overview of data collection elements - Nursing Home Help
overview of data collection elements - Nursing Home Help
overview of data collection elements - Nursing Home Help
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
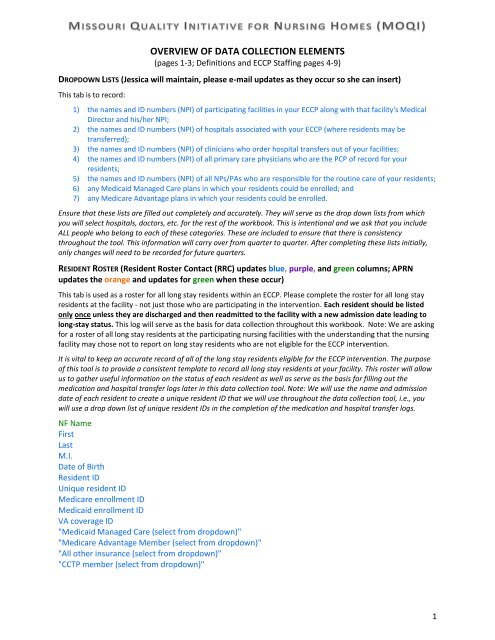
OVERVIEW OF DATA COLLECTION ELEMENTS<br />
(pages 1-3; Definitions and ECCP Staffing pages 4-9)<br />
DROPDOWN LISTS (Jessica will maintain, please e-mail updates as they occur so she can insert)<br />
This tab is to record:<br />
1) the names and ID numbers (NPI) <strong>of</strong> participating facilities in your ECCP along with that facility's Medical<br />
Director and his/her NPI;<br />
2) the names and ID numbers (NPI) <strong>of</strong> hospitals associated with your ECCP (where residents may be<br />
transferred);<br />
3) the names and ID numbers (NPI) <strong>of</strong> clinicians who order hospital transfers out <strong>of</strong> your facilities;<br />
4) the names and ID numbers (NPI) <strong>of</strong> all primary care physicians who are the PCP <strong>of</strong> record for your<br />
residents;<br />
5) the names and ID numbers (NPI) <strong>of</strong> all NPs/PAs who are responsible for the routine care <strong>of</strong> your residents;<br />
6) any Medicaid Managed Care plans in which your residents could be enrolled; and<br />
7) any Medicare Advantage plans in which your residents could be enrolled.<br />
Ensure that these lists are filled out completely and accurately. They will serve as the drop down lists from which<br />
you will select hospitals, doctors, etc. for the rest <strong>of</strong> the workbook. This is intentional and we ask that you include<br />
ALL people who belong to each <strong>of</strong> these categories. These are included to ensure that there is consistency<br />
throughout the tool. This information will carry over from quarter to quarter. After completing these lists initially,<br />
only changes will need to be recorded for future quarters.<br />
RESIDENT ROSTER (Resident Roster Contact (RRC) updates blue, purple, and green columns; APRN<br />
updates the orange and updates for green when these occur)<br />
This tab is used as a roster for all long stay residents within an ECCP. Please complete the roster for all long stay<br />
residents at the facility - not just those who are participating in the intervention. Each resident should be listed<br />
only once unless they are discharged and then readmitted to the facility with a new admission date leading to<br />
long-stay status. This log will serve as the basis for <strong>data</strong> <strong>collection</strong> throughout this workbook. Note: We are asking<br />
for a roster <strong>of</strong> all long stay residents at the participating nursing facilities with the understanding that the nursing<br />
facility may chose not to report on long stay residents who are not eligible for the ECCP intervention.<br />
It is vital to keep an accurate record <strong>of</strong> all <strong>of</strong> the long stay residents eligible for the ECCP intervention. The purpose<br />
<strong>of</strong> this tool is to provide a consistent template to record all long stay residents at your facility. This roster will allow<br />
us to gather useful information on the status <strong>of</strong> each resident as well as serve as the basis for filling out the<br />
medication and hospital transfer logs later in this <strong>data</strong> <strong>collection</strong> tool. Note: We will use the name and admission<br />
date <strong>of</strong> each resident to create a unique resident ID that we will use throughout the <strong>data</strong> <strong>collection</strong> tool, i.e., you<br />
will use a drop down list <strong>of</strong> unique resident IDs in the completion <strong>of</strong> the medication and hospital transfer logs.<br />
NF Name<br />
First<br />
Last<br />
M.I.<br />
Date <strong>of</strong> Birth<br />
Resident ID<br />
Unique resident ID<br />
Medicare enrollment ID<br />
Medicaid enrollment ID<br />
VA coverage ID<br />
"Medicaid Managed Care (select from dropdown)"<br />
"Medicare Advantage Member (select from dropdown)"<br />
"All other insurance (select from dropdown)"<br />
"CCTP member (select from dropdown)"<br />
1
NF admission date<br />
MDS Q0400A<br />
ECCP coverage date<br />
Opt-out date<br />
"Opt-out reason (select from dropdown)"<br />
NF permanent discharge date<br />
"NF permanent discharge reason (select from dropdown)"<br />
NF readmission date for beneficiaries readmitted within 30 days Hospice Election Date<br />
"Eligible for Intervention (select from dropdown)"<br />
PCP Name<br />
"NP/PA Name (select from dropdown)"<br />
Plan <strong>of</strong> Care (POC)<br />
Advance Directive (AD) Discussions<br />
Medication Management<br />
"Did the resident experience a hospital transfer during this quarter (select from dropdown)"<br />
"Did this resident experience a change <strong>of</strong> condition* during this quarter (select from dropdown)"<br />
Change <strong>of</strong> Condition<br />
"Does POC include documentation <strong>of</strong> resident/family preferences for care (select from dropdown)"<br />
Signed Advance Directive order date<br />
Date <strong>of</strong> last Advance Directive discussion<br />
"Types <strong>of</strong> Advance Directives documented (select from dropdown)"<br />
"Conducted by NF or ECCP staff (select from dropdown)"<br />
Medication Review #1<br />
Medication Review #2<br />
Medication Review #3<br />
Medication Review #4<br />
Change <strong>of</strong> Condition #1<br />
Change <strong>of</strong> Condition #2<br />
Change <strong>of</strong> Condition #3<br />
Change <strong>of</strong> Condition #4<br />
Date <strong>of</strong> medication review<br />
"Outcome <strong>of</strong> medication review (select from dropdown)"<br />
Date <strong>of</strong> change <strong>of</strong> condition<br />
"Which tools were used to assess and communicate a change <strong>of</strong> condition (select from dropdown)"<br />
"Did an MD or ECCP NP assess the resident (select from dropdown)"<br />
"Was a root cause analysis tool used (select from dropdown)"<br />
Identified root cause<br />
"What was the outcome (select from dropdown)"<br />
HOSPITALIZATION TRACKING (APRN updates all items as they occur, at least monthly)<br />
This tab is used as a log for each resident transfer from the nursing facility to a hospital. If a resident had multiple<br />
transfers during the reporting quarter, then enter the resident's ID with each transfer listed.<br />
This tab collects information for each instance your residents are transferred out <strong>of</strong> your facilities and into a<br />
hospital.<br />
2
Resident ID<br />
Transfer initiation information<br />
"Date <strong>of</strong> transfer to Hospital"<br />
"Day <strong>of</strong> transfer to Hospital"<br />
Transfer: approximate* time <strong>of</strong> day<br />
Hospital name<br />
"Entity who initially triggered (requested) transfer (select from dropdown)"<br />
Clinician ordering transfer<br />
"Primary nursing facility reasons for transfer: SYMPTOMS (select from dropdown)"<br />
"Secondary nursing facility reasons for transfer: SYMPTOMS (select from dropdown)"<br />
"Primary nursing facility reasons for transfer: DIAGNOSIS (select from dropdown)"<br />
"Secondary nursing facility reasons for transfer: DIAGNOSIS (select from dropdown)"<br />
Additional secondary symptoms or diagnoses contributing to decision to transfer (free text)<br />
"Was a structured communication tool sent to the hospital (select from dropdown)"<br />
Were the advanced directives reviewed at the time <strong>of</strong> transfer<br />
Were the advanced directives followed<br />
"Outcome <strong>of</strong> transfer (select from dropdown)"<br />
Transfer from hospital to nursing facility<br />
Hospital discharge date<br />
Length <strong>of</strong> stay<br />
Hospital primary discharge diagnosis (ICD-9 code)*<br />
Hospital secondary discharge diagnoses (ICD-9 code)*<br />
"Was a structured communication tool received from the hospital (select from dropdown)"<br />
Was the information received from the hospital adequate* to care for the resident during this<br />
transition<br />
Additional Information<br />
Additional comments about this transfer<br />
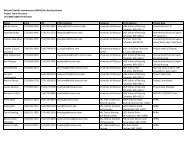
FACILITY TURNOVER (DON or designee such as HR) submit monthly with form to Jessica)<br />
This tab is used for tracking turnover among CNA, LVN/LPN, and RN nursing facility staff. These <strong>data</strong> are facilityspecific<br />
and should be completed for each nursing facility participating in the ECCP interventions. Please include all<br />
roles (e.g., RNs who fulfill clinical or administrative roles).<br />
The purpose <strong>of</strong> this tool is to gather <strong>data</strong> to track the stability <strong>of</strong> the nursing facility staff. We understand that<br />
these categories may not encompass all staff in the nursing facility.<br />
The MOQI team needs six numbers from your nursing home each month.<br />
1. Number <strong>of</strong> CNA staff employed on the First Day <strong>of</strong> Each Month<br />
2. Number <strong>of</strong> CNA Terminated by the Last Day <strong>of</strong> Each Month<br />
3. Number <strong>of</strong> LPN staff employed on the First Day <strong>of</strong> Each Month<br />
4. Number <strong>of</strong> LPN Terminated by the Last Day <strong>of</strong> Each Month<br />
5. Number <strong>of</strong> RN staff employed on the First Day <strong>of</strong> Each Month<br />
6. Number <strong>of</strong> RN Terminated by the Last Day <strong>of</strong> Each Month<br />
Below are Q&As from CMS that should help you or your delegated staff to complete the task.<br />
Q: Do I include nurses who perform administrative roles<br />
A: Include nurses who perform direct care and those who fulfill clinical or administrative roles.<br />
3
Q: What is a termination<br />
A: An employee departure, either due to firing or quitting, whereby the employee receives a final<br />
paycheck.<br />
Q: Do part-time or per diem staff termination count equally as a full-time staff termination<br />
A: Yes, the calculation is measuring turnover <strong>of</strong> all nursing staff regardless <strong>of</strong> individual employment<br />
status.<br />
Q: What about a member <strong>of</strong> the nursing staff who changes his/her job title and stays in the<br />
organization; does this count as a termination if the employee is still a member <strong>of</strong> the nursing staff<br />
A: No. Do not count this individual as a termination.<br />
Q: What about a member <strong>of</strong> the nursing staff who changes his/her job title and stays in the<br />
organization; does this count as a termination if the employee leaves the nursing staff<br />
A: No. Do not count this individual as a termination.<br />
Q: What if a nursing staff member works at two facilities owned by the same corporation and leaves<br />
one <strong>of</strong> the facilities, but stays at the other<br />
A: The staff member would be coded as a termination by the facility from which he/she departed.<br />
Q: What if a nursing staff employee leaves via a termination, but then is re-hired 3 weeks later<br />
A: He/she would count as a termination.<br />
Q: If a home has 30 budgeted staff positions, but only 25 <strong>of</strong> the positions are filled, is the number <strong>of</strong><br />
staff 30 or 25<br />
A: The number <strong>of</strong> positions is 25.<br />
Q: What about agency staff Do they count in any <strong>of</strong> the calculations<br />
A: No. Agency staff are not employed by the nursing home and therefore are not included.<br />
RESIDENT ROSTER DEFINITIONS<br />
The purpose <strong>of</strong> the <strong>Nursing</strong> Facility Long-Stay Resident Roster is to capture information on ALL long-stay<br />
residents in the nursing facility during the quarter covered by the report. The requested <strong>data</strong> <strong>elements</strong><br />
are defined in this tab.<br />
These definitions should explain all <strong>of</strong> the requested <strong>data</strong> <strong>elements</strong> in the Beneficiary Roster in sufficient<br />
detail. As mentioned above, technical assistance and additional clarification will be given by the<br />
Operations Support Contractor during <strong>of</strong>fice hours.<br />
<strong>Nursing</strong> Facility Name: The name under which the nursing facility does business.<br />
<strong>Nursing</strong> Facility Number: The facility's Medicare Provider Number (AUTOMATICALLY GENERATED).<br />
Resident Name: First, Last and Middle Initial – Enter the First and Last name and Middle Initial for the<br />
long-stay resident as shown on their Medicare, Medicaid or VA account or legal name <strong>of</strong> a resident who<br />
is covered by LTC insurance or is uninsured.<br />
Date <strong>of</strong> Birth: Date on which the resident was born (MM/DD/YY).<br />
Resident ID: The identification number assigned by the nursing facility to the resident while she/he is in<br />
the nursing facility.<br />
Unique Resident ID: This Unique Resident ID will be AUTOMATICALLY GENERATED by this tool and is<br />
based on the resident's name and date <strong>of</strong> admission. It will generate a drop-down list in other resident-<br />
4
level tabs. This ID will be consistently assigned to the resident throughout the course <strong>of</strong> his/her stay in<br />
the facility. This ID is being created for purpose <strong>of</strong> consistency within this <strong>data</strong> <strong>collection</strong> workbook.<br />
Medicare Enrollment ID: Enter the ID for a resident eligible/enrolled in Medicare A and/or B at any time<br />
during the reporting quarter.<br />
Medicaid Enrollment ID: Enter the ID for a resident eligible/enrolled in Medicaid at any time during the<br />
reporting quarter.<br />
VA Coverage ID: Enter the ID for a resident for whom the primary payer is the Veterans Administration<br />
regardless <strong>of</strong> their eligibility for either Medicare and/or Medicaid. (Long stay residents whose care is<br />
paid for by the VA ARE eligible for the intervention.)<br />
Medicaid Managed Care Member: Enter the name <strong>of</strong> the Medicaid managed care plan in which the<br />
resident is enrolled. If not applicable, enter "None". (Medicaid managed care enrollees ARE eligible for<br />
the intervention.)<br />
Medicare Advantage Plan Member: Enter the name <strong>of</strong> the plan if the resident is enrolled in a Medicare<br />
Advantage Plan, including Special Needs Plans, and PACE. (Medicare Advantage enrollees ARE NOT<br />
eligible for the intervention.)<br />
All Other Insurance: Enter the status, long-term care insurance or uninsured, for any resident who is<br />
NOT eligible/enrolled in Medicare (A and/or B) or Medicaid or whose care is paid for by the VA.<br />
(Residents who are not eligible/enrolled in Medicare, Medicaid or their nursing facility stay is not paid<br />
for by the VA are NOT eligible for the intervention.)<br />
CCTP Member: Enter Yes if the resident is enrolled in CMS’ Community-based Care Transitions Program<br />
(CCTP) during the reporting quarter. CCTP test models for improving care transitions from the hospital<br />
to other settings and reducing readmissions for high-risk Medicare beneficiaries.<br />
FACILITY-BASED RESIDENT INFORMATION DEFINITIONS<br />
NF Admission Date: Enter the date the resident was admitted to the nursing facility (e.g., on a Medicare<br />
Part A benefit, on a Medicaid covered stay) for use in qualifying the resident as long-stay. This is the<br />
date <strong>of</strong> the admission that led to the resident becoming long-stay. Examples follow.<br />
a) Mary Smith was first admitted to the nursing facility 06/02/2012, she was transferred to a<br />
hospital on 12/15/2012 and was readmitted to the same nursing facility January 1, 2013. The<br />
NF Admission Date used should be 06/02/2012 as this is the admission that lead to Ms. Smith<br />
becoming a long-stay resident. She would be eligible for the ECCP’s intervention starting<br />
2/1/2013 as she has remained in the facility for greater than 100 days (101st day was<br />
9/11/2012).<br />
b) Mr. Berry was admitted to the nursing facility on 02/01/2012 from the hospital for post-acute<br />
rehab. He was then discharged from the nursing facility on 03/01/2012 back to his home in the<br />
community. After another hospitalization, Mr. Berry was admitted to the nursing facility on<br />
07/01/2012 and has continued to reside in the facility. The NF Admission Date used should be<br />
07/01/2012 as this is the admission that lead to Mr. Berry becoming a long-stay resident. He<br />
would be eligible for the ECCP’s intervention starting 2/1/2013 as he has remained in the facility<br />
for greater than 100 days (101st day was 10/10/2012).<br />
c) Ms. Jones was admitted to the nursing facility on 12/15/2012. He was transferred to the<br />
hospital on 1/5/2013 and returned to the same nursing facility on 1/12/2013. On 2/3/2013 the<br />
facility marked MDS section Q 0400A “0” (no active discharge plan). The NF Admission Date<br />
used should be 12/15/2012 and Ms. Jones is eligible for the ECCP intervention starting 2/3/2013<br />
as the MDS indicated he had no active discharge plan as <strong>of</strong> this date.<br />
5
MDS Q0400A: Enter the answer as reported on MDS Questions 0400 A.<br />
ECCP Coverage Date: Enter the date that the resident began to be covered by the ECCP intervention.<br />
Opt-out Date: Enter the date that the resident chose not be part <strong>of</strong> the ECCP intervention.<br />
Opt-out Reason: Enter the reason the resident/resident’s representative chose not to participate in the<br />
ECCP intervention.<br />
NF Permanent Discharge Date: Enter the date that the resident was permanently discharged from the<br />
nursing facility. (Any resident returning to the community for more than 30 days is to be removed from<br />
the intervention. Should s/he return to the nursing facility after more than 30 days, s/he will have to<br />
meet the eligibility requirements anew before being covered by the intervention.)<br />
NF Permanent Discharge Reason: Enter the reason for the resident being permanently discharged from<br />
the nursing facility.<br />
NF Readmission Date for Beneficiaries Readmitted within 30 days: Enter the readmission date for a<br />
resident who was discharged to the community and returned to the facility within 30 days. (These<br />
individuals WILL CONTINUE to be eligible for the ECCP intervention.)<br />
Hospice Election Date: Enter the date that a resident chose to receive hospice care IN THE NURSING<br />
FACILITY.<br />
Eligible: Enter Yes or No based on your determination that the resident is eligible to participate in the<br />
intervention based on CMS’ eligibility criteria.<br />
ELIGIBILITY CRITERIA FOR THE INTERVENTION<br />
Residents ARE eligible for the intervention if they:<br />
• Enrolled in Medicare A and/or B and/or Medicaid or their nursing facility stay is paid for by the<br />
VA and<br />
• Have resided in the nursing facility for 101 or more days (including the day <strong>of</strong> admission) or<br />
• Are identified on the Minimum Data Set assessment Section Q 0400A ("0" - No Active Discharge<br />
Plan)<br />
Residents ARE NOT eligible for the intervention if they meet any <strong>of</strong> the following criteria:<br />
• Have not resided in the facility for 101 or more days and do not have an answer <strong>of</strong> "0" for MDS<br />
Section Q 0400A<br />
• Are enrolled in a Medicare Managed Care Plan<br />
• Are not eligible/enrolled in Medicare, Medicaid or their nursing facility stay is not paid for by the<br />
VA<br />
Residents’ eligibility must be re-determined anew if they:<br />
• Return to the community for more than 30 days<br />
6
ADVANCE DIRECTIVES DISCUSSION DEFINITIONS<br />
Signed Directive order date: Date that any Advance Directives were signed. If none were signed, then<br />
leave this blank.<br />
Date <strong>of</strong> most recent Advance Directive discussion: Date <strong>of</strong> most recent Advance Directive discussion. If<br />
no discussion has been had, then leave this blank.<br />
Conducted by ECCP or NF staff: Select whether this discussion was conducted by a staff person from<br />
the nursing facility or from the ECCP.<br />
Advance Directive documentation: Select whether there is no signed advance directives, signed DNR,<br />
signed DNH, signed DNI, no enteral feeding, or signed full treatment (signed full code).<br />
PCP OF RECORD DEFINITIONS<br />
PCP First Name and National Provider Identification Number: Select the name and the CMS National<br />
Provider Identification Number for the physician <strong>of</strong> record or primary care provider and who provides<br />
routine care (e.g., visits) for the resident. This category does NOT include the ECCP's staff.<br />
ROUTINE CARE NP/PA DEFINITIONS<br />
NP/PA First Name and National Provider Identification Number: Select the name and the CMS National<br />
Provider Identification Number for nurse practitioner (NP) or physician's assistant (PA) who provides<br />
routine care (e.g., visits) for the resident. This category does NOT include the ECCP's staff.<br />
CARE COORDINATION DEFINITIONS<br />
Does POC include documentation <strong>of</strong> resident/family preferences for care: Enter Yes or No.<br />
Signed Advance Directive (AD) order date: Enter the date that the current AD documents were signed.<br />
Date <strong>of</strong> last Advance Directive Discussion: Enter the date that the most recent AD discussion took place.<br />
Advance Directives documentation: Select which AD documents were signed. Note that resident<br />
information must be filled out for the selection box to appear.<br />
Conducted by NF or ECCP staff: Was the AD discussion conducted by NF or ECCP staff<br />
Did this resident experience a change <strong>of</strong> condition during this quarter: Enter Yes or No.<br />
Date <strong>of</strong> change <strong>of</strong> condition: Enter the date the change <strong>of</strong> condition occurred.<br />
Which Interact tools (or equivalent) were used: Enter which Interact tools were used, if any. If AMDA<br />
or other equivalent tools were used, enter "other".<br />
Did an MD or ECCP NP assess the resident: Enter Yes or No.<br />
Was a root cause analysis tool used: Enter Yes or No.<br />
Identified root cause: What was the result <strong>of</strong> the root cause analysis If no tool was used, leave blank.<br />
7
FOR ECCP USE ONLY<br />
ECCP Staffing<br />
This tab is used for tracking ECCP staffing levels. It is useful for seeing what type <strong>of</strong> employees/skills the<br />
ECCP is using to implement its intervention. These job types may include: NP Lead, Dental Hygienist,<br />
Dentist, Pharmacy Technician, IT Specialist, HIT Lead, NP, RN, APRN, Care Pathways Coach, Care<br />
Transitions Coach, INTERACT Specialist, Social Worker, Physician Extender, Medical Director, and<br />
Pharmacy Consultant/Pharmacy Faculty Coach. There may also be administrative/support staff<br />
including: Project Coordinator, Financial and Data Analyst, Administrative Assistant,<br />
Intervention/Practice Expert, Care Transitions Lead, and QI Specialist. Additionally, this template<br />
provides a structured tool to track how these ECCP staff spend their time and at which participating<br />
nursing facilities they are working. Note that this tab is for the ECCP itself, and is not facility-dependent<br />
or specific.<br />
Fill these out based on your experience over each month <strong>of</strong> the reporting quarter. We realize that<br />
staffing levels change and time spent engaging in different activities do as well--please use your best<br />
judgment to determine these percentages.<br />
ECCP Employee Name<br />
ECCP Employee Role<br />
NPI or Alternate ID<br />
Hours per week at facilities<br />
Current resident caseload<br />
% <strong>of</strong> time providing direct care<br />
% <strong>of</strong> time providing education<br />
% <strong>of</strong> time engaging in communication<br />
% <strong>of</strong> time engaged in activities related to advanced care planning and/or advance directives<br />
% <strong>of</strong> time performing administrative tasks<br />
Scheduled hours spent in the facilities (Days)<br />
8