Full Provider Guide in PDF - Geisinger Health Plan
Full Provider Guide in PDF - Geisinger Health Plan
Full Provider Guide in PDF - Geisinger Health Plan
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
WVUHS TPA<br />
January 2012<br />
1
Geis<strong>in</strong>ger <strong>Health</strong> Options<br />
West Virg<strong>in</strong>ia United <strong>Health</strong> System TPA<br />
Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong><br />
January 2012<br />
This Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> (<strong>Guide</strong>) is <strong>in</strong>corporated by reference to the Agreement. The <strong>Guide</strong> is<br />
specific to West Virg<strong>in</strong>ia United <strong>Health</strong> System’s Third-Party Adm<strong>in</strong>istrator (TPA) health plan. The<br />
<strong>Guide</strong> is designed for use by, and applicable to, all Participat<strong>in</strong>g West Virg<strong>in</strong>ia United <strong>Health</strong> System<br />
<strong>Provider</strong>s, exclud<strong>in</strong>g Pharmacy <strong>Provider</strong>s, who <strong>in</strong> accordance with the terms and conditions set forth <strong>in</strong><br />
their respective Agreements, provide Covered Services or supplies to Members.<br />
West Virg<strong>in</strong>ia United <strong>Health</strong> System TPA services are adm<strong>in</strong>istered through Geis<strong>in</strong>ger <strong>Health</strong> Options, a<br />
subsidiary of Geis<strong>in</strong>ger Indemnity Insurance Company.<br />
For purposes of the Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong>:<br />
<br />
<br />
West Virg<strong>in</strong>ia United <strong>Health</strong> System shall be referred to as “WVUHS”<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options shall be referred to as “GHO”<br />
Please contact your designated <strong>Provider</strong> Relations Representative if you have questions concern<strong>in</strong>g the<br />
<strong>in</strong>formation with<strong>in</strong> this <strong>Guide</strong>.<br />
This <strong>Guide</strong> and the content conta<strong>in</strong>ed here<strong>in</strong> is the confidential and proprietary property of Geis<strong>in</strong>ger <strong>Health</strong><br />
Options. Any unauthorized use, replication, <strong>in</strong>fr<strong>in</strong>gement, or other form of dissem<strong>in</strong>ation of the <strong>in</strong>formation<br />
conta<strong>in</strong>ed here<strong>in</strong> is strictly prohibited and occurrence of such may result <strong>in</strong> legal action.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Introduction and Table of Contents 2
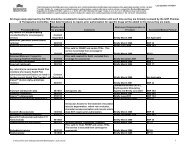
SECTION 1: GENERAL INFORMATION..............................................................................................6<br />
Geis<strong>in</strong>ger Insurance Services .........................................................................................................................7<br />
Copayment, Co<strong>in</strong>surance and Deductibles ....................................................................................................7<br />
Membership Identification.............................................................................................................................7<br />
GHO Responsibilities ....................................................................................................................................8<br />
Protected <strong>Health</strong> Information.......................................................................................................................10<br />
Population Management Programs ..............................................................................................................10<br />
Preventive <strong>Health</strong> Program ..........................................................................................................................15<br />
Departments Available for Assistance.........................................................................................................16<br />
Case Management Department ................................................................................................................16<br />
Customer Service Teams .........................................................................................................................16<br />
Medical Directors and Quality Improvement (Q.I.) Nurses ....................................................................17<br />
Medical Director and Q.I. Nurse..............................................................................................................17<br />
<strong>Provider</strong> Network Management ...............................................................................................................18<br />
Pharmacy Department..............................................................................................................................18<br />
Tel-A-Nurse .............................................................................................................................................19<br />
Medical Management Department...........................................................................................................19<br />
GHO Web Site Information .........................................................................................................................20<br />
Interactive Voice Response (IVR) System ..................................................................................................23<br />
SECTION 2: PRECERTIFICATION REQUIREMENTS....................................................................25<br />
Precertification Requirements......................................................................................................................25<br />
Verification of Eligibility and Benefit Limit ...........................................................................................27<br />
Request<strong>in</strong>g Precertification ......................................................................................................................27<br />
1) Inpatient Hospitalization......................................................................................................................27<br />
2) Skilled Level of Care Admissions .......................................................................................................29<br />
3) Home <strong>Health</strong>/Hospice, Home Infusion and Home Phlebotomy Services ...........................................31<br />
4) Durable Medical Equipment (“DME”)................................................................................................34<br />
5) Outpatient Physical, Occupational and Speech Therapy Services ......................................................34<br />
6) Other Services Requir<strong>in</strong>g Precertification ...........................................................................................35<br />
7) Pharmacy WVUHS Formulary Precertification and non-WVUHS Formulary Exception Process ....36<br />
8) Specialty Drug List and Preferred Specialty Pharmacy.......................................................................38<br />
Services Requir<strong>in</strong>g <strong>Provider</strong> Coord<strong>in</strong>ation ..................................................................................................39<br />
Outpatient Prescription Drugs..................................................................................................................39<br />
Outpatient Laboratory Services................................................................................................................40<br />
Urgent/Emergency Services.....................................................................................................................41<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Introduction and Table of Contents 3
Orthotic and Prosthetic Service................................................................................................................41<br />
Behavioral <strong>Health</strong> and Substance Abuse Services...................................................................................42<br />
Outpatient Dialysis Services ....................................................................................................................42<br />
Experimental/Investigational or Unproven Services ...............................................................................42<br />
Transplant Services ..................................................................................................................................43<br />
Preventive Services ..................................................................................................................................43<br />
SECTION 3: REIMBURSEMENT AND CLAIM SUBMISSION.......................................................45<br />
GHO Reimbursement...................................................................................................................................46<br />
Payment Schedules ..................................................................................................................................46<br />
Copayments/Co<strong>in</strong>surance and Deductibles..............................................................................................46<br />
Claim Submission ....................................................................................................................................47<br />
GHO Explanation of Payment (EOP) ......................................................................................................47<br />
Electronic Claim Submission...................................................................................................................47<br />
EDI Clear<strong>in</strong>ghouse Reports .....................................................................................................................48<br />
Claim Report<strong>in</strong>g Requirements or <strong>Guide</strong>l<strong>in</strong>es .........................................................................................48<br />
For Professional <strong>Provider</strong>s ...........................................................................................................................49<br />
For Ancillary/Facility <strong>Provider</strong>s ..................................................................................................................56<br />
<strong>Health</strong> Insurance Prospective Payment System (HIPPS) Codes Report<strong>in</strong>g Requirement.......................59<br />
Outpatient Hospital Revenue Code Report<strong>in</strong>g Requirements..................................................................59<br />
SECTION 4: MEMBER & PARTICIPATING PROVIDER RIGHTS & RESPONSIBILITIES ...65<br />
TPA Member Rights and Responsibilities...................................................................................................67<br />
Participat<strong>in</strong>g <strong>Provider</strong> Adm<strong>in</strong>istrative Rights ..............................................................................................67<br />
Participat<strong>in</strong>g <strong>Provider</strong> Medical Management Denial Review Procedure ................................................67<br />
Participat<strong>in</strong>g <strong>Provider</strong> Responsibilities........................................................................................................67<br />
Time Limits..............................................................................................................................................67<br />
Non-eligible Claims .................................................................................................................................67<br />
Proper Process<strong>in</strong>g.....................................................................................................................................68<br />
Non-Covered Services .............................................................................................................................68<br />
Penalty for Late Payment.........................................................................................................................68<br />
Coord<strong>in</strong>ation of Benefits..........................................................................................................................68<br />
Third Party Payments...............................................................................................................................68<br />
<strong>Provider</strong> List.............................................................................................................................................69<br />
Audit.........................................................................................................................................................69<br />
Advance Directives ..................................................................................................................................69<br />
Compliance with Grievance, Compla<strong>in</strong>t and Appeal Procedures............................................................69<br />
Participat<strong>in</strong>g <strong>Provider</strong> Locations..............................................................................................................69<br />
Establishment of a Confidentiality Policy ...............................................................................................70<br />
Copy<strong>in</strong>g of Member Medical Records-F<strong>in</strong>ancial Responsibility ............................................................70<br />
Hospitalization .........................................................................................................................................70<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Introduction and Table of Contents 4
Missed Appo<strong>in</strong>tments by Members .........................................................................................................70<br />
Term<strong>in</strong>ation of Physician/Member Relationship .....................................................................................70<br />
Network Access/Reciprocity....................................................................................................................71<br />
Advertis<strong>in</strong>g <strong>Guide</strong>l<strong>in</strong>es.............................................................................................................................71<br />
Coverage dur<strong>in</strong>g PCP/SCP Absence........................................................................................................73<br />
PCP Practice Acceptance Status Member Limitations ............................................................................73<br />
M<strong>in</strong>imum Standards for Medical Record Documentation.......................................................................73<br />
Laboratory Results ...................................................................................................................................76<br />
General Provisions: ..................................................................................................................................78<br />
GHO Compliance Program......................................................................................................................80<br />
SECTION 5: MEDICAL MANAGEMENT AND QUALITY IMPROVEMENT AND<br />
ACCREDITATION ...................................................................................................................................84<br />
Medical Management <strong>Plan</strong>...........................................................................................................................85<br />
Philosophy................................................................................................................................................85<br />
Mission.....................................................................................................................................................85<br />
Goals ........................................................................................................................................................85<br />
Authority ..................................................................................................................................................86<br />
Structure ...................................................................................................................................................86<br />
Scope........................................................................................................................................................92<br />
Quality Improvement <strong>Plan</strong> .........................................................................................................................103<br />
Purpose...................................................................................................................................................103<br />
Goals and Objectives .............................................................................................................................103<br />
Scope of Program...................................................................................................................................106<br />
Cl<strong>in</strong>ical Programs...................................................................................................................................106<br />
Service Initiatives...................................................................................................................................108<br />
Coord<strong>in</strong>ated Activities ...........................................................................................................................109<br />
QI Program Structure .............................................................................................................................109<br />
Quality Improvement and Accreditation Personnel...............................................................................113<br />
Delegated Activities...............................................................................................................................116<br />
SECTION 6: GLOSSARY AND ACRONYMS ...................................................................................117<br />
Glossary .....................................................................................................................................................118<br />
Acronyms ...................................................................................................................................................127<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Introduction and Table of Contents 5
Section 1: General Information<br />
GEISINGER INSURANCE SERVICES ...................................................................................................7<br />
COPAYMENT, COINSURANCE AND DEDUCTIBLES ......................................................................7<br />
MEMBERSHIP IDENTIFICATION.........................................................................................................7<br />
GHO RESPONSIBILITIES........................................................................................................................8<br />
PROTECTED HEALTH INFORMATION............................................................................................10<br />
POPULATION MANAGEMENT PROGRAMS ...................................................................................10<br />
PREVENTIVE HEALTH PROGRAM ...................................................................................................15<br />
DEPARTMENTS AVAILABLE FOR ASSISTANCE ..........................................................................16<br />
Case Management Department..................................................................................................... 16<br />
Customer Service Teams .............................................................................................................. 16<br />
Medical Directors and Quality Improvement (Q.I.) Nurses ......................................................... 17<br />
Medical Director and Q.I. Nurse................................................................................................... 17<br />
<strong>Provider</strong> Network Management.................................................................................................... 18<br />
Pharmacy Department................................................................................................................... 18<br />
Tel-A-Nurse .................................................................................................................................. 19<br />
Medical Management Department................................................................................................ 19<br />
GHO WEB SITE INFORMATION.........................................................................................................20<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
6
Geis<strong>in</strong>ger Insurance Services<br />
Insurance services are provided through three Geis<strong>in</strong>ger affiliates. Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> (GHP)<br />
was first offered to the public <strong>in</strong> 1985, provid<strong>in</strong>g fully <strong>in</strong>sured <strong>Health</strong> Ma<strong>in</strong>tenance Organization<br />
(HMO) coverage. It is a non-profit HMO with 501(C) (4) status, licensed by the Pennsylvania<br />
Insurance Department. Geis<strong>in</strong>ger Gold, a Medicare Advantage plan, is also offered through<br />
GHP.<br />
Geis<strong>in</strong>ger Indemnity Insurance Company is a for-profit entity created <strong>in</strong> 1994 to provide<br />
third-party adm<strong>in</strong>istrator (TPA) services via Geis<strong>in</strong>ger <strong>Health</strong> Options (GHO).<br />
The newest affiliate, Geis<strong>in</strong>ger Quality Options, Inc. is a for-profit risk-assum<strong>in</strong>g non-licensed<br />
PPO. Geis<strong>in</strong>ger Choice, a commercial PPO, is offered through this affiliate.<br />
Copayment, Co<strong>in</strong>surance and Deductibles<br />
A Member’s f<strong>in</strong>ancial liability for certa<strong>in</strong> Covered Services may be determ<strong>in</strong>ed by review<strong>in</strong>g the<br />
front of a Member’s Identification Card. You may also register for the onl<strong>in</strong>e <strong>Provider</strong> Service<br />
Center at www.thehealthplan.com/wvuh_providers_us/ to view a Member’s detailed eligibility<br />
and benefit <strong>in</strong>formation. When a Member’s benefit structure denotes f<strong>in</strong>ancial liability <strong>in</strong> the<br />
form of a Copayment, such liability typically applies to evaluation and management services<br />
performed <strong>in</strong> the follow<strong>in</strong>g sett<strong>in</strong>g: office, consultation, preventive medic<strong>in</strong>e and emergency<br />
department. Additionally, certa<strong>in</strong> Members may have a per day or per visit Copayment<br />
responsibility for certa<strong>in</strong> services such as; outpatient rehabilitative services, outpatient radiology<br />
tests, home health services, ambulance services and outpatient surgery.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s should access the <strong>Provider</strong> Service Center at<br />
www.thehealthplan.com/wvuh_providers_us/ and review a Member’s benefit document or<br />
GHO’s onl<strong>in</strong>e Explanation of Payment (EOP) to appropriately determ<strong>in</strong>e a Member’s f<strong>in</strong>ancial<br />
liability.<br />
Membership Identification<br />
Each Member is issued an Identification Card as well as a unique identification number at the<br />
time of enrollment. The identification number appears <strong>in</strong> the left mid-section of the front of the<br />
Identification Card and should be readily available when contact<strong>in</strong>g the Customer Service Team<br />
with questions specific to Members’ benefits. Common Member Copayment/Co<strong>in</strong>surance<br />
<strong>in</strong>formation is also displayed on the front of the Identification Card. The reverse side of the<br />
Identification Card should be reviewed for additional <strong>in</strong>formation.<br />
Employers, Groups or Members may enroll or disenroll from GHO throughout the calendar year.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s can access the <strong>Provider</strong> Service Center at<br />
www.thehealthplan.com/wvuh_providers_us/ to confirm a Member’s eligibility onl<strong>in</strong>e. Members<br />
are <strong>in</strong>structed to present their Identification Card whenever they seek medical care. A newly<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
7
enrolled Member should present a copy of their enrollment form as verification of enrollment<br />
until their Identification Card is received.<br />
The Customer Service Team is available for enrollment confirmation, Member benefit<br />
<strong>in</strong>formation, and claims questions.<br />
GHO’s IVR (Interactive Voice Response) system is available for provider use, 24 hours a day, 7<br />
days a week. Our Customer Service Representatives are available to assist you dur<strong>in</strong>g normal<br />
bus<strong>in</strong>ess hours.<br />
GHO CUSTOMER SERVICE: (866) 580-3531<br />
GHO Responsibilities<br />
GHO will:<br />
Adjudicate and pay Clean Claims with<strong>in</strong> thirty (30) days of receipt of a Clean Claim<br />
submitted electronically and forty (40) days of receipt of a Clean Claim for all other<br />
claims.<br />
Orient Participat<strong>in</strong>g <strong>Provider</strong>s to GHO policies and procedures.<br />
Provide ongo<strong>in</strong>g communication about any changes to GHO policies and procedures and<br />
other operational issues that will affect the provision of services to Members<br />
Provide adm<strong>in</strong>istrative services to Members <strong>in</strong>clud<strong>in</strong>g, but not limited to, communicat<strong>in</strong>g<br />
GHO policies; distribut<strong>in</strong>g Identification Cards, Member handbooks, and a list<strong>in</strong>g of<br />
Participat<strong>in</strong>g <strong>Provider</strong>s.<br />
Market its various product l<strong>in</strong>es to diverse purchasers of health care, <strong>in</strong>clud<strong>in</strong>g employer<br />
Groups, Governmental Agencies, Medicare beneficiaries and <strong>in</strong>dividuals.<br />
Provide assistance to membership through the Customer Service Teams or Tel-A-Nurse<br />
Service.<br />
Assure availability and accessibility of adequate Participat<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong>s <strong>in</strong> a<br />
timely manner, enabl<strong>in</strong>g applicable Members to have access to quality care and cont<strong>in</strong>uity<br />
of health services.<br />
Consult with Participat<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong>s <strong>in</strong> active cl<strong>in</strong>ical practice regard<strong>in</strong>g<br />
professional qualifications and if additional <strong>Health</strong> Care <strong>Provider</strong>s need to be <strong>in</strong>cluded <strong>in</strong><br />
the Network.<br />
Ensure that Members have the right to access Emergency Services twenty-four (24) hours<br />
a day, seven (7) days a week and provide reasonable payment or reimbursement for<br />
Emergency Services.<br />
Ensure <strong>Health</strong> Care Services, when Medically Necessary, are available twenty-four (24)<br />
hours a day, seven (7) days a week.<br />
Ensure that there are Participat<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong>s who are physically accessible to<br />
people with disabilities and can communicate with Members with sensory disabilities <strong>in</strong><br />
accordance with Title III of the Americans with Disabilities Act of 1990.<br />
Not penalize or restrict a Participat<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong> from discuss<strong>in</strong>g:<br />
a) The process that GHO or any <strong>in</strong>dividual, partnership or entity contract<strong>in</strong>g with<br />
GHO uses or proposes to use to deny payment for a Covered Service; and<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
8
) Medically Necessary and appropriate care with or on behalf of a Member,<br />
<strong>in</strong>clud<strong>in</strong>g <strong>in</strong>formation regard<strong>in</strong>g the nature of treatment; risks of treatment;<br />
alternative treatments; or the availability of alternate therapies, consultation or<br />
tests; and<br />
c) The decision of GHO to deny payment for a Covered Service.<br />
Not use any f<strong>in</strong>ancial <strong>in</strong>centives that compensate a Participat<strong>in</strong>g <strong>Provider</strong> for provid<strong>in</strong>g<br />
less than Medically Necessary and appropriate care to a Member.<br />
Ensure that a Member’s Protected <strong>Health</strong> Information (PHI) is adequately protected and<br />
rema<strong>in</strong>s confidential <strong>in</strong> compliance with all applicable federal and state laws and<br />
regulations and professional ethical standards.<br />
Not exclude, discrim<strong>in</strong>ate aga<strong>in</strong>st or penalize any Participat<strong>in</strong>g <strong>Provider</strong> for their refusal to<br />
allow, perform, participate <strong>in</strong> or refer for <strong>Health</strong> Care Services, when the refusal of the<br />
Participat<strong>in</strong>g <strong>Provider</strong> or GHO is based on moral or religious grounds.<br />
Not be responsible for Covered Services provided to a Member follow<strong>in</strong>g the date of<br />
term<strong>in</strong>ation of the Agreement with a Participat<strong>in</strong>g <strong>Provider</strong> when the Participat<strong>in</strong>g <strong>Provider</strong><br />
has been term<strong>in</strong>ated for cause, <strong>in</strong>clud<strong>in</strong>g breach of contract, fraud, crim<strong>in</strong>al activity or<br />
pos<strong>in</strong>g a danger to a Member, or the health, safety or welfare of the public as determ<strong>in</strong>ed<br />
by GHO.<br />
Ma<strong>in</strong>ta<strong>in</strong> policies and procedures that allow for <strong>in</strong>dividual Medical Necessity<br />
determ<strong>in</strong>ations.<br />
Allow the Participat<strong>in</strong>g <strong>Provider</strong> to consider a Member’s <strong>in</strong>put <strong>in</strong>to the Participat<strong>in</strong>g<br />
<strong>Provider</strong>’s proposed treatment plan, irrespective of coverage; potential and known side<br />
effects of treatment and planned/proposed management of symptoms. Examples may<br />
<strong>in</strong>clude: a) education of Members regard<strong>in</strong>g their health care needs and b) shar<strong>in</strong>g f<strong>in</strong>d<strong>in</strong>gs<br />
of history and physical exam<strong>in</strong>ations.<br />
Ensure that <strong>Health</strong> Care Services are provided <strong>in</strong> a culturally competent manner to all<br />
Members, <strong>in</strong>clud<strong>in</strong>g those with limited English proficiency or read<strong>in</strong>g skills, diverse<br />
cultural and ethnic backgrounds, and physical or mental disabilities.<br />
Ensure that Participat<strong>in</strong>g <strong>Provider</strong>s who ma<strong>in</strong>ta<strong>in</strong> a current drug enforcement agency<br />
(DEA) certificate shall receive a WVUHS Formulary, which <strong>in</strong>cludes procedures that<br />
describe the process to be used to obta<strong>in</strong> coverage of a drug that is an exception to the<br />
WVUHS Formulary.<br />
In the event GHO suspends or term<strong>in</strong>ates the Agreement between GHO and a Participat<strong>in</strong>g<br />
<strong>Provider</strong> physician, GHO will provide suspended or term<strong>in</strong>ated Participat<strong>in</strong>g <strong>Provider</strong><br />
physician written notice of the follow<strong>in</strong>g: (i) the reasons for the action, <strong>in</strong>clud<strong>in</strong>g, if<br />
relevant, the standards and profil<strong>in</strong>g data used by GHO to evaluate the Participat<strong>in</strong>g<br />
<strong>Provider</strong> physician and the numbers and mix of such physicians needed by GHO, and (ii)<br />
the affected physician’s right to appeal the action, process, and timel<strong>in</strong>e for request<strong>in</strong>g a<br />
hear<strong>in</strong>g. Participat<strong>in</strong>g <strong>Provider</strong>s that are excluded from participat<strong>in</strong>g <strong>in</strong> the Medicare<br />
program shall not be afforded the opportunity to appeal a suspension or term<strong>in</strong>ation action<br />
by GHO.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
9
Protected <strong>Health</strong> Information<br />
GHO will ensure that Members and Participat<strong>in</strong>g <strong>Provider</strong>s receive communication that <strong>in</strong>forms<br />
them of GHO policies and procedures regard<strong>in</strong>g the collection, use and disclosure of Members’<br />
Protected <strong>Health</strong> Information. Communication will <strong>in</strong>clude the five (5) follow<strong>in</strong>g criteria:<br />
GHO’s rout<strong>in</strong>e uses and disclosure of PHI. GHO uses and discloses PHI <strong>in</strong> connection<br />
with Members’ treatment, to make payment for <strong>Health</strong> Care Services and for GHO’s health<br />
care operations.<br />
Uses of Authorizations. Special authorizations are required by Pennsylvania law to permit<br />
disclosures of certa<strong>in</strong> highly sensitive personal <strong>in</strong>formation. In certa<strong>in</strong> situations, consistent<br />
with applicable regulations or laws, GHO will request Members’ written authorization<br />
before us<strong>in</strong>g or disclos<strong>in</strong>g identifiable health <strong>in</strong>formation. Except for the treatment,<br />
payment and health care operations, GHO will not use or disclose Members’ PHI unless<br />
the Member has signed a form that allows GHO to do so.<br />
Access to PHI. Members have the right to look at or get a copy of their PHI <strong>in</strong> a designated<br />
record set (i.e. medical/bill<strong>in</strong>g record) <strong>in</strong> accordance with all applicable laws perta<strong>in</strong><strong>in</strong>g to<br />
access of PHI.<br />
Internal Protection of Oral, Written and Electronic PHI across the Organization. GHO has<br />
procedures <strong>in</strong> place to prevent unauthorized access to Members’ PHI, which <strong>in</strong>cludes<br />
employees’ signed statements <strong>in</strong> which they have agreed to protect Members’<br />
confidentiality, us<strong>in</strong>g computer passwords to limit access to Members’ PHI.<br />
Protection of Information Disclosed to <strong>Plan</strong> Sponsors or Employers. GHO may release<br />
Members’ PHI to a plan sponsor or Employer, provided the plan sponsor or Employer has<br />
certified that the <strong>in</strong>formation provided will be ma<strong>in</strong>ta<strong>in</strong>ed <strong>in</strong> a confidential manner and not<br />
used for employment related decisions or for other employee benefit determ<strong>in</strong>ations or <strong>in</strong><br />
any other manner not permitted by law.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s can access GHO’s entire Privacy Notice onl<strong>in</strong>e at<br />
www.thehealthplan.com/wvuh_providers_us/ or a paper copy may be obta<strong>in</strong>ed by contact<strong>in</strong>g<br />
your <strong>Provider</strong> Relations Representative.<br />
Population Management Programs<br />
GHO offers Population Management Programs for Members across the healthcare cont<strong>in</strong>uum<br />
<strong>in</strong>clud<strong>in</strong>g complex case management (CM) and disease management (DM). CM/DM programs<br />
offer education and support for Members with chronic conditions. To refer a Member to a<br />
Population Management Program, or to learn more about a specific Case Management/Disease<br />
Management Program, visit GHO’s <strong>Provider</strong> Information Center at<br />
www.thehealthplan.com/wvuh_providers_us/ or contact:<br />
Case Management Department<br />
Monday through Friday, 8:00 a.m. to 4:30 p.m.<br />
(800) 883-6355<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
10
GHO registered nurses (Case Managers/<strong>Health</strong> Managers) provide the follow<strong>in</strong>g services and<br />
programs.<br />
Coord<strong>in</strong>ate Care After Discharge<br />
The Case Manager contacts Members with certa<strong>in</strong> health conditions, <strong>in</strong>clud<strong>in</strong>g heart failure and<br />
pneumonia, after a hospitalization, rehabilitation or Skilled Nurs<strong>in</strong>g Facility admission. The<br />
purpose of the contact is to ensure a safe transition of care. This <strong>in</strong>cludes medication<br />
reconciliation, facilitat<strong>in</strong>g a return appo<strong>in</strong>tment with their Primary Care and/or Specialty Care<br />
provider and to review other important issues.<br />
Complement the Care provided by the Primary and/or Specialty Care <strong>Provider</strong><br />
The Case Manager/<strong>Health</strong> Manager works with the Member, their family, and the PCP/SCP to<br />
assist Members <strong>in</strong> the community with chronic health/social problems. The Case<br />
Manager/<strong>Health</strong> Manager provides monitor<strong>in</strong>g and education to help Members better manage the<br />
follow<strong>in</strong>g health conditions.<br />
Adult and Pediatric Asthma<br />
Education is a key factor <strong>in</strong> the Asthma Care Program. Case Manager/<strong>Health</strong> Manager work with<br />
Members and their families to help them understand and manage asthma triggers and symptoms<br />
and adhere to treatment plans.<br />
Chronic Kidney Disease (CKD)<br />
The purpose of the CKD program is to improve the coord<strong>in</strong>ation of appropriate services with a<br />
PCP or nephrologist (kidney specialist) for Members with kidney disease. Members learn about<br />
the importance of proper nutrition, medications, blood pressure control, and receive other<br />
important health care <strong>in</strong>formation from a Case Manager.<br />
Heart Failure<br />
An ongo<strong>in</strong>g comb<strong>in</strong>ation of education and follow up by a Case Manager teaches Members the<br />
importance of medications, diet, and life-style habits to improve the management of heart failure<br />
and adherence to a <strong>Plan</strong> of Care. Ongo<strong>in</strong>g follow up by the case manager with an <strong>in</strong>dividualized<br />
treatment plan with exacerbation management is a key element of case management.<br />
Chronic Obstructive Pulmonary Disease (COPD)<br />
The Chronic Obstructive Pulmonary Disease (COPD) Program helps Members with COPD to<br />
better manage the condition. Information about tobacco cessation, pulmonary function test<strong>in</strong>g,<br />
medication management and life-style modification is provided by a Case Manager. Ongo<strong>in</strong>g<br />
follow up by the case manager with an <strong>in</strong>dividualized treatment plan with exacerbation<br />
management is a key element of case management<br />
Diabetes<br />
Members <strong>in</strong> the Diabetes Care Program work with a Community Case Manager who provides<br />
education on topics <strong>in</strong>clud<strong>in</strong>g diet and exercise, medication management, and ways to improve<br />
glucose control. The Case Manager/<strong>Health</strong> Manager also coord<strong>in</strong>ates services for Members such<br />
as eye exams and kidney screen<strong>in</strong>gs. This comb<strong>in</strong>ation of education and coord<strong>in</strong>ation of care<br />
assists Members <strong>in</strong> tak<strong>in</strong>g control of diabetes.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
11
HeartWise<br />
Manag<strong>in</strong>g risk factors and promot<strong>in</strong>g proper medication management is the focus of the<br />
HeartWise program for Members with heart disease. Cholesterol and blood pressure<br />
management are key aspects of the program. Case Manager/<strong>Health</strong> Manager also provide<br />
education about diet and exercise strategies, and work with providers to coord<strong>in</strong>ate<br />
recommended therapies.<br />
Hypertension<br />
A Case Manager/<strong>Health</strong> Manager assists Members <strong>in</strong> learn<strong>in</strong>g what they can do to control blood<br />
pressure and reduce the risk of develop<strong>in</strong>g other health problems that can result from poorly<br />
controlled blood pressure. Nurses work with providers and Members to optimize medication<br />
treatment plans and control hypertension.<br />
Osteoporosis<br />
This program provides education to women and men at risk for osteoporosis, as well as those<br />
who have already been diagnosed. A Case Manager/<strong>Health</strong> Manager outl<strong>in</strong>es steps to prevent<br />
osteoporosis, reduce the risk of complications, and ecourage safety to prevent falls and fractures<br />
dur<strong>in</strong>g education sessions provided <strong>in</strong> the office or by telephone.<br />
Tobacco Cessation<br />
In the Tobacco Cessation Program, professional support is provided through phone, group, webbased,<br />
or <strong>in</strong>dividual coach<strong>in</strong>g. The program goal is to help break the addiction to tobacco<br />
products such as cigarettes, pipes, and smokeless tobacco, and help Members quit.<br />
A GHO discharge planner is available to assist <strong>in</strong> coord<strong>in</strong>at<strong>in</strong>g the discharge plan for the<br />
Member. GHO can assist <strong>in</strong> cord<strong>in</strong>at<strong>in</strong>g services; <strong>in</strong>clud<strong>in</strong>g transfers to other facilities, referrals<br />
to case management and disease management programs, and evaluation of community resources.<br />
To refer a Member to a Population Management Program, or to learn more about a specific Case<br />
Management/Disease Management Program, visit GHO’s <strong>Provider</strong> Information Center at<br />
www.thehealthplan.com/wvuh_providers_us/ or contact:<br />
Case Management Department<br />
Monday through Friday, 8:00 a.m. to 4:30 p.m.<br />
(800) 883-6355<br />
Case Management/Disease Management Program Development<br />
Case Management conducts an analysis of the disease under consideration prior to the<br />
development of a Case Management/Disease Management program. The follow<strong>in</strong>g criteria are<br />
evaluated:<br />
1. Disease prevalence.<br />
2. Disease complexity.<br />
3. Potential for reduc<strong>in</strong>g complications and improv<strong>in</strong>g quality.<br />
4. Current cost of manag<strong>in</strong>g the disease.<br />
5. Existence of an evidence-based cl<strong>in</strong>ical guidel<strong>in</strong>e to assist practitioners <strong>in</strong> the<br />
management of the disease.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
12
6. Value to the Member and GHO if the program is implemented.<br />
Case Management leadership determ<strong>in</strong>es the need for a specific Case Management/Disease<br />
Management program based upon the criteria listed above and submits a proposal to GHO’s<br />
Medical Management/Adm<strong>in</strong>istrative Committee and Quality Improvement Committee for<br />
review and approval. Actively practic<strong>in</strong>g practitioners are participat<strong>in</strong>g members of Case<br />
Management/Disease Management teams and assist <strong>in</strong> the development, implementation, and<br />
monitor<strong>in</strong>g of new and established Case Management/Disease Management management<br />
programs.<br />
Practitioner Program Content<br />
The design of all Case Management/Disease Management programs <strong>in</strong>cludes, but is not limited<br />
to: evidence-based cl<strong>in</strong>ical guidel<strong>in</strong>es, Member identification, passive or active enrollment,<br />
stratification, <strong>in</strong>terventions based on stratification level, practitioner decision support, and<br />
evaluation of program effectiveness.<br />
Evidence-based cl<strong>in</strong>ical guidel<strong>in</strong>es are a core component of all Disease Management programs.<br />
Board certified specialty and/or primary care practitioners are <strong>in</strong>volved <strong>in</strong> the review and<br />
approval of evidenced-based guidel<strong>in</strong>es.<br />
Cl<strong>in</strong>ical guidel<strong>in</strong>es are reviewed every two years or when recommendations are revised by the<br />
appropriate guidel<strong>in</strong>e team, GHO’s <strong>Guide</strong>l<strong>in</strong>e Committee and the GHO Quality Improvement<br />
Committee. Identified primary and specialty care practitioners are <strong>in</strong>volved <strong>in</strong> the development<br />
and review of new Case Management/Disease Management programs. The Case Management<br />
Department and the accompany<strong>in</strong>g teams are responsible for program content that is consistent<br />
with current cl<strong>in</strong>ical practice guidel<strong>in</strong>es.<br />
Evidence-based guidel<strong>in</strong>es are posted onl<strong>in</strong>e at www.thehealthplan.com/wvuh_providers_us/ and<br />
announcements are made <strong>in</strong> the publication Briefly to <strong>in</strong>form practitioners of their availability.<br />
Pr<strong>in</strong>ted copies or electronic <strong>PDF</strong> files are available upon request for practitioners who do not<br />
have Internet access by contact<strong>in</strong>g GHO’s Case Management Department at (570) 271-8763 or<br />
toll free (800) 883-6355, Monday through Friday from 8:00 a.m. to 4:30 p.m.<br />
Identification of Members who will benefit from Case Management/Disease Management<br />
programs is accomplished through claims analysis us<strong>in</strong>g standard cl<strong>in</strong>ical specifications from<br />
criteria such as the <strong>Health</strong> <strong>Plan</strong> Employer Data & Information Set (HEDIS). Member<br />
identification is also facilitated by direct referrals from primary and specialty care practitioners,<br />
the Member and/or family, and from various GHO departments <strong>in</strong>clud<strong>in</strong>g Medical Management,<br />
Customer Service, Appeals, and Quality Improvement.<br />
Passive/active enrollment<br />
All Members with a disease-specific diagnosis are identified by claims analysis and/or HEDIS<br />
criteria and mailed a disease-specific <strong>in</strong>formational newsletter. The Members are <strong>in</strong>formed of<br />
their enrollment <strong>in</strong> the program and have the opportunity to “opt out” by contact<strong>in</strong>g GHO’s Case<br />
Management department. Members that do not opt out are considered passive enrollees.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
13
All passive enrollees receive disease-specific <strong>in</strong>formational newsletters each year to <strong>in</strong>crease<br />
their knowledge of disease self-management. Each newsletter also encourages the Members to<br />
become “active” enrollees <strong>in</strong> the Case Management/Disease Management program.<br />
A Member becomes actively enrolled <strong>in</strong> the appropriate Case Management/Disease Management<br />
program when the Member contacts GHO’s Case Management department directly, is referred<br />
by a <strong>Health</strong> Care <strong>Provider</strong> or a GHO department, or accepts an <strong>in</strong>vitation extended by GHO’s<br />
Case Management Department (through disease-specific Member newsletters or direct Member<br />
<strong>in</strong>vitation by letter or phone as the result of claims analysis <strong>in</strong>formation). The Case<br />
Manager/<strong>Health</strong> Manager (CM/HM) reviews the referral <strong>in</strong>formation and contacts the Member<br />
to either schedule an office appo<strong>in</strong>tment with the nurse or to arrange rout<strong>in</strong>e communication with<br />
the Member telephonically. After the Member’s verbal and/or written consent for participation is<br />
obta<strong>in</strong>ed, the Member is actively enrolled <strong>in</strong> the appropriate program.<br />
Risk stratification<br />
The CM/HM stratifies active Members based on cl<strong>in</strong>ical criteria accord<strong>in</strong>g to low, moderate or<br />
high risk. For example, Members enrolled <strong>in</strong> the Heart Failure program are stratified accord<strong>in</strong>g<br />
to the American College of Cardiology (ACE). Members with diabetes are stratified us<strong>in</strong>g<br />
glycosolated hemoglob<strong>in</strong> (A1c) control and the presence of risk factors.<br />
Interventions<br />
The degree of <strong>in</strong>tervention is based on the Member’s risk stratification. For example, a Member<br />
classified as low risk will receive a m<strong>in</strong>imum of one (1) program <strong>in</strong>formational newsletter each<br />
year, self-management education, a plan of care, and one or more follow-up office or phone<br />
appo<strong>in</strong>tments. A Member with a high-risk stratification will receive these <strong>in</strong>terventions <strong>in</strong><br />
addition to more frequent office/phone visits and referrals for necessary services.<br />
Practitioner decision support: How GHO works sith your patients <strong>in</strong> the program<br />
The Case Management/Disease Management decision support model <strong>in</strong>cludes evidence-based<br />
cl<strong>in</strong>ical guidel<strong>in</strong>es (previously described), CM/HMs, and the plan of care. The program is<br />
designed for actively practic<strong>in</strong>g primary and/or specialty care practitioners.<br />
The CM/HM is key to provid<strong>in</strong>g collaborative “real time” decision support to primary and/or<br />
specialty care practitioners. The CM/HM follows <strong>in</strong>ternally developed Care Paths (Algorithms)<br />
that complement the cl<strong>in</strong>ical guidel<strong>in</strong>e. The Care Paths (Algorithms) provide a framework for<br />
self-management education, the recommended laboratory/diagnostic studies, and targeted<br />
cl<strong>in</strong>ical goals.<br />
The plan of care <strong>in</strong>cludes <strong>in</strong>formation regard<strong>in</strong>g the Member’s self-management of their<br />
condition, barriers, special considerations or exceptions, review of medical test results,<br />
management of co-morbidities, collaborative goal-sett<strong>in</strong>g and problem-solv<strong>in</strong>g, medication<br />
review, plans for follow-up, and preventive health monitor<strong>in</strong>g. The plan of care is reviewed and<br />
discussed by the primary and/or specialty care practitioner and CM/HM <strong>in</strong> person, by phone, or<br />
through an electronic medical record messag<strong>in</strong>g process.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
14
The <strong>in</strong>volvement of the practitioner is <strong>in</strong>tegral <strong>in</strong> the design of program content for all Case<br />
Management/Disease Management programs. Practitioner participation ensures program content<br />
is appropriate for the actively practic<strong>in</strong>g primary care practitioner. All primary care practitioners<br />
are surveyed annually <strong>in</strong> order to elicit feedback regard<strong>in</strong>g the program(s).<br />
Evaluation of program effectiveness<br />
Program effectiveness is measured by conduct<strong>in</strong>g a pre-and post-analysis of pert<strong>in</strong>ent cl<strong>in</strong>ical<br />
measures, annual Member/practitioner program satisfaction surveys and pre- and post<br />
comparisons of services utilized by Members <strong>in</strong> the programs.<br />
Practitioner’s rights<br />
Practitioners who care for GHO Members have the right to:<br />
1. Obta<strong>in</strong> <strong>in</strong>formation regard<strong>in</strong>g Case Management/Disease Management programs and<br />
services <strong>in</strong> conjunction with GHO as outl<strong>in</strong>ed here<strong>in</strong>; and<br />
2. Obta<strong>in</strong> <strong>in</strong>formation regard<strong>in</strong>g the qualifications of the Case Management staff; and<br />
3. Obta<strong>in</strong> <strong>in</strong>formation regard<strong>in</strong>g how the Case Management staff facilitates <strong>in</strong>terventions via<br />
treatment plans for <strong>in</strong>dividual Members; and<br />
4. Know how to contact the CM/HM responsible for manag<strong>in</strong>g and communicat<strong>in</strong>g with<br />
their patients; and<br />
5. Request the support of the CM/HM to make decisions <strong>in</strong>teractively with Members<br />
regard<strong>in</strong>g their health care; and<br />
6. Receive courteous and respectful treatment from Case Management staff at all times; and<br />
7. File a compla<strong>in</strong>t when dissatisfied with any component of the Case Management/Disease<br />
Management programs by contact<strong>in</strong>g the Case Management Department at (570) 271-<br />
8763, toll free at (800) 883-6355, or the customer service team at the number listed on<br />
your patient’s <strong>in</strong>surance card..<br />
Preventive <strong>Health</strong> Program<br />
GHO strives to keep Members healthy through a preventive health program.<br />
Members are <strong>in</strong>formed and encouraged to take advantage of preventive health measures such as<br />
immunizations, breast and cervical cancer screen<strong>in</strong>gs and diabetic eye exams. GHO cont<strong>in</strong>ually<br />
expands this program <strong>in</strong> order to ensure that more Members will receive recommended<br />
preventive health measures. Current <strong>in</strong>itiatives <strong>in</strong>clude:<br />
Childhood immunizations<br />
Adolescent immunizations<br />
Cervical cancer screen<strong>in</strong>g<br />
Breast cancer screen<strong>in</strong>g<br />
Program Goal: The goal of the program is to educate and encourage Members to have the<br />
recommended preventive services and to encourage communication between Participat<strong>in</strong>g<br />
<strong>Provider</strong>s.<br />
How the Program Works: Nurses employed by GHO will be communicat<strong>in</strong>g with Members or<br />
their PCPs concern<strong>in</strong>g those Members need<strong>in</strong>g preventive services. If the Member has not<br />
received the recommended service, the Member is educated on its importance and is encouraged<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
15
to call their Primary Care Site. In some cases GHO will schedule the services for the Member. If<br />
the Member has received the preventive service, <strong>in</strong>formation perta<strong>in</strong><strong>in</strong>g to the date and location<br />
of the provided service is obta<strong>in</strong>ed for reference.<br />
For more <strong>in</strong>formation on preventive health services, visit GHO’s <strong>Provider</strong> Information Center at<br />
www.thehealthplan.com/wvuh_providers_us/ or contact GHO’s Quality Improvement (QI)<br />
department at (570) 271-5108.<br />
Departments Available for Assistance<br />
Case Management Department<br />
The Case Management Department is available to assist Participat<strong>in</strong>g <strong>Provider</strong>s and Members<br />
with its various disease management programs. Cl<strong>in</strong>ical guidel<strong>in</strong>es for each of these programs<br />
are available on GHO’s Web site, www.thehealthplan.com/wvuh_providers_us/.<br />
To refer a Member <strong>in</strong>to a Disease management Program, or to learn more about a specific<br />
Disease management Program, Participat<strong>in</strong>g <strong>Provider</strong>s should contact the Case Management<br />
Department.<br />
Case Management Department<br />
Monday through Friday, 8:00 a.m. to 4:30 p.m.<br />
(800) 883-6355<br />
Customer Service Teams<br />
Customer Service Teams (CSTs) are comprised of customer service representatives who process<br />
Member enrollment, claims, and respond to Member and <strong>Health</strong> Care <strong>Provider</strong> <strong>in</strong>quiries. GHO<br />
makes every effort to assure that Members will be well <strong>in</strong>formed and able to participate <strong>in</strong><br />
decision mak<strong>in</strong>g for their health care needs and benefits. Most Member questions stem from: i)<br />
the need for a clear def<strong>in</strong>ition of benefits, ii) an understand<strong>in</strong>g of the role of managed care, and<br />
iii) the access process to obta<strong>in</strong> necessary medical care. Responsibilities of the teams <strong>in</strong>clude:<br />
Respond<strong>in</strong>g to Members’ questions about their GHO coverage and protocol for access<strong>in</strong>g<br />
medical care.<br />
Resolv<strong>in</strong>g Members concerns and coord<strong>in</strong>at<strong>in</strong>g the compla<strong>in</strong>t, grievance and appeals<br />
processes.<br />
Promot<strong>in</strong>g Member education.<br />
Process<strong>in</strong>g all <strong>Health</strong> Care <strong>Provider</strong> claims and Member enrollment/disenrollment activity.<br />
Conduct<strong>in</strong>g follow-up calls to assure Member satisfaction.<br />
Review<strong>in</strong>g trends to determ<strong>in</strong>e areas that may require Member education.<br />
Most <strong>in</strong>quiries can also be addressed by visit<strong>in</strong>g GHO’s Website,<br />
www.thehealthplan.com/wvuh_providers_us/, where a multitude of onl<strong>in</strong>e tools and resources<br />
are available at the click of a button.<br />
GHO’s IVR system is available for provider use, 24 hours a day, 7 days a week. Our Customer<br />
Service Representatives are available to assist you dur<strong>in</strong>g normal bus<strong>in</strong>ess hours.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
16
GHO CUSTOMER SERVICE: (866) 580-3531.<br />
Medical Directors and Quality Improvement (Q.I.) Nurses<br />
GHO uses Medical Directors, <strong>in</strong> addition to the Vice President Chief Medical Officer, to serve<br />
the needs of the Network and the Members. Medical Directors are also practic<strong>in</strong>g Participat<strong>in</strong>g<br />
<strong>Provider</strong>s. GHO believes Medical Directors should rema<strong>in</strong> close to cl<strong>in</strong>ical practice <strong>in</strong> order to<br />
understand the effect managed care has on a physician practice. GHO ma<strong>in</strong>ta<strong>in</strong>s an on-duty and<br />
on-call schedule assur<strong>in</strong>g Medical Director availability twenty-four (24) hours a day, seven (7)<br />
days a week.<br />
A Medical Director and Q.I. Nurse is designated for each region of the Service Area and are<br />
available to Participat<strong>in</strong>g <strong>Provider</strong>s. The roles and responsibilities of the Medical Directors and<br />
their staff fall <strong>in</strong>to five major categories:<br />
1) Quality Improvement:<br />
Medical Directors work with the Q.I. Nurses to develop, implement, monitor, analyze and<br />
cont<strong>in</strong>ue to improve GHO’s Quality Improvement Program.<br />
2) <strong>Health</strong> Services:<br />
Medical Directors are responsible for assur<strong>in</strong>g that GHO’s <strong>Health</strong> Services Department achieves<br />
the highest quality outcomes with the most efficient use of resources. Activities <strong>in</strong>clude: review<br />
of medical policies and procedures, development of preventive health, acute and chronic care<br />
guidel<strong>in</strong>es, identification and achievement of best practices; development, implementation and<br />
measurement of Disease management and Case Management programs, oversight of data<br />
production and provide feedback to Participat<strong>in</strong>g <strong>Provider</strong>s.<br />
3) Liaison/Insurer to <strong>Provider</strong>:<br />
Medical Directors are responsible for cont<strong>in</strong>uously look<strong>in</strong>g for ways to improve GHO’s<br />
relationship with Participat<strong>in</strong>g <strong>Provider</strong>s.<br />
4) Balanced Advocacy:<br />
Medical Directors are responsible for assur<strong>in</strong>g a balanced approach by GHO toward all<br />
stakeholders, <strong>in</strong>clud<strong>in</strong>g the Member, Participat<strong>in</strong>g <strong>Provider</strong>s, GHO and, as appropriate, the<br />
public and media as it relates to medical issues.<br />
5) Credential<strong>in</strong>g:<br />
Medical Directors are responsible for the implementation and function of GHO’s credential<strong>in</strong>g<br />
process to assure that it meets all regulatory and accreditation requirements.<br />
Medical Director and Q.I. Nurse<br />
Medical Director<br />
100 North Academy Avenue, Danville, PA 17822-3220<br />
(570) 214-9574<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
17
Q.I. Nurse<br />
100 North Academy Avenue, Danville, PA 17822-3220<br />
(570) 214-2594<br />
<strong>Provider</strong> Network Management<br />
<strong>Provider</strong> Network Management (PNM) acts as the primary liaison between the Network and<br />
GHO. Each Participat<strong>in</strong>g <strong>Provider</strong> has a specific <strong>Provider</strong> Relations Representative assigned to<br />
their practice or facility. PNM’s primary focus is to enhance Participat<strong>in</strong>g <strong>Provider</strong> satisfaction<br />
and retention and to ensure a long-term partnership between GHO and each Participat<strong>in</strong>g<br />
<strong>Provider</strong>.<br />
Your <strong>Provider</strong> Relations Representative will schedule an <strong>in</strong>itial orientation with your practice to<br />
review GHO’s policies and procedures, product l<strong>in</strong>es, benefit <strong>in</strong>formation, and other standard<br />
operat<strong>in</strong>g procedures. Periodic telephonic or on-site visits will also be scheduled to review<br />
changes <strong>in</strong> products or services, as well as f<strong>in</strong>ancial or utilization reports.<br />
Your <strong>Provider</strong> Relations Representative should be contacted immediately to discuss any changes<br />
related to your practice, <strong>in</strong>clud<strong>in</strong>g tax identification number, remittance address, bus<strong>in</strong>ess name<br />
or the addition or term<strong>in</strong>ation of a physician/provider.<br />
<strong>Provider</strong> Network Management Offices<br />
Monday through Friday, 8:00 a.m. to 5:00 p.m.,<br />
Call (800) 876-5357 to request GHO education and<br />
<strong>in</strong>formation.<br />
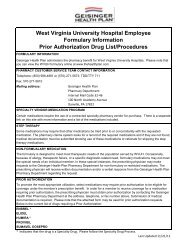
Pharmacy Department<br />
GHO’s Pharmacy Department is available to assist Participat<strong>in</strong>g <strong>Provider</strong>s and Members with<br />
pharmacy-related questions. A list of drugs, known as the WVUHS Formulary, is developed to<br />
optimize patient care through the rational selection and use of drugs, and to ensure quality<br />
prescrib<strong>in</strong>g practices. The WVUHS Formulary is a culm<strong>in</strong>ation of efforts by the GHO Pharmacy<br />
& Therapeutics (P&T) Committee.<br />
Medications <strong>in</strong> each therapeutic class are reviewed with respect to safety, efficacy, currently<br />
available agents and cost-effectiveness for Members. The most appropriate agents are then<br />
selected for <strong>in</strong>clusion <strong>in</strong> the WVUHS Formulary. Ma<strong>in</strong>tenance of the WVUHS Formulary is<br />
ongo<strong>in</strong>g as the P&T Committee cont<strong>in</strong>ually reviews new medications and <strong>in</strong>formation<br />
concern<strong>in</strong>g exist<strong>in</strong>g medications.<br />
Specific <strong>in</strong>formation available through the Pharmacy Department <strong>in</strong>cludes, but is not limited to:<br />
Information related to new drugs, or exist<strong>in</strong>g WVUHS Formulary products<br />
WVUHS Formulary status<br />
Drug manufacturer pharmaceutical recall<br />
Information on pharmacy benefits for specific Members<br />
Answers to questions regard<strong>in</strong>g prescription coverage, or quantity limitation<br />
Additional benefits; such as, mail order and applicable pharmacy Rider<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
18
The precertification process for certa<strong>in</strong> WVUHS Formulary or restricted drug<br />
o Drugs requir<strong>in</strong>g precertification and their associated criteria can be found <strong>in</strong> the<br />
<strong>Provider</strong> Information Center section of GHO’s Web site at<br />
www.thehealthplan.com/wvuh_providers_us/. Participat<strong>in</strong>g <strong>Provider</strong>s may also<br />
refer to <strong>in</strong>formation <strong>in</strong>cluded under “WVUHS Formulary Precertification and<br />
non-WVUHS Formulary Exception Process” <strong>in</strong>cluded <strong>in</strong> the Precertification<br />
Requirements section of this <strong>Guide</strong>.<br />
Status or submission of requests for additions to the exist<strong>in</strong>g WVUHS Formulary can be<br />
faxed or mailed to:<br />
Fax: (570) 271-5610<br />
Mail: Geis<strong>in</strong>ger <strong>Health</strong> Options Pharmacy Department<br />
100 North Academy Avenue<br />
Mail Code 30-45<br />
Danville, PA 17822<br />
Written and verbal <strong>in</strong>quires perta<strong>in</strong><strong>in</strong>g to whether a specific medication, either <strong>in</strong>cluded or<br />
excluded from the then-current WVUHS Formulary, will be responded to with<strong>in</strong> applicable<br />
regulatory timeframes by GHO Pharmacy Department. Please refer to the Precertification<br />
Requirements section of this <strong>Guide</strong> for the complete process.<br />
Pharmacy Department Representatives<br />
Monday through Friday, 8:00 a.m. to 5:00 p.m.<br />
(800) 988-4861; Fax: (570) 271-5610<br />
Tel-A-Nurse<br />
Tel-A-Nurse is a valuable health <strong>in</strong>formation service featur<strong>in</strong>g a twenty-four (24) hour, seven (7)<br />
days a week nurs<strong>in</strong>g hotl<strong>in</strong>e for Members. Tel-A-Nurse is provided free to Members and is<br />
staffed by licensed registered nurses who are available to answer health related questions.<br />
An additional service available through Tel-A-Nurse is an audio library, which provides more<br />
than 200 recorded health topics that a Member may listen to or request a brochure on at any time.<br />
Tel-A-Nurse<br />
(877) 543-5061<br />
Medical Management Department<br />
The Medical Management Department encourages and facilitates the use of the most appropriate<br />
level of care provid<strong>in</strong>g Medically Necessary services to Members. The Medical Management<br />
Department utilizes nationally recognized guidel<strong>in</strong>es as well as <strong>in</strong>ternal medical benefit policies<br />
and other resources to guide precertification, prior authorization, Concurrent Review, and<br />
retrospective review processes <strong>in</strong> accordance with the Member’s applicable Benefit Document<br />
and eligibility. Beg<strong>in</strong>n<strong>in</strong>g January 1, 2012, GHO will utilize Milliman Care <strong>Guide</strong>l<strong>in</strong>es® for<br />
medical necessity reviews.<br />
The Medical Management Department is available to assist Participat<strong>in</strong>g <strong>Provider</strong>s with:<br />
Precertification of planned <strong>in</strong>patient, rehabilitative, long-term care, and skilled level of care<br />
admissions<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
19
Concurrent Review of all admission <strong>in</strong>formation<br />
Notification processes related to Intermediate level of Care admissions and discharges<br />
Precertification of non-emergency ambulance transportation services<br />
Requests related to services requir<strong>in</strong>g GHO required precertification<br />
Requests related to medical policy criteria, Medical Management processes, or provider<br />
appeals<br />
Requests to speak with a GHO Medical Director<br />
The decision-mak<strong>in</strong>g process for authorization of <strong>Health</strong> Care Services is based on Medical<br />
Necessity us<strong>in</strong>g cl<strong>in</strong>ical, psychosocial and access/availability <strong>in</strong>formation for each case. A<br />
Medical Director renders any denial of coverage on the basis of Medical Necessity.<br />
Medical Management Statement<br />
Participat<strong>in</strong>g <strong>Provider</strong>s are rem<strong>in</strong>ded that utilization criteria are available upon request.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s may request a copy of the applicable criteria utilized as part of the denial<br />
decision. Criteria may be distributed <strong>in</strong> writ<strong>in</strong>g by mail, fax, email or on the web. Complete<br />
criteria can be reviewed at GHO’s home office located <strong>in</strong> Danville, Pa. Written requests should<br />
be submitted to the Medical Management Department:<br />
GHO Web Site Information<br />
Medical Management Department<br />
100 N. Academy Ave.<br />
Danville, Pa 17822-3218<br />
Monday through Friday, 8:00 a.m. to 4:30 p.m.<br />
(800) 544-3907 or (570) 271-6497;<br />
Fax: (570) 214-6796<br />
GHO is cont<strong>in</strong>ually work<strong>in</strong>g to improve the capability of its World Wide Web site,<br />
www.thehealthplan.com/wvuh_providers_us/, which affords Participat<strong>in</strong>g <strong>Provider</strong>s a plethora of<br />
onl<strong>in</strong>e <strong>in</strong>formation, resources and tools.<br />
Registration process<br />
Because certa<strong>in</strong> provider <strong>in</strong>formation is secured, Participat<strong>in</strong>g <strong>Provider</strong>s must enter specific<br />
identification <strong>in</strong>formation as part of the registration process, <strong>in</strong> order to access all sections of the<br />
Web site. The follow<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong>s <strong>in</strong>formation is required:<br />
GHO provider number.<br />
Date of birth.<br />
Social security number.<br />
Medical license number and State of licensure.<br />
After successfully enter<strong>in</strong>g this <strong>in</strong>formation, Participat<strong>in</strong>g Physicians will be able to establish a<br />
user ID and password immediately to complete the registration and log<strong>in</strong> process.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
20
Some onl<strong>in</strong>e tools and resources may require additional registration criteria. Please contact your<br />
<strong>Provider</strong> Relations Representative with any questions regard<strong>in</strong>g GHO’s Web site and onl<strong>in</strong>e<br />
services.<br />
<strong>Provider</strong> Information Center<br />
A provider’s access <strong>in</strong>cludes, but is not limited to:<br />
An up-to-date version of GHO’s WVUHS Formulary, searchable by both therapeutic<br />
category(s) and <strong>in</strong>dividual drug.<br />
A search of GHO’s provider Network, which is updated nightly.<br />
GHO WVUHS TPA <strong>Provider</strong> <strong>Guide</strong>.<br />
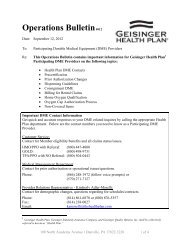
Operations Bullet<strong>in</strong>s.<br />
<strong>Provider</strong> newsletters.<br />
Disease management program descriptions.<br />
Case management program description.<br />
Cl<strong>in</strong>ical guidel<strong>in</strong>es.<br />
Onl<strong>in</strong>e CME courses.<br />
Precertification list.<br />
Laboratory Utilization Report.<br />
Physician Utilization Activity Report.<br />
Pharmacy Utilization Report.<br />
Member <strong>Health</strong> Alerts.<br />
o A Web tool that is designed to assist Primary Care Practices <strong>in</strong> identify<strong>in</strong>g<br />
Members who are eligible for certa<strong>in</strong> preventive services (i.e. mammograms and<br />
colorectal exams). Each PCP or their office personnel will be able to access a<br />
list<strong>in</strong>g of Members who, based on claim data, are due for the services listed.<br />
These services should be performed by a Participat<strong>in</strong>g <strong>Provider</strong> and may be<br />
eligible for Member cost shar<strong>in</strong>g. As you beg<strong>in</strong> schedul<strong>in</strong>g services for these<br />
Members, your Member <strong>Health</strong> Alerts list<strong>in</strong>g will automatically be updated based<br />
on claim and medical record data received by GHO.<br />
<strong>Provider</strong> Service Center<br />
The <strong>Provider</strong> Service Center is available at www.thehealthplan.com/wvuh_providers_us/.<br />
Registered Participat<strong>in</strong>g <strong>Provider</strong>s can access:<br />
Real-time Member eligibility data.<br />
Detailed benefit plan <strong>in</strong>formation, <strong>in</strong>clud<strong>in</strong>g cost-shar<strong>in</strong>g amounts.<br />
Current authorizations for Members.<br />
Current explanations of payment (EOP).<br />
Comprehensive <strong>in</strong>formation on claim status, history and payments.<br />
Medical and pharmaceutical policies.<br />
CareEnhance Resource Management Systems (CRMS).<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
21
For more <strong>in</strong>formation about the Service Center, <strong>in</strong>clud<strong>in</strong>g registration <strong>in</strong>structions, please contact<br />
your <strong>Provider</strong> Relations Representative or visit the <strong>Provider</strong> Information Center at<br />
www.thehealthplan.com/wvuh_providers_us/.<br />
Please contact your <strong>Provider</strong> Relations Representative to enroll <strong>in</strong> the follow<strong>in</strong>g Electronic<br />
Data Interchange (EDI) capabilities:<br />
Electronic EOP (835 Transaction)<br />
Electronic EOP is a quick and easy way to verify the accuracy of claim payment. To request<br />
electronic Explanation of Payment (EOP), please complete and submit the Electronic<br />
Explanation of Claim Payment <strong>Provider</strong> Enrollment Form, available by request or onl<strong>in</strong>e at<br />
www.thehealthplan.com/wvuh_providers_us/, to:<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options<br />
CSST/EDI Enrollment 32-27<br />
100 North Academy Avenue<br />
Danville PA 17821-3227<br />
Once your enrollment form has been received, we will contact you to beg<strong>in</strong> set up.<br />
Electronic Claim Submission<br />
Electronic claim submission allows <strong>Health</strong> Care <strong>Provider</strong>s to bill with decreased delay and costs.<br />
It streaml<strong>in</strong>es the bill<strong>in</strong>g process and proves to be more accurate. Electronic bill<strong>in</strong>g also reduces<br />
your paperwork burden and affords office staff the time to handle other important tasks.<br />
Visit www.thehealthplan.com/wvuh_providers_us/ to complete GHO’s EDI Submission Form<br />
onl<strong>in</strong>e.<br />
Electronic Fund Transfer<br />
Claims payments can be made faster and easier through GHO’s new electronic fund transfer<br />
(EFT) system. Payments will be deposited directly <strong>in</strong>to your specified bank account.<br />
A registration form is available by visit<strong>in</strong>g the <strong>Provider</strong> Information Center at<br />
www.thehealthplan.com/wvuh_providers_us/. Once this form is received, we will validate your<br />
bank account and rout<strong>in</strong>g <strong>in</strong>formation by send<strong>in</strong>g a pre-note to your bank. Once your bank<br />
account <strong>in</strong>formation has been verified, we will contact you to expla<strong>in</strong> when to expect your first<br />
EFT transaction.<br />
Please note: Paper explanation of payment (EOP) will cont<strong>in</strong>ue to be generated and distributed<br />
by mail; however, no checks will accompany the EOP.<br />
EFT payments can start <strong>in</strong> as little as two weeks. You will be notified prior to this occurr<strong>in</strong>g.<br />
EFT payments for all l<strong>in</strong>es of bus<strong>in</strong>esses except Third Party Adm<strong>in</strong>istrator (TPA) are processed<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
22
on Mondays (except bank holidays). TPA transfers will be made when funded. This is the same<br />
as without EFT.<br />
Interactive Voice Response (IVR) System<br />
The Interactive Voice Response (IVR) system will give you direct telephonic access to claim<br />
<strong>in</strong>formation, Member eligibility <strong>in</strong>formation, and Member benefit <strong>in</strong>formation 24 hours/day, 7<br />
days/week. The IVR system uses voice recognition and/or touch tone <strong>in</strong>terfaces to connect you<br />
to the <strong>in</strong>formation you need, when you need it. IVR is a secure system that protects Members’<br />
Protected <strong>Health</strong> Information. Both provider and Member <strong>in</strong>formation is validated before<br />
provid<strong>in</strong>g self-service functionalities.<br />
GHO’s IVR system is available 24 hours/day, 7 days/week, and representatives are always<br />
available to assist you dur<strong>in</strong>g normal bus<strong>in</strong>ess hours.<br />
Self-service options available through IVR:<br />
‣ Claims Address – Provides mail<strong>in</strong>g address for claim submission<br />
‣ Claims Status – Verifies receipt of a claim, amount billed, claim process date, amount<br />
paid, to whom payment was made, Co<strong>in</strong>surance, Copayment and/or Deductible amounts<br />
as applicable, for services rendered by provider<br />
‣ Eligibility – Verify type of plan<br />
‣ Benefits – Verifies Primary Care <strong>Provider</strong> Copayment, Specialist Copayment,<br />
Emergency Room Copayment, In-Network Deductible per Member and In-Network<br />
Deductible per Family<br />
Pharmacy IVR:<br />
‣ FAX Pharmacy Authorization Form – Records request for WVUHS Formulary<br />
Exception/Prior Authorization Request Form<br />
‣ Pharmacy Location – Provides up to five participat<strong>in</strong>g pharmacy locations per zip code<br />
Information you’ll need when us<strong>in</strong>g IVR:<br />
‣ <strong>Provider</strong> 9-Digit Tax Identification Number<br />
‣ Member’s 11-digit Member Identification Number<br />
‣ Member’s First Name<br />
‣ Date of Service<br />
GHO CUSTOMER SERVICE: (866) 580-3531<br />
PRECERTIFICATION LINE<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
23
Record precertification details for planned admissions through the<br />
Medical Management IVR:<br />
Monday through Friday, 8:00 a.m. to 4:30 p.m.<br />
(800) 544-3907 or (570) 271-6497<br />
Information you’ll need when us<strong>in</strong>g Medical Management IVR:<br />
‣ Member’s 11-digit Member Identification Number<br />
‣ Member’s First Name<br />
‣ Date of Service<br />
‣ <strong>Provider</strong>’s Telephone Number<br />
‣ <strong>Provider</strong>’s Fax Number<br />
‣ <strong>Provider</strong>’s <strong>Full</strong> Name, <strong>in</strong>clud<strong>in</strong>g spell<strong>in</strong>g of Last Name<br />
‣ Date of planned Admission<br />
‣ Hospital or Facility Name<br />
‣ Diagnosis Code and Description<br />
‣ Procedure Code and Description<br />
All of the <strong>in</strong>formation available through the IVR system (except for precertification) is also<br />
available onl<strong>in</strong>e to Registered Participat<strong>in</strong>g <strong>Provider</strong>s at<br />
www.thehealthplan.com/wvuh_providers_us/.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – General Information<br />
24
Section 2: Precertification Requirements<br />
PRECERTIFICATION REQUIREMENTS...........................................................................................25<br />
Verification of Eligibility and Benefit Limit ................................................................................ 27<br />
Request<strong>in</strong>g Precertification........................................................................................................... 27<br />
1) Inpatient Hospitalization........................................................................................................... 27<br />
2) Skilled Level of Care Admissions............................................................................................ 29<br />
3) Home <strong>Health</strong>/Hospice, Home Infusion and Home Phlebotomy Services................................ 31<br />
4) Durable Medical Equipment (“DME”)..................................................................................... 34<br />
5) Outpatient Physical, Occupational and Speech Therapy Services ........................................... 34<br />
6) Other Services Requir<strong>in</strong>g Precertification................................................................................ 35<br />
7) Pharmacy WVUHS Formulary Precertification and non-WVUHS Formulary Exception<br />
Process .......................................................................................................................................... 36<br />
8) Specialty Drug List and Preferred Specialty Pharmacy ........................................................... 38<br />
SERVICES REQUIRING PROVIDER COORDINATION .................................................................39<br />
Outpatient Prescription Drugs....................................................................................................... 39<br />
Outpatient Laboratory Services .................................................................................................... 40<br />
Urgent/Emergency Services.......................................................................................................... 41<br />
Orthotic and Prosthetic Service .................................................................................................... 41<br />
Behavioral <strong>Health</strong> and Substance Abuse Services........................................................................ 42<br />
Outpatient Dialysis Services......................................................................................................... 42<br />
Experimental/Investigational or Unproven Services .................................................................... 42<br />
Transplant Services....................................................................................................................... 43<br />
Precertification Requirements<br />
Precertification is GHO’s response to <strong>in</strong>formation presented relat<strong>in</strong>g to a request for specified<br />
<strong>Health</strong> Care Services.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
25
Precertification does not guarantee a Member’s coverage or GHO payment.<br />
A Member’s coverage is pursuant to the terms and conditions of coverage set forth <strong>in</strong> a<br />
Member’s applicable Benefit Document. Precertification requirements may vary based on the<br />
Member’s applicable product l<strong>in</strong>e. Please contact the Customer Service Department (CST) for<br />
verification of precertification requirements (contact <strong>in</strong>formation available on follow<strong>in</strong>g page).<br />
A Member is not f<strong>in</strong>ancially responsible for a Participat<strong>in</strong>g <strong>Provider</strong>’s failure to (i) obta<strong>in</strong><br />
precertification, or (ii) provide required and accurate <strong>in</strong>formation to GHO.<br />
Copayments, Co<strong>in</strong>surance and/or Deductibles are the f<strong>in</strong>ancial responsibility of the Member,<br />
when applicable.<br />
Precertification Determ<strong>in</strong>ation and Communication Process<br />
Precertification may be performed by GHO Medical Management staff, or through delegated<br />
vendor relationships.<br />
Precertification staff, which <strong>in</strong>cludes appropriate practitioner reviewers, utilize nationally<br />
recognized medical guidel<strong>in</strong>es as well as <strong>in</strong>ternally developed medical benefit policies,<br />
<strong>in</strong>dividual assessment of the Member, and other resources to guide precertification, Concurrent<br />
Review, and retrospective review processes <strong>in</strong> accordance with the Member’s eligibility and<br />
benefits.<br />
Upon submission of required <strong>in</strong>formation, the Precertification staff will provide notification of<br />
determ<strong>in</strong>ation of coverage <strong>in</strong> accordance with regulatory timeframes.<br />
As it relates to urgent Concurrent Review approvals, GHO has an understand<strong>in</strong>g<br />
with Participat<strong>in</strong>g <strong>Provider</strong>s that, once approval has been given it rema<strong>in</strong>s <strong>in</strong> effect until GHO<br />
notifies the provider otherwise. This means that as Concurrent Review of care is ongo<strong>in</strong>g and<br />
the case cont<strong>in</strong>ues to meet criteria for approval, GHO does not provide repeated notices of<br />
approval. Participat<strong>in</strong>g <strong>Provider</strong>s will be notified every time a Concurrent Review results <strong>in</strong> a<br />
denial.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s are notified of any medical review denial(s) and are provided the<br />
opportunity to supply additional supportive <strong>in</strong>formation and discuss adverse decision(s) directly<br />
with an appropriate practitioner reviewer who made the <strong>in</strong>itial determ<strong>in</strong>ation; or reviewer<br />
available at a time convenient for the Participat<strong>in</strong>g <strong>Provider</strong>. The Participat<strong>in</strong>g <strong>Provider</strong>’s request<br />
to discuss the determ<strong>in</strong>ation is required to occur with<strong>in</strong> one (1) Bus<strong>in</strong>ess Day of GHO’s denial<br />
notification <strong>in</strong> order to meet str<strong>in</strong>gent regulatory timel<strong>in</strong>es for the generation of denial notices.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s are encouraged to notify the Member of a GHO's decision with<strong>in</strong><br />
the same Bus<strong>in</strong>ess Day of the decision notification from GHO to the Participat<strong>in</strong>g <strong>Provider</strong>.<br />
It's important that any discussion regard<strong>in</strong>g a GHO's decision be documented <strong>in</strong> the<br />
Member's medical record and should <strong>in</strong>clude key components, such as contact<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
26
person/Member's name, date of notification, GHO's decision, alternative plan of care, if<br />
applicable and Member's appeal opportunities.<br />
Medical Management’s IVR system is available 24 hours a day, 7 days a week at (800) 544-3907<br />
or (570) 271-6497. You will be prompted to say “admission” for calls perta<strong>in</strong><strong>in</strong>g to acute<br />
<strong>in</strong>patient precertification. Or say “other” if you are call<strong>in</strong>g for someth<strong>in</strong>g other than acute<br />
<strong>in</strong>patient precertification. The IVR system also allows you to make multiple precertification<br />
requests dur<strong>in</strong>g the same call.<br />
Contact the Medical Management Department at the number listed above for a list<strong>in</strong>g of<br />
delegated vendors and contact numbers.<br />
Verification of Eligibility and Benefit Limit<br />
Prior to coord<strong>in</strong>at<strong>in</strong>g <strong>Health</strong> Care Services, a Member’s eligibility and benefits should always be<br />
verified through the onl<strong>in</strong>e <strong>Provider</strong> Service Center at<br />
www.thehealthplan.com/wvuh_providers_us/ or by call<strong>in</strong>g the Customer Service Team.<br />
<strong>Provider</strong>s should contact GHO Customer Service Team to verify eligibility and benefits.<br />
GHO’s IVR system is available for provider use, 24 hours a day, 7 days a week. Our Customer<br />
Service Representatives are available to assist you dur<strong>in</strong>g normal bus<strong>in</strong>ess hours.<br />
GHO CUSTOMER SERVICE: (866) 580-3531<br />
The Customer Service Team telephone number is pr<strong>in</strong>ted on the reverse side of each Member<br />
Identification Card.<br />
Request<strong>in</strong>g Precertification<br />
Prior to an outpatient service or planned <strong>in</strong>patient admission, the admitt<strong>in</strong>g or treat<strong>in</strong>g<br />
Participat<strong>in</strong>g <strong>Provider</strong> is responsible for <strong>in</strong>itiat<strong>in</strong>g precertification by contact<strong>in</strong>g the Medical<br />
Management Department anytime at the telephone number listed below.<br />
Medical Management Department<br />
Precertification l<strong>in</strong>e is available 24 hours/day, 7 days/week<br />
(800) 544-3907 or (570) 271-6497<br />
Fax: (570) 214-6796<br />
1) Inpatient Hospitalization<br />
Requests for precertification of a planned <strong>in</strong>patient Hospital admission is the responsibility of the<br />
admitt<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong>.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
27
Please note:<br />
For assistance with mental health and substance abuse precertification, contact the Medical<br />
Management Department.<br />
For <strong>in</strong>patient rehabilitation admissions, refer to the Section titled “Inpatient Rehabilitation<br />
Admissions” with<strong>in</strong> this <strong>Guide</strong>.<br />
Copayments, Co<strong>in</strong>surance and/or Deductibles are the f<strong>in</strong>ancial responsibility of the<br />
Member, when applicable.<br />
Hospitals should verify authorization has occurred by contact<strong>in</strong>g either the admitt<strong>in</strong>g<br />
Participat<strong>in</strong>g <strong>Provider</strong> or GHO’s Medical Management Department.<br />
Inpatient admissions excluded from precertification:<br />
Emergency and/or Urgent Care <strong>in</strong>patient admissions, which may be an (i) admission from<br />
an emergency room that results <strong>in</strong> a direct admission, (ii) a direct admission from an<br />
ambulatory surgery center or (iii) an admission directly from a physician’s office.<br />
An <strong>in</strong>patient admission to a Hospital <strong>Provider</strong> where GHO is secondary to another payer<br />
who requires precertification and authorization has been obta<strong>in</strong>ed from the primary carrier.<br />
However, notification for Concurrent Review is required.<br />
A full term pregnancy with <strong>in</strong>tent to deliver, either vag<strong>in</strong>al or cesarean section<br />
Please note: Any other planned <strong>in</strong>patient Hospital admission dur<strong>in</strong>g the course of<br />
pregnancy requires precertification.<br />
A transfer from one Participat<strong>in</strong>g Hospital <strong>Provider</strong> to another Participat<strong>in</strong>g Hospital<br />
<strong>Provider</strong> where the first <strong>in</strong>patient admission was precertified and/or followed by GHO<br />
Concurrent Review for the same level of care.<br />
Retrieval of a Member from a non-participat<strong>in</strong>g facility to a Hospital <strong>Provider</strong> through<br />
GHO’s out-of-Network retrieval process. Transfer may only occur at such time when the<br />
Member’s condition has stabilized and the Member can be transported safely to a Hospital<br />
<strong>Provider</strong> without suffer<strong>in</strong>g detrimental consequences or aggravat<strong>in</strong>g the Member’s<br />
condition.<br />
Observation Services furnished by a Hospital <strong>Provider</strong> <strong>in</strong> an outpatient sett<strong>in</strong>g that <strong>in</strong>clude<br />
the use of a bed and periodic monitor<strong>in</strong>g by a Hospital <strong>Provider</strong>’s nurs<strong>in</strong>g or other staff and<br />
does not exceed a maximum of twenty-three (23) hours <strong>in</strong> duration.<br />
<strong>Plan</strong>ned Inpatient Admission: Precertification for a planned <strong>in</strong>patient Hospital admission is<br />
requested no less than two (2) Bus<strong>in</strong>ess Days prior to the planned date of admission.<br />
Please note: <strong>Plan</strong>ned admissions to an acute rehabilitation facility or rehabilitation unit with<strong>in</strong> a<br />
Hospital are considered <strong>in</strong>patient Hospital admissions and are subject to the precertification<br />
requirements listed <strong>in</strong> the Section titled “Inpatient Rehabilitation Admission” with<strong>in</strong> this <strong>Guide</strong>.<br />
Information Required when Request<strong>in</strong>g Precertification<br />
The follow<strong>in</strong>g <strong>in</strong>formation should be readily available when the admitt<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong><br />
<strong>in</strong>itiates the request for precertification:<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
28
Demographics (i.e., Member’s name, GHO Member identification number, admission<br />
date, admitt<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong>’s full name, name of Hospital <strong>Provider</strong> with<br />
requestor’s name, fax number and telephone number).<br />
Reason for Admission <strong>in</strong>clud<strong>in</strong>g all pert<strong>in</strong>ent diagnoses and applicable diagnosis codes.<br />
Procedure Scheduled, if applicable <strong>in</strong>clud<strong>in</strong>g procedure to be performed, procedure<br />
codes, and date scheduled (if available).<br />
Severity of Illness Indicators:<br />
o Cl<strong>in</strong>ical F<strong>in</strong>d<strong>in</strong>gs<br />
o Pert<strong>in</strong>ent Imag<strong>in</strong>g /ECG F<strong>in</strong>d<strong>in</strong>gs<br />
o Pert<strong>in</strong>ent Laboratory F<strong>in</strong>d<strong>in</strong>gs<br />
Intensity of Service Indicators:<br />
o Pert<strong>in</strong>ent Treatment/Medication Ordered, <strong>in</strong>clud<strong>in</strong>g frequency of adm<strong>in</strong>istration<br />
o Discharge <strong>Plan</strong>n<strong>in</strong>g/Case Management/Social Service’s Assessment and <strong>Plan</strong><br />
An <strong>in</strong>patient admission to a Participat<strong>in</strong>g <strong>Provider</strong> determ<strong>in</strong>ed cl<strong>in</strong>ically <strong>in</strong>appropriate by the<br />
Medical Director will be paid at an appropriate alternate level of care or denied completely.<br />
Concurrent Review<br />
Participat<strong>in</strong>g <strong>Provider</strong>s are requested to <strong>in</strong>itiate Concurrent Review telephonically with the<br />
Medical Management Department with<strong>in</strong> one (1) Bus<strong>in</strong>ess Day of an <strong>in</strong>patient admission. Each<br />
<strong>in</strong>patient admission is subject to the Concurrent Review process, <strong>in</strong>clud<strong>in</strong>g <strong>in</strong>stances where a<br />
case rate/MS-DRG may apply.<br />
Dur<strong>in</strong>g Concurrent Review, a determ<strong>in</strong>ation of cont<strong>in</strong>ued coverage and a subsequent assigned<br />
Concurrent Review date will be provided by the Medical Management Department staff. The<br />
follow<strong>in</strong>g <strong>in</strong>formation will be discussed dur<strong>in</strong>g the <strong>in</strong>itial Concurrent Review:<br />
verification of admission date and attend<strong>in</strong>g physician<br />
current <strong>in</strong>patient care needs<br />
plan of care<br />
overall goals and anticipated length of stay (if known), and<br />
discharge plann<strong>in</strong>g.<br />
2) Skilled Level of Care Admissions<br />
Please note:<br />
A three (3) day Hospital stay is not required by GHO prior to a skilled admission.<br />
Copayments, Co<strong>in</strong>surance and/or Deductibles are the f<strong>in</strong>ancial responsibility of the<br />
Member, when applicable.<br />
Information Required when Request<strong>in</strong>g Precertification<br />
The <strong>in</strong>formation below should be readily available when the accept<strong>in</strong>g SNF or Hospital<br />
<strong>Provider</strong> <strong>in</strong>itiates the request for precertification:<br />
Demographics: Member’s name, GHO identification number, admission date, admitt<strong>in</strong>g<br />
Participat<strong>in</strong>g <strong>Provider</strong>’s full name, SNF or Hospital <strong>Provider</strong> and Member’s PCP, with<br />
requestor’s name, fax number and telephone number.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
29
Reason for Admission: objective, subjective f<strong>in</strong>d<strong>in</strong>gs, and Member’s primary diagnosis.<br />
Cl<strong>in</strong>ical F<strong>in</strong>d<strong>in</strong>gs: current functional status and rehabilitative therapy evaluations or<br />
recommendations (if known).<br />
Previous Cl<strong>in</strong>ical F<strong>in</strong>d<strong>in</strong>gs: level of function<strong>in</strong>g and anticipated disposition (if known).<br />
Anticipated plan of care.<br />
Concurrent Review of a Skilled Admission<br />
Initial Concurrent Review: SNF or Hospital <strong>Provider</strong>s are required to <strong>in</strong>itiate Concurrent<br />
Review with the Medical Management Department staff with<strong>in</strong> two (2) Bus<strong>in</strong>ess Days of the<br />
skilled admission. All skilled admissions will be subject to the Concurrent Review process,<br />
<strong>in</strong>clud<strong>in</strong>g SNF admissions where GHO is not the Member’s primary <strong>in</strong>surance coverage, as well<br />
as a Member who transfers from one SNF or Hospital <strong>Provider</strong> to another SNF or Hospital<br />
<strong>Provider</strong>. Dur<strong>in</strong>g Concurrent Review, a determ<strong>in</strong>ation for cont<strong>in</strong>ued coverage at the appropriate<br />
level of care and a subsequent assigned Concurrent Review date will be provided by the Medical<br />
Management Department staff.<br />
The follow<strong>in</strong>g Member <strong>in</strong>formation will be discussed dur<strong>in</strong>g the <strong>in</strong>itial Concurrent Review:<br />
Verification of admission date and attend<strong>in</strong>g physician.<br />
Current skilled needs to <strong>in</strong>clude skilled nurs<strong>in</strong>g and/or therapies.<br />
Rehabilitative therapy evaluations and plan of care (if appropriate), and<br />
Overall goals and anticipated length of stay (if known).<br />
Subsequent Concurrent Review: Subsequent Concurrent Review is required to occur<br />
telephonically with the assigned Medical Management Department staff.<br />
The follow<strong>in</strong>g Member <strong>in</strong>formation will be discussed dur<strong>in</strong>g each subsequent<br />
Concurrent Review:<br />
Skilled nurs<strong>in</strong>g or therapy updates <strong>in</strong>clud<strong>in</strong>g quantitative progress toward goals (nurs<strong>in</strong>g<br />
notes, therapy notes or logs may be requested by the UM Department staff).<br />
A plan of care with anticipated disposition and estimated length of stay.<br />
SNF Services Requir<strong>in</strong>g Coord<strong>in</strong>ation<br />
Hospice Election: The SNF or Hospital <strong>Provider</strong> is requested to notify GHO’s Home<br />
<strong>Health</strong>/Hospice Management Department and Medical Management Department at (800)<br />
544-3907 immediately upon a Member’s decision to <strong>in</strong>voke their Hospice benefit.<br />
Personal Care Facility: GHO does not consider a Personal Care Facility (PCF) an<br />
<strong>in</strong>stitutionalized facility, regardless of a PCF’s affiliation with a SNF or Hospital <strong>Provider</strong>.<br />
A PCF is considered an alternative to home liv<strong>in</strong>g.<br />
Infusion Therapy Services: Participat<strong>in</strong>g <strong>Provider</strong>s are encouraged to refer to their<br />
Agreement for specific <strong>in</strong>formation regard<strong>in</strong>g the reimbursement <strong>in</strong>clusions/exclusions for<br />
<strong>in</strong>fusion therapy services. Questions regard<strong>in</strong>g <strong>in</strong>fusion therapy services should be<br />
reviewed dur<strong>in</strong>g the Concurrent Review process with the Medical Management<br />
Department.<br />
Mental <strong>Health</strong> and Substance Abuse Services: Participat<strong>in</strong>g <strong>Provider</strong>s may assist<br />
Members <strong>in</strong> obta<strong>in</strong><strong>in</strong>g authorization and coord<strong>in</strong>at<strong>in</strong>g mental health and substance abuse<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
30
services. Refer to the reverse side of the Member’s Identification Card or contact the<br />
Customer Service Team for further assistance.<br />
Laboratory/Pathology Services: All laboratory/pathology specimens for Members<br />
admitted to a SNF/Hospital under any level of care or PCF, must be forwarded to a<br />
Participat<strong>in</strong>g <strong>Provider</strong> for analysis.<br />
Outpatient Rehabilitative Therapy Services: Participat<strong>in</strong>g <strong>Provider</strong>s are encouraged to<br />
refer to their Agreement for specific <strong>in</strong>formation regard<strong>in</strong>g the <strong>in</strong>clusion/exclusion of<br />
outpatient physical, occupational or speech therapy services for Members orig<strong>in</strong>ally<br />
admitted under a skilled level of care, but no longer meet<strong>in</strong>g skilled criteria or who have<br />
exhausted their skilled level of care benefit.<br />
A Participat<strong>in</strong>g <strong>Provider</strong> with an Agreement which <strong>in</strong>cludes outpatient physical, occupational<br />
and speech therapy services should refer to the section of this <strong>Guide</strong> titled “Outpatient Physical,<br />
Occupational and Speech Therapy Services” for specific <strong>in</strong>struction regard<strong>in</strong>g GHO’s policy and<br />
procedure for coord<strong>in</strong>at<strong>in</strong>g outpatient rehabilitative therapy services.<br />
Precertification of outpatient physical, occupational and speech therapy services is the<br />
responsibility of the rehabilitative Participat<strong>in</strong>g <strong>Provider</strong> (or designee) render<strong>in</strong>g the service.<br />
Notification of a Non-Skilled Admission<br />
Prior to a non-skilled admission and aga<strong>in</strong> upon discharge of a Member, SNF or Hospital<br />
<strong>Provider</strong> accept<strong>in</strong>g the admission is required to notify the Medical Management Department.<br />
3) Home <strong>Health</strong>/Hospice, Home Infusion and Home Phlebotomy Services<br />
Precertification for Home <strong>Health</strong>/Hospice Services and/or home phlebotomy services is the sole<br />
responsibility of the render<strong>in</strong>g Home <strong>Health</strong>/ Hospice <strong>Provider</strong> or home phlebotomy<br />
Participat<strong>in</strong>g <strong>Provider</strong>.<br />
Please note:<br />
Certa<strong>in</strong> Home Infusion services may require precertification.<br />
Copayments, Co<strong>in</strong>surance and/or Deductibles are the f<strong>in</strong>ancial responsibility of the<br />
Member, when applicable.<br />
Hospice Election and Notice<br />
When a Member elects Hospice Services, the hospice must complete an election notice. In<br />
addition, the hospice must complete a change form when the election is for a patient who has<br />
changed an election from one hospice to another. The hospice provider is responsible for<br />
submitt<strong>in</strong>g all hospice forms to GHO.<br />
When hospice coverage is elected, the beneficiary waives all rights to standard coverage<br />
payments for services that are related to the treatment and management of his/her term<strong>in</strong>al illness<br />
dur<strong>in</strong>g any period his/her hospice benefit election is <strong>in</strong> force, except for professional services of<br />
an attend<strong>in</strong>g physician, which may <strong>in</strong>clude a nurse practitioner.<br />
To be covered, Hospice Services must be reasonable and necessary for the palliation or<br />
management of the term<strong>in</strong>al illness and related conditions. The <strong>in</strong>dividual must elect hospice<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
31
care and; a certification that the <strong>in</strong>dividual is term<strong>in</strong>ally ill must be completed by the patient’s<br />
attend<strong>in</strong>g physician (if there is one), and the Medical Director. Nurse practitioners serv<strong>in</strong>g as the<br />
attend<strong>in</strong>g physician may not certify or re-certify the term<strong>in</strong>al illness. A plan of care must be<br />
established before services are provided. To be covered, services must be consistent with the<br />
plan of care. Certification of term<strong>in</strong>al illness is based on the physician’s or medical director’s<br />
cl<strong>in</strong>ical judgment regard<strong>in</strong>g the normal course of an <strong>in</strong>dividual’s illness. It should be noted that<br />
predict<strong>in</strong>g life expectancy is not always exact.<br />
Home <strong>Health</strong>/Hospice Management Department Determ<strong>in</strong>ation<br />
Concurrent Review Process<br />
Concurrent Review is required on all Home <strong>Health</strong> Services. The Home <strong>Health</strong> <strong>Provider</strong> is<br />
required to contact the Home <strong>Health</strong>/Hospice Management Department Community Case<br />
Manager to provide cl<strong>in</strong>ical <strong>in</strong>formation <strong>in</strong>clud<strong>in</strong>g a Member’s treatment plan. Based on<br />
Concurrent Review, a determ<strong>in</strong>ation of cont<strong>in</strong>ued coverage will be provided by the Home<br />
<strong>Health</strong>/Hospice Management Department.<br />
Home phlebotomy services are discont<strong>in</strong>ued when concurrent Home <strong>Health</strong> Services end, unless<br />
unique circumstances warrant cont<strong>in</strong>ued consideration for coverage.<br />
The Home <strong>Health</strong>/Hospice Management Department utilizes nationally recognized guidel<strong>in</strong>es as<br />
well as <strong>in</strong>ternal medical benefit policies, and other resources to guide Concurrent Review and<br />
retrospective review processes <strong>in</strong> accordance with the Member’s applicable Benefit Document<br />
and eligibility.<br />
Home <strong>Health</strong>/Hospice <strong>Provider</strong> Responsibilities<br />
Participation <strong>in</strong> Scheduled Home <strong>Health</strong>/Hospice <strong>Provider</strong> Meet<strong>in</strong>gs: Home <strong>Health</strong>/Hospice<br />
<strong>Provider</strong> meet<strong>in</strong>gs are scheduled by the Home <strong>Health</strong>/Hospice Management Department <strong>in</strong><br />
regional locations to address changes, concerns and updated <strong>in</strong>formation. Home <strong>Health</strong>/Hospice<br />
<strong>Provider</strong>s are expected to have representation at each scheduled Home <strong>Health</strong>/Hospice <strong>Provider</strong><br />
meet<strong>in</strong>g.<br />
Home <strong>Health</strong>/Hospice <strong>Provider</strong>s Participate <strong>in</strong> Program Development: All Home<br />
<strong>Health</strong>/Hospice <strong>Provider</strong>s are required to periodically participate <strong>in</strong> the development of new<br />
programs to meet the needs of the Member population served by the Home <strong>Health</strong>/ Hospice<br />
Management Department. Such programs may require specialized care from the Home <strong>Health</strong>/<br />
Hospice <strong>Provider</strong>s for the program to produce positive quality outcomes. As these programs are<br />
developed, the Home <strong>Health</strong>/Hospice Management Department will release care guidel<strong>in</strong>es to<br />
the Home <strong>Health</strong>/Hospice <strong>Provider</strong>s that should be followed for GHO Members.<br />
Discharge Reports of Home <strong>Health</strong> and Hospice Services: As designated by the Home<br />
<strong>Health</strong>/Hospice Management Department, the Home <strong>Health</strong>/Hospice <strong>Provider</strong> will provide<br />
verbal or written periodic progress reports to the Home <strong>Health</strong>/Hospice Management Department<br />
for each Member under the Home <strong>Health</strong>/Hospice <strong>Provider</strong>’s care. In order to provide cont<strong>in</strong>uity<br />
of care, the Home <strong>Health</strong>/Hospice Management Department requires a discharge report via fax to<br />
the Home <strong>Health</strong> Hospice Management Department with<strong>in</strong> one week of discharge.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
32
Scope of Services: Home <strong>Health</strong> <strong>Provider</strong><br />
Home Skilled Nurs<strong>in</strong>g Services: Care provided <strong>in</strong> the home by physician-supervised skilled<br />
nurs<strong>in</strong>g personnel <strong>in</strong> accordance with recognized nurs<strong>in</strong>g standards of practice.<br />
Home Rehabilitative Services: Physical, occupational, and/or speech therapy services provided<br />
<strong>in</strong> the Member’s home.<br />
Home Medical Social Services: Any services provided by medical social workers made<br />
available by the Home <strong>Health</strong> <strong>Provider</strong> to assist the Member or his/her family <strong>in</strong> cop<strong>in</strong>g with a<br />
Member’s medical condition.<br />
Home <strong>Health</strong> Aide: Custodial nurs<strong>in</strong>g services consist<strong>in</strong>g of care provided <strong>in</strong> the home by home<br />
health aides.<br />
Influenza Vacc<strong>in</strong>ation: The <strong>in</strong>fluenza vacc<strong>in</strong>ation may be adm<strong>in</strong>istered to home-bound<br />
Members only.<br />
Home Phlebotomy Services: Laboratory services for Members meet<strong>in</strong>g homebound criteria as<br />
def<strong>in</strong>ed by GHO.<br />
Scope of Services: Hospice <strong>Provider</strong><br />
Payment for hospice agencies is a daily rate for each day a beneficiary is enrolled <strong>in</strong> the hospice<br />
benefit. The daily payments are made regardless of the amount of services furnished on a given<br />
day and are <strong>in</strong>tended to cover costs that the hospice <strong>in</strong>curs <strong>in</strong> furnish<strong>in</strong>g services identified <strong>in</strong><br />
patients’ care plans. Payments are made based on the level of care required by the beneficiary:<br />
<br />
<br />
<br />
<br />
Rout<strong>in</strong>e home care;<br />
Cont<strong>in</strong>uous home care;<br />
Inpatient respite care; and<br />
General <strong>in</strong>patient care.<br />
Payment for physicians’ adm<strong>in</strong>istrative and general supervisory activities is <strong>in</strong>cluded <strong>in</strong> the<br />
hospice payment rates. These activities <strong>in</strong>clude participat<strong>in</strong>g <strong>in</strong> the establishment, review and<br />
updat<strong>in</strong>g of plans of care, supervis<strong>in</strong>g care and services and establish<strong>in</strong>g govern<strong>in</strong>g policies.<br />
Where the service is considered a hospice service (i.e., a service related to the hospice patient’s<br />
term<strong>in</strong>al illness that was furnished by someone other than the designated “attend<strong>in</strong>g physician”<br />
[or a physician substitut<strong>in</strong>g for the attend<strong>in</strong>g physician]) the physician or other provider must<br />
look to the hospice for payment.<br />
Claims for all other services related to the term<strong>in</strong>al illness furnished by <strong>in</strong>dividuals or entities<br />
other than the designated attend<strong>in</strong>g physician will be denied. Such claims <strong>in</strong>clude bills for any<br />
DME, supplies or <strong>in</strong>dependently practic<strong>in</strong>g speech or physical therapists that are related to the<br />
term<strong>in</strong>al condition. These services are <strong>in</strong>cluded <strong>in</strong> the hospice rate and paid through the hospice<br />
provider.<br />
Hospice Admission Criteria<br />
Hospice eligibility is determ<strong>in</strong>ed after the referr<strong>in</strong>g physician verifies that Member’s life<br />
expectancy is less than six (6) months.<br />
Member chooses to accept Hospice.<br />
Hospice Services are provided by a Hospice <strong>Provider</strong>.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
33
Acknowledgment that Member understands Hospice Services, as outl<strong>in</strong>ed <strong>in</strong> the Hospice<br />
Election Form (Contact GHO by phone or check onl<strong>in</strong>e for form availability).<br />
Regular GHO benefits are waived for care related to the term<strong>in</strong>al illness diagnosis<br />
Member agrees to palliative care treatment.<br />
Hospice Discharge<br />
The Hospice <strong>Provider</strong> will discharge any Member from the hospice program, who, as determ<strong>in</strong>ed<br />
by the Hospice Medical Director and Hospice <strong>Provider</strong>, no longer meets the hospice admission<br />
criteria.<br />
4) Durable Medical Equipment (“DME”)<br />
Concurrent Review for outpatient DME Services are the sole responsibility of the render<strong>in</strong>g<br />
DME Participat<strong>in</strong>g <strong>Provider</strong>. DME Participat<strong>in</strong>g <strong>Provider</strong>s are required to submit the applicable<br />
precertification forms to the Medical Management department with<strong>in</strong> one (1) Bus<strong>in</strong>ess Day of<br />
receipt of a DME order even if Medical Necessity <strong>in</strong>formation is not yet available. This <strong>in</strong>cludes<br />
Urgent Care DME requests (i.e., oxygen) received dur<strong>in</strong>g non-bus<strong>in</strong>ess hours. A coverage<br />
decision is required <strong>in</strong> advance of release, delivery or purchase of DME, except <strong>in</strong> the case of<br />
after hours or weekend Urgent Care DME requests (i.e., oxygen). Items delivered prior to<br />
determ<strong>in</strong>ation of coverage by GHO require clear and detailed advance notice of potential cost<br />
with signature of <strong>in</strong>sured. No reimbursement will be provided for delivery of purchased items<br />
without such advance notice and signature.<br />
When a Member requires outpatient DME, a Participat<strong>in</strong>g <strong>Provider</strong> should issue a verbal or<br />
written order to a DME Participat<strong>in</strong>g <strong>Provider</strong> that <strong>in</strong>cludes the follow<strong>in</strong>g:<br />
Member Demographics: Member’s name, primary residence address, telephone number,<br />
and GHO identification number.<br />
Requested DME service/item.<br />
Cl<strong>in</strong>ical F<strong>in</strong>d<strong>in</strong>gs: Diagnosis and applicable diagnosis code.<br />
Prescrib<strong>in</strong>g or order<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong> name and telephone number.<br />
Anticipated duration of DME need.<br />
Additional cl<strong>in</strong>ical <strong>in</strong>formation to support request for DME.<br />
Consignment DME<br />
Consignment DME provided by a non-branch location (i.e., physician office stocked with DME<br />
by a DME Participat<strong>in</strong>g <strong>Provider</strong>) are limited to those approved <strong>in</strong> advance by the DME<br />
Management Department. No purchased items with value greater than $100 can be provided on a<br />
consignment basis. The scheduled delivery date should be the dispense date appear<strong>in</strong>g on the<br />
applicable precertification form(s). Consignment DME provided by a non-branch location is<br />
required to be submitted for retrospective review with<strong>in</strong> 30 days of issuance utiliz<strong>in</strong>g the<br />
applicable precertification form(s). The form must be clearly marked to show “consignment”<br />
with clear <strong>in</strong>dication of the date equipment was provided to the Member. Misrepresentation of<br />
issue date will result <strong>in</strong> denial of payment and the Member may not be held liable for payment <strong>in</strong><br />
these circumstances.<br />
5) Outpatient Physical, Occupational and Speech Therapy Services<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
34
Concurrent Review for outpatient rehabilitative Services are the sole responsibility of the<br />
render<strong>in</strong>g Outpatient Therapy Participat<strong>in</strong>g <strong>Provider</strong>.<br />
Please note:<br />
Concurrent Review is also required when GHO is not the Member’s primary <strong>in</strong>surance<br />
coverage or when workers’ comp or auto <strong>in</strong>surance may be primary.<br />
Co-payments, Co<strong>in</strong>surance and/or Deductibles are the f<strong>in</strong>ancial responsibility of the<br />
Member, when applicable.<br />
6) Other Services Requir<strong>in</strong>g Precertification<br />
Please note:<br />
Copayments, Co<strong>in</strong>surance and/or Deductibles are the f<strong>in</strong>ancial responsibility of the<br />
Member, when applicable.<br />
Other services requir<strong>in</strong>g precertification<br />
The list<strong>in</strong>g of other services requir<strong>in</strong>g precertification can be found on GHO’s Web site at<br />
www.thehealthplan.com/wvuh_providers_us/. This list<strong>in</strong>g is subject to change. A m<strong>in</strong>imum of<br />
thirty (30) days advance notice is provided to Participat<strong>in</strong>g <strong>Provider</strong>s regard<strong>in</strong>g changes to this<br />
list<strong>in</strong>g. Please contact the Medical Management Department if you have questions regard<strong>in</strong>g the<br />
precertification of a particular service, or refer to our onl<strong>in</strong>e list<strong>in</strong>g.<br />
Information required when request<strong>in</strong>g precertification<br />
Demographics: Member’s name, GHO identification number, admission date (if<br />
applicable), date of service, and <strong>Provider</strong> of service full name, Request<strong>in</strong>g physician with<br />
phone number and fax number.<br />
Reason for Service: objective and subjective f<strong>in</strong>d<strong>in</strong>gs.<br />
Pert<strong>in</strong>ent Treatment/Medication Ordered.<br />
If request is for utilization of a non-Participat<strong>in</strong>g <strong>Provider</strong>, submission should <strong>in</strong>clude<br />
specifics as to why the service is not obta<strong>in</strong>able from a Participat<strong>in</strong>g <strong>Provider</strong>. Any<br />
<strong>in</strong>formation submitted by hard copy should clearly identify the requestor’s name and<br />
contact <strong>in</strong>formation.<br />
Submission of photographs and/or medical records.<br />
Submission of photographs is considered confidential medical record <strong>in</strong>formation and<br />
should be forwarded to the above address <strong>in</strong> a sealed envelope labeled “CONFIDENTIAL<br />
MEDICAL RECORDS.”<br />
Upon submission of required <strong>in</strong>formation, the Medical Management Department will provide<br />
verbal and/or written notification of determ<strong>in</strong>ation of coverage relative to the precertification<br />
request <strong>in</strong> accordance with regulatory timeframes.<br />
It is the obligation of the Participat<strong>in</strong>g <strong>Provider</strong> to discuss all treatment alternatives and options<br />
with the Member. This should <strong>in</strong>clude a discussion of GHO approval process and the importance<br />
of identify<strong>in</strong>g the best alternatives for care. The optimal method for accomplish<strong>in</strong>g this is to<br />
<strong>in</strong>clude GHO <strong>in</strong> the review process prior to mak<strong>in</strong>g any arrangements. Failure to follow this<br />
process leads the Member and/or the Member’s family to hav<strong>in</strong>g <strong>in</strong>accurate expectations.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
35
7) Pharmacy WVUHS Formulary Precertification and non-WVUHS<br />
Formulary Exception Process<br />
GHO’s Pharmacy Department ma<strong>in</strong>ta<strong>in</strong>s a process by which <strong>Health</strong> Care <strong>Provider</strong>s can:<br />
Request precertification for medication(s) designated <strong>in</strong> the WVUHS Formulary by an<br />
asterisk (*) as requir<strong>in</strong>g such.<br />
Request a WVUHS Formulary exception for specific drugs, drugs used for an off-label<br />
purpose, and biologicals and medication(s) not <strong>in</strong>cluded <strong>in</strong> GHO’s then current WVUHS<br />
Formulary.<br />
Request<strong>in</strong>g Precertification<br />
<strong>Health</strong> Care <strong>Provider</strong>s can <strong>in</strong>itiate such requests by contact<strong>in</strong>g the Pharmacy<br />
Department by telephone, fax or written request at the follow<strong>in</strong>g:<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options<br />
Pharmacy Department<br />
100 North Academy Avenue<br />
Mail Code 32-46<br />
Danville, PA 17822<br />
Monday through Friday, 8:00 a.m. to 5:00 p.m.<br />
(800) 988-4861; Fax: (570) 271-5610<br />
Information required to process the request <strong>in</strong>cludes:<br />
Caller’s name and telephone number.<br />
Member’s GHO identification number and, if applicable medical record number.<br />
Prescrib<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong>’s name and telephone number.<br />
The medication requested.<br />
Support<strong>in</strong>g cl<strong>in</strong>ical rationale, which may <strong>in</strong>clude, but is not limited to, relevant pages from<br />
the medical record, laboratory studies, prior medication treatment history and other<br />
documentation, as determ<strong>in</strong>ed by GHO to be relevant.<br />
Step Therapy<br />
Some medications may require that other medications be tried prior to or concomitantly with the<br />
requested medication. The pharmacy claims system looks for a record of the required<br />
medications and if they are not found, medical documentation must be submitted show<strong>in</strong>g use of<br />
these medications or rationale for skipp<strong>in</strong>g the step therapy medications.<br />
Non-WVUHS Formulary Medication<br />
The WVUHS Formulary is designed to meet most therapeutic needs of the population served by<br />
WVUHS. Occasionally, because of allergy, therapeutic failure, or a specific diagnostic-related<br />
need, medications may not meet the special needs of an <strong>in</strong>dividual member. In these special<br />
<strong>in</strong>stances, the prescrib<strong>in</strong>g physician may make requests to the Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> Pharmacy<br />
Department for non-WVUHS Formulary or restricted medications. The prescrib<strong>in</strong>g physician<br />
will receive written documentation and/or a verbal response from the Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong><br />
Pharmacy Department regard<strong>in</strong>g the request.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
36
Prior Authorization<br />
To promote the most appropriate utilization, select medications may require prior authorization<br />
to be eligible for coverage under the member’s prescription benefit. In order for a member to<br />
receive coverage for a medication requir<strong>in</strong>g prior authorization, the prescrib<strong>in</strong>g physician must<br />
obta<strong>in</strong> prior authorization by contact<strong>in</strong>g the Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> Pharmacy Department at the<br />
address, telephone, or fax number above. Submission of medical documentation is required.<br />
Determ<strong>in</strong>ation Process<br />
WVUHS Formulary exception requests will be evaluated and a determ<strong>in</strong>ation of coverage made<br />
utiliz<strong>in</strong>g all the follow<strong>in</strong>g criteria:<br />
Member’s eligibility to receive requested services (enrollment <strong>in</strong> the plan, prescription<br />
drug coverage, specific exclusions <strong>in</strong> Member’s contract).<br />
Utilization of the requested agent for a cl<strong>in</strong>ically proven treatment <strong>in</strong>dication or diagnosis.<br />
Therapeutic failure, <strong>in</strong>tolerance or contra<strong>in</strong>dication to use of WVUHS Formulary agent<br />
and/or agents designated as therapeutically equivalent.<br />
Appropriateness of the non-WVUHS Formulary agent compared with available WVUHS<br />
Formulary agents, <strong>in</strong>clud<strong>in</strong>g but not limited to:<br />
a. Safety<br />
b. Efficacy<br />
c. Therapeutic advantage as demonstrated by head to head cl<strong>in</strong>ical trails<br />
d. Meets GHO criteria for drug or drug class WVUHS Formulary exception<br />
The prescrib<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong> will be contacted to review the request and available<br />
WVUHS Formulary alternatives. If an exception is still requested, appropriate medical record<br />
documentation and treatment <strong>in</strong>formation will be requested verbally and <strong>in</strong> writ<strong>in</strong>g. A due date<br />
for the required <strong>in</strong>formation (fifteen (15) days from the date of the request) will be <strong>in</strong>cluded <strong>in</strong><br />
the verbal and written notifications. When all requested <strong>in</strong>formation has been received, it will be<br />
attached to a flow sheet for documentation as a pre or post-service request.<br />
If the requested <strong>in</strong>formation is not received with<strong>in</strong> fifteen (15) days, the <strong>Health</strong> Care<br />
<strong>Provider</strong> will be contacted and a second request for <strong>in</strong>formation will be made both verbally<br />
and <strong>in</strong> writ<strong>in</strong>g. The date by which the <strong>in</strong>formation is required will be <strong>in</strong>cluded <strong>in</strong> the verbal<br />
and written request.<br />
If the required <strong>in</strong>formation is not received by the due date, a determ<strong>in</strong>ation of coverage will<br />
be rendered based on the <strong>in</strong>formation available. Requests for exception are reviewed and a<br />
determ<strong>in</strong>ation of coverage made with<strong>in</strong> a time frame <strong>in</strong> accordance with the follow<strong>in</strong>g:<br />
o When the request for coverage is related to an Urgent Care claim, a determ<strong>in</strong>ation<br />
of coverage will be made with<strong>in</strong> twenty-four (24) hours of receipt of all necessary<br />
<strong>in</strong>formation.<br />
o When the request for coverage is deemed to be a pre- service or post service, a<br />
determ<strong>in</strong>ation of coverage will be made with<strong>in</strong> forty-eight (48) hours of receipt of<br />
all necessary <strong>in</strong>formation.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
37
A GHO Pharmacist will perform the <strong>in</strong>itial review of the necessary <strong>in</strong>formation and assemble<br />
documents necessary to recommend a course of action. A licensed physician shall make the f<strong>in</strong>al<br />
decision <strong>in</strong> those <strong>in</strong>stances where a WVUHS Formulary exception decision results <strong>in</strong> a denial<br />
based on Medical Necessity and appropriateness. Based on the determ<strong>in</strong>ation of coverage made,<br />
one (1) of the follow<strong>in</strong>g will occur:<br />
If the WVUHS Formulary exception is approved:<br />
An electronic override will be entered <strong>in</strong>to the pharmacy claims adjudication system. The<br />
Member (or Member’s authorized representative) and provider will be notified of the<br />
determ<strong>in</strong>ation of coverage with<strong>in</strong> twenty-four (24) hours of decision be<strong>in</strong>g made.<br />
o At the time of notification, GHO will <strong>in</strong>dicate the coverage provided <strong>in</strong> the<br />
amount disclosed by GHO for the service requested.<br />
A written confirmation of the approval will be sent to the provider and Member with<strong>in</strong> two<br />
(2) days after the determ<strong>in</strong>ation of coverage is made.<br />
If the request for a WVUHS Formulary exception is denied, result<strong>in</strong>g <strong>in</strong> an adverse benefit<br />
determ<strong>in</strong>ation, the follow<strong>in</strong>g will occur:<br />
1. The <strong>Health</strong> Care <strong>Provider</strong> and Member (or Member’s authorized representative)<br />
will be verbally notified of the adverse determ<strong>in</strong>ation with<strong>in</strong> twenty-four (24)<br />
hours of the decision.<br />
2. This verbal notification will <strong>in</strong>clude <strong>in</strong>struction on how to <strong>in</strong>itiate a grievance and/<br />
or appeal process.<br />
3. The prescrib<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong> will be offered the opportunity to discuss<br />
the determ<strong>in</strong>ation of coverage with a GHO Pharmacist or Medical Director.<br />
4. The Member (or Member’s authorized representative) and <strong>Health</strong> Care <strong>Provider</strong><br />
will be sent confirmation of the adverse benefit determ<strong>in</strong>ation with<strong>in</strong> two (2) days<br />
of the decision be<strong>in</strong>g made. The written notification shall <strong>in</strong>clude; (1) the specific<br />
reason for the determ<strong>in</strong>ation, (2) the basis and cl<strong>in</strong>ical rationale utilized <strong>in</strong><br />
render<strong>in</strong>g the determ<strong>in</strong>ation of coverage, if applicable, (3) any <strong>in</strong>ternal policy or<br />
criterion applied, if applicable, (4) as well as <strong>in</strong>structions regard<strong>in</strong>g <strong>in</strong>itiation of<br />
the grievance and/or appeal process.<br />
WVUHS Formulary changes are available at www.thehealthplan.com/wvuh_providers_us/. A<br />
m<strong>in</strong>imum of thirty (30) days advance notice is provided to participat<strong>in</strong>g physicians regard<strong>in</strong>g<br />
WVUHS Formulary changes, except when the WVUHS Formulary change is due to the approval<br />
or withdrawal of a medication by the Food and Drug Adm<strong>in</strong>istration.<br />
8) Specialty Drug List and Preferred Specialty Pharmacy<br />
Certa<strong>in</strong> prescription and <strong>in</strong>jectable drugs are covered only through the preferred specialty<br />
pharmacy. The preferred specialty pharmacy is:<br />
Medical Center Pharmacy<br />
1 Medical Center Drive<br />
Morgantown, West Virg<strong>in</strong>ia 26506<br />
(304) 598-4848<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
38
Please contact Medical Center Pharmacy for all specialty vendor drug new starts. In the event<br />
that Medical Center Pharmacy is unable to obta<strong>in</strong> a specialty drug, they will contact GHO and<br />
arrangements will be made to obta<strong>in</strong> the drug from another source. For more detail and a<br />
complete list of specialty drugs, refer to www.thehealthplan.com/wvuh_providers_us/, or call the<br />
GHO Pharmacy department at (800) 988-4861. Medication requests are the responsibility of the<br />
prescrib<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong>.<br />
Please note: All specialty vendor drugs have a maximum of thirty (30) days supply per dispense<br />
unless otherwise noted.<br />
Medical Benefit Policies<br />
A medical policy is the written description of GHO’s position concern<strong>in</strong>g the use or application<br />
of a biologic, device, pharmaceutical, or procedure, based on any or all of the follow<strong>in</strong>g:<br />
Medicare guidel<strong>in</strong>es, cl<strong>in</strong>ical practice guidel<strong>in</strong>es, nationally accepted standards, and the f<strong>in</strong>d<strong>in</strong>gs<br />
and conclusions drawn from a complete Technology Assessment (TA). Additionally, a medical<br />
policy is an <strong>in</strong>formational resource that establishes the Medical Necessity criteria for the<br />
biologic, device, pharmaceutical, or procedure. It also functions as an <strong>in</strong>formational resource by<br />
describ<strong>in</strong>g any special requirements for claims process<strong>in</strong>g.<br />
New and revised medical benefit policies are communicated <strong>in</strong> GHO’s quarterly newsletter,<br />
Briefly. Briefly is accessible onl<strong>in</strong>e at www.thehealthplan.com/wvuh_providers_us/, or a hard<br />
copy may be obta<strong>in</strong>ed from your <strong>Provider</strong> Relations Representative.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s with questions about the above medical policies can contact the<br />
Medical Management Department at the number listed below:<br />
Monday through Friday 8:00 a.m. to 4:30 p.m.<br />
(800) 544-3907 or (570) 271-6497<br />
Fax: (570) 214-6796<br />
Services Requir<strong>in</strong>g <strong>Provider</strong> Coord<strong>in</strong>ation<br />
Verification of Eligibility and Benefit Limit<br />
Prior to coord<strong>in</strong>at<strong>in</strong>g <strong>Health</strong> Care Services, a Member’s eligibility and benefits should always be<br />
verified through the onl<strong>in</strong>e <strong>Provider</strong> Service Center at<br />
www.thehealthplan.com/wvuh_providers_us/ or by call<strong>in</strong>g the Customer Service Team.<br />
<strong>Provider</strong>s should contact GHO Customer Service Team correspond<strong>in</strong>g to the Member’s product<br />
type to verify eligibility and benefits:<br />
GHO’s IVR system is available for provider use, 24 hours a day, 7 days a week. Our Customer<br />
Service Representatives are available to assist you dur<strong>in</strong>g normal bus<strong>in</strong>ess hours.<br />
GHO CUSTOMER SERVICE: (866) 580-3531<br />
Outpatient Prescription Drugs<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
39
GHO utilizes the WVUHS Formulary for purposes of Member care through the rational selection<br />
and use of medications, and to ensure quality, cost-effective prescrib<strong>in</strong>g. The WVUHS<br />
Formulary is developed with the <strong>in</strong>put of practic<strong>in</strong>g physicians and pharmacists. Medications <strong>in</strong><br />
each therapeutic class have been reviewed for efficacy, safety, and cost. Ma<strong>in</strong>tenance of the<br />
WVUHS Formulary is a dynamic process; the Pharmacy and Therapeutics Committee<br />
cont<strong>in</strong>ually review new medications as well as <strong>in</strong>formation related to medications currently<br />
<strong>in</strong>cluded <strong>in</strong> the WVUHS Formulary.<br />
GHO ma<strong>in</strong>ta<strong>in</strong>s sole discretion of assign<strong>in</strong>g drugs to tiers and mov<strong>in</strong>g drugs from one tier to<br />
another. Several factors are considered when assign<strong>in</strong>g drugs to tiers.<br />
These factors <strong>in</strong>clude, but are not limited to:<br />
Availability of a generic equivalent.<br />
Cost of a drug.<br />
Cost of the drug relative to other drugs <strong>in</strong> the same therapeutic class.<br />
Availability of over-the-counter alternatives.<br />
Cl<strong>in</strong>ical and economic factors.<br />
Please note: A drug may change <strong>in</strong> tier status without notice due to immediate generic<br />
availability.<br />
Non-WVUHS Formulary medications: The WVUHS Formulary is designed to meet most<br />
therapeutic needs of the population served by GHO. Occasionally, because of allergy,<br />
therapeutic failure, or a specific diagnostic-related need, WVUHS Formulary medications may<br />
not meet the special needs of an <strong>in</strong>dividual Member. In these special <strong>in</strong>stances, the prescrib<strong>in</strong>g<br />
physician may make requests to GHO Pharmacy Department for non-WVUHS Formulary or<br />
restricted medications. The prescrib<strong>in</strong>g physician will receive written documentation and/or a<br />
verbal response from GHO Pharmacy Department regard<strong>in</strong>g the request. Under the triple choice<br />
plan, non-WVUHS Formulary medications not requir<strong>in</strong>g precertification will be available at the<br />
highest Copayment level.<br />
WVUHS Formulary addition requests: Requests for changes or additions to the WVUHS<br />
Formulary can be made by written request to GHO Pharmacy Department at the address listed<br />
below.<br />
Mail<strong>in</strong>g address:<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options<br />
Pharmacy Department<br />
Internal Mail Code: 32-46<br />
100 North Academy Avenue<br />
Danville, PA 17822<br />
(800) 988-4861; Fax: (570) 271-5610<br />
Outpatient Laboratory Services<br />
Outpatient laboratory services may be:<br />
Provided by the Member’s Participat<strong>in</strong>g <strong>Provider</strong>.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
40
Ordered by a Participat<strong>in</strong>g <strong>Provider</strong> who has been Directly Accessed by a Member <strong>in</strong><br />
accordance with the terms and conditions of coverage set forth <strong>in</strong> their Benefit<br />
Document(s).<br />
Please refer to GHO’s Participat<strong>in</strong>g <strong>Provider</strong> search at<br />
www.thehealthplan.com/wvuh_providers_us/ for a list of laboratory and radiology Participat<strong>in</strong>g<br />
<strong>Provider</strong>s.<br />
Urgent/Emergency Services<br />
A Member is directed to discuss their Emergency with their Participat<strong>in</strong>g <strong>Provider</strong> either prior to<br />
or follow<strong>in</strong>g their emergency room visit.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s agree to have Medical Services available and accessible to Members,<br />
twenty-four (24) hours per day, seven (7) days per week. When a Participat<strong>in</strong>g <strong>Provider</strong> is not<br />
available and accessible to Member, the Participat<strong>in</strong>g <strong>Provider</strong> is responsible for ensur<strong>in</strong>g<br />
appropriate arrangements are made for another Participat<strong>in</strong>g <strong>Provider</strong> to provide Medical<br />
Services to Member, <strong>in</strong> accordance GHO Access and Availability Standards.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s can utilize the follow<strong>in</strong>g to ensure Members have access to medical<br />
direction or care:<br />
An answer<strong>in</strong>g service that forwards callers (i.e., Members) directly to the Participat<strong>in</strong>g<br />
<strong>Provider</strong> or a designated cover<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong> for medical direction or care<br />
dur<strong>in</strong>g non-bus<strong>in</strong>ess hours.<br />
An answer<strong>in</strong>g device (i.e. voice mail, pager, answer<strong>in</strong>g mach<strong>in</strong>e, etc) that provides callers<br />
with a pre-recorded message direct<strong>in</strong>g the Member on how the Participat<strong>in</strong>g <strong>Provider</strong> or<br />
designated cover<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong> can be contacted for medical direction or care<br />
dur<strong>in</strong>g non-bus<strong>in</strong>ess hours.<br />
Any other delivery method that would provide the Member with direct access to a<br />
Participat<strong>in</strong>g <strong>Provider</strong> or designated cover<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong> with medical direction<br />
or care dur<strong>in</strong>g non-bus<strong>in</strong>ess hours.<br />
All out-of-Network services immediately follow<strong>in</strong>g an emergency department discharge or an<br />
<strong>in</strong>patient Hospital discharge, require precertification.<br />
Orthotic and Prosthetic Service<br />
An orthotic is a rigid appliance or apparatus used to support, align or correct bone and muscle<br />
deformities. Orthotic Devices range from arm sl<strong>in</strong>gs to corsets and f<strong>in</strong>ger spl<strong>in</strong>ts. They may be<br />
made from a variety of materials, <strong>in</strong>clud<strong>in</strong>g rubber, leather, canvas and plastic. A prosthetic is an<br />
appliance or apparatus that replaces a miss<strong>in</strong>g body part.<br />
When an orthotic or prosthetic has been determ<strong>in</strong>ed to be Medically Necessary, the prescrib<strong>in</strong>g<br />
Participat<strong>in</strong>g <strong>Provider</strong> should verify benefit and eligibility with the Customer Service Team and<br />
then issue a written prescription <strong>in</strong> the Member’s name for the applicable device. Written<br />
prescriptions issued by a Participat<strong>in</strong>g <strong>Provider</strong> for the Orthotic or Prosthetic Device should be<br />
kept on file <strong>in</strong> the Member’s medical record.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
41
Orthotic or Prosthetic Participat<strong>in</strong>g <strong>Provider</strong>s are located <strong>in</strong> “Orthotic or Prosthetic” section of<br />
GHO’s then-current <strong>Provider</strong> List or at www.thehealthplan.com/wvuh_providers_us/.<br />
Behavioral <strong>Health</strong> and Substance Abuse Services<br />
Participat<strong>in</strong>g <strong>Provider</strong>s should refer to the Member’s benefit document for <strong>in</strong>formation on<br />
behavioral health and substance abuse benefits. Inpatient and outpatient behavioral health and<br />
substance abuse services may require authorization. Participat<strong>in</strong>g <strong>Provider</strong>s may contact the<br />
Customer Service Team for assistance dur<strong>in</strong>g GHO’s normal bus<strong>in</strong>ess hours.<br />
Outpatient Dialysis Services<br />
To ensure that GHO receives accurate reimbursement for Members with a primary diagnosis of<br />
end-stage renal disease (ESRD) or has had a kidney transplant, GHO requests a copy of the<br />
completed CMS-2728-U3 form. This form should be completed by the treat<strong>in</strong>g nephrologist and<br />
the Facility Participat<strong>in</strong>g <strong>Provider</strong> render<strong>in</strong>g the outpatient dialysis services. Forms can be<br />
submitted via fax to the Customer Service Team at (866) 580-3531.<br />
Experimental/Investigational or Unproven Services<br />
Experimental, <strong>in</strong>vestigational or unproven services are any medical, surgical, psychiatric,<br />
substance abuse or other health care technologies, supplies, treatments, diagnostic procedures,<br />
drug therapies or devices that are determ<strong>in</strong>ed by GHO to be:<br />
Not approved by the U.S. Food and Drug Adm<strong>in</strong>istration (FDA) to be lawfully marketed<br />
for the proposed use, or not identified <strong>in</strong> the American Hospital Formulary Service as<br />
appropriate for the proposed use, and are referred to by the treat<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong><br />
as be<strong>in</strong>g <strong>in</strong>vestigational, experimental, research based or educational; or<br />
The subject of an ongo<strong>in</strong>g cl<strong>in</strong>ical trial that meets the def<strong>in</strong>ition of a Phase I, II, or III<br />
cl<strong>in</strong>ical trial set forth <strong>in</strong> the FDA regulation, regardless of whether the trial is subject to<br />
FDA oversight; or<br />
The subject of a written research or <strong>in</strong>vestigational treatment protocol be<strong>in</strong>g used by the<br />
treat<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong> or by another <strong>Health</strong> Care <strong>Provider</strong> who is study<strong>in</strong>g the same<br />
service.<br />
If the requested service is not represented by criteria listed above, GHO reserves the right to<br />
require demonstrated evidence available <strong>in</strong> the published, peer-reviewed medical literature. This<br />
demonstrated evidence should support:<br />
The service has a measurable, reproducible positive effect on health outcomes as<br />
evidenced by well designed <strong>in</strong>vestigations, and has been endorsed by national medical<br />
bodies, societies or panels with regard to the efficacy and rationale for use; and<br />
The proposed service is at least as effective <strong>in</strong> improv<strong>in</strong>g health outcomes as are<br />
established treatments or technologies or is applicable <strong>in</strong> cl<strong>in</strong>ical circumstances <strong>in</strong> which<br />
established treatments or technologies are unavailable or cannot be applied; and<br />
The improvement <strong>in</strong> health outcome is atta<strong>in</strong>able outside of the cl<strong>in</strong>ical <strong>in</strong>vestigation<br />
sett<strong>in</strong>g; and<br />
The majority of <strong>Health</strong> Care <strong>Provider</strong>s practic<strong>in</strong>g <strong>in</strong> the appropriate medical specialty<br />
recognize the service or treatment to be safe and effective <strong>in</strong> treat<strong>in</strong>g the particular medical<br />
condition for which it is <strong>in</strong>tended; and<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
42
The beneficial effect on health outcomes outweighs any potential risk or harmful effects.<br />
GHO reserves the right to make judgment regard<strong>in</strong>g coverage of experimental, <strong>in</strong>vestigational<br />
and/or unproven procedures and treatments. Participat<strong>in</strong>g <strong>Provider</strong>s are encouraged to contact the<br />
MM Department for precertification review as <strong>in</strong>dicated <strong>in</strong> the Section of this <strong>Guide</strong> titled “Other<br />
Medical Services Requir<strong>in</strong>g Precertification”.<br />
Transplant Services<br />
Members are required to utilize designated transplant centers. Precertification is required for<br />
transplant evaluations test<strong>in</strong>g and related services for organ, bone marrow and/or stem cell<br />
transplants. Participat<strong>in</strong>g <strong>Provider</strong>s should contact the Medical Management Department at (800)<br />
544-3907.<br />
Preventive Services<br />
In accordance with the Patient Protection and Affordable Care Act (PPACA), plans effective on<br />
or after September 23, 2010, must cover certa<strong>in</strong> preventive services without any Member costshar<strong>in</strong>g.<br />
GHO will abide by the PPACA’s regulations upon renewal, start<strong>in</strong>g October 1, 2010.<br />
Services requir<strong>in</strong>g coverage:<br />
Evidence-based services as def<strong>in</strong>ed by the United States Preventive Services Task<br />
Force (USPSTF) <strong>in</strong>clud<strong>in</strong>g screen<strong>in</strong>gs for diabetes, cholesterol, common cancers, and<br />
depression, as well as behavioral counsel<strong>in</strong>g for obesity, tobacco, and alcohol misuse.<br />
These preventive recommendations also <strong>in</strong>clude prescriptions for aspir<strong>in</strong> to prevent<br />
cardiovascular disease, iron supplementation for anemic children, fluoride for<br />
preschool children, and folic acid supplementation dur<strong>in</strong>g pregnancy.<br />
Immunizations for rout<strong>in</strong>e use <strong>in</strong> children, adolescents, and adults recommended by<br />
the Advisory Committee on Immunization Practices of the Centers for Disease<br />
Control and Prevention (ACIP).<br />
Preventive care and screen<strong>in</strong>gs for <strong>in</strong>fants, children, and adolescents supported by the<br />
<strong>Health</strong> Resources and Services Adm<strong>in</strong>istration (HRSA) <strong>in</strong>clud<strong>in</strong>g regular pediatrician<br />
visits, developmental assessments, various screen<strong>in</strong>gs, counsel<strong>in</strong>g, and much more.<br />
Preventive care and screen<strong>in</strong>gs for women supported by HRSA.<br />
For a comprehensive outl<strong>in</strong>e of recommended preventive services and l<strong>in</strong>ks to more detailed<br />
<strong>in</strong>formation, please visit:<br />
http://www.healthcare.gov/center/regulations/prevention/recommendations.html.<br />
Cost-shar<strong>in</strong>g:<br />
Generally, no Member cost-shar<strong>in</strong>g requirements will be imposed with respect to covered<br />
preventive services. Exceptions are as follows.<br />
Cost-shar<strong>in</strong>g will apply to preventive services rendered by a non-participat<strong>in</strong>g<br />
provider.<br />
Cost-shar<strong>in</strong>g will apply to office visits billed separately from the preventive service,<br />
or when the preventive service is not the primary purpose of the office visit.<br />
Cost-shar<strong>in</strong>g may apply to a treatment not described <strong>in</strong> the regulations even if that<br />
treatment results from a preventive service that is.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
43
Please note that GHO may use Medical Management processes to determ<strong>in</strong>e coverage of<br />
preventive services to the extent that they are not specified <strong>in</strong> the relevant recommendation or<br />
guidel<strong>in</strong>e.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Precertification Requirements<br />
44
Section 3: Reimbursement and Claim Submission<br />
GHO REIMBURSEMENT.......................................................................................................................46<br />
Payment Schedules ....................................................................................................................... 46<br />
Copayments/Co<strong>in</strong>surance and Deductibles................................................................................... 46<br />
Claim Submission ......................................................................................................................... 47<br />
GHO Explanation of Payment (EOP)........................................................................................... 47<br />
Electronic Claim Submission........................................................................................................ 47<br />
EDI Clear<strong>in</strong>ghouse Reports .......................................................................................................... 48<br />
Claim Report<strong>in</strong>g Requirements or <strong>Guide</strong>l<strong>in</strong>es.............................................................................. 48<br />
FOR PROFESSIONAL PROVIDERS ....................................................................................................49<br />
FOR ANCILLARY/FACILITY PROVIDERS.......................................................................................56<br />
<strong>Health</strong> Insurance Prospective Payment System (HIPPS) Codes Report<strong>in</strong>g Requirement............ 59<br />
Outpatient Hospital Revenue Code Report<strong>in</strong>g Requirements ...................................................... 59<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
45
GHO Reimbursement<br />
Participat<strong>in</strong>g <strong>Provider</strong>s are reimbursed for the provision of Medical Services to Members<br />
pursuant to the payment provisions of their Agreement. Participat<strong>in</strong>g <strong>Provider</strong>s may collect from<br />
Members, amounts for non-Covered Services, Copayments, Co<strong>in</strong>surance and/or Deductibles that<br />
may be due from Member <strong>in</strong> accordance with the Member’s Benefit Document. A Member’s<br />
cost shar<strong>in</strong>g amount appears on the Participat<strong>in</strong>g <strong>Provider</strong>’s explanation of payment (EOP)<br />
generated by GHO <strong>in</strong> response to reported services. GHO reimbursement <strong>in</strong> conjunction with<br />
applicable Member cost shar<strong>in</strong>g amounts for Covered Services constitutes payment <strong>in</strong> full. GHO<br />
will not use any f<strong>in</strong>ancial <strong>in</strong>centive that compensates a Participat<strong>in</strong>g <strong>Provider</strong> for provid<strong>in</strong>g less<br />
than Medically Necessary and appropriate care to a Member. The follow<strong>in</strong>g <strong>in</strong>formation<br />
provides an overview of fee-for-service payment methodology used to reimburse Participat<strong>in</strong>g<br />
<strong>Provider</strong>s. Participat<strong>in</strong>g <strong>Provider</strong>s should contact their designated <strong>Provider</strong> Relations<br />
Representative with any questions regard<strong>in</strong>g reimbursement.<br />
Please note: GHO coverage is subject to the Member’s eligibility and benefits as of the date of<br />
service.<br />
Payment Schedules<br />
Payment schedules are designed to allow competitive reimbursement appropriate to the cl<strong>in</strong>ical<br />
tra<strong>in</strong><strong>in</strong>g, expertise and credentials of Participat<strong>in</strong>g <strong>Provider</strong>s. GHO payment schedules reflect<br />
reimbursement rates for designated CPT®/HCPCS codes and are not a reflection of a Member’s<br />
benefit coverage. Reimbursement through a payment schedule is determ<strong>in</strong>ed by the services<br />
reported <strong>in</strong> accordance with the coverage outl<strong>in</strong>ed <strong>in</strong> the Member’s Benefit Document. Services<br />
determ<strong>in</strong>ed to be non-covered accord<strong>in</strong>g to such Benefit Documents are not reimbursable by<br />
GHO and are the f<strong>in</strong>ancial responsibility of the Member.<br />
HIPAA regulations require that GHO accept only valid ICD-9-CM and CPT®/HCPCS codes<br />
accord<strong>in</strong>g to the date of service reported. Participat<strong>in</strong>g <strong>Provider</strong>s should reference the applicable<br />
current cod<strong>in</strong>g manuals associated with the date of service to accurately report acceptable<br />
diagnoses and procedure code(s). Due to the potential cosmetic nature or limitation of benefits,<br />
certa<strong>in</strong> services and/or procedures represented on GHO’s payment schedule(s) may require<br />
precertification by GHO. Contact the Medical Management Department at (800) 544-3907 for<br />
assistance.<br />
Copayments/Co<strong>in</strong>surance and Deductibles<br />
Copayment, Co<strong>in</strong>surance and Deductible <strong>in</strong>formation is listed on the front of the Member<br />
Identification Card. Please refer to the “Current Benefit Information” section of the <strong>Provider</strong><br />
Information Center onl<strong>in</strong>e at www.thehealthplan.com/wvuh_providers_us/. Participat<strong>in</strong>g<br />
<strong>Provider</strong>s can also utilize GHO’s Explanation of Payment (EOP) to accurately determ<strong>in</strong>e a<br />
Member’s f<strong>in</strong>ancial responsibility. GHO’s EOP is also available onl<strong>in</strong>e to Participat<strong>in</strong>g <strong>Provider</strong>s<br />
registered for access to the <strong>Provider</strong> Service Center at<br />
www.thehealthplan.com/wvuh_providers_us/. GHO’s EOP will reflect the Member’s<br />
Copayment, Deductible and/or Co<strong>in</strong>surance amounts owed for the services reported. In addition,<br />
any service/charge determ<strong>in</strong>ed to be a Non-Covered Service <strong>in</strong> accordance with the Member’s<br />
Benefit Document, will be the Member’s f<strong>in</strong>ancial responsibility.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
46
Participat<strong>in</strong>g <strong>Provider</strong>s are required to notify Members of credit balances and/or provide refunds<br />
of such credit balances to the Member that were a result of the Participat<strong>in</strong>g <strong>Provider</strong>’s collection<br />
of amounts not owed by Member for Covered Services.<br />
Claim Submission<br />
Participat<strong>in</strong>g <strong>Provider</strong>s are required to submit claims to GHO for all services rendered to<br />
Members. Claims must be submitted <strong>in</strong> accordance with GHO’s then current claim submission<br />
processes, which may be amended from time to time, and are required to be submitted<br />
electronically through an approved clear<strong>in</strong>ghouse vendor; or if a provider does not have the<br />
capability to submit claim forms electronically, claims may be submitted us<strong>in</strong>g a CMS-1500 or<br />
UB-04 claim form.<br />
A CMS-1500 or UB-04 claim form is required to <strong>in</strong>clude the applicable data elements as listed <strong>in</strong><br />
this section and current cod<strong>in</strong>g conventions, such as the then current CPT® and/or HCPCS Level<br />
II procedure codes, revenue codes, ICD-9-CM diagnosis cod<strong>in</strong>g to the highest level of<br />
specificity, as applicable to the diagnosis, for all services reported.<br />
All paper claims should be submitted to:<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options or Claims Adm<strong>in</strong>istrator<br />
P.O. Box 8200<br />
Danville, PA 17821-8200<br />
GHO Explanation of Payment (EOP)<br />
An EOP (Contact GHO by phone or check onl<strong>in</strong>e for form availability) is returned to<br />
Participat<strong>in</strong>g <strong>Provider</strong>s list<strong>in</strong>g services reported on the claim form. GHO’s payment will be the<br />
contractual allowance for Covered Services and will be reflected <strong>in</strong> the column titled<br />
“AMOUNT PAID”. The amount paid reflects the contractual allowance less any Member costshar<strong>in</strong>g.<br />
A Member’s cost shar<strong>in</strong>g amount is reflected <strong>in</strong> the column titled “AMOUNT<br />
DED&COPAY”. This amount is the f<strong>in</strong>ancial responsibility of the Member. The column titled<br />
“EXPLAIN CODES” represent additional <strong>in</strong>formation related to the claim or l<strong>in</strong>e item and<br />
should be reviewed to determ<strong>in</strong>e whether additional action is necessary.<br />
Claim Submission Do’s<br />
Submit 90% or more of your claims electronically to GHO.<br />
Medical documentation should be attached beh<strong>in</strong>d the claim form.<br />
The primary <strong>in</strong>surance carrier’s EOP should be attached beh<strong>in</strong>d the claim form.<br />
Use the <strong>Provider</strong> Service Center to determ<strong>in</strong>e a claims status.<br />
Claim Submission Don'ts<br />
Do not staple separate claim forms together.<br />
Electronic Claim Submission<br />
Participat<strong>in</strong>g <strong>Provider</strong>s should utilize GHO’s Electronic Data Interchange program (EDI) to<br />
submit claims and Member encounter data electronically to GHO. In order to receive payment<br />
for Medical Services, Participat<strong>in</strong>g <strong>Provider</strong> should forward all claims electronically to GHO <strong>in</strong> a<br />
format as may be required by the <strong>Health</strong> Insurance Portability and Accountability Act<br />
(“HIPAA”) or other regulation and <strong>in</strong> accordance with GHO’s policies and procedures.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
47
Participat<strong>in</strong>g <strong>Provider</strong>s should use GHO’s electronic portal as the primary source for obta<strong>in</strong><strong>in</strong>g<br />
the status of any claim submitted for payment.<br />
Prior to <strong>in</strong>itiat<strong>in</strong>g electronic claim transactions with GHO, our Electronic Data Interchange (EDI)<br />
Enrollment Form must be fully processed. The EDI Enrollment Form is available on GHO’s<br />
Website at www.thehealthplan.com/wvuh_providers_us/, or by contact<strong>in</strong>g your <strong>Provider</strong><br />
Relations Representative. When the EDI Enrollment Form is completed <strong>in</strong> its entirety, it should<br />
be submitted, either via facsimile or US Mail, to the follow<strong>in</strong>g:<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options<br />
CSST/EDI Enrollment 32-27<br />
100 North Academy Avenue<br />
Danville PA 17821-3227<br />
Fax: (570) 271-5341<br />
When the EDI Enrollment Form has been fully processed, you will receive email notification to<br />
beg<strong>in</strong> bill<strong>in</strong>g electronically, us<strong>in</strong>g your National <strong>Provider</strong> Identifier (NPI). Formatt<strong>in</strong>g<br />
specifications are outl<strong>in</strong>ed <strong>in</strong> the Companion <strong>Guide</strong> (also available at<br />
www.thehealthplan.com/wvuh_providers_us/).<br />
GHO has contracted with Emdeon and Relay <strong>Health</strong>, who receive and send electronic<br />
transactions on our behalf. For further <strong>in</strong>formation regard<strong>in</strong>g Emdeon, please contact them<br />
directly at (800) 735-8254 or onl<strong>in</strong>e at www.webmdenvoy.com; Relay <strong>Health</strong> at (800) 527-8133<br />
or onl<strong>in</strong>e at www.relayhealth.com.<br />
GHO strongly encourages its EDI enrollees to ensure that their claim submission software<br />
vendor/bill<strong>in</strong>g company has taken all necessary steps to confirm all required data elements are<br />
captured and populat<strong>in</strong>g <strong>in</strong> accordance with applicable GHO Companion Document.<br />
NPI numbers (type 1 and 2) are required on all electronic claims submissions.<br />
EDI Clear<strong>in</strong>ghouse Reports<br />
Understand<strong>in</strong>g and us<strong>in</strong>g clear<strong>in</strong>ghouse reports is crucial for ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g and manag<strong>in</strong>g<br />
electronic claims. These reports conta<strong>in</strong> concise <strong>in</strong>formation regard<strong>in</strong>g the status of electronic<br />
claims, identify<strong>in</strong>g those that have been accepted and those that need to be resubmitted.<br />
A claim reported electronically is not considered received by GHO until it has been accepted <strong>in</strong>to<br />
its claim process<strong>in</strong>g system. Please contact Emdeon or Relay <strong>Health</strong> to receive and review the<br />
necessary reports to track your electronic claims and to ensure that they have been submitted and<br />
processed properly.<br />
Questions related to GHO’s electronic claim submission process and procedures should be<br />
directed to your <strong>Provider</strong> Relations Representative.<br />
Claim Report<strong>in</strong>g Requirements or <strong>Guide</strong>l<strong>in</strong>es<br />
The follow<strong>in</strong>g shall function as an <strong>in</strong>formational resource that describes GHO’s requirements for<br />
professional and facility type claim submission, process<strong>in</strong>g, and reimbursement. Please note:<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
48
Cod<strong>in</strong>g conventions, such as CPT®/HCPCS, ICD-9-CM, revenue codes referenced throughout<br />
this <strong>Guide</strong> are subject to change when published for release by Medicare and/or various<br />
organizations. Participat<strong>in</strong>g <strong>Provider</strong>s should always utilize the then current procedural codes, as<br />
applicable, and the then current ICD-9-CM diagnosis cod<strong>in</strong>g to the highest level of specificity, as<br />
applicable to the diagnosis, for all services reported.<br />
For Professional <strong>Provider</strong>s<br />
Anesthesiology<br />
CPT ® procedure codes 00100 through 01992 should be used to report the adm<strong>in</strong>istration of<br />
anesthesia.<br />
Anesthesia Participat<strong>in</strong>g <strong>Provider</strong>s are required to report the applicable anesthesia procedure<br />
code modifier to identify the render<strong>in</strong>g provider. Anesthesia services reported without the<br />
appropriate anesthesia modifiers will be denied. Anesthesia modifiers, <strong>in</strong>clude the follow<strong>in</strong>g:<br />
AA: Anesthesia services performed personally by an anesthesiologist<br />
AD: Medical supervision by a physician: more than four concurrent anesthesia procedures<br />
QK: Medical direction of two, three, or four concurrent anesthesia procedures <strong>in</strong>volv<strong>in</strong>g<br />
qualified <strong>in</strong>dividuals<br />
QX: CRNA service: with medical direction by a physician<br />
QY: Medical direction of one CRNA by an anesthesiologist<br />
QZ: CRNA without medical direction by a physician<br />
Anesthesia<br />
For anesthesiology services related to the extraction of partially or totally bony impacted third<br />
molars, report the anesthesiology procedures codes (D9220 and D9221), when applicable.<br />
Anesthesia Base Units<br />
The American Society of Anesthesiologists (ASA) has assigned base value units to each<br />
anesthesia procedure code to reflect the difficulty of the anesthesia service, <strong>in</strong>clud<strong>in</strong>g the unusual<br />
pre-operative and post- operative care and evaluation. Additional units are not recognized for the<br />
Member’s age, physical status or unusual risk.<br />
Anesthesia Time<br />
Anesthesia time starts when the anesthesia provider beg<strong>in</strong>s to prepare the Member for the<br />
<strong>in</strong>duction of anesthesia <strong>in</strong> the operat<strong>in</strong>g room (or equivalent area) and ends when the provider is<br />
no longer <strong>in</strong> personal attendance. An anesthesia provider is def<strong>in</strong>ed as a physician who performs<br />
anesthesia services alone, a Certified Registered Nurse Anesthetist (CRNA) who is not medically<br />
directed or a CRNA who is medically directed.<br />
When report<strong>in</strong>g anesthesia adm<strong>in</strong>istration services, the time reported should represent the<br />
cont<strong>in</strong>uous actual presence of the anesthesiologist or CRNA. The total elapsed time (m<strong>in</strong>utes)<br />
should be reported <strong>in</strong> Block 24G of the CMS 1500 Claim Form.<br />
If the m<strong>in</strong>utes reported grossly exceed the national average for the procedure performed,<br />
progress notes are required to be submitted. Reimbursement for anesthesia adm<strong>in</strong>istration<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
49
services is based on the base unit value assigned to the procedure code, the total m<strong>in</strong>utes reported<br />
and the payment schedule anesthesia conversion factor.<br />
In <strong>in</strong>stances where anesthesia services are performed by a CRNA medically directed by an<br />
anesthesiologist, the CRNA will receive 50% of the total reimbursement rate and the<br />
anesthesiologist will receive 50% of the total reimbursement rate. Reimbursement will not<br />
exceed 100% of the total reimbursement rate regardless of how anesthesia services are rendered.<br />
When multiple surgical procedures are performed dur<strong>in</strong>g a s<strong>in</strong>gle anesthetic adm<strong>in</strong>istration, the<br />
anesthesia code represent<strong>in</strong>g the most complex procedure is reported. The time reported is the<br />
comb<strong>in</strong>ed total for all procedures.<br />
Anesthesia Bill<strong>in</strong>g for Canceled Anesthesia<br />
To report canceled anesthesia after the pre-op exam but before the Member is prepared for<br />
surgery, providers should report the applicable evaluation and management procedure code.<br />
To report canceled anesthesia after the patient has been prepared for surgery but before<br />
<strong>in</strong>duction, providers should report the applicable anesthesia adm<strong>in</strong>istration code with the<br />
appropriate anesthesia procedure code modifier and modifier -53 to <strong>in</strong>dicate the service was<br />
discont<strong>in</strong>ued.<br />
To report canceled anesthesia after <strong>in</strong>duction, providers should report the applicable anesthesia<br />
adm<strong>in</strong>istration code with the appropriate anesthesia procedure code modifier and the total<br />
elapsed time (m<strong>in</strong>utes).<br />
Assistant at Surgery Services<br />
Report one of the follow<strong>in</strong>g modifiers as appropriate to the situation:<br />
80 – Assistant Surgeon<br />
81 – M<strong>in</strong>imum Assistant Surgeon<br />
82 – Assistant Surgeon (when qualified resident surgeon not available)<br />
The <strong>Health</strong> <strong>Plan</strong> does not separately reimburse physician assistants (PA), nurse practitioners<br />
(NP) and/or cl<strong>in</strong>ical nurse specialists (CNS) for assistant at surgery services. The <strong>Health</strong> <strong>Plan</strong><br />
requests that Participat<strong>in</strong>g <strong>Provider</strong>s not submit claims for these provider types. However, if such<br />
services must be reported, the follow<strong>in</strong>g must be present on the claim:<br />
The supervis<strong>in</strong>g physician name must be listed <strong>in</strong> Field 31 on the CMS1500 Claim Form.<br />
Modifier –AS must be appended to the services reported as be<strong>in</strong>g rendered by a PA, NP or<br />
CNS.<br />
Do not use modifier –80, -81, or –82 to represent non-physician assistant at surgery<br />
services.<br />
Consultation<br />
GHO will reimburse appropriately coded consultations. Cod<strong>in</strong>g guidel<strong>in</strong>es for report<strong>in</strong>g<br />
consultation codes are as follows:<br />
A request for a consultation from an appropriate source and the reason for the<br />
consultation must be documented <strong>in</strong> the patient’s medical record.<br />
The consultant’s op<strong>in</strong>ion and any services that were ordered or performed must also be<br />
documented <strong>in</strong> the patient’s medical record.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
50
Communication back to the request<strong>in</strong>g physician must be by written report and<br />
documented <strong>in</strong> the medical record.<br />
History <strong>in</strong>cludes: Must have three (3) of three (3) documented <strong>in</strong> the progress notes to<br />
meet consultation guidel<strong>in</strong>es:<br />
o HPI – History of Present Illness<br />
o ROS – Review of Systems<br />
o PFSH – Past, Family, Social History<br />
Exam<strong>in</strong>ation: Must document all that is pert<strong>in</strong>ent to the nature of the present<strong>in</strong>g problem<br />
and cl<strong>in</strong>ical judgment.<br />
Medical decision mak<strong>in</strong>g: Must have three (3) of three (3) documented <strong>in</strong> the progress<br />
notes to meet consultation guidel<strong>in</strong>es:<br />
o Number of diagnosis or treatment options<br />
o Amount or complexity of data reviewed, <strong>in</strong>clud<strong>in</strong>g old records, or <strong>in</strong>formation<br />
from another physician. Review<strong>in</strong>g lab and radiology results.<br />
o Risks of complications and/or morbidity or mortality, <strong>in</strong>clud<strong>in</strong>g but not limited to:<br />
medication(s) ordered, whether you are schedul<strong>in</strong>g surgery, or have performed a<br />
m<strong>in</strong>or surgery <strong>in</strong> the office.<br />
Complete documentation of the patient consultation is required. Without such documentation<br />
upon request of GHO, the consults level may be lowered or changed to a different evaluation and<br />
management code. CMS has created modifier AI (Pr<strong>in</strong>cipal Physician of Record) to be used to<br />
dist<strong>in</strong>guish the physician who oversees the Member's care from all other physicians who may be<br />
furnish<strong>in</strong>g specialty care. The modifier should be appended to the evaluation and management<br />
procedure code only. There is no reimbursement tied to the AI modifier.<br />
Locum Tenens<br />
Locum Tenens provide temporary coverage when physicians are unavailable, or if a site requires<br />
additional staff<strong>in</strong>g. When a locum tenens covers for a Member’s designated attend<strong>in</strong>g physician,<br />
the services of the locum tenens are to be billed by the designated attend<strong>in</strong>g physician. The Q6<br />
modifier is required when report<strong>in</strong>g services rendered by a locum tenens provider. Field 31 on<br />
the CMS1500 Claim Form must reflect the designated physician’s name.<br />
Immunizations<br />
Immunizations for the purpose of travel, employment, sports camp, education, <strong>in</strong>surance,<br />
marriage or adoption are generally excluded from coverage as <strong>in</strong>dicated <strong>in</strong> the Member’s Benefit<br />
Document(s).<br />
Mastectomy Bra Bill<strong>in</strong>g <strong>Guide</strong>l<strong>in</strong>es<br />
Participat<strong>in</strong>g <strong>Provider</strong>s should follow Medicare's bill<strong>in</strong>g guidel<strong>in</strong>es when submitt<strong>in</strong>g claims for<br />
mastectomy bra prostheses, as follows:<br />
Participat<strong>in</strong>g <strong>Provider</strong>s should have the Member sign an Advance Beneficiary Notice of<br />
Non-Coverage (ABN) form and reta<strong>in</strong> on file. If an ABN is not on file, Participat<strong>in</strong>g<br />
<strong>Provider</strong> will be held accountable for the balance.<br />
Claim should be submitted us<strong>in</strong>g code L8000 with GA modifier that <strong>in</strong>dicates the waiver<br />
of liability is on file.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s can bill the Member for the cost difference between GHO's<br />
reimbursement for the standard device and the upgraded bra only. Participat<strong>in</strong>g<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
51
<strong>Provider</strong>s cannot bill the Member for charges related to shipp<strong>in</strong>g and handl<strong>in</strong>g, labor<br />
and/or overhead.<br />
Maternity Care and Delivery<br />
When a solo Participat<strong>in</strong>g <strong>Provider</strong> or participat<strong>in</strong>g group practice, which the Participat<strong>in</strong>g<br />
<strong>Provider</strong> is a part of, provides the antepartum, delivery and postpartum care, the appropriate<br />
“Global OB CPT® code” should be reported on the CMS1500 Claim Form (e.g., 59400, 59510,<br />
59610). Please note: Field 24A on the CMS1500 Claim Form is required to <strong>in</strong>dicate the delivery<br />
date <strong>in</strong> both the “from” and “to” Fields.<br />
When only antepartum care was provided, follow the guidel<strong>in</strong>es listed below. Do not report<br />
antepartum care separately when the Participat<strong>in</strong>g <strong>Provider</strong> is part of a group practice or cover<strong>in</strong>g<br />
practice that has or will be provid<strong>in</strong>g the delivery.<br />
Services for Members seen by a Participat<strong>in</strong>g <strong>Provider</strong> for seven (7) or more antepartum<br />
care visits should be reported with CPT® code 59426 <strong>in</strong> Field 24D with a unit of one (1)<br />
reported <strong>in</strong> Field 24G on the CMS 1500 Claim Form.<br />
Services for Members seen by a Participat<strong>in</strong>g <strong>Provider</strong> for four (4) to six (6) antepartum<br />
care visits should be reported with CPT® code 59425 <strong>in</strong> Field 24D with a unit of one (1)<br />
<strong>in</strong> Field 24G on the CMS 1500 Claim Form.<br />
Please note: When report<strong>in</strong>g CPT® code 59425 or 59426, Field 24A on the CMS1500 Claim<br />
Form, Participat<strong>in</strong>g <strong>Provider</strong> should <strong>in</strong>dicate the last date the Member was seen by the<br />
Participat<strong>in</strong>g <strong>Provider</strong> for antepartum care <strong>in</strong> both the “from” and “to” Fields. CPT® codes<br />
59425 and 59426 may not be reported more than one (1) time per Member, per pregnancy.<br />
Individual antepartum care visits must be documented <strong>in</strong> the Member’s medical record.<br />
In accordance with standard CPT® guidel<strong>in</strong>es, if a Member is seen by a Participat<strong>in</strong>g <strong>Provider</strong><br />
for antepartum care less than four (4) times, <strong>in</strong>dicate the appropriate evaluation and management<br />
(E&M) code for each <strong>in</strong>dividual visit. Report E&M code(s) <strong>in</strong> Field 24D with a unit of one (1)<br />
for each <strong>in</strong>dividual date of service <strong>in</strong> Field 24G on the CMS 1500 Claim Form.<br />
When multiple birth delivery was provided, follow the guidel<strong>in</strong>es listed below. GHO provides<br />
additional reimbursement for multiple vag<strong>in</strong>al birth deliveries dur<strong>in</strong>g a s<strong>in</strong>gle pregnancy.<br />
However, antepartum and postpartum care services will be reimbursed one (1) time per<br />
pregnancy.<br />
Vag<strong>in</strong>al tw<strong>in</strong> delivery cod<strong>in</strong>g example: 59400 Tw<strong>in</strong> A-rout<strong>in</strong>e obstetric care <strong>in</strong>clud<strong>in</strong>g<br />
antepartum care, vag<strong>in</strong>al delivery, and postpartum care. 59409-51 Tw<strong>in</strong> B-vag<strong>in</strong>al<br />
<br />
delivery only.<br />
Multiple cesarean birth deliveries should be reported with one of the appropriate CPT®<br />
code (e.g., 59510, 59414, 59515) and a unit of one (1) reported <strong>in</strong> Field 24G on the CMS<br />
1500 Claim Form.<br />
Claims for newborns should be submitted to GHO us<strong>in</strong>g the newborn’s member identification<br />
number, not that of a parent.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
52
Appropriate Modifier Usage<br />
Per CPT guidel<strong>in</strong>e, a modifier provides the means by which the report<strong>in</strong>g physician can <strong>in</strong>dicate<br />
that a service or procedure that has been performed has been altered by some specific<br />
circumstance but not changed <strong>in</strong> its def<strong>in</strong>ition or code. Invalid procedure code and modifier<br />
comb<strong>in</strong>ations will be denied as such and a corrected claim will be needed to process the service.<br />
J & Q Code Modifier <strong>Guide</strong>l<strong>in</strong>e<br />
HCPCS Level II - J & Q codes are used to report drugs that ord<strong>in</strong>arily cannot be selfadm<strong>in</strong>istered<br />
and should be reported us<strong>in</strong>g the appropriate dosage adm<strong>in</strong>istered. It is not<br />
appropriate to append anatomical site modifiers to these services.<br />
Global versus Technical/Professional <strong>Guide</strong>l<strong>in</strong>es<br />
<strong>Provider</strong>s should not append the -TC modifier to procedure codes that aptly describe and<br />
represent only the technical component of a procedure or service. Also, providers should not<br />
append the -26 modifier to procedure codes that aptly describe and represent only the<br />
professional component of a procedure or service. Inappropriate report<strong>in</strong>g of such services with<br />
a -TC or -26 modifier will be denied as an <strong>in</strong>valid procedure code/modifier comb<strong>in</strong>ation.<br />
Modifier –25 <strong>Guide</strong>l<strong>in</strong>es<br />
Modifier –25 is used to report a significant separately identifiable evaluation and management<br />
(E&M) service that was performed by the same physician on the same day of the procedure or<br />
other service. Modifier-25 may be reported with an E&M code on the day a procedural service<br />
was performed and the physician <strong>in</strong>dicates the Member’s condition required a significantly<br />
separately identifiable service from the procedure(s) performed that day or the E&M was above<br />
and beyond the usual pre-procedure or post-procedure case that is associated with the<br />
procedure(s) performed.<br />
The E&M service may be prompted by the condition or symptom for which the procedure was<br />
provided. Different diagnoses are not required for report<strong>in</strong>g the E&M on the same date as the<br />
procedure. Participat<strong>in</strong>g <strong>Provider</strong>s are advised that an E&M reported with modifier –25 that has<br />
a diagnosis the same as, or related, to the diagnosis reported for the procedure may require<br />
medical documentation to support payment. GHO will review and determ<strong>in</strong>e the relatedness of<br />
the diagnosis codes reported and approve for payment or deny accord<strong>in</strong>gly. <strong>Provider</strong>s are<br />
encouraged to submit paper claims with medical documentation when report<strong>in</strong>g an E&M service<br />
with modifier-25 and a procedure on the same date of service when the diagnosis codes<br />
reported are the same or related.<br />
Medical record documentation should provide clear evidence that the E&M service is above and<br />
beyond the exam component <strong>in</strong>herent to the reported procedure(s) or that the E&M is a<br />
significant, separately identifiable service.<br />
If medical documentation does not support the criteria, the E&M service will be denied.<br />
Additionally, <strong>in</strong>sufficient documentation (i.e., the E&M level of service reported is not supported<br />
by the medical record, the record does not support that a separate service was provided) will<br />
result <strong>in</strong> denial of the E&M.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
53
Please note: A Member’s office visit Copayment is not applicable when a reported E&M service<br />
is denied. Additionally, GHO conducts retrospective audits, which may <strong>in</strong>clude E&M services<br />
reported with modifier-25 on the same day as a procedure when the diagnosis codes are dist<strong>in</strong>ct<br />
or unrelated.<br />
Modifier –50 <strong>Guide</strong>l<strong>in</strong>es<br />
Participat<strong>in</strong>g <strong>Provider</strong> render<strong>in</strong>g bilateral procedures performed dur<strong>in</strong>g the same operative<br />
session should report modifier “-50” follow<strong>in</strong>g the appropriate CPT® code. The unit reported <strong>in</strong><br />
Field 24G on the CMS 1500 Claim Form should equal one (1). GHO reimbursement for bilateral<br />
procedures is calculated us<strong>in</strong>g 150% of GHO payment schedule amount, tak<strong>in</strong>g <strong>in</strong>to<br />
consideration any multiple surgery reduction adjustments.<br />
Multiple Surgical Procedures<br />
When more than one surgical procedure is performed dur<strong>in</strong>g a s<strong>in</strong>gle operative session, the full<br />
fee schedule payment amount will be made for the primary procedure. All applicable procedures<br />
performed dur<strong>in</strong>g the same operative session are paid at a 50 % reduction. This discount reflects<br />
the sav<strong>in</strong>gs realized by prepar<strong>in</strong>g the patient only once and the <strong>in</strong>cremental cost associated with<br />
anesthesia, operat<strong>in</strong>g and recovery room use, and other services required for the second and<br />
subsequent procedures.<br />
New Technology or Unusual and Rare Procedures<br />
Participat<strong>in</strong>g <strong>Provider</strong>s should contact the Medical Management Department at (800) 544-3907<br />
to ensure a Medical Necessity review is conducted prior to render<strong>in</strong>g an unusual, rare or new<br />
technological procedure. Pert<strong>in</strong>ent <strong>in</strong>formation should <strong>in</strong>clude a def<strong>in</strong>ition or description of the<br />
nature, extent and need for the procedure, and the time, effort and equipment necessary to<br />
provide the service. Additionally, the follow<strong>in</strong>g may be required, complexity of symptoms, f<strong>in</strong>al<br />
diagnosis, pert<strong>in</strong>ent physical f<strong>in</strong>d<strong>in</strong>gs, diagnostic/therapeutic procedures, concurrent problems (if<br />
known), and follow up care.<br />
Once the procedure is deemed payable, GHO will determ<strong>in</strong>e the reimbursement rate accord<strong>in</strong>g to<br />
standard <strong>in</strong>dustry reimbursement methodologies.<br />
Outpatient Hyperbaric Oxygen Therapy Services (HBO)<br />
HBO Therapy is a modality <strong>in</strong> which the entire body is exposed to oxygen under <strong>in</strong>creased<br />
atmospheric pressure.<br />
Outpatient claims for HBO therapy are billed us<strong>in</strong>g HCPCS code C1300 to <strong>in</strong>dicate a 30-m<strong>in</strong>ute<br />
session <strong>in</strong> the hyperbaric oxygen chamber. Facilities should report any surgical procedure for<br />
wound care with revenue code 761 (Treatment room) with a correspond<strong>in</strong>g CPT/HCPCS code<br />
that represents the surgical procedure <strong>in</strong> addition to the hyperbaric oxygen services.<br />
Outpatient Rehabilitative Services<br />
Physical medic<strong>in</strong>e/rehabilitation and special otorh<strong>in</strong>olaryngologic encounter based CPT® codes<br />
(i.e. 92507, 97001, 97003) are designed to be reported with one (1) unit per date of service<br />
regardless of the length of visit/treatment time.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
54
Outpatient rehabilitative therapy services Participat<strong>in</strong>g <strong>Provider</strong>s are required to report the<br />
applicable then current modifier to identify the render<strong>in</strong>g provider. Services reported without the<br />
appropriate modifiers will be denied and should be corrected prior to resubmission. Applicable<br />
modifiers, <strong>in</strong>clude the follow<strong>in</strong>g:<br />
GN: Service delivered personally by a speech language pathologist or under an outpatient<br />
speech language pathology plan of care.<br />
GO: Service delivered personally by an occupational therapist or under an outpatient<br />
occupational therapy plan of care.<br />
GP: Services delivered personally by a physical therapist or under an outpatient physical<br />
therapy plan of care.<br />
Professional Site of Service Payment Differential<br />
Site of service payment differential is a reimbursement methodology utilized by Medicare and<br />
other health <strong>in</strong>surance payors to ma<strong>in</strong>ta<strong>in</strong> equity of reimbursement for certa<strong>in</strong> services when<br />
performed <strong>in</strong> different sett<strong>in</strong>gs (i.e., physician’s office, hospital, ambulatory surgery center, etc.).<br />
GHO may apply this reimbursement methodology to certa<strong>in</strong> services as deemed appropriate.<br />
Skilled Nurs<strong>in</strong>g Care<br />
Participat<strong>in</strong>g <strong>Provider</strong>s are required to report the place of service code 31 (skilled nurs<strong>in</strong>g<br />
facility) or 32 (nurs<strong>in</strong>g facility) <strong>in</strong> Field 24B on the CMS 1500 Claim Form when render<strong>in</strong>g<br />
services to Members <strong>in</strong> a Skilled Nurs<strong>in</strong>g Facility (SNF).<br />
Unattended Electrical Stimulation Therapy<br />
HCPCS codes G0281 and G0283 are required to be utilized when report<strong>in</strong>g “unattended<br />
electrical stimulation therapy” <strong>in</strong> any sett<strong>in</strong>g. CPT® code 97014 is not accepted by GHO for the<br />
report<strong>in</strong>g of “unattended electrical stimulation therapy”. In accordance with standard cod<strong>in</strong>g<br />
guidel<strong>in</strong>e, G0282 should be utilized to report wound care services not previously described <strong>in</strong><br />
G0281. Coverage for such services reported under G0282 are based on the Medical Necessity<br />
and/or the benefits specifically outl<strong>in</strong>ed <strong>in</strong> the each Member’s applicable Benefit Document(s)<br />
and may be considered non-covered.<br />
Unlisted Service or Procedure<br />
At times, a service or procedure may need to be reported as “not otherwise specified”, “unlisted”<br />
or “unclassified”. This dist<strong>in</strong>ction occurs when a valid description and code does not exist <strong>in</strong> the<br />
current cod<strong>in</strong>g manuals for the service rendered. For example: J3490 ”unclassified drugs” is<br />
used when a valid drug “J code” has not been established.<br />
In this circumstance, the appropriate “unlisted” or “unclassified” code may be used to report the<br />
service provided. Medical documentation is required for each “unlisted” or “unclassified” code<br />
reported to GHO. If medical documentation is not submitted, the service reported as “unlisted”<br />
or “unclassified” cannot accurately be reviewed for coverage aga<strong>in</strong>st a Member’s Benefit<br />
Document, which may result <strong>in</strong> an unnecessary denial or delay <strong>in</strong> reimbursement. Because<br />
unlisted/unclassified codes could represent more than one service or procedure, GHO’s payment<br />
schedules do not <strong>in</strong>clude reimbursement rates for “unlisted” or “unclassified” codes. Once the<br />
“unlisted” or “unclassified” code/procedure/service is determ<strong>in</strong>ed to be payable, GHO will<br />
determ<strong>in</strong>e the reimbursement rate accord<strong>in</strong>g to the contract.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
55
Well-Child Office Visits<br />
No Member Copayment is required for well-child office visits. Well-child office visits, through<br />
21 years of age, can be coded by us<strong>in</strong>g one of the applicable preventive CPT codes, 99381 to<br />
99385 or 99391 to 99395 with the applicable diagnosis. Please note: The CPT code<br />
correspond<strong>in</strong>g to the age of the child at the time of the visit should be reported. If you utilize a<br />
regular Evaluation and Management code to report the visit, you must also report the appropriate<br />
preventive diagnosis code V20.2, V20.31, V20.32 and V70.0.<br />
Wisdom Teeth Extraction<br />
Participat<strong>in</strong>g <strong>Provider</strong>s report<strong>in</strong>g the extraction of partially or totally bony impacted third molars<br />
to GHO should utilize HCPCS codes D7230 & D7240. For anesthesiology services related to the<br />
extraction of partially or totally bony impacted third molars, report the anesthesiology<br />
procedures codes (D9220 and D9221), when applicable.<br />
For Ancillary/Facility <strong>Provider</strong>s<br />
Ambulance Services<br />
Ambulance transportation services Participat<strong>in</strong>g <strong>Provider</strong>s are required to use the applicable<br />
ambulance services modifiers. There are s<strong>in</strong>gle alpha characters with dist<strong>in</strong>ct def<strong>in</strong>itions that are<br />
paired together to form a two-character modifier. The first character <strong>in</strong>dicates the orig<strong>in</strong>ation of<br />
the Member (e.g., Member’s home, physician office, etc.) and the second character <strong>in</strong>dicates the<br />
dest<strong>in</strong>ation of the Member (e.g., hospital, skilled nurs<strong>in</strong>g facility, etc.). When report<strong>in</strong>g<br />
ambulance services, the name of the hospital or facility may be <strong>in</strong>cluded <strong>in</strong> Field 32 of the CMS<br />
1500 Claim Form. If report<strong>in</strong>g the scene of an accident or acute event as the orig<strong>in</strong> of the<br />
Member, a written description of the actual location of the scene or the event may be <strong>in</strong>cluded <strong>in</strong><br />
Field 32 of the CMS 1500 Claim Form.<br />
D: Diagnostic or therapeutic site/free stand<strong>in</strong>g facility (i.e., dialysis center, radiation<br />
therapy center) other than “P” or “H”<br />
E: Nurs<strong>in</strong>g home<br />
G: Hospital-based dialysis facility (hospital or hospital-associated)<br />
H: Hospital-<strong>in</strong>patient/outpatient<br />
I: Site of transfer (e.g., airport or hospital pad) between modes of transfer<br />
J: Non-hospital based dialysis facility<br />
N: Skilled nurs<strong>in</strong>g facility<br />
P: Physician office<br />
R: Private residence<br />
S: Scene of accident or acute event<br />
X: Intermediate stop at physician’s office on the way to the hospital (Dest<strong>in</strong>ation code<br />
only)<br />
Please note: When the orig<strong>in</strong> or dest<strong>in</strong>ation is a rehabilitation facility, hospital based nurs<strong>in</strong>g<br />
facility or sw<strong>in</strong>g bed, modifier “N” should be utilized. The zip code of the po<strong>in</strong>t of pick up<br />
should be reported <strong>in</strong> Field 23 of CMS 1500 Claim Form.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
56
Ambulance transportation services Participat<strong>in</strong>g <strong>Provider</strong>s are required to <strong>in</strong>clude the applicable<br />
place of service code (e.g., 41 [land] or 42 [air]) on the CMS1500 Claim Form <strong>in</strong> Field 24B.<br />
Ambulatory Surgical Services For Outpatient Hospital Report<strong>in</strong>g<br />
Charges should be comb<strong>in</strong>ed and reported via revenue code 360, when report<strong>in</strong>g general<br />
ambulatory surgical care services (revenue code 490) and operat<strong>in</strong>g room services (revenue code<br />
360).<br />
Case Rate Payments for Readmissions Related to an Orig<strong>in</strong>al Admission<br />
Inpatient claims for readmission of a Member to the same Hospital <strong>Provider</strong> less than 31 days<br />
from the discharge are subject to review by GHO or its review organization, when it appears the<br />
two admissions could be related. If it is determ<strong>in</strong>ed that the readmission was Medically<br />
Necessary and related to the orig<strong>in</strong>al admission, payment will be adjusted to reimburse a s<strong>in</strong>gle<br />
case rate payment.<br />
Diagnosis Related Group (MS-DRG)<br />
GHO utilizes the applicable MS-DRG software to calculate and assign the appropriate MS-DRG<br />
for <strong>in</strong>patient acute care claims regardless of payment terms. GHO and/or its designated agent<br />
will conduct MS-DRG validation audits to ensure accuracy of the <strong>in</strong>formation reported by<br />
Participat<strong>in</strong>g <strong>Provider</strong>s to retrospectively ensure the accuracy of the payment made to the<br />
facility. All requests to provide medical records associated with facilities services must be<br />
promptly returned to GHO with<strong>in</strong> the timel<strong>in</strong>e <strong>in</strong>dicated on the request.<br />
Durable Medical Equipment (DME) Services<br />
DME Participat<strong>in</strong>g <strong>Provider</strong>s are required to report services with the applicable modifiers. For<br />
example: 22 Unusual Procedural Service, NU new equipment (purchased), MS ma<strong>in</strong>tenance and<br />
service, RR rental rate, UE used rate.<br />
DME Participat<strong>in</strong>g <strong>Provider</strong>s submitt<strong>in</strong>g hard copy claims to GHO are required to report the full<br />
rental period beg<strong>in</strong>n<strong>in</strong>g with the start to the end date <strong>in</strong> Field 24A. Electronically submitted<br />
claims should reflect the rental period end date <strong>in</strong> Field 24A.<br />
Please note: Claims should not be submitted nor will claims be accepted until the rental cycle’s<br />
end date has passed.<br />
Home <strong>Health</strong>/Hospice Prior Authorization Number<br />
Home <strong>Health</strong>/Hospice <strong>Provider</strong>s must submit the precertification number assigned by the Home<br />
<strong>Health</strong>/Hospice Management Department <strong>in</strong> Field 63 on the UB-04 Claim Form.<br />
Hospice <strong>Provider</strong>s are required to list the hours of cont<strong>in</strong>uous care <strong>in</strong> Field 46 on the UB-04<br />
Claim Form.<br />
Observation Services<br />
Observation Services should be reported us<strong>in</strong>g revenue code 762. Revenue codes 760, 761 and<br />
769 are not appropriate for report<strong>in</strong>g Observation Services to GHO and will not be considered<br />
for reimbursement. The applicable units of service (total bed hours) must accompany revenue<br />
code 762 to <strong>in</strong>dicate the total number of Observation Service hours rendered. The units of service<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
57
should be reported <strong>in</strong> whole hours as follows:<br />
Partial hours less than or equal to 30 m<strong>in</strong>utes should be rounded down to the nearest hour;<br />
and<br />
Partial hours greater than 30 m<strong>in</strong>utes should be rounded up to the nearest hour.<br />
When report<strong>in</strong>g Observation Services that were provided to a Member who was subsequently<br />
admitted to the same Hospital <strong>Provider</strong> as the Observation Services, such services are required to<br />
be reported us<strong>in</strong>g revenue code 762 as described above. Such Observation Services are not<br />
separately reimbursed as outpatient services but may be considered as the first day of the<br />
<strong>in</strong>patient reimbursement.<br />
Outpatient Services Prior to an Admission<br />
Certa<strong>in</strong> outpatient preadmission services furnished by a Hospital (or an entity wholly owned<br />
and/or operated by the Hospital) to a Member up to 3 days before the Member’s admission are<br />
<strong>in</strong>cluded <strong>in</strong> the <strong>in</strong>patient payment*. If outpatient services are diagnostic or related to the Hospital<br />
admission, the services/charges are to be <strong>in</strong>cluded on the <strong>in</strong>patient claim. Services that are<br />
subject to the payment w<strong>in</strong>dow (and covered under the <strong>in</strong>patient payment) <strong>in</strong>clude all diagnostic<br />
services and those non-diagnostic outpatient services that are related to the admission.<br />
Ma<strong>in</strong>tenance dialysis and ambulance services are excluded.<br />
*Applicable on all Member admissions when GHO reimburses the Participat<strong>in</strong>g <strong>Provider</strong> based<br />
on a case rate <strong>in</strong>patient payment methodology.<br />
Skilled Nurs<strong>in</strong>g Care<br />
UB-04 claim forms must reflect the appropriate discharge status code <strong>in</strong> Field 22 and appropriate<br />
date range <strong>in</strong> Field 6. For example: If the through date on the claim is 1/31/08 and the discharge<br />
status is 30 (still an <strong>in</strong>patient), but the Member was actually discharged on 1/31/08, the claim<br />
will be denied.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s can submit multiple skilled levels of care on a s<strong>in</strong>gle claim. Intermediate<br />
Care and skilled care, however, cannot be billed together. Separate claims are required.<br />
Participat<strong>in</strong>g <strong>Provider</strong>s should <strong>in</strong>dicate the skilled level of care <strong>in</strong> Field 84 (Remarks) on the UB-<br />
04 Claim Form.<br />
Therapies rendered while the Member is <strong>in</strong> a skilled level of care are <strong>in</strong>cluded <strong>in</strong> the per diem<br />
payment. A separate claim form should not be generated.<br />
Please note: GHO does not reimburse for the day of discharge.<br />
Never Events/Hospital Acquired Conditions (HAC) / Present on Admission Indicators<br />
(POA)<br />
GHO has developed policies that address the quality of care and improve the medical safety of<br />
its Members to reduce avoidable medical errors. These policies address Never Events, Hospital<br />
Acquired Conditions and the report<strong>in</strong>g of Present on Admission <strong>in</strong>dicators.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
58
Never Events are def<strong>in</strong>ed as rare medical errors such as surgery performed on the wrong body<br />
part, leav<strong>in</strong>g a foreign object <strong>in</strong>side a patient after surgery, or an <strong>in</strong>fant discharged to the wrong<br />
person.<br />
Hospital Acquired conditions are def<strong>in</strong>ed as conditions which could reasonably have been<br />
prevented through application of evidence-based guidel<strong>in</strong>es. These conditions are not present<br />
when patients are admitted to a hospital, but present dur<strong>in</strong>g the course of the stay.<br />
Present on Admission <strong>in</strong>dicators are used to identify a condition that is present at the time the<br />
order for <strong>in</strong>patient admission occurs. Conditions that develop dur<strong>in</strong>g an outpatient encounter,<br />
<strong>in</strong>clud<strong>in</strong>g the emergency department, observation or outpatient surgery, are considered as Present<br />
on Admission.<br />
GHO will follow CMS guidel<strong>in</strong>es and process claims <strong>in</strong> a similar manner and reserves the right<br />
to withhold payment or a portion thereof for services associated with a Never Event and/or an<br />
HAC. We encourage you to view our medical policies onl<strong>in</strong>e at GHO’s web site,<br />
www.thehealthplan.com/wvuh_providers_us/ for additional <strong>in</strong>formation on this subject.<br />
<strong>Health</strong> Insurance Prospective Payment System (HIPPS) Codes Report<strong>in</strong>g<br />
Requirement<br />
HIPPS five digit alpha-numeric codes conta<strong>in</strong> a specific set of patient characteristics (or case<br />
mix). The first three positions of the code represent the Resource Utilization Group (RUG) case<br />
mix group and the last two represent the Assessment Indicator.<br />
For purposes of bill<strong>in</strong>g applicable HIPPS codes, please follow these <strong>in</strong>structions:<br />
Place HIPPS codes <strong>in</strong> data element SV202 on electronic 837 <strong>in</strong>stitutional claims transactions or<br />
<strong>in</strong> Field 44 (HCPCS/rate) on a paper UB-04 claims form. The associated revenue code is placed<br />
<strong>in</strong> data element SV201 or <strong>in</strong> Field 42. In certa<strong>in</strong> circumstances, multiple HIPPS codes may<br />
appear on separate l<strong>in</strong>es of a s<strong>in</strong>gle claim. Claims submitted without this data element will be<br />
considered <strong>in</strong>complete.<br />
Outpatient Hospital Revenue Code Report<strong>in</strong>g Requirements<br />
Please Note:<br />
Report services rendered to the highest level of specificity supported by the Member’s<br />
medical record.<br />
Failure to submit a CPT®/HCPCS code with the revenue codes listed below will result <strong>in</strong><br />
denial of that l<strong>in</strong>e item.<br />
GHO requires professional services to be reported on a CMS1500 Claim Form.<br />
CPT®/HCPCS codes identify<strong>in</strong>g professional services are denied when reported on the<br />
UB-04 Claim Form. For example, GHO does not separately reimburse for cl<strong>in</strong>ic charges<br />
represented by CPT® codes such as 99201-99499 reported on the UB-04 Claim Form. The<br />
cost of such charges is reimbursed to the applicable professional provider as payment <strong>in</strong><br />
full for Covered Services.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
59
GHO requires a correspond<strong>in</strong>g CPT®/HCPCS code with revenue codes for services reported <strong>in</strong><br />
an outpatient Hospital sett<strong>in</strong>g:<br />
260 General IV therapy<br />
261 Infusion Pump<br />
269 Other IV Therapy<br />
274 Medical/Surgical Supplies/Devices- Prosthetic/Orthotic Devices<br />
300-309 Laboratory<br />
310-319 Laboratory Pathological<br />
320-329 Radiology-Diagnostic<br />
330-339 Radiology-Therapeutic<br />
340-349 Nuclear Medic<strong>in</strong>e<br />
350-359 Computed Tomographic (CT) Scans<br />
360-369 Operat<strong>in</strong>g Room Services<br />
400-409 Other Imag<strong>in</strong>g Services<br />
410 Respiratory Services-General<br />
413 Respiratory Services-Hyperbaric Oxygen Therapy<br />
420 Physical Therapy-General<br />
430 Occupational Therapy-General<br />
440 Speech-Language Pathology-General<br />
441 Speech-Language Pathology-Visit Charge<br />
450-452,456,459 Emergency Room Services<br />
460-469 Pulmonary Function<br />
470-471 Audiology<br />
480-489 Cardiology<br />
490 Ambulatory Surgical Care-General<br />
499 Ambulatory Surgical Care-Other Ambulatory Surgical Care<br />
510-519 Cl<strong>in</strong>ic<br />
520-529 Freestand<strong>in</strong>g Cl<strong>in</strong>ic<br />
540 Ambulance-General<br />
545 Ambulance-Air Ambulance<br />
610-619 Magnetic Resonance Technology (MRT)<br />
623 Medical/Surgical Supplies-Surgical Dress<strong>in</strong>gs<br />
634 Pharmacy, Erythropoiet<strong>in</strong> (EPO) Less Than 10,000 Units<br />
635 Pharmacy, Erythropoiet<strong>in</strong> (EPO) 10,000 or More Units<br />
636 Pharmacy, Drugs Requir<strong>in</strong>g Detailed Cod<strong>in</strong>g<br />
730-739 EKG/ECG (Electrocardiogram)<br />
740-749 EEG (Electroencephalogram)<br />
750 Gastro<strong>in</strong>test<strong>in</strong>al Services-General<br />
759 Gastro<strong>in</strong>test<strong>in</strong>al Services-Other Gastro<strong>in</strong>test<strong>in</strong>al<br />
761 Treatment Room Services<br />
771 Preventive Care Services-Vacc<strong>in</strong>e Adm<strong>in</strong>istration<br />
790 Lithotripsy-General<br />
799 Lithotripsy-Other Lithotripsy<br />
900-909 Psychiatric/Psychological Treatments<br />
910-911 Psychiatric/Psychological Services<br />
914-919 Psychiatric/Psychological Services<br />
920-929 Other Diagnostic Services<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
60
940 Other Therapeutic Services-General<br />
941 Other Therapeutic Services-Recreational Therapy<br />
943 Other Therapeutic Services-Cardiac Rehabilitation<br />
944 Other Therapeutic Services-Drug Rehabilitation<br />
945 Other Therapeutic Services-Alcohol Rehabilitation<br />
949 Other Therapeutic Services<br />
960-989 Professional Fees<br />
Claim Status Inquiry<br />
Participat<strong>in</strong>g <strong>Provider</strong>s are encouraged to visit the <strong>Provider</strong> Service Center at<br />
www.thehealthplan.com/wvuh_providers_us/ or should contact the Customer Service Team<br />
(CST) dur<strong>in</strong>g the follow<strong>in</strong>g timel<strong>in</strong>es to determ<strong>in</strong>e the status of any claim:<br />
45-60 days from <strong>in</strong>itial claim submission: Participat<strong>in</strong>g <strong>Provider</strong>s should verify claim<br />
status onl<strong>in</strong>e through the <strong>Provider</strong> Service Center at<br />
www.thehealthplan.com/wvuh_providers_us/ or by call<strong>in</strong>g GHO’s applicable CST; or<br />
GHO receipt of claim if an EOP has not been received by the Participat<strong>in</strong>g <strong>Provider</strong> with<strong>in</strong><br />
45-60 days from the <strong>in</strong>itial claim submission. Participat<strong>in</strong>g <strong>Provider</strong>s are encouraged to<br />
document the date of <strong>in</strong>quiry as well as the name of the CST representative with whom the<br />
<strong>in</strong>quiry was discussed.<br />
60 days from <strong>in</strong>itial claim submission: A duplicate of any <strong>in</strong>itially submitted claim may be<br />
resubmitted to GHO when an EOP has not been received by the Participat<strong>in</strong>g <strong>Provider</strong><br />
with<strong>in</strong> 60 days from the <strong>in</strong>itial claim submission; and claim status and/or receipt by GHO<br />
cannot be verified through direct <strong>in</strong>quiry with the applicable CST representative as<br />
described above. To expedite this resubmission process, a duplicate of any <strong>in</strong>itially<br />
submitted claim may alternatively be transmitted via facsimile. Please note that all claims<br />
transmitted via facsimile should be specifically addressed to the attention of the CST<br />
representative with whom you have spoken.<br />
Claim Reconsideration Procedure<br />
Participat<strong>in</strong>g <strong>Provider</strong>s who wish to file claim reconsideration should utilize the Claim Research<br />
Request Form (Contact GHO by phone or check onl<strong>in</strong>e for form availability) to register the<br />
reconsideration. Claim reconsideration is not a <strong>Health</strong> Care <strong>Provider</strong> <strong>in</strong>itiated grievance.<br />
Claim Research Request Form Process<br />
Completion of a Claim Research Request Form is necessary when request<strong>in</strong>g reconsideration of<br />
a claim for the follow<strong>in</strong>g:<br />
Procedure/service denials that are the result of GHO’s claim edit<strong>in</strong>g software “Deny-Claim<br />
Edit.”<br />
Claim payment or denial when a coord<strong>in</strong>ation of benefit adjustment is required.<br />
Claim denial when additional medical documentation is be<strong>in</strong>g presented (i.e.,<br />
miscellaneous code submission).<br />
Data element correction of an approved/paid service (i.e., Member identification number,<br />
date of service, billed charge, or number of units).<br />
Reconsideration of an <strong>in</strong>correct payment or denial.<br />
Completion of a Claim Research Request Form is not required when request<strong>in</strong>g reconsideration<br />
for any of the follow<strong>in</strong>g reason(s):<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
61
Reconsideration of a claim denial due to a Participat<strong>in</strong>g <strong>Provider</strong>’s bill<strong>in</strong>g error (i.e.,<br />
<strong>in</strong>valid diagnosis code [ICD-9-CM], procedural code [CPT®/HCPCS], revenue code,<br />
<strong>in</strong>valid modifier, <strong>in</strong>valid place of service code, miss<strong>in</strong>g or <strong>in</strong>valid Participat<strong>in</strong>g <strong>Provider</strong><br />
name and tax identification number [TIN]). These claims can be corrected by the<br />
Participat<strong>in</strong>g <strong>Provider</strong> and resubmitted via the provider’s usual submission method.<br />
Corrections to the Member identification number or date of service require the use of the<br />
Claim Research Request Form.<br />
Request retraction of claim payment (i.e., overpayment, duplicate claim payment,<br />
cancelled charge).<br />
Reconsideration of a claim denial for exceed<strong>in</strong>g the timely fil<strong>in</strong>g requirement (refer to the<br />
“Time Limits” section for applicable claim submission time limits).<br />
Claim Research Request Forms and the necessary accompany<strong>in</strong>g documentation must be<br />
submitted with<strong>in</strong> one hundred eighty (180) days from the date of EOP. Please check off the<br />
applicable reason for the reconsideration request and <strong>in</strong>clude the name and telephone number of<br />
the person complet<strong>in</strong>g the form. Any reconsideration request submitted without the required<br />
documentation is not eligible for reconsideration and will be returned to the Participat<strong>in</strong>g<br />
<strong>Provider</strong> office.<br />
Please note: For electronic claims, a copy of the Emdeon/Relay <strong>Health</strong> Payer<br />
Reject/Unprocessed Claims Report, or vendor equivalent report, should be submitted along with<br />
a Claim Research Request Form to the Claims Department. Claim reconsiderations submitted<br />
us<strong>in</strong>g the Claim Research Request Form will be f<strong>in</strong>alized with<strong>in</strong> forty-five (45) days of receipt.<br />
Participat<strong>in</strong>g <strong>Provider</strong> will be notified of GHO’s determ<strong>in</strong>ation via:<br />
A new EOP with an explanation code; or<br />
A returned Claim Research Request Form with a brief explanation of the reconsideration<br />
denial.<br />
Please contact the Customer Service Team with any questions regard<strong>in</strong>g the Claim Research<br />
Request Form or these <strong>in</strong>structions. Claim Research Request Forms should be submitted to the<br />
follow<strong>in</strong>g address:<br />
Claims Department<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options<br />
PO Box 8200<br />
Danville, PA 17821-8200<br />
Customer Service Team:<br />
(866) 580-3531<br />
Refund Process<br />
When an overpayment on a claim is discovered, we ask that you notify GHO of the overpayment<br />
<strong>in</strong> one of the follow<strong>in</strong>g ways:<br />
1. Complete the Claim Research Request form and submit to:<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options, PO Box 8200, Danville, PA 17821; or<br />
2. Contact the Customer Service Team at (866) 580-3531.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
62
An off set to future payment may occur. Further questions regard<strong>in</strong>g this process can be<br />
discussed with the Customer Service Team or your <strong>Provider</strong> Relations Representative. Timely<br />
fil<strong>in</strong>g guidel<strong>in</strong>es must be followed when resubmitt<strong>in</strong>g claims.<br />
Coord<strong>in</strong>ation of Benefits<br />
With<strong>in</strong> one hundred eighty (180) days of the time of service, the Participat<strong>in</strong>g <strong>Provider</strong> is<br />
responsible for mak<strong>in</strong>g a reasonable <strong>in</strong>quiry to determ<strong>in</strong>e all applicable health care coverage,<br />
<strong>in</strong>clud<strong>in</strong>g subord<strong>in</strong>ate coverage for the Member. If another <strong>in</strong>surance carrier is primary to GHO,<br />
the Participat<strong>in</strong>g <strong>Provider</strong> is entitled to and responsible for collect<strong>in</strong>g first from the other<br />
<strong>in</strong>surance carrier, amounts covered by the other plan(s), to the extent that GHO or other<br />
<strong>in</strong>surance carrier is subord<strong>in</strong>ate, pursuant to the Member’s Benefit Document. Likewise, the<br />
Participat<strong>in</strong>g <strong>Provider</strong> recognizes that GHO may be subrogated to a Member’s rights of recovery<br />
<strong>in</strong> the event of third party damages and agrees to cooperate with the recovery of third party<br />
payments.<br />
Participat<strong>in</strong>g <strong>Provider</strong> agrees that GHO has the right to coord<strong>in</strong>ate benefits as set forth <strong>in</strong> the<br />
Member’s application and Benefit Documents. When GHO is a secondary <strong>in</strong>surance carrier,<br />
claims submitted to GHO should <strong>in</strong>clude the primary <strong>in</strong>surance carrier’s explanation of payment<br />
(EOP) for consideration of coverage not to exceed the contracted GHO reimbursement.<br />
Anti-Fraud and Abuse Activities<br />
GHO is committed to a policy of zero tolerance for fraudulent <strong>in</strong>surance acts that victimize GHO<br />
and its’ stakeholders. Accord<strong>in</strong>gly, GHO ma<strong>in</strong>ta<strong>in</strong>s an Anti-Fraud Program. The primary role of<br />
the Anti-Fraud Program is to identify suspected fraud and abuse, analyze and evaluate the<br />
circumstances, and take appropriate action to ensure GHO and its’ stakeholders are not harmed<br />
and that any necessary corrective actions are implemented.<br />
What is Fraud and Abuse<br />
Generally, deceptions or misrepresentations made by a person or entity that knows or<br />
should know that the deception or misrepresentation could result <strong>in</strong> some unauthorized<br />
benefit to himself/herself or some other person(s) or entity(ies) constitutes FRAUD.<br />
Generally, deception or misrepresentations made by a person or entity that is unaware that<br />
the deception or misrepresentation could result <strong>in</strong> some unauthorized benefit to<br />
himself/herself or some other person(s) or entity(ies) constitutes ABUSE.<br />
What is the Participat<strong>in</strong>g <strong>Provider</strong>’s Responsibility<br />
Participat<strong>in</strong>g <strong>Provider</strong>s have the responsibility to uphold all contractual requirements, <strong>in</strong>clud<strong>in</strong>g,<br />
but not limited to:<br />
Prohibit<strong>in</strong>g the submission of false or fraudulent statements and claims related to any of<br />
GHO’s benefit programs.<br />
Cooperat<strong>in</strong>g with GHO audits-this may <strong>in</strong>clude the exchange of <strong>in</strong>formation related to<br />
services rendered and/or release of medical record documentation.<br />
Notify<strong>in</strong>g GHO if the Participat<strong>in</strong>g <strong>Provider</strong> discovers that reimbursement by GHO is not<br />
<strong>in</strong> accordance with the provisions of their Agreement, or that payments made were<br />
erroneous.<br />
Reconcil<strong>in</strong>g Member payments with GHO Explanation of Payment (EOP).<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
63
It is important that Participat<strong>in</strong>g <strong>Provider</strong>s reconcile the EOP with Member accounts. An<br />
important element of the EOP <strong>in</strong>cludes the section display<strong>in</strong>g any applicable Member liability<br />
(i.e., Copayment, Co<strong>in</strong>surance, Deductible). Collect<strong>in</strong>g monies from Members when a Member<br />
liability is not displayed on the EOP is <strong>in</strong>appropriate. Us<strong>in</strong>g the EOP is the most effective tool <strong>in</strong><br />
determ<strong>in</strong><strong>in</strong>g Member liability. If Participat<strong>in</strong>g <strong>Provider</strong> collects monies from the Member and<br />
Participat<strong>in</strong>g <strong>Provider</strong> discovers that the payment was not due, Participat<strong>in</strong>g <strong>Provider</strong> must<br />
promptly refund the Member.<br />
GHO recognizes that Participat<strong>in</strong>g <strong>Provider</strong>s strive to render excellent care and to utilize<br />
appropriate bill<strong>in</strong>g practices. When questions arise, contact your <strong>Provider</strong> Relations<br />
Representative for clarification. Misunderstand<strong>in</strong>gs can lead to unnecessary audits and associated<br />
problems.<br />
If you become aware of a fraudulent or abusive <strong>in</strong>surance act, please contact GHO. You may<br />
rema<strong>in</strong> anonymous.<br />
E-mail at FA@thehealthplan.com<br />
Call your <strong>Provider</strong> Relations Representative at (800) 876-5357<br />
Toll free <strong>in</strong>dependent hotl<strong>in</strong>e at (800) 292-1627 is available for anonymous report<strong>in</strong>g<br />
send written correspondence to:<br />
Geis<strong>in</strong>ger <strong>Health</strong> Options Anti-Fraud Program<br />
100 North Academy Avenue<br />
Danville, PA 17822-3220<br />
Additional <strong>in</strong>formation regard<strong>in</strong>g Anti-Fraud Program activities can be found at<br />
www.thehealthplan.com/wvuh_providers_us/.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Reimbursement and Claim Submission<br />
64
Section 4: Member & Participat<strong>in</strong>g <strong>Provider</strong> Rights<br />
& Responsibilities<br />
PARTICIPATING PROVIDER ADMINISTRATIVE RIGHTS .........................................................67<br />
Participat<strong>in</strong>g <strong>Provider</strong> Medical Management Denial Review Procedure ..................................... 67<br />
PARTICIPATING PROVIDER RESPONSIBILITIES ........................................................................67<br />
Time Limits................................................................................................................................... 67<br />
Non-eligible Claims...................................................................................................................... 67<br />
Proper Process<strong>in</strong>g.......................................................................................................................... 68<br />
Non-Covered Services .................................................................................................................. 68<br />
Penalty for Late Payment.............................................................................................................. 68<br />
Coord<strong>in</strong>ation of Benefits............................................................................................................... 68<br />
Third Party Payments.................................................................................................................... 68<br />
<strong>Provider</strong> List.................................................................................................................................. 69<br />
Audit ............................................................................................................................................. 69<br />
Advance Directives....................................................................................................................... 69<br />
Compliance with Grievance, Compla<strong>in</strong>t and Appeal Procedures................................................. 69<br />
Participat<strong>in</strong>g <strong>Provider</strong> Locations................................................................................................... 69<br />
Establishment of a Confidentiality Policy .................................................................................... 70<br />
Copy<strong>in</strong>g of Member Medical Records-F<strong>in</strong>ancial Responsibility ................................................. 70<br />
Hospitalization .............................................................................................................................. 70<br />
Missed Appo<strong>in</strong>tments by Members .............................................................................................. 70<br />
Term<strong>in</strong>ation of Physician/Member Relationship.......................................................................... 70<br />
Network Access/Reciprocity ........................................................................................................ 71<br />
Advertis<strong>in</strong>g <strong>Guide</strong>l<strong>in</strong>es ................................................................................................................. 71<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
65
Coverage dur<strong>in</strong>g PCP/SCP Absence............................................................................................. 73<br />
PCP Practice Acceptance Status Member Limitations ................................................................. 73<br />
M<strong>in</strong>imum Standards for Medical Record Documentation............................................................ 73<br />
Laboratory Results........................................................................................................................ 76<br />
General Provisions:....................................................................................................................... 78<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
66
TPA Member Rights and Responsibilities<br />
TPA Member rights and responsibilities are def<strong>in</strong>ed by the Employer. Contact the TPA<br />
Customer Service Team for specific details. <strong>Provider</strong>s can contact the Customer Service Team<br />
below to obta<strong>in</strong> a copy of the Member’s compla<strong>in</strong>t and grievance Procedure.<br />
GHO’s IVR system is available for Member use, 24 hours a day, 7 days a week. Our Customer<br />
Service Representatives are available to assist you dur<strong>in</strong>g normal bus<strong>in</strong>ess hours.<br />
GHO CUSTOMER SERVICE: (866) 580-3531<br />
Participat<strong>in</strong>g <strong>Provider</strong> Adm<strong>in</strong>istrative Rights<br />
Participat<strong>in</strong>g <strong>Provider</strong> Medical Management Denial Review Procedure<br />
Treat<strong>in</strong>g or attend<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong>s have the opportunity to speak to a GHO Medical<br />
Director to discuss any denial made on the basis of Medical Necessity. Written requests for an<br />
appeal must be received by GHO with<strong>in</strong> one hundred eighty (180) days follow<strong>in</strong>g receipt of the<br />
notification of the determ<strong>in</strong>ation of coverage or it will be rejected for untimely fil<strong>in</strong>g. Appeal<br />
requests must be submitted <strong>in</strong> writ<strong>in</strong>g <strong>in</strong>dicat<strong>in</strong>g the requested outcome to GHO Medical<br />
Director at 100 North Academy Avenue, Danville, PA 17822-3220.<br />
GHO Medical Directors are available to discuss GHO Medical Management denials at (800)<br />
544-3907 or (570) 271-6497 Monday through Friday 8:00 a.m. to 4:30 p.m.<br />
Participat<strong>in</strong>g <strong>Provider</strong> Responsibilities<br />
The Agreement between GHO and each Participat<strong>in</strong>g <strong>Provider</strong> conta<strong>in</strong>s terms and conditions<br />
relative to GHO operations. In addition to the provisions set forth <strong>in</strong> the Agreement, Participat<strong>in</strong>g<br />
<strong>Provider</strong>s are responsible for the follow<strong>in</strong>g:<br />
Time Limits<br />
The <strong>in</strong>itial submission of any claim must be received by GHO with<strong>in</strong> one hundred eighty (180)<br />
days of the date of service for outpatient claims and/or one hundred eighty (180) days of the date<br />
of discharge for <strong>in</strong>patient claims, as applicable. Any claim which GHO has previously paid or<br />
denied may be resubmitted for reconsideration.<br />
Non-eligible Claims<br />
Any <strong>in</strong>itial or resubmitted claim received after the time limits identified here<strong>in</strong> will not be<br />
considered a valid claim and will be denied by GHO and is not billable to the Member. Failure to<br />
verify claim status or receipt with<strong>in</strong> one hundred eighty (180) days of the date of service and/or<br />
one hundred eighty (180) days of the date of discharge for <strong>in</strong>patient claims may result <strong>in</strong> noneligible<br />
claims.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
67
Proper Process<strong>in</strong>g<br />
All claims submitted by Participat<strong>in</strong>g <strong>Provider</strong> to GHO for <strong>Health</strong> Care Services provided to<br />
Members under the terms of the Agreement will be subject to edit<strong>in</strong>g for compliance with<br />
standard cod<strong>in</strong>g format <strong>in</strong>clud<strong>in</strong>g, but not limited to, GHO’s right to re-bundle to the primary<br />
procedure those services determ<strong>in</strong>ed by GHO to be part of, <strong>in</strong>cidental to, or <strong>in</strong>clusive of the<br />
primary procedure. GHO reserves the right to process the claim accord<strong>in</strong>g to said standards.<br />
Non-Covered Services<br />
Neither GHO nor an Employer shall have any obligation to pay for services which a Member is<br />
not entitled to benefits under the terms of a valid Benefit Document. Such services are<br />
considered Non-Covered Services. Participat<strong>in</strong>g <strong>Provider</strong> shall be solely responsible for<br />
collect<strong>in</strong>g payment directly from Members for Non-Covered Services and may at any time bill a<br />
Member or former Member for any Non-Covered Services. However, claims denied due to<br />
Participat<strong>in</strong>g <strong>Provider</strong>’s failure to meet GHO’s precertification, Concurrent Review and/ or<br />
retroactive review processes are not considered Non-Covered Services and Participat<strong>in</strong>g <strong>Provider</strong><br />
agrees that it will not hold Members liable for payment of such denied claims.<br />
Penalty for Late Payment<br />
If GHO fails to reimburse Participat<strong>in</strong>g <strong>Provider</strong> with<strong>in</strong> thirty (30) days of receipt of a Clean<br />
Claim submitted electronically and forty (40) days of receipt of a Clean Claim for all other<br />
claims, <strong>in</strong>terest of ten percent (10%) per annum shall be paid on the amount owed on the Clean<br />
Claim. Interest shall be calculated beg<strong>in</strong>n<strong>in</strong>g the day after the required payment date and end<strong>in</strong>g<br />
on the date the claim is paid.<br />
Coord<strong>in</strong>ation of Benefits<br />
With<strong>in</strong> one hundred eighty (180) days of the time of service, Participat<strong>in</strong>g <strong>Provider</strong> shall be<br />
responsible for mak<strong>in</strong>g a reasonable <strong>in</strong>quiry to determ<strong>in</strong>e entitlement to benefits under GHO, an<br />
Employer-Sponsored Program or any other form of healthcare coverage. Should such <strong>in</strong>quiry<br />
uncover or should GHO notify Participat<strong>in</strong>g <strong>Provider</strong> of the existence of additional healthcare<br />
coverage to <strong>in</strong>clude, without limitation, <strong>in</strong>surance carriers, Workers’ Compensation, federal,<br />
state, or local government benefit plans, health ma<strong>in</strong>tenance organizations or any form of<br />
service, <strong>in</strong>demnity or reimbursement benefit plans (“Third Party Payors”), Participat<strong>in</strong>g <strong>Provider</strong><br />
shall be entitled to and responsible for collection directly from Member or others such amounts<br />
also covered by GHO, or Employer-Sponsored Programs or such other benefit plans to the extent<br />
that GHO or an Employer-Sponsored Program coverage is subord<strong>in</strong>ate pursuant to the Benefit<br />
Document. Likewise, Participat<strong>in</strong>g <strong>Provider</strong> recognizes that GHO or an Employer may be<br />
subrogated to a Member’s rights of recovery <strong>in</strong> the event of third party damages and agrees to<br />
cooperate with GHO and Members <strong>in</strong> the recovery of third party payments.<br />
Third Party Payments<br />
Upon request, Participat<strong>in</strong>g <strong>Provider</strong> agrees to give assistance to GHO for purposes of<br />
coord<strong>in</strong>at<strong>in</strong>g benefits with primary carriers. If GHO is the primary carrier and its payment does<br />
not cover all billed charges, Participat<strong>in</strong>g <strong>Provider</strong> may submit claims to the secondary carrier.<br />
If GHO is the secondary carrier, it shall pay Participat<strong>in</strong>g <strong>Provider</strong> for Covered Services that<br />
were not paid by the primary carrier. However, GHO’s liability shall not exceed the payment<br />
provisions of this Agreement and payment by GHO (as a secondary payor) shall be reduced by<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
68
the amounts received or due from a primary carrier. In the event payments made by Third Party<br />
Payors exceed the payment provisions of this Agreement, neither GHO nor an Employer, as<br />
applicable, will be required to remit payment under the terms hereof and Participat<strong>in</strong>g <strong>Provider</strong><br />
may reta<strong>in</strong> the excess. Noth<strong>in</strong>g conta<strong>in</strong>ed here<strong>in</strong> shall restrict or otherwise affect Participat<strong>in</strong>g<br />
<strong>Provider</strong>’s right or obligations with respect to compensation from other Third-Party Payors at its<br />
regular rates.<br />
<strong>Provider</strong> List<br />
Participat<strong>in</strong>g <strong>Provider</strong> permits the <strong>in</strong>clusion of its name, address(es) and the names and<br />
professional designation(s) of its healthcare professionals <strong>in</strong> GHO’s Participat<strong>in</strong>g <strong>Provider</strong><br />
List(s) for purposes of <strong>in</strong>form<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong>s and prospective and exist<strong>in</strong>g Members<br />
of the locations, services and Participat<strong>in</strong>g <strong>Provider</strong>s available to them. Such list is ma<strong>in</strong>ta<strong>in</strong>ed<br />
and distributed by GHO and is additionally accessible on GHO’s <strong>Provider</strong> Information Center at<br />
www.thehealthplan.com/wvuh_providers_us/.<br />
Audit<br />
Participat<strong>in</strong>g <strong>Provider</strong> agrees that GHO or its respective representative(s) may audit any and all<br />
aspects of Participat<strong>in</strong>g <strong>Provider</strong>’s performance under this Agreement by review<strong>in</strong>g any records<br />
or documentation related to such performance. GHO agrees to provide written notification to<br />
Participat<strong>in</strong>g <strong>Provider</strong> of its <strong>in</strong>tent to conduct an audit of Participat<strong>in</strong>g <strong>Provider</strong> and/or any of<br />
Participat<strong>in</strong>g <strong>Provider</strong>’s location(s) under the Agreement. Such audit shall occur dur<strong>in</strong>g normal<br />
bus<strong>in</strong>ess hours at a time mutually agreeable to the parties hereto no later than thirty (30) days<br />
after Participat<strong>in</strong>g <strong>Provider</strong>’s receipt of such written notice from GHO. Participat<strong>in</strong>g <strong>Provider</strong><br />
shall cooperate fully with any such audit and provide all records and documentation directly<br />
related to the services Participat<strong>in</strong>g <strong>Provider</strong> renders hereunder, subject to appropriate medical<br />
records’ confidentiality safeguards. GHO may, at its sole expense, reproduce any record;<br />
however, no orig<strong>in</strong>al record may be removed from Participat<strong>in</strong>g <strong>Provider</strong>’s premises.<br />
Advance Directives<br />
Participat<strong>in</strong>g <strong>Provider</strong> agrees to comply with the Patient Self-Determ<strong>in</strong>ation Act (Section 4751 of<br />
the Omnibus Budget Reconciliation Act of 1990) and state regulations and requirements relat<strong>in</strong>g<br />
to advance directives as such regulations and requirements are applicable to the Participat<strong>in</strong>g<br />
<strong>Provider</strong>. Participat<strong>in</strong>g <strong>Provider</strong> shall document <strong>in</strong> a prom<strong>in</strong>ent place <strong>in</strong> Member’s current<br />
medical record whether or not the Member has executed an advance directive.<br />
Compliance with Grievance, Compla<strong>in</strong>t and Appeal Procedures<br />
Participat<strong>in</strong>g <strong>Provider</strong> agrees to adhere to and cooperate with compla<strong>in</strong>t, grievance and appeal<br />
procedures <strong>in</strong> connection with a GHO compla<strong>in</strong>t, grievance and/or appeal.<br />
Participat<strong>in</strong>g <strong>Provider</strong> Locations<br />
Participat<strong>in</strong>g <strong>Provider</strong> shall provide <strong>Health</strong> Care Services at the location(s) approved by <strong>Health</strong><br />
Partners Network, Inc. (HPN). Participat<strong>in</strong>g <strong>Provider</strong> shall notify HPN of any additional<br />
location(s) where Participat<strong>in</strong>g <strong>Provider</strong> provides <strong>Health</strong> Care Services to Members prior to<br />
render<strong>in</strong>g those services to Members at such location(s). HPN reserves the right to approve<br />
additional Participat<strong>in</strong>g <strong>Provider</strong> location(s) based on, but not limited to, Participat<strong>in</strong>g <strong>Provider</strong>’s<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
69
compliance with the terms and conditions of the Agreement, HPN’s development of appropriate<br />
geographic Participat<strong>in</strong>g <strong>Provider</strong> coverage, as applicable, and HPN bus<strong>in</strong>ess need.<br />
Establishment of a Confidentiality Policy<br />
Participat<strong>in</strong>g <strong>Provider</strong> agrees to ensure the confidentiality of a Member’s Personal <strong>Health</strong><br />
Information (PHI) and will establish and ma<strong>in</strong>ta<strong>in</strong> a confidentiality policy to assure the<br />
appropriate handl<strong>in</strong>g of the Member’s <strong>in</strong>formation and records. Such confidentiality policy shall<br />
be <strong>in</strong> accordance with all state and federal laws perta<strong>in</strong><strong>in</strong>g to PHI and confidentiality.<br />
Participat<strong>in</strong>g <strong>Provider</strong> agrees to furnish a copy of its confidentiality policy to GHO upon request.<br />
Copy<strong>in</strong>g of Member Medical Records-F<strong>in</strong>ancial Responsibility<br />
In the event GHO requests copies of a Member’s medical records, either <strong>in</strong> whole or <strong>in</strong> part, all<br />
charges related to copy<strong>in</strong>g the records shall be considered fully compensated pursuant to the<br />
payment provisions of the Agreement. The Member will not be responsible for any charges<br />
related to the copy<strong>in</strong>g of medical records <strong>in</strong> this <strong>in</strong>stance.<br />
In the event the Member requests copies of his or her personal medical records for reasons other<br />
than Member selection/transfer to another Participat<strong>in</strong>g <strong>Provider</strong>, the Participat<strong>in</strong>g <strong>Provider</strong> may<br />
adm<strong>in</strong>ister their standard policy regard<strong>in</strong>g f<strong>in</strong>ancial responsibility for replicat<strong>in</strong>g medical<br />
records.<br />
Hospitalization<br />
For Hospital Covered Services, PCP and/or SCP will admit Members to a Participat<strong>in</strong>g <strong>Provider</strong>.<br />
PCP and/or SCP may refer a Member to a non-Participat<strong>in</strong>g <strong>Provider</strong> for Covered Services as<br />
may be Medically Necessary and upon the prior approval of the Medical Director, unless<br />
otherwise permitted <strong>in</strong> accordance with the terms and conditions of coverage set forth <strong>in</strong> the<br />
Member's Benefit Document.<br />
Missed Appo<strong>in</strong>tments by Members<br />
In the event a Member fails to present for a scheduled appo<strong>in</strong>tment, the Participat<strong>in</strong>g <strong>Provider</strong><br />
may collect from the Member the amount owed for a missed appo<strong>in</strong>tment charge pursuant to the<br />
Participat<strong>in</strong>g <strong>Provider</strong>’s current policy, which shall not be discrim<strong>in</strong>atory to GHO Members.<br />
GHO will not be responsible to reimburse the Participat<strong>in</strong>g <strong>Provider</strong> for missed appo<strong>in</strong>tment<br />
charges.<br />
Term<strong>in</strong>ation of Physician/Member Relationship<br />
In circumstances when a mutually beneficial physician/Member relationship cannot be atta<strong>in</strong>ed,<br />
the Participat<strong>in</strong>g <strong>Provider</strong> may proceed with formal term<strong>in</strong>ation of the physician/patient<br />
relationship; however, the Participat<strong>in</strong>g <strong>Provider</strong> may not term<strong>in</strong>ate the physician/patient<br />
relationship with any Member on the basis of health status or as otherwise prohibited by<br />
applicable laws. GHO encourages Participat<strong>in</strong>g <strong>Provider</strong> to make every effort to resolve disputes<br />
prior to tak<strong>in</strong>g any formal action to term<strong>in</strong>ate the relationship. The Participat<strong>in</strong>g <strong>Provider</strong><br />
<strong>in</strong>itiat<strong>in</strong>g a physician/Member term<strong>in</strong>ation must provide the Member and GHO (i.e., <strong>Provider</strong><br />
Relations Representatives) with thirty (30) days prior written notification of the <strong>in</strong>tent to<br />
term<strong>in</strong>ate the physician/patient relationship. For thirty (30) days from the date GHO receives<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
70
notification, the Participat<strong>in</strong>g <strong>Provider</strong> must cont<strong>in</strong>ue to provide all rout<strong>in</strong>e, urgent and<br />
Emergency <strong>Health</strong> Care Services for the affected Member until the transfer of the Member’s care<br />
to another provider occurs. These services need to be available and accessible 24 hours per day<br />
and 7 days per week.<br />
Network Access/Reciprocity<br />
Participat<strong>in</strong>g <strong>Provider</strong> acknowledges and agrees that GHO may, from time to time, enter <strong>in</strong>to<br />
arrangements with other entities for purposes of: Network rental; and/or Network reciprocity,<br />
whereby GHO makes its Network available to another Payor <strong>in</strong> exchange for access to the other<br />
Payor’s provider network. Notwithstand<strong>in</strong>g anyth<strong>in</strong>g to the contrary <strong>in</strong> the Agreement,<br />
Participat<strong>in</strong>g <strong>Provider</strong> agrees to provide covered services <strong>in</strong> accordance with the terms and<br />
conditions of the Agreement to <strong>in</strong>sureds/Members access<strong>in</strong>g GHO’s Network through such<br />
network rental or reciprocity arrangement. In addition, Participat<strong>in</strong>g <strong>Provider</strong> acknowledges and<br />
agrees that GHO is not responsible for payment for services provided to such <strong>in</strong>sureds/Members.<br />
GHO agrees that such arrangements will require access<strong>in</strong>g entities to comply with the terms and<br />
conditions of the Agreement. In addition, GHO will provide written notice to Participat<strong>in</strong>g<br />
<strong>Provider</strong> prior to an entity access<strong>in</strong>g Participat<strong>in</strong>g <strong>Provider</strong>’s services through the Network<br />
pursuant to this provision.<br />
Advertis<strong>in</strong>g <strong>Guide</strong>l<strong>in</strong>es<br />
Use of GHO’s name and likeness is permitted only with prior written approval from GHO’s<br />
Market<strong>in</strong>g Department. GHO’s Market<strong>in</strong>g Department limits and controls how, when, and <strong>in</strong><br />
what context the name and any representations about GHO are employed <strong>in</strong> any Advertis<strong>in</strong>g.<br />
The general Advertis<strong>in</strong>g policy for GHO is outl<strong>in</strong>ed <strong>in</strong> the follow<strong>in</strong>g paragraphs and may be used<br />
as a reference.<br />
Def<strong>in</strong>itions: In addition to the def<strong>in</strong>itions set forth elsewhere <strong>in</strong> this Agreement and/or other<br />
sources, the follow<strong>in</strong>g def<strong>in</strong>itions are applicable to this <strong>Guide</strong>:<br />
Advertis<strong>in</strong>g: Advertis<strong>in</strong>g is considered any written, electronic, visual or audio medium<br />
created for any person or employer group whose <strong>in</strong>tent is to <strong>in</strong>form them of the<br />
advantages of GHO or of authorized services.<br />
Approval, Written or Verbal: Any advertis<strong>in</strong>g created and planned for public doma<strong>in</strong><br />
requires prior review and approval by GHO’s Market<strong>in</strong>g Department. Verbal approvals<br />
are not given.<br />
GHO’s Market<strong>in</strong>g Department: The Director, Manager or designee, employed by GHO<br />
Market<strong>in</strong>g Department whose job is to provide written approval for Advertis<strong>in</strong>g.<br />
Advertis<strong>in</strong>g That Does NOT Require Approval:<br />
The follow<strong>in</strong>g Advertis<strong>in</strong>g does not require written approval and does not constitute<br />
advertis<strong>in</strong>g:<br />
Slide presentations designed solely for <strong>in</strong>ternal audiences<br />
Slide presentations designed solely for colleagues/peers<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
71
Advertis<strong>in</strong>g That Requires Approval:<br />
Any Advertis<strong>in</strong>g that is not listed above requires submission to GHO for written approval by<br />
GHO’s Market<strong>in</strong>g Department. A general guidel<strong>in</strong>e for Advertis<strong>in</strong>g suggests gett<strong>in</strong>g anyth<strong>in</strong>g <strong>in</strong><br />
doubt approved before use. Contact the GHO Market<strong>in</strong>g Department at:<br />
GHO Market<strong>in</strong>g Department<br />
100 North Academy Avenue<br />
Danville, PA 17822-3240<br />
Phone: (570) 271-8135<br />
Fax: (570) 271-7218<br />
Good Advertis<strong>in</strong>g and Level Play<strong>in</strong>g Field:<br />
All are encouraged to follow these general Advertis<strong>in</strong>g guidel<strong>in</strong>es:<br />
Approval: If GHO approves an advertisement, the follow<strong>in</strong>g will be provided:<br />
A copy of the Advertisement with mandatory changes, if any.<br />
Written confirmation of GHO’s approval.<br />
An offer to assist you <strong>in</strong> ensur<strong>in</strong>g GHO’s name is used and placed<br />
<br />
correctly.<br />
The name of a person <strong>in</strong> GHO’s Market<strong>in</strong>g Department who can assist you<br />
by answer<strong>in</strong>g questions and/or help<strong>in</strong>g you understand the changes<br />
required.<br />
Denial: If GHO disapproves an Advertisement, GHO will provide a written explanation<br />
of the problem with suggestions on how to correct it. Contact GHO’s Market<strong>in</strong>g<br />
Department to receive immediate assistance and directions regard<strong>in</strong>g re-submission of the<br />
corrected Advertisement. In general, anyth<strong>in</strong>g that is with<strong>in</strong> the limits of good bus<strong>in</strong>ess<br />
practice, is truthful and that requires only m<strong>in</strong>or changes will be approved. Any<br />
Advertisement that requires a 20% or more re-write cannot be approved because it no<br />
longer resembles the orig<strong>in</strong>al submission.<br />
Advertis<strong>in</strong>g Without Approval:<br />
Pursuant to the terms and condition of the underly<strong>in</strong>g Agreement, use of GHO’s name, likeness<br />
or logo without GHO approval constitutes breach of the Agreement.<br />
Accessibility of Primary Care Services<br />
GHO requires PCP and/or Primary Care Site(s) to meet the follow<strong>in</strong>g m<strong>in</strong>imum standards for<br />
accessibility of primary care services for Member(s):<br />
PCP Accessibility<br />
Emergency Services<br />
Urgent Care Services<br />
Rout<strong>in</strong>e Care Appo<strong>in</strong>tment(s)<br />
Preventative Care Appo<strong>in</strong>tment<br />
GHO Standards<br />
Seen immediately by PCP or designee (<strong>in</strong> office or<br />
emergency room, if appropriate)<br />
Appo<strong>in</strong>tment with PCP or designee with<strong>in</strong> twentyfour<br />
(24) hours from the date of the <strong>in</strong>itial request<br />
Appo<strong>in</strong>tment with PCP or designee with<strong>in</strong> twentyone<br />
(21) days from the date of the <strong>in</strong>itial request<br />
Appo<strong>in</strong>tment with PCP or designee with<strong>in</strong> forty-two<br />
(42) days from the date of the <strong>in</strong>itial request (i.e.,<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
72
well child check, physical/wellness exam<br />
24 Hour Availability PCPs should be available 24 hours a day/7 days a<br />
week<br />
Non-Bus<strong>in</strong>ess Hours Access (answer<strong>in</strong>g<br />
service or answer<strong>in</strong>g device)<br />
Appo<strong>in</strong>tment Wait Time<br />
An answer<strong>in</strong>g service or device should answer 100%<br />
of the time. Answer<strong>in</strong>g devices, if utilized, will<br />
provide caller with the PCP or designated cover<strong>in</strong>g<br />
PCP’s telephone and/or pager number, <strong>in</strong>clud<strong>in</strong>g<br />
emergency <strong>in</strong>structions.<br />
PCP or designee should see a Member with<strong>in</strong> thirty<br />
(30) m<strong>in</strong>utes of scheduled appo<strong>in</strong>tment time.<br />
Accessibility of primary care services will be monitored by GHO no less than semi-annually<br />
utiliz<strong>in</strong>g the “Primary Care Site Access Review Form” (Contact GHO by phone or check onl<strong>in</strong>e<br />
for form availability).<br />
Coverage dur<strong>in</strong>g PCP/SCP Absence<br />
A PCP or SCP Participat<strong>in</strong>g <strong>Provider</strong> must arrange for another PCP or SCP Participat<strong>in</strong>g<br />
<strong>Provider</strong> with appropriate tra<strong>in</strong><strong>in</strong>g or specialty to assume such provider’s responsibility dur<strong>in</strong>g an<br />
absence. Additionally, the coverage arrangement must be with another Participat<strong>in</strong>g <strong>Provider</strong><br />
who has admitt<strong>in</strong>g privileges at a Hospital Participat<strong>in</strong>g <strong>Provider</strong>.<br />
PCP Practice Acceptance Status Member Limitations<br />
In the event a PCP determ<strong>in</strong>es it is necessary to limit their cl<strong>in</strong>ical practice to new GHO<br />
membership as a result of the PCP practice membership capacity, the follow<strong>in</strong>g conditions are<br />
required:<br />
Advanced written notification of a m<strong>in</strong>imum of thirty (30) Bus<strong>in</strong>ess Days prior to the<br />
effective date of the limitation.<br />
PCP acknowledges that they will cont<strong>in</strong>ue to accept all current GHO membership and<br />
will cont<strong>in</strong>ue to provide Medical Services to assigned Member(s), regardless of a preexist<strong>in</strong>g<br />
physician-patient relationship.<br />
PCP acknowledges that chang<strong>in</strong>g to “accept<strong>in</strong>g exist<strong>in</strong>g patients only” status represents<br />
that the they will cont<strong>in</strong>ue to accept all patients who may change to GHO coverage and<br />
the change will not be published <strong>in</strong> written Member and/or provider material until next<br />
applicable pr<strong>in</strong>t<strong>in</strong>g, and<br />
PCP must concurrently establish a limited membership acceptance status with all other<br />
health benefit plans with which PCP participates.<br />
M<strong>in</strong>imum Standards for Medical Record Documentation<br />
GHO ma<strong>in</strong>ta<strong>in</strong>s m<strong>in</strong>imum standards for written and/or electronic medical records and reviews<br />
Participat<strong>in</strong>g Physicians’ (referred to hereafter as “Practitioner”) medical records to ensure<br />
compliance with these m<strong>in</strong>imum standards.<br />
The standards listed below exist to enhance Member care through, (i) the consistent<br />
documentation of the Member care; and (ii) the improvement of communication between<br />
caregivers, which occurs via the medical record.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
73
I. Medical record guidel<strong>in</strong>es/content:<br />
1. General: The accurate record<strong>in</strong>g and compilation of diagnoses, treatment, and results<br />
of treatment are most important to the practice of medic<strong>in</strong>e, and its successful<br />
execution requires the cooperation of the entire health care team.<br />
a. All pages conta<strong>in</strong> <strong>in</strong>sured <strong>in</strong>dividual identification number (<strong>in</strong>clud<strong>in</strong>g pr<strong>in</strong>ted<br />
<strong>in</strong>formation from the EMR)<br />
b. Biographical and personal data is documented/recorded.<br />
c. The medical record reflects the total <strong>in</strong>sured <strong>in</strong>dividual care by all<br />
departments and Practitioners.<br />
d. All contributors to the medical record bear the common responsibility of<br />
<strong>in</strong>sur<strong>in</strong>g that the record is legible, current, and completed with<strong>in</strong> one (1)<br />
bus<strong>in</strong>ess day of the visit.<br />
e. Telephone messages pert<strong>in</strong>ent to medical care and subsequent follow-up, are<br />
documented <strong>in</strong> the medical record. Telephone messages are dated, timed and<br />
<strong>in</strong>itialed.<br />
f. Insured <strong>in</strong>dividual’s failure to keep appo<strong>in</strong>tments and cancellations are<br />
documented <strong>in</strong> the medical record.<br />
g. There is a separate problem list on each medical record conta<strong>in</strong><strong>in</strong>g a current<br />
list of diagnoses, and significant surgeries. Each specialist is responsible for<br />
the <strong>in</strong>formation perta<strong>in</strong><strong>in</strong>g to his or her specialty care.<br />
h. Medical records have a current, separate health ma<strong>in</strong>tenance flow sheet.<br />
i. Allergies, absence of allergies and adverse reactions are documented <strong>in</strong> the<br />
appropriate location <strong>in</strong> the medical record<br />
j. Medical records are required to have a current immunization list.<br />
k. A current separate medication list is ma<strong>in</strong>ta<strong>in</strong>ed <strong>in</strong> the medical record.<br />
l. All cl<strong>in</strong>ic notes identify the author of the notes. Each site ma<strong>in</strong>ta<strong>in</strong>s a sheet<br />
with signatures and <strong>in</strong>itials.<br />
m. Signature stamps are not allowed (reference Centers for Medicare and<br />
Medicaid Services regulations).<br />
2. Initial Cl<strong>in</strong>ic Visit Documentation:<br />
a. Date is recorded. Department is recorded, when applicable<br />
b. Pert<strong>in</strong>ent history and physical is recorded for each problem <strong>in</strong>clud<strong>in</strong>g chief<br />
compla<strong>in</strong>t or purpose of visit, subjective and objective f<strong>in</strong>d<strong>in</strong>gs.<br />
c. Diagnostic impression.<br />
d. <strong>Plan</strong>- Diagnostic and Therapeutic: Laboratory data ordered, procedures<br />
performed or scheduled, medications prescribed, <strong>in</strong>structions given to the<br />
Member, disposition (follow-up).<br />
e. Allergies, absence of allergies and adverse reactions to medications are<br />
documented <strong>in</strong> the appropriate location <strong>in</strong> the medical record.<br />
f. Current separate medication list is <strong>in</strong>itiated when applicable.<br />
g. Past medical history<br />
h. There must be documentation <strong>in</strong>dicat<strong>in</strong>g whether or not an Advance <strong>Health</strong><br />
Care Directive has been executed for <strong>in</strong>sured <strong>in</strong>dividuals age 65 years or older<br />
and/or those with serious and/or complex medical conditions. If an Advance<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
74
<strong>Health</strong> Care Directive has been executed it must be prom<strong>in</strong>ently displayed <strong>in</strong><br />
the medical record<br />
3. Interval or Follow-Up Cl<strong>in</strong>ic Notes Documentation:<br />
a. Date is recorded. Department is recorded when applicable.<br />
b. Adequate <strong>in</strong>formation is recorded for each problem <strong>in</strong>clud<strong>in</strong>g chief compla<strong>in</strong>t<br />
or purpose of visit, subjective and objective f<strong>in</strong>d<strong>in</strong>gs.<br />
c. Diagnostic impression.<br />
d. <strong>Plan</strong>- Diagnostic and Therapeutic: Laboratory data ordered, procedures<br />
performed or scheduled, medications prescribed, <strong>in</strong>structions given to the<br />
<strong>in</strong>sured <strong>in</strong>dividual, disposition (follow-up). Especially note any changes from<br />
previous visits.<br />
e. Update problem lists, medication lists, health ma<strong>in</strong>tenance flow sheets,<br />
allergies, immunization records, and other applicable documents at each visit,<br />
as needed.<br />
4. <strong>Provider</strong> Orders: <strong>Provider</strong> orders adm<strong>in</strong>istered by the office staff are marked as<br />
completed.<br />
5. Diagnostics and Consults:<br />
a. Diagnostic test results, procedures, ancillary services and consults (specialty<br />
physician) are reviewed and <strong>in</strong>itialed/signed by the order<strong>in</strong>g Practitioner.<br />
b. Follow-up communication and documentation to the <strong>in</strong>sured <strong>in</strong>dividual for<br />
abnormal results.<br />
6. Other Communications: Other communications received are reviewed and<br />
<strong>in</strong>itialed/signed by the primary care giver or his/her designee and filed appropriately.<br />
This may <strong>in</strong>clude home health reports, hospital discharge reports and physical therapy<br />
results.<br />
7. Tobacco/Alcohol/Substance Use: A documented annual assessment of tobacco,<br />
alcohol, and other substance use for <strong>in</strong>sured <strong>in</strong>dividual age 11 and over.<br />
II. Organization and fil<strong>in</strong>g of <strong>in</strong>formation <strong>in</strong> the medical record should have a systematic<br />
approach.<br />
1. Medical records are organized and stored <strong>in</strong> a manner that allows easy retrieval and<br />
only allows access by authorized personnel. All <strong>in</strong>sured <strong>in</strong>dividual’s medical records<br />
conta<strong>in</strong> the seven (7) follow<strong>in</strong>g organizational components: (not necessarily <strong>in</strong> order<br />
listed)<br />
a. Cl<strong>in</strong>ic visit/progress notes<br />
b. Correspondence<br />
c. Diagnostics/Procedures<br />
d. Immunization records<br />
e. Problem lists/Medication lists<br />
f. Other flow sheets<br />
g. Demographics<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
75
III. Medical record Accessibility<br />
1. Medical records are easily retrievable at the time of the <strong>in</strong>sured <strong>in</strong>dividual encounter.<br />
2. Medical records are available for GHO adm<strong>in</strong>istrative/Quality Improvement purposes<br />
(<strong>in</strong>clud<strong>in</strong>g external review organization needs) to the extent permitted by applicable<br />
state and federal laws.<br />
IV. Confidentiality of medical records<br />
1. Participat<strong>in</strong>g Practitioners agree to ensure the confidentiality of an <strong>in</strong>sured<br />
<strong>in</strong>dividual’s Protected <strong>Health</strong> Information (PHI) and establish and ma<strong>in</strong>ta<strong>in</strong> a<br />
confidentiality policy to assure the appropriate handl<strong>in</strong>g of <strong>in</strong>sured <strong>in</strong>dividual<br />
<strong>in</strong>formation and records. Such confidentiality policy shall be <strong>in</strong> accordance with all<br />
state and federal laws perta<strong>in</strong><strong>in</strong>g to PHI and confidentiality. All records must be<br />
stored securely with access only by authorized personnel who receive periodic<br />
tra<strong>in</strong><strong>in</strong>g on confidentiality.<br />
V. Standards and Performance goals for Practitioners<br />
1. Standards and Performance goals are monitored through the Ambulatory Medical<br />
Record Review process as outl<strong>in</strong>ed <strong>in</strong> the Quality Improvement Department Policy #4<br />
Medical Record Review<br />
a. A score of 85% or higher is required on the Medical Record Review.<br />
b. Those scor<strong>in</strong>g below 85% are required to submit an action plan and are subject to<br />
a re-audit <strong>in</strong> six (6) months.<br />
2. Monitor<strong>in</strong>g of Participat<strong>in</strong>g Practitioner’s medical records is part of GHO’s Patient<br />
Safety <strong>Plan</strong>. Specific questions utilized for this purpose <strong>in</strong>clude those perta<strong>in</strong><strong>in</strong>g to:<br />
a. Patient identification on chart<br />
b. Allergies or absence of allergies<br />
c. History and physical<br />
d. Return communications, and<br />
e. Medication lists<br />
Other medical record reviews/studies may be conducted as needed for Quality Improvement<br />
purposes with identified separate performance goals.<br />
Laboratory Results<br />
Annually, the National Committee for Quality Assurance (NCQA) who establishes the<br />
<strong>Health</strong>care Effectiveness Data and Information Set (HEDIS®) measures, requests health plans to<br />
evaluate applicable Members who are identified as hav<strong>in</strong>g certa<strong>in</strong> cl<strong>in</strong>ical <strong>in</strong>dicators.<br />
Part of the HEDIS® measures <strong>in</strong>clude obta<strong>in</strong><strong>in</strong>g a copy of each Member’s laboratory test results.<br />
Laboratory results should be submitted to GHO on a monthly ongo<strong>in</strong>g basis. We are focus<strong>in</strong>g on<br />
a m<strong>in</strong>imum necessary set of data elements and not requir<strong>in</strong>g the submission of specific CPT<br />
codes.<br />
The follow<strong>in</strong>g are the Laboratory Specifications:<br />
Acceptable type of media for file download:<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
76
FTP (File Transfer Protocol) through GHO secure site by the 6 th bus<strong>in</strong>ess day of the month<br />
represent<strong>in</strong>g the previous month’s lab tests.<br />
File Requirements:<br />
All files must be <strong>in</strong> ASCII format<br />
Are TAB delimited<br />
All data files should <strong>in</strong>clude field name column headers on the first l<strong>in</strong>e of the file.<br />
M<strong>in</strong>imum Necessary Fields:<br />
Data should perta<strong>in</strong> to GHO Members only.<br />
Fields denoted with an [M] are m<strong>in</strong>imum necessary for report<strong>in</strong>g purposes and must be<br />
provided with correct data <strong>in</strong> the specified format.<br />
All other fields are optional.<br />
Report<strong>in</strong>g Date Requirements:<br />
Initially data from 1/1/08 thru current available should be reported, thereafter monthly<br />
feeds of new data should be transmitted.<br />
Field Requirements:<br />
Data fields must not conta<strong>in</strong> any padd<strong>in</strong>g with zeros or blank spaces.<br />
Numeric fields must not conta<strong>in</strong> dollar signs ($) or commas (,).<br />
Only 0 - 9, decimal, and plus/m<strong>in</strong>us characters are acceptable for numeric data fields.<br />
All dates must be <strong>in</strong> the YYYYMMDD, except where <strong>in</strong>dicated otherwise.<br />
Policy Holder IDs must NOT conta<strong>in</strong> dashes or s<strong>in</strong>gle-quotation marks.<br />
All text fields must be <strong>in</strong> upper case.<br />
There should be only one row per lab test performed.<br />
In the case of field No. 9 (LOINC Code) and No. 10 (Proccode), both are not required,<br />
either one should be fully populated.<br />
Field<br />
No.<br />
Field<br />
Description Field Name<br />
Data<br />
Type Size Data Doma<strong>in</strong> Comments<br />
1. Policy Holder Policy_Holder_ID Varchar 36 GHO Member ID<br />
Number [M]<br />
2.<br />
Lab Vendor [M] Vendor_ID Text 16<br />
ID number or code identify<strong>in</strong>g<br />
lab provider.<br />
3. Date of Service<br />
[M]<br />
DOS Date 8 Format:<br />
YYYYDDMM<br />
4. Referr<strong>in</strong>g Ref_Phys_Name Text 60 Physician who ordered test<strong>in</strong>g<br />
Physician Name<br />
5. UPIN UPIN Text 8 Unique Physician Identification Number<br />
6. Diagnosis Code Diag_Cd Text 7 ICD-9 diagnosis code,<br />
if provided by physician<br />
7. Local Lab Order<br />
Code<br />
Order_Cd Text 10 Local_Order_Code Code represent<strong>in</strong>g tests<br />
requested<br />
8. Test Name [M] Test_Name Text 30 Lab test name<br />
9. LOINC Code [M] LOINC Text 10 Lab_Code Universal code for<br />
identify<strong>in</strong>g lab data.<br />
10. Proccode [M] Procedure Code Char 5<br />
11. Local Lab Result Result_Code Text 10<br />
Code<br />
12. Result Name Result_Name Text 30<br />
13. Lab Result<br />
Numeric [M]<br />
Lab_Val Num 13 Result_Numeric Numeric lab result value<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
77
Field<br />
No.<br />
Field<br />
Description Field Name<br />
Data<br />
Type Size Data Doma<strong>in</strong> Comments<br />
14. Lab Result<br />
Literal Lab_Lit Text 18<br />
Result_Value<br />
Literal (Alpha) lab result value<br />
15. Unit of Measure Meas_Unit Text 20 Units of measure for the result<br />
16. Reference<br />
Range Low Ref_Rng_Low Num 13 9999999V9999999<br />
17. Reference<br />
Range High Ref_Rng_High Num 13 9999999V9999999<br />
18. Reference<br />
Range Alpha Ref_Rng_Alpha Text 20<br />
19. Abnormal Flag Abnormal_Flag Text 2 A – abnormal<br />
AB – Abnormal<br />
ABN – abnormal<br />
CH - cl<strong>in</strong>ical high<br />
CL - cl<strong>in</strong>ical low<br />
HH - high, high<br />
L - low<br />
LL - low, low<br />
N – normal<br />
20. Result<br />
Comments Result_Comments Text 300<br />
Notes:<br />
<br />
<br />
Please report LDLs <strong>in</strong> milligrams per deciliters (mg/dL) when populat<strong>in</strong>g field 13 (lab<br />
result numeric. Common Proccodes (field 10) used to report this data are 80061, 83700,<br />
83701, 83704, 83721.<br />
HbA1c conventional results normal range is between 4.2 and 5.9. International units or<br />
the estimated average glucose level is not what we expect to see reported <strong>in</strong> field 13 (lab<br />
result numeric). Common Proccodes (field 10) used to report this data are 83036 &<br />
83037.<br />
General Provisions:<br />
Participat<strong>in</strong>g <strong>Provider</strong> and GHO agree to abide by the follow<strong>in</strong>g General Provisions:<br />
A. Compliance. The parties agree to comply with all applicable federal and state laws and rules<br />
<strong>in</strong>clud<strong>in</strong>g, but not limited to (i) Title VII of the Civil Rights Act of 1964; (ii) The Age<br />
Discrim<strong>in</strong>ation Act of 1975; (iii) The Rehabilitation Act of 1973; (iv) The Americans With<br />
Disabilities Act; (v) other laws applicable to recipients of Federal funds; (vi) Medicare laws,<br />
regulations and Centers for Medicare and Medicaid Services (“CMS”) <strong>in</strong>structions; (vii)<br />
Patients’ bill of Rights <strong>in</strong> accordance with OPM; (viii) the Genetic Information<br />
Nondiscrim<strong>in</strong>ation Act of 2008; and (ix) all other applicable laws and rules. Furthermore,<br />
Participat<strong>in</strong>g <strong>Provider</strong> hereby warrants and represents that it shall comply and shall be<br />
responsible for requir<strong>in</strong>g any party that it may subcontract with to furnish services to Members to<br />
comply with GHO’s policies and procedures and all other terms and conditions of the<br />
Agreement. Additionally, it is hereby disclosed that payments made by GHO to related entities,<br />
contractors and subcontractors are, <strong>in</strong> whole or <strong>in</strong> part, from federal funds received by GHO<br />
through its contracts with the Centers for Medicare and Medicaid Services.<br />
B. Exhibits. All exhibits with<strong>in</strong> the Agreement are <strong>in</strong>corporated by reference and made part of<br />
the Agreement as if they were fully set forth <strong>in</strong> the text of the Agreement.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
78
C. Indemnification. The parties agree to protect, <strong>in</strong>demnify and hold harmless the other party(s)<br />
from and aga<strong>in</strong>st any and all loss, damage, cost and expense (<strong>in</strong>clud<strong>in</strong>g attorneys’ fees) which<br />
may be suffered or <strong>in</strong>curred under the Agreement as a result of the negligent or <strong>in</strong>tentional acts<br />
of the <strong>in</strong>demnify<strong>in</strong>g party, its employees, agents, consultants or subcontractors. Said <strong>in</strong>demnity is<br />
<strong>in</strong> addition to any other rights that the <strong>in</strong>demnified party may have aga<strong>in</strong>st the <strong>in</strong>demnify<strong>in</strong>g<br />
party and will survive the term<strong>in</strong>ation of the Agreement.<br />
D. Nondiscrim<strong>in</strong>ation. Participat<strong>in</strong>g <strong>Provider</strong> agrees to comply with all federal, state and local<br />
laws respect<strong>in</strong>g discrim<strong>in</strong>ation <strong>in</strong> employment and nonsegregation of facilities <strong>in</strong>clud<strong>in</strong>g, but not<br />
limited to, requirements set out at 41 CFR 60-1.4, 60-250.4 and 60-741.4, which equal<br />
opportunity clauses are hereby <strong>in</strong>corporated by reference. Notification is hereby given that<br />
compliance with these clauses may require Participat<strong>in</strong>g <strong>Provider</strong> to annually file certa<strong>in</strong> reports<br />
(e.g., the EEO-1 Report and VETS-100 Report) with the federal government and may require the<br />
contractor/ Participat<strong>in</strong>g <strong>Provider</strong> to develop written Affirmative Action Programs for Women<br />
and M<strong>in</strong>orities, covered Veterans and/or Handicapped Persons.<br />
E. Notification of Incidents. The parties agree to notify the other party (s) with<strong>in</strong> twenty-four<br />
(24) hours after the discovery of any <strong>in</strong>cidents, occurrences, claims or other causes of action<br />
<strong>in</strong>volv<strong>in</strong>g the Agreement. Upon receipt of discovery by any party of any <strong>in</strong>cident, occurrence,<br />
claim (either asserted or potential), notice of lawsuit or lawsuit <strong>in</strong>volv<strong>in</strong>g the Agreement, said<br />
party agrees to immediately notify the other party(s). The parties hereto agree to provide<br />
complete access, as may be provided by law, to records and other relevant <strong>in</strong>formation as may be<br />
necessary or desirable to resolve such matters. This Section shall survive the term<strong>in</strong>ation of the<br />
Agreement.<br />
F. Partial Invalidity/Interpretation. If any term or provision of the Agreement is determ<strong>in</strong>ed to<br />
be <strong>in</strong>valid or unenforceable, the rema<strong>in</strong>der of the Agreement will not be affected thereby. The<br />
section head<strong>in</strong>gs <strong>in</strong> the Agreement are solely for reference purposes. Participat<strong>in</strong>g <strong>Provider</strong><br />
acknowledges that portions of the Agreement are subject to review by Governmental Agencies<br />
and/or their designated representatives, as applicable, and <strong>in</strong> the event that such Governmental<br />
Agencies and/or their designated representatives require any material change to the terms and<br />
conditions of the Agreement, Participat<strong>in</strong>g <strong>Provider</strong> agrees to renegotiate the affected terms and<br />
conditions upon be<strong>in</strong>g notified of such required change by GHO.<br />
G. Promotional Materials. Participat<strong>in</strong>g <strong>Provider</strong> consents to GHO’s use of its name, address<br />
and the names and professional designations of its healthcare professionals <strong>in</strong> traditional<br />
membership and market<strong>in</strong>g materials. The parties hereto agree not to use the name of or any<br />
trademark, service mark or design registered to the other parties or their affiliates or any other<br />
party <strong>in</strong> any additional publicity, promotional or advertis<strong>in</strong>g material, unless review and written<br />
approval of the <strong>in</strong>tended use shall first be obta<strong>in</strong>ed from the releas<strong>in</strong>g party(s) prior to the release<br />
of any such material. Said approval shall not be unreasonably withheld by any of the parties.<br />
Notwithstand<strong>in</strong>g anyth<strong>in</strong>g to the contrary <strong>in</strong> the preced<strong>in</strong>g sentences, GHO shall have the right to<br />
publish Participat<strong>in</strong>g <strong>Provider</strong>’s summary rat<strong>in</strong>g as part of GHO’s Physician Quality Summary<br />
Program without obta<strong>in</strong><strong>in</strong>g the consent by Participat<strong>in</strong>g <strong>Provider</strong> prior to the release of such<br />
rat<strong>in</strong>g.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
79
H. Relationship Among Parties. The parties hereto expressly acknowledge and agree that: (i)<br />
GHO’s duties and responsibilities under the Agreement apply solely to GHO Members; (ii) <strong>in</strong> its<br />
capacity as third party adm<strong>in</strong>istrator, Company’s duties and responsibilities under the Agreement<br />
apply to Members of an Employer-Sponsored Program; and (iii) with the exception of (ii) of this<br />
Section, Company’s duties and responsibilities under the Agreement apply to Company<br />
Members. Each party hereto shall be considered <strong>in</strong>dependent entities with respect to each other.<br />
None of the provisions of the Agreement are <strong>in</strong>tended to create nor shall be deemed or construed<br />
to create any relationship between the parties other than that of <strong>in</strong>dependent entities contract<strong>in</strong>g<br />
with each other solely for the purpose of effect<strong>in</strong>g the provisions of the Agreement. Neither the<br />
parties nor any of their respective agents or employees shall be construed to be the agent,<br />
employee, jo<strong>in</strong>t Employer or representative of the other. The parties shall not have any express<br />
or implied rights or authority to assume or create any obligation or responsibility on behalf of or<br />
<strong>in</strong> the name of the other, except as may be otherwise set forth <strong>in</strong> the Agreement.<br />
I. Unforeseen Circumstances. In the event either party’s operations are substantially <strong>in</strong>terrupted<br />
by war, fire, <strong>in</strong>surrection, the elements, earthquakes, acts of God or, without limit<strong>in</strong>g the<br />
forego<strong>in</strong>g, any other cause beyond the control of the affected party (<strong>in</strong>clud<strong>in</strong>g GHO no longer<br />
meet<strong>in</strong>g all material requirements imposed on GHO by Federal or State law result<strong>in</strong>g <strong>in</strong> a<br />
significant impact on GHO’s operations), the affected party shall be relieved of its obligations<br />
only as to those affected portions of this Agreement for the duration of such <strong>in</strong>terruption. In the<br />
event that the performance of the affected party hereunder is substantially <strong>in</strong>terrupted pursuant to<br />
such event, the other party shall have the right to term<strong>in</strong>ate this Agreement upon ten (10) days’<br />
prior written notice to the affected party.<br />
GHO Compliance Program<br />
GHO’s Compliance Program is designed to oversee the development, implementation and<br />
ma<strong>in</strong>tenance of a compliance and privacy program that meets or exceeds federal and state laws<br />
and regulations, as well as contractual and accreditation obligations. GHO is committed to<br />
ethical and legal conduct that is compliant with all relevant laws and regulations, and to<br />
correct<strong>in</strong>g wrongdo<strong>in</strong>g whenever it may occur <strong>in</strong> the adm<strong>in</strong>istration of any of our plans. This<br />
commitment encompasses our organization and any of the parties that we contract with to<br />
provide services related to the adm<strong>in</strong>istration of our plans. For more detail on our compliance<br />
standards, please refer to our Code of Conduct onl<strong>in</strong>e at thehealthplan.com.<br />
Who do you contact with compliance questions<br />
You can contact our Compliance Department at (570) 271-7389.<br />
What do you do if you suspect Fraud, Waste, and/or Abuse<br />
It is very important for <strong>in</strong>dividuals who participate with our plans to report all cases of suspected<br />
fraud, waste and/or abuse.<br />
GHO has made available several methods for report<strong>in</strong>g this <strong>in</strong>formation.<br />
o You can call GHO’s Fraud and Abuse Hotl<strong>in</strong>e at 1-800-292-1627. (Calls to the hotl<strong>in</strong>e<br />
may be made anonymously)<br />
o You can contact our Chief Compliance Officer at (570) 271-7389.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
80
Def<strong>in</strong><strong>in</strong>g Fraud, Waste, and Abuse<br />
o Fraud – A deception or misrepresentation made by a person or entity that knows or<br />
should know the deception or misrepresentation could result <strong>in</strong> some unauthorized<br />
benefit to himself/herself or some other person(s) or entity(ies).<br />
o Waste – Waste occurs when an act of carelessness <strong>in</strong> performance and/or lack of<br />
tra<strong>in</strong><strong>in</strong>g result <strong>in</strong> otherwise unnecessary repetition of services.<br />
o Abuse – A deception or misrepresentation made by a person or entity that is unaware<br />
the deception or misrepresentation could result <strong>in</strong> some unauthorized benefit to<br />
himself/herself or some other person(s) or entity(ies).<br />
Examples of Risks for Fraud, Waste and Abuse<br />
Prescriber Fraud, Waste and Abuse<br />
o Illegal remuneration schemes: Prescriber is offered, or paid, or solicits, or receives<br />
unlawful remuneration to <strong>in</strong>duce or reward the prescriber to write prescriptions for drugs<br />
or products.<br />
o Prescription drug switch<strong>in</strong>g: Drug switch<strong>in</strong>g <strong>in</strong>volves offers of cash payments or other<br />
benefits to a prescriber to <strong>in</strong>duce the prescriber to prescribe certa<strong>in</strong> medications rather<br />
than others.<br />
o Script mills: <strong>Provider</strong> writes prescriptions for drugs that are not Medically Necessary,<br />
often <strong>in</strong> mass quantities, and often for patients that are not theirs. These scripts are<br />
usually written, but not always, for controlled drugs for sale on the black market, and<br />
might <strong>in</strong>clude improper payments to the provider.<br />
o Provision of false <strong>in</strong>formation: Prescriber falsifies <strong>in</strong>formation (not consistent with<br />
medical record) submitted through a prior authorization or other formulary oversight<br />
mechanism <strong>in</strong> order to justify coverage. Prescriber misrepresents the dates, descriptions<br />
of prescriptions or other services furnished, or the identity of the <strong>in</strong>dividual who<br />
furnished the services.<br />
o Theft of prescriber’s DEA number or prescription pad: Prescription pads and/or DEA<br />
numbers can be stolen from prescribers. This <strong>in</strong>formation could illegally be used to write<br />
prescriptions for controlled substances or other medications often sold on the black<br />
market. In the context of e-prescrib<strong>in</strong>g, <strong>in</strong>cludes the theft of the provider’s authentication<br />
(log <strong>in</strong>) <strong>in</strong>formation.<br />
Medicare Beneficiary Fraud, Waste and Abuse Risks<br />
o Misrepresentation of status: A Medicare beneficiary misrepresents personal<br />
<strong>in</strong>formation, such as identity, eligibility, or medical condition <strong>in</strong> order to illegally receive<br />
the drug benefit. Enrollees who are no longer covered under a drug benefit plan may still<br />
attempt to use their identity card to obta<strong>in</strong> prescriptions.<br />
o Identity theft: Perpetrator uses another person’s Medicare card to obta<strong>in</strong> prescriptions.<br />
o Prescription forg<strong>in</strong>g or alter<strong>in</strong>g: Where prescriptions are altered, by someone other<br />
than the prescriber or pharmacist with prescriber approval, to <strong>in</strong>crease quantity or number<br />
of refills.<br />
o Prescription diversion and <strong>in</strong>appropriate use: Beneficiaries obta<strong>in</strong> prescription drugs<br />
from a provider, possibly for a condition from which they do not suffer, and gives or sells<br />
this medication to someone else. Also can <strong>in</strong>clude the <strong>in</strong>appropriate consumption or<br />
distribution of a beneficiary’s medications by a caregiver or anyone else.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
81
o Resale of drugs on black market: Beneficiary falsely reports loss or theft of drugs or<br />
feigns illness to obta<strong>in</strong> drugs for resale on the black market.<br />
o Prescription stockpil<strong>in</strong>g: Beneficiary attempts to “game” their drug coverage by<br />
obta<strong>in</strong><strong>in</strong>g and stor<strong>in</strong>g large quantities of drugs to avoid out-of-pocket costs, to protect<br />
aga<strong>in</strong>st periods of non-coverage (i.e., by purchas<strong>in</strong>g a large amount of prescription drugs<br />
and then disenroll<strong>in</strong>g), or for purposes of resale on the black market.<br />
o Doctor shopp<strong>in</strong>g: Beneficiary or other <strong>in</strong>dividual consults a number of doctors for the<br />
purpose of <strong>in</strong>appropriately obta<strong>in</strong><strong>in</strong>g multiple prescriptions for narcotic pa<strong>in</strong>killers or<br />
other drugs. Doctor shopp<strong>in</strong>g might be <strong>in</strong>dicative of an underly<strong>in</strong>g scheme, such as<br />
stockpil<strong>in</strong>g or resale on the black market.<br />
o Improper Coord<strong>in</strong>ation of Benefits: Improper coord<strong>in</strong>ation of benefits where<br />
beneficiary fails to disclose multiple coverage policies, or leverages various coverage<br />
policies to “game” the system.<br />
o Market<strong>in</strong>g Schemes: A beneficiary may be victimized by a market<strong>in</strong>g scheme where a<br />
Sponsor, or its agents or brokers, violates the Medicare Market<strong>in</strong>g <strong>Guide</strong>l<strong>in</strong>es, or other<br />
applicable Federal or state laws, rules, and regulations to improperly enroll the<br />
beneficiary <strong>in</strong> a Part D <strong>Plan</strong>.<br />
Pharmacy Fraud, Waste and Abuse<br />
o Inappropriate bill<strong>in</strong>g practices: Inappropriate bill<strong>in</strong>g practices at the pharmacy level<br />
occur when pharmacies engage <strong>in</strong> the follow<strong>in</strong>g types of bill<strong>in</strong>g practices:<br />
o Incorrectly bill<strong>in</strong>g for secondary payers to receive <strong>in</strong>creased reimbursement<br />
o Bill<strong>in</strong>g for non-existent prescriptions<br />
o Bill<strong>in</strong>g multiple payers for the same prescriptions, except as required for<br />
coord<strong>in</strong>ation of benefit transactions<br />
o Bill<strong>in</strong>g for brand when generics are dispensed<br />
o Bill<strong>in</strong>g for non-covered prescriptions as covered items<br />
o Bill<strong>in</strong>g for prescriptions that are never picked up (i.e., not revers<strong>in</strong>g claims that<br />
are processed when prescriptions are filled but never picked up)<br />
o Bill<strong>in</strong>g based on “gang visits,” e.g., a pharmacist visits a nurs<strong>in</strong>g home and<br />
bills for numerous pharmaceutical prescriptions without furnish<strong>in</strong>g any specific<br />
service to <strong>in</strong>dividual patients<br />
o Inappropriate use of dispense as written (“DAW”) codes<br />
o Prescription splitt<strong>in</strong>g to receive additional dispens<strong>in</strong>g fees<br />
o Drug diversion<br />
o Prescription drug short<strong>in</strong>g: Pharmacist provides less than the prescribed quantity and<br />
<strong>in</strong>tentionally does not <strong>in</strong>form the patient or make arrangements to provide the balance but<br />
bills for the fully-prescribed amount.<br />
o Bait and switch pric<strong>in</strong>g: Bait and switch pric<strong>in</strong>g occurs when a beneficiary is led to<br />
believe that drug will cost one price, but at the po<strong>in</strong>t of sale the beneficiary is charged a<br />
higher amount.<br />
o Prescription forg<strong>in</strong>g or alter<strong>in</strong>g: Where exist<strong>in</strong>g prescriptions are altered, by an<br />
<strong>in</strong>dividual without the prescriber’s permission to <strong>in</strong>crease quantity or number of refills.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
82
o Dispens<strong>in</strong>g expired or adulterated prescription drugs: Pharmacies dispense drugs that<br />
are expired, or have not been stored or handled <strong>in</strong> accordance with manufacturer and<br />
FDA requirements.<br />
o Prescription refill errors: A pharmacist provides the <strong>in</strong>correct number of refills<br />
prescribed by the provider.<br />
o Illegal remuneration schemes: Pharmacy is offered, or paid, or solicits, or receives<br />
unlawful remuneration to <strong>in</strong>duce or reward the pharmacy to switch patients to different<br />
drugs, <strong>in</strong>fluence prescribers to prescribe different drugs, or steer patients to plans.<br />
o TrOOP manipulation: When a pharmacy manipulates TrOOP to either push a<br />
beneficiary through the coverage gap, so the beneficiary can reach catastrophic coverage<br />
before they are eligible, or manipulates TrOOP to keep a beneficiary <strong>in</strong> the coverage gap<br />
so that catastrophic coverage is never realized.<br />
o Failure to offer negotiated prices: Occurs when a pharmacy does not offer a<br />
beneficiary the negotiated price of a Part D drug.<br />
Pharmacy Benefit Manager (PBM) Fraud, Waste and Abuse<br />
o Prescription drug switch<strong>in</strong>g: The PBM receives a payment to switch a beneficiary<br />
from one drug to another or <strong>in</strong>fluence the prescriber to switch the patient to a different<br />
drug.<br />
o Unlawful remuneration: PBM receives unlawful remuneration <strong>in</strong> order to steer a<br />
beneficiary toward a certa<strong>in</strong> plan or drug, or for formulary placement. Includes unlawful<br />
remuneration from vendors beyond switch<strong>in</strong>g fees.<br />
o Inappropriate formulary decisions: PBM or their P&T committee makes formulary<br />
decisions where cost takes precedence over cl<strong>in</strong>ical efficacy and appropriateness of<br />
formulary drugs.<br />
o Prescription drug splitt<strong>in</strong>g or short<strong>in</strong>g: PBM mail order pharmacy <strong>in</strong>tentionally<br />
provides less than the prescribed quantity and does not <strong>in</strong>form the patient or make<br />
arrangements to provide the balance but bills for the fully-prescribed amount. Splits<br />
prescription to receive additional dispens<strong>in</strong>g fees.<br />
o Failure to offer negotiated prices: Occurs when a PBM does not offer a beneficiary<br />
negotiated price of a Part D drug<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> –Participat<strong>in</strong>g <strong>Provider</strong> Rights & Responsibilities<br />
83
Section 5: Medical Management and Quality<br />
Improvement and Accreditation<br />
MEDICAL MANAGEMENT PLAN .......................................................................................................85<br />
Philosophy..................................................................................................................................... 85<br />
Mission.......................................................................................................................................... 85<br />
Goals ............................................................................................................................................. 85<br />
Authority....................................................................................................................................... 86<br />
Structure........................................................................................................................................ 86<br />
Scope............................................................................................................................................. 92<br />
QUALITY IMPROVEMENT PLAN.....................................................................................................103<br />
Purpose........................................................................................................................................ 103<br />
Goals and Objectives .................................................................................................................. 103<br />
Scope of Program........................................................................................................................ 106<br />
Cl<strong>in</strong>ical Programs........................................................................................................................ 106<br />
Service Initiatives........................................................................................................................ 108<br />
Coord<strong>in</strong>ated Activities ................................................................................................................ 109<br />
QI Program Structure.................................................................................................................. 109<br />
Quality Improvement and Accreditation Personnel.................................................................... 113<br />
Delegated Activities.................................................................................................................... 116<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
84
Medical Management <strong>Plan</strong><br />
The 2011 Medical Management <strong>Plan</strong> def<strong>in</strong>es and clarifies the structure and function of the<br />
<strong>Health</strong> Services Department. This document provides a def<strong>in</strong>ition of authority and accountability<br />
for medical management activities with<strong>in</strong> the organization, articulates the scope and content of<br />
the Medical Management program, identifies the roles and responsibilities of <strong>in</strong>dividuals<br />
<strong>in</strong>volved, and outl<strong>in</strong>es the program evaluation process.<br />
The Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong>/Geis<strong>in</strong>ger Indemnity Insurance Company/Geis<strong>in</strong>ger Quality Options<br />
(GHP/GIIC/GQO) Medical Management <strong>Plan</strong> is structured to encompass all product l<strong>in</strong>es<br />
<strong>in</strong>clud<strong>in</strong>g, but not limited to, Commercial HMO/POS, Gatekeeper PPO and Medicare product<br />
l<strong>in</strong>es.<br />
Philosophy<br />
It is GHP/GIIC/GQO’s philosophy to assure the Medical Management Department is structured<br />
to manage the use of resources, and to maximize the effectiveness of care and services provided<br />
to Members. The Medical Management Department functions are described below.<br />
Mission<br />
<br />
<br />
<br />
<br />
<br />
To respect all Members and strive to respond appropriately to Members’ care and<br />
service needs.<br />
To improve the health and quality of life of Members by offer<strong>in</strong>g quality, wellcoord<strong>in</strong>ated<br />
health care education and services.<br />
To measure, evaluate, report, and implement <strong>in</strong>terventions that improve the health<br />
status of members.<br />
To facilitate the delivery of quality care to members <strong>in</strong> the most cost efficient manner<br />
utiliz<strong>in</strong>g the appropriate level of care to meet the cl<strong>in</strong>ical need.<br />
To facilitate the Member appeal, compla<strong>in</strong>t, and grievance process <strong>in</strong> a manner that is<br />
timely, supportive to the member, and guided by the member benefit document.<br />
Goals<br />
The overall goal of the Medical Management <strong>Plan</strong> is to assure that covered health care<br />
services are accessible, medically appropriate and cost effective.<br />
Objectives <strong>in</strong>clude:<br />
To identify processes appropriate for medical management review <strong>in</strong> order to<br />
promote improvement <strong>in</strong> care delivery.<br />
To communicate to <strong>Provider</strong>s and Members topics related to optimum use of services.<br />
To serve as a resource for analysis of reports of the medical management experiences,<br />
share with <strong>Provider</strong>s and develop appropriate action plans.<br />
To encourage a “process improvement” philosophy when address<strong>in</strong>g medical<br />
management issues.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
85
To conduct an annual review/revision/evaluation of the Medical Management <strong>Plan</strong>,<br />
policies /procedures, and criteria.<br />
Evaluate new technologies and implement medical policies that reflect current<br />
medical practices<br />
To assure medical appropriateness is the basis for Medical Management (MM)<br />
decision- mak<strong>in</strong>g and to assure f<strong>in</strong>ancial <strong>in</strong>centives do not impact denials of coverage<br />
or service.<br />
To provide appropriate, consistent and timely MM decisions us<strong>in</strong>g evidenced-based<br />
medical criteria and Member benefits.<br />
To promote the use of mechanisms that assesses consistent adjudication of denials<br />
and appeals across all MM decision-makers.<br />
To assure reasonable access to covered care and service for Members throughout the<br />
network.<br />
To facilitate exchange of <strong>in</strong>formation between Medical Management, Case<br />
Management, appeals, Medical Claims Research and Quality Improvement (QI)<br />
functions to facilitate process improvement, cont<strong>in</strong>uity of care, proactive services,<br />
and issue resolution.<br />
To analyze results of the <strong>Provider</strong> Satisfaction Survey related to Medical<br />
Management functions, identify areas of improvement, and develop any appropriate<br />
action plans.<br />
Comply with all state, federal and accreditation agency requirements.<br />
Authority<br />
Medical Management personnel have the authority to review the medical record of any Geis<strong>in</strong>ger<br />
<strong>Health</strong> <strong>Plan</strong> Member; to discuss f<strong>in</strong>d<strong>in</strong>gs with the physician or other providers, and to <strong>in</strong>itiate<br />
appropriate actions as directed by the Vice President, Chief Medical Officer or his designee (VP<br />
<strong>Health</strong> Services, Medical Directors/<strong>Health</strong> Services, and Regional Medical Directors). This<br />
authority is documented <strong>in</strong> the GHP Subscription Certificate.<br />
GHP has the authority to delegate MM activities to another agency. Should the <strong>Plan</strong> exercise that<br />
authority, the Medical Management Department will be responsible to assure the delegated<br />
agency is <strong>in</strong> compliance with the contractual agreement, <strong>Plan</strong>’s policies, and all applicable<br />
regulations / standards.<br />
Structure<br />
1. Key Staff Responsibilities and Activities:<br />
A. The Vice President, Chief Medical Officer and Vice President of <strong>Health</strong> Services<br />
hold adm<strong>in</strong>istrative responsibility for the <strong>Health</strong> Services Department and are<br />
<strong>in</strong>volved <strong>in</strong> program implementation. (Attachment A – <strong>Health</strong> Services<br />
Organizational Chart)<br />
* The Vice President, Chief Medical Officer is the designated physician for<br />
provid<strong>in</strong>g cl<strong>in</strong>ical leadership <strong>in</strong> the development, implementation, oversight,<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
86
cont<strong>in</strong>uous improvement and effectiveness of the Medical Management programs.<br />
The VP, Chief Medical Officer reports to the Board of Directors, chairs the<br />
Medical Management Adm<strong>in</strong>istrative committee (MMAC) and serves on the<br />
Pharmacy and Therapeutics committee, and the Technology Assessment<br />
committee among others.<br />
* The Vice President, <strong>Health</strong> Services is the Adm<strong>in</strong>istrator <strong>in</strong> charge of oversee<strong>in</strong>g<br />
all medical management operations. The VP, <strong>Health</strong> Services reports to the CMO<br />
and serves on MMAC and a multitude of other committees.<br />
B. The Medical Directors/<strong>Health</strong> Services and Regional Medical Directors of the<br />
Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> serve as the designees for the CMO for decisions based on<br />
medical appropriateness, authorization of referral to out of network providers, and<br />
dialogue with providers related to services and the appeal of MM denials.<br />
* Medical Director/<strong>Health</strong> Services/Medical Informatics- Licensed physician who<br />
has leadership responsibility for the Medical Management area related to <strong>in</strong>patient<br />
and out patient care. Works closely with the VP <strong>Health</strong> Services and reports<br />
directly to the CMO.<br />
* Medical Director/<strong>Health</strong> Services- Licensed physician who has leadership<br />
responsibility for the Medical Management area related to patient care. Works<br />
closely with the VP <strong>Health</strong> Services and reports directly to the CMO.<br />
* Medical Director/VP Pharmacy- Licensed physician designated as the lead<br />
medical authority for all <strong>Health</strong> <strong>Plan</strong> activities with<strong>in</strong> the North Central Region<br />
and takes a leadership role <strong>in</strong> relationship build<strong>in</strong>g with<strong>in</strong> the region. Also<br />
responsible for all Pharmacy activities with<strong>in</strong> the <strong>Health</strong> <strong>Plan</strong>. Works closely with<br />
the VP <strong>Health</strong> Services and reports directly to the CMO.<br />
* Medical Director/<strong>Health</strong> Services/Proven <strong>Health</strong> Navigator Licensed physician<br />
designated as the medical team leader for all <strong>Health</strong> <strong>Plan</strong> activities with<strong>in</strong> the<br />
Western Region and takes a leadership role <strong>in</strong> relationship build<strong>in</strong>g with<strong>in</strong> the<br />
region. Also responsible for work<strong>in</strong>g with the VP, <strong>Health</strong> Services to champion<br />
the <strong>Health</strong> Navigator care model. Works closely with the VP <strong>Health</strong> Services and<br />
reports directly to the CMO.<br />
* Medical Director/<strong>Health</strong> Services/Quality and Performance Licensed physician<br />
responsible for all activity related to quality of care rendered to <strong>Health</strong> <strong>Plan</strong><br />
members and by participat<strong>in</strong>g providers. Works closely with the VP <strong>Health</strong><br />
Services and reports directly to the CMO.<br />
All GHP Medical Directors have authority to make MM decisions <strong>in</strong>clud<strong>in</strong>g denials.<br />
All GHP Medical Directors are board-certified physicians engaged <strong>in</strong> a variety of<br />
cl<strong>in</strong>ical specialties. The Medical Directors <strong>in</strong>teract on a regular basis with the MM<br />
staff <strong>in</strong> the processes to support MM decision-mak<strong>in</strong>g. The MM Professional Staff<br />
are licensed <strong>in</strong> the State of Pennsylvania and are the <strong>in</strong>itial contact for MM decision-<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
87
mak<strong>in</strong>g; however, this staff does not issue denials on the basis of Medical Necessity.<br />
All Medical Directors report directly to the CMO.<br />
C. Behavioral <strong>Health</strong> Practitioner: The <strong>Health</strong> <strong>Plan</strong> VP, Chief Medical Officer works<br />
closely with the <strong>Health</strong> <strong>Plan</strong> CMO and the Medical Director/<strong>Health</strong> Services for<br />
oversee<strong>in</strong>g and implement<strong>in</strong>g programs related to Behavioral <strong>Health</strong> and all<br />
participate <strong>in</strong> both the Behavioral <strong>Health</strong> oversight committee and the Quality<br />
Improvement committee.<br />
D. Medical Management Professional Staff: The professional staff with<strong>in</strong> the Medical<br />
Management area <strong>in</strong>cludes RN’s, LPN’s, Occupational, Physical and Respiratory<br />
Therapists. All professional staff are licensed <strong>in</strong> Pennsylvania and have the ability to<br />
approve requests based on specified criteria. They can recommend denials based on<br />
specified criteria, and those recommendations will be reviewed by a Medical Director<br />
for the f<strong>in</strong>al decision. All professional staff report to a Director who is a licensed<br />
respiratory therapist, and to the Vice President, <strong>Health</strong> Services who is an RN.<br />
E. Outpatient Case Management Nurs<strong>in</strong>g Staff: The nurs<strong>in</strong>g staff <strong>in</strong>clud<strong>in</strong>g<br />
Disease/Case Management nurses and Medical Home Case Managers, who provide<br />
disease management, case management and coord<strong>in</strong>ation of care services.<br />
2. Committee Structure (Attachment B)<br />
The follow<strong>in</strong>g describes the Medical Management Adm<strong>in</strong>istrative Committee report<strong>in</strong>g<br />
structure and responsibilities:<br />
A. Medical Management Adm<strong>in</strong>istrative Committee (MMAC) meets monthly.<br />
1. Role<br />
The MMAC is responsible for function<strong>in</strong>g as the oversight committee for the<br />
Medical Management process and activities. This committee receives and<br />
makes recommendations on <strong>in</strong>formation and reports received from the<br />
subcommittees.<br />
2. Committee/Chairman<br />
Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> Vice President, Chief Medical Officer.<br />
Committee is comprised of Medical Directors, VP <strong>Health</strong> Services,<br />
Adm<strong>in</strong>istrative staff, Medical Management, Case/Disease Management,<br />
Pharmacy, Accreditation, Appeals, QI and <strong>Provider</strong> Network Management<br />
etc.<br />
3. Reports to Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> Quality Improvement Committee through the<br />
Vice President of <strong>Health</strong> Services at least semi-annually.<br />
4. Responsibilities<br />
Review/approval of the Medical Management <strong>Plan</strong> and Evaluation.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
88
Review/approval of MM criteria.<br />
Review/approval of Medical Policies.<br />
Oversight of Pharmacy & Therapeutics Committee and their activities.<br />
Oversight of Physician Advisory Group and their activities.<br />
Oversight of Technology Assessment Committee and their activities.<br />
Oversight of The Behavioral <strong>Health</strong> Oversight Committee and their activities<br />
related to Medical Management.<br />
Oversight of the Medical Management Committee and their activities.<br />
Oversight of the MM portion of the <strong>Provider</strong>/Member Satisfaction Surveys.<br />
At least semi-annual report to the GHP Quality Improvement Committee<br />
Oversight of any delegated MM activity<br />
Technology Assessment Committee reports related to approvals and denials.<br />
Oversight of the MM portion of the CAHPS Survey.<br />
5. Subcommittees of MMAC<br />
a. The Medical Management Committee (MMC) meets twice monthly (first<br />
and third Monday).<br />
1. Role<br />
The MMC is responsible for coord<strong>in</strong>at<strong>in</strong>g operational activities<br />
throughout the <strong>Health</strong> Services department along with operational<br />
policy review/approval. MMC is also responsible for an <strong>in</strong>itial review<br />
of medical policies and cl<strong>in</strong>ical guidel<strong>in</strong>es with recommendations to<br />
MMAC.<br />
2. Chairperson/Committee membership<br />
Medical Policy/Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es Manager<br />
Committee is comprised of Medical Directors, Pharmacy, Appeals,<br />
Medical Management, Case/Disease Management, Accreditation,<br />
Reimbursement and Benefits/Configuration departments.<br />
3. Reports to MMAC<br />
b. Pharmacy and Therapeutics (P&T) Committee Meets quarterly<br />
1. Role<br />
The P&T committee is responsible for ensur<strong>in</strong>g that procedures for<br />
pharmaceutical management promote the cl<strong>in</strong>ically appropriate use of<br />
pharmaceuticals. This committee is also responsible for review<strong>in</strong>g new<br />
pharmaceuticals for possible <strong>in</strong>clusion <strong>in</strong> the formulary/medical<br />
benefit determ<strong>in</strong>ations.<br />
2. Chairperson/Committee membership<br />
Vice President, Chief Medical Officer<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
89
Committee is comprised of Medical Directors, Pharmacy representatives,<br />
participat<strong>in</strong>g physician representation and Manager of Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es.<br />
As an adjunct to this committee there are several advisory committees<br />
from multiple cl<strong>in</strong>ical specialty areas who provide expertise related to<br />
specific cl<strong>in</strong>ical issues.<br />
3. Reports to MMAC<br />
c. Technology Assessment Committee- meets quarterly<br />
1. Role<br />
Responsible for evaluat<strong>in</strong>g new medical technologies and new<br />
applications of exist<strong>in</strong>g technologies for possible <strong>in</strong>clusion <strong>in</strong> the<br />
benefit package. This may <strong>in</strong>clude medical technologies, behavioral<br />
health procedures or other devices. (All new<br />
pharmaceuticals/pharmaceutical procedures will be taken through the<br />
P&T committee).<br />
2. Chairperson/Committee Membership<br />
GHP Medical Director, <strong>Health</strong> Services<br />
Committee is comprised of up to 17 physicians from multiple specialties,<br />
up to 3 lay members and support staff.<br />
3. Reports to MMC, MMAC, QIC and GHP Board of Directors<br />
d. Behavioral <strong>Health</strong> Oversight Committee- meets quarterly<br />
1. Role<br />
Responsible for oversight of behavioral health services to <strong>in</strong>clude, but<br />
not limited to, review of report<strong>in</strong>g received from the delegated entity<br />
and HEDIS data.<br />
2. Chairperson/Committee membership<br />
Medical Director/ <strong>Health</strong> Services<br />
Committee is comprised of Adm<strong>in</strong>istration, PNM, Pharmacy,<br />
Accreditation, QI, Medical Management, Case/Disease Management.<br />
3. Reports to MMAC and then QIC<br />
e. Physician Advisory Group (PAG) (Meets electronically on an ad hoc basis)<br />
1. Role<br />
Responsible for provid<strong>in</strong>g <strong>in</strong>put related to cl<strong>in</strong>ical, service,<br />
adm<strong>in</strong>istrative or regulatory issues.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
90
2. Chairperson/committee membership<br />
One of the GHP Medical Directors or any GHP employed designee of<br />
the Medical Director<br />
Committee composition <strong>in</strong>cludes 5-10 multi-specialty physicians.<br />
3. Reports to MMC and then MMAC<br />
3. Committee M<strong>in</strong>utes<br />
M<strong>in</strong>utes will be generated for all Medical Management Adm<strong>in</strong>istrative Committee<br />
and Sub-committee meet<strong>in</strong>gs, with review and approval by each Committee.<br />
The m<strong>in</strong>utes will reflect the activity, discussion, analysis and recommendations of the<br />
committees as well as follow-up and resolution of prior recommendations.<br />
The m<strong>in</strong>utes will be dated and signed by the chairperson and the record<strong>in</strong>g secretary.<br />
4. Medical Management <strong>Plan</strong>/Evaluation<br />
The Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> Medical Management Program is designed to provide the<br />
structure and processes for cont<strong>in</strong>uously monitor<strong>in</strong>g, analyz<strong>in</strong>g and improv<strong>in</strong>g the cl<strong>in</strong>ical<br />
care and services managed through the <strong>Health</strong> Services Department. At the beg<strong>in</strong>n<strong>in</strong>g of<br />
each year (and when necessary) the <strong>Health</strong> Services Department reviews/revises the<br />
Medical Management <strong>Plan</strong>. The Medical Management <strong>Plan</strong> def<strong>in</strong>es the mission, goals,<br />
structure and scope of the Medical Management, Case/Disease Management, Medical<br />
Home and Appeal Departments. The <strong>Plan</strong> also outl<strong>in</strong>es the committee report<strong>in</strong>g structure.<br />
An evaluation is conducted annually by the <strong>Health</strong> Services Department and impacts the<br />
forthcom<strong>in</strong>g MM plan. The annual evaluation serves to evaluate the impact of the<br />
Medical Management Program. This document describes the activities conducted by the<br />
Medical Management Department under the direction of the MMAC and evaluates (by<br />
track<strong>in</strong>g and trend<strong>in</strong>g) the effectiveness of these activities. The impact of the program<br />
with respect to delivery of services is monitored and evaluated through the follow<strong>in</strong>g:<br />
MM Data Report<strong>in</strong>g<br />
CAHPS Survey<br />
HEDIS<br />
Physician Satisfaction Surveys<br />
The Medical Management <strong>Plan</strong> and the Medical Management Annual Evaluation are<br />
reviewed and approved by the Medical Management Adm<strong>in</strong>istrative committee, then the<br />
Quality Improvement committee, on an annual basis.<br />
5. MM/QI Program Integration<br />
The Medical Management Department plays a vital role <strong>in</strong> the Quality Improvement<br />
Process. The MMAC Committee comprised of Senior Medical Management personnel<br />
oversees Medical Management processes and reports directly to the Quality Improvement<br />
Committee. The flow of <strong>in</strong>formation between departments goes <strong>in</strong> both directions.<br />
Opportunities identified <strong>in</strong> either area may be shared through multiple methods such as<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
91
committee meet<strong>in</strong>gs and face-to-face <strong>in</strong>teractions and may be the basis of development of<br />
a QI activity or change to a MM procedure.<br />
6. Behavioral <strong>Health</strong> Aspects of the MM Program<br />
Management of behavioral health care is conducted by <strong>Health</strong> <strong>Plan</strong> Medical Directors<br />
and MM staff.<br />
7. Appeal Procedures for Adverse Determ<strong>in</strong>ations<br />
The <strong>Plan</strong> has a formal process for appeals and grievances to meet the<br />
standards/requirements of regulatory and accredit<strong>in</strong>g bodies. Policies and procedures<br />
have been developed for Member and <strong>Provider</strong> appeals processes and are managed by the<br />
Appeals Department for Member appeals and through the MM department for the<br />
<strong>Provider</strong> appeals. More specific details are described <strong>in</strong> the associated policies.<br />
8. Delegation of MM (Attachment C-Delegation Agreements)<br />
The <strong>Health</strong> <strong>Plan</strong> is accountable for the decisions of any entity to whom a specific MM<br />
activity is delegated. Oversight activities <strong>in</strong>clude a pre-delegation assessment of the<br />
delegate’s ability to perform the delegated activities, an annual review of the delegate’s<br />
performance, review and approval of delegate’s MM program description and annual<br />
evaluation and review of quarterly reports from the delegated entity to assess the impact<br />
of activities on quality and delivery of health care to members. All delegated<br />
arrangements are described <strong>in</strong> the attachment, <strong>in</strong>clud<strong>in</strong>g NCQA accreditation status.<br />
Scope<br />
“Medical Necessity” or “Medically Necessary” is def<strong>in</strong>ed by Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> as covered<br />
services rendered by a health care provider, that the <strong>Health</strong> <strong>Plan</strong> determ<strong>in</strong>es are:<br />
A. Appropriate for the symptoms and diagnosis or treatment of the member’s condition,<br />
illness, disease or <strong>in</strong>jury.<br />
B. Provided for the diagnosis and the direct care and treatment of the member’s<br />
condition, illness, disease or <strong>in</strong>jury.<br />
C. In accordance with current standards of good medical treatment practice by the<br />
general medical community.<br />
D. Not primarily for the convenience of the member or the member’s health care<br />
provider.<br />
E. The most appropriate source or level of service that can safely be provided to the<br />
member. When applied to hospitalization this further means that the member requires<br />
acute care as an <strong>in</strong>patient due to the nature of services rendered or the member’s<br />
condition and the member cannot receive safe or adequate care as an outpatient.<br />
The <strong>Plan</strong>’s Medical Management decision process will be supported by evidence-based criteria<br />
<strong>in</strong> order to assure decisions are made <strong>in</strong> a fair, impartial, and consistent manner.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
92
Review and selection of MM criteria will be the responsibility of the MMAC, with<br />
recommendations from the Medical Directors, PAG, MMC and MM staff. The criteria will serve<br />
as a guidel<strong>in</strong>e, with opportunity for the Medical Director to consider all the factors <strong>in</strong> a case and<br />
determ<strong>in</strong>e the decision.<br />
Evidence-based cl<strong>in</strong>ical criteria used to support MM decisions will be managed through MMAC<br />
us<strong>in</strong>g the follow<strong>in</strong>g process:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Criteria adoption or revisions will be supported by appropriate cl<strong>in</strong>ical evidence.<br />
Criteria are made available for <strong>in</strong>put from the PAG.<br />
After review of all <strong>in</strong>put, the MMAC will record their formal vote on acceptance of<br />
the criteria;<br />
The MM Department ma<strong>in</strong>ta<strong>in</strong>s a policy/procedure to def<strong>in</strong>e application of the<br />
criteria us<strong>in</strong>g cl<strong>in</strong>ical and psychosocial <strong>in</strong>formation on a given case, <strong>in</strong>clud<strong>in</strong>g<br />
specifics of the local delivery system;<br />
Criteria will be revised as necessary and reviewed no less than annually;<br />
Inter-rater reliability test<strong>in</strong>g will be performed and documented at least annually for<br />
all nurs<strong>in</strong>g, therapy and physician staff <strong>in</strong>volved <strong>in</strong> the application of the criteria; and<br />
The provider guide will provide direction as to how a participat<strong>in</strong>g practitioner can<br />
avail themselves of the criteria, as def<strong>in</strong>ed by an exist<strong>in</strong>g vendor copyright.<br />
Data sources which may be used dur<strong>in</strong>g the decision mak<strong>in</strong>g process <strong>in</strong>clude but are not limited<br />
to the follow<strong>in</strong>g:<br />
Cl<strong>in</strong>ical Information from the treat<strong>in</strong>g physician such as: patient demographics,<br />
diagnosis, requested service, cl<strong>in</strong>ical f<strong>in</strong>d<strong>in</strong>gs, pert<strong>in</strong>ent imag<strong>in</strong>g, pert<strong>in</strong>ent lab f<strong>in</strong>d<strong>in</strong>g<br />
and pert<strong>in</strong>ent treatment/medications.<br />
In addition, <strong>in</strong>dividual needs and local delivery system assessments are considered. These<br />
may <strong>in</strong>clude age, co-morbidities, complications, progress of treatment, psychosocial<br />
situations, home environment and availability of appropriate services <strong>in</strong> the identified<br />
<strong>Health</strong> <strong>Plan</strong> service area.<br />
Behavioral <strong>Health</strong> to <strong>in</strong>clude Mental <strong>Health</strong> and Substance abuse is an <strong>in</strong>tegral part of the<br />
Medical Management Program. The <strong>Health</strong> <strong>Plan</strong> requires rout<strong>in</strong>e report<strong>in</strong>g, which is reviewed at<br />
multiple levels, <strong>in</strong>clud<strong>in</strong>g Behavioral <strong>Health</strong> Oversight Committee and also the Quality<br />
Improvement Committee to assure the best possible outcomes for the member.<br />
1. MM Functions<br />
A. Precertification<br />
Precertification of non-emergency facility admissions must be <strong>in</strong>itiated by the<br />
admitt<strong>in</strong>g physician or facility through telephone or fax contact with the Medical<br />
Management staff at the <strong>Plan</strong>. The Medical Management staff utilizes Milliman<br />
SI/IS cl<strong>in</strong>ical guidel<strong>in</strong>es, as a basis for determ<strong>in</strong>ations, accord<strong>in</strong>g to the cl<strong>in</strong>ical detail<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
93
presented to them. The Medical Management Staff will utilize the Milliman SI/IS<br />
guidel<strong>in</strong>es to determ<strong>in</strong>e the follow<strong>in</strong>g:<br />
<br />
<br />
<br />
<br />
Medical Necessity of the requested care<br />
Appropriateness of the service, location and level of care<br />
Appropriateness of the length of stay<br />
Assignment of the next anticipated review<br />
Cases fail<strong>in</strong>g the Milliman SI/IS guidel<strong>in</strong>es or not meet<strong>in</strong>g GHP Medical Policy, <strong>in</strong><br />
the judgment of the nurse, are referred to a GHP Medical Director for f<strong>in</strong>al decision.<br />
Discussion with the request<strong>in</strong>g physician and/or an appropriate licensed specialty<br />
physician may be <strong>in</strong>cluded <strong>in</strong> the decision mak<strong>in</strong>g process.<br />
Precertification provides an opportunity to <strong>in</strong>tervene when any of the follow<strong>in</strong>g are<br />
identified:<br />
Potential <strong>in</strong>appropriate health care services and admissions<br />
Complex cases appropriate for Case Management<br />
Discharge plann<strong>in</strong>g needs<br />
Potential quality of care issues<br />
Members who would benefit from Disease Management Programs.<br />
Clarification of par provider's availability to provide the service.<br />
<strong>Provider</strong>s are <strong>in</strong>structed to utilize their GHP <strong>Provider</strong> <strong>Guide</strong> to assist them with the<br />
pre-certification process.<br />
Timel<strong>in</strong>es for decision mak<strong>in</strong>g are as follows:<br />
Pre service non-urgent (HMO, PPO)—with<strong>in</strong> 15 days of receipt of the request<br />
Pre service urgent (HMO, PPO)—with<strong>in</strong> 72 hours of receipt of the request<br />
Pre service non-urgent (Medicare)—with<strong>in</strong> 14 calendar days of receipt of the<br />
request<br />
Pre service urgent (Medicare)—with<strong>in</strong> 72 hours of receipt of the request<br />
B. Concurrent Review<br />
Concurrent Review of acute, subacute, rehab, and SNF admissions are performed by<br />
the MM nurses and/or therapists as <strong>in</strong>itiated by the physician or facility of admission.<br />
As with precertification, the concurrent review process is supported by Milliman<br />
guidel<strong>in</strong>es and the <strong>Plan</strong>’s Medical Directors. Reviews are conducted by nurses and<br />
<strong>in</strong>clude the follow<strong>in</strong>g:<br />
Evaluation for appropriateness (Medical Necessity, level of care, length of<br />
stay);<br />
Evaluation and coord<strong>in</strong>ation of discharge plann<strong>in</strong>g and transitions of care to<br />
next po<strong>in</strong>t of care (nurs<strong>in</strong>g home, home health, rehab, etc);<br />
Referral to Case Management or Disease Management programs;<br />
Referral to Transplant Management Nurses; and<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
94
Identification of potential quality of care issues.<br />
The MM nurses and therapists evaluate and participate <strong>in</strong> discharge plann<strong>in</strong>g <strong>in</strong><br />
conjunction with the facility Medical Management Review nurse, and GHP Complex<br />
Case Management Case Managers to facilitate the transition of the Member from an<br />
<strong>in</strong>patient sett<strong>in</strong>g to a less acute sett<strong>in</strong>g that is more appropriate to the Member’s<br />
condition and to coord<strong>in</strong>ate efficient management of benefits. The MM nurses and<br />
therapists refer appropriate facility admissions to Outpatient Case Management for<br />
assessment and management.<br />
Timel<strong>in</strong>es for decision mak<strong>in</strong>g are as follows:<br />
Concurrent urgent (HMO, PPO)—with<strong>in</strong> 24 hours of receipt of the request<br />
C. The Determ<strong>in</strong>ation of Coverage Process<br />
The Determ<strong>in</strong>ation of Coverage (DOC) process is coord<strong>in</strong>ated through an LPN Case<br />
Manager (or MM RN if the scope is transplant services) <strong>in</strong> response to pre-service<br />
requests from a member or provider for authorization of coverage. The <strong>Plan</strong>’s<br />
Medical Directors are consulted <strong>in</strong> the DOC process and licensed specialty physician<br />
<strong>in</strong>put is <strong>in</strong>corporated as <strong>in</strong>dicated. Any denial, on the basis of Medical Necessity, is<br />
made by the Medical Director. Determ<strong>in</strong>ation of Coverage decisions are made<br />
consider<strong>in</strong>g these factors (other factors may also be used):<br />
Member’s benefit document;<br />
Member’s <strong>in</strong>dividual needs<br />
The <strong>Plan</strong>’s local delivery system available to the Member,<br />
participat<strong>in</strong>g/preferred provider’s ability to provide service, availability of<br />
skilled, sub-acute, and home services and coverage of these services;<br />
NCQA, CMS, and other state and federal regulations;<br />
Standards of medical practice;<br />
The <strong>Plan</strong>’s Medical Policies;<br />
Articles, literature, and research studies;<br />
Pert<strong>in</strong>ent cl<strong>in</strong>ical <strong>in</strong>formation from other providers <strong>in</strong>volved <strong>in</strong> the Member’s<br />
care; and<br />
Recommendations from the Geis<strong>in</strong>ger Technology Assessment Committee.<br />
If coverage for the request does not require a Medical Necessity determ<strong>in</strong>ation<br />
because it is addressed as a specific exclusion with<strong>in</strong> the Member’s benefit document,<br />
the nurse will generate a notice to the Member identify<strong>in</strong>g the specific contract<br />
exclusion.<br />
Timel<strong>in</strong>es for pre-service determ<strong>in</strong>ations are noted under Section VI, 1.A.<br />
The nurse coord<strong>in</strong>ates a Member’s care needs with both participat<strong>in</strong>g and nonparticipat<strong>in</strong>g<br />
providers <strong>in</strong> order to assure cont<strong>in</strong>uity of care and optimal outcomes.<br />
These nurses work closely with the Case/Disease Management nurses <strong>in</strong> the<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
95
management of cases requir<strong>in</strong>g both benefit and Case/Disease Management services,<br />
as well as <strong>in</strong> cooperation with the Transplant management vendor.<br />
A list of services/procedures requir<strong>in</strong>g determ<strong>in</strong>ation of coverage is ma<strong>in</strong>ta<strong>in</strong>ed by the<br />
MM department and is available to providers <strong>in</strong> their <strong>Provider</strong> guide.<br />
D. Retrospective Review<br />
Retrospective Reviews are reviews conducted after services have been provided to<br />
the Member. Retrospective review <strong>in</strong>cludes a Medical Necessity evaluation of the<br />
care/service provided to the Member, and physician compliance with the MM<br />
program requirements. Retrospective review <strong>in</strong>cludes consideration of medical<br />
criteria, member benefit <strong>in</strong>formation, adm<strong>in</strong>istrative guidel<strong>in</strong>es, and national cod<strong>in</strong>g<br />
guidel<strong>in</strong>es. The <strong>in</strong>dividual needs of the Member as well as local delivery system<br />
availability are considered. Retrospective reviews and reconsideration of medical<br />
claims denied through claim edit or claim review processes are performed by a<br />
Medical Claims Research Coord<strong>in</strong>ator. These reconsideration decisions are based on<br />
medical documentation, CPT and ICD-9 cod<strong>in</strong>g pr<strong>in</strong>ciples, government regulations,<br />
and current contracts along with the aforementioned criteria. The <strong>Plan</strong>’s Medical<br />
Directors are consulted for Medical Necessity evaluation.<br />
Timel<strong>in</strong>es for decision mak<strong>in</strong>g are as follows:<br />
Post service (HMO, PPO)—with<strong>in</strong> 30 days of receipt of the request<br />
E. Out of Network Management<br />
The MM professional staff follows the care of Members admitted to a nonparticipat<strong>in</strong>g<br />
facility for emergency care. When the cl<strong>in</strong>ical case supports the ability<br />
of the Member to be safely transported, retrieval to a participat<strong>in</strong>g facility may be<br />
offered. The nurse <strong>in</strong> cooperation with the GHP Medical Director and/or triage<br />
physician at the Emergency Department of Geis<strong>in</strong>ger Medical Center, Danville,<br />
coord<strong>in</strong>ate this transport.<br />
F. Transplant Services<br />
The MM professional staff provides coord<strong>in</strong>ation of benefits and case management to<br />
members approved or considered for organ and bone marrow transplantation. The<br />
GHP Medical Director oversees the transplant process and has ultimate responsibility<br />
for any decisions based on Medical Necessity. These decisions are based on the<br />
criteria noted as described <strong>in</strong> the scope section of this document.<br />
G. Discharge <strong>Plan</strong>n<strong>in</strong>g:<br />
<strong>Health</strong> Services nurs<strong>in</strong>g staff evaluate and coord<strong>in</strong>ate health services and care to<br />
encourage the transition of the patient from an <strong>in</strong>patient sett<strong>in</strong>g to a less acute sett<strong>in</strong>g<br />
which is more appropriate to the patient’s condition. <strong>Health</strong> Services staff participate<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
96
<strong>in</strong> discharge plann<strong>in</strong>g to coord<strong>in</strong>ate efficient management of benefits and<br />
coord<strong>in</strong>ation of services through discharge.<br />
H. Case Management Process<br />
Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> Benefit Nurse Coord<strong>in</strong>ators provide limited case management<br />
activity <strong>in</strong> relation to requests for certa<strong>in</strong> out-of-network services that are required by<br />
members. Serious and complex medical care needs are referred to case managers for<br />
triage <strong>in</strong>to case management/disease management programs.<br />
I. Transition of Care<br />
Members identified as hav<strong>in</strong>g exhausted a limited benefit are referred to Case<br />
Management. These nurses evaluate and assist <strong>in</strong> transition<strong>in</strong>g care to any exist<strong>in</strong>g<br />
alternative resources if available. This is performed through referral to local or state<br />
funded agencies, community services and/or other resources.<br />
J. Cont<strong>in</strong>uity of Care<br />
The <strong>Plan</strong> is committed to ensur<strong>in</strong>g the Member’s cont<strong>in</strong>uity and coord<strong>in</strong>ation of care<br />
with their provider if the Member is undergo<strong>in</strong>g an active course of treatment for an<br />
acute episode of a chronic illness or acute medical condition or if the Member is <strong>in</strong><br />
the second or third trimester of pregnancy when that provider’s participation<br />
agreement is discont<strong>in</strong>ued. The <strong>Plan</strong> is also committed to a new Member’s right to<br />
cont<strong>in</strong>uity and coord<strong>in</strong>ation of care if Member’s provider is not participat<strong>in</strong>g with the<br />
<strong>Plan</strong>. Certa<strong>in</strong> conditions must be satisfied prior to cont<strong>in</strong>uity be<strong>in</strong>g approved. These<br />
conditions are described <strong>in</strong> the established <strong>Health</strong> <strong>Plan</strong> policy. These conditions are<br />
designed to meet the needs of the Member while meet<strong>in</strong>g the requirements of all<br />
external regulatory and accredit<strong>in</strong>g bodies.<br />
K. Emergency Services Management<br />
Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> currently does not deny emergency service claims. All<br />
emergency service claims are adjudicated for payment without review for coverage<br />
determ<strong>in</strong>ation.<br />
L. On-site Review Process<br />
On-site review services may be conducted at participat<strong>in</strong>g facilities throughout the<br />
service areas. Functions <strong>in</strong>clude concurrent and retrospective review when applicable.<br />
<strong>Guide</strong>l<strong>in</strong>es have been established for identification of GHP MM staff at the facility, a<br />
process for schedul<strong>in</strong>g the review <strong>in</strong> advance and a process for ensur<strong>in</strong>g GHP staff<br />
follow facility rules. This process is described <strong>in</strong> more detail <strong>in</strong> the policy. On-site<br />
reviews are not currently be<strong>in</strong>g conducted.<br />
M. Medical Policy/Technology Assessment<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
97
Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> has a formal mechanism to evaluate and address new<br />
developments <strong>in</strong> technology and new applications of exist<strong>in</strong>g technologies for<br />
consideration of <strong>in</strong>clusion <strong>in</strong> the benefit package. This evaluation is conducted <strong>in</strong> an<br />
effort to keep pace with changes <strong>in</strong> services which may be available to our<br />
membership. This program ensures members have equitable access to safe and<br />
effective care. The four elements to be evaluated <strong>in</strong>clude:<br />
Medical Technologies<br />
Behavioral <strong>Health</strong> Procedures<br />
Pharmaceuticals<br />
Devices<br />
The Medical Policy Manager utilizes resources such as (but not limited to) Geis<strong>in</strong>ger<br />
<strong>Health</strong> <strong>Plan</strong> Technology Assessment Committee, Hayes Inc. and ECRI Institute<br />
Technology Assessment resources, current professional literature reviews, Geis<strong>in</strong>ger<br />
<strong>Health</strong> <strong>Plan</strong> Medical Directors, pharmacists, and physician consultants/experts. These<br />
policies direct <strong>in</strong>formed decisions about medical care with<strong>in</strong> the benefit structure.<br />
Once developed, Medical Policies are reviewed and approved by the MMAC. F<strong>in</strong>al<br />
approval by the Vice President, Chief Medical Officer is required.<br />
New pharmaceuticals are evaluated through the Pharmacy and Therapeutics<br />
committee, us<strong>in</strong>g specific criteria.<br />
N. DME, Home <strong>Health</strong> and Outpatient Rehab Services<br />
Management of services for DME, Home <strong>Health</strong>, and Outpatient Rehab is directed<br />
through the Medical Management Committee.<br />
O. Disease/Case Management Program<br />
1. Disease Management<br />
Please note: 1). Disease/Case Management programs overlap with quality and<br />
medical management. The specific DM programs are described <strong>in</strong> more detail <strong>in</strong><br />
the QI plan. 2). Case/Disease Management and Medical Home are the <strong>Health</strong><br />
<strong>Plan</strong> departments responsible for the coord<strong>in</strong>ation and delivery of disease/case<br />
management services.<br />
Disease Management is def<strong>in</strong>ed as the application and coord<strong>in</strong>ation of resources<br />
for a population of Members characterized by the presence of a chronic condition<br />
(such as diabetes, asthma, or heart failure). Resources are applied across the<br />
cont<strong>in</strong>uum of care and through the life cycle of disease to achieve optimum levels<br />
of wellness. The key words <strong>in</strong> disease management are “population” and “chronic<br />
illness.”<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
98
The goal of The <strong>Plan</strong>’s Disease Management Program is to promote quality health<br />
outcomes rely<strong>in</strong>g on Disease Management nurses work<strong>in</strong>g <strong>in</strong> concert with the<br />
patient, family, provider and other members of the health care team.<br />
The Disease Management Programs are established utiliz<strong>in</strong>g evidence-based<br />
Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es (developed from nationally accepted best practice parameters,<br />
specialty and practitioner <strong>in</strong>put), Stratification and Assessment <strong>Guide</strong>l<strong>in</strong>es, and<br />
<strong>in</strong>ternally developed Intervention Pathways. Members are eligible to receive<br />
education by Disease Management nurses to improve self-management skills and<br />
<strong>in</strong>dividualized support for optimal health outcomes.<br />
The goals of the Disease Management Programs are to:<br />
Improve self-management skills of Members;<br />
Promote quality healthcare <strong>in</strong>clud<strong>in</strong>g appropriate monitor<strong>in</strong>g and<br />
treatment strategies;<br />
Enhance wellness through appropriate preventive screen<strong>in</strong>gs;<br />
Coord<strong>in</strong>ate appropriate utilization of services;<br />
Facilitate and coord<strong>in</strong>ate appropriate outpatient, <strong>in</strong>patient and emergency<br />
room utilization, as <strong>in</strong>dicated.<br />
Disease Management Programs <strong>in</strong>volve voluntary participation from the Member.<br />
The <strong>Health</strong> <strong>Plan</strong> encourages active Member participation <strong>in</strong> Disease Management<br />
through direct mail<strong>in</strong>gs, Newsletters (Member Updates) and direct<br />
communication with Practitioner and Member.<br />
Current Disease Management Programs <strong>in</strong>clude:<br />
Diabetes Care Program<br />
Adult and Pediatric Asthma Care Program<br />
Stop Tobacco Use Program<br />
Osteoporosis Management Program<br />
Hypertension Program<br />
Chronic Obstructive Pulmonary Disease (COPD)<br />
Heart Failure (HF)<br />
Coronary Artery Disease (CAD)<br />
2. Complex Case Management<br />
Complex Case Management is the coord<strong>in</strong>ation of care and services for members<br />
with multiple or complex conditions or other special needs. Case Management is<br />
a collaborative process of assessment, plann<strong>in</strong>g, implementation, coord<strong>in</strong>ation,<br />
monitor<strong>in</strong>g, evaluation and advocacy for options and services to meet Member’s<br />
health care needs and to promote appropriate, cost-effective outcomes.<br />
The goals of Case Management <strong>in</strong>clude the follow<strong>in</strong>g:<br />
To assess Member/family needs and provide access to needed services;<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
99
To coord<strong>in</strong>ate care based on a strong understand<strong>in</strong>g of Member’s benefit<br />
(<strong>in</strong> cooperation with MM professional staff);<br />
To develop a plan of care <strong>in</strong> conjunction with the member/family and<br />
provider, that addresses the specific care needs relevant to the Member<br />
and to implement delivery of Case Management services <strong>in</strong> a timely<br />
fashion;<br />
To <strong>in</strong>volve the Member/family <strong>in</strong> the formulation of the Case<br />
Management plan of care and <strong>in</strong> the decision mak<strong>in</strong>g process;<br />
To focus on cont<strong>in</strong>uity of care, m<strong>in</strong>imize care fragmentation and provide a<br />
smooth transition between providers and levels of care, especially <strong>in</strong> the<br />
areas of medication reconciliation and coord<strong>in</strong>ation of services;<br />
To maximize the appropriate, efficient, and cost effective utilization of<br />
available resources.<br />
A. Nurs<strong>in</strong>g Staff<br />
The majority of Case Managers are Registered Nurses licensed <strong>in</strong> the state of<br />
Pennsylvania who provide support services, education, and coord<strong>in</strong>ation of<br />
care for serious and complex medical cases. The Case Management Program<br />
is provided directly to the Member at the practitioner’s office at owned or<br />
contracted primary care sites and/or telephonically.<br />
The Case/Disease Management staff seeks guidance when manag<strong>in</strong>g<br />
complicated cases by contact<strong>in</strong>g the on-call Medical Director and work<strong>in</strong>g<br />
directly with the member’s primary/specialty care provider.<br />
3. Proven <strong>Health</strong> Navigator<br />
The <strong>Health</strong> <strong>Plan</strong> developed and implemented a Proven <strong>Health</strong> Navigator<br />
(formerly Medical Home) program based <strong>in</strong> primary care sites across the network.<br />
The program is designed to improve the quality and efficiency of care based on<br />
primary care redesign, onsite case management, team-based care, improved<br />
access, QI strategies, care systems management and redesigned reimbursement<br />
strategies.<br />
2. Ensur<strong>in</strong>g Appropriate Utilization<br />
Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> facilitates the delivery of appropriate care and monitors the impact<br />
of the medical management program. This process is designed to assist <strong>in</strong> detect<strong>in</strong>g<br />
potential under/over utilization of services. The review consists of exam<strong>in</strong><strong>in</strong>g utilization<br />
data aga<strong>in</strong>st established thresholds and tak<strong>in</strong>g appropriate action on identified<br />
opportunities for improvement.<br />
Over/under utilization is monitored for the GOLD population us<strong>in</strong>g the follow<strong>in</strong>g HEDIS<br />
metrics.<br />
Inpatient days/1000<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
100
ALOS<br />
Outpatient visits/1000<br />
Mental health Ambulatory services<br />
Thresholds are based on the Medicare HEDIS Means, Percentiles and Ratios report, us<strong>in</strong>g<br />
the 90th and 10th percentiles.<br />
The affirmative statement regard<strong>in</strong>g the MM Decision Mak<strong>in</strong>g process is distributed to<br />
practitioners, providers, employees and members. The statement notes:<br />
MM decision mak<strong>in</strong>g is based on (1) the Medical Necessity and the<br />
appropriateness of care and services and (2) the existence of coverage tak<strong>in</strong>g <strong>in</strong>to<br />
consideration the member’s <strong>in</strong>dividual circumstances and the applicable contract<br />
language conta<strong>in</strong>ed with<strong>in</strong> the member’s benefit document concern<strong>in</strong>g covered<br />
services and exclusions.<br />
The <strong>Health</strong> <strong>Plan</strong> does not specifically reward practitioners or other <strong>in</strong>dividuals<br />
conduct<strong>in</strong>g utilization review for issu<strong>in</strong>g approvals or denials of coverage or<br />
services.<br />
The <strong>Health</strong> <strong>Plan</strong> does not offer <strong>in</strong>centives for MM decision makers that encourage<br />
decisions that might result <strong>in</strong> under utilization.<br />
3. Related Medical Management Functions<br />
A. Drug Utilization Review<br />
Drug Utilization Review (DUR) will be managed through the <strong>Plan</strong>’s Pharmacy<br />
Department, utiliz<strong>in</strong>g the processes and timeframes designated by the PA Department<br />
of <strong>Health</strong>, PA Department of Insurance, NCQA, DOL, and CMS. DUR will <strong>in</strong>clude<br />
precertification, retrospective review, provider profil<strong>in</strong>g, formulary management, and<br />
formulary design. The Medical Directors are consulted for medical necessity issues<br />
and denials. Application of new drugs, as well as formulary status decisions will be<br />
determ<strong>in</strong>ed by the Pharmacy and Therapeutics Committee, and then reported to the<br />
MMAC.<br />
B. Tel-A-Nurse<br />
Support to members for medical <strong>in</strong>formation and advice on a 24/7 basis is provided<br />
through the Tel-A-Nurse program. This program is available to all Members through<br />
a toll free telephone number.<br />
C. <strong>Provider</strong> Satisfaction Survey<br />
<strong>Provider</strong> Satisfaction Survey is utilized by the <strong>Plan</strong> to survey participat<strong>in</strong>g providers<br />
and office managers <strong>in</strong> order to determ<strong>in</strong>e areas of strength and to identify<br />
opportunities for improvement. Medical Management processes are <strong>in</strong>cluded <strong>in</strong> this<br />
survey. This survey is conducted on a yearly basis and the results are reviewed at<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
101
MMC. The results are compared to those from the year before and an action plan is<br />
presented to MMAC.<br />
D. Member Satisfaction Survey<br />
Member Satisfaction is measured <strong>in</strong> several ways. These methods <strong>in</strong>clude CAHPS<br />
Survey (annual) and post discharge surveys (on-go<strong>in</strong>g). These surveys evaluate<br />
member satisfaction with the medical management process. The results are presented<br />
to the MMAC committee.<br />
E. Notification of Review Determ<strong>in</strong>ations<br />
The MM staff provides telephonic and/or written notification of benefit<br />
determ<strong>in</strong>ations for precertification, concurrent review and retrospective review.<br />
Communication and documentation of the denial are provided to both practitioner and<br />
Member as designated by the applicable regulatory bodies.<br />
Written notification of adverse determ<strong>in</strong>ations (denials) <strong>in</strong>clude the follow<strong>in</strong>g:<br />
Pr<strong>in</strong>ciple reason(s) <strong>in</strong> easily understandable language<br />
Reference to the benefit provision, guidel<strong>in</strong>e, protocol etc, which support the<br />
denial<br />
Cl<strong>in</strong>ical rationale<br />
Explanation of the appeal/grievance/compla<strong>in</strong>t procedure<br />
Availability of the benefit provision, guidel<strong>in</strong>e, protocol, etc. that was used.<br />
F. Confidentiality<br />
To ensure Member and practitioner confidentiality, staff tra<strong>in</strong><strong>in</strong>g beg<strong>in</strong>s dur<strong>in</strong>g the<br />
Medical Management orientation program. Only confidential <strong>in</strong>formation required for<br />
the purpose of perform<strong>in</strong>g Medical Management processes is collected. Access to this<br />
<strong>in</strong>formation is limited to those employees who have a need to know and/or those<br />
employees who have authority to receive such <strong>in</strong>formation. On-l<strong>in</strong>e confidential<br />
<strong>in</strong>formation is password protected. This process adheres to the Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong><br />
confidentiality policy.<br />
Medical Management employees sign a confidentiality statement on an annual basis.<br />
G. Hours of Operation<br />
Medical Management regular hours of bus<strong>in</strong>ess are Monday through Friday from<br />
8:00 a.m. to 4:30 p.m. Medical Directors are on duty or on call 24 hours a day, seven<br />
days a week to be available for the decision processes regard<strong>in</strong>g the care of the <strong>Plan</strong>’s<br />
Members. This process is outl<strong>in</strong>ed <strong>in</strong> the MM Communications <strong>Guide</strong>l<strong>in</strong>es Policy.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
102
Quality Improvement <strong>Plan</strong><br />
Purpose<br />
The Geis<strong>in</strong>ger <strong>Health</strong> System mission is to enhance the quality of life through an <strong>in</strong>tegrated<br />
health service organization based on balanced patient care, education, research and community<br />
service. Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong>/Geis<strong>in</strong>ger Indemnity Insurance Company/Geis<strong>in</strong>ger Quality<br />
Options (“<strong>Health</strong> <strong>Plan</strong>”) supports the overall mission of Geis<strong>in</strong>ger <strong>Health</strong> System. The <strong>Health</strong><br />
<strong>Plan</strong> Quality Improvement Program provides the structure and processes for cont<strong>in</strong>uously<br />
monitor<strong>in</strong>g, analyz<strong>in</strong>g, and improv<strong>in</strong>g the cl<strong>in</strong>ical care and services provided under <strong>Health</strong> <strong>Plan</strong><br />
products <strong>in</strong> order to further that mission.<br />
The <strong>Health</strong> <strong>Plan</strong> Quality Improvement program is structured to support all product l<strong>in</strong>es<br />
<strong>in</strong>clud<strong>in</strong>g, but not limited to, Commercial HMO/POS and Gatekeeper PPO. Medicare product<br />
l<strong>in</strong>es are described <strong>in</strong> a separate document.<br />
Goals and Objectives<br />
The follow<strong>in</strong>g goals and objectives of the QI program (not <strong>in</strong> any specific order) function to<br />
support the concepts of cont<strong>in</strong>uous quality improvement.<br />
To promote optimum health care <strong>in</strong> a managed care environment.<br />
1. To conduct quality improvement activities to improve the quality of<br />
cl<strong>in</strong>ical care and services provided to members.<br />
2. To identify, through data collection and analysis, provider practice<br />
patterns, operational procedures, and other activities where improvement<br />
will enhance the quality or efficiency of health care.<br />
3. To conduct the quality improvement program based on identification of<br />
activities through methods <strong>in</strong>clud<strong>in</strong>g, but not limited to, demographic<br />
analysis, member feedback, and provider feedback.<br />
4. To prioritize quality improvement activities based on high-volume, highrisk<br />
analysis.<br />
5. To implement strong <strong>in</strong>terventions for those activities identified as<br />
opportunities for improvement.<br />
6. To conduct analysis of activity results us<strong>in</strong>g both a quantitative and barrier<br />
analysis methodology.<br />
7. To assess effectiveness of <strong>in</strong>terventions based on re-measurement and<br />
follow-up.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
103
8. To promote efficient delivery of health care by evaluat<strong>in</strong>g the utilization<br />
of primary and specialty services.<br />
9. To regularly assess the availability, accessibility and<br />
cont<strong>in</strong>uity/coord<strong>in</strong>ation of care provided to Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong><br />
members.<br />
10. To provide educational opportunities based on quality improvement<br />
f<strong>in</strong>d<strong>in</strong>gs.<br />
11. To cont<strong>in</strong>ually strive to further <strong>in</strong>tegrate quality improvement <strong>in</strong>to<br />
operations.<br />
12. To <strong>in</strong>corporate behavioral health activities <strong>in</strong>to the QI program through<br />
workgroup participation, adoption of cl<strong>in</strong>ical guidel<strong>in</strong>es and quality<br />
improvement studies/activities.<br />
13. To specify policies and procedures specific to QI activities for the <strong>Health</strong><br />
<strong>Plan</strong>.<br />
To enhance our <strong>in</strong>ter-discipl<strong>in</strong>ary approach <strong>in</strong> the care of and service to <strong>Health</strong> <strong>Plan</strong><br />
patients and/or members.<br />
1. To <strong>in</strong>clude representatives of the various health care discipl<strong>in</strong>es <strong>in</strong> the<br />
quality improvement process.<br />
2. To <strong>in</strong>volve both contracted and employed practitioners <strong>in</strong> various aspects<br />
of the QI program.<br />
3. To emphasize the importance of a team effort to produce patient<br />
satisfaction and cont<strong>in</strong>uous quality improvement.<br />
4. To enhance communication among health care team members.<br />
5. To provide <strong>in</strong>put <strong>in</strong>to the organization and content of the <strong>Health</strong> <strong>Plan</strong><br />
provider guide.<br />
6. To contribute to the formal orientation of <strong>Health</strong> <strong>Plan</strong> providers and<br />
practitioners.<br />
7. To <strong>in</strong>volve lay members of the <strong>Health</strong> <strong>Plan</strong> <strong>in</strong> multiple aspects of quality<br />
improvement.<br />
8. To assure cont<strong>in</strong>uity and coord<strong>in</strong>ation of care, <strong>in</strong>clud<strong>in</strong>g how it relates to<br />
Behavioral <strong>Health</strong> Care and services.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
104
9. To work cooperatively with the delegated entities to promote the highest<br />
level of member care and service.<br />
C. To assure <strong>in</strong>itial credential<strong>in</strong>g of all qualified practitioners and providers<br />
and subsequent recredential<strong>in</strong>g of same, <strong>in</strong> compliance with regulatory<br />
requirements.<br />
D. To assure the ma<strong>in</strong>tenance of quality medical records.<br />
1. To provide, through the <strong>Health</strong> <strong>Plan</strong> provider guide, guidel<strong>in</strong>es for<br />
documentation of medical record <strong>in</strong>formation.<br />
2. To facilitate evaluation of quality of care and cont<strong>in</strong>uity/coord<strong>in</strong>ation of<br />
care through rout<strong>in</strong>e medical record audits, as def<strong>in</strong>ed by GHP policies.<br />
E. To improve satisfaction of Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> members and<br />
providers/practitioners.<br />
1. To obta<strong>in</strong> member/provider/practitioner feedback through multiple<br />
mechanisms <strong>in</strong>clud<strong>in</strong>g but not limited to:<br />
<br />
<br />
<br />
<br />
Focus groups<br />
Member concerns/compla<strong>in</strong>ts/appeals/grievances<br />
Member surveys<br />
Practitioner/<strong>Provider</strong> feedback surveys<br />
2. To analyze member/provider/practitioner satisfaction data from the above<br />
sources, identify opportunities for improvement and implement service<br />
improvement activities with strong actions and re-measurement as<br />
appropriate.<br />
F. To assure that preventive health services are appropriately provided to<br />
members.<br />
1. To target for CQI preventive health measures required for HEDIS and<br />
NCQA standards, as well as other measures mean<strong>in</strong>gful to the<br />
membership.<br />
2. To educate members about available health promotion, health education<br />
and preventive health services<br />
G. To improve patient safety.<br />
1. To educate members regard<strong>in</strong>g cl<strong>in</strong>ical safety as it relates to their care.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
105
2. To assess and <strong>in</strong>tervene to improve the cont<strong>in</strong>uity and coord<strong>in</strong>ation of care<br />
and safety through monitor<strong>in</strong>g of return communication between PCPs<br />
and Specialists.<br />
3. To monitor physician medical record legibility and documentation to<br />
improve safe practices.<br />
H. To serve the cultural and l<strong>in</strong>guistic needs of the membership.<br />
1. To assess the cultural and l<strong>in</strong>guistic needs of the membership through onl<strong>in</strong>e<br />
and hard copy surveys and telephone <strong>in</strong>teractions.<br />
2. To employ strategies to meet the cultural and l<strong>in</strong>guistic needs of the<br />
membership through telephonic translation services and translation of<br />
member materials.<br />
I. To serve members with complex health needs.<br />
1. To serve members with complex health needs as identified <strong>in</strong> the Case<br />
Management policy through the Proven <strong>Health</strong> Navigator structure and the<br />
Case Management team.<br />
Scope of Program<br />
The scope of the quality improvement program is focused on deliver<strong>in</strong>g the highest level<br />
of quality care and service and to cont<strong>in</strong>ually enhance member satisfaction. To this end,<br />
the comprehensive program uses a wide variety of data and techniques to monitor,<br />
analyze, and evaluate proposed and ongo<strong>in</strong>g improvement activities. S<strong>in</strong>ce the <strong>in</strong>ception<br />
of the program <strong>in</strong> 1985, this process has been applied to hundreds of studies, activities,<br />
and monitors with<strong>in</strong> the <strong>Health</strong> <strong>Plan</strong>. A separate annual QI Work <strong>Plan</strong> is developed,<br />
which details the schedule of activities and tracks progress on these quality <strong>in</strong>itiatives.<br />
An Annual Evaluation is also prepared which documents the effectiveness of the QI<br />
program and measures how well it is achiev<strong>in</strong>g its goals and objectives.<br />
The QI program identifies cl<strong>in</strong>ical issues through review of HEDIS and other cl<strong>in</strong>ical<br />
data results. The QI program identifies service <strong>in</strong>itiatives through member satisfaction<br />
surveys, compla<strong>in</strong>t and appeal analysis, monitor<strong>in</strong>g systems and <strong>Health</strong> <strong>Plan</strong> operations.<br />
The scope of the QI program is broadly divided <strong>in</strong>to three areas: Cl<strong>in</strong>ical programs,<br />
Service Initiatives, and Coord<strong>in</strong>ated Activities. QI activities are described <strong>in</strong> detail <strong>in</strong> the<br />
annual QI Work <strong>Plan</strong>.<br />
QI activities performed by delegated entities are outl<strong>in</strong>ed <strong>in</strong> the delegated entity’s QI<br />
plan/workplan/annual evaluations. These documents are reviewed by the <strong>Health</strong> <strong>Plan</strong> on<br />
an annual basis.<br />
Cl<strong>in</strong>ical Programs<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
106
Preventive <strong>Health</strong> Program – The preventive health program is structured to assist<br />
physicians <strong>in</strong> assur<strong>in</strong>g members receive the preventive services they need. Education of<br />
members and providers occurs through the publication and distribution of recommended<br />
age-specific preventive services <strong>in</strong> newsletters and on the web site. QI specialists use<br />
targeted phone calls and surveys to reach out to members identified as need<strong>in</strong>g services.<br />
To ensure the effectiveness of the program, member compliance with recommended<br />
health services is measured, ma<strong>in</strong>ly us<strong>in</strong>g HEDIS methodology. Measurement and<br />
improvement activities are wide <strong>in</strong> range. Examples <strong>in</strong>clude; cervical and breast cancer<br />
screen<strong>in</strong>g, childhood and adolescent immunization, and prenatal care.<br />
Disease and Complex Case Management –The <strong>Health</strong> <strong>Plan</strong> develops and implements<br />
disease and complex case management programs. Nurses with cl<strong>in</strong>ical expertise<br />
proactively educate, manage and coord<strong>in</strong>ate care for groups of members with def<strong>in</strong>ed<br />
chronic conditions. Disease management programs that are ongo<strong>in</strong>g <strong>in</strong>clude, but are not<br />
limited to: Diabetes, Heart Failure (HF), Chronic Obstructive Pulmonary Disease<br />
(COPD), Osteoporosis, Asthma, Coronary Artery Disease (CAD), and Hypertension.<br />
Program data is reviewed at least quarterly. Programs and/or processes are revised as<br />
<strong>in</strong>dicated by data results, cl<strong>in</strong>ical guidel<strong>in</strong>e revisions, and staff feedback. The need for<br />
additional disease management programs is also evaluated on a regular basis. Complex<br />
case management <strong>in</strong>cludes post-discharge follow-up of members with targeted conditions<br />
and care of members with multiple conditions.<br />
Proven <strong>Health</strong> Navigator – The <strong>Health</strong> <strong>Plan</strong> developed and implemented a Proven <strong>Health</strong><br />
Navigator (formerly Medical Home) program based <strong>in</strong> primary care sites across the<br />
network. The program is designed to improve the quality and efficiency of care based on<br />
primary care redesign, onsite case management, team-based care, improved access, QI<br />
strategies, care systems management and redesigned reimbursement strategies.<br />
Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es – The Medical Policy/Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es Manager leads the<br />
development, implementation, and updates to cl<strong>in</strong>ical guidel<strong>in</strong>es to assist practitioners<br />
and members <strong>in</strong> the health care decision-mak<strong>in</strong>g process. Cl<strong>in</strong>ical guidel<strong>in</strong>es <strong>in</strong>clude but<br />
are not limited to: diabetes, s<strong>in</strong>usitis, asthma, pediatric otitis media, depression,<br />
hyperlipidemia <strong>in</strong> CAD, UTI and Pediatric ADHD. Cl<strong>in</strong>ical guidel<strong>in</strong>es are used as the<br />
basis for all <strong>Health</strong> <strong>Plan</strong> Disease Management programs. The <strong>Health</strong> <strong>Plan</strong> systematically<br />
assesses performance aga<strong>in</strong>st several guidel<strong>in</strong>es annually.<br />
Ongo<strong>in</strong>g Cl<strong>in</strong>ical Monitors and Studies – Based on data analysis and recommendations<br />
from the QIC and other related QI committees/work groups, relevant quality <strong>in</strong>itiatives<br />
and monitors are identified for <strong>in</strong>clusion <strong>in</strong> the QI program. All departments are<br />
responsible for the QI processes (quantitative measurements, implementation of<br />
<strong>in</strong>terventions, etc.) relat<strong>in</strong>g to these <strong>in</strong>itiatives. Active <strong>in</strong>itiatives <strong>in</strong>clude, but are not<br />
limited to the follow<strong>in</strong>g:<br />
<br />
<br />
ADHD<br />
Follow-up After A Hospital Admission for Mental Illness<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
107
Colorectal Cancer Screen<strong>in</strong>gs<br />
Breast Cancer Screen<strong>in</strong>g<br />
Cholesterol Management after a cardiac event<br />
Childhood Immunizations<br />
Other <strong>in</strong>itiatives that are cont<strong>in</strong>u<strong>in</strong>g activities <strong>in</strong>clude, but are not limited to:<br />
<br />
<br />
Persistence of Beta Blocker treatment after a heart attack<br />
Ambulatory Medical Record Review<br />
Behavioral <strong>Health</strong> Aspects of QI –<strong>Health</strong> <strong>Plan</strong> direction for these activities is provided by<br />
the Behavioral <strong>Health</strong> Oversight committee and the GHP Quality Improvement<br />
Committee led by the <strong>Health</strong> <strong>Plan</strong> VP, Chief Medical Officer. Activities be<strong>in</strong>g conducted<br />
<strong>in</strong>clude but are not limited to, follow-up after mental health admission, antidepressant<br />
medication management, readmissions with<strong>in</strong> 30 days of discharge from <strong>in</strong>patient care<br />
and <strong>in</strong>itiation and engagement of alcohol and other drug dependence treatment.<br />
Pharmaceutical Management/Coord<strong>in</strong>ation - The Pharmacy Department ma<strong>in</strong>ta<strong>in</strong>s a<br />
closed formulary that is reviewed at least annually. Coord<strong>in</strong>ation is ongo<strong>in</strong>g between<br />
pharmacy and QI to identify and conduct relevant QI/Pharmacy studies. One pharmacy<br />
related activity is asthma control.<br />
Service Initiatives<br />
Access and Availability Standards – Service <strong>in</strong>itiatives <strong>in</strong>clude measur<strong>in</strong>g performance<br />
aga<strong>in</strong>st access and availability standards and implement<strong>in</strong>g <strong>in</strong>terventions as appropriate.<br />
Access standards have been established by the <strong>Health</strong> <strong>Plan</strong> and are monitored on an<br />
annual basis. These <strong>in</strong>clude access to rout<strong>in</strong>e care appo<strong>in</strong>tments, urgent care<br />
appo<strong>in</strong>tments and after hours care. Practitioner availability is also measured on an annual<br />
basis. Two standards are used for this measurement; practitioner to member ratio and<br />
geographic distribution of practitioners. These f<strong>in</strong>d<strong>in</strong>gs are then tied <strong>in</strong>to <strong>Provider</strong><br />
Network Management recruitment plans, as feasible.<br />
Member Satisfaction Initiatives – The QI program uses <strong>in</strong>formation <strong>in</strong>clud<strong>in</strong>g: data from<br />
compla<strong>in</strong>ts and appeals, member satisfaction surveys (<strong>in</strong>clud<strong>in</strong>g CAHPS) and telephone<br />
<strong>in</strong>teractions to identify activities for improv<strong>in</strong>g member satisfaction. Ongo<strong>in</strong>g <strong>in</strong>itiatives<br />
<strong>in</strong>clude monitor<strong>in</strong>g telephone access standards, track<strong>in</strong>g compla<strong>in</strong>ts and appeals, close<br />
monitor<strong>in</strong>g of compla<strong>in</strong>t and appeal turnaround times and member satisfaction survey<br />
results analysis. The Service Improvement Committee reviews all of this <strong>in</strong>formation<br />
separately and <strong>in</strong> aggregate. Practitioner satisfaction is also assessed through an annual<br />
survey. Data is reviewed by the Service Improvement committee along with member<br />
satisfaction data to determ<strong>in</strong>e similarities/differences. This aggregate analysis is then<br />
used for identification of opportunities for improvement.<br />
Patient Safety Activities - Although the <strong>Health</strong> <strong>Plan</strong> does not adm<strong>in</strong>ister direct patient<br />
care, the safety of members is vital. Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> encourages and promotes<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
108
safety through monitor<strong>in</strong>g of member compla<strong>in</strong>ts and appeals, member education,<br />
encourag<strong>in</strong>g return communication between practitioners and monitor<strong>in</strong>g medical record<br />
legibility and documentation.<br />
Cultural and L<strong>in</strong>guistic Needs Initiatives- Collect<strong>in</strong>g data on the cultural and l<strong>in</strong>guistic<br />
needs of the membership will assist the <strong>Health</strong> <strong>Plan</strong> <strong>in</strong> identify<strong>in</strong>g areas of need.<br />
Other Service Initiatives – Service <strong>in</strong>itiatives identified through data analysis, as<br />
opportunities for improvement will be moved forward as service activities.<br />
Coord<strong>in</strong>ated Activities<br />
Over and Under Utilization Monitor<strong>in</strong>g –Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> facilitates the delivery of<br />
appropriate care and monitors the impact through the Medical Management program.<br />
This process is designed to assist <strong>in</strong> detect<strong>in</strong>g potential under/over utilization of services.<br />
Areas of focus are identified by relevancy to the <strong>Health</strong> <strong>Plan</strong> population <strong>in</strong> conjunction<br />
with high volume activities. The review consists of exam<strong>in</strong><strong>in</strong>g utilization data and tak<strong>in</strong>g<br />
appropriate action on identified opportunities for improvement.<br />
Cont<strong>in</strong>uity and Coord<strong>in</strong>ation of Care Monitor<strong>in</strong>g – The Cont<strong>in</strong>uity and Coord<strong>in</strong>ation of<br />
Care workgroup monitors care and services that members receive across the cont<strong>in</strong>uum<br />
of care and across the delivery system. Examples <strong>in</strong>clude: evaluat<strong>in</strong>g the coord<strong>in</strong>ation of<br />
medical care, tak<strong>in</strong>g action to improve the cont<strong>in</strong>uity and coord<strong>in</strong>ation of care as<br />
appropriate, and us<strong>in</strong>g medical record audit data to improve practitioner cont<strong>in</strong>uity and<br />
coord<strong>in</strong>ation of care efforts.<br />
Cont<strong>in</strong>uity and Coord<strong>in</strong>ation of Behavioral <strong>Health</strong> Care – This is monitored through both<br />
the <strong>Health</strong> <strong>Plan</strong>’s QI process. Examples <strong>in</strong>clude evaluat<strong>in</strong>g return communication<br />
between primary care and behavioral health care practitioners and assur<strong>in</strong>g follow-up for<br />
members who have been discharged from the hospital after a mental health admission.<br />
Credential<strong>in</strong>g and Recredential<strong>in</strong>g of Practitioners – The <strong>Provider</strong> Network<br />
Management, Credential<strong>in</strong>g, Accreditation and QI Departments work closely together to<br />
ma<strong>in</strong>ta<strong>in</strong> a seamless process for the credential<strong>in</strong>g and recredential<strong>in</strong>g of practitioners. The<br />
<strong>Health</strong> <strong>Plan</strong> re-credentials on a 36 month cycle.<br />
QI Program Structure<br />
The Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> QI report<strong>in</strong>g structure br<strong>in</strong>gs together work groups and<br />
committees with<strong>in</strong> the network to coord<strong>in</strong>ate QI activities across the cont<strong>in</strong>uum of care<br />
and across the organizations and facilities that deliver care. The <strong>Health</strong> <strong>Plan</strong> Board of<br />
Directors (the govern<strong>in</strong>g body) designates the <strong>Health</strong> <strong>Plan</strong> Quality Improvement<br />
Committee as the committee to oversee QI activities. As the govern<strong>in</strong>g body, the Board<br />
of Directors annually approves the QI <strong>Plan</strong>, QI Work <strong>Plan</strong> and Annual Evaluation.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
109
The QI structure consists of one ma<strong>in</strong> committee (QIC), a number of subcommittees<br />
report<strong>in</strong>g to the QIC, and a number of work groups report<strong>in</strong>g to subcommittees. Each<br />
committee or group keeps m<strong>in</strong>utes that reflect the activity, discussion, analysis, and<br />
recommendations/decisions, as well as, follow-up and resolution of prior<br />
recommendations. M<strong>in</strong>utes are dated and signed by the appropriate <strong>in</strong>dividual and<br />
available at the next meet<strong>in</strong>g.<br />
The follow<strong>in</strong>g describes the QI report<strong>in</strong>g structure:<br />
A. Quality Improvement Committee (QIC): Meets on a Quarterly Basis.<br />
1. Role –Provides direction and oversight to the Quality Improvement<br />
process and activities. It receives and acts on reports from subcommittees<br />
and work groups.<br />
2. Chairman – VP, Chief Medical Officer. (The chair is responsible for<br />
adm<strong>in</strong>istrative management of the <strong>Plan</strong>’s quality improvement<br />
activities/program.)<br />
3. Membership: (Attachment A)<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Chair—Vice President, Chief Medical Officer/Rheumatologist<br />
President and CEO<br />
Director, Pharmacy Services<br />
Vice President, <strong>Health</strong> Services<br />
Appeals Manager<br />
Director Quality Improvement/Appeals<br />
Director, Case Management/Disease Management<br />
Director, Medical Management<br />
Director, Government Programs<br />
Manager, <strong>Provider</strong> Credential<strong>in</strong>g<br />
Senior Accreditation Coord<strong>in</strong>ator<br />
Accreditation Coord<strong>in</strong>ator<br />
Manager, Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es<br />
Medical Director/VP Pharmacy, <strong>Health</strong> <strong>Plan</strong>s, North Central<br />
Region-Family Practice<br />
Medical Director, <strong>Health</strong> <strong>Plan</strong>s, Eastern Region-Family Practice<br />
Medical Director, <strong>Health</strong> <strong>Plan</strong>s, Western Region- Family Practice<br />
Medical Director, <strong>Health</strong> Services- Pediatrics<br />
Medical Director, <strong>Health</strong> Services—Pediatrics<br />
Medical Director, <strong>Health</strong> Services<br />
Practitioners (employed/contracted)<br />
United Behavioral <strong>Health</strong> representative, as needed<br />
Lay member for Commercial L<strong>in</strong>e of Bus<strong>in</strong>ess<br />
Lay member for Medicare L<strong>in</strong>e of Bus<strong>in</strong>ess<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
110
4. Reports to the <strong>Health</strong> <strong>Plan</strong> Board of Directors quarterly through the<br />
Quality Improvement Committee Chairperson.<br />
5. Responsibilities:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
To establish and approve the Quality Improvement <strong>Plan</strong> annually.<br />
To establish and approve the annual Quality Improvement Work<br />
<strong>Plan</strong>.<br />
To annually review policies and procedures related to QI activities<br />
and recommend policy decisions.<br />
To review and evaluate the results from Quality Improvement<br />
activities.<br />
To review the work and action taken by various Quality<br />
Improvement sub-committees and to give advice, direction or<br />
recommendations on further action.<br />
To assist <strong>in</strong> <strong>in</strong>stitut<strong>in</strong>g needed actions, as appropriate.<br />
To assure follow-up of open items.<br />
To oversee additional Quality Improvement activities unique to the<br />
managed care (Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong>) aspects of care, i.e.,<br />
appo<strong>in</strong>tment access, availability of services, telephone access,<br />
HEDIS, cl<strong>in</strong>ical guidel<strong>in</strong>es, disease management, care<br />
management programs, etc.<br />
To provide oversight and assure appropriate credential<strong>in</strong>g activities<br />
of practitioners contracted with Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong>.<br />
To assure practitioner participation <strong>in</strong> the QI program through<br />
committee membership and/or plann<strong>in</strong>g, design, implementation or<br />
review of activities related to the QI program.<br />
To review results and approve recommended actions of the Service<br />
Improvement Committee based on the <strong>Health</strong> <strong>Plan</strong>’s satisfaction<br />
surveys and other service data such as compla<strong>in</strong>ts and appeals.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
111
To review reports of quality issues and aggregate data on quality<br />
issues and provide oversight to recommended actions of the<br />
Medical Directors office or Peer Review Committee as applicable.<br />
To assure l<strong>in</strong>kages between the various committees and<br />
departments of the <strong>Plan</strong> as they relate to quality activities.<br />
To assure adequacy of the scope of the QI program and<br />
documentation of its effectiveness.<br />
To assure the <strong>Plan</strong> has appropriate oversight on any delegated<br />
activities.<br />
<br />
To assure a planned annual evaluation of the QI <strong>Plan</strong>, Work <strong>Plan</strong><br />
and overall QI program is conducted.<br />
B. Sub-Committees of QIC (Attachment B)<br />
1. Compliance and Privacy Committee: Meets monthly. Responsible for<br />
coord<strong>in</strong>at<strong>in</strong>g and oversee<strong>in</strong>g the implementation and completion of the<br />
Compliance <strong>Plan</strong>, <strong>in</strong>clud<strong>in</strong>g review<strong>in</strong>g and approv<strong>in</strong>g policies and<br />
procedures relat<strong>in</strong>g to compliance and privacy issues. Chair is the Vice<br />
President, Legal Services. The Committee is comprised of departmental<br />
representation with<strong>in</strong> the <strong>Health</strong> <strong>Plan</strong> <strong>in</strong>clud<strong>in</strong>g legal services,<br />
accreditation, health services, etc.<br />
2. Credential<strong>in</strong>g Committee: Meets monthly. This committee is responsible<br />
for credential<strong>in</strong>g and recredential<strong>in</strong>g of physicians for the <strong>Health</strong> <strong>Plan</strong>.<br />
Chair is the <strong>Health</strong> <strong>Plan</strong>'s Western Region Medical Director. The Vice<br />
President, Chief Medical Officer is Chairman Emeritus and a permanent<br />
committee member. The <strong>Health</strong> <strong>Plan</strong>s Peer Review Committee is a subcommittee<br />
of Credential<strong>in</strong>g. The Credential<strong>in</strong>g Committee is comprised<br />
of physicians from multiple specialties.<br />
3. Technology Assessment Committee: Meets quarterly. Responsible for<br />
evaluation of new medical technologies and new uses of exist<strong>in</strong>g<br />
technologies for <strong>in</strong>clusion <strong>in</strong> the benefit package. Chair is Medical<br />
Director, Medical Management. Committee is comprised of up to 17<br />
physicians from multiple specialties, up to 3 lay members and support<br />
staff.<br />
4. Service Improvement Committee: Meets monthly. Responsible for<br />
monitor<strong>in</strong>g and analysis of all <strong>Plan</strong> satisfaction and compla<strong>in</strong>t data with<br />
recommendations taken to and from the HEDIS Steer<strong>in</strong>g committee. The<br />
committee is also responsible for monitor<strong>in</strong>g access and availability data<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
112
on a rout<strong>in</strong>e basis. Chair is Accreditation Coord<strong>in</strong>ator. Committee is<br />
comprised of representation from Cl<strong>in</strong>ical report<strong>in</strong>g, <strong>Provider</strong> Network<br />
Management, Market<strong>in</strong>g, <strong>Health</strong> Services and Pharmacy.<br />
5. Medical Management Adm<strong>in</strong>istrative Committee: Meets monthly.<br />
Responsible for function<strong>in</strong>g as the oversight committee for the Medical<br />
Management arena. Chair is Vice President, Chief Medical Officer.<br />
Committee is comprised of multiple physicians and Adm<strong>in</strong>istrative<br />
personnel with<strong>in</strong> the <strong>Health</strong> Services, Pharmacy and <strong>Provider</strong> Network<br />
Management departments.<br />
6. Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es Committee: Meets monthly. Responsible for<br />
oversee<strong>in</strong>g and monitor<strong>in</strong>g cl<strong>in</strong>ical guidel<strong>in</strong>es, educat<strong>in</strong>g practitioners and<br />
members and ensur<strong>in</strong>g quality medical care to be measured aga<strong>in</strong>st<br />
benchmarks. Chair is Medical Policy/Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es Manager.<br />
Committee is comprised of a Medical Director, <strong>Provider</strong> Network<br />
Management, Disease/case management, Accreditation, etc.<br />
7. Delegation oversight Committee: Meets monthly. Responsible for<br />
oversee<strong>in</strong>g all delegation arrangements and assur<strong>in</strong>g compliance with all<br />
applicable external delegation regulations. Chair is Accreditation<br />
Coord<strong>in</strong>ator. Committee is comprised of legal services, medical<br />
management, pharmacy, customer service, provider network, accreditation<br />
and market research.<br />
8. M<strong>in</strong>utes:<br />
<br />
<br />
<br />
Will be generated for each meet<strong>in</strong>g and approved by the<br />
Committee.<br />
Will reflect the activity, discussion, analysis and recommendations<br />
of the Committee, as well as, follow-up and resolution of prior<br />
recommendations.<br />
Will be signed and dated.<br />
9. Work group structure:<br />
Work groups are structured to report through the Sub-Committees of the<br />
QIC. This provides more direction and oversight of the various activities,<br />
which then is reported to the QIC by the sub-committees. Refer to the<br />
Committee organizational chart attached as Attachment B.<br />
Quality Improvement and Accreditation Personnel<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
113
Role – Operational Staff for the Quality Improvement Program<br />
Vice President, Chief Medical Officer:<br />
The Vice President, Chief Medical Officer is the senior executive responsible for<br />
development, implementation and management of the <strong>Plan</strong>’s Quality<br />
Improvement program. The Chief Medical Officer has management<br />
responsibility for the QI department and the Accreditation department as well as<br />
management responsibilities for the Medical Management Program <strong>in</strong>clud<strong>in</strong>g the<br />
MM Staff, Network Management, <strong>Health</strong> <strong>Plan</strong> Pharmacy and Disease/case<br />
management. The Chief Medical Officer is ultimately responsible for<br />
implementation of all aspects of the QI program.<br />
Vice President, <strong>Health</strong> Services:<br />
The Vice President, <strong>Health</strong> Services holds adm<strong>in</strong>istrative responsibility for the<br />
Quality Improvement and Accreditation Departments, <strong>in</strong> conjunction with the<br />
Medical Management and Disease/case management Departments. The VP,<br />
<strong>Health</strong> services reports directly to the Chief Medical Officer to coord<strong>in</strong>ate the<br />
vision and direction for all Quality Improvement activities.<br />
Behavioral <strong>Health</strong> Practitioner:<br />
The <strong>Health</strong> <strong>Plan</strong> VP, Chief Medical Officer works closely with the <strong>Health</strong> <strong>Plan</strong><br />
CMO and the Behavioral <strong>Health</strong> Oversight committee for oversee<strong>in</strong>g and<br />
implement<strong>in</strong>g programs related to Behavioral <strong>Health</strong>.<br />
Staff:<br />
1. Director of Quality Improvement and Appeals reports directly to<br />
the Vice President <strong>Health</strong> services; functions to facilitate<br />
coord<strong>in</strong>ation of activities <strong>in</strong> order to assure successful<br />
implementation and ongo<strong>in</strong>g evaluation of processes, which<br />
support the QI <strong>Plan</strong>, QI Work <strong>Plan</strong> and Annual Evaluation.<br />
Responsible for staff<strong>in</strong>g and equipment and overall management of<br />
the QI and Appeals departments. Interfaces with other operational<br />
departments to assure appropriate processes that are critical to<br />
quality and service measures.<br />
2. Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> Quality Improvement Nurse Manager<br />
reports to the Director of QI and is responsible for coord<strong>in</strong>at<strong>in</strong>g<br />
and support<strong>in</strong>g the <strong>Health</strong> <strong>Plan</strong> Quality Improvement activities.<br />
The activities <strong>in</strong>clude, but are not limited to data ma<strong>in</strong>tenance,<br />
preventive health <strong>in</strong>itiatives, chart reviews, work group<br />
participation, and any relevant education (i.e., Preventive <strong>Health</strong>,<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
114
Support Staff:<br />
Tasks:<br />
HEDIS) to members and practitioners. There is feedback on all<br />
quality improvement activities at the appropriate levels.<br />
3. <strong>Health</strong> <strong>Plan</strong> Senior Accreditation Coord<strong>in</strong>ator: The <strong>Health</strong> <strong>Plan</strong><br />
Senior Accreditation Coord<strong>in</strong>ator works under the direction of the<br />
Vice President, <strong>Health</strong> services, to assure ongo<strong>in</strong>g compliance with<br />
all external regulatory standards. The Senior Accreditation<br />
Coord<strong>in</strong>ator has responsibility for education of all departments on<br />
an ongo<strong>in</strong>g basis to assure understand<strong>in</strong>g and compliance with<br />
applicable standards/regulations.<br />
4. <strong>Health</strong> <strong>Plan</strong> Accreditation Coord<strong>in</strong>ator: The <strong>Health</strong> <strong>Plan</strong><br />
Accreditation Coord<strong>in</strong>ator works under the direction of the Senior<br />
Accreditation Coord<strong>in</strong>ator. The Coord<strong>in</strong>ator is responsible for<br />
assist<strong>in</strong>g with ongo<strong>in</strong>g compliance with external regulatory<br />
standards and education of departments to assure understand<strong>in</strong>g<br />
and compliance with applicable standards/regulations.<br />
5. Regional QI Nurses (5)<br />
6. Quality Improvement Specialists (8)<br />
7. QI Service/Data Coord<strong>in</strong>ator<br />
8. HEDIS coord<strong>in</strong>ator<br />
9. Cont<strong>in</strong>uous QI Coord<strong>in</strong>ator<br />
1. Information Technology staff<br />
2. Disease/case management staff<br />
3. Cl<strong>in</strong>ical and Operational report<strong>in</strong>g team staff<br />
4. MM Department<br />
5. <strong>Provider</strong> Network Representatives<br />
6. Credential<strong>in</strong>g<br />
1. Responsible for all <strong>in</strong>ventory, track<strong>in</strong>g and follow-up of <strong>Health</strong><br />
<strong>Plan</strong>s QI activities. To obta<strong>in</strong>, assess, and act upon Quality<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
115
Improvement data, <strong>in</strong>clud<strong>in</strong>g Quality Improvement Committee<br />
m<strong>in</strong>utes and Quality Improvement <strong>Plan</strong>s.<br />
2. To assure completion of chart audits and other data gather<strong>in</strong>g<br />
activities required by the Quality Improvement Committee.<br />
3 To attend cont<strong>in</strong>u<strong>in</strong>g education programs <strong>in</strong> Quality Improvement<br />
to provide expertise to the Quality<br />
Improvement Committee.<br />
4. To facilitate Quality Improvement accreditation processes and to<br />
meet regulatory agency requirements.<br />
5. To meet standards set for compliance with applicable law.<br />
Quality Improvement at Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> Contracted Facilities<br />
Geis<strong>in</strong>ger <strong>Health</strong> <strong>Plan</strong> contracts with multiple facilities. To assure quality care for our<br />
members, these facilities/providers are assessed and monitored us<strong>in</strong>g established criteria<br />
prior to the sign<strong>in</strong>g of a contract and at least every three years thereafter.<br />
Delegated Activities<br />
The <strong>Health</strong> <strong>Plan</strong> has the ability to delegate activities as described with<strong>in</strong> the NCQA<br />
standards. Specific criteria must be met for delegation to occur as described <strong>in</strong> the<br />
Delegation Oversight policy (Attachment D). Specific delegation arrangements are<br />
outl<strong>in</strong>ed <strong>in</strong> the attached spreadsheet (Attachment E).<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Medical Management and Quality Improvement and Accreditation<br />
116
Section 6: Glossary and Acronyms<br />
GLOSSARY..............................................................................................................................................118<br />
ACRONYMS............................................................................................................................................127<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
117
Glossary<br />
Agreement: The Agreement to provide <strong>Health</strong> Care Services, together with any attachments,<br />
exhibits, applicable <strong>Provider</strong> <strong>Guide</strong>(s), Benefit Documents, as amended from time to time and<br />
made a part of this Agreement by reference between Participat<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong> or<br />
Participat<strong>in</strong>g <strong>Provider</strong> and GHO.<br />
Ambulatory Surgical Center: A facility or portion thereof not located upon the premises of a<br />
hospital which provides specialty or multi-specialty outpatient surgical treatment. This does not<br />
<strong>in</strong>clude <strong>in</strong>dividual or group practice offices of private physicians or dentists, unless the offices<br />
have a dist<strong>in</strong>ct part used solely for outpatient surgical treatment on a regular and organized basis.<br />
Ambulatory Surgical Center <strong>Provider</strong>: An ambulatory surgical center licensed, certified or<br />
otherwise regulated under the laws of the state <strong>in</strong> which it operates, that has an agreement with<br />
GHO to provide Covered Services to Members.<br />
Benefit Document(s): The Subscription Certificate, Schedule of Benefits and any Rider(s)<br />
thereto and/or Summary <strong>Plan</strong> Document which sets forth the terms, conditions and benefits of<br />
coverage for Members enrolled <strong>in</strong> GHO WVUHS TPA.<br />
Billed Charges: Those charges, determ<strong>in</strong>ed prior to deduction for discounts and contractual<br />
adjustments, which are usually and customarily billed by a provider to all its patients for a<br />
particular service, as adjusted from time to time.<br />
Bus<strong>in</strong>ess Day: A day other than Saturday, Sunday or a legal holiday when commercial banks are<br />
generally open for bus<strong>in</strong>ess.<br />
Medical Management: A method of manag<strong>in</strong>g a Member’s health care by coord<strong>in</strong>at<strong>in</strong>g care,<br />
improv<strong>in</strong>g cont<strong>in</strong>uity and quality of care <strong>in</strong> the most efficient manner.<br />
Clean Claim: A claim for payment for a Covered Service which has no defect or impropriety. A<br />
defect or impropriety shall <strong>in</strong>clude lack of required substantiat<strong>in</strong>g documentation or a particular<br />
circumstance requir<strong>in</strong>g special treatment which prevents timely payment from be<strong>in</strong>g made on the<br />
claim. The term shall not <strong>in</strong>clude a claim from a <strong>Health</strong> Care <strong>Provider</strong> who is under <strong>in</strong>vestigation<br />
for fraud or abuse regard<strong>in</strong>g that claim.<br />
Cl<strong>in</strong>ical <strong>Guide</strong>l<strong>in</strong>es: Systematically developed statements to assist a provider and patient <strong>in</strong><br />
mak<strong>in</strong>g decisions about appropriate health care for specific cl<strong>in</strong>ical circumstances.<br />
Co<strong>in</strong>surance: A form of cost shar<strong>in</strong>g which requires the Member to pay a portion of the cost of<br />
Covered Services. A Co<strong>in</strong>surance is a set percentage of this cost.<br />
Company: Shall mean Geis<strong>in</strong>ger Indemnity Insurance Company.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
118
Concurrent Review: A medical management technique used by managed care organizations to<br />
ensure that Medically Necessary and appropriate care is delivered dur<strong>in</strong>g a Member’s<br />
hospitalization or other <strong>in</strong>patient episode.<br />
Covered Person: An <strong>in</strong>dividual eligible to receive Covered Services or other benefits under the<br />
terms of the applicable Benefit Documents as the Subscriber or an eligible enrolled family<br />
dependent. A Covered Person may also be referred to as a Member.<br />
Covered Service: A Medically Necessary (unless otherwise <strong>in</strong>dicated) service or supply<br />
specified <strong>in</strong> a Member’s Subscription Certificate for which benefits will be provided pursuant to<br />
the terms of a Subscription Certificate or any Medically Necessary Supplemental <strong>Health</strong> Services<br />
set forth <strong>in</strong> any Riders supplement<strong>in</strong>g a Subscription Certificate.<br />
Customer Service Team (CST): GHO representatives who can answer Member and <strong>Health</strong><br />
Care <strong>Provider</strong> questions and provide <strong>in</strong>formation regard<strong>in</strong>g GHO and a Member’s Coverage.<br />
The telephone number for the Customer Service Team is set forth on the back of the Member‘s<br />
Identification Card.<br />
Deductible: A specific dollar amount that must be <strong>in</strong>curred and paid by a Member or a<br />
Member’s family before GHO will assume any liability for all or part of the cost of Covered<br />
Services.<br />
Durable Medical Equipment: Equipment designed to serve a medical purpose and which is not<br />
generally useful for a Member <strong>in</strong> the absence of illness or <strong>in</strong>jury, is able to withstand repeated<br />
use, is appropriate for use <strong>in</strong> the home and is not a disposable supply.<br />
Emergency: A medical condition with acute symptoms of severity or severe pa<strong>in</strong> such that a<br />
prudent layperson, who possesses an average knowledge of health and medic<strong>in</strong>e, could<br />
reasonably expect the absence of immediate medical attention to result <strong>in</strong> plac<strong>in</strong>g the health of<br />
the Member, or, with respect to a pregnant woman, the health of the Member or her unborn<br />
child, <strong>in</strong> serious jeopardy; serious impairment to bodily functions; or serious dysfunction of any<br />
organ or body part.<br />
Emergency Services: Any <strong>Health</strong> Care Service provided to a Member after the sudden onset of<br />
a medical condition that manifests itself by acute symptoms of sufficient severity or severe pa<strong>in</strong>,<br />
such that a prudent lay person, who possesses an average knowledge of health and medic<strong>in</strong>e,<br />
could reasonably expect the absence of immediate medical attention to result <strong>in</strong>:<br />
• Plac<strong>in</strong>g the health of the Member, or, with respect to a pregnant women, the health of the<br />
Member or her unborn child, <strong>in</strong> serious jeopardy;<br />
• Serious impairment to bodily functions; or<br />
• Serious dysfunction of any bodily organ or part.<br />
Transportation and related Emergency Services provided by a licensed ambulance service shall<br />
constitute an Emergency Service if the condition is as described <strong>in</strong> this def<strong>in</strong>ition.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
119
Employer: An employer who has an agreement with Company for the provision of third party<br />
adm<strong>in</strong>istrative services by Company, and access to GHO’s Network for Employer’s health<br />
benefits plan(s).<br />
Employer-Sponsored Program: A program established and ma<strong>in</strong>ta<strong>in</strong>ed by an Employer for the<br />
purpose of provid<strong>in</strong>g its members with health care benefits which may be subject to the<br />
requirements of the Employee Retirement Income Security Act of 1974 (ERISA).<br />
Formulary: A cont<strong>in</strong>ually updated list of prescription medications that represents the current<br />
covered drugs by GHO based upon the cl<strong>in</strong>ical judgment of GHO’s Pharmacy and Therapeutics<br />
Committee. The Formulary conta<strong>in</strong>s both brand name drugs and generic drugs, all of which<br />
have been approved by the Federal Food and Drug Adm<strong>in</strong>istration (FDA).<br />
Formulary Committee: A committee comprised of physicians, pharmacists and adm<strong>in</strong>istrative<br />
staff which makes recommendations regard<strong>in</strong>g Formulary decisions.<br />
Governmental Agency: Shall refer to the applicable state requirements pursuant to GHO’s<br />
licensure, the Centers for Medicare and Medicaid Services or other government departments or<br />
their respective agents with direct responsibilities to access records for the purpose of quality<br />
assurance, <strong>in</strong>vestigation of compla<strong>in</strong>ts or grievances, enforcement or other activities related to<br />
compliance with applicable laws and regulations and shall specifically <strong>in</strong>clude the National<br />
Committee for Quality Assurance, as applicable.<br />
Group: The employer, association, union or trust through which the Subscriber is enrolled.<br />
<strong>Health</strong> Care <strong>Provider</strong>: A licensed Hospital or health care facility, medical equipment supplier<br />
or person who is licensed, certified or otherwise regulated to provide <strong>Health</strong> Care Services under<br />
any applicable law <strong>in</strong>clud<strong>in</strong>g a physician, podiatrist, optometrist, psychologist, physical therapist,<br />
certified nurse practitioner, registered nurse, nurse midwife, physician’s assistant, chiropractor,<br />
dentist, pharmacist or an <strong>in</strong>dividual accredited or certified to provide behavioral health services.<br />
<strong>Health</strong> Care Service: Any covered treatment, admission, procedure, medical supplies and<br />
equipment, or other services, <strong>in</strong>clud<strong>in</strong>g behavioral health, prescribed or otherwise provided or<br />
proposed to be provided by a <strong>Health</strong> Care <strong>Provider</strong> to a Member as deemed Medically<br />
Necessary.<br />
<strong>Health</strong> Insurance Portability and Accountability Act of 1996 (HIPAA): A federal law, as<br />
may be amended from time-to-time, <strong>in</strong>clud<strong>in</strong>g, but not limited to, the follow<strong>in</strong>g: a) limit<strong>in</strong>g<br />
exclusions for pre-exist<strong>in</strong>g conditions (as def<strong>in</strong>ed under HIPAA); b) prohibit<strong>in</strong>g discrim<strong>in</strong>ation<br />
aga<strong>in</strong>st employees and dependents based on their health status; c) guarantee<strong>in</strong>g renewability and<br />
availability of health coverage to certa<strong>in</strong> employers and <strong>in</strong>dividuals; d) protect<strong>in</strong>g certa<strong>in</strong><br />
Members who lose Group health coverage by provid<strong>in</strong>g access to <strong>in</strong>dividual health <strong>in</strong>surance<br />
coverage; and e) regulat<strong>in</strong>g the use and disclosure of protected health <strong>in</strong>formation.<br />
<strong>Health</strong> Ma<strong>in</strong>tenance Organization (HMO): An organized system that comb<strong>in</strong>es the delivery<br />
and f<strong>in</strong>anc<strong>in</strong>g of health care and which provides or arranges for the provision of basic health<br />
services to voluntarily enrolled members for a fixed prepaid fee.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
120
Home <strong>Health</strong>/Hospice <strong>Provider</strong> or Home <strong>Health</strong> <strong>Provider</strong> or Hospice <strong>Provider</strong>: A<br />
Medicare-certified agency under agreement with GHO which provides: (i) <strong>in</strong>termittent skilled<br />
nurs<strong>in</strong>g services and other therapeutic services <strong>in</strong> a Member’s home when Medically Necessary;<br />
and when authorized by a Participat<strong>in</strong>g <strong>Provider</strong> unless otherwise permitted <strong>in</strong> accordance with<br />
the terms and conditions set forth <strong>in</strong> a Member’s Benefit Document; and/or (ii) hospice services,<br />
as applicable. A Home <strong>Health</strong>/Hospice <strong>Provider</strong> or Home <strong>Health</strong> <strong>Provider</strong> or Hospice <strong>Provider</strong><br />
must be Medicare-certified <strong>in</strong> order to render care to a Gold Member.<br />
Home <strong>Health</strong> Services: Medically Necessary <strong>Health</strong> Care Services, which are: (i) rendered <strong>in</strong><br />
the Member’s place of residency by health care personnel; (ii) referred to a Home <strong>Health</strong><br />
<strong>Provider</strong> by the Home <strong>Health</strong>/Hospice Management Department; (iii) provided <strong>in</strong> accordance<br />
with the Member’s Benefit Document; (iv) rendered <strong>in</strong> accordance with a treatment plan<br />
established by a Home <strong>Health</strong> <strong>Provider</strong> and a Member’s physician; or if so required by the terms<br />
and conditions of coverage set forth <strong>in</strong> a Member’s Benefit Document, by a Member’s physician<br />
Participat<strong>in</strong>g <strong>Provider</strong>: and (v) authorized by the Home <strong>Health</strong>/Hospice Management<br />
Department. Home <strong>Health</strong> Services may <strong>in</strong>clude the adm<strong>in</strong>istration of Home Infusion, as<br />
applicable.<br />
Hospice: A Covered Service rendered by a Preferred <strong>Provider</strong> who is licensed as a provider of<br />
Hospice services <strong>in</strong> accordance with the state requirements where services are provided and is a<br />
certified provider of Hospice services under Medicare.<br />
Hospice Services: Medically Necessary <strong>Health</strong> Care Services which are: (i) referred to a<br />
Hospice <strong>Provider</strong> by the Home <strong>Health</strong>/Hospice Management Department; (ii) provided <strong>in</strong><br />
accordance with a Member’s Benefit Document; (iii) rendered <strong>in</strong> accordance with a <strong>Plan</strong> of Care<br />
established by a Hospice <strong>Provider</strong> and a Member’s physician; or if so required by the terms and<br />
conditions of coverage set forth <strong>in</strong> a Member’s Benefit Document, by a Member’s physician<br />
Participat<strong>in</strong>g <strong>Provider</strong> and authorized by the Home <strong>Health</strong>/Hospice Management Department;<br />
(iv) rendered for conditions related to the Term<strong>in</strong>al Illness; and (v) provided <strong>in</strong> accordance with<br />
the Member’s executed advance directive.<br />
Hospital: An <strong>in</strong>stitution which: (i) provides diagnostic, surgical and therapeutic services for the<br />
diagnosis, treatment and care of <strong>in</strong>jured or ill persons by or under the supervision of physicians;<br />
and (ii) is licensed, certified or otherwise regulated to provide such services and to operate as a<br />
hospital under the laws of the state <strong>in</strong> which it operates and/or federal laws, as applicable. The<br />
term “Hospital” does NOT <strong>in</strong>clude a Skilled Nurs<strong>in</strong>g Facility, convalescent nurs<strong>in</strong>g home,<br />
custodial care home, health resort, spa or sanitarium. A Hospital must be Medicare-certified <strong>in</strong><br />
order for a Gold Member to receive care at the Hospital.<br />
Hospital <strong>Provider</strong>: A Hospital that has an agreement with GHO to provide Covered Services to<br />
Members.<br />
Hospital Services: The Covered Services to be provided by Hospital <strong>Provider</strong> to Members as set<br />
forth <strong>in</strong> the Agreement.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
121
Identification Card: The card issued by GHO to identify Members enrolled <strong>in</strong> Geis<strong>in</strong>ger <strong>Health</strong><br />
Options WVUHS TPA. Possession of an Identification Card confers no right to Covered<br />
Services or other benefits. To be entitled to Covered Services or other benefits, the holder of the<br />
card must, <strong>in</strong> fact, be a Member on whose behalf all amounts due to GHO have been paid by an<br />
Employer.<br />
Intermediate Care: A level of care that is less than the degree of care and treatment that Skilled<br />
Nurs<strong>in</strong>g Facility is designed to provide, but greater than the level of room and board.<br />
Medical Director: The licensed physician designated by GHO to direct the medical and<br />
scientific aspects of GHO, and to monitor and oversee the quality and appropriateness of<br />
managed health services.<br />
Medically Necessary or Medical Necessity means Covered Services rendered by a <strong>Health</strong> Care<br />
<strong>Provider</strong> that GHO determ<strong>in</strong>es are: (i) appropriate for the symptoms and diagnosis or treatment<br />
of the Member’s condition, illness, disease or <strong>in</strong>jury; (ii) provided for the diagnosis and the<br />
direct care and treatment of the Member’s condition, illness, disease or <strong>in</strong>jury; (iii) <strong>in</strong> accordance<br />
with current standards of good medical treatment practiced by the general medical community;<br />
(iv) not primarily for the convenience of the Member, or the Member’s <strong>Health</strong> Care <strong>Provider</strong>;<br />
and (v) the most appropriate source or level of service that can safely be provided to the<br />
Member. When applied to hospitalization, this further means that the Member requires acute care<br />
as an <strong>in</strong>patient due to the nature of the services rendered or the Member’s condition, and the<br />
Member cannot receive safe or adequate care as an outpatient.<br />
Medical Services or Professional Services: Those services normally provided by a PCP or SCP<br />
<strong>in</strong> the diagnosis and treatment of Members to the extent that they are Medically Necessary and<br />
covered under the terms of a Member’s applicable Benefit Document. This <strong>in</strong>cludes supplies,<br />
<strong>in</strong>jections, diagnostic tests and other services and procedures with<strong>in</strong> the scope of the<br />
practitioner’s professional competence and normal practice.<br />
Medicare (Program): The programs of health care for the aged and disabled established by<br />
Title XVIII of the United States Social Security Act of 1965, as may be amended from time to<br />
time.<br />
Member: An <strong>in</strong>dividual eligible to receive Covered Services or other benefits under the terms of<br />
the applicable Benefit Documents as the Subscriber or an eligible enrolled family dependent. A<br />
Member may also be referred to as a Covered Person.<br />
Network: The Participat<strong>in</strong>g <strong>Provider</strong>s who have entered <strong>in</strong>to a written agreement with GHO to<br />
provide Covered Services to its Members.<br />
Non-Covered Services: Any service not covered under the terms of a Member’s Benefit<br />
Document.<br />
Observation Services: Those certa<strong>in</strong> outpatient services furnished by Participat<strong>in</strong>g <strong>Provider</strong> to<br />
Members that <strong>in</strong>clude the use of a bed and periodic monitor<strong>in</strong>g by Participat<strong>in</strong>g <strong>Provider</strong>’s<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
122
nurs<strong>in</strong>g or other staff which are reasonable and necessary to monitor a Member’s condition; or to<br />
determ<strong>in</strong>e the need for a Member’s admission to Participat<strong>in</strong>g <strong>Provider</strong> as an <strong>in</strong>patient.<br />
Observation Services may be extended beyond twenty-three (23) hours upon advance<br />
authorization by GHO Medical Director.<br />
Orthotic Device: A device which is a rigid appliance or apparatus used to support, align or<br />
correct bone and muscle deformities.<br />
Participat<strong>in</strong>g <strong>Health</strong> Care <strong>Provider</strong> or Participat<strong>in</strong>g <strong>Provider</strong>: A physician, medical group,<br />
pharmacy, Hospital or other provider of health services, licensed, certified or otherwise regulated<br />
under the laws of the state <strong>in</strong> which it operates, that has an agreement with GHO to provide<br />
Covered Services to Members.<br />
Payor: An employer, ERISA plan sponsor or trust fund <strong>in</strong>surance carrier or any other entity that<br />
accepts fiduciary responsibility for an established program of health benefits to Payor’s<br />
<strong>in</strong>sureds/members, or any other entity which has contracted with GHO to use GHO’s Network.<br />
Policy: The certificate and/or agreement, as may be amended, which sets forth the terms,<br />
conditions and benefits of coverage, as awarded by GHO to its Members, as applicable. A<br />
Policy may also be referred to as a Subscription Certificate.<br />
Policy Holder: An <strong>in</strong>dividual who meets the requirements for eligibility, who has enrolled <strong>in</strong><br />
GHO, and for whom payment has actually been received by GHO. A Subscriber is also a<br />
Member. A Policy Holder may also be referred to as a Subscriber.<br />
Protected <strong>Health</strong> Information (“PHI”): Individually Identifiable <strong>Health</strong> <strong>in</strong>formation (as<br />
def<strong>in</strong>ed by HIPAA), whether oral or transmitted by electronic media, ma<strong>in</strong>ta<strong>in</strong>ed by electronic<br />
media or transmitted or ma<strong>in</strong>ta<strong>in</strong>ed <strong>in</strong> any form or medium, <strong>in</strong>clud<strong>in</strong>g demographic <strong>in</strong>formation<br />
collected from an <strong>in</strong>dividual, and a.) created or received by a <strong>Health</strong> Care <strong>Provider</strong>, GHO,<br />
employer or health care clear<strong>in</strong>ghouse; and b.) relates to the past, present or future physical or<br />
mental condition of an <strong>in</strong>dividual, as well as the provision of health care to an <strong>in</strong>dividual or the<br />
past, present or future payment for the provision of healthcare to an <strong>in</strong>dividual and (i) that<br />
identifies the <strong>in</strong>dividual; or (ii) with respect to which there is a reasonable basis to believe the<br />
<strong>in</strong>formation can be used to identify the <strong>in</strong>dividual.<br />
Primary Care Physician (PCP): A Participat<strong>in</strong>g <strong>Provider</strong> physician who, with<strong>in</strong> the scope of<br />
the physician’s practice; (i) supervises, coord<strong>in</strong>ates, prescribes or otherwise provides <strong>Health</strong> Care<br />
Services to a Member and <strong>in</strong>itiates a Gatekeeper Product Member’s Referral for specialty care,<br />
as may be required <strong>in</strong> accordance with a Member’s applicable Benefit Document; (ii) ma<strong>in</strong>ta<strong>in</strong>s<br />
cont<strong>in</strong>uity of care; and (iii) is so designated by GHO.<br />
Primary Care Site: The medical office, health center, or other facility, or a designated<br />
department of a medical facility, staffed by one or more Primary Care Physicians, and designated<br />
a Primary Care Site by GHO.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
123
Professional Services or Medical Services: Those services normally provided by a SCP <strong>in</strong> the<br />
diagnosis and treatment of Members to the extent that they are Medically Necessary and covered<br />
under the terms of a Member’s applicable Benefit Document. This <strong>in</strong>cludes diagnostic tests and<br />
other services and procedures with<strong>in</strong> the scope of the practitioner’s professional competence and<br />
normal practice.<br />
Prosthetic Device: A device, which is an externally worn appliance or apparatus, which replaces<br />
a miss<strong>in</strong>g body part.<br />
<strong>Provider</strong> List: A published list<strong>in</strong>g (as amended from time to time) provided to Members by<br />
GHO which sets forth the names, addresses and telephone numbers of current <strong>Provider</strong>s who<br />
have contracted with GHO to provide Covered Services. The current <strong>Provider</strong> List can be found<br />
on GHO’s website (www.thehealthplan.com/wvuh_providers_us/) or obta<strong>in</strong>ed by call<strong>in</strong>g the<br />
Customer Service Team at the number on the back of the Member’s Identification Card.<br />
Rider: A document that sets forth the terms and conditions for coverage of certa<strong>in</strong> Supplemental<br />
<strong>Health</strong> Services <strong>in</strong> effect for the Subscriber and all family dependents enrolled under the<br />
Subscription Certificate.<br />
Schedule of Benefits: A summary of coverage for a Member that identifies the Subscriber,<br />
applicable Copayment, Deductible and Co<strong>in</strong>surance amounts for Covered Services and any<br />
Riders <strong>in</strong> force of the Benefit Documents.<br />
Service Area: The counties where GHO is licensed to operate by the applicable state regulatory<br />
agency and/or CMS, as applicable, as may be amended from time to time.<br />
Skilled Nurs<strong>in</strong>g Facility (SNF): A facility which: (i) provides <strong>in</strong>patient skilled nurs<strong>in</strong>g care,<br />
rehabilitation services or other related health services; (ii) is licensed, certified or otherwise<br />
regulated to provide such services under the laws of the state where SNF Services are rendered;<br />
and (iii) is certified by Medicare. The term Skilled Nurs<strong>in</strong>g Facility does NOT <strong>in</strong>clude a<br />
convalescent nurs<strong>in</strong>g home, rest facility or facility for the aged which furnishes primarily<br />
custodial care, <strong>in</strong>clud<strong>in</strong>g tra<strong>in</strong><strong>in</strong>g <strong>in</strong> activities of daily liv<strong>in</strong>g.<br />
Skilled Nurs<strong>in</strong>g Facility (SNF) <strong>Provider</strong>: A Skilled Nurs<strong>in</strong>g Facility that has an agreement<br />
with GHO to provide Covered Services to Members.<br />
Skilled Nurs<strong>in</strong>g Facility (SNF) Services: Skilled Nurs<strong>in</strong>g Facility (SNF) Services are certa<strong>in</strong><br />
Medically Necessary skilled health care services which: (i) consist of comprehensive, <strong>in</strong>patient<br />
care designed for the medically stable Member who requires skilled nurs<strong>in</strong>g or skilled<br />
rehabilitation services as identified by the then current <strong>in</strong>dustry-standard medical review<br />
criterion <strong>in</strong> use by GHO <strong>in</strong>clud<strong>in</strong>g, but not limited to, Milliman and Medicare guidel<strong>in</strong>es; (ii) are<br />
covered under the terms of a Member’s applicable Benefit Document; and (iii) are for<br />
Gatekeeper Product Members, when authorized by a Primary care Physician of such Member’s<br />
Primary Care Site or the Medical Director unless otherwise permitted <strong>in</strong> accordance with the<br />
terms and conditions of coverage set forth <strong>in</strong> the Member’s Benefit Document. SNF Services do<br />
not <strong>in</strong>clude custodial, convalescent or domiciliary care.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
124
Solicitation: Any conduct by a Participat<strong>in</strong>g <strong>Provider</strong>, its agents, employees, assignees or<br />
successors, which may be reasonably <strong>in</strong>terpreted as an attempt to persuade Members, Employers,<br />
Groups or others to: (i) discont<strong>in</strong>ue their enrollment with GHO but cont<strong>in</strong>ue to obta<strong>in</strong> <strong>Health</strong><br />
Care Services from the Participat<strong>in</strong>g <strong>Provider</strong>; and/or (ii) encourage Members to participate <strong>in</strong><br />
any other prepaid health plan or program of third party reimbursement.<br />
Specialist: A <strong>Health</strong> Care <strong>Provider</strong> whose practice is not limited to primary health care<br />
services and who has additional postgraduate or specialized tra<strong>in</strong><strong>in</strong>g, board certification or<br />
practices <strong>in</strong> a licensed specialized area of health care.<br />
Specialty Care <strong>Provider</strong>: A Participat<strong>in</strong>g <strong>Provider</strong> Specialist who provides the necessary<br />
evaluation, treatment and follow-up care for GHO Members.<br />
Subscriber: An <strong>in</strong>dividual who meets the requirements for eligibility, who has enrolled <strong>in</strong> GHO,<br />
and for whom payment has actually been received by GHO. A Subscriber is also a Member. A<br />
Subscriber may also be referred to as a Policy Holder.<br />
Subscription Certificate: The certificate and/or agreement, as may be amended, which sets<br />
forth the terms, conditions and benefits of coverage, as awarded by GHO to its Members, as<br />
applicable. A Subscription Certificate may also be referred to as a Policy.<br />
Summary <strong>Plan</strong> Document (SPD): An Employer document which sets forth the terms,<br />
conditions and benefits of coverage for Members enrolled through an Employer-Sponsored<br />
Program.<br />
Supplemental <strong>Health</strong> Services: Benefits of coverage provided under the Riders listed on the<br />
Schedule of Benefits.<br />
Technology Assessment Committee: A committee of cl<strong>in</strong>icians and/or other <strong>in</strong>dividuals, which<br />
review new or presently non-covered medical equipment, procedures and treatments <strong>in</strong> order to,<br />
among other th<strong>in</strong>gs, advise GHO on the experimental or non-experimental nature of any<br />
equipment, procedure or treatment and/or appropriate coverage status of any equipment,<br />
procedure treatment.<br />
Tel-A-Nurse (TANS): A twenty-four (24) hour per day, toll free telephone number for Members<br />
to access nurse advice. The toll free telephone number is set forth on Member’s Identification<br />
Card. Tel-A-Nurse is not an authorized agent for purposes of coverage determ<strong>in</strong>ation or<br />
appo<strong>in</strong>tment schedul<strong>in</strong>g.<br />
Third Party Adm<strong>in</strong>istrator (TPA): An organization which performs adm<strong>in</strong>istrative services<br />
such as claims process<strong>in</strong>g, claims payment, membership services and utilization review for<br />
employee health benefits plans. Company is a TPA for Employers<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
125
Urgent Care: Any Covered <strong>Health</strong> Care Service provided to a Member <strong>in</strong> a situation, which<br />
requires care with<strong>in</strong> twenty-four (24) hours. Urgent Care does not rise to the level of an<br />
Emergency as it allows the Member and provider to consider alternative sett<strong>in</strong>gs of care.<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
126
Acronyms<br />
ALJ: Adm<strong>in</strong>istrative Law Judge<br />
ASC: Ambulatory Surgical Center<br />
ATOD: Alcohol, Tobacco and/or Drugs<br />
CCM: Catastrophic Case Management<br />
CHAP: Community <strong>Health</strong> Accreditation Program<br />
CHDR: Center for <strong>Health</strong> Dispute Resolution<br />
CHF: Congestive Heart Failure<br />
CME: Cont<strong>in</strong>u<strong>in</strong>g Medical Education<br />
CMN: Certificate of Medical Necessity<br />
CMS: Center for Medicare and Medicaid Services<br />
COB: Coord<strong>in</strong>ation of Benefits<br />
COPD: Chronic Obstructive Pulmonary Disease<br />
CPC: Cl<strong>in</strong>ical Practice Committee<br />
CPT®: Physician’s Current Procedural Term<strong>in</strong>ology<br />
CRDQ: Chronic Respiratory Disease Questionnaire<br />
CRMS: Care Enhance Resource Management System<br />
CST: Customer Service Team<br />
DAB: Department Appeals Board<br />
DEC: Diagnostic Equivalent Category<br />
DME: Durable Medical Equipment<br />
DRG: Diagnostic Related Groups<br />
EDI: Electronic Data Interchange<br />
EOP: Explanation of Payment<br />
ERISA: Employee Retirement Security Income Act of 1974<br />
HAC: Hospital Acquired Condition<br />
HAP: Hospital and <strong>Health</strong> System Association of Pennsylvania<br />
HEDIS®: <strong>Health</strong>care Effectiveness Data and Information Set<br />
HHS: <strong>Health</strong> and Human Services<br />
HIPAA: <strong>Health</strong> Insurance Portability and Accountability Act of 1996<br />
HIPPS: <strong>Health</strong> Insurance Prospective Payment System<br />
HMO: <strong>Health</strong> Ma<strong>in</strong>tenance Organization<br />
ICD-9-CM: International Classification of Disease, 9th Edition<br />
INR: International Normalized Ratio<br />
JCAHO: Jo<strong>in</strong>t Commission on Accreditation of <strong>Health</strong> Care Organizations<br />
LCM: Large Case Management<br />
LOB: L<strong>in</strong>e of Bus<strong>in</strong>ess<br />
LOS: Length of Stay<br />
MCE: Medical Care Evaluations<br />
MDS: M<strong>in</strong>imum Data Set<br />
MHAC: Modified <strong>Health</strong> Assessment Questionnaire<br />
MI: Myocardial Infarction<br />
MMT: Manual Muscle Tone<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
127
NCQA: National Committee for Quality Assurance<br />
NOMNC: Notice of Medicare Non-Coverage<br />
OPM: Office of Personnel Management<br />
PCF: Personal Care Facility<br />
PCP: Participat<strong>in</strong>g Primary Care Physician<br />
PDCA: <strong>Plan</strong>, Do, Check, Act<br />
PNM: <strong>Provider</strong> Network Management<br />
POA: Present on Admission<br />
POS: Po<strong>in</strong>t of Service<br />
PPO: Preferred <strong>Provider</strong> Organization<br />
PRA: Predictive Resource Assessment<br />
PRO: Peer Review Organization<br />
QI: Quality Improvement<br />
QIO: Quality Improvement Organization<br />
QIC: Quality Improvement Committee<br />
RUG: Resource Utilization Group<br />
SCP: Participat<strong>in</strong>g Specialty Care <strong>Provider</strong><br />
SNF: Participat<strong>in</strong>g Skilled Nurs<strong>in</strong>g Facility<br />
SPD: Summary <strong>Plan</strong> Document<br />
TPA: Third Party Adm<strong>in</strong>istrator<br />
TSI: Transition Systems Inc.<br />
UCR: Usual, Customary, Reasonable Fee<br />
UM: Utilization Management<br />
USPHTF: United States Preventive <strong>Health</strong> Task Force<br />
1/1/2012 Participat<strong>in</strong>g <strong>Provider</strong> <strong>Guide</strong> – Glossary and Acronyms<br />
128