Download - CBHNP
Download - CBHNP
Download - CBHNP
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
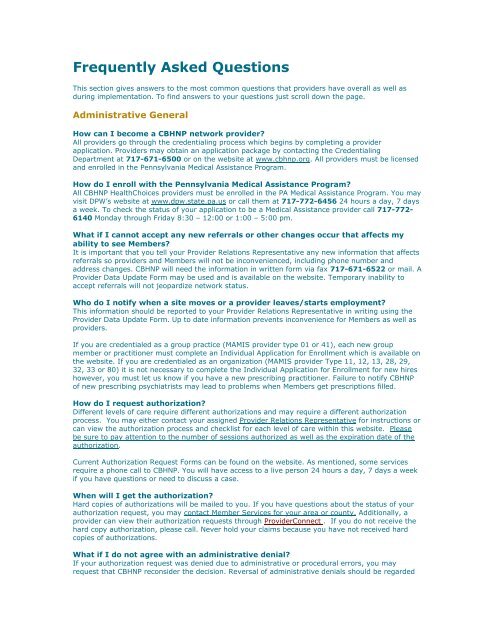
Frequently Asked Questions<br />
This section gives answers to the most common questions that providers have overall as well as<br />
during implementation. To find answers to your questions just scroll down the page.<br />
Administrative General<br />
How can I become a <strong>CBHNP</strong> network provider?<br />
All providers go through the credentialing process which begins by completing a provider<br />
application. Providers may obtain an application package by contacting the Credentialing<br />
Department at 717-671-6500 or on the website at www.cbhnp.org. All providers must be licensed<br />
and enrolled in the Pennsylvania Medical Assistance Program.<br />
How do I enroll with the Pennsylvania Medical Assistance Program?<br />
All <strong>CBHNP</strong> HealthChoices providers must be enrolled in the PA Medical Assistance Program. You may<br />
visit DPW’s website at www.dpw.state.pa.us or call them at 717-772-6456 24 hours a day, 7 days<br />
a week. To check the status of your application to be a Medical Assistance provider call 717-772-<br />
6140 Monday through Friday 8:30 – 12:00 or 1:00 – 5:00 pm.<br />
What if I cannot accept any new referrals or other changes occur that affects my<br />
ability to see Members?<br />
It is important that you tell your Provider Relations Representative any new information that affects<br />
referrals so providers and Members will not be inconvenienced, including phone number and<br />
address changes. <strong>CBHNP</strong> will need the information in written form via fax 717-671-6522 or mail. A<br />
Provider Data Update Form may be used and is available on the website. Temporary inability to<br />
accept referrals will not jeopardize network status.<br />
Who do I notify when a site moves or a provider leaves/starts employment?<br />
This information should be reported to your Provider Relations Representative in writing using the<br />
Provider Data Update Form. Up to date information prevents inconvenience for Members as well as<br />
providers.<br />
If you are credentialed as a group practice (MAMIS provider type 01 or 41), each new group<br />
member or practitioner must complete an Individual Application for Enrollment which is available on<br />
the website. If you are credentialed as an organization (MAMIS provider Type 11, 12, 13, 28, 29,<br />
32, 33 or 80) it is not necessary to complete the Individual Application for Enrollment for new hires<br />
however, you must let us know if you have a new prescribing practitioner. Failure to notify <strong>CBHNP</strong><br />
of new prescribing psychiatrists may lead to problems when Members get prescriptions filled.<br />
How do I request authorization?<br />
Different levels of care require different authorizations and may require a different authorization<br />
process. You may either contact your assigned Provider Relations Representative for instructions or<br />
can view the authorization process and checklist for each level of care within this website. Please<br />
be sure to pay attention to the number of sessions authorized as well as the expiration date of the<br />
authorization.<br />
Current Authorization Request Forms can be found on the website. As mentioned, some services<br />
require a phone call to <strong>CBHNP</strong>. You will have access to a live person 24 hours a day, 7 days a week<br />
if you have questions or need to discuss a case.<br />
When will I get the authorization?<br />
Hard copies of authorizations will be mailed to you. If you have questions about the status of your<br />
authorization request, you may contact Member Services for your area or county. Additionally, a<br />
provider can view their authorization requests through ProviderConnect . If you do not receive the<br />
hard copy authorization, please call. Never hold your claims because you have not received hard<br />
copies of authorizations.<br />
What if I do not agree with an administrative denial?<br />
If your authorization request was denied due to administrative or procedural errors, you may<br />
request that <strong>CBHNP</strong> reconsider the decision. Reversal of administrative denials should be regarded
as an exception and will not be routinely approved without compelling evidence that the provider<br />
did not follow protocol due to legitimate special circumstances as determined by <strong>CBHNP</strong>.<br />
All requests for review of administrative denial must be submitted in writing within 30 days of<br />
the authorization request denial or date of service. Providers requesting review of<br />
administrative denial will be instructed to send a letter to the attention of PROVIDER RELATIONS,<br />
ADMINISTRATIVE DENIAL REVIEW stating the following:<br />
<br />
<br />
<br />
<br />
<br />
<br />
Member name, service provided, and dates of service<br />
Explanation of circumstances<br />
Steps taken to correct and prevent future occurrences<br />
Documentation of Members seen/dates services provided and billable amount(s)<br />
Desired action from <strong>CBHNP</strong><br />
Documentation relevant to the request (i.e. EVS slip verifying that EVS was checked for<br />
eligibility and wrongly indicated enrollment status, fax confirmation page, etc.)<br />
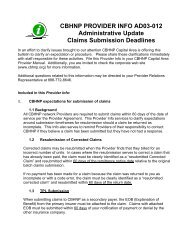
How will I know about changes in authorization processes and other procedures at<br />
<strong>CBHNP</strong>?<br />
<strong>CBHNP</strong> will share this information with providers through their assigned Provider Relations<br />
Representative as well as through the Provider Portal. Provider Info's should be regarded as<br />
supplements and clarifications to the <strong>CBHNP</strong> Provider Manual. All such communication can be found<br />
on the website and is available for download.<br />
If a Member wants to transfer services, who is responsible for transferring the<br />
services?<br />
<strong>CBHNP</strong> requests the provider take the lead on transferring the service to another provider. This<br />
includes the current provider working to secure the new provider, unless the Member has already<br />
identified which provider they want to use.<br />
BHRS Evaluation Process Clarification<br />
Do services like OP and TCM send weekly capacity reports to <strong>CBHNP</strong>?<br />
No, the requirement regarding capacity for all services other than BHRS is to notify <strong>CBHNP</strong> when<br />
you are not able to take new referrals.<br />
After OP, TCM and Crisis registration of consumers, does an approval notice come<br />
back to the provider?<br />
Yes, an authorization is mailed to Members (parent) and providers for each client registration. The<br />
authorization number is to be included on the claim.<br />
Claims<br />
How do I submit a claim for payment?<br />
Depending on the service provided, one of two claim forms may be used.<br />
<br />
<br />
CMS 1500 is used for ambulatory services or services billed with a procedure code<br />
Note: This form has been revised. For details please see the link below.<br />
NUCC – for information about the NEW CMS 1500<br />
UB 92 should be used for inpatient or other services that are billed with a revenue code<br />
Note: This form has been revised to UB 04. For details please see the link below.<br />
NUBC – for information about the UB 04<br />
What address do paper claims get mailed to?<br />
Submit all paper claims to this address:<br />
Community Behavioral HealthCare Network of PA<br />
Attention: Claims Department
PO Box 6600<br />
Harrisburg, PA 17112<br />
Can claims be faxed?<br />
Original claims must be mailed to the above address. Corrected claims can be faxed to<br />
717-671-6522. For guidelines on corrected claims, reference the claims section of the Provider<br />
Manual.<br />
What if I have a question about a paper claim?<br />
Contact the claims department by telephone or fax for all paper claims questions or problems at:<br />
<br />
<br />
1-888-700-7370 – Telephone<br />
717-671-6522 – Fax number<br />
What information is needed when calling the claims helpdesk?<br />
The following information is needed:<br />
<br />
<br />
<br />
<br />
Caller’s name and phone number<br />
Provider’s name<br />
Member’s name and SSN<br />
CPT code and date of service<br />
***If you are calling to check on the status of a claim, please review your most recent <strong>CBHNP</strong> EOB<br />
prior to calling.<br />
What is the timely filing limit for claims submissions?<br />
Depending on the type of claims submission, the time frames are:<br />
<br />
<br />
<br />
Original submission – 60 days from date of service<br />
TPL submission – 60 days from primary insurance EOB date<br />
Corrected claim – 60 days from <strong>CBHNP</strong> EOB Date<br />
How can a provider appeal an administrative denial?<br />
Reference Provider Info, Administrative Appeal Request for detailed instructions.<br />
What are the benefits of submitting claims electronically?<br />
Filing claims electronically is more efficient in several ways:<br />
<br />
<br />
<br />
Because the processing is done electronically rather that manually, claims can be paid<br />
quicker<br />
Keeping track of or filing paper claims is no longer necessary<br />
Confirmation of receipt of claims is sent out within two days of filing on a Processing<br />
Confirmation Report. This report includes the details of the file, including the total amount<br />
billed, the total number of claims within the file, and any errors on claims within the file<br />
Can paper claims still be submitted?<br />
Yes. Paper claims will continue to be accepted.<br />
What is the process for submitting claims electronically?<br />
Providers can submit electronic claims using an 837 and the steps to begin the process are as<br />
follows:<br />
<br />
<br />
Step One – <strong>Download</strong> the companion document and supplemental guide form<br />
Step Two – Establish a Trading Partner Agreement with <strong>CBHNP</strong> using the forms in the<br />
companion document
Step Three – Procure software or service with a clearinghouse or other entity that will<br />
generate an 837 in the HIPAA compliant format<br />
Step Four – Begin testing with <strong>CBHNP</strong> using the guidelines in the companion document<br />
<strong>CBHNP</strong> will soon deploy a web-based direct entry claim submission tool on our website. The<br />
tool will permit entry of claims using the CMS Form 1500 or the UB-04 and will be useful for<br />
providers who choose not to use the 837 files.<br />
What if I have a question or need help with electronic claims submission?<br />
Contact the claims helpdesk with problems or questions about electronic claims from 8:00 a.m. until<br />
4:30 p.m. Monday through Friday at:<br />
<br />
edi@cbhnp.org<br />
Is there a fee for submitting claims electronically?<br />
No. <strong>CBHNP</strong> does not charge a fee for receiving electronic claims submitted using ANY of the<br />
methods above.<br />
What should be done if a claim is rejected for payment?<br />
First – Read rejection notices thoroughly. If you still have questions, call the claims phone number<br />
on the notice (Processing Confirmation Report) for further assistance.<br />
Second – Correct the error and re-submit the claim. If all errors detailed in the notice are not<br />
corrected, the claim will be rejected repeatedly.<br />
What if a notice (Processing Confirmation Report) is received stating claims were<br />
accepted but payment is not received?<br />
Call the claims phone number on the Processing Confirmation Report.<br />
Do not re-submit the claim as this will result in a duplicate claim denial and you may be subject<br />
to unnecessary clearinghouse charges.<br />
What if a different clearinghouse is being used?<br />
To submit claims electronically to <strong>CBHNP</strong>, your clearinghouse would need to contact <strong>CBHNP</strong> to<br />
establish a Trading Partner Agreement and begin testing.<br />
Can a small practice submit claims electronically?<br />
Yes. Any size practice can submit claims electronically.<br />
When will I get paid?<br />
Ninety percent (90%) of all clean claims are paid within 30 days. All clean claims are paid within 45<br />
days. A clean claim includes all of the information necessary to process your claim. Necessary<br />
information is listed in Chapter VI of the <strong>CBHNP</strong> Provider Manual.<br />
If Gateway Assured (Medicare product handled by <strong>CBHNP</strong>) is the primary payer, do<br />
we bill Gateway Assured or directly to HealthChoices <strong>CBHNP</strong>?<br />
HealthChoices/Medicaid is always the payor of last resort. Therefore, pre-cert would be needed with<br />
Gateway for all levels of care covered under Gateway Assured Behavioral Health Plan. This does not<br />
include any BHRS levels of care since they are only Medicaid funded. For services such as inpatient<br />
and outpatient that are covered by Gateway, providers do not need to pre-certify with<br />
HealthChoices. They would notify <strong>CBHNP</strong> (if inpatient) and send in the claim with the Explanation Of<br />
Benefits. Please refer to <strong>CBHNP</strong>s Third Party Liability / Coordination of Benefits letter and policies for<br />
further information.<br />
The 60 day time frame to re-submit a bill is of concern. Is there any flexibility here,<br />
other than an Administrative Appeal if the deadline is not met?<br />
Providers need to adhere to the 60-day timeframe from date of service or EOB, whichever applies.<br />
If there are circumstances outside provider control, the Admin Appeal process should be used.<br />
Providers in the Capital Area were initially worried about this as well but soon came to realize that it
is not as difficult as anticipated. It actually helps providers keep cash flow moving and improves<br />
documentation.<br />
Eligibility<br />
How do I check Member eligibility?<br />
Due to volatility of membership, we strongly recommend that providers check eligibility frequently.<br />
<strong>CBHNP</strong> has no involvement with determining eligibility. Member files are downloaded to <strong>CBHNP</strong> on a<br />
daily basis from Department of Public Welfare (DPW). Further, authorization is not a guarantee of<br />
payment. The provider must verify that the Member continues to be eligible prior to rendering the<br />
service.<br />
Providers should check the Members eligibility by using the State’s Electronic Verification System<br />
at 1-800-766-5387 at no cost to you. When calling EVS, be prepared to supply your provider MA<br />
ID, the Member identification number and date of birth. You can check eligibility 24 hours a day, 7<br />
days a week using this phone number.<br />
If you are interested in obtaining EVS software or have questions about the system, contact DPW at<br />
717-975-6045.<br />
What would be some of the reasons why Members would get switched back between<br />
<strong>CBHNP</strong> and MA on a weekly and even daily basis? What does the provider need to do<br />
when this occurs?<br />
Eligibility is the responsibility of the CAO. Changes could be caused by Member not reapplying, jail,<br />
placement in nursing home, error, etc. Providers are advised to keep a record of the eligibility check<br />
so if the record is retroactively updated, they can show the Member was not eligible when they<br />
checked, therefore did not get authorization.<br />
How do we, as providers, know when a Member goes back and forth from FFS to<br />
<strong>CBHNP</strong>?<br />
The provider is responsible for checking EVS on a regular basis (<strong>CBHNP</strong> recommends daily).<br />
The funding gap between start of care in Inpatient and the HealthChoices start date<br />
is of concern. Does this apply to Inpatient as well as Outpatient?<br />
<strong>CBHNP</strong> is the payer as of the date noted in the eligibility verification system. Medical Assistance<br />
Fee-For-Service does typically backdate to the date of admission. However it is possible that a<br />
Member could have FFS coverage from the Admit Date and a different <strong>CBHNP</strong> effective date. If<br />
there are problems with DPW not backdating to the admission date, they should discuss this with<br />
the County Assistance Office. Providers are encouraged to verify eligibility frequently during an<br />
inpatient stay (at least weekly for long term stays) and before every outpatient visit.<br />
Behavioral Health Rehabilitative Services<br />
For BHRS initial packets, can the initial treatment plan be written by a bachelor's<br />
level staff? If a master's level person is writing the treatment plan for the initial<br />
packet, is it billable and how (if this is an initial and authorization is not in place yet<br />
for the provider)?<br />
Medical Assistance Bulletins and billing requirements always apply and need to be followed. BHRS<br />
providers are not required to have a full treatment plan submitted with the initial packet; however<br />
goals must be identified. This usually occurs at a very basic level at the ISPT meeting. There is a<br />
form for this. The formal treatment plan is not completed until after the authorization and services<br />
begin.<br />
What services can the MT, BSC, and TSS bill for?<br />
A reference, as this could be altered to some degree in the new HealthChoices area, can be<br />
reviewed in the link below:
BHRS Update Clarification of MT, BSC, and TSS<br />
Can we bill for doing the packets for the review meetings?<br />
For the initial BHRS request, when BSC, MT, or TSS service is authorized, the ISPT payment will be<br />
automatically authorized.<br />
Exactly when are we allowed to have the ISPT meeting? Are we permitted to have<br />
the ISPT before the evaluation date or does it have to be the evaluation date or<br />
later?<br />
Typically the ISPT meeting is held the day of the evaluation or after so the team can discuss the<br />
evaluator’s recommendations at the ISPT meeting.<br />
What is included in "BHRS?" Is it just BSC, MT and TSS or does the new procedure<br />
involve after-school, TAG and others?<br />
BHRS in the flow chart includes BSC, MT, and TSS as well as BHR exception services such as TAG,<br />
Stepping Stones, IDT, ASP, etc. The ISPT payment is for BSC, MT, and TSS as indicated in the April<br />
18, 2007 memo ―New BHRS policies-billing for preparation time for Members who meet MNC for<br />
BHRS (BSC, MT, TSS)‖ which is available on the <strong>CBHNP</strong> website.<br />
Is provider 50 Case Management an allowable service?<br />
<strong>CBHNP</strong> does not pay for provider 50 case management.<br />
Is <strong>CBHNP</strong> willing to review packets that do not have school feedback in them?<br />
The request will go the CCM for review. The request may get denied if there isn’t enough clinical<br />
information to justify medical necessity for services in the school setting. Team members can use<br />
the OPTIONAL <strong>CBHNP</strong> feedback form to submit school information or they can submit school<br />
feedback/information in another format.<br />
The treatment plan that gets submitted will continue to be an initial treatment plan,<br />
correct?<br />
A proposed treatment plan should be submitted with the initial request for the MNC review. Then,<br />
within 30 days of the start of services the Initial Treatment Plan should be submitted.<br />
If Members haven't received services yet and we need to get them re-authorized,<br />
how do we note that in the re-auth packet?<br />
Progress, lack of progress, or lack of service delivery should be clearly noted. <strong>CBHNP</strong> also<br />
recommends submitting to the evaluator the provider report to the evaluator form which is located<br />
on the website. This form clearly states the services, and quantity provided, which assists the<br />
evaluator in assessment for the next prescription.<br />
Will this process generate more complaints and grievances?<br />
Complaints about access should not increase due to this process. In fact, they may decrease as the<br />
family is working with the provider of their choice directly. The level of grievance is closely tied to<br />
the level of service denials, which is not known at this time.<br />
Can transition packets be sent in bulk or do they need sent individually? Do they get<br />
sent to <strong>CBHNP</strong>—Clinical Dept. PO Box 6600, Harrisburg, PA 17112?<br />
You can send those in Bulk. Yes, that is the correct address.<br />
For new clients coming in for services to begin on the “go live date”, where do we<br />
send those packets?<br />
<strong>CBHNP</strong>, PO Box 6600, Harrisburg, PA 17112<br />
How can we find out which of our clients will be transitioning to <strong>CBHNP</strong> and which<br />
ones will be staying with the state?<br />
<strong>CBHNP</strong> will not know who is transitioning to HealthChoices. Providers need to check EVS frequently,<br />
as Member status can change for many unforeseen circumstances.<br />
Timeframes
If a provider has a child due for BHRS services June 1, can they submit to the state<br />
for the authorization for only one month and also submit a request for authorization<br />
to <strong>CBHNP</strong> beginning July 1 simultaneously?<br />
A provider could do this but would result in double work for the provider. The provider needs only to<br />
make the normal request (4-months or up to 12 months, if ASD, as applicable) to the State FFS<br />
system. On July 1, the provider needs only to submit a transition packet which is essentially a copy<br />
of the packet submitted to the State along with the Prior Authorization Notice (PAN) for TSS. For MT<br />
or BSC only cases the state does not give an approval notice for these services, in this case the<br />
provider would submit a copy of the Plan of Care (POC) signed by the County Authorizing Agent<br />
along with a copy of the packet. <strong>CBHNP</strong> then honors the existing auth as a transition packet.<br />
Regarding the process for initial requests for BHRS services, on the flow chart that<br />
indicates that providers are to submit a copy of the written report within 10 days to<br />
the provider and the assigned CCM-does that pertain to the psychiatric evaluation?<br />
Evaluations recommending BHR services need to be submitted as described within the 10 days. This<br />
has been the previous expectation for evaluators so this does not reflect a change.<br />
What if a provider has difficulty getting an evaluation scheduled within 7 days?<br />
It is understood that the 7-day timeframe is difficult to adhere to at times. Providers are to ensure<br />
that they are able to explain any delay and that the family has the option to wait for this provider or<br />
to choose another. The 7-day timeframe expectation does not reflect a change.<br />
If a provider has capacity when they are chosen but by the time they receive the<br />
packet back they no longer have capacity, what happens then?<br />
Once the provider has accepted the Member then they are the designated provider. If they cannot<br />
fulfill the obligation then they should assist the family in locating a new provider (similar to the<br />
transfer process).<br />
When a provider receives the referral and isn’t able to staff the referral immediately,<br />
is the treatment plan expected within 30 days?<br />
A proposed treatment plan is submitted with the BHRS submission sheet, ISPT meeting sign<br />
in/concurrent form, evaluation, plan of care, ISPT notes as part of the complete request. The initial<br />
treatment plan should still be submitted 30 days from the start date of services.<br />
Evaluations<br />
Are evaluators expected to review with families the Children’s Services Guide and<br />
the Preferred Provider List within the context of the one hour psychiatric evaluation?<br />
Best practice evaluations as described by the State and fully supported by <strong>CBHNP</strong> require the<br />
evaluator to be knowledgeable about all levels of care for children and to ensure the family<br />
understands the service delivery system (this expectation is not limited to Specialized Evaluators<br />
only). The Children’s Services Guide was developed to assist evaluators in describing all available<br />
services and can be reproduced and handed out to families as well. The Children’s Services Guide is<br />
purely informational in which the first page indicates clarification on access and expectations for<br />
families; the second page indicates the different level of care that any Evaluator should be going<br />
over with the families; and the third page indicates acronyms and specific county contact numbers.<br />
The Preferred Provider Form (otherwise known as freedom of choice) is to be presented to the<br />
family at the end of the evaluation only when the Evaluator knows they will be recommending<br />
BHRS. They are simply to provide and indicate the providers available to the family in that specific<br />
county and have the family mark their choice of provider. They can also rank the providers if they<br />
prefer.<br />
Does the evaluator need to get the report completed and submitted within 10 days?<br />
Does this refer to psychiatric evaluations?<br />
Yes, this pertains to all evaluations.<br />
Who is responsible for making referrals if they choose a provider other than the one<br />
who did the evaluation?
As noted on the flow chart, the evaluator will send the <strong>CBHNP</strong> BHRS evaluation/addendum<br />
registration form to the provider the family has chosen. This will trigger the provider to move<br />
forward with scheduling an ISPT meeting.<br />
Will we get paid for that activity?<br />
The evaluator currently sends in this form to <strong>CBHNP</strong> for payment and this is not a change.<br />
Who sets up the ISPT?<br />
The chosen provider or TCM (if assigned) is triggered to set up the ISPT when they receive the<br />
<strong>CBHNP</strong> BHRS evaluation/addendum registration form and Preferred Provider Form. If RTF or CRR-<br />
HH is recommended then the TCM (if assigned) or <strong>CBHNP</strong> will take the lead with arranging an ISPT<br />
meeting.<br />
If the Member is recommended for BHRS and BHRS exception services also<br />
(TAG/ASP/St St), who takes the lead for submitting the packet and scheduling the<br />
ISPT meeting?<br />
The BHRS provider is considered ―primary‖ or ―lead‖ for this particular example. As the flowchart<br />
indicates, the BHRS provider (lead) or TCM (if assigned) will be responsible for putting together the<br />
request and coordinating with the BHRS exception service provider.<br />
Are there differences when evaluations come from outside the BHR<br />
evaluator/provider, for example from an IP unit?<br />
In our experience, it is rare that an evaluation comes from an IP unit with initial BHR<br />
recommendations (usually services are already in place and the IP evaluation can at times be as<br />
brief as a one page document which is not within the Best Practice standards for BHRS evaluations).<br />
More usual is the child with BHR and the IP unit is recommending an increase in hours on existing<br />
services. In those cases, the IP unit should be coordinating with the existing provider. If the<br />
Member did not have a BHRS provider already in place then the family would be directed to the<br />
provider of their choice to continue with the process and move forward with scheduling an ISPT<br />
meeting and submitting a request for services.<br />
Providers requested a list of evaluators and were referred to use the provider<br />
directory on the website. The concern was raised that this is only updated once a<br />
year.<br />
There are not that many applications that come in for new evaluators so the list is up to date.<br />
What if the provider doesn’t have capacity for BHRS but they do for the evaluation,<br />
what happens with the referral for services?<br />
The parent/guardian can choose to have the evaluation completed by the evaluator of their choice.<br />
The provider agency that the evaluator is associated with does not necessarily need to be the<br />
provider chosen by the parent/guardian to render the BHR services. A Member can have an<br />
evaluation completed by an evaluator from one provider agency and then referred to another for<br />
the services. The family can choose to wait until the provider of their choice has capacity or they<br />
can seek out a different provider.<br />
If an evaluator at one agency does the evaluation but the family chooses another<br />
provider for the BHRS for whatever reason, who is responsible for submitting the<br />
complete request to <strong>CBHNP</strong>?<br />
The provider who will be doing the BHRS services or TCM (if assigned)<br />
If a provider does not have capacity and the family is waiting for that particular<br />
provider, does that accepting provider need to schedule another evaluation if the<br />
authorization runs out?<br />
If the family chooses a particular provider, that provider must send in the complete request within<br />
60 days, even if they don’t have capacity, to get the request reviewed. If the Member is approved,<br />
the authorization will be generated to the provider who submitted the request and they will need to<br />
keep track of the authorization period. They may need to schedule the Member for another<br />
evaluation to re-authorize services, even if services haven’t started.<br />
What if a provider receives a referral that they are not able to accept for reasons<br />
beyond capacity?
The provider is still responsible for the referral and needs to discuss this issue with the family, assist<br />
them with choosing another provider, and making the referral to the new provider.<br />
Provider Choice<br />
What if a family only picks one provider? What if the family doesn’t choose a<br />
provider?<br />
Typically, families present for the evaluation at the provider they already believe they want for<br />
services. They can choose only one provider as long as they indicate this on the Preferred Provider<br />
Form and have been informed of the choice of providers who provide service within their county.<br />
The family should pick who they want to provide services.<br />
As many families select first available, and not a specific provider, are we then going<br />
to be responsible to contact every provider to determine that, and then somehow<br />
coordinate that selection with the family?<br />
The selection pertaining to first available was facilitated by <strong>CBHNP</strong> as an attempt to drive quicker<br />
access. It is usual for the family to already have a provider identified as their choice. As outlined in<br />
the flow chart, the evaluator will send the preliminary service recommendations to that preferred<br />
provider. This means the family needs to choose whom they would like to serve their child. This<br />
form then triggers the provider to schedule the ISPT meeting.<br />
Who is responsible for finding a provider with capacity?<br />
The family chooses the provider they wish to serve their child. The chosen provider then is notified<br />
and can begin to prepare to deliver services. The evaluator notifies the provider through the <strong>CBHNP</strong><br />
BHRS evaluation/addendum registration form and Preferred Provider Form. For capacity, please<br />
continue to follow the current process in notifying <strong>CBHNP</strong> weekly. Provider capacity information will<br />
be posted weekly to the <strong>CBHNP</strong> website.<br />
Who will be monitoring capacity?<br />
Providers will still inform <strong>CBHNP</strong> capacity reports as they currently do. Please keep in mind that<br />
capacity changes daily and not all providers notify <strong>CBHNP</strong> as to their most recent status.<br />
Are we going to be provided with the list from providers with their current<br />
openings?<br />
Please note that <strong>CBHNP</strong> historically has not been consistently informed of capacity from all<br />
providers. For capacity, please continue to follow the current process in notifying <strong>CBHNP</strong>. Evaluators<br />
and providers can access current reported capacity on the <strong>CBHNP</strong> website under the provider forms<br />
section<br />
Can provider fax numbers be added to the preferred provider forms?<br />
Space is limited. Please contact the provider directly for their fax and other contact information.<br />
What if the provider has capacity for TSS but not a clinician? Can this be<br />
differentiated on the capacity form so evaluators and providers know exactly what<br />
services are available?<br />
Capacity means the provider accepts the Member and then begins serving the Member as soon as<br />
possible while they recruit to staff the full prescription.<br />
What happens when a family selects “first available” as their choice?<br />
Families need to select a provider of choice that they prefer. The evaluator will then send the<br />
<strong>CBHNP</strong> BHRS Evaluation/Addendum Registration Form and Preferred Provider Form to evaluation<br />
will be sent to that provider. Evaluators and Families can look at the <strong>CBHNP</strong> web site for current<br />
provider capacity in order to assist them with making their decision about their provider of choice.<br />
The evaluation will be sent to the provider that the family chose.<br />
What if there are no providers with immediate capacity in my county?<br />
Provider capacity changes rapidly. Provider choice and referral to the families chosen provider is not<br />
limited to the providers reported availability. All providers need to work to staff referrals as quickly<br />
as possible.
ISPTs<br />
How does the 7 day window for notifying <strong>CBHNP</strong> impact upon the provider? Can they<br />
really give us 7 days notice if the ISPT has to be held within 10 days?<br />
When the provider receives the <strong>CBHNP</strong> BHRS Evaluation/Addendum Registration Form (this is sent<br />
immediately while the evaluation must be sent within 10 days) they will begin to schedule the ISPT<br />
meeting. <strong>CBHNP</strong> will be part of the team called to participate in the ISPT meeting.<br />
How can we ensure that providers and evaluators know when/if a TCM is involved?<br />
Families cannot always provide this info.<br />
As part of coordination of care, the TCM should be aware, if not involved with the evaluation process<br />
as part of monitoring their caseload. If no TCM has been identified and the family reports none to<br />
the provider, the provider should pursue the process for the ISPT meeting and packet submission<br />
(keeping in mind that the provider will be reimbursed for this time once request is approved).<br />
The flow chart indicates that providers will receive reimbursement for 2 hours of MT<br />
to cover the ISPT--upon approval of BHRS. If BHRS is not approved, there will be no<br />
reimbursement?<br />
That is correct. It is the expectation that Evaluators are recommending services that match Member<br />
needs.<br />
If there is a TCM on the case are they required to schedule the ISPT?<br />
The flowchart indicates ―the provider or TCM if assigned‖ which means the provider and the TCM<br />
should do this in coordination with each other.<br />
What occurs for billing of ISPT time if the services are then not approved?<br />
If BHRS (MT, BSC, TSS) are not approved, the time for the ISPT is not billable.<br />
How can a provider be expected to do the ISPT meeting right after the evaluation<br />
when they don’t know what the recommendations are going to be, what provider<br />
choice is going to be, or who they should invite, if there is going to be<br />
recommendations for school then school would need to be invited.<br />
Having the meeting immediately following the evaluation is NOT a requirement. This information<br />
was obtained as part of provider feedback to <strong>CBHNP</strong> in which some providers do engage in this<br />
process.<br />
If only a BHRS exception service is recommended can the BHRS exception service<br />
provider bill for the 2 hrs of MT for coordinating the ISPT?<br />
No, the reimbursement for the ―MH-BHRS-Initial ISPT‖ (which is comparable to the reimbursement<br />
rate of 2 hrs of MT) only applies to BHRS (TSS, BSC, MT requests).<br />
What if a combination of services is requested BHRS and BHRS exception services,<br />
who can bill for the 2 hrs of MT for coordinating the ISPT?<br />
The BHRS (TSS, BSC, MT) provider would be considered primary and could bill for the ―MH-BHRS-<br />
Initial ISPT‖ event for coordinating the ISPT.<br />
Family Based Mental Health Services<br />
Will <strong>CBHNP</strong> be monitoring the Family Support monies and how we spend it?<br />
Requirements under HealthChoices are a little different with regard to Family Support Services<br />
spending. <strong>CBHNP</strong> expects that a minimum of 2.4% spending requirement for FSS be met. This<br />
requirement is notated on the <strong>CBHNP</strong> fee schedule. Policies and procedures are located on the<br />
website. The policy related to FFS spending and documentation is found at this link. <strong>CBHNP</strong> may<br />
audit records for quality and to confirm minimum spending requirements are met.<br />
Can the treatment plans be handwritten?
Handwriting is not recommended but is acceptable as long as the treatment plan is legible. If the<br />
treatment plan is not legible, it will be returned to the provider.<br />
Is there a contact person at <strong>CBHNP</strong> for general questions about Family Based?<br />
Please contact your regional Provider Relations Representative. Use this link to locate the Regional<br />
Provider Relations Representative for your area or county.<br />
Pam Wilshire, Children’s System Coordinator, may also be contacted through the Members County<br />
specific Member Services line. Use this link to locate the Member Service number for your area or<br />
county.<br />
Who are the care managers that will handle the Family Based cases, and what is<br />
their phone number?<br />
You will be able to reach the care managers through the Member Services number for your county<br />
or area that are located using this link. There are not designated ―FBMHS‖ Care Managers per se as<br />
Care Managers handle multiple levels of care.<br />
Does the family also attend the 30 day initial interagency meeting?<br />
Family participation is required with the family members and necessary team members (ie: other<br />
providers in the home, etc). All systems must be invited to determine the therapeutic needs/goals<br />
for the family.<br />
If a psychiatrist is recommending Family Based, do I need to send a FBMHS<br />
Recommendation Letter, the Initial FBMHS Request/Referral Form, the POC, and the<br />
Provider of Choice Form? Do I need any other report from the doctor?<br />
Yes, you also need the Submission Sheet. If the psychiatrist recommended FBMHS in an evaluation<br />
within the past 6 months, then the evaluation along with the POC, Preferred Provider Form and<br />
Submission Sheet is all that would be needed. No other reports are needed from the doctor.<br />
Does the care manager get invited to the 30 day initial interagency meeting?<br />
The Care Manager should be invited/notified. Since they are in Harrisburg, they will attend if<br />
possible. The Children’s Information Specialist (CIS) who is stationed in the regional offices will<br />
most likely attend. The CCM’s can be notified/invited via the <strong>CBHNP</strong> ISPT Meeting Notification Form.<br />
Is the interagency meeting the same as the ISPT meeting for the 45 day concurrent<br />
review?<br />
An ISPT meeting is not required for a 45-day concurrent review since this is being taken care of at<br />
the 30-day initial interagency meeting. This meeting is used to gather/collect the clinical information<br />
that is submitted for the 45-day concurrent review. A completed Interagency Treatment Team<br />
Meeting Form which includes outcomes showing current services occurring for all the family’s<br />
children and the Member. This meeting must include recommendations for all ongoing services for<br />
all the family’s children and the Member, invitees to the meeting, who attended and type of<br />
attendance, and agreement or disagreement with services recommended. While the FBMH Services<br />
Interagency Treatment Team Meeting Form is preferred, other forms which include all the required<br />
information are acceptable. The form is located at <strong>CBHNP</strong>’s Provider Portal under Forms.<br />
Does the FBMHS team schedule another interagency meeting for the 120 day review,<br />
or do they send another copy of the initial review meeting?<br />
The FBMHS team submits the required information for the 120-day review per <strong>CBHNP</strong> Policy and<br />
Procedure. The team should have another meeting to review the Member’s status. The Interagency<br />
Treatment Team Meeting Form , which should specify current services occurring for all the family’s<br />
children and Member, recommendations for ongoing services for all the family’s children and<br />
Member, invitees to the meeting, who attended and type of attendance, and agreement or<br />
disagreement with services recommended. The <strong>CBHNP</strong> form is preferable however, any form<br />
indicating all information required may be used.<br />
Once a case has been approved through <strong>CBHNP</strong>, who is the person that receives the<br />
phone calls and the paperwork for the reviews? Is it the care manager?<br />
The case will ultimately be assigned to a care manager, but initially will go to the children’s staff<br />
(Clinical Associates) for processing. Packets should be mailed to:
Community Behavioral HealthCare Network of Pennsylvania (<strong>CBHNP</strong>)<br />
Attention: Clinical Department<br />
PO Box 6600<br />
Harrisburg, PA 17112<br />
Phone calls should go to Member Services. Use this link to locate the Member Service number for<br />
your area or county.<br />
Can the director of a FBMH program act as one of the team members for<br />
implementation of direct services?<br />
Yes, as long as the director meets the FBMH regulations for qualifications and stays within the<br />
allocated caseload as identified in the regulations.<br />
Outpatient Mental Health Services<br />
Is there an electronic process that could register the thousands of Outpatients with<br />
a provider, rather than thousands of faxes at the end of June if July 1 is the<br />
implementation date?<br />
Not at this time. Please note that the only registrations required for OP are those where <strong>CBHNP</strong> is<br />
the PRIMARY insurance. If <strong>CBHNP</strong> is secondary, only a claim with an EOB from the primary is<br />
required. Requests can be faxed or mailed. When a Member is first seen for OP under<br />
HealthChoices, requests can normally be submitted up to 10 calendar days after that 1st OP<br />
appointment or 30 days for ICM/RC requests. For implementation, <strong>CBHNP</strong> is relaxing this<br />
requirement to 30 days for all requests. Therefore, the ideal approach for providers would be to<br />
stagger mailed or faxed registrations of OP and ICM / RC requests throughout the first month after<br />
the implementation date. Requests can be received as early as 2 weeks before implementation.<br />
If a BA person does an intake how do we fill out the Outpatient Treatment Request<br />
Form (OTR)?<br />
Count the intake as the first individual OP session (90806). However, this must be a clinical<br />
assessment intake and not just a paper administrative intake. If Bachelors level therapists are used,<br />
the provider must closely adhere to all the licensing requirements regarding supervision and<br />
oversight. The full staff roster should also have been submitted as part of credentialing to <strong>CBHNP</strong>.<br />
Is a BA person paid $60.00 (code- 90806) for doing an intake?<br />
Yes, if the requirements are met.<br />
Is it ok to ask for the maximum units for services (individual, family, or group) on<br />
the first request to cover all the possible needs for the year?<br />
As of 7/1/07 – providers will not be requesting variable units – standardized units will be issued for<br />
requested services. If the units are exhausted prior to the end of the one-year authorization period,<br />
the provider would simply request re-authorization of services.<br />
Can a BA person provide individual, family, and group therapy, and if so, are they<br />
paid at the 90806/90847, etc. rate?<br />
<strong>CBHNP</strong> does not have requirements above those designated in licensing and Medical Assistance<br />
payment regulations. If it permitted under MA Fee–For-Service, it is permitted under HealthChoices.<br />
For all MA cases already open as of the date of implementation, does a new intake<br />
have to be done?<br />
No, new intakes are not required for persons who began treatment prior to the implementation<br />
date.<br />
If a new intake in not needed for persons who began treatment prior to the<br />
implementation date, on the request form, can we simply ask for whatever sessions<br />
we need under the CPT codes?<br />
Yes, if not listed, the provider would list the requested CPT codes and units requested.
Regarding discharge, some of our clients sit in "limbo" for weeks while the therapist<br />
is trying to determine if they should be closed (i.e.: writing letters, phone calls, etc.).<br />
Does <strong>CBHNP</strong> have an issue with any specific timeline on this other then to fax a<br />
discharge within 2 weeks of the final decision to discharge?<br />
Providers should follow their own internal policies in this regard. A general rule of thumb is to<br />
discharge if the Member has not responded within 30 days. <strong>CBHNP</strong> will want to see the efforts to<br />
engage documented in the medical record.<br />
If a Member has used up their 60 units of individual, but the therapist believes that<br />
more sessions are necessary, is there an appeal process, and does that have to start<br />
before the use of the last unit?<br />
No appeal is necessary. Simply fax a re-authorization request for more units with rationale. Request<br />
additional units before the last authorized unit is completed. Care Managers may require them to<br />
submit the treatment plan and clinical notes along with the OTR for determination, but this is not<br />
routine. Reauthorization requests can be submitted up to 10 calendar days after the ―first‖ session<br />
of the reauthorized period (i.e. if the current authorization expires on 8/1/07 the reauthorization<br />
requesting another authorization to begin on 8/2/07 would need to be submitted by 8/12/07.)<br />
In an instance where a person has insurance with MA as secondary, do we open<br />
those cases as MA starting on the date of implementation?<br />
No, it is not necessary to submit a request form to <strong>CBHNP</strong>. Registration is not required if you have<br />
authorization through the primary payer. Just send in the claim with an EOB. <strong>CBHNP</strong> is the payer of<br />
last resource so the primary payer will always be responsible first. The Member must access<br />
services through the primary payer’s network. If the provider is on the primary payer’s panel and<br />
<strong>CBHNP</strong> panel, provider gets auth & bills primary until exhausted. When primary is known to be<br />
exhausted, that would be the point where provider needs to get an auth through <strong>CBHNP</strong>.<br />
What is the minimum number of clients for a group?<br />
The minimum is 2 clients to hold a group. One person is an individual session. The requirement is<br />
the same as Fee-For-Service MA and is defined in Medical Assistance Billing Regulations Chapter<br />
1153 which providers should be familiar with as an OP provider. The maximum number is 10 clients.<br />
The OTR for treatment contains a statement about "communication with Primary<br />
Care Physicians". We get a release to the PCP at intake if the client agrees. Do we<br />
need to go beyond this?<br />
Yes, getting a ―release‖ or authorization for disclosure is really only Step 1. It is not a regulation,<br />
but <strong>CBHNP</strong> strongly encourages the best practice of obtaining a release and then communicating<br />
(via form letter, treatment plan, or other document) at the following times: at the time of<br />
admission; at the time of a significant change in medication or level of care; at the time of<br />
discharge. Compliance with this best practice is reviewed during <strong>CBHNP</strong>’s annual Treatment Record<br />
Reviews.<br />
Under Diagnostic Interview section of OTR Request Form # 3 asks about the date<br />
Member requested treatment etc. Please explain if this is the timeline for an intake<br />
or the first therapy appointment?<br />
The date Member requested treatment is the initial date of contact either by phone or by referral<br />
form from the Member or another provider requested the service.<br />
Is an unlicensed master’s level person allowed to do intakes at the master’s rate for<br />
an intake?<br />
Yes, as long as they are working under the OP facility license.<br />
On the OTR Form is the contact person the therapist and the provider name the<br />
facility?<br />
The contact person field is intended to be the one who fills out the form. That may be the therapist<br />
or possibly an administrative person. Provider name is the agency or facility.<br />
Would you anticipate getting several OTR forms on the same person for different<br />
services (i.e. pharmacologic management on a form and individual therapy on<br />
another)?
Ideally the requests will come to <strong>CBHNP</strong> on 1 form. This demonstrates coordination of treatment by<br />
the provider. Separate forms are allowable but not preferred.<br />
Targeted Case Management<br />
When the implementation takes place, how is the conversion handled? Does <strong>CBHNP</strong><br />
honor the last authorization in place? When does the provider request the new<br />
authorization? What about TCM? Providers do not necessarily get a "hard copy" of<br />
an authorization.<br />
See attached basic Transition policies. All prior DPW authorizations are honored for RTF and BHRS.<br />
Partial Hospitalization, Inpatient Mental Health and Substance Abuse will require a phone call to<br />
<strong>CBHNP</strong> within the first week of start up. TCM and Outpatient are registration services so providers<br />
will simply request authorization by completing and faxing a form to <strong>CBHNP</strong> or using<br />
ProviderConnect to request the authorization for Members in treatment. Links to Transition Policies<br />
are located here:<br />
<br />
<br />
<br />
CM-TR-001 Identification of Members<br />
CM-TR-002 Authorization for Members Receiving OP Services<br />
CM-TR-003 Authorization for Members Receiving IP Services<br />
Are there a "standard" number of units authorized for TCM?<br />
Yes,<br />
ICM - 1 year - 500 Units<br />
RC - 1 year - 250 Units<br />
In emergency cases, RC’s at times see a patient and will open them for services as<br />
the first contact. We can do a face sheet to open and then bill for the remainder of<br />
the time as an RC service. However, now, we need to get pre-auth, so I assume we<br />
should stop seeing these emergent types of cases for the purpose of expediting<br />
entry into TCM if we can’t get paid for that contact. Or can we somehow get paid for<br />
that first contact?<br />
Crisis staff should bill for any crisis work, including referral work. RC’s should then begin billing for<br />
TCM when they pick up the case. Any initial TCM request can be submitted up to 30 calendar days<br />
after the requested start date – this allows for an assessment period.<br />
What documents or paperwork will be needed from TCM providers to enroll existing<br />
clients into <strong>CBHNP</strong> on the day of implementation?<br />
Use the MH-TCM Authorization Request Form. See the document on our website entitled ―Revised<br />
TCM Authorization Request Instructions.‖ You can submit registrations any time during the month of<br />
implementation and starting 2 weeks before implementation.<br />
Will re-authorization packets for RTF need reviewed by <strong>CBHNP</strong> or will they continue<br />
to go to the county administrator for signature?<br />
If <strong>CBHNP</strong> is payer, we need to review them. The County will remain involved through the CASSP<br />
Team.<br />
Will clients be authorized for 1 year of RC services initially once implementation<br />
occurs or will some of them be time limited?<br />
All will be authorized for 1 year. Limit is on units: ICM 500, Blended 300, RC 250. If more units are<br />
needed they can be requested.<br />
Will we use the same discharge criteria along with Matrix that we currently utilize?<br />
Yes, if <strong>CBHNP</strong> sees a need for discharge we will notify you.<br />
If a client requires Wraparound, typically providers review and allow client to choose<br />
provider. In addition we look at availability. I know we will no longer be responsible<br />
for finding an RTF for a Consumer, however, will this be the case with other services
such as Wraparound, OPD, Med Management, etc? How will access services for<br />
clients be affected?<br />
Continue to work as you have and make referrals with the consumer and family choosing a<br />
provider. The provider will need to get authorization.<br />
Will our referrals go to a central location or will we be responsible for referrals?<br />
You remain responsible for referrals. The provider will then authorize.<br />
For a voluntary Inpatient, can the ICM call the care manager and update them if they<br />
saw the Member that day, or do they need to see them face-to-face?<br />
Call can be made if the staff already saw the Member that day, no need for the face-to-face.<br />
Is there any help with writing appropriate treatment goals/plans?<br />
<strong>CBHNP</strong> does not regularly offer trainings on treatment plan writings, although one was offered<br />
recently. DPW, through Drexel and Western Psych does regularly offer service plan training for TCM<br />
providers. <strong>CBHNP</strong> encourages providers to attend trainings on treatment plan writing. Historically,<br />
<strong>CBHNP</strong> has offered stipends on a first-come, first-serve basis to direct line staff to attend selected<br />
DPW-approved trainings, due to the loss in billable hours that occurs. We are currently evaluating<br />
whether such a program can be offered in newly contracted counties.<br />
Will <strong>CBHNP</strong> make sure that the TCM is contacted if someone presents at the ER?<br />
According to the staff, the ER staff is not consistent with contacting TCM, or<br />
sometimes they don’t know that there is a TCM involved.<br />
Yes, this is coordinated with <strong>CBHNP</strong>.<br />
If more than 500 units are used, what is the process to get additional units and will<br />
it be difficult to obtain additional units?<br />
Requests can be made anytime there is a need to go beyond the 500 units. Decisions are made on<br />
an individual, case-by-case basis. The TCM Request Form has a place for requesting additional<br />
units. Providers can see the TCM Instructions for how to utilize, but basically you note the number<br />
of additional units you are requesting and make a brief comment on the reason for the request.<br />
Is the Matrix completed before or after the authorization is issued?<br />
Before, since the Matrix results are required for the auth request.<br />
Is the TCM “assessment” (Matrix) a billable service? Is it a separate service or billed<br />
under TCM?<br />
It can be billed as the first billable service as you would need the Matrix to request authorization<br />
after determining the level of TCM appropriate for the Member. It is part of the units authorized by<br />
<strong>CBHNP</strong> and is not a separate code or service. The start date of the authorization requested would<br />
reflect the assessment date. You may not bill for this if the Member does not meet the Matrix<br />
requirements as we cannot issue an authorization.<br />
Who can do the assessment and when can it happen? Can it happen on the<br />
Assessment Unit level?<br />
The assessment needs completed by someone who is TCM eligible. That means they have to meet<br />
the same criteria as staff you hire for the TCM positions, and be core trained, and have matrix<br />
training (matrix training might be internal now and not done by the state). Assessment of course<br />
needs to be done face to face.<br />
If a consumer comes to our office, asks for an MA eligible service and is not<br />
currently MA eligible, we send them to the CAO. Is there any retroactive part of a<br />
<strong>CBHNP</strong> authorization that means we can get them started prior to that occurring?<br />
<strong>CBHNP</strong> can only pay as of the eligibility date, which is the system date that the CAO enters the<br />
information.<br />
Do we still need to do BSU sheet when opening someone?<br />
Unless the county changes the process, you would still need to follow the same guidelines set by<br />
them. This is more of a county question. Being entered into the BSU is not a requirement for any<br />
service by <strong>CBHNP</strong>.
How will the on-call system work?<br />
The provider has to have an ICM on-call system and inform <strong>CBHNP</strong> how to access it this system.<br />
Do you separate kids and Adults in the on-call system?<br />
Appropriate coverage needs to be met for all Members. If you can meet this need with one system,<br />
fine. If not, you may need to develop two systems.<br />
Can Case Manager bill same time as Partial Hospitalization or Family Based?<br />
No, this is a duplication of services.<br />
Who is responsible for referrals?<br />
CCM’s will have a role in this, but you will be responsible for referrals. CCM’s will identify and refer<br />
our Members for TCM as clinically indicated.<br />
If client is in prison or Torrance State Hospital, will they still be eligible for CM<br />
services?<br />
For Torrance State Hospital-for first 30 days - yes CM; and last 30 days for discharge planning.<br />
For state prison - No CM.<br />
This becomes a non billable service. In many counties, people are reassigned to administrative case<br />
management in order to follow the person and assist with discharge. Sometimes they close the case<br />
and re-open closer to return to the community. Some case management units have a state hospital<br />
liaison that carries all the consumers in the hospital and assists with d/c planning.<br />
Will we have a clinical care manager?<br />
Not one specific CCM, but a pool of CCM’s designated to each county. CCM’s will be assigned per<br />
provider for adult MH/SA IP & PHP. Adults are not assigned one specific primary CCM. Each child<br />
Member who is currently receiving services will have an assigned primary CCM who will follow that<br />
child’s case across levels of treatment/care.<br />
For 302, will case managers be expected to have face-to-face contact at hospitals?<br />
If it is BEFORE a 302 is completed yes. If the 302 is already done, no.<br />
Under Policy # CM-036-7.1.5 TCM services should not duplicate services provided by<br />
FBMH a. Who should access funds to assist with rent/utilities?<br />
Communicate with team to discuss and decide on a case-by-case basis.<br />
b. Who should complete RTF packet?<br />
A TCM. If no CM, then <strong>CBHNP</strong> will assist in this role as needed.<br />
RTF Services<br />
When must an Attachment 8 be submitted to <strong>CBHNP</strong> for RTF packets?<br />
The Attachment 8 must be submitted to <strong>CBHNP</strong> when requesting initial JCAHO and non JCAHO<br />
treatment services. <strong>CBHNP</strong> will accept a completed, signed or unsigned copy of the Attachment 8. A<br />
copy of this information must be sent to <strong>CBHNP</strong> with the initial complete request for these levels of<br />
care.<br />
When requesting a reauthorization of JCAHO and non JCAHO RTF the Attachment 8 will not need<br />
submitted to <strong>CBHNP</strong>.<br />
Does <strong>CBHNP</strong> pay for CRR-Group Homes?<br />
Yes, for existing MA enrolled programs.<br />
Substance Abuse Services<br />
How is CPT code H0034 to be used in services and billing found in both D&A and OP<br />
Psych (medication training and support, drug admin provided by an RN or LPN)?<br />
Does provider’s use RNs/LPNs now? How do they use RNs and LPNs?
H0034 is typically used for med training, med packing, and injections by nurses (this is not<br />
separately billable while in partial hospitalization). Also, unfortunately DPW payment rules prevent<br />
billing of 90862 medication checks and H0034 medication training on the same date of service.<br />
Please note that <strong>CBHNP</strong>’s use of particular codes may differ from DPW’s use in Fee-For-Service.<br />
Are there any restrictions on having a client open in D&A IOP and Psych Med<br />
Management at the same time, or served on the same day with both?<br />
No, D&A and MH can even occur on the same day.<br />
How is 90801 requested? Is the treatment request form used and put it under other,<br />
or is there a separate form? Where is the name and credentials of the person<br />
completing this service listed?<br />
90801 is only available to SA OP providers as a psychiatric evaluation. SA OP providers will use<br />
90806 - the first therapy session - to do the intake. The intake must be more than an administrative<br />
intake - there must be therapeutic value in order to bill for the session. The form itself has a<br />
designated area for persons completing the service as-well-as for person’s completing the form.<br />
Where can a list of ICD-9 codes be found? Are these codes used to list a diagnosis,<br />
not DSM?<br />
You can use the DSM codes for diagnosis. ICD-9 code lists are readily available via the internet.<br />
Is eligibility verified on the PROMISe system? Will there be any system changes<br />
after implementation?<br />
Providers can verify insurance the same three ways they currently do—phone, computer, or swipe<br />
card machine.<br />
What are the educational requirements for someone to do a D&A assessment and for<br />
someone to do therapy?<br />
We have no requirements beyond what licensing and MA permits in terms of staff education levels.<br />
If a D&A program refers someone to a facility for something like detox, is a precert<br />
done by the referring provider or the detox facility?<br />
The detox facility or the provider you refer to will do the needed authorization/precert.<br />
Inpatient and Partial Hospitalization Mental Health Services<br />
Is the 30 day maximum Length of Stay (LOS) in Acute Partial calendar days or<br />
attendance days?<br />
LOS would be days attending. Also, it is the average LOS so some may stay longer, others shorter<br />
stays - average being 30.<br />
Who completes bed searches for Inpatient?<br />
The bed search process will not change under HealthChoices. In general, the facility holding the<br />
Member and requesting admission will conduct the bed search.<br />
If no in-network facilities have accepted the Member within 8 hours of the determination of medical<br />
clearance, Referral Source will contact <strong>CBHNP</strong>’s Member Services and provide the information on<br />
which facilities were contacted and reasons for rejection. <strong>CBHNP</strong> will then provide assistance and<br />
direction which may result in contacting out-of-network facilities.<br />
If no in-network or appropriate out-of-network facilities are able to accept the Member, MSS will<br />
contact CCM to determine need to continue bed search until the next day.<br />
In the event that a Member has been approved for inpatient admission and a placement has not<br />
been located for over 24 hours, the Referral Source will contact <strong>CBHNP</strong>’s Member Services who will<br />
then follow policy ―Member in ER more than 24 hours‖ in notifying the Clinical Manager of Member’s<br />
status.
Crisis Intervention Services<br />
What do I do if a Member needs emergency services?<br />
<strong>CBHNP</strong> expects the provider to take immediate action to ensure the safety of the Member and<br />
others. <strong>CBHNP</strong> should be contacted for service authorization after the situation is stabilized. Use this<br />
link to find the member services department for your county or area.<br />
Is a separate “Choice Form” that consumers sign needed? Or is documenting that a<br />
patient was given the opportunity to choose a provider enough?<br />
It is necessary to offer choice for most services but not for Crisis.<br />
Are Encounter Forms for Crisis to be completed for telephone contacts as well? What<br />
about anonymous callers? Is all anonymous callers accumulated on one Encounter<br />
Form as done with identified patients?<br />
Yes, complete telephone contacts if billing <strong>CBHNP</strong>. Anonymous callers cannot be billed to <strong>CBHNP</strong>.<br />
Keep the data you need to bill the county on anonymous callers. Crisis permits one signature per<br />
month per client on the Encounter Form to bill all components of the service.<br />
Regarding the Encounter Form, can providers have staff do their own for their<br />
respective shift so that there is little chance of confusion in passing the form from<br />
one shift to the next?<br />
Yes, do a form for each shift.<br />
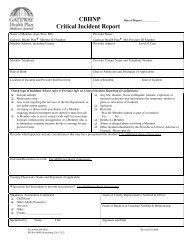
For the Critical Incident Report, would this be the responsibility of the primary<br />
therapists for open cases only? Or does Crisis staff need to report suicide attempts<br />
on every MA client that presents to the Crisis Center (or calls the Center)?<br />
No, suicide attempts do not have to be submitted by Crisis staff. They would be reported for the<br />
most part as part of inpatient request. The intent of this category is suicide attempts that occur in<br />
the presence of treatment personnel or during treatment (for example, in an RTF, partial, or<br />
inpatient unit).<br />
For pre-auth on admissions to Inpatient, can a simple checklist of items needed for<br />
Crisis to prep for the case manager be supplied?<br />
These items include:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Face-to-face assessment<br />
Information on physical health plan and any other primary insurance<br />
Presenting Problem<br />
Risk Assessment<br />
Substance Abuse (current and history)<br />
Medications<br />
Treatment (current and history)<br />
Axis I – V<br />
Natural supports<br />
Structured supports<br />
Emergency contact information<br />
Can Member return home<br />
Referrals to inpatient treatment<br />
Symptom-free periods<br />
Relapse triggers<br />
If a client has used their 30 days, but needs admitted again, what process is used to<br />
get an exception? Does Crisis call for pre-auth as usual?<br />
Yes, contact Care Management in Harrisburg. There are no benefit limits under HealthChoices.<br />
There are circumstances where <strong>CBHNP</strong> is the secondary insurer, and Members have exhausted their
commercial 30-day inpatient limit, or Medicare limits. If Crisis Intervention is aware that the limit is<br />
exceeded, they should pre-cert with <strong>CBHNP</strong>. For the claim, providers would still need to show that<br />
benefits are exhausted with the primary insurer.<br />
If an admission is denied, will <strong>CBHNP</strong> arrange an alternative service at a lesser level<br />
of care?<br />
Yes, Clinical Care Managers will work with you to arrange alternate services based on the medical<br />
necessity criteria met for the Member.