Diagnostic Value of Fine-Needle Aspiration in Supraclavicular ...
Diagnostic Value of Fine-Needle Aspiration in Supraclavicular ...
Diagnostic Value of Fine-Needle Aspiration in Supraclavicular ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
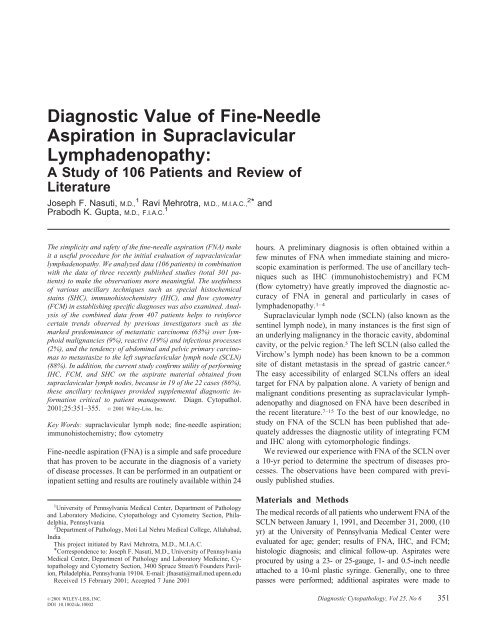
<strong>Diagnostic</strong> <strong>Value</strong> <strong>of</strong> <strong>F<strong>in</strong>e</strong>-<strong>Needle</strong><br />
<strong>Aspiration</strong> <strong>in</strong> <strong>Supraclavicular</strong><br />
Lymphadenopathy:<br />
A Study <strong>of</strong> 106 Patients and Review <strong>of</strong><br />
Literature<br />
Joseph F. Nasuti, M.D., 1 Ravi Mehrotra, M.D., M.I.A.C., 2 * and<br />
Prabodh K. Gupta, M.D., F.I.A.C. 1<br />
The simplicity and safety <strong>of</strong> the f<strong>in</strong>e-needle aspiration (FNA) make<br />
it a useful procedure for the <strong>in</strong>itial evaluation <strong>of</strong> supraclavicular<br />
lymphadenopathy. We analyzed data (106 patients) <strong>in</strong> comb<strong>in</strong>ation<br />
with the data <strong>of</strong> three recently published studies (total 301 patients)<br />
to make the observations more mean<strong>in</strong>gful. The usefulness<br />
<strong>of</strong> various ancillary techniques such as special histochemical<br />
sta<strong>in</strong>s (SHC), immunohistochemistry (IHC), and flow cytometry<br />
(FCM) <strong>in</strong> establish<strong>in</strong>g specific diagnoses was also exam<strong>in</strong>ed. Analysis<br />
<strong>of</strong> the comb<strong>in</strong>ed data from 407 patients helps to re<strong>in</strong>force<br />
certa<strong>in</strong> trends observed by previous <strong>in</strong>vestigators such as the<br />
marked predom<strong>in</strong>ance <strong>of</strong> metastatic carc<strong>in</strong>oma (63%) over lymphoid<br />
malignancies (9%), reactive (19%) and <strong>in</strong>fectious processes<br />
(2%), and the tendency <strong>of</strong> abdom<strong>in</strong>al and pelvic primary carc<strong>in</strong>omas<br />
to metastasize to the left supraclavicular lymph node (SCLN)<br />
(88%). In addition, the current study confirms utility <strong>of</strong> perform<strong>in</strong>g<br />
IHC, FCM, and SHC on the aspirate material obta<strong>in</strong>ed from<br />
supraclavicular lymph nodes, because <strong>in</strong> 19 <strong>of</strong> the 22 cases (86%),<br />
these ancillary techniques provided supplemental diagnostic <strong>in</strong>formation<br />
critical to patient management. Diagn. Cytopathol.<br />
2001;25:351–355. © 2001 Wiley-Liss, Inc.<br />
Key Words: supraclavicular lymph node; f<strong>in</strong>e-needle aspiration;<br />
immunohistochemistry; flow cytometry<br />
<strong>F<strong>in</strong>e</strong>-needle aspiration (FNA) is a simple and safe procedure<br />
that has proven to be accurate <strong>in</strong> the diagnosis <strong>of</strong> a variety<br />
<strong>of</strong> disease processes. It can be performed <strong>in</strong> an outpatient or<br />
<strong>in</strong>patient sett<strong>in</strong>g and results are rout<strong>in</strong>ely available with<strong>in</strong> 24<br />
1 University <strong>of</strong> Pennsylvania Medical Center, Department <strong>of</strong> Pathology<br />
and Laboratory Medic<strong>in</strong>e, Cytopathology and Cytometry Section, Philadelphia,<br />
Pennsylvania<br />
2 Department <strong>of</strong> Pathology, Moti Lal Nehru Medical College, Allahabad,<br />
India<br />
This project <strong>in</strong>itiated by Ravi Mehrotra, M.D., M.I.A.C.<br />
*Correspondence to: Joseph F. Nasuti, M.D., University <strong>of</strong> Pennsylvania<br />
Medical Center, Department <strong>of</strong> Pathology and Laboratory Medic<strong>in</strong>e, Cytopathology<br />
and Cytometry Section, 3400 Spruce Street/6 Founders Pavilion,<br />
Philadelphia, Pennsylvania 19104. E-mail: jfnasuti@mail.med.upenn.edu<br />
Received 15 February 2001; Accepted 7 June 2001<br />
hours. A prelim<strong>in</strong>ary diagnosis is <strong>of</strong>ten obta<strong>in</strong>ed with<strong>in</strong> a<br />
few m<strong>in</strong>utes <strong>of</strong> FNA when immediate sta<strong>in</strong><strong>in</strong>g and microscopic<br />
exam<strong>in</strong>ation is performed. The use <strong>of</strong> ancillary techniques<br />
such as IHC (immunohistochemistry) and FCM<br />
(flow cytometry) have greatly improved the diagnostic accuracy<br />
<strong>of</strong> FNA <strong>in</strong> general and particularly <strong>in</strong> cases <strong>of</strong><br />
lymphadenopathy. 1–4<br />
<strong>Supraclavicular</strong> lymph node (SCLN) (also known as the<br />
sent<strong>in</strong>el lymph node), <strong>in</strong> many <strong>in</strong>stances is the first sign <strong>of</strong><br />
an underly<strong>in</strong>g malignancy <strong>in</strong> the thoracic cavity, abdom<strong>in</strong>al<br />
cavity, or the pelvic region. 5 The left SCLN (also called the<br />
Virchow’s lymph node) has been known to be a common<br />
site <strong>of</strong> distant metastasis <strong>in</strong> the spread <strong>of</strong> gastric cancer. 6<br />
The easy accessibility <strong>of</strong> enlarged SCLNs <strong>of</strong>fers an ideal<br />
target for FNA by palpation alone. A variety <strong>of</strong> benign and<br />
malignant conditions present<strong>in</strong>g as supraclavicular lymphadenopathy<br />
and diagnosed on FNA have been described <strong>in</strong><br />
the recent literature. 7–15 To the best <strong>of</strong> our knowledge, no<br />
study on FNA <strong>of</strong> the SCLN has been published that adequately<br />
addresses the diagnostic utility <strong>of</strong> <strong>in</strong>tegrat<strong>in</strong>g FCM<br />
and IHC along with cytomorphologic f<strong>in</strong>d<strong>in</strong>gs.<br />
We reviewed our experience with FNA <strong>of</strong> the SCLN over<br />
a 10-yr period to determ<strong>in</strong>e the spectrum <strong>of</strong> diseases processes.<br />
The observations have been compared with previously<br />
published studies.<br />
Materials and Methods<br />
The medical records <strong>of</strong> all patients who underwent FNA <strong>of</strong> the<br />
SCLN between January 1, 1991, and December 31, 2000, (10<br />
yr) at the University <strong>of</strong> Pennsylvania Medical Center were<br />
evaluated for age; gender; results <strong>of</strong> FNA, IHC, and FCM;<br />
histologic diagnosis; and cl<strong>in</strong>ical follow-up. Aspirates were<br />
procured by us<strong>in</strong>g a 23- or 25-gauge, 1- and 0.5-<strong>in</strong>ch needle<br />
attached to a 10-ml plastic syr<strong>in</strong>ge. Generally, one to three<br />
passes were performed; additional aspirates were made to<br />
© 2001 WILEY-LISS, INC. <strong>Diagnostic</strong> Cytopathology, Vol 25, No 6 351<br />
DOI 10.1002/dc.10002
NASUTI ET AL.<br />
Fig. C-1. A: FNA <strong>of</strong> tuberculosis, note the epithelioid granuloma <strong>in</strong> a background <strong>of</strong> acute <strong>in</strong>flammation and necrotic debris (Papanicolaou sta<strong>in</strong>ed, 95%<br />
ethanol-fixed direct smear, 200). B: Note the magenta-sta<strong>in</strong>ed bacilli scattered with<strong>in</strong> the cytoplasm <strong>of</strong> histocytes and <strong>in</strong> the background <strong>of</strong> the same FNA<br />
material obta<strong>in</strong>ed from the case depicted <strong>in</strong> Figure 2A (acid-fast sta<strong>in</strong> performed on 95% ethanol-fixed direct smear, 1,000).<br />
Fig. C-2. A: <strong>F<strong>in</strong>e</strong>-needle aspiration (FNA) <strong>of</strong> metastatic prostate carc<strong>in</strong>oma conta<strong>in</strong><strong>in</strong>g pleomorphic epithelial tumor cells characterized by irregular<br />
vesicular nuclei with prom<strong>in</strong>ent nucleoli (Papanicolaou sta<strong>in</strong>ed, 95% ethanol-fixed direct smear, 400). B: Note the cytoplasmic sta<strong>in</strong><strong>in</strong>g <strong>of</strong> prostatespecific<br />
antigen (PSA) <strong>in</strong> tumor cells from the cell block FNA material obta<strong>in</strong>ed from same case depicted <strong>in</strong> Figure 1A (PSA antigen-antibody reaction<br />
performed on cell block processed material with diam<strong>in</strong>obenzid<strong>in</strong>e chromagen, 800).<br />
<strong>in</strong>crease the harvest <strong>of</strong> cells for possible ancillary studies (FCM<br />
and IHC). Aspirated material was smeared onto glass slides,<br />
with half the smears immediately fixed <strong>in</strong> 95% alcohol for<br />
Papanicolaou sta<strong>in</strong><strong>in</strong>g and the other half allowed to air-dry for<br />
Diff-Quick sta<strong>in</strong> (Becton-Dick<strong>in</strong>son, San Jose, CA). The residual<br />
material from each pass was r<strong>in</strong>sed <strong>in</strong> Normosol solution<br />
for Millipore filter preparation, cell block, and possible<br />
ancillary studies (FCM and IHC).<br />
352 <strong>Diagnostic</strong> Cytopathology, Vol 25, No 6
ASPIRATION IN SUPRACLAVICULAR LYMPHADENOPATHY<br />
On-site cytomorphologic evaluation was performed by<br />
exam<strong>in</strong>ation <strong>of</strong> air-dried, Diff-Quik sta<strong>in</strong>ed (Becton-Dick<strong>in</strong>son)<br />
smears to provide prelim<strong>in</strong>ary diagnostic <strong>in</strong>formation<br />
to the cl<strong>in</strong>icians and to determ<strong>in</strong>e the need based on cellular<br />
adequacy for additional passes to optimize diagnostic accuracy<br />
or for possible ancillary studies. The results <strong>of</strong> the f<strong>in</strong>al<br />
cytology diagnosis from each case were based on the <strong>in</strong>terpretation<br />
<strong>of</strong> all the cytology material obta<strong>in</strong>ed and processed<br />
as described above along with all available cl<strong>in</strong>ical <strong>in</strong>formation<br />
and data obta<strong>in</strong>ed from any ancillary studies performed<br />
(FCM and IHC). The results were categorized as<br />
benign/reactive, malignant ,or nondiagnostic and compared<br />
with histologic results when available.<br />
Results<br />
Of the 17,937 f<strong>in</strong>e-needle aspirations performed over a<br />
10-yr period (January 1, 1991, to December 31, 2000) 106<br />
patients (108 cases, 0.6%) underwent the diagnostic procedure<br />
for the evaluation <strong>of</strong> an enlarged supraclavicular lymph<br />
node with two patients be<strong>in</strong>g aspirated twice due to a<br />
nondiagnostic aspirates <strong>in</strong> the first attempt. The average age<br />
<strong>of</strong> the patients was 59 yr with a range <strong>of</strong> 26-90 yr; 49 were<br />
male and 56 female. The average size <strong>of</strong> the supraclavicular<br />
lymph nodes aspirated was 2.3 cm with a range <strong>of</strong> 1.5 to 5<br />
cm. A malignant tumor was diagnosed on FNA <strong>in</strong> 77 (73%)<br />
patients. Follow-up excisional biopsies were available <strong>in</strong> 19<br />
cases (18%) with no false-positive or -negative results.<br />
Forty-four patients (57%) with a malignant diagnosis on<br />
FNA had a prior tissue diagnosis <strong>of</strong> cancer, whereas 33<br />
patients (43%) were newly diagnosed with malignancy.<br />
Five patients (5%) presented with an abnormal lymph node<br />
that was classified as benign reactive hyperplasia by FNA.<br />
Two patients were diagnosed with tuberculosis based on the<br />
cytomorphologic f<strong>in</strong>d<strong>in</strong>gs <strong>of</strong> a granulomatous <strong>in</strong>flammation<br />
and the results <strong>of</strong> a K<strong>in</strong>youn sta<strong>in</strong> that confirmed the presence<br />
<strong>of</strong> acid-fast bacilli <strong>in</strong> the aspirate material obta<strong>in</strong>ed<br />
(Fig. C-1). Two (2%) <strong>of</strong> the 108 cases were nondiagnostic<br />
on FNA, both <strong>of</strong> which were subsequently diagnosed with<br />
malignancy: one on follow-up FNA alone (metastatic adenocarc<strong>in</strong>oma,<br />
lung primary), and the other on repeat FNA<br />
and subsequent surgical excision (metastatic teratoma, mediast<strong>in</strong>al<br />
primary).<br />
Of the 77 patients diagnosed with malignancy, 69(90%)<br />
were nonlymphoid (66 metastatic carc<strong>in</strong>omas, 1 melanoma,<br />
1 teratoma, and 1 liposarcoma) and 8 (10%) were lymphoid<br />
(5 non-Hodgk<strong>in</strong>’s B-cell lymphomas and 3 Hodgk<strong>in</strong>’s lymphomas).<br />
These lesions were distributed nearly equally 49%<br />
(37 cases) and 51% (39 cases) between the right and left<br />
sides, respectively. A similar distribution was observed<br />
among supradiaphragmatic tumors: 15 lung (7 right, 8 left)<br />
and 10 breast (5 right, 5 left) carc<strong>in</strong>omas. The 10 <strong>in</strong>fradiaphragmatic<br />
primary malignancies (3 gastro<strong>in</strong>test<strong>in</strong>al, 2<br />
bladder, and 1 ovarian, 1 cervical, 1 endometrial, 1 renal, 1<br />
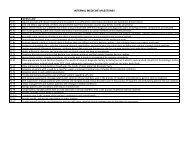
Table I.<br />
Type <strong>of</strong> study<br />
performed<br />
Summary <strong>of</strong> Ancillary Studies a<br />
Number <strong>of</strong> cases<br />
performed<br />
Number<br />
<strong>of</strong> cases<br />
positive<br />
Number <strong>of</strong> cases<br />
diagnostically<br />
helpful results<br />
IHC 12 10 11<br />
Cytokerat<strong>in</strong>s 8 6 7<br />
PSA, PSAP 3 1 3<br />
EMA, viment<strong>in</strong> 2 2 2<br />
Neuroendocr<strong>in</strong>e<br />
markers 4 2 3<br />
Germ cell markers 2 0 2<br />
CEA 1 0 0<br />
LCA 2 1 2<br />
ER, PR 2 0 0<br />
SHC 8 5 5<br />
Mucicarm<strong>in</strong>e 6 3 3<br />
K<strong>in</strong>youn 2 2 2<br />
FCM 5 5 5<br />
B-cell markers 3 3 3<br />
T-cell markers 2 2 2<br />
Monoclonality 3 3 3<br />
a IHC, immunohistochemistry; cytokerat<strong>in</strong>s, AE1/AE3, CAM 5.2, PAN<br />
CK; PSA, prostate specific antigen; PSAP, prostatic acid phosphatase;<br />
EMA, epithelial membrane antigen; neuroendocr<strong>in</strong>e markers, neuron specific<br />
enolase, synaptophys<strong>in</strong>, chromogran<strong>in</strong>; germ cell markers, placental<br />
alkal<strong>in</strong>e phosphatase, alpha-fetal prote<strong>in</strong>, human chorionic gonotrop<strong>in</strong>;<br />
CEA, carc<strong>in</strong>o embryonic antigen; LCA, leukocyte common antigen; ER,<br />
estrogen receptors; PR, progesterone receptors; SHC, special histochemical<br />
sta<strong>in</strong>s; FCM, flow cytometry.<br />
prostate) did, however, demonstrate a preference for the left<br />
SCLN with 8 <strong>of</strong> the 10 (80%) metastasiz<strong>in</strong>g to that side.<br />
Ancillary studies <strong>in</strong>clud<strong>in</strong>g special histochemical sta<strong>in</strong>s<br />
(8), IHC (12), and FCM (5) were performed on the aspirate<br />
material obta<strong>in</strong>ed <strong>in</strong> 22 (21%) cases, with special histochemical<br />
sta<strong>in</strong>s and IHC used jo<strong>in</strong>tly <strong>in</strong> three cases (Table<br />
I). IHC was useful <strong>in</strong> further characteriz<strong>in</strong>g tumors <strong>in</strong> 10 <strong>of</strong><br />
the 12 cases <strong>in</strong> which it was used, <strong>in</strong>clud<strong>in</strong>g confirm<strong>in</strong>g the<br />
presence <strong>of</strong> metastatic renal cell carc<strong>in</strong>oma <strong>in</strong> two patients<br />
with a known primary and <strong>in</strong> the diagnosis <strong>of</strong> metastatic<br />
prostate carc<strong>in</strong>oma <strong>in</strong> patient with no known primary (Fig.<br />
C-2). In addition to usefulness the acid fast sta<strong>in</strong> <strong>in</strong> the<br />
diagnosis <strong>of</strong> tuberculosis, special histochemical sta<strong>in</strong> mucicarm<strong>in</strong>e<br />
was also helpful <strong>in</strong> further typ<strong>in</strong>g poorly differentiated<br />
carc<strong>in</strong>omas as adenocarc<strong>in</strong>omas <strong>in</strong> three <strong>of</strong> six (50%)<br />
cases. In one <strong>of</strong> these cases, mucicarm<strong>in</strong>e sta<strong>in</strong> was helpful<br />
<strong>in</strong> confirm<strong>in</strong>g a diagnosis <strong>of</strong> a metastatic poorly differentiated<br />
rectal adenocarc<strong>in</strong>oma.<br />
Flow cytometry was performed on the aspirate material<br />
<strong>of</strong> five patients present<strong>in</strong>g with supraclavicular lymphadenopathy<br />
suspected <strong>of</strong> non-Hodgk<strong>in</strong>’s lymphoma. These <strong>in</strong>clude<br />
two patients with reactive hyperplasia <strong>in</strong> whom FCM<br />
revealed a mixed population <strong>of</strong> predom<strong>in</strong>ately small T-<br />
lymphocytes with no evidence <strong>of</strong> monoclonality. Three<br />
patients subsequently diagnosed with lymphoma also had<br />
FCM performed, which revealed a monotypic B-cell population,<br />
two <strong>of</strong> which were CD19 and CD20 positive, CD5<br />
negative, and lambda restricted. The rema<strong>in</strong><strong>in</strong>g case was<br />
CD19, CD20, CD23, CD10 positive and kappa restricted.<br />
<strong>Diagnostic</strong> Cytopathology, Vol 25, No 6 353
NASUTI ET AL.<br />
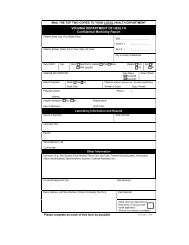
Table II.<br />
Comparison With Other Studies a<br />
Authors Cerv<strong>in</strong> (1995) Carson (1996) McHenry (1999) Present (2001) Total<br />
Number <strong>of</strong> patients 149 100 52 106 407<br />
Malignancies 96 (64%) 83 (83%) 42 (81%) 77 (73%) 298 (73%)<br />
Metastatic carc<strong>in</strong>omas 85 70 35 66 256<br />
Supradiaphragmatic<br />
primary T 51, L 26, R 25 T 38, L 21, R 17 T 20, L 10, R 10 T 25, L 12, R 13 T 134, L 69, R 65<br />
Infradiaphragmatic<br />
primary T 25, L 22, R 3 T 18, L 15, R 3 T 11, L 11, R 0 T 10, L 8, R 2 T 64, L 56, R 8<br />
Lymphoid malignancies 10 11 9 8 38<br />
Others malignancies 1 2 2 3 8<br />
Reactive/benign 32 15 4 25 76<br />
Infectious 8 — — 2 10<br />
Nondiagnostic 13 2 6 2 23<br />
a T, total; L, left supraclavicular lymph node; R, right supraclavicular node.<br />
Discussion<br />
Several studies, <strong>in</strong>clud<strong>in</strong>g our own, have found that a large<br />
percentage <strong>of</strong> patients present<strong>in</strong>g with persistent supraclavicular<br />
lymphadenopathy were subsequently diagnosed<br />
with malignancy based on tissue studies (58–83%). 7–12,15<br />
Of these, the vast majority (65–90%) are metastatic carc<strong>in</strong>omas<br />
from primary tumors orig<strong>in</strong>at<strong>in</strong>g from visceral sites<br />
<strong>in</strong>ferior to the supraclavicular nodal groups. Viacava and<br />
Pack <strong>in</strong> 1944 reviewed 4,365 patients with primary visceral<br />
cancers and found that a disproportionate number <strong>of</strong> abdom<strong>in</strong>al<br />
and pelvic tumors metastasized to the left SCLN. 7<br />
More recent FNA studies <strong>in</strong>volv<strong>in</strong>g a comb<strong>in</strong>ed 306 patients<br />
reported that 83–100% <strong>of</strong> known abdom<strong>in</strong>al and pelvic<br />
primary carc<strong>in</strong>omas metastasized to the left SCLN (Table<br />
II). 8–10 These same studies found no such preference for<br />
laterality <strong>in</strong> SCLN metastasis from thorax, head, and neck<br />
malignancies. The results <strong>of</strong> the current study are similar,<br />
with 80% <strong>of</strong> <strong>in</strong>fradiaphragmatic tumors metastasiz<strong>in</strong>g to the<br />
left SCLN and a virtually even distribution for supradiaphragmatic<br />
primary tumors (right 48%, left 52%).<br />
On-site evaluation <strong>of</strong> FNA Diff-Quik sta<strong>in</strong>ed specimen,<br />
we believe is extremely valuable <strong>in</strong> not only provid<strong>in</strong>g an<br />
accurate on the spot <strong>in</strong>terpretation <strong>in</strong> a large majority <strong>of</strong><br />
cases (4,829 <strong>of</strong> 5,872, 82% unpublished data) but also help<br />
triage specimens for ancillary studies. The utility <strong>of</strong> ancillary<br />
techniques such as IHC, flow cytometry, and special<br />
histochemical sta<strong>in</strong>s on SCLN FNA perta<strong>in</strong><strong>in</strong>g to the<br />
amount <strong>of</strong> additional relevant cl<strong>in</strong>ical <strong>in</strong>formation provided<br />
has not, to our knowledge, been addressed <strong>in</strong> previous<br />
reports. In the current study, these techniques were used <strong>in</strong><br />
21% (22 <strong>of</strong> 107) <strong>of</strong> the cases; these methods led to useful<br />
diagnostic <strong>in</strong>formation <strong>in</strong> 19 <strong>of</strong> 22 cases (86%) <strong>in</strong>clud<strong>in</strong>g<br />
detection <strong>of</strong> acid-fast bacilli <strong>in</strong> a background <strong>of</strong> granulomatous<br />
<strong>in</strong>flammation; muc<strong>in</strong> <strong>in</strong> poorly differentiated carc<strong>in</strong>oma;<br />
the presence <strong>of</strong> PSA, LCA, EMA, and viment<strong>in</strong> <strong>in</strong><br />
metastatic cancer cells, which either confirmed a metastasis<br />
from a known primary or helped to establish the tissue <strong>of</strong><br />
orig<strong>in</strong> <strong>in</strong> patients who <strong>in</strong>itially presented with metastatic<br />
disease. As was the case <strong>in</strong> the previously published reports<br />
(7–13%) lymphoid malignancy represented a m<strong>in</strong>ority <strong>of</strong><br />
the tumors <strong>in</strong> the current study (9%); however, the use <strong>of</strong><br />
FCM on the FNA material obta<strong>in</strong>ed was found to be extremely<br />
helpful <strong>in</strong> rul<strong>in</strong>g out lymphoma <strong>in</strong> two patients with<br />
reactive lymphadenopathy and <strong>in</strong> the detection and characterization<br />
<strong>of</strong> a monoclonal population <strong>of</strong> lymphoma cells <strong>in</strong><br />
three patients.<br />
The data obta<strong>in</strong>ed <strong>in</strong> the current study and <strong>in</strong> recently<br />
published reports confirm the diagnostic utility <strong>of</strong> FNA <strong>in</strong><br />
the evaluation <strong>of</strong> patients present<strong>in</strong>g with supraclavicular<br />
lymphadenopathy. Also, the comb<strong>in</strong>ed data from this and<br />
the prior studies (407 patients) help to re<strong>in</strong>force certa<strong>in</strong><br />
trends observed by previous <strong>in</strong>vestigators such as the<br />
marked predom<strong>in</strong>ance <strong>of</strong> metastatic carc<strong>in</strong>oma over lymphoid<br />
malignancies, reactive and <strong>in</strong>fectious processes along<br />
with the tendency <strong>of</strong> abdom<strong>in</strong>al and pelvic primary carc<strong>in</strong>omas<br />
to metastasize to the left SCLN. 8–10 In addition, the<br />
current observations support the use <strong>of</strong> IHC, FCM, and<br />
special histochemical sta<strong>in</strong>s on the aspirate material obta<strong>in</strong>ed<br />
from SCLN. These ancillary techniques have shown<br />
the potential <strong>in</strong> some cases to provide additional cl<strong>in</strong>ical<br />
<strong>in</strong>formation critical to patient management. This potential<br />
may be <strong>in</strong>creased <strong>in</strong> the near future due to the development<br />
<strong>of</strong> new immunohistochemical antibodies to tissue specific<br />
markers such as uroplak<strong>in</strong> (urothelium) detectable <strong>in</strong> metastatic<br />
transitional cell carc<strong>in</strong>oma. 16<br />
References<br />
1. Nasuti JF, Yu G, Boudusquie A, Gupta PK. <strong>Diagnostic</strong> value <strong>of</strong> lymph<br />
node f<strong>in</strong>e-needle aspiration cytology: an <strong>in</strong>stitutional experience <strong>of</strong> 387<br />
cases observed over a 5-year period. Cytopathology 2000;11:18–31.<br />
2. Cafferty LL, Katz RL, Ordenz NG. <strong>F<strong>in</strong>e</strong>-needle aspiration diagnosis <strong>of</strong><br />
<strong>in</strong>traabdom<strong>in</strong>al and retroperitoneal lymphomas by a morphologic and<br />
immunocytochemical approach. Cancer 1990;65:72–77.<br />
3. Rob<strong>in</strong>s DB, Katz RL, Swan F. Immunophenotyp<strong>in</strong>g <strong>of</strong> lymphoma by<br />
f<strong>in</strong>e-needle aspiration: a comparison study <strong>of</strong> cytosp<strong>in</strong> preparations<br />
and flow cytometry. Am J Cl<strong>in</strong> Pathol 1994;101:569–576.<br />
4. Sneiger N, Kekmezian R, El-Naffer A, Mann<strong>in</strong>g J. Cytomorphological,<br />
immunocytochemical and nucleic acid flow cytometric study <strong>of</strong> 50<br />
lymph nodes by f<strong>in</strong>e-needle aspiration. Cancer 1991;67:1003–1007.<br />
354 <strong>Diagnostic</strong> Cytopathology, Vol 25, No 6
ASPIRATION IN SUPRACLAVICULAR LYMPHADENOPATHY<br />
5. Moore KL. The thorax. In: Moore KL, editor. Cl<strong>in</strong>ically oriented<br />
anatomy, 2nd ed. Baltimore: William and Wilk<strong>in</strong>s; 1985. p 49–148.<br />
6. Morgenstern L. The Virchow-Troisier node: a historical note. Am J<br />
Surg 1979;138:703.<br />
7. Viacava EP, Pack GT. Significance <strong>of</strong> supraclavicular signal node <strong>in</strong><br />
patients with abdom<strong>in</strong>al and thoracic cancer. Arch Surg 1944;48:109–<br />
119.<br />
8. Cerv<strong>in</strong> JR, Silverman JF, Loggie BW, Geis<strong>in</strong>ger KR. Virchow’s node<br />
revisited: analysis with cl<strong>in</strong>icopathologic correlation <strong>of</strong> 152 f<strong>in</strong>e-needle<br />
aspiration biopsies <strong>of</strong> supraclavicular nodes. Arch Pathol Lab Med<br />
1995;119:727–730.<br />
9. Carson HJ, Candel AG, Gattuso P, Castelli MJ. <strong>F<strong>in</strong>e</strong>-needle aspiration<br />
<strong>of</strong> supraclavicular lymph nodes. Diagn Cytopathol 1996;14:<br />
216–220.<br />
10. McHenry CR, Cooney MW, Slusarczyk SJ, Khiyami A. <strong>Supraclavicular</strong><br />
lymphadenopathy: the spectrum <strong>of</strong> pathology and evaluation by<br />
f<strong>in</strong>e-needle aspiration biopsy. Am Surg 1999;65:742–746.<br />
11. McMenam<strong>in</strong> PG, Anderson JD, Baker JJ. Prostatic carc<strong>in</strong>oma present<strong>in</strong>g<br />
with neck metastasis. J Otolaryngol 1989;18:119–124.<br />
12. Yoa ZH, Wu AR. <strong>Supraclavicular</strong> lymph node metastasis from carc<strong>in</strong>oma<br />
<strong>of</strong> the uter<strong>in</strong>e cervix after radiotherapy: analysis <strong>of</strong> 219 patients.<br />
Chung-Hua Chung Liu Tsa Chih 1988;10:230–232.<br />
13. Ereno C, Lopez JI, Elizalde JM, Ibanez T, Fernandez-Larriano A,<br />
Toledo JD. A case <strong>of</strong> Whipples’s disease present<strong>in</strong>g as supraclavicular<br />
lymphadenopathy. A case report. APMIS 1993;101:865–868.<br />
14. Pithie AD, Chicksen B. <strong>F<strong>in</strong>e</strong>-needle extrathoracic lymph node aspiration<br />
<strong>in</strong> HIV associated sputum negative tuberculosis. Lancet 1992;340:<br />
1504–1505.<br />
15. Khorsand J, Katz RL, Savaraj N. Malignant carc<strong>in</strong>oid <strong>of</strong> pancreas: a<br />
cytologic, ultrastructural and immunocytochemical study <strong>of</strong> a case<br />
diagnosed by f<strong>in</strong>e-needle aspiration <strong>of</strong> a supraclavicular node metastasis.<br />
Diagn Cytopathol 1987;3:222–227.<br />
16. Xu X, Sun TT, Gupta PK, Nasuti JF. Uroplak<strong>in</strong>s as a marker for typ<strong>in</strong>g<br />
metastatic transitional cell carc<strong>in</strong>oma on f<strong>in</strong>e-needle aspiration specimens.<br />
Cancer Cytopathol 2001;83:216–221.<br />
<strong>Diagnostic</strong> Cytopathology, Vol 25, No 6 355