong>of</strong><br />
exercise. Likewise, since childhood I had<br />
been proud <strong>of</strong> my intellect, my speech<br />
and my abilities to connect with people.<br />
I think this was partly the reason why I<br />
didn’t want to know what was going on<br />
with my body. I told myself it was some<br />
temporary malaise that would right itself<br />
in time. I didn’t want to confront the<br />
idea that something wasn’t working<br />
properly; that I was getting older and<br />
certainly not that it might be something<br />
serious. So I ignored it some more.<br />
A few months later, it was getting more<br />
difficult to avoid. I was having trouble<br />
getting dressed. I was experiencing<br />
cramping and pain in my arm, shoulder<br />
and across my back. The muscles down<br />
my spine were as hard as chestnuts and<br />
I couldn’t find a comfortable position for<br />
sleeping, sitting or standing. My right arm<br />
was developing a crook, as if I was<br />
holding a can <strong>of</strong> beer at a party, and<br />
people were beginning to notice. I<br />
began to wonder if perhaps I had had<br />
a little stroke.<br />
I had bought a large and expensive<br />
motorbike the previous year. Riding it<br />
was just about the most pleasurable<br />
thing I could do at the time, but I<br />
noticed that I was having increasing<br />
trouble with my neck against the wind<br />
pressure. If the day was cool, I would<br />
get shivers and shivers would become<br />
shakes, making it difficult to ride<br />
smoothly. I could still ride quite well,<br />
but the concentration required was<br />
increasing noticeably and reached a<br />
point where I could not simply relax and<br />
enjoy the scenery and the experience.<br />
At my 48th birthday, someone<br />
commented that I was shaking. It was<br />
April (the month, not the person) and<br />
I had just taken the traditional birthday<br />
suit dip in the swimming pool. It was<br />
quite cool (the water, not the<br />
atmosphere) and again, the shivering<br />
became shakes and the more I tried to<br />
control it, the worse it became. I think I<br />
said to someone “I should see a doctor”<br />
and I made the appointment for the<br />
next week.<br />
I saw my doctor <strong>of</strong> many years for what<br />
would be our last appointment. He was<br />
retiring, ironically, because he had<br />
developed Parkinson’s disease himself.<br />
But he must have been in his late 60s or<br />
early 70s. I was in my late 40s and didn’t<br />
On one level, I was pleased to have a diagnosis and know<br />
that there was something actually amiss. On another level, I<br />
was disappointed that it had not been something less serious.<br />
“<br />
”<br />
really consider myself to be in the same<br />
boat. He examined me and referred me<br />
to a neurologist, saying, “I hope it’s not<br />
Parkinson’s.” There was a three month<br />
wait for the next available appointment.<br />
I could say that I spent those three<br />
months anxiously, or with bouts <strong>of</strong><br />
depression, but that would be untrue.<br />
My father has had, for many years,<br />
benign essential tremor, which I believe<br />
has some hereditary characteristics,<br />
so I reasoned that it must be the same<br />
for me.<br />
But on some level, I knew different. Bits<br />
<strong>of</strong> me just didn’t work properly. I have<br />
been a musician since I can remember,<br />
playing clarinet primarily and was still<br />
performing with a jazz band. However,<br />
when we did a big performance, I would<br />
get nervous and my right arm would<br />
lock, my fingers became claws and I<br />
would tremble uncontrollably. Every<br />
morning I would have to stretch to free<br />
up my back and I <strong>of</strong>ten had pain in my<br />
legs. Normally, I could consume a<br />
creditable amount <strong>of</strong> alcohol and still<br />
function effectively on most levels. Now,<br />
I was finding that after two or three<br />
drinks, my speech became unintelligible<br />
and my body would slow to a crawl. I<br />
was experiencing occasional impotence,<br />
although again I could put that down to<br />
ageing. Another thing I put down to<br />
getting older was a gradually reducing<br />
sense <strong>of</strong> smell, which I could actually<br />
remember being affected at least 10<br />
years ago, but hadn’t really connected<br />
it with what was happening to me now.<br />
While waiting for the appointment<br />
with the neurologist, my new doctor<br />
suggested I try acupuncture. It would be<br />
nice to report that it was a rewarding<br />
experience, but it wasn’t. It was<br />
interesting, somewhat uncomfortable<br />
and when I was sitting still with the<br />
needles inserted I didn’t shake so much,<br />
although perhaps that was fear <strong>of</strong><br />
puncturing something vital. The effect<br />
lasted for an hour or two, and after<br />
several sessions, I gave up that line <strong>of</strong><br />
treatment.<br />
By the time the appointment with the<br />
neurologist came around, I had already<br />
decided that I probably had Parkinson’s<br />
disease. As it turned out, I was right and<br />
the appointment was a formality.<br />
On one level, I was pleased to have<br />
a diagnosis and know that there was<br />
something actually amiss. On another<br />
level, I was disappointed that it had not<br />
been something less serious. I don’t<br />
think the reality <strong>of</strong> the confirmation<br />
really came to light until sometime later.<br />
The neurologist prescribed a dopamine<br />
agonist and told me it would make me<br />
nauseous for three days, which it did,<br />
but then my body started to work and<br />
feel a lot better, which was a relief but<br />
also a strong indication that the<br />
diagnosis was correct. The next part<br />
<strong>of</strong> the saga began.<br />
Editor: We thank Peter and Gillian for<br />
their personal and thoughtful accounts<br />
and look forward to Peter’s follow-up<br />
article in the September edition <strong>of</strong><br />
Connections where he will discuss his life<br />
after the prognosis.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
13<br />
So how did I get here<br />
By Victor McConvey MRCNA, Parkinson’s Nurse Consultant,<br />
Parkinson’s Victoria<br />
Victor McConvey<br />
As the dust cloud obscures the road<br />
ahead and I slow to 20km per hour, I<br />
reflect back upon the conversation I<br />
had with a farmer an hour ago. It took<br />
10 minutes <strong>of</strong> talking about the<br />
drought before we were able to start<br />
discussing the difficulties he was having<br />
with his Parkinson’s disease.<br />
As the nurse who is responsible<br />
for supporting people living with<br />
Parkinson’s disease in Victoria, the<br />
driving conditions and the<br />
conversations that occur in a<br />
roundabout way are common place.<br />
I work for Parkinson’s Victoria, the peak<br />
body for People Living with Parkinson’s<br />
(PLWP), and am the only nurse on the<br />
team. Much <strong>of</strong> my role involves<br />
providing advice and signposting<br />
people living with Parkinson’s to the<br />
most appropriate and local service to<br />
them, explaining symptoms and how<br />
they are managed. Encouraging PLWP<br />
to participate in their disease<br />
management and coaching on how to<br />
get the most out <strong>of</strong> interactions with<br />
neurologists and the health care system<br />
is a pivotal aspect <strong>of</strong> the role.<br />
Secondary consultation with other<br />
health care pr<strong>of</strong>essionals on best<br />
practice ways <strong>of</strong> delivering care and<br />
providing education, increasing<br />
awareness and knowledge <strong>of</strong><br />
treatments, is another essential<br />
element.<br />
Parkinson’s is a complex illness<br />
involving the Motor, Non Motor and<br />
Autonomic symptoms and while<br />
incurable there are some very effective<br />
treatments. The biggest challenge is that<br />
the symptom control is supported by<br />
some very complex pharmacology,<br />
with medications being administered<br />
frequently (two hourly is common) and<br />
the margin between being on time or<br />
not is about 10 minutes. If it’s not on<br />
time the symptoms will worsen and it<br />
will be harder to catch up on the next<br />
dose. Not getting medication on time<br />
is the biggest difficulty experienced by<br />
PLWP when they are in hospital and<br />
can have some adverse effects. The<br />
issue is complex and multi factorial;<br />
staffing levels are <strong>of</strong>ten insufficient<br />
to support complex drug regimes,<br />
compounded by a limited<br />
understanding <strong>of</strong> the condition and the<br />
need for medication. <strong>Nursing</strong> staff are<br />
further compromised by policies and<br />
procedures that do not adequately<br />
support patients being able to self<br />
administer their own medications.<br />
A way <strong>of</strong> addressing this issue and<br />
enhancing patient support is the<br />
development <strong>of</strong> a dedicated<br />
Parkinson’s support nurse. I can<br />
appreciate the value <strong>of</strong> this, having<br />
worked in Leeds in the United<br />
Kingdom as a Parkinson’s Disease<br />
Specialist Nurse (PDNS), a role I<br />
consider to be the most satisfying <strong>of</strong><br />
my career. The National Health Service<br />
in Britain is never seen as a great<br />
innovator and is frequently criticised,<br />
however in the case <strong>of</strong> Parkinson’s<br />
disease it has worked collaboratively<br />
with Parkinson’s UK to support the<br />
growth <strong>of</strong> the PDNS and there are<br />
now over 300 PDNS’s across the<br />
United Kingdom.<br />
In my role in Leeds I was able to<br />
develop nurse lead clinics involving<br />
other members <strong>of</strong> the multi-disciplined<br />
team, work within the neurology clinics<br />
and carry out home visits, enabling me<br />
to assess home situations and make<br />
referrals for aids and assistance where<br />
required. The effectiveness <strong>of</strong> this role<br />
was supported by some additional<br />
training allowing me to become a<br />
non-medical prescriber.<br />
The current situation in <strong>Australia</strong> is that<br />
there are very few Parkinson’s nurses<br />
and those that are in posts are <strong>of</strong>ten<br />
employed to support research, specific<br />
therapies or work within a set health<br />
care network. In <strong>Australia</strong> there are less<br />
than 20 Parkinson’s nurses for an<br />
estimated 80 000 people living with<br />
Parkinson’s. It is an objective <strong>of</strong><br />
Parkinson’s <strong>Australia</strong> to grow this<br />
number, so that all people with<br />
Parkinson’s have access to a nurse.<br />
Some achievements are being made<br />
with four Parkinson’s nurses’ positions<br />
opening in Tasmania and some success<br />
in developing pilots for nurse positions<br />
in many states.<br />
This specialist nursing role <strong>of</strong>fers<br />
tremendous satisfaction, enabling<br />
you to work independently and in<br />
partnership with neurologists and<br />
allied health care pr<strong>of</strong>essionals to<br />
address your patient’s needs and<br />
more efficiently use the health care<br />
resources available. However, the most<br />
satisfying part <strong>of</strong> the role is that your<br />
patients value you, your skills and<br />
interventions, which for me is the<br />
essence <strong>of</strong> nursing.<br />
Victor navigating his way through a dust storm<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
14<br />
new generation <strong>of</strong> nurses FACULTY<br />
A third year nursing student<br />
with a world <strong>of</strong> experience<br />
By Kathryn Hind<br />
Peter Kieseker is a third year nursing student, but his life has been a series <strong>of</strong> lessons in helping<br />
people. He is the kind <strong>of</strong> man who has a vault <strong>of</strong> wild and adventurous stories which have informed<br />
a spectrum <strong>of</strong> theories and ideas. Whether he’s undertaking famine aid work in Somalia, working<br />
with refugees in Kosovo, or completing his nursing placement at the emergency department (ED)<br />
<strong>of</strong> a QLD hospital, Peter is always testing boundaries.<br />
He engages deeply with the situations<br />
he throws himself into, collecting<br />
observations and experiences to<br />
brimming point and then <strong>of</strong>fering his<br />
own innovations. If these are the kind <strong>of</strong><br />
traits we can look forward to seeing in<br />
our new generation <strong>of</strong> nurses, the<br />
nursing pr<strong>of</strong>ession is in for quite a ride.<br />
Peter left school at the age <strong>of</strong> 15 and<br />
joined the <strong>Australia</strong>n Army; he wanted<br />
to be a nurse, but he says, ‘things were<br />
different back then’. Men working in<br />
nursing roles were rare and carried a<br />
certain stigma. So Peter shifted his aim<br />
to becoming a mine warfare specialist.<br />
He was selected for <strong>of</strong>ficer training<br />
when he was 19 and following<br />
graduation to commissioned rank, Peter<br />
joined the Medical Corps. He served in<br />
Papua New Guinea, specialising in<br />
malaria field work. This exposure to the<br />
medical world <strong>of</strong> a third-world country<br />
prompted a thirst for knowledge and a<br />
will to contribute that formed the basis<br />
for his future path. Remembering his<br />
time in Papua New Guinea, Peter says<br />
“We would track from one village to<br />
another collecting blood supplies and<br />
samples, doing screen tests and some<br />
eradication education and it got me<br />
interested in the whole primary health<br />
care area.”<br />
Peter put this new desire for knowledge<br />
into action; he left the army and<br />
enrolled in the four year Bachelor <strong>of</strong><br />
Human Movement Studies at the<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
15<br />
University <strong>of</strong> Queensland. He specialised<br />
in physical activity for the atypical,<br />
something close to his heart due to the<br />
experiences <strong>of</strong> his disabled sister. He<br />
landed the job <strong>of</strong> QLD Health Regional<br />
Superintendent for disability services in<br />
Central Queensland but after 5 years in<br />
this position, things began to feel a little<br />
stale. Bored <strong>of</strong> the public service life,<br />
Peter took a leap <strong>of</strong> faith and launched<br />
himself into a new career in the world<br />
<strong>of</strong> international aid. When asked what<br />
prompted this decision he says, “I went<br />
to find adventure. I joined the army for<br />
a bit <strong>of</strong> adventure, but it was a<br />
peacetime army so there wasn’t any<br />
adventure to be had.” It was a huge<br />
change, and one that took Peter to<br />
rarely explored corners <strong>of</strong> the world.<br />
Peter led primary health and emergency<br />
aid teams in Somalia for three years, a<br />
veterinary health and development<br />
team in South Sudan (until the project<br />
was bombed out <strong>of</strong> existence), refugee<br />
work in Serbia and Kosovo, and was the<br />
<strong>Australia</strong>n representative for Freedom<br />
from Hunger in Cambodia, responsible<br />
for refugee repatriation and irrigation<br />
rehabilitation. Peter claims Somalia is the<br />
most extreme place he’s been. He says<br />
“The government had fallen apart and<br />
it was just the wild west out there.<br />
Everywhere we went we had to go<br />
armed, had to take escorts with us. It<br />
was very hard to do primary health care<br />
in that setting, but <strong>of</strong> course if you don’t,<br />
a lot <strong>of</strong> people die unnecessarily.”<br />
In between assignments, Peter found<br />
time to work for a year as the<br />
establishing CEO for Unicare, the then<br />
Uniting Church <strong>of</strong> Queensland’s state<br />
wide disability service. Peter’s next<br />
assignment was <strong>of</strong> a different nature; the<br />
birth <strong>of</strong> his daughter, Telissa. He gave up<br />
full-time aid work in order to be close<br />
to her, though he still went to the aid<br />
field for short missions. It was during this<br />
time at home that Peter decided to<br />
return to university and undertake a<br />
Bachelor <strong>of</strong> <strong>Nursing</strong> Science (Graduate<br />
Entry) at University <strong>of</strong> the Sunshine<br />
Coast. His studies are by no means a<br />
different direction to aid work; Peter<br />
sees nursing as a tool to greatly enhance<br />
the aid he delivers. He says “Whenever<br />
you’re in the aid world, people come up<br />
to you with their health problems and<br />
nursing fills in the square; I have more<br />
knowledge, more ability and more skills<br />
which means I can actually help in the<br />
short-term as well as the long-term.<br />
If someone comes up with an injury,<br />
I can do something. Well, I will be able<br />
to, if I pass!”<br />
Peter believes there is enormous scope<br />
for nurses to play an integral role in<br />
international aid. Opportunities include<br />
front line nursing intervention, nurse<br />
education and primary health care.<br />
Peter states, “This role is for someone<br />
who’s got a bit <strong>of</strong> adventure in them.<br />
You can go for short periods <strong>of</strong> time<br />
so you don’t have to lose your career<br />
structure. It’s just a broadening<br />
experience.” Peter goes on to talk about<br />
a period in Somalia when he was<br />
working with a small team <strong>of</strong> nurses<br />
and midwives; “I was helping with<br />
miscarriages and things like ventouse<br />
extractions, not knowing what I was<br />
doing but just following the midwife’s<br />
instructions. You’re the only person<br />
there, you’ve got to try and do<br />
something. And now I’ll know more<br />
about what to do.” Equipped with<br />
formal training, Peter will be able to<br />
educate these communities in need <strong>of</strong><br />
aid. “Education is always a fundamental<br />
aim <strong>of</strong> any primary health care<br />
intervention and the measure <strong>of</strong> its<br />
success is if when you leave the project,<br />
a local person can take over your job.”<br />
Before taking on these missions,<br />
Peter must first finish his own nursing<br />
education and in this he is not alone. His<br />
daughter, Telissa, is currently in her third<br />
year <strong>of</strong> a degree in midwifery at the<br />
Queensland University <strong>of</strong> Technology<br />
and his partner, Bhavana, is in her third<br />
year <strong>of</strong> nursing, currently undertaking<br />
placement in mental health on the<br />
Sunshine Coast. Peter plans to do a<br />
graduate year in the Northern Territory<br />
and when he and his family have<br />
finished their studies, they plan to take<br />
on aid work. “We will be heading to<br />
Africa; it’s the place I know best. Because<br />
my daughter is coming, I’ll probably go<br />
to tamer places than where I’ve been<br />
before”, he says. With Peter’s track<br />
record, it is bound to be a wild<br />
adventure. Wherever they end up,<br />
there’s no doubt this family team <strong>of</strong> new<br />
generation nurses will be a force to be<br />
reckoned with.<br />
Left page: Delivering food to a remote village<br />
in west Somalia – there was no food as an<br />
opposing war lord’s gang had destroyed all<br />
food and seed stock<br />
Top: A refugee camp where diarrhoeal<br />
diseases were killing about 70 children a day<br />
– the woman was asking Peter for help with<br />
her infected eye, a turning point that inspired<br />
him to extend his medical knowledge into<br />
nursing<br />
Middle: An extremely remote village in Papua<br />
New Guinea – Peter and his team took blood<br />
samples looking for malaria epidemiology<br />
pr<strong>of</strong>iles and blood infection and followed up<br />
with vector control programs<br />
Bottom: Bhavana, Telissa and Peter<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
16<br />
new generation <strong>of</strong> nurses FACULTY<br />
Making the connection: Reflections <strong>of</strong><br />
first semester tutorial for third year nursing students<br />
By Susan Austin MRCNA, Senior Project Officer, Dementia Workforce Development Officer<br />
Health care is<br />
constantly evolving<br />
with advances in<br />
person-centred<br />
care becoming<br />
more complex<br />
Susan Austin<br />
in addition to<br />
technological progression; this results in<br />
a greater need for higher order thinking<br />
skills. <strong>Nursing</strong> students have a vast<br />
quantity <strong>of</strong> information to consume in<br />
the undergraduate nursing curricula in<br />
preparation for their first qualified<br />
nursing position. Due to the nature<br />
<strong>of</strong> the pr<strong>of</strong>ession, it is necessary to<br />
develop undergraduate nurses as<br />
lifelong learners (H<strong>of</strong>fman, 2008).<br />
Sessional academics like myself are an<br />
essential part to the process <strong>of</strong> learning.<br />
This is partly due to the promising<br />
number <strong>of</strong> nursing students, the delivery<br />
<strong>of</strong> course <strong>of</strong>ferings or the opportunity<br />
to act as a temporary replacement for<br />
faculty staff (The University <strong>of</strong><br />
Queensland, 2003). Sessional academics<br />
can at times feel isolated and excluded<br />
from faculty communication due to the<br />
time spent on campus and the nature<br />
<strong>of</strong> the business (Gottschalk, &<br />
McEachern, 2007).<br />
In preparation for the first tutorial <strong>of</strong><br />
the semester, I found myself doing<br />
hours <strong>of</strong> preparation, even though I had<br />
been given the outline <strong>of</strong> what to cover<br />
and activities to conduct in class. Having<br />
done a Graduate Certificate in Higher<br />
Education last year, I call myself a late<br />
bloomer even though I have conducted<br />
workshops in hospitals, given<br />
conference presentations and<br />
guest lectures at universities.<br />
One <strong>of</strong> the primary concerns for<br />
the first tutorial, dealing with health<br />
promotion, was how well would I<br />
connect with third year students to<br />
assist them in actively embracing the<br />
subject, so that they will return to<br />
further tutorials in preparation for<br />
assessment and clinical competency.<br />
Like any first class, nerves play a part<br />
for educator and student. For me this<br />
meant more preparation than usual,<br />
developing ice breakers to assist in<br />
learning names and gaining information<br />
One <strong>of</strong> my aims was to facilitate an experience<br />
that students would not get anywhere else and<br />
to make sense <strong>of</strong> the unit content.<br />
“<br />
”<br />
on backgrounds, establishing the ground<br />
rules and conducting small group<br />
activities. One <strong>of</strong> my aims was to<br />
facilitate an experience that students<br />
would not get anywhere else and<br />
to make sense <strong>of</strong> the unit content.<br />
Knowing that my cohort was <strong>of</strong> the<br />
generations X and Y, I needed to be<br />
flexible in my delivery but still cover<br />
what was necessary. I took into<br />
consideration the various types <strong>of</strong><br />
learners (visual, audio, kinesthetic) and<br />
different cultural identities by finding<br />
examples <strong>of</strong> each to demonstrate key<br />
points. The whiteboard became my<br />
friend – posing questions related to<br />
everyday issues created discussion and<br />
links to students’ experiences. I also<br />
incorporated different perspectives,<br />
involved students to think outside the<br />
box and allowed time for students to<br />
focus on psychosocial and interpersonal<br />
issues that confront consumers <strong>of</strong><br />
health care. This was beneficial as it<br />
presented awareness and depth <strong>of</strong><br />
knowledge <strong>of</strong> the topic being discussed.<br />
At the end <strong>of</strong> the tutorial, I asked<br />
students for comments and feedback,<br />
which was minimal as they headed for<br />
the door. However, a few students<br />
came up and asked the normal<br />
questions concerning assessment. Later<br />
that afternoon, I received an email from<br />
the Unit Coordinator on feedback from<br />
some <strong>of</strong> the students indicating they<br />
had really enjoyed the session. To me<br />
that was the icing on the cake, because<br />
I had enjoyed the experience just as<br />
much and it helped me to develop<br />
more confidence. I wrote down my<br />
reflections to help my recognition <strong>of</strong><br />
what had worked well, and what had<br />
been learnt, what could be improved<br />
and what would be different next time.<br />
I believe that dedication to providing a<br />
holistic undergraduate experience can<br />
be very gratifying for both the student<br />
and educator. Reflective practice is after<br />
all an integral part <strong>of</strong> lifelong learning,<br />
which our nursing pr<strong>of</strong>ession strives<br />
to represent.<br />
References<br />
Gottschalk, L., & McEachern, S. (2007). Casual<br />
and Sessional Employment: Motivation and Work/<br />
life Balance. Retrieved March 24, 2011, from<br />
http://www.ballarat.edu.au/ard/business/<br />
resources/casual_sessional_employ.pdf<br />
H<strong>of</strong>fman, J. (2008). Teaching strategies to<br />
facilitate nursing students’ critical thinking.<br />
Annual Review <strong>of</strong> <strong>Nursing</strong> Education, 6, 225-236.<br />
The University <strong>of</strong> Queensland, (2003).<br />
Literature review: Training Support and<br />
Management <strong>of</strong> Sessional Teaching Staff.<br />
Retrieved March 24, 2011, from http://www.<br />
tedi.uq.edu.au/sessionalteaching/pdfs/Lit_<br />
review/Lit_review2.pdf<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
17<br />
The ‘Matures’<br />
By Natalie Ellis RCNA Student Member<br />
have travelled to Walgett, Deniliquin<br />
and Terrigal for my practicals and found<br />
welcoming and supportive people<br />
throughout. I am learning skills that<br />
I will use for a lifetime and making<br />
friends I am sure I will keep forever.<br />
Juggling four children, working parttime<br />
and studying full-time for the past<br />
18 months has been hectic, to say the<br />
least, for my family and I. The first four<br />
weeks <strong>of</strong> full-time study were the most<br />
challenging, as I had submitted my first<br />
essay and was exhausted – I was just<br />
about ready to give it all up. I said to<br />
one <strong>of</strong> my friends that if I failed the<br />
essay it would be a sign that I am mad<br />
for trying to go back to university!<br />
Fortunately this was not to be as I<br />
received a distinction and proceeded<br />
to ‘walk on air’ for the next two weeks.<br />
I think this was the point I realised I<br />
could do it.<br />
Natalie (right) and Heidi Mackay, (left) a fellow ‘mature’<br />
For all those people who have dreamt<br />
<strong>of</strong> becoming a nurse, but worried it<br />
may not eventuate please read on as<br />
my story will show that it is possible!<br />
I have known since I was five years old<br />
that I wanted to be a nurse. I started<br />
my training when I was 19 but deferred<br />
to look after my ill mother. I then went<br />
on to marry and have four children.<br />
During this period I did work in<br />
medical related fields thinking that<br />
would satisfy me however it only made<br />
me want to be a nurse even more.<br />
One day I finally had the courage to<br />
talk with staff at Charles Sturt<br />
University and they suggested I do a<br />
single subject to see how I coped with<br />
juggling studying, working and<br />
parenthood. Seeing as 18 years had<br />
now lapsed between my initial training,<br />
I was terrified at the thought <strong>of</strong> writing<br />
an essay. I quickly discovered that there<br />
is so much help and support that you<br />
can access through the university<br />
setting – especially if the staff can see<br />
that you are enthusiastic and eager to<br />
work hard. There are also learning<br />
advisors who can assist you with essay<br />
writing skills and review your grammar<br />
and formatting. Away from the campus<br />
setting, you can also access numerous<br />
websites for information. I found this to<br />
be especially true for subjects such as<br />
anatomy and physiology.<br />
After passing one subject I realised that<br />
studying was a feasible option for me<br />
and my family, so in 2010 I commenced<br />
as a full-time student, studying a<br />
Bachelor <strong>of</strong> <strong>Nursing</strong>. As a mature aged<br />
student I thought I would be on my<br />
own but was amazed to find several<br />
more people in a similar life situation<br />
to me – in their late thirties, with<br />
families, who had returned to university.<br />
Over the last 18 months we have<br />
managed to form a small network<br />
where we support and encourage one<br />
another. Our little group has been<br />
nicknamed the ‘Matures’ by some <strong>of</strong><br />
the younger students (who I have also<br />
become firm friends with) and I think<br />
that name will stick! During this time I<br />
I have now embarked on my second<br />
year <strong>of</strong> study. While I realise there<br />
will be many more late nights and<br />
challenges to come, I know with great<br />
certainty that come what may, I am<br />
going to graduate as a registered<br />
nurse.<br />
Natalie and her family<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
18<br />
COMMUNITY AND PRIMARY HEALth C ARE FACULTY<br />
Community nursing:<br />
A career to be proud <strong>of</strong><br />
By Patricia Shepherd FRCNA, Regal Health Services, Executive Director <strong>of</strong> <strong>Nursing</strong><br />
Looking back over 50 years in the nursing pr<strong>of</strong>ession, and 45<br />
years <strong>of</strong> service to the community after founding Regal Health<br />
Services, one <strong>of</strong> the most rewarding aspects has been the lifestyle<br />
that Regal has provided for my family. This is something that many<br />
<strong>of</strong> us think <strong>of</strong> as secondary, but as a young mother raising two<br />
small children, finding my feet in a pr<strong>of</strong>ession I love was an<br />
astounding piece <strong>of</strong> luck.<br />
In 1954 I had not yet recognised the<br />
career <strong>of</strong> nursing as one for me and<br />
was busily working for a stock broker<br />
in Sydney. Luckily, said stock broker did<br />
recognise nursing as a good fit for me<br />
and encouraged me to apply. It took<br />
me a further year <strong>of</strong> indecision until I<br />
realised nursing was the career for me<br />
and I commenced my general training<br />
at Repatriation General Hospital<br />
(RGH) Concord. I feel incredibly<br />
fortunate to have trained at Concord<br />
as the training school was excellent,<br />
frequently topping the state in the final<br />
examinations despite its then status<br />
as an emerging ‘new’ hospital. On<br />
completion <strong>of</strong> my general training I<br />
was encouraged to go to the Mater<br />
Maternity Hospital to obtain my<br />
midwifery certificate, where Sister<br />
Margaret Mary was the Matron, an<br />
inspiration to all nurses who had the<br />
good fortune to train there. On<br />
returning to Concord I was sent to the<br />
training school part-time, spending the<br />
remainder <strong>of</strong> my time in a wonderful<br />
ward to learn about becoming a<br />
registered nurse and the responsibilities<br />
that went with holding this position.<br />
I had the utmost respect for the<br />
Charge Sister (Sister Clare Gill) and<br />
shall be eternally grateful to her, as<br />
she was a great mentor to me.<br />
In 1961 I moved to London with my<br />
husband, returning in 1962 with a one<br />
year old daughter, Anna, and six months<br />
pregnant with my second child, John.<br />
By then nursing was very much in my<br />
blood and with the help <strong>of</strong> my mother<br />
I worked two nights a week in<br />
hospitals. I soon realised I needed<br />
more. My mother, as well as the owner<br />
Anna and Patricia Shepherd<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
19<br />
Community nursing was not as big as it is today<br />
and I quickly discovered that there was a need for a<br />
good private community nursing service.<br />
“<br />
”<br />
<strong>of</strong> the nursing club I was working for,<br />
encouraged me to consider going it<br />
alone and in 1966 Regal Aid Service<br />
(now Regal Health Services) was born.<br />
Community nursing was not as big as<br />
it is today and I quickly discovered that<br />
there was a need for a good private<br />
community nursing service. At first<br />
there was just me, but I gradually<br />
added friends and other nursing<br />
colleagues. Right from the start my love<br />
<strong>of</strong> education was the ‘driver’ behind<br />
Regal. I quickly introduced evening<br />
educational lectures, which were well<br />
attended by our nurses hungry for<br />
more knowledge. We started these<br />
VENUE & ACCOMODATION<br />
lectures in a private home then moved<br />
to the <strong>College</strong> <strong>of</strong> <strong>Nursing</strong>. Strangely<br />
enough the shift into the area <strong>of</strong><br />
community nursing, where I saw a need<br />
for additional training and services, was<br />
the real breakthrough for Regal.<br />
Thankfully this need has lessened<br />
over the years and perhaps the most<br />
significant change in the nursing<br />
industry has been the recognition <strong>of</strong><br />
community nursing by the health funds.<br />
The Fourth Tasmanian Infection Control Association<br />
Biennial conference will be held at the<br />
Wrest Point Casino, Hobart, Tasmania.<br />
Wrest Point is a Tasmanian icon – a world<br />
class hotel, convention and entertainment<br />
centre located in the yachting precinct <strong>of</strong><br />
Sandy Bay. With breathtaking views <strong>of</strong> the<br />
Derwent River and Mount Wellington, and a<br />
range <strong>of</strong> facilities that are unequalled in the<br />
State, Wrest Point is the ultimate convention<br />
venue.<br />
The TICA conference will be held in the Wellington<br />
rooms at Wrest Point Casino. The Wellington<br />
rooms enjoys beautiful views <strong>of</strong> the<br />
marina and Derwent River, and features natural<br />
lighting.<br />
Wrest Point Casino - 410 Sandy Bay Rd<br />
Hobart, TAS 7000<br />
Throughout my career I have also had<br />
a commitment to the war veteran’s<br />
community, being the daughter <strong>of</strong> an<br />
army <strong>of</strong>ficer who fought in both WWI<br />
and WWII and having three brothers<br />
TICA Conference 2011 Registration Costs<br />
nce can be undertaken who fought in WWII. I had Early Bird also trained Full<br />
erence website –<br />
prior 10/07/2010 Registration<br />
website you can register at the veterans’ hospital, so it was a<br />
TICA Member $175 $220<br />
and request an invoice.<br />
Non TICA Member $220 $270<br />
cated on the conference<br />
natural fit for Regal to move into this<br />
Student $200 $200<br />
health area. We have now treated<br />
more than 20 000 veterans and<br />
engaged over 1000 community nurses.<br />
become the first private community<br />
nursing service in <strong>Australia</strong> to be ACHS<br />
accredited.<br />
Through all these years <strong>of</strong> business<br />
establishment and growth I was also<br />
busy caring for my two children and in<br />
1983 these two ‘worlds’ were to join.<br />
Anna joined Regal when she was just<br />
21 to help out for a short time – Anna<br />
is still here today! We are very proud<br />
<strong>of</strong> the high standard Regal continues<br />
to provide to the community, for the<br />
benefit <strong>of</strong> our patients and our nurses.<br />
After 50 years working in the<br />
community nursing sector I remain<br />
optimistic about the future. I believe<br />
we need to focus on further health<br />
care services being delivered in the<br />
community, coupled with a recognition<br />
that our community deserves and<br />
needs highly skilled and experienced<br />
community nurses. It concerns me<br />
to see that some services in the<br />
community are being delivered by<br />
organisations that do not necessarily<br />
match the skill set with the service<br />
requirement.<br />
I am very proud to be a nurse, and <strong>of</strong><br />
my career in community nursing. I was<br />
honoured to be recognised by RCNA<br />
when they invited me to become an<br />
RCNA Fellow in 2009.<br />
Register today<br />
Keeping It Clean<br />
4th Biennial TICA Conference<br />
Another important milestone in my<br />
career was when my daughter and I<br />
worked with the <strong>Australia</strong>n Council<br />
on Healthcare Standards (ACHS) to<br />
establish community nursing standards<br />
for Regal. In 1994 Regal was to<br />
www.thetica.net.au<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
20<br />
HEALth AND WELLBEING IN AGEING FACULTY<br />
Duty <strong>of</strong> care to vulnerable adults<br />
By Associate Pr<strong>of</strong>essor Linda Starr FRCNA<br />
June 15 is World Elder Abuse Awareness Day and an opportunity<br />
for all health practitioners (and indeed members <strong>of</strong> the community)<br />
to consider how we can contribute to the prevention, identification<br />
and prosecution <strong>of</strong> elder abuse and help to protect older people.<br />
The World Health Organization has<br />
defined elder abuse as:<br />
“A single or repeated act or lack <strong>of</strong><br />
appropriate action, occurring within<br />
any relationship where there is an<br />
expectation <strong>of</strong> trust, which causes<br />
harm or distress to an older person.”<br />
(WHO, 2008)<br />
Abuse <strong>of</strong> the older person is not only<br />
a breach <strong>of</strong> their civil rights but a crime.<br />
Elder abuse presents in many different<br />
forms:<br />
Physical abuse – hitting, kicking,<br />
punching whether or not these actions<br />
cause serious or permanent injury.<br />
Psychological abuse – belittling,<br />
intimidation, humiliation and verbal<br />
abuse with the intent <strong>of</strong> causing<br />
emotional pain (Gray-Vickrey, 2004).<br />
Financial abuse – where the older<br />
person’s assets are misappropriated<br />
through theft, fraud, forceful changing<br />
<strong>of</strong> documents such as land title deeds<br />
and wills and unlawfully accessing the<br />
older person’s income entitlements<br />
(Lewis, 2004).<br />
Sexual abuse – this includes any kind<br />
<strong>of</strong> non-consensual sexual activity.<br />
Neglect – intentional or unintentional<br />
acts where the care provider fails to<br />
meet the elder’s needs such as<br />
withholding food, medicine, access<br />
to health care, hygiene, and the like.<br />
Self neglect – where the older<br />
person places their own health and<br />
safety at risk due to their own<br />
behaviour when they are unable to<br />
provide adequate food and clothing for<br />
themselves, medical care, access aids<br />
such as glasses, hearing aids, dentures<br />
and mobility aids (Pearsall, 2005).<br />
Institutional abuse – less<br />
acknowledged as a ‘type or form’ <strong>of</strong><br />
abuse, institutional abuse is evident<br />
when any <strong>of</strong> the previous behaviours<br />
are exhibited against an elderly resident<br />
by staff.<br />
Even though the Commonwealth<br />
Government introduced compulsory<br />
reporting <strong>of</strong> elder abuse through<br />
amending the Aged Care Act 1997<br />
(Cth) in 2007, many older people<br />
remain unprotected. There are several<br />
reasons for this. In the first place the<br />
only type <strong>of</strong> abuse that must be<br />
reported is excessive use <strong>of</strong> force and<br />
sexual assault; hence there is no legal<br />
compulsion to report any <strong>of</strong> the other<br />
forms <strong>of</strong> abuse listed above. Secondly,<br />
the scope <strong>of</strong> the law is limited as it only<br />
compels employees <strong>of</strong> Commonwealth<br />
approved residential care facilities and<br />
subsidised in-home care services to<br />
report a suspicion <strong>of</strong> or witnessed<br />
abuse <strong>of</strong> residents. As the majority<br />
<strong>of</strong> older people (approx 92%)<br />
(Productivity Commission, 2011) do<br />
not live in these environments they<br />
remain outside <strong>of</strong> the protection <strong>of</strong> the<br />
Aged Care Act and dependent on<br />
‘good Samaritans’ to report any abuse<br />
to organisations such as Aged Rights<br />
Advocacy Services and the Health<br />
Care Complaints Commission.<br />
Nonetheless, all those involved in the<br />
care <strong>of</strong> the older person have both a<br />
legal and an ethical obligation that is<br />
inextricably entwined within our role<br />
File photo<br />
to act according to the demands set<br />
down by our pr<strong>of</strong>ession. Ethically there<br />
is an obligation to ‘do no harm’ and in<br />
law this is translated into a ‘duty <strong>of</strong> care<br />
to avoid causing harm and to act<br />
reasonably’ (Donoghue v. Stevenson).<br />
Furthermore there is a non–delegable<br />
duty <strong>of</strong> care, which is a duty <strong>of</strong> care<br />
owed for example, by a hospital to its<br />
patients and by a nursing home to its<br />
residents and also to their staff (Ellis v.<br />
Wallsend District Hospital).<br />
Hence, it is arguable that a health<br />
practitioner who has an older person<br />
as a client, would not only have a moral<br />
and ethical duty but also a legal duty <strong>of</strong><br />
care to ensure the safety <strong>of</strong> their client<br />
and to act if they witness or suspect<br />
that the person is being abused or<br />
neglected and at risk <strong>of</strong> suffering<br />
foreseeable harm. The appropriate<br />
action to take would be what could<br />
reasonably be expected <strong>of</strong> the health<br />
practitioner, according to their level <strong>of</strong><br />
skill and expertise in the circumstances<br />
<strong>of</strong> the matter. It is here that health<br />
pr<strong>of</strong>essionals need to be familiar with<br />
expected standards <strong>of</strong> care and policy<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
21<br />
guidelines <strong>of</strong> their organisation and to<br />
follow these closely when the need<br />
arises.<br />
Notwithstanding the legal obligations<br />
to report abuse and the paucity <strong>of</strong><br />
these cases going to court, there is also<br />
an alarming deficit in the number <strong>of</strong><br />
actions initiated by the older person<br />
(or someone acting on their behalf)<br />
in claims <strong>of</strong> civil negligence, breach <strong>of</strong><br />
contract or fiduciary duty or trespass<br />
when they have suffered some form<br />
<strong>of</strong> abuse. Why this is so is open to<br />
speculation. Nonetheless, there is a<br />
developing body <strong>of</strong> case law in the<br />
United States <strong>of</strong> America, where courts<br />
have found the institution liable for<br />
abuse residents have suffered ‘on their<br />
watch’ regardless <strong>of</strong> any actual<br />
knowledge <strong>of</strong> it. This was the case in<br />
Caretenders, Inc v. Commonwealth where<br />
the corporate defendant was found<br />
liable for the abuse <strong>of</strong> an elderly<br />
resident who suffered from multiple<br />
extensive pressure sores whilst in their<br />
care, and also in State v. Boone<br />
Retirement Ctr., where a court found<br />
that the defendant corporation<br />
knowingly tolerated the <strong>of</strong>fending<br />
conduct <strong>of</strong> elder abuse and held that it<br />
could be held criminally responsible for<br />
this (Morgan & Scott, 2003).<br />
Therefore, it would seem prudent for<br />
employers under their non-delegable<br />
duty <strong>of</strong> care to recognise their legal<br />
obligation and ensure that their staff<br />
are aware <strong>of</strong> the expected standard <strong>of</strong><br />
care in elder abuse cases, and provide<br />
the appropriate policy and support for<br />
staff to report any suspicion or<br />
knowledge <strong>of</strong> abuse or neglect <strong>of</strong> their<br />
clients whether or not they are<br />
mandated to do so. This would be a<br />
step forward in the mission to protect<br />
all older people from abuse regardless<br />
<strong>of</strong> where they reside.<br />
References<br />
Aged Care Act 1997 (Cth) (Austl.).<br />
Donoghue v. Stevenson 1932 AC 562<br />
Ellis v. Wallsend District Hospital 1989 17<br />
NSWLR 553<br />
Gray-Vickrey, P., (2004). Combating Elder<br />
Abuse. <strong>Nursing</strong>, 34(10), 47.<br />
Lewis, R., (2004). Elder Law in <strong>Australia</strong>.<br />
<strong>Australia</strong>: Lexis Nexis Butterworths.<br />
Morgan, S., & Scott, J., (2003). Prosecution <strong>of</strong><br />
Elder Abuse, Neglect & Exploitation: Criminal<br />
Liability, Due Process, and Hearsay. American<br />
Prosecutors Research Institute Special Topics<br />
Series, Protecting America’s senior citizens,1-57.<br />
Pearsall, C., (2005). Forensic Biomarkers <strong>of</strong><br />
Elder Abuse: What Clinicians Need to Know.<br />
Journal <strong>of</strong> Forensic <strong>Nursing</strong>, 1(4),182-186.<br />
Productivity Commission, (2011). Caring for<br />
Older <strong>Australia</strong>ns: Draft Inquiry Report. Canberra.<br />
World Health Organisation [WHO], (2008). A<br />
Global Response to Elder Abuse and Neglect:<br />
Building Primary Health Care Capacity to deal<br />
with the Problem World Wide: Main Report.<br />
Geneva, Switzerland.<br />
Join one <strong>of</strong> RCNA’s faculties...<br />
Community and Primary Health Care Faculty<br />
Health and Wellbeing in Ageing Faculty<br />
Collaboration, integration and reform<br />
Movement Disorders and Parkinson’s Nurses Faculty<br />
New Generation <strong>of</strong> Nurses Faculty<br />
Rural <strong>Nursing</strong> and Midwifery Faculty<br />
Voice, views and values<br />
RCNA<br />
freecall 1800 061 660<br />
canberra@rcna.org.au<br />
www.rcna.org.au<br />
<strong>Australia</strong>’s peak pr<strong>of</strong>essional nursing organisation<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN
22<br />
ACUTE CARE NAtioNAL NETWORK<br />
Editor: Position vacant<br />
Sub-editor: Position vacant<br />
Nurse educators in acute care:<br />
Envisioning renewal<br />
By Jan Sayers MRCNA, Lecturer, UWS and PhD Candidate, Curtin University and Michelle<br />
DiGiacomo , Post doctoral fellow, University <strong>of</strong> Technology Sydney and Curtin University and<br />
Patricia M. Davidson FRCNA, Pr<strong>of</strong>essor <strong>of</strong> Cardiovascular and Chronic Care, University <strong>of</strong><br />
Technology Sydney and Curtin University<br />
Jan Sayers<br />
Introduction<br />
<strong>Australia</strong>’s health workforce is<br />
responsible for patient safety and<br />
quality. <strong>Nursing</strong> practice is underpinned<br />
by nurses’ clinical, pr<strong>of</strong>essional and<br />
organisational learning throughout their<br />
career. As societal demands have<br />
changed, nurse education has moved<br />
from the hospital setting to colleges<br />
and universities. In tandem with these<br />
changes, the nurse educator role in the<br />
hospital environment has also changed.<br />
<strong>Nursing</strong> literature frequently refers to<br />
nursing faculty, their role and workforce<br />
issues. However the literature is<br />
relatively devoid <strong>of</strong> discussion regarding<br />
the pivotal role <strong>of</strong> the nurse educator<br />
in hospitals in <strong>Australia</strong>.<br />
Study and findings<br />
This article reports on the Nurse<br />
Educators in Acute Care Hospitals<br />
(NEACH) study that identified the<br />
characteristics and role <strong>of</strong> the nurse<br />
educator workforce in <strong>Australia</strong> (Sayers<br />
& Davidson, 2009). A recent national<br />
survey <strong>of</strong> nurse educators across<br />
<strong>Australia</strong> was undertaken to describe<br />
the demographics and dimensions <strong>of</strong><br />
the role. Factors examined included<br />
role criteria and enactment,<br />
performance standards, appraisal and<br />
career intentions, workplace issues and<br />
the practice environment. A diverse<br />
group <strong>of</strong> 425 nurse educators<br />
completed the survey with<br />
representation from all states and<br />
territories. The majority were female<br />
(88%). All respondents reported role<br />
blurring and overlap <strong>of</strong> activities<br />
performed by nurse educators and<br />
other nursing roles. Although 81% held<br />
a specialty clinical qualification few held<br />
a Masters degree (22%). 65% had a<br />
performance review in the preceding<br />
12 months and 62% had their learning<br />
needs identified.<br />
Discussion<br />
This study has demonstrated role<br />
blurring and overlap between the<br />
nurse educator role and other nursing<br />
roles with responsibility for education.<br />
Where there is role ambiguity, role<br />
conflict may also arise, adversely<br />
influencing pr<strong>of</strong>essional identity, job<br />
satisfaction and performance (Dubois<br />
& Singh, 2009). This is an important<br />
issue as the role may be ‘at risk’ when<br />
it is not clearly defined, performance<br />
outcomes are not measured and<br />
importantly where nursing roles not<br />
directly providing clinical care are<br />
increasingly scrutinized (Conway &<br />
Elwin, 2007; Sayers & DiGiacomo,<br />
2010). Engagement in research and<br />
policy debate is essential for nurse<br />
educators to influence decision-making<br />
regarding their role in education in<br />
practice settings (Sayers & DiGiacomo,<br />
2010).<br />
Nurse educators need to provide role<br />
clarification by redefining and<br />
redesigning their role to address role<br />
blurring and ambiguity. An important<br />
part <strong>of</strong> this process is the development<br />
and application <strong>of</strong> frameworks for<br />
career role design, embracing group<br />
engagement by service users, nurses,<br />
service managers, education providers<br />
and researchers to achieve clientfocused<br />
services (Lockhart, 2004). Role<br />
clarity and validation <strong>of</strong> performance is<br />
crucial to role enactment, effectiveness<br />
and workforce engagement (Dubois &<br />
Singh, 2009).<br />
Consideration <strong>of</strong> the qualifications and<br />
pr<strong>of</strong>essional development essentials<br />
supporting the role is another<br />
imperative as is the development <strong>of</strong><br />
curricula reflecting role requirements.<br />
A grounding in teaching and learning<br />
theories, frameworks and processes in<br />
clinical practice are necessary<br />
foundations for nurse educators<br />
(Billings & Halstead, 2005). Learning<br />
about management and partnership<br />
concepts that underpin clinical learning<br />
environments are required<br />
(Henderson, Briggs, Schoonbeek, &<br />
Paterson, 2011). Leadership capabilities<br />
to support reconfiguration <strong>of</strong> practices<br />
and processes inspiring practice<br />
development and acquisition <strong>of</strong> new<br />
knowledge are also vital (Cook &<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
23<br />
Leathard, 2004). Nurse educators who<br />
model and foster expert behaviors will<br />
be transformational clinical leaders<br />
(Benner, Stutphen, Leonard, & Day,<br />
2010). The impact <strong>of</strong> these<br />
characteristics on learning is influential<br />
on student and graduate nurses’<br />
attitudes, behaviors and practices and<br />
their importance cannot be<br />
underestimated (Brammer 2006;<br />
Dickson, Walker, & Bourgouis, 2006;<br />
Eaton, Henderson, & Winch 2007).<br />
Leadership is an essential nurse<br />
educator attribute for creating and<br />
sustaining vibrant learning<br />
environments that build nursing<br />
excellence, workforce capacity and<br />
positively influence patient outcomes<br />
(Henderson, et al., 2011).<br />
Conclusion<br />
Engagement in policy and practice<br />
debate to define and redesign the<br />
nurse educator role and address<br />
blurring and ambiguity is a strategic<br />
imperative. Role development,<br />
underpinned by pr<strong>of</strong>essional education<br />
and development may enhance<br />
specialty recruitment and career<br />
opportunities. Performance review and<br />
articulation <strong>of</strong> performance outcomes<br />
acknowledges the contribution <strong>of</strong><br />
nurse educators to clinical practice and<br />
may enhance their performance as<br />
clinical leaders in education and drivers<br />
<strong>of</strong> policy and practice initiatives. The<br />
development <strong>of</strong> career pathways and<br />
qualifications to enhance continued<br />
recruitment to the specialty is a<br />
requirement for pr<strong>of</strong>essional credibility<br />
and career advancement.<br />
References<br />
Benner, P., Sutphen, M., Leonard, V., & Day, L.<br />
(2010). Educating nurses: A Call for Radical<br />
Transformation. San Francisco: Jossey-Bass.<br />
Billings, D. M. & Halstead, J. A. (2005). Teaching<br />
in <strong>Nursing</strong>. St. Louis: Elsevier Saunders.<br />
Brammer, J. (2006). A phenomenographic study<br />
<strong>of</strong> registered nurses’ understanding <strong>of</strong> their<br />
role in student learning - An <strong>Australia</strong>n<br />
perspective. International Journal <strong>of</strong> <strong>Nursing</strong><br />
Studies, 43, 963-973.<br />
Conway, J. & Elwin, C. (2007). Mistaken,<br />
misshapen and mythical images <strong>of</strong> nurse<br />
education: Creating a shared identity for clinical<br />
nurse educator practice. Nurse Education in<br />
Practice, 7, 187-194.<br />
Cook, M. J. & Leathard, H. L. (2004). Learning<br />
for clinical leadership. Journal <strong>of</strong> <strong>Nursing</strong><br />
Management, 12, 436-444.<br />
Dickson, C., Walker, J., & Bourgouis, S. (2006).<br />
Facilitating undergraduate nurses clinical<br />
practicum: the lived experience <strong>of</strong> clinical<br />
facilitators. Nurse Education Today, 26(5),<br />
416-422.<br />
Dubois, C. A. & Singh, D. (2009). From staff-mix<br />
to skill-mix and beyond: towards a systemic<br />
approach to health workforce management.<br />
Human Resources for Health, 7(87), 1-55.<br />
Eaton, E., Henderson, A., & Winch, S. (2007).<br />
Enhancing nurses’ capacity to facilitate learning<br />
in nursing students; effective dissemination and<br />
uptake <strong>of</strong> bets practice guidelines. International<br />
Journal <strong>of</strong> <strong>Nursing</strong> Practice, 15(3), 316-320.<br />
Henderson, A., Briggs, J., Schoonbeek, S., &<br />
Paterson, K. (2011). A framework to develop a<br />
clinical learning culture in heath facilities: ideas<br />
from the literature. International <strong>Nursing</strong> Review<br />
(early view). doi:<br />
10.1111/j.1466-7657.2010.00858.x<br />
Lockhart, K. (2004). Presenting a framework<br />
for developing nursing roles in Scotland. Journal<br />
<strong>of</strong> Research in <strong>Nursing</strong>, 10(1), 7-25.<br />
Sayers, J. M. & Davidson, P. M. (2009). Under<br />
the spotlight: nurse educators in acute care.<br />
Connections, 12(1), 35.<br />
Sayers, J. M. & DiGiacomo, M. (2010). The nurse<br />
educator role in <strong>Australia</strong>n Hospitals:<br />
implications for health policy. Collegian, 17,<br />
77-84.<br />
Acknowledge the pr<strong>of</strong>essionalism <strong>of</strong> your staff<br />
Demonstrates you as a workplace <strong>of</strong> choice<br />
Increase access to networking opportunities<br />
Join RCNA as a corporate partner<br />
and become part <strong>of</strong> nursing’s future!<br />
RCNA<br />
freecall 1800 061 660<br />
membership@rcna.org.au<br />
www.rcna.org.au<br />
<strong>Australia</strong>’s peak pr<strong>of</strong>essional nursing organisation<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
24<br />
BREAST CARE NAtioNAL NETWORK<br />
Editor: Elisabeth Coyne MRCNA<br />
Sub-editor: Position vacant<br />
Mastitis: How to diagnose and treat<br />
By Danielle Gleeson, Midwifery Lecturer, Griffith University<br />
©iStockphoto<br />
Mastitis is a condition estimated to affect between 3% and 33%<br />
<strong>of</strong> breastfeeding women (World Health Organization [WHO],<br />
2000), while a recent <strong>Australia</strong>n study found an incidence <strong>of</strong> 17%<br />
(Amir, Forster, Lumley & McLachlan, 2007).<br />
It is a condition<br />
which can have a<br />
significant negative<br />
impact on<br />
women’s<br />
experiences <strong>of</strong><br />
Danielle Gleeson<br />
breastfeeding<br />
(Amir & Lumley, 2006) and is <strong>of</strong>ten<br />
associated with early breastfeeding<br />
cessation (Crepinsek, Crow, Michener<br />
& Smart, 2010; Lewallen et al., 2006;<br />
Scott, Robertson, Fitzpatrick, Knight &<br />
Mullholland, 2008).<br />
To minimise the pain and distress<br />
encountered by women with mastitis,<br />
it is important for health pr<strong>of</strong>essionals<br />
working with breastfeeding women to<br />
have a thorough understanding <strong>of</strong> this<br />
condition and the associated treatment<br />
options.<br />
Definition and predisposing factors<br />
The literal meaning <strong>of</strong> mastitis is<br />
inflammation <strong>of</strong> the breast which may<br />
or may not be associated with infection<br />
<strong>of</strong> the breast tissue (Jahanfar, Ng &<br />
Teng, 2009). If not treated early, mastitis<br />
seems to follow a continuum from<br />
engorgement to inflammation to<br />
infection and finally to abscess<br />
(Crepinsek, et al., 2010; Academy <strong>of</strong><br />
Breastfeeding Medicine [ABM], 2008).<br />
Staphylococcus aureus, is the most<br />
common cause <strong>of</strong> infective mastitis<br />
(Kvist, Larsson, Hall-Lord, Steen &<br />
Shalén, 2008). The majority <strong>of</strong><br />
predisposing factors for mastitis such as<br />
infrequent feedings, incorrect<br />
attachment, rapid weaning and a<br />
blocked duct, relate to milk stasis.<br />
Other factors include damaged nipples,<br />
maternal illness and Candida infection<br />
(ABM, 2008).<br />
Symptoms and diagnosis<br />
The clinical symptoms <strong>of</strong> mastitis can<br />
mimic other conditions such as flu-like<br />
illnesses. Confirmation <strong>of</strong> mastitis can<br />
normally be made through associated<br />
breast symptoms which <strong>of</strong>ten occur in<br />
a wedge shape (ABM, 2008). The most<br />
common symptoms are:<br />
• breast erythema<br />
• breast tension<br />
• fever (>38.5°C)<br />
• breast pain<br />
• breast lumps<br />
• muscular aches (ABM, 2008)<br />
Due to the ease <strong>of</strong> identifying the<br />
above symptoms, it is uncommon for<br />
laboratory investigations, such as<br />
breastmilk culture, to be carried out.<br />
Kvist et al. (2008) found that bacterial<br />
counts in breastmilk cultures were <strong>of</strong><br />
little value in determining appropriate<br />
treatments. Diagnosis should specify<br />
whether an infection or abscess is<br />
thought to be present as this will<br />
effect treatment requirements.<br />
Treatment<br />
Treatment for mastitis can be divided<br />
into three categories: supportive, breast<br />
care and pharmacological. Supportive<br />
measures include general measures to<br />
improve the mother’s wellbeing such<br />
as adequate rest, fluids and nutrition<br />
(Jahanfar et al., 2009).<br />
Regular breast emptying through<br />
continued breastfeeding or expressing<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
RCNA’s Life Long Learning Program<br />
fr eca l 18 0 2 3 705<br />
3lp@rcna.org.au<br />
w.rcna.org.au<br />
<strong>Australia</strong>’s peak pr<strong>of</strong>e sional nursing organisation<br />
For more information:<br />
Visi the 3LP website<br />
www.3lp.rcna.org.au<br />
or call 18 0 2 3 705.<br />
If you are not an RCNA<br />
member, pleas email<br />
us at 3LP@rcna.org.au<br />
to set up a fr e triaL.<br />
<strong>Royal</strong> Co lege <strong>of</strong> <strong>Nursing</strong>, <strong>Australia</strong> | Volume 13 | I sue 2 | June 2010<br />
<strong>Nursing</strong> and<br />
Health Expos<br />
Canbe ra, ACT<br />
Sunday 6 March 20 1<br />
National Convention Centre<br />
Sydney, NSW<br />
Sunday 27 March 20 1<br />
Sydney Convention & Exhibition Centre<br />
Brisbane, QLD<br />
Sunday 10 April 20 1<br />
Brisbane Convention & Exhibition Centre<br />
Melbourne, VIC<br />
Sunday 15 May 20 1<br />
<strong>Royal</strong> Exhibition Building<br />
Adelaide, SA<br />
Sunday 5 June 20 1<br />
Adelaide Convention Centre<br />
For more information contact RCNA Events:<br />
NuRsiNg iN the outbACk – page 14<br />
fr eca l 18 061 60<br />
events@rcna.org.au<br />
w.rcna.org.au<br />
An event <strong>of</strong> RCNA, <strong>Australia</strong>’s peak pr<strong>of</strong>e sional nursing organisation<br />
Perth, WA<br />
Sunday 26 June 20 1<br />
Perth Convention & Exhibition Centre<br />
Hobart, TAS<br />
Sunday 10 July 20 1<br />
Hotel Grand Chance lor<br />
As the only expo in <strong>Australia</strong> to pr<strong>of</strong>ile a l<br />
nursing options under the one r <strong>of</strong>, RCNA’s<br />
<strong>Nursing</strong> and Health Expo provides direct<br />
a ce s to leading universities, hospitals<br />
and specialty nursing groups.<br />
The RCNA <strong>Nursing</strong> and Health Expo is a<br />
must for anyone interested in the nursing<br />
pr<strong>of</strong>e sion.<br />
RCN <strong>Australia</strong>n<br />
member <strong>of</strong> ICN<br />
<strong>Royal</strong> Co lege <strong>of</strong> <strong>Nursing</strong>, <strong>Australia</strong> | Volume 14 | I sue 1 | March 20 1<br />
ageing in the northern territory<br />
25<br />
aims to reduce milk stasis and<br />
according to WHO (2000) is the<br />
mainstay <strong>of</strong> mastitis treatment. Sudden<br />
weaning during an acute bout <strong>of</strong><br />
mastitis is likely to exacerbate<br />
symptoms and increase the risk <strong>of</strong><br />
abscess formation (ABM, 2008). It is<br />
important for health pr<strong>of</strong>essionals to<br />
inform the woman that continued<br />
breastfeeding is not only safe but will<br />
assist in her recovery from mastitis.<br />
Heat packs to the breast are<br />
recommended prior to feeds to<br />
assist in milk flow and cold packs are<br />
recommended after feeds for the<br />
reduction <strong>of</strong> pain and oedema (ABM,<br />
2008; Crepinsek et al., 2010). Support<br />
should be provided to women who<br />
have nipple damage, nipple pain or are<br />
having difficulties latching their baby to<br />
the breast (Jahanfar, et al., 2010).<br />
Compromised nipple integrity can<br />
allow an easy entry point for infection,<br />
thus correct attachment will minimise<br />
the risk for further episodes <strong>of</strong> mastitis.<br />
Pharmacological treatment includes<br />
pain relief and antibiotic therapy. The<br />
Academy <strong>of</strong> Breastfeeding Medicine<br />
(ABM, 2008) recommends an antiinflammatory<br />
drug such as ibupr<strong>of</strong>en<br />
as it is more likely to target the many<br />
symptoms related to inflammation than<br />
other simple analgesics such as<br />
paracetamol. Ibupr<strong>of</strong>en, given at<br />
recommended dosages, is not<br />
detectable in breastmilk and is thus<br />
compatible with breastfeeding (ABM,<br />
2008).<br />
Antibiotics are regularly prescribed for<br />
women presenting with infective<br />
mastitis or mastitis associated with a<br />
fever. Kvist et al. (2008) suggests that<br />
studies show between 77% and 97%<br />
<strong>of</strong> women are treated for mastitis with<br />
antibiotics. The preferred antibiotics are<br />
those that are effective against<br />
Staphylococcus aureus. Such antibiotics<br />
are penicillinase-resistant penicillins and<br />
Cephalexin or Clindamycin may be<br />
used for women with penicillin allergy<br />
(ABM, 2008). It is important to note<br />
that a 2009 Cochrane review (Jahanfar<br />
As a nurse,<br />
et al., 2009) suggested that the<br />
effectiveness <strong>of</strong> antibiotic therapy<br />
for the treatment <strong>of</strong> mastitis in<br />
breastfeeding women was still in<br />
question with further research<br />
recommended.<br />
Mastitis will effect up to a third <strong>of</strong> all<br />
breastfeeding women so it is important<br />
for health care pr<strong>of</strong>essionals to be<br />
familiar with the symptoms and<br />
evidence-based treatments for this<br />
condition. Providing supportive and<br />
pharmacological care and encouraging<br />
and assisting women with breast care<br />
will hopefully ensure women continue<br />
to breastfeed successfully beyond their<br />
recovery.<br />
References<br />
Academy <strong>of</strong> Breastfeeding Medicine. (2008).<br />
ABM Clinical Protocol: Mastitis (Revision).<br />
Breastfeeding Medicine, 3(3), 177-180.<br />
Amir, L. & Lumley, J. (2006). Women’s<br />
experience <strong>of</strong> lactational mastitis – ‘I have<br />
never felt worse’. <strong>Australia</strong>n Family Physician,<br />
35(9), 745-747.<br />
Amir, L., Forster, D., Lumley, J., & McLachlan, H.<br />
(2007). A descriptive study <strong>of</strong> mastitis in<br />
<strong>Australia</strong>n breastfeeding women: incidence and<br />
determinants. BMC Public Health, 7, 62.<br />
are you ready for the continuing pr<strong>of</strong>essional<br />
development (CPD) requirements under<br />
national registration<br />
RCNA’s Life Long Learning Program, 3LP, has a new<br />
look and easy navigation to a sist you with developing<br />
your learning plan, acce sing online learning activities,<br />
recording your CPD hours and much more.<br />
RCNA<br />
RCNAratecard<br />
advertise today and reach over 14 000<br />
rcna members and pr<strong>of</strong>essional partners.<br />
advertising rates and specifications for 2011<br />
<strong>CONNECTIONS</strong><br />
Nurturing the<br />
new generation<br />
<strong>of</strong> nurses<br />
New Generation <strong>of</strong> Nurses Faculty<br />
Mentoring nurse practitioners<br />
Adolescent sexual health<br />
Paediatric pa liative care<br />
<strong>CONNECTIONS</strong><br />
<strong>Royal</strong> Co lege <strong>of</strong> <strong>Nursing</strong>, <strong>Australia</strong> | Volume 13 | I sue 3 | September 2010<br />
Celebrating<br />
International<br />
Year <strong>of</strong> the Nurse<br />
Recognising excellence in nursing<br />
Celebrating nurse-led services<br />
Commemorating our service nurses<br />
<strong>Nursing</strong> beyond the bedside<br />
<strong>CONNECTIONS</strong><br />
<strong>Royal</strong> Co lege <strong>of</strong> <strong>Nursing</strong>, <strong>Australia</strong> | Volume 13 | I sue 4 | December 2010<br />
RCNA 11<br />
RCNA thANks the<br />
goveRNoR-geNeRAl – page 13<br />
Visit the RCNA <strong>Nursing</strong> and Health Expo<br />
and find out where your career in nursing can take you<br />
RCNA lAuNChes New movemeNt disoRdeRs fACulty – page 13<br />
the sileNt issue iN the Asylum seekeR debAte – page 4<br />
goiNg the extRA miles foR heAlth pRomotioN – page 42<br />
RCNA<br />
<strong>Australia</strong>’s peak pr<strong>of</strong>essional<br />
nursing organisation<br />
<strong>CONNECTIONS</strong><br />
From the city<br />
to the country<br />
stories from our nursing students<br />
RCNA<br />
From reFug e to nursing student<br />
Breaking the silence on sti lBirth<br />
Crepinsek, M.A., Crowe, L., Michener, K., &<br />
Smart, N.A. (2010). Interventions for<br />
preventing mastitis after childbirth (Cochrane<br />
Review). The Cochrane Library. In Cochrane<br />
Database <strong>of</strong> Systematic Reviews, 2010 (1).<br />
Retrieved February 24, 2010, from http://<br />
onlinelibrary.wiley.com/o/cochrane/clsysrev/<br />
articles/CD007239/frame.html<br />
Jahanfar, S., Ng, C., & Teng, C. (2009). Antibiotics<br />
for mastitis in breastfeeding women (Cochrane<br />
Review). In Cochrane Database <strong>of</strong> Systematic<br />
Reviews 2009 (1), Retrieved February 24, 2010,<br />
from http://onlinelibrary.wiley.com/o/cochrane/<br />
clsysrev/articles/CD005458/frame.html<br />
Kvist, L., Larsson, B., Hall-Lord, M., Steen, A. &<br />
Shalén, C. (2008). The role <strong>of</strong> bacteria in<br />
lactational mastitis and some considerations <strong>of</strong><br />
the use <strong>of</strong> antibiotic treatment. International<br />
Breastfeeding Journal, 3, 6.<br />
Lewallen, L., Dick, M., Flowers, J., Powell, W.,<br />
Zickefoose, K., Wall, Y., et al. (2006).<br />
Breastfeeding Support and Early Cessation.<br />
Journal <strong>of</strong> Obstetric, Gynecologic, & Neonatal<br />
<strong>Nursing</strong>, 35(2), 166-172.<br />
Scott, J., Robertson, M., Fitzpatrick, J., Knight, C.<br />
& Mulholland, S. (2008). Occurrence <strong>of</strong><br />
lactational mastitis and medical management: A<br />
prospective cohort study in Glasgow.<br />
International Breastfeeding Journal, 3, 21.<br />
World Health Organization [WHO] (2000).<br />
Mastitis: Causes and Management. Available<br />
from http://whqlibdoc.who.int/hq/2000/<br />
WHO_FCH_CAH_00.13.pdf<br />
New<br />
RCNAratecard<br />
available<br />
now!<br />
For more info:<br />
rcna.org.au/<br />
advertising<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
26<br />
ETHICS NAtioNAL NETWORK<br />
Editor: Dr Evdokia Kalaitzidis MRCNA<br />
Sub-editor: Position vacant<br />
<strong>Nursing</strong>, employers and the<br />
distribution <strong>of</strong> ethical responsibilities<br />
By Dr Evdokia Kalaitzidis MRCNA, Lecturer, Flinders University<br />
Dr Evdokia Kalaitzidis<br />
Most nurses, not surprisingly, are<br />
employed by hospitals (<strong>Australia</strong>n<br />
Bureau <strong>of</strong> Statistics, 2006). Individual<br />
nurses are responsible for looking after<br />
their patients. Hospital managers and<br />
administrators are responsible for<br />
keeping the hospitals running. The<br />
<strong>Australia</strong>n <strong>Nursing</strong> and Midwifery<br />
Council has the responsibility <strong>of</strong><br />
co-ordinating the development and<br />
maintenance <strong>of</strong> pr<strong>of</strong>essional standards<br />
and the code <strong>of</strong> ethics.<br />
When it comes to ethical decision<br />
making, it is useful for both parties to<br />
be clear about who is responsible for<br />
what. In this article I want to explore<br />
the proper distribution and allocation<br />
<strong>of</strong> ethical responsibilities between<br />
nurses and their employing institutions.<br />
The shift from hospital-based nurse<br />
education and training to the higher<br />
education sector represents a major<br />
evolutionary development <strong>of</strong> the<br />
nursing pr<strong>of</strong>ession. <strong>Nursing</strong> has become<br />
increasingly complex work. It requires<br />
nurses to apply sophisticated problem<br />
solving skills and other competencies to<br />
deal with complex problems associated<br />
with moment to moment client care.<br />
The nursing pr<strong>of</strong>ession as a whole<br />
does not control the management<br />
<strong>of</strong> hospitals, nor do individual nurses<br />
on the wards. An individual nurse’s<br />
responsibilities to their employer are<br />
also related to the pr<strong>of</strong>essional<br />
standards. Hospitals rely on the work <strong>of</strong><br />
pr<strong>of</strong>essional associations and affiliations<br />
to keep nurses accountable to the<br />
wider community. So to an employer,<br />
pre-existing pr<strong>of</strong>essional standards are<br />
important.<br />
Setting standards for nursing practice is<br />
a responsibility <strong>of</strong> the nursing pr<strong>of</strong>ession<br />
as a whole. As with any pr<strong>of</strong>ession,<br />
there are generic bodies <strong>of</strong> knowledge<br />
and application techniques universal for<br />
all members <strong>of</strong> the same pr<strong>of</strong>ession.<br />
These bodies <strong>of</strong> knowledge and<br />
application techniques are standards<br />
<strong>of</strong> pr<strong>of</strong>essional practice, and hence<br />
transferable from one workplace<br />
to another. In a nurse-employer<br />
relationship, the nurse has an overriding<br />
ethical obligation to practise according<br />
to the standards <strong>of</strong> the nursing<br />
pr<strong>of</strong>ession. These ‘institutionalised’<br />
standards <strong>of</strong> practice distinguish the<br />
type <strong>of</strong> work performed by nurses from<br />
other forms <strong>of</strong> work. Pr<strong>of</strong>essional<br />
standards are not open for negotiation<br />
between the nurse and the client, nor<br />
between the nurse and employer.<br />
Employment relations pose difficulties<br />
for nurses when employers expect<br />
them to provide a service that is<br />
beyond the boundaries <strong>of</strong> their<br />
pr<strong>of</strong>essional expertise.<br />
Hospitals supply the human and<br />
material resources necessary to provide<br />
medical and nursing care for sick and<br />
injured people in the community and<br />
are responsible for environmental<br />
impacts. They are largely responsible<br />
for the effective management and<br />
facilitation <strong>of</strong> services according to<br />
institutional interests. More importantly,<br />
each hospital establishes its own set <strong>of</strong><br />
routines and policies, and these vary<br />
considerably from one hospital to<br />
another.<br />
As such perhaps the hospitals should<br />
consider developing a code <strong>of</strong><br />
management practice to address<br />
concerns <strong>of</strong> privacy, information, policy<br />
development and relations with the<br />
community.<br />
Employment relations pose difficulties for nurses when<br />
employers expect them to provide a service that is<br />
beyond the boundaries <strong>of</strong> their pr<strong>of</strong>essional expertise.<br />
“<br />
”<br />
I call upon your insights and to invite<br />
member contributions to the Ethics<br />
National Network. If you wish to remain<br />
anonymous your name and identity will<br />
be withheld. Please contact me at<br />
evdokia.kalaitzidis@flinders.edu.au<br />
Reference<br />
<strong>Australia</strong>n Bureau <strong>of</strong> Statistics. (2006). 4102.0<br />
- <strong>Australia</strong>n Social Trends, 2005. Retrieved<br />
February 10, 2011 from www.abs.gov.au/<br />
Ausstats/abs@.nsf/0/8A87EF112B5BCF8BCA2<br />
5703B0080CCD9<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
Leading the way to local care<br />
RCNA<br />
Community and Primary 19–21 October<br />
11<br />
Health Care <strong>Nursing</strong> Conference Hobart<br />
CaLL for abstraCts now open<br />
To find out more and register go to www.rcna.org.au<br />
For more information contact RCNA Events:<br />
RCNA<br />
freecall 1800 061 660<br />
events@rcna.org.au<br />
www.rcna.org.au<br />
An event <strong>of</strong> RCNA, <strong>Australia</strong>’s peak pr<strong>of</strong>essional nursing organisation<br />
See you in Hobart!<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN
28<br />
HISTORY NAtioNAL NETWORK<br />
Editor: Sue DeVries FRCNA<br />
Sub-editor: Position vacant<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
29<br />
Nurses in WAR<br />
The <strong>Australia</strong>n War Memorial’s Nurses: from Zululand to Afghanistan<br />
exhibition opens in Canberra in December. This beautifully<br />
evocative display tells the story <strong>of</strong> nursing in overseas conflicts,<br />
an important but <strong>of</strong>ten neglected aspect <strong>of</strong> <strong>Australia</strong>’s wartime<br />
experience.<br />
It draws on the Memorial’s rich collection to highlight the work <strong>of</strong> <strong>Australia</strong>n nurses<br />
in war and focuses on the men and women who served as military nurses in<br />
overseas conflicts. With a strong focus on photographs and private records it traces<br />
the involvement <strong>of</strong> nurses from the first known <strong>Australia</strong>n contribution in the Zulu<br />
War <strong>of</strong> 1879 to today’s operations in Afghanistan.<br />
Most <strong>Australia</strong>ns are familiar with the stories <strong>of</strong> <strong>Australia</strong>n nurses in recent conflicts<br />
but the experiences <strong>of</strong> nurses in previous wars stand in danger <strong>of</strong> being forgotten.<br />
Nurses: from Zululand to Afghanistan will remind <strong>Australia</strong>ns how difficult it was for<br />
many women to serve in extremely primitive and dangerous conditions. Like other<br />
<strong>Australia</strong>n service personnel, many paid the ultimate price.<br />
Left page: London, England. c. 1917. 4TH London General Hospital. A nurse helps a soldier<br />
use a passive ankle exerciser, an item <strong>of</strong> medical equipment<br />
Top: Kent, England. Queen Mary (centre) escorted by an unidentified <strong>of</strong>ficer, Sister Edith<br />
Horton (far right) and another unidentified nurse visiting a patient with a heavily bandaged<br />
face at Sidcup Hospital in Kent. An <strong>Australia</strong>n facio-maxillary section was based at this<br />
hospital which was designed especially to treat soldiers with severe facial injuries (Donor H.<br />
Crompton)<br />
Top right: A nurse at Antwerp Hospital tending to a heavily bandaged Belgian patient whose<br />
face and arms have been severely wounded by shell splinters. Two other patients lie in beds<br />
beside him (Donor M. Wolfer)<br />
Bottom right:Victoria Barracks, Sydney, c. 1921. Lord Frederick William Forster (right), the<br />
Governor-General <strong>of</strong> <strong>Australia</strong>, presenting the Military Medal to Staff Nurse Pearl Corkhill at a<br />
medal investiture ceremony. Nurse Corkhill received the award for her courage and presence<br />
<strong>of</strong> mind when the British Army’s No. 38 Casualty Clearing Station, to which she was<br />
temporarily attached, was twice bombed by enemy aircraft in 1918–07. (Original print housed<br />
in P run in AWM Archive Store) (Donor G. Smith)<br />
Images courtesy <strong>of</strong> the <strong>Australia</strong>n War Memorial<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
30<br />
LEADERSHIP NAtioNAL NETWORK<br />
Editor: Julie Shepherd FRCNA<br />
Sub-editor: Lynne Slater MRCNA<br />
Utilising practice development concepts<br />
to establish an effective team<br />
By Elizabeth Newham MRCNA and Leigh Darcy, Members <strong>of</strong> the Hunter New England Essentials<br />
<strong>of</strong> Care Team<br />
In 2009 a team was established to develop and implement a cultural change program, the Essentials<br />
<strong>of</strong> Care (EOC) program, based on emancipatory practice development (ePD) principles. EOC is a<br />
framework for the evaluation <strong>of</strong> the essential care provided at the clinical ward and unit level.<br />
Clinical staff are engaged in the evaluation and development <strong>of</strong> the clinical care provided. The aims <strong>of</strong><br />
the project are to improve patient safety and outcomes and to enhance the experiences <strong>of</strong> patients,<br />
families and carers as well as staff involved in the delivery <strong>of</strong> care. (NSW Health, 2009)<br />
The first construct <strong>of</strong> this framework<br />
is having prerequisites that will enable<br />
person-centred outcomes to occur.<br />
Attributes such as pr<strong>of</strong>essional<br />
competence, well developed<br />
interpersonal skills, commitment to the<br />
job, clarity <strong>of</strong> beliefs and values and<br />
knowing self are integral to PCN<br />
(McCormack, et al., 2008, p. 195).<br />
Back Row L–R Maria Relf, Catherine Turner, Penny Cummings, Mary Downey, Di Targett and<br />
Elizabeth Newham; Front Row Kim Glash<strong>of</strong>f & Leigh Darcy<br />
The team itself had members situated<br />
in diverse geographical areas. The<br />
program was being implemented in<br />
what was the Hunter New England<br />
Area Health Service (now Local Health<br />
Network) which still covers a large<br />
geographical area <strong>of</strong> 130 000 square<br />
kilometres, with 45 inpatient health<br />
facilities providing care to<br />
approximately 840 000 people. Over<br />
the last 18 months the team has been<br />
able to utilise the practice development<br />
principles <strong>of</strong> the program to effectively<br />
establish and maintain the team in<br />
introducing and maintaining the<br />
Essentials <strong>of</strong> Care program.<br />
One <strong>of</strong> the underlying concepts <strong>of</strong><br />
ePD is the Person-Centred <strong>Nursing</strong><br />
(PCN) framework (McCormack et al,<br />
2008). This concept provides links<br />
between caring and personcenteredness<br />
with expected outcomes<br />
from an effective PCN including<br />
satisfaction and involvement <strong>of</strong> care,<br />
feelings <strong>of</strong> wellbeing and the creation<br />
<strong>of</strong> a therapeutic culture (McCormack<br />
et al., 2008, p. 194).<br />
During the planning <strong>of</strong> the roll-out <strong>of</strong><br />
the Essentials <strong>of</strong> Care program, it was<br />
established that the principles <strong>of</strong> ePD<br />
needed to be used not only with the<br />
nursing units engaging in the program,<br />
but also within the team that was being<br />
established to accomplish the work.<br />
The first challenge was to identify the<br />
necessary essential skills and attributes<br />
that would enable the new team<br />
members to be able to work effectively<br />
in a person-centred way within the<br />
team and with others, while working in<br />
geographical isolation. By applying the<br />
ePD framework to the establishment<br />
<strong>of</strong> the team, a group <strong>of</strong> prerequisites<br />
for interview were developed prior to<br />
the recruitment process. These<br />
prerequisites included problem-solving,<br />
knowledge <strong>of</strong> the Area Health Service,<br />
flexibility and self motivation.<br />
The second challenge was to create<br />
ways <strong>of</strong> working to ensure new staff<br />
inter-connected as a team and<br />
maintained a person-centred<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
31<br />
environment while <strong>of</strong>ten working in<br />
isolation; most members <strong>of</strong> the team<br />
were based in different regions <strong>of</strong> the<br />
vast geographical area.<br />
In the PCN framework, care<br />
environments that support effective<br />
person-centeredness include:<br />
appropriate skill mix, shared decision<br />
making, effective staff relationships,<br />
supportive organisational systems,<br />
power sharing and potential for<br />
innovation and risk taking (McCormack<br />
et al, p. 196). This framework was<br />
introduced to the establishment <strong>of</strong> the<br />
team and was adopted as an<br />
underpinning vision.<br />
It was essential to ensure that all team<br />
members were able to develop the<br />
skills needed to conduct the EOC<br />
program. This included developing a<br />
structured orientation program for<br />
participants involving course<br />
attendance, familiarisation <strong>of</strong> the<br />
program and workplaces and the time<br />
to deconstruct the various<br />
components <strong>of</strong> the work involved in<br />
the program. To facilitate the inclusion<br />
<strong>of</strong> all the team and group participation<br />
in decision-making, various ePD tools<br />
The first construct <strong>of</strong><br />
this framework is having<br />
prerequisites that will<br />
enable person-centred<br />
outcomes to occur.<br />
“<br />
”<br />
and strategies were used such as<br />
facilitated group discussions and<br />
teleconferences.<br />
The next step was for the EOC team<br />
to undertake a values clarification<br />
exercise. This exercise enabled team<br />
members to acknowledge each<br />
individual’s beliefs and values and to<br />
begin to develop a statement that<br />
outlined shared values. Some <strong>of</strong> the<br />
core bases in the team include<br />
role-modelling, sharing <strong>of</strong> skills and<br />
ideas, mentoring, co-facilitation and<br />
communication plans. The team has<br />
established a collaborative way <strong>of</strong><br />
working so that the power is shared by<br />
the group and an environment <strong>of</strong> high<br />
challenge and high support has been<br />
established which enables innovation<br />
and risk taking to occur. During this<br />
venture the ethos <strong>of</strong> utilising ePD<br />
principles and person-centredness as a<br />
way <strong>of</strong> working has been reinforced.<br />
As a result <strong>of</strong> utilising the concepts <strong>of</strong><br />
the PCN framework, the EOC team<br />
was able to rapidly establish effective<br />
ways <strong>of</strong> working. Team members<br />
continue to work both independently<br />
and collaboratively by supporting each<br />
other’s portfolios. This has facilitated<br />
learning from each other and the<br />
engagement with other nursing teams.<br />
One more part <strong>of</strong> maintaining an<br />
effective team and an essential principle<br />
<strong>of</strong> ePD is reflecting on our practice.<br />
Throughout the process, reflection has<br />
been vital and at present the team is<br />
conducting a formal evaluation to<br />
review if the functioning <strong>of</strong> the team<br />
reflects person-centredness.<br />
References<br />
McCormack, B., McCance, T., Slater, P.,<br />
McCormick, J., McArdle, C., & Dewing, J. (2008).<br />
Person-Centred Outcomes and Cultural<br />
Change. In K. Manley, B. McCormack & V.<br />
Wilson (Eds)., International Practice<br />
Development in <strong>Nursing</strong> and Healthcare<br />
(pp. 189-214). Oxford: Blackwell.<br />
NSW Department <strong>of</strong> Health (2009). Working<br />
with Essentials <strong>of</strong> Care: A resource guide for<br />
Facilitators. NSW Department <strong>of</strong> Health.<br />
all you need<br />
to know about<br />
nurSing!<br />
rCna nurSing & health expo<br />
<br />
held on SundayS from 10am–3pm<br />
Expo datEs:<br />
wa – 26 June<br />
Perth Convention Centre<br />
taS –10 July<br />
Hotel Grand Chancellor, Hobart<br />
RCNA<br />
freecall 1800 061 660<br />
events@rcna.org.au<br />
www.rcna.org.au<br />
An event <strong>of</strong> RCNA, <strong>Australia</strong>’s peak pr<strong>of</strong>essional nursing organisation<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
32<br />
LEGAL ISSUES NAtioNAL NETWORK<br />
Editor: Associate Pr<strong>of</strong>essor Linda Starr FRCNA<br />
Sub-editor: Position vacant<br />
Do we take the principle <strong>of</strong><br />
double effect for granted<br />
By Anne Milln MRCNA, Registered Nurse, Masters in Health and Medical Law Student<br />
Registered nurses (RNs) all over <strong>Australia</strong> will be familiar with<br />
giving a dose <strong>of</strong> morphine to a terminally ill patient, with the<br />
intent <strong>of</strong> alleviating the patient’s pain and distress. The morphine<br />
has been ordered by a doctor and a range <strong>of</strong> dosage has been<br />
given – let’s say 2.5-5mg, to be given subcutaneously, and the<br />
frequency is as necessary (prn). How <strong>of</strong>ten does the RN consider<br />
the possible other effect, that it might kill the patient<br />
Anne Milln<br />
That other effect is part <strong>of</strong> what is<br />
known as the principle <strong>of</strong> double effect.<br />
This is an ethical principle which<br />
suggests that for an action there are<br />
two possible outcomes – one desired<br />
and the other not desired, the good<br />
effect or the bad effect. The ethics <strong>of</strong><br />
giving that dose <strong>of</strong> morphine is a<br />
debate in itself.<br />
In some jurisdictions in <strong>Australia</strong>,<br />
health pr<strong>of</strong>essionals are protected<br />
by legislation. For instance in South<br />
<strong>Australia</strong> the legislation states that<br />
where the treatment or care <strong>of</strong> a<br />
patient is given with the intent <strong>of</strong><br />
relieving pain or distress, according to<br />
proper pr<strong>of</strong>essional standards, but<br />
hastens the death <strong>of</strong> the patient, the<br />
health pr<strong>of</strong>essional is protected from<br />
civil or criminal liability (Consent to<br />
Medical Treatment and Palliative Care Act<br />
1995 (SA)(Austl.)) This makes it very<br />
clear that the intent must be to relieve<br />
pain or distress. How do we prove that<br />
intent to make ourselves invulnerable<br />
to criminality<br />
A case in the UK occurred at the<br />
Airedale NHS Trust in Yorkshire<br />
England. Anne Grigg Booth was<br />
charged in 2004 with “3 <strong>of</strong>fences <strong>of</strong><br />
murder, one <strong>of</strong>fence <strong>of</strong> attempted<br />
murder and 13 <strong>of</strong>fences <strong>of</strong><br />
administering noxious substances with<br />
intent to cause grievous bodily harm<br />
or harm” (Thirlwall, Kinsella & Mullan,<br />
2010, pp. 3). Unfortunately Anne Grigg<br />
Booth committed suicide before her<br />
case came to court.<br />
The case has been vigorously<br />
examined in The Airedale Inquiry:<br />
Report to the Yorkshire and The<br />
Humber Strategic Health Authority<br />
(Thirlwall, Kinsella & Mullan, 2010),<br />
which was presented in June 2010, and<br />
it is this document which gives us the<br />
facts <strong>of</strong> the case.<br />
To look at all the charges would take<br />
more time and space than is available<br />
here, but one charge is particularly<br />
interesting in the context <strong>of</strong> the principle<br />
<strong>of</strong> double effect. The <strong>of</strong>fence is alleged<br />
to have occurred in November 2001.<br />
CX, a 75 year old woman with a long<br />
history <strong>of</strong> smoking, presented to the<br />
hospital with a possible diagnosis <strong>of</strong><br />
pneumonia; an X-ray suggested lung<br />
cancer. On admission to the ward she<br />
was found to have a cyanosed and<br />
discoloured arm and was taken<br />
immediately to theatre for a right<br />
brachial embolectomy under local<br />
anaesthetic. Post operatively she<br />
developed renal problems and was very<br />
hypotensive, despite fluid resuscitation.<br />
She was conscious and agitated so the<br />
medical staff ordered diamorphine<br />
1.25–2.5mg to be given IV prn (Thirlwall,<br />
Kinsella & Mullan, 2010, pp. 63). An initial<br />
dose was given and it was recorded in<br />
the notes that CX was ‘very settled after<br />
administering diamorphine’ (Thirlwall,<br />
Kinsella & Mullan, 2010, pp. 63). Further<br />
attempts were made at fluid<br />
resuscitation without effect. After<br />
discussion with the family it was decided<br />
not to attempt further active treatment<br />
and in effect that CX was to be kept<br />
comfortable. One and a half hours later,<br />
a further dose <strong>of</strong> diamorphine was<br />
given, and signed for appropriately by<br />
Booth and another RN, however there<br />
was no explanatory documentation to<br />
support why the diamorphine was given.<br />
Hence there is no way to determine<br />
whether CX was in distress at the time.<br />
The patient died about 30 minutes after<br />
the diamorphine was given.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
33<br />
In order for murder to be proved there must either be an intent to kill or<br />
extreme irresponsibility which leads to someone’s death.<br />
“<br />
”<br />
Witness statements are contradictory<br />
about whether the patient was<br />
distressed or not and the expert<br />
witnesses consulted by the police for<br />
the inquiry also contradict one another.<br />
Booth said that “she would not have<br />
given the diamorphine unless the<br />
patient was in pain or distress”<br />
(Thirlwall, Kinsella & Mullan, 2010, pp.<br />
65). Booth was charged with the<br />
murder <strong>of</strong> CX.<br />
What is at issue here is the intent <strong>of</strong><br />
Booth when she gave the second dose<br />
<strong>of</strong> diamorphine. In order for murder to<br />
be proved there must either be an<br />
intent to kill or extreme irresponsibility<br />
which leads to someone’s death. In the<br />
eyes <strong>of</strong> a court, the absence <strong>of</strong> proper<br />
documentation means that the intent is<br />
open to interpretation. If it hasn’t been<br />
documented it hasn’t been done<br />
(Staunton & Chiarella, 2008).<br />
Timely and objective documentation is<br />
the RNs’ greatest protection from such<br />
a charge <strong>of</strong> murder. It leaves no doubt<br />
about the intent to relieve pain or<br />
distress, rather than intent to hasten<br />
death or indeed to kill the patient. This<br />
is conjecture, but if Booth completed<br />
adequate documentation <strong>of</strong> her<br />
nursing care, she almost certainly<br />
would not have been charged with<br />
murder.<br />
References<br />
Consent to Medical Treatment and Palliative Care<br />
Act 1995 (SA) (Austl.).<br />
Staunton, P., & Chiarella, M. (2008). <strong>Nursing</strong> and<br />
the law (6th ed.). Marrickville, NSW: Elsevier.<br />
Thirlwall, K., Kinsella, E., & Mullan, A. (2010). The<br />
Airedale Inquiry: Report to the Yorkshire and The<br />
Humber Strategic Health Authority. Available from<br />
http://www.airedale-trust.nhs.uk/docs/<br />
Inquiry%20-%20full%20report.pdf.<br />
Online Computer Training Program<br />
Do you need help with your computer skills<br />
RCNA has a fantastic online learning program that can solve all your problems!<br />
The RCNA endorsed program is based on Micros<strong>of</strong>t Office<br />
2007 (including: Word; Excel; Access; Power Point and Outlook)<br />
and will greatly increase your general IT skills.<br />
This continuing pr<strong>of</strong>essional development opportunity is<br />
available to all health pr<strong>of</strong>essionals and support staff.<br />
The program is:<br />
• targeted for beginners and self-taught users <strong>of</strong> the<br />
computer<br />
• conveniently available online<br />
• able to be completed at work and/or home<br />
• available as a printable resource<br />
• available for a period <strong>of</strong> 12 months<br />
• supported by RCNA via phone and email<br />
• worth up to 79 RCNA Continuing Nurse Education<br />
points.<br />
Cost:<br />
$200 GST inclusive<br />
Registrations close:<br />
31 August 2011<br />
Registration form:<br />
email itprogram@rcna.org.au<br />
freecall 1800 061 660<br />
www.rcna.org.au/faculties/<br />
rural_faculty<br />
Note:<br />
Discounts available for organisational group bookings over 10.<br />
This program is not designed for Mac users.<br />
RCNA<br />
freecall 1800 061 660<br />
itprogram@rcna.org.au<br />
www.rcna.org.au<br />
<strong>Australia</strong>’s peak pr<strong>of</strong>essional nursing organisation<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN
34<br />
NURSES IN BUSINESS NAtioNAL NETWORK<br />
Editor: Dr Jane Truscott MRCNA<br />
Sub-editor: Position vacant<br />
Essentials<br />
for successful<br />
business<br />
planning<br />
By Dr Jane Truscott MRCNA,<br />
Senior Consultant, TEPL Consulting<br />
One <strong>of</strong> the most critical aspects <strong>of</strong> starting a business is effective<br />
planning. You may be thinking <strong>of</strong> providing services within the<br />
public or private sectors or for people living in the community.<br />
You may have found that product development and delivery to<br />
market is your niche. Whether you aim to provide a service or<br />
product, business success is highly contingent upon thoughtful<br />
and realistic planning (Johnson, 1990).<br />
A business plan, sometimes confused<br />
with a business case, is a plan for a<br />
start-up business. It is a formal<br />
statement that outlines all aspects <strong>of</strong><br />
the economic viability <strong>of</strong> your business.<br />
A business case is the justification for<br />
an initiative within an existing business,<br />
such as a new service, piece <strong>of</strong><br />
equipment or s<strong>of</strong>tware. While the<br />
development <strong>of</strong> a business case may be<br />
familiar to many nurses within <strong>Australia</strong>,<br />
Dr Jane Truscott<br />
few may have experience with the<br />
actual development <strong>of</strong> a business plan.<br />
Business plans vary depending on the<br />
type <strong>of</strong> service or product. The<br />
following elements are usually<br />
considered: executive summary,<br />
company description, market analysis,<br />
service or product description,<br />
marketing and competition, financials,<br />
key personnel and an appendices.<br />
Executive summary<br />
The executive summary is a critical<br />
aspect <strong>of</strong> your plan and probably the<br />
first thing the reader will access.<br />
However, it should be written last, after<br />
you have researched and developed<br />
other components <strong>of</strong> the plan. There’s<br />
a good chance the reader <strong>of</strong> your plan,<br />
possibly a potential investor (e.g banker,<br />
venture capitalist, or business angel),<br />
will not have much time to study your<br />
plan in detail. The executive summary<br />
should peak their interest and<br />
encourage them to read more (Mason<br />
& Stark, 2004). Typically one to two<br />
pages, it should include a mission<br />
statement, a description <strong>of</strong> the business,<br />
a description <strong>of</strong> your service or<br />
product, marketing, financial<br />
considerations and key personnel.<br />
Company description<br />
The company description should be<br />
fairly straight-forward, providing a vital<br />
description <strong>of</strong> what you do, why you<br />
do it, who you do it for and why you’ll<br />
be successful doing it. It should provide<br />
the vision and direction <strong>of</strong> the<br />
company. At a minimum, it should<br />
include: company name, mission<br />
statement, company objective and<br />
goals, service or product, target<br />
customer, ownership structure, current<br />
status and business history. You may<br />
also wish to include such topics as the<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
35<br />
strengths and skills <strong>of</strong> the business, legal<br />
form <strong>of</strong> ownership and business<br />
philosophy.<br />
Market analysis<br />
Consider who you want to reach and<br />
why. This is one area where many<br />
companies do not devote sufficient<br />
research, <strong>of</strong>ten contributing to<br />
avoidable failure. Identify and define<br />
your market; know what population<br />
and/or group <strong>of</strong> people would be<br />
interested in your service or product<br />
and develop a well-defined statement<br />
that is supported by evidence.<br />
Consider such questions as:<br />
• What is the size <strong>of</strong> your target<br />
market<br />
• How old are they<br />
• What gender are they<br />
• Where do they live<br />
• What is their family structure<br />
• What is their income<br />
• Are there cultural or ethnic<br />
considerations<br />
• How do they spend their spare<br />
time<br />
• What motivates them<br />
Service or product description<br />
Now that you have described your<br />
market, you want to provide a<br />
convincing argument; why is there a<br />
substantial need for your service or<br />
product A detailed service or product<br />
description should identify the specific<br />
benefits, your ability to meet the<br />
consumer’s needs and competitive<br />
advantages. Provide supporting<br />
evidence as to why your service or<br />
product is needed with numerical data<br />
and information supported by<br />
testimonials.<br />
Marketing plan<br />
The marketing plan will describe how<br />
you plan to get your service or product<br />
to your customer. Essentially, you will<br />
want to describe your sales strategy,<br />
pricing plan, proposed advertising and<br />
promotion activities and the benefits <strong>of</strong><br />
your service or product. Traditionally, a<br />
market plan would address the four ‘Ps’<br />
<strong>of</strong> marketing, that is: product, price,<br />
promotion and place. While this<br />
framework <strong>of</strong>ten forms the core <strong>of</strong><br />
many marketing plans, it has also been<br />
criticised as obsolete, and somewhat<br />
simplistic for the modern market place<br />
(Constantinides, 2006). Other areas,<br />
referred to as the additional four Ps,<br />
should also be considered: process,<br />
people (frontline staff), physical<br />
environment (appearance <strong>of</strong> your<br />
location) and productivity and quality<br />
(ways to improve productivity and<br />
quality as defined by your customer),<br />
depending on your type <strong>of</strong> service or<br />
product (Lovelock &Wirtz, 2007).<br />
Financials<br />
Provide an overview <strong>of</strong> your financial<br />
plan, including your start-up budget,<br />
start-up expenses and operating<br />
expenses. You will also want to include<br />
details regarding your financial goals,<br />
how you plan to receive payment from<br />
your customers and what accounting<br />
system you plan to use. Commonly<br />
included here is a balance sheet, break<br />
even analysis, pr<strong>of</strong>it and loss statement,<br />
equipment list and any needed<br />
investment or loan requests. This is<br />
another opportunity for you to<br />
convince a potential investor to invest<br />
in your business.<br />
Key personnel<br />
One <strong>of</strong> the most important aspects <strong>of</strong><br />
a business, particularly in the health<br />
care service sector, is its people.<br />
Success is <strong>of</strong>ten contingent upon<br />
having experienced and qualified staff<br />
who are competent to meet consumer<br />
needs. Identify the company<br />
organisational structure and include a<br />
brief biography with details <strong>of</strong> their<br />
pr<strong>of</strong>essional and educational history.<br />
Also identify appropriate pr<strong>of</strong>essional<br />
licensure, endorsements and<br />
credentials.<br />
“<br />
While the development <strong>of</strong> a business case may be familiar<br />
to many nurses within <strong>Australia</strong>, few may have experience<br />
with the actual development <strong>of</strong> a business plan.<br />
”<br />
Appendix<br />
Include supplemental information that<br />
provides supporting evidence to your<br />
plan. This may be things like tables,<br />
charts, graphs and spread sheets that<br />
you’d like to include but don’t<br />
necessarily fit within the other sections.<br />
With thoughtful and detailed<br />
development <strong>of</strong> these basic elements,<br />
you will be well equipped to address<br />
the challenges <strong>of</strong> starting a business<br />
and growing it to success. Adequate<br />
detail will help inform potential<br />
investors as well as put your business<br />
idea in a realistic position, without<br />
overlooking potential pitfalls. Being<br />
realistic and objective with your vision,<br />
goals and expectations will help you<br />
address any unforeseen problems<br />
down the road, and position you well<br />
as a nurse-lead business.<br />
References<br />
Constantinides, E. (2006). The marketing mix<br />
revisited: Towards the 21st century marketing.<br />
Journal <strong>of</strong> Marketing Management, 22, 407-438.<br />
Johnson, J.E. (1990). Developing an effective<br />
business plan. <strong>Nursing</strong> Economics, 8(3),152-154.<br />
Lovelock, C. &Wirtz J. (2007). Services<br />
marketing: People, technology, strategy (6th ed.).<br />
New Jersey, USA: Pearson International –<br />
Pearson/Prentice Hall.<br />
Mason, C. & Stark M. (2005). What do<br />
investors look for in a business plan A<br />
comparison <strong>of</strong> the investment criteria <strong>of</strong><br />
bankers, venture capitalists and business angels.<br />
International Small Business Journal, 22(3),<br />
227-248.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
36<br />
NURSES IN BUSINESS NAtioNAL NETWORK<br />
Editor: Dr Jane Truscott MRCNA<br />
Sub-editor: Position vacant<br />
A successful nursing business model<br />
By Casey Hamilton<br />
Suzie Hoitink completed her Bachelor <strong>of</strong><br />
<strong>Nursing</strong> degree at the University <strong>of</strong> Canberra<br />
in 1996 and has since nursed in a variety <strong>of</strong><br />
clinical settings. After struggling with acne-prone<br />
skin since her teenage years and finding very<br />
little help available, she turned her attention<br />
to skin care.<br />
In 2005 Suzie founded the first Clear Complexions Clinic in<br />
Canberra after seeing a need to provide a medical approach<br />
for people with skin care problems.<br />
In just five short years her business has come a long way. Her<br />
original staff <strong>of</strong> two nurses has grown to 15 and Suzie now has<br />
two beautiful clinics, one <strong>of</strong> which has training facilities. Over<br />
the five years the clinics’ nurses have treated over 10 000 <strong>of</strong><br />
Canberra’s men, women and teenagers. With plans to expand<br />
this year, it is clear to Suzie that her clinics have indeed found<br />
a niche market.<br />
Clear Complexion Clinics are unique; they exclusively employ<br />
highly skilled nurses to perform all treatments. This has allowed<br />
the clinics to source the latest medical grade technology and<br />
products that aren’t available to those without a medical<br />
background. Suzie knows that when you combine the best<br />
possible technology with the highest qualified people, the<br />
client benefits. That’s what she has done at Clear Complexions.<br />
This investment in her staff and equipment has meant clients<br />
are better analysed, more informed and ensures they receive<br />
the most effective outcome.<br />
The clinic employs enrolled nurses and registered nurses as<br />
well as a nurse practitioner from a variety <strong>of</strong> backgrounds such<br />
as accident and emergency, remote and rural nursing and<br />
midwifery. Along with an extensive training program, all nurses<br />
undertake independently accredited IPL/Laser Safety<br />
certification conducted by the Australasian Academy <strong>of</strong><br />
Cosmetic Dermal Science.<br />
Suzie strongly believes that nurses have the right mix <strong>of</strong> skills<br />
to thrive in this industry. They think critically, work<br />
independently as well as part <strong>of</strong> a team and they empathise<br />
with clients. While there are a lot <strong>of</strong> cosmetic skin care clinics<br />
out there, Suzie’s clinics are about good skin medicine, not just<br />
cosmetic medicine. The staff at the clinics are specialists<br />
because they stick to a narrow field; they only treat skin and<br />
this is why Suzie believes her business is such a success.<br />
Conditions she treats include acne, scarring, rosaceous skin,<br />
sun damage, pigmentation and unwanted hair.<br />
This year Clear Complexions have forged a partnership with<br />
a local charity, Lifeline Canberra. Apart from being able to give<br />
back to the local community, which has supported the clinics,<br />
the nurses at the Clear Complexions clinic will also undertake<br />
the Lifeline Accidental Counsellor course. This will ensure that<br />
the clinic remains focused on building the client’s confidence.<br />
In many circumstances a client’s skin issues have affected their<br />
self-esteem. Clear Complexions give clients direction and it is<br />
a thrill to see them grow in confidence with good skin.<br />
Although her business has expanded considerably, Suzie still<br />
works in the clinics every day and thrives on the regular<br />
contact with her clients. She believes this attitude, her own<br />
personal journey and immense pr<strong>of</strong>essional pride are the<br />
foundations behind this successful nursing model <strong>of</strong> business.<br />
Suzie Hoitink, registered nurse, founder, Clear Complexions<br />
For more information contact the Clear Complexions Clinics at<br />
www.clearcomplexions.com.au<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
37<br />
RCNA’s Life Long Learning Program<br />
As a nurse,<br />
are you ready for the continuing pr<strong>of</strong>essional<br />
development (CPD) requirements under<br />
national registration<br />
For more information:<br />
Visit the 3LP website<br />
www.3lp.rcna.org.au<br />
or call 1800 233 705.<br />
If you are not an RCNA<br />
member, please email<br />
us at 3LP@rcna.org.au<br />
to set up a free triaL.<br />
RCNA’s Life Long Learning Program, 3LP, has a new<br />
look and easy navigation to assist you with developing<br />
your learning plan, accessing online learning activities,<br />
recording your CPD hours and much more.<br />
RCNA<br />
freecall 1800 233 705<br />
3lp@rcna.org.au<br />
www.rcna.org.au<br />
<strong>Australia</strong>’s peak pr<strong>of</strong>essional nursing organisation<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN
38<br />
NURSE PRACtitioNER NAtioNAL NETWORK<br />
Editor: Debbie Deasey MRCNA<br />
Sub-editor: Tim Crowley MRCNA<br />
Complex Care and Trauma Mental Health<br />
Nurse Practitioner<br />
By Tim Crowley MRCNA, Nurse Practitioner, Complex Care and Trauma Mental Health, Child and<br />
Adolescent Mental Health Services, Child, Youth and Women’s Health Service, South <strong>Australia</strong><br />
I have worked<br />
with the Child,<br />
Youth and<br />
Women’s Health<br />
Service for the<br />
past 14 years. I<br />
Tim Crowley<br />
have always found<br />
it a privilege to work with young people<br />
with mental health concerns. Seeing<br />
them respond to treatment and more<br />
importantly the natural process <strong>of</strong><br />
maturation is something to admire.<br />
More <strong>of</strong>ten than not, they are a<br />
marginalised group <strong>of</strong> young people<br />
whom require high level care, therapy<br />
and expertise. These requirements are<br />
what formed the catalyst to my<br />
undertaking further training to become<br />
a Nurse Practitioner (NP).<br />
My key responsibilities as a Complex<br />
Care and Trauma Mental Health NP<br />
include the assessment, management<br />
and treatment/therapy <strong>of</strong> young people<br />
who have experienced trauma and or<br />
complex developmental trauma. The<br />
impact <strong>of</strong> this trauma effects their<br />
functioning in many domains including<br />
affectively, cognitively and with<br />
interpersonal relationships – just to<br />
name a few. My role also includes<br />
managing systemic issues and concerns<br />
related to this cohort <strong>of</strong> young people<br />
as well as working with key stakeholders<br />
in the coordination <strong>of</strong> care.<br />
An additional key responsibility <strong>of</strong> my<br />
role is to provide education to<br />
stakeholders on the assessment and<br />
management <strong>of</strong> young people with<br />
mental health concerns with a particular<br />
focus on trauma, disaster and complex<br />
developmental disturbances. I also<br />
provide clinical supervision and<br />
leadership to multi-disciplinary staff. My<br />
role as an educator extends to the<br />
writing and development <strong>of</strong> resources<br />
related to complex care and trauma<br />
“<br />
I have always found it a privilege to work with young<br />
people with mental health concerns. Seeing them respond<br />
to treatment and more importantly the natural process <strong>of</strong><br />
maturation is something to admire.<br />
”<br />
mental health. Through my writing and<br />
research I have found that the body <strong>of</strong><br />
science surrounding young people and<br />
mental health is constantly evolving and<br />
to maintain contemporary practice, I<br />
have found that my knowledge needs to<br />
be a melding <strong>of</strong> the old and the new<br />
evidence. I also have national and state<br />
involvement in the psychological<br />
responses to disaster and trauma events<br />
and act as an adviser for systems <strong>of</strong> care.<br />
My career evolvement to that <strong>of</strong> an NP<br />
has presented me with vast<br />
opportunities. I am able to work and<br />
observe other clinicians; their<br />
conceptualisations <strong>of</strong> cases and care and<br />
their motivation to act in the best<br />
interest <strong>of</strong> young people. The<br />
collaborative nature <strong>of</strong> the NP role and<br />
the sharing <strong>of</strong> knowledge and skills with<br />
other health pr<strong>of</strong>essionals <strong>of</strong>ten bring<br />
another layer <strong>of</strong> skill and understanding.<br />
This additional layer adds value to the<br />
care process <strong>of</strong> young people and<br />
therefore ultimately improves outcomes<br />
for young people.<br />
Like any career progression, there have<br />
been challenges along the way. The initial<br />
process <strong>of</strong> application to become an NP<br />
was one <strong>of</strong> these challenges. Once I<br />
accepted that it was to be more <strong>of</strong> a<br />
marathon rather than a sprint to an NP,<br />
it made the process a little easier to<br />
fathom. There are also everyday clinical<br />
challenges but the biggest by far is<br />
ensuring there is enough time in the day<br />
and week to complete all tasks – from<br />
direct clinical care, to teaching, to<br />
researching, it <strong>of</strong>ten feels like an<br />
endless list.<br />
However, these challenges are<br />
insignificant to the huge rewards my<br />
role as an NP affords me. My role allows<br />
me to think outside the square, always<br />
with the best interest <strong>of</strong> young people<br />
foremost. I am able to see young people<br />
develop and replace previous unhelpful<br />
thinking and coping strategies with new<br />
and appropriate self-management skills.<br />
I also feel immense pr<strong>of</strong>essional<br />
satisfaction through my teaching and<br />
input into the development <strong>of</strong> other<br />
non-mental health service staff.<br />
I am currently involved in teaching and<br />
training school counsellors across the<br />
state. This allows me to reflect on my<br />
own clinical practice whilst teaching and<br />
sharing skills with others.<br />
As you can see, my role as an NP allows<br />
me the scope <strong>of</strong> practice to be a leader,<br />
a clinician, an educator, a collaborator, a<br />
learner and an observer – sometimes all<br />
<strong>of</strong> these roles simultaneously.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
The <strong>Australia</strong>n Government has established the <strong>Nursing</strong> & Allied Health Rural<br />
Locum Scheme (NAHRLS) to support nurses, midwives and allied health<br />
pr<strong>of</strong>essionals in rural and regional <strong>Australia</strong> to get away to do the pr<strong>of</strong>essional<br />
development training they need to continue their vital work.<br />
NAHRLS will find you and your workplace a suitable locum for the period you<br />
are away. The scheme supports all locum recruitment, travel and accommodation<br />
costs. Applications for this Scheme will be accepted four times a year.<br />
First round applications are now open and you can apply online.<br />
For more information visit:<br />
www.nahrls.com.au<br />
Funded by the <strong>Australia</strong>n Government<br />
Can’t get away to do your<br />
Continuing Pr<strong>of</strong>essional<br />
Development training<br />
Apply to the <strong>Nursing</strong><br />
& Allied Health Rural<br />
Locum Scheme for<br />
someone to fill in for<br />
you while you are<br />
away...<br />
Apply Online!
40<br />
oral health NAtioNAL NETWORK<br />
Editor: Marlene Carlin<br />
Sub-editor: Nina Christ<strong>of</strong>i<br />
Temporomandibular Disorder<br />
By Marlene Carlin, Dental Assistant, Oral Medicine Department, The <strong>Royal</strong> Dental Hospital <strong>of</strong> Melbourne<br />
©iStockphoto<br />
“I have been told I have TMJ<br />
problems – can you help me”<br />
This is a common cry that clinicians<br />
working in the area <strong>of</strong><br />
temporomandibular joints (TMJ)<br />
or more accurately TMD<br />
(temporomandibular disorder)<br />
encounter on a daily basis. Below is<br />
some information that might help<br />
answer some <strong>of</strong> the fundamental<br />
questions about this disorder.<br />
What are the temporomandibular<br />
joints (TMJ)<br />
TMJs are the two joints that connect<br />
the jaw to the skull. They are the joints<br />
that slide and rotate in front <strong>of</strong> each<br />
ear. When properly aligned, a smooth<br />
muscle action such as chewing can<br />
eventuate. When these components<br />
are not aligned nor synchronized in<br />
movement, several difficulties can<br />
occur. Some <strong>of</strong> these problems are<br />
headaches, neck and shoulder aches,<br />
and back pain.<br />
What is the cause <strong>of</strong> TMD<br />
Any problem that prevents the<br />
complex system <strong>of</strong> muscles, bones, and<br />
joints working in harmony may result<br />
in TMD. Several theories have been<br />
proposed with multiple factors<br />
responsible, including an incorrect bite,<br />
direct or indirect physical injury, stress<br />
or emotional factors and tooth<br />
grinding. Common or more obvious<br />
causes <strong>of</strong> TMD can include motor<br />
vehicle and sporting accidents, falls or<br />
a blow to the face. Less obvious causes<br />
can include a wide uncontrolled yawn,<br />
prolonged playing <strong>of</strong> a musical<br />
instrument (such as a wind or a string<br />
instrument) or opening too wide to<br />
bite into a hamburger or hard food.<br />
Teeth grinding or clenching occurs<br />
frequently in patients with TMD.<br />
There is no evidence for a genetic<br />
predisposition.<br />
“<br />
A good analogy for TMD<br />
is that <strong>of</strong> an individual with<br />
a sprained ankle who<br />
continues to walk or run.<br />
”<br />
A good analogy for TMD is that <strong>of</strong> an<br />
individual with a sprained ankle who<br />
continues to walk or run. The ankle<br />
becomes sore and the surrounding<br />
muscles protecting the ankle become<br />
tight. A similar situation is seen in TMD.<br />
If an individual does not seek treatment<br />
and continues daily function by eating,<br />
speaking, yawning, not allowing the jaw<br />
to rest or is a night time teeth grinder<br />
(as if they are running a marathon in<br />
their mouth), this can result in TMD<br />
and if left untreated can result in<br />
chronic pain.<br />
What are the symptoms <strong>of</strong> TMD<br />
Symptoms <strong>of</strong> TMD include:<br />
• jaw discomfort or soreness (early<br />
morning /late afternoon)<br />
• headaches<br />
• pain radiating behind eyes, shoulder,<br />
neck and back<br />
• ear aches, ringing in the ears<br />
• clicking/popping <strong>of</strong> the jaw<br />
• locking <strong>of</strong> the jaw<br />
• clenching <strong>of</strong> the teeth<br />
• dizziness.<br />
Treatment <strong>of</strong> TMD includes:<br />
• resting the TMJ<br />
• medication and/or pain relievers<br />
• relaxation and stress management<br />
techniques<br />
• behavior modification (to reduce<br />
or eliminate the clenching <strong>of</strong> the<br />
teeth)<br />
• physical therapy such as massage<br />
and physiotherapy<br />
• an orthopaedic appliance or mouth<br />
guard worn at night to reduce<br />
teeth grinding<br />
• posture training<br />
• diet modification (to rest the jaw<br />
muscles)<br />
• heat packs<br />
• surgery.<br />
Intra-oral appliances such as occlusal<br />
splints may be required to alter the jaw<br />
position, to reduce muscle activity as<br />
well as for protection <strong>of</strong> the teeth from<br />
grinding habits. These are usually only<br />
required to be worn at night and over<br />
time will relieve the pain <strong>of</strong> TMD.<br />
If simple conservative measures fail and<br />
the pain becomes severe and chronic,<br />
then referral to an oral medicine<br />
specialist for further management is<br />
required. Surgery is rarely needed and<br />
should only be contemplated after<br />
extensive conservative management<br />
has failed and where there is definitive<br />
evidence <strong>of</strong> joint disorder.<br />
Surgery should only be undertaken by<br />
an experienced oral and maxill<strong>of</strong>acial<br />
surgeon.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
PASTORAL NURSING CARE NAtioNAL NETWORK<br />
Editor: Leonie Rastas FRCNA<br />
Sub-editor: Carmel McLeod MRCNA<br />
41<br />
BOOK REVIEW<br />
Five Wishes: Honouring ones personal,<br />
spiritual and medical wishes<br />
Reviewer Rose Hoey MRCNA<br />
File photo<br />
“Getting the care<br />
you want when it<br />
matters most.”<br />
Dr Charlie Corke<br />
spoke <strong>of</strong> his father’s<br />
attitude toward death<br />
in the documentary entitled In the End,<br />
filmed in Geelong in 2009. His dad<br />
made something very clear; he only<br />
wanted to die once. When his time<br />
came he didn’t want to have several<br />
goes, he wanted to die without all the<br />
medical intervention that is available<br />
today. According to Dr Corke, older<br />
<strong>Australia</strong>ns are increasingly being<br />
nursed in intensive care, <strong>of</strong>ten<br />
prolonging their lives without any<br />
hope <strong>of</strong> recovery.<br />
There is a recognised gap in the<br />
medical system in relation to Advanced<br />
Care Planning (ACP); dying is becoming<br />
a medical moment complete with tubes<br />
and alarms rather than a peaceful time<br />
with family and loved ones.<br />
Leonie Rastas, in conjunction with<br />
health promotion charity, Pastoral<br />
Healthcare Network <strong>Australia</strong> (PHNA),<br />
has recently introduced an innovative<br />
program called Five Wishes. Developed<br />
in Florida in 1997 by Aging with<br />
Dignity’s Jim Towey, Five Wishes is<br />
helping address some <strong>of</strong> the issues<br />
surrounding ACP.<br />
Unlike most hospital-based ACP<br />
programs, Five Wishes is communitybased<br />
and presented by specialist<br />
pastoral nurses. Five Wishes is taken to<br />
community groups, health care facilities<br />
and faith communities to provide a<br />
simple and sensitive means <strong>of</strong><br />
empowering people about their future<br />
health care choices, before they<br />
become ill. This ACP program<br />
specifically incorporates personal,<br />
spiritual and emotional care in its plan.<br />
Individuals can rest assured that their<br />
cultural and personal faith practices<br />
will be honoured if they can no longer<br />
speak for themselves. The Five Wishes<br />
ACP is designed for people over 18.<br />
There is also a My Wishes booklet<br />
especially designed for children under<br />
18 suffering life-limiting illnesses.<br />
Fives Wishes presents an opportunity<br />
for patients to express their wishes in<br />
regard to their end <strong>of</strong> life treatment<br />
and support, an important opportunity<br />
in the instance that they’re unable<br />
to express their own needs when<br />
it comes time.<br />
The Five Wishes ask the following<br />
questions:<br />
1. Who do you want to make health<br />
care decisions for you when you<br />
cannot make them yourself<br />
2. What kind <strong>of</strong> medical treatment<br />
do you want or not want<br />
3. How comfortable do you want<br />
to be<br />
4. How do you want people to<br />
treat you<br />
5. What do you want your loved<br />
ones to know<br />
Five Wishes also covers issues like<br />
pain management, life support, organ<br />
donation options and funeral wishes.<br />
The thought <strong>of</strong> having to make<br />
decisions about another person’s health<br />
care is daunting for most people. The<br />
Five Wishes booklet helps take the guess<br />
work out <strong>of</strong> difficult situations such as<br />
continuing life support after a<br />
devastating accident or stroke. Most<br />
ACPs are left until too late when<br />
emotions <strong>of</strong>ten distort decision making.<br />
The common fears around end <strong>of</strong> life<br />
care are fully addressed in the Five<br />
Wishes booklet and it is highly<br />
recommended for all health care<br />
providers to complete the process for<br />
themselves too. Five Wishes truly is a<br />
gift to oneself and one’s family.<br />
For more information, please go to<br />
www.pastoralhealthcarenetwork.org<br />
References<br />
Roseby, C. (Director). (2010). In the End.<br />
[Motion picture]. Geelong, VIC: Screen<br />
<strong>Australia</strong>. Available from www.in-the-end.com<br />
Aging with Dignity. Aging with Dignity Five<br />
Wishes. (2010). Retrieved from www.<br />
agingwithdignity.org<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
10 ePoints<br />
10 ePoints<br />
Feature Product<br />
HOT<br />
PRICE<br />
Yellow<br />
Black<br />
Orange<br />
White<br />
Teal<br />
Purple<br />
Green Navy Light<br />
Blue<br />
Silicone FOB Watch<br />
Why not add some colour to<br />
your ward with this fun Nurse<br />
watch!<br />
Cleanable silicone<br />
Complete Nurse Card Pack<br />
- I.V. Drip rates<br />
- Maths Conversions<br />
- Advanced Life Support<br />
- Adult Paed ALS CPR<br />
- ECG Translations<br />
- Rhythm Analysis<br />
- Patient Assessment<br />
- Blood Gas Analysis<br />
- Pathology Values<br />
ESSENTIAL<br />
Durable<br />
&<br />
Waterpro<strong>of</strong><br />
$<br />
24 00 ea<br />
Cyan Pink Red<br />
Silicone Band<br />
Watch & Band<br />
$<br />
4 00 ea<br />
$<br />
15 95 ea<br />
Quartz movement<br />
Changeable bands<br />
BULK DISCOUNT<br />
Order 20 or more and pay<br />
$12.50/watch.<br />
10 ePoints 15 ePoints 15 ePoints<br />
Frosted Mauve<br />
Frozen Pink<br />
Electric Blue<br />
Ice Blue<br />
Purple<br />
Matte Silver<br />
$<br />
16 50 ea<br />
Colours<br />
$<br />
27 50 ea<br />
Accessory Colours<br />
Neurological LED Penlight Elite Care - Sprague Style Premium Nurse Utility Kit<br />
- Long life LED bulb<br />
- Pupil Gauge & GCS Categories<br />
- 2 x AAAs included<br />
SAVE<br />
$4.50<br />
Light<br />
Blue<br />
Red<br />
Black<br />
Yellow<br />
Pink<br />
Green<br />
Navy<br />
Blue<br />
Purple<br />
- Adult /Paed Dual Head<br />
- Five functions with attachments<br />
- 24 month warranty<br />
SAVE<br />
$7.50<br />
Pink<br />
Red<br />
Navy<br />
Blue<br />
Green<br />
Purple<br />
- Uniform material Joey Jr Pouch<br />
with quality accessories.<br />
- All kits have Navy Pouch<br />
SAVE<br />
$16.00<br />
$<br />
69 00 ea<br />
NURSING SUPERSTORE Equipment | Books | Apparel<br />
JOIN ONLINE<br />
FREE<br />
Shopper Account<br />
Specials & Discounts<br />
Order Tracking<br />
Rewards Points<br />
Join this month and receive<br />
100 FREE POINTS<br />
100%<br />
Satisfaction Policy<br />
24 Hour<br />
Order Processing<br />
$6.50<br />
Standard Postage<br />
* GST included<br />
* See conditions online<br />
* While stocks last<br />
TO ORDER<br />
Call 1300 886 814<br />
Visit eNurse.com.au<br />
Online | Mail | Cheque |<br />
Money Order | Telephone<br />
VIEW THE FULL<br />
PRODUCT RANGE<br />
ONLINE<br />
Equip. Educate. Connect.<br />
R
RESEARCH NAtioNAL NETWORK<br />
Editor: Raymond Chan FRCNA<br />
Sub-editor: Judith Anderson MRCNA<br />
43<br />
Enhancing self-management<br />
program to improve<br />
outcomes in cardiac<br />
patients with diabetes<br />
By Dr Jo Wu MRCNA, Research Fellow, School <strong>of</strong> <strong>Nursing</strong> and<br />
Midwifery, Institute <strong>of</strong> Health and Biomedical Innovation,<br />
Queensland University <strong>of</strong> Technology<br />
Dr Jo Wu<br />
I am a Research Fellow at the School<br />
<strong>of</strong> <strong>Nursing</strong> and Midwifery, Queensland<br />
University <strong>of</strong> Technology (QUT) – one<br />
<strong>of</strong> only 3 <strong>Australia</strong>n nursing schools<br />
receiving an ERA Ranking 5/5, indicating<br />
outstanding performance well above<br />
world standard. I am also an Early<br />
Career Researcher, an affiliate member<br />
<strong>of</strong> the Institute <strong>of</strong> Health and<br />
Biomedical Innovation (IHBI) at QUT<br />
being mentored by Pr<strong>of</strong>essor Anne<br />
Chang (local) and Pr<strong>of</strong>essor Mary<br />
Courtney (international). I have held<br />
positions as a clinical nurse in critical<br />
care units for over 16 years in <strong>Australia</strong><br />
and overseas. My research interests<br />
evolved from this clinical experience<br />
and have made a significant<br />
contribution to promoting selfmanagement<br />
for patients with<br />
coronary heart disease and diabetes.<br />
Current literature supports the success<br />
<strong>of</strong> self-management programs based<br />
on improving self-efficacy levels in<br />
modifying lifestyles for different patient<br />
groups with chronic diseases such as<br />
type 2 diabetes and cardiac disease.<br />
However, existing models <strong>of</strong> discharge<br />
planning and follow-up care for people<br />
with these two major co-morbidities<br />
do not address the need to provide<br />
self-management programs tailored for<br />
these patients, who are confronted<br />
with highly complex self-management<br />
needs when transitioning from the<br />
Coronary Care Unit (CCU) to home.<br />
My studies have addressed these gaps.<br />
The aim <strong>of</strong> my doctoral research was<br />
to gain in-depth understanding <strong>of</strong> the<br />
characteristics, needs and experiences<br />
<strong>of</strong> patients with type 2 diabetes who<br />
were hospitalised for a critical cardiac<br />
event (Wu & Chang, 2008; Wu, Chang,<br />
& McDowell, 2008). A further aim was<br />
to develop and pilot test a selfmanagement<br />
program (Wu, Chang, &<br />
McDowell, 2009). The research results<br />
from these studies have provided<br />
clinically relevant knowledge <strong>of</strong> the<br />
potential for a self-management<br />
program to promote continuity <strong>of</strong> care<br />
from the critical care environment to<br />
home, thereby contributing to clinical<br />
practice. The implications include<br />
enhancing transition from hospital to<br />
home, potentially reducing hospital<br />
re-admissions, and incorporating more<br />
effective self-management behaviour in<br />
patients’ daily life.<br />
My post-doctoral studies have<br />
continued to advance knowledge in<br />
the promotion <strong>of</strong> self-management for<br />
patients with coronary heart disease<br />
and diabetes. Projects planned for the<br />
future include refinement <strong>of</strong> the<br />
cardiac-diabetes self-management<br />
program, incorporating telephone and<br />
text-messaging (Wu, Chang, Courtney,<br />
Shortridge-Baggett, & Kostner, in press)<br />
and peer supporters (Wu et al., in<br />
press) in the delivery <strong>of</strong> the program,<br />
evaluating these delivery modes for<br />
transitional care, and undertaking the<br />
intervention in different cultural<br />
contexts.<br />
References:<br />
Wu, C.-J., & Chang, A.M. (2008). Audit <strong>of</strong><br />
patients with type 2 diabetes following a<br />
critical cardiac event. International <strong>Nursing</strong><br />
Review, 55, 327-332.<br />
Wu, C.-J., Chang, A., & McDowell J. (2008).<br />
Perspectives <strong>of</strong> patients with type 2 diabetes<br />
following a critical cardiac event - an<br />
interpretive approach. Journal <strong>of</strong> <strong>Nursing</strong> and<br />
Healthcare <strong>of</strong> Chronic Illness in association with<br />
Journal <strong>of</strong> Clinical <strong>Nursing</strong>, 17(5a), 16-24.<br />
Wu, C.-J., Chang, A., & McDowell J. (2009).<br />
Innovative self-management program for<br />
diabetics following CCU admission.<br />
International <strong>Nursing</strong> Review, 56, 396-399.<br />
Wu, C.-J., Chang, A.M., Courtney, M.,<br />
Shortridge-Baggett, L.M., & Kostner, K. (in<br />
press). Development and pilot test <strong>of</strong> a<br />
Peer-support based Cardiac-Diabetes<br />
Self-Management Program using randomised<br />
controlled trial: A study protocol, BMC Health<br />
Services Research.<br />
Wu, C.-J., Chang, A.M., Courtney, M., & Ramis,<br />
M. (in press). Using user-friendly<br />
telecommunications to improve cardiac and<br />
diabetes self-management program: A pilot<br />
study. Journal <strong>of</strong> Evaluation in Clinical Practice.<br />
For further information on this research<br />
program, please contact me at<br />
c3.wu@qut.edu.au.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
44<br />
RESEARCH NAtioNAL NETWORK<br />
Editor: Raymond Chan FRCNA<br />
Sub-editor: Judith Anderson MRCNA<br />
Celebrating an emerging<br />
research and development culture<br />
By Dr Katrina Cubit MRCNA, Innovation Coordinator, Calvary Health Care ACT<br />
The National Health and Hospitals Reform Commission<br />
(2009:202) identified continuous improvement, innovation and<br />
research as the fifth level <strong>of</strong> reform needed to create an agile and<br />
self improving health system.<br />
Based on this report, the focus <strong>of</strong><br />
<strong>Australia</strong>n health reform will include<br />
building a “vibrant culture <strong>of</strong> innovation<br />
and research” that permeates health<br />
services. This undertaking is to be<br />
underpinned by collaborative and<br />
cohesive partnerships between<br />
universities, research institutes, hospitals<br />
and health services.<br />
As a Catholic health care provider, the<br />
vision <strong>of</strong> Calvary Health Care ACT<br />
(CHCACT) is to excel and be<br />
recognised as a continuing source <strong>of</strong><br />
healing, hope and nurturing to the<br />
Canberra community. To reach these<br />
goals, embracing a cultural shift toward<br />
recognising the importance <strong>of</strong> research<br />
and development is paramount.<br />
CHCACT is proud to promote two<br />
new research projects whose aims are<br />
to improving the care <strong>of</strong> people with<br />
delirium.<br />
What is delirium<br />
Delirium is a disturbance <strong>of</strong><br />
consciousness where inattention is<br />
accompanied by a change in cognition<br />
or perceptual disturbance that<br />
develops over a short period <strong>of</strong> time<br />
(DSM IV, 2000). It is characterised by<br />
an acute confusion defined by<br />
fluctuating mental status, inattention<br />
and either disorganised thinking or an<br />
altered level <strong>of</strong> consciousness<br />
(Maldonado, 2008; Girard et al., 2008).<br />
Delirium is reported to occur in up to<br />
62% <strong>of</strong> hospitalised older orthopaedic<br />
patients (Ol<strong>of</strong>sson, Lundström, Borssén,<br />
Nyberg & Gustafson, 2005). The<br />
incidence <strong>of</strong> delirium increases up to<br />
80% in critically ill ICU patients<br />
receiving mechanical ventilation (Pun &<br />
Ely, 2007; Girard et al., 2008) and to<br />
89% <strong>of</strong> patients who have dementia<br />
(Fick, Agostini & Inouye, 2002).<br />
Most <strong>of</strong> the mechanisms involved in<br />
developing delirium are reported to be<br />
related to imbalances in<br />
neurotransmitters that modulate<br />
cognition, behaviour and mood, thus<br />
generating different subcategories <strong>of</strong><br />
delirium according to psychomotor<br />
symptoms experienced, such as<br />
‘hyperactive’, ‘hypoactive’ and ‘mixed’<br />
delirium (Maldonado, 2008; Girard et<br />
al., 2008).<br />
The aetiology <strong>of</strong> delirium is considered<br />
to be multifactorial, a result <strong>of</strong><br />
predisposing factors (age, dementia)<br />
and precipitating factors (polypharmacy,<br />
bladder catheterisation, sleep<br />
deprivation) (Siddiqi, House & Holmes,<br />
2006; Inouye & Charpentier, 1996).<br />
Although delirium may result from<br />
patients’ specific underlying illness, it is<br />
<strong>of</strong>ten an outcome <strong>of</strong> different<br />
iatrogenic factors and thus preventable<br />
sources (Pandharipande et al., 2006).<br />
Observational prospective and<br />
retrospective studies have documented<br />
increased evidence linking delirium and<br />
a higher risk <strong>of</strong> long-term cognitive<br />
impairment, including dementia<br />
(MacLullich, Beaglehole, Hall & Meagher,<br />
2009), as well as decreased survival,<br />
functional outcomes, and quality <strong>of</strong> life<br />
(Girard et al., 2010; Meyer & Hall,<br />
2006). Published work refers to these<br />
patients exhibiting deficits in executive<br />
functions (planning, organisation,<br />
behavioural inhibition, and decision<br />
making); attention deficits, problem<br />
solving and onset or worsening <strong>of</strong><br />
dementia. This increases the risk <strong>of</strong><br />
discharge to a residential aged care<br />
facility and patient mortality in hospital<br />
as well as 12 months post discharge<br />
(Pun & Ely, 2007).<br />
Delirium prevention, early detection<br />
and management program<br />
The first <strong>of</strong> the two delirium research<br />
projects at CHCACT is an<br />
interdisciplinary nurse-led delirium<br />
prevention, early detection and<br />
CHCACT is proud to promote two new research<br />
projects whose aims are to improving the care <strong>of</strong><br />
people with delirium.<br />
“<br />
”<br />
management program which<br />
commenced in March 2011. The aim <strong>of</strong><br />
this pilot project is to provide delirium<br />
specific education to nursing and<br />
medical staff at CHCACT. The<br />
education will focus on prevention,<br />
early detection, diagnosis,<br />
documentation and the environmental<br />
and pharmacological management <strong>of</strong><br />
delirium.<br />
While there is some evidence to<br />
suggest that antipsychotics are effective<br />
in treating the behavioural problems<br />
associated with delirium, additional<br />
resources and education focussing on<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
45<br />
Dr Katrina Cubit, Gary Mercer and Daniella Bulic<br />
the non-pharmacological management<br />
<strong>of</strong> delirium will be provided as part <strong>of</strong><br />
the pilot project. This component <strong>of</strong><br />
the project will be supported by Ms<br />
Stefanie Pearce (Occupational<br />
Therapist). The project team comprises<br />
<strong>of</strong> Dr Katrina Cubit (Innovation<br />
Coordinator); Mr Gary Mercer (Older<br />
Persons Mental Health Unit); Dr Anna<br />
Burger (Senior Staff Specialist and<br />
Liaison Psychiatrist); and Dr Pravin<br />
Kumar (Consultant Psychiatrist). The<br />
team was awarded an ACT Health<br />
Practice Development Scholarship for<br />
2011.<br />
Cognitive and psychosocial impact <strong>of</strong><br />
delirium on mechanically ventilated<br />
patients in ICU<br />
The second project is a prospective,<br />
observational pilot study in the<br />
CHCACT Intensive Care Unit (ICU)<br />
which aims to explore cognitive and<br />
psychosocial outcomes <strong>of</strong> mechanically<br />
ventilated ICU patients with and<br />
without delirium. The study seeks to<br />
investigate the effects <strong>of</strong> delirium on<br />
patients’ cognitive functioning and<br />
psychosocial outcomes, in particular<br />
their potential for developing<br />
depression and anxiety, and/or Post<br />
Traumatic Stress Disorder (PTSD).<br />
These psychological outcomes seem to<br />
be significant markers <strong>of</strong> a decline in<br />
cognitive function, daily functioning,<br />
quality <strong>of</strong> life and (in)ability to return to<br />
work, which can result in discharge to<br />
aged care facilities (Oeyen, Vandijck,<br />
Benoit, Annemans & Decruyenaere,<br />
2010). This project is coordinated by<br />
Daniella Bulic (Social Worker, PhD<br />
Candidate) with Associate Pr<strong>of</strong>essor<br />
Michael Bennett (supervisor UNSW),<br />
Yahya Shehabi (Consultant Intensivist,<br />
UNSW supervisor), Associate Pr<strong>of</strong>essor<br />
Jeffrey Looi (Psychiatrist, ANU<br />
supervisor) and Dr Paul Lambeth<br />
(Director <strong>of</strong> ICU CHCACT).<br />
Both projects will contribute to<br />
improving the patient experience<br />
and reducing length <strong>of</strong> stay through<br />
enhancing staff skill and competence.<br />
References<br />
American Psychiatric Association, (2000).<br />
Diagnostic and Statistical Manual <strong>of</strong> Mental<br />
Disorders. (4th ed.). Washington, DC: American<br />
Psychiatric Association.<br />
Bulic, D., (2009). ‘We Thought We’d Never Sleep<br />
Again’, exploration <strong>of</strong> couples’ relationships one<br />
year after their participation in standard and<br />
“Bringing Baby Home”, (BBH modified antenatal<br />
classes in Calvary Health Care antenatal<br />
education), paper presented at ANZAME,<br />
Launceston, Tasmania 30th June - 4th July.<br />
Fick, D.M., Agostini, J.V., & Inouye, S.K. (2002).<br />
Delirium superimposed on dementia: a<br />
systematic review. Journal <strong>of</strong> the American<br />
Geriatrics Society, 50(10), 1723-1732.<br />
Girard, T.D., Jackson, J.C., Pandharipande, P.P.,<br />
Pun, B.T., Thompson, J.L., Shintani, A.K., ... Ely,<br />
E.W. (2010) Delirium as a predictor <strong>of</strong><br />
long-term cognitive impairment in survivors <strong>of</strong><br />
critical illness. Critical Care Medicine, 38(7),<br />
1513-1520.<br />
Girard, C.I., Pandharpipande, P.P., & Ely, E.W.<br />
(2008). Delirium in the intensive care unit.<br />
Critical Care, (Supplement 3), S3.<br />
Inouye, S.K., & Charpentier P.A. (1996).<br />
Precipitating factors for delirium in hospitalized<br />
elderly patients: predictive model and<br />
interrelationship with baseline vulnerability.<br />
JAMA, 275, 852-857.<br />
National Health and Hospital Reform<br />
Commission (2009). A healthier future for all<br />
<strong>Australia</strong>ns. Retrieved from http://www.health.<br />
gov.au/internet/nhhrc/publishing.nsf/Content/<br />
nhhrc-report<br />
MacLulluich, A.M.J., Beaglehole, A., Hall, R.J., &<br />
Meagher, D.J. (2009). Delirium and long-term<br />
cognitive impairment. International Review <strong>of</strong><br />
Psychiatry, 21(12), 30-42.<br />
Maldonado, J.R. (2008). Pathoetiological Model<br />
<strong>of</strong> Delirium: A comprehensive understanding<br />
<strong>of</strong> the neurobiology <strong>of</strong> delirium and an<br />
evidence-based approach to prevention and<br />
treatment. Critical Care Clinics, 24, 789-856.<br />
Meyer, N.J., & Hall, J.B. (2006). Bench-tobedside<br />
review: Brain dysfunction in critically ill<br />
patients - the intensive care unit and beyond.<br />
Critical Care, 10, 223.<br />
Ol<strong>of</strong>sson, B., Lundström, M., Borssén, B.,<br />
Nyberg, L. & Gustafson, Y. (2005). Delirium is<br />
associated with poor rehabilitation outcome in<br />
elderly patients treated for femoral neck<br />
fractures. Scandinavian Journal <strong>of</strong> Caring<br />
Sciences, 19(2), 119-127.<br />
Oeyen, S.G., Vandijck, D.M., Benoit, D.,<br />
Annemans, L. & Decruyenaere, J.M. (2010).<br />
Quality <strong>of</strong> life after intensive care: a systematic<br />
review <strong>of</strong> the literature. Critical Care Medicine,<br />
38(12), 1-15.<br />
Pandharipande, P., Shintani, A., Peterson, J., Pun,<br />
B.T., Wilkinson, G.R., Dittus, R.S., ... Ely, E.W<br />
(2006). Lorazepam is an independent risk<br />
factor for transitioning to delirium in intensive<br />
care unit patients. Anesthesiology, 104(1), 21-6.<br />
Pun, B. & Ely, E.W. (2007). The importance <strong>of</strong><br />
diagnosing and managing ICU delirium. Chest,<br />
132, 624-636.<br />
Siddiqi N., House A.O. & Holmes J.D. (2006).<br />
Occurrence and outcome <strong>of</strong> delirium in<br />
medical in-patients; a systematic literature<br />
review. Age Ageing, 35, 350-364.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011
46<br />
TRANSCULtuRAL NAtioNAL NETWORK<br />
Editor: Pr<strong>of</strong>essor Violeta Lopez FRCNA<br />
Sub-editor: Dr Sue Webster MRCNA<br />
Glenn Yepes<br />
From the Philippines to <strong>Australia</strong>:<br />
A career spanning great ethnic diversity<br />
Glenn Yepes<br />
By Pr<strong>of</strong>essor Violeta Lopez FRCNA, School <strong>of</strong> <strong>Nursing</strong> (NSW and ACT), <strong>Australia</strong>n Catholic University<br />
Glenn Yepes completed his nursing degree with honours in the<br />
Philippines and received a silver medal for clinical expertise. He was<br />
employed as a company nurse in a construction company and was<br />
responsible for the care <strong>of</strong> 100 construction workers.<br />
Glenn went on to complete a course in<br />
paediatric cardiology, which prepared<br />
him to work in the Philippines<br />
Children’s Medical Centre, Neonatal<br />
Intensive Care Unit. He worked there<br />
for seven years, until accepting a job in<br />
Saudi Arabia, working as a neonatal<br />
intensive care nurse in a 700 bed<br />
military hospital. Glenn stayed in Saudi<br />
Arabia for two years before taking<br />
another position at Our Lady’s Children<br />
Hospital in Ireland, also as a neonatal<br />
intensive care nurse. He continued to<br />
attend several courses in newborn care<br />
including skills in intravenous<br />
cannulation and cardiac resuscitation.<br />
It was the long, cold climate in Ireland<br />
that drove Glenn to move to <strong>Australia</strong>.<br />
It was a warmer place to live and was<br />
also the home <strong>of</strong> some <strong>of</strong> his friends<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
47<br />
from Saudi Arabia and Ireland. Glenn<br />
says that working in Saudi Arabia and<br />
Ireland had broadened his perspective<br />
on cultural issues that contributed to<br />
his understanding when caring for his<br />
patients and families, especially those<br />
parents who had premature infants.<br />
He also said that he learned to speak<br />
a little bit <strong>of</strong> Arabic but found it difficult<br />
to imitate the Irish way <strong>of</strong> speaking.<br />
Glenn now works at Canberra Hospital<br />
Centre for Newborn Care. With his<br />
knowledge and experience working in<br />
neonatal intensive care units for the last<br />
12 years, he found it easy to adjust<br />
working in another environment,<br />
especially one which provided him<br />
with a mentor during his first months<br />
at work. Glenn is an ambitious person<br />
and decided to enrol in the Graduate<br />
Certificate in Clinical <strong>Nursing</strong>, Neonatal<br />
Care, at the <strong>Australia</strong>n Catholic<br />
University. He completed this course<br />
with distinction and now plans to enrol<br />
in a master’s program.<br />
Hospital colleagues are helpful and easy to work<br />
with and there are always opportunities to upgrade<br />
skills and knowledge in my chosen specialty.<br />
“<br />
”<br />
When asked about his experience<br />
working in <strong>Australia</strong>, Glenn says “People<br />
here are friendly and hospitable.<br />
Hospital colleagues are helpful and easy<br />
to work with and there are always<br />
opportunities to upgrade skills and<br />
knowledge in my chosen specialty.<br />
Glenn goes on to say, “Coming to<br />
<strong>Australia</strong> has been the best career<br />
decision I have ever made.”<br />
Glenn is also a member <strong>of</strong> the<br />
<strong>Australia</strong>n <strong>College</strong> <strong>of</strong> Neonatal Nurses<br />
and takes every opportunity to be<br />
involved in its activities. Glenn plans to<br />
spend his annual leave in the Philippines<br />
and visit his alma mater and the<br />
hospitals he used to work in. He hopes<br />
to share his experiences working in<br />
different parts <strong>of</strong> the world as well as<br />
share his knowledge and skills with<br />
other neonatal nurses back home.<br />
Glenn believes in giving back what has<br />
been given to him, in passing on the<br />
experiences and lessons that have<br />
prepared him for his work and success<br />
in life.<br />
EffEctivE advocacy<br />
CAN iNflueNCe the heAlth RefORm AGeNdA<br />
RCNA provides a singular voice and united policy<br />
focus for the nursing pr<strong>of</strong>ession. RCNA actively<br />
participates on many national and state/territory<br />
forums <strong>of</strong> significance to the nursing pr<strong>of</strong>ession.<br />
We take your ideas forward to Government and<br />
other health stakeholders.<br />
RCNA’s strength comes from the participation<br />
<strong>of</strong> and support from its members.<br />
Our members are able to provide a diverse<br />
nursing perspective to our policy development.<br />
WE WaNt yoUR iNvoLvEMENt!<br />
As an RCNA member you can:<br />
contribute to an RCNA submission – provide<br />
your ideas, feedback, experiences or comments<br />
to inform RCNA submission development<br />
raise pr<strong>of</strong>essional issues that concern you –<br />
send us your thoughts on issues affecting the<br />
nursing pr<strong>of</strong>ession<br />
apply to become an RCNA representative –<br />
RCNA regularly seeks experienced and enthusiastic<br />
members and fellows to represent us on a wide<br />
variety <strong>of</strong> working groups, advisory bodies and<br />
at pr<strong>of</strong>essional functions.<br />
visit rcna.org.au/getinvolved<br />
RCNA<br />
freecall 1800 061 660<br />
canberra@rcna.org.au<br />
www.rcna.org.au<br />
<strong>Australia</strong>’s peak pr<strong>of</strong>essional nursing organisation<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | june 2011<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN
48<br />
rcna chapter committees<br />
ACT/SOUTHERN NSW<br />
Chairperson<br />
Eric Daniels FRCNA<br />
Vice Chair<br />
Shane Lenson FRCNA<br />
Secretary<br />
Narelle Caligari MRCNA<br />
Committee members<br />
Associate Pr<strong>of</strong>essor Laurie Grealish FRCNA<br />
Kaye Hogan AM FRCNA<br />
Lacey Smale MRCNA<br />
Daniel Gordon MRCNA<br />
Link member<br />
Pamela Brinsmead FRCNA<br />
Student member<br />
Leeanne Thompson<br />
Board member<br />
Paula Elliott FRCNA<br />
HUNTER VALLEY/<br />
NORtheRN NSW<br />
Chairperson<br />
Beverley Bailey MRCNA<br />
Vice Chairperson<br />
Maria Gorton MRCNA<br />
Secretary<br />
Elizabeth Newham MRCNA<br />
Committee members<br />
Lynne Slater MRCNA<br />
Lynette Bowen FRCNA<br />
Whenua Oner MRCNA<br />
Link members<br />
Jennifer Carney MRCNA<br />
Susan Creech MRCNA<br />
Kerry Harman MRCNA<br />
Raelene Kenny MRCNA<br />
Tiana Trappel MRCNA<br />
Student representatives<br />
Donovan Friel<br />
Elizabeth Kepreotes MRCNA<br />
Board member<br />
Julie Shepherd FRCNA<br />
NORTHERN TERRitoRY<br />
Chairperson<br />
Beryl McEwan MRCNA<br />
Vice Chairperson<br />
Associate Pr<strong>of</strong>essor Peter Brown FRCNA<br />
Secretary<br />
Dr Beverly Turnbull FRCNA<br />
Committee members<br />
Catherine Brown MRCNA<br />
Gylo Hercelinskyj MRCNA<br />
Elizabeth Webb FRCNA<br />
Christine Quirke MRCNA<br />
Board member<br />
Gay Lavery FRCNA<br />
QUEENSLAND<br />
Chairperson<br />
John Brown FRCNA<br />
Vice Chairperson<br />
Susan DeVries FRCNA<br />
Secretary<br />
Mark Kearin MRCNA<br />
Committee members<br />
Belynda Abbott MRCNA<br />
Lieutenant Colonel Kerry Clifford MRCNA<br />
Robyn Dickie MRCNA<br />
Dr Judith Gonda MRCNA<br />
Lorraine McMurtrie MRCNA<br />
Carolyn Robinson FRCNA<br />
Kathryn Wooldridge MRCNA<br />
Debra Culter MRCNA<br />
Anne-Marie Goes MRCNA<br />
Kate Kunzelmann MRCNA<br />
Board member<br />
Associate Pr<strong>of</strong>essor Stephanie Fox-Young<br />
FRCNA FCN<br />
SOUTH AUSTRALIA<br />
Chairperson<br />
Lesley Siegl<strong>of</strong>f FRCNA<br />
Vice Chairperson<br />
Ian Thackray FRCNA<br />
Secretary<br />
Anne Davies MRCNA<br />
Committee members<br />
James Bonello MRCNA<br />
Tiffany Conroy FRCNA<br />
Heather Schubert OAM FRCNA<br />
Collette Lancaster-Lockwood MRCNA<br />
Esther Michelsen MRCNA<br />
Board member<br />
Ian Thackray FRCNA<br />
TASMANIA<br />
Chairperson<br />
Associate Pr<strong>of</strong>essor John Field FRCNA<br />
Past Chairperson<br />
Jenny Tuffin FRCNA<br />
Vice Chairperson<br />
Elaine Hosken FRCNA<br />
Committee members<br />
Helen Bryan FRCNA<br />
Karen Linegar FRCNA<br />
Dianne Miller MRCNA<br />
Karen O’Shea MRCNA<br />
Wayne Smith MRCNA<br />
Deanne West MRCNA<br />
Simone Baxter MRCNA<br />
Link members<br />
Francine Douce MRCNA<br />
Alison Keleher MRCNA<br />
Pr<strong>of</strong>essor Mary Fitzgerald FRCNA<br />
Board member<br />
Gayle Heckenberg FRCNA<br />
VICTORIA<br />
Chairperson<br />
Donna Watmuff FRCNA<br />
Vice Chairperson<br />
Sussan Pleunik FRCNA<br />
Secretary<br />
Kay Plymat FRCNA<br />
Committee members<br />
Maryanne Craker MRCNA<br />
Michelle Gardner MRCNA<br />
Hyder Gulam FRCNA<br />
Pamela Ingram MRCNA<br />
Jill Linklater FRCNA<br />
Suzanne Metcalf MRCNA<br />
Adjunct Pr<strong>of</strong>essor Penny Newsome FRCNA<br />
Yvette Gomez FRNCA<br />
Link member<br />
Julieanne Crow MRCNA<br />
Student Representative<br />
Melissa Bloomer MRCNA<br />
Board member<br />
Christine Smith FRCNA<br />
WESTERN AUSTRALIA<br />
Chairperson<br />
Cheryle Poultney MRCNA<br />
Past Chairperson<br />
Vicki Cope FRCNA<br />
Vice Chairperson<br />
Tony Patton FRCNA<br />
Secretary<br />
Janet Anderson MRCNA<br />
Committee members<br />
Jane Cranley MRCNA<br />
Sarah Hession MRCNA<br />
Pr<strong>of</strong>essor Linda Shields FRCNA<br />
Colleen Van Lochem MRCNA<br />
Marie Tyrell-Clark FRCNA<br />
Patricia Canning FRCNA<br />
Board member<br />
Carmen Morgan FRCNA<br />
Correction<br />
The credit for the photo <strong>of</strong><br />
Kathleen Kehoe FRCNA, Cr Judith<br />
Klepner and Cr Frank O’Connor,<br />
featured on page 2 <strong>of</strong> the March<br />
edition <strong>of</strong> Connections was omitted.<br />
The Mayor’s <strong>of</strong>fice <strong>of</strong> the City <strong>of</strong><br />
Port Phillip kindly gave us<br />
permission to publish this photo.<br />
<strong>CONNECTIONS</strong> | VOL 14 | ISSUE 2 | June 2011
Exciting RCNA<br />
Member Offer<br />
10 % <strong>of</strong>f<br />
Standard membership fees *<br />
• Initial Once Off Start Up Fee *<br />
Includes:<br />
• Starter Backpack<br />
• Induction Program<br />
• Benefits & Rewards<br />
• Over 90 Clubs across <strong>Australia</strong> †<br />
Offer valid from 1 st February 2011<br />
until 28 th February 2012<br />
fitnessfirst.com.au<br />
Please take a copy <strong>of</strong> this flyer and<br />
pro<strong>of</strong> <strong>of</strong> your RCNA membership to<br />
your local Fitness First club to join.<br />
Lifestyle Passport<br />
(min term 12 months)<br />
Premier Passport<br />
(month to month -<br />
min term 1 month)<br />
Lifestyle Platinum<br />
(min term 12 months)<br />
Premier Platinum<br />
(month to month -<br />
min term 1 month)<br />
Weekly Rates WAS $23.95<br />
NOW $21.55<br />
WAS $28.95<br />
NOW $26.05<br />
WAS $25.95<br />
NOW $23.35<br />
WAS $30.95<br />
NOW $27.85<br />
Joining Fee $69.95 $69.95 $69.95 $69.95<br />
Total Price $1,190.55 $174.15 $1,284.15 $181.35<br />
*Subject to Fitness First terms and conditions <strong>of</strong> membership (available in club). Not valid with any other <strong>of</strong>fer. Start Up fee payable on joining or transferring to this <strong>of</strong>fer. If a Lifestyle<br />
membership is taken up under this <strong>of</strong>fer (whether by a new or existing member), the minimum term <strong>of</strong> that membership is 12 months from the date <strong>of</strong> taking up this <strong>of</strong>fer. Discount <strong>of</strong>f<br />
Standard Memberships are based on the current standard membership pricing available in club and do not include Concessionary or Off Peak Memberships. The Corporate Offer is only<br />
valid when there is a current agreement signed between Fitness First and your employer corporation. Offer valid from 1st February 2011 until 28th February 2012.<br />
† ‘Passport’ memberships exclude ‘Platinum’ clubs.
GPYR MDFT3059<br />
NOT ALL HOSPITALS HAVE WARDS.<br />
As a <strong>Nursing</strong> Officer in the Navy, Army or Air Force, you’ll have opportunities that you won’t get in the<br />
private sector. For instance, your patients will be your co-workers, as well as civilians on deployment.<br />
You will get the chance to lead a team <strong>of</strong> health pr<strong>of</strong>essionals and provide humanitarian aid. You’ll<br />
have the opportunity to further your career, specialise and progress into senior roles. Along with<br />
adventure, you’ll enjoy job security and excellent working conditions. You’ll also receive a favourable<br />
salary with subsidised accommodation and free medical & dental care. If you’re a Registered Nurse<br />
and would like further information call 13 19 01 or visit www.defencejobs.gov.au/graduate<br />
NURSING OFFICER<br />
IT’S NOT YOUR GENERAL PRACTICE<br />
NOW RECRUITING: NURSES.<br />
AG43032
InspIrIng,<br />
progressIng and<br />
promotIng the<br />
pr<strong>of</strong>essIon <strong>of</strong><br />
nursIng.<br />
Become an RCNA member, and<br />
contribute to influencing health policy in <strong>Australia</strong><br />
access resources for nurses<br />
receive advice and support<br />
apply for RCNA grants and awards<br />
receive RCNA publications.<br />
Your RCNA membership entitles you to receive discounts on<br />
Guild Pr<strong>of</strong>essional liabilities Insurance.<br />
To find out more visit guildinsurance.com.au/nurses or freecall 1800 810 213<br />
Employment Status<br />
Limit <strong>of</strong><br />
Indemnity<br />
NSW<br />
VIC/WA/<br />
ACT/NT<br />
QLD SA TAS<br />
Employed/Part time $10M $232.76 $242.00 $232.10 $244.20 $235.84<br />
Employed/Full time $10M $384.06 $399.30 $382.96 $402.92 $389.13<br />
Self Employed/Part time $10M $465.52 $484.00 $464.20 $488.40 $471.68<br />
Self Employed/Full time $10M $698.28 $726.00 $696.30 $732.60 $707.52<br />
*Price variations are in accordance with Government and Stamp Duty Fees as applicable in each State.<br />
Part time – Less than 20 hours per week<br />
Full time – 20 hours or more per week<br />
Join today!<br />
www.rcna.org.au<br />
RCNA <strong>Australia</strong>n<br />
member <strong>of</strong> ICN<br />
RCNA does not provide advice on whether insurance selected is appropriate or suitable for an RCNA member. RCNA<br />
members should rely on their own enquiries as to whether the insurances are appropriate or suitable for their needs.