Using Reagent Strips for Rapid Diagnosis of Peritonitis in Peritoneal ...
Using Reagent Strips for Rapid Diagnosis of Peritonitis in Peritoneal ...
Using Reagent Strips for Rapid Diagnosis of Peritonitis in Peritoneal ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
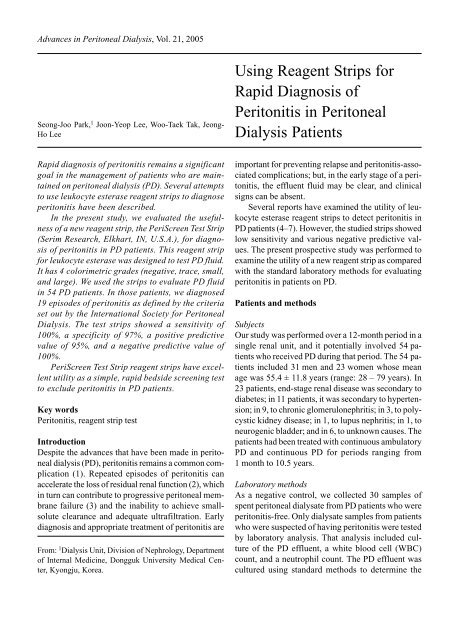
Advances <strong>in</strong> <strong>Peritoneal</strong> Dialysis, Vol. 21, 2005<br />
Seong-Joo Park, 1 Joon-Yeop Lee, Woo-Taek Tak, Jeong-<br />
Ho Lee<br />
<strong>Us<strong>in</strong>g</strong> <strong>Reagent</strong> <strong>Strips</strong> <strong>for</strong><br />
<strong>Rapid</strong> <strong>Diagnosis</strong> <strong>of</strong><br />
<strong>Peritonitis</strong> <strong>in</strong> <strong>Peritoneal</strong><br />
Dialysis Patients<br />
<strong>Rapid</strong> diagnosis <strong>of</strong> peritonitis rema<strong>in</strong>s a significant<br />
goal <strong>in</strong> the management <strong>of</strong> patients who are ma<strong>in</strong>ta<strong>in</strong>ed<br />
on peritoneal dialysis (PD). Several attempts<br />
to use leukocyte esterase reagent strips to diagnose<br />
peritonitis have been described.<br />
In the present study, we evaluated the usefulness<br />
<strong>of</strong> a new reagent strip, the PeriScreen Test Strip<br />
(Serim Research, Elkhart, IN, U.S.A.), <strong>for</strong> diagnosis<br />
<strong>of</strong> peritonitis <strong>in</strong> PD patients. This reagent strip<br />
<strong>for</strong> leukocyte esterase was designed to test PD fluid.<br />
It has 4 colorimetric grades (negative, trace, small,<br />
and large). We used the strips to evaluate PD fluid<br />
<strong>in</strong> 54 PD patients. In those patients, we diagnosed<br />
19 episodes <strong>of</strong> peritonitis as def<strong>in</strong>ed by the criteria<br />
set out by the International Society <strong>for</strong> <strong>Peritoneal</strong><br />
Dialysis. The test strips showed a sensitivity <strong>of</strong><br />
100%, a specificity <strong>of</strong> 97%, a positive predictive<br />
value <strong>of</strong> 95%, and a negative predictive value <strong>of</strong><br />
100%.<br />
PeriScreen Test Strip reagent strips have excellent<br />
utility as a simple, rapid bedside screen<strong>in</strong>g test<br />
to exclude peritonitis <strong>in</strong> PD patients.<br />
Key words<br />
<strong>Peritonitis</strong>, reagent strip test<br />
Introduction<br />
Despite the advances that have been made <strong>in</strong> peritoneal<br />
dialysis (PD), peritonitis rema<strong>in</strong>s a common complication<br />
(1). Repeated episodes <strong>of</strong> peritonitis can<br />
accelerate the loss <strong>of</strong> residual renal function (2), which<br />
<strong>in</strong> turn can contribute to progressive peritoneal membrane<br />
failure (3) and the <strong>in</strong>ability to achieve smallsolute<br />
clearance and adequate ultrafiltration. Early<br />
diagnosis and appropriate treatment <strong>of</strong> peritonitis are<br />
From: 1 Dialysis Unit, Division <strong>of</strong> Nephrology, Department<br />
<strong>of</strong> Internal Medic<strong>in</strong>e, Dongguk University Medical Center,<br />
Kyongju, Korea.<br />
important <strong>for</strong> prevent<strong>in</strong>g relapse and peritonitis-associated<br />
complications; but, <strong>in</strong> the early stage <strong>of</strong> a peritonitis,<br />
the effluent fluid may be clear, and cl<strong>in</strong>ical<br />
signs can be absent.<br />
Several reports have exam<strong>in</strong>ed the utility <strong>of</strong> leukocyte<br />
esterase reagent strips to detect peritonitis <strong>in</strong><br />
PD patients (4–7). However, the studied strips showed<br />
low sensitivity and various negative predictive values.<br />
The present prospective study was per<strong>for</strong>med to<br />
exam<strong>in</strong>e the utility <strong>of</strong> a new reagent strip as compared<br />
with the standard laboratory methods <strong>for</strong> evaluat<strong>in</strong>g<br />
peritonitis <strong>in</strong> patients on PD.<br />
Patients and methods<br />
Subjects<br />
Our study was per<strong>for</strong>med over a 12-month period <strong>in</strong> a<br />
s<strong>in</strong>gle renal unit, and it potentially <strong>in</strong>volved 54 patients<br />
who received PD dur<strong>in</strong>g that period. The 54 patients<br />
<strong>in</strong>cluded 31 men and 23 women whose mean<br />
age was 55.4 ± 11.8 years (range: 28 – 79 years). In<br />
23 patients, end-stage renal disease was secondary to<br />
diabetes; <strong>in</strong> 11 patients, it was secondary to hypertension;<br />
<strong>in</strong> 9, to chronic glomerulonephritis; <strong>in</strong> 3, to polycystic<br />
kidney disease; <strong>in</strong> 1, to lupus nephritis; <strong>in</strong> 1, to<br />
neurogenic bladder; and <strong>in</strong> 6, to unknown causes. The<br />
patients had been treated with cont<strong>in</strong>uous ambulatory<br />
PD and cont<strong>in</strong>uous PD <strong>for</strong> periods rang<strong>in</strong>g from<br />
1 month to 10.5 years.<br />
Laboratory methods<br />
As a negative control, we collected 30 samples <strong>of</strong><br />
spent peritoneal dialysate from PD patients who were<br />
peritonitis-free. Only dialysate samples from patients<br />
who were suspected <strong>of</strong> hav<strong>in</strong>g peritonitis were tested<br />
by laboratory analysis. That analysis <strong>in</strong>cluded culture<br />
<strong>of</strong> the PD effluent, a white blood cell (WBC)<br />
count, and a neutrophil count. The PD effluent was<br />
cultured us<strong>in</strong>g standard methods to determ<strong>in</strong>e the
70<br />
organisms responsible <strong>for</strong> peritonitis and the sensitivity<br />
<strong>of</strong> those organisms to antibiotics.<br />
<strong>Peritonitis</strong><br />
<strong>Diagnosis</strong> <strong>of</strong> peritonitis was made <strong>in</strong> the presence <strong>of</strong><br />
two or more <strong>of</strong> these signs: cl<strong>in</strong>ical symptoms <strong>of</strong> peritoneal<br />
<strong>in</strong>flammation (abdom<strong>in</strong>al pa<strong>in</strong>, cloudy dialysate);<br />
a peritoneal dialysis effluent leukocyte count<br />
greater than 100 cells/mm 3 , with neutrophils constitut<strong>in</strong>g<br />
more than 50% <strong>of</strong> all leukocytes; and organisms<br />
isolated by Gram sta<strong>in</strong> or a subsequent culture<br />
<strong>of</strong> PD effluent (8,9). The peritonitis was treated accord<strong>in</strong>g<br />
to the sensitivity test results.<br />
<strong>Reagent</strong> strip<br />
In patients on PD with peritonitis, peritoneal leukocyte<br />
esterase is elevated and is associated with an <strong>in</strong>creased<br />
neutrophil count. We collected samples <strong>of</strong><br />
peritoneal dialysate effluent <strong>in</strong> clean conta<strong>in</strong>er. We<br />
then immersed the reagent strip <strong>in</strong> the effluent and<br />
read it at 4 m<strong>in</strong>utes accord<strong>in</strong>g to a visual scale. The<br />
test-strip color <strong>in</strong>dicated the presence or absence <strong>of</strong><br />
leukocyte esterase, graded as negative, trace, small,<br />
or large. We considered reagent strips show<strong>in</strong>g a result<br />
<strong>of</strong> “trace” or more to <strong>in</strong>dicate peritonitis.<br />
Results<br />
Table I shows the raw data <strong>for</strong> the reagent strip results,<br />
<strong>for</strong> visual clarity <strong>of</strong> the effluent, and <strong>for</strong> WBC<br />
counts <strong>in</strong> patients with and without peritonitis. We<br />
diagnosed 19 episodes <strong>of</strong> peritonitis by the presence<br />
<strong>of</strong> at least two <strong>of</strong> the three criteria outl<strong>in</strong>ed earlier.<br />
One patient had 2 episodes <strong>of</strong> peritonitis dur<strong>in</strong>g the<br />
study period.<br />
In all patients without peritonitis, the visual clarity<br />
<strong>of</strong> the PD effluent was clear. In the patients with<br />
peritonitis, visual clarity was cloudy <strong>in</strong> 16 cases, but<br />
clear <strong>in</strong> 3 cases. The reagent strips gave read<strong>in</strong>gs <strong>of</strong><br />
trace or more <strong>for</strong> all but one <strong>of</strong> the samples from patients<br />
with peritonitis. A patient with vague abdom<strong>in</strong>al<br />
pa<strong>in</strong> had a false negative test strip read<strong>in</strong>g with<br />
clear peritoneal effluent and an absolute peritoneal<br />
effluent leukocyte count <strong>of</strong> 105 cells/mm 3 (68% neutrophils)<br />
without any bacteriologic evidence <strong>of</strong><br />
peritonitis.<br />
The test strips showed a sensitivity <strong>of</strong> 100%, a<br />
specificity <strong>of</strong> 97%, a positive predictive value <strong>of</strong> 95%,<br />
and a negative predictive value <strong>of</strong> 100%. The strip<br />
tests had high sensitivity and specificity (Table 2).<br />
TABLE I<br />
Park et al.<br />
Cl<strong>in</strong>ical, laboratory, and reagent test strip results<br />
Leukocyte Laboratory<br />
Visual clarity esterase (WBCs/mm 3 )<br />
Cloudy Clear Positive Negative >100
<strong>Reagent</strong> <strong>Strips</strong> <strong>for</strong> <strong>Rapid</strong> <strong>Diagnosis</strong> <strong>of</strong> <strong>Peritonitis</strong> <strong>in</strong> PD<br />
71<br />
This test uses phenyl pyrrole as the substrate, which<br />
is hydrolyzed to an <strong>in</strong>termediate product that reacts<br />
with a diazonium salt to produce a purple color. (The<br />
Cytur-Test is impregnated with an <strong>in</strong>doxyl ester that<br />
is oxidized to the blue compound <strong>in</strong>digo.) Prelim<strong>in</strong>ary<br />
results <strong>for</strong> the new strip from a European study<br />
showed a sensitivity <strong>of</strong> 100% and a specificity <strong>of</strong><br />
96%, together with an ability to detect as few as<br />
50 leukocytes/mm 3 (11). In our study, the PeriScreen<br />
Test Strip could detect as few as 100 leukocytes/mm 3<br />
(with a neutrophil count <strong>of</strong> not less than 50%). The<br />
results <strong>of</strong> the present study were achieved with 100%<br />
sensitivity and 97% specificity, with a positive predictive<br />
value <strong>of</strong> 95% and a negative predictive value<br />
<strong>of</strong> 100%.<br />
It should be noted that, <strong>in</strong> addition to neutrophils,<br />
the leukocyte esterase–conta<strong>in</strong><strong>in</strong>g granulocytes encompass<br />
the eos<strong>in</strong>ophils and basophils (13). Whether<br />
the large number <strong>of</strong> eos<strong>in</strong>ophils present <strong>in</strong> peritoneal<br />
effluent dur<strong>in</strong>g eos<strong>in</strong>ophilia can also elicit positive<br />
esterase strip results rema<strong>in</strong>s to be determ<strong>in</strong>ed.<br />
Conclusions<br />
The new reagent strip that we used <strong>for</strong> test<strong>in</strong>g PD effluent<br />
is a sensitive and specific method <strong>for</strong> diagnos<strong>in</strong>g<br />
PD peritonitis. It can be used as a simple bedside<br />
screen<strong>in</strong>g test whenever peritonitis is suspected. A<br />
positive result should mean the start <strong>of</strong> empirical antibiotic<br />
therapy, and a negative result should exclude<br />
peritonitis.<br />
References<br />
1 Ste<strong>in</strong> A, Baker F, Moorhouse J, Walls J. <strong>Peritonitis</strong><br />
rate: traditional versus low calcium dialysate. Am J<br />
Kidney Dis 1995; 26:632–3.<br />
2 Davies SJ, Bryan J, Phillips L, Russell GI. Longitud<strong>in</strong>al<br />
changes <strong>in</strong> peritoneal k<strong>in</strong>etics: the effects <strong>of</strong> peritoneal<br />
dialysis and peritonitis. Nephrol Dial<br />
Transplant 1996; 11:498–506.<br />
3 Topley N. Membrane longevity <strong>in</strong> peritoneal dialysis:<br />
impact <strong>of</strong> <strong>in</strong>fection and bio-<strong>in</strong>compatible solutions.<br />
Adv Ren Replace Ther 1998; 5:179–84.<br />
4 Brahm M. A simple diagnostic method <strong>of</strong> peritonitis<br />
<strong>in</strong> patients on CAPD. Scand J Urol Nephol 1984; 18:<br />
223–5.<br />
5 Antonsen S, Pedersen FB, Wang P. Detection <strong>of</strong> neutrophil<br />
granulocytes <strong>in</strong> peritoneal dialysis effluents<br />
by means <strong>of</strong> the Cytur-Test. Danish Study Group <strong>of</strong><br />
<strong>Peritonitis</strong> <strong>in</strong> Dialysis (DASPID). Scand J Cl<strong>in</strong> Lab<br />
Invest 1991; 51:149–54.<br />
6 Chan LK, Oliver DO. Simple method <strong>for</strong> early detection<br />
<strong>of</strong> peritonitis <strong>in</strong> patients on cont<strong>in</strong>uous ambulatory<br />
peritoneal dialysis. Lancet 1979; 2:1336–7.<br />
7 Antonsen S, Wang P, Pedersen FB. Comparison <strong>of</strong><br />
Cytur-Test and chemostrip LN <strong>for</strong> detect<strong>in</strong>g neutrophils<br />
<strong>in</strong> CAPD-effluents. Perit Dial Int 1990; 10:<br />
310–11.<br />
8 Leehey DJ, Gandhi VC, Daugirdas JT. <strong>Peritonitis</strong> and<br />
exit site <strong>in</strong>fection. In: Daugerdas JT, Blake PG, Ing<br />
TS, eds. Handbook <strong>of</strong> dialysis. Philadelphia:<br />
Lipp<strong>in</strong>cott Williams and Wilk<strong>in</strong>s; 2001: 375–6.<br />
9 Keane WF, Vas SI. <strong>Peritonitis</strong>. In: Gokal R, Nolph<br />
KD, eds. The textbook <strong>of</strong> peritoneal dialysis.<br />
Dordrecht: Kluwer Academic Publishers; 1994: 480.<br />
10 United States Department <strong>of</strong> Health and Human Services,<br />
Public Health Service, National Institutes <strong>of</strong><br />
Health, National Institute <strong>of</strong> Diabetes and Digestive<br />
and Kidney Diseases. USRDS 1998 Annual Data Report.<br />
Bethesda: United States Renal Data System;<br />
1998.<br />
11 Farmer CK, Hobbes H, Mann S, et al. Leukocyte esterase<br />
reagent strips <strong>for</strong> early detection <strong>of</strong> peritonitis<br />
<strong>in</strong> patients on peritoneal dialysis. Perit Dial Int 2000;<br />
20:237–9.<br />
12 Hurley RM, Wright DW, Wilson GW, Ali MA. Detection<br />
<strong>of</strong> leukocytes <strong>in</strong> peritoneal effluent by test<br />
strip. Lancet 1981; 1:437–8.<br />
13 L<strong>in</strong>né JJ, R<strong>in</strong>gsrud KM. Ur<strong>in</strong>alysis. In: Basic techniques<br />
<strong>in</strong> cl<strong>in</strong>ical laboratory science. 3rd ed.<br />
St. Louis: Mosby Year Book; 1992: 351–2.<br />
Correspond<strong>in</strong>g author:<br />
Jeong-Ho Lee, MD, Division <strong>of</strong> Nephrology, Department<br />
<strong>of</strong> Internal Medic<strong>in</strong>e, Dongguk University Medical<br />
Center, 1090-1 Sukjang-dong, Kyongju 780-350<br />
Korea.<br />
E-mail:<br />
jhlee@dongguk.ac.kr