Vaginal examinations in labour Queensland Maternity and Neonatal ...
Vaginal examinations in labour Queensland Maternity and Neonatal ...
Vaginal examinations in labour Queensland Maternity and Neonatal ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Queensl<strong>and</strong></strong> <strong>Maternity</strong> <strong>and</strong> <strong>Neonatal</strong> Cl<strong>in</strong>ical Guidel<strong>in</strong>es Program<br />
Version 3.0 last updated: 05/04/2013<br />
<strong>Vag<strong>in</strong>al</strong> <strong>exam<strong>in</strong>ations</strong> <strong>in</strong> <strong>labour</strong><br />
Parent <strong>in</strong>formation sheet<br />
This <strong>in</strong>formation sheet aims to answer some questions you might have<br />
about hav<strong>in</strong>g a vag<strong>in</strong>al exam<strong>in</strong>ation <strong>in</strong> <strong>labour</strong>.<br />
IMPORTANT: The <strong>in</strong>formation conta<strong>in</strong>ed <strong>in</strong> this <strong>in</strong>formation sheet is general<br />
<strong>in</strong>formation only. It is not <strong>in</strong>tended to be treated by you as professional advice for a<br />
particular factual situation <strong>and</strong> is no substitute for seek<strong>in</strong>g professional advice from<br />
your health care provider. In all procedures your health care provider will expla<strong>in</strong> what<br />
will happen, the risks <strong>and</strong> benefits <strong>and</strong> will ask for your <strong>in</strong>formed consent. If you choose<br />
not to have an <strong>in</strong>tervention your decision will be respected.<br />
What is a vag<strong>in</strong>al<br />
exam<strong>in</strong>ation<br />
A vag<strong>in</strong>al exam<strong>in</strong>ation is an <strong>in</strong>ternal<br />
exam<strong>in</strong>ation of the vag<strong>in</strong>a <strong>and</strong><br />
cervix (bottom part of the uterus at<br />
the <strong>in</strong>side end of the vag<strong>in</strong>a) <strong>and</strong> is<br />
sometimes called an ‘<strong>in</strong>ternal,’ ‘VE’<br />
or ‘<strong>in</strong>ternal exam<strong>in</strong>ation.’<br />
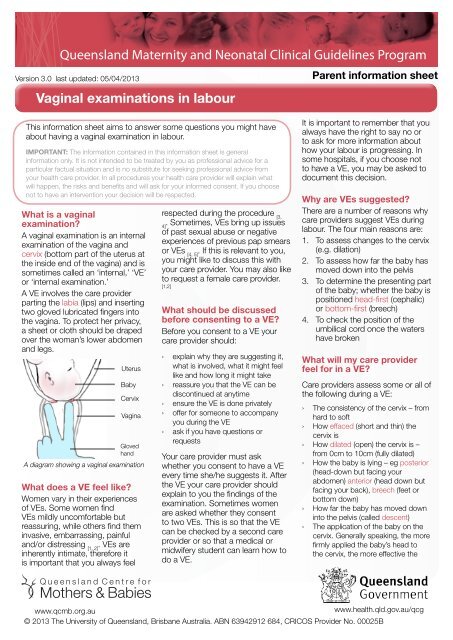
A VE <strong>in</strong>volves the care provider<br />
part<strong>in</strong>g the labia (lips) <strong>and</strong> <strong>in</strong>sert<strong>in</strong>g<br />
two gloved lubricated f<strong>in</strong>gers <strong>in</strong>to<br />
the vag<strong>in</strong>a. To protect her privacy,<br />
a sheet or cloth should be draped<br />
over the woman’s lower abdomen<br />
<strong>and</strong> legs.<br />
Uterus<br />
Baby<br />
Cervix<br />
Vag<strong>in</strong>a<br />
Gloved<br />
h<strong>and</strong><br />
A diagram show<strong>in</strong>g a vag<strong>in</strong>al exam<strong>in</strong>ation<br />
What does a VE feel like<br />
Women vary <strong>in</strong> their experiences<br />
of VEs. Some women f<strong>in</strong>d<br />
VEs mildly uncomfortable but<br />
reassur<strong>in</strong>g, while others f<strong>in</strong>d them<br />
<strong>in</strong>vasive, embarrass<strong>in</strong>g, pa<strong>in</strong>ful<br />
<strong>and</strong>/or distress<strong>in</strong>g [1, 2]<br />
. VEs are<br />
<strong>in</strong>herently <strong>in</strong>timate, therefore it<br />
is important that you always feel<br />
respected dur<strong>in</strong>g the procedure [3,<br />
. Sometimes, VEs br<strong>in</strong>g up issues<br />
4]<br />
of past sexual abuse or negative<br />
experiences of previous pap smears<br />
or VEs [4, 5]<br />
. If this is relevant to you,<br />
you might like to discuss this with<br />
your care provider. You may also like<br />
to request a female care provider.<br />
[1,2]<br />
What should be discussed<br />
before consent<strong>in</strong>g to a VE<br />
Before you consent to a VE your<br />
care provider should:<br />
››<br />
expla<strong>in</strong> why they are suggest<strong>in</strong>g it,<br />
what is <strong>in</strong>volved, what it might feel<br />
like <strong>and</strong> how long it might take<br />
››<br />
reassure you that the VE can be<br />
discont<strong>in</strong>ued at anytime<br />
››<br />
ensure the VE is done privately<br />
››<br />
offer for someone to accompany<br />
you dur<strong>in</strong>g the VE<br />
››<br />
ask if you have questions or<br />
requests<br />
Your care provider must ask<br />
whether you consent to have a VE<br />
every time she/he suggests it. After<br />
the VE your care provider should<br />
expla<strong>in</strong> to you the f<strong>in</strong>d<strong>in</strong>gs of the<br />
exam<strong>in</strong>ation. Sometimes women<br />
are asked whether they consent<br />
to two VEs. This is so that the VE<br />
can be checked by a second care<br />
provider or so that a medical or<br />
midwifery student can learn how to<br />
do a VE.<br />
It is important to remember that you<br />
always have the right to say no or<br />
to ask for more <strong>in</strong>formation about<br />
how your <strong>labour</strong> is progress<strong>in</strong>g. In<br />
some hospitals, if you choose not<br />
to have a VE, you may be asked to<br />
document this decision.<br />
Why are VEs suggested<br />
There are a number of reasons why<br />
care providers suggest VEs dur<strong>in</strong>g<br />
<strong>labour</strong>. The four ma<strong>in</strong> reasons are:<br />
1. To assess changes to the cervix<br />
(e.g. dilation)<br />
2. To assess how far the baby has<br />
moved down <strong>in</strong>to the pelvis<br />
3. To determ<strong>in</strong>e the present<strong>in</strong>g part<br />
of the baby; whether the baby is<br />
positioned head-first (cephalic)<br />
or bottom-first (breech)<br />
4. To check the position of the<br />
umbilical cord once the waters<br />
have broken<br />
What will my care provider<br />
feel for <strong>in</strong> a VE<br />
Care providers assess some or all of<br />
the follow<strong>in</strong>g dur<strong>in</strong>g a VE:<br />
››<br />
The consistency of the cervix – from<br />
hard to soft<br />
›How › effaced (short <strong>and</strong> th<strong>in</strong>) the<br />
cervix is<br />
›How › dilated (open) the cervix is –<br />
from 0cm to 10cm (fully dilated)<br />
››<br />
How the baby is ly<strong>in</strong>g – eg posterior<br />
(head-down but fac<strong>in</strong>g your<br />
abdomen) anterior (head down but<br />
fac<strong>in</strong>g your back), breech (feet or<br />
bottom down)<br />
››<br />
How far the baby has moved down<br />
<strong>in</strong>to the pelvis (called descent)<br />
››<br />
The application of the baby on the<br />
cervix. Generally speak<strong>in</strong>g, the more<br />
firmly applied the baby’s head to<br />
the cervix, the more effective the<br />
www.qcmb.org.au<br />
www.health.qld.gov.au/qcg<br />
© 2013 The University of <strong>Queensl<strong>and</strong></strong>, Brisbane Australia. ABN 63942912 684, CRICOS Provider No. 00025B
dilation. In breech births, the baby’s<br />
bottom/foot is softer than the head<br />
<strong>and</strong> therefore the dilation may be a<br />
little slower.<br />
How are cervical changes<br />
related to <strong>labour</strong> progress<br />
In general, the more soft, dilated<br />
<strong>and</strong> effaced the cervix, <strong>and</strong> the<br />
more applied the head (or bottom)<br />
is to the cervix, the more effective<br />
the contractions will be <strong>and</strong> the<br />
quicker the woman will progress <strong>in</strong><br />
<strong>labour</strong>.<br />
Is a VE the only way to<br />
assess <strong>labour</strong> progression<br />
Uterus<br />
Cervix<br />
Vag<strong>in</strong>a<br />
1 cm 5 cm<br />
<strong>labour</strong>. While a VE can provide<br />
<strong>in</strong>formation about how a woman<br />
has progressed so far <strong>in</strong> <strong>labour</strong>, it<br />
cannot predict how much longer<br />
you will be <strong>in</strong> <strong>labour</strong> or when you will<br />
give birth.<br />
How accurate are VEs<br />
Care providers assess effacement<br />
<strong>and</strong> dilation differently <strong>and</strong><br />
sometimes <strong>in</strong>accurately [8, 9]<br />
. If<br />
possible, VEs should be done by<br />
the same care provider [10]<br />
.<br />
How often are VEs done<br />
There is currently no evidence about<br />
how often VEs should be suggested<br />
dur<strong>in</strong>g <strong>labour</strong> [1]<br />
. One VE every four<br />
hours is common <strong>in</strong> <strong>Queensl<strong>and</strong></strong><br />
10 cm<br />
hospitals [11]<br />
. In general, VEs should<br />
only be suggested if it is:<br />
››<br />
Believed to be necessary; <strong>and</strong> if it’s<br />
Why are VEs suggested upon<br />
arrival to hospital <strong>in</strong> <strong>labour</strong><br />
It is common to be offered a VE<br />
when you arrive to hospital. This is<br />
to determ<strong>in</strong>e whether or not you are<br />
<strong>in</strong> ‘established’ <strong>labour</strong>. Established<br />
<strong>labour</strong> is when a woman is hav<strong>in</strong>g<br />
regular, pa<strong>in</strong>ful contractions with<br />
greater than 3 - 5cm cervical<br />
dilation [11, 15]<br />
. The term ‘early<br />
<strong>labour</strong>’ describes the period before<br />
established <strong>labour</strong>.<br />
VEs are suggested upon arrival to<br />
hospital because be<strong>in</strong>g admitted<br />
to the <strong>labour</strong> ward <strong>in</strong> early <strong>labour</strong><br />
is associated with <strong>in</strong>creased<br />
<strong>in</strong>terventions (e.g. augmentation,<br />
epidural, <strong>in</strong>strumental birth) [16, 17]<br />
.<br />
This is why some hospital staff<br />
suggest women to walk around<br />
or return home until they are <strong>in</strong><br />
established <strong>labour</strong>.<br />
1. Cervix is not effaced<br />
(cervix is long <strong>and</strong> thick)<br />
or dilated<br />
2. Cervix is fully effaced<br />
(cervix is short <strong>and</strong> th<strong>in</strong>)<br />
<strong>and</strong> 1 cm dilated<br />
3. Cervix [12, 13] is fully effaced<br />
<strong>and</strong> 5 cm dilated<br />
4. Cervix is fully effaced<br />
››<br />
Judged to benefit <strong>and</strong> the 10 woman’s<br />
cm dilated<br />
<strong>labour</strong> care <strong>and</strong> decision mak<strong>in</strong>g -<br />
tak<strong>in</strong>g <strong>in</strong>to account women’s needs<br />
<strong>and</strong> preferences<br />
[13]<br />
y effaced<br />
<strong>and</strong> th<strong>in</strong>)<br />
ed<br />
5 cm<br />
3. Cervix is fully effaced<br />
<strong>and</strong> 5 cm dilated<br />
10 cm<br />
4. Cervix is fully effaced<br />
<strong>and</strong> 10 cm dilated<br />
A diagram show<strong>in</strong>g the effacement <strong>and</strong> dilation<br />
VEs are the most common method<br />
of assess<strong>in</strong>g progress <strong>in</strong> <strong>labour</strong>,<br />
however they are not the only<br />
<strong>in</strong>dicator [6, 7]<br />
. There are other factors<br />
such as the strength, duration <strong>and</strong><br />
length of contractions as well as a<br />
woman’s behaviour <strong>and</strong> wellbe<strong>in</strong>g<br />
that can <strong>in</strong>dicate progress <strong>in</strong><br />
Repeated VEs are associated with<br />
a risk of <strong>in</strong>fection [7]<br />
. After rupture of<br />
membranes (when the ‘waters’ or<br />
amniotic sac has broken) the risk of<br />
<strong>in</strong>fection is significantly <strong>in</strong>creased<br />
after 3 or more VEs<br />
[14] .<br />
Are there times when VEs are<br />
required<br />
In some hospitals certa<strong>in</strong><br />
<strong>in</strong>terventions <strong>in</strong> <strong>labour</strong> require a VE,<br />
e.g. an <strong>in</strong>duction of <strong>labour</strong> (when a<br />
care provider tries to artificially start<br />
off <strong>labour</strong>) or epidural (a drug used<br />
to numb the lower half of the body).<br />
If you have comments about this<br />
parent <strong>in</strong>formation sheet please email<br />
<strong>in</strong>fo@qcmb.org.au<br />
Comfort, support & Information<br />
13 HEALTH (13 432584) provides health <strong>in</strong>formation, referral <strong>and</strong> services to the publicover the phone.<br />
www.health.qld.gov.au/13health<br />
Pregnancy, Birth & Baby Helpl<strong>in</strong>e 1800 882 436 (free call). Free, confidential, professional <strong>in</strong>formation <strong>and</strong><br />
counsell<strong>in</strong>g for women, their partners <strong>and</strong> families relat<strong>in</strong>g to issues of conception, pregnancy, birth<strong>in</strong>g <strong>and</strong> postnatal<br />
care.<br />
Lifel<strong>in</strong>e 13 11 14 Lifel<strong>in</strong>e offers a telephone crisis support service.<br />
References: Available from www.qcmb.org.au/media/doc/References_VE.docx