tb meningitis adult1.pdf - Nursing Crib
tb meningitis adult1.pdf - Nursing Crib
tb meningitis adult1.pdf - Nursing Crib
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
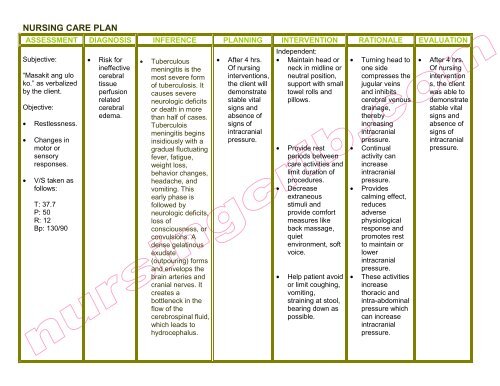
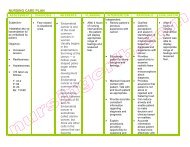
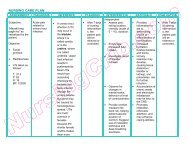
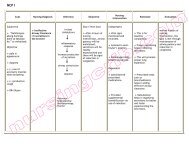
NURSING CARE PLAN<br />
ASSESSMENT DIAGNOSIS INFERENCE PLANNING INTERVENTION RATIONALE EVALUATION<br />
Subjective:<br />
“Masakit ang ulo<br />
ko.” as verbalized<br />
by the client.<br />
Objective:<br />
• Restlessness.<br />
• Changes in<br />
motor or<br />
sensory<br />
responses.<br />
• V/S taken as<br />
follows:<br />
T: 37.7<br />
P: 50<br />
R: 12<br />
Bp: 130/90<br />
• Risk for<br />
ineffective<br />
cerebral<br />
tissue<br />
perfusion<br />
related<br />
cerebral<br />
edema.<br />
• Tuberculous<br />
<strong>meningitis</strong> is the<br />
most severe form<br />
of tuberculosis. It<br />
causes severe<br />
neurologic deficits<br />
or death in more<br />
than half of cases.<br />
Tuberculois<br />
<strong>meningitis</strong> begins<br />
insidiously with a<br />
gradual fluctuating<br />
fever, fatigue,<br />
weight loss,<br />
behavior changes,<br />
headache, and<br />
vomiting. This<br />
early phase is<br />
followed by<br />
neurologic deficits,<br />
loss of<br />
consciousness, or<br />
convulsions. A<br />
dense gelatinous<br />
exudate<br />
(outpouring) forms<br />
and envelops the<br />
brain arteries and<br />
cranial nerves. It<br />
creates a<br />
bottleneck in the<br />
flow of the<br />
cerebrospinal fluid,<br />
which leads to<br />
hydrocephalus.<br />
• After 4 hrs.<br />
Of nursing<br />
interventions,<br />
the client will<br />
demonstrate<br />
stable vital<br />
signs and<br />
absence of<br />
signs of<br />
intracranial<br />
pressure.<br />
Independent:<br />
• Maintain head or<br />
neck in midline or<br />
neutral position,<br />
support with small<br />
towel rolls and<br />
pillows.<br />
• Provide rest<br />
periods between<br />
care activities and<br />
limit duration of<br />
procedures.<br />
• Decrease<br />
extraneous<br />
stimuli and<br />
provide comfort<br />
measures like<br />
back massage,<br />
quiet<br />
environment, soft<br />
voice.<br />
• Help patient avoid<br />
or limit coughing,<br />
vomiting,<br />
straining at stool,<br />
bearing down as<br />
possible.<br />
• Turning head to<br />
one side<br />
compresses the<br />
jugular veins<br />
and inhibits<br />
cerebral venous<br />
drainage,<br />
thereby<br />
increasing<br />
intracranial<br />
pressure.<br />
• Continual<br />
activity can<br />
increase<br />
intracranial<br />
pressure.<br />
• Provides<br />
calming effect,<br />
reduces<br />
adverse<br />
physiological<br />
response and<br />
promotes rest<br />
to maintain or<br />
lower<br />
intracranial<br />
pressure.<br />
• These activities<br />
increase<br />
thoracic and<br />
intra-abdominal<br />
pressure which<br />
can increase<br />
intracranial<br />
pressure.<br />
• After 4 hrs.<br />
Of nursing<br />
intervention<br />
s, the client<br />
was able to<br />
demonstrate<br />
stable vital<br />
signs and<br />
absence of<br />
signs of<br />
intracranial<br />
pressure.
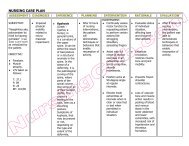
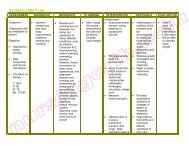
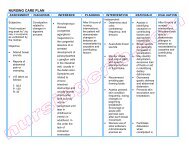
• Observe for<br />
seizure activity<br />
and protect<br />
patient from<br />
injury.<br />
Collaborative:<br />
• Restrict fluid<br />
intake as<br />
indicated.<br />
• Administer<br />
supplemental<br />
oxygen as<br />
indicated.<br />
• Seizure can<br />
occur as result<br />
of cerebral<br />
irritation,<br />
hypoxia or<br />
increase<br />
intracranial<br />
pressure.<br />
• Fluid restriction<br />
may be needed<br />
to reduce<br />
cerebral<br />
edema.<br />
• Reduces<br />
hypoxemia.