Generic Concept Note - Chittorgarh
Generic Concept Note - Chittorgarh
Generic Concept Note - Chittorgarh
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
INDEX<br />
A. Problem Statement 3-4<br />
B. Pharma Scenario in India - Poverty Amidst Plenty 5-13<br />
& How doctors are used as an instrument<br />
1. Prescription by brand name<br />
2. Prescription of non essential drugs<br />
3. Irrational Prescriptions<br />
C. Aggressive Drug Promotion 14-23<br />
1. Influencing Doctors<br />
2. Lack of objective drug information<br />
3. “False” evidence based medical practice<br />
4. Promotion of hazardous, banned and bannable drugs<br />
5. Doctors as Key Opinion Leaders<br />
6. Biased clinical trials<br />
7. Disease Mongering<br />
8. Direct to consumer advertising<br />
9. Influencing Government Policies<br />
D. Implications of unethical promotion 24-25<br />
E. The Solution 26-28<br />
1. Rational use of drugs – Prescription by generic name<br />
– Adoption of Essential Drug List<br />
– Use of standard treatment guidelines<br />
2. Availability of low cost drugs at govt. run medical shops<br />
F. <strong>Chittorgarh</strong> Model 29-31<br />
G. <strong>Concept</strong> <strong>Note</strong> on generic drugs 32-33<br />
H. Frequently Asked Questions 34-35<br />
Annexures<br />
Alphabetical List of 570 low cost generic medicines<br />
Comparative list of 300 low cost ethical drugs<br />
List of 54 IV fluids<br />
List of 142 surgical items<br />
Documentation by<br />
Dr. Samit Sharma<br />
Collector & District Magistrate<br />
<strong>Chittorgarh</strong> (Rajasthan)<br />
(This also contains excepts from "A Lay Person's Guide to Medicines" by S. Srinivasan)<br />
1
PROBLEM STATEMENT<br />
Huge gap in access to drugs<br />
TOP<br />
With a population of nearly 100 crores, India accounts for 16 per cent of the global<br />
population. Sizeable population lives below the poverty line and 48 per cent of the<br />
people are illiterate. India accounts for huge morbidity & mortality burden due to<br />
large number of deprived & extremely poor people. WHO says that 65% of the<br />
population still lacks regular access to essential medicines. With the rise in health<br />
care cost, over 23 % of the sick don’t seek treatment because they are not having<br />
enough money to spend. A study by World Bank shows that as a result of single<br />
hospitalization 30 % of people fall below poverty line. Over 40% of those<br />
hospitalized, need to borrow money or sell their assets.<br />
Healthcare costs are high and are increasing further. Expenditure on drugs<br />
constitutes about 50 % of the health care cost which increases up to 80 % in rural<br />
areas. (In fact expenditure on health care is the second most common cause for<br />
rural indebtedness in India)<br />
Where does the money for health expenditure (in India) come from<br />
Private out of pocket 79%<br />
expenditure<br />
State govt. 14%<br />
Central govt. 4%<br />
Private investment 3%<br />
Private insurance 0 – 1%<br />
India accounts for 22 per cent of the global illness with only 2 per cent of the global<br />
drug production of which only 0.7 per cent are essential drugs. Yet 1.3 per cent are<br />
non essential, profit-oriented formulations which are highly priced, irrational or<br />
useless. Crores of our people, living in abject poverty, can barely afford a square<br />
meal a day, can they afford to spend on costly medicines.<br />
People are being pushed further into poverty, disability and death because of these<br />
costs. Completely irrational drugs, which do nothing but waste people’s money, are<br />
widely sold. More and more drugs flood our markets every year. There are over<br />
20,000 pharmaceutical units in the country producing over 1,00,000 (one lakh)<br />
formulations of drugs. It is paradoxical that while essential and life-saving drugs<br />
are in short supply, more and more drugs which are not therapeutically more<br />
effective, irrational and may be even dangerous, are being produced and pushed in<br />
the market with absolute disregard to the country's health needs. The problem<br />
becomes more acute in developing countries where resources for the purchase of<br />
drugs are scarce.<br />
In the pharmaceuticals sector, the cost of manufacturing a drug is relatively low,<br />
compared to the price it is sold at. By selling drugs at inflated prices, big<br />
companies and retailers pocket a large share of the money paid out by the<br />
consumer. Retail prices of drugs show complete arbitrary variation between<br />
brands. There are abnormally high trade margins with wasteful, unregulated and<br />
unethical drug promotion. There is a nexus between drug companies, stockists,<br />
retailers, Medical Representatives (M.R.) & some medical practitioners which<br />
disproportionately inflates the cost of medicines & the overall treatment. Each<br />
2
gains down the line, the only loser being the poor patient for whom the drugs<br />
become unaffordable.<br />
TOP<br />
Issue of Research Cost Recovery<br />
The life cycle of a drug has four phases:<br />
1. Research<br />
2. Development<br />
3. Patentee commercialization<br />
4. <strong>Generic</strong> commercialization<br />
When the product is in the research mode, a research institution invents a new<br />
drug. Then a patent application is filed to preserve rights. When the institution<br />
starts pre-clinical and clinical testing of the drugs, the development phase begins.<br />
In the patentee commercialization phase, the innovator (patent holder) begins<br />
selling in at least one country. In this process, doctors, patients, hospitals, public<br />
health agencies and insurers get involved. <strong>Generic</strong> commercialization commences<br />
when the patent expires in any given country and generic companies start to sell<br />
the drug at lower prices. Intellectual property is a vital factor for discovery of new<br />
drugs.<br />
Without patents, research and development would be reduced. Without<br />
generics, access to medicine would be impaired. Thus, we have to strike a balance<br />
between encouraging research and development of new drugs and the drugs which<br />
are already discovered should be affordable and accessible to the entire mankind.<br />
All research should be carried out with the intention of improving the health of the<br />
crores of people of this world and not with the intention of getting more and more<br />
money out of their pocket. Studies suggest that the money spent on research is just<br />
2 – 20% of the total turnover, but huge profits are reaped in the name of recovering<br />
research expenditure. During the patent period cost should be such so as to<br />
recover R & D cost and not in form of monopoly pricing. And after the expiring of<br />
patents the cost of generic version should be a reasonable profit added to cost of<br />
manufacturing the drug.<br />
Drugs which are similar to their predecessors are ‘invented’ just by making some<br />
minor change in the original drug chemical and are then patented and aggressively<br />
promoted – Me too drugs (higher priced alternatives of a parent drug without a<br />
clear therapeutic advantage). In contrast to the breakthrough drugs, they have no<br />
significant treatment benefit, but are just created to continue to enjoy the patent<br />
protection (ever greening of patents) and thereby reap huge profits after anyhow<br />
convincing the doctors to prescribe them.<br />
The country where 3 out of 4 children & every other woman are anemic & iron<br />
defensive anemia is the most prevalent public health problem; the drug companies<br />
are free to sell the iron preparation at any cost which comes to about five to ten<br />
times in certain cases.<br />
Do we really want to help our anemic children<br />
So, whether it is about the patented drugs or about the out of patent (generic)<br />
drugs – the story is the same, drug industry is operating with the motive of making<br />
huge profits rather than the intention of serving the sick and the needy. The<br />
ultimate aim of drug production should be, to make drugs affordable and<br />
accessible to all so that people of the world can be cured of their diseases. The<br />
pharma industry has to sub serve human goals of promoting health, and that<br />
industry cannot operate in a manner that just helps the business elite. Should we<br />
allow commercial interests to dominate us so completely<br />
3
Pharma Scenario in India - Poverty Amidst Plenty<br />
TOP<br />
India has a vast pharma market, and is rightly celebrated in international circles<br />
for making medicines very affordable and low-priced. As of 2003, Indian industry<br />
was supplying 20 percent of the world’s drugs and is currently one of the largest<br />
pharma industries in the world. At least 60 manufacturing plants in India have US<br />
Federal Drug Administration (FDA) approval, second only to the Unites States.<br />
Currently a dozen top Indian companies are major suppliers to the US and<br />
European market as well as China. India has one of the best developed<br />
pharmaceutical industries among the developing countries with over 20,000 units<br />
producing between 60,000 to one lakh formulations. The drug industry has a total<br />
annual turnover of approximately Rs 52,000 crores. Nevertheless, the booming<br />
Indian pharma market coming to the rescue of generic world over, especially by<br />
making low priced antiretroviral, is a good part of the story.<br />
The not so good part is that the Indian pharma scenario, as far as the<br />
ordinary poor consumer is concerned, is a failure of the market. As a result of this<br />
extreme market failure of regulation in the absence of well-functioning markets, the<br />
drug (medicines) availability situation in India is one of the poverty amidst<br />
adequacy – there is inadequate access and supply of even essential drugs to the<br />
poor despite adequate drug production. Adding to this misery is the poorly<br />
functioning public health system. While the sales of Indian pharma companies are<br />
increasing steadily, drugs are getting away from the people, more so for the poor.<br />
Share of drugs to total treatment costs can vary from 50 to 80 percent depending<br />
on rural / urban locations and inpatient / out patient treatment. All-India figures<br />
for per capita annual drugs and other medical expenditure (rural) is Rs. 294 out of<br />
Rs. 380 for health as a whole.<br />
Although there are over 20 thousand drug companies & over 1 lac<br />
formulations are sold in the drug market, medicines are out of reach of millions of<br />
people, because they are unaffordable. The large scale production has not had any<br />
significant improvement in the availability of drugs to meet the country's needs.<br />
One of the major reasons for this situation is that, as we have noted before, most of<br />
the formulations produced are unnecessary, unaffordable, irrational and very<br />
costly.<br />
The fact is that the no. of active pharmaceutical ingredients (APIs) is just 550.<br />
When the actual number of ingredients is so small the large numbers of<br />
pharmaceutical products are just to confuse the doctors & exploit the ignorance of<br />
the patients. It has been estimated that barely 20 per cent of the medicines<br />
available today are necessary to treat over 80 per cent of the prevailing diseases.<br />
About 70 - 80 per cent of the output of some major MNCs in India consists of<br />
simple household remedies like cough syrups and vitamin preparations. But lifesaving<br />
drugs account for only 20-30 per cent of the total value of the formulations<br />
sold by these companies.<br />
It is paradoxical that essential & life saving drugs are inaccessible &<br />
unaffordable & newer drugs which have no therapeutic advantages , irrational &<br />
even dangerous are being produces & marketed at very high prices with utter<br />
disregard to country's health requirements.<br />
In 1975, the Hathi Committee which was appointed by the Government of India to<br />
analyze the Indian drug industry, recommended a restricted list of essential drugs<br />
and that measures be implemented to ensure their production, that a gradual shift<br />
4
e made from brand names to generic names, that price control measures be<br />
effected with the aim of making life-saving drugs and essential drugs affordable,<br />
that public sector play a leading role in drug production and certain drugs be<br />
reserved to encourage the growth of Indian drug companies. The Committee also<br />
recommended elimination of irrational drugs.<br />
The situation assumes menacing proportions when the manufacture, import,<br />
distribution and sale of drugs continue in our country although they are banned,<br />
withdrawn or restricted in other countries, including the country of the parent<br />
company in the case of MNCs. Despite knowledge of the ban, many pharmaceutical<br />
companies continue to market the banned drug, making false claims regarding<br />
their safety and efficacy. For example, the ban order on estrogen-progesterone<br />
drugs was challenged by certain drug companies and a stay was obtained in 1982<br />
on technical grounds. Anabolic steroids were marketed as appetite stimulants for<br />
growing children in the developing countries. Drugs which have a sizeable stake in<br />
our country are not marketed by MNCs in their countries, e.g. cough expectorant,<br />
pain killers, growth tonics, appetite stimulants and anti-inflammatory containing<br />
phenyl- and oxyphenbutazone. Another such drug that has now acquired some<br />
notoriety is analgin and analgin-based drugs like Novalgin, Baralgan, etc. It is<br />
banned in Germany, parent country of Hoecsht, and in several countries of the<br />
West but marketed in India (Baralgan has since been banned in India by an order<br />
of the Supreme Court).<br />
TOP<br />
How doctors are used as an instrument to promote these unhealthy &<br />
unethical practices of pharmaceutical industry<br />
Once their medical education is over, the doctors largely depend on MRs for<br />
information about drugs. MRs knows that for most of the doctors the cure of the<br />
patient is of utmost importance. Thus, doctors are made to believe that although a<br />
particular brand is a bit costly but it is of the best quality and is the most effective<br />
one in the market, which will definitely cure the patient. They are also introduced<br />
to so called latest discoveries which will lead to a magical cure, but which are in<br />
fact minor chemical alterations in the parent drug & are just introduced with the<br />
sole purpose of ever greening of patent and to enjoy monopoly pricing & are non<br />
essential drugs. Similarly with utter disregard to patients health needs drugs which<br />
are neither indicated nor required for a disease are promoted just to increase the<br />
sales figure of the company. Unfortunately most doctors highly depend on MRs for<br />
updation of their medical knowledge and their prescription pattern is largely<br />
influenced by them. Unsuspecting doctors fail to understand that the person<br />
5
coming to them has been hired by a drug company to promote its sale and make<br />
profits.<br />
TOP<br />
Thus, unknowingly doctors help the drug companies and adversely harm the<br />
patients in three different ways.<br />
1. Prescription by brand name<br />
2. Prescription of non essential drugs<br />
3. Irrational Prescriptions<br />
1. Prescription by brand name<br />
In India there are 72 salts which come under drug price control order (DPCO). It<br />
means that the selling price of these drugs is under control & decided by the NPPA<br />
(National Pharmaceutical Pricing Authority). This also means that for all the<br />
remaining drugs, the drug companies are free to decide the selling price (MRP).<br />
Although it is said that in free market economy, market forces will decide the price<br />
to the consumer but in case of drugs it is not so. The reality is that the same salt is<br />
being marketed by different companies under different brand names but the selling<br />
price is to the extent of 10 times to its cost price, which means 1000% profit is<br />
reaped. This is made possible using a marketing strategy of employing Medical<br />
Representatives, who using various means persuade the doctors to prescribe<br />
medicines by brand name of the company & the unsuspecting patient has no<br />
choice except to buy that particular brand even when less costly alternatives are<br />
available in the market. So, due to brand names artificial monopolies are created in<br />
the pharmaceutical market which prevents price competition amongst the same<br />
product and consequently all the brands are sold at high prices.<br />
For example: Amikacin<br />
Drug<br />
manufacturing<br />
company<br />
Name given<br />
by<br />
company<br />
(Brand<br />
Name)<br />
Amistar<br />
500<br />
Salt name of<br />
medicine<br />
(<strong>Generic</strong><br />
Name)<br />
Cadila<br />
Amikacin<br />
500 mg<br />
German Amee 500 Amikacin<br />
Remedies<br />
500 mg<br />
Wockhardt Zekacin Amikacin<br />
500 500 mg<br />
Alembic Amikanex Amikacin<br />
500 500 mg<br />
Intas Kami 500 Amikacin<br />
500 mg<br />
Unichem Unimika Amikacin<br />
500 500 mg<br />
Ranbaxy Alfakim Amikacin<br />
500 500 mg<br />
Cipla Amicip 500 Amikacin<br />
500 mg<br />
Rate at which drug<br />
is purchased by the<br />
chemist (Stockiest<br />
price)<br />
One Injection<br />
Rate at which<br />
drug is sold<br />
to the<br />
customer<br />
(Printed MRP)<br />
8.00/- 70/-<br />
8.00/- 70/-<br />
9.90/- 70/-<br />
8.22/- 64.25/<br />
-<br />
8.13/- 60/-<br />
7.80/- 72/-<br />
8.50/- 70/-<br />
7.42/- 72/-<br />
6
For example if doctor has to treat a patient of blood cancer, he may advice the salt<br />
Imatinib by various brand names. If he has prescribed brand Glivec a months<br />
course will cost Rs.1,14,400/- to the patient. Whereas, the same anti cancer drug,<br />
but with a different brand name Veenat costs just Rs.11,400/-. And Cipla supplies<br />
the generic equivalent of this drug (@-imitib) at Rs. 8,000/- only, also Gelnmark<br />
supplies it for Rs. 5,720/-! All these brands contain the same salt Imatinib, in the<br />
same quantity, conform to the same quality standards and are equally effective. TOP<br />
See an example where the same company markets the same salt by different brand<br />
names and use differential pricing policy.<br />
Drug<br />
manufacturin<br />
g company<br />
Name<br />
given by<br />
company<br />
(Brand<br />
Name)<br />
Salt name of<br />
medicine<br />
(<strong>Generic</strong> Name)<br />
Rate at which Rate at<br />
drug is which drug<br />
purchased by is sold to the<br />
the chemist customer<br />
for 10 Tablets (Printed<br />
(Stockiest price) MRP)<br />
Cipla Alerid Cetrizine 10 mg 28.85/- 37.50<br />
/-<br />
Cipla Cetcip Cetrizine 10 mg 1.88/- 33.65<br />
/-<br />
Cipla Okacet Cetrizine 10 mg 1.84/- 27.50<br />
/-<br />
7
If you don’t believe this then see the list below.<br />
TOP<br />
MRP Printed on the pack<br />
Stockist Price<br />
8
Brand name also violates the right of the patient to choose a product as per his<br />
pocket condition. If doctors prescribe by salt name instead of brand name then<br />
various products can be compared & the one with the lowest price can be offered to<br />
the patients which are at times even 5-10 % of the MRP.<br />
Even oldest of the drugs like paracetamol, iron, etc for which there is no<br />
patent protection and anybody can manufacture and sell it continues to be<br />
marketed at high prices. This is done by appending a brand name to these out of<br />
patent drugs. The same salt is being marketed by different companies under<br />
different brand names but the selling price is to the extent of 10 times to its cost<br />
price, which means 1000% profit is reaped. This happens because the Medical<br />
Representatives of the company persuade the doctors to prescribe medicines by<br />
brand names & the patient has no choice except to buy that particular brand even<br />
when less costly alternatives are available in the market.<br />
BRAND MONOPOLY ELIMINATES PRICE COMPETITION<br />
TOP<br />
There are a number of reasons why the prices of drugs in India, indeed all over the<br />
world, are so high. One of them is the business of branding. In many developing<br />
countries, consumers buy the same drug marketed by several different producers<br />
under different brand names, not realizing that they are all the same product.<br />
Paracetamol, for example, is the generic name, for a painkiller. It is available under<br />
more than 20 brand names -- Crocin, Calpol, Metacin, Pyrin - all of which are<br />
paracetamols. The consumer, however, is not aware of this. Drug companies and<br />
doctors may swear that one particular drug is more effective than the other,<br />
although this cannot be so as they all contain the same ingredient and conform to<br />
the same quality control standards.<br />
Similarly, metronidazole is sold by the name of Amivan, Flagyl, Aristogyl, etc.<br />
The same with different names<br />
Thus, by branding a drug and advertising it, the drug company plays on a<br />
consumer's psyche and brings about an increase in the price of the drug. For<br />
example, it costs around 15 paise to produce one tablet of paracetamol.<br />
Pharmaceutical companies sell the same drug for around 80-90 paise under the<br />
brand name Crocin. That branded drug is sold to consumers through<br />
advertisements; companies spend huge amounts of money on television<br />
advertisements and other kinds of marketing techniques. Brands compete with<br />
each other in the market and the cost is passed on to the consumer. This is the<br />
reason why drugs are so expensive. The pharmaceutical sector thus earns profits at<br />
the cost of the poor and ignorant consumer. The creation of brand names, leading<br />
invariably to high prices, monopolies by big companies and the vulnerability of<br />
consumers, are all aspects related to profiteering in the pharmaceutical sector. This<br />
monopolisation of the market by the drugs industry is one of the main reasons why<br />
drugs are so costly.<br />
9
A look at the growing list of branded drugs also emphasises monopolies in the market. Take<br />
the case of Ciproflaxacin -- an antibiotic used to fight typhoid. Almost half the Ciproflaxacin<br />
sold in the market comes from one company; effectively this drug is the brand leader as well<br />
as the price leader. Being a brand leader, a company, whether it be Cipla, Alembic or Glaxo,<br />
is able to control the market using various marketing strategies and offering huge margins to<br />
retailers and doctors. This way, even if prices are kept high, people will continue to buy the<br />
drug. It is assumed that market forces promote competition. In a free market the<br />
competition results in lowering and more importantly, levelling the prices. But this may be<br />
true in generic drug market but not in proprietary (branded) drug market like that exists in<br />
India. Monopolies are created artificially by means of brand names. In India the<br />
prescription and dispensing of medicines is mostly by brand names. This is in fact the “Trade<br />
Secret” of the pharma business. Different companies manufacture the same salt by different<br />
brand names. The companies allure doctors (via M.R.s ) and induce them to write a particular<br />
brand. The patient has no option but to buy the brand at the M.R.P. which the company has<br />
decided to print. Besides this, the consumers/patients have no choice as they do not select<br />
the medicines like in other consumer goods. The doctors or chemists decide it. Thus, even<br />
when so many companies are manufacturing the same salt there is virtually no price<br />
competition in the market. And all brands are sold at very high rates. The same salt of equal<br />
potency is made by different companies and marketed under different brand names for<br />
different prices (MRP)<br />
2. Promotion of Non essential drugs TOP<br />
There are a total of 354 drugs in the National List of Essential Medicines<br />
(NLEM), which are adequate to take care of the majority of the health needs of the<br />
population. But when we analyze the sales of top 300 brands only 38% of brands<br />
are of the drugs mentioned in the NLEM. The other 62% brands comprise drugs<br />
that are higher priced alternatives without a clear therapeutic advantage and many<br />
are unnecessary, irrational and even hazardous.<br />
Doctor<br />
should act as<br />
FILTER<br />
ESSENTIAL<br />
DRUGS<br />
NON<br />
ESSENTIAL<br />
DRUGS<br />
For the<br />
Patient<br />
10
This indicates that contrary to what is advocated by WHO & as adopted in our<br />
national health policy, the drugs which are most useful & cost effective for the<br />
treatment are not being prescribed & the non costlier & irrational drugs are sold<br />
more often (The government of Rajasthan has directed that at least 85% of the<br />
drugs prescribed should be from EDL)<br />
TOP<br />
Top 300 Brands and their Relation to the National Essential Medicines List<br />
The moving annual total (MAT) from the retail sales of top 300 brands alone is Rs.<br />
18,000 crores.<br />
Some of the top-selling Brands in India as per ORG-Nielsen Retail Audit<br />
Brand name Uses and Remarks<br />
Moving Annual Total<br />
in rupees crore (Oct<br />
2003)<br />
Corex Cough suppressant. Abused as drug of<br />
88.18<br />
addicition because of presence of codeine<br />
Becosules Multivitamin, unnecessary preparation 79.74<br />
Liv-52 Ayurvedic liver preparation 62.67<br />
Neurobion Irrational Multivitamin preparation 60.27<br />
Nise Hazardous drug for pain relief 58.31<br />
Dexorange Irrational preparation for anemia 57.65<br />
Top – Selling Drugs Outside the NLEM include:<br />
(i) Higher priced brand of either the same drug or a higher priced alternative to a<br />
lower cost essential drug<br />
Example: Cifran brand of ciprofloxacin is the largest selling antibiotic, whereas it is<br />
the costliest among the ciprofloxacins. Other brands of ciprofloxacin (e.g. Zoxan)<br />
although three times cheaper, sell five times lesser than Cifran.<br />
(ii) Irrational combinations of drugs, which only add cost but are of no therapeutic<br />
value, are touted as effective remedies and promoted aggressively. In our country<br />
about 75 % of the children & 50 % of the women suffers from Anemia and iron<br />
deficiency anemia is responsible for 1/3 of all maternal deaths. But the most<br />
popular prescription is of fancy multivitamin formulations instead of iron and folic<br />
acid preparations.<br />
The sales figures reflect the fact that in India, drugs which are not considered<br />
essential sell more than rational & essential drugs, that costlier drugs most often<br />
sell more than cheaper alternatives (even<br />
those made by well known<br />
manufacturers), and downright irrational<br />
and hazardous drugs are among the topsellers.<br />
The majority of sales are coming<br />
from the sales of drugs not considered<br />
relevant by experts for inclusion into an<br />
essential medicines list, and not<br />
considered important by the government<br />
for regulation of their price.<br />
Brief analysis of the top 300 brands<br />
suggests that the Indian doctors are<br />
prescribing drugs without adequate<br />
11
concern for evidence of their efficacy, safety and cost. This is because of poor<br />
access to unbiased information on drugs, aggressive and often misleading drug<br />
promotion by the drug industry. The result is increased health care costs, irrational<br />
use of drugs and exposure of patients to the risk of unsafe drugs.<br />
Vitamins and Tonics<br />
These are some of the most highly selling and highly priced products in India.<br />
Vitamin and tonics are in many cases a mixture of Vitamin B-complex or vitamins<br />
in solutions of sugar and alcohol. Among the top-selling 25 medicines in India are<br />
Becosules, Neurobion and Dexorange; the first two are irrational and / or<br />
unnecessary multivitamin preparations and the last is an irrational iron “tonic”.<br />
Vitamins deficiency should be treated with specific vitamins in dry tablet form.<br />
Tonics are hazardous when substances like caffeine, leptazol, are combined with<br />
vitamins. Regular intake of Vitamin A and D can be excessive and hence<br />
hazardous. Bangladesh had banned tonics, enzyme mixture / preparations and<br />
restorative product because such products “flourish on consumer ignorance…and<br />
of no therapeutic value. The United Kingdom does not recognize tonics as drugs.<br />
The production of the high-potency or “Forte” preparations of multivitamins is a<br />
sheer economic waste. It is a drain on the consumers and government<br />
dispensaries. High-potency preparations are also a drain on the country’s foreign<br />
exchange as most of the raw materials have to be imported.<br />
The table below shows that the sale of these rarely required tonics is in hundred of<br />
crore rupees.<br />
TOP<br />
S.N. Brand Name Moving Annual Total (rupees crores)<br />
1 Becosules 79.74<br />
2 Revital 47.64<br />
3 Polybion 40.85<br />
4 Zincovit 32.26<br />
5 Cobadex Forte 26.10<br />
6 Methycobal 21.87<br />
7 Zincovit 21.65<br />
8 Neogadine 21.52<br />
9 Riconia 20.78<br />
10 R.B. Tone 20.21<br />
11 A to Z 19.07<br />
12 M2tone 18.22<br />
13 Supradyn 15.25<br />
14 Becadexamin 14.63<br />
15 Raricap 13.89<br />
16 Becosules-Z 12.03<br />
17 Optineuron 11.97<br />
Total 437.68<br />
It shows: According to the Pharmaceutical Industry, Most Common Public Health<br />
Problem of India is Not Anemia, but B-Complex Deficiency!<br />
12
3. Irrational Prescriptions TOP<br />
Ideally use of drugs should be only when there is an appropriate indication, but<br />
this is not in the interest of the drug industry which is more interested in sales<br />
promotion. Higher the sales, higher the profit. Therefore doctors under constant<br />
persuasion of MRs sometimes follow what is being promoted by the brochures of<br />
drug companies instead of prescribing what they have read in their standard<br />
medical text books. For example:<br />
-> A one year old with low body weight for age is seen in the OPD, because the<br />
parents noticed a pot belly. This is due to under nutrition. The family is poor but<br />
the child has not been weaned and given solid foods. Should the child receive<br />
advice on feeding or an alcohol-based 'multi-vitamin tonic'<br />
-> A computer professional has low-backache because of long hours of sitting at<br />
the desk in a faulty posture on a faulty chair. Should he receive long term painkillers<br />
like indomethacin, valdecoxib, tramadol, etc (all of which have well known<br />
serious side effects) or advice on posture, exercise and a proper chair which<br />
supports lower back<br />
-> A chronic smoker comes with cough off and on, especially in the morning. There<br />
is no shortness of breath. The clinical examination is normal. Should he receive a<br />
cough suppressant, an antibiotic or advice and support for stopping smoking<br />
Reasons for Irrational Prescribing:<br />
1. The MR said so.<br />
2. The latest is the best (latest antimalarials, antibiotics, analgesics, etc.)<br />
3. Costlier the drug, the better it is.<br />
4. The more I write the more I earn.<br />
5. Availability of Irrational Drugs in the Market<br />
6. The patients demand it (or, I will lose my practice…).<br />
Aggressive Drug Promotion:<br />
There are more than 100,000 formulations (at five products per company for the<br />
estimated 20,000 manufacturing units India) in the Indian market, many of which<br />
are similar except for different brand names or for a few unnecessary additional<br />
ingredients. Pharmaceutical companies therefore indulge in aggressive marketing to<br />
promote the sale of their brands. Sometimes, it results in unethical marketing<br />
practices.<br />
As pharmaceutical business is very profitable, it is hardly any wonder that<br />
pharmaceutical companies spend at least 20 percent of their sales revenue on<br />
promoting their products. Drug promotion is carried out by means of heavy<br />
advertising, frequent visits to private medical practitioners by the medical<br />
representatives of pharmaceutical companies with literature on their drugs, free<br />
sample of drugs, and even gifts like diaries, posters, calendars, pens and<br />
sometimes also invitations to medical conferences held in five-star hotels. The<br />
companies also encourage articles in newspapers and magazines, television and<br />
radio programs, release promotional materials as news stories about latest<br />
developments in medical field and sponsoring television programs. Thus, drug<br />
promotion is a comprehensive attempt to influence the doctors to suspend their<br />
critical judgment and prescribe what is profitable for the manufacturer.<br />
13
1. Influencing Doctors to prescribe<br />
irrational, non essential drugs by brand<br />
name<br />
Companies prefer to spend more on drug<br />
promotion because they recover their<br />
expenses by pricing the drug highly. Doctors<br />
are influenced into prescribing a particular<br />
brand which is often more expensive. The<br />
Hathi Committee in its report, made this<br />
observation about the multinational drug<br />
industry: "High pressure sales techniques<br />
coupled with distribution of medical samples on a liberal scale to the medical<br />
profession was their (MNC's) forte". According to David Jones, former vice president<br />
of Public Affairs for Abbott Laboratories, and former Executive Director of Public<br />
and Professional Affairs for Ciba-Geigy, "Prescription drugs are marketed as if they<br />
are candy. Claims are made beyond what the product will do. Demand is inflated<br />
beyond the medical need. Uses are promoted that are neither healthy nor wise"<br />
World over, and in India specially, medicines are promoted by all means fair and<br />
foul. Drug industry treats doctors as prescribers and not cares givers.<br />
2. Lack of Objective Drug Information TOP<br />
It is doubtful whether the majority of doctors in India are in the habit of regularly<br />
referring to standard textbooks or standard medical journals. In Britain, all<br />
practicing doctors are supplied every six months with a copy of the British National<br />
Formulary (BNF) which contains reliable, updated information including costs on<br />
the preparations on sale in the UK.<br />
In the absence of objective information on new drugs, doctors in many Third World<br />
Countries, are fully dependent on drug information supplied by the pharmaceutical<br />
companies. And owing to the profit-oriented nature of the drug companies, the<br />
information provided in its literature is bound to be in favor of the drug.<br />
The prescribing information in most publications cannot be relied upon. Some of<br />
these journals bring out "Review of New Drugs", which are actually based on<br />
unreliable information. These publications even bring out pseudo-scientific reviews<br />
of irrational drugs!<br />
Doctors in India usually rely on information supplied by medical representatives<br />
and drug companies which can be very biased and selective. Also, doctors are led to<br />
believe a lot of new products are being marketed every day. Many of these are not<br />
new discoveries, which radically alter the course of treatment.<br />
3. “False” Evidence-based medical practice: The practice of medicine based on<br />
scientific evidence is more talked about and less practiced. Some times evidence is<br />
selectively quoted or false evidence is produced to promote a drug. For Example:<br />
• Glaxo Laboratories cited the authority of a British medical journal, the<br />
Lancet to promote its sales of Ostocalcium B-12 even though there was no<br />
such endorsement of the product in the Lancet.<br />
14
• Boehringer-Knoll quoted UNICEF and used their logo to promote the use of<br />
streptomycin-chloramphenicol combination for diarrhoea treatment,<br />
whereas UNICEF promotes simple ORT for most diarrhoea.<br />
• Franco-Indian Laboratories misquoted Goodman and Gilman to promote<br />
their tonic, whereas Vitamin B-12 has no role in ordinary anaemia.<br />
• S.G. Chemicals (Indian subsidiary of Ciba-Geigy) misquoted Goodman and<br />
Gilman and Martindale to promote a combination of two dangerous drugs<br />
analgin and oxyphenbutazone, whereas in fact the texts warn against this<br />
dangerous combination.<br />
• There also exist double standards in the information given on drugs by<br />
MNCs in the developed and developing countries. In the developing<br />
countries, warnings about the side-effects or contraindications are not given;<br />
drugs are recommended when their efficacy is not proven and even when its<br />
safety is not established fully. For instance, oral contraceptive drugs are not<br />
recommended in U.S.A. and Britain for premenstrual tension, menstrual<br />
cramps, and menopausal problems and in dysfunction of the female<br />
reproductive system.<br />
TOP<br />
Opinions of International Panel on Drugs Advertised in Indian Edition of<br />
BMJ<br />
Trental 400 (pentoxifylline): “The advertisement makes unsubstantiated claims<br />
of improvement in mental function.” (This drug is marketed only for peripheral<br />
vascular disease in America and Britain; in India it is indicated for<br />
cerebrovascular disease as well)<br />
Relaxyl (diclofenac): “The claim ‘gentle on the gastrointestinal tract’ is not in<br />
accord with the reported high incidence of gastrointestinal side effects (up to<br />
30% in Australian approved product information).”<br />
4. Promotion of Hazardous, Banned and<br />
Bannable Drugs<br />
Internationally, a whole group of "block<br />
buster" drugs have been in serious<br />
trouble. These include rofecoxib ("Vioxx"),<br />
valdecoxib ("Bextra"), celecoxib<br />
("Celebrex"), atoravastin ("Lipitor"), etc. as<br />
of writing there is enough evidence to<br />
doubt the safety of a host of cyclooxygenase<br />
(COX) -2 inhibitors.<br />
(i) The case of Rofecoxib shows how a leading MNC drug company with a block<br />
buster does anything to ensure its continued presence in the market, how research<br />
studies are reported and interpreted selectively and how meta-analyses can be<br />
used to support contrary positions, and how the US FDA acts ever so haltingly and<br />
indecisively.<br />
Rofecoxib was first marketed by Merck in 1999. The following year, a<br />
randomized trial revealed increased rates of adverse cardiovascular events. Merck<br />
15
aggressively defended rofecoxib's safety with a series of meta-analyses and<br />
retrospective studies, and spent hundreds of millions of dollars marketing rofecoxib<br />
to physicians and consumers. Merck's eventual decision to withdraw -effective<br />
September 30, 2004 from the market was based on an increased risk for heart<br />
attacks and strokes. US FDA analysts estimated that Vioxx caused between 88,000<br />
and 139,000 heart attacks, 30 to 40 per cent of which were probably fatal, in the<br />
five years the drug was on the market.<br />
TOP<br />
(ii) Valdecoxib was eventually withdrawn on April 7, 2005 after a US FDA request<br />
asking Pfizer to voluntarily remove Bextra (valdecoxib) from the market, a decision<br />
based on an incidence of severe skin reactions and evidence of increased risk of<br />
cardiovascular malfunction.<br />
(iii) Celecoxib is the only COX-2 inhibitor still available. It now carries a boxed<br />
warning regarding cardiovascular and gastrointestinal risks. The Drug Controller<br />
General Of India (DCGI) has asked drug companies to carry a warning on the label<br />
of selected Cox-2 inhibitors. "This drug should be used with caution in patients<br />
from Coronary Heart Disease (CHD) / Cardiovascular Disease.<br />
(iv) Atorvastatin. Pfizer misled consumers into using its anti-cholesterol drug<br />
brand Lipitor despite the absence of evidence from clinical trials that the drug or<br />
others in its class are of any benefit to large segments of the population, according<br />
to a consumer class action lawsuit filed against the world’s largest maker.<br />
Lipitor is in the class of cholesterol lowering drugs and it is the best selling<br />
drug in the world, with sales in 2004 of more than $10 billion. “The idea that<br />
lowering cholesterol always reduces the risk of heart disease had become the<br />
conventional wisdom, which drug companies like Pfizer have taken great pains to<br />
promote. But for women under 65 and people over 65 with no history of heart<br />
disease or diabetes, the evidence isn’t just there. Millions of women and seniors are<br />
spending huge sums to take Atorvastatin every day despite a lack of proof that it’s<br />
doing anything beneficial for them, and may actually be harming the elderly with<br />
its side effects.<br />
(v) Thalidomide: most women experience nausea during pregnancy which is a<br />
physiological condition, but interestingly a drug was invented to cure it and blindly<br />
propagated with the sole purpose of making money. It is another example where a<br />
drug was pushed into the market without adequate evaluation of its safety.<br />
Unfortunately above 8,000 mothers who unsuspectingly took the drug bore<br />
children without arms and legs, the condition which is known among doctors as<br />
phocomelia (seal like limbs).<br />
16
(vi) Clioquinol a widely used over the counter drug to treat diarrhoea and marketed<br />
as Entero-Vioform, Mexaform, etc. It damages the central nervous system resulting<br />
in paralysis, blindness (Subacute myelo-optic neuropathy, SMON). About 11,000<br />
people in Japan were victims of these side effects caused by the drug. The Swiss<br />
drug company, Ciba-Geigy, was found guilty of marketing this drug without<br />
revealing its hazards.<br />
TOP<br />
(vii) Nimeuslide was discovered by an American Company, 3M Pharmaceuticals,<br />
but never got approval for use in the US, Canada, Britain, Australia, New Zealand<br />
and 140 other countries around the world. It was banned in Spain and England in<br />
2001 on reports of its hepatotoxicity. Even in Sri Lanka and Bangladesh, it is not<br />
allowed to be marketed. In August 2003, the European Medicine Evaluation Agency<br />
(EMEA) had banned the use of nimesulide in all the 25-member countries. Its use<br />
for fever is not permitted.<br />
Numerous studies have established the life-threatening adverse events with<br />
nimesulide such as hepatotoxicity, renal toxicity, severe skin reactions including<br />
fixed eruptions, gastrointestinal toxicity, potentiation of seizures, potentiation of<br />
colitis in passive cigarette smoking. There is no reason for selecting nimesulide as<br />
the first drug of choice for fever or pain.<br />
In India, marketing approval for the drug was granted in 1994 for painful<br />
inflammatory febrile disorders but unfortunately due to huge profit potential it is<br />
being promoted as first line antipyretic therapy. Despite of serious side effects and<br />
its indication for specific clinical conditions, there is abundance of Nimesulide<br />
Formulations in our country. Pharmabiz.com reports that, “...200 nimesulide<br />
formulations are marketed without the approval of Drug Controller General of<br />
India. Out of these 200 products, 70 are nimesulide suspensions and the<br />
remaining 130 are fixed dose combinations of nimesulide with a number of other<br />
drugs. Combinations of nimesulide and paracetamol, numbering 50, are the largest<br />
segment in this group. Top selling brands in<br />
all the three categories are being marketed<br />
by major pharmaceutical companies in the<br />
country…”<br />
Studies have shown that nimesulide<br />
should not be used as the primary mode of<br />
treatment as an antipyretic or analgesic,<br />
especially in children, for whom much better<br />
and safer choices are available. But there<br />
are over 70 brands of pediatric suspensions,<br />
including Nise of Dr. Reddy’s Labs and<br />
Nimulid of Panacea Biotec. Two account for<br />
more than 50 per cent of the market. And the nimesulide market is around Rs. 700<br />
crores with profit percentage over 1500%.<br />
When a PIL was filed in Delhi High Court seeking a ban on nimesulide, it was<br />
informed by DCGI that on the basis of an “opinion poll” among just 50 doctors of<br />
the over 4,00,000 doctors, the Indian Medical Association (IMA), Delhi branch, has<br />
come to the conclusion that nimesulide was “safe and effective for all age groups<br />
starting with day one to over 60 years”. In the wake of media reports the Indian<br />
Academy of Pediatrics (IAP) also advocated use of nimesulide by Indian children. It<br />
is indeed disturbing that while the leading countries of the world have not allowed<br />
/ banned or withdrawn the drug, the opinion of a mere 50 private doctors has tilted<br />
17
the scale towards allowing the drug to continue to be marketed in India, because of<br />
the vested interests of the powerful pharma industry lobby.<br />
TOP<br />
(viii) Depo Provera is an injectable contraceptive for use by women manufactured<br />
by the American multinational, Upjohn. This drug is not allowed for use as<br />
contraceptive in USA. Yet the drug is sold in the Third World for contraceptive use.<br />
The drug is associated with breast and endometrial cancers and lowered resistance<br />
to infection. The drug causes severe birth defects if a woman who is unaware of her<br />
pregnancy, take the drug.<br />
(ix) Dexorange: An outstanding example of a patently irrational drug is that of<br />
Dexorange. This formulation is used for treatment of one of the most common and<br />
serious health problems of people, anemia. It is one of the top selling preparations<br />
in India with a Moving Annual total in retail sales of Rs. 57 crores. Till 2000 this<br />
company, for over a decade and a half, was adding minute amounts of hemoglobin<br />
obtained from slaughterhouses under unhygienic conditions to its otherwise<br />
irrational formulation of iron. The amount of hemoglobin added to the preparation<br />
was such as to provide a meager additional 2-3 mg of iron per 15 ml.<br />
Finally, the Government banned hemoglobin. But, the addition of<br />
hemoglobin of animal origin to an iron preparation is without parallel in the<br />
pharmaceutical sector worldwide. No other formulary mentions it, and no other<br />
country ever allowed it. This particular preparation still contains an iron salt,<br />
which is less efficiently absorbed, in a concentration that is low, and is still<br />
marketed at a price that is extravagant. The cost of treating iron deficiency anemia<br />
with this preparation can be up to Rs. 600 per month, against the cost of a simple<br />
iron-folic acid preparation that should cost Rs. 9 per month. The case of the<br />
consistent marketing success of Dexorange is not a mere example but stands as a<br />
damning indictment of the state of affairs in the pharmaceutical sector, the<br />
government and the prescribers. It has put the interests of the voiceless patient /<br />
consumer in the background.<br />
(x) Cisapride: Causes acidity, constipation, etc. Reason for ban: Irregular<br />
heartbeat. But continues to be marketed by brand name: Ciza, Syspride, etc. even<br />
as suspensions for our children.<br />
5. Doctors as Key Opinion Leaders:<br />
Key Opinion Leaders (KOLs) are influential specialists in their fields such as<br />
doctors at teaching hospitals, senior consultants, authors etc. An endorsement by<br />
a KOL in favor of new products or new uses of old products is a top priority for<br />
pharma companies. Aggressive, often highly unethical, tools are employed to<br />
capture KOLs.<br />
Consider the following actions of drug companies and their KOLs.<br />
1. Sun Pharmaceuticals sponsored over a dozen “educational seminars” all over<br />
India to advocate Letrozole’s use in infertile young women. KOLs were paid<br />
up to Rs. 30,000 per lecture to endorse the new indication. It is illegal to<br />
promote any drug for unapproved indications.<br />
2. According to one KOL of Jammu, he has already prescribed cisapride to<br />
40,000 patients. Another KOL from Jammu says the same thing in the same<br />
language and he too has prescribed for 40,000 patients and from 1990 at<br />
that when the drug was not even marketed! Another KOL says it is okay to<br />
give it to infants for pain in abdomen when it is prohibited for use in<br />
18
children and yet another has determines that the side effects of cisapride are<br />
to be found in 0.0001% of the patients whereas the US FDA says it is about<br />
5 percent! TOP<br />
3. Professional associations endorse products: Delhi branch of the Indian<br />
Medical Association endorsed nimesulide and in its so-called survey for the<br />
purpose, the sample of adults to children taken if extrapolated results in the<br />
number of children of India being more than the population of India!<br />
4. The Journal of Indian Medical Association has a “Research Analysis<br />
Section” that in effect provides a platform to Pharma companies to market<br />
their products.<br />
Example: JIMA (Volume 99, No 3, July-Sep 2001) published two articles in a<br />
span of a few months. Both promoting iron polymaltose (IP) preparations<br />
claiming superiority of IP over ferrous fumerate and then quotes the<br />
publication of these papers in marketing Mumfer, its brands of IP!<br />
A further and more blatantly unethical form of manufacturing “consent” is<br />
by ghostwriting research papers. Estimates suggest that almost half of all articles<br />
published in journals are by ghostwriters. While doctors who have put their names<br />
to the papers can be paid handsomely for ‘lending’ their reputations, the<br />
ghostwriters remain hidden. They, and the involvement of the pharmaceutical<br />
firms, are rarely revealed.<br />
6. Biased Clinical Trials<br />
The medical fraternity believes in evidence based medicines but many times: trials<br />
are sponsored, evidence is created and favorable results are arrived at. Research<br />
that is sponsored by a drug manufacturer is more likely to yield a positive result for<br />
the company’s product.<br />
Examples of Methods for Pharmaceutical Companies to get the Results they want<br />
from Clinical Trials:<br />
1. Conduct a trial of your drug against a treatment known to be inferior.<br />
2. Trial your drugs against too low a dose of a competitor drug<br />
3. Conduct a trial of your drug against too high a dose of a competitor drug<br />
(making your drug seem less toxic)<br />
4. Conduct trials that are too small to show differences from competitor drug<br />
5. Do multi centre trials and select for publication results from centers that are<br />
favorable.<br />
6. Conduct subgroup analyses and select for publication those that are<br />
favorable.<br />
7. Present results that are most likely to impress.<br />
When we talk of scams involving drug trials in India, none can forget unethical<br />
trials of G4N which was discovered in USA but was unlawfully tested on oral<br />
cancer patients at Regional Cancer Center in Kerala.<br />
Drug companies, driven by economic pressure conduct often post-approval studies.<br />
Merck and Pharmacia did extensive post-approval studies to show that their<br />
arthritis pain medications, Vioxx and Celebrex, were easier on the stomach.<br />
Merck’s study, involving 8000 adults, showed Vioxx causes fewer stomach<br />
complications but also found it increases the risk of heart attacks. Despite that<br />
only the advantages were selectively revealed, intentionally hiding the life<br />
threatening side effects. In fact, it is better to kill a new hazardous drug which is<br />
19
ought into the market without adequate clinical trials rather than to kill many<br />
unsuspecting patients.<br />
TOP<br />
7. Disease Mongering: “Corporate Construction of Disease”<br />
One of the important ways drug companies make money is by telling people they<br />
are sick, even when they are passing through one of life’s many normal transitions.<br />
This “Disease Mongering” suits the medical profession too, as it helps medicalising<br />
problems.<br />
1. In India, piractecam is being promoted for vague conditions like<br />
“intellectual decay”, “social maladjustment,” “lack of alertness,” “change of<br />
mood,” “ deterioration in behavior” and “learning disabilities in children<br />
associated with the written word.” The recommended duration of treatment<br />
for the last indication is “entire school year” in dose of “3g per day” i.e. 7-8<br />
capsules of 400mg daily. If the drug is administered for the entire school<br />
year as recommended, it will mean parents buying at least 2700 capsules at<br />
a cost of Rs. 12,775 year after year. The unending claims of the drug’s<br />
efficacy include the treatment of sickle cell anaemia, stroke and vertigo. In<br />
Britain, piracetam (Nootropil) is permitted for use in just a single indication,<br />
a rare disorder called cortical myoclonus, that too only as an adjunctive<br />
therapy. While in India, the drug is being promoted for use in young<br />
children, in Britain its use is contraindicated for adolescents under the age<br />
of 16 years. If the Indian company marketing piracetam is to be believed, the<br />
drug is nothing short of nectar. It has no contraindications; no need to<br />
observe any precautions and no adverse drug reactions. In Britain, the drug<br />
is contraindicated in hepatic and renal impairment, during pregnancy and<br />
lactation. It is not marketed in USA.<br />
2. Buclizine (brand Longifene in India) is being promoted as appetite<br />
stimulant while the drug itself is not commercially available in the US and<br />
is restricted worldwide for treatment of migraine in combination with<br />
analgesics. Internationally reported adverse effects include: drowsiness,<br />
blurred vision, diarrhoea, difficulty in passing urine, dizziness, dryness,<br />
tachycardia, headache, nervousness, restlessness, hallucinations, skin rash<br />
and upset stomach. Bottles of Longifene, the only brand of buclizine being<br />
sold in Indian do not contain either the package insert or the patient<br />
information leaflet.<br />
3. Warner Lambert invented a condition called “halitosis” which makes<br />
ordinary bad smell in the breath sound serious. Sales of Listerine rose from<br />
US $ 100,000 to US $4 million in six years.<br />
4. In the 1980s Glaxo needed to expand their market for ranitidine (brand<br />
Zantac). They again created a condition called “gastro-oesophageal” reflux<br />
disease (GERD)” which is a serious sounding name for heartburn, an age-old<br />
complaint. The companies also setup a platform called the Glaxo Institute<br />
for Digestive Health, which in due course led to a PR exercise called<br />
Heartburn Across America. Annual sales of Zantac peaked at US $2 billion.<br />
5. “Capturing impotence in an acronym”: During the 1990s Pfizer had to create<br />
a market for sildenafil citrate (“Viagra”) and it ended up calling the broader<br />
condition of impotence as “erectile dysfunction” (ED). Calling impotence<br />
20
ED caused probably less embarrassment to shy patients as they could now<br />
discuss a medical problem called ED with their doctors.<br />
TOP<br />
6. “A legendary example of this condition (called) branding strategy was the<br />
development of Xanax (alprazolam) for panic disorder. A conference then<br />
published diagnostic criteria for panic disorder and how best to treat it. Of<br />
course, Xanas was the first to receive an exclusive indication, thereby<br />
maintaining its leadership in anxiety disorders.<br />
7. In Australia, baldness in men was medicalised by merck to sell its hairgrowth<br />
drug finasteride (Propecia).<br />
8. Manufactures of fluoxetine as a marketing strategy eulogized premenstrual<br />
syndrome which is a routine physiological hormonal transition.<br />
9. Roche started promoting its antidepressant Aurorix (moclobemide) as a<br />
valuable treatment for “social phobia”. Its press release says more than one<br />
million Australians suffers from this “soul-destroying condition”.<br />
Where most of the drug research is funded by the pharmaceutical industry,<br />
truthful reporting is unlikely to occur.<br />
8. Direct to consumer advertising (DTCA)<br />
Some products which should be taken under medical guidance are marketed<br />
through advertisements using electronic & print media. Tall claims are made about<br />
the results they will bring about but they are silent on the side effects which will<br />
occur. Thus medicines are promoted like any other consumer item just to increase<br />
the sales. For example<br />
Oral emergency contraceptive pill: Unwanted 72 and I-Pill<br />
Cough Syrups<br />
Cough Syrups and expectorants are mixtures of drugs which stimulate coughing<br />
(ammonium chloride, ipecac) as well as those which suppress coughing (codeine,<br />
noscapine) and antihistamines that dry the secretions (some common brand names<br />
are Benadryl Expectorant, Piriton Expectorant, Avil Expectorant).<br />
Prolonged use of cough syrup is habit-forming, it may cause stomach upsets,<br />
reduce food intake and cause drowsiness. Coughing is a protective activity of the<br />
body. It should not be suppressed except in certain conditions. Simple steam<br />
21
inhalation is advised. If it is necessary to use drugs, use only a single ingredient<br />
cough suppressants such as codeine, dextromethorphan. There is no scientific<br />
basis for using cough suppressants and cough stimulants together. The WHO List<br />
of Essential Drugs does not include cough syrups and lozenges. Bangladesh has<br />
banned them on the grounds they are "of little or no therapeutic value and<br />
amounts to great wastage of meager resources"<br />
TOP<br />
9. Influencing Government Policies<br />
Multinational companies (MNCs) are complex, highly technical structures, with<br />
economic and political clout often exceeding that of the governments of the<br />
countries where they operate. In a bid to expand their markets internationally,<br />
MNCs resort to business practices which may be unethical. They are known to take<br />
advantage of the economic weaknesses of the host countries to conduct operations<br />
of a nature which have deep adverse effects on the host country's economy, human<br />
health and environment.<br />
The companies repeatedly and illegally influence policy makers, to keep the essential drugs<br />
out of price control and to keep on utilizing pharmaceuticals that have been banned in<br />
developed countries and dumped on the Third World. All in all, the abuses and false promotion<br />
of needless, costly, and irrationally combined medications have reached alarming and healththreatening<br />
proportions, particularly in India.<br />
HISTORY OF DRUG PRICE CONTROL IN INDIA<br />
India being a socialistic country, decided to control the prices of medicines. Two<br />
important policy interventions had helped keep drug prices from spiralling. One,<br />
the 1970 Patents Act and the other, the Drug Prices Control Order (DPCO). The<br />
former did so by making process patents valid in India for pharmaceuticals. This<br />
dramatically brought down the prices, facilitating local bulk drug manufacture at<br />
costs one-tenths of international drug companies. The latter is issued under<br />
Essential Commodities Act,1955 which empowers the central govt. to keep a check<br />
(ceiling) on drug prices by issuing Drug Price Control Order (DPCO).<br />
In 1979, 347 essential drugs were under control. Subsequently drug companies,<br />
national and multinational, had their way, and have succeeded in persuading the<br />
government to reduce the basket of price controlled drugs from 347 in 1979 to 142<br />
drugs in 1987. In 1995 this came down to 76 and at present only 74 out of over<br />
500 commonly used drugs are under statutory price control. It means for all the<br />
remaining drugs the companies are free to charge any price from the patient, as<br />
there is no ceiling on M.R.P. This is an irony that most of the essential drugs and<br />
their formulations are outside the PRICE CONTROLLED DRUGS LIST. This means<br />
that for all other drugs, the companies are free to fix MRP of their choice , which<br />
could be 5 to 10 times the actual production cost (even at the cost of many lives).<br />
22
Implications of Unethical Promotion and<br />
Irrational Use of Drugs<br />
TOP<br />
THE SUFFERING<br />
The consequences of this widespread uncontrolled misuse are devastating:<br />
1. MEDICINES BECOME UNAFFORDABLE.- Suffering and deaths Profiteering<br />
and huge expenditure incurred on marketing & commissions by drug companies<br />
inflates the cost of medicines many times. By selling drugs at inflated prices, big<br />
companies and retailers pocket a large share of the money paid out by the<br />
consumer. In low and middle-income countries including India, public medicine<br />
expenditure does not cover the basic medicine needs of the majority of the<br />
population. In these countries, patients pay for 50-90 per cent of the medicines<br />
from their own pockets. Consequently, many families are driven into debt. Many<br />
Indian families shift below poverty line, annually due to health expenditures.<br />
Many patients spend their lifetime savings to procure them. Many who have no<br />
savings have no option, but to die without treatment. WHO estimated in 1999<br />
that the percentage of Indian population had sustainable access to essential<br />
drugs was in 0-49 range, categorized as very low access country. This is the most<br />
unfortunate part of the story. It is important to remember that consumers of<br />
pharmaceutical products are extremely vulnerable. They are in no position to<br />
reject or postpone buying medicines, even if the medicines are expensive. If a<br />
doctor prescribes a particular drug, the patient has to buy it. Drug companies<br />
exploit this vulnerability, especially in India where drug consumers are<br />
fragmented and unrepresented, unlike in the West. In the West, people either get<br />
themselves insured or are insured by their employers. The insurance company<br />
buys the patient's medicines. Expenditure on health is also responsible for APL to<br />
BPL shift, rural indebtness & failure to rise above poverty line.<br />
Let’s take an example. A doctor has prescribed an injection (Amikacin 500) for<br />
pneumonia which bears MRP of Rs. 70. In India there are many patients who have<br />
just Rs. 10 in their pocket and hence are not able to purchase injection Amikacin<br />
as it is sold in the market at Rs.70 (MRP). Therefore, many poor patients are forced<br />
to die for want of medicines. Although, the actual cost is less than Rs. 10. In our<br />
country where millions live below poverty line, many poor people die like this,<br />
every day, in this criminally exploitative and brutally unjust system. If, the<br />
injection which actually costs Rs. 8 could be supplied at Rs. 10 instead of Rs.70<br />
(printed MRP), many more patients could afford treatment and many more lives<br />
could be saved.<br />
2. INAPPROPRIATE MEDICATION Approximately 4 million children die each<br />
year from diarrhea-related causes, primarily dehydration, according to the WHO.<br />
Many of these deaths can be prevented through oral rehydration therapy, which is<br />
simply the replacement of fluid and mineral losses caused by the diarrhea with a<br />
mixture of clean water, salt and sugar. Yet, according to WHO appropriate<br />
treatment "often remains the exception rather than the rule”. A large number of<br />
pharmaceutical agents of dubious efficacy and potential toxicity are widely<br />
used. Tragically, many spend their scant savings on medicines that are ineffective,<br />
23
worthless and sometimes even harmful.<br />
delays or replaces appropriate treatment.<br />
The inappropriate use of drugs often<br />
TOP<br />
Many drugs eg. protein powders, vitamins, health tonics, etc which are not<br />
required for the patient are prescribed, virtually regardless of the condition being<br />
treated, just to increase the sale of a particular brand and draw commissions from<br />
this sale. Side effects are inevitable in such cases. Also, indiscriminate use of<br />
antibiotics could lead to resistance.<br />
3. CIRCULATION OF BANNED DRUGS. Drugs banned or withdrawn in Europe<br />
are widely available in the Third World. Right now, 85 types of drugs, considered<br />
hazardous and therefore banned in the West, are being sold in India . The majority<br />
of the drugs on the list are analgesics and antibacterials, for which there are<br />
several safer alternatives that appear on the World Health Organization essential<br />
drugs list. Many such drugs are available in India, for eg. Analgin, Cisapride,<br />
Droperidol, Furazolidone, Nemisulide, Nitrofurazone, Phenopthlein,<br />
Phenylpropanalamine, Oxyphenbutazone, Piperazine, Quinodochlor.(source: MIMS)<br />
4. EXTRA BURDEN ON GOVT. EXCHEQUER. The govt. hospitals indent and<br />
receive medicines by generic name. Thus, medicines written by brand name are<br />
usually not available in hospital supply. Therefore, pensioners and other govt.<br />
servants buy these overpriced branded medicines from private chemists, and claim<br />
medical reimbursement from the govt. This leads to a heavy burden on the govt.<br />
exchequer. This money can be saved very easily by generic prescribing and making<br />
low cost drugs available to the patients and this money, can be used to treat more<br />
patients.<br />
5. DRAIN ON FOREIGN EXCHANGE. ‘Importation of pharmaceuticals is one of<br />
the fastest growing drains on hard foreign currency for developing countries’,<br />
explains WHO. The Third World pays the rich world an estimated nine billion<br />
dollars a year for drugs. And prices are rising: four times as fast as GNP in many<br />
poor countries. In fact, some health ministries are spending over 50 per cent of<br />
their budgets on drugs alone. Poorer countries waste limited currency on<br />
unnecessary drugs.<br />
6. RISK OF ADVERSE EFFECTS: All drugs carry the risk of side - effects, e.g.<br />
majority of the pain killers carries the risk of side - effects on the stomach. The<br />
unnecessary use of drugs exposes patients to the risk of side effects. About 4% to<br />
10% of hospital in-patients suffer an adverse drug reaction in developed countries.<br />
This is the fourth to sixth leading cause of death in the US.<br />
7. RISK OF TRANSMISSION OF DISEASES THROUGH UNSAFE INJECTIONS:<br />
An average Indian receives 2.9-5.8 injections per year. The safety of such injections<br />
was abysmal with 62.9 per cent of injections being adjudged as unsafe and nearly<br />
32 percent were considered to be capable of transmitting serious blood borne viral<br />
infections. A proof of the hazard of unsafe injections has been in outbreaks of<br />
hepatitis B with high fatality. Unsafe injections contributes to 80,000-1,60,000 HIV<br />
infections, 2.7-4.7 million Hepatitis C virus infections, and 8-16 million Hepatitis B<br />
virus infections globally every year.<br />
8. RISK OF ANTIMICROBIAL RESISTANCE: Globally there is a rise in the<br />
resistance to antibiotics and a major cause is the wrong use of these medicines.<br />
24
E. The Solution<br />
1. Rational use of Drugs TOP<br />
(i). <strong>Generic</strong> Prescribing: <strong>Generic</strong> drugs play an important role in health care and<br />
the prescription and availability of generic drugs eliminates the monopoly of the<br />
drug companies. WHO calculates that generic prescribing of essential drugs could<br />
save 70 per cent of the drugs bill in rich countries alone. In poor countries benefit<br />
to the patients will be much more.<br />
A generic medicine provides the same quality, safety and efficacy as the original<br />
brand name product and undergoes strict scrutiny before it is licensed and given<br />
market approval by the authorities. A generic medicine is typically 20% to 80% less<br />
expensive than the brand-name original. In addition, the availability of lower-priced<br />
generic medicines brings down the price of originator drugs through market<br />
competition.<br />
Advantages of having a generics-only policy<br />
<br />
<br />
<br />
<br />
Ensure production, sale and dispensing of more rational single ingredient<br />
drugs.<br />
Quality drugs are much cheaper when purchased under their generic<br />
names rather than their brand names.<br />
Ensure clarity and avoids confusion arising out of many dissimilar brand<br />
names of the same drug.<br />
Curtail the heavy promotion of brands and their high cost.<br />
(ii) Adoption of essential drugs list WHO points out<br />
that a selection of just few drugs are needed to treat the<br />
majority of diseases i.e. Essential Drugs. But there are<br />
over 1,00,000 available in India. The govt. of Rajasthan<br />
acknowledges that “high profits in pharmaceutical<br />
industry has led to a large number of drugs and<br />
medicinal products under various brand names and<br />
number of them have been reported to be irrational<br />
combinations as per WHO criteria”. Thus to promote<br />
rational use of drugs on basis of suitability and cost<br />
effectiveness, the state govt. has adopted an essential<br />
drug list (EDL) which includes about 350 medicines.<br />
The govt. hospitals have been directed to spend 85<br />
percent of their budget to procure medicines from EDL<br />
and the govt. doctors shall prescribe medicines out of<br />
EDL as far as possible. The need of the hour is to give<br />
effect to these govt. orders.<br />
(iii) Adoption of Standard Treatment Guidelines to<br />
discourage “Luxury drugs” WHO believes that<br />
expenditure on preparations which are not in EDL is a<br />
criminal waste of resources. Many health tonics,<br />
vitamins, antioxidants, etc. are promoted by<br />
companies just to increase sales and reap profits. Any<br />
new product, including a new analgesic or antibiotic,<br />
generates enthusiasm in physicians, which is<br />
multiplied many times through the persuasive<br />
25
influence of M.R.s who claims this costly new drug is more effective. Tragically,<br />
millions of poor spend their scant savings in medicines that are worthless and<br />
sometimes even harmful. Though they can be easily treated with help of essential<br />
drugs. Thus, curbing the marketing of useless or harmful drugs is equally<br />
important. This can be done by putting Standard Treatment Guidelines (STG)<br />
into practice. This will prevent the doctor from prescribing useless drugs<br />
unnecessarily.<br />
2. Availability of Low cost drugs. TOP<br />
I. Drug procurement by generic name through open tender system: The<br />
prerequisite for such a system is identification of required drugs by generic<br />
name. Drugs are then procured by a two stage transparent tender system.<br />
This ensures that only those companies that are capable of supplying<br />
products of adequate quality receive orders. The tender process is limited to<br />
companies that fulfill the "quality" criteria. Through a two stage tender system<br />
(technical bid and price bid), it is ensured that the purchases are made from<br />
companies complying with the good manufacturing practices. The prices<br />
offered by pharmaceutical companies to the Government during quality<br />
conscious bulk procurement are only to the tune of 2 – 20 % of the retail price<br />
(MRP). The Tamil Nadu model and Delhi Model of centralized procurement are<br />
being followed by many other states in the country. This has enhanced the<br />
supply of prescription drugs in the hospitals, besides causing a substantial<br />
reduction in drugs procurement cost.<br />
II. Distribution of Low cost drugs through govt. drug counters.<br />
The drugs procured through centralized procurement system or manufactured<br />
by PSUs costs very low. It is not enough to supply these in govt. hospitals, but<br />
they should be made available to all the patients at govt. run drug counters at<br />
low cost. For example tab. Diazepam is being supplied to govt. hospitals at 90<br />
paise per 10 tabs. However, the same drug is available to the patients by the<br />
brand name of Valium, for Rs. 19.50. A mechanism needs to be devised to<br />
provide all the commonly used medicines at their actual costs to all citizens.<br />
26
The possible drug counters could be:<br />
TOP<br />
1. Life-line drug stores (run by RMRS)<br />
2. Co-operative Medical Stores<br />
3. Kray Vikray Sahakari Samiti (KVSS)<br />
4. Medical shop runs by Red Cross societies<br />
5. Jan Aushadhi Kendra<br />
In Rajasthan the life-line fluid stores run by RMRS in govt. hospitals are<br />
already providing cheap injections and IV fluids. In 2004, the govt. instructed to<br />
upgrade these fluid stores to life-line drug stores i.e. apart from fluids they will<br />
also sell other drugs as well but these drug stores have come up only in few cities.<br />
Moreover, these are procuring and supplying medicines by brand names which are<br />
costly. If such stores are opened in all govt. hospitals and they procure and<br />
provide all essential drugs by generic name, then it will improve the supply of<br />
low cost medicines to the patients. Rates must be displayed prominently outside<br />
the stores. If these low cost generic medicines are made available at govt. stores<br />
counters the cost of medicines can be reduced to more than half in most cases and<br />
this price fall will come down to the extent of one tenth of the prevailing market<br />
rate in certain cases, like cetrizine and nimesulide. Once choice of low cost drugs is<br />
available to the consumer, market competition will ensure that private medical<br />
shops also reduce their prices.<br />
27
LOW COST MEDICINES INITIATIVE – CHITTORGARH<br />
TOP<br />
DISTRICT LEVEL INTERVENTIONS – THE MODEL<br />
We knew that the actual cost of most of the drugs is very low. But, these were not<br />
available to patients at low rates because of three obstacles:<br />
1. The doctors prescribe medicines by brand name of a particular drug company.<br />
This prevents competition and creates monopoly in the drug market and<br />
enables the drug company to put a very high MRP.<br />
2. As very high MRP is printed on the drugs, the chemists charge the same<br />
amount from the patient.<br />
3. Consumers are not aware that the actual cost of production of most of the<br />
drugs is very low. Moreover, once doctor has prescribed a particular brand, the<br />
patient has got no option, but to buy it, even when other low cost brands are<br />
available in the market. For example if doctor has prescribed a brand Glivec to<br />
a patient of blood cancer, a months course will cost Rs.1,14,400/- to the<br />
patient. Whereas, the same anti cancer drug, but with a different brand name<br />
Veenet costs just Rs.11,400/-. And Cipla supplies the generic equivalent of<br />
this drug (imitib) at Rs. 8,000/- & Gelnmark supplies it for Rs. 5,720/-!!!!!<br />
So, the district administration adopted the following strategy to provide low cost<br />
medicines to the patients. <strong>Generic</strong> medicines are on an average 5 times less the cost<br />
of branded medicines. We broke the monopoly of drug manufacturers by pursuing<br />
doctors to prescribe by the salt name and we made arrangements to sell medicines<br />
below the MRP at govt. drug counters and made consumer aware. This was done in<br />
three steps: -<br />
1. Ensuring that doctors prescribe drugs by generic (salt) name, as directed<br />
by the state govt.<br />
The state govt. has issued various circulars/ orders, which directs all govt.<br />
doctors to use generic names, instead of brand names.<br />
1. Circular No. P13 (108) M.E/gh1/98 dated 03.09.05<br />
2. Circular No. P4/PMF/2005/20VBOT/5892-0037 dated 26.09.05<br />
3. Circular No. P31(108) M.E./gh1/98 dated 18.08.05<br />
4. Circular No. F.22(1) M.R./96 dated 24.05.96<br />
5. Circular dated 24.04.02<br />
6. Circular dated 04.12.04<br />
7. Circular No HA/MR/ Circular05/10 dated 19.07.05<br />
8. Circular No chi/pra/05/MR/1802-1887 dated 01.09.05<br />
9. Circular No P(193)(a) RPMF/2005/6041-6107 dated 13.10.06<br />
10. Rule 32 of Raj.C.S.Medical (Attendance) Rules, 1970.<br />
The following issues were addressed before the project could take off.<br />
A. Quality<br />
A team of doctors was constituted to suggest the companies, which they<br />
believe, produce good quality drugs. Only these were procured and supplied<br />
at co-op. stores.<br />
B. Combination preparations<br />
Commonly used combination generic drugs were made available at co-op.<br />
stores.<br />
28
C. Chemists will give brand of his choice and will charge the printed MRP<br />
If the patient gets medicine from hospital supply or is educated to buy low<br />
cost drugs from co-op. store, the problem is no more. Once, patients<br />
understand that the same drugs are available at co-op. store at much<br />
cheaper rate, market competition ensures that the chemists also sell at<br />
lower rates. Eventually the patient benefits.<br />
TOP<br />
D. Govt. can put a ceiling on MRP<br />
This cannot be done at the state govt. level. Central govt. can do it using the<br />
provisions of Essential Commodities Act and Drug Price Control Order.<br />
Doctors were convinced that by the time a ceiling on MRP is put by the<br />
central government they should not wait and start helping their patients,<br />
specially the poor.<br />
2. Govt. Cooperative Medical Stores and Life-line drug stores (run by RMRS)<br />
provide low cost medicines of well reputed companies.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Medicines which are commonly used by the patients and prescribed by<br />
Doctors were listed after discussions with various medical specialists.<br />
A committee of doctors was consulted which recommended that drugs of<br />
reputed companies like Cipla, Cadila, Ranbaxy, German Remedies,<br />
Alembic, etc. can be purchased . (Initially 22 and now 57 companies are<br />
approved)<br />
Finally, the tender was floated for these medicines. The tender included<br />
564 generic medicines and more than 100 surgical and I.V. fluids.<br />
Cooperative store invited bids to purchase the drugs of these companies<br />
from the local stockists at competitive prices, after preparing comparative<br />
statement and finding out the most economical company (L1).<br />
The medicines are then sold at 20% profit margin to the patients. This<br />
money goes to the coop. deptt. and will make the project self sustainable.<br />
Thus, medicines of reputed drug manufacturers (which are unthinkably<br />
cheap) were made available at government co-op. medical stores for sale.<br />
Pricelists are displayed outside the coop. stores to advertise the rates and<br />
educate the patients.<br />
Once choice of low cost drugs is available to the consumer, market<br />
competition will ensure that private medical shops also reduce their prices.<br />
3. Awareness generation. Doctors were sensitized by organizing discussions.<br />
Training of co-op. pharmacists was carried out. The consumers were made<br />
aware by displaying boards showing comparative price lists and positive use of<br />
local electronic and print media.<br />
Quality control and Audit:-<br />
The quality control Officer is Dr. Dinesh Vaishnav who is assisted by drug<br />
Inspector Sh. Jain. This team ensures that the drugs of the companies approved by<br />
the committee of doctors only are available. So far 33 samples of generic drugs<br />
from various shops have been tested and all of them have been found to be of<br />
standard quality.<br />
29
THE IMPACT: many human lives saved<br />
TOP<br />
1. Medicines are available at unbelievably low prices, at govt. co-op. store, much<br />
below the printed market rate i.e. MRP. See the (illustrative) list.<br />
<strong>Generic</strong> Name of Drug<br />
<strong>Chittorgarh</strong><br />
Bhandar Rate*<br />
(Rs.)<br />
Unit<br />
MRP Printed on<br />
pack / strip (Rs.)<br />
Albendazole Tab IP 400 mg 1.37 1 tablet 25.00<br />
Alprazolam Tab IP 0.5 mg 1.75 10 tablets 14.00<br />
Arteether 2 ml Inj 11.72 1 Injection 99.00<br />
Amlodipine Tab 5 mg 3.12 10 tablets 22.00<br />
Cetrizine 10 mg 1.50 10 tablets 35.00<br />
Ceftazidime 1000 mg 64.90 1 Injection 370.00<br />
Atorvastatin Tab 20 mg 22.59 10 tablets 170.00<br />
Diclofenac Tab IP 100mg 2.75 10 tablets 25.00<br />
Diazepam Tab IP 5 mg 1.90 10 tablets 29.40<br />
Amikacin 500 mg 8.67 1 Injection 70.00<br />
2. Treatment cost of most illnesses falls sharply.<br />
3. Increase in number of patients getting free drugs from hospital supply.<br />
4. Decrease in expenditure from Rajasthan Pensioners Medical Fund (RPMF), so<br />
more patients can now be benefited.<br />
This can be made possible if two things happen simultaneously:<br />
Rational Prescription<br />
(by Doctor )<br />
1. Prescription of drugs by<br />
generic (salt) name.<br />
2. Prescription out of essential<br />
drugs list.<br />
3. As per Standard Treatment<br />
Guidelines.<br />
Low cost drugs made<br />
available<br />
(at govt. medical shops)<br />
1. Transparent procurement<br />
through open tender system.<br />
2. Distribution of Low cost<br />
drugs through Life Line/ Coop.<br />
Store.<br />
3. Display of Rates<br />
30
THE ULTIMATE SOLUTION: Statutory price control for all essential drugs TOP<br />
It is the government, which can provide medicines at an affordable cost and<br />
improve medicine accessibility. In India, an effective price control mechanism is a<br />
must, failing which the medicine accessibility will become less and lesser as most of<br />
the countrymen pay for medicines from their own pocket. The need is that Central<br />
Government should introduce a more effective drug pricing policy that would bring<br />
down the high profit margins for the pharmaceutical trade and make medicines more<br />
affordable for the common man.<br />
Liberalisation has nothing to do with a price protective mechanism in a sector<br />
as vital as healthcare. The medicines under national list of essential drugs must be<br />
kept under price control domain and the provision to control of newer necessary<br />
medicines useful in public health should be made.<br />
Supreme Court in its interim order dated, March 10, 2003 in Gopi Nath case<br />
has directed the central government to ensure that essential and life saving drugs<br />
are kept under price control. The fact that Karnataka High Court and subsequently<br />
Supreme Court stayed the implementation of pharmaceutical policy 2002<br />
questioning the stand of Government over the exclusion of many essential drugs<br />
under the ambit of price control speaks the importance of price controlled essential<br />
drugs in India. This is yet to be complied with.<br />
At present only 74 drugs have ceiling prices. If SC orders of 10 Mar.03 are<br />
complied with, it would result in control on ceiling prices (ie control on MRP) of about<br />
350 Essential Drugs and many other life saving drugs as well. Even if these drugs<br />
could be provided at affordable prices many more human lives could be saved.<br />
CONCEPT NOTE ON GENERIC DRUGS:<br />
COST EFFECTIVE ALTERNATE TO BRANDED DRUGS<br />
A <strong>Generic</strong> Drug is a copy that is the same as a brand name drug in dosage,<br />
safety, strength, how it is taken, quality, performance and intended use. <strong>Generic</strong><br />
simply means that the drug is not sold as the brand name, but it has the identical<br />
strength, dosage and route of administration and the same active ingredients as<br />
the brand-name drug. The use of generic drugs is now widely accepted and they are<br />
commonly prescribed by physicians and dispensed at hospitals. While<br />
manufacturing generic drugs, the drug companies use the same active ingredients<br />
and are shown to work the same way in the body, they have the same risks and<br />
benefits as their brand name counterparts. Also, generic drugs have the same<br />
quality, strength, purity and stability as brand name drugs. It is seen that <strong>Generic</strong><br />
Drugs work in the same way and in the same amount of time as branded drugs.<br />
The generic drugs are less expensive as compared to branded drugs as generic<br />
manufacturers do not have the investment costs of the developer of a new drug.<br />
New drugs are generally developed under patent protection. The patent protects<br />
the investment and the associated expense, viz. research, development,<br />
marketing and promotion. When patents are nearing expiration, manufacturers<br />
usually approach the Government/Drug Control Department to sell generic<br />
versions. In the process, the consumers get genetic drugs at substantially lower<br />
costs. Both branded and generic drugs are manufactured by conforming to<br />
International standards. Brand name drugs are usually given patent protection<br />
for 20 years from the date of submission of the patent. This provides protection<br />
for the innovator of such drugs to make good the initial costs incurred by him,<br />
31
viz., research development and marketing expenses, to develop the new drug.<br />
Many drug companies start manufacturing generic drugs once the patent<br />
license expires for a branded drug. The physician plays a vital role to determine<br />
whether his patient needs a branded drug or generic drug.<br />
TOP<br />
Patients should become assertive and insist upon the doctors to prescribe<br />
generic drugs if available, so that the patient would get the product at the best<br />
possible price. Pharmacists also play a vital role in educating the doctors about<br />
the availability of generic drugs. Thus the right medication could be given to the<br />
patients at the best possible price. <strong>Generic</strong>s are as good as branded drugs. Thus<br />
if generic drugs are bought by the patient, the patient may not lose money by<br />
going in for branded drugs, which are too costly. Health care costs continue to<br />
rise. Therefore, consumers, providers and policymakers need to assess the best<br />
way to keep health care affordable without adversely affecting access to quality<br />
care. With prescription drug (branded drug) costs serving as a major contributor<br />
to cost escalations,<br />
<strong>Generic</strong> drugs offer an important tool for reducing the rate of growth in<br />
overall health expenditure. <strong>Generic</strong> drugs play an important role in health care<br />
and the availability of generic drugs reduces the monopoly and oligopoly powers<br />
of the patent holder. The Government may also impose compulsory licensing so<br />
as to make available the much needed generic drugs. It is seen that many<br />
countries do not have the technological capability for manufacturing and<br />
supplying generic drugs even if the laws of those countries permit them to do<br />
so. It has also been found that prices fall substantially once the drugs are off<br />
the patent, if there are generic producers. When more generic producers enter<br />
the market, more is the fall in the prices.<br />
Differences between a Brand name Drug and a <strong>Generic</strong> Drug:<br />
• The innovator of a branded drug does research to discover the new<br />
biochemical substances that eventually become new drugs.<br />
• This research is essential for finding new and better treatments for various<br />
diseases. This process is expensive.<br />
• The expense incurred by a pharmaceutical industry for coming out with a<br />
branded drug is passed on to the consumer, but most of the money is<br />
ploughed back into research and development of new products.<br />
• In America, FDA grants the innovator company a patent of exclusivity making it the<br />
only company able to produce and sell the drug. The patent expires 20 years from the<br />
commencement of drug development to drug marketing. When it does, generic<br />
companies are then allowed to manufacture and sell the drug.<br />
• <strong>Generic</strong> drugs offer significant savings to consumers. The cost of generic<br />
drugs averages 40 to 60 per cent below the cost of the innovator or brand<br />
name drug.<br />
• It may be noted that the generic company’s version of the drug has the same<br />
active ingredient with the same chemical purity as the brand name drug.<br />
Obviously this results in cost savings for the generic as it does not involve<br />
doing research as was done by the original inventor. Also, it would cost less<br />
for the generic company to market its drugs and thus the savings passed on<br />
to the patient.<br />
• <strong>Generic</strong> drugs are regulated like band name drugs. Consequently, both are<br />
safe and effective when properly used.<br />
32
• <strong>Generic</strong> drugs today are manufactured by branded drug manufacturers also<br />
employing the same technology and processes. The only differences are the<br />
labeling, tablet or capsule design and the price.<br />
TOP<br />
• A generic drug is pharmaceutically and therapeutically equivalent to brand<br />
name drug<br />
Frequently Asked Questions about <strong>Generic</strong> Drugs<br />
1. Are generic drugs as safe as brand-name drugs<br />
Yes, since generics use the same active ingredients and are shown to work<br />
the same way in the body, they have the same safety and benefits as their<br />
brand-name counterparts.<br />
2. Are generic drugs as strong as brand-name drugs<br />
Yes, generic drugs to have the same quality, strength, purity and stability as<br />
brand-name drugs. The standards of quality, laid down in the<br />
pharmacopoeias are the same for branded and generic drugs.<br />
3. Do generic drugs take longer to work in the body<br />
No. <strong>Generic</strong> drugs work in the same way and in the same amount of time as<br />
brand-name drugs.<br />
4. Why are generic drugs less expensive<br />
<strong>Generic</strong>s cost less than brand-name drugs, mostly because manufacturers<br />
of generic drugs do not have the expense of research, development,<br />
advertisement and marketing related to a new drug. New drugs are<br />
developed under patent protection. The patent protects the investment by<br />
giving the company the sole right to sell the drug while it is in effect. As<br />
patents near expiration, other manufacturers can apply to sell generic<br />
versions. Because those manufacturers don't have the same development<br />
costs, they can sell their product at substantial discounts. Also, once generic<br />
drugs are approved, there is greater competition, which keeps the price<br />
down. Today, in U.S. almost half of all prescriptions are filled with generic<br />
drugs. <strong>Generic</strong> drugs save consumers an estimated $10 billion a year at<br />
retail pharmacies. Even more billions are saved when hospitals use<br />
generics.<br />
5. Are brand-name drugs made in more modern facilities than generic<br />
drugs<br />
No. Both brand-name and generic drug facilities must meet the same<br />
standards of good manufacturing practices. Drug authorities won't permit<br />
drugs to be made in substandard facilities. Inspections are conducted to<br />
ensure that prescribed standards are met. <strong>Generic</strong> firms have facilities<br />
comparable to those of brand-name firms. In fact, brand-name firms are<br />
linked to an estimated 50 percent of generic drug production. They<br />
frequently make copies of their own or other brand-name drugs but sell<br />
them without the brand name.<br />
33
6. Does every brand-name drug have a generic counterpart<br />
No. Brand-name drugs are generally given patent protection for 20 years<br />
from the date of submission of the patent. This provides protection for the<br />
innovator who laid out the initial costs (including research, development,<br />
and marketing expenses) to develop the new drug. However, when the patent<br />
expires, other drug companies can introduce competitive generic versions,<br />
but only after they have been thoroughly tested by the manufacturer and<br />
approved by the FDA.<br />
TOP<br />
7. Is my generic drug made by the same company that makes the brandname<br />
drug<br />
It is possible. Brand-name firms are responsible for manufacturing<br />
approximately 50 percent of generic drugs.<br />
8. Why do medicines have more than one name<br />
Medicines will often have more than one name:<br />
<br />
<br />
a generic name, which is the active ingredient of the medicine<br />
a brand name, which is the trade name the manufacturer gives to the<br />
medicine.<br />
The generic name is the official medical name for the active ingredient of the<br />
medicine. The brand name is chosen by the manufacturer, usually on the<br />
basis that it can be recognized, pronounced and remembered by health<br />
professionals and members of the public. An example would be Viagra - this<br />
is the well-known brand name given by Pfizer to the generic medicine<br />
sildenafil. (Brand names are capitalized; generic names are not.)<br />
9. How does this affect me<br />
When a doctor is writing a prescription, or a consumer is buying an overthe-counter<br />
medicine, they may have a choice between a branded medicine<br />
and the generic version of that medicine. <strong>Generic</strong> medicines are mostly<br />
cheaper than brand-name medicines, but the active ingredient (the<br />
ingredient that produces the therapeutic effect of the medicine) is the same<br />
in both. If your doctor has prescribed a medicine by its brand name, your<br />
pharmacist must dispense that brand. However, if a medicine has been<br />
prescribed by its generic name, your pharmacist can dispense whatever<br />
version of the medicine they have available, because each version will have<br />
the same therapeutic effect.<br />
34


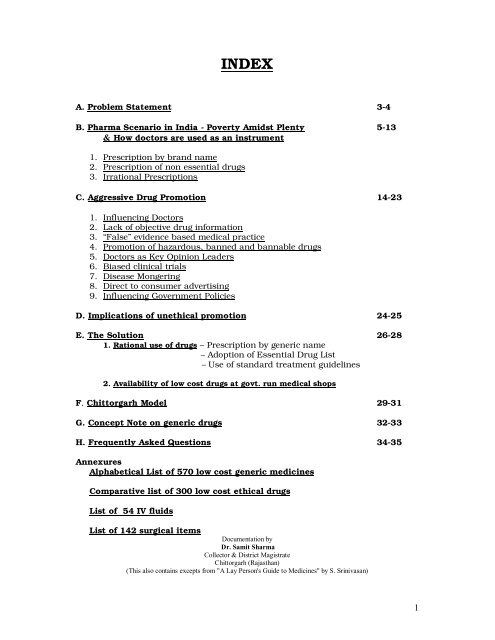

![Jheku uohu egktu] izc a/ k funs' kd] jhdks ftyk izH kkjh vf ... - Chittorgarh](https://img.yumpu.com/48385941/1/184x260/jheku-uohu-egktu-izc-a-k-funs-kd-jhdks-ftyk-izh-kkjh-vf-chittorgarh.jpg?quality=85)