SOP Heparin Pathologies Total.pdf - Oscp.ca
SOP Heparin Pathologies Total.pdf - Oscp.ca
SOP Heparin Pathologies Total.pdf - Oscp.ca
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
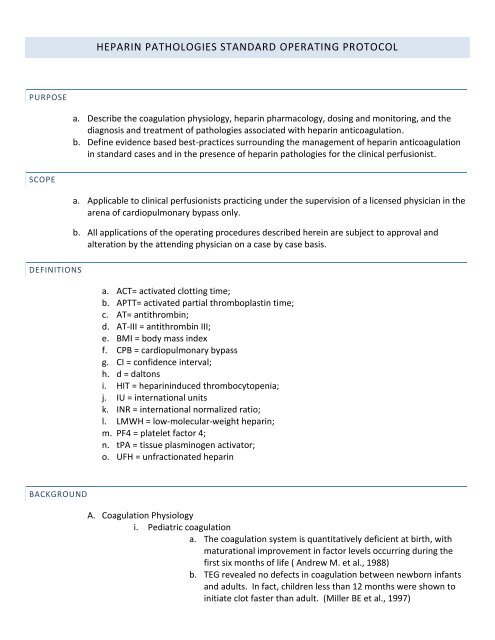
HEPARIN PATHOLOGIES STANDARD OPERATING PROTOCOL<br />
PURPOSE<br />
a. Describe the coagulation physiology, heparin pharmacology, dosing and monitoring, and the<br />
diagnosis and treatment of pathologies associated with heparin anticoagulation.<br />
b. Define evidence based best-practices surrounding the management of heparin anticoagulation<br />
in standard <strong>ca</strong>ses and in the presence of heparin pathologies for the clini<strong>ca</strong>l perfusionist.<br />
SCOPE<br />
a. Appli<strong>ca</strong>ble to clini<strong>ca</strong>l perfusionists practicing under the supervision of a licensed physician in the<br />
arena of <strong>ca</strong>rdiopulmonary bypass only.<br />
b. All appli<strong>ca</strong>tions of the operating procedures described herein are subject to approval and<br />
alteration by the attending physician on a <strong>ca</strong>se by <strong>ca</strong>se basis.<br />
DEFINITIONS<br />
a. ACT= activated clotting time;<br />
b. APTT= activated partial thromboplastin time;<br />
c. AT= antithrombin;<br />
d. AT-III = antithrombin III;<br />
e. BMI = body mass index<br />
f. CPB = <strong>ca</strong>rdiopulmonary bypass<br />
g. CI = confidence interval;<br />
h. d = daltons<br />
i. HIT = heparininduced thrombocytopenia;<br />
j. IU = international units<br />
k. INR = international normalized ratio;<br />
l. LMWH = low-molecular-weight heparin;<br />
m. PF4 = platelet factor 4;<br />
n. tPA = tissue plasminogen activator;<br />
o. UFH = unfractionated heparin<br />
BACKGROUND<br />
A. Coagulation Physiology<br />
i. Pediatric coagulation<br />
a. The coagulation system is quantitatively deficient at birth, with<br />
maturational improvement in factor levels occurring during the<br />
first six months of life ( Andrew M. et al., 1988)<br />
b. TEG revealed no defects in coagulation between newborn infants<br />
and adults. In fact, children less than 12 months were shown to<br />
initiate clot faster than adult. (Miller BE et al., 1997)
ii. Adult coagulation<br />
1. Understanding current concepts of coagulation is important in<br />
determining the preoperative bleeding risk of patients and in managing<br />
hemostatic therapy perioperatively. (Tanaka KA., 2009)<br />
2. Below is a diagram (A) of the intrinsic and extrinsic pathways. (B)<br />
represents the regulation of thrombin generation.<br />
B. <strong>Heparin</strong> pharmacology is compli<strong>ca</strong>ted by variability in molecular composition, activity, and<br />
clearance as well as multiple binding sites and storage <strong>ca</strong>pabilities.<br />
i. Heterogeneous molecular size ranging from 3000 to 30000 d (Johnson 1976)<br />
ii. Negatively charged repeating sulfated disaccharide units referred to as a<br />
glycosaminogly<strong>ca</strong>n (Ng 2009)<br />
iii. 1/3 rd binds with antithrombin, thus only 1/3 rd of heparin dose is responsible<br />
for the majority of anticoagulant activity (Lam 1976)<br />
iv. Binds to multiple plasma proteins, platelets, macrophages, and endothelial<br />
cells (Hirsh 2001)<br />
v. <strong>Heparin</strong>-AT complex inactivates factors IIa, IXa, Xa, XIa, XIIa with greatest<br />
affinity for factor Xa (Rosenberg 1994)<br />
vi. Inactivating thrombin prevents fibrin formation and inhibits factors V and<br />
VIII, increases secretion of tissue factor pathway inhibitor, and reduces VIIa<br />
complex effi<strong>ca</strong>cy (Ofosu 1987)<br />
vii. Amplifies vessel wall permeability, reduces vascular smooth muscle cell<br />
production, and has an osteopenic effect (Clowes 1977, Shaughnessy 1995)<br />
viii. Cleared first by saturable phase, secondarily by renal clearance, therefore<br />
half-life is dose dependent ranging from 30 minutes for 25U/kg to 150<br />
minutes for 150U/kg (de Swart 1982)
. Dosing Protocols<br />
i. Empiri<strong>ca</strong>l Dosing vs. <strong>Heparin</strong> Concentration Dosing- conflicting reports<br />
1. No signifi<strong>ca</strong>nt difference in ACT, protamine requirement, or post<br />
operative bleeding found, however greater heparin was administered<br />
in <strong>Heparin</strong> Concentration Regimen in pediatrics (Olshove 2000)<br />
2. Individualized heparin and protamine management in pediatrics has<br />
been shown to reduce platelet activation and coagulopathies,<br />
although the immature systems of neonates needs further study<br />
(Gruenwald 2010)<br />
3. HDR protocol resulted in less heparin administered and a signifi<strong>ca</strong>nt<br />
reduction in post-operative blood loss in adults (Runge 2009)<br />
ii. Algorithm Dosing<br />
1. An evidence-based decision tree <strong>ca</strong>n be used to arrive at an adequate<br />
heparin dosage and guide health<strong>ca</strong>re providers to a consistent and<br />
cost-effective use of resources. (McKinney 2007)<br />
iii. Obese patient dosing<br />
1. LBM <strong>ca</strong>n be used to reduce the amount of heparin and protamine<br />
administered up to 25% in patients with a BMI >30 (Baker2007)<br />
c. Anticoagulation Monitoring: no definitive test accurately represents the entire<br />
picture of anticoagulation and is reproducible laboratory to laboratory, device to<br />
device, or operator to operator.<br />
i. ACTs have little evidence of their accuracy and multiple studies have shown<br />
signifi<strong>ca</strong>nt lack of agreement between devices, yet the standard of 480<br />
seconds is widely used. It has been quoted that “target times employed<br />
stem more from histori<strong>ca</strong>l clinician comfort than outcome studies” (Ng<br />
2009).<br />
ii. aPTT is useful in the detection of coagulation disorders when used in<br />
combination with PT with the ability to differentiate between the intrinsic,<br />
extrinsic, common and multiple pathway deficiencies (Cowell 2007). PTT is a<br />
measure of the intrinsic pathway with the prolongation of PTT as a result of<br />
the inhibition of thrombin activity. A PTT of 1.5-2.5 normal is histori<strong>ca</strong>lly<br />
considered therapeutic for thromboembolic prophylaxis, however wide interlaboratory<br />
variations in testing make comparison and correlation of values<br />
difficult (Ng 2009).<br />
iii. PT test is instrumental in detecting Factor VII deficiency and will not be<br />
detected by the aPTT or ACT tests alone (Cowell 2007).<br />
iv. <strong>Heparin</strong> concentration of whole blood as measured by the HMS has had<br />
conflicting reports of effi<strong>ca</strong>cy. Multiple reports state a higher heparin dose is<br />
used, yet a lower protamine dose is needed, possibly due to less coagulation<br />
system activation. Some have confirmed this and also demonstrated a<br />
reduction in inflammation marker activation (Dunning 2008). However, one<br />
study found the Hepcon does not correlate to plasma heparin concentration<br />
using a chromogenic substrate for factor Xa and is not recommended for<br />
monitoring heparin concentrations during bypass (Hardy 1996). The HMS<br />
was not been shown in a large study to be signifi<strong>ca</strong>ntly more effi<strong>ca</strong>cious than<br />
an ACT-based heparinization protocol with regards to length of stay and<br />
blood usage (Slight 2008). The STS report gives the HMS system a grade B<br />
level of evidence, thus its use is recommended where available.
v. Anti-factor Xa heparin assay determined by the amount of anti-Xa factor by a<br />
chromogenic substrate which releases a colored compound detected by a<br />
spectrophotometer is the most reliable form. Many different tests are<br />
available, and variability is large.<br />
vi. TEG is useful in the guidance of blood product administration. TEG may<br />
decrease blood product administration when used with a specific algorithm<br />
in the post-operative period (Dunning 2008). TEG was found to be superior<br />
to ACT, PT, and PTT in predicting bleeding with the need for blood products<br />
versus bleeding from surgi<strong>ca</strong>l sources (Ti 2002).<br />
d. <strong>Heparin</strong> Associated <strong>Pathologies</strong> and Problems<br />
i. <strong>Heparin</strong> Induced Thrombocytopenia Type I & II<br />
1. HIT type I is a benign, non-immune mediated, transient drop in<br />
platelet count found in 10-20% of patients treated with IV heparin<br />
(Newkirk 2010). Although monitoring is needed for these patients,<br />
without treatment platelet counts will return to normal within a few<br />
days and should not drop below 100000/mm3.<br />
2. HIT type II is suspected with a 30-50% drop in platelet count 5 to 10<br />
days after IV heparin therapy is started and found in less than 5% of<br />
patients on IV heparin (Newkirk 2010).<br />
a. HIT II is potentially fatal: platelet count decreases to less than<br />
100000/mm3, and thrombosis begins. Disseminated<br />
intravascular clotting is a serious risk.<br />
b. PT and PTT are prolonged. Platelet aggregation and serotonin<br />
assays are useful in the differential diagnosis.<br />
c. Alternative anticoagulation therapy should be started<br />
immediately.<br />
ii. <strong>Heparin</strong> Allergy<br />
1. Few <strong>ca</strong>ses of heparin anaphylaxis have been reported. Bottio 2003<br />
and Berkun 2004 each published <strong>ca</strong>se studies in which heparin<br />
anaphylaxis were confirmed. In one <strong>ca</strong>se danaparoid was used as an<br />
anticoagulant alternative for hemodialysis, and in the other<br />
<strong>ca</strong>rdiogenic shock ensued with heparin bolus for CPB. The CPB<br />
patient required large doses of epinephrine and methylprednisone,<br />
but was weaned from bypass and recovered uneventfully.<br />
iii. <strong>Heparin</strong> Resistance<br />
1. <strong>Heparin</strong> resistance <strong>ca</strong>n be defined as the need for higher than normal<br />
heparin concentrations (>600USP units/kg) to achieve a safe ACT for<br />
the initiation of CPB. (Hensley, Martin and Gravlee, 2005). In fact,<br />
failure to attain an ACT>300 seconds after >600 USP units/kg of<br />
heparin is a presumptive process. (Gravlee, 1993)<br />
a. ATIII deficiency (inherited or acquired) <strong>ca</strong>n be linked to<br />
heparin resistance in most patients.<br />
b. True heparin resistance is rare. Acquired ATIII deficiency is<br />
common among the criti<strong>ca</strong>lly ill, but should not decrease ATIII<br />
levels to that of hereditary/inherited ATIII deficiency (Ng<br />
2009).<br />
i. AT III deficiency is treated with fresh frozen plasma<br />
(FFP) or human AT III concentrate.
1. Normally, 2 to 3 units of FFP is sufficient to<br />
increase the ACT to a safe level for CPB.<br />
(Gravlee, 1993)<br />
2. Human AT III is pooled from human plasma, but<br />
it is has been heat treated so that it should be<br />
free of disease transmission risk. ATIII is only<br />
approved by the FDA for hereditary ATIII<br />
deficiency.<br />
a. Recommendations for the<br />
administration of AT III, is 100 x (weight<br />
in kgs) to increase AT III levels from 0%<br />
to 100%. (Gravlee, 1993)<br />
b. The half life of AT III is 22 hours.<br />
c. Other <strong>ca</strong>uses of heparin resistance include nitroglycerin<br />
administration, thrombocytosis, hemodilution, and immature<br />
coagulation systems.<br />
iv. <strong>Heparin</strong> Rebound<br />
1. <strong>Heparin</strong> is bound nonspecifi<strong>ca</strong>lly to plasma proteins which lead to<br />
incomplete neutralization of heparin by protamine. <strong>Heparin</strong> rebound<br />
occurs when heparin which is not neutralized exhibits an<br />
anticoagulant effect 1-6 hours after neutralization (Teoh 2004).<br />
2. A slow continuous protamine infusion post-operatively <strong>ca</strong>n<br />
signifi<strong>ca</strong>ntly reduce heparin rebound (Teoh 2004).<br />
SAFETY<br />
e. Medi<strong>ca</strong>tion administration safety.<br />
i. The six “rights” will be verified before any and all drug administration. These<br />
include:<br />
1. Right patient: patient will be verified by two identifiers upon entry to<br />
the operating suite as well as all known allergies.<br />
2. Right drug: all drugs will be checked by two licensed providers<br />
(perfusionist and RN, MD, or another perfusionist) for proper drug<br />
name, concentration, and expiration date.<br />
3. Right dosage: dose will be verified by perfusionist and anesthesia<br />
resident or attending.<br />
4. Right route: the lo<strong>ca</strong>tion for drug administration (IV, central/cpb, etc)<br />
will be verified with anesthesia before administering via the CPB<br />
mannifold.<br />
5. Right time: perfusionist will verify with anesthesia that the drug is<br />
indeed to be administered at that time.<br />
6. Right documentation: the perfusionist will document the time and<br />
dose of the drug administered. If the administration is a variance<br />
from the standard protocol, “per (ordering physician’s name)” is to be<br />
added to the pump record.<br />
ii. All vials will be entered in a sterile fashion using a five second alcohol wipe,<br />
and new sterile needle and syringe.<br />
f. <strong>Heparin</strong> storage and labeling: multiple incidences of <strong>Heparin</strong> overdose and related<br />
deaths have been reported.
i. The ONLY concentration of heparin to be stored in the operating suite is<br />
1000 units per ml. These may be in 30 or 10 ml vials and will have orange<br />
labeling.<br />
ii. The ONLY concentration of heparin to be used in the pediatric and neonatal<br />
intensive <strong>ca</strong>re areas is 100 units per ml.<br />
1. <strong>Heparin</strong> is NOT to be stored in pediatric and neonatal treatment areas<br />
with the exception of factory pre-drawn heparin flush/heplock<br />
syringes.<br />
2. <strong>Heparin</strong> for systemic anticoagulation in pediatric and neonatal<br />
patients must be obtained from the pharmacy in pre-mixed diluted<br />
bags, labeled for individual patient administration only.<br />
RESPONSIBILITIES<br />
g. The perfusionist is responsible for:<br />
i. An accurate and up to date patient history including the discovery of all<br />
pertinent laboratory data.<br />
ii. Making the surgi<strong>ca</strong>l and anesthesia team aware of the discovery of any<br />
information which may influence the anticoagulation process.<br />
iii. Obtaining and recording patient demographics, <strong>ca</strong>lculating the BSA, BMI, and<br />
heparin bolus dose.<br />
iv. Obtaining and recording the initial ACT.<br />
v. Communi<strong>ca</strong>ting to the attending anesthesiologist the recommended heparin<br />
bolus.<br />
vi. Obtaining, recording, and communi<strong>ca</strong>ting any heparin sensitivity or HDR tests<br />
run.<br />
vii. Obtaining, recording, and communi<strong>ca</strong>ting all subsequent ACTs and heparin<br />
doses on bypass.<br />
viii. Obtaining and recording the post-protamine ACT.<br />
PROCEDURES<br />
h. Evidence-based heparin dosing protocol<br />
i. Thoroughly review the <strong>ca</strong>rdiac surgi<strong>ca</strong>l patient record.<br />
1. Note the age, sex, height, weight, BSA, and BMI of the patient and<br />
any allergies.<br />
a. If the patient is obese (BMI>30, <strong>ca</strong>lculate ideal or lean body<br />
mass for use in <strong>ca</strong>lculations).<br />
b. Calculate the patient blood volume and initial standard<br />
heparin loading dose (300IU/kg).<br />
2. Has the patient been administered pre-operative heparin Have a<br />
platelet count > 300k/mm3, or have an albumin concentration less<br />
than 3.5 grams per dL Will the patient be profoundly hemo-diluted<br />
or undergo deep hypothermia<br />
a. If yes to any of these questions, an HDR may be warranted,<br />
and a heparin concentration management protocol may be<br />
more appropriately followed or a simple heparin sensitivity<br />
test may be performed.
. If HDR < 80 sec/U/cc, ATIII activity should be measured where<br />
availbale, and recombinant ATIII made available. If ATIII<br />
activity is less than 60%, administration is warranted.<br />
c. Alternatively, where HDR testing is not available, a simple in<br />
vitro heparin sensitivity test is recommended.<br />
ii. Measure the initial activated clotting time.<br />
1. If the ACT is less than 95 seconds or greater than 145 seconds, a<br />
repeat ACT should be drawn. If the ACT is still out of range the<br />
history of the patient and laboratory tests should be revisited to<br />
determine a source/reason for the deviation.<br />
2. If the history is all clear and the initial ACT is consistent with the<br />
clini<strong>ca</strong>l history of the patient, the heparin loading dose may be<br />
administered at the appropriate time.<br />
3. A simple heparin sensitivity test is recommended at this time.<br />
a. In a syringe add 6IU of heparin/ml of blood, mix well, and<br />
clearly label.<br />
b. Run the heparin sensitivity ACT.<br />
i. If ACT
heparin resistance<br />
(thromocytosis).<br />
4. Re-measure the ACT after any action and repeat steps as necessary.<br />
i. Evidence-based anticoagulation management protocol<br />
i. Maintain ACT >600 seconds for all patients with heparin anticoagulation on<br />
<strong>ca</strong>rdiopulmonary bypass.<br />
1. Those patients being anticoagulated with heparin alternatives will<br />
need to be treated according to the alternate drug-specific protocol.<br />
2. Obtain an ACT at an interval no greater than every 30 minutes while<br />
on CPB for adult patients and no greater than every 20 minutes while<br />
on CPB for pediatric and neonatal patients. Obtain ACTs more<br />
frequently while warming, especially on DHCA <strong>ca</strong>ses.<br />
3. Treat ACTs less than 600 seconds with 1/5 or 20% of the heparin<br />
loading dose. (ie for a loading dose of 30k IU to the patient and 10k<br />
IU in the pump, a subsequent heparin dose would be 8k IU).<br />
4. If repeat heparin administration is required, an ACT is to be drawn<br />
within 10 minutes of administration, and anesthesia is to be<br />
informed.<br />
ii. Anesthesia will reverse heparin with Protamine after <strong>ca</strong>rdiopulmonary<br />
bypass. (See Anesthesia Protamine protocol for more information- this is<br />
provided for information purposes.)<br />
1. Protamine dose should be diluted in 100ml of NSS.<br />
2. Dose may be determined by the HMS, or <strong>ca</strong>lculated @ 1mg per 100IU<br />
of heparin given.<br />
3. A test dose of 1microgram/ml of Protamine is recommended after<br />
venous de<strong>ca</strong>nnulation. Cardiotomy suction should be terminated at<br />
this point.<br />
4. If no reaction to Protamine test dose, a slow infusion of no more than<br />
50mg/10min should be started after arterial de<strong>ca</strong>nnulation.<br />
5. If a Protamine reaction is suspected, it may be necessary to resume<br />
<strong>ca</strong>rdiopulmonary bypass. See protamine reaction protocol.<br />
6. A slow Protamine drip is recommended upon transfer to the ICU for<br />
the prevention of heparin rebound.<br />
j. Guidelines for heparin pathologies in the <strong>ca</strong>rdiac operating room.<br />
i. <strong>Heparin</strong> resistance is addressed in the heparin dosing protocol.<br />
ii. History of heparin anaphylaxis and current HIT type II (surgeon preference)<br />
may warrant an alternative anticoagulation strategy. The preference in such<br />
<strong>ca</strong>ses will be anticoagulation with bivalirudin. See the bivalirudin protocol<br />
for further information. The CDI cell contains heparin and should not be<br />
used on these patients. Current circuitry is NOT heparin coated.<br />
1. Unknown heparin anaphylaxis (or heparin contamination) may<br />
require immediate commencement of <strong>ca</strong>rdiopulmonary bypass.<br />
2. Plasmapheresis should be considered for these patients.<br />
iii. A current history of a positive HIT type I, as well as HIT type II patients<br />
(surgeon preference) will be anticoagulated with heparin and on-bypass<br />
plasmapheresis, as well as post-operative plasmapheresis will be utilized.<br />
Careful monitoring of condition with frequent platelet counts and<br />
coagulation profiles will be performed post-bypass.
iv. A remote history of HIT type I will proceed on bypass with the usual heparin<br />
anticoagulation protocol. Platelet counts should be monitored <strong>ca</strong>refully in<br />
the post operative period.<br />
v. A small, slow continuous Protamine infusion should be used<br />
(anesthesiologist’s preference) with any suspicion of heparin rebound (Teoh<br />
2004). TEG and anti-factor Xa assays <strong>ca</strong>n help determine <strong>ca</strong>use of nonsurgi<strong>ca</strong>l<br />
bleeding and best course of action.<br />
ASSOCIATED MATERIALS<br />
k. <strong>Heparin</strong><br />
l. Sterile syringes<br />
m. Sterile needles<br />
n. ACT machine<br />
o. ACT tubes or <strong>ca</strong>rtridges<br />
p. Other laboratory testing equipment as needed by laboratory technicians<br />
ADDITIONAL INFORMATION<br />
q. See Bivalirudin Protocol.<br />
r. See Anesthesia Protamine Protocol.<br />
REFERENCES<br />
s. Bottio, T., Pittarello, G., Bonato, R., & Fagiolo, U. (2003). Life-threatening<br />
anaphylactic shock <strong>ca</strong>used by porcine heparin intravenous infusion during mitral<br />
valve repair. J Thoac Cardiovasc Surg, 126, 1194-1195.<br />
t. Berkun, Y., Haviv, Y., Schwartz, L., & Shalit, M. (2004). <strong>Heparin</strong>-induced recurrent<br />
anaphylaxis. Clini<strong>ca</strong>l and Experimental Allergy, 34, 1916-1918.<br />
u. Brown, M., Gallagher, J., & Armitage, J. (2000). The use of antithrombin III<br />
concentrate for treatment of heparin resistance during <strong>ca</strong>rdiopulmonary bypass.<br />
JECT, 32(2), 75-78.<br />
v. Clowes AW, Karnovsky MJ. Suppression by heparin of smooth muscle cell<br />
proliferation in injured arteries. Nature 1977; 265: 625-626.<br />
w. Conley, J., & Plunkett, P. (1998). Antithrombin III in Cardiac Surgery: An Outcome<br />
Study. JECT, 30(4), 178-183.
x. DeBois, W., Liu, J., Elmer, B., & Ebrahimi, H. (2007). <strong>Heparin</strong> sensitivity test for<br />
patients requiring <strong>ca</strong>rdiopulmonary bypass. JECT, 38, 307-309.<br />
y. Despotis GJ, Joist JH, Hogue CW Jr, Alsoufiev A, Joiner-Maier D, Santoro SA,<br />
Spitznagel E, Weitz JI, Goodnough LT. (1996) More effective suppression of<br />
hemostatic system activation in patients undergoing <strong>ca</strong>rdiac surgery by heparin<br />
dosing based on heparin blood concentrations rather than ACT. Thrombosis and<br />
Haemostasis. Dec;76(6):902-8.<br />
z. Gravlee GP, Davis RF, (&) Utley JR. (1993) <strong>Heparin</strong> Resistance. Cardiopulmonary<br />
Bypass: Principles and Practice. Williams and Wilkins Publishing. Section III, Chapter<br />
14: 362-64.<br />
aa. Grayoso, J. (1999). 5-year incidence of thrombocytosis and the effect on heparin<br />
dose response and heparin requirements. JECT, 31(4), 184-190.<br />
bb. Gris et al. Monitoring the effects and managing the side effects of anticoagulation<br />
during pregnancy. Obstetrics and Gynecology Clinics. Volume 33(3):397-411.<br />
cc. Hirsh, J., Anand, S. S., Halperin, J. L., & Valentin, F. (2001). Mechanism of Action and<br />
Pharmacology of Unfractionated <strong>Heparin</strong>. Journal of the Ameri<strong>ca</strong>n Heart Association,<br />
21, 1094-1096.<br />
dd. Hirsh, J., Warkentin, T.E., Shaughnessy, S.G., Sonia S , Ohman, M., Dalen J.E.,<br />
Halperin, J., Raschke, R., Granger, C.,. (2001) <strong>Heparin</strong> and Low Molecular Weight<br />
<strong>Heparin</strong> Dosing, Monitoring, Effi<strong>ca</strong>cy, and Safety Mechanisms of Action,<br />
Pharmacokinetics Chest 119;64S-94S<br />
ee. Johnson EA, Mulloy B. The molecular weight range of commercial heparin<br />
preparations. Carboydr Res 1976; 51: 119-127.<br />
ff. Krishnaswamy A, Lincoff AM, Cannon CP. (2010) The Use and Limitations of<br />
Unfractionated <strong>Heparin</strong>. Criti<strong>ca</strong>l Pathways in Cardiology. Mar;9(1):35-40.
gg. Lam LII, Silbert JE, Rosenberg RD. The separation of active and inactive forms of<br />
heparin. Biochem Biophys Res Commun 1976; 69:570-577.<br />
hh. Marco Ranucci, Giuseppe Isgrò, Anna Cazzaniga, Giorgio Soro. (1999) Predictors for<br />
heparin resistance in patients undergoing coronary artery bypass grafting. Perfusion;<br />
14: 437–442.<br />
ii. Mirow, N., Zittermann, A., Koertke, H., Maleszka, A., Knobl, H., Coskun, T., Kleesiek,<br />
K., & Koerfer, R.. (2008). <strong>Heparin</strong>-coated extracorporeal circulation in combination<br />
with low dose systemic heparinization reduces early postoperative blood loss in<br />
<strong>ca</strong>rdiac surgery. Journal of Cardiovascular Surgery, 49(2), 277-84. Retrieved June 28,<br />
2010, from ProQuest Nursing & Allied Health Source. (Document ID: 1499767111).<br />
jj. Newkirk, C.E., 2010 <strong>Heparin</strong>-induced Thrombocytopenia (HIT): A Case Study. Clini<strong>ca</strong>l<br />
Laboratory Science, VOL 23(1): 5-11<br />
kk. Ng, V. (2009) Anticoagulation Monitoring. Clin Lab Med 29: 2833-304.<br />
ll. Ofson FA, Sie P, Modi GJ, et al. The inhibition of thrombin-dependent feedback<br />
reactions is criti<strong>ca</strong>l to the expression of anticoagulant effects of heparin. Biochem J<br />
1987; 243:579-588.<br />
mm.<br />
Oliver WC. (2005) Hemostasis, Coagulation, and Transfusion in the Pediatric<br />
Cardiac Patient. Pediatric Cardiac Anesthesia. Chapter 16:304-314.<br />
nn. Priziola, et al., (2010) Drug-induced thrombocytopenia in criti<strong>ca</strong>lly ill patients. Criti<strong>ca</strong>l<br />
Care Medicine, 38(6); Suppl. S145-S154<br />
oo. Rosenberg RD, Bauer KA. The heparin-antithrombin system: a natural anticoagulant<br />
mechanism. In: Cohman RW, Hirsh J, Marder VJ, et al, eds. Hemostasis and<br />
thrombosis: basic principles and clini<strong>ca</strong>l practice. 3 rd ed. Philadelphia, PA: JB<br />
Lippincott, 1994; 837-860.
pp. Shaughnessy SG, Young E, Deschamps P, et al. The effects of low molecular weight<br />
and stardard heparin on <strong>ca</strong>lcium loss from the fetal rat <strong>ca</strong>lvaria. Blood 1995; 86:<br />
1368-1373.<br />
qq. Tanaka KA, Key NS, Levy JH. (2009) Blood coagulation: hemostasis and thrombin<br />
regulation. Anesth Analg. May;108(5):1433-46.<br />
rr. Teoh, K.H., Young, E., Blackall, M.H., Roberts, R.S., Hirsh, J., (2004) Can extra<br />
Protamine eliminate heparin rebound following <strong>ca</strong>rdiopulmonary bypass surgery<br />
Journal of Thoracic and Cardiovascular Surgery 128; 211-209.<br />
ss. Uprichard J, Manning RA, Laffan MA. (2010) Monitoring heparin anticoagulation in<br />
the acute phase response. British Journal of Haemotology. May;149(4):613-9.<br />
tt. Van Cott EM. (2009) Point of <strong>ca</strong>re testing in coagulation. Clini<strong>ca</strong>l Laboratory<br />
Medicine. Sep;29(3):543-53.<br />
uu. Warkentin T.E., (2006) Think of HIT, Hematology. 408 - 414.<br />
vv. Welsby IJ., (2010) Plasmapheresis and <strong>Heparin</strong> Reexposure as a Management<br />
Strategy for Cardiac Surgi<strong>ca</strong>l Patients with <strong>Heparin</strong>-Induced Thrombocytopenia.<br />
Anesthesia and Analgesia; 110(1):30-35.