Forslag til vedtak - NRR
Forslag til vedtak - NRR
Forslag til vedtak - NRR
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
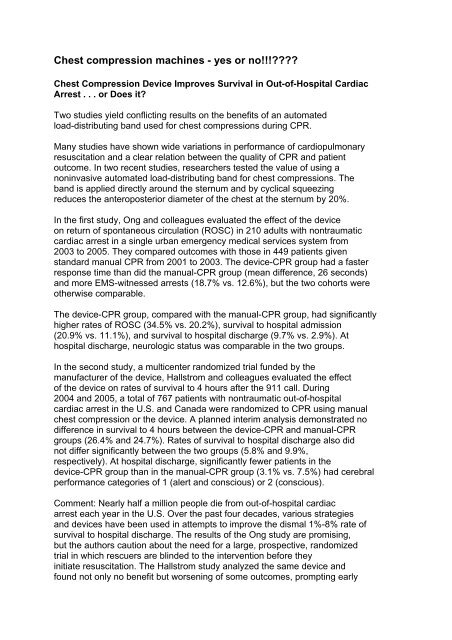
Chest compression machines - yes or no!!!<br />
Chest Compression Device Improves Survival in Out-of-Hospital Cardiac<br />
Arrest . . . or Does it<br />
Two studies yield conflicting results on the benefits of an automated<br />
load-distributing band used for chest compressions during CPR.<br />
Many studies have shown wide variations in performance of cardiopulmonary<br />
resuscitation and a clear relation between the quality of CPR and patient<br />
outcome. In two recent studies, researchers tested the value of using a<br />
noninvasive automated load-distributing band for chest compressions. The<br />
band is applied directly around the sternum and by cyclical squeezing<br />
reduces the anteroposterior diameter of the chest at the sternum by 20%.<br />
In the first study, Ong and colleagues evaluated the effect of the device<br />
on return of spontaneous circulation (ROSC) in 210 adults with nontraumatic<br />
cardiac arrest in a single urban emergency medical services system from<br />
2003 to 2005. They compared outcomes with those in 449 patients given<br />
standard manual CPR from 2001 to 2003. The device-CPR group had a faster<br />
response time than did the manual-CPR group (mean difference, 26 seconds)<br />
and more EMS-witnessed arrests (18.7% vs. 12.6%), but the two cohorts were<br />
otherwise comparable.<br />
The device-CPR group, compared with the manual-CPR group, had significantly<br />
higher rates of ROSC (34.5% vs. 20.2%), survival to hospital admission<br />
(20.9% vs. 11.1%), and survival to hospital discharge (9.7% vs. 2.9%). At<br />
hospital discharge, neurologic status was comparable in the two groups.<br />
In the second study, a multicenter randomized trial funded by the<br />
manufacturer of the device, Hallstrom and colleagues evaluated the effect<br />
of the device on rates of survival to 4 hours after the 911 call. During<br />
2004 and 2005, a total of 767 patients with nontraumatic out-of-hospital<br />
cardiac arrest in the U.S. and Canada were randomized to CPR using manual<br />
chest compression or the device. A planned interim analysis demonstrated no<br />
difference in survival to 4 hours between the device-CPR and manual-CPR<br />
groups (26.4% and 24.7%). Rates of survival to hospital discharge also did<br />
not differ significantly between the two groups (5.8% and 9.9%,<br />
respectively). At hospital discharge, significantly fewer patients in the<br />
device-CPR group than in the manual-CPR group (3.1% vs. 7.5%) had cerebral<br />
performance categories of 1 (alert and conscious) or 2 (conscious).<br />
Comment: Nearly half a million people die from out-of-hospital cardiac<br />
arrest each year in the U.S. Over the past four decades, various strategies<br />
and devices have been used in attempts to improve the dismal 1%-8% rate of<br />
survival to hospital discharge. The results of the Ong study are promising,<br />
but the authors caution about the need for a large, prospective, randomized<br />
trial in which rescuers are blinded to the intervention before they<br />
initiate resuscitation. The Hallstrom study analyzed the same device and<br />
found not only no benefit but worsening of some outcomes, prompting early
termination of the trial. Editorialists suggest that the trials'<br />
contradictory results might result from differences in patient selection,<br />
presenting rhythm, time from cardiac arrest to initial CPR, and time to<br />
deployment of the device.<br />
Of note, the manufacturer has promoted the device based in part on the<br />
results obtained in the Ong study. To prevent the cart-before-the-horse<br />
sagas of military antishock trousers and of methylprednisolone for blunt<br />
spinal cord injury, this device's efficacy, or lack thereof, must be<br />
established according to the highest scientific standards. Un<strong>til</strong> that time,<br />
enthusiasm for the device should be tempered.<br />
-- John A. Marx, MD, FAAEM, FACEP<br />
Citation(s): Ong MH et al. Use of an automated, load-distributing band<br />
chest compression device for out-of-hospital cardiac arrest resuscitation.<br />
JAMA 2006 Jun 14; 295:2629-37.<br />
Hallstrom A et al. Manual chest compression vs use of an automated chest<br />
compression device during resuscitation following out-of-hospital cardiac<br />
arrest: A randomized trial. JAMA 2006 Jun 14; 295:2620-8.<br />
Lewis RJ and Niemann JT. Manual vs device-assisted CPR: Reconciling<br />
apparently contradictory results. JAMA 2006 Jun 14; 295:2661-4.<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .