Anesthesiology Special book rEvIEwS - The IHE Website
Anesthesiology Special book rEvIEwS - The IHE Website
Anesthesiology Special book rEvIEwS - The IHE Website
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
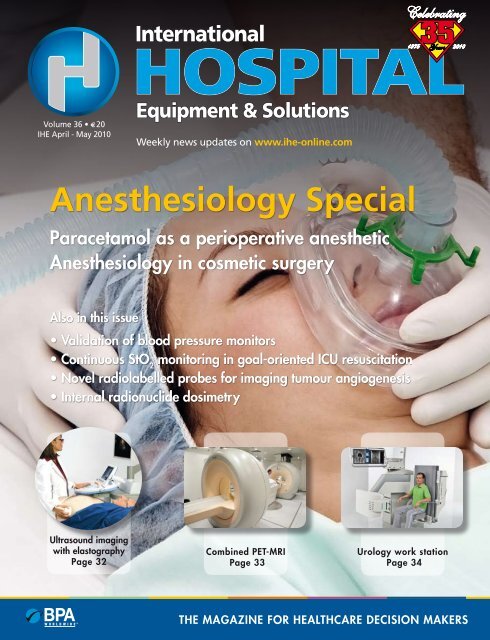
Volume 36 • E 20<br />
<strong>IHE</strong> April - May 2010<br />
also in this issue<br />
international<br />
hospital<br />
1975 2010<br />
Equipment & solutions<br />
Weekly news updates on www.ihe-online.com<br />
<strong>Anesthesiology</strong> <strong>Special</strong><br />
Paracetamol as a perioperative anesthetic<br />
<strong>Anesthesiology</strong> in cosmetic surgery<br />
• Validation of blood pressure monitors<br />
• Continuous StO 2 monitoring in goal-oriented ICU resuscitation<br />
• Novel radiolabelled probes for imaging tumour angiogenesis<br />
• Internal radionuclide dosimetry<br />
Ultrasound imaging<br />
with elastography<br />
Page 32<br />
Combined PET-MRI<br />
Page 33<br />
Celebrating<br />
Urology work station<br />
Page 34<br />
<strong>The</strong> Magazine for healThcare decision Makers
A New Class of Analytical Performance<br />
Patented* New Multi-Well TM Measuring<br />
Technology Creates Significant<br />
Performance Improvements<br />
• Eliminates Interferences From<br />
Hematocrit<br />
Maltose<br />
Oxygen<br />
Acetaminophen<br />
Ascorbic Acid<br />
Uric Acid<br />
• Eliminates Calibration Codes<br />
• Results Reported in 6 Seconds<br />
• Uses Only 1.2 Microliters of Sample<br />
• Advanced Meter Provides<br />
Flexible POC Control<br />
Color Touch Screen<br />
* Patented Technology<br />
Patents US 6,258,229 US 6,287,451 US 6,837,976 US 6,942,770<br />
EP 1 212 609 CA 2,375,089 CA 2,375,092<br />
www.ihe-online.com & search 45545<br />
Nova Hospital Glucose Monitoring System<br />
IN THE U.S., call toll-free 800-458-5813 or 781-894-0800 • IN CANADA, call toll-free 800-263-5999<br />
www.novastatstrip.com
It’s only ten years<br />
ago when they were<br />
first pronounced<br />
but already they<br />
seem to have faded<br />
away into history.<br />
As part of the<br />
apparently irresistible human reflex not<br />
to let an anniversary pass without taking<br />
the opportunity to summarize the<br />
past or to predict the future, the Millennium<br />
Development Goals (MDG) were<br />
solemnly adopted in 2000 by no fewer<br />
than 189 different countries, specifying<br />
eight global objectives that should<br />
be attained by 2015. Laudable as these<br />
objectives were, there were few details as<br />
to how exactly the objectives were to be<br />
reached, or, even more crucially, where<br />
the necessary investment and resources<br />
would come from. Of the eight MDG<br />
objectives, three were health-related,<br />
namely to reduce child mortality, to<br />
improve maternal health and to combat<br />
HIV/AIDS, malaria and other diseases,<br />
all of which are, of course, easier to say<br />
than do. Since 2000 there have been so<br />
many non health-related crises such<br />
as 9/11, wars, global recession, credit<br />
crunches, etc., not to mention numerous<br />
natural disasters such as tsunamis and<br />
earthquakes, that it is easy to overlook<br />
the particular MDG health goals and the<br />
progress being made to attain them.<br />
Luckily the assiduous statisticians at the<br />
World Health Organization (WHO)<br />
don’t get distracted and regularly produce<br />
their progress report on how<br />
close we are to achieving the MDG<br />
goals (www.who.int/topics/millenium_<br />
development_goals). <strong>The</strong> latest WHO<br />
progress report has just been published<br />
and, although there is some good news,<br />
there is little room for complacency.<br />
<strong>The</strong> percentage of underweight children<br />
is estimated to have declined from<br />
25% to 16% in 2010, and annual deaths<br />
of children under five years of age has<br />
fallen to 8.8 million, but it is estimated<br />
that 104 million children throughout the<br />
world are still under-nourished. Almost<br />
inevitably, however, the global results<br />
mask inequalities between countries<br />
and regions. For example, few developing<br />
countries (some of which have been<br />
held back by conflict, poor governance,<br />
or humanitarian and economic crises)<br />
Editor’s LEttEr 3 Apr/May 2010<br />
Progress report on the Millenium<br />
development Goals: must do better<br />
are on track to reach the MDG objectives<br />
for a reduction in maternal mortality<br />
although there has been progress in<br />
other countries. In the field of infectious<br />
diseases, the picture is also varied. While<br />
there has been a welcome decline in new<br />
HIV infections and TB mortality in non-<br />
HIV infected patients has dropped by<br />
approximately one third, the challenge<br />
of malaria remains particularly tough:<br />
there are still nearly a million malaria<br />
deaths per year and access to appropriate<br />
medication is still inadequate. With five<br />
years still to run till the 2015 deadline, a<br />
huge amount of progress still remains to<br />
be achieved.<br />
Comments<br />
on this article?<br />
please feel free to post them at<br />
www.ihe-online.com/comment/MDG<br />
Anywhere,<br />
when (you) need.<br />
Cardiovascular diseases are the world’s largest killers, claiming<br />
17.1 million deaths a year*. Over 40% are caused by heart attack<br />
in the presence of a witness. Today the de� brillator is one of the<br />
most effective solutions to help save life.<br />
* World Health Organization, Fact sheet No. 317, Sept, 2009<br />
www.progettimedical.com<br />
www.ihe-online.com & search 45478<br />
Rescue SAM<br />
Public access de� brillator<br />
Rescue Life<br />
Professional monitor de� brillator<br />
concept: www.glamlab.it
Contents<br />
FRONT COVER PRODUCTS<br />
[32] Ultrasound imaging<br />
with elastography<br />
FEATURES<br />
[6 - 11] PATiENT MONiTORiNg<br />
[33] Combined PEt- Mri [34] Urology Work<br />
station<br />
[6 - 7] Validation of blood pressure monitors.<br />
<strong>The</strong> ESH- IP: a success story and its future<br />
[8 - 11] Continuous StO 2 monitoring in goal-directed<br />
shock and ICU resuscitation<br />
[14 - 21] ANESThESiOlOgy SPECiAl<br />
[14] scientific literature review — anesthesiology<br />
[16 - 17] Paracetamol: a major role in peri-operative anesthesiology<br />
[18 - 21] <strong>Anesthesiology</strong> in cosmetic surgery<br />
[21] Book reviews:<br />
• Pediatric <strong>Anesthesiology</strong> review<br />
• Anesthesia student survival guide<br />
[22 - 26] NUClEAR MEDiCiNE<br />
[22 - 23] internal radionuclide dosimetry<br />
[24 - 26] Novel radiolabelled probes for imaging tumor angiogenesis<br />
[28 - 29] ENDOSCOPy<br />
[28 - 29] Enteroscopy: yesterday, today and tomorrow<br />
REgUlARS<br />
[3] Editor’s letter<br />
[12 - 13] News in brief<br />
[27] scientific literature review — hospital management<br />
[30 - 34] Product news<br />
[34] Calendar of upcoming events<br />
As part of <strong>IHE</strong>’s continuing policy of encouraging reader feedback, we are<br />
inviting our readers to post comments, suggestions or questions on our website.<br />
At the foot of each feature article in each issue of <strong>IHE</strong>, you will find a<br />
specific <strong>IHE</strong> web address for comments relating to the article in question.<br />
Comments on<br />
this article?<br />
If you have comments,<br />
additional data, alternative<br />
points of view or simply questions<br />
regarding the above article,<br />
please feel free to post them at<br />
www.ihe-online.com/comment/<br />
international<br />
hospital<br />
Equipment & solutions<br />
rue royale 326<br />
1030 Brussels, Belgium<br />
tel. +32-2-240 26 11<br />
Fax: +32-2-240 26 18<br />
www.ihe-online.com<br />
Managing Editors<br />
Alan Barclay, Ph.d.<br />
a.barclay@panglobal.be<br />
Frances Bushrod, Ph.d.<br />
Editorial and Advertising Coordinator<br />
Anna Hyrkäs, M.sc.<br />
Circulation Manager<br />
Arthur Léger<br />
Publisher / Editor in Chief<br />
Bernard Léger, M.d.<br />
Advertising Sales Manager<br />
Astrid Wydouw<br />
a.wydouw@panglobal.be<br />
Webmaster<br />
damien Noël de Burlin<br />
©2010 by PanGlobal Media bvba-sprl. Production &<br />
Lay-out by studiopress Communication, Brussels.<br />
Circulation Controlled by Business of<br />
Performing Audits, shelton, Ct, UsA.<br />
the publisher assumes no responsibility for opinions or statements<br />
expressed in advertisements or product news items.<br />
the opinions expressed in by-lined articles are those of the<br />
author and do not necessarily reflect those of the publisher. No<br />
conclusion can be drawn from the use of trade marks in this<br />
publication as to whether they are registered or not.<br />
issN 0306-7904<br />
CoMiNG UP iN JUNE 2010<br />
Cardiology special<br />
Pediatrics<br />
Ultrasound<br />
For submission of editorial material, contact Alan<br />
Barclay at a.barclay@panglobal.be<br />
For advertising information, go online to<br />
www.ihe-online.com, simply click on ‘Magazine’<br />
and ‘Media information’ or contact<br />
Astrid Wydouw at a.wydouw@panglobal.be<br />
Free Subscription for<br />
Healthcare professionals<br />
Healthcare professionals are entitled to receive<br />
iHE’s digital edition for the next 12 months<br />
completely free of charge. to begin a new<br />
subscription or to continue your existing free<br />
subscription go to<br />
www.ihe-online.com<br />
Click on Free subscription and follow instructions
www.ihe-online.com & search 45558
Apr/May 2010<br />
Blood pressure measurement and<br />
protocols for device validation<br />
Blood pressure measurement is widely used<br />
across the healthcare system, by clinicians of<br />
almost all specialties, nurses, medical assistants<br />
and even patients themselves. People with high<br />
blood pressure generally have their blood pressure<br />
measured in the office or clinic and because<br />
of the phenomenon of “white coat hypertension”,<br />
such measurements are often falsely elevated,<br />
so 24-hour ambulatory blood pressure<br />
monitoring and/or self-monitoring by patients<br />
at home is often recommended [1]. In all cases,<br />
the accuracy of the blood pressure monitor is<br />
therefore an important prerequisite for the reliable<br />
assessment of the level of blood pressure so<br />
as to enable the accurate diagnosis of high blood<br />
pressure and to enable reliable decision making<br />
and long-term drug treatment [1].<br />
In 1987 the US Association for the Advancement<br />
of Medical Instrumentation (AAMI) published<br />
the first protocol for formal validation of<br />
all blood pressure monitors against the mercury<br />
standard [2]. This was followed in 1990 by the<br />
British Hypertension Society (BHS) protocol<br />
[3] and revised versions of these protocols were<br />
published in 1993. In 2002, the European Society<br />
of Hypertension Working Group on Blood<br />
Pressure Monitoring published the International<br />
Protocol (ESH-IP) for the validation of blood<br />
pressure monitors [4]. <strong>The</strong> ESH-IP was developed<br />
on the evidence of a large number of validation<br />
studies performed using the AAMI and<br />
BHS protocols. <strong>The</strong> purpose of developing the<br />
ESH-IP protocol was to simplify the validation<br />
procedure and reduce the sample size required<br />
without losing the evaluation accuracy of the<br />
previous more complicated, cumbersome and<br />
costly protocols. In the rapidly expanding market<br />
6 BLood PrEssUrE MoNitoriNG<br />
EsH-iP for the validation of blood<br />
pressure monitors:<br />
a success story and its future<br />
the validation of blood pressure monitors is an important prerequisite for the accurate<br />
measurement of blood pressure. in the last decade the European society of<br />
Hypertension international Protocol (EsH-iP) has expanded the device validation<br />
procedure worldwide by three to four-fold compared to the period before its original<br />
publication in 2002 and is now the preferred validation protocol. in keeping<br />
with improvements in device technology, the international Protocol was revised, in<br />
2010 and imposes stricter requirements for device accuracy.<br />
by dr G.s. stergiou, dr N Karpettas, dr N Atkins and dr E. o’Brien<br />
of blood pressure monitors for home, ambulatory<br />
and office measurements, it was anticipated<br />
that such a simplified protocol would facilitate<br />
greater use of the validation procedure by more<br />
centers throughout the world, thereby facilitating<br />
independent validation of greater numbers<br />
of devices.<br />
Application of the ESH-IP for device<br />
validation (2002-2009)<br />
A systematic review of the use of the ESH-IP<br />
for validating blood pressure measuring devices<br />
was recently performed [5]. <strong>The</strong> review covered<br />
the number of reported validation studies<br />
(compared to the use of other protocols), the<br />
main study results, the performance in following<br />
the protocol’s requirements and criteria, the<br />
problems in data reporting, the issues within<br />
the protocol that might need modification or<br />
clarification, and the impact of applying more<br />
stringent validation criteria. This analysis, which<br />
relies on data from 104 validation studies conducted<br />
using the protocol between 2002 (ESH-<br />
IP publication) and 2009, forms the basis for the<br />
recommendations in the revised ESH-IP [5].<br />
According to the systematic review, within 8<br />
years after the publication of the ESH-IP there<br />
were 48 studies reported using the BHS protocol,<br />
38 using the AAMI and 104 using the ESH-<br />
IP [5]. In particular, between January 2007 and<br />
June 2009, 29 studies have been reported using<br />
the BHS and/or the AAMI protocols compared<br />
to 67 using the ESH-IP [5]. Thus, it appears<br />
that the ESH-IP has succeeded in expanding<br />
the validation procedure worldwide by three<br />
to four-fold compared to the period before its<br />
publication [5] and now is the preferred validation<br />
protocol. A total of 26 different research<br />
groups performed ESH-IP studies and evaluated<br />
devices from 32 different manufacturers [5].<br />
Whether a blood pressure monitor is designed for use by a healthcare professional or by the patient himself,<br />
it is vital that the monitor be validated. <strong>The</strong> European Society of Hypertension<br />
International Protocol (ESH-IP) is now the most widely used protocol for BP monitor validation.<br />
<strong>The</strong> 2010 revision to the protocol tightens the validation criteria
ESH-IP validations have been conducted in 18<br />
countries, the vast majority of them in Europe<br />
(70%), with some in the USA, in China and<br />
elsewhere [5]. Of these studies, 80% validated<br />
oscillometric devices, 80% upper arm devices<br />
(the rest being wrist devices); 65% of devices<br />
were designed for self-home monitoring, 20%<br />
were professional devices for office/clinic use<br />
and 15% were for ambulatory blood pressure<br />
measurement [5].<br />
Interestingly, the proportion of the reported<br />
validation studies that fulfilled the ESH-IP criteria<br />
is impressively high (85%) [5]. This success<br />
might reflect improved accuracy of devices<br />
due to advancement in technology. However,<br />
other reasons are possible, such as a publication<br />
bias whereby negative studies are not published,<br />
and that the ESH-IP criteria are too easy<br />
to fulfil and need to be made more stringent.<br />
<strong>The</strong>re were also problems in conducting and<br />
reporting some of the ESH-IP validation studies<br />
that make the interpretation of the results rather<br />
questionable. A total of 21 different types of violations<br />
of the ESH-IP were detected, appearing<br />
33 times and involving 23 studies [5]. Twenty<br />
per cent of the violations were regarded as major<br />
(affecting the protocol integrity, requirements<br />
and stringency of criteria), whereas the rest<br />
were minor with negligible impact [5]. Some of<br />
the studies did not provide a complete report of<br />
recruited and excluded subjects and others did<br />
not report the cuff sizes used, particularly for<br />
observer measurements. <strong>The</strong>se findings suggest<br />
that a more standardized report of the validation<br />
study results is necessary.<br />
With the aim of determining which of the ESH-<br />
IP validation criteria were easily passed by the<br />
currently available accurate devices and which<br />
were only marginally passed, several ‘arbitrarily<br />
chosen’ changes in all the validation criteria<br />
of the protocol were tested [5]. <strong>The</strong> impact of<br />
applying these arbitrary criteria on the evaluation<br />
of devices that had passed the ESH-IP in<br />
published validation studies was also investigated<br />
and helped to decide on which criteria to<br />
tighten in the revision of the ESH-IP.<br />
ESH-IP revision 2010<br />
On the basis of these analyses a revised version<br />
of the protocol was published in February<br />
2010 [6]. <strong>The</strong>re are several changes in the<br />
revised protocol, regarding participants’ age,<br />
blood pressure limits for inclusion, distribution<br />
of observer blood pressure measurements and<br />
validation results reporting [6]. However, the<br />
most challenging change is the tightening of<br />
the validation criteria for the pass level. It has<br />
been estimated that about one third of validations<br />
that passed the ESH-IP 2002 will not satisfy<br />
the criteria of the revised ESH-2010 (Stergiou<br />
G, et al. unpublished data 2010). Thus, the<br />
application of the revised ESH-IP is expected<br />
to more than double the validation fail rate.<br />
Indeed it appears that time has come to increase<br />
the level of minimal accuracy requirements for<br />
device approval. First, 85% of the devices tested<br />
so far using the ESH-IP have been successful<br />
[5], implying an improvement in current technology<br />
of blood pressure monitors (although<br />
as mentioned above a publication bias cannot<br />
be excluded). Second, a recent analysis of successful<br />
ESH-IP validation studies showed a<br />
trend towards an improvement in accuracy of<br />
the electronic devices in the period between<br />
2002-2010, as assessed by their performance in<br />
passing several validation criteria (Stergiou G,<br />
et al. unpublished data 2010).<br />
Conclusions<br />
Eight years after its publication, the ESH-IP<br />
has proven to be successful in achieving its<br />
goals. <strong>The</strong> large number of published studies,<br />
devices tested, and investigators involved<br />
indicate that the protocol has succeeded in<br />
expanding the validation procedure worldwide<br />
by three to four-fold compared with the<br />
period before its initial publication. However,<br />
there is a need to tighten the accuracy criteria<br />
so as to encourage the manufacture of better<br />
devices and there is also a need to improve the<br />
validation methodology by standardizing the<br />
reporting of validation studies. <strong>The</strong>se issues<br />
have been successfully addressed in the 2010<br />
revision of the ESH-IP.<br />
References<br />
1. O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM,<br />
Mancia G, et al. European Society of Hypertension<br />
recommendations for conventional, ambulatory<br />
and home blood pressure measurement. J Hypertens<br />
2003;21:821-48.<br />
2. Association for the Advancement of Medical<br />
Instrumentation. <strong>The</strong> national standard of electronic<br />
or automated sphygmomanometers. Arlington,<br />
VA: AAMI;1987.<br />
3. O’Brien E, Petrie J, Littler W, De Swiet M, Padfield<br />
P, O’Malley K, et al. <strong>The</strong> British Hypertension<br />
Society protocol for the evaluation of automated<br />
and semi-automated blood pressure measuring<br />
devices with special reference to ambulatory systems.<br />
J Hypertens 1990;8:607-19.<br />
4. O’Brien E, Pickering T, Asmar R, Myers M, Parati<br />
G, Staessen J, et al. European Society of Hypertension<br />
International Protocol for validation of blood<br />
pressure measuring devices in adults. Blood Press<br />
Monit 2002;7:3-17.<br />
5. Stergiou G, Karpettas N, Atkins N, O’Brien E. European<br />
Society of Hypertension International Protocol<br />
for the validation of blood pressure monitors:<br />
a critical review of its application and rationale for<br />
revision. Blood Press Monit 2010;15:39-48.<br />
6. O’Brien E, Atkins N, Stergiou G, Karpettas N, Parati<br />
G, Asmar R, et al. European Society of Hypertension<br />
International Protocol revision 2010 for the<br />
7 Apr/May 2010<br />
validation of blood pressure measuring devices in<br />
adults. Blood Press Monit 2010;15:23-38.<br />
<strong>The</strong> authors<br />
George S. Stergiou 1 * MD, FRCP,<br />
Associate Professor of Medicine & Hypertension<br />
Nikos Karpettas 1 MD, Clinical Research Fellow<br />
Neil Atkins 2 PhD, Statistician<br />
Eoin O’Brien 3 Professor of Molecular Pharmacology<br />
1 Hypertension Center, Third University Department<br />
of Medicine, Sotiria Hospital, Athens,<br />
Greece.<br />
2 dabl Ltd, 34 Main Street, Blackrock, Co. Dublin,<br />
Ireland.<br />
3 Conway Institute of Biomolecular & Biomedical<br />
Research, University College Dublin, Ireland.<br />
* Corresponding author:<br />
George S. Stergiou, MD<br />
Hypertension Center<br />
Third University Department of Medicine<br />
Sotiria Hospital<br />
152 Mesogion Avenue<br />
Athens 11527, Greece<br />
Tel: +30 210 7763117<br />
E-mail: gstergi@med.uoa.gr<br />
Comments on this article?<br />
Feel free to post them at<br />
www.ihe-online.com/comment/ESH-IP<br />
This disposable<br />
Eschmann-style<br />
“bougie” is used<br />
to guide the<br />
endotracheal<br />
tube during<br />
difficult<br />
intubations. <strong>The</strong><br />
tube slides over<br />
the introducer<br />
which helps to<br />
guide the way,<br />
especially<br />
helpful for<br />
“blind”<br />
intubations.<br />
straight curved Malleable<br />
U.S.A. 813-889-9614 • Fax 813-886-2701<br />
www.ihe-online.com & search 45555
Apr/May 2010<br />
Near-infrared Spectroscopy (NIRS) has<br />
emerged as a new monitoring tool that is a reliable,<br />
noninvasive means of continuously measuring<br />
tissue perfusion. In this review we summarize<br />
our experience with the value of StO 2<br />
monitoring in a number of settings including<br />
a) ICU shock resuscitation, b) predicting outcomes<br />
in the emergency department, c) ICU<br />
sepsis resuscitation.<br />
ICU traumatic shock resuscitation<br />
In the 1980s, William Shoemaker wrote a<br />
series of papers addressing the use of physiological<br />
monitoring to predict outcome and<br />
assist in clinical decision making [1-3]. He<br />
identified two key variables, oxygen delivery<br />
(DO 2 ) and oxygen consumption (VO 2 ),<br />
as predictors of survival and popularised<br />
“supranormal oxygen delivery” as a resuscitation<br />
strategy. He proposed that unrecognised<br />
flow-dependent oxygen consumption<br />
contributed to the devel opment of multiple<br />
organ failure (MOF) and believed that this<br />
deficit could be corrected by maximising<br />
DO 2 [2, 3]. Although, it is now recognised<br />
that resuscitation to achieve supranormal<br />
indices is not beneficial in all patients, the<br />
use of physiological parameters to guide<br />
resuscitation and predict outcomes is central<br />
to all ICU resuscitation.<br />
<strong>The</strong> introduction of new technology into<br />
intensive care units, including continuous<br />
venous oximetry and continuous cardiac<br />
output monitoring with PA catheters [4] permitted<br />
wide spread use of oxygen transport<br />
variables to guide resuscitation. In an effort<br />
to further refine the logic for traumatic shock<br />
resuscitation, surgical intensivists employed<br />
computerised clinical decision support to<br />
prospectively collect data on responders and<br />
nonresponders and optimise resuscitation<br />
strategies. Computerised protocols also provided<br />
the opportunity to test the utility of<br />
various monitors in shock resuscitation, such<br />
8 PAtiENt MoNitoriNG<br />
Continuous sto 2 monitoring in goaldirected<br />
shock and iCU resuscitation<br />
throughout the years, iCU technology has allowed physicians to obtain reliable<br />
physiological parameters to guide goal-oriented iCU resuscitation. A number of<br />
studies have validated the use of tissue hemoglobin oxygen saturation (sto 2 ) as a<br />
reliable index of tissue perfusion. sto 2 monitoring offers a continuous assessment<br />
of the adequacy of ongoing shock resuscitation and aids in early identification of<br />
high-risk patients in septic and hemorrhagic shock.<br />
by dr rachel J. santora and dr Frederick A. Moore<br />
as the tissue hemoglobin oxygen saturation<br />
(StO 2 ) monitor. Prospective studies utilising<br />
protocol-driven shock resuscitation demonstrated<br />
that changes in skeletal muscle StO 2<br />
showed a strong correlation with changes in<br />
DO 2 , blood base deficit (BD, and lactate. This<br />
observation that the StO 2 as an index of perfusion<br />
that tracks DO 2 during active resuscitation<br />
led laboratory investigators to explore the<br />
role of StO 2 monitors in large animal models<br />
of hemorrhagic shock [5].<br />
In these studies, hemodynamic and NIR<br />
spectroscopic measurements were used to<br />
identify early predictors of irreversible shock.<br />
Measurements of hind-limb StO 2 in each<br />
group diverged within 30 minutes of shock,<br />
such that by the end of the 90 minute period,<br />
the StO 2 value for unresuscitatable remained<br />
low despite resuscitation. Animals destined<br />
to survive shock and resuscitation did not<br />
exhibit an irreversible decline in StO 2 . <strong>The</strong>se<br />
findings demonstrate that skeletal StO 2 is a<br />
reliable, noninvasive means for early differentiation<br />
between resuscitatable and nonresuscitatable<br />
animals. Similarly, studies utilising<br />
noninvasive StO 2 to guide fluid resuscitation<br />
after traumatic shock showed StO 2 as<br />
a reliable assessment tool to determine the<br />
adequacy of shock resuscitation in response<br />
to colloids [6].<br />
Taken together these clinical and research<br />
data suggest that StO 2 (derived from a noninvasive<br />
monitor) could provide information<br />
about the effectiveness of resuscitation<br />
equivalent to that of a invasive PA catheter or<br />
serial blood draws to measure base deficit or<br />
lactate levels.<br />
Predicting outcomes in MOF<br />
Post injury Multiple Organ Failure is well<br />
recognized as a significant cause of mortality<br />
following traumatic injury. In an effort to<br />
identify critically ill patients at risk, a number<br />
of studies focused on identifying early predictors<br />
of postinjury MOF [7,8]. Through a<br />
series of studies, investigators determined<br />
base deficit as the earliest independent predictor<br />
of postinjury MOF [9], an observation<br />
that was validated by a number of clinical<br />
studies [10].<br />
With this in mind, Cohn et al decided to perform<br />
a study using StO 2 monitoring in the<br />
<strong>The</strong> use of modern oxygenation monitors to determine StO 2 levels can identify life-threatening conditions before<br />
there are any visible clinical signs.
emergency room to determine if it could predict<br />
MOF [11]. <strong>The</strong> group performed a prospective<br />
observational study involving seven<br />
US trauma centers evaluating the efficacy of<br />
thenar StO 2 as an early predictor of MOF in<br />
major torso trauma patients compared to the<br />
accepted standard (base deficit). StO 2 monitors<br />
were placed upon arrival and MOF and death<br />
were the primary outcomes. <strong>The</strong>y determined<br />
that 1) StO 2 was equal to base deficit analysis<br />
for predicting MOF development and 2) StO 2<br />
out-performed both base deficit and systolic<br />
blood pressure as an early predictor of death<br />
[11]. Subset analysis comparing StO 2 levels to<br />
lactate levels also validated StO 2 as an early predictor<br />
of death when compared to conventional<br />
parameters[12].<br />
Figure 1<br />
(A)<br />
(B)<br />
24h Sepsis Protocol<br />
24 Hour Sepsis Protocol- First 12 Hours<br />
From these observations, we conclude that<br />
StO 2 obtained within the first hour after ED<br />
admission is an equally reliable predictor of<br />
adverse outcomes as the more conventionally<br />
used parameters of lactate and base deficit in a<br />
continuous, noninvasive fashion.<br />
ICU sepsis resuscitation and the role<br />
of the StO 2 monitor<br />
In recent years, it has been recognized that<br />
severe sepsis and septic shock are the leading<br />
cause of ICU mortality [13-16]. Recent efforts<br />
have been directed at updating the surviving<br />
sepsis campaign guidelines and improving<br />
early delivery [16]. To assist with consistent<br />
implementation of these interventions, surgical<br />
intensivists at the Methodist Hospital in<br />
Physiologic Parameters Interventions<br />
Hour MAP CVP HR StO 2 [Hb] LR Hextend PRBCs<br />
1 103 10 150 58 10.1 1000<br />
2 93 11 158 57 1000<br />
3 77 15 99 51<br />
4 77 10 151 61 9.0 1000 1 unit<br />
5 73 8 140 69 500<br />
6 71 9 141 66 7.9 500 1 unit<br />
7 67 11 134 67 250<br />
8 67 8 140 68 9.4 250<br />
9 69 9 134 71 250<br />
10 70 12 117 71<br />
11 69 11 109 72<br />
12 71 12 106 69 9.6<br />
Figure 1 A & B: Case Report<br />
StO 2 tracings over the first 36 hours of postoperative ICU admission, where the first 24 hours represents<br />
ongoing resuscitation with our sepsis protocol (A). Physiologic Parameters and Interventions corresponding<br />
with the StO 2 tracings above (B); Hour, hour on sepsis resuscitation protocol; MAP, mean arterial pressure;<br />
CVP, central venous pressure; HR, heart rate; StO 2 , skeletal muscle tissue hemoglobin saturation; [Hb],<br />
hemoglobin concentration; LR, lactated ringers; PRBCs, packed red blood cells.<br />
9 Apr/May 2010<br />
Houston, TX, USA have developed a computerized<br />
clinical decision support application.<br />
To facilitate early identification of sepsis and<br />
facilitate implantation of this support application,<br />
a three step screening process was<br />
developed to collect physiologic parameters<br />
that characterize the systemic inflammatory<br />
response syndrome (SIRS) and to compile a<br />
SIRS score. If the SIRS score exceeds 4, efforts<br />
are focused on ascertaining presence of an<br />
infection. For patients that are identified as<br />
having sepsis, the computerized clinical decision<br />
support application is utilized to implement<br />
our sepsis protocol and provide a tool<br />
for ongoing assessment.<br />
Our current sepsis protocol is composed of two<br />
distinct phases. Phase one is for management<br />
of simple sepsis; it dictates that the patient get<br />
appropriate cultures, antibiotics, a fluid challenge<br />
and repeat laboratory determinations.<br />
Phase two of our protocol is for septic shock,<br />
which is much more complex and is a data<br />
driven protocol that insures the appropriate<br />
use of fluid resuscitation, inotropes, vasopressors<br />
and testing for adrenal insufficiency. In<br />
this setting, we have been using StO 2 data and<br />
have found it to provide valuable information<br />
regarding the adequacy of resuscitation.<br />
<strong>The</strong> following case presentation emphasizes the<br />
ability of StO 2 monitoring to detect life-threatening<br />
clinical deterioration before derangement<br />
of other physiologic parameters.<br />
Case Report: A 38 year old man who initially<br />
presented with pancreatitic necrosis and retroperitoneal<br />
abscesses managed with IV antibiotics<br />
and percutaneous drainage, was transferred<br />
to our institution after developing severe sepsis<br />
from methicillin resistant staphylococcus<br />
aureus (MRSA) bacteremia. Upon arrival in<br />
our ICU, we implemented our sepsis protocol<br />
and he responded to our sepsis resuscitation.<br />
Despite improved percutaneous drainage<br />
for source control, he continued to have SIRS,<br />
characterized by spiking temperatures and<br />
tachycardia. He remained ventilator dependent<br />
and required ongoing dialysis. Based on<br />
repeat CT scans, the left IR drain was upsized<br />
to a chest tube in the ICU for improved source<br />
control. As his SIRS resolved, he was weaned<br />
from the ventilator and his renal failure also<br />
resolved. <strong>The</strong> patient was transferred to the<br />
floor with tachycardia and purulent drainage<br />
material from the left chest tube. Repeat CT<br />
showed resolution of the upper retroperitoneal<br />
abscesses, however lower retroperitoneal<br />
abscesses extending into his scrotum were now<br />
present. After operative drainage and debridement<br />
of these retroperitoneal fluid collections<br />
through a bilateral groin retroperitoneal exploration,<br />
he was readmitted to the intensive care<br />
unit for worsening sepsis and was placed on<br />
phase II of our sepsis protocol.
Apr/May 2010<br />
Figure 1 illustrates the StO 2 tracings over the<br />
first 36 hours, where the first 24 hours represents<br />
ongoing resuscitation with our sepsis<br />
protocol. <strong>The</strong> patient initially dropped his<br />
StO 2 as he became septic, and it rose up to the<br />
70 range over the first 4 hours with ongoing<br />
resuscitation. <strong>The</strong>re was some variability over<br />
the next several hours and then the StO 2 value<br />
increased and plateaued and remained constant<br />
until the completion of this sepsis protocol.<br />
Following sepsis resuscitation, the StO 2<br />
monitor was left in place. That evening the<br />
patient remained persistently tachycardic, his<br />
urine output decreased and his hemoglobin<br />
Figure 1<br />
(A)<br />
(B)<br />
24h Sepsis Protocol<br />
10<br />
concentration decreased from 9.6 to 7.9. During<br />
this time he received three 500ml boluses<br />
of isotonic crystalloid. Initially the decrease in<br />
hemoglobin was attributed to hemodilution;<br />
due to his persistent tachycardia, he was given<br />
2 units of packed red blood cells. At 6 am the<br />
next morning the ICU resident examined the<br />
patient, noted the patient to be persistently<br />
tachycardic but with a good MAP and adequate<br />
urine output. His dressings were noted<br />
to be nonsanguinous, however, at 8 am, during<br />
ICU team rounds the dressing was soaked<br />
with blood. <strong>The</strong> patient returned to operating<br />
room for immediate exploration and was<br />
24 Hour Sepsis Protocol- First 12 Hours<br />
Physiologic Parameters Interventions<br />
PAtiENt MoNitoriNG<br />
Hour MAP CVP HR StO 2 [Hb] LR Hextend PRBCs<br />
1 103 10 150 58 10.1 1000<br />
2 93 11 158 57 1000<br />
3 77 15 99 51<br />
4 77 10 151 61 9.0 1000 1 unit<br />
5 73 8 140 69 500<br />
6 71 9 141 66 7.9 500 1 unit<br />
7 67 11 134 67 250<br />
8 67 8 140 68 9.4 250<br />
9 69 9 134 71 250<br />
10 70 12 117 71<br />
11 69 11 109 72<br />
12 71 12 106 69 9.6<br />
Figure 1 A & B: Case Report<br />
StO 2 tracings over the first 36 hours of postoperative ICU admission, where the first 24 hours represents ongoing<br />
resuscitation with our sepsis protocol (A). Physiologic Parameters and Interventions corresponding with the<br />
StO 2 tracings above (B); Hour, hour on sepsis resuscitation protocol; MAP, mean arterial pressure; CVP, central<br />
venous pressure; HR, heart rate; StO 2 , skeletal muscle tissue hemoglobin saturation; [Hb], hemoglobin<br />
concentration; LR, lactated ringers; PRBCs, packed red blood cells.<br />
found to have a small arterial bleeder that was<br />
ligated. Postoperative mesenteric angiography<br />
confirmed that there was no pseudoaneurysm<br />
or sources of ongoing bleeding. After<br />
reviewing the StO 2 tracing, at approximately 8<br />
pm prior to this event, there was a presumptuous<br />
drop in StO 2 from 70 down to 35. With<br />
ongoing fluid resuscitation and blood transfusions<br />
the StO 2 value and went back up to 70<br />
[Figure 2].<br />
However, in the early morning hours, the StO 2<br />
number began to drift downwards prior to<br />
recognition of the patient’s ongoing bleeding.<br />
Comparison of the StO 2 tracings with other<br />
physiologic parameters shows that the StO 2<br />
monitor provides more precise information<br />
regarding the adequacy of resuscitation at specific<br />
points in time. This case is an example of<br />
how the StO 2 can provide additional information<br />
that could help a clinician identify a life<br />
threatening complication long before it is clinically<br />
recognized.<br />
Conclusion<br />
In our ongoing experience with ICU resuscitation,<br />
NIRS or StO 2 monitoring offers a continuous,<br />
non-invasive index of tissue perfusion.<br />
Early clinical trials utilizing StO 2 monitors during<br />
active shock resuscitation validated changes<br />
in skeletal muscle StO 2 as an index of perfusion<br />
that was equivalent to serial measurements of<br />
base deficit and lactate levels. In the setting of<br />
ICU sepsis we have observed that StO 2 responds<br />
to interventions, and may be useful in titrating<br />
vasopressors to avoid excessive vasocontrictors<br />
and for monitoring for significant clinical deteriorations.<br />
We concluded with a case presentation<br />
in which StO 2 identified life threatening<br />
postoperative bleeding nearly 12 hours before<br />
it became clinically evident to the clinicians.<br />
Competing interests<br />
Dr. Frederick Moore is a member of the Hutchinson<br />
Technology Inc. Trauma and Critical<br />
Care Advisory Board.<br />
References<br />
1. Shoemaker WC, Appel P, Bland R. Use of physiologic<br />
monitoring to predict outcome and to assist<br />
in clinical decisions in critically ill postoperative<br />
patients. Am J Surg 1983, 146(1):43-50.<br />
2. Shoemaker WC, Appel PL, Kram HB, Waxman K,<br />
Lee TS. Prospective trial of supranormal values<br />
survivors as therapeutic goals in high risk surgical<br />
patients. Chest 1988, 94: 1176-1183<br />
3. Shoemaker WC. Invasive and Noninvasive Hemodynamic<br />
Monitoring of High-Risk Patients to<br />
Improve Outcome. Sem in Anesth, Periop Medicine<br />
and Pain, 1999, 18(1):63-70.<br />
4. Nelson L. Continous Venous Oximetry in Surgical<br />
Patients. Ann Surg 1986, 203(3): 329-33.<br />
5. Taylor JH, Mulier KE, Myers DE, Beilman GJ.<br />
Use of Near Infrared Spectroscopy in Early
Determination of Irreversible Hemorrhagic<br />
Shock. J Trauma 2005, 58: 1119-1125.<br />
6. Crookes BA, Cohn SM, Burton EA, Nelson J,<br />
Proctor KG. Noninvasive muscle oxygenation to<br />
guide fluid resuscitation after shock. Surgery 2004,<br />
135:662-70.<br />
7. Davis J, Shckford SR, Mackersie RC, Hoyt DB.<br />
Base Deficit as a Guide to Volume Resuscitation. J<br />
Trauma 1988, 28(10):1464-7.<br />
8. Davis JW, Parks S, Kaups K, Gladen HE, O’Donnell-<br />
Nicol. Admission Base Deficit Predicts Transfusion<br />
Requirements and Risk of Complications. J<br />
Trauma 1996, 41(5): 769-774.<br />
9. Sauaia A, Moore FA, Moore EE, Haenal JB, Read<br />
RA, Lezotte DC. Early predictors of Postinjury<br />
Multiple Organ Failure. Arch Surg 1994, 129(1):39-<br />
45.<br />
10. Sauaia A, Moore FA, Moore EE, Norris JM, Lezotte<br />
DC. Multiple Organ Failure can be Predicted<br />
as Early as 12 Hours after Injury. J Trauma 1998,<br />
45(2):291-301.<br />
11. Cohn SM, Nathens AB, Moore FA, Rhee P, Puyana<br />
JC, Moore EE, Beilman GJ, and the StO2<br />
in Trauma Patients Trail Investigators. Tissue<br />
Oxygen Saturation Predicts the Development<br />
of Organ Dysfunction During Traumatic Shock<br />
Resuscitation. J Trauma 2007, 62:44-55.<br />
12. Moore FA. Tissue oxygen saturation predicts<br />
the development of organ failure during traumatic<br />
shock resuscitation. In: Faist E, ed. International<br />
Proceedings of the 7th World Congress<br />
on Trauma, Shock, Inflammation and Sepsis.<br />
Munich, Germany, 13-17 March 2007. Bologna,<br />
Italy: Medimond; 2007:111–114.<br />
13. Dellinger RP, Carlet JM, Masur H, Gerlach H,<br />
Calandra T, Cohen J, Gea-Banacloche J, Keh D,<br />
Marshall JC, Parker MM, Ramsay G, Zimmerman<br />
JL, Vincent JL, Levy MM; Surviving Sepsis<br />
Campaign Management Guidelines Committee.<br />
Surviving Sepsis Campaign guidelines for managment<br />
of severe sepsis and shock. Crit Care Med<br />
2004, 32(3):858-73.<br />
14. Hollenberg SM, Ahrens TS, Annane D, Astiz<br />
ME, Chalfin DB, Dasta JF, Heard SO, Martin C,<br />
Napolitano LM, Susla GM, Totaro R, Vincent JL,<br />
Zanotti-Cavazzoni S. Practice Parameters for<br />
hemodynamic support of sepsis in adult Patients:<br />
2004 Update. Crit Care Med 2004, 32(9):1928-<br />
48.<br />
15. Berenholtz SM, Pronovost PJ, Ngo K,<br />
Barie PS, Hitt J, Kuti JL, Septimus E,<br />
Lawler N, Schilling L, Dorman T; Core Sepsis<br />
Measurement Team. Developing Quality Measures<br />
for Sepsis Care in the ICU. Jt Comm J Qual<br />
and Patient Saf. 2007, 33(9):559-68.<br />
16. Dellinger RP, Levy MM, Carlet JM, Bion J,<br />
Parker MM, Jaeschke R, Reinhart K, Angus DC,<br />
Brun-Buisson C, Beale R, Calandra T, Dhainaut<br />
JF, Gerlach H, Harvey M, Marini JJ, Marshall J,<br />
Ranieri M, Ramsay G, Sevransky J, Thompson<br />
BT, Townsend S, Vender JS, Zimmerman JL, Vincent<br />
JL; International Surviving Sepsis Campaign<br />
Guidelines Committee; American Association of<br />
Critical-Care Nurses; American College of Chest<br />
11<br />
Physicians; American College of Emergency<br />
Physicians; Canadian Critical Care Society;<br />
European Society of Clinical Microbiology and<br />
Infectious Diseases, et al. Surviving Sepsis Campaign:<br />
International guidelines for management<br />
of severe sepsis and septic shock: 2008. Crit Care<br />
Med 2008, 36(1):296-327.<br />
<strong>The</strong> authors<br />
Rachel J. Santora 1 & Frederick A. Moore 1,2<br />
1 Department of Surgery,<br />
<strong>The</strong> Methodist Hospital,<br />
Houston, TX, USA<br />
&<br />
2 Department of Surgery,<br />
Weill Cornell Medical College,<br />
New York, NY, USA<br />
Corresponding author:<br />
Rachel J. Santora MD<br />
<strong>The</strong> Methodist Hospital<br />
Department of Surgery<br />
6550 Fannin Street, SM 1661<br />
Houston, TX 77030,<br />
USA<br />
E-mail: rjsantora@tmhs.org<br />
Apr/May 2010<br />
Comments on this article?<br />
Feel free to post them at<br />
www.ihe-online.com/comment/ST02<br />
A New Vital Sign for the 21 st Century<br />
<strong>The</strong> InSpectra StO2 Tissue<br />
Oxygenation Monitor provides<br />
continuous, real-time information<br />
for perfusion status monitoring;<br />
a new hemodynamic parameter<br />
that assists clinicians in the early<br />
detection of inadequate tissue<br />
perfusion (hypoperfusion).<br />
How the InSpectra StO2 System<br />
can provide critical value to<br />
clinicians<br />
• Identifies critically ill patients by<br />
detecting hypoperfusion early.<br />
• Tracks patient status, regardless<br />
of cause of hypoperfusion<br />
(e.g., hypovolemia, early sepsis,<br />
cardiogenic shock).<br />
• Responds to interventions<br />
real-time, assisting with<br />
fluid management.<br />
• A noninvasive, easy-to-use<br />
alternative for monitoring<br />
hypoperfusion.<br />
• Helps guide interventions<br />
by monitoring resuscitation<br />
progress.<br />
Interested in knowing more?<br />
To learn more about the InSpectra<br />
StO2 System, visit our website at<br />
www.htibiomeasurement.com or<br />
contact our Customer Care Center:<br />
EU: + 31263653370<br />
biom.eu@hti.htch.com<br />
US: 1-800-419-1007<br />
biom.usa@hti.htch.com<br />
> Noninvasive<br />
> Continuous<br />
> Real-time<br />
> Direct<br />
<strong>The</strong> InSpectra StO2 Tissue Oxygenation Monitor is a noninvasive monitoring system that measures an approximated value<br />
of percent hemoglobin oxygen saturation in tissue (StO2). Visit us online at www.htibiomeasurement.com for our full<br />
contact information and Instructions for Use.<br />
InSpectra is a registered trademark of Hutchinson Technology Inc. in the United States of America, the European<br />
Community, Canada, China and Japan.<br />
© 2010 Hutchinson Technology Inc. 5024835 A 01/10 All Rights Reserved. 0086<br />
www.ihe-online.com & search 45562
Apr/May 2010<br />
Whole body MRI is highly<br />
accurate in the early detection<br />
of breast cancer metastases<br />
Whole body magnetic resonance imaging<br />
(MRI) should be the imaging modality of<br />
choice for the detection of breast cancer metastases,<br />
as it is highly accurate and can detect bone<br />
metastases while a patient is still asymptomatic,<br />
according to a study presented at the American<br />
Roentgen Ray Society (ARRS) 2010 Annual<br />
Meeting in San Diego, CA, USA. Breast cancer<br />
cells commonly spread to the bones, lungs, liver<br />
or brain; metastatic breast cancer tumours may<br />
be found before or at the same time as the primary<br />
tumour, or months and even years later.<br />
<strong>The</strong> study, performed at Deenanath Mangeshkar<br />
Hospital and Research Center in Pune,<br />
India, included 99 patients with known breast<br />
cancer who were evaluated for metastases<br />
using whole body MRI. Of the 99 patients, MRI<br />
accurately revealed that 47 patients were positive<br />
for metastases while 52 were negative. Of<br />
those patients who were positive for metastases,<br />
whole body MRI frequently detected bone<br />
metastases earlier when the patient was still<br />
asymptomatic. Whole body MRI is an effective<br />
tool for the detection of metastases and unlike<br />
other procedures commonly used in this role,<br />
it emits no radiation.<br />
http://womensimagingonline.arrs.org/<br />
High-pressure jobs increase younger<br />
women’s heart disease risk<br />
A large study of female nurses, published<br />
recently in Occupational and Environmental<br />
Medicine, suggests that high pressure jobs<br />
increase the risk of ischemic heart disease in<br />
women. Previous research has indicated a link<br />
12 NEWs iN BriEF<br />
between a demanding job and heart disease<br />
risk, but the findings have been largely confined<br />
to men.<br />
This research assessed the impact of work pressure<br />
and degree of personal influence in the<br />
workplace on the heart health of 12,116 nurses,<br />
who were taking part in the Danish Nurse<br />
Cohort Study. <strong>The</strong> nurses were all aged between<br />
45 and 64 in 1993, when they were quizzed<br />
about their daily work pressures and personal<br />
influence, after which their health was tracked<br />
for 15 years, using hospital records.<br />
By 2008, 580 nurses had been admitted to hospital<br />
with ischemic heart disease, which included<br />
369 cases of angina and 138 heart attacks.<br />
Nurses who indicated that their work pressures<br />
were a little too high were 25% more<br />
likely to have ischemic heart disease as those<br />
who said their work pressures were manageable<br />
and appropriate; those who felt work<br />
pressures were much too high were almost<br />
50% more likely to have ischemic heart disease.<br />
After taking account of risk factors for<br />
heart disease, such as smoking and lifestyle,<br />
the risk fell to 35%, but still remained significant.<br />
Poor job control in the workplace<br />
did not influence heart disease risk, while<br />
the amount of physical activity at work,<br />
which is known to affect health, had a small<br />
although significant impact. When the findings<br />
were analysed by age, only the nurses<br />
under the age of 51 were at significant risk of<br />
heart disease.<br />
In a separate analysis, the researchers looked<br />
at the impact of work pressures on the same<br />
group, but for just five years up to 1998. Nurses<br />
who felt themselves to be moderately pressurised<br />
at work were 60% more likely to have<br />
ischemic heart disease while those who said<br />
they faced excessive pressures at work were<br />
almost twice as likely to have it. <strong>The</strong>se findings<br />
held true even after taking account of other<br />
risk factors.<br />
http://www.bma.org.uk/<br />
On-site pathology improves the<br />
inadequacy rate of ultrasound-guided<br />
thyroid biopsies<br />
Having a pathologist on-site during ultrasound-guided<br />
thyroid biopsies can decrease<br />
the number of repeat biopsies that are often<br />
performed due to an inadequate sample from<br />
the first procedure, according to a study presented<br />
at the ARRS 2010 Annual Meeting in<br />
San Diego, CA, USA.<br />
Requests for ultrasound-guided biopsies for<br />
the diagnosis of thyroid nodules have increased<br />
rapidly in recent years, putting a strain on radiology<br />
departments everywhere, according to<br />
Wui K. Chong, MD, lead author of the study.<br />
Unfortunately, there are a number of inadequate<br />
biopsies (where the pathologist deems there is<br />
an insufficient amount of information to make<br />
a diagnosis) that ultimately must be repeated.<br />
Repeat biopsy is unpleasant and inconvenient<br />
for the patient and is obviously wasteful. Having<br />
a pathologist on-site to review the specimen<br />
can cut down on the number of patients<br />
returning for repeat biopsy, thus making more<br />
efficient use of resources.<br />
<strong>The</strong> study compared 200 biopsies that were<br />
performed with a pathologist on-site and 200<br />
that were not. It was found that all other factors<br />
being equal, 13.5 percent of biopsies performed<br />
without a pathologist on-site were inadequate,<br />
compared to only 5 percent that were performed<br />
with a pathologist on-site. <strong>The</strong> authors<br />
thus recommend that radiologists performing<br />
large numbers of thyroid biopsies use on-site<br />
pathology as it may reduce the need for repeat<br />
biopsy by up to 60 percent.<br />
http://womensimagingonline.arrs.org/<br />
Study finds everolimus-eluting<br />
stent safer, more effective than<br />
paclitaxel-eluting stent<br />
Results from the SPIRIT IV clinical trial, which<br />
were first presented at the Transcatheter Cardiovascular<br />
<strong>The</strong>rapeutics (TCT) 2009 scientific<br />
symposium, were published recently in the<br />
New England Journal of Medicine.<br />
Data from the trial, a large-scale multi-centre<br />
study of nearly 4,000 patients in the US, showed<br />
that everolimus-eluting stents demonstrated<br />
enhanced safety and efficacy in the treatment<br />
of de novo native coronary artery lesions when<br />
compared to paclitaxel-eluting stents. <strong>The</strong> trial,<br />
which was powered for superiority for clinical<br />
endpoints without angiographic follow up, also<br />
examined the differences in performance of the<br />
two stents in patients with diabetes.<br />
<strong>The</strong> primary endpoint of the trial was targetlesion<br />
failure (TLF) at one year, a composite<br />
measure of cardiac death, target-vessel heart<br />
attack or ischemia-driven target-lesion revascularization<br />
(TLR). Major secondary endpoints
of the trial were ischemia-driven TLR at one<br />
year, and the composite rate of cardiac death or<br />
target-vessel heart attack at one year.<br />
For everolimus-eluting stents, TLF at one<br />
year was 4.2 percent, and for paclitaxeleluting<br />
stents, TLF was 6.8 percent, a significant<br />
38 percent reduction. At one-year,<br />
ischemia-driven TLR was 2.5 percent for<br />
everolimus-eluting stents and 4.6 percent for<br />
paclitaxel-eluting stents, a significant 45 percent<br />
reduction. <strong>The</strong> composite rates of cardiac<br />
death or target-vessel myocardial infarction<br />
through one year were not statistically<br />
different with the two stents (2.2 percent<br />
for everolimus-eluting stents and 3.2 percent<br />
for paclitaxel-eluting stents). <strong>The</strong> oneyear<br />
rates of myocardial infarction and stent<br />
thrombosis, however, were also lower with<br />
everolimus-eluting stents than with paclitaxel-eluting<br />
stents (1.9 percent vs. 3.1 percent<br />
for myocardial infarction and 0.17 percent<br />
vs. 0.85 percent stent thrombosis). <strong>The</strong><br />
results were consistent regardless of lesion<br />
length, vessel size and the number of lesions<br />
treated. However, in the diabetic-patient subgroup,<br />
the study found a comparable rate of<br />
TLF with both stents, whereas in patients<br />
without diabetes, everolimus-eluting stents<br />
reduced TLF by 53 percent compared to<br />
paclitaxel-eluting stents.<br />
http://tinyurl.com/37sfo7s<br />
Outcomes of early vs. late<br />
tracheotomy for mechanically<br />
ventilated ICU patients<br />
Adult ICU patients who received tracheotomy<br />
6 to 8 days vs. 13 to 15 days after mechanical<br />
ventilation did not have a significant reduction<br />
in the risk of ventilator-associated pneumonia,<br />
according to a study published in a recent issue<br />
of JAMA.<br />
Tracheotomy replaces endotracheal intubation<br />
in patients who are expected to require prolonged<br />
mechanical ventilation. Advantages of<br />
tracheotomy include prevention of ventilatorassociated<br />
pneumonia (VAP), earlier weaning<br />
from respiratory support and reduction in<br />
sedative use. <strong>The</strong>re is considerable variability<br />
in the time considered optimal for performing<br />
tracheotomy.<br />
Pier Paolo Terragni, M.D., of the Uni¬versita di<br />
Torino, Turin, Italy, and colleagues inestigated<br />
NEWs iN BriEF Apr/May 2010<br />
whether tracheotomy performed earlier (6-8<br />
days) vs. later (13-15 days) after laryngeal (larynx)<br />
intubation would reduce the incidence of<br />
VAP and increase the number of ventilatorfree<br />
and intensive care unit (ICU)-free days.<br />
<strong>The</strong> randomized controlled trial, performed<br />
in 12 Ital¬ian ICUs from June 2004 to June<br />
2008, enrolled 600 adult patients without lung<br />
infection who had been ventilated for 24 hours.<br />
Patients who had worsening of respiratory conditions,<br />
unchanged or worse sequential organ<br />
failure assessment score, and no pneumonia<br />
48 hours after inclusion were randomized to<br />
early tracheotomy (n = 209; 145 received tracheotomy)<br />
or late tracheotomy (n = 210; 119<br />
received tracheotomy).<br />
<strong>The</strong> researchers found that 30 patients (14 percent)<br />
had VAP in the early tracheotomy group<br />
and 44 patients (21 percent) had VAP in the<br />
late tracheotomy group. <strong>The</strong> numbers of ventilator-free<br />
and ICU-free days and the incidences<br />
of successful weaning and ICU discharge were<br />
significantly greater in patients randomized to<br />
the early tracheotomy group compared with<br />
patients randomized to the late tracheotomy<br />
group; there were no differences between the<br />
groups in survival at 28 days.<br />
<strong>The</strong> data show that in intubated and mechanically<br />
ventilated adult ICU patients with a<br />
high mortality rate, early tracheotomy did not<br />
result in a significant reduction in incidence<br />
of VAP compared with late tracheotomy.<br />
Although the number of ICU-free and ventilator-free<br />
days were higher in the early tracheotomy<br />
group than in the late tracheotomy<br />
group, long-term outcome did not differ. Considering<br />
that anticipation for tracheotomy of<br />
1 week increased the number of patients who<br />
received a tracheotomy, and more than onethird<br />
of the patients experienced an adverse<br />
event related to tracheotomy, these data suggest<br />
that a tracheotomy should not be performed<br />
earlier than after 13 to 15 days of<br />
endotracheal intubation.<br />
www.jamamedia.org<br />
Harm caused by nicotine withdrawal<br />
during intensive care<br />
Nicotine withdrawal can cause dangerous<br />
agitation in intensive care patients. Researchers<br />
writing in BioMed Central’s open access<br />
journal Critical Care found that, compared<br />
to non-smokers, agitated smokers were more<br />
likely to accidentally remove tubes and catheters,<br />
require supplemental sedative, analgesic<br />
or anti-psychotic medications, or need physical<br />
restraints.<br />
Damien du Cheyron, from Caen University<br />
Hospital, France, worked with a team of<br />
researchers to study the effects of nicotine<br />
withdrawal in 44 smokers and 100 non-smokers<br />
in the hospital’s intensive care unit, finding<br />
that agitation was twice as common in smokers<br />
than controls. He said that agitation was<br />
13<br />
significantly more common in smokers than<br />
in non-smokers. <strong>The</strong>se results suggest the need<br />
to be aware of nicotine withdrawal syndrome<br />
in critically ill patients, and support the need<br />
for improved strategies to prevent agitation or<br />
treat it earlier”.<br />
None of the smokers in the study were<br />
allowed nicotine replacement therapy (NRT)<br />
during the study period. According to du<br />
Cheyron, NRT remains a controversial topic<br />
in intensive care and has been associated with<br />
mortality. Due to the serious consequences<br />
of withdrawal-induced agitation, including<br />
sedation and physical restraint, the authors<br />
suggest that the use of nicotine replacement<br />
therapy should be tested by a well-designed,<br />
randomized controlled clinical trial in the<br />
ICU setting.<br />
http://tinyurl.com/37ko8d5<br />
www.ihe-online.com & search 45344
<strong>Anesthesiology</strong> special<br />
Selection of peer-reviewed literature<br />
on anesthesiology<br />
the number of peer-reviewed papers<br />
covering the vast field of anesthesiology<br />
is huge, to such an extent that it is<br />
frequently difficult for healthcare professionals<br />
to keep up with the literature.<br />
As a special service to our readers,<br />
iHE presents a selection of key literature<br />
abstracts from the clinical and scientific<br />
literature chosen by our editorial<br />
board as being particularly worthy<br />
of attention.<br />
An anesthesiologist’s perspective on<br />
inhaled anesthesia decision-making.<br />
<strong>The</strong> practice of anesthesiology requires complex<br />
monitoring, detailed knowledge of pharmacology,<br />
and the ability to make quick decisions<br />
about patient management. In the United<br />
States, most general anesthesia involves inhaled<br />
agents. <strong>The</strong> minimum alveolar concentration<br />
(MAC) of inhaled anesthetic agents, which<br />
anesthesiologists use in dosing these drugs,<br />
can be affected by age, a variety of medications<br />
and other patient-specific factors. MAC can be<br />
thought of as a measure of drug potency. Both<br />
MAC and solubility in blood and tissues differ<br />
among inhaled anesthetic agents. Agents with<br />
low solubility have a rapid onset and offset of<br />
effect and may allow for faster recovery. <strong>The</strong><br />
choice among inhaled anesthetic agents may<br />
depend on their solubility, as well as the propensity<br />
to cause airway irritation and coughing,<br />
drug cost and characteristics such as patient<br />
age, obesity and duration of surgery. Anesthesia<br />
care providers’ experience and habits may also<br />
influence drug choice. Emergence delirium<br />
(i.e., agitation) can occur with all three inhaled<br />
anesthetic agents in common use (isoflurane,<br />
desflurane, and sevoflurane). Other potential<br />
issues such as hepatotoxicity and nephrotoxicity<br />
are of minimal concern with these agents.<br />
Using low flow rates of fresh gas is one strategy<br />
for minimising inhaled anesthesia costs, but it<br />
is not always feasible.<br />
Prielipp RC. Am J Health Syst Pharm. 2010 Apr<br />
15;67(8 Suppl 4):S13-20.<br />
Risk in anesthesia.<br />
Modern anesthesia is still associated with a risk<br />
of serious complications. This article focusses<br />
on frequency, causes, and prevention of the<br />
most important anesthetic complications. <strong>The</strong><br />
article is based on literature identified through<br />
a non-systematic search in Pub-Med, and the<br />
author’s research and experience in this field.<br />
<strong>The</strong> risk of death associated with anesthesia is<br />
closely related to patient age and physical status.<br />
In otherwise healthy patients (ASA 1), the<br />
risk of such deaths is approximately 1:250 000.<br />
Medication errors occur in approximately 1:1<br />
000 anesthetic procedures. <strong>The</strong> risk of awareness<br />
during general anesthesia is approximately<br />
1:650. Neural injury from epidural and spinal<br />
anesthesia is rare, especially in obstetrics. Anaphylaxis<br />
caused by muscle relaxant drugs is<br />
more common in Norway than in many other<br />
industrialised countries. Pulmonary aspiration<br />
occurs in approximately 1:7 000 anesthetic<br />
procedures, but with low morbidity in<br />
healthy patients. <strong>The</strong> incidence of anesthetic<br />
accidents is higher in infants than older children,<br />
and requires special competence. Serious<br />
anesthetic complications are most often related<br />
to the cardiovascular and respiratory system.<br />
<strong>The</strong> complications are often multicausal, and<br />
human errors and organisational factors contribute<br />
in 50-70 % of the cases. Optimisation<br />
of the patient’s preoperative health is important<br />
to improve safety. <strong>The</strong> focus of the anesthesiology<br />
department should be education and<br />
guidelines. Systems and routines for improved<br />
safety must also take into account that<br />
human and organisational factors may cause<br />
anesthetic accidents.<br />
Fasting S. Tidsskr Nor Laegeforen. 2010 Mar<br />
11;130(5):498-502.<br />
General anesthesia occurs frequently<br />
in elderly patients during<br />
propofol-based sedation and spinal<br />
anesthesia.<br />
This study tested the hypothesis that sedation<br />
in elderly patients is often electrophysiologically<br />
equivalent to general anesthesia (GA). Forty elderly<br />
patients (>or=65 yrs of age) undergoing hip<br />
fracture repair with spinal anesthesia and propofol-based<br />
sedation were observed. In the routine<br />
practice group (RP; n = 15), propofol sedation<br />
was administered as usual. In the targeted sedation<br />
group (TS; n = 25), sedation was titrated to<br />
an observer’s assessment of alertness/sedation.<br />
Both patient groups underwent processed electroencephalographic<br />
monitoring using bispectral<br />
index (BIS) intraoperatively. BIS levels were compared<br />
between groups to determine amount of<br />
surgical time spent in GA (BIS
GE Healthcare<br />
Power of Innovation.<br />
Here at GE Healthcare we develop the breakthrough technologies and clinical applications which redefi ne<br />
standards in ultrasound image quality, boosting diagnostic confi dence and improving patient care.<br />
Reliable, state - of - the - art ultrasound equipment for Cardiology, <strong>Anesthesiology</strong>, Radiology and Ob/Gyn,<br />
backed up by comprehensive service & support – so relax, confi dent in the knowledge that you and your<br />
patients are in capable hands.<br />
For more information please visit www.gehealthcare.com<br />
© 2010 General Electric Company<br />
GE Medical Systems Ultrasound & Primary Care<br />
Diagnostics, LLC, a subsidiary of General Electric<br />
Company, doing business as GE Healthcare.<br />
GE imagination at work<br />
GE Ultraschall Deutschland GmbH<br />
Beethovenstr. 239, D-42655 Solingen<br />
T: 49-212-28 02-0, F: 49-212-28 02-28<br />
www.ihe-online.com & search 45458
Apr/May 2010<br />
<strong>The</strong> introduction onto the market of a ready-touse<br />
intravenous paracetamol formulation has<br />
created a new future for a drug that is in fact<br />
more than 100 years old. <strong>The</strong> new formulation<br />
has stimulated interest on the part of anesthesiologists<br />
to use paracetamol in the peri-operative<br />
setting. <strong>The</strong> most popular over-the-counter<br />
pain relieving and antipyretic drug has become<br />
a major protagonist in operating rooms. However,<br />
physicians still have many questions and<br />
concerns about its use, its mechanism of action<br />
and its safety profile.<br />
Is paracetamol a NSAID? — a look<br />
at its mechanism of action<br />
Paracetamol, also known as acetaminophen,<br />
was first synthesised in 1878 but had only limited<br />
use until the 1950s, when it was identified<br />
as the active metabolite of two well-known<br />
antipyretic drugs, acetanilide and phenacetin,<br />
which were themselves withdrawn from the<br />
market for their nephrotoxicity.<br />
Despite its widespread use, the detailed mechanism<br />
of action of paracetamol is still poorly<br />
understood; questions remain open as to<br />
whether it acts peripherally and/or centrally, as<br />
16 ANEstHEsioLoGy<br />
Paracetamol : the otC pain reliever<br />
becomes a protagonist in operating theatres<br />
the new intravenous formulation of paracetamol has transformed the most popular<br />
over-the-counter (otC) pain reliever into a valuable analgesic option for pain<br />
management in the peri-operative setting. However, more than 100 years after its<br />
original introduction into clinical practice, there are still many questions about the<br />
drug’s mechanism of action, its analgesic efficacy and safety.<br />
by Prof. Flaminia Coluzzi, dr Giada Nardecchia and dr Consalvo Mattia<br />
Figure 1. <strong>The</strong> effect of hydroperoxide concentration<br />
on the action of paracetomol.<br />
well as which analgesic pathway is principally<br />
affected by its administration.<br />
A commonly posed question is whether paracetamol<br />
inhibits cyclooxygenase (COX)<br />
like nonsteroidal anti-inflammatory drugs<br />
(NSAIDs) or whether its analgesic activity<br />
is due to modulation of other endogenous<br />
pathways. In 1972, Flower and Vane showed<br />
that the anti-pyretic effect of paracetamol<br />
was related to the inhibition of prostaglandin<br />
synthetase in the brain. Recent investigations<br />
showed that paracetamol has no direct affinity<br />
for the active site of COX, but rather acts as a<br />
reducing agent — by reducing the active oxidised<br />
form of the enzyme to an inactive form,<br />
it blocks the activity of COX. Because COX is<br />
sensitive to the local oxidation environment,<br />
which is influenced by a high organic peroxide<br />
concentration such as is found in peripheral<br />
sites of inflammation and in platelets, paracetamol<br />
is a weak inhibitor of prostaglandin<br />
synthesis. In the central nervous system and<br />
in the endothelial cells, however, where the<br />
concentration of hydroperoxides is low, paracetamol<br />
selectively inhibits the enzyme [Figure<br />
1]. This explains why paracetamol is not associated<br />
with the gastric side-effects and inhibition<br />
of platelet activity traditionally observed with<br />
NSAIDs. However, paracetamol does not have<br />
the anti-inflammatory efficacy of NSAIDs, but<br />
only analgesic and antipyretic activity.<br />
<strong>The</strong> hypothesis that paracetamol could selectively<br />
inhibit a particular isoform of the COX<br />
enzyme, namely COX-3, which is highly<br />
expressed in the brain and in the heart, has<br />
been recently ruled out. COX-3 is just a variant<br />
of COX-1, with a significantly lower potency<br />
(about 1/5th) in generating prostaglandins.<br />
Other possible mechanisms of the analgesic<br />
action have been postulated:<br />
a) Paracetamol interacts with the endogenous<br />
opioid pathways, but it does not bind to opioid<br />
receptors.<br />
b) Paracetamol is associated with changes in<br />
the serotoninergic system, the endogenous<br />
descending pain inhibitory pathway, known<br />
as the “analgesic system”.<br />
c) Paracetamol inhibits substance P-mediated<br />
hyperalgesia, by interaction with the nitric<br />
oxide pathway.<br />
d) Paracetamol can indirectly activate cannabinoid<br />
receptors (CB1) by increasing brain levels<br />
of endogenous cannabinoids. One of the<br />
metabolites of paracetamol, namely AM404,<br />
acts as an inhibitor of cellular re-uptake of<br />
anandamide, which is the first recognised<br />
endocannabinoid.<br />
Hepatotoxicity: myth or reality?<br />
Paracetamol is a safe drug when used at the<br />
recommended therapeutic doses. However,<br />
overdose can lead to serious and even fatal liver<br />
injury. This potential hepatotoxicity could still<br />
represent a perceived barrier to its use by some<br />
physicians. Paracetamol is responsible for up to<br />
40% of cases of acute liver failure in the United<br />
States and the United Kingdom.<br />
Damage to the liver following paracetamol<br />
ingestion is not due to the drug itself, but to a<br />
toxic metabolite, namely N-acetyl-p-benzoquinine<br />
imine (NAPQI). Once absorbed, approximately<br />
90% of the paracetamol is metabolised<br />
by conjugation and sulphation, 5% is eliminated<br />
unchanged, and the remaining 5% is oxidised to<br />
form NAPQI. This is quickly combined in the<br />
liver with the endogenous antioxidant, glutathione,<br />
to form non-toxic conjugates, which are<br />
eliminated in the urine. After an overdose, when<br />
glutathione stores in the liver become depleted,<br />
free NAPQI begins to accumulate and causes<br />
life-threatening liver injury.<br />
Excluding suicide attempts, unintentional overdoses<br />
constitute at least half of all paracetamolrelated<br />
hepatotoxicity cases. <strong>The</strong> median dose<br />
ingested in subjects who developed acute liver<br />
failure was 24 g, i.e. six times the maximum 4g<br />
daily dosage. Risk factors include excessive dosing<br />
(repeated dosing in excess of package labelling<br />
specified doses, or use of multiple paracetamol-containing<br />
products), increased P450<br />
activation, simultaneous use or abuse of alcohol<br />
and narcotics, very young age, and comorbidities<br />
including liver disease and depression.<br />
<strong>The</strong> recommended dose for intravenous paracetamol<br />
injection in adults is 1 g every 6 hours. Recent<br />
studies evaluated the efficacy and safety of higher<br />
doses. Serum hepatic aminotransferase activity<br />
remained in the normal ranges, even when up to
8 g/day of paracetamol was used for three days<br />
in healthy young adults. Similarly, in alcoholic<br />
patients treated with 4 g/day for three consecutive<br />
days, no increases in serum transaminases<br />
or other measures of liver injury were observed.<br />
<strong>The</strong> perception that paracetamol should be<br />
avoided in patients with chronic liver disease arose<br />
from the awareness of the association between<br />
massive paracetamol overdose and acute liver<br />
failure. However, the literature supports the use of<br />
paracetamol in patients with liver disease.<br />
Optimal formulation and dose<br />
Different routes of administration have been<br />
extensively studied for the peri-operative use of<br />
paracetamol. With oral administration, a large<br />
variability is observed in individual plasma paracetamol<br />
levels. Intravenous administration is the<br />
route of choice when oral administration is not<br />
possible or when rapid analgesia is required, such<br />
as in the post-operative setting.<br />
What is the right dose for adequate analgesia?<br />
<strong>The</strong> minimum plasma paracetamol level required<br />
for analgesia and anti-pyresis is thought to be<br />
10-20 mg/L. However, recent studies have shown<br />
that it is the concentration in of the drug in the<br />
effect compartment, rather than in plasma, that<br />
relates more consistently to the analgesic effect.<br />
It is therefore important to administer the right<br />
dose at the right time in order to reach an adequate<br />
concentration in the central nervous system<br />
— the ready-to-use intravenous formulation<br />
shows the best pharmacokinetic profile for postoperative<br />
pain management. This formulation<br />
penetrates readily into the cerebrospinal fluid and<br />
provides rapid and predictable analgesia in the<br />
post-operative setting.<br />
Paracetamol in adults<br />
In adults, the standard dose of paracetamol is 1g<br />
every 6 hours administered as an intravenous<br />
infusion every 15 minutes. Several studies have<br />
demonstrated that the efficacy of 2g of intravenous<br />
paracetamol is significantly superior<br />
to 1g. In healthy subjects, the administration<br />
of a 2g starting dose and 5g during the first 24<br />
hours does not change the pharmacokinetics<br />
of paracetamol, and the<br />
peak plasma concentration<br />
did not rise above the<br />
toxic threshold. When a<br />
single intravenous dose<br />
of 3g of paracetamol<br />
was administered, no<br />
serious adverse events<br />
were observed, but the<br />
opioid-sparing effect was<br />
similar to that reported<br />
after conventional doses<br />
of paracetamol. In conclusion,<br />
even though no<br />
hepatotoxicity has been<br />
reported, the administration<br />
of paracetamol at doses higher than 4g daily<br />
is not recommended, since it does not improve<br />
the drug’s analgesic efficacy.<br />
Paracetamol in children<br />
Rectal administration is preferred in children,<br />
even though absorption is slower and more<br />
variable compared with intravenous administration.<br />
Plasma concentrations after administering<br />
1g paracetamol are 1.2µg/mL for the<br />
rectal route versus 2.7 µg/mL for the oral route.<br />
In children, the analgesic efficacy of rectal<br />
paracetamol increases in a linear manner as the<br />
dose is increased from 0 to 60 mg/kg. However,<br />
rectal doses greater than 30 mg/kg are not recommended.<br />
In pediatric surgical patients, the<br />
recommended dose of intravenous paracetamol<br />
is 15 mg/kg. Precautions must be taken when<br />
using paracetamol in neonates and infants, as<br />
they have an increased risk of forming the reactive<br />
intermediate metabolite that causes hepatocellular<br />
damage, particularly after multiple<br />
doses. Neonates and infants have an immature<br />
glucuronide conjugation system, and the sulphation<br />
metabolic pathway is the main route<br />
of metabolism for paracetamol.<br />
Opioid sparing<br />
<strong>The</strong> opioid-sparing effect of paracetamol,<br />
when used in combination with opioid receptor<br />
agonist for multimodal analgesia, is still<br />
controversial. After major surgery, the use of<br />
paracetamol significantly reduced morphine<br />
use by approximately 20%, compared to 40%<br />
with NSAIDs, and 25% with COX-2 inhibitors.<br />
However, it did not change the incidence<br />
of morphine-related adverse events during the<br />
post-operative period. A meta-analysis proved<br />
that adding an NSAID may increase the analgesic<br />
efficacy of paracetamol, but their combination<br />
does not provide a better analgesic effect<br />
than NSAID alone.<br />
Paracetamol in combination with<br />
other drugs<br />
Paracetamol is also available in fixed combinations<br />
with other molecules, such as codeine, tramadol<br />
and oxycodone, for oral administration<br />
17 Apr/May 2010<br />
only. <strong>The</strong>se formulations have proved effective<br />
for post-operative pain management, especially<br />
in day-surgery, where analgesia must be provided<br />
at home. Combining drugs from different<br />
classes with different modes of action may offer<br />
the opportunity to optimise efficacy and tolerability,<br />
by using lower doses of each drug to reach<br />
a similar degree of pain relief. After orthopedic<br />
surgery, a paracetamol/tramadol combination<br />
(325 mg/37.5 mg) showed an analgesic efficacy<br />
significantly superior to placebo and comparable<br />
to that obtained with codeine/paracetamol,<br />
with better tolerability and a lower incidence<br />
of constipation.<br />
Conclusion<br />
In conclusion, paracetamol is a safe and effective<br />
centrally-acting analgesic for acute and<br />
chronic pain management. <strong>The</strong> multiple interactions<br />
with different endogenous systems<br />
(cyclooxygenase, opioid, serotoninergic, nitric<br />
oxide, and endocannabinoid pathways) make<br />
it difficult to identify the exact mechanism of<br />
action of the molecule. Its role in the peri-operative<br />
setting has been widely demonstrated.<br />
Advantages compared to traditional NSAIDs<br />
are the lack of gastrointestinal side effects and<br />
low interaction with platelet aggregation.<br />
References<br />
1. Mattia C, Coluzzi F. What anesthesiologists should know<br />
about paracetamol (acetaminophen). Minerva Anestesiol<br />
2009; 75: 644-53<br />
2. Oscier CD, Milner QJ. Peri-operative use of paracetamol.<br />
Anaesthesia 2009; 64: 65-72<br />
3. Bertolini A, Ferrari A, Ottani A, Guerzoni S, Tacchi R,<br />
Leone S. Paracetamol: new vistas of an old drug. CNS<br />
Drug Reviews 2006; 12: 250-75<br />
4. Elia N, Lysakowski C, Tramer MR. Does multimodal<br />
analgesia with acetaminophen, nonsteroidal antiinflammatory<br />
drugs, or selective cyclooxygenase-2 inhibitors<br />
and patient-controlled analgesia morphine offer advantages<br />
over morphine alone? <strong>Anesthesiology</strong> 2005; 103:<br />
1296-304<br />
5. Remy C, Marret E, Bonnet F. Effects of acetaminophen<br />
on morphine side-effects and consumption after major<br />
surgery: meta-analysis of randomized controller trials.<br />
Br J Anesth 2005; 94: 505-13<br />
6. Mattia C, Coluzzi F, Sarzi Puttini P, Viganò R. Paracetamol/Tramadol<br />
association: the easy solution for mildmoderate<br />
pain. Minerva Med 2008; 99: 369-90<br />
<strong>The</strong> authors<br />
Flaminia COLUZZI, M.D, Giada NARDEC-<br />
CHIA, M.D. and Consalvo MATTIA, M.D.<br />
I.C.O.T. – Polo Pontino<br />
Department of <strong>Anesthesiology</strong>, Intensive Care<br />
Medicine and Pain <strong>The</strong>rapy<br />
Sapienza University of Rome, Rome, Italy<br />
Corresponding author:<br />
Prof. Flaminia COLUZZI<br />
Research Associate Professor<br />
Via India, 7 – 00196 Rome, Italy<br />
E-mail: flaminia.coluzzi@uniroma1.it
Apr/May 2010<br />
<strong>The</strong> American Board of Plastic Surgeons<br />
(ABPS) recently reported that more than 11<br />
million cosmetic procedures were performed<br />
last year in the United States [1]. Many expect<br />
this number to rise as plastic surgery procedures<br />
become more advanced and less invasive.<br />
Largely because of meticulous preoperative<br />
screening and technological advances<br />
in outpatient anesthesia for elective cosmetic<br />
surgery, morbidity and mortality resulting<br />
from outpatient anesthesia are rare [2].<br />
Pre-hospital care<br />
Patients should be medically optimized<br />
before receiving any type of anesthetic. In<br />
preparing for surgery, the American Society<br />
of Anesthesiologists has developed a Physical<br />
Status Score (ASA PS) that places patients<br />
into one of six categories. Class I (completely<br />
healthy) or Class II (mild controlled illness or<br />
disease with no interference to the patient’s<br />
daily life) patients are generally deemed suitable<br />
for cosmetic surgery, while a Class III<br />
patient would most likely need additional<br />
assessment before being cleared for such<br />
procedures. In addition to a thorough history<br />
and physical exam, laboratory screenings<br />
are often required. Commonly ordered tests<br />
include hemoglobin and hematocrit, electrolytes,<br />
blood glucose, urinalysis, an electrocardiogram<br />
(EKG) and a pregnancy test for<br />
women within child-bearing age.<br />
Prior to surgery, the American Society of<br />
Anesthesiologists Task Force on Preoperative<br />
Fasting recommended a minimum fasting<br />
period for clear liquids of two hours and<br />
a minimum of six hours for milk or a light<br />
meal. <strong>The</strong>y further recommended a fasting<br />
period of eight hours for patients who<br />
have ingested any meal containing fried or<br />
fatty foods [3]. Since it is easiest and safest<br />
to adopt a single “nothing by mouth” rule<br />
prior to elective surgery, eight hours is the<br />
18 ANEstHEsioLoGy<br />
Anesthesia for cosmetic surgery<br />
the number of patients undergoing cosmetic surgery is steadily increasing as the<br />
surgical procedures themselves become more advanced and less invasive. However,<br />
just as patients undergoing cosmetic surgery are generally well informed<br />
regarding the nature of the procedure and the reputation of their surgeon, they<br />
frequently overlook the importance of the anesthetic technique needed to effectively<br />
perform the procedure. An overall successful procedure involves not only a<br />
plastic surgeon skilled in cosmetic surgery but also an anesthesiologist proficient<br />
in cosmetic anesthesia. this article reviews the principal aspects to be considered<br />
in the anesthesiology of cosmetic surgery.<br />
by dr Peter J. taub and dr Laurence Hausman<br />
most appropriate since it covers all foods<br />
and liquids.<br />
It is common for patients to feel anxiety and<br />
apprehension before surgery. A preoperative benzodiazepine,<br />
such as alprazolam or lorazepam, is<br />
suitable because in addition to inducing somnolence,<br />
this class of drug is also associated with<br />
anxiolysis. In fact, many plastic surgeons treat<br />
preoperative anxiety prophylactically.<br />
Pre-operative care<br />
Prior to the induction of anesthesia, an intravenous<br />
line is inserted for administration<br />
of medications. <strong>The</strong> American Society of<br />
<strong>Anesthesiology</strong> (ASA) has outlined a standard<br />
for which monitoring devices should be<br />
used during outpatient general anesthesia.<br />
<strong>The</strong>se include a continuous electrocardiogram<br />
(EKG), a cycling blood pressure cuff,<br />
a pulse oximeter for oxygen saturation measurements,<br />
an end tidal carbon dioxide monitor,<br />
and a temperature probe. A constant stable<br />
blood pressure in the low-normal range<br />
for the duration of the cosmetic procedure is<br />
desirable to minimize blood loss and bleeding<br />
into the tissues that could contribute to<br />
prolonged postoperative ecchymosis and<br />
edema. Compression boots should be placed<br />
prior to the induction of general anesthesia<br />
to prevent the incidence of deep venous<br />
thrombosis [4]. A bladder catheter is recommended<br />
for cases longer than four hours<br />
to safely manage fluid resuscitation and<br />
to keep the bladder decompressed during<br />
abdominal procedures.<br />
Although there are currently more cosmetic surgical and nonsurgical procedures performed in the<br />
United States than in Europe, the inevitable tendency is that the Europe follows the practices carried out<br />
in the United States. <strong>The</strong> statistics above show the dramatic increase in procedures carried out<br />
over the decade prior to 2008 (latest data available).<br />
It can be seen that breast augmentation and lipoplasty remain the most common cosmetic surgical procedures.<br />
For each surgical procedure it is estimated that there are four non-surgical procedures or minimally invasive<br />
procedures. <strong>The</strong>se include Botulinum Toxin A ( so-called Botox), soft tissue peelers, chemical peel,<br />
microdermabrasion and laser hair removal.
<strong>The</strong> temperature of the operating<br />
room is a vital consideration when<br />
planning a surgical procedure.<br />
Due to the vasodilatory nature<br />
and the direct inhibition of the<br />
hypothalamus caused by many<br />
anesthetic agents, all patients are<br />
susceptible to hypothermia during<br />
surgery. Consequences of this can<br />
be platelet dysfunction and bleeding,<br />
enzymatic inactivity, cardiac<br />
dysfunction, or postoperative<br />
shivering [5]. Hence, the ambient<br />
temperature of the operating<br />
room should be kept at a temperature<br />
that minimizes body heat loss<br />
and a warming blanket be used for<br />
longer procedures.<br />
It is believed that a patient’s state<br />
on induction (i.e. when the patient<br />
loses consciousness) mirrors that<br />
of emergence (i.e. when the patient<br />
regains consciousness). Accordingly,<br />
a smooth induction with<br />
minimal hypertension and tachycardia<br />
is desirable for cosmetic<br />
anesthesia. Prior to induction,<br />
the anesthesiologist should consider<br />
giving several medications.<br />
Midazolam, a short-acting benzodiazepine,<br />
can produce sedativehypnotic<br />
effects or can even induce<br />
anesthesia at very high doses. It is<br />
also characterized by its ability to<br />
cause amnesia, hypnosis, and the<br />
relaxation of muscles with relative<br />
celerity. As far as cardiac sensitivity<br />
is concerned, the use of midazolam<br />
is associated with decreases<br />
in mean arterial pressure (MAP),<br />
cardiac output (CO), stroke volume<br />
(SV), and systemic vascular<br />
resistance (TPR). Consequently,<br />
midazolam is contraindicated in<br />
patients with acute pulmonary<br />
insufficiency or severe chronic<br />
obstructive pulmonary disease.<br />
Postoperative nausea and vomiting<br />
(PONV) is a major concern<br />
with any anesthetic procedure.<br />
Preoperative antiemetics should<br />
be used to prevent PONV following<br />
the use of numerous anesthetic<br />
agents, including narcotics and<br />
nitrous oxide. Many anesthesiologists<br />
avoid narcotics altogether to<br />
minimize the incidence of PONV.<br />
Alternative analgesics include local<br />
anesthetics, ketamine, and ketorolac.<br />
Other anesthesiologists advocate<br />
the use of narcotics for heavy<br />
pain cases and use a variety of<br />
available antiemetics to minimize<br />
PONV. Granisitron and Ondansetron<br />
are serotonin antagonists that<br />
reduce the autonomic neuro-activity<br />
in the vomiting center of the<br />
brain. Dexamethasone, a steroid,<br />
and Scopalamine, a tropane alkaloid,<br />
may both be used to resolve<br />
dizziness and nausea. Additionally,<br />
metochlopromide and Amend,<br />
a newer antiemetic, are increasingly<br />
being used. Combination<br />
therapy using several antiemetics<br />
is advisable for patients that have<br />
a high risk of PONV, including<br />
Professionals<br />
Demand<br />
the Best<br />
in Medical<br />
Technology<br />
ADS II<br />
Anesthesia Delivery System<br />
young women and non-smokers<br />
who have a history of PONV<br />
or car-sickness.<br />
12151 62nd St N #5 • Largo FL 33773 • USA<br />
Phone: (1) 727-531-8434 • Fax: (1) 727-531-8436<br />
Web: www.infiniummedical.com • Email: sales@infiniummedical.com<br />
General anesthesia<br />
General anesthesia is defined as<br />
the controlled state of unconsciousness<br />
accompanied by a loss<br />
of protective airway reflexes [6].<br />
With this type of anesthesia, the<br />
patient may require respiratory<br />
or cardiovascular support. <strong>The</strong><br />
insertion of an endotracheal tube<br />
or laryngeal mask airway (LMA)<br />
that sits just above the vocal cords<br />
OMNI II<br />
Touch Screen Patient Monitor<br />
19 Apr/May 2010<br />
OMNI III<br />
Anesthesia Monitor<br />
after induction will allow control<br />
of ventilation. For procedures that<br />
do not involve frequent head turning,<br />
the LMA provides a safe alternative<br />
to the ETT since it does not<br />
risk vocal cord injury and has less<br />
of an incidence of postoperative<br />
laryngeal irritation and “bucking<br />
on the tube” [7]. However, since<br />
the LMA does not occlude the trachea,<br />
a traditional ETT should be<br />
used for patients at high risk for<br />
aspiration.<br />
General anesthesia can be divided<br />
into three phases: induction<br />
INFINIUM MEDICAL . Advanced Medical Technology For <strong>The</strong> World<br />
Infinium Medical has been manufacturing and distributing patient monitors and<br />
anesthesia systems since 2001, and we have been progressively expanding ever<br />
since. Our products are used throughout the entire world. Our patient monitors are<br />
preferred by physicians because they expertly engineered, user-friendly, and they<br />
have the technology necessary to support total patient care.<br />
By reason of superiority product design, ease of use, and product affordability<br />
Infinium Medical has one of the most highly respected reputations in the medical<br />
device community. Our patient monitors have multiple capabilities, offering<br />
everything from basic bedside monitoring to advanced anesthesia monitoring.<br />
With various features such as telemetry, advanced arrhythmia detection, built in<br />
recorders ,and touch screens patient care will be optimized. Infinium patient<br />
monitors provide consistent, reliable support at all times.<br />
OMNI EXPRESS<br />
Transport Monitor<br />
OMNI-VS<br />
Vital Signs Monitor<br />
www.ihe-online.com & search 45557
Apr/May 2010 20 ANEstHEsioLoGy<br />
(loss of consciousness); maintenance (i.e.<br />
when unconsciousness is maintained during<br />
the procedure), and emergence (regaining<br />
of consciousness).<br />
Drugs for anesthesia induction<br />
Various drugs can be used for the induction of<br />
general anesthesia. One commonly used agent<br />
is propofol, a short-acting intravenous drug<br />
used in adult and pediatric patients. It may<br />
also be utilized during the procedure for the<br />
maintenance of anesthesia. Side effects include<br />
hypotension and apnea, as well as pain on injection,<br />
which can be ameliorated by pretreatment<br />
with intravenous lidocaine [8]. Propofol is<br />
often used for cosmetic procedures because it<br />
is associated with reduced PONV and can even<br />
be used as an antiemetic. Thiopental, another<br />
induction agent, is a barbituate that affects fine<br />
motor skills and is notorious for producing a<br />
heavy “hangover” effect and significant PONV<br />
[9]. Midazolam and ketamine can also be used<br />
for induction, although they are associated<br />
with a longer recovery time postoperatively.<br />
Ketamine, a phencyclidine derivitive, is an<br />
anesthetic agent approved for human and veterinary<br />
use, whose popularity in the outpatient<br />
arena has increased over the past several years.<br />
Its effects include analgesia and sedation with<br />
minimal to no respiratory depression. However,<br />
hallucinations, hypertension, increased intracranial<br />
pressure and salivation have limited its<br />
appeal. It has been used successfully with propofol<br />
and midazolam for cosmetic procedures<br />
since it may be used without the need for<br />
endotracheal intubation, supplemental oxygen,<br />
or narcotics [10, 11].<br />
Drugs for anesthesia maintenance<br />
<strong>The</strong> choice of drugs used to maintain anesthesia<br />
is also important to minimize PONV and<br />
allow for a rapid recovery process. Nitrous<br />
oxide is commonly used as an inhalational<br />
agent to maintain anesthesia. Its use reduces<br />
the need for higher concentrations of the<br />
volatile inhalational agents for maintenance<br />
of anesthesia. It is, however, associated with<br />
PONV and should be limited to concentrations<br />
under fifty percent, especially in patients<br />
with evident coronary disease [12].<br />
Isoflurane is one of a number of volatile inhalation<br />
agents commonly used for maintenance<br />
of anesthesia. Desflurane is a shorter acting<br />
member of this class of drugs and may be<br />
more suitable for cosmetic surgery. However,<br />
desflurane often causes postoperative respiratory<br />
irritation and coughing largely due to its<br />
pungent smell. Sevoflurane is better tolerated<br />
than desflurane since it lacks a characteristic<br />
odor. As a result of the lower solubility of<br />
these newer volatile agents, cognitive functions<br />
return to baseline more rapidly when<br />
compared to inhaled isoflurane.<br />
Continuous intravenous anesthetics are commonly<br />
employed in cosmetic surgery. Propofol,<br />
remifentanil, dexmetatomidine and ketamine<br />
are among the most commonly used. Remifentanil<br />
may be used just prior to induction to<br />
suppress the autonomic responses to intubation<br />
and during maintenance to suppress<br />
other autonomic responses to surgical stimuli.<br />
Because it is also a short acting narcotic, it is<br />
ideal for the end of the procedure since it is a<br />
potent cough suppressant. However, like all narcotics<br />
it can cause PONV [13]. Ketamine, like<br />
Propofol, can be used for both induction and<br />
maintenance, though it is often associated with<br />
an increase in blood pressure and salivation, as<br />
well as bad hallucinations. Fortunately, it is not<br />
associated with PONV.<br />
...Patients about to undergo<br />
cosmetic surgery should<br />
be medically optimized<br />
before receiving any type of<br />
anesthetic. A Physical Status<br />
Score (ASA PS) developed by<br />
the the American Society of<br />
Anesthesiologists can help to<br />
determine whether the patient is<br />
suitable for cosmetic surgery...<br />
Emergence<br />
<strong>The</strong> ideal emergence from anesthesia following<br />
cosmetic surgery should not increase blood<br />
pressure or heart rate, lead to “bucking” from<br />
irritation of the endotracheal tube, or have<br />
any respiratory complications [14]. While the<br />
concentration of inhalational and intravenous<br />
anesthetics are lowered to allow the patient<br />
to regain consciousness, additional medications<br />
are administered to restore muscle activity<br />
and allow the patient to breathe spontaneously<br />
to permit extubation. Maneuvers that are<br />
particularly stimulating, such as nasogastric<br />
decompression or suctioning, are done while<br />
the patient is still deeply sedated to prevent<br />
hypertension and gagging. Patients should be<br />
reminded as they emerge from anesthesia that<br />
they may have blurred vision due to the ointment<br />
and should be prevented from attempting<br />
to rub their eyes.<br />
Monitored anesthetic care<br />
Most patients associate surgery with general<br />
anesthesia but other forms of anesthesia exist<br />
along the spectrum of choices for intraoperative<br />
sedation/analgesia and are effectively utilized<br />
for such procedures. Monitored anesthesia care<br />
(MAC) may be offered to patients undergoing<br />
compatible procedures. In this technique,<br />
a combination of local anesthetic and intravenous<br />
analgesic and sedative drugs produces a<br />
“minimally depressed level of consciousness<br />
that retains the patient’s ability to maintain an<br />
airway independently and continuously and to<br />
respond to physical stimuli and verbal commands”<br />
[15, 16]. This anesthetic technique is<br />
often referred to as “conscious sedation” and<br />
the patient will be sedated so as to not feel any<br />
pain or have any keen sense of environmental<br />
awareness. However, unlike in general anesthesia<br />
where unconsciousness is induced and<br />
spontaneous respiration is depressed, patients<br />
will continue to breathe on their own.<br />
Monitored anesthetic care has been shown to be<br />
effective and safe in large study populations [17,<br />
18 , 19]. Typically, a combination of two or more<br />
medication types is used to achieve the desired<br />
level of sedation and analgesia. Commonly used<br />
agents include rapid acting opioids, such as fentanyl,<br />
and sedatives, such as midazolam, and<br />
propofol [20, 21].<br />
Postoperative care<br />
Anesthetic care does not end once the patient<br />
is restored to consciousness. Patients must be<br />
closely monitored postoperatively for signs<br />
and symptoms of hypoxia, hypertension, pain,<br />
PONV and even unconsciousness. A patient<br />
may be discharged once an assessment of<br />
home readiness test is conducted to ensure<br />
that their vital signs are stable, to make sure<br />
they are environmentally aware, and to make<br />
sure they can walk without falling or becoming<br />
excessively dizzy [22]. Patients are also<br />
evaluated for pain, PONV, and bleeding at<br />
the surgical site. Most delays in discharge are<br />
due to pain, PONV, hypotension and dizziness<br />
upon ambulating [23]. All patients require<br />
analgesia postoperatively and some may<br />
require stronger medications than acetaminophen<br />
or NSAID type drugs as part of their<br />
postoperative regimen.<br />
Patients undergoing cosmetic surgery are<br />
generally well informed regarding the nature<br />
of the procedure and the reputation of their<br />
surgeon, but overlook the importance of the<br />
anesthetic technique needed to effectively<br />
perform the procedure. A successful procedure<br />
involves both a plastic surgeon skilled<br />
in cosmetic surgery and an anesthesiologist<br />
proficient in cosmetic anesthesia.<br />
References<br />
1. “2000/2005/2006 National Plastic Surgery Statistics.”<br />
American Society of Plastic Surgeons (ASPS)<br />
www.plasticsurgery.org/<br />
2. “Overall risk of ambulatory anesthesia morbidity<br />
and mortality” In: Miller’s Anesthesia 6th Edition.<br />
Churchill Livingstone, 2004, p. 2234.
3. Practice guidelines for preoperative fasting and<br />
the use of pharmacologic agents to reduce the risk<br />
of pulmonary aspiration: Application to healthy<br />
patients undergoing elective procedures. <strong>Anesthesiology</strong>.<br />
1999; 90, 896-905.<br />
4. Okuda Y et al. Surg Endosc. 2002; 5: 781-4.<br />
5. Rundgren M et al. Anesth Analg. 2008 Nov;107(5):<br />
1465-8.<br />
6. Nique, TA. “Ambulatory Office General Anesthesia.”<br />
In: Anesthesia for Facial Plastic Surgery. New<br />
York: Thieme Medical Publishers, 1993.<br />
7. Cork RC et al. Anesth Analg. 1994; 79: 719-27.<br />
8. Maleck, Mattinger, Piper, Rohm, Papsdorf and<br />
Boldt “Dolasetron reduces pain on injection of<br />
propofol.” Anasthesiol, Intensivmed, Notfallmed,<br />
Schmerzther. [German].2004; 37: 528-31.<br />
9. “Thiopental produces hangover-like effect” In:<br />
Miller’s Anesthesia 5th Edition. Churchill Livingstone,<br />
2000, p. 2224.<br />
10. Friedberg BL. Dermatol Surg 1999; 25:569.<br />
11. Friedberg BK. Aesthetic Plast Surg 1999; 23:70.<br />
12. Moffitt EA et al. Can Anaesth Soc J. 1983; 30:<br />
5-9.<br />
13. Egan TD et al. <strong>Anesthesiology</strong>. 1993; 79(5):881-<br />
92<br />
14. Koga K et al. Anaesthesia 1998; 53(6): 540-4.<br />
15. “MAC” In: Miller’s Anesthesia 5th Edition.<br />
Churchill Livingstone, 2000, p. 2230.<br />
16. Task Force on Sedation and Analgesia by Non-<br />
Anesthesiologists. Practice guidelines for sedation<br />
and analgesia by non-anesthesiologists:<br />
An updated report by the American Society of<br />
Anesthesiologists Task Force of Sedation and<br />
BooK rEViEWs<br />
Pediatric <strong>Anesthesiology</strong> Review<br />
Clinical Cases for Self-assessment<br />
by Holzman R, Mancuso Th J, Sethna N F, DiNardo J A<br />
1st Edition, 340 p., Softcover, Publ. by Springer, 2010<br />
Based on a program of study developed in<br />
the Department of <strong>Anesthesiology</strong> and the<br />
Department of Perioperative and Pain Medicine<br />
at the Children’s Hospital Boston, this<br />
<strong>book</strong> provides essential medical information<br />
for the subspecialty of pediatric anesthesiology.<br />
Illustrating the broad spectrum of the<br />
pediatric anesthesiologist’s practice, the <strong>book</strong><br />
utilizes an interactive question and answer<br />
dialogue which imitates the simplicity of conversation<br />
and affords the reader high-yield<br />
benefits. <strong>The</strong> case-based approach encourages readers to collaborate<br />
with colleagues, improve their oral presentation skills, and prepare for<br />
challenging situations by explaining various anesthesia care plans and<br />
why specific data are required before and during the care of the pediatric<br />
patient. <strong>The</strong> <strong>book</strong> is written by a panel of specialists recognized<br />
internationally for their efforts in their respective areas.<br />
SpRingeR<br />
new York, USA<br />
www.ihe-online.com & search 45565<br />
Analgesia by Non-Anesthesiologists. <strong>Anesthesiology</strong><br />
2002; 4,1004.<br />
17. Bitar G et al. Plast Reconstr Surg 2003;<br />
111, 150.<br />
18. Kryger ZB et al. Plast Reconstr Surg 2004;<br />
113, 1807.<br />
19. Marcus JR et al. Plast Reconstr Surg<br />
1999;104(5):1338-1345.<br />
20. Cinella G et al. Plast Reconstr Surg. 2007; 119(7):<br />
2263-2270.<br />
21. Yoon HD et al. Plast Reconstr Surg 2002;<br />
109, 956.<br />
22. “Assessment of home readiness” In: Miller’s<br />
Anesthesia 5th Edition. Churchill Livingstone,<br />
2000, p. 2232.<br />
23. “Delays in discharge” In: Miller’s Anesthesia<br />
5th Edition. Churchill Livingstone, 2000,<br />
p. 2232.<br />
<strong>The</strong> authors<br />
Peter J. Taub MD, FACS, FAAP<br />
and<br />
Laurence Hausman, MD<br />
Division of Plastic and Reconstructive Surgery<br />
and<br />
Department of <strong>Anesthesiology</strong><br />
Mount Sinai Medical Center<br />
New York, New York, USA<br />
Comments on this article?<br />
Feel free to post them at<br />
www.ihe-online.com/comment/anesthesia<br />
21<br />
Anesthesia Student Survival Guide<br />
A Case-Based Approach<br />
Ed by Ehrenfeld J M, Urman R D & Segal S<br />
1st Edition, 515 p. Softcover, Publ. by Springer, 2010<br />
Apr/May 2010<br />
Monitor Your Costs While<br />
You Monitor Temperature<br />
with Crystaline ®<br />
U.S.A. 813-889-9614 • Fax 813-886-2701<br />
www.ihe-online.com & search 45554<br />
An indispensable introduction to the specialty, this<br />
concise, easy-to-read, affordable hand<strong>book</strong> is ideal<br />
for medical students, nursing students, and others<br />
during the anesthesia rotation. Written in a structured<br />
prose format and supplemented with many<br />
diagrams, tables, and algorithms, the pocket-sized<br />
guide contains essential material. <strong>The</strong> editors, who<br />
are academic faculty at Harvard Medical School,<br />
summarize the essential content with 32 informative<br />
and compelling case studies designed to help<br />
students apply new concepts to real situations.<br />
Pharmacology, basic skills, common procedures and anesthesia subspecialties<br />
are covered, too, with just the right amount of detail for an introductory<br />
text. <strong>The</strong> unique <strong>book</strong> also offers a section containing career advice and<br />
insider tips on how to receive good evaluations from supervising physicians.<br />
<strong>The</strong> <strong>book</strong> combines astute clinical instruction, basic science explanation<br />
and practical tips from physicians that have been there before.<br />
SpRingeR<br />
new York, USA<br />
www.ihe-online.com & search 45566
Apr/May 2010<br />
<strong>The</strong> energy absorbed per unit mass of tissue, the<br />
absorbed dose, mediates the biologic responses<br />
of radionuclide therapy. Specifically for radionuclide<br />
therapy the energy absorbed, E, in a<br />
particular mass of tissue is defined as:<br />
Ε = number of radionuclide disintegrations in<br />
a particular volume X energy emitted per<br />
disintegration of the radionuclide X fraction<br />
of emitted energy that is absorbed by<br />
a particular (target) mass [1].<br />
Nevertheless, to state that the absorbed dose<br />
alone would predict the radiobiologic response<br />
of tissue is an oversimplification that would<br />
certainly lead to hypo- or hyper- estimation of<br />
radiation-induced effects.<br />
Currently, nuclear medicine dosimetry is based<br />
on the measurement of the biokinetics of the<br />
radionuclide by serial gamma camera scans,<br />
followed by calculations comprising three steps.<br />
Firstly, the percentage of administered activity<br />
of the radiopharmaceutical must be determined<br />
for the accumulating organs for several<br />
scan times. Secondly, these biokinetic data must<br />
be integrated to obtain the percentage of the<br />
number of decays in the source organs, i.e the<br />
residence times. Thirdly, the radiation absorbed<br />
doses of critical organs must be determined.<br />
<strong>The</strong> significance of patient<br />
specific dosimetry<br />
In order to understand the limitations, problems,<br />
challenges and research directions of Patient Specific<br />
Dosimetry (PSD), it is useful to consider its<br />
standard clinical practice and compare it with<br />
external beam therapy. Currently, in almost all<br />
PSD treatments the administered activity is fixed;<br />
the clinician empirically modifies it according<br />
to patient characteristics including age, size and<br />
clinical findings [2]. However, clinical studies<br />
have shown that this approach leads to errors in<br />
the order of 30%-100% or even higher. <strong>The</strong> main<br />
reason for such errors is that the absorbed dose is<br />
not only a function of the administered dose, but<br />
is highly correlated to a number of other factors<br />
22 NUCLEAr MEdiCiNE<br />
internal radionuclide dosimetry<br />
the development of patient – specific treatment planning systems is of outmost<br />
importance in the evolvement of radionuclide dosimetry, because the quantification<br />
of the activity in different organs from planar data is hampered by inaccurate<br />
attenuation and scatter correction as well as by background and organ overlay.<br />
Quantitative three-dimensional nuclear medical imaging can be utilized towards<br />
this direction, allowing a more individualized approach.<br />
by dr i. tsougos, dr P. Georgoulias and dr K. theodorou<br />
that are patient-specific, including both anatomical<br />
and functional variations. It is obvious that no<br />
radiation oncologist or medical physicist would<br />
suggest the same protocol in all patients with a<br />
given type of cancer [3]; Variations in beam type,<br />
energy, beam exposure time, geometry, etc are<br />
decided individually for different patients.<br />
Moreover the radioisotope type defines the particles<br />
emitted by the used radionuclide. <strong>The</strong> emitted<br />
particles can be alpha, beta particles, gamma<br />
rays or a combination. <strong>The</strong> type of the emitted<br />
particles and their energy is known. However, the<br />
interaction between the particles and tissue is a<br />
statistical process and accurate calculations are<br />
not straightforward. Radiopharmaceutical kinetics<br />
gives information about a) where the radionuclide<br />
is concentrated, b) in what percentage (at<br />
least theoretically), c) how fast it accumulates in<br />
target organs (both tumors and normal organs)<br />
and d) for how long it remains in these areas [4].<br />
Patient anatomy provides accurate information<br />
about tumor(s) and organs size, as well as possible<br />
non homogeneous areas. Finally, the disease type<br />
plays a critical role in the selection of radiopharmaceuticals<br />
and can affect their kinetic properties.<br />
Patient Specific Dosimetry aims to personalize<br />
the above-mentioned parameters and overcome<br />
the limitations of the standard procedures [5],<br />
resulting in an accurate dose calculation model<br />
that addresses all those issues.<br />
Equation-based dosimetry software<br />
<strong>The</strong> system that defined medical internal dosimetry<br />
for many years is the system developed in<br />
1988 by the Medical Internal Radiation Dose<br />
(MIRD) Committee of the Society of Nuclear<br />
Medicine [6]. <strong>The</strong> equation for absorbed dose<br />
in the MIRD system is as follows:<br />
In this equation, r k represents a target region and<br />
r h represents a source region. <strong>The</strong> cumulated<br />
activity is given in the term Ã. Hence all other<br />
terms of the basic equation are lumped in the S<br />
factor, that is:<br />
<strong>The</strong> use of the ‘S factor’ approach greatly facilitated<br />
dose calculations. <strong>The</strong> S values were initially<br />
calculated based on idealized models of human<br />
anatomy defined as a collection of appropriately<br />
placed distinct organ volumes with mass and<br />
composition that were selected to reflect a typical<br />
or standard human anatomy. <strong>The</strong>se calculations<br />
were performed with very limited computational<br />
power, with the result that there had to<br />
be several simplifying assumptions.<br />
Phantom-based dosimetry software<br />
<strong>The</strong> MIRD methodology has been utilized by<br />
several groups who develop software in which<br />
the S factors were implemented. <strong>The</strong> software<br />
known as MABDOSE [7] allows the user to<br />
place spherically shaped tumors within the<br />
simplified anatomic model originally described<br />
by the MIRD Committee. <strong>The</strong> most widely<br />
used software was the MIRDOSE software<br />
which has had versions 1, 2, 3 and 3.1 [8]. <strong>The</strong><br />
code automated, with great success the calculation<br />
of internal dose for a large number<br />
(>200) of radiopharmaceuticals in 10 different<br />
anthropomorphic models, until it was replaced<br />
by a newer code called OLINDA/EXM (Organ<br />
Level INternal Dose Assessment with EXponential<br />
Modelling) [9].<br />
Image-based dosimetry software<br />
Imaging plays a critical role since the image<br />
provides personalized anatomical as well as<br />
functional information [5]. <strong>The</strong> most evident<br />
information that (tomographic) imaging provides<br />
is the location, the size and the volume<br />
of the organs and the tumor. While anatomical<br />
imaging has obvious importance, the functional<br />
imaging techniques SPECT and PET provide<br />
complementary information about tracers<br />
kinetics and the functionality of tumors<br />
Furthermore the use of 3D imaging modalities,<br />
such as PET/CT and SPECT/CT has allowed<br />
the use of both tomographic functional data and<br />
anatomical data in the development of patientspecific<br />
nuclear medicine dosimetrical systems.<br />
This is made possible by the increase in computer<br />
processing power and the implementation of<br />
point-kernel or Monte Carlo calculation methodologies<br />
for the estimation of absorbed fractions.
In order to achieve 3D image based dosimetry,<br />
there are two requisites. <strong>The</strong> first is a 3D anatomic<br />
imaging study, in order to define the anatomy<br />
and provide tissue density information (e.g CT or<br />
MRI), in conjunction with a 3D imaging of the<br />
radioactivity distribution (e.g. PET or SPECT).<br />
<strong>The</strong> second requisite is appropriate software that<br />
implements the absorbed fraction calculation<br />
(point kernel or Monte Carlo) in order to estimate<br />
the spatial distribution of the absorbed dose.<br />
Based on the above approach several groups<br />
have sought to contribute to the development<br />
of such software, including the following: the<br />
3D-Internal Dosimetry (3D-ID) code [10], the<br />
RTDS code [11] the DOSE3D code [12] and<br />
the SIMDOS code [13].<br />
Monte Carlo and dose kernel-based<br />
dosimetry software<br />
Monte Carlo (MC)<br />
MC is a widely used tool for the simulation, study<br />
and modeling of several processes that limit accuracy<br />
of tomographic and planar images [14]. In<br />
dosimetry the role of MC is to provide additional<br />
tools and methods that will improve image quantification,<br />
thus increasing the accuracy of functional<br />
planar, SPECT or PET images. <strong>The</strong> main<br />
steps include i) scanner and source simulation ii)<br />
study of scatter distributions, attenuation effects,<br />
collimator penetration etc and iii) incorporation<br />
of all this information in reconstruction probability<br />
matrix. Especially in attenuation correction,<br />
MC can be used to correlate CT X-ray attenuation<br />
coefficients to gamma ray photons attenuation,<br />
resulting in improved quantification.<br />
In addition, MC allows the introduction of<br />
advanced phantoms, including patient imaging<br />
data. This leads to advanced correction techniques<br />
optimized for human studies and specific<br />
scanners; When scanner geometry is accurately<br />
modeled, it is possible to assess the effects<br />
of patient size and injected dose on the system’s<br />
count rate e.g. NECR estimation in PET [15].<br />
Anthropomorphic phantoms and MC simulations<br />
are increasingly being used for modeling<br />
heart and respiratory motion. <strong>The</strong> latter can<br />
severely affect image quantification, especially<br />
in the case of CT attenuation correction [16].<br />
Dose kernels<br />
<strong>The</strong>se are defined as the absorbed dose per decay<br />
at a point r distant from the source. A common<br />
strategy is the MC simulation of a point source in<br />
a homogeneous media, after which the absorbed<br />
dose is calculated using convolution methods [17].<br />
This method assumes a uniform patient body,<br />
although recently CT values were used to define<br />
different regions and dose kernels were calculated<br />
by MC for other materials [18]. Dose is determined<br />
by convolving those kernels with the activity of the<br />
nuclear medicine image in 3D space.<br />
<strong>The</strong> main drawback of the method is the difficulty<br />
of incorporating tissue inhomogeneity,<br />
even though it is known from anatomical<br />
images. <strong>The</strong> dose kernel can only be generated<br />
assuming an infinite, homogeneous medium.<br />
In the paper by Loudos et al a method is analytically<br />
described in order to have an accurate<br />
dose estimation that takes into account the CT<br />
information [18]. In that sense the structure of<br />
each patient has to be taken into account. This<br />
information can be obtained by analyzing the<br />
CT image, which provides accurate information<br />
about anatomy and tissue density, provided<br />
that image values in the CT image are scaled as<br />
Hounsfield units. However it has to be taken<br />
into account that the conversion of Hounsfield<br />
units to attenuation coefficients that correspond<br />
to different materials is a complicated<br />
and challenging problem.<br />
Conclusion<br />
Internal radionuclide dosimetry still stands<br />
at an early stage of development, although<br />
it has evolved greatly with the development<br />
of the MIRD models and advanced calculational<br />
techniques. <strong>The</strong> physics of absorbed<br />
dose estimation is improving through active<br />
research in the fields of patient-specific<br />
dosimetry supported by the application<br />
of 3D quantitative imaging. <strong>The</strong> availability<br />
of faster and more powerful computers,<br />
improved and accurate Monte Carlo methods<br />
and imaging devices that support both<br />
anatomy and radioactivity tomography (PET/<br />
CT) will push internal dosimetry into a new<br />
era of individualized therapy.<br />
Nevertheless, it has to be noted that the correction<br />
of the images for all effects that degrade<br />
the quantitative content is especially difficult<br />
to achieve for SPECT or PET images obtained<br />
using non-pure positron emitting nuclides<br />
[19]. However, a treatment-planning approach<br />
23 Apr/May 2010<br />
to radionuclide therapy as in external radiotherapy<br />
will eventually require incorporation<br />
of biologic and radiobiologic considerations<br />
in order to predict response in an individual<br />
patient [20]. Work on this is just beginning.<br />
References<br />
1. Sgouros G. J Nucl Med. 2005 Jan;46 Suppl 1:18S-27S.<br />
2. Flux G et al. Med. Phys. 2006 16 47–59.<br />
3. Siegel JA et al. Cell Mol Biol 2002; 48(5):451-9.<br />
4. Stabin MG et al. Biomed Imaging Interv J 2007;<br />
3(2):e28.<br />
5. Cremonesi M et al. J Nucl Med 2006; 47:1467–1475.<br />
6. Loevinger R et al. MIRD Primer for Absorbed Dose<br />
Calculations 1988 (New York: Society of Nuclear<br />
Medicine).<br />
7. Johnson TK et al. Med Phys. 1999; 26:1389 –1395.<br />
8. Stabin M. J. Nucl. Med. 1996 37 538–46.<br />
9. Stabin M G et al. J. Nucl. Med. 2005 46 1023–7.<br />
10. Kolbert K S et al. J. Nucl. Med. 1997 38 301–8.<br />
11. Liu A et al. J. Nucl. Med. 1999 40 1151–3.<br />
12. Clairand I et al. J. Nucl. Med. 1999 40 1517–23.<br />
13. Dewaraja Y K et al. J. Nucl. Med. 2005 46 840–9.<br />
14. Zaidi H et al. J Nucl Med. 2003 Feb; 44(2):291-315.<br />
15. Watson CC et al. J Nucl Med 2005; 46:1825–1834.<br />
16. Osman MM et al. Eur J Nucl Med Mol Imaging<br />
2003; 30:603–606.<br />
17. Furhang EE et al. Med. Phys. 1996; 23 (5).<br />
18. G Loudos et al. Nucl Med Commun. 2009<br />
Jul;30(7):504-12.<br />
19. Glatting G et al. Nuklearmedizin. 2006;<br />
45(6):269-72.<br />
20. Tsougos I et al. Phys. Med. Biol. 2005; 50 3535-54.<br />
<strong>The</strong> authors<br />
Ioannis Tsougos 1,2 , Panagiotis Georgoulias 2 , Kiki<br />
<strong>The</strong>odorou 1<br />
1 Department of Medical Physics and<br />
2 Department of Nuclear Medicine<br />
Medical School,<br />
University of <strong>The</strong>ssaly, Larissa, Greece
Apr/May 2010<br />
Introduction<br />
Angiogenesis, the formation of new blood<br />
vessels from existing ones, is an essential<br />
process if solid tumors are to grow beyond<br />
2 to 3 mm 3 , since diffusion is no longer sufficient<br />
to supply the tissue with oxygen and<br />
nutrients. Tumor-induced angiogenesis is<br />
a complex multistep process that follows a<br />
characteristic cascade of events mediated<br />
and controlled by growth factors, cellular<br />
receptors and adhesion molecules. Based on<br />
a balance between pro-angiogenic and antiangiogenic<br />
factors, a tumor can stay dormant<br />
for a very long time period until the so-called<br />
“angiogenic switch” occurs. In most tissues<br />
tumors can only grow to a life threatening<br />
size if the tumor is able to trigger angiogenesis.<br />
In tissues with high vessel densities<br />
(e.g. liver, brain, among others), tumors may<br />
also progress via angiogenesis-independent<br />
co-option of the pre-existent vasculature.<br />
Inhibition of angiogenesis is a new cancer treatment<br />
strategy that is now widely investigated<br />
clinically. Researchers have begun to search<br />
for objective measures that indicate pharmacological<br />
responses to anti-angiogenic drugs.<br />
<strong>The</strong>refore there is a great interest in techniques<br />
to visualize angiogenesis in growing tumors<br />
noninvasively. During the past decade several<br />
markers of angiogenesis have been identified<br />
and specific tracers targeting these markers<br />
have been developed.<br />
<strong>The</strong> α v β 3 integrin receptor<br />
<strong>The</strong> α v β 3 integrin is a transmembrane protein<br />
consisting of two non-covalently bound<br />
subunits, α and β. Integrin α v β 3 is minimally<br />
24 NUCLEAr MEdiCiNE<br />
radiolabeled probes for imaging of<br />
tumor angiogenesis<br />
Positron Emission tomography (PEt) and single Photon Emission Computed tomography<br />
(sPECt) are the two radiotracer-based imaging modalities for noninvasive<br />
depiction and quantification of biochemical processes. the development of angiogenesis-targeted<br />
radiotracers is mainly concentrated on peptides, proteins and<br />
antibodies which bind to the α v β 3 integrin receptor, vascular endothelial growth<br />
factor (VEGF) and its receptor, prostate-specific membrane antigen (PMsA), matrix<br />
metalloproteinases (MMPs) and robo-4. several ligands targeting these markers<br />
have been tested as a radiotracer for imaging angiogenesis in tumors in animal<br />
models. the potential of some of these tracers has already been tested in cancer<br />
patients. in this article we present a brief overview of the imaging probes currently<br />
used for noninvasive visualization using PEt and sPECt of α v β 3 and VEGF<br />
expression is given.<br />
by dr i. dijkgraaf and dr o. C. Boerman<br />
expressed on normal quiescent endothelial<br />
cells, but significantly upregulated on activated<br />
endothelial cells during angiogenesis. In addition,<br />
α v β 3 is expressed on the cell membrane of<br />
various tumor cell types such as: ovarian cancer,<br />
neuroblastoma, breast cancer, melanoma,<br />
among others.<br />
This integrin interacts with the arginine-glycine-aspartic<br />
acid (RGD) amino acid sequence<br />
present in extracellular matrix proteins such as<br />
vitronectin, fibrinogen, and laminin.<br />
Several research groups have investigated the<br />
potential of RGD-containing peptides to target<br />
with gamma- or positron-emitting radionuclides<br />
α v β 3 expressed in tumors [Table 1]. Over<br />
the past decade, many radiolabeled cyclic RGD<br />
peptides have been evaluated as potential radiotracers<br />
for noninvasive imaging of integrin<br />
α v β 3 -positive tumors by SPECT or PET. After a<br />
systematic search, the group in Munich developed<br />
a stable 18 F-labeled galactosylated cyclic<br />
pentapeptide ([ 18 F]Galacto-RGD), with a high<br />
affinity and selectivity for α v β 3 that accumulates<br />
specifically in α v β 3 -positive tumors and clears<br />
rapidly via the kidneys. [ 18 F]Galacto-RGD and<br />
[ 18 F]-AH111585 (of which the core peptide<br />
sequence was originally discovered from a<br />
phage display library as ACDRGDCFCG), are<br />
currently under clinical investigation. Recently,<br />
a 99m Tc-labeled RGD-containing peptide<br />
(NC100692) was evaluated in ischemic models<br />
and showed high uptake in areas of neovascularization<br />
with α v β 3 integrin overexpression.<br />
In these models it was shown that NC100692<br />
bund to α v β 3 -expressing endothelial cells in the<br />
regions of angiogenesis.<br />
Clinical studies<br />
[ 18 F]Galacto-RGD was the first radiotracer<br />
applied in patients and could successfully<br />
image α v β 3 expression in human tumors with<br />
good tumor-to-background ratios. It has been<br />
shown that molecular imaging in humans of<br />
α v β 3 expression using [ 18 F]Galacto-RGD correlated<br />
with α v β 3 expression as determined by<br />
immunohistochemistry. In another study, the<br />
tracer uptake of [ 18 F]FDG was compared with<br />
that of [ 18 F]Galacto-RGD in patients with<br />
non-small cell lung cancer (NSCLC, n=10)<br />
and various other tumors (n=8). It was found<br />
that [ 18 F]FDG uptake in tumor lesions did<br />
not correlate with [ 18 F]Galacto-RGD uptake.<br />
Isotope Half-life (h)<br />
γ-emitter (SPECT) 99mTc 6.02<br />
111In 67.2<br />
123I 13.0<br />
125I 59.4 days<br />
β+-emitter (PET) 18F 1.83<br />
11C 20.4 min<br />
64Cu 12.9<br />
68Ga 1.14<br />
124I 100.3<br />
Table 1. Half-life of several radionuclides for SPECT or PET. Half-life is given in hours unless stated otherwise.
<strong>The</strong>se results showed that α v β 3 expression and<br />
glucose metabolism are not closely correlated<br />
in tumor lesions and consequently [ 18 F]FDG<br />
cannot provide similar information as [ 18 F]<br />
Galacto-RGD [Figure 1].<br />
<strong>The</strong> second radiotracer which was applied<br />
in patients was 99m Tc-NC100692. A clinical<br />
study was performed to provide an initial<br />
indication of the efficacy and safety of imaging<br />
malignant breast tumors. Nineteen out of<br />
22 tumors were detected with this radiotracer.<br />
In an additional study, integrin scintimammography<br />
with 99m Tc-NC100692 using a<br />
dedicated γ-camera was performed to investigate<br />
the ability to detect malignant breast<br />
cancer lesions. All patients were known to<br />
have lesions highly suspicious of malignancy.<br />
Dedicated integrin scintimammography<br />
(DISM) detected malignant lesions in seven<br />
out of eight patients with focal uptake in all<br />
but two tumor lesions. In a subsequent openlabel,<br />
multicenter, phase 2a study in late-stage<br />
cancer patients, 99m Tc-NC100692 was able to<br />
detect lung and brain metastases from breast<br />
and lung cancer with scintigraphy.<br />
Multimeric RGD peptides<br />
To improve the efficiency of tumor targeting<br />
and to obtain better in vivo imaging properties,<br />
multimeric RGD peptides were synthesized and<br />
characterized. <strong>The</strong> first cyclic RGD multimers<br />
that were developed, were E[c(RGDfK)] 2 -based<br />
dimers. Subsequently, the use of E[c(RGDyK)] 2 -<br />
based dimers labeled with 64 Cu or 18 F for PET<br />
imaging was reported.<br />
During the last years, various other RGD dimers,<br />
tetramers, and even octamers labeled with<br />
different radionuclides have been developed<br />
and studied in vitro and in vivo. Generally, the<br />
results of these studies have demonstrated that<br />
increasing the multiplicity of the peptide can<br />
significantly enhance the integrin α v β 3 -binding<br />
affinity of RGD peptides and improve tumor<br />
targeting capability of the radiotracer. In addition,<br />
incorporation of the right spacer between<br />
the RGD motifs can enhance the affinity for<br />
α v β 3 and improve the tumor uptake even further.<br />
Among mono-, di-, tetra- and octameric<br />
cyclo(RGDfK)-based peptides, the octamer had<br />
the highest α v β 3 affinity and usually the highest<br />
tumor uptake. From this point of view, further<br />
increase of RGD peptide multiplicity may<br />
result in formation of oligomeric or polymeric<br />
cyclic RGD peptides with improved integrin<br />
α v β 3 -binding affinity and tumor targeting efficacy.<br />
So far, no radiolabeled multimeric RGD<br />
peptide have been tested in patients. <strong>The</strong> studies<br />
on multimeric RGD peptides have recently<br />
been reviewed [1].<br />
VEGF receptors<br />
Vascular endothelial growth factor (VEGF) is a<br />
key regulator of angiogenesis during embryogenesis,<br />
skeletal growth and reproductive functions.<br />
<strong>The</strong> expression of VEGF is upregulated<br />
by environmental stress caused by hypoxia,<br />
Figure 2. Scintigraphic images of 3 athymic male mice with s.c. LS174T tumors immediately after injection and<br />
at 1, 3 and 7 days p.i. of 111 In-bevacizumab (0.9 MBq/mouse, 3 µg/mouse).<br />
25 Apr/May 2010<br />
Figure 1. [ 18 F]FDG-PET of a patient with non-small cell lung cancer (NSCLC) showed intense tracer uptake in<br />
the lesion (a). PET imaging of αvβ3 integrin expression with [ 18 F]Galacto-RGD showed heterogeneous tracer<br />
uptake in the lesion, with a different pattern compared to the [ 18 F]FDG-PET (b). PET/CT (c) and PET/MRI (T2w)<br />
image fusion (d) are useful for a good correlation of anatomical and biological information.<br />
anemia, myocardial ischemia and tumor progression<br />
to initiate neovascularization. Via<br />
alternative mRNA splicing, the human VEGF-A<br />
gene gives rise to four isoforms having 121, 165,<br />
189 and 206 amino acids (VEGF 121 , VEGF 165 ,<br />
VEGF 189 and VEGF 206 , respectively).<br />
VEGF binds two related receptor tyrosine<br />
kinases (RTKs), VEGFR-1 and VEGFR-2. Both<br />
receptors consist of seven Ig-like domains in<br />
the extracellular domain, a single transmembrane<br />
region and a consensus tyrosine kinase<br />
sequence that is interrupted by a kinase-insert<br />
domain. VEGFR-1 binds VEGF with a higher<br />
affinity compared to VEGFR-2 (K d : 25 vs.<br />
75-250 pM).<br />
Bevacizumab is a humanized variant of the<br />
anti-VEGF-A monoclonal antibody (mAb)<br />
A.4.6.1. Nagengast et al were the first to<br />
demonstrate non-invasive VEGF imaging<br />
using radiolabeled bevacizumab [2]. In their<br />
study, they demonstrated the potential of<br />
89 Zr-bevacizumab and 111 In-bevacizumab as<br />
a specific VEGF tracer in nude mice with<br />
human SKOV-3 ovarian tumor xenografts.<br />
At the same time, our group showed specific<br />
imaging of VEGF-A expression using 111 Inbevacizumab<br />
in mice with s.c. human colon<br />
carcinoma xenografts LS174T [Figure 2].<br />
Recently, the potential of 111 In-labeled bevacizumab<br />
to image the expression of VEGF-A
Apr/May 2010 26 NUCLEAr MEdiCiNE<br />
in tumors was investigated in cancer patients.<br />
In a study in colorectal cancer patients with<br />
liver metastases, the liver metastases in nine<br />
out of 12 patients were visualized with 111 Inbevacizumab.<br />
In this study, the liver metastases<br />
were resected after scintigraphic imaging<br />
allowing further immunohistochemical<br />
analysis. <strong>The</strong> VEGF-A expression in these<br />
resected liver metastases was determined by<br />
in situ hybridization and by ELISA. Surprisingly,<br />
no correlation was found between the<br />
level of antibody accumulation and expression<br />
of VEGF-A.<br />
Cai et al. labeled VEGF 121 with 64 Cu via DOTA for<br />
PET imaging of VEGFR expression [3]. Smallanimal<br />
PET imaging revealed rapid, specific<br />
and prominent uptake of 64 Cu-DOTA-VEGF 121<br />
in highly vascularized small U87MG human<br />
glioblastoma tumors (high VEGFR expression),<br />
and significantly lower uptake in large U87MG<br />
tumors (low VEGFR expression).<br />
Conclusions<br />
Numerous markers of tumor vasculature have<br />
been identified, but only a few radiotracers of<br />
angiogenesis have been tested clinically. <strong>The</strong><br />
most extensively studied marker of angiogenesis<br />
is the integrin α v β 3 . For this marker the SPECTtracer,<br />
99m Tc-NC100692, and the PET-tracer<br />
18 F-galacto-RGD have been successfully tested<br />
in cancer patients.<br />
Other targets exclusively expressed on activated<br />
endothelial cells may eventually be better<br />
targets for imaging angiogenesis.<br />
In conclusion, a few radiotracers for imaging<br />
angiogenesis in tumors have been tested in<br />
humans. <strong>The</strong> role of these tracers in assessing<br />
the response to anti-angiogenic therapies has<br />
yet to be assessed.<br />
References<br />
1. Liu S. Radiolabeled multimeric cyclic RGD peptides<br />
as integrin alpha-v-beta-3 targeted radiotracers<br />
for tumor imaging. Mol Pharm 2006; 3,<br />
472-487.<br />
2. Nagengast WB et al. 89 Zr-bevacizumab PET of<br />
early antiangiogenic tumor response to treatment<br />
with HSP90 inhibitor NVP-AUY922. J<br />
Nucl Med. 2010 May; 51(5):761-7. Epub 2010<br />
Apr 15.<br />
3. Cai W et al. PET of vascular endothelial growth<br />
factor receptor expression. J Nucl Med. 2006 Dec;<br />
47(12): 2048-56.<br />
Acknowledgment<br />
<strong>The</strong> authors would like to thank Dr. Ambros J.<br />
Beer at the Technische Universität München<br />
for providing the PET and the PET/CT-, PET/<br />
MRI images.<br />
<strong>The</strong> authors<br />
Dr Ingrid Dijkgraaf and<br />
Dr Otto C. Boerman<br />
Department of Nuclear Medicine<br />
Radboud University<br />
Nijmegen Medical Center,<br />
Nijmegen,<br />
<strong>The</strong> Netherlands<br />
KiMEs 2010 FULFiLs HiGH ExPECtAtioNs As GLoBAL ECoNoMiC<br />
rECoVEry BEGiNs<br />
<strong>The</strong> bustling exhibition was complemented by<br />
many high level symposia and presentations.<br />
<strong>The</strong> 26th edition of the<br />
Korean International Medical<br />
and Hospital Equipment<br />
(KIMES) opened in Seoul,<br />
South Korea in mid-March<br />
so becoming for four days<br />
the place to be for leading<br />
international and Korean<br />
medical and hospital devices<br />
and service providers.<br />
Since KIMES first opened in 1980, the show has grown in parallel with the<br />
rapid development and advances of the Korean medical and healthcare<br />
industry. Over the years, KIMES has always tried to ensure that the show<br />
is the “must be” place so that everyone in the industry can gather information<br />
on advanced medical and healthcare-related items and can share the<br />
latest trends and developments in the sector. As always, there was strong<br />
support from Korean government ministries at this year’s KIMES. <strong>The</strong><br />
supporting organisations included the Ministry of Knowledge Economy,<br />
the Ministry of Health, Welfare and Family Affairs, the Seoul Metropolitan<br />
Government, and the Korean Food & Drug Administration. Recently,<br />
the Korean government specified the medical industry as the one of the<br />
key leading industries driving the Korean economy in the future, and the<br />
government has accordingly provided a blueprint for the financial and<br />
political backing of the industry. Globalization of the medical and healthcare<br />
service industry sector is of particular interest in Korea nowadays; in<br />
the global environment the sharing of information and visions is vital.<br />
Correspondence to:<br />
Ingrid Dijkgraaf<br />
Department of Nuclear Medicine<br />
Radboud University Nijmegen Medical Center<br />
PO Box 9101<br />
6500 HB Nijmegen,<br />
<strong>The</strong> Netherlands<br />
E-mail: I.Dijkgraaf@nucmed.umcn.nl<br />
Comments on this article?<br />
Feel free to post them at<br />
www.ihe-online.com/comment/radiolabels<br />
<strong>The</strong> recent global economy downturn has caused severe difficulties<br />
in the entire Korean economy; this only reinforces the need for the<br />
development of new technologies and new markets, which is more<br />
important than ever<br />
Providing a timely vision of the future of the medical industry, KIMES<br />
2010 attracted 1045 exhibitors from 35 countries. Unaffected by today’s<br />
global shifts, the expectation for KIMES to play its role as a platform<br />
for further development of the industry is as high as ever. <strong>The</strong> organisers<br />
of KIMES are confident that tough conditions can yield rare<br />
opportunities of high potential - future success is often founded in<br />
difficult times like the present.<br />
Many Korean medical product providers launched their newly developed<br />
products at KIMES this year. <strong>The</strong> various exhibit categories at<br />
KIMES this year included: consultation; clinical examination; hospital<br />
accommodation; emergency room equipment; radiology; medical<br />
information systems; surgical equipment; oriental medicine; pharmaceuticals,<br />
physiotherapy equipment; obesity therapies; general healthcare;<br />
ophthalmic and dental equipment; and many others.<br />
In addition, there were more than 40 academic and practical seminars<br />
during the 4 days of the exhibition, providing the opportunity for<br />
KIMES visitors to have a chance to listen to or participate in high level<br />
discussion and perspectives and insights on emerging trends.<br />
<strong>The</strong> 27th edition of KIMES will take place in Seoul, Korea in March 2011.
sCiENtiFiC LitErAtUrE rEViEW: HosPitAL MANAGEMENt<br />
on this page iHE presents a few key<br />
abstracts from the clinical literature<br />
about hospital management, selected<br />
by our editorial board.<br />
Computerised physician order<br />
entry as a new technology for<br />
patients’ safety.<br />
Concern about patient safety is a priority in the<br />
quality policy of health systems. In the pharmacotherapeutic<br />
process, from prescription<br />
to administration of drugs, failures that cause<br />
unwanted effects in patients may occur. This<br />
is especially common in patients with multiple<br />
pathologies and polypharmacy, common<br />
in medical specialities services. It is essential to<br />
analyse and identify the causes that trigger medical<br />
errors to prevent their occurrence. In this<br />
context, computerised physician order entry is<br />
an attractive tool for ensuring patients safety.<br />
Villamañán E, Herrero A, Alvarez-Sala R. Med Clin<br />
(Barc). 2010 Apr 29.<br />
Different usage of the same<br />
oncology information system in two<br />
hospitals in Sydney - lessons go<br />
beyond the initial introduction.<br />
<strong>The</strong> experience of clinicians at two public hospitals<br />
in Sydney, Australia, with the introduction<br />
and use of an oncology information system<br />
(OIS) was examined to extract lessons to guide<br />
the introduction of clinical information systems<br />
in public hospitals. Semi-structured interviews<br />
were conducted with 12 of 15 radiation oncologists<br />
employed at the two hospitals. <strong>The</strong> personnel<br />
involved in the decision making process for<br />
the introduction of the system were contacted<br />
and their decision-making process revisited. <strong>The</strong><br />
transcribed data were analysed using NVIVO<br />
software. <strong>The</strong>mes emerged included implementation<br />
strategies and practices, the radiation oncologists’<br />
current use and satisfaction with the OIS,<br />
project management and the impact of the OIS<br />
on clinical practice. <strong>The</strong> hospitals had contrasting<br />
experiences in their introduction and use of<br />
the OIS. Hospital A used the OIS in all aspects of<br />
clinical documentation. Its implementation was<br />
associated with strong advocacy by the Head of<br />
Department, input by a designated project manager,<br />
and use and development of the system by<br />
all staff, with timely training and support. With<br />
no vision of developing a paperless information<br />
system, Hospital B used the OIS only for <strong>book</strong>ing<br />
and patient tracking. A departmental policy that<br />
data entry for the OIS was centrally undertaken<br />
by administrative staff distanced clinicians from<br />
the system. All the clinicians considered that the<br />
OIS should continuously evolve to meet changing<br />
clinical needs and departmental quality improvement<br />
initiatives. This case study indicates that<br />
critical factors for the successful introduction of<br />
clinical information systems into a hospital environment<br />
were an initial clear vision to be paperless,<br />
strong clinical leadership and management<br />
at the departmental level, committed project<br />
management, and involvement of all staff, with<br />
appropriate training. Clinician engagement is<br />
essential for post-adoption evolution of clinical<br />
information systems.<br />
Yu P, Gandhidasan S, Miller AA. Int J Med Inform<br />
2010 Jun;79(6):422-9.<br />
A critical appraisal of physicianhospital<br />
integration models.<br />
<strong>The</strong> economic environment and the current<br />
healthcare debate have prompted a critical reevaluation<br />
of previous and current physician-hospital<br />
integration models. Even though the independent,<br />
self-employed, private practice, medical staff<br />
remains the most common model, surgical specialists<br />
such as vascular surgeons are increasingly<br />
being employed and integrated into healthcare<br />
delivery systems. <strong>The</strong> degree of integration varies<br />
from minimal to full integration or full employment.<br />
This review defines the forces driving these<br />
changes and analyses the strengths and weaknesses<br />
of each employment model from the physicians’<br />
point of view. Strategies for the successful<br />
implementation of a 21st century integrative<br />
employment model are discussed.<br />
Satiani B, Vaccaro P. J Vasc Surg. 2010 Apr;51(4):<br />
1046-53.<br />
Implementing an electronic<br />
change-of-shift report using<br />
transforming care at the bedside<br />
processes and methods.<br />
Bedside nurses are well positioned to make<br />
changes that positively affect operations and<br />
practice. Using Transforming Care at the<br />
Bedside processes and methods, the authors<br />
describe the clinical nurse-led development,<br />
testing and implementation of an electronic<br />
template and process for change-of-shift report.<br />
Outcomes included a reduction in time spent<br />
in change-of-shift reports, reduced end-of-shift<br />
overtime and a more standardised process,<br />
27 Apr/May 2010<br />
and staff who perceived improved information<br />
quality and were satisfied with the process.<br />
Nelson BA, Massey R. J Nurs Adm. 2010<br />
Apr;40(4):162-8.<br />
Human factors engineering<br />
in healthcare systems:<br />
the problem of human error<br />
and accident management.<br />
This paper discusses some crucial issues associated<br />
with the exploitation of data and information<br />
about healthcare for the improvement of<br />
patient safety. In particular, the issues of human<br />
factors and safety management are analysed in<br />
relation to exploitation of reports about nonconformity<br />
events and field observations. A<br />
methodology for integrating field observation<br />
and theoretical approaches for safety studies is<br />
described. Two sample cases are discussed in<br />
detail: the first one makes reference to the use of<br />
data collected in the aviation domain and shows<br />
how these can be utilised to define hazard and<br />
risk; the second one concerns a typical ethnographic<br />
study in a large hospital structure for the<br />
identification of most relevant areas of intervention.<br />
<strong>The</strong> results show that, if national authorities<br />
find a way to harmonise and formalise critical<br />
aspects, such as the severity of standard events,<br />
it is possible to estimate risk and define auditing<br />
needs, well before the occurrence of serious<br />
incidents, and to indicate practical ways forward<br />
for improving safety standards.<br />
Cacciabue PC, Vella G. Int J Med Inform 2010<br />
Apr;79(4):e1-17.<br />
Effect of point-of-care computer<br />
reminders on physician behaviour:<br />
a systematic review.<br />
<strong>The</strong> opportunity to improve care using computer<br />
reminders is one of the main incentives<br />
for implementing sophisticated clinical information<br />
systems. A systematic review was conducted<br />
to quantify the expected magnitude of<br />
improvements in processes of care from computer<br />
reminders delivered to clinicians during<br />
their routine activities. <strong>The</strong> MEDLINE, Embase<br />
and CINAHL databases (to July 2008) were<br />
searched and the bibliographies of retrieved<br />
articles were scanned. Studies were included<br />
in the review if they used a randomised or<br />
quasi-randomised design to evaluate improvements<br />
in processes or outcomes of care from<br />
computer reminders delivered to physicians<br />
during routine electronic ordering or charting<br />
activities. <strong>The</strong> results were that computer<br />
reminders produced much smaller improvements<br />
than those generally expected from the<br />
implementation of computerised order entry<br />
and electronic medical record systems. Further<br />
research is required to identify features of<br />
reminder systems consistently associated with<br />
clinically worthwhile improvements.<br />
Shojania KG et al. CMAJ. 2010 Mar 23;182(5):<br />
E216-25.
Apr/May 2010<br />
<strong>The</strong> wireless videocapsule was released in<br />
2000 and has opened the last ‘black box’ of<br />
the gastrointestinal tract, enabling complete<br />
endoscopic visualisation of the small bowel<br />
[1]. Since then numerous new developments<br />
from various companies have emerged, with<br />
improvements in image quality, number<br />
of images recorded per second and length<br />
of battery life. In addition the software to<br />
read the images is becoming ever faster and<br />
smarter, and newer developments focus upon<br />
the design of an “interventional” capsule enabling<br />
tissue sampling, directed medication<br />
delivery and functional evaluation of the<br />
small bowel.<br />
Parallel to the development of the diagnostic<br />
wireless videocapsule, conventional enteroscopy<br />
was also subjected to a new evolution in<br />
order to perform all conventional endoscopic<br />
interventions throughout the small bowel. An<br />
overview of the endoscopic developments to<br />
explore the small bowel is given below.<br />
Yesterday’s enteroscopy<br />
Already in the 1970s complete enteroscopy<br />
using a conventional fibre endoscope was<br />
shown to be possible [2]. By means of the ropeway<br />
method, a long fibre endoscope was pulled<br />
down the gastrointestinal tract after a rope<br />
loaded with a weight travelled from mouth to<br />
anus along with gastrointestinal peristalsis.<br />
<strong>The</strong> sonde type method involved a long thin fiberscope<br />
with an inflatable balloon at its distal<br />
tip. <strong>The</strong> scope was inserted through the nose<br />
into the stomach from where it was further<br />
progressed beyond the pylorus using a conventional<br />
endoscope. <strong>The</strong>n the balloon at the<br />
tip of the fiberscope was inflated to serve as a<br />
bolus that was acted on by intestinal peristalsis<br />
to carry the fiberscope down the small intestine<br />
[3]. Although both the ropeway and sonde type<br />
method were effective to visualise the entire<br />
small bowel, and gave the possibility of tissue<br />
sampling, the procedures were very inconvenient<br />
and could last several days.<br />
28 ENdosCoPy<br />
Enteroscopy:<br />
yesterday, today and tomorrow<br />
the small bowel is the most difficult segment of the gastrointestinal tract to investigate.<br />
the present review describes the evolution of enteroscopy, from the first<br />
complete enteroscopy in 1971 through the current balloon-assisted and overtubeguided<br />
methods to likely future development directions aiming for enteroscopic<br />
perfection.<br />
by dr tom G. Moreels<br />
In the 1980s intraoperative enteroscopy became<br />
available as a feasible alternative that is still used<br />
today, although it requires a surgical approach<br />
through laparotomy. It can be performed via<br />
the oral route or the anal route but often enterotomy<br />
is necessary [4]. Because of its invasiveness<br />
the technique is generally reserved as a<br />
last-choice approach.<br />
At the same time push enteroscopy was developed<br />
during the 1990s and rightfully replaced<br />
the previous inconvenient and invasive<br />
enteroscopy methods [5]. Longer conventional<br />
endoscopes were developed to proceed<br />
beyond Treitz’s angulus. Push enteroscopy<br />
allows endoscopic evaluation of the proximal<br />
jejunum through the oral route. Because<br />
of the flexibility of the enteroscope and the<br />
tortuous length of the small bowel, complete<br />
enteroscopy is not possible. <strong>The</strong> pushing force<br />
used to progress the enteroscope throughout<br />
the small bowel results in stretching of the<br />
jejunum, thus hampering further progress and<br />
causing patient discomfort.<br />
<strong>The</strong> introduction of a semi-rigid overtube<br />
allows deeper intubation of the jejunum<br />
because it helps to straighten the enteroscope<br />
and avoids jejunal stretching [6]. <strong>The</strong> use of<br />
an overtube was an important development,<br />
Figure 1: Fujinon Double-Balloon Enteroscope.<br />
leading to a major improvement in insertion<br />
depth and an increase in the yield of push<br />
enteroscopy. However, overtube-guided push<br />
enteroscopy only allows intubation of the<br />
jejunum without complete enteroscopy [7].<br />
Today’s enteroscopy<br />
Although both intraoperative enteroscopy<br />
and overtube-guided push enteroscopy are<br />
still in use, new developments have emerged<br />
which have given rise to improved enteroscopy<br />
performance. <strong>The</strong> concept of balloonassisted<br />
enteroscopy is a second major breakthrough<br />
in the evolution of the endoscopic<br />
disclosure of the small bowel. In 2001 the<br />
Japanese endoscopist Hirohito Yamamoto<br />
revolutionised the concept of overtubeguided<br />
enteroscopy by adding an inflatable<br />
latex balloon at the distal end of the flexible<br />
overtube, allowing better mucosal grip of the<br />
overtube, stabilising its position within the<br />
intestinal lumen. In addition, a second inflatable<br />
latex balloon was added to the distal end<br />
of the enteroscope. With this self-made double-balloon<br />
model, he was able to intubate<br />
the entire small bowel through the oral route<br />
[8]. Since 2003 the double-balloon enteroscope<br />
has been commercially available from<br />
Fujinon [Figure 1].<br />
Following the success of double-balloon<br />
enteroscopy, the Olympus company developed<br />
another system of balloon-assisted<br />
enteroscopy that became commercially<br />
available in 2007, namely single-balloon<br />
enteroscopy that is largely comparable to<br />
double-balloon enteroscopy. It consists of a<br />
latex-free balloon-loaded overtube lacking<br />
the balloon at the distal end of the endoscope<br />
[Figure 2].
Figure 2: Olympus Single-Balloon Enteroscope.<br />
Both balloon-assisted methods are based<br />
upon the push-and-pull principle [9]. It is<br />
a stepwise progression of the enteroscope<br />
through the small intestine with the balloon-loaded<br />
overtube used as a straightening<br />
device, allowing stable position within<br />
the intestinal lumen. <strong>The</strong> extra balloon at<br />
the distal end of the endoscope in the double-balloon<br />
system allows better anchoring<br />
of the endoscope within the lumen, whereas<br />
the single-balloon system allows faster<br />
progression of the endoscope throughout<br />
the small bowel. Both balloon-assisted<br />
methods allow complete intubation of the<br />
small bowel within a reasonable procedure<br />
time, although often a combined approach<br />
through the mouth and the anus is necessary<br />
to complete enteroscopy. In addition,<br />
all conventional endoscopic interventions,<br />
ranging from mucosal tissue sampling, local<br />
hemostasis, polypectomy and balloon dilation,<br />
can now be performed throughout the<br />
length of the small bowel thanks to balloonassisted<br />
enterosopy. Moreover, excluded gastrointestinal<br />
segments after previous small<br />
bowel surgery have come within endoscopic<br />
reach, allowing ERCP procedures in patients<br />
with Roux-en-Y reconstruction of the small<br />
bowel [10]. <strong>The</strong>se important advantages<br />
have led to a rapid spread of both balloonassisted<br />
enteroscopy systems in endoscopy<br />
suites throughout the world.<br />
A novel alternative balloon-assisted method<br />
is the NaviAid balloon-guided enteroscopy,<br />
developed by Smart Medical Systems and distributed<br />
in Europe by Pentax. It consists of a<br />
standard enteroscope loaded with a stabilising<br />
latex-free inflatable balloon at the distal end<br />
of the endoscope and an advancing ballooncatheter<br />
mounted on the outer perimeter of<br />
the endoscope. <strong>The</strong> principle is comparable<br />
to double-balloon enteroscopy, without an<br />
overtube. Preliminary results reveal that this<br />
technique allows deep intubation of the small<br />
bowel, but complete enteroscopy has not been<br />
achieved [11]. <strong>The</strong> results of multicenter trials<br />
are awaited in order to determine the true clinical<br />
value of this new device.<br />
Next to balloon-assisted enteroscopy, Spirus<br />
Medical adapted the overtube resulting in the<br />
development of the EndoEase discovery small<br />
bowel overtube. This spiral overtube enteroscopy<br />
allows rapid and deep intubation of the small<br />
bowel through the oral route [12]. <strong>The</strong> endoscope<br />
remains in a stable position and by rotating<br />
the overtube with its raised helices, the small<br />
bowel is pulled backwards over the endoscope.<br />
It seems to be a feasible, rapid method, however<br />
mucosal and transmural traction lesions have<br />
been reported. Comparative studies between<br />
balloon-assisted enteroscopy and spiral overtube-guided<br />
enteroscopy are awaited.<br />
...wireless video capsule<br />
endoscopy on the one hand and<br />
balloon-assisted or overtube-<br />
guided enteroscopy on the other,<br />
will remain “yin and yang”<br />
techniques, complementing<br />
each other’s imperfections....<br />
Tomorrow’s enteroscopy<br />
Both wireless video capsule enteroscopy on the<br />
one hand and balloon-assisted and overtubeguided<br />
enteroscopy on the other are undergoing<br />
significant development processes, since<br />
no single method is ideal. Although wireless<br />
video capsule enteroscopy allows complete<br />
visualisation of the small bowel without discomfort,<br />
it remains a merely diagnostic procedure<br />
with significant level of false negative<br />
results. On the other hand, balloon-assisted<br />
and overtube-guided enteroscopy are invasive<br />
and time-consuming techniques with a lower<br />
chance of complete enteroscopy, allowing all<br />
conventional endoscopic interventions within<br />
the small bowel.<br />
<strong>The</strong> aims of each of the current development<br />
activities are a higher yield, reduced<br />
patient discomfort, no complications and<br />
better interventional options, which would<br />
represent the ideal, perfect objective. However,<br />
it is unlikely that both approaches will<br />
ever come together in one final, perfect<br />
endoscopic tool for the investigation and<br />
treatment of small bowel pathology. It looks<br />
as though, over the next few years at least,<br />
wireless video capsule enteroscopy and balloon-assisted<br />
and overtube-guided enteroscopy<br />
will remain the “yin and yang” of small<br />
29<br />
Apr/May 2010<br />
bowel visualisation, perfectly complementing<br />
each other’s imperfections.<br />
References<br />
1. Moreels TG. History of endoscopic devices for<br />
the exploration of the small bowel. Acta Gastroenterol<br />
Belg 2009;72:335-337.<br />
2. Hiratsuka H, Hasegawa M, Ushiromachi K,<br />
Endo T, Suzuki S, Nishikawa F. Endoscopic<br />
diagnosis in the small intestine. Stomach Intestine<br />
1972;7:1679-1685.<br />
3. Tada M, Akasaka Y, Misaki F, Kawai K. Clinical<br />
evaluation of a sonde-type small intestinal fiberscope.<br />
Endoscopy 1977;9:33-38.<br />
4. Bosseckert H, Schramm H, Lungershausen G,<br />
Machnik G. Oral intraoperative enteroscopy for<br />
diagnosis of multiple jejunal ulcers. Endoscopy<br />
1981;13:7-8.<br />
5. Foutch PG, Sawyer R, Sanowski RA. Push-enteroscopy<br />
for diagnosis of patients with gastrointestinal<br />
bleeding of obscure origin. Gastrointest<br />
Endoscopy 1990;36:337-341.<br />
6. Shimizu S, Tada M, Kawai K. Development of a<br />
new insertion technique in push-type enteroscopy.<br />
Am J Gastroenterol 1987;82:844-847.<br />
7. Wilmer A, Rutgeerts P. Push enteroscopy. Technique,<br />
depth, and yield of insertion. Gastrointest<br />
Clin N Am 1996;6:759-776.<br />
8. Yamamoto H, Sekine Y, Sato Y, Higashizawa T,<br />
Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy<br />
with a nonsurgical steerable doubleballoon<br />
method. Gastrointest Endosc 2001;<br />
53:216-220.<br />
9. Gerson LB, Flodin JT, Miyabayashi K. Balloon-assisted<br />
enteroscopy: technology and<br />
troubleshooting Gastrointest Endosc 2008;68:<br />
1158-1167.<br />
10. Moreels TG, Hubens GJ, Ysebaert DK, Op de<br />
Beeck B, Pelckmans PA. Diagnostic and therapeutic<br />
double-balloon enteroscopy after small<br />
bowel Roux-en-Y reconstructive surgery.<br />
Digestion 2009;80:141-147.<br />
11. Adler SN, Bjarnason I, Metzger YC. New balloon-guided<br />
technique for deep small intestine<br />
endoscopy using standard endoscopes. Endoscopy<br />
2008;40:502-505.<br />
12. Akerman PA, Agrawal D, Cantero D, Pangtay J.<br />
Spiral enteroscopy with the new DSB overtube:<br />
a novel technique for deep peroral small-bowel<br />
intubation. Endoscopy 2008:40:974-978.<br />
<strong>The</strong> author<br />
Tom G. Moreels<br />
Antwerp University Hospital<br />
Department of Gastroenterology & Hepatology<br />
Wilrijkstraat 10<br />
B-2650 Antwerp, Belgium<br />
Tel. +32-3-821 4974<br />
E-mail: tom.moreels@uza.be<br />
Comments on this article?<br />
Feel free to post them at<br />
www.ihe-online.com/comment/enteroscopy
Apr/May 2010<br />
Rapid blood gas analyzer for<br />
point-of-care<br />
<strong>The</strong> new ABL90 FLEX system from Radiometer<br />
is a cassette-based blood gas analyzer<br />
developed for point-of-care testing (POCT)<br />
and gives healthcare professionals more time<br />
for patient care by providing the fastest blood<br />
gas results available on the market today. It only<br />
takes 35 seconds to perform a test on the comprehensive<br />
acute care panel with 17 parameters.<br />
This is about a third of the time spent on testing<br />
with other analyzers. Rapid test results shorten<br />
the time needed before an accurate diagnosis<br />
can be made and the correct medical treatment<br />
initiated. This provides clinical benefits in the<br />
treatment of patients and contributes to a redution<br />
in in-patient days and costs. For patients<br />
under surveillance e.g. patients suffering from<br />
respiratory diseases or postoperative patients,<br />
it becomes less time consuming to get test<br />
results regularly and it equally frees time for<br />
essential patient care. A turnaround time of 60<br />
seconds reduces time waiting for the analyzer<br />
to be ready for the next test and thus helps to<br />
avoid queues to use the analyzer. <strong>The</strong> ABL90<br />
FLEX is a compact solution with a weight of<br />
only 11 kg; it is portable or can be placed on<br />
a rolling stand. This means that the caregivers<br />
can perform the test and diagnose the patient<br />
close to the bedside, which is proven to provide<br />
better patient outcomes. <strong>The</strong> compact design<br />
is also convenient in hospital wards that are<br />
frequently already packed with equipment.<br />
RAdiometeR<br />
Brønshøj, denmark<br />
www.ihe-online.com & search 45581<br />
Interventional radiology<br />
<strong>The</strong> innovative Advantage Workstation Volume-<br />
Share 4 from GE Healthcare is a complete interventional<br />
suite that gives interventional radiologists<br />
the tools they need to take image-based diagnosis<br />
and minimally invasive therapy to a higher level.<br />
<strong>The</strong> system now incorporates advanced guidance<br />
tools that not only provide precise anatomical<br />
detail, but also help simplify and expedite even<br />
the most complex and challenging diagnostic<br />
and interventional procedures. <strong>The</strong> new system<br />
30<br />
ProdUCt NEWs<br />
delivers excellent image quality, thanks to the builtin<br />
Innova Vision software, at the lowest possible<br />
dose in the industry. <strong>The</strong> software dynamically<br />
overlays 2D fluoroscopic images and 3D models<br />
from multiple modalities, and creates a fused road<br />
mapping display that helps advance guidewires,<br />
catheters, coils and other devices more confidently<br />
by visualizing them on the 3D model in<br />
real time. 3D models can be reconstructed from a<br />
choice of subtracted or non-subtracted rotational<br />
angiography (X-ray), CT or MR images. Registration<br />
of the fused images adjusts automatically in<br />
real time for all changes in C-arm angulations,<br />
source-to-image distance, field of view, table<br />
height and lateral/longitudinal<br />
position, to<br />
provide device<br />
l o c a l i z at i on<br />
at all times.<br />
Fused images<br />
are displayed<br />
on a dedicated<br />
monitor in<br />
the procedure<br />
room and are<br />
easily controlled<br />
from the<br />
central touch<br />
screen at the<br />
tableside.<br />
ge HeAltHCARe<br />
Buc, France<br />
www.ihe-online.com & search 45584<br />
Quantitative MR flow analysis<br />
software<br />
<strong>The</strong> CAAS MR Flow software enables health professionals<br />
to perform quantitative flow analysis on<br />
phase-contrast MR images. <strong>The</strong> system reduces<br />
the time spent on interpreting velocity-encoded<br />
MR data by providing fast and reliable automatic<br />
contour detection for the analysis of the blood<br />
flow in vessels and through heart valves. <strong>The</strong><br />
new software offers the possibility that phase offset<br />
correction based on phantom images can be<br />
directly applied to the images under analysis for<br />
faster and more accurate flow quantification. In<br />
addition, phase offset correction can be applied<br />
based on gradient ROIs and it is now possible to<br />
add and remove datasets while working on an<br />
analysis. It is also possible to add and save user<br />
defined anatomical designations.<br />
pie mediCAl imAging<br />
maastricht, <strong>The</strong> netherlands<br />
www.ihe-online.com & search 45582<br />
Contrast injection system <strong>The</strong> EmpowerCTA<br />
dual-syringe, fixedrate<br />
contrast injector<br />
incorporates<br />
advanced technology<br />
and patient<br />
safety features, to<br />
meet all clinical<br />
and management<br />
requirements. <strong>The</strong><br />
automatic syringe<br />
initialization and<br />
fill volume are<br />
based on selected<br />
protocols, which can be set to meet the requirements<br />
of MDCT scanners. With its flexible<br />
mounting options to meet space requirements,<br />
the system has an exclusive tilt lockout that helps<br />
minimize the likelihood of air embolism.<br />
ACiSt mediCAl SYStemS<br />
eden prairie, mn, USA<br />
www.ihe-online.com & search 45583<br />
Bedside patient monitor and workstation<br />
Bringing superiormonitoringperformance<br />
and patient<br />
information efficiencies<br />
to the<br />
most demanding<br />
care areas,<br />
the Ultraview<br />
SL2800 from<br />
Spacelabs offers<br />
complete monitoring<br />
and<br />
workstation performance in a single bedside<br />
package. In addition, the SL2800 delivers<br />
charting, lab, intranet and HIS applications<br />
to the bedside. <strong>The</strong> system facilitates the<br />
creation of concise and complete electronic<br />
patient records and allows the review of<br />
information from multiple sources without<br />
the need to leave the patient.<br />
SpACelABS HeAltHCARe<br />
issaquah, WA, USA<br />
www.ihe-online.com & search 45580
5-7 October 2010<br />
Marina Bay Sands, Singapore<br />
www.clinicalxasia.com<br />
Asia’s largest CME-led Clinical<br />
Excellence Exhibition & Congress<br />
• Surgery Asia Congress • Imaging & Diagnostics Asia Congress<br />
• Cardiology Asia Congress • Oncology Asia Congress<br />
• Medlab Asia Congress - Laboratory Management, Clinical Chemistry & Microbiology<br />
• Obstetrics & Gynaecology Asia Congress<br />
• Otolaryngology Asia Congress<br />
FREE Admission to the 3-Day Exhibition! *<br />
Please fax back to register at +65 6319 2669<br />
� I would like to register as a visitor to Clinical Excellence Asia Exhibition & Congress 2010<br />
Name: ........................................................................................................<br />
Company: ....................................................................................................<br />
Designation: .................................................................................................<br />
Country: ......................................................................................................<br />
Email: .........................................................................................................<br />
Telephone: ...................................................................................................<br />
Telephone: +65 6319 2668 Fax: +65 6319 2669 Email: clinicalxasia@iirx.com.sg<br />
BOOK<br />
TODAY!<br />
Advance Booking<br />
Discount: Book & Pay<br />
By 2 July 2010 to Enjoy<br />
30% Off! *<br />
*Terms & conditions apply<br />
ORGANISED BY
Apr/May 2010<br />
Meters for X-ray service and QA<br />
<strong>The</strong> Solo range of products from Unfors is a<br />
line of meters specifically developed for quality<br />
assurance and service of diagnostic X-ray<br />
machines. Designed for specific X-ray modalities<br />
to provide the user with essential features<br />
and high precision adapted to fit a defined<br />
need, the Unfors Solo products share the core<br />
technology of the market leader Unfors Xi.<br />
Thanks to its intuitive user interface and builtin<br />
intelligence, users can rapidly learn how to<br />
use the system and can focus on interpreting<br />
the measured data instead of focusing on how<br />
to obtain the data. Not only does the ease of use<br />
of the system save time but, more importantly,<br />
it minimizes the risk of user errors. Depending<br />
on the model used, parameters such as kVp,<br />
dose, dose rate, pulses, time, mA and mAs are<br />
simultaneously measured, with options such<br />
as direct HVL measurements and waveform<br />
display being further enhancements.<br />
UnFoRS<br />
Billdal, Sweden<br />
www.ihe-online.com & search 45571<br />
POC test for Clostridium difficile<br />
Providing results to healthcare<br />
professionals in just 20<br />
minutes, the Remel Xpect<br />
C. difficile Toxin A/B test<br />
from Oxoid is a valuable<br />
diagnostic tool for use in the<br />
rapid detection of Clostridium<br />
difficile infection (CDI).<br />
Extremely easy to use, the<br />
test provides accurate and<br />
reliable results, with a speed and convenience<br />
that enables healthcare professionals to initiate<br />
appropriate patient care and infection control<br />
procedures quickly and decisively. Elderly and<br />
immunocompromised patients who have recently<br />
received antibiotic therapy are most at risk of C. difficile-associated<br />
diarrhoea (CDAD), and infection<br />
can spread quickly throughout hospital wards and<br />
32<br />
ProdUCt NEWs<br />
other healthcare institutions. Early diagnosis is<br />
recognized as one of several factors (including<br />
surveillance, education and infection control<br />
measures) that combine to prevent the spread<br />
of CDI. <strong>The</strong> Xpect Clostridium difficile Toxin<br />
A/B Test allows the direct detection of both<br />
C. difficile toxins A and B.<br />
oxoid<br />
Basingstoke, UK<br />
www.ihe-online.com & search 45572<br />
sNowhere is the processing of CR cassettes more<br />
inconvenient than in a portable environment. To<br />
meet this challenge, a new retrofit kit has been introduced.<br />
<strong>The</strong> kit enables<br />
popular portable<br />
systems to use<br />
the wireless, cassettesized<br />
DRX-1 detector<br />
from Carestream for<br />
instant, high-quality<br />
DR images. With the<br />
DRX-Mobile Retrofit<br />
Kit, images captured<br />
at the point of care<br />
are available in seconds<br />
and can be forwarded<br />
to multiple<br />
network destinations via wireless communications or<br />
cable plug-in, so clinicians can make rapid diagnoses<br />
and begin immediate treatment. <strong>The</strong> new technology<br />
also improves patient positioning and comfort<br />
by eliminating cables and tethers typically required<br />
by most DR-based systems. This makes it ideal for<br />
confined spaces, remote locations and imaging of<br />
patients with limited mobility in addition to emergency<br />
rooms, operating rooms and the ICU. Facilities<br />
that have already implemented a DRX-1 System or<br />
a DRX-Evolution suite can use one of their existing<br />
detectors for portable exams.<br />
CAReStReAm HeAltH<br />
Rochester, nY, US<br />
www.ihe-online.com & search 45573<br />
Protective clothing in radiology<br />
Designed for applications in interventional radiology<br />
and cardiology procedures, CT labs, surgery, and<br />
general radiology, Kiran protective products are made<br />
from proprietary materials, which can be light-weight,<br />
lead-free or, leaded material, all giving the same level<br />
of protection.<br />
<strong>The</strong> company’s most<br />
popular sheeting,<br />
Ultralite, replaces<br />
a large part of lead<br />
with a combination<br />
of tungsten,<br />
bismuth, and antimony,<br />
providing<br />
the same protection<br />
FroNt CoVEr ProdUCt<br />
Ultrasound imaging with<br />
elastography<br />
With its Aixplorer product, the SuperSonic<br />
Imagine company has developed a unique<br />
ultrasound system with an innovative medical<br />
platform that can measure and visualise<br />
tissue elasticity. It is well known that manual<br />
palpation of tissue is part of a routine medical<br />
exam.Today, it is essential to obtain additional<br />
information on tissue elasticity since this can<br />
have a correlation with pathology. Quantitative<br />
values for tissue elasticity can provide more<br />
information about a lesion; more information<br />
leads to enhanced diagnostic confidence. <strong>The</strong><br />
Aixplorer system uses the proprietary Sonic-<br />
Software system, an all software-based architecture<br />
that is extremely rapid and flexible and<br />
provides impeccable image quality. Acquiring<br />
data up to 200 times faster than conventional<br />
ultrasound technology, the Aixplorer is fast<br />
enough to achieve ShearWave Elastography<br />
with ultrafast imaging. <strong>The</strong> system produces,<br />
in real time, a color coded map which represents<br />
tissue elasticity expressed in kilopascals.<br />
A colorscale indicates the level of tissue elasticity<br />
ranging from very soft (blue) to very stiff<br />
(red). With a cutting edge compact design,<br />
intuitive control and touch panels, ultra lightweight<br />
transducer and cables, the system has<br />
many features designed to provide optimal<br />
working conditions.<br />
SUpeRSoniC imAgine<br />
Aix-en-provence, France<br />
www.ihe-online.com & search 45575<br />
as leaded sheeting but at a significantly lower weight.<br />
<strong>The</strong> company’s Leadlite sheeting is the lightest leaded<br />
material in the world, thanks to the use of lead particles<br />
together with mineral oils and bonding materials<br />
replacing artificial plasticizers.<br />
KiRAn mediCAl SYStemS<br />
mumbai, india<br />
www.ihe-online.com & search 45574
Multi-channel ECG<br />
<strong>The</strong> new EPG 6 VIEW Plus system from Progetti<br />
is a 3/6/12 channel electrogardiograph that provides<br />
Hes analysis and interpretation. <strong>The</strong> system<br />
has an internal memory that can store up to 300<br />
tests, and has a pacemaker-detection function.<br />
<strong>The</strong> output is displayed on a LCD TFT color<br />
display. <strong>The</strong> system has USB output ports and is<br />
fully autonomous with built-in PC-compatible<br />
software for data management.<br />
pRogetti<br />
moncalieri, italy<br />
www.ihe-online.com & search 45577<br />
Blood flow monitor<br />
<strong>The</strong> CardioTrace system from Advanced Global<br />
Health is a non-invasive clip that monitors<br />
the blood flow in the arteries to identify<br />
fitness levels or abnormalities, allowing users<br />
to discover in real time whether their lifestyle,<br />
diet and exercise routines need to change. <strong>The</strong><br />
monitor is attached to the patient’s finger and<br />
connected to a computer by a USB connector.<br />
<strong>The</strong> technology then measures for 90 seconds<br />
the speed of the blood travelling through the<br />
larger arteries, calculating the Arterial Stiffness<br />
Index, before comparing the reading against<br />
normal data collected from all ages and ethnicities.<br />
Measuring a person’s pulse speed not<br />
only determines their personal health levels but<br />
also identifies if they are potentially at risk, for<br />
example with a likelihood of developing diseases<br />
such as diabetes or high blood pressure<br />
in the future. <strong>The</strong> device also offers the possibility<br />
of mass screening of populations at low<br />
cost, and with medically accepted accuracy and<br />
correlation. Arterial stiffness continues to be<br />
associated with an increasing number of health<br />
risks and is increasingly used alongside other<br />
ProdUCt NEWs 33 Apr/May 2010<br />
common health markers, strengthening the<br />
value of screening in the community.<br />
AdvAnCed gloBAl HeAltH<br />
gravesend, Kent, UK<br />
www.ihe-online.com & search 45578<br />
Ultra-clean operating theatres and<br />
suites<br />
Jointly developed with the<br />
internationally acclaimed<br />
orthopaedic surgeon, Sir<br />
John Charnley, the Exflow<br />
air unit from Howorth has<br />
a graded velocity airflow,<br />
vertical in the central area<br />
and radially outwards at<br />
the periphery, thus creating<br />
an exponential airflow<br />
profile. <strong>The</strong> system is now available in two<br />
sizes: both models provide microbiological cleanliness<br />
and airflow results that exceed all current<br />
regulatory requirements. <strong>The</strong> latest addition to the<br />
Exflow family has an enlarged ultra clean operating<br />
zone of 3.2 X 3.2m, allowing the entire operating<br />
team and all their instrument tables to be<br />
accommodated beneath the canopy.<br />
HoWoRtH AiR teCHnologY<br />
Farnworth, UK<br />
www.ihe-online.com & search 45579<br />
FroNt CoVEr ProdUCt<br />
Combined PET - MRI scanner<br />
With the installation of the first system that<br />
combine both Magnetic Resonance (MRI )<br />
and Positron Emission Tomography ( PET)<br />
modalities in one single unit, Philips has<br />
achieved a technical breakthrough by overcoming<br />
the potential problems that could be<br />
caused by the magnetic field generated by the<br />
MRI scanner interfering with the operation<br />
of the PET system. Two combined PET-MRI<br />
systems have already been installed (one in<br />
the Geneva University Hospital in Switzerland,<br />
and the other in Mount Sinai Hospital<br />
in New York City, US) and are currently being<br />
extensively evaluated. <strong>The</strong> use of MRI images,<br />
EyeGard is the<br />
safe, effective way<br />
to protect the eyes<br />
during surgery.<br />
• Latex free, hypo-allergenic material<br />
• Reduces lash removals<br />
• Faster and easier than tape<br />
• Adult and pediatric sizes<br />
• Gentler adhesive also available<br />
U.S.A. 813-889-9614 • Fax 813-886-2701<br />
www.ihe-online.com & search 45556<br />
which give anatomical information (without<br />
any of the ionizing radiation associated with<br />
CT X-ray), together with PET images giving<br />
functional information, is synergistic in<br />
diagnostic efficacity and precision. Until now,<br />
PET and MRI investigations were carried out<br />
separately, on two separate instruments and<br />
for scheduling reasons, often on two different<br />
days for the same patient. <strong>The</strong> results of such<br />
separate examinations are difficult to correlate<br />
since the patient can never have exactly<br />
the same position or orientation in the two<br />
separate scanners. <strong>The</strong>re are many reasons for<br />
combining PET and MR scanners together.<br />
<strong>The</strong> most straightforward are the excellent<br />
soft tissue contrast, the elimination of the<br />
extra radiation from the CT (used to provide<br />
both anatomical and attenuation-correction<br />
information) and the multifunctional imaging<br />
ability (thanks to a wide spectrum of<br />
MR sequences and techniques) that complements<br />
the functional molecular information<br />
from the PET. <strong>The</strong> new system are currently<br />
being evaluated in oncology, neurology and<br />
cardiology patients.<br />
pHilipS HeAltHCARe<br />
Eindhoven, <strong>The</strong> Netherlands<br />
www.ihe-online.com & search 45576
Apr/May 2010<br />
FroNt CoVEr ProdUCt<br />
Urology workstation<br />
Thanks to its new dynamic flat detector technology,<br />
the new UROSKOP Omnia system<br />
allows the urologist to cover the entire kidney,<br />
ureter and bladder (KUB) tract with only one<br />
single exposure and in exceptional image quality.<br />
With its curved X-ray column, the new<br />
system allows truly unrestricted patient access<br />
from all table sides. Regardless of the type of<br />
examination, the urologist does not have to<br />
reposition his patient, and the anesthesiologist<br />
can always stay in place. This is very helpful, for<br />
example in case of lateral percutaneous interventions<br />
and increases safety , lowers costs for<br />
room equipment and infrastructure as there is<br />
no need to have a mobile anesthesia workplace.<br />
<strong>The</strong> system allows a variety of clinical applications<br />
such as transurethral and percutaneous<br />
urological interventions, urologic diagnostics<br />
and even gastroenterological cases and general<br />
radiographic applications.Thanks to the large<br />
field-of-view it’s possible to receive a real KUB<br />
image with just one single exposure. Compared<br />
with standard image intensifier systems this<br />
means reduced examination time and less dose<br />
for the patient. Moreover, the system’s resolution<br />
of more than 2800 X 2800 pixels exceeds<br />
that of standard image intensifier systems. <strong>The</strong><br />
high-resolution images enable the physician to<br />
zoom in without any quality loss and to see the<br />
finest details which increases diagnostic confidence.<br />
In addition, the UROSKOP Omnia<br />
allows for digital RAD images, saving costs as<br />
no cassettes are needed.<br />
SiemenS HeAltHCARe<br />
erlangen, germany<br />
www.ihe-online.com & search 45567<br />
34<br />
Multi-modality, vendor neutral PACS<br />
for breast imaging<br />
<strong>The</strong> new IMPAX for Breast Imaging module<br />
from Agfa extends the company’s PACS solution<br />
into breast imaging with unique new features.<br />
For example, it implements the <strong>IHE</strong> Mammography<br />
Image profile, which solves image display<br />
problems typically encountered in mixed vendor<br />
environments, such as: orientation, size,<br />
justification, consistency of grayscale contrast and<br />
ProdUCt NEWs<br />
completeness of annotations.<br />
AgFA HeAltHCARe<br />
mortsel, Belgium<br />
www.ihe-online.com & search 45569<br />
Fetal doppler system<br />
<strong>The</strong> FM-200 fetal doppler system from Shenzhen<br />
Biocare features a signal<br />
strength indicating function<br />
so that the probe can<br />
be located easily. <strong>The</strong> system<br />
is equipped with a<br />
physiological and system<br />
alarm function, with the<br />
alarm limit ranges being<br />
: lower 50 - 120 bpm and<br />
the upper range 160 bpm - 240 bpm. Portable<br />
(with a user belt clamp so that it can be carried<br />
conveniently) and especially designed for pregnancy<br />
monitoring, the system has an adjustable<br />
volume with optional headphone use. <strong>The</strong>re are<br />
three work modes to satisfy the requirements<br />
of all users. <strong>The</strong> system automatically powers<br />
off if there is a signal or probe failure that lasts<br />
for 2 minutes.<br />
SHenZHen BioCARe<br />
Shenzhen, p.R. China<br />
www.ihe-online.com & search 45568<br />
Contrast media delivery system<br />
In addition to the development of high performance<br />
contrast media, the Guerbet company is also<br />
committed to improving their<br />
presentation and delivery systems.<br />
<strong>The</strong> first bag developed<br />
specifically for medical imaging,<br />
the ScanBag, is based on<br />
the IV infusion bag concept,<br />
which were initially made of<br />
polyvinyl chloride (PVC) and<br />
later of polypropylene (PP).<br />
Polypropylene bags are light,<br />
resistant, simple to use, safe to<br />
handle, and provide maximum<br />
asepsis, meet current environmental<br />
requirements and<br />
don’t break if dropped. For all these reasons, PP<br />
was chosen for ScanBag. <strong>The</strong> ScanBag project was<br />
initiated following a study of the current practices<br />
and needs of contrast media users and is based on<br />
technologies widely proven in medical applications,<br />
and on technical innovations which guarantee<br />
the compliance to current requirements in<br />
matters of safety, convenience and environmental<br />
protection.<br />
gUeRBet<br />
Roissy, France<br />
www.ihe-online.com & search 45570<br />
CALENdAr oF EVENts<br />
June 1-3, 2010<br />
Hospital Build Middle East Exhibition<br />
and Congress 2010<br />
Dubai, United Arab Emirates<br />
Tel. +971 4 3365161<br />
Fax +971 4 3364021<br />
e-mail: hospitalbuild@iirme.com<br />
www.hospitalbuild-me.com<br />
June 7-9, 2010<br />
UKRC 2010<br />
Birmingham, UK<br />
Tel. +44 20 7307 1410<br />
e-mail: conference@ukrc.org.uk<br />
www.ukrc.org.uk<br />
June 10-13, 2010<br />
15th Congress of the European<br />
Hematology Association<br />
Barcelona, Spain<br />
Tel. +31 70 3455563<br />
Fax +31 70 3923663<br />
e-mail: info@ehaweb.org<br />
www.ehaweb.org<br />
June 12-15, 2010<br />
Euroanaesthesia 2010<br />
Helsinki, Finland<br />
Tel. +32-2-743 3290<br />
Fax +32-2-743 3298<br />
e-mail: registration@euroanaesthesia.org<br />
www.euroanaesthesia.com<br />
June 16-19, 2010<br />
World Congress of Cardiology<br />
Scientific Sessions 2010<br />
Featuring the 3rd International<br />
Conference on Women, Heart<br />
Disease and Stroke<br />
Beijing, China<br />
e-mail: congress@worldheart.org<br />
www.worldcardiocongress.org<br />
June 16-19, 2010<br />
CARDIOSTIM 2010<br />
17th World Congress in Cardiac<br />
Electrophysiology & Cardiac<br />
Techniques<br />
Nice, France<br />
www.cardiostim.fr?xtor=ADI-5<br />
June 23-26, 2010<br />
CARS 2010 - Computer Assisted<br />
Radiology and Surgery<br />
Geneva, Switzerland<br />
Tel. +49 7742 922 434<br />
Fax +49 7742 922 438<br />
e-mail: office@cars-int.org<br />
www.cars-int.org<br />
August 24-26, 2010<br />
Medifest South Africa 2010<br />
Capetown, South Africa<br />
Tel. +91 11 30580444<br />
e-mail: info@vantagemedifest.com<br />
www.vantagemedifest.com<br />
August 28 – Sep 1, 2010<br />
ESC Congress 2010<br />
Stockholm, Sweden<br />
Tel. +33 492 947 600<br />
Fax +33 492 947 601<br />
www.escardio.org/congresses/<br />
esc-2010<br />
September 14-15, 2010<br />
MHealth 2010<br />
Dubai, UAE<br />
Tel. +44 20 7067 1830<br />
www.m-healthconference.com<br />
September 15-17, 2010<br />
Medical Fair Asia 2010<br />
Suntec Singapore<br />
Tel: + 65 6332 9620<br />
Fax: +65 6332 9655 / 6337<br />
e-mail:<br />
medicalfair-asia@mda.com.sg<br />
www.medicalfair-asia.com<br />
October 5-7, 2010<br />
Clinical Excellence Asia<br />
Marina Bay Sands, Singapore<br />
www.iirme.com/clinicalasia<br />
October 9-13, 2010<br />
23rd ESICM Annual Congress<br />
Barcelona, Spain<br />
Tel. +32 2 559 03 55<br />
Fax +32 2 527 00 62<br />
e-mail: Barcelona2010@esicm.org<br />
www.esicm.org<br />
October 13-16, 2010<br />
CMEF Autumn 2010<br />
Shenyang, Liaoning Province, China<br />
Tel. +86 10 6202 8899 ext 3825<br />
Fax +86 20 6235 9314<br />
e-mail:<br />
jin.liu2@ReedSinopharm.com<br />
http://en.cmef.com.cn/<br />
November 17-20, 2010<br />
MEDICA<br />
Düsseldorf, Germany<br />
e-mail: info@medica.de<br />
www.medica.de<br />
November 28 – December 3<br />
RSNA 2010<br />
Chicago, IL, USA<br />
Tel. +1 630 571 2670<br />
www.rsna.org<br />
December 10-12, 2010<br />
Medifest India 2010<br />
New Delhi, India<br />
Tel. +91 11 30580444<br />
e-mail: info@vantagemedifest.com<br />
www.vantagemedifest.com<br />
February 24-27, 2011<br />
International Conference on Prehypertension<br />
& Cardio Metabolic<br />
Syndrome<br />
Vienna, Austria<br />
Tel. +41 22 5330948<br />
Fax +41 22 5802953<br />
e-mail:<br />
Secretariat@prehypertension.org<br />
www.prehypertension.org<br />
For more events see<br />
www.ihe-online.com/events/<br />
dates and descriptions of future events have been obtained from<br />
usually reliable official industrial sources. iHE cannot be held<br />
responsible for errors, changes or cancellations.
www.ihe-online.com & search 45549
A partnership founded on a promise of limitless commitment<br />
will get your success started immediately.<br />
<strong>The</strong> healthcare business is undergoing fundamental changes. Thanks to our experience, adaptive business models and<br />
our products and solutions, we can offer you expert advice that will keep you moving forward. <strong>The</strong> heart of the matter<br />
of a good partnership is a promise. And our promise to you is support across-the-board. Long-term.<br />
www.siemens.com/healthcare-partnership<br />
A91CC-9071-A1-7600<br />
Answers for life.<br />
www.ihe-online.com & search 45543<br />
Now that we know what doesn’t work,<br />
can anybody tell us what does?<br />
Read the QR<br />
code with the<br />
QR code reader<br />
in your mobile!