Orbital unifocal Langerhans cell histiocytosis (eosinophilic granuloma)
Orbital unifocal Langerhans cell histiocytosis (eosinophilic granuloma)
Orbital unifocal Langerhans cell histiocytosis (eosinophilic granuloma)
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Case Review<br />
<strong>Orbital</strong> <strong>unifocal</strong> <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong><br />
(<strong>eosinophilic</strong> <strong>granuloma</strong>)<br />
Yahya Al-Muazen 1 , Mohamed El-Shawarby 2 , Saleh Al-Sowayan 2<br />
Abstract: <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong> (LCH) is a clinical entity characterized by abnormal proliferation of<br />
<strong>Langerhans</strong> <strong>cell</strong>s that probably results from an immunoregulatory defect which can be triggered by several different<br />
factors. <strong>Orbital</strong> involvement by LCH most often represents <strong>unifocal</strong> disease (<strong>eosinophilic</strong> <strong>granuloma</strong>). The condition<br />
is uncommon and descriptions of <strong>eosinophilic</strong> <strong>granuloma</strong> of the orbit generally have been limited to single case<br />
reports or small case series. A case of orbital <strong>eosinophilic</strong> <strong>granuloma</strong> is reported, followed by a discussion<br />
encompassing a literature review. (p66-69)<br />
Introduction<br />
<strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong> (LCH), previously termed<br />
‘<strong>histiocytosis</strong> X’, is a clinical entity characterized by abnormal<br />
proliferation of <strong>Langerhans</strong> <strong>cell</strong>s, which exert a mass<br />
effect. The disease primarily involves bones but can also<br />
affect other organ systems. <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong> is<br />
actually a term that encompasses three related disease<br />
subtypes: acute disseminated LCH (Letterer-Siwe disease),<br />
multifocal LCH (Hand-Schuller-Christian syndrome) and<br />
<strong>unifocal</strong> LCH (also known as <strong>eosinophilic</strong> <strong>granuloma</strong>,<br />
which represents about 70% of cases of LCH). 1<br />
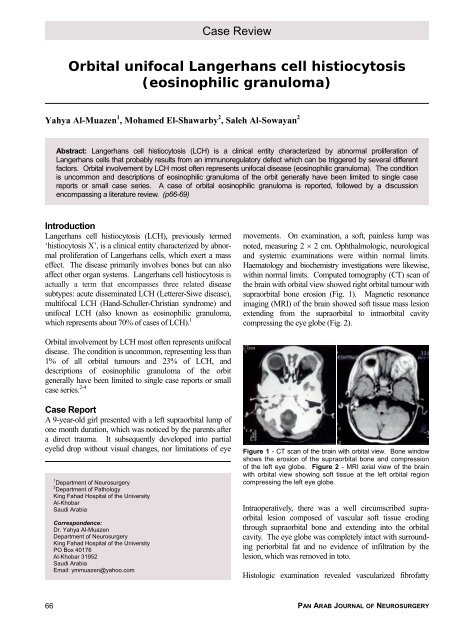
movements. On examination, a soft, painless lump was<br />
noted, measuring 2 × 2 cm. Ophthalmologic, neurological<br />
and systemic examinations were within normal limits.<br />
Haematology and biochemistry investigations were likewise,<br />
within normal limits. Computed tomography (CT) scan of<br />
the brain with orbital view showed right orbital tumour with<br />
supraorbital bone erosion (Fig. 1). Magnetic resonance<br />
imaging (MRI) of the brain showed soft tissue mass lesion<br />
extending from the supraorbital to intraorbital cavity<br />
compressing the eye globe (Fig. 2).<br />
<strong>Orbital</strong> involvement by LCH most often represents <strong>unifocal</strong><br />
disease. The condition is uncommon, representing less than<br />
1% of all orbital tumours and 23% of LCH, and<br />
descriptions of <strong>eosinophilic</strong> <strong>granuloma</strong> of the orbit<br />
generally have been limited to single case reports or small<br />
case series. 2-4<br />
Case Report<br />
A 9-year-old girl presented with a left supraorbital lump of<br />
one month duration, which was noticed by the parents after<br />
a direct trauma. It subsequently developed into partial<br />
eyelid drop without visual changes, nor limitations of eye<br />
1 Department of Neurosurgery<br />
2 Department of Pathology<br />
King Fahad Hospital of the University<br />
Al-Khobar<br />
Saudi Arabia<br />
Correspondence:<br />
Dr. Yahya Al-Muazen<br />
Department of Neurosurgery<br />
King Fahad Hospital of the University<br />
PO Box 40176<br />
Al-Khobar 31952<br />
Saudi Arabia<br />
Email: ymmuazen@yahoo.com<br />
Figure 1 - CT scan of the brain with orbital view. Bone window<br />
shows the erosion of the supraorbital bone and compression<br />
of the left eye globe. Figure 2 - MRI axial view of the brain<br />
with orbital view showing soft tissue at the left orbital region<br />
compressing the left eye globe.<br />
Intraoperatively, there was a well circumscribed supraorbital<br />
lesion composed of vascular soft tissue eroding<br />
through supraorbital bone and extending into the orbital<br />
cavity. The eye globe was completely intact with surrounding<br />
periorbital fat and no evidence of infiltration by the<br />
lesion, which was removed in toto.<br />
Histologic examination revealed vascularized fibrofatty<br />
66 PAN ARAB JOURNAL OF NEUROSURGERY
ORBITAL UNIFOCAL LANGERHANS CELL HISTIOCYTOSIS • Muazen, et al<br />
tissue with variable infiltration by an eosinophil rich<br />
inflammatory <strong>cell</strong> infiltrate that also included mature<br />
lymphocytes and aggregates of histiocytic <strong>cell</strong>s with indented<br />
nuclei and abundant cytoplasm, that showed strong<br />
cytoplasmic and nuclear immunoreactivity for S-100<br />
protein. There were also few scattered multinucleate giant<br />
<strong>cell</strong>s exhibiting the same nuclear and immunohistochemical<br />
features. There was no nuclear pleomorphism and mitoses<br />
could not be demonstrated (Figs. 3 - 7).<br />
One year postoperatively, MRI was done and showed no<br />
recurrence of lesion (Fig. 8).<br />
Figure 3 - Eosinophilic <strong>granuloma</strong>: note numerous eosinophils, histiocytes and lymphocytes (HE × 200). Figure 4 - Eosinophilic<br />
<strong>granuloma</strong>: note aggregates of histiocytes (HE × 100).<br />
Figure 5 - Eosinophilic <strong>granuloma</strong>: note histiocytes with abundant cytoplasm and indented nuclei (consistent with <strong>Langerhans</strong><br />
<strong>cell</strong>s). There is also a multinucleate giant <strong>cell</strong> and few eosinophils (HE × 400). Figure 6 - Eosinophilic <strong>granuloma</strong>: note positive<br />
nuclear and cytoplasmic staining of histiocytes for S-100 protein. Immunohistochemistry × 200.<br />
Figure 7 - Eosinophilic <strong>granuloma</strong>: note positive nuclear and cytoplasmic staining of histiocytes for S-100 protein. Immunohistochemistry<br />
× 400. Figure 8 - Postoperative MRI axial view of the brain with orbital, after 1 year showing no evidence of<br />
recurrence.<br />
VOLUME 13, NO. 2, OCTOBER 2009<br />
67
ORBITAL UNIFOCAL LANGERHANS CELL HISTIOCYTOSIS • Muazen, et al<br />
Discussion<br />
Normal <strong>Langerhans</strong> <strong>cell</strong>s begin as pleuripotential stem <strong>cell</strong>s<br />
in active bone marrow. 11,17 Under the influence of multiple<br />
cytokines, those stem <strong>cell</strong>s differentiate into two major<br />
classes of histiocyte: antigen-processing macrophages and<br />
antigen-presenting dendritic <strong>cell</strong>s. Cytokines further induce<br />
dendritic <strong>cell</strong>s to diverge along multiple phenotypic paths,<br />
with one leading to the <strong>Langerhans</strong> <strong>cell</strong>. The normal bone<br />
marrow does not retain a large permanent population of<br />
<strong>Langerhans</strong> <strong>cell</strong>s 2 . Following migration to the epidermis,<br />
oral mucosa, lungs and other sites, the <strong>cell</strong>s participate in<br />
immunosurveillance by engaging extrinsic antigens. 17<br />
<strong>Langerhans</strong> <strong>cell</strong>-antigen complexes then travel via<br />
lymphatics to regional lymph nodes, where the antigens are<br />
presented to paracortical T-<strong>cell</strong>s. The primary agent or<br />
event that disrupts this orderly process and causes an<br />
accumulation of pathologic <strong>Langerhans</strong> <strong>cell</strong>s is unknown<br />
but an immunoregulatory defect has been postulated that<br />
can be triggered by several different factors, such as a viral<br />
infection, a genetic defect, lymphoma or leukaemia. 21<br />
<strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong> has a predilection for haemopoietically<br />
active bone marrow (the residence of <strong>Langerhans</strong><br />
<strong>cell</strong> precursors) and skeletal lesions are present in the<br />
majority of isolated and multisystem cases. 9,17<br />
<strong>Orbital</strong> involvement by LCH most often represents <strong>unifocal</strong><br />
disease (i.e. an <strong>eosinophilic</strong> <strong>granuloma</strong>). Patients with<br />
orbital <strong>eosinophilic</strong> <strong>granuloma</strong> tend to be males in their first<br />
or second decade. Symptoms include swelling, upper<br />
eyelid oedema and erythema, ptosis, rapidly progressive<br />
proptosis, brow pain, and tenderness. 5,8,16,18 This patient, a<br />
9-year-old female, presented with a supraorbital lump that<br />
subsequently developed into partial eyelid drop. A destructive<br />
bone lesion is commonly seen in the superior or<br />
superotemporal orbit as was present in this patient. 4 A soft<br />
tissue mass with irregular but clearly demarcated bone<br />
destruction is thought to be a characteristic CT finding of<br />
LCH involving the orbit. 20<br />
The clinical differential diagnosis of LCH includes<br />
metastatic tumours (e.g. Ewing’s sarcoma, neuroblastoma<br />
and Wilms’ tumour), lacrimal gland neoplasms (e.g. mixed<br />
tumour, adenoid cystic carcinoma and mucoepidermoid<br />
carcinoma), primary bone tumours (e.g. giant <strong>cell</strong> reparative<br />
<strong>granuloma</strong>, aneurysmal bone cyst and brown tumour of<br />
hyperparathyroidism), lymphoma, haemangioma, cholesteatoma,<br />
granulocytic sarcoma, inflammatory pseudotumour<br />
and dacryoadenitis. 1,6,7,12 Considering the patient’s<br />
age, the presence of bone destruction and the location of the<br />
lesion, the initial clinical impression in our case was a<br />
rhabdomyosarcoma.<br />
Tissue biopsy is necessary for the diagnosis of LCH and to<br />
rule out more aggressive lesions in the differential<br />
diagnosis. Histologically, LCH lesions show sheets of large<br />
histiocytes with grooved nuclei that exhibit immunoreactivity<br />
for CD1a and S-100 protein (<strong>Langerhans</strong> <strong>cell</strong>s),<br />
interspersed with multinucleate giant <strong>cell</strong>s, eosinophils,<br />
lymphocytes and plasma <strong>cell</strong>s. Electron microscopy<br />
reveals characteristic intracytoplasmic inclusions known as<br />
Birbeck granules in the <strong>Langerhans</strong> <strong>cell</strong>s. 3,10 Although<br />
electron microscopy was not performed in our case,<br />
characteristic histologic findings and S-100 protein positivity,<br />
supported by clinical features and the presence of<br />
bone erosion on CT were considered adequate for the<br />
diagnosis of LCH. In an appropriate clinicoradiologic<br />
setting, a typical cytopathology can alone be used for<br />
effective diagnosis. 13 Absence of multifocal and multiple<br />
system involvement ruled out Hand-Schuller-Christian<br />
syndrome and Lettere-Siwe disease, respectively.<br />
The outcome for LCH patients without multisystem<br />
involvement or organ dysfunction is usually very good. 5<br />
There are no definitive recommendations on how to best<br />
manage a case of orbital <strong>eosinophilic</strong> <strong>granuloma</strong>. No<br />
modality has been proven to be more effective than the<br />
other but lesions generally resolve after minimal intervention,<br />
with a good prognosis. 1 Complete surgical removal of the<br />
lesion is not even necessary. There are many reports of<br />
complete resolution of an orbital <strong>eosinophilic</strong> <strong>granuloma</strong><br />
after biopsy and subtotal curettage alone. 14 Even lesions<br />
with significant bone destruction and soft tissue involvement<br />
respond to this minimal intervention. 5 In these cases,<br />
it is unclear if the biopsy and curettage had a therapeutic<br />
impact or if the lesions would have spontaneously resolved<br />
without any intervention at all. The response to observation<br />
alone is not clear however, since almost all patients are<br />
diagnosed through tissue biopsy. 5 In the present case, an<br />
MRI performed one year after surgical excision of the<br />
lesion showed no evidence of recurrence.<br />
Successful interventions have also been reported with the<br />
use of low-dose radiation and intralesional corticosteroids.<br />
Chemotherapy is considered for recurrent disease. 19<br />
References<br />
1. Allen RC, Nerad JA: The little boy with an allergy that wouldn’t<br />
go away. Eyenet (Morning Rounds) 2005, 9(6): 41-42<br />
2. Chu T, Jaffe R: The normal <strong>Langerhans</strong> <strong>cell</strong> and the LCH <strong>cell</strong>.<br />
Br J Cancer 1994, 70(Suppl 23): S4-S10<br />
3. Favara BE, Feller AC, Pauli M, et al: Contemporary<br />
classification of histiocytic disorders. The WHO Committee On<br />
Histiocytic/Reticulum Cell Proliferations. Reclassification<br />
Working Group of the Histiocyte Society. Med Pediatr Oncol<br />
1997, 29: 157-66<br />
4. Furuta S, Sakaki S, Hatakeyama T, Kumon Y, Nakamura K:<br />
Paediatric orbital <strong>eosinophilic</strong> <strong>granuloma</strong> with intra and extra<br />
cranial extension – case report. Neurol Med Chir (Tokyo)<br />
1991, 31: 590-592<br />
68<br />
PAN ARAB JOURNAL OF NEUROSURGERY
ORBITAL UNIFOCAL LANGERHANS CELL HISTIOCYTOSIS • Muazen, et al<br />
5. Harris GJ, Woo KI: Eosinophilic <strong>granuloma</strong> of the orbit: A<br />
paradox of aggressive destruction responsive to minimal<br />
intervention. Trans Am Ophthalmol Soc 2003, 101: 93-106<br />
6. Harris GJ, Schweisow TK: Acute proptosis in childhood. In:<br />
Tasman W, Jaeger EA (eds), Clinical Ophthalmology, Vol 2.<br />
Philadelphia, Lippincott Williams & Wilkins 2001, pp 1-26<br />
7. Jakobiec FA, Trokel SL, Aron-Rose D: Localized <strong>eosinophilic</strong><br />
<strong>granuloma</strong> (<strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong>) of the orbital frontal<br />
bone. Arch Ophthalmol 1980, 98: 1814-1820<br />
8. Kramer TR, Noecker RJ, Miller JM, Clark LC: <strong>Langerhans</strong> <strong>cell</strong><br />
<strong>histiocytosis</strong> with orbital involvement. Am J Ophthalmol 1997,<br />
124: 814-824<br />
9. McLelland J, Pritchard J, Chu AC: Current controversies.<br />
Hematol Oncol Clin North Am 1987, 1: 147-162<br />
10. Michael PG, David FC, John PD: <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong>:<br />
clinical presentation, pathogenesis and treatment. Univ Pennsylvania<br />
Orthop J 2002, 15: 67-73<br />
11. Nezelof C, Basset F: <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong> research:<br />
past, present, and future. Hematol Oncol Clin North Am 1998,<br />
12: 385-405<br />
12. Parke DW, Font RL, Boniuk M, et al: Cholesteatoma of the<br />
orbit. Arch Ophthalmol 1982, 100: 612-616<br />
13. Pohar-Marinsek Z, Us-Krasovec M: Cytology of <strong>Langerhans</strong><br />
<strong>cell</strong> <strong>histiocytosis</strong>. Acta Cytol 1996, 40: 1257-64<br />
14. Rajendram R, Rose G, Luthert P, et al: Biopsy-confirmed<br />
spontaneous resolution of orbital <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong>.<br />
Orbit 2005, 24(1): 39-41<br />
15. Shetty SB, Mehta C: <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong> of the orbit.<br />
Indian J Ophthalmol 2001, 49(4): 267-8<br />
16. Nag SS, Singh M, Nag D, et al: A case report of <strong>unifocal</strong><br />
<strong>Langerhans</strong>’ <strong>cell</strong> <strong>histiocytosis</strong> or <strong>eosinophilic</strong> <strong>granuloma</strong>. J<br />
Indian Med Assoc 2007, 105: 218-20<br />
17. Schmitz L, Favara BE: Nosology and pathology of <strong>Langerhans</strong><br />
<strong>cell</strong> <strong>histiocytosis</strong>. Hematol Oncol Clin North Am 1998, 12: 221-<br />
246<br />
18. Smith JH, Fulton L, O’Brien JM: Spontaneous regression of<br />
orbital <strong>Langerhans</strong> <strong>cell</strong> <strong>granuloma</strong>tosis in a three year old girl.<br />
Am J Ophthalmol 1999, 128: 119-121<br />
19. Song A, Johnson TE, Dubovy SR, et al. Treatment of recurrent<br />
<strong>eosinophilic</strong> <strong>granuloma</strong> with systemic therapy. Ophthalmic<br />
Plast Reconstr Surg 2003, 19: 140-144<br />
20. Yi G, Yoon HK, Han BK, Kim KA, Choo IW: CT Findings of<br />
orbital <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong>. J Korean Radiol Soc<br />
2000, 42(5): 841-846<br />
21. Zegler B: <strong>Langerhans</strong> <strong>cell</strong> <strong>histiocytosis</strong>: a reactive or neoplastic<br />
disorder Med Pediatr Oncol 2001, 37: 543-544<br />
VOLUME 13, NO. 2, OCTOBER 2009<br />
69