Immune Thrombocytopenic Purpura - the European Oncology ...
Immune Thrombocytopenic Purpura - the European Oncology ...
Immune Thrombocytopenic Purpura - the European Oncology ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
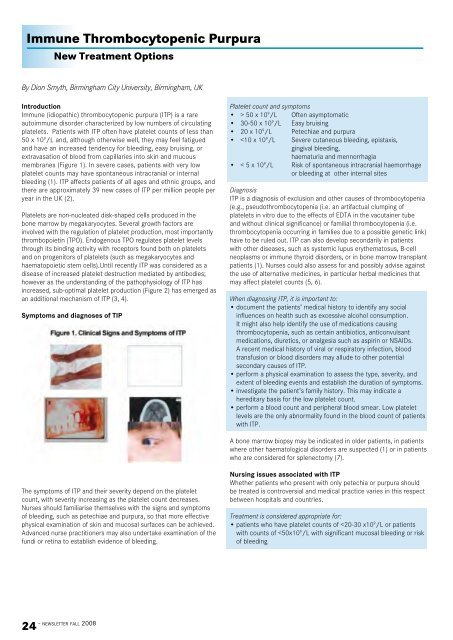
<strong>Immune</strong> <strong>Thrombocytopenic</strong> <strong>Purpura</strong><br />
New Treatment Options<br />
By Dion Smyth, Birmingham City University, Birmingham, UK<br />
Platelet count and symptoms<br />
Introduction<br />
24 - newsletter fall 2008<br />
<strong>Immune</strong> (idiopathic) thrombocytopenic purpura (ITP) is a rare • > 50 x 10 9 /L Often asymptomatic<br />
autoimmune disorder characterized by low numbers of circulating • 30-50 x 10 9 /L Easy bruising<br />
platelets. Patients with ITP often have platelet counts of less than • 20 x 10 9 /L Petechiae and purpura<br />
50 x 10 9 /L and, although o<strong>the</strong>rwise well, <strong>the</strong>y may feel fatigued<br />
and have an increased tendency for bleeding, easy bruising, or<br />
extravasation of blood from capillaries into skin and mucous<br />
•
• patients planning to undergo medical or dental procedures likely to<br />
provoke or bring about blood loss, such as <strong>the</strong> extraction of a tooth<br />
• patients with lifestyles associated with an increased risk of<br />
bleeding, such as those participating in hazardous or dangerous<br />
activities such as full-on contact sports.<br />
Current treatments for patients with ITP<br />
Currently, four treatment options that focus on reducing<br />
platelet destruction are commonly used: corticosteroids, anti-D<br />
immunoglobulin, intravenous immunoglobulins (IVIGs), and<br />
splenectomy. Corticosteroids, typically prednisone, are considered<br />
<strong>the</strong> first line of <strong>the</strong>rapy and are effective in 50-75% of patients.<br />
(8) Unfortunately, <strong>the</strong> long-term use of corticosteroids can be<br />
associated with various side effects, including hypertension, diabetes,<br />
osteoporosis, glaucoma, and in extreme cases, Cushing’s syndrome<br />
as well as an increased risk of infection associated with steroidinduced<br />
immunosuppression.<br />
Anti-D immunoglobulin is equally effective, but only in 70-75% of<br />
Rhesus+ patients in <strong>the</strong> non-splenectomised setting (4). IVIGs<br />
are recommended for patients unresponsive to corticosteroids, or<br />
those with severe bleeding (7). Possible side effects associated with<br />
immunoglobulins include fever, chills, headache, nausea, dyspnea,<br />
and chest pain. In rare cases, patients may develop acute kidney<br />
failure, aseptic meningitis, or haemolytic anaemia following <strong>the</strong><br />
administration of immunoglobulins.<br />
Splenectomy is an option for patients with severe ITP refractory to<br />
corticosteroids but <strong>the</strong> trend now is for more conservative medical<br />
management of patients. Patients can have a lifelong increased risk<br />
of infection following splenectomy, and 40-50% of splenectomised<br />
patients later relapse (1).<br />
Rituximab is not currently approved for <strong>the</strong> treatment of ITP but has<br />
demonstrated efficacy. (9,10). Approximately 45-65% of patients have<br />
a response to rituximab (11) but treatment can be complicated due<br />
to unpredictable patterns of response. Some patients have an early<br />
increase in platelet counts (after <strong>the</strong> first or second infusion) which<br />
peak between weeks 6 and 10; o<strong>the</strong>rs may have a late response<br />
where increases in platelet count are first achieved 6 to 8 weeks after<br />
treatment initiation and reached a peak count quickly.(12,13)<br />
New treatment options for patients with ITP<br />
New <strong>the</strong>rapies developed to address sub-optimal platelet production<br />
include growth factors that stimulate platelet production (4). The<br />
first recombinant TPO—manufactured by adding <strong>the</strong> relevant DNA<br />
into <strong>the</strong> existing genome of bacteria so that proteins are created<br />
that stimulate <strong>the</strong> production of platelets—was similar to endogenous<br />
TPO produced naturally in <strong>the</strong> body. The recombinant TPOs proved<br />
to be immunogenic and <strong>the</strong> body’s immune system identified <strong>the</strong><br />
recombinant TPO as ‘foreign’ leading to <strong>the</strong> production of autoantibodies<br />
and <strong>the</strong> destruction of endogenous TPO. The second<br />
recombinant TPO receptor agonist, romiplostim and <strong>the</strong> small<br />
molecule TPO receptor agonist, eltrombopag, currently in late phase<br />
clinical development have no structural similarity to endogenous TPO<br />
and do not stimulate an autoimmune response.<br />
Romiplostim<br />
Romiplostim is a thrombopoeisis-stimulating Fc-peptide fusion<br />
protein (peptibody) which binds to <strong>the</strong> TPO receptor on <strong>the</strong> surface<br />
of platelet-producing megakaryocytes (Figure 3). The binding of<br />
romiplostim activates cell signalling pathways which lead to activation<br />
of platelet production (4). Romiplostim is administered as a onceweekly,<br />
subcutaneous injection and <strong>the</strong> dose of romiplostim is<br />
individualised for each patient and <strong>the</strong>ir specific platelet level. The<br />
efficacy and safety of romiplostim (1μg/kg weekly) was investigated<br />
in two 24-week, parallel, placebo-controlled, double-blinded, phase<br />
III trials, one in splenectomised patients (romiplostim N= 42; placebo<br />
N = 21) and <strong>the</strong> o<strong>the</strong>r in non splenectomised patients (romiplostim<br />
N=41; placebo N= 21) (14). Patients could receive concurrent ITP<br />
<strong>the</strong>rapy with corticosteroids, azathioprine, and danazol. The primary<br />
endpoint of both studies was durable platelet response defined as<br />
a weekly platelet count of ≥ 50 x 10 9 /L during at least 6 of <strong>the</strong> last<br />
8 weeks of treatment, in <strong>the</strong> absence of rescue medication at any<br />
time during <strong>the</strong> study. Transient response was defined as 4 or more<br />
weekly platelet responses without a durable response from week<br />
2-25. Platelet responses that occurred within 8 weeks of rescue<br />
treatment were not included in any measures of platelet outcome.<br />
Altoge<strong>the</strong>r 83% of <strong>the</strong> romiplostim-treated patients achieved an<br />
overall platelet response (ei<strong>the</strong>r durable or transient) compared<br />
with 7% of patients receiving placebo (p
similar or worse compared with patients with diabetes or arthritis<br />
(19). Patients report that <strong>the</strong> bruising and bleeding resulting from ITP<br />
has a substantial negative effect on <strong>the</strong>ir quality of life, and fatigue<br />
(possibly due to <strong>the</strong> anaemia caused by bleeding) hinders <strong>the</strong>ir<br />
ability to perform <strong>the</strong>ir routine daily activities. (20). When presented<br />
with a patient with ITP, <strong>the</strong> nurse <strong>the</strong>refore has to help <strong>the</strong> patient<br />
adapt to <strong>the</strong> physical and psychosocial demands of <strong>the</strong> disease. The<br />
changes to body image associated with corticosteroid treatment,<br />
<strong>the</strong> implications of a potential splenectomy, rehabilitation, roles and<br />
responsibilities, and <strong>the</strong> risk of sepsis are examples of some of <strong>the</strong><br />
fears and concerns that nurses should be assessing and addressing<br />
when informing patients about, and explaining, different treatment<br />
options to patients with ITP. Keeping up to date with <strong>the</strong> developing<br />
and future <strong>the</strong>rapeutic options enables <strong>the</strong> nurse to educate and<br />
reassure <strong>the</strong> patient, <strong>the</strong>reby potentially alleviating fears of treatment<br />
failure or that eventual splenectomy is unavoidable.<br />
The long-term efficacy and safety of romiplostim are now being<br />
confirmed in an ongoing, open-label, extension study (15). The<br />
<strong>European</strong> Medicines Evaluation Agency is currently reviewing <strong>the</strong><br />
Marketing Authorisation Application for romiplostim. Romiplostim<br />
was recently approved for <strong>the</strong> treatment of adults with chronic ITP in<br />
<strong>the</strong> US and Australia.<br />
Eltrombopag<br />
Eltrombopag is a small molecule TPO receptor agonist that is<br />
administered orally once-daily. It activates <strong>the</strong> TPO receptor by<br />
binding to <strong>the</strong> transmembrane region. Although eltrombopag binds<br />
to <strong>the</strong> receptor differently than endogenous TPO or romiplostim, <strong>the</strong><br />
final pathways seem to be identical (4). The results from a 6-week<br />
treatment-period, placebo-controlled phase II trial where <strong>the</strong> primary<br />
end point was a platelet count of ≥50 x 10 9 /L on day 43 of treatment<br />
showed that 28%, 70%, and 81% of patients receiving, respectively,<br />
30 mg, 50 mg or 75 mg of eltrombopag daily achieved this endpoint<br />
(versus 11% in <strong>the</strong> placebo group). (16)<br />
When considering <strong>the</strong> management of <strong>the</strong> patient, two important<br />
Mild to moderate headache was <strong>the</strong> most commonly reported issues during <strong>the</strong> treatment of ITP arise: firstly, <strong>the</strong> need for treatment<br />
adverse event followed by aspartate aminotransferase elevation, concordance and secondly, regular platelet count monitoring. A onceweekly<br />
subcutaneous <strong>the</strong>rapy such as romiplostim may facilitate<br />
constipation, fatigue, and rash. Cataracts have been noted in both<br />
preclinical and clinical studies of eltrombopag, and elevated alanine concordance; it also combines treatment with frequent platelet<br />
transaminase in conjunction with raised bilirubin levels have been count monitoring and reinforces regular contact with medical staff<br />
observed in some patients treated with eltrombopag (17). Phase III which may be reassuring for <strong>the</strong> patient. This approach facilitates<br />
studies of eltrombopag are currently ongoing and <strong>the</strong> published data individually tailored and controlled dosing schedules and minimises<br />
are awaited soon.<br />
<strong>the</strong> risk of thrombosis that might occur if platelet counts increase<br />
(e.g. due to irregular drug intake).<br />
Discussion<br />
With <strong>the</strong> development of <strong>the</strong> TPO receptor agonists, <strong>the</strong> treatment In adults, ITP is a chronic disease often associated with a remitting<br />
options for patients with ITP have been widened. Current treatments – relapsing course. Many patients do not require treatment and <strong>the</strong><br />
can have many side effects and <strong>the</strong> treatment of ITP may result decision to introduce <strong>the</strong>rapeutic interventions will be based upon<br />
in increased morbidity from adverse effects and opportunistic <strong>the</strong> laboratory findings, clinical circumstances, and individual patient<br />
infections, which often surpass <strong>the</strong> problems actually caused by ITP risk factors. The development of <strong>the</strong> upcoming TPO receptor agonists<br />
(18). The phase III trials investigating romiplostim and <strong>the</strong> phase II provides patients with a new perspective to living with this chronic<br />
trials on eltrombopag show that TPO receptor agonists appear to be medical condition.<br />
well-tolerated and effective in patients with ITP (14, 16). As <strong>the</strong> TPO<br />
receptor agonists are not immunosuppressive agents, <strong>the</strong> problems Acknowledgements<br />
associated with immunosuppressive treatment can be avoided and This article was supported by Amgen Europe GmbH, Zug, Switzerland.<br />
<strong>the</strong> overall health of <strong>the</strong> patient better maintained.<br />
Author for Correspondence: 033 Bevan House, Birmingham City<br />
Both <strong>the</strong> symptoms of ITP and its treatment affect <strong>the</strong> quality of life University, Edgbaston , Birmingham, B15 3TN, UK E-mail: dion.<br />
of <strong>the</strong> patient; indeed <strong>the</strong> impact on quality of life is perceived as smyth@bcu.ac.uk<br />
26 - newsletter fall 2008
References<br />
1. Cines DB, McMillan R: Management of adult idiopathic<br />
thrombocytopenic purpura. Annu Rev Med 56:425-42, 2005.<br />
2. Kaye J, Schoonen M, Fryzek J: ITP incidence and mortality in<br />
UK general practice research database. Haematologica 92<br />
(Suppl.1):280 (Abstract 0751), 2007.<br />
3. Bussel J: Treatment of immune thrombocytopenic purpura in<br />
adults. Semin Hematol 43 (3 Suppl 5):S3-10; discussion S18-9,<br />
2006.<br />
4. Stasi R, Evangelista ML, Amadori S: Novel thrombopoietic agents:<br />
A review of <strong>the</strong>ir use in idiopathic thrombocytopenic purpura.<br />
Drugs 68 (7):901-12, 2008.<br />
5. Arnold J, Ouwehand WH, Smith GA, Cohen H. A young woman<br />
with petechiae. Lancet 352:618, 1998.<br />
6. Azuno Y, Yaga K, Sasayama T, Kimoto K. Thrombocytopenia<br />
induced by Jui,<br />
a traditional Chinese herbal medicine [Letter]. Lancet 354:304-5,<br />
1999.<br />
7. George J, et al.: Idiopathic thrombocytopenic purpura: a practice<br />
guideline developed by explicit methods for <strong>the</strong> American Society<br />
of Hematology [see comments]. Blood 88 (1):3-40, 1996.<br />
8. Cines DB, Blanchette VS. <strong>Immune</strong> thrombocytopenic purpura. N<br />
Engl J Med 346: 995-1008, 2002<br />
9. Provan D, et al.: Activity and safety profile of low-dose rituximab<br />
for <strong>the</strong> treatment of autoimmune cytopenias in adults.<br />
Haematologica 92 (12):1695-8, 2007.<br />
10. Godeau B, et al.: Rituximab efficacy and safety in adult<br />
splenectomy candidates with chronic immune thrombocytopenic<br />
purpura - results of a prospective multicenter phase 2 study.<br />
Blood:Epub ahead of print, 2008.<br />
11. Arnold DM, Dentali F, Crow<strong>the</strong>r MA, et al. Systematic Review:<br />
Efficacy and Safety of Rituximab for Adults with Idiopathic<br />
<strong>Thrombocytopenic</strong> <strong>Purpura</strong>. Ann Intern Med. 2007;146(1):25-33.<br />
12. Stasi R, Pagano A, Stipa E, et al. Rituximab chimeric anti-CD20<br />
monoclonal a ntibody treatment for adults with chronic<br />
idiopathic thrombocytopenic purpura. Blood. 2001;98(4):952-<br />
957. Clinical trial.<br />
13. Stasi R, Stipa E, Forte V, et al. Variable patterns of response<br />
to rituximab treatment in adults with chronic idiopathic<br />
thrombocytopenic purpura. Blood. 2002;99(10):3872-3873.<br />
14. Kuter DJ, et al.: Efficacy of romiplostim in patients with chronic<br />
immune thrombocytopenic purpura: a double-blind randomised<br />
controlled trial. Lancet 371 (9610):395-403, 2008.<br />
15. Newland C, et al.: Evaluating <strong>the</strong> long-term efficacy of<br />
romiplostim (AMG 531) in patients with chronic immune<br />
thrombocytopenic purpura (ITP) during an open-label extension<br />
study. Haematologica 93 (Suppl.1):377 (Abstract 0945), 2008.<br />
16. Bussel JB, et al.: Eltrombopag for <strong>the</strong> treatment of chronic<br />
idiopathic thrombocytopenic purpura. N Engl J Med 357<br />
(22):2237-47, 2007.<br />
17. FDA Oncologic Drug Advisory Committee Briefing Document.<br />
Promacta (Eltrombopag Tablets) http://www.fda.gov/ohrms/<br />
dockets/AC/08/briefing/2008-4366b1-02-GSK.pdf. Accessed<br />
July 21st 2008<br />
18. Portielje JEA, et al.: Morbidity and mortality in adults with<br />
idiopathic thrombocytopenic purpura. Blood 97 (9):2549-2554,<br />
2001.<br />
19. McMillan R, et al.: Self-reported health-related quality of life in<br />
adults with chronic immune thrombocytopenic purpura. Am J<br />
Hematol 83 (2):150-4, 2008.<br />
20. Mathias SD, et al.: Impact of chronic <strong>Immune</strong> <strong>Thrombocytopenic</strong><br />
<strong>Purpura</strong> (ITP) on health-related quality of life: a conceptual model<br />
starting with <strong>the</strong> patient perspective. Health Qual Life Outcomes<br />
Feb 8;6:13, 2008<br />
Update accreditation<br />
• Diploma of Advanced Studies Berner Fachhochschule in Onkologiepflege, Lindenhof Schule, Bern<br />
Switzerland, educational programme of study. For more information: www.lindenhof-schule.ch<br />
• Chemo<strong>the</strong>rapy course for oncology nurses, Estonian <strong>Oncology</strong> Nursing society, 14,15,16 April 2008,<br />
educational event<br />
• ESO “11 Internationales seminar: Onkologische pflege Fortgeschrittene Praxis”., September 2008,<br />
educational event. For more information: www.oncoconferences.ch<br />
newsletter fall 2008 -<br />
27