KIN Global: Health and Wellness Prevention and Partnerships: What ...
KIN Global: Health and Wellness Prevention and Partnerships: What ...
KIN Global: Health and Wellness Prevention and Partnerships: What ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>KIN</strong> <strong>Global</strong>: <strong>Health</strong> <strong>and</strong> <strong>Wellness</strong><br />
<strong>Prevention</strong> <strong>and</strong> <strong>Partnerships</strong>:<br />
<strong>What</strong> is the right mix for the next generation of health <strong>and</strong> wellness?<br />
Hetal Desai, Jamie Jones, Shaina Morphew<br />
Executive Summary<br />
<strong>Global</strong> health efforts have traditionally focused on treatment of a disease state. However, as health issues become<br />
increasingly complex <strong>and</strong> expensive to treat, preventing them becomes essential. Although the arguments in favor of<br />
preventative medicine are intuitive, there are a number of roadblocks hindering funding allocation <strong>and</strong> public attention<br />
to prevention programs, especially in the developing world. This project is meant to be a discussion of the opportunity<br />
to exp<strong>and</strong> global health efforts on programs promoting disease prevention <strong>and</strong> healthy lifestyles. The <strong>KIN</strong> working group<br />
seeks input from the delegation on the following issues:<br />
1. Currently funding is not channeled to prevention programs because it is inherently difficult to measure. <strong>What</strong> is<br />
the right balance of measurement <strong>and</strong> who is responsible for its execution <strong>and</strong> funding?<br />
2. The private sector can be a powerful mobilization force on social issues. <strong>What</strong> incentives can be used to promote<br />
private sector involvement in prevention?<br />
3. <strong>Partnerships</strong> have proven to be a successful model for addressing health issues in low <strong>and</strong> middle-income<br />
countries. When should partnerships be used in prevention <strong>and</strong> what is the most effective model?<br />
<strong>Health</strong> <strong>and</strong> <strong>Wellness</strong><br />
The study of health <strong>and</strong> wellness can be divided into three mutually-dependant segments: prevention, diagnosis <strong>and</strong><br />
treatment. Ideally, the first priority is to prevent a disease before it causes physical/mental distress or death. To do so,<br />
there must be effective diagnostic tools that are readily available, accessible <strong>and</strong> affordable for all populations. If the<br />
diagnosis is negative, preventative efforts are continued. If the diagnosis is positive, treatment ensues. Treatment not<br />
only treats the infected, it often prevents further contamination. Due to the immediacy of infection <strong>and</strong> the ability to<br />
measure results, treatment currently receives the most funding for research <strong>and</strong> development <strong>and</strong> implementation.<br />
Although prevention provides an enormous opportunity to improve the health of populations, it does not receive<br />
enough funding or implementation support. As a result, this project will focus specifically on prevention efforts.<br />
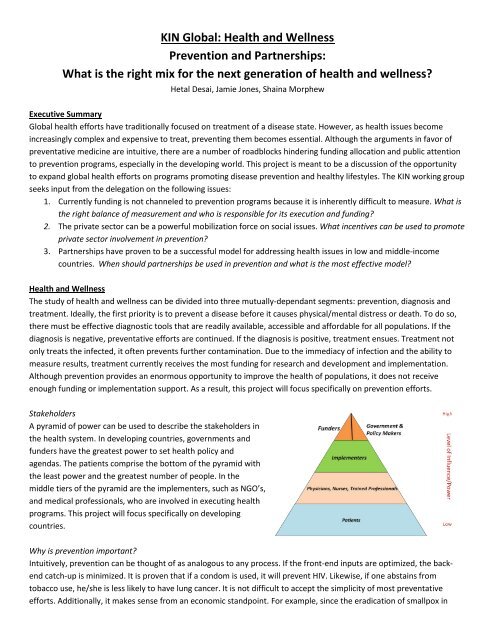
Stakeholders<br />
A pyramid of power can be used to describe the stakeholders in<br />
the health system. In developing countries, governments <strong>and</strong><br />
funders have the greatest power to set health policy <strong>and</strong><br />
agendas. The patients comprise the bottom of the pyramid with<br />
the least power <strong>and</strong> the greatest number of people. In the<br />
middle tiers of the pyramid are the implementers, such as NGO’s,<br />
<strong>and</strong> medical professionals, who are involved in executing health<br />
programs. This project will focus specifically on developing<br />
countries.<br />
Why is prevention important?<br />
Intuitively, prevention can be thought of as analogous to any process. If the front-end inputs are optimized, the backend<br />
catch-up is minimized. It is proven that if a condom is used, it will prevent HIV. Likewise, if one abstains from<br />
tobacco use, he/she is less likely to have lung cancer. It is not difficult to accept the simplicity of most preventative<br />
efforts. Additionally, it makes sense from an economic st<strong>and</strong>point. For example, since the eradication of smallpox in
1979, it is estimated that 30 million lives have been saved. The program cost $25M for 12 years, but it is estimated that<br />
it has saved an additional $275 in direct costs every year since. Some global public goods should be understood not in<br />
terms of their “cost” but in terms of the social <strong>and</strong> economic costs of delaying their eradication. 1<br />
Why isn’t prevention a major focus in society today?<br />
Given the aforementioned benefits of preventive efforts, why is it not at the forefront of the global health agenda<br />
today? The success or failure of a prevention effort is inherently difficult to measure. The result of a specific effort either<br />
occurs many years in the future or is based on the avoidance of a negative. Additionally, providing evidence for the<br />
effectiveness of a drug, vaccine or biomedical prevention mechanism is much easier than for a behavioral or structural<br />
prevention program which is usually a combination of several efforts. 2<br />
Since measurement of prevention programs is difficult, governments <strong>and</strong> funders find it challenging to create a business<br />
case for funding <strong>and</strong> implementing these initiatives. Governments hesitate to allocate funding to an effort that shows<br />
little benefit to constituents in the near-term. Funders also often fail to provide resources to prevention programs as<br />
they are not always proven, due to inherent measurement issues, to succeed. Additionally, they have thus far failed to<br />
reach consensus on the appropriate mix of behavioral, biomedical <strong>and</strong> structural preventative efforts. Finally, funders<br />
often fail to partner with the right organizations to achieve maximum results, burdening countries with parallel <strong>and</strong><br />
duplicative processes. 3 Both governments <strong>and</strong> funders fail to recognize the sustained effort necessary to wipe out a<br />
disease or to continue to lower prevalence. Where polio has been eradicated in the developed world for 30 years, it is<br />
now returning in several developing nations due to lack of continued funding. Finally, there is a lack of human <strong>and</strong><br />
physical infrastructure in developing countries to implement programs funded by international funders. To address the<br />
aforementioned barriers, we will look to successful models in the treatment <strong>and</strong> diagnosis areas of health management.<br />
<strong>Health</strong> <strong>Partnerships</strong><br />
<strong>Partnerships</strong> have become the prevailing model for addressing health problems for low <strong>and</strong> middle-income countries. 4<br />
The partnership usually includes government, funders, NGOs <strong>and</strong> possibly the private sector. Collectively, the<br />
partnership provides financial <strong>and</strong> non-financial resources, increased attention on the issue, increased attention on the<br />
NGO <strong>and</strong> an opportunity to align the incentives of all stakeholders. There are many examples of partnerships in the<br />
treatment arena <strong>and</strong> an increasing number of partnerships facilitating R&D for market-neglected diseases. However,<br />
according to Julie Smith, CDC Foundation, little to no literature has been completed on best practices in health<br />
partnerships. 5 Now that they have become the norm in developing world public health efforts, organizations must<br />
decide when partnerships are necessary, choose the correct partners, <strong>and</strong> set up the most effective structure <strong>and</strong><br />
governance for the partnership. Can partnerships help to effectively increase the focus on prevention efforts?<br />
1 Stansfield, Harper, Lamb, Lob-Levyt. “Innovative Financing of International Public Goods for <strong>Health</strong>,” CMH Working Paper Series,<br />
Commission on Macroeconomics <strong>and</strong> <strong>Health</strong>, January, 2002.<br />
2 Bertozzi, Stefano M., Laga, Marie, Baustista-Arredondo, Sergio, <strong>and</strong> Coutinho, Alex, “HIV <strong>Prevention</strong> 5: Making HIV prevention<br />
programs work,” Lancet 2008: 372: 831-44.<br />
3 Conway, Michael D., Gupta, Srishti, <strong>and</strong> Prakash Srividya, “Building Better <strong>Partnerships</strong> for <strong>Global</strong> <strong>Health</strong>,” The McKinsey Quarterly,<br />
December 2006.<br />
4 Ibid.<br />
5 Smith, Julie. CDC Interview, 12 May, 2009.