Improvements in OR Performance and Efficiency Performance and ...
Improvements in OR Performance and Efficiency Performance and ...
Improvements in OR Performance and Efficiency Performance and ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
1<br />
<strong>Improvements</strong> <strong>in</strong> <strong>OR</strong><br />
<strong>Performance</strong> <strong>and</strong> <strong>Efficiency</strong><br />
American Academy of Ophthalmology 2010<br />
Course #289<br />
Chicago<br />
Faculty<br />
Richard J. Ruckman, MD – Lufk<strong>in</strong>,TX<br />
Preoperative Protocols<br />
R. Bruce Wallace, III, MD – Alex<strong>and</strong>ria, LA<br />
Operative Protocols<br />
Larry E. Patterson, MD – Crossville, TN<br />
Postoperative Protocols<br />
R. Bruce Wallace, III, MD, FACS<br />
Alex<strong>and</strong>ria, Louisiana<br />
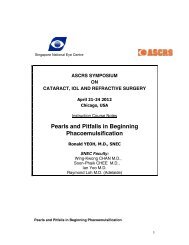
Chang<strong>in</strong>g Demographics:<br />
Grow<strong>in</strong>g Population for Cataract <strong>and</strong><br />
RLE Surgery<br />
80<br />
70 55 to 74 years<br />
Cl<strong>in</strong>ical Professor of Ophthalmology,<br />
Louisiana State University<br />
Assistant Cl<strong>in</strong>ical Professor of<br />
Ophthalmology, Tulane University<br />
Consultant for AMO, Allergan, B+L, LenSAR<br />
Population (millions)<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
1995 2000 2010 2030<br />
Preoperative Protocols<br />
No f<strong>in</strong>ancial <strong>in</strong>terest <strong>in</strong> products discussed.<br />
Richard J. Ruckman, M.D.<br />
Lufk<strong>in</strong>, , TX<br />
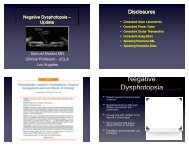
Cataract Surgery<br />
<strong>in</strong> the Ambulatory Sett<strong>in</strong>g<br />
• The Past, Present <strong>and</strong> Future<br />
• 3.1 million cataract surgeries <strong>in</strong> 2008<br />
• 75% performed <strong>in</strong> ASC’s<br />
• Presbyopia correct<strong>in</strong>g lens 6.2%,<br />
down from 7%<br />
• Refractive lens exchange 2.3% of<br />
lens extractions<br />
• Expected to grow 6-15% by 2015<br />
Market Scope, Sept. 25, 2009
2<br />
What are the Challenges<br />
to Your ASC<br />
• Healthcare Reform<br />
• ASC’s will not go away: “quality, low<br />
cost providers”<br />
• Payments<br />
• Overall 0.6% <strong>in</strong>crease to ASC’s<br />
• Cataract 66982/66984, 3%<br />
• Ret<strong>in</strong>a <strong>and</strong> glaucoma up<br />
TOA Newsletter, Oct. 2009<br />
Fed. Register, July 20, 2009<br />
Surgistrategies, Sept. 09, Vol. 8,<br />
#9<br />
• Increased ASC costs – <strong>in</strong>fection<br />
#10<br />
Oct. 09, Vol. 8,<br />
What are the Challenges<br />
to Your ASC<br />
• Static reimbursements<br />
• High cost of technology <strong>in</strong> both equipment <strong>and</strong><br />
supplies<br />
• Increas<strong>in</strong>g overhead costs<br />
• Necessity of certification <strong>and</strong> its associated costs<br />
• Need for highly tra<strong>in</strong>ed staff<br />
Improved efficiency is not a matter of choice;<br />
it is a matter of survival.<br />
What are the Challenges to the Success<br />
of Your ASC<br />
• Static reimbursements<br />
• High cost of technology <strong>in</strong> both equipment<br />
<strong>and</strong> supplies<br />
• Increas<strong>in</strong>g overhead costs<br />
• Recent <strong>in</strong>creased CMS scrut<strong>in</strong>y<br />
• Necessity of certification <strong>and</strong> its associated<br />
costs<br />
• Need for highly tra<strong>in</strong>ed staff<br />
Improved efficiency is not a matter of choice,<br />
it is a matter of survival.<br />
The Importance of <strong>Efficiency</strong><br />
Where does the Money Go<br />
• ASC expense*<br />
• Salaries 43%<br />
• Overhead 33%<br />
• Supplies 23%<br />
The majority of expense is time dependent.<br />
You cannot control reimbursement, but you<br />
can <strong>in</strong>fluence your costs through<br />
efficiency of time.<br />
* Multi specialty ASC<br />
Federated Ambulatory Surgery Association, 1996<br />
The Importance of<br />
F<strong>in</strong>ancial Benchmark<strong>in</strong>g<br />
Successful ambulatory surgery<br />
centers are diligent <strong>in</strong> gather<strong>in</strong>g,<br />
measur<strong>in</strong>g, <strong>and</strong> manag<strong>in</strong>g data. .<br />
Management Ratio Examples<br />
Payroll/Gross Income 15-20%<br />
Net <strong>in</strong>come 20-40%<br />
Man hours per case 9-12 hrs per<br />
case<br />
Bruce S. Maller, The ABC’s of<br />
ASC’s ASOA 2004<br />
The Importance of Benchmark<strong>in</strong>g<br />
Compare Yourself to National Norms<br />
• Accreditation Association For Ambulatory Health Care<br />
(AAAHC)<br />
• <strong>Performance</strong> Measurement Initiative (PMI)<br />
• Institute for Quality Improvement<br />
Cataract extraction with lens <strong>in</strong>sertion 2008<br />
77 organizations<br />
64 to 12,000 Procedures<br />
Total 143,491 Sample size<br />
71% Free st<strong>and</strong><strong>in</strong>g s<strong>in</strong>gle specialty<br />
22% Multi-specialty<br />
.07% Office based surgery practices<br />
AAAHC – 2009
3<br />
Practice Comparison - PMI<br />
• 65% S<strong>in</strong>gle specialty<br />
• 24% Multispecialty<br />
• 11% Other<br />
Annual volume 70-8,000<br />
Practice Comparison - PMI<br />
Pre-Procedure Procedure Time<br />
Time patient checks <strong>in</strong>to facility to time <strong>in</strong> O.R.<br />
Median 76 m<strong>in</strong>utes<br />
Range 37-138 m<strong>in</strong>utes<br />
Best case<br />
• Paperwork completed when schedul<strong>in</strong>g patient<br />
• Patient is sent home with a packet, vision function<br />
questionnaire, pre-surgery <strong>in</strong>structions<br />
• Compounded dilat<strong>in</strong>g drops are begun <strong>in</strong> “dress<strong>in</strong>g<br />
room”<br />
• Rout<strong>in</strong>e cases early <strong>in</strong> day<br />
AAAHC -<br />
2008<br />
AAAHC - 2009<br />
Practice Comparison - PMI Procedure<br />
Times<br />
• Time from start of procedure to end<br />
• Median 15 m<strong>in</strong>utes<br />
• Range 7-33 m<strong>in</strong>utes<br />
• “Best case”<br />
• 3 autoclaves <strong>and</strong> 2 O.R.’s<br />
• Streaml<strong>in</strong>ed paperwork<br />
• Specific O.R. staff<br />
• Second O.R. ready by time surgeon arrives<br />
• M<strong>in</strong>imal <strong>in</strong>struments<br />
• “Practic<strong>in</strong>g” with patients while they are drap<strong>in</strong>g<br />
• Scrubs/circulators “never” leave room<br />
Practice Comparison - PMI Discharge<br />
Time<br />
• Out of operat<strong>in</strong>g room to discharge<br />
• Median 23 m<strong>in</strong>utes<br />
• Range 3-41 m<strong>in</strong>utes<br />
• “Best case”<br />
• M<strong>in</strong>imal sedation<br />
• Rout<strong>in</strong>e post-op op orders<br />
• Teach<strong>in</strong>g patients <strong>in</strong> pre-operative phase<br />
to expedite discharge<br />
• Patient stays on stretcher with monitor<br />
• Give post-op op kits at pre-op visit<br />
AAAHC -<br />
2008<br />
AAAHC - 2008<br />
Practice Comparison - PMI<br />
Facility Time<br />
• Time patient checks <strong>in</strong> to discharge<br />
• Median 121 m<strong>in</strong>utes<br />
• Range 62-189 m<strong>in</strong>utes<br />
• “Top performance may be attributed<br />
to the reasons for each component<br />
with streaml<strong>in</strong><strong>in</strong>g the procedure<br />
process.”<br />
Does Size Matter:<br />
“How Does Your<br />
Cataract Service Compare”<br />
Facility Size<br />
Check <strong>in</strong><br />
to Check out<br />
Surgery<br />
Time<br />
2000-4000 sq. ft. 104.31 m<strong>in</strong>. 17.8 m<strong>in</strong>.<br />
4500-6500 sq. ft. 104.76 m<strong>in</strong>. 14.62 m<strong>in</strong>.<br />
7000+ sq. ft. 94.75 m<strong>in</strong>. 14.35 m<strong>in</strong>.<br />
AAAHC - 2008<br />
Outpatient Surgery Magaz<strong>in</strong>e, October<br />
2007
4<br />
Pre-Operative Protocols<br />
Pre-Operative Protocols<br />
• <strong>Efficiency</strong> beg<strong>in</strong>s at <strong>in</strong>itial exam <strong>and</strong><br />
schedul<strong>in</strong>g of procedure<br />
• Exam (patient education beg<strong>in</strong>s at this<br />
time)<br />
• F<strong>in</strong>ancial/Insurance<br />
• Pre-op<br />
• Entire “blank” chart available<br />
• Check boxes on all forms<br />
• Kits, Rx’s, <strong>and</strong> prepr<strong>in</strong>ted, color-coded coded<br />
pre-op<br />
<strong>and</strong> post-op op <strong>in</strong>struction sheets<br />
are given<br />
• Pre-op<br />
• Plan the day – summary sheet<br />
•List eye, IOL, special<br />
procedures<br />
•Use patients ID sticker<br />
•Post <strong>in</strong> all areas of O.R.<br />
•Charge nurse keeps master<br />
copy<br />
Pre-Operative Protocols<br />
Pre-Operative Protocols<br />
• Patient flow<br />
• ID attached to patient cloth<strong>in</strong>g<br />
• 1 st set of dilat<strong>in</strong>g drops <strong>in</strong>stilled<br />
~ we use compounded dilat<strong>in</strong>g<br />
drops<br />
• To pre-op via patient bathroom<br />
• Patient does not change clothes<br />
• Patient flow<br />
• Patient placed on stretcher<br />
• Monitor is attached with limb<br />
leads<br />
• Sal<strong>in</strong>e lock for medications on<br />
all patients<br />
• Basel<strong>in</strong>e vital signs taken by<br />
RN<br />
Pre-Operative Protocols<br />
• Patient flow<br />
• Patient identification sheet<br />
on stretcher with name,<br />
operative eye, allergies<br />
• Physician marks site<br />
• Patient transferred <strong>in</strong>to O.R.<br />
on same stretcher with<br />
monitors already <strong>in</strong> place<br />
Anesthesia Choices<br />
• IV Sedation<br />
• 1-2 mg Versed <strong>in</strong> pre-op<br />
• Occasionally Fentanyl <strong>in</strong> O.R.<br />
• Topical<br />
• Tetraca<strong>in</strong>e (TetraVisc)*<br />
• Intracameral<br />
• Lidoca<strong>in</strong>e 1% MPF<br />
* OCuSOFT
5<br />
Cataract Anesthesia Survey<br />
Primary Anesthetic Technique<br />
80<br />
60<br />
40<br />
20<br />
0<br />
2000 2002 2004 2006 2008<br />
RB<br />
Periocular<br />
Topical<br />
Blunt cannula subtenons<br />
• Between 1995 <strong>and</strong> 2000 topical anesthesia went from<br />
11% to 50%<br />
• Of those us<strong>in</strong>g topical anesthesia for cataract<br />
surgery 76% use it with <strong>in</strong>tracameral lidoca<strong>in</strong>e<br />
Number<br />
of Cases<br />
900<br />
800<br />
700<br />
600<br />
500<br />
400<br />
300<br />
200<br />
100<br />
0<br />
IV + Topical<br />
IV + Peribulbar<br />
IV<br />
IV + Retrobulbar<br />
Topical + Oral<br />
Peribulbar<br />
AAAHC 2009<br />
Practice Styles <strong>and</strong> Preferences of U.S. ASCRS Members – 2008 Survey<br />
David Leam<strong>in</strong>g, M.D., ASCRS – 2009 Posters on Dem<strong>and</strong><br />
Anesthesia Options<br />
• Topical<br />
• Eye drops (TetraVisc*) or<br />
lidoca<strong>in</strong>e gel<br />
• Gives good conjunctival<br />
anesthesia<br />
• No lid ak<strong>in</strong>esia<br />
• Eye movement present<br />
• Deep eye pa<strong>in</strong> present<br />
* Ocusoft<br />
Regional Anesthesia<br />
• How to decide when more is needed<br />
• Problems with A-scan<br />
• Alzheimer’s/Mental retardation<br />
• Hard of hear<strong>in</strong>g/Language barrier<br />
• Lack of cooperation dur<strong>in</strong>g first eye<br />
• Younger age<br />
• Significant prescription drug history<br />
• Physical problems – “bad back”<br />
• Rout<strong>in</strong>e second eyes – may need<br />
Mov<strong>in</strong>g the Patient<br />
to the O.R.<br />
• Communication is the key<br />
• RN to RN h<strong>and</strong>off<br />
• Direct observation by staff<br />
• Signals – lights go on <strong>in</strong> O.R.<br />
• Video monitor<strong>in</strong>g