ECHOCARDIOGRAPHY IN CARDIAC SURGERY - TSDA
ECHOCARDIOGRAPHY IN CARDIAC SURGERY - TSDA
ECHOCARDIOGRAPHY IN CARDIAC SURGERY - TSDA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 943 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
CHAPTER<br />
49<br />
<strong>ECHOCARDIOGRAPHY</strong><br />
<strong>IN</strong> <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
Samia Mora, Katherine C. Wu<br />
PR<strong>IN</strong>CIPLES OF <strong>ECHOCARDIOGRAPHY</strong><br />
Since 1976, echocardiography (echo) has been used to<br />
evaluate cardiac structure and function. Echo uses sound<br />
in the high-frequency range (2 to 10 MHz). Frequency<br />
ranges between 2 and 5 MHz are typically used for imaging<br />
adults, while frequencies of 7.5 to 10 MHz are used for<br />
children and specialized adult applications. The transducer<br />
contains a piezoelectric crystal that converts electrical to<br />
sound energy, producing sound waves that are transmitted<br />
in the form of a beam. A complete transthoracic echocardiogram<br />
(TTE) consists of a group of interrelated applications<br />
including two-dimensional (2D) anatomic imaging,<br />
M-mode, and three Doppler techniques: pulsed-wave<br />
(PW), continuous-wave (CW), and color-flow (CF) imaging.<br />
1–7 In addition, the quantification of cardiac chamber<br />
dimensions, areas, and volumes is an important aspect of a<br />
complete examination. Using a combination of these ultrasound<br />
techniques, one can assess the anatomy and function<br />
of the cardiac valves, myocardium, and pericardium.<br />
TWO-DIMENSIONAL <strong>ECHOCARDIOGRAPHY</strong><br />
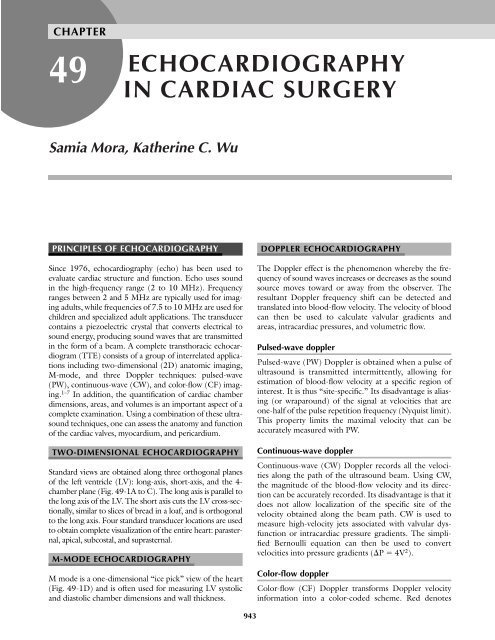
Standard views are obtained along three orthogonal planes<br />
of the left ventricle (LV): long-axis, short-axis, and the 4-<br />
chamber plane (Fig. 49-1A to C). The long axis is parallel to<br />
the long axis of the LV. The short axis cuts the LV cross-sectionally,<br />
similar to slices of bread in a loaf, and is orthogonal<br />
to the long axis. Four standard transducer locations are used<br />
to obtain complete visualization of the entire heart: parasternal,<br />
apical, subcostal, and suprasternal.<br />
M-MODE <strong>ECHOCARDIOGRAPHY</strong><br />
M mode is a one-dimensional “ice pick” view of the heart<br />
(Fig. 49-1D) and is often used for measuring LV systolic<br />
and diastolic chamber dimensions and wall thickness.<br />
DOPPLER <strong>ECHOCARDIOGRAPHY</strong><br />
The Doppler effect is the phenomenon whereby the frequency<br />
of sound waves increases or decreases as the sound<br />
source moves toward or away from the observer. The<br />
resultant Doppler frequency shift can be detected and<br />
translated into blood-flow velocity. The velocity of blood<br />
can then be used to calculate valvular gradients and<br />
areas, intracardiac pressures, and volumetric flow.<br />
Pulsed-wave doppler<br />
Pulsed-wave (PW) Doppler is obtained when a pulse of<br />
ultrasound is transmitted intermittently, allowing for<br />
estimation of blood-flow velocity at a specific region of<br />
interest. It is thus “site-specific.” Its disadvantage is aliasing<br />
(or wraparound) of the signal at velocities that are<br />
one-half of the pulse repetition frequency (Nyquist limit).<br />
This property limits the maximal velocity that can be<br />
accurately measured with PW.<br />
Continuous-wave doppler<br />
Continuous-wave (CW) Doppler records all the velocities<br />
along the path of the ultrasound beam. Using CW,<br />
the magnitude of the blood-flow velocity and its direction<br />
can be accurately recorded. Its disadvantage is that it<br />
does not allow localization of the specific site of the<br />
velocity obtained along the beam path. CW is used to<br />
measure high-velocity jets associated with valvular dysfunction<br />
or intracardiac pressure gradients. The simplified<br />
Bernoulli equation can then be used to convert<br />
velocities into pressure gradients (P 4V 2 ).<br />
Color-flow doppler<br />
Color-flow (CF) Doppler transforms Doppler velocity<br />
information into a color-coded scheme. Red denotes<br />
943
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 944 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
944 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
A<br />
B<br />
C<br />
D<br />
Figure 49-1 Standard 2D TTE (A to C) and M-mode (panel D) views in a normal individual.<br />
A. Parasternal long-axis view of the right ventricle (RV), interventricular septum, left<br />
ventricle (LV) cavity and posterior wall, and both mitral and aortic valves. Since the RV is<br />
the most anterior structure, it will be located closest to the transducer beam and is seen at<br />
the top of the image display, while the LV and LA (both posterior structures) are farther<br />
away from the transducer and are seen at the bottom of the image. B. Parasternal shortaxis<br />
view of the ventricles at the papillary muscle midventricular level obtained by rotating<br />
the transducer 90 degrees. C. Apical four-chamber view, important for evaluation of ventricular<br />
function, apical thrombus, mitral and tricuspid valve function. D. M-mode view<br />
through the RV and mitral leaflets. This view is useful for detecting RV diastolic collapse in<br />
tamponade.<br />
flow toward the transducer, while blue represents flow<br />
away from the transducer. The relative velocity of blood<br />
flow is also depicted, with brighter shades of blue or red<br />
representing higher velocities. Turbulent flow is seen as<br />
multicolored jets (e.g., due to valvular disease or intracardiac<br />
shunts).<br />
TRANSESOPHAGEAL <strong>ECHOCARDIOGRAPHY</strong><br />
TEE was first introduced clinically in the United States<br />
in the 1980s. By placing an echocardiographic probe in<br />
the esophagus, which is in close proximity to cardiac<br />
structures, TEE obtains significantly enhanced images
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 945 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 945<br />
with excellent resolution. The development of transducer<br />
crystals that rotate from 0 to 180 degrees also allows for<br />
examination of each cardiac structure from different<br />
planes and angles. Acquisition of images is from two basic<br />
locations: midesophageal (30 to 35 cm from the incisors)<br />
and midgastric (40 to 45 cm from the incisors).<br />
Indications<br />
TEE is useful for the evaluation of patients with limiting<br />
body habitus, such as obesity or emphysema, who are not<br />
optimally imaged by the transthoracic approach. In addition,<br />
certain structures that are not well visualized by<br />
transtracheal echo (TTE) [such as the left atrial (LA)<br />
appendage, thoracic aorta, and prosthetic valves] can be<br />
assessed by the transesophageal approach. A third common<br />
indication is to guide intraoperative management during<br />
cardiac surgery. Class I indications for perioperative TEE<br />
(conditions for which there is evidence and/or general<br />
agreement that TEE is useful and effective) are listed in<br />
Table 49-1. 8 There are other situations in which TEE may<br />
also be useful but is not required (i.e., class II indications:<br />
conditions in which there is a divergence of opinion about<br />
the usefulness/efficacy of a procedure but in which the<br />
weight of opinion is in favor of usefulness/efficacy). These<br />
include ongoing surgical procedures in patients at increased<br />
risk of myocardial ischemia or hemodynamic instability,<br />
during minimally invasive surgery or the Cox-Maze procedure<br />
cardiac tumor resection or aneurysm repair, intracardiac<br />
thrombectomy or pulmonary embolectomy, for<br />
detection of intracardiac air or aortic atheromatous disease,<br />
and for selecting anastomotic sites during heart/lung<br />
transplantation. 8 Antibiotic prophylaxis for infective endocarditis<br />
is usually unnecessary but is optional in the high-risk<br />
patient (e.g., complex congenital heart disease, prosthetic<br />
valve, poor dentition, or prior history of endocarditis). 9<br />
Contraindications and complications<br />
Relative contraindications for TEE include significant<br />
esophageal pathology (e.g., strictures, varices), history<br />
Table 49-1<br />
Class I indications for perioperative<br />
transesophageal echocardiography<br />
Acute and life-threatening hemodynamic instability<br />
Valve repair or complex valve replacements<br />
Hypertrophic obstructive cardiomyopathy<br />
Aortic dissection with possible aortic valve involvement<br />
Endocarditis (perivalvular involvement)<br />
Congenital heart surgery<br />
Pericardial windows (posterior or loculated effusions)<br />
Placement of intracardiac devices<br />
Source: Data modified from Cheitlin MD, Armstrong WF, Aurigemma GP,<br />
et al. ACC/AHA/ASE 2003 guideline update for the clinical application of<br />
echocardiography: summary article: a report of the American College of<br />
Cardiology/American Heart Association Task Force on Practice Guidelines<br />
(ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical<br />
Application of Echocardiography). Circulation 2003;108:1146–1162.<br />
of radiation therapy to the mediastinum, and recent<br />
esophageal or gastric surgery. Serious complications of TEE<br />
are uncommon ( 1 percent) but may include aspiration<br />
and other problems related to oversedation, mucosal<br />
trauma, laryngospasm, esophageal or pharyngeal laceration<br />
or perforation, methemoglobinemia, and rarely death.<br />
TEE probe passage is “blind” and is done without direct<br />
visualization. The more severe complications of esophageal<br />
or pharyngeal trauma are signaled by patient complaints of<br />
severe pain and inability to swallow, which usually occur<br />
after the procedure has ended and sedation has worn off.<br />
Esophageal perforation during intraoperative TEE can go<br />
undetected for a period of time because of the anesthetized<br />
state of the patient and the lack of patient feedback regarding<br />
pain during probe passage.<br />
ASSESSMENT OF VENTRICULAR FUNCTION<br />
Routinely, a qualitative “eyeball” estimate of global LV<br />
systolic function is obtained visually by examining LV wall<br />
thickening and motion. In addition, quantitative measures<br />
of LV systolic function can also be obtained. LV segmental<br />
wall function can be analyzed using a semiquantitative<br />
grading scale (wall motion score).<br />
LEFT VENTRICULAR EJECTION FRACTION<br />
Ejection fraction (EF) is often reported qualitatively as<br />
increased (hyperdynamic), normal, mildly, moderately, or<br />
severely reduced. 8 In addition, the reader often assigns an<br />
estimated value to the qualitative assessment. Normal LV<br />
EF is 61 10 percent. 10<br />
Visual estimation of EF by experienced readers is generally<br />
reliable but is limited by reader variability and<br />
depends on optimal echocardiographic delineation of the<br />
endocardium.<br />
EF can also be quantified from the equation below<br />
after determining end-diastolic volume (EDV) and endsystolic<br />
volume (ESV):<br />
EF SV/EDV (EDV – ESV)/EDV<br />
Where SV stroke volume, EDV end-diastolic volume,<br />
and ESV end-systolic volume.<br />
Volumes can be obtained by the modified Simpson’s<br />
method, which divides the LV cavity into a series of<br />
stacked cylinders of equal height that are summed to<br />
estimate the entire ventricular volume at end-diastole<br />
and end-systole. Further details of the technique can be<br />
found in several of the references. 1,2,11<br />
LEFT VENTRICULAR FRACTIONAL<br />
SHORTEN<strong>IN</strong>G (PERCENT FRACTIONAL<br />
SHORTEN<strong>IN</strong>G)<br />
Percent FS is another method for estimating LV systolic<br />
function and reflects a percent change in LV
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 946 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
946 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
dimension with systolic contraction. It is calculated<br />
from LV end-diastolic and end-systolic dimensions measured<br />
by M mode. For ventricles that are roughly symmetrical<br />
without regional wall motion abnormalities, EF<br />
is approximately 2 (percent FS).<br />
Percent FS (EDD – ESD) / EDD 100<br />
Where EDD end-diastolic dimension and ESD endsystolic<br />
dimension.<br />
LEFT VENTRICULAR REGIONAL<br />
WALL MOTION<br />
For the assessment of LV regional wall motion, the LV is<br />
divided into 16 segments (Fig. 49-2), each of which is<br />
given a score from 1 to 5 (1, normal or hyperkinetic; 2,<br />
hypokinetic; 3, akinetic; 4, dyskinetic; 5, aneurysmal or<br />
diastolically deformed). This grading system differs from<br />
the 1-to-5 grading system of TEE often used by cardiac<br />
anesthesiologists 12 [1, normal ( 30 percent thickening);<br />
2, mildly hypokinetic (10 to 30 percent thickening); 3,<br />
severely hypokinetic ( 10 percent thickening); 4, akinetic<br />
(no thickening); 5, dyskinetic (paradoxical systolic<br />
motion)]. The wall motion score index is calculated as<br />
the sum of segmental wall motion scores divided by the<br />
number of segments seen. A score of 1 is normal and<br />
higher wall motion scores indicate more extensive ventricular<br />
dysfunction. However, this grading system is<br />
more useful for research databases than for clinical use.<br />
LEFT VENTRICULAR FILL<strong>IN</strong>G<br />
LV preload is the LV volume at end-diastole. Normal LV<br />
end-diastolic size is 3.5 to 5.7 cm in the parasternal longaxis<br />
view. The size of the ventricles and atria may be used<br />
for the qualitative evaluation of filling pressures and<br />
assessment of hyper- or hypovolemia, particularly intraoperatively<br />
with TEE. 13 Small LA size and near cavity<br />
obliteration of the LV can indicate hypovolemia. 14<br />
Conversely, ventricular and atrial enlargement may indicate<br />
hypervolemia. Doming of the interatrial septum<br />
toward the right suggests elevated LA pressure and<br />
increased LV preload (the septum bulges toward the side<br />
with lower pressure). One limitation to using TEE for<br />
indirect measurement of volume status is that the LV<br />
may be foreshortened; it is therefore recommended that<br />
the LV be imaged from several different planes to get a<br />
more accurate estimate of LV volume. 14<br />
LEFT VENTRICULAR DIASTOLIC FUNCTION<br />
Doppler echo is the most common diagnostic tool for<br />
assessing diastolic function. Indices of transmitral and<br />
pulmonary venous Doppler flows are commonly used to<br />
identify patterns of diastolic dysfunction. 11<br />
Figure 49-2 Sixteen-segment model of the left ventricle.<br />
According to guidelines of the American Society of<br />
Echocardiography and the Society of Cardiac Anesthesia,<br />
the left ventricle is divided into 16 segments (6 basal, 6 mid<br />
ventricular, and four apical segments) for evaluation of wall<br />
motion and calculation of the wall motion score. (From<br />
Shanewise et al. 12 With permission.)<br />
Mitral valve inflow<br />
When sinus rhythm is present, PW Doppler at the level of the<br />
mitral valve (MV) leaflets records two velocities separated by<br />
a period of diastasis (no flow), as shown in Fig. 49-3. After<br />
the MV opens, early rapid (E wave) diastolic filling of the<br />
LV occurs, followed by a period of diastasis, after which late<br />
filling occurs due to atrial contraction (A wave). Normally,<br />
in individuals less than 60 years old, the peak E:A wave<br />
velocity ratio is greater than 1. When there is impaired<br />
relaxation without elevated filling pressures, the peak E<br />
decreases, hence the E:A ratio becomes less than 1. In contrast,<br />
a “restrictive” filling pattern is seen when both<br />
impaired relaxation and elevated filling pressures are present,<br />
resulting in a smaller contribution of atrial contraction<br />
and an increased E:A ratio ( 1.5 to 2).
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 947 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 947<br />
LA pressure seen after MV opening. The fourth velocity is<br />
the atrial flow reversal velocity (PV a<br />
) that is related to LA<br />
contraction. A pulmonary vein systolic velocity peak less<br />
than the diastolic velocity peak is suggestive of elevated LA<br />
pressures. Restrictive filling indicative of very high filling<br />
pressures is seen when PV S2<br />
is much less than PV D<br />
. When<br />
higher filling pressures are present, both the duration and<br />
peak velocity of PV a<br />
are increased. Another sign of elevated<br />
LA pressure is when the duration of PV a<br />
is longer than the<br />
duration of the mitral inflow A wave (by 0.03 s).<br />
Figure 49-3 Pulsed-wave (PW) Doppler of the mitral valve<br />
inflow. This figure shows a normal pattern of blood flow<br />
through the mitral valve in diastole. The two peaks indicate<br />
early (E wave) and late (A wave) diastolic filling separated<br />
by a brief period of diastasis (no flow). In individuals less<br />
than 65 years old, a normal E:A ratio is 2:1. Deceleration<br />
time is the time interval from peak E velocity to baseline.<br />
Pulmonary vein flow<br />
Four velocities are seen in PW Doppler of the pulmonary<br />
veins (Fig. 49-4). Occurring in early systole, the first systolic<br />
forward flow velocity (PV S1<br />
) is due to the relaxation<br />
of the LA, which promotes pulmonary venous flow into<br />
the LA. In mid- to late systole, a second systolic forward<br />
flow (PV S2<br />
) occurs that is produced by the increase in<br />
pulmonary venous pressure occurring after right ventricular<br />
(RV) systole. In diastole, a third pulmonary vein<br />
velocity is seen (PV D<br />
). This is related to the decrease in<br />
RIGHT VENTRICULAR FUNCTION<br />
AND FILL<strong>IN</strong>G PRESSURES<br />
Qualitative evaluation of RV wall thickening and motion is<br />
done visually, as in the evaluation of LV function, although<br />
it is more difficult to estimate RV function. Normal RV<br />
size is less than two-thirds of LV size (see Fig. 49-1). Septal<br />
wall flattening (resulting in a D-shaped LV in the shortaxis<br />
view) or septal deviation into the LV can be see in both<br />
pressure- and volume-overload conditions of the RV. 12<br />
When tricuspid regurgitation is present, the RV systolic<br />
pressure (RVSP) can be estimated (see also “Pulmonary<br />
Hypertension,” below), although TTE is preferred to<br />
TEE for measuring RVSP because of better alignment<br />
of the transducer beam with the direction of the regurgitant<br />
jet.<br />
Examination of the size and respiratory changes of the<br />
venae cavae and hepatic veins can give helpful clues to<br />
the patient’s volume status and is also used in the evaluation<br />
of pericardial disease. Although TTE is preferred for<br />
examination of respirophasic collapse of the inferior vena<br />
Figure 49-4 Pulsed-wave (PW) Doppler of the pulmonary vein. This figure shows a normal<br />
pattern of blood flow through the pulmonary veins with four velocities seen (PV S1<br />
,<br />
PV S2<br />
, PV D<br />
, PV a<br />
). Duration of peak reverse flow velocity during atrial contraction (PV a<br />
dur)<br />
is also measured. (From Oh et al. 11 With permission.)
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 948 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
948 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
cava, TEE provides better visualization of the superior<br />
vena cava. Dilatation of the superior vena cava (greater<br />
than one-half the aortic dimension in the short-axis<br />
view) is suggestive of hypervolemia. 14<br />
VALVULAR DISEASE<br />
MITRAL VALVE<br />
Mitral valve morphology<br />
Normal MV function depends on the normal function<br />
of all its component parts, including the mitral leaflets,<br />
annulus, chordae tendineae, papillary muscles, and LV.<br />
The rectangular posterior leaflet is composed of three<br />
scallops (P1, P2, P3), while the semicircular anterior<br />
leaflet is divided into thirds for descriptive purposes<br />
(Fig. 49-5). Normal MV area is 4 to 6 cm 2 .<br />
Mitral stenosis<br />
Rheumatic heart disease is the most common cause of<br />
mitral stenotic lesions (Fig. 49-6), with leaflet thickening<br />
and fusion of the commissures (characteristic fish-mouth<br />
valve in the short-axis view and hockey-stick appearance<br />
in the long-axis view).<br />
Two-dimensional (2D) echo is the “gold standard” for<br />
evaluating mitral stenosis (MS) and allows assessment of<br />
the structure and function of the mitral annulus, leaflets,<br />
chordae, papillary muscles, LV size and function, LA size,<br />
and pulmonary hypertension (RVSP). The Wilkins echo<br />
score 15 for rheumatic MS is based on four variables (leaflet<br />
mobility, leaflet thickening, subvalvular thickening, and<br />
calcifications). Each variable receives a score of 1 to 4 and<br />
the individual scores are summed up. A total score equal<br />
to or greater than 8 is associated with better outcomes for<br />
mitral balloon valvuloplasty. For valves with less favorable<br />
scores ( 8), cardiac surgery with valve replacement may<br />
be the preferred treatment modality.<br />
Mitral valve area<br />
Calculation of MV area is usually obtained using the<br />
pressure half-time (PHT) method. PHT is the time (milliseconds)<br />
for the maximal pressure gradient to decrease<br />
by half and is usually equal to the deceleration time multiplied<br />
by 0.29.<br />
MV area (cm 2 ) 220 / PHT (ms)<br />
The PHT method has several important shortcomings.<br />
It is affected by concomitant aortic regurgitation or<br />
decreased LV compliance. 4 The rapid increase in LV diastolic<br />
pressure associated with either of these conditions<br />
may shorten the PHT and underestimate the extent of<br />
stenosis. Other techniques to estimate valve area include<br />
planimetry and the continuity equation. 1,4 The latter<br />
approach is also less reliable in the presence of significant<br />
aortic and mitral regurgitation. Details of this approach<br />
are outlined in the references 1 through 11.<br />
Mitral valve pressure gradients<br />
As the degree of obstruction to blood flow caused by a<br />
stenotic valve increases, the velocity of the blood flow also<br />
increases in order to maintain constant flow (conservation<br />
of mass or flow). Velocities can then be transformed<br />
into pressures with the simplified Bernoulli equation:<br />
ΔP 4V 2<br />
Figure 49-5 Mitral valve structure. The mitral valve consists<br />
of two leaflets, the anterior and posterior leaflets,<br />
which are separated at the annulus by the posteromedial<br />
and anterolateral commissures. The posterior leaflet is rectangular<br />
and composed of three scallops (P1, P2, P3). The<br />
anterior leaflet is semicircular and is divided into three segments<br />
for descriptive purposes (A1, A2, A3). (From<br />
Shanewise et al. 12 With permission.)<br />
Where P MV pressure gradient (mmHg) and V <br />
velocity of blood flow across the MV (ms).<br />
Severity of mitral stenosis<br />
The mean MV pressure gradient and MV area are used<br />
to estimate the severity of mitral stenosis and the need<br />
for intervention (Table 49-2).<br />
Mitral regurgitation<br />
There are three basic mechanisms of mitral regurgitation<br />
(MR): primary abnormalities of the mitral leaflets, commissures,<br />
or annulus; malfunctioning of the subvalvular
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 949 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 949<br />
A<br />
B<br />
Figure 49-6 Rheumatic mitral stenosis. A. Transesophageal transgastric<br />
long-axis view of the left ventricle, the anterolateral papillary muscle<br />
(ALPM), the posteromedial papillary muscle (PMPM), mitral valve (MV)<br />
leaflets, and left atrium (LA). Note the thickened and partially calcified<br />
subvalvular and valvular structures (short arrow). The patient had severe<br />
three-vessel coronary artery disease in addition to rheumatic aortic stenosis<br />
and atrial fibrillation and underwent successful mitral and aortic valve<br />
replacements and coronary artery bypass grafting. B. Continuous-wave<br />
(CW) Doppler of the mitral valve intraoperatively. MR mitral regurgitation;<br />
MS mitral stenosis.<br />
structures (chordae tendineae and papillary muscles); and<br />
alterations in LV and LA dimensions and function.<br />
The most common cause of isolated severe MR is<br />
myxomatous degeneration (Fig. 49-7). The valve itself<br />
can also be deformed from rheumatic fever, mitral annular<br />
calcification, infective endocarditis, and congenital<br />
lesions (cleft MV). Other less common causes of leaflet<br />
abnormalities include endomyocardial fibrosis, carcinoid<br />
Table 49-2<br />
Severity of mitral stenosis<br />
Mitral valve area Mean gradient a<br />
Severity (cm 2 ) (mmHg)<br />
None 4–6 —<br />
Mild 1.6–2.0 5<br />
Moderate 1.1–1.5 5–10<br />
Severe 1 10<br />
a Assumes normal cardiac output.<br />
Source: ACC/AHA Guidelines for the Management of Patients with<br />
Valvular Heart Disease. 9 With permission.<br />
disease, drugs (e.g., fenfluramine hydrochloride and<br />
phentermine, or Fen-Phen), radiation therapy, trauma,<br />
and collagen vascular disease.<br />
Abnormalities in the subvalvular structures include<br />
dysfunctional and/or ruptured chordae tendineae and<br />
papillary muscles. Ruptured chordae tendineae account<br />
for a large proportion of MR lesions. Etiologies include<br />
idiopathic causes, MV prolapse, infective endocarditis,<br />
and thoracic trauma. Papillary muscle dysfunction (with<br />
or without frank rupture) is most often seen in the setting<br />
of myocardial ischemia or infarction. The posteromedial<br />
head of the papillary muscle is most vulnerable to<br />
ischemia because of its end-artery vascular supply. Other<br />
causes of dysfunction include dilated cardiomyopathy,<br />
myocarditis, hypertension, and chest trauma.<br />
Global or regional LV enlargement may dilate the<br />
mitral annulus and change the position and axis of contraction<br />
of the papillary muscles, leading to dysfunction.<br />
Progressive LA and LV enlargement associated with<br />
chronic MR further exacerbate the extent of MR because<br />
of continued changes in chamber geometry.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 950 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
950 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
A<br />
B<br />
Figure 49-7 Myxomatous mitral valve prolapse and mitral<br />
regurgitation. A. Transthoracic parasternal long-axis view<br />
of the mitral valve with a greater than 2-mm prolapse of the<br />
posterior leaflet (MVP) beyond the plane of the annulus.<br />
B. Apical four-chamber view shows biatrial enlargement.<br />
C. Color-flow Doppler shows severe mitral regurgitation<br />
(MR) with an eccentric jet that is “wall hugging” and anteriorly<br />
directed (opposite the side of leaflet prolapse).<br />
degree preoperatively, particularly for ischemic MR,<br />
because of different hemodynamic and ischemic conditions<br />
(e.g., lower blood pressure or relief of ischemia will<br />
reduce the amount of regurgitation). 17<br />
Severity of mitral regurgitation<br />
Echo findings in severe MR 4,16 include:<br />
● Large regurgitant jet: 40 percent of LA area.<br />
● Wide vena contracta (the narrowest part of the regurgitant<br />
color jet at its origin): 7 mm.<br />
● Eccentric wall-impinging regurgitant jet (Fig. 49-7B).<br />
● Dilated LV: end-systolic dimension 45 mm or enddiastolic<br />
dimension 70 mm.<br />
● LV EF 55 to 60 percent.<br />
● Dilated LA ( 5.5 cm), although the LA may not be<br />
dilated in acute MR.<br />
● Pulmonary hypertension: resting RVSP 50 mmHg.<br />
● Restrictive mitral filling pattern: high peak early transmitral<br />
velocity (E wave) 1.5 ms.<br />
● Pulmonary vein systolic flow reversal: A normal pulmonary<br />
vein Doppler pattern has a systolic (S) wave<br />
larger than the diastolic (D) wave. As the MR progresses,<br />
the S wave decreases until it may become<br />
reversed. While a reduced S wave is a nonspecific finding,<br />
18 the presence of a reversed S wave has high specificity<br />
for significant MR. The absence of a reversed S<br />
wave does not exclude significant MR.<br />
● Effective orifice area (ERO) 0.4 cm 2 .<br />
Table 49-3 summarizes the important echo features of<br />
MV stenosis and regurgitation.<br />
Mitral valve prolapse<br />
Mitral valve prolapse (MVP) is the most common cause<br />
of MR in patients undergoing cardiac surgery in the<br />
United States. 19 MVP is the systolic billowing or displacement<br />
of at least 2 mm of either mitral leaflet into<br />
Two-dimensional echocardiography<br />
Unlike the case in MS, where echo is the accepted gold<br />
standard for diagnosis, there is no gold standard for the<br />
assessment of MR; therefore multiple parameters are<br />
used in estimating the severity of MR. 16 The purpose of<br />
echo in MR is to determine the etiology, mechanism,<br />
and severity of regurgitation; determine the need for<br />
surgery and the type of surgery that is necessary; and<br />
evaluate other valves, RV and LV function, and the presence<br />
of pulmonary hypertension. The most important<br />
aspect is to determine the hemodynamic significance of<br />
the regurgitation based on LV size (particularly end-systolic<br />
dimension), LV systolic function (EF), and the<br />
presence and degree of LA enlargement and pulmonary<br />
hypertension (RVSP). Regurgitant jet size and area may<br />
contribute to the assessment of MR but often correlate<br />
poorly with MR severity. 16 The degree of MR intraoperatively<br />
may appear less or more severe compared to the<br />
Table 49-3<br />
Morphology<br />
Stenosis<br />
Regurgitation<br />
Echocardiographic assessment of the<br />
mitral valve<br />
Mitral annulus, leaflets, chordae, papillary<br />
muscles, LV size and function,<br />
LA size, pulmonary hypertension (RVSP)<br />
Often rheumatic<br />
Echo score: leaflet mobility, thickening,<br />
subvalvular thickening, calcifications,<br />
8 favors valvuloplasty<br />
Severe MS: area 1 cm 2 or mean gradient<br />
10 mmHg<br />
Regurgitant jet size does not correlate well<br />
with severity<br />
Severe MR: dilated LV (ESD 45 mm), ↓ LV<br />
systolic function (EF 55–60%), dilated LA,<br />
pulmonary hypertension (RVSP 50)<br />
LV left ventricle; RVSP right ventricular systolic pressure;<br />
MS mitral stenosis; MR mitral regurgitation; ESD endsystolic<br />
dimension; LA left atrium; EF ejection fraction.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 951 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 951<br />
the LA beyond the plane of the mitral annulus in the<br />
parasternal or apical long-axis views (see Fig. 49-7).<br />
Recent criteria for echo diagnosis of MVP 20 have<br />
become more stringent, leading to increased specificity<br />
of the criteria for MVP while at the same time preserving<br />
sensitivity for the detection of MVP complications.<br />
Classic MVP is defined as equal to or greater than 5 mm<br />
of leaflet thickening (myxomatous changes) of the prolapsing<br />
leaflet, while nonclassic prolapse is leaflet thickening<br />
less than 5 mm. Compared to nonclassic MVP,<br />
classic MVP has a worse prognosis, with most complications<br />
of MVP (significant MR and congestive heart failure,<br />
MV surgery, infectious endocarditis) arising in<br />
patients with classic MVP. 19 Asymmetrical prolapse of<br />
the leaflets is associated with progression to more significant<br />
disease (flail leaflet and severe MR).<br />
Determining which segment of the mitral leaflet tissue<br />
is prolapsing is essential for proper MV repair. MR associated<br />
with MVP often has an eccentric jet directed<br />
opposite to the prolapsing leaflet (e.g., anteriorly<br />
directed jet if posterior leaflet prolapse is present). In<br />
contrast, in MR associated with rheumatic mitral stenosis,<br />
the regurgitant jet is directed toward the affected<br />
leaflet due to restricted leaflet motion (e.g., anteriorly<br />
directed jet if the anterior leaflet is calcified). MR associated<br />
with MVP may be due to flail leaflet or chordal rupture<br />
resulting from myxomatous involvement of the<br />
chordae or leaflet. Chordal rupture is diagnosed when<br />
the chords are seen as mobile echodensities attached to a<br />
flail or partially flail leaflet (Fig. 49-8). 21 These may be<br />
confused with or may be difficult to distinguish from<br />
vegetations of infective endocarditis. Mitral annulus calcification<br />
(MAC) may also be seen in patients who have<br />
MVP.<br />
Figure 49-8 Ruptured chord attached to a flail segment of<br />
the posterior mitral leaflet due to myxomatous disease.<br />
Intraoperative transesophageal echocardiogram showing<br />
the ruptured chord as an echodense linear filament<br />
attached to the flail leaflet, prolapsing into the left atrium<br />
during systole.<br />
Figure 49-9 Flail mitral leaflet with severe mitral regurgitation.<br />
Intraoperative transesophageal echocardiogram with<br />
color-flow Doppler consistent with severe mitral regurgitation.<br />
This patient underwent successful mitral valve repair<br />
with posterior leaflet quadrangular resection and an annuloplasty<br />
band.<br />
Flail leaflet<br />
Flail leaflet encompasses a spectrum of disease severity<br />
from partially to completely flail leaflets, resulting in<br />
excessive motion of the mitral leaflets and various degrees<br />
of MR (Fig. 49-9). Flail mitral leaflet is diagnosed when<br />
the leaflet tip is “upturned” toward the LA during MV<br />
closure (due to loss of coaptation). Most commonly, it is<br />
caused by MVP or endocarditis resulting in chordal rupture,<br />
but it may also be caused by ischemia or infarction<br />
of the papillary muscle (usually affecting the posteromedial<br />
papillary muscle). A partially flail leaflet (due to chordal<br />
rupture) is usually associated with moderate to severe MR,<br />
while a completely flail mitral leaflet is almost always associated<br />
with severe MR necessitating surgery. 21<br />
Ruptured papillary muscle<br />
Dysfunction of the papillary muscle results in severe MR<br />
and is most often due to acute myocardial infarction.<br />
Papillary muscle dysfunction should be differentiated<br />
from acute chordal rupture. Papillary muscle rupture is<br />
diagnosed in the appropriate clinical context when a triangular<br />
mass (the head of the papillary muscle), seen<br />
attached to the flail leaflet, prolapses into the LA during<br />
systole, accompanied by severe MR. 17<br />
Leaflet perforation<br />
This is most commonly caused by valvular endocarditis,<br />
while less common etiologies include congenital (cleft<br />
MV) or iatrogenic causes. With leaflet perforation, the<br />
regurgitant jet is often eccentric and originates at the site<br />
of perforation.<br />
Mitral valve repair<br />
TEE is essential in determining the suitability of a valve<br />
for repair. It can assess the mechanism and severity of
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 952 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
952 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
Figure 49-10 Posterior leaflet prolapse and dilated mitral annulus. Note the<br />
anteriorly directed eccentric jet of mitral regurgitation seen on transesophageal<br />
echocardiography. Following the repair (posterior leaflet quadrangular resection<br />
and annuloplasty ring), the patient had good ventricular function and no residual<br />
mitral regurgitation.<br />
MR, identify the affected leaflets, determine the presence<br />
of coexisting valvular lesions, and estimate RV and LV<br />
function. The prognosis of MV repair differs based on<br />
the mechanism of MR (organic/primary vs. functional/secondary)<br />
and is strongly influenced by the preoperative<br />
EF. The most common indication for MV<br />
repair is myxomatous disease. Determining which leaflet<br />
or segment is involved is important in deciding on the<br />
suitability of the repair, the likelihood of successful repair<br />
(better with posterior leaflet prolapse), and the method<br />
of repair. This is done by analyzing the motion of the<br />
leaflets and the direction of the regurgitant jet.<br />
TEE is also helpful intraoperatively to assess the success<br />
of the repair. Immediately postrepair (Fig. 49-10),<br />
the competency of the valve can be assessed for residual<br />
MR (1, mild; 2, moderate; 3, moderate to severe;<br />
4, severe). Phenylephrine and volume may be administered<br />
in order to assess the effect of increased afterload<br />
and preload on the degree of residual MR. If there is MR<br />
postrepair equal to or greater than 2, further surgery is<br />
indicated. Repeat imaging is also done after the patient is<br />
off cardiopulmonary bypass. Other findings that may be<br />
detected on TEE include residual mitral stenosis, global<br />
or regional LV systolic dysfunction, suture dehiscence or<br />
leaflet perforation, and MV systolic anterior motion<br />
(SAM) with outflow obstruction. Limitations to intraoperative<br />
TEE include the effect of changing hemodynamics,<br />
which may significantly affect the appearance and<br />
severity of valvular lesions, since the evaluation depends<br />
on preload and afterload conditions as well as ventricular<br />
function. Hence, it is important that loading conditions<br />
be similar in comparing the severity of MR.<br />
AORTIC VALVE<br />
Aortic valve morphology<br />
Normally, the aortic valve (AV) is composed of three semilunar<br />
leaflets (cusps) that open and close passively due to<br />
pressure differences between the LV and the aorta. Small<br />
strands may be seen on the cusps (Lambl’s excrescences),<br />
particularly on TEE, and represent a normal variant.<br />
Bicuspid and rarely unicuspid or quadricuspid valves may<br />
be seen on echo (Fig. 49-11). The normal valve area is<br />
3 to 4 cm 2 with a 2-cm leaflet separation during systole.<br />
A bicuspid AV is the most common congenital heart<br />
defect and occurs in about 1 to 2 percent of the U.S. population.<br />
The morphologic features of a bicuspid AV are<br />
somewhat variable. In some patients, there are two equalsized<br />
cusps with a single central commissure. In many others,<br />
the cusps may be unequal in size with an eccentric<br />
commissure, with the larger of the two cusps containing<br />
a raphe. 1,22 In the parasternal long-axis views, bicuspid<br />
valves are characterized by systolic doming. In the shortaxis<br />
views, the hallmark is an elliptical “football”-shaped<br />
systolic orifice. The valve leaflets themselves may be thickened<br />
and fibrotic, particularly with increasing patient age.<br />
A bicuspid valve may be functionally normal with no significant<br />
stenosis or regurgitation, particularly in adolescents<br />
and young adults, among whom up to one-third have no<br />
significant valvular dysfunction. 23 However, over time,<br />
progressive “wear and tear” with resulting fibrosis and<br />
valve calcification leads to functional abnormalities. By the<br />
age of 60 years, over 50 percent of bicuspid valves are significantly<br />
stenotic. Valve regurgitation is frequently present
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 953 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 953<br />
Figure 49-11 Bicuspid, tricuspid, and quadricuspid aortic valves. The normal<br />
aortic valve is trileaflet (central panel). Bicuspid valve is the most common congenital<br />
anomaly of the aortic valve (left panel), with quadricuspid (right panel)<br />
aortic valves being much less common.<br />
as well and may be the predominant functional abnormality<br />
in younger patients. Etiology of the regurgitation may<br />
be retraction and fibrosis of the commissures or leaflets,<br />
cusp prolapse, dilatation of the aortic root or valve annulus,<br />
or damage from infective endocarditis.<br />
It is important to recognize that bicuspid AVs are<br />
often associated with abnormalities of the aorta.<br />
Concomitant aortic coarctation occurs in a minority.<br />
Aortic dissection is another known association, with 5 to<br />
9 percent of patients with dissecting aortic aneurysms<br />
having bicuspid valves. Aortic root dilatation may be due<br />
to a common developmental defect that affects both the<br />
aorta and the valve. 24 Poststenotic dilatation of the<br />
ascending aorta can also occur.<br />
Aortic stenosis<br />
Rheumatic aortic stenosis (AS) (Fig. 49-12A) is usually<br />
associated with MV disease. Calcium deposits are present<br />
on both sides of the aortic cusps, resulting in commissural<br />
fusion and aortic regurgitation. Degenerative calcific disease<br />
is the most common cause of AS in the United States.<br />
It is often associated with MAC and coronary artery disease.<br />
Nodular calcification is often present on the aortic<br />
aspect of the valve along the bases of the cusps and may<br />
protrude into the sinuses of Valsalva (Fig. 49-12B and C).<br />
In contrast to rheumatic AS, there is no commissural fusion<br />
in degenerative AS, hence aortic regurgitation is rare.<br />
Two-dimensional echocardiography<br />
A thorough echo evaluation includes assessing the thickness<br />
and calcification of the leaflets, their mobility, looking<br />
for the etiology of stenosis (e.g., bicuspid, rheumatic,<br />
degenerative calcific) and its extent, the presence of<br />
other valvular lesions, and assessing LV size and function.<br />
TTE is often superior to TEE in assessing the severity<br />
of AS because obtaining maximal velocity jets (i.e.,<br />
absolutely parallel to flow) is often difficult with TEE.<br />
Aortic valve area<br />
In aortic stenotic lesions, the AV area decreases by approximately<br />
0.1 cm 2 per year, although large variations from<br />
patient to patient exist. 25 The AV area is usually determined<br />
using the continuity equation. Direct planimetry (visualization<br />
of the orifice area) is less reliable for patients with heavily<br />
calcified valves (due to shadowing of the valve) and for<br />
critical (“pinhole”) stenoses. 22 The continuity equation is<br />
based on the principle of conservation of flow (or mass),<br />
whereby flow before the valve must equal flow across the<br />
valve. Since the area of the LV outflow tract (LVOT) can be<br />
directly measured, as can velocities in the LVOT and across<br />
the valve, the AV area can then be calculated:<br />
A 1<br />
V 1<br />
A 2<br />
V 2<br />
Where A area or r 2 ; V velocity; A 1<br />
V 1<br />
flow proximal<br />
to the valve (LVOT); A 2<br />
V 2 <br />
flow across the valve.<br />
The major limitation to the continuity equation is<br />
that small errors in the LVOT diameter become magnified<br />
in estimating the AV area (since the radius is squared<br />
in the equation). As a general rule, one may assume that<br />
the LVOT diameter is 2 cm (r 1<br />
1 cm) with generally<br />
good estimates of the AV area. Another limitation is in<br />
obtaining the maximal aortic jet velocity, which requires<br />
that the echocardiographic Doppler beam be exactly parallel<br />
to the direction of blood flow.<br />
Aortic valve pressure gradients<br />
Like pressure gradients obtained for mitral stenosis, the<br />
simplified Bernoulli equation is used for estimating AV<br />
pressure gradients:<br />
P 4V 2<br />
Where P AV pressure gradient (mmHg) and V <br />
velocity of blood flow across the AV (ms).
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 954 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
954 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
A<br />
B<br />
C<br />
D<br />
Figure 49-12 Rheumatic and calcific aortic stenosis. A. Rheumatic aortic stenosis with<br />
calcium deposits in the commissures resulting in commissural fusion. B and D. Short and<br />
long-axis views: Calcific aortic stenosis, with calcium deposits on the aortic aspect of the<br />
valve on the bases of the cusps and no commissural fusion. C. Continuous-wave (CW)<br />
Doppler of the aortic valve (shown in B and C) is consistent with severe aortic stenosis<br />
(aortic velocity 4 ms, mean gradient 50 mmHg). RA right atrium; LA left atrium;<br />
AV aortic valve; LAA left atrial appendage; IAS interatrial septum; Ao aorta;<br />
PG peak gradient; MG mean gradient.<br />
AV pressure gradients may be significantly underestimated<br />
because of inadequate envelopes (because the<br />
Doppler beam is not parallel to the blood flow) or an<br />
inadequate number of measurements from different<br />
locations. Maximal velocities may be present or obtainable<br />
from only certain locations in an individual patient.<br />
Hence complete assessment from all locations is needed.<br />
In addition, the velocity of flow is highly dependent on<br />
overall LV function. Pressure gradients may significantly<br />
underestimate the severity of AS in the presence of severe<br />
LV dysfunction (“low-gradient AS”). The opposite is<br />
also true, whereby increased flow velocity across the<br />
valve is seen in situations of increased cardiac output<br />
(i.e., anemia, aortic regurgitation, hyperthyroidism) and<br />
may not reflect true aortic stenosis. In such situations,<br />
valve area calculations may be more accurate, and correlation<br />
with valve morphology and visual assessment of<br />
leaflet mobility is important.<br />
Severity of aortic stenosis<br />
The mean AV pressure gradient and the AV area are used<br />
to estimate severity of AS and the need for surgical intervention<br />
(Table 49-4). If there is a significant discrepancy<br />
between the pre- and intraoperative grading of the severity<br />
of AS, the following should be considered:<br />
1. Change in hemodynamic conditions: changes in<br />
heart rate or rhythm, contractility, and hemodynamics<br />
influence the gradients across the AV. The AV area<br />
is usually less affected by loading conditions.<br />
2. Measurement variability in data recording: measurement<br />
errors in the LVOT diameter greatly influence<br />
the AV area, since the LVOT radius is squared in the<br />
continuity equation.<br />
Table 49-4<br />
Severity of aortic stenosis<br />
Velocity Area Mean gradient a<br />
Severity (ms) (cm 2 ) (mmHg)<br />
None 1 3–4 —<br />
Mild 2.5–2.9 1.5 25<br />
Moderate 3–4 1–1.5 25–50<br />
Severe 4 1 50<br />
a Assumes normal cardiac output.<br />
Source: ACC/AHA Guidelines for the Management of Patients with<br />
Valvular Heart Disease. 9 With permission.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 955 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 955<br />
Aortic regurgitation<br />
Echo assessment of aortic regurgitation (AR) includes a<br />
comprehensive examination of AV morphology, aortic<br />
root dilatation, and LV size and function. 16 TTE is generally<br />
the initial diagnostic test used for evaluating the<br />
severity of AR. However, TEE is also helpful particularly<br />
for patients with poor transthoracic windows, if prosthetic<br />
valves are present, and intraoperatively to guide<br />
surgical repair. TEE is particularly useful for determining<br />
the mechanism of regurgitation by distinguishing<br />
valvular from nonvalvular causes of AR. Common etiologies<br />
for AR include congenital malformations (bicuspid<br />
valves); degenerative calcific, rheumatic, and infective<br />
endocarditis; aortic aneurysm (Fig. 49-13) or dissection,<br />
Marfan’s syndrome, drug-induced (e.g., Fen-Phen) AR,<br />
and prosthetic valve dysfunction. 9 Acute and chronic AR<br />
differ in both pathophysiology and echo findings. Many<br />
of the echo findings in chronic AR (e.g., LV dilatation<br />
and systolic dysfunction) may not be present in acute<br />
AR. Chronic AR is a state of both pressure and volume<br />
overload of the LV, resulting in LV hypertrophy and<br />
dilatation.<br />
Two-dimensional echocardiography<br />
This is helpful for evaluating LV size and function, AV<br />
structure and leaflet mobility, aortic root dilatation, aortic<br />
dissection, associated vegetations, diastolic fluttering<br />
motion of MV leaflets, and premature MV closure (indicative<br />
of significant AR).<br />
Severity of aortic regurgitation<br />
In assessing the severity of chronic AR, it is essential to<br />
combine data on LV size and function with Doppler data<br />
and not to rely solely on color Doppler, since it is often<br />
misleading. No study has yet demonstrated that quantification<br />
of the severity of AR by Doppler criteria alone is<br />
predictive of outcome. Instead, LV size and function are<br />
used for risk stratification of asymptomatic patients with<br />
chronic AR. Echo findings in severe AR include:<br />
● Dilated LV: minor-axis dimension 50 to 55 mm in<br />
systole or 70 to 75 mm in diastole<br />
● LV ejection fraction 55 percent<br />
● Pressure half-time 200 ms<br />
● Proximal regurgitant color jet width/LVOT diameter<br />
65 percent<br />
● Vena contracta 6 mm<br />
● Holodiastolic flow reversal in the descending thoracic<br />
aorta<br />
● Restrictive filling pattern to the MV inflow<br />
In comparison to men, women with AR should be considered<br />
for surgery before severe symptoms have developed<br />
Figure 49-13 Aortic aneurysm of the sinuses of Valsalva and secondary aortic regurgitation.<br />
The aortic wall is thin at the sinuses of Valsalva and aneurysmal dilatation results in<br />
aortic regurgitation. Note the wide base of the regurgitant jet (vena contracta) consistent<br />
with severe aortic regurgitation (arrow). SoV sinuses of Valsalva; LV left ventricle;<br />
Ao aorta; LA left atrium; AR aortic regurgitation.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 956 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
956 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
Table 49-5<br />
Morphology<br />
Stenosis<br />
Regurgitation<br />
and for smaller LV dimensions. In a recent study, intraoperative<br />
mortality was similar for men and women, but<br />
10-year survival was significantly worse for women than<br />
for men (39 vs. 72 percent, respectively). 26<br />
In acute AR, many of the features of chronic volume<br />
overload will not be present. The severity will be need to<br />
be assessed by evaluation of color-flow Doppler jet<br />
width, presence of significant pulmonary hypertension,<br />
and evidence by Doppler of rapid equilibration of aortic<br />
and LV diastolic pressure (short diastolic half-time<br />
200 ms, short mitral deceleration time 150 ms, or<br />
premature closure of the MV). Echo assessment of the<br />
AV is summarized in Table 49-5.<br />
TRICUSPID VALVE<br />
Tricuspid valve morphology<br />
Normal function of the TV depends on the normal function<br />
of its components: annulus, leaflets, chordae, papillary<br />
muscles, right atrium, and ventricle.<br />
Tricuspid stenosis<br />
The most common cause of tricuspid stenosis (TS) is<br />
rheumatic, which results in both stenosis and regurgitation<br />
of the TV and is often associated with concomitant<br />
mitral or AV disease. Echo assessment of TS is similar to<br />
that of MS. The mean gradient across the TV is normally<br />
2 mmHg. Tricuspid stenosis is considered severe when<br />
the mean gradient is 7 mmHg and the pressure halftime<br />
(PHT) is 190 ms.<br />
Tricuspid regurgitation<br />
Echocardiographic assessment of the<br />
aortic valve<br />
Three semilunar leaflets/cusps, LV size and<br />
function<br />
Often degenerative/calcific<br />
Severe AS: area 1 cm 2 or mean gradient<br />
50 mmHg<br />
Regurgitant jet size does not correlate well<br />
with severity<br />
Severe AR: dilated LV (ESD 50–55 mm),<br />
LVH, ↓ LV systolic function (EF 55%)<br />
Acute AR: LV dilatation/systolic dysfunction<br />
may be absent<br />
LV left ventricle; AS aortic stenosis; AR aortic regurgitation;<br />
ESD end-systolic dimension; LVH left ventricular hypertrophy;<br />
EF ejection fraction.<br />
As in the case of the AV and MV, TTE or TEE evaluation<br />
of tricuspid regurgitation (TR) focuses on the identification<br />
of the etiology or mechanism of TR as well as its<br />
hemodynamic severity. TR is the most common abnormality<br />
of the TV. Mild TR is a normal finding in 70 percent<br />
of individuals. 16 Pathologic TR is often secondary<br />
to RV dysfunction, RV dilatation, or significant systolic<br />
pulmonary hypertension (systolic pulmonary artery pressures<br />
55 mmHg). Primary causes of TR are less common<br />
(Ebstein’s anomaly, endocarditis, trauma, anorectic<br />
drugs, carcinoid, myxomatous or rheumatic valvular disease,<br />
radiation). Patients with severe TR of any cause<br />
have poor long-term outcomes because of RV dysfunction<br />
and/or systemic venous congestion. TV reconstruction,<br />
annuloplasty, or valve replacement is indicated in<br />
some cases of severe TR.<br />
TEE is useful intraoperatively to assess the need for<br />
TV surgery when TR is secondary to annular dilatation<br />
and/or elevated pulmonary artery pressures, particularly<br />
during MV surgery. After correction of MV disease,<br />
TV surgery may be required if persistent severe<br />
TR or annular dilatation ( 30 mm) is still present<br />
(Fig. 49-14). 27<br />
Severity of tricuspid regurgitation<br />
Echo findings in severe TR include 16 :<br />
● A large regurgitant (color) jet ( 10 cm 2 ), vena contracta<br />
7 mm, or eccentric jet<br />
● Annular dilatation ( 30 mm), leaflet coaptation,<br />
anatomic clues (e.g., vegetations, myxomatous disease)<br />
● Dilated right atrial (RA)<br />
● Dilated RV and paradoxical interventricular septal wall<br />
motion<br />
● Pulmonary hypertension<br />
● Dilated venae cavae and hepatic veins with minimal<br />
respiratory flow variation and systolic flow reversal<br />
Pulmonary hypertension<br />
In the absence of pulmonary stenosis, pulmonary artery<br />
systolic pressure is equal to RV systolic pressure (RVSP).<br />
RVSP is estimated using the simplified Bernoulli equation<br />
(P 4V 2 ) from the peak TR velocity (V). P is<br />
then the pressure gradient across the TV, or the pressure<br />
difference between the RA and RV (P P RV<br />
P RA<br />
). In<br />
the absence of elevated RA pressures, the right atrial<br />
pressure (P RA<br />
) is estimated at 10 mmHg. Therefore,<br />
RVSP P RA<br />
P 10 4V 2<br />
Where RVSP RV systolic pressure and V peak TR<br />
velocity (ms).<br />
Severity of pulmonary hypertension<br />
Normal pulmonary artery systolic values are 18 to 25<br />
mmHg with a mean of 12 to 16 mmHg. 2 Pulmonary<br />
hypertension is defined as systolic pulmonary artery pressure<br />
greater than 30 mmHg or mean pulmonary artery<br />
pressure less than 20 mmHg at rest. 2 Commonly used<br />
values using RVSP to estimate the severity of pulmonary<br />
hypertension are shown in Table 49-6.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 957 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 957<br />
Figure 49-14 Tricuspid valve annuloplasty. This patient had infective endocarditis resulting<br />
in flail posterior mitral valve leaflet and tricuspid regurgitation. He underwent mitral<br />
valve repair and tricuspid valve annuloplasty. Note the dilated atria and tricuspid annulus<br />
preprocedure and the pacer spikes on the rhythm strip postprocedure. RA right atrium;<br />
TR tricuspid regurgitation; RV right ventricle.<br />
PROSTHETIC VALVES<br />
Any evaluation of prosthetic valve function should<br />
include an assessment of transvalvular pressure gradients<br />
and valve area, similar to the evaluation of native<br />
valve function. TTE is helpful in the initial assessment of<br />
prosthetic valve dysfunction. However, its sensitivity is<br />
impaired by difficulty in visualizing structures around<br />
and behind the prosthesis, particularly for mechanical<br />
valves. Prosthetic material attenuates the ultrasound<br />
beam and causes multiple reverberations, hampering<br />
interpretation. TEE is often required for the complete<br />
evaluation of prosthetic valve structure and function.<br />
Cinefluoroscopy may also be a relatively quick and useful<br />
method for determining leaflet mobility in mechanical<br />
valves and is indicated when mechanical valve thrombosis<br />
is suspected. When valve dysfunction is suspected, 2D<br />
echo with Doppler and color flow in addition to TEE<br />
may be necessary for a comprehensive evaluation of<br />
Table 49-6<br />
Severity of pulmonary hypertension<br />
RVSP (mmHg)<br />
Normal 18–25<br />
Mild 30–40<br />
Moderate 40–70<br />
Severe<br />
70<br />
RVSP right ventricular systolic pressure.<br />
valve function. Such an evaluation of valve function is<br />
summarized in Table 49-7. 28 TEE findings in common<br />
complications of prosthetic valves are shown in Table<br />
49-8. 28<br />
Prosthetic valve pressure gradients<br />
Like native valve gradients, prosthetic valve pressure<br />
gradients can be obtained using the simplified Bernoulli<br />
Table 49-7<br />
Evaluation of prosthetic valves<br />
Pressure gradients P 4V 2<br />
Valve area<br />
MV prostheses: area 220/PHT<br />
AV or MV prostheses: A 1<br />
V 1<br />
A 2<br />
V 2<br />
Regurgitation/leaks Size, symmetry, velocity, eccentricity<br />
Leaflet mobility/ Degree of leaflet excursion<br />
restriction<br />
LV size/function LV dimensions, EF<br />
Pulmonary RVSP 4V 2 10<br />
hypertension<br />
Compare with Change in gradients, area, leaks<br />
prior echo<br />
P pressure gradient; V velocity; MV mitral valve; PHT <br />
pressure half-time; AV aortic valve; A 1<br />
V 1<br />
flow (area 1<br />
velocity<br />
1<br />
) proximal to the valve prosthesis; A 2<br />
V 2<br />
flow (area 2<br />
velocity<br />
2<br />
) across the valve prosthesis; LV left ventricle; EF ejection<br />
fraction; RVSP right ventricular systolic pressure.<br />
Source: From Zabalgoitia. 28 With permission.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 958 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
958 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
Table 49-8<br />
Paravalvular leak<br />
Pannus formation<br />
Structural<br />
deterioration<br />
Nonstructural<br />
dysfunction<br />
Thrombosis<br />
TEE Findings in prosthetic valve<br />
complications<br />
Source: From Zabalgoitia. 28 With permission.<br />
Large, wide, eccentric jet with<br />
high-velocity turbulent flow<br />
Dehiscence, regurgitation, stenosis<br />
Calcific degeneration (bioprostheses)<br />
Often due to inappropriate sizing,<br />
stenosis, or regurgitation<br />
Decreased range of motion or<br />
maximum excursion<br />
Stenosis ( regurgitation)<br />
Distinguish from fibrin strands, which<br />
are small filaments on the atrial<br />
aspect of mitral or ventricular<br />
aspect of aortic valves<br />
Stenosis<br />
Irregular echogenic mobile mass<br />
or masses on valve<br />
Regurgitation ( stenosis)<br />
Leaflet destruction (bioprostheses)<br />
Perivalvular abscess (valve rocking,<br />
periaortic root thickening,<br />
echolucency)<br />
Perivalvular dehiscence, fistular tract<br />
equations may be used for the calculation of prosthetic<br />
TV areas.<br />
Paravalvular leaks<br />
Normal amounts of regurgitation are expected with<br />
prosthetic valves owing to the built-in transvalvular<br />
regurgitation (“closing volume”). The amount of<br />
regurgitation increases with valve size, the size of the<br />
gap between the occluder and the rim, and lower heart<br />
rates. Echo findings 4 of normal prosthetic valve regurgitation<br />
include:<br />
1. AV: regurgitant area 1 cm 2 and length of jet<br />
1.5 cm<br />
2. MV: regurgitant area 2 cm 2 and length of jet<br />
2.5 cm<br />
3. Characteristic flow patterns (Medtronic-Hall, one<br />
central jet; Star-Edwards, two curved side jets; Bjork-<br />
Shiley, two unequal side jets; St. Jude Medical, two<br />
side jets and one central jet)<br />
Larger leaks in other locations (Fig. 49-15) are abnormal<br />
and may be associated with significant hemodynamic<br />
compromise, hemolysis, or valve dehiscence. 28 TEE is<br />
often required to fully assess prosthetic valve regurgitation<br />
because of the limited sensitivity of TTE. Echo characteristics<br />
that differentiate physiologic from nonphysiologic<br />
regurgitation are summarized in Table 49-9. 28<br />
equation (P 4V 2 ). Compared to normal native<br />
valves, homografts and the newer nonstented bioprostheses<br />
have similar velocities and pressure gradients,<br />
while mechanical valves have higher flow velocities.<br />
Prosthetic valves except ball-cage valves normally have<br />
pressure gradients since they are by design obstructive,<br />
with gradients increasing as valve size decreases. High<br />
gradients are often seen with 19-mm AV prostheses.<br />
High gradients in prosthetic valves may be seen for<br />
other reasons as well, such as high cardiac output, valve<br />
obstruction, or significant valvular regurgitation (due to<br />
increased flow).<br />
Prosthetic valve area<br />
As in the case of native valves, prosthetic valve area can<br />
be calculated using the continuity equation or pressure<br />
half-time method. For AV prostheses, the continuity<br />
equation (A 1<br />
V 1<br />
A 2<br />
V 2<br />
) is usually used. The LV outflow<br />
tract (LVOT) diameter or outer diameter of the sewing<br />
ring (not its internal diameter) should be measured for<br />
accurate estimation of A 1<br />
. For MV prostheses, use of the<br />
continuity equation is preferred, since the pressure halftime<br />
equation may overestimate the true prosthetic MV<br />
area. The continuity equation should not be used if<br />
there is significant aortic regurgitation or MR. The same<br />
<strong>IN</strong>FECTIVE ENDOCARDITIS<br />
TEE is the procedure of choice for the detection of<br />
vegetations in infective endocarditis, with better sensitivity<br />
(50 percent for TTE vs. 90 percent for TEE) and<br />
specificity (95 percent for TTE vs. 95 percent for<br />
TEE) for native valve endocarditis compared to<br />
TTE. 29,30 Characteristics of valvular vegetations are<br />
listed in Table 49-10. 29 However, early in the course of<br />
infective endocarditis, vegetations may not have these<br />
typical characteristics and TEE should be repeated if<br />
the clinical suspicion is high. Compared with native<br />
valve endocarditis, it is more difficult to identify vegetations<br />
on prosthetic valves because of artifact from the<br />
prosthetic materials. Often both TTE and TEE are<br />
useful to detect vegetations, although TTE has lower<br />
sensitivity compared with TEE for prosthetic valve<br />
endocarditis. 8 TEE is particularly sensitive for identifying<br />
ring abscesses. Complications of infective endocarditis<br />
(Fig. 49-16) include:<br />
1. Paravalvular abscesses<br />
2. Valve destruction or perforation, leaflet rupture, or<br />
dehiscence of prosthetic valves<br />
3. Fistulas<br />
4. Pseudoaneurysms<br />
5. Emboli
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 959 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 959<br />
A<br />
B<br />
Figure 49-15 Paravalvular and valvular leaks. A. Bileaflet mechanical mitral prosthesis<br />
with severe paravalvular regurgitation secondary to endocarditis and partial valve dehiscence,<br />
requiring valve replacement. B. Aortic bioprosthesis with severe aortic regurgitation<br />
due to calcific degeneration and a torn leaflet. LA left atrium; LV left ventricle; MR <br />
mitral regurgitation; Ao aorta.<br />
EVALUATION OF SPECIFIC DISORDERS<br />
CORONARY ARTERY DISEASE<br />
Myocardial ischemia/infarction<br />
The echo manifestation of myocardial ischemia is a<br />
decrease in contractility or systolic wall thickening of the<br />
ischemic territory that is manifest within seconds of the<br />
onset of ischemia, prior to evidence of electrocardiographic<br />
ischemia. 4 Abnormal wall thickening is a better<br />
indicator of ischemia than wall motion, since infarcted<br />
myocardium may be passively pulled or tethered by adjacent<br />
normal myocardium, resulting in apparent wall<br />
motion without active contraction. Ancillary signs of<br />
ischemia include an increase in end-systolic LV volume<br />
and a decrease in global contractility or EF. 4 Hypokinesis<br />
is decreased contractility (30 percent wall thickening);<br />
akinesis is the absence of contractility (10 percent wall<br />
Table 49-9<br />
Physiologic and nonphysiologic valvular<br />
regurgitation<br />
Regurgitant Jet Physiologic Nonphysiologic<br />
Size Small, narrow Large, wide<br />
Symmetrical Yes No<br />
Velocity Low High<br />
Eccentric No Yes<br />
Source: Modified from Zabalgoitia. 28 With permission.<br />
thickening); and dyskinesis is outward motion during<br />
systole. Echo is accurate at localizing the site of coronary<br />
obstruction (Fig. 49-17). However, it usually overestimates<br />
infarct size due to myocardial stunning, which has<br />
resulted in a lack of correlation between wall motion<br />
abnormalities detected on echo in the setting of an acute<br />
myocardial infarction and infarct extent. 31<br />
Ischemic, infarcted, stunned, or<br />
hibernating myocardium<br />
Myocardial segments may be dysfunctional secondary<br />
to ischemia, infarction/scar, or stunned or hibernating<br />
myocardium. Stunned myocardium is postischemic ventricular<br />
dysfunction that occurs when reperfusion of the<br />
occluded artery has been achieved but the wall motion<br />
and thickening of the corresponding myocardial segment<br />
remain abnormal—a condition that may last for days to<br />
weeks. Hibernating myocardium results from chronic<br />
ischemic dysfunction when the myocardial tissue is chronically<br />
hypoperfused owing to inadequate blood flow,<br />
resulting in abnormal wall motion and thickening, but it<br />
usually recovers after successful revascularization. Resting<br />
echo may help differentiate viable (stunned or hibernating)<br />
myocardium from nonviable (infarcted or scarred)<br />
myocardium based on wall thickness. Thicker myocardium<br />
is more likely to be viable, while thinned and fibrotic<br />
myocardium most likely represents scar. 4 The specificity of<br />
these criteria is quite low, however. Viability assessment
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 960 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
960 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
Table 49-10 Echocardiographic characteristics of vegetative and nonvegetative valvular masses<br />
Characteristic Vegetation Nonvegetation<br />
Echogenicity Similar to myocardium Similar to pericardium<br />
Low echogenicity/gray<br />
High echogenicity/white<br />
Location Upstream surface of valve near the Downstream surface of valve<br />
regurgitant jet<br />
Motion Mobile, prolapses Less mobile<br />
Shape Amorphous, lobulated Filamentous, strand-like narrow base of<br />
Wide base of attachment<br />
attachment<br />
Regurgitation Severe regurgitant jet Mild or no regurgitant jet<br />
Vegetation located near jet<br />
Other Paravalvular abscess/leak None<br />
Fistula<br />
Valve dehiscence<br />
Source: Modified from Schiller. 29 With permission.<br />
can be significantly improved with dobutamine or stress<br />
echocardiography. 8 A biphasic response on dobutamine<br />
echo is the most sensitive parameter for viable myocardium<br />
and is associated with improved survival after revascularization.<br />
This is evidenced by an improvement in wall<br />
motion and thickening or recruitment at low-dose dobutamine<br />
(10 to 20 g/kg/min) followed by worsening<br />
of wall motion and thickening at higher doses (30 to<br />
40 g/kg/min) when the ischemic threshold is reached.<br />
Left ventricular aneurysm and mural thrombus<br />
A true ventricular aneurysm consists of a thin wall ( 7<br />
mm) that is echogenic (and sometimes calcified) and has<br />
A<br />
B<br />
C<br />
D<br />
Figure 49-16 Complications of infective endocarditis. A. Large vegetation on bioprosthetic<br />
tricuspid valve seen on transesophageal echocardiogram. B. Sinus of Valsalva<br />
aneurysm and aortic–right ventricular fistula. C. Bicuspid aortic valve with bacterial endocarditis<br />
complicated by large aortic root (annular) abscess (note the thickened perivalvular<br />
tissue) and complete heart block requiring emergent surgery. D. Large aortic valve vegetation<br />
prolapsing into the left ventricular outflow tract during systole. LA left atrium; TV <br />
tricuspid valve; RV right ventricle; SoV sinus of Valsalva; Ao aorta; AV aortic<br />
valve; LV left ventricle.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 961 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 961<br />
myocardial infarcts. Spontaneous echo contrast (SEC) or<br />
mural thrombus may be present within an LV aneurysm<br />
and is associated with an increased risk of embolic events.<br />
The appearance of an acute mural thrombus (same<br />
echogenicity as myocardium) generally differs from that<br />
of a chronic thrombus, which tends to be layered with<br />
areas of calcification. 31 Compared to TTE, TEE may be<br />
limited in detecting apical thrombi because of the often<br />
suboptimal visualization of the true LV apex with TEE.<br />
Pseudoaneurysms can also be complications of acute<br />
myocardial infarction and are characterized by the lack of a<br />
true myocardial wall. They result from contained free wall<br />
myocardial rupture in which a portion of the pericardial<br />
space limits frank rupture. Pseudoaneurysms can generally<br />
be differentiated from true aneurysms by the presence of a<br />
narrow neck (less than half of the maximum diameter)<br />
compared to the wider base of a true aneurysm. 31<br />
Figure 49-17 Common myocardial perfusion patterns by<br />
each of the three major coronary arteries. LAD left anterior<br />
descending; Cx left circumflex; RCA right coronary<br />
artery. (From Shanewise et al. 12 With permission.)<br />
outward motion in both systole and diastole. 31 Most<br />
aneurysms occur apically, with inferobasal aneurysms<br />
being the second most common. Aneurysms are complications<br />
of adverse remodeling following transmural<br />
Postinfarct ventricular septal defect<br />
Life-threatening mechanical complications after acute<br />
myocardial infarction include free wall rupture, papillary<br />
muscle dysfunction/rupture, and ventricular septal defect<br />
(VSD) (Fig. 49-18). TTE is usually sufficient for the<br />
diagnosis of mechanical complications, although TEE<br />
may be used as an adjunct. Postinfarct VSD is uncommon<br />
(less than 1 percent of total infarcts), although it is associated<br />
with the worst outcome of mechanical complications<br />
in patients with cardiogenic shock. Unlike postinfarct<br />
papillary muscle rupture, VSD occurs with approximately<br />
equal frequency after anterior and inferior infarcts. The posteroapical<br />
septum is the most common site of postinfarct<br />
A<br />
B<br />
Figure 49-18 Postinfarct ventricular septal defect (VSD). This patient had suffered an<br />
acute anterior myocardial infarction that was treated with thrombolytics but subsequently<br />
developed a high septal VSD. A. Intraoperative transesophageal echocardiogram with<br />
color-flow Doppler diagnostic of VSD with high-velocity turbulent flow across the septum.<br />
B. Surgical repair with a pericardial patch and coronary artery bypass grafting to the ostial<br />
left anterior descending artery was successful. Color-flow Doppler shows no flow across<br />
the septum. LV left ventricle; RV right ventricle.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 962 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
962 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
Table 49-11<br />
Diagnostic tests for acute aortic dissection<br />
Sensitivity Specificity<br />
Test (%) (%) Pluses and minuses<br />
TEE 99–100 89 Pluses: Quick, semi-invasive, assesses AR, coronaries, pericardial effusion,<br />
may assess IH<br />
Minuses: Limited assessment of IH, “blind spot” of distal ascending aorta<br />
and anterior aortic arch, reverberation artifact<br />
CT 90 85 Pluses: Quick, noninvasive<br />
Minuses: Cannot assess branch vessels or IH, dye load/allergy<br />
MRI 98–100 100 Pluses: Noninvasive, assesses branch vessels, IH<br />
Minuses: Slow, may not be available, pacemakers/device, breath-hold<br />
necessary<br />
Angiography 88–91 95 Pluses: Assesses coronaries, AR, branch vessels<br />
Minuses: Slow, invasive, dye load, may miss dissection if lumen is<br />
completely thrombosed, does not detect IH<br />
IH intramural hematoma; AR aortic regurgitation.<br />
Sources: From Erbel et al., 32 Sabatine, 33 and Nienaber et al. 34 With permission.<br />
VSD. Echo is the gold standard for diagnosing ventricular<br />
septal rupture complicating myocardial infarction. TTE<br />
using color-flow Doppler has a sensitivity of 85 to 95 percent,<br />
while TEE has a sensitivity and specificity of 100 percent.<br />
31 Echo characteristics of postinfarct VSD, in addition<br />
to the septal defect, include the presence of a small pericardial<br />
effusion with possible intrapericardial thrombus<br />
(echogenic mobile mass in the pericardial space) and echo<br />
evidence of tamponade. 31<br />
THORACIC AORTIC ANEURYSM<br />
AND DISSECTION<br />
TTE may diagnose aortic dissection by detecting an intimal<br />
flap in the aorta (specificity 95 percent), but it has<br />
low sensitivity (80 percent) for ascending aortic dissection<br />
and even lower sensitivity for distal thoracic aortic<br />
dissection (70 percent). 32 TEE is one of three imaging<br />
modalities used for the diagnosis of acute aortic dissection—TEE,<br />
computed tomography (CT), and magnetic<br />
resonance imaging (MRI) 33,34 —and for the diagnosis of<br />
perioperative aortic dissections (Table 49-11). The<br />
choice of imaging modality depends primarily on the<br />
availability of the imaging procedure and patient characteristics<br />
(e.g., hemodynamic instability, presence of a<br />
pacemaker, or contrast allergy), since the overall diagnostic<br />
accuracy for TEE, CT, and MRI is comparable. 32<br />
TEE is the imaging procedure of choice for patients who<br />
are hemodynamically unstable. Compared to CT or<br />
MRI, one limitation of TEE is that it cannot image the<br />
aortic segment located between the distal ascending<br />
aorta and the proximal arch, which may decrease its sensitivity<br />
for detection of aortic dissection, hematoma, or<br />
atheroma in this region.<br />
The main criterion for TEE diagnosis of suspected<br />
acute aortic dissection is the presence of two lumina<br />
(false and true) separated by an intimal flap (Table 49-12<br />
and Fig. 49-19). Other findings for diagnosing aortic<br />
dissection by TEE 32 include:<br />
1. Tear or disruption of the flap continuity or jets seen<br />
with color Doppler across the flap<br />
2. Complete obstruction of the false lumen; presence of<br />
thrombus<br />
3. Central displacement of intimal calcification or separation<br />
of intimal layers from thrombus<br />
4. Periaortic hematoma (echo-free spaces around the<br />
aorta)<br />
5. Intramural hematoma (crescent-shaped echodensity<br />
with vacuolization within it on the aortic short-axis<br />
view)<br />
6. Pericardial or pleural effusion<br />
7. AR<br />
It is important to define the anatomic site and extension<br />
of the dissection, the degree of AR, involvement of the<br />
coronary arteries, LV dysfunction, and the presence of<br />
pericardial effusion or tamponade.<br />
Intraoperatively, TEE is used during reconstructive<br />
surgery for hemodynamic status, entry/exit sites, evaluation<br />
of decompression of the false lumen, and assessment<br />
of concomitant valve surgery. 13 Postoperatively, TEE is<br />
used for the detection of residual regurgitation and LV<br />
dysfunction. TEE is also indicated for defining the<br />
anatomic site and size of aortic aneurysms.<br />
Table 49-12<br />
True versus false lumen in aortic dissection<br />
True lumen<br />
False lumen<br />
Systole Expansion Collapse<br />
Diastole Collapse Expansion<br />
SEC/thrombus Absent or minimal Present<br />
Blood flow Systolic forward flow Reversed or<br />
absent flow<br />
SEC spontaneous echo contrast.<br />
Source: Erbel et al. 32 With permission.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 963 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 963<br />
A<br />
B<br />
C<br />
Figure 49-19 Dissection of the descending thoracic aorta. Transesophageal echocardiogram<br />
showing a large aortic dissection with the diagnostic flap separating the true (TL) and<br />
false lumen (FL). A. Short-axis view. B. Long-axis view. C. Long-axis with color-flow<br />
Doppler shows flow in both the true and false lumens.<br />
PERICARDIAL DISEASE<br />
Pericardial effusion and tamponade<br />
Echo is the diagnostic test of choice for detection of<br />
pericardial effusion (PE) and assessing its hemodynamic<br />
significance. TEE is usually superior to TTE for<br />
evaluating pericardial thickness and adjacent structures,<br />
although CT and/or MRI are preferred for evaluating<br />
the pericardium. Normally, the pericardial space contains<br />
10 to 50 mL of fluid and the pericardium measures 1 to<br />
3 mm in thickness. An increase in the volume of the pericardial<br />
fluid results in elevated pericardial pressures, leading<br />
to reduced RV filling, followed by reduced LV filling<br />
(Fig. 49-20). PE usually appears as an echo-free space<br />
surrounding the myocardium, although as protein or<br />
cellular debris increases in the fluid, it becomes increasingly<br />
echogenic. 35 PE is differentiated from pleural effusion<br />
by the anterior location of PE relative to the<br />
proximal descending thoracic aorta, while pleural effusion<br />
is located posteriorly to the aorta. Epicardial fat<br />
may be confused with PE, since it is also echolucent,<br />
although epicardial fat is usually more echogenic than<br />
pericardial fluid and is usually located anteriorly. 35 TEE is<br />
useful in the postoperative patient with tamponade and a<br />
small loculated PE that may be difficult to visualize on<br />
TTE. Loculated PE in postoperative cardiac surgery<br />
patients may cause tamponade in the absence of typical<br />
Figure 49-20 Large pericardial effusion and cardiac tamponade.<br />
Transthoracic echocardiogram of the apical fourchamber<br />
view reveals an atrial myxoma attached to the<br />
interatrial septal with a large echolucent circumferential<br />
pericardial effusion (PE) and evidence of elevated intrapericardial<br />
pressure. Classic features of tamponade are shown<br />
with right ventricular (RV) diastolic collapse and abnormal<br />
interventricular septal motion (shifted toward the left during<br />
inspiration). RA right atrium; LA left atrium; LV left<br />
ventricle.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 964 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
964 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
Table 49-13<br />
RA collapse<br />
RV diastolic collapse<br />
LA, LV collapse<br />
Abnormal<br />
interventricular<br />
septal motion<br />
Respiratory variation<br />
in ventricular size<br />
Respiratory variation<br />
in transvalvular<br />
inflow velocities<br />
Respiratory variation<br />
in PV and HV<br />
velocities<br />
Dilated IVC and<br />
blunted respiratory<br />
changes<br />
Echocardiographic signs of cardiac<br />
tamponade<br />
echo signs (Table 49-13). In these patients, any evidence<br />
of LA or LV collapse or other localized chamber compression<br />
may be indicative of hemodynamically significant<br />
elevated intrapericardial pressures.<br />
Constrictive pericardial disease<br />
Sensitive but not specific.<br />
Ranges from inward dip to complete<br />
collapse of RV free wall in diastole;<br />
specific sign but may be absent if<br />
elevated RV pressures or adhesions<br />
tether RV.<br />
May be the only sign of tamponade<br />
in postoperative cardiac surgery<br />
patients.<br />
Inspiration: septum shifts to the left.<br />
Inspiration: LV becomes smaller,<br />
RV larger.<br />
Inspiration: mitral inflow E velocity<br />
decreases, tricuspid inflow velocity<br />
increases.<br />
Inspiration: PV velocities decrease<br />
and HV velocities increase.<br />
Not very specific.<br />
RA right atrium; RV right ventricle; LA left atrium; LV left<br />
ventricle; PV pulmonary vein; HV hepatic vein; IVC inferior<br />
vena cava.<br />
Sources: From Oh 4 and Munt et al. 35 With permission.<br />
In constrictive pericardial disease, the pericardium is thickened<br />
(3 mm) and often calcified, which reduces ventricular<br />
filling in diastole and causes diastolic heart failure.<br />
However, the absence of pericardial calcification does not<br />
rule out the diagnosis of constriction. Although echo<br />
signs of constriction (Table 49-14) are not very sensitive<br />
or specific, a completely normal echo study usually rules<br />
out constriction. 36 Other imaging modalities, such as CT<br />
or MRI, may be necessary to further evaluate the pericardium<br />
and distinguish constriction from restriction.<br />
<strong>CARDIAC</strong> SOURCES OF EMBOLI<br />
One of the most common indications for TEE is for the<br />
evaluation for cardiac sources of emboli, since TTE does<br />
not visualize well the potential sources of emboli (LA<br />
appendage thrombus, aortic atheroma, patent foramen<br />
ovale or atrial septal defect, LV thrombus, valvular<br />
lesions, intracardiac tumors). Small thrombi in the LA or<br />
Table 49-14<br />
Pericardial thickening<br />
and calcification<br />
Dilated RA, LA, IVC<br />
Diastolic flattening of<br />
the LV posterior wall<br />
Abnormal interventricular<br />
septal motion<br />
Premature pulmonary<br />
valve opening<br />
Respiratory variation in<br />
ventricular size<br />
Respiratory variation in<br />
transvalvular and<br />
venous (pulmonary/<br />
hepatic) flow velocities<br />
Echocardiographic signs of constriction<br />
LA appendage can be detected using TEE. In addition,<br />
factors that may contribute to or accompany atrial<br />
thrombi are often seen in the absence of an obvious<br />
thrombus: LA or LA appendage enlargement, SEC consistent<br />
with blood stasis, and decreased LA appendage<br />
contraction with low PW Doppler velocities ( 20<br />
mm/s). Aortic atheromas are evaluated for mobile components,<br />
plaque rupture, and ulceration and are graded<br />
as mild ( 1 mm), moderate (1 to 3.9 mm), and severe<br />
( 4 mm).<br />
ATRIAL SEPTAL DEFECTS<br />
TEE better than TTE, but additional<br />
imaging with CT or MRI may<br />
be necessary<br />
Nonspecific findings<br />
Secondary to reduced filling in<br />
mid- to late diastole, sensitive<br />
but not specific<br />
Inspiration: septum shifts to<br />
the left<br />
RV diastolic pressure PA<br />
diastolic pressure in middiastole<br />
Inspiration: LV becomes smaller,<br />
RV larger<br />
As in tamponade, respiratory<br />
variation may be more<br />
prominent in constriction<br />
RA right atrium; LA left atrium; IVC inferior vena cava;<br />
LV left ventricle; RV right ventricle; PA pulmonary artery.<br />
Sources: From Oh, 4 Munt et al., 35 and Hoit. 36 With permission.<br />
TEE is superior to TTE for visualizing atrial septal<br />
defects (ASDs). The anatomic defect is visualized using<br />
two-dimensional echo and confirmed with Doppler and<br />
contrast (bubble study) using maneuvers that increase<br />
RA pressure, such as Valsalva or cough. The hemodynamic<br />
significance of the shunt is assessed using Doppler<br />
by quantifying the shunt size and determining the presence<br />
of pulmonary hypertension. Shunt quantification is<br />
obtained as the ratio of pulmonary to systemic flow<br />
(Q p<br />
:Q s<br />
) using Doppler cardiac outputs across the pulmonary<br />
valve and AV. 4 All four pulmonary veins should<br />
be visualized and the presence of associated anomalies<br />
excluded. TEE plays an important role in determining<br />
the suitability of ASDs for device closure versus cardiac<br />
surgery based on the size of the ASD and the rim of tissue<br />
surrounding it as well as the degree of septal tissue<br />
redundancy. 23 TEE has become essential for guiding<br />
placement of catheter-deployed closure devices and in<br />
assessing residual shunts (Fig. 49-21).
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 965 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 965<br />
A<br />
B<br />
C<br />
D<br />
Figure 49-21 Secundum atrial septal defect (ASD) and clamshell closure. A. Secundum<br />
ASD seen as a defect in the mid-interatrial septum along with a dilated right atrium (RA)<br />
on transesophageal echocardiography. The size of the rim of tissue between the ASD and<br />
the aortic valve is critical in determining likelihood of success with device closure. C.<br />
Color-flow Doppler of the ASD shows a high-turbulence jet consistent with shunt (arrow).<br />
B. The clamshell has been deployed across the ASD. D. Postprocedure color-flow<br />
Doppler with small residual shunt that usually resolves spontaneously after a period of<br />
several weeks to months. AV aortic valve.<br />
<strong>CARDIAC</strong> TUMORS<br />
TEE, because of its high sensitivity, is the imaging modality<br />
of choice and is superior to TTE, CT, MRI, and angiography<br />
for detecting cardiac tumors. 1,4 Although MRI may<br />
not detect small cardiac tumors, it is usually performed<br />
after TEE for further differentiation of thrombus (presence<br />
of methemoglobin or hemosiderin) from neoplasm,<br />
since it is superior to TEE for tissue characterization.<br />
MRI examinations are multiplanar and typically include<br />
fast T1- and T2-weighted techniques with administration<br />
of gadolinium (a paramagnetic contrast agent) and a technique<br />
for imaging moving structures with single-slice<br />
breath-hold, such as fast gradient-echo sequences (e.g.,<br />
FLASH). Primary tumors are more likely to affect the<br />
myocardium, while secondary tumors usually involve the<br />
pericardium with secondary intramyocardial infiltation. 37<br />
Atrial myxomas are the most common (up to 25 percent)<br />
primary cardiac tumors. Atrial myxomas as seen on TEE or<br />
TTE show several typical features 37 (Fig. 49-22A):<br />
● Ninety percent originate in the interatrial septum, near<br />
the fossa ovalis.<br />
● A spherical mass with a speckled appearance is often<br />
seen in RA myxomas, while a villous amorphous mass<br />
may be seen in LA myxomas.<br />
● Ninety percent attach to the wall of the atrium via a<br />
stalk, which may allow prolapse through the MV.<br />
● Intramural hemorrhage (cysts) and necrosis result in a<br />
heterogeneous appearance of echodensity; calcifications<br />
are uncommon but may be seen.<br />
● They may be highly mobile and a cardiac source of<br />
embolus.<br />
Metastatic tumors to the heart most commonly arise<br />
from the breast or lung but may include leiomyosarcoma<br />
(Fig. 49-22B). Metastatic tumors usually affect the pericardium<br />
and result in pericardial effusion. In addition,<br />
some tumors metastasize through the inferior vena cava<br />
(renal cell, hepatoma), affecting the right heart more than<br />
the left; TEE allows for visualization of the route of extension.<br />
37 Tumors involving the cardiac valves are rare (often<br />
fibroelastomas) and may affect valve competence and<br />
global LV function. MRI and ultrafast CT may be a useful<br />
adjunct in delineating tumors of the cardiac valves. 38<br />
LEFT VENTRICULAR OUTFLOW<br />
TRACT OBSTRUCTION<br />
TEE is used intraoperatively for septal myectomy for treatment<br />
of obstruction of the LV outflow tract (LVOT) due
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 966 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
966 PART II ● ADULT <strong>CARDIAC</strong> <strong>SURGERY</strong><br />
A<br />
B<br />
Figure 49-22 Cardiac tumors. A. Large atrial myxoma attached to the interatrial septum,<br />
seen as a spherical mass with a speckled appearance. B. Metastatic leiomyosarcoma of<br />
genitourinary tract origin with myocardial invasion of the left ventricular (LV) apex.<br />
to hypertrophic cardiomyopathy. Systolic anterior motion<br />
(SAM) of the MV may cause LVOT obstruction; TEE is<br />
used to define the structures involved in the SAM (e.g.,<br />
chordae, anterior leaflet). As in aortic stenosis, LVOT gradients<br />
may differ intraoperatively versus preoperatively<br />
owing to different hemodynamics. Color-flow Doppler<br />
typically demonstrates turbulent blood flow (mosaic pattern)<br />
at the site of LVOT obstruction. An eccentric jet of<br />
MR may also be seen if there is abnormal coaptation of<br />
the mitral leaflets (usually a posteriorly directed jet owing<br />
to abnormal coaptation of the anterior mitral leaflet).<br />
TEE is also helpful during resection of lesions causing<br />
subaortic stenosis. It can determine the location and<br />
severity of obstruction. It is also useful for evaluating the<br />
success of the surgery in relieving the obstruction and in<br />
detecting MR that may result from the surgery. 22<br />
References<br />
1. Otto CM. The Practice of Clinical Echocardiography.<br />
Philadelphia: Saunders, 2002:977.<br />
2. Braunwald EB. Heart Disease. Philadelphia: Saunders,<br />
2001:2297.<br />
3. Maurer G, Mohl W. Echocardiography and Doppler in<br />
Cardiac Surgery. New York: Igaku-Shoin, 1989:355.<br />
4. Oh JK. The Echo Manual. Philadelphia: Lippincott<br />
Williams & Wilkins, 1999:278.<br />
5. Murphy JG. Mayo Clinic Cardiology Review. Philadelphia:<br />
Lippincott Williams & Wilkins, 2000:1381.<br />
6. Quinones MA, Otto CM, Stoddard M, et al. American<br />
Society of Echocardiography: Recommendations for<br />
Quantification of Doppler Echocardiography. Raleigh, NC:<br />
American Society of Echocardiography, 2001.<br />
7. Hagan AD, DeMaria AN. Clinical Applications of Two-<br />
Dimensional Echocardiography and Cardiac Doppler.<br />
Boston/Toronto: Little, Brown, 1989:1556.<br />
8. Cheitlin MD, Armstrong WF, Aurigemma GP, et al.<br />
ACC/AHA/ASE 2003 guideline update for the clinical<br />
application of echocardiography: Summary article: A<br />
report of the American College of Cardiology/American<br />
Heart Association Task Force on Practice Guidelines<br />
(ACC/AHA/ASE Committee to Update the 1997<br />
Guidelines for the Clinical Application of<br />
Echocardiography). Circulation 2003;108:1146–1162.<br />
9. ACC/AHA Guidelines for the Management of Patients<br />
with Valvular Heart Disease. A report of the American<br />
College of Cardiology/American Heart Association. Task<br />
Force on Practice Guidelines (Committee on Management<br />
of Patients with Valvular Heart Disease). J Am Coll<br />
Cardiol 1998; 32:1486–1588.<br />
10. Goldstein SA, Harry M. American Society of<br />
Echocardiography Core Curriculum for Physicians. Raleigh,<br />
NC: American Society of Echocardiography, Vol. 2003.<br />
11. Oh JK, Appleton CP, Hatle LK, et al. The noninvasive<br />
assessment of left ventricular diastolic function with twodimensional<br />
and Doppler echocardiography. J Am Soc<br />
Echocardiogr 1997;10:246–270.<br />
12. Shanewise JS, Cheung AT, Aronson S, et al. ASE/SCA<br />
guidelines for performing a comprehensive intraoperative<br />
multiplane transesophageal echocardiography examination:<br />
Recommendations of the American Society of<br />
Echocardiography Council for Intraoperative<br />
Echocardiography and the Society of Cardiovascular<br />
Anesthesiologists Task Force for Certification in<br />
Perioperative Transesophageal Echocardiography. J Am<br />
Soc Echocardiogr 1999;12:884–900.<br />
13. Practice guidelines for perioperative transesophageal<br />
echocardiography. A report by the American Society of<br />
Anesthesiologists and the Society of Cardiovascular<br />
Anesthesiologists Task Force on Transesophageal<br />
Echocardiography. Anesthesiology 1996;84:986–1006.<br />
14. Schiller NB. Hemodynamics derived from transesophageal<br />
echocardiography (TEE). Cardiol Clin 2000;18:699–709.<br />
15. Wilkins GT, Weyman AE, Abascal VM, et al. Percutaneous<br />
balloon dilatation of the mitral valve: An analysis of<br />
echocardiographic variables related to outcome and the<br />
mechanism of dilatation. Br Heart J 1988; 60:299–308.<br />
16. Zoghbi WA, Enriquez-Sarano M, Foster E, et al.<br />
Recommendations for evaluation of the severity of native<br />
valvular regurgitation with two-dimensional and Doppler<br />
echocardiography. J Am Soc Echocardiogr 2003;16:777–802.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 967 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks<br />
Chapter 49 ● Echocardiography in Cardiac Surgery 967<br />
17. Griffin BP, Stewart WJ. Echocardiography in patient selection,<br />
operative planning, and intraoperative evaluation of<br />
mitral valve repair. In: Otto CM (ed). The Practice of<br />
Clinical Echocardiography. Philadelphia: Saunders,<br />
2002:417–434.<br />
18. Thomas JD. Doppler echocardiographic assessment of<br />
valvular regurgitation. Heart 2002;88:651–657.<br />
19. Playford D, Weyman AE. Mitral valve prolapse: Time for a<br />
fresh look. Rev Cardiovasc Med 2001;2:73–81.<br />
20. Freed LA, Levy D, Levine RA, et al. Prevalence and clinical<br />
outcome of mitral-valve prolapse. N Engl J Med<br />
1999;341:1–7.<br />
21. Zaroff JG, Picard MH. Transesophageal echocardiographic<br />
(TEE) evaluation of the mitral and tricuspid<br />
valves. Cardiol Clin 2000;18:731–750.<br />
22. Shively BK. Transesophageal echocardiographic (TEE)<br />
evaluation of the aortic valve, left ventricular outflow tract,<br />
and pulmonic valve. Cardiol Clin 2000;18:711–729.<br />
23. King MEE. Echocardiographic evaluation of the adult<br />
with unoperated congenital heart disease. In: Otto<br />
CM (ed). The Practice of Clinical Echocardiography.<br />
Philadelphia: Saunders, 2002:868–899.<br />
24. Hahn RT, Roman MJ, Mogtader AH, Devereux RB.<br />
Association of aortic dilation with regurgitant, stenotic<br />
and functionally normal bicuspid aortic valves. J Am Coll<br />
Cardiol 1992;19:283–288.<br />
25. Otto CM, Burwash IG, Legget ME, et al. Prospective<br />
study of asymptomatic valvular aortic stenosis. Clinical,<br />
echocardiographic, and exercise predictors of outcome.<br />
Circulation 1997;95:2262–2270.<br />
26. Klodas E, Enriquez-Sarano M, Tajik AJ, et al. Surgery for<br />
aortic regurgitation in women. Contrasting indications<br />
and outcomes compared with men. Circulation<br />
1996;94:2472–2478.<br />
27. Raman SV, Wooley CF. Tricuspid valvular regurgitation.<br />
Curr Treat Options Cardiovasc Med 2001;3:37–43.<br />
28. Zabalgoitia M. Echocardiographic recognition and quantitation<br />
of prosthetic valve dysfunction. In: Otto CM (ed).<br />
The Practice of Clinical Echocardiography. Philadelphia:<br />
Saunders, 2002:525–550.<br />
29. Schiller NB. Clinical decision making in endocarditis. In:<br />
Otto CM (ed). The Practice of Clinical Echocardiography.<br />
Philadelphia: Saunders, 2002:451–468.<br />
30. Ryan EW, Bolger AF. Transesophageal echocardiography<br />
in the evaluation of infective endocarditis. Cardiol Clin<br />
2000;18:773–787.<br />
31. Foster E, Tseng ZH. Echocardiography in the coronary<br />
care unit. In: Otto CM (ed). The Practice of Clinical<br />
Echocardiography. Philadelphia: Saunders, 2002:251–274.<br />
32. Erbel R, Alfonso F, Boileau C, et al. Diagnosis and management<br />
of aortic dissection. Eur Heart J 2001;22:1642–1681.<br />
33. Sabatine MS. Pocket Medicine. Philadelphia: Lippincott<br />
Williams and Wilkins, 2000:31.<br />
34. Nienaber CA, von Kodolitsch Y, Nicolas V, et al. The diagnosis<br />
of thoracic aortic dissection by noninvasive imaging<br />
procedures. N Engl J Med 1993;328:1–9.<br />
35. Munt BI, Kinnaird T, Thompson CR. Pericardial disease.<br />
In: Otto CM (ed). The Practice of Clinical<br />
Echocardiography. Philadelphia: Saunders, 2002:639–657.<br />
36. Hoit BD. Management of effusive and constrictive pericardial<br />
heart disease. Circulation 2002;105:2939–2942.<br />
37. Goldman JH, Foster E. Transesophageal echocardiographic<br />
(TEE) evaluation of intracardiac and pericardial<br />
masses. Cardiol Clin 2000;18:849–860.<br />
38. Wintersperger BJ, Becker CR, Gulbins H, et al. Tumors of<br />
the cardiac valves: Imaging findings in magnetic resonance<br />
imaging, electron beam computed tomography, and<br />
echocardiography. Eur Radiol 2000;10:443–449.
MHBD054-CH49[943-968].qxd 11/10/06 12:00 Page 968 p-mac292 27A:MHBD054:Chapters:CH-49: TechBooks