View - BANTAO Journal
View - BANTAO Journal
View - BANTAO Journal
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
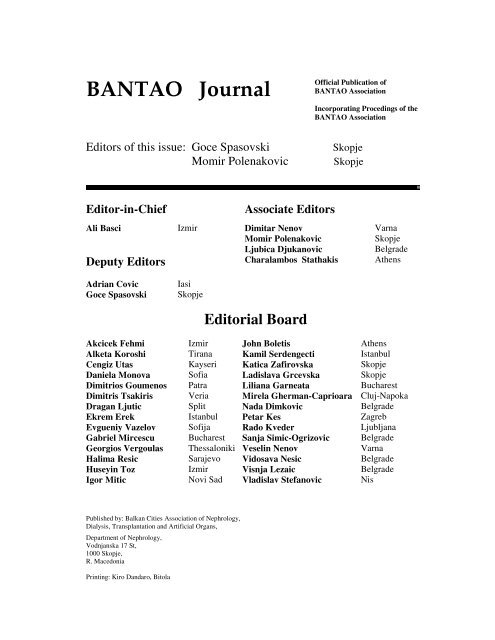
<strong>BANTAO</strong> <strong>Journal</strong><br />
Editors of this issue: Goce Spasovski<br />
Momir Polenakovic<br />
Official Publication of<br />
<strong>BANTAO</strong> Association<br />
Incorporating Procedings of the<br />
<strong>BANTAO</strong> Association<br />
Skopje<br />
Skopje<br />
Editor-in-Chief<br />
Associate Editors<br />
Ali Basci Izmir Dimitar Nenov Varna<br />
Momir Polenakovic<br />
Skopje<br />
Ljubica Djukanovic<br />
Belgrade<br />
Deputy Editors Charalambos Stathakis Athens<br />
Adrian Covic<br />
Goce Spasovski<br />
Iasi<br />
Skopje<br />
Editorial Board<br />
Akcicek Fehmi Izmir John Boletis Athens<br />
Alketa Koroshi Tirana Kamil Serdengecti Istanbul<br />
Cengiz Utas Kayseri Katica Zafirovska Skopje<br />
Daniela Monova Sofia Ladislava Grcevska Skopje<br />
Dimitrios Goumenos Patra Liliana Garneata Bucharest<br />
Dimitris Tsakiris Veria Mirela Gherman-Caprioara Cluj-Napoka<br />
Dragan Ljutic Split Nada Dimkovic Belgrade<br />
Ekrem Erek Istanbul Petar Kes Zagreb<br />
Evgueniy Vazelov Sofija Rado Kveder Ljubljana<br />
Gabriel Mircescu Bucharest Sanja Simic-Ogrizovic Belgrade<br />
Georgios Vergoulas Thessaloniki Veselin Nenov Varna<br />
Halima Resic Sarajevo Vidosava Nesic Belgrade<br />
Huseyin Toz Izmir Visnja Lezaic Belgrade<br />
Igor Mitic Novi Sad Vladislav Stefanovic Nis<br />
Published by: Balkan Cities Association of Nephrology,<br />
Dialysis, Transplantation and Artificial Organs,<br />
Department of Nephrology,<br />
Vodnjanska 17 St,<br />
1000 Skopje,<br />
R. Macedonia<br />
Printing: Kiro Dandaro, Bitola
Congress report<br />
The dream is now a reality - The seventh Congress of the Balkan<br />
Cities Association of Nephrology, Dialysis, Transplantation and<br />
Artificial Organs (<strong>BANTAO</strong>) Ohrid, Republic of Macedonia, 8-11<br />
September 2005<br />
The 7 th <strong>BANTAO</strong> Congress was held from 8 th to 11 th September<br />
2005 in Ohrid, Republic of Macedonia. Ohrid is also the place where<br />
<strong>BANTAO</strong> was born in October 9 th , 1993.<br />
The main goal of <strong>BANTAO</strong> is to promote scientific and technical<br />
cooperation in the fields of renal disease and artificial organs among the<br />
Balkan cities, giving an opportunity for exchange of experience and<br />
knowledge among the experts in the area and to engage them in<br />
collaborative projects in order to demonstrate that cooperation is possible<br />
even on the turbulent Balkan Peninsula.<br />
Following the first six successful congresses: Varna (1995),<br />
Belgrade (1998), Izmir (1999), Thessaloniki (2001) and Varna (2003),<br />
the <strong>BANTAO</strong> Congress was established as the major and institutional<br />
forum for Balkan nephrologists, with its own journal including our will<br />
to communicate, to collaborate, to get to know each other and to share<br />
our difficulties. More than just a professional event, the <strong>BANTAO</strong><br />
congress became a cultural phenomenon, through which we discovered<br />
that we have many more things in common than we previously thought,<br />
and that we must now take every advantage of being able to live and to<br />
communicate in a world without political boundaries. At present, the<br />
<strong>BANTAO</strong> Council has managed in a spirit of peace, friendship and<br />
collaboration to continuously strengthen this association and moreover,<br />
to make it a reputable part of the European and international ones. In this<br />
spirit the constitution of <strong>BANTAO</strong> has already been created.<br />
The Congress was attended by 570 physicians from the Balkan<br />
Peninsula cities as well as from Europe and USA. The Congress was<br />
held under the patronage of the President of the Republic of Macedonia,<br />
Mr. Branko Crvenkovski, Prof. M. Polenakovic was the Congress<br />
President and Doc. G. Spasovski the Secretary General.<br />
In the fields of the Epidemiology of Renal Disease, Basic Science,<br />
Clinical Nephrology, Dialysis, Transplantation and Artificial Organs we<br />
had 43 invited guest lectures, 42 oral and 223 poster presentations.<br />
The Congress was focused on several topics for example: how to<br />
improve the Balkan renal registry, prevention in nephrology, prevention<br />
of progression of renal diseases, understanding renal fibrosis and kidney<br />
transplantation on the Balkan Peninsula.
Companies invited speakers presented in six symposia, one<br />
workshop and three mini lectures their latest achievements in specific<br />
fields of nephrology, especially in dialysis.<br />
R. Vanholder, A. Perna, J. Jankowski and A. Argiles, on behalf of<br />
ESAO/EUTOX group, presented: An update on uremic toxicity- the role<br />
of EUTOX. D. Kerjaschki and H. Regele presented clinico-pathological<br />
correlation in renal transplant patients.<br />
For the first time at this 7 th <strong>BANTAO</strong> Congress we organized<br />
CME Course - Frontiers in nephrology, sponsored by ERA/EDTA and<br />
ISN/COMGAN. Six distinguished speakers: F. Locatelli, J. Mann, J.<br />
Floege, T. Risler, A. Wiecek, and M. Klinger presented the newest<br />
achievements in their fields.<br />
The abstracts were published in <strong>BANTAO</strong> <strong>Journal</strong> Vol. 3 (1),<br />
2005, pp 1-121, editor G. Spasovski as Abstract Book and 50 papers<br />
from the Congress in the <strong>BANTAO</strong> <strong>Journal</strong> Vol. 3 (2), 2005, pp 1-160,<br />
as Proceedings of the 7 th <strong>BANTAO</strong> Congress, editors G. Spasovski and<br />
M. Polenakovic. A. Basci (Izmir) was elected Editor in Chief. A. Covic<br />
(Iasi) and G. Spasovski (Skopje) were elected as deputy editors.<br />
The 7 th Congress of <strong>BANTAO</strong>, Ohrid, was a resounding success<br />
and confirmed our good will for mutual collaboration and friendship, so<br />
we can say our dream is now a reality.<br />
M. Polenakovic was elected President of <strong>BANTAO</strong> Association.<br />
The next - 8 th <strong>BANTAO</strong> Congress will be held in Belgrade in 2007. Prof.<br />
Ms. V. Nesic was elected as President of the Congress.<br />
M. Polenakovic<br />
G. Spasovski
Preface<br />
<strong>BANTAO</strong> <strong>Journal</strong> is an official publication of the <strong>BANTAO</strong><br />
Association. The aim/intention of the <strong>Journal</strong> is to cover the issues of<br />
early diagnosis, prevention and treatment of kidney diseases, as well as<br />
other specific problems Balkan nephrologists are facing with.<br />
The <strong>Journal</strong> should improve the medical education and knowledge<br />
of nephrologists and other doctors through an integrative process for<br />
appropriate management of chronic kidney disease (CKD) as an<br />
increasing worldwide problem.<br />
After the successful 7 th <strong>BANTAO</strong> Congress in Ohrid, September<br />
2005, a need to improve Balkan renal registry, the early diagnosis of<br />
CKD, prevention and management of renal diseases in order to postpone<br />
the development of end stage renal failure (ESRF) was imposed.<br />
Papers published in this volume are dedicated to aforementioned<br />
problems, presented during our last <strong>BANTAO</strong> Congress. At the General<br />
Assembly of our <strong>BANTAO</strong> Association, A. Basci (Izmir) was elected<br />
Editor in Chief. A. Covic (Iasi) and G. Spasovski (Skopje) were elected<br />
as Deputy Editors. We congratulate them and wish a good and successful<br />
work in the <strong>Journal</strong>.<br />
Guest Editors of this issue:<br />
Momir Polenakovic<br />
President of <strong>BANTAO</strong> Association<br />
Goce Spasovski<br />
Deputy Editor of the <strong>BANTAO</strong> <strong>Journal</strong>
Contents:<br />
Correlation between sera levels of sVCAM-1 and severity of kidney lesions in<br />
patients with lupus nephritis<br />
T. Ilic, I. Mitic, B. Milic and S. Curic......................................................................................... 1<br />
Continuous convective renal replacement (CCRR) system: A new modality of<br />
wearable artificial kidney<br />
M.N. Aboras and I.A. Kawalit…………………………………………………………………. 3<br />
Prevalence of hepatitis C virus infection in dialysis patients<br />
P. Dzekova, A. Slavkovska, L. Simjanovska, I. Nikolov, A. Sikole, R. Grozdanovski,<br />
A. Asani, G. Selim, S. Gelev, V. Amitov, G. Spasovski and M. Polenakovic............................ 6<br />
Influence of inflammation on nutritional status of dialysis patients<br />
P. Dzekova, I. Nikolov, G. Severova-Andreevska, A. Sikole, R. Grozdanovski, A. Asani,<br />
G. Selim, S. Gelev, V. Amitov, G. Spasovski and M. Polenakovic……………………………. 8<br />
Unfavorable prognostic factors in Immunoglobulin A Nephropathy<br />
L. Petrovic, S. Curic, I. Mitic, D. Bozic, S. Vodopivec, V. Sakac, T. Djurdjevic-Mirkovic<br />
and T. Ilic……………………………………………………………………………………...... 10<br />
Congestive heart failure and renal dysfunction<br />
D. Monova, E. Peneva and S. Monov………………………………………………………….. 13<br />
Sporadic Balkan Endemic Nephropathy (BEN) beyond the known regions of<br />
BEN<br />
J. Nikolic, T. Pejcic, D. Crnomarkovic, Z. Gavrilovic and C. Tulic…………………………… 15<br />
Amyloidosis in Turkish patients<br />
C. Ensari and A. Ensari………………………………………………………………………... 18<br />
Frequency of Alport syndrome at dialysis center “Vrsac”- Vrsac<br />
K. Djordjev, D. Tintor, G. Djurdjev, O. Vasilic-Kokotovic, I. Sokolovac and S. Bozic………. 21<br />
Eearly effects of the AT 2 receptor antagonist eprosartane mesylate (EM) in<br />
diabetic patients with and without chronic renal failure<br />
N. Nnchev, B. Deliyska, M. Bankova, P. Radulova, G. Kimenov and E. Marinova…………. 23<br />
Prealbumin and inflammatory markers in dialysis patients<br />
S. Chrysostomou, K. A. Poulia, Y. Jeanes, D. Perrea, M. Poulakou, B. Filiopoulos,<br />
D. Stamatiades and Ch. P. Stathakis…………………………………………………………… 26<br />
Liver and kidney damage in acute poisonings<br />
M. Mydlik and K. Derzsiova…………………………………………………………………… 30<br />
Vascular calcifications in patients on hemodialysis<br />
T. Damjanovic, N. Markovic, S. Djorovic, T. Djordjevic and N. Dimkovic………………… 34<br />
Is there a seasonal variation in mortality in hemodialysis patients?<br />
J. Popovic, N. Dimkovic, Z. Djuric, G. Popovic and N. Lazic………………………………… 36<br />
Propyl gallate-induced platelet aggregation in patients with end stage renal<br />
disease – The influence of the hemodialysis procedure<br />
T. Eleftheriadis, G. Antoniadi, V. Liakopoulos, A. Tsiandoulas, K. Barboutis<br />
and I. Stefanidis……………………………………………………………………….………... 40<br />
Serum cystatin C as an endogenous marker of kidney function in elderly with<br />
chronic kidney failure<br />
H. Resic and A. Mataradzija…………………………………………………………………… 46
Thyroid disfunction and ultrasonographic abnormalities in uremic patients<br />
undergoing conservative management and haemodialysis<br />
A. Mataradzija , H. Resic and E. Kucukalic-Selimovic…………………………………………. 50<br />
Prednisone/Cyclophosphamide treatment in adult-onset autosomal dominant<br />
familial focal segmental glomerulosclerosis (FSGS 1)<br />
L. Grcevska, S. Dzikova, V. Ristovska, M. Milovanceva Popovska, G. Petrusevska<br />
and M. Polenakovic…………………………………………………………………………….. 56<br />
Microalbuminuria – The new marker for Balkan Endemic Nephropathy?<br />
G. Imamovic, S. Trnacevic, M. Tabakovic, E. Mesic, M. Uzeirbegovic, M. Malohodzic, A.<br />
Halilbasic, V. Habul, D. Tulumovic, E. Hodzic, M. Atic, S. Lekic M. Dugonjic,<br />
A. Becirovic and E. Hasanovic..................................................................................................... 58<br />
Lymphatic neoangiogenesis in human neoplasia and transplantation as<br />
experiments of nature<br />
D. Kerjaschki…………………………………………………………………………………… 60<br />
Cytokines and acute renal failure<br />
K. Cakalaroski………………………………………………………………………………….. 62<br />
Amyloidosis<br />
M. Tunca……………………………………………………………………………………….. 66<br />
Oxidative stress evaluation in uraemic patients undergoing continuous<br />
ambulatory peritoneal dialysis<br />
G. Mircescu, C. Capusa, I. Stoian, D. Lixandru, E. Rus, L. Coltan and L. Gaman…….……… 69<br />
Hyperhomocysteinemia in ESRD<br />
A. F. Perna, C. Lombardi, R. Capasso, F. Acanfora, E. Satta, D. Ingrosso,<br />
M. G. Luciano and N. G. De Santo.............................................................................................. 74<br />
C.E.R.A. (Continuous Erythropoietin Receptor Activator): A new perspective<br />
in anaemia management<br />
W. Sulowicz……………………………………………………………………………………. 78<br />
Diagnosis and treatment of renal bone disease<br />
G. B. Spasovski………………………………………………………………………………… 82<br />
Efficiency of mycophenolate-mofetil in resistant nephrotic syndrome – case<br />
reports<br />
B. Milic, T. Ilic, I. Mitic, I. Budosan and S. Curic……………………………………………... 84<br />
Bacterial infections associated with double lumen central venous catheters<br />
M. S. Simin, M. Milosevic, S. Vodopivec, I. Mitic and S. Curic……………………………… 86<br />
Early renal protocol biopsies: beneficial effects of treatment of borderline<br />
changes and subclinical rejections on the histological changes for chronic<br />
allograft nephropathy<br />
J. Masin-Spasovska, N. Ivanovski, S. Dzikova, G. Petrusevska, B. Dimova, Lj. Lekovski,<br />
Z. Popov and G. Spasovski……………………………......................………………............... 88<br />
Factors associated with carotid and femoral atherosclerosis in non-diabetic<br />
hemodialysis patients<br />
S. Gelev, S. Dzikova, A. Sikole, Gj. Selim, P. Dzekova, V. Amitov and G. Spasovski............. 93<br />
Acid-base disorders in patients with hypoproteinemia<br />
P. Mavromatidou, N. Sotirakopoulos, T. Tsitsios, I. Skandalos, M. Peiou,<br />
and K. Mavromatidis.................................................................................................................... 99<br />
Instructions to authors…………………………………………………………………...… 104
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 1<br />
Correlation between sera levels of sVCAM-1 and severity of kidney lesions<br />
in patients with lupus nephritis<br />
T. Ilic, I. Mitic, B. Milic and S. Curic<br />
Department of Nephrology, Clinical Center Novi Sad, Serbia and Montenegro<br />
Abstract<br />
We determined sera concentrations of soluble vascular<br />
adhesion molecule-1 (sVCAM-1) in group of 80 patients with<br />
SLE. Our aim was to investigate correlation between level of<br />
sVCAM-1 and degree of disease activity, also severity of<br />
lupus nephritis. Using ELISA procedure we determined sera<br />
levels of sVCAM-1 in 80 patients with SLE and in group of<br />
27 healthy volunteers. Patients with SLE had significantly<br />
higher sera levels of sVCAM-1 comparing healthy controls<br />
(p < 0,001). Patients with disease in active phase had higher<br />
sera levels of this adhesive molecule comparing patients with<br />
disease in phase of remission (p < 0,001). There was a high<br />
positive correlation between sera levels of sVCAM-1 and<br />
concentration of anti-ds DNK antibodies in sera of patients<br />
with SLE (r = 0,77, p < 0,001) and there was also negative<br />
correlation between sera levels of sVCAM-1 and sera<br />
concentrations of C 3 and C 4 component of complement (r = -<br />
0,64, r = - 0,58). In group of patients with lupus nephritis<br />
were detected significantly higher sera concentrations of<br />
sVCAM-1 comparing patients without nephritis. Using WHO<br />
classification, patients with lupus nephritis were systematized<br />
in three categories: class II (5 patients), classes III and IV (18<br />
patients) and class V (7 patients). Patients with class III and<br />
class IV of kidney changes had significantly higher levels of<br />
sVCAM-1 comparing patients with class II of kidney<br />
changes. At the same time, in group of patients with activity<br />
index (AI) of kidney changes over 4 sVCAM-1 sera levels<br />
were significantly higher comparing group with AI < 4. Sera<br />
level of sVCAM-1 is reliable parameter in evaluation of<br />
autoreactivity degree in SLE. At the same time, sVCAM-1<br />
sera level can be used as reliable marker in evaluation of<br />
renal lesion extensivity in SLE.<br />
Key words: SLE, sVCAM-1, lupus nephritis<br />
Introduction<br />
Systemic Lupus Erythematosus (SLE) is chronic, inflamatory<br />
connective tissue disease which contains loss of<br />
autotolerancy as main immunological disorder accompanied<br />
with breakdown of T lymphocytes, collapse of cytokine<br />
production and B lymphocite hiperactivity (1). Cytokines are<br />
essential regulating factors of immunology response which<br />
are included in migration process of inflammatory cells into<br />
the place of immunology caused inflammatory tissue<br />
reaction, together with adhesive molecules (2). The vascular<br />
cell adhesion molecule-1 (VCAM-1) is a member of the<br />
immunoglobulin gene superfamily. VCAM-1 supports the<br />
adhesion of lymphocytes, monocytes, natural killer cells,<br />
eosinophils and basophils through its interaction with<br />
leukocyte very late antigen-4 (VLA-4). VCAM-1/VLA-4<br />
interaction mediates firm adherence of circulating nonneutrophilic<br />
leukocyte to endothelium. VCAM-1 also<br />
participates in leukocyte adhesion outside of the vasculature,<br />
mediating presursor lymphocyte adhesion to bone marrow<br />
stromal cells and B cell binding to lymph node follicular<br />
dendritic cells (3). A soluble form of VCAM-1 (sVCAM-1)<br />
has been described. Soluble VCAM-1 levels have been found<br />
in the sera of healthy individuals and increased levels of<br />
sVCAM-1 can be detected in several diseases including<br />
connective tissue diseases (4). Studies have shown that<br />
elevated levels of sVCAM-1 are related to disease activity in<br />
patients with SLE (5).<br />
The aim of our study was to investigate changes of adhesive<br />
molecule sera levels in patients with SLE comparing different<br />
phases of disease activity and comparing presence/absence of<br />
lupus nephritis. At the same time relation of vascular cell<br />
adhesion molecule sera concentrations were analized with<br />
concentrations of other disease parameters (titre of ANA,<br />
SLED AI, titre of anti-ds DNA antibodies, concentrations of<br />
C3 and C4).<br />
Patients and methods<br />
The study was carried out in 80 patients included in<br />
crossection study and 10 patients included in longitudinaly<br />
study. We used ELISA procedure to determine sVCAM-1<br />
sera levels in 80 patients with SLE and in group of 27 healthy<br />
volunteers. An anti-sVCAM-1 monoclonal coating antibody<br />
is adsorbed onto microwells. sVCAM-1 present in the sample<br />
binds to antibodies adsorbed to the microwells. A mixtureof<br />
biotin–conjugated monoclonal anti-sVCAM-1 antibody and<br />
Streptavidin–HRP is added. Biotin conjugated anti-sVCAM-<br />
1 captured by the first antibody. Streptavidin-HRP binds to<br />
the biotin conjugated anti-VCAM-1. Following incubation<br />
unbound biotin conjugated anti-sVCAM-1 and Streptavidin –<br />
HRP is removed during a wash step and substrate solution<br />
reactive with HRP is added to the wells. Acoloured product is<br />
formed in proportion to the amount of soluble VCAM-1<br />
present in the sample. The reaction is terminated by addition<br />
of acid and absorbance is measured at 450 nm. A standard<br />
curve is prepared from six sVCAM-1 standard dilutions and<br />
sVCAM-1 sample concentration determined.<br />
______________________<br />
Correspodence to: T. Ilic, Department of Nephrology, Clinical Center Novi Sad, Serbia and Montenegro
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 2<br />
Results and discussion<br />
Patients with SLE had significantly higher sera levels of<br />
sVCAM-1 comparing healthy controls (p < 0,001). Patients<br />
with disease in active phase had higher sera levels of this<br />
adhesive molecule comparing patients with disease in phase<br />
of remission (p < 0,001). There was high positive correlation<br />
between sera levels of sVCAM-1 and concentration of anti-ds<br />
DNK antibodies in sera of patients with SLE (r = 0,77, p <<br />
0,001) and a negative correlation between sera levels of<br />
sVCAM-1 and sera concentrations of C 3 and C 4 component<br />
of complement (r = -0,64, r = - 0,58). In group of patients<br />
with lupus nephritis a significantly higher sera concentrations<br />
of sVCAM-1 were detected comparing patients without<br />
nephritis. Using WHO classification, patients with lupus<br />
nephritis were systematized in three categories: class II (5<br />
patients), classes III and IV (18 patients) and class V (7<br />
patients). Patients with class III and class IV of kidney<br />
changes had significantly higher levels of sVCAM-1<br />
comparing patients with class II of kidney changes. In the<br />
same time, in group of patients with activity index of kidney<br />
changes (AI) over 4 sVCAM-1 sera levels were significantly<br />
higher comparing group with AI < 4.<br />
Conclusions<br />
Sera level of sVCAM-1 is reliable parameter in evaluation of<br />
autoreactivity degree in SLE. Serial measurements of<br />
sVCAM-1 may be helpful for monitoring disease activity in<br />
patients with SLE and lupus nephritis. The serum level of<br />
sVCAM-1 was correlated with the clinical and histological<br />
activity score. Active lupus nephritis (proliferative lupus<br />
nephritis, WHO classes III and IV) was associated with<br />
significantly elevated sVCAM-1 levels.<br />
References<br />
1. Glandman DD, Urowitz MB. Systemic Lupus Erythematosus.<br />
In. Klippel JH, Dieppe PA. Rheumatology, Mosby, London<br />
1998; 7: 11-118<br />
2. Sfikakis PP, Mavrikakis M. Adhesion and lymphocyte<br />
costimulatory molecules in systemic rheumatic disease. Clin<br />
Rheumatol 1999; 18(4): 317-327<br />
3. Sharah SR, Winn R, Harlan J M. The adhesion cascade and<br />
anti-adhesion therapy: An overview. Springer Semin<br />
Immunopathol 1995; 16: 359<br />
4. Gearing AJ, Hemingway I, Pigott R et al. Circulating adhesion<br />
molecules in disease. Immunol Today 1993; 14: 506.<br />
5. Ikeda Y, Fujimoto T, Ameno M et al. Relationship between<br />
lupus nephritis activity and the serum level of soluble VCAM-<br />
1. Lupus 1998; 7: 347-354
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 3<br />
Continuous convective renal replacement (CCRR) system: A new modality<br />
of wearable artificial kidney<br />
M.N. Aboras and I.A. Kawalit<br />
Saad Specialist Hospital, Al-Khobar, Kingdom of Saudi Arabia<br />
Abstract<br />
Wearable artificial kidney (WAK) has undergone clinical<br />
trials with results comparable to those of standard<br />
hemodialysis. Although they could have been excellent<br />
programs to rehabilitate End Stage Renal Disease (ESRD)<br />
patients and show them that despite their kidney problems,<br />
they could still enjoy the life. Unfortunately they were<br />
inconvenient due to different reasons, one of which includes<br />
the huge amount of hemofiltration and consequently the<br />
amount of replacement fluids. In this article will present our<br />
design of the WAK that theoretically intended to over come<br />
previous problems.<br />
Key words: hemodialysis, End Stage Renal Disease,<br />
wearable artificial kidney<br />
patients, the feasibility of using continuous hemofiltration in<br />
the regular design, as long-term dialysis program is very<br />
difficult. But the concept of continuous renal replacement<br />
therapy encouraged scientist to develop the wearable model<br />
of artificial kidney.<br />
Although “Wearable artificial kidneys” were intended to be<br />
excellent programs to rehabilitate renal patients and show<br />
them that despite their kidney problems, they could still enjoy<br />
the life. Unfortunately, they were inconvenient due to<br />
different reasons, such as the huge amount of hemofiltration<br />
and consequently the amount of replacement fluids, the<br />
volume of the design, the weight, the vascular access, and<br />
anticoagulation that made the realization of such a design not<br />
feasible.<br />
Diffusive versus Convective transport systems<br />
Introduction<br />
Dialysis as a practical treatment for kidney failure has<br />
evolved over centuries. Many have played a role in<br />
developing this medical technology, starting with Thomas<br />
Graham of Glasgow, who first presented the principles of<br />
solute transport across a semi permeable membrane in 1854<br />
(1). And since then continuous efforts were made to develop<br />
the ideal dialysis machine for patients with End Stage Renal<br />
Disease (ESRD) and while medical technology has made<br />
tremendous strides in treating kidney disease, quality of life<br />
issues and high mortality rates underscore the limitations of<br />
long-term dialysis.<br />
Intermittent Hemodialysis (HD) the most popular treatment<br />
for ESRD consumes about 12 to 15 hours weekly of the<br />
patient’s life during the dialysis sessions. Continuous<br />
Ambulatory Peritoneal Dialysis (CAPD) is a more<br />
convenient method but it needs special kind of intellectual<br />
and well-educated patients in order to reduce the frequency of<br />
peritonitis episodes. Haemofiltration has been developing<br />
during the last three decades as a possible alternative to the<br />
haemodialysis treatment.<br />
Recent clinical data comparing effective dose delivery by<br />
three acute dialysis therapies: continuous venovenous<br />
hemofiltration (CVVH), daily HD, and sustained lowefficiency<br />
dialysis (SLED), found that effective small solute<br />
clearance in CVVH is 8% and 60% higher than in SLED and<br />
daily HD, respectively. Differences were more pronounced<br />
for middle and large solute categories, the superior middle<br />
and large solute removal for CVVH is due to the powerful<br />
combination of convection and continuous operation (3, 4).<br />
Although it would seem an excellent program for ESRD<br />
______________________<br />
Correspodence to:<br />
Before going over our design we will give a brief description<br />
on the differences between diffusive transport and convective<br />
transport systems to help understand our design of the<br />
Wearable artificial kidney (5-8).<br />
Diffusive transport<br />
Diffusion is the physical phenomenon upon which the<br />
process of hemodialysis depends. It is driven by the<br />
concentration differences between blood and dialysate<br />
compartments and the solutes pass through the<br />
semiperemeable membrane and it is most efficient for the<br />
non-protein bound, low-molecular weight solutes.<br />
Convective transport<br />
In contrast, in the convective therapies, the solvents are<br />
eliminated by solvent drag, secondary to the removal of<br />
plasma water from the blood stream.<br />
Convective transport is more efficient for transport of middle<br />
and high molecular weight non-protein bound molecules,<br />
which can pass through the greater pores in the applied<br />
membranes.<br />
Of course, also the elimination of potentially toxic middle<br />
and high molecular weight molecules could be improved. At<br />
least this has been shown for β 2 micro globulin which might<br />
be involved in arthralgia, carpal tunnel syndrome, neuropathy<br />
and bone disease. Also other molecules, like for instance the<br />
advanced glycation end products (AGEs) (9,10), which<br />
recently have been shown to be associated with<br />
cardiovascular disease, might be eliminated in a more<br />
M.N. Aboras, Saad Specialist Hospital, Al-Khobar, Kingdom of Saudi Arabia
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 4<br />
efficient way, as well as inflammatory molecules like<br />
interleukins and endotoxins<br />
Continuous Convective Renal Replacement Therapy as a<br />
Wearable Artificial Kidney<br />
Haemofiltration, being superior to haemodialysis in its<br />
efficacy (5,10), could not be applied as an alternative for<br />
chronic renal failure treatment, due to the huge amounts of<br />
highly purified fluid and electrolytes replacement needed to<br />
be infused intravascularly. We present here our suggested<br />
innovation, which could overcome all the inconveniences of<br />
both haemodialysis and haemofiltration.<br />
Definition<br />
It is a continuous, portable, wearable and disposable renal<br />
replacement therapy system, depending on convective<br />
elimination of water and nitrogenous waist products, which<br />
can be used as a long-term treatment of end-stage renal<br />
failure.<br />
Description<br />
1. Vascular Access:<br />
Is a prerequisite for initiation of the therapy? The most<br />
convenient vascular access modality is Titanium<br />
subcutaneous catheters product of PakuMed® Medical<br />
products gmbh. Two ports are surgically inserted: one in the<br />
central venous system through the right internal jugular vein<br />
or the right subclavian vein, the other is installed in the<br />
arterial system through the right internal jugular or the right<br />
subclavian (innominate artery) Figure 1. (1)<br />
A third Titan Port catheter could optionally be implanted<br />
surgically opposite the suprapubic area, subcutaneously<br />
extending to inside of the urinary bladder.<br />
Fig 1. Graphic design illustrating the Continuous Convective Renal Replacement system<br />
Belt<br />
Arterial line<br />
Hollow fiber<br />
hemofilter<br />
Venous line<br />
Hemofiltrate<br />
collecting bag<br />
The Continuous Convective Renal Replacement system<br />
(Figure 1) is designed in the form of a tight jacket or belt to<br />
be worn by the patient. The material of the jacket can be any<br />
solid, light, leathery non-allergic substance or tissue water<br />
resistant. The jacket extends from the shoulders superiorly<br />
down to the hypogastrium inferiorly. The outside surface of<br />
the jacket is grooved for embedded bloodlines. Two sets of<br />
bloodlines are embedded. Another groove is prepared for the<br />
site of a small haemofilter. On the inside surface, there is two<br />
protruding needles gage 14 to 16, situated opposite the sites<br />
of the Titan Port. These needles are protected with plastic<br />
covers, to be removed at the time of wearing the jacket, and<br />
the needles will puncture the skin opposite the Titan Ports.<br />
In the blood line grooves, are embedded two sets of lines: a<br />
red coded set extending from the arterial needle to the arterial<br />
port of the haemofilter, while the blue coded set extends from<br />
the venous port of the haemofilter to the venous needle. A<br />
third wide bored needle (gage 14) protrudes from the lower<br />
end of the jacket opposite the vesicle Teten Port. This needle<br />
is connected to the ultrafiltration orifice of the haemofilter<br />
through a drainage line.<br />
The whole system of bloodlines, hemofilter and the needles<br />
are primed with heparinized sterile normal saline.<br />
2. The haemofilter:<br />
Is a hollow fiber, or parallel plate dialyser composed of a<br />
high flux, biocompatible membrane. The total surface area,<br />
the porosity, the membrane thickness and the length of the<br />
dialyser are to be calculated to give a rate of hemofiltration is<br />
about 250 ml/hour. Blood inlet and outlet are situated at both<br />
ends of the haemofilter, and a hemofiltrate drainage outlet is<br />
situated on the side of the haemofilter at the arterial end. It’s<br />
connected to either a urine bag or to the vesicle TITAN<br />
PORT.<br />
The whole system is completely sterile and packed in a sterile<br />
elegant package labeled with sufficient information and<br />
instructions about the system usage. A user manual is<br />
included inside the pack.<br />
The driving force of the extracorporeal circulation depends<br />
on the arterio-venous pressure gradient without the use of any<br />
sort of pump or any source of power.<br />
3. Replacement fluid:<br />
In this modality, the replacement fluid is to be given orally to<br />
the patient. Sachets containing salts, replacement materials,
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 4<br />
vitamins and sugar are to be prepared. Different formulae of<br />
these sachets are to be prepared according to the nature of the<br />
most common clinical presentations: e.g. those patients who<br />
are salt loosing or salt retaining, those who are usually<br />
acidotic should be given high alkali (sodium bicarbonate)<br />
content and so on.<br />
The patient is to be instructed to dissolve the contents of one<br />
or two sachets in an amount of water to be calculated by his<br />
physician according to the degree of water retention, the<br />
degree of dehydration or over hydration, and the degree of<br />
residual renal function etc…<br />
4. Anticoagulation:<br />
Could be achieved either by an oral anticoagulant<br />
(Coumadine) with adjustment of PT and INR; or low<br />
molecular weight heparin (Clexan) in a prophylactic 12<br />
hourly dose.<br />
Modified design<br />
This model is designed for patient who can’t tolerate large<br />
volume of replacement fluid. It has the same idea of a<br />
continuous, portable, disposable renal replacement therapy<br />
system, it depends on hemofiltration properties (convection)<br />
but, in addition, it has hemodialysis properties (diffusion) and<br />
better control of ultrafiltrate volume and consequently fluid<br />
replacement. This design is techniquely sophisticated.<br />
Description:<br />
The modified design (Figure 2) is divided into three filters;<br />
the first one is a high flux filter will refer to as dialyzer-1,<br />
second one is very low flux filter will refer to as V-filter and<br />
a third one is a low flux-high efficiency filter with dialysate<br />
compartment will refer to as dialyzer-2.<br />
Fig 2.<br />
Dialyzer-1 intended for the medium and large molecular<br />
weight solutes clearance and the V-Filter is used to<br />
ultrafiltrate the drainage from dialyzer-1 to decrease volume<br />
loss (fluid loss), and by doing so the filtrate blood from<br />
dialyzer-1 and the ultafiltrate from the V-Filter will pass to<br />
dialyzer-2 which has a high surface area and small to medium<br />
size pores. Dialyzer-2 has fluid, which act as dialysate fluid<br />
contains removable adsorbent cartilages around its casing bag<br />
to keep the fluid at continuous lower concentration of<br />
diffusible solutes.<br />
The filtrate drainage from the V-Filter, which contains a<br />
concentrated large molecular weight waist solutes with low<br />
volume, will be drained with the drained filtered of the<br />
Dilayzer-2 into a one-way valve urinal bag attached to the<br />
patient’s leg.<br />
In addition, the dialyzer-2 dialysate fluid casing will have a<br />
sensor for the most important diffusible solutes that will<br />
alarm or change in colour to notify the patients to change the<br />
adsorbent cartilage and/or exchange dialysate fluid. Our<br />
intention is to be once daily.<br />
References<br />
1. Graham T. The Bakeries lecture on osmotic force.<br />
Philosophical Transactions of the Royal Society in London.<br />
1854; 144: 177–228<br />
2. Ludger A, Graf H, Prager R et al. Continuous arteriovenous<br />
hemofiltration in the therapy of acute renal insufficiency. Wien<br />
Klin Wochenschr 1984; 6: 96(1): 1-4<br />
3. Liao Z, Zhang W, Hardy PA et al. Kinetic comparison of<br />
different acute dialysis therapies. Artif Organs 2003; 27 (9):<br />
802-7<br />
4. Graham T. The Bakerian lecture—on osmotic force. Philos<br />
Trans R Soc Lond 1854; 144:177–228<br />
5. Bland LA, Favero MS. Microbiologic aspects of hemodialysis<br />
systems. In AAMI Standards and Recommended Practices, vol.<br />
3. Arlington, VA: Association for the Advancement of Medical<br />
Instrumentation 1993; 257–265<br />
6. Daniels F, Alberty RA. Physical Chemistry. New York : John<br />
Wiley& Sons 1955.<br />
7. Gottschalk CW, Fellner SK. History of the science of dialysis.<br />
Am J Nephrol 1997; 17(3-4): 289-98<br />
8. Gerdemann A. Wagner Z, Solf A, et al. Plasma levels of<br />
advanced glycation end products during haemodialysis,<br />
haemodiafiltration and haemofiltration: potential importance of<br />
dialysate quality. Nephrol Dial Transplant 2002; 17(6): 1045-9<br />
9. Lin CL, Huang CC, Yu CC et al. Reduction of advanced<br />
glycation end product levels by on-line hemodiafiltration in<br />
long-term hemodialysis patients. Am J Kidney Dis 2003; 42(3):<br />
524<br />
10. Subramanian, Sanjay; Kellum, John A. Convection of diffusion<br />
in continuous renal replacement therapy for sepsis. Current<br />
Opinion in Critical Care 2000; 6(6): 426-430
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 6<br />
Prevalence of hepatitis C virus infection in dialysis patients<br />
P. Dzekova 1 , A. Slavkovska 2 , L. Simjanovska 2 , I. Nikolov 1 , A. Sikole 1 , R. Grozdanovski 1 , A. Asani 1 , G.<br />
Selim 1 , S. Gelev 1 , V. Amitov 1 , G. Spasovski 1 and M. Polenakovic 1<br />
1 Department of Nephrology, Clinical Center, Skopje, Republic of Macedonia<br />
2 Research Center for genetic engineering and biotechnology, Macedonian Academy of Sciences and Arts, Skopje,<br />
Republic of Macedonia<br />
Abstract<br />
Hemodialysis patients are at particularly high risk for<br />
hepatitis C virus infection because of the exposure to blood<br />
products and contaminated equipment. The high prevalence<br />
of HCV infection in dialysis patients is of great concern<br />
because these patients have a higher mortality than HCV<br />
negative patients.<br />
Our study aimed to evaluate the prevalence of HCV infection<br />
among patients at our dialysis unit.<br />
A cohort of 178 patients on maintenance hemodialysis at the<br />
Department of Nephrology, Clinical Center Skopje, was<br />
retrospectively evaluated for the levels of transaminases and<br />
the number of transfused blood products. The presence of<br />
HCV antibodies was determined by second-generation assay<br />
and the presence or absence of HCV RNA in the serum of the<br />
patients was determined by reverse-transcriptase PCR.<br />
The results from this study showed that from 178 patients,<br />
114 (64%) were anti-HCV positive and 64 (36%) were anti-<br />
HCV negative. The duration of dialysis, transaminase levels<br />
and number of transfusions was significantly higher in anti-<br />
HCV positive group of patients when compared with the anti-<br />
HCV negative group.<br />
The high prevalence of anti-HCV positive patients in our<br />
dialysis unit was associated with greater dialysis duration,<br />
blood products transfusions and liver enzyme levels.<br />
Measures to prevent the spread of HCV in dialysis units<br />
should include isolation of HCV RNA positive patients<br />
equipment and possibly their treatment with interferon<br />
therapy.<br />
Key words: hepatitis C virus, prevalence, dialysis patients<br />
Introduction<br />
Hemodialysis patients are at particularly high risk for<br />
hepatitis C (HCV) virus infection because of the exposure to<br />
blood products and contaminated equipment. There is<br />
considerable variation in the prevalence of anti-HCV in<br />
dialysis units worldwide, ranging from as low as 1% to as<br />
high as 63%. Risk factors for spread include a history of<br />
transfusion, number of blood products transfused, and<br />
number of years on hemodialysis therapy (1). The high<br />
prevalence of HCV infection in dialysis patients is of great<br />
concern because these patients have a higher mortality than<br />
HCV negative patients (2). Although HCV transmission<br />
through blood products transfusion previously was a<br />
significant source of infection, current cases are more likely<br />
related to nosocomial exposure (3). Hepatitis C virus is<br />
characterized by spectrum of outcomes. Asymptomatic in the<br />
vast majority of patients, transition from acute to chronic<br />
infection is usually without notice (4,5). In addition to viral<br />
and environmental factors, host genetic and immunological<br />
factors are believed to exert an impact on outcome of HCV<br />
infection (6). The mechanisms involved in viral clearance are<br />
not yet fully understood, although increasing evidence<br />
suggests that cellular immune responses to HCV play a<br />
central role (7). The aim of this study was to evaluate the<br />
prevalence of HCV infection among patients at our dialysis<br />
unit.<br />
Patients and Methods<br />
The study was carried on 178 (113 men) patients on<br />
maintenance hemodialysis at the Department of Nephrology,<br />
Clinical Center, Skopje. The mean age of patients was 54.8<br />
years and mean time on dialysis 86 months. The levels of<br />
liver aminotransferase enzymes: alanine aminotransferase<br />
(ALT) and aspartate aminotransferase (AST), and the number<br />
of transfused blood products, were recorded from the<br />
histories of the patients. The presence of HCV antibodies was<br />
determined by second-generation assay. The presence or<br />
absence of HCV RNA in the serum of the patients was<br />
determined by reverse-transcriptase PCR (RT/PCR) at<br />
Research Center for genetic engineering and biotechnology,<br />
Macedonian Academy of Sciences and Arts, Skopje.<br />
Student’s t-test was used for group mean comparison<br />
between anti-HCV positive and anti-HCV negative patients.<br />
Results<br />
Fig 1. Distribution of anti-HCV positive and anti-HCV<br />
negative patients in the study<br />
anti-HCV -<br />
64(36%)<br />
anti-HCV + anti-HCV -<br />
anti-HCV +<br />
114 (64%)<br />
The results from this study showed that from 178 patients,<br />
114 (64%) were anti-HCV positive and 64 (36%) were anti-<br />
______________________<br />
Correspodence to: P. Dzekova, Department of Nephrology, Clinical Center Skopje, Medical Faculty,<br />
University "Sts. Cyril and Methodius", Republic of Macedonia
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 7<br />
HCV negative (Figure.1).<br />
The mean values of age, duration on dialysis, levels of AST<br />
and ALT, and number of transfusions in anti-HCV positive<br />
and anti-HCV negative patients, and comparison between<br />
them are given in Table 1.<br />
Table 1. Mean values of age, duration on dialysis, levels of AST and ALT, and number of transfusions, and<br />
comparison between anti-HCV positive and anti-HCV negative patients<br />
anti-HCV positive anti-HCV negative p value<br />
age (years) 53.81 ± 13.61 56.62 ± 12.06 NS<br />
duration (months) 103.7 ± 71.6 53.41 ±33.7 0.00<br />
AST (U/L) 37.87 ± 21.96 23.05 ±11.63 0.00<br />
ALT (U/L) 53.74 ± 34.71 25.06 ± 14.05 0.00<br />
No. of transfusions 8.91 ± 13.53 4.84 ± 5.27 0.03<br />
The duration of dialysis in months was significantly longer in<br />
anti-HCV positive than in anti-HCV negative patients (103<br />
vs. 53, p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 8<br />
Influence of inflammation on nutritional status of dialysis patients<br />
P. Dzekova, I. Nikolov, G. Severova-Andreevska, A. Sikole, R. Grozdanovski, A. Asani, G. Selim,<br />
S. Gelev, V. Amitov, G. Spasovski and M. Polenakovic<br />
Department of Nephrology, Clinical Center Skopje, Medical Faculty, University Sts Cyril and Methodius, Republic of Macedonia<br />
Abstract<br />
Malnutrition and inflammation are frequently observed in<br />
maintenance hemodialysis patients as risk factors for poor<br />
quality of life and increased morbidity and mortality. The<br />
causes and consequences of both are anorexia,<br />
hypoalbuminemia, muscle wasting, refractory anemia, and,<br />
possibly accelerated arteriosclerosis.<br />
The aim of our study was to evaluate the influence of<br />
inflammation on parameters of nutritional status dialysis<br />
patients at the Department of Nephrology, Clinical Center<br />
Skopje.<br />
We crossectionally analysed 154 dialysis patients (93 men)<br />
which were then followed in a period of six consecutive<br />
months. A number of biochemical and anthropometrical<br />
parameters were evaluated as measures of nutritional status.<br />
The mean (±SD) age of all patients was 54.8 ± 12.7 years and<br />
vintage (duration of dialysis therapy) from 7 to 288 months.<br />
CRP and serum albumin levels were significantly greater in<br />
men than in women (12.9 vs. 7.97, p < 0.04 and 40.2 vs. 38.8,<br />
p < 0.02, respectively). Triceps skin fold, mid arm<br />
circumference and body mass index measurements were<br />
statistically greater in women than in men (p < 0.01). CRP<br />
level strongly correlated only with serum concentration of<br />
cholesterol (r =0.49, p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): p 9<br />
Results<br />
Our results showed that CRP level was significantly greater<br />
in men than in women (12.9 vs. 7.97, p < 0.04). Serum<br />
albumin level was significantly greater in men than in women<br />
(40.2 vs. 38.8, p < 0.02). Serum cholesterol level tended to be<br />
greater in men than in women (p=NS). Triceps skin fold<br />
measurements were statistically greater in women than in<br />
men (1.37 vs. 0.96, p < 0.001). Mid arm circumference and<br />
body mass index were greater in women, whereas mid arm<br />
muscle circumference was greater in men, but not statistically<br />
(Table 1).<br />
Table 1. Laboratory and anthropometrical data, and a comparison<br />
between men and women<br />
men women p<<br />
No. of patients 93 61<br />
CRP (mg/l) 12.9 ±16.9 7.97 ± 10.9 0.04<br />
albumin (g/l) 40.2 ±4.0 38.8 ± 3.7 0.02<br />
cholesterol<br />
(mmol/L) 3.7 ± 1.4 3.2 ± 1.5 NS<br />
TSF (cm) 0.96 ±0.3 1.37 ± 0.6 0.0001<br />
MAC (cm) 26.3 ± 2.7 27.3 ± 4.4 NS<br />
MAMC (cm) 23.27 ± 3.1 23.03 ± 3.5 NS<br />
BMI (kg/m2) 23.03 ± 3.2 23.7 ± 4.7 NS<br />
CRP level showed strong correlation only with serum<br />
concentration of cholesterol (r =0.49, p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): p 10<br />
Unfavorable prognostic factors in Immunoglobulin A Nephropathy<br />
L. Petrovic, S. Curic, I. Mitic, D. Bozic, S. Vodopivec, V. Sakac, T. Djurdjevic-Mirkovic and T. Ilic<br />
Clinical Centar Novi Sad, Clinic for Nephrology and Clinical Immunology, Novi Sad, Serbia and Montenegro<br />
Abstract<br />
Immunoglobulin A nephropathy (IgAN) is a<br />
clinicopathological entity characterized by diffuse glomerular<br />
mesangial deposition of IgA as the predominant<br />
immunoglobulin. Renal biopsy reveals a spectrum of changes<br />
in the glomerul, tubulointerstitium and blood vessels. 20-50%<br />
of all patients develope end-stage renal failure 20 years after<br />
onset of the disease.<br />
The aim of this stady was to analized influence of<br />
clinicopathological and laboratory changes to prognosis of<br />
IgAN. The study included 60 patients with biopsy-proven<br />
IgAN without some other systemic diseases or purpura<br />
Henoch-Schnlein. We analized influence of clinical features<br />
of the disease, laboratory and immunofluorescence/light<br />
microscopy findings on the prognosis of IgAN. The study<br />
was partly retrospective and partly prospective. At the<br />
moment of renal biopsy 63,16% of patients had normal renal<br />
function, 31,58% had stage I and 5,25% had stage II chronic<br />
renal failure. At the end of study 21,05% of investigated<br />
patients progressed to a worse stage of renal failure with<br />
regard to the initial stage.<br />
In this study we found severe histopathological changes in<br />
the group with already impaired renal function and these<br />
changes correlated with laboratory findings, clinical features<br />
and prognosis of the disease. Normal renal function at the<br />
moment of renal biopsy provides smaller risk of further<br />
damage. Changes in the tubulointerstitium, mesangium,<br />
heavy proteinuria and hypertension influence to worse<br />
prognosis of disease. Crossing to the higher stage of renal<br />
failure was 1,24% per year and this requires long-term<br />
follow-up of patients with IgAN.<br />
Key words: IgA nephropathy, renal biopsy, outcome<br />
Introduction<br />
Immunoglobulin A nephropathy (IgAN), immunoglobulin A<br />
glomerulonephritis (IgAGN) or Berger’s disease is a special<br />
clinical/pathological entity which is characterized by the<br />
finding of immunofluorescent microscopy with predominant<br />
IgA deposits in mesangium of the glomerul.<br />
Morphological characteristics of the nephrotic damages in<br />
IgAN, similarly to clinical manifestation of the disease, are of<br />
a different form and degree of attack on glomerul, tubule,<br />
interstitium and blood vessels. Clinical progress of the<br />
disease is in correlation with histopathological changes with<br />
existence of significant clinical/pathological correlation with<br />
disease prognosis (1,2). Clinical and histopathological<br />
indicators (present at the moment of diagnosis) of the<br />
unfavorable disease prognosis are: 1) older age, 2) male sex,<br />
3) absence of episodes of macrohematuria, 4) lower intensity<br />
value of glomerular filtration (IGF), 5) heavier proteinuria<br />
(>1000mg/24h) or proteinuria of nephrotic rank, 6) arterial<br />
hypertension, 7) more pronounced histopathological changes,<br />
8) intensive IgA and C3 immunofluorescent deposits in<br />
glomerul and capillary wall, commonly associated with IgG<br />
deposits and fibrinogen are also considered to be the markers<br />
of unfavorable prognosis, 9) as the independent factors of the<br />
unfavorable disease prognosis, one can account for diabetes<br />
mellitus, hypertriglyceridemia, hyperuricemia, period of<br />
disease duration, positive family history (3-8).<br />
IgA nephropathy was firstly called benign recurrent<br />
hematuria, however, a long-term follow-up of the renal<br />
function has shown that IgAN represents a slow, progressive<br />
illness of a different result which includes a high incidence of<br />
progressive damage of renal function with development of<br />
terminal nephritic insufficiency in 20-50% of the diseased, 20<br />
years after the beginning of the disease. The research has<br />
shown that the damage of the renal function is developed<br />
faster in patients with an initial impairment of renal function,<br />
in contrast to patients with relatively normal renal function at<br />
diagnosis (4,6). The most significant prognostic factors in<br />
IgA nephropathy are histopathological changes, so that the<br />
expressed mesangial proliferation, glomerulosclerosis,<br />
presence of crescent formations, arteriosclerosis, interstitial<br />
fibrosis represent histological markers of unfavorable<br />
prognosis. Glomerulosclerosis, focal-segmented and<br />
especially diffuse, influence renal function substantially more<br />
intensively than the proliferative changes. Tubulointerstitial<br />
infiltrate, especially T cellular (CD4+, CD8+) is in<br />
correlation with faster progression of the disease. Interstitial<br />
fibrosis, regardless of simultaneous presence or absence of<br />
glomerulosclerosis, is also a significant prognostic factor.<br />
This explains different rate of renal function damaging in<br />
patients with the same level of glomerular damage, but<br />
different considering the tubulointerstitial inflammatory<br />
infiltrate or sclerosis (1,3,6,9,10).<br />
The aim of this study was to analyze the influence of clinicalpathological<br />
and laboratory changes on prognosis of IgAN.<br />
Considering the possibility of development and progression<br />
of chronic renal insufficiency, the justification of longer<br />
follow-up of the diseased was reviewed.<br />
Patients and methods<br />
Testing covered 60 patients, who had percutaneous renal<br />
biopsy at the Clinic of Nephrology and Clinical Immunology<br />
of Clinical Center Novi Sad. The tested patients had<br />
documentation which consisted of at least, the first control<br />
______________________<br />
Correspodence to: L. Petrovic, Clinical Centar Novi Sad, Clinic for Nephrology and Clinical Immunology,<br />
Novi Sad, Serbia and Montenegro
<strong>BANTAO</strong> <strong>Journal</strong>2006: 4 (1): p 11<br />
examination, i.e. they were followed-up for at least one<br />
month up to maximum 17 years. Criterion for inclusion into<br />
the study was the finding of IgA deposits, as a dominant<br />
immunoglobulin in the mesangium of glomerul, which was<br />
deduced by immunofluorescent microscopy, while the<br />
presence of Henoch-Schonlein purpura and some other<br />
systematic illness were excluded.<br />
Immunohistological technique included the application of<br />
standard antiserums: anti-IgA, -IgG, -IgM, -C3, -C4, -C1q, -<br />
fibrin. The intensity of positive immunofluorescent finding<br />
was estimated semi-quantitatively with a precise localization<br />
of the deposits.<br />
Results<br />
Patients’ age ranged from 14-56 years, with an average of<br />
34.19 years. From the cohort of 60 patients, 70% were of<br />
male sex, while 30% of them were female.<br />
At the moment of renal biopsy, i.e. the diagnostics of the<br />
disease, 36 patients (63.16%) had a normal renal function<br />
(creatinine < 107 mol/l, clearance creatinine > 90<br />
ml/min/m 2 ), 18 patients (31.58%) were in stadium I of renal<br />
insufficiency (creatinine < 133 mol/l, clearance of creatinine<br />
60-90 ml/min/m 2 ) and 3 patients (5.26%) were in stadium II<br />
of renal insufficiency (creatinine 133-440 mol/L, clearance<br />
of creatinine 10-60 ml/min/m 2 ). Out of 36 patients, who at<br />
the moment of diagnostics had normal renal function, 31<br />
patient (86,11%) preserved the renal function until the end of<br />
the follow-up, 5 patients (13,89%) moved to stadium I of<br />
renal insufficiency. 12 patients (66.67%) from the group of<br />
18 patients with initial stadium I of renal insufficiency<br />
remained in this stadium, while 6 patients (33.33%) moved to<br />
stadium II. 2 patients (66.67%) from the group of 3 patients<br />
with initial stadium II remained in this stadium, while 1<br />
patient (33.37%) moved to stadium III.<br />
If we observe the total number of patients who moved from<br />
one stadium of renal insufficiency to another (0I, III,<br />
IIIII), their total number was 12 (21.05%) for the follow-up<br />
period of 17 years, i.e. 1.24% of patients annually moved to a<br />
higher stadium in relation to the initial renal function (Table<br />
1).<br />
Table 1. Relationship between beginning and end stage renal failure<br />
Beginning<br />
stage<br />
Normal<br />
function<br />
Number<br />
Percent<br />
36 63,16 %<br />
Stage of renal function at the<br />
end of the study<br />
Number<br />
Percent<br />
Normal function 31 86,11%<br />
I stage of renal failure 5 13,89%<br />
I stage of<br />
renal<br />
failure<br />
II stage of<br />
renal<br />
failure<br />
18 31,58 %<br />
3 5,26 %<br />
I stage of renal failure 12 16,67%<br />
II stage of renal failure 6 33,33%<br />
II stage of renal failure 2 66,67%<br />
III stage of renal failure 1 33,37%<br />
57 100 % 57 100%<br />
Within the group of patients with normal initial renal<br />
function, the existence of positive correlation was identified<br />
among: 1) changes in mesangium and increase of creatinine<br />
concentration, 2) changes in mesangium and appearance of<br />
microhematuria in clinical manifestation of the disease, 3)<br />
glomerulosclerosis and higher values of systolic blood<br />
pressure, 4) crescent formations and severity of proteinuria<br />
(Table 2).<br />
Table 2. Positive correlation between pathological findings with<br />
clinical features and laboratory parameters in the group of patients<br />
with normal renal function at the beginning<br />
Pathological<br />
Degree of<br />
Laboratory findings<br />
findings<br />
correlation<br />
Creatinine concentraction<br />
Mesangium increase<br />
r=0,47<br />
Microhematuria<br />
r=0,35<br />
Glomerulosclerosis Systolic blood presure r=0,21<br />
Crescent Proteinuria r=0,24<br />
The conclusions of the testing of patients with the initial<br />
stadium I renal insufficiency are the following: 1) there is an<br />
easy connection of changes in mesangium with the increase<br />
of creatinine concentration, higher values of systolic and<br />
diastolic blood pressure, 2) there is a significant correlation<br />
of glomerulosclerosis with microhematuria and heavier<br />
proteinuria, 3) there is an easy correlation between the<br />
presence of crescent formations and heavier proteinuria, 4)<br />
the changes in interstitium are in correlation with systolic,<br />
diastolic blood pressure and heavier proteinuria, 5) the<br />
changes in tubule are in easy correlation with a heavier<br />
proteinuria and the appearance of microhematuria (Table 3).<br />
Table 3. Positive correlation between pathological findings with<br />
clinical features and laboratory parameters in the group of patients<br />
with Ist stage of renal failure<br />
Pathological<br />
findings<br />
Laboratory findings<br />
Degree of<br />
correlation<br />
Creatinine concentration<br />
increase<br />
r=0,30<br />
Mesangium Systolic blood pressure r=0,37<br />
Diastolic blood pressure r=0,31<br />
Glomerulosclerosis Proteinuria r=0,35<br />
Microhematuria<br />
r=0,66<br />
Crescent Proteinuria r=0,35<br />
Proteinuria<br />
r=0,71<br />
Intestitium Systolic blood pressure r=0,39<br />
Diastolic blood pressure r=0,35<br />
Tubulus<br />
Proteinuria<br />
r=0,33<br />
Microhematuria<br />
r=0,25
<strong>BANTAO</strong> <strong>Journal</strong>2006: 4 (1): p 12<br />
Conclusions<br />
In this study, we found severe histopathological changes in<br />
the group with already impaired renal function and these<br />
changes correlated with laboratory findings, clinical features<br />
and prognosis of disease. Normal renal function at the<br />
moment of renal biopsy provides smaller risk of further<br />
damage. Changes in the tubulointerstitium, mesangium,<br />
heavy proteinuria and hypertension influence the worsening<br />
of prognosis of the disease. Crossing to the higher stage of<br />
renal failure was 1.24% per year and this requires a long-term<br />
follow-up of patients with IgAN.<br />
References<br />
1. Amico GD. Natural history of idiopathic IgA nephropathy: role<br />
of clinical and histological prognostic factors. Am J Kidney Dis<br />
2000; 36 (2): 227-37<br />
2. Droz D. IgA nephropathy: clinicopathologic correlations. In:<br />
Clarkson A. IgA Nephropathy. Martinus Nijhoff Publishing,<br />
Boston 1987; 97-101<br />
3. Wyatt RJ, Kritchevsky SB, Woodford SY et al. IgA<br />
nephropathy: long-term prognosis for pediatric patients. J<br />
Pediatr 1995; 127 (6): 913-919<br />
4. Ibels LS, Gyory AZ. IgAN: analysis of the natural history,<br />
important factors in the progression of of renal disease, and<br />
review of the literature. Medicine-Baltimore 1994; 73(2): 79-<br />
102<br />
5. Droz D. IgA nephropathy: clinicopathologic correlations. In:<br />
Clarkson A. IgA Nephropathy. Martinus Nijhoff Publishing,<br />
Boston, 1987; 101-102<br />
6. Donadio JV, Bergstra EJ, KP. Offord et al. Clinical and<br />
histopathologic associations with impaired renal function in<br />
IgAN. Clin Nephrol 1994; 41(2): 65-71<br />
7. Kenji W, Shigene N, Seicli M et al. Risk Factors for IgA<br />
Nephropathy: A Case-Control Study with Incident Cases in<br />
Japan. Nephron 2002; 90(1): 16-23<br />
8. Mustonen J, Syrjanen J, Rantala I et al. A. Clinical course and<br />
treatment of IgA nephropathy. J Nephrol 2001; 14: 440-446<br />
9. Alexopoulos E, Papaghianni A, Papadimitriou M. The<br />
pathogenetic significance of C5b-9 in IgA nephropathy.<br />
Nephrol Dial Transplant 1995; 10(7): 1166-72<br />
10. Daniel L, Saingra Y, Giorgi R et al. Tubular lesions determine<br />
prognosis of IgA nephropathy. Am J Kidney Dis 2000; 35(1):<br />
13-20
<strong>BANTAO</strong> <strong>Journal</strong>2006: 4 (1): p 13<br />
Congestive heart failure and renal dysfunction<br />
D. Monova 1 , E. Peneva 1 and S. Monov 2<br />
Department of Internal Diseases, Medical Institute 1 – MIA, Medical University 2 , Sofia, Bulgaria<br />
Abstract<br />
The kidney plays a key role in the homeostatic maintenance<br />
of fluids and electrolytes in the context of chronic congestive<br />
heart failure (CHF). CHF carries a spectrum of<br />
pathophysiological aberrations, which constitute a stress on<br />
the respective renal regulatory mechanisms.<br />
We defined bedside clinical, laboratory and<br />
electrocardiographic parameters characterizing CHF patients<br />
with and without concomitant renal failure (RF), and<br />
analyzed their impact on mortality. We studied 146<br />
symptomatic unselected consecutive furosemide-treated CHF<br />
patients hospitalized for various acute conditions. On<br />
admission, history taking, physical examination, chest x-ray,<br />
ECG and routine laboratory tests were performed.<br />
Subsequently, patients were divided into 2 subgroups, those<br />
with serum creatinine > 140 µmol/l (58) and those with<br />
lower values (88). Prevailing in RF subgroup were older age,<br />
male gender, admission pulmonary edema, cardiac<br />
arrhythmias, cardiac condition disturbances, lower ejection<br />
fraction, anemia, higher furosemide maintenance dosages,<br />
insulin treatment and receiving less ACE inhibitors. RF being<br />
the parameter most significantly associated with low survival.<br />
Using multivariate analysis in the RF subgroup, older age,<br />
female gender and diabetes mellitus proved most<br />
significantly associated with poorer survival. In the non-RF<br />
subgroup, only older age and diabetes mellitus were<br />
significantly associated with low survival.<br />
Renal failure is a marker of severity in CHF. Its full-blown<br />
deleterious prognostic effect is already manifested at serum<br />
creatinine 140 µmol/l. Older age, diabetes mellitus and<br />
female gender significantly heralded a shorter survival. Such<br />
patients require special care.<br />
Key words: congestive heart failure, renal failure, diabetes<br />
mellitus, gender, age<br />
Introduction<br />
The kidney plays a key role in the homeostatic maintenance<br />
of fluids and electrolytes in the context of chronic congestive<br />
heart failure (CHF)(1). CHF carries a spectrum of<br />
pathophysiological aberrations, which constitute a stress on<br />
the respective renal regulatory mechanisms. It has been<br />
shown that the presence of renal failure in patients with<br />
congestive heart failure is associated with shorter survival (2-<br />
4). Moreover, renal failure, even moderate, represents not<br />
only a marker for poor prognosis, but also an independent<br />
risk factor for increased mortality (3).<br />
We defined bedside clinical, laboratory and<br />
electrocardiographic parameters, characterizing CHF patients<br />
with and without concomitant renal failure (RF), and<br />
analyzed their impact on mortality.<br />
Patients and methods<br />
We studied 146 symptomatic unselected furosemide-treated<br />
patients with congestive heart failure, hospitalized for various<br />
acute conditions. Congestive heart failure was of various<br />
etiologies and had been present for at least 6 months prior to<br />
admission. All patients had been on chronic furosemide<br />
treatments of at least 40 mg/day for more than 3 months.<br />
On admission, blood was drawn for serum biochemical<br />
determinations, including glucose, creatinine, chloride,<br />
potassium, sodium, bicarbonate, blood pH, calcium,<br />
phosphorus, cholesterol, triglycerides and blood count. All<br />
determinations were performed using conventional methods.<br />
The history taking, physical examination, chest x-ray and<br />
ECG were performed. Subsequently, patients were divided<br />
into 2 subgroups, those with serum creatinine > 140 µmol/l<br />
(58 patients) and those with lower values (88 patients).<br />
Results and discussion<br />
The study group included 146 patients (84 females and 62<br />
males, mean (±SD) age 71,4±19,6 years). Renal failure was<br />
present in 58 (39,73%) patients. Table 1 depicts the mean<br />
values of quantitative variables in the patients with renal<br />
failure as compared to those with normal creatinine values.<br />
Table 1. Mean values of quantitative variables in congestive heart<br />
failure patients with versus without renal failure<br />
Characteristic<br />
Patients with Patients without<br />
renal failure renal failure<br />
Weight (kg) 68,7±12,4 70,4±13,6<br />
Age (years) 65,4±6,4 60,3±8,3<br />
Serum potassium 4,71±0,82 4,5±0,52<br />
(mmol/l)<br />
Serum bicarbonate 24,4±4,22 26,24±3,96<br />
(mmol/l)<br />
Serum chloride<br />
104,0±5,4 102,88±4,6<br />
(mmol/l)<br />
Serum phosphorous 3,8±0,8 3,5±0,5<br />
(mmol/l)<br />
Blood pH 7,37±0,06 7,39±0,05<br />
It can be seen that patients with renal failure were<br />
significantly older (P
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): p 14<br />
Table 2. Qualitative variables prevailing in congestive heart failure<br />
patients with versus without renal failure<br />
Characteristic<br />
Patients with<br />
renal failure<br />
- N(%)<br />
Patients<br />
without renal<br />
failure – N(%)<br />
Male gender 37 (63,79%) 25 (28,41%)<br />
Pulmonary edema on<br />
admission<br />
36 (62,07%) 29 (32,95%)<br />
Cardiac arrhythmias on<br />
34 (58,62%) 28 (31,82%)<br />
admission<br />
NYHA class III-IV 35 (60,34%) 31 (35,23%)<br />
Ejection fraction < 30% 25 (43,10%) 15 (17,04%)<br />
Presence of anaemia 30 (51,72%) 20 (22,73%)<br />
Furosemide dosage>80mg 20 (34,48%) 10 (11,36%)<br />
Treatment with ACE<br />
inhibitors<br />
28 (48,28%) 59 (67,04%)<br />
Male gender, admission pulmonary edema, cardiac<br />
arrhythmias (atrial or ventricular premature beats >6 min,<br />
couplets, atrial fibrillation, supraventricular or ventricular<br />
tachycardia), severe CHF, lower ejection fraction, anemia,<br />
higher furosemide maintenance dosages and receiving less<br />
ACE inhibitors prevailed in the subgroup with renal failure.<br />
Duration of furosemide treatment, presence of hypertension,<br />
periferal vascular disease, ischemic heart disease, chronic<br />
obstructive pulmonary disease, hypokalemia or hyponatremia<br />
on admission, treatment with calcium channel blockers,<br />
nitrates or digoxin, were not significantly different between<br />
the two subgroups.<br />
The follow-up period extended up to 40 months, median<br />
34±12 months. During this period 24 (16,44%) patients died.<br />
17 patients (70,83%) were from subgroup with renal failure.<br />
Renal failure was the parameter most significantly associated<br />
with low survival. Using multivariate analysis in the<br />
subgroup with renal failure, older age, severity of CHF,<br />
female gender proved to be significantly associated with<br />
poorer survival. In the subgroup without renal failure, only<br />
older age was significantly associated with low survival.<br />
Parameters which did not influence survival in the subgroup<br />
with renal failure, included duration of furosemide treatment,<br />
hypertension, hyperlipidemia, anaemia, various cardiac<br />
arrhythmias, use of vasodilators or digoxin and hypokalemia<br />
or hyponatremia on admission.<br />
The pathophysiological interrelationship between CHF and<br />
renal insufficiency is bidirectional, involving a variety of<br />
factors (1). Activation of the neurohormonal and reninangiotensin<br />
systems, mainly via reduction of effective blood<br />
volume in CHF leads to stimulation of aldosterone and ADH<br />
secretion. These may produce a rise in cardiac filling<br />
pressure, increased extracelular volume, edema and organ<br />
dysfunction, including deterioration of CHF. Within the<br />
context of the kidney, intravascular volume depletion and the<br />
ensuing GFR reduction, eventually limit natriuresis and<br />
diuretic capacity despite enhanced nitric oxide production<br />
and activation of natriuretic substances. Superposition of<br />
renal failure on CHF implies an additional burden of poor<br />
prognostic factors. These may include various electrolite and<br />
acid-base balance aberrations, decreased immunological<br />
competence, osteoporosis, enhanced bleeding tendency and<br />
other factors, which may shorten survival from cardiac and<br />
non-cardiac death (5).<br />
Conclusions<br />
Renal failure is a marker of severity in CHF. Its full-blown<br />
deleterious prognostic effect is already manifested at serum<br />
creatinine of 140 µmol/l. Older age and a female gender<br />
significantly heralded a shorter survival. We were unable to<br />
find such association in the literature (3). Such patients<br />
require special care. Following discharge, patients were<br />
managed exclusively by their primary physicians. Therefore<br />
our results are not biased by other factors such as those<br />
introduced by pharmaceutically oriented studies or those<br />
involving intervention by specialized heart failure clinics.<br />
References<br />
1. Zanchetti, A and Stella A. Cardiovascular disease and the<br />
kidney: an epidemiologic overview. – J Cardiovasc. Pharmacol<br />
1999; 33, 1-6<br />
2. Al-Ahmad, Rand WM, Manjundth G et al. Reduced kidney<br />
function and anemia as risk factors for mortality in patients<br />
with left ventricular dysfunction. – J Am Coll Cardiol 2001;<br />
38: 955-962<br />
3. Dries DL, Exner DV, Domanski MJ et al. The prognostic<br />
implications of renal insufficiency in asymptomatic and<br />
symptomatic patients with left ventricular systolic dysfunction.<br />
– J Am Coll Cardiol 2000; 35: 681-689<br />
4. Mosterd A, Cast B, Hoes AW et al. The prognosis of heart<br />
failure in the general population: The Rotterdam Study - Eur<br />
Heart J 2001; 22: 1318-1327<br />
5. Muntner P, Hamm L, Lorid C et al. Renal insufficiency and<br />
subsequent death resulting from cardiovascular disease in the<br />
United States. – J Am Soc Nephrol 2002; 13: 745-75
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): p 15<br />
Sporadic Balkan Endemic Nephropathy (BEN) beyond the known regions of<br />
BEN<br />
J. Nikolic¹, T. Pejcic¹, D. Crnomarkovic¹, Z. Gavrilovic² and C. Tulic¹<br />
¹Urologic Clinic-Faculty of Medicine Belgrade, ² Institute for developement of water resources, Jaroslav Cerni,<br />
Belgrade, Serbia and Montenegro<br />
Abstract<br />
There is an very old opinion that we diagnose only most<br />
prominent BEN cases and miss latent and mild ones, that<br />
unrecognized BEN is possible in endemic villages and the<br />
number of such cases, their characteristics, and origin are<br />
unknown.<br />
From 1955 to 1998 year we evaluated 1235 patients with<br />
histologicaly proven upper urothelial tumors, who underwent<br />
surgery. The diagnosis of sporadic BEN, was made after<br />
exclusion of other known nephropaties.<br />
In the analyzed region, BEN was present in 170 of 808<br />
settlements, and in 104 of them, 534 cases of UUT were<br />
reported. In 66 possible BEN settlements, there were no UUT<br />
cases. In the next 457 of 808 settlements (56.6%) neither<br />
BEN, or UUT were registered.<br />
Sporadic BEN is an atypical, mild clinical variety of BEN,<br />
with simultaneous presence of UUT. Both sexes were equally<br />
affected, with the majority of patients in sixth and seventh<br />
decade of. The presence of sporadic BEN cases gives a<br />
possibility to speculate that the existence of BEN without<br />
familiar agreggations is possible elsevere, not only in<br />
Balkans.<br />
Key words: Balkan Endemic Nephropathy, familiar<br />
agreggations, distribution<br />
Introduction<br />
The idea of »ice berg phenomenon«, (1,2) suggesting that we<br />
diagnose only most prominent BEN cases and miss latent and<br />
mild ones, is very old. There is a similar opinion, that<br />
unrecognized BEN is possible in endemic villages (in<br />
»healthy« famillies), and in the neighborhood of BEN areas,<br />
(3) but the number of such cases, their characteristics, and<br />
origin are unknown. Territorial distribution of cases with<br />
upper urothelial tumors (UUT) in Serbia is much wider than<br />
distribution of BEN (4, 5), suggesting the similar distribution<br />
of BEN.<br />
The diagnosis of sporadic BEN , presented as non-famillar,<br />
non-endemic disease (6), is hardly possible with standard<br />
criteria, because two main criteria for the diagnosis are<br />
missing.<br />
Patients and methods<br />
urologists and patients from Serbia came from the region of<br />
31 communities with 808 settlements, with total of 1.162.225<br />
inhabitants (5).<br />
The diagnosis of sporadic BEN, was made in patients that<br />
underwent surgery because of UUT, after exclusion of other<br />
known nephropaties. The presence of UUT in all such cases,<br />
enables the diagnosis, knowing that other nephropaties<br />
followed by UUT (CHN, AN etc.) are extremely rare in<br />
Serbia. The data source of territorial distribution of BEN, was<br />
standard one (7).<br />
Non-endemic villages with sporadic BEN cases were divided<br />
into three groups, according to the number of cases (more<br />
than 3, 2, or 1 case) in settlement, during four decades of<br />
observation. The first group of settlements with sporadic<br />
BEN (≥ 3 cases) from non-endemic settlements is shown on<br />
the map, compared to 104 villages from BEN register, with<br />
simultaneous UUT presence.<br />
Results<br />
In the analyzed region, BEN was present in 170 of 808<br />
settlements (7), and in 104 of them, 534 cases of UUT were<br />
reported. In 66 possible BEN settlements, there were no UUT<br />
cases. In the next 457 of 808 settlements (56.6% ) neither<br />
BEN, or UUT were registered (Table 1).<br />
Table 1. The presence of BEN and the number of UUT in the<br />
analyzed region villages, according to BEN register (1955- 1998<br />
year)<br />
BEN Villages UUT cases<br />
From 1955 to 1998 year, 1235 patients with histologicaly<br />
proven UUT, underwent surgery. Data collected from<br />
______________________<br />
Correspodence to: J. Nikolic, Urologic Clinic-Faculty of Medicine Belgrade, Jaroslav Cerni,<br />
Belgrade, Serbia and Montenegro<br />
Tumors per<br />
village<br />
BEN present 40 301 7,5<br />
BEN possible 64 233 3,6<br />
No BEN 33 145 4,39<br />
No BEN 36 72 2<br />
No BEN 95 95 1<br />
No BEN 457 0 0<br />
BEN possible 66 0 0<br />
The UUT was registered in 285 of 808 settlements. The UUT<br />
cases from 16 cities (182 pts.) and Belgrade (207 pts. ), with<br />
no autochtonous BEN cases, were excluded from the study.<br />
We found 312 sporadic BEN cases, with concomitant UUT,<br />
in 164 non-endemic settlements. The both sexes were equally<br />
affected: 140 males with average age of 61.06 years, and 172<br />
females with an average age of 64.99 years.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): p 16<br />
Table 2. The number and sex distribution of sporadic BEN cases in settlements<br />
Settlement Community<br />
Sporadic<br />
BEN<br />
Males Females Inhabitants<br />
1 Orljevo Petrovac 3 3 - 546<br />
2 Srpce Kuevo 3 2 1 293<br />
3 Rakinac Vel.Plana 3 - 3 1404<br />
4 Kula M.Crnie 3 - 3 908<br />
5 Klievac Požarevac 3 2 1 2084<br />
6 Nemenikue Sopot 3 2 1 1933<br />
7 Brzohode Žabari 3 - 3 1225<br />
8 Bošnjak Petrovac 3 2 1 696<br />
9 V.Crnie M.Crnie 3 - 3 926<br />
10 irikovac Požarevac 3 1 2 1645<br />
11 Kuevo Kuevo 3 1 2 4846<br />
12 Živica Požarevac 3 - 3 914<br />
13 Sopot Sopot 3 - 3 1720<br />
14 M.Ivana Sopot 3 1 2 1857<br />
15 Vrani Barajevo 3 1 2 3288<br />
16 Golubac Golubac 3 1 2 1995<br />
17 Viteževo Žabari 4 2 2 1402<br />
18 Voluja Kuevo 4 1 3 1318<br />
19 Vel.Selo M.Crnie 4 2 2 694<br />
20 Brgule Ub 4 2 2 1356<br />
21 Selevac Sm.Palanka 4 2 2 4618<br />
22 Dubravica Požarevac 4 1 3 1521<br />
23 Boževac M.Crnie 5 1 4 2480<br />
24 Toponica M.Crnie 5 3 2 1374<br />
25 Vel.Laole Petrovac 5 1 4 2694<br />
26 Mala Krsna Smederevo 5 2 3 1829<br />
27 Carevac V.Gradište 5 2 3 1102<br />
28 Rabrovo Kuevo 5 2 3 1441<br />
29 Ranovac Petrovac 6 1 5 2787<br />
30 Vrin Grocka 8 6 2 8034<br />
31 Dragovac Požarevac 8 2 6 1166<br />
32 Barajevo Barajevo 10 6 4 6243<br />
33 Porodin Žabari 11 6 5 3454<br />
145 59 86 69793<br />
Discussion<br />
The diagnosis of BEN is not absolutely accurate, just very<br />
possible (8). The similar situation is with sporadic BEN<br />
cases, where simultaneous occurrence of UUT, after<br />
exclusion of all other nephropathies, makes a diagnosis more<br />
accurate. Both sexes were affected equally, the patients were<br />
in sixth or seventh decade of life, with mild to moderate<br />
degree of renal failure in 39,4%. In the most endemic BEN<br />
areas, the patients with BEN and UUT, had renal failure in<br />
60% (9). The cases with BEN and UUT, presented without<br />
the signs of renal damage at the time of surgery for UUT,<br />
developed renal failure later on.<br />
The distribution of 312 sporadic BEN cases in 164 nonendemic<br />
settlements was: 33 villages with ≥ 3 cases (4.39 per<br />
settlement), 36 villages with two, and 95 with only one case.<br />
Like in our previous report (5), the territorial distribution of<br />
villages with various UUT incidence had a concentric, rather<br />
than mosaic pattern. The endemic villages with highest<br />
incidence, were situated in central and the lowest parts of the<br />
river valleys, and less endemic, in their surroundings and<br />
higher altitudes. These 33 villages with sporadic BEN, were<br />
located like a ring, around groups of BEN villages. The same<br />
pattern existed in the valleys of rivers Kolubara, Morava and<br />
Mlava.The villages with two and one sporadic BEN cases,<br />
were located over wider territory.<br />
The basic differencies between BEN and sporadic BEN, are<br />
that there are no young sporadic BEN cases with very small<br />
kidneys and severe renal failure, and there is no familiar<br />
occurence of the disease. The incidence of sporadic cases in<br />
the settlements, during 40 years of observation, was one case<br />
every 10, 20 or 40 years.<br />
One can speculate that sporadic BEN is the result of low<br />
concentration of ethiological agent in nature and therefore the<br />
incidence is minimal, the age of onset is high, and the renal<br />
failure is not severe, with normal or slightly smaller kidneys.<br />
Here documented territory, endangered with BEN, including<br />
sporadic BEN cases, is actually much larger, which means<br />
that the distribution of ethiologic agent in the nature is not<br />
limited only in known endemic or hypoendemic areas.<br />
Conclusions<br />
Sporadic BEN is an atypical, mild clinical variety of BEN,<br />
with simultaneous presence of UUT, characterized with very<br />
low incidence in the non-endemic areas and without familiar<br />
aglommeration, which are the crucial caracteristics of BEN.<br />
The number of sporadic BEN cases without UUT, remains<br />
undetected, because of rigidity in diagnostic criteria and the<br />
abscence of specific findings.<br />
We found 312 sporadic BEN cases in 164 non-endemic<br />
villages.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): p 17<br />
Both sexes were equally affected, with the majority of<br />
patients in sixth and seventh decade of life (male average age<br />
was 61.06, and female average age was 64.99 years).<br />
Moderate or mild renal failure was found in 39.4%.<br />
The 33 villages with ≥ 3 sporadic BEN, were located in the<br />
circle arround the known BEN zones, certifying the diagnosis<br />
of BEN. The rest of villages were spread over wider territory.<br />
The presence of sporadic BEN cases gives a possibility to<br />
speculate that the existence of BEN without familar<br />
agreggations, with low incidence in the settlement (one case<br />
per few decades) is possible elsevere, not only in Balkans,<br />
but it is still impossible to detect sporadic BEN using the<br />
standard diagnostic procedures.<br />
Map 1. Territorial distribution of 33 settlements with sporadic BEN cases associated with UUT cases,<br />
localized out of known BEN regions.<br />
References<br />
1. Zacharia C. Uber endemische Nephropatien (Nierenatrophien)<br />
eine epidemioologische untersuchung. In: Int Symp on<br />
Endemic Nephropathy. Sofia 1963. Bulg. Acad Sc Press, Sofia<br />
1965; 73-76<br />
2. Zacharia C. A modern approach to the concept of familiar<br />
endemic nephropathy. Rev Roum Med 1978; Med Int 16:2<br />
3. Polenakovi M, Stefanovi V. Balkan Nephropathy. In: Oxford<br />
Textbook of Clinical Nephrology. Oxford medical Publications.<br />
Sec ed. Eds. Davidson A., Cameron JS, Grunfeld JP, Kerr<br />
DNS, Ritz E and Winearls Ch. Oxford, Oxford University<br />
Press, 1998; 1202-1210<br />
4. Nikoli J, Djoki M, Todorovi D et al. 1998; Characteristic of<br />
patients suffering from ureteral or renal pelvic tumors in lower<br />
flow of the Morava and Mlava rivers: Third Congr.of the<br />
Balkan Cities Associastion of Nephrology, Dialysis,<br />
Transplantation and Arteficial organs, Belgrade, 1998; abstract<br />
book p42<br />
5. Nikoli J, Djoki M, Crnomarkovi D et al. Upper urothelial<br />
tumors and Balkan nephropathy-dose responsible diseases in<br />
Facta Universitatis univ of Nis, vol 9, No1, 2002; 114-118<br />
6. Danilovi V. Endemic nephropathy in Yugoslavia. In: Endemic<br />
(Balkan) nephropathy, Proc. 4th Symp., Niš 1979. Eds. S.<br />
Strahinji V. Stefanovi Instr Nephr Haemod Niš 1981; 1-5<br />
7. Radovanovi Z. Topographical distribution of the Balkan<br />
endemic nephropathy in Serbia (Yugoslavia). Trop geogr Med<br />
1979; 31: 185-189<br />
8. Radoni M, eovi S, Radoševi Z. Clinical picture of<br />
Endemic nephropathy 3rd simp on Endemic Nephropathy,<br />
Beograd 1982 ed.S. Petkovi SANU, book XXlll Beograd<br />
1985; 87-196 (in serbo-croat)<br />
9. Djoki M, Hadžidjoki J, Nikoli J et al. Comparison des<br />
tumeurs de haut appareil urinaire dans la region de la<br />
nepphropatie balkanique avec celles d,autres regions de<br />
Yugoslavie. Prog Urol 1999; 61-68<br />
10. Cancer incidence in five continents, data for Vojvodina. 2005;<br />
htpp//www.janc.fr
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): p 18<br />
Amyloidosis in Turkish patients<br />
C. Ensari 1 and A. Ensari 2<br />
1 Ankara Atatürk Research Hospital Dialysis Unit, 2 University of Ankara, Medical School - Turkey<br />
Abstract<br />
Amyloidosis is characterized by the systemic or localized<br />
extra cellular deposition of amyloid, a proteinaceous fibrillar<br />
material in various tissues and organs, mainly classified into<br />
primary (AL) or secondary (AA) groups according to the<br />
biochemical nature of the fibril forming protein.<br />
The histopathological diagnosis was made on Congo red<br />
stained biopsy specimens using polarized light and the<br />
subtyping of amyloidosis was made by immunohistochemical<br />
analysis. One hundred twenty eight amyloid positive biopsies<br />
obtained from 111 patients whose paraffin blocks were<br />
available for immunohistochemical analysis were included in<br />
the study. 111 patients (70 male) with an average age of 34.2<br />
years (range 6-65 years), were included in the study.<br />
Amyloid deposits were subtyped immunohistochemically in<br />
128 biopsies. The vast majority (90.9 %) of patients in our<br />
study presented with AA amyloidosis.<br />
This retrospective study demonstrates that the patient<br />
population with amyloidosis in Turkey is significantly<br />
different from the western countries. Our results indicate the<br />
predominance of AA amyloidosis and also suggest that<br />
routine immunohistochemical analysis of amyloidosis cases<br />
with certain ethnic background is sufficient to classify the<br />
subtype of amyloid fibril protein and the related disease.<br />
Key words: amyloidosis, histopathological diagnosis,<br />
immunohistochemistry<br />
Introduction<br />
Amyloidosis is characterized by the systemic or localized<br />
extra cellular deposition of amyloid, a proteinaceous fibrillar<br />
material in various tissues and organs. Although many types<br />
of fibril proteins have been defined, amyloidosis is mainly<br />
classified into primary (AL) or secondary (AA) groups<br />
according to the biochemical nature of the fibril forming<br />
protein. The results of previously published reports on<br />
amyloidosis including autopsy series strongly suggested that<br />
the frequency and type of amyloidosis and related disease<br />
may vary significantly in different patient populations (1-4).<br />
There is not much information in the literature concerning the<br />
accuracy of immunohistochemical subtyping in relation to<br />
clinical diagnosis (5-7), though classifying primary<br />
amyloidosis by immunohistochemistry has been reported to<br />
be more difficult (8).<br />
The aim of the present study was, therefore, to classify<br />
amyloidosis by means of immunohistochemical subtyping of<br />
amyloid fibril proteins and assessing the correlation of<br />
immunohistochemistry with clinical diagnosis in order to<br />
retrieve useful epidemiological data from these patients.<br />
Patients and methods<br />
The histopathological diagnosis was made on Congo red<br />
stained biopsy specimens using polarized light and the<br />
subtyping of amyloidosis was made by immunohistochemical<br />
analysis. One hundred twenty eight amyloid positive biopsies<br />
obtained from 111 patients whose paraffin blocks were<br />
available for immunohistochemical analysis were included in<br />
the study. Mean patient age was 34.2 years with a range of 6-<br />
65 years. There were 70 male, 41 female patients in the<br />
study.<br />
Paraffin sections, 4 microns thick, were taken from 128<br />
biopsy specimens comprising 69 renal, 36 rectal, 15<br />
testicular, 5 liver, 2 small intestinal biopsies and 1 bladder<br />
biopsy. An antibody panel including monoclonal antibodies<br />
to Amyloid A (1:100), lambda (1:50) and kappa (1:50) light<br />
chains, transthyretin (1:100), and beta-2-microglobulin (1:50)<br />
(DAKO), leaving out the extremely rare forms of amyloid<br />
fibrils, was selected for the study. Patient files were reviewed<br />
and clinical histories were recorded.<br />
Table 1: The results of immunohistochemical analysis<br />
Biopsy site # of<br />
biopsies<br />
AA AL AK ATTR β2MG Mixed<br />
Kidney 69 65 4 (2 AA+AL)<br />
(2 AA+ATTR)<br />
Rectum 36 35 1 (AA+ATTR)<br />
Testicle 15 10 4 1<br />
(AA+AL+ATTR)<br />
Liver 5 0 2 1 2 (1 AA+AL)<br />
(1 AA+β2MG)<br />
Small Int. 2 2<br />
Bladder 1 1<br />
Total 128 113 6 0 0 1 8<br />
______________________<br />
Correspodence to: C. Ensari, Ankara Atatürk Research Hospital Dialysis Unit, Ankara, Turkey
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 19<br />
Results<br />
Amyloid deposits were subtyped immunohistochemically in<br />
128 biopsies taken from 111 cases. In 17 cases, multiple<br />
organ biopsies were taken; 10 cases had renal + rectal<br />
biopsies, whereas 7 cases had renal + testicular biopsies.<br />
The results of the immunohistochemical analysis are<br />
presented in Table 1. Amyloid deposits were stained by a<br />
single antibody in 120 (93.8 %) whereas 8 biopsies (6.2 %)<br />
stained positively by more than one antibody.<br />
Table 2: The relation of clinical diagnosis to biopsy site<br />
Disease<br />
# of # of<br />
Small<br />
Kidney Rectum Testicle Liver<br />
cases biopsy<br />
Intestine<br />
Bladder<br />
FMF 81 98 48 36 10 2 1 1<br />
Tuberculosis 8 8 8<br />
Bronchiectasis 4 4 4<br />
RA 7 7 7<br />
Crohn’s Disease 1 1 1<br />
Plasma CD 7 7 1 4 2<br />
Hemodialysis 1 1 1<br />
Unknown 2 2 1 1<br />
Total 111 128 69 36 15 5 2 1<br />
FMF: Familial Mediterranean Fever, RA: Rheumatoid Arthritis, Plasma CD: Plasma cell dyscrasias<br />
The relation between clinical diagnosis and biopsy site is<br />
presented in Table 2. The correlation of<br />
immunohistochemical subtyping and clinical diagnosis is<br />
summarized in Table 3.<br />
Table 3: The correlation of immunohistochemical sub typing and clinical diagnosis<br />
Disease<br />
# of<br />
cases<br />
# of<br />
biopsy<br />
AA AL AK ATTR β2MG Mixed<br />
3 (1 AA+AL)<br />
FMF 81 98 95 (1 AA+ATTR)<br />
(1 AA+β2MG)<br />
Tuberculosis 8 8 8<br />
Bronchiectasis 4 4 4<br />
RA 7 7 5 2 (2 AA+ATTR)<br />
Plasma CD 7 7 6 1 (1 AL+AA)<br />
Crohn’s Disease 1 1 1<br />
Hemodialysis 1 1 1<br />
Unknown 2 2<br />
2 (1 AA+AL)<br />
(1AA+AL+ATTR)<br />
Total 111 128 113 6 0 0 1 8<br />
FMF: Familial Mediterranean Fever, RA: Rheumatoid Arthritis, Plasma CD: Plasma cell dyscrasias<br />
Discussion<br />
Lachmann et al (8), reported that immunohistochemistry is<br />
usually definitive in identifying reactive (AA) amyloidosis,<br />
though, it is frequently not diagnostic with respect to AL<br />
amyloidosis either due to abnormal fibril conformation of<br />
light chain fragments or to the background staining caused by<br />
normal immunoglobulins in the tissues. In a recent study,<br />
immunofluorescence technique yielded negative staining in<br />
35.3 % of cases with proven AL amyloidosis in renal<br />
biopsies (9). Since the vast majority (90.9 %) of patients in<br />
our study presented with AA amyloidosis, the technical<br />
limitations of immunohistochemistry are not evident in our<br />
patients except for two cases (1.8 %) in which no clinical<br />
condition related to amyloidosis could be documented. In<br />
contrast to the reports from western countries where the<br />
majority of cases are AL amyloidosis (8, 9), the few cases<br />
with AL amyloidosis in the present study were also<br />
accurately diagnosed by means of immunohistochemistry.<br />
Amyloidosis can be diagnosed and classified in any affected<br />
tissue sample. Nevertheless, it is still important to define the<br />
most suitable diagnostic site to be biopsied and examined for<br />
the early detection of amyloid deposition. For systemic<br />
amyloidosis, however, no such favorite site has been<br />
documented in any of the studies performed so far (2, 3)<br />
although rectal biopsy seems to be more commonly used<br />
mainly because of its easy access by the clinician (3, 10).<br />
Another easy access, abdominal fat biopsy has been reported<br />
as insensitive for AA amyloidosis while renal biopsy,<br />
probably due to the increase in the number of well-trained<br />
nephrologists, is becoming more popular in the diagnosis of<br />
amyloidosis (4). Similarly, it was the most commonly used<br />
intervention to diagnose amyloidosis in our study. In practice,<br />
however, clinical presentation seems to be the main<br />
determinant of the biopsy site; i.e. a patient with proteinuria<br />
would undergo a renal rather than a rectal biopsy. Renal or<br />
rectal biopsies were performed commonly in our cases<br />
depending on the presenting clinical symptoms. Though a<br />
variety of anatomical sites have been used for the detection of<br />
amyloid (3,4), we found only few reports mentioning<br />
testicular biopsy despite the high incidence observed in our<br />
study (11,12). In one of these reports, testis biopsy was found<br />
valuable and more sensitive than rectal biopsy in the<br />
diagnosis of systemic amyloidosis (12).<br />
In many developed countries primary amyloidosis is the more<br />
common form of systemic amyloidosis (1-3). With the virtual
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 20<br />
abolition of chronic infectious diseases, the incidence of<br />
secondary amyloidosis has been reduced in such countries.<br />
However, it still occurs mainly in patients suffering from RA<br />
followed by chronic infectious diseases and Crohn’s disease<br />
while TBC and FMF were found to be very rare as amyloid<br />
related diseases (5,13). On the other hand, secondary<br />
amyloidosis is still the more common type of systemic<br />
amyloidosis in developing countries (1,3) where TBC<br />
together with other chronic infectious diseases are the leading<br />
causes of systemic amyloidosis followed by RA which is<br />
observed only in a small percentage of patients with<br />
amyloidosis (14,15). In the Middle East, however, among<br />
patients with different ethnic origins, FMF is the leading<br />
etiologic condition in the development of amyloidosis. This<br />
ethnically restricted genetic disorder mainly affects<br />
populations originated from the Mediterranean-Middle<br />
Eastern populations such as Jews, Arabs, Armenians and<br />
Turks (16). In a recent report, a lower incidence of<br />
amyloidosis was observed in a group of Italian patients with<br />
FMF (17). Although the true Figures are not well<br />
documented, Turkey is known to have a high prevalence of<br />
FMF and FMF-related amyloidosis (18,19).<br />
Not surprisingly, secondary amyloidosis is the main form of<br />
systemic amyloidosis in our cases, many with a clinical<br />
diagnosis of FMF followed by TBC, RA and bronchiectasis<br />
in similar frequencies. This finding seems to be in<br />
concordance with previous reports from Turkey (19,20).<br />
Conclusions<br />
This retrospective study demonstrates that the patient<br />
population with amyloidosis in Turkey is significantly<br />
different from the western countries. Our results indicate the<br />
predominance of AA amyloidosis associated with FMF and<br />
also suggest that routine immunohistochemical analysis of<br />
amyloidosis cases with certain ethnic background is sufficient<br />
to classify the subtype of amyloid fibril protein and the<br />
related disease. However, detailed clinical information is<br />
mandatory before making a definite diagnosis based solely on<br />
immunohistochemical observations. Moreover, due to<br />
increased rate of immigration affecting the ethnic structure of<br />
the developed countries, physicians’ awareness of the<br />
prevalence of certain diseases related to ethnic origin is<br />
essential to prevent long term serious complications such as<br />
amyloidosis and improve the quality of patients’ lives.<br />
References<br />
1. Simms RW, Prout MN, Cohen AS. The epidemiology of AL<br />
and AA amyloidosis. Baillieres Clin Rheumatol 1994; 8: 627-<br />
634<br />
2. Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses.<br />
N Eng J Med 1997; 337: 898-909<br />
3. Sipe JD, Cohen AS. Amyloidosis. In Braunwald A, Fauci AS,<br />
Kasper DL, Hauser SL, Longo DL, Jameson JL, Eds.<br />
Harrison’s Principles of Internal Medicine (15 th edn). New-<br />
York: McGraw-Hill 2001; 1974-1979<br />
4. Röcken C, Sletten K. Amyloid in surgical pathology. Virchows<br />
Arch 2003; 443: 3-16<br />
5. Hoshii Y, Takahashi M, Ishihara T, Uchino F.<br />
Immunohistochemical classification of 140 autopsy cases with<br />
systemic amyloidosis. Am J Pathol 1994; 4: 352-358<br />
6. Röcken C, Schwotzer EB, Linke RP, Saeger W. The<br />
classification of amyloid deposits in clinicopathological<br />
practice. Histopathol 1996; 29: 325-335<br />
7. Strege RJ, Saeger W, Linke RP. Diagnosis and<br />
immunohistochemical classification of systemic amyloidoses.<br />
Virchows Arch 1998; 433: 19-27<br />
8. Lachmann HS, Booth DR, Booth SE, Bybee A, Gilbertson JA,<br />
Gilmore JD, Pepys MB, Hawkins PN: Misdiagnosis of<br />
hereditary amyloidosis as AL (primasy) amyloidosis. N Eng J<br />
Med 2002; 346: 1786-1791<br />
9. Novak L, Cook WJ, Herrera GA, Sanders PW. AL-amyloidosis<br />
is underdiagnosed in renal biopsies. Nephrol Dial Transplant<br />
2004; 19: 3050-3053<br />
10. Lee JG, Wilson JA, Gottfried MR. Gastrointestinal<br />
manifestations of amyloidosis. South Med J 1994; 87: 243-247<br />
11. Haimov-Kochman R, Prus D, Ben-Chetrit E. Azoospermia due<br />
to testicular amyloidosis in a patient with familial<br />
Mediterranean fever. Hum Reprod 2001; 16: 1218-1220<br />
12. Ozdemir BH, Ozdemir OG, Ozdemir FN, Ozdemir AI. Value<br />
of testis biopsy in the diagnosis of systemic amyloidosis.<br />
Urology 2002; 59: 201-205<br />
13. Joss N, McLaughlin K, Simpson K, Boulton-Jones JM.<br />
Presentation, survival and prognostic markers in AA<br />
amyloidosis. QJM 2000; 93: 535-542<br />
14. Shah VB, Phatak AM, Shah BS, Kandalkar BM, Haldankar<br />
AR, Ranganathan S. Renal amyloidosis – a clinicopathologic<br />
study. Indian J Pathol Microbiol 1996; 39: 179-185<br />
15. McAdam KP, Raynes JG, Alpers MP, Westermark GT,<br />
Westermark P. Amyloidosis: a global problem common in<br />
Papua New Guinea. P N G Med J 1996; 39: 284-296<br />
16. Orbach H, Ben-Chetrit E. Familial Mediterranean fever – a<br />
review and update. Minerva Med 2001; 92: 421-430<br />
17. Regina ML, Nucera G, Diaco M, Procopio A, Gasbarrini G,<br />
Notarnicola C, Kone-Paut I, Touitou I, Manna R. Familial<br />
Mediterranean fever is no longer a rare disease in Italy. Eur J<br />
Hum Genet 2003; 11: 50-56<br />
18. Yazici H, Özdogan H. Familial Mediterranean Fever in Turkey.<br />
In: Sohar E, Gafni J, Pras M Eds. Familial Mediterranean<br />
Fever. London and Tel Aviv: Freund Publishing House Ltd<br />
1997; 66-71<br />
19. Tuglular S, Yalcinkaya F, Paydas S, Oner A, Utas C,<br />
Bozfakioglu S, Ataman R, Akpolat T, Ok E, Sen S, Dusunsel<br />
R, Evrenkaya R, Akoglu E. A retrospective analysis for<br />
etiology and clinical findings of 287 secondary amyloidosis<br />
cases in Turkey. Nephrol Dial Transplant 2002; 17: 2003-2005<br />
20. Paydas S. Report on 59 patients with renal amyloidosis. Int<br />
Urol Nephrol 1999; 31: 619-631
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 21<br />
Frequency of Alport syndrome at dialysis center “Vrsac”- Vrsac<br />
K. Djordjev¹, D. Tintor¹, G. Djurdjev¹, O. Vasilic-Kokotovic¹, I. Sokolovac² and S. Bozic³<br />
¹Department of Nephrology and Haemodialysis, Health Center “Vrsac”, Vrsac; ²Clinic of ORL,University of Medicine,<br />
Novi Sad; ³Department of Ophtalmology, Health Center “Vrsac”, Vrsac, Serbia and Montenegro<br />
Abstract<br />
Patients and methods<br />
Alport syndrome (AS) is a hereditary nephropathy<br />
characterized by persistent haematuria that may evolve to end<br />
stage renal disease, associated with sensorineural hearing loss,<br />
ocular abnormalities. Th aim of the study was to establish<br />
correct diagnosis and to estimate the frequency of disease.<br />
We evauated 44 members in four generations from one Gipsy<br />
family in Vrsac county. Through the family inquiry and a<br />
review of medical records, the genealogic tree was made. The<br />
frequency of Alport syndrome in Dialysis Center Vrsac is<br />
12.5% (5 out of 40 patients).<br />
Considerably great frequency of AS in our dialysis center is<br />
confirmed in comparison to other centers in our country,<br />
which is probably caused by consanguinity or mutation that<br />
is not connected with X chromosome, or due to other factors<br />
that are not of genetic nature like lifestyle, diet, infections or<br />
something else.<br />
Key words: Alport syndrome, disease frequency<br />
Introduction<br />
Alport syndrome (AS) is a hereditary nephropathy<br />
characterized by persistent haematuria that may evolve to end<br />
stage renal disease (ESRD). This syndrome is associated with<br />
sensorineural hearing loss, ocular abnormalities (anterior<br />
lenticonus, macular or peripheral flecks), and ultrastructural<br />
abnormalities of the glomerular basement membrane (GBM)<br />
(1). Mutation in collagen type IV genes are responsible for<br />
disorders of glomerular basement membrane, that produce<br />
broad spectrum of disease phenotypes ranging from benign<br />
haematuria to most severe forms of AS. This leads us to<br />
agglutinate different entities under the name of “collagen<br />
type IV” nephropathy (2). AS displays considerable<br />
phenotypic and genetic heterogeneity (3), and this syndrome<br />
is relatively rare. There are three genetic forms of AS exist:<br />
X-linked form (accounts for 85% cases), autosomal-recessive<br />
(responsible for approximately 10-15% of cases; and<br />
autosomal-dominant form (less than 1%), in at least some<br />
families. The estimated gene frequency ratio of AS is 1:5000<br />
(5).<br />
This study is implemented with the aim to establish correct<br />
diagnosis, to estimate frequency of disease, to make a<br />
genealogical tree, to collect data from epidemiological,<br />
ophthalmic, audiometric tests and to compare them with the<br />
other experiences from literature, and to confirm the type of<br />
heredity through a review the genealogic tree.<br />
A great frequency of Alport syndrome is presented in Vrsac<br />
county. There is a large percentage of this phenomenon<br />
causing end stage renal disease (ESRD) at our center and it is<br />
12.5% (5 out of 40); and this percentage is high and is very<br />
likely to increase. All the patients are from one Gipsy family,<br />
at this moment with 44 members in four generations, and all<br />
of them live in the same village 65 km away from Belgrade.<br />
The oldest alive member is 40, and the youngest one is onemonth-old<br />
baby.<br />
Results<br />
Through the family inquiry, as well as the review of medical<br />
records, the genealogic tree was made (Figure 1). The<br />
frequency of Alport syndrome in Dialysis Center Vrsac is<br />
12.5% (5 out of 40 patients). AS is considered the be a cause<br />
of approximately 0.6 to 2.3% of ESRD in Europe and the<br />
United States (6,7), and from the registry 2004 in Serbia and<br />
Montenegro it is less than 1%. This proportion is probably<br />
underestimated because of the diagnostic difficulties.<br />
Average ages when started with dialysis is 21.5 years for<br />
males and for females is 35 years (with the deceased family<br />
members). The male patients III:5, III:6, III:12 and III:13<br />
started the dialysis at the age of 22, 21, 23 and 24<br />
respectively, and the female patient II:2 started at the age of<br />
34. At present, the male patients spent average 4 years and<br />
female spent on dialysis 6 years. Thus the deceased members<br />
(two female and one male patient) from the same family,<br />
started the dialysis at the age of 41 and 31(females), and 17<br />
(male) and spent less than one month, the first, and less than<br />
two years, the other female; and less than a year for the male.<br />
All patients have had macroscopic haematuria before they<br />
started with dialysis. They should probably have started<br />
sooner, given the fact that they had come in a very bad<br />
condition, with extremely high values of serum creatinine and<br />
blood urea concentrations and had urgently started with<br />
haemodialysis. They have not consulted a doctor before,<br />
considering that they had painful haematuria, nausea,<br />
frequent vomiting, and a peripheral edema. Clinical<br />
examinations have shown a great percentage of extrarenal<br />
abnormalities with variability of signs, which is rare. All the<br />
patients who were on dialysis have progressive sensorineural<br />
deaffnes (5 out of 5), both for high and low frequencies with<br />
similar findings in the study of autosomal dominant<br />
nephropathy (8). Ocular abnormalities had 4 out of 5 patients,<br />
except a female patient. They had lenticonus anterior and<br />
retinitis pigmentosa. Two biopsies at light microscopy<br />
indicated disorders of GBM. Three out of five patients on<br />
______________________<br />
Correspodence to: K. Djordjev, Department of Nephrology and Haemodialysis, Health Center “Vrsac”,<br />
Vrsac, Serbia and Montenegro
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 22<br />
dialysis had hypercholesterolaemia (total cholesterol more<br />
than 8.3, 7.1 and 6.7 mm/l) (9), but unlike those who had<br />
Fetchner syndrome, they didn’t have trombopenia (10).<br />
Complications occured in a form of arterial hypertension in 4<br />
out of 5 patients. All of them are anemic (average value of<br />
haemaglobin was 11.7 g/dl) and they were all on Epoetin<br />
Beta (Recormon®). Two out of five patients were hepatitis<br />
“B” seropositive. They had mild intellectual deficit. In<br />
addition to this, the patients were very undisciplined, had a<br />
great increase in weight interdialysis and had a poor social<br />
background.<br />
Conclusions<br />
This data obviously leads to a confirmation of the diagnosis<br />
of Alport syndrome, as a severe (juvenile) form (
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 23<br />
Eearly effects of the AT 2 receptor antagonist eprosartane mesylate (EM) in<br />
diabetic patients with and without chronic renal failure<br />
N. Nnchev, B. Deliyska, M. Bankova, P. Radulova, G. Kimenov and E. Marinova<br />
Medical University, Sofia, Bulgaria<br />
Abstract<br />
ATII receptor antagonists are effective in the control of the<br />
arterial hypertension (AH) in patients with CRF. Different<br />
factors take part in the pathogenesis of the AH in the diabetic<br />
mellitus (DM) patients: volume overload, sodium retention,<br />
renin-angiotensin system (RAAS), activity of the sympatic<br />
system (SNS) and endothelin system.<br />
The aim of the study is assessment of the effectiveness of the<br />
EM on the blood pressure (BP) and pulse pressure (PP)<br />
which are incriminated factors for the cardiovascular<br />
morbidity and mortality.<br />
22 patients (14 male and 8 female) with DM and AH, mean<br />
age 52±8 years, divided in 2 groups were followed for 3-<br />
month period. On 0, 1 st , 4 th , 12 th week the following<br />
parameters were followed: systolic BP, diastolic BP, mean<br />
arterial pressure (MAP), PP, heart rate, weight, height, basic<br />
laboratory tests. All the patients received 600 mg EM<br />
(Teveten ® ) once a day in the morning (10 of them as a mono<br />
therapy and the rest in a combination with other<br />
antihypertensive therapy, which was not changed during the<br />
study).<br />
There were significant changes in the mean blood pressure<br />
and PP in both groups at 4 and 12 week. There were not<br />
significant changes in HF between the groups. At the end of<br />
the study mean BP decreased in group A for 20,4% and in<br />
group B for 26,9%. PP decreased in group A for 35,7% and<br />
in group B for 38,9%. Serum creatinine did not changed<br />
significantly neither in group A nor in group B (group A<br />
from 98+/-11,1 to 95,9+/-8,4 mol/l; group B from 321+/-76<br />
to 349+/-21,3 mol/l). We did not observed also a significant<br />
changes in creatinine clearance in the two groups (group A<br />
from 111+/-15,1 to102+/-11 mmol/min; group B from 18+/-<br />
2, 2 to 20,6+/-4,8 mmol/min).<br />
ATII receptor blocker EM leads to significant control over<br />
BP and PP after 4 th week in DM patients with and without<br />
CRF. This effect is probably due to a dual mechanism of<br />
action over AH – control over RAAS and SNS. The drug is<br />
well tolerated with no side effects.<br />
Key words: AT 2 receptor antagonist, diabetes mellitus, renal<br />
failure<br />
Introduction<br />
There is a relationship between cardiovascular and kidney<br />
diseases. Treatment of an early nephropathy has also<br />
cardioprotective effect in the hypertensive patients.<br />
Renoprotective drugs improve the renal and endothelial<br />
dysfunction that is connected with overactivation of the<br />
______________________<br />
Correspodence to: N. Nnchev, Medical University, Sofia, Bulgaria<br />
renin-angiotensin-aldosterone system (RAAS). RAASdirected<br />
antihypertensive agents are both angiotensin<br />
converting enzyme (ACE) inhibitors and angiotensin II<br />
receptor blockers (ARBs) that have renoprotective effects.<br />
They decrease both high blood pressure and proteinuria (8).<br />
Metabolic syndrome is a cluster of common cardiovascular<br />
risk factors that includes hypertension and insulin resistance.<br />
Hypertension and diabetes mellitus are frequent<br />
comorbidities and like metabolic syndrome, increase the risk<br />
of cardiovascular events. Eprosartane, an antihypertensive<br />
agent with evidence of partial peroxisome proliferatoractivated<br />
receptor activity-gamma (PPARgamma) activity,<br />
may improve insulin sensitivity and lipid profile in patients<br />
with metabolic syndrome (1).<br />
The aim of the study was to evaluate early efficacy of<br />
eprosartane mesilate (EM) (Teveten ® -Solvei) on the blood<br />
pressure (BP) and pulse pressure (PP) in diabetic patients<br />
with and without chronic renal failure (CRF).<br />
Patients and methods<br />
The study was conducted in 22 patients with diabetic<br />
nephropathy. Fourteen from them were males with a mean<br />
age of 52±8 years. The patients were divided into 2 groups.<br />
Group A, 8 patients without CRF and group B, 14 CRF<br />
patients. The follow-up period was 12 weeks. At 0, 4 and 12<br />
week the followed parameters were: mean blood pressure<br />
(BP), PP, hearth frequency (HF), body weight, high, serum<br />
creatinine and creatinine clearance. All patients were treated<br />
with EM, 600 mg once daily. Ten patients were with<br />
monotheray by EM, all others received before EM another<br />
antihypertensive treatment and EM were additional included.<br />
Results<br />
The results of PB, PP, HF of the patients from two groups are<br />
shown in Table 1.<br />
Group A<br />
1 st<br />
Parameter Baseline<br />
week<br />
4 th week 12 th week<br />
MAP 113 ± 6 110 ± 5 96 ± 7 * 90 ± 5 **<br />
(mm Hg)<br />
PP<br />
70 ± 8 62 ± 6 51 ± 5 * 45 ± 4 **<br />
(mm Hg)<br />
Heart rate 75 ± 9 75 ± 4 70 ± 4 72 ± 6<br />
There were significant changes in the mean blood pressure<br />
and PP in both groups at 4 and 12 week. There were not<br />
significant changes in HF between the groups. At the end of
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 24<br />
the study mean BP decreased in group A for 20,4% and in<br />
group B for 26,9%. PP decreased in group A for 35,7% and<br />
in group B for 38,9%. Serum creatinine did not changed<br />
significantly neither in group A nor in group B (group A<br />
from 98+/-11,1 to 95,9+/-8,4 mol/l; group B from 321+/-76<br />
to 349+/-21,3 mol/l). We did not observe also a significant<br />
changes in creatinine clearance in the two groups (group A<br />
from 111+/-15,1 to102+/-11 mmol/min; group B from 18+/-<br />
2, 2 to 20,6+/-4,8 mmol/min).<br />
Group B<br />
Parameter<br />
Baseline<br />
1 st<br />
week<br />
4 th<br />
week<br />
12 th week<br />
MAP<br />
(mm Hg)<br />
130 ± 9 127 ± 4 105 ± 7 * 95 ± 8<br />
PP<br />
(mm Hg)<br />
90 ± 8 100 ± 2 80 ± 5 * 55 ± 9 **<br />
Heart rate 88 ± 9 86 ± 3 82 ± 4 75 ± 4<br />
* p < 0,01 ; ** p< 0,001<br />
Discussion<br />
Eprosartane is a well tolerated ARB drug. There were<br />
evidences for its reno- and cardioprotection especially in<br />
diabetic patients. Therapy with ARB is suitable also for<br />
patients with primary and secondary glomerulonephritis. The<br />
effectiveness of a combined therapy with ARB and ACE<br />
inhibitors may have been at least partly due to the greater<br />
inhibition of the action of angiotensin II in patients with IgA<br />
nephropathy. This strategy apparently reduced mild-tomoderate<br />
proteinuria in patients with normotensive IgA<br />
nephropathy (9). The angiotensin II changes glomerular<br />
permeselective function via the opening of large pores after<br />
elevations in transmembrane pressure and by acting on the<br />
glomerular pressure, too. There is evidence that angiotensinconverting<br />
enzyme inhibitors (ACEI) alone or with the<br />
ARB’s may improve the glomerular size-selective function<br />
and the hemodynamic intrarenal accounted output of plasma<br />
proteins that result in decreasing of proteinuria. It was not<br />
only by the drug related reduction in systemic blood pressure<br />
(4). The combination of ARB and ACEI seems to be<br />
beneficial and may offer an additional renoprotective effect<br />
(10). Hemodialysis patients have uremic dyslipidemia,<br />
represented by elevated serum intermediate-density<br />
lipoprotein cholesterol (IDL-C) levels, and an increased<br />
cardiovascular mortality rate. The effect may be in<br />
connection with changes on pulse wave velocity (PWV),<br />
which predicts cardiovascular morbidity and mortality. Longterm<br />
blockade of the RAAS may have a beneficial effect on<br />
the acceleration of atherosclerosis and uremic dyslipidemia in<br />
hemodialysis patients (5). Several recent morbidity and<br />
mortality trials with ARB’s provide an evidence-based<br />
rationale for the use of the drugs in patients with<br />
hypertension. Studies with comparison to conventional<br />
antihypertensive agents showed improved morbidity and<br />
mortality outcomes in patients with hypertension and left<br />
ventricular hypertrophy (Losartan ® ) and diabetes mellitus<br />
(Losartan ® and Irbesartan ® ) (13). Systemic and renal<br />
hemodynamic responses to acute AT1R blockade are, at least<br />
in part, genetically determined (12). The Seventh Report of<br />
the Joint National Committee on Prevention, Detection,<br />
Evaluation, and Treatment of High Blood Pressure<br />
emphasizes the urgent need to lower blood pressure to a goal<br />
of
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 25<br />
converting enzyme inhibitors alone or in combination for<br />
treatment of primary glomerulonephritis. Scand J Urol Nephrol<br />
2004; 38(5): 427-33<br />
10. Scheen AJ. Renin-angiotensin system inhibition prevents type<br />
2 diabetes mellitus. Part 1. A meta-analysis of randomised<br />
clinical trials. Diabetes Metab 2004; 30(6): 487-96<br />
11. Makris TK, Stavroulakis G, Papadopoulos DP. Eprosartan<br />
effect on fibrinolytic/hemostatic variables in arterial<br />
hypertension: a comparative study to losartan. Drugs Exp Clin<br />
Res 2004; 30(3): 125-32<br />
12. Spiering W, Kroon AA, Fuss-Lejeune MJ et al. Genetic<br />
contribution to the acute effects of angiotensin II type 1<br />
receptor blockade. J Hypertens 2005; 23(4): 753-8<br />
13. Vitale C, Mercuro G, Castiglioni C et al. Metabolic effect of<br />
telmisartan and losartan in hypertensive patients with metabolic<br />
syndrome. Cardiovasc Diabetol 2005; 15: 4(1): 6-9
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 26<br />
Prealbumin and inflammatory markers in dialysis patients<br />
S. Chrysostomou, 1 K. A. Poulia, 1 Y. Jeanes, 2 D. Perrea, 3 M. Poulakou, 3 B. Filiopoulos, 4<br />
D. Stamatiades 4 and Ch. P. Stathakis 4<br />
1 Department of Nutrition and Dietetics, Laikon General Hospital of Athens, 2 School of Human and Life Sciences, Roehampton<br />
University, UK, 3 Laboratory for Experimental Surgery and Surgical Research "Christeas Hall", University of Athens, 4 Division of<br />
Nephrology, General Hospital of Athens, Greece<br />
Abstract<br />
Inflammation is one of the main causes of high mortality and<br />
morbidity rates in patients with chronic renal failure treated<br />
with dialysis. In these cases, the use of anthropometric or<br />
biochemical markers alone, is not enough, but it is important<br />
to use the combination of them.<br />
The aim of this study is to evaluate serum prealbumin as an<br />
inflammatory and nutritional marker and determine whether<br />
there is an association between prealbumin and other<br />
anthropometric and biochemical markers.<br />
A total of 30, clinically stable dialysis patients (15 HD and 15<br />
PD) participated in the study. The investigated<br />
anthropometric and biochemical measurements of the study<br />
are body weight (BW), Body Mass Index (BMI), serum<br />
prealbumin, albumin, transferrin, C - reactive protein (CRP),<br />
creatinine, ferritin, Interleukin-6 (IL-6), cholesterol, Iron (Fe)<br />
and Prognostic Inflammatory and Nutritional index (PINI).<br />
There are no significant differences in age, duration of<br />
dialysis, dry weight and BMI between patients on HD or PD.<br />
Albumin is significantly lower in the PD group, whereas,<br />
transferrin and total cholesterol are significantly greater in the<br />
HD group. A higher percentage of the HD patients have<br />
inflammation with CRP>5g/l and IL-6>8.8ng/ml compared<br />
with the PD patients.<br />
According to the present study, prealbumin levels are lower<br />
in the PD group compared with the HD group but it is not<br />
significantly correlated with any of the investigated<br />
parameters, apart from ferritin, in the HD group. Moreover,<br />
further analysis showed that patients are malnourished<br />
independently whether they have inflammation or not.<br />
Key words: inflammation, dialysis, prealbumin, morbidity,<br />
mortality<br />
Introduction<br />
Inflammation is one of the main causes of high mortality and<br />
morbidity rates in patients with chronic renal failure treated<br />
with dialysis methods (1). In these cases, the use of<br />
anthropometric or biochemical markers alone, is not enough.<br />
It is very important to use the combination of them, in order<br />
to have more reliable assessment (1). Further studies in this<br />
area, are required to examine the association between<br />
markers of visceral protein stores, inflammatory markers and<br />
clinical outcomes, in dialysis patients (2).<br />
Prealbumin is a visceral protein with short half-life (2-3<br />
days), a rapid turnover and a simple method exists to measure<br />
serum levels (3). It is an earlier nutritional marker compared<br />
with serum albumin and more responsive to immediate<br />
changes in nutritional intake and clinical status than albumin.<br />
Although prealbumin is considered as a more sensitive index<br />
compared with albumin (4), it is not commonly used and its<br />
associations with other inflammatory and nutritional indices,<br />
during End Stage Renal Disease (ESRD), have not been well<br />
documented (4).<br />
Inflammation is a key determinant of serum prealbumin (an<br />
acute phase protein) (4). However, a few studies support that<br />
prealbumin is a reliable marker of inflammation but still more<br />
studies are required to confirm this hypothesis (2).<br />
The aim of this study is to evaluate serum prealbumin as an<br />
inflammatory and nutritional marker and determine whether<br />
there is an association between prealbumin and other<br />
anthropometric and biochemical markers. Furthermore, this<br />
study will compare the nutritional and inflammatory status<br />
between HD and PD patients, through prealbumin and other<br />
indices.<br />
Patients and methods<br />
The study is performed at the Outpatient Dialysis Unit at<br />
“Laikon” General Hospital (Athens, Greece). A total of 30<br />
dialysis patients (15 HD and 15 PD) participated in the study.<br />
Moreover, only clinically stable patients are included in this<br />
study.<br />
An Ethical approval is granted from University of Surrey<br />
Roehampton ethics committee and approval from the director<br />
of Laikon General Hospital of Athens.<br />
The investigated anthropometric and biochemical<br />
measurements of the study are body weight (BW), Body<br />
Mass Index (BMI), percentage body fat derived from skinfold<br />
thickness measurements (%BF) and serum prealbumin,<br />
albumin, transferrin, C - reactive protein (CRP), creatinine,<br />
ferritin, Interleukin-6 (IL-6), cholesterol, Iron (Fe) and<br />
Prognostic Inflammatory and Nutritional index (PINI). The<br />
investigated variables of this study are compared with the<br />
outcome goals for dialysis patients based on Kidney Disease<br />
Outcome Quality Initiative (K/DOQI). Inflammatory markers<br />
are compared with the laboratory reference ranges.<br />
BMI (in kilograms per meter²) is calculated from patient<br />
height and dry body weight. This study considers<br />
undernourished patients as those with BMI< 18.5 kg/m².<br />
The same observer took the anthropometric measurements,<br />
immediately before the dialysis session (weight empty of<br />
dialysis fluid). Skinfold measurement was taken at 4 sites in<br />
triplicate (triceps, biceps, superilliac and subscapular<br />
______________________<br />
Correspodence to: S. Chrysostomou, “Laikon” General Hospital of Athens, Department of Nephrology,<br />
Agiou Thoma 17, 11527, Athens-Greece
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 27<br />
skinfolds) using Harpenden callipers (Baty, British Indicators<br />
CE 0120). Percentage body fat was calculated using Durnin<br />
and Womersley equation.<br />
Non-fasting blood samples were taken before dialysis<br />
treatment for serum prealbumin, albumin, creatinine, ferritin,<br />
transferrin, IL-6, CRP, cholesterol and iron. All these<br />
parameters, apart from prealbumin and IL-6 immunoassays,<br />
were analysed on the day of sampling at the Department of<br />
Clinical Chemistry Laboratory at “Laikon” General Hospital.<br />
Prealbumin and IL-6 mmunoassays were performed at the<br />
laboratory for Experimental Surgery and Surgical Research<br />
“Christeas Hall”. Serum prealbumin was measured by a<br />
photometric enzyme-linked assay (ELISA, Immune<br />
Diagnostic, Cat. No: K 6331) and serum albumin was<br />
determined with a photometric method (bromcresol method,<br />
BCG-Olympus). Cholesterol was analysed by a photometric<br />
enzyme-linked assay with Olympus analysers (RA-XT 1000).<br />
Serum transferrin, iron and ferritin were analysed by<br />
Tholosimetry (Hitachi 912). CRP was analysed by<br />
nephelometry (SEAC, RADIM GROUP, DELTA) and High-<br />
Sensitive IL-6 was analysed by a photometric enzyme-linked<br />
assay (ELISA, Quantikine HS, Cat. No: HS 600B).<br />
The PINI value was calculated using markers from the<br />
biochemical tests, in the following equation: (C-reactive<br />
protein X alpha (1)-acid glycoprotein): (albumin x<br />
transthyretin) (16).<br />
The statistical programme SPSS for Windows (version 11.5)<br />
is used for data analysis. Results are presented as mean ±<br />
standard deviation (Mean ± SD). A P-value of 8.8ng/ml<br />
compared with the PD patients. Results are shown in Table 3.<br />
Table 3. Prevalence of inflammation based on CRP, IL-6 and<br />
ferritin cut off points, in our study-group<br />
Haemodialysis<br />
Group<br />
Peritoneal<br />
dialysis Group<br />
Marker of inflammation % %<br />
CRP (>5g/l) 46.7 40<br />
IL-6 (>8.8ng/ml) 53.3 30.8<br />
Ferritin Males<br />
(>400ng/ml)<br />
37.5 50<br />
Females<br />
(>150ng/ml)<br />
85.7 88.9<br />
The prevalence of malnutrition based only on prealbumin<br />
levels shows that a much higher percentage of PD patients<br />
are severely malnourished with prealbumin
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 28<br />
prevalence on malnutrition based on the other investigated<br />
variables is presented.<br />
Table 4. Prevalence of malnutrition based on prealbumin<br />
Haemodialysis<br />
Group<br />
Peritoneal dialysis<br />
Group<br />
Prealbumin<br />
(mg/ml)<br />
Percent<br />
Percent<br />
0-200 13 46<br />
200-300 0 23<br />
300+ 87 31<br />
Malnutrition and inflammation: Malnutrition indices are<br />
analysed against inflammation indices. In the current study, a<br />
patient is characterised as malnourished if he/she is found<br />
malnourished for at least one nutritional marker. Moreover, a<br />
patient is considered to have inflammation if he/she is found<br />
to have values above the cut-off points for of the<br />
inflammatory markers. A higher percentage of PD patients<br />
have both malnutrition and inflammation compared with the<br />
HD patients as shown in Table 6.<br />
Table 5. Prevalence of malnutrition based on Albumin, BMI,<br />
Creatinine, Cholesterol, Transferrin and % Body fat cut off point in<br />
our study-group<br />
Haemodialysis<br />
group<br />
Peritoneal<br />
dialysis<br />
group<br />
Marker of malnutrition Percent (%) Percent (%)<br />
Albumin (
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 29<br />
with any of the investigated parameters, apart from ferritin, in<br />
the HD group. Moreover, further analysis showed that<br />
patients are malnourished independently whether they have<br />
inflammation or not. None of the patients have inflammation<br />
without being malnourished at the same time.<br />
References<br />
1. Kaysen G. Malnutrition and the acute-phase reaction in dialysis<br />
patients-how to measure and how to distinguish. Nephrol Dial<br />
Transplant 2000; 15: 1521-1524<br />
2. Mehrotra R, Kopple J. Nutritional management of maintenance<br />
dialysis patients: why aren’t we doing better? Annual Review of<br />
Nutrition 2001; 21: 243-379<br />
3. Holland D, Meers C, Lawlor M et al. Serial prealbumin levels<br />
as predictors of outcomes in a retrospective cohort of peritoneal<br />
and hemodialysis patients. <strong>Journal</strong> of Renal Nutrition, 2002;<br />
11(3): 129-138<br />
4. Sreedhara R, Avram M, Blanco M et al. Prealbumin is the best<br />
nutritional predictor of survival in hemodialysis and peritoneal<br />
dialysis. Am J Kidney Dis 1996; 28: 937-942<br />
5. Qureshi A, Alvestrand A, Danielsson A et al. Factors<br />
predicting malnutrition in hemodialysis patients: A crosssectional<br />
study. Kidney Int, 1998; 53: 773-782<br />
6. Herzig K, Purdie D, Chang W et al. Is C-reactive protein a<br />
usefull predictor of outcome in peritoneal dialysis patients. J<br />
Am Soc Nephrol, 2001; 12: 814-821<br />
7. Owen W, Lowrie E. C-reactive protein as an outcome predictor<br />
for maintenance hemodialysis patients. Kidney Int 1998; 54:<br />
627-636<br />
8. Goldwasser P, Feldman J, Barth R. Serum prealbumin is higher<br />
in peritoneal dialysis than in hemodialysis: A meta-analysis.<br />
Kidney International 2002; 62: 276-281<br />
9. Chumlea C, Dwyer J, Bergen C et al. Nutritional status<br />
assessed from anthropometric measures in the HEMO study.<br />
<strong>Journal</strong> of Renal Nutrition, 2003; 13(1): 31-38<br />
10. Kooistra M, Niemantsverdriet E, Van Es A et al. Iron<br />
absorption in erythropoietin-treated hemodialysis patients:<br />
effects of iron availability, inflammation and aluminium.<br />
Nephrol Dial Transplant 1998; 13: 82-88
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 30<br />
Liver and kidney damage in acute poisonings<br />
M. Mydlik and K. Derzsiova<br />
Nephrological Clinic, Faculty Hospital of L. Pasteur, Kosice, Slovak Republic<br />
Abstract<br />
In the paper the retrospective analysis of simultaneous<br />
damage of liver and kidneys after acute carbon tetrachloride<br />
poisoning in 60 patients, after mushroom poisoning (Amanita<br />
phalloides) in 81 patients and after ethylene glycol poisoning<br />
in 20 patients from the view of differential diagnosis,<br />
conservative, intra- and extracorporeal elimination therapy is<br />
described. Acute toxic hepatitis with the different degree of<br />
severity was present in all patients and even acute renal<br />
failure was present in some patients. After acute carbon<br />
tetrachloride poisoning acute hepatitis developed<br />
approximately simultaneously with the development of acute<br />
renal failure. After acute Amanita phalloides poisoning acute<br />
toxic hepatitis, which was the cause of death in liver coma in<br />
16 patients, quickly developed in the foreground of the<br />
clinical picture. Renal damage was less frequent and it was<br />
not the cause of death even in one patient. After acute<br />
ethylene glycol poisoning acute renal failure dominated with<br />
severe metabolic acidosis, oxaluria and leucocytosis, acute<br />
toxic hepatitis was less severe. After ethylene glycol<br />
poisoning 3 patients died in the period before the use of the<br />
bicarbonate haemodialysis was possible. During 30 years the<br />
intra- and extracorporeal elimination therapy qualitatively<br />
developed (bicarbonate haemodialysis, haemoperfusion<br />
through active charcoal and other sorbents, plasmapheresis,<br />
haemofiltration), which participates to the significant degree<br />
on the recovery and improvement of the prognosis of patients<br />
after acute poisonings with simultaneous damage of liver and<br />
kidneys.<br />
Key words: acute poisoning, carbon tetrachloride,<br />
mushroom (Amanita phalloides), ethylene glycol, hepatic<br />
and renal damage, extracorporeal elimination therapy<br />
Introduction<br />
Simultaneous damage of liver and kidneys in acute poisoning<br />
occurs very often in present times (Table 1). This fact is very<br />
important from the diagnostic, differential diagnostic and<br />
therapeutic point of view (1-6). Besides that a damage of<br />
other organs after acute poisoning can cause multiorgan<br />
failure in patients previously healthy (2,5). This finding is<br />
very important in patients with preceding illness (2,7,8).<br />
The aim of the study was the retrospective analysis of 60<br />
patients after carbon tetrachloride poisoning, of 81 patients<br />
after mushroom poisoning (Amanita phalloides) and of 20<br />
patients after ethylene glycol poisoning with the liver and<br />
kidney damage from the diagnostic, differential diagnostic,<br />
conservative, intra- and extracorporeal elimination treatment<br />
Table 1. Simultaneous damage of liver and kidneys in acute<br />
poisonings<br />
Acute<br />
Damage of<br />
poisoning Liver Kidneys<br />
1. Carbon tetrachloride + +<br />
2. Dichlorethane + +<br />
3. Ethylene glycol + +<br />
4. Paraquat, Diquat + +<br />
5. Mushroom + +<br />
(Amanita phalloides)<br />
6. Arsenic hydride + +<br />
7. Mercury chloride - +<br />
8. Trichloroethylene + -+<br />
9. Paracetamol + -+<br />
10. Carbamazepine -+ -<br />
11. Isoniazid + -<br />
12. Other -+ -+<br />
Patients and Methods<br />
Sixty men, mean age was 41±9 years, after carbon<br />
tetrachloride poisoning were investigated. Among them 52<br />
patients were poisoned by inhalation way and 8 patients<br />
drunk carbon tetrachloride in mistake of other drinks. At the<br />
beginning of acute poisoning dyspeptic syndrome was<br />
dominated, especially after oral poisoning. All patients used<br />
ethylalcohol for „the treatment of acute dyspepsia“. Use of<br />
ethylalcohol potentiated carbon tetrachloride poisoning<br />
(2,7,8). Clinical and laboratory signs after acute carbon<br />
tetrachloride poisoning from liver damage were present<br />
earlier ( several hours or days) in comparison to the signs of<br />
kidney damage. From that reason one third of poisoned<br />
patients was admitted to the Clinic for Infection Diseases in<br />
Faculty Hospital, Košice or to the other Departments of<br />
Infection Diseases in Eastern Slovakian region. That<br />
diagnostic mistake was caused by insufficient anamnesis,<br />
minimization of the contact with carbon tetrachloride by<br />
patients or deliberate concealment of the contact with that<br />
poison. Carbon tetrachloride is a very good lipid solvent and<br />
in the past it was used in home setting and in many<br />
workplaces (1,7,8). Except this carbon tetrachloride was<br />
used as a filling in fire-extinguishers (2).<br />
Eighty-one patients were investigated after mushroom<br />
poisoning (Amanita phalloides), mean age was 30.5±9 years.<br />
Among them were 28 children and 53 adult patients. Clinical<br />
and laboratory signs after acute poisoning of Amanita<br />
phalloides were present first of all during the several hours as<br />
an acute dyspepsia with the rapid increase of serum bilirubin<br />
and of activity of serum transaminases. Acute renal failure<br />
developed later or was not present. All acute poisoning<br />
caused by Amanita phalloides were accidental except one<br />
point of view.<br />
______________________<br />
Correspondence to: M. Mydlik, Nephrological Clinic, Faculty Hospital of<br />
L. Pasteur, Rastislavova 43, 041 90 Košice, Slovak Republic; E-mail: k.derzsiova@ fnlp.sk
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 31<br />
young lady, who ate Amanita phalloides in attempted suicide<br />
(3,9,10).<br />
The third group of patients were 20 patients after ethylene<br />
glycol poisoning. Mean age was 41± 8 years, among them<br />
were 2 women and 18 men. Ethylene glycol was the most<br />
frequent oral poisoning in a form of antifreeze agent which<br />
was used in the cars. That poison was used frequently in the<br />
change for ethylalcohol or from „ absence of ethylalcohol<br />
drinks“ in three soldiers. Ethylene glycol is a very dangerous<br />
poisoning nowadays and it is relatively frequent in our<br />
country in present times (3,5,6,11,12).<br />
In three groups of patients with those poisonings all available<br />
diagnostic and therapeutic methods were used including<br />
various forms of intra-and extracorporeal elimination<br />
methods (1-8,10-16). In the treatment of carbon tetrachloride<br />
poisoning we did not use a hyperbaric oxygen therapy (17).<br />
Results<br />
Clinical signs and some laboratory parameters, conservative<br />
and intra-and extracorporeal elimination treatment in the<br />
patients after carbon tetrachloride, mushroom (Amanita<br />
phalloides) and ethylene glycol poisonings were described in<br />
Tables 2-4.<br />
Table 2. Liver damage in acute poisoning<br />
Poisoning Number of Hepatomegaly Bi Serum AST Coma<br />
patients<br />
(µmol/L) ALT (µkat/L)<br />
1. Carbon tetrachloride 60 57 78.4±20.5 16.2±3.3 - 4<br />
2. Mushroom<br />
81 81 76.8±14.1 89.5±12.4 88.7±12.8 16<br />
(Amanita phalloides)<br />
3. Ethylene glycol 20 16 17.5± 2.0 1.23± 0.45 1.12±0.4 5<br />
Bi-bilirubin<br />
Table 3. Kidney damage in acute poisoning<br />
Poisoning Number of<br />
patients<br />
Proteinuria<br />
(g/24h)<br />
K<br />
(mmol/L)<br />
Serum<br />
Urea<br />
Creatinine<br />
(µmol/L)<br />
Metabolic<br />
acidosis (pH)<br />
1. Carbon tetrachloride 60 57 78.4±20.5 16.2±3.3 - 4<br />
2. Mushroom<br />
81 81 76.8±14.1 89.5±12.4 88.7±12.8 16<br />
(Amanita phalloides)<br />
3. Ethylene glycol 20 16 17.5± 2.0 1.23± 0.45 1.12±0.4 5<br />
Table 4. Intra-and extracorporeal elimination therapy in acute poisoning<br />
Poisoning<br />
Number of Intra-and extracorporeal elimination therapy<br />
patients PD HD ET HP PF<br />
Mortality<br />
1. Carbon tetrachloride 60 8 81 6 - 4 2 (3.3%)<br />
2. Mushroom<br />
81 - 20 2 128 23 24 (29.6%)<br />
(Amanita phalloides)<br />
3. Ethylene glycol 20 - 28Ac+147Bic - 5 - 3 (15%)<br />
PD-peritoneal dialysis, HD-haemodialysis, Ac-acetate, Bic-bicarbonate, ET-exchange transfuzion,<br />
HP-haemoperfusion, PF-plasmapheresis<br />
Discussion<br />
In differential diagnosis of the patients with simultaneous<br />
damage of the liver and kidneys, a direct anamnesis of<br />
patients is very important, but also an indirect anamnesis<br />
from family members or from co-workers. It is necessary to<br />
distinguish acute viral hepatitis from acute carbon<br />
tetrachloride poisoning, from poisoning by dichloroethane,<br />
mushroom poisoning (Amanita phalloides), arsenic hydride,<br />
ethylene glycol and from acute leptospirosis (1-3, 5,6,8-<br />
10,12,16,18). After acute paraquat poisoning and<br />
simultaneously with a damage of the liver and kidneys,<br />
the damage of lung and heart is developed. The patient who<br />
is insufficiently treated after paraquat poisoning is dying<br />
during the following 10-14 days. Cause of death after that<br />
poisoning is alveolocapillary block in the lung (19,20). Acute<br />
arsenic hydride poisoning in our department was not present<br />
during the last 35 years (5,21-23). Acute mercury chloride<br />
poisoning leads to acute renal failure without liver damage<br />
(5). Acute trichloroethylene poisoning is manifested by<br />
cerebral and liver damage. Damage of the kidneys is very<br />
rare but it was described (24). Acute paracetamol poisoning<br />
leads to liver damage, but kidney damage in some patients<br />
was also described (25-27). After oral carbamazepine<br />
poisoning important liver damage was observed (28). Liver<br />
damage after isoniazid poisoning was also observed. High<br />
intravenous dose of pyridoxine (5g/24 h) as an antidote in<br />
that poisoning was recommended (5). We successfully used<br />
this therapy in one our patient after severe isoniazid<br />
poisoning.<br />
Acute toxic hepatitis dominated in the first group of patients<br />
who were poisoned by carbon tetrachloride, in four of them<br />
developed liver coma. Two patients suffering from preceding<br />
chronic hepatitis died in liver coma despite of the use of<br />
repeated haemodialyses and exchange transfusions.<br />
Anamnestic serum titres against Leptospira grippotyphosa<br />
were found in one patient suffering from acute carbon<br />
tetrachloride poisoning and in another patient with the same<br />
poisoning acute leptospirosis developed caused by Leptospira<br />
sejr. Dynamics of titres testified to acute illness (2).<br />
Determination of serum titres against leptospirosis was very<br />
important especially in the patients from agricultural region.<br />
Uremic syndrome as a sign of acute renal failure in acute<br />
carbon tetrachloride poisoning developed relatively slowly in<br />
comparison to other acute poisonings (2). Duration of acute<br />
carbon tetrachloride poisoning until to restore to normal of<br />
hepatic tests and of renal functions was in average 39±9 days.<br />
The treatment of carbon tetrachloride poisoning included: use
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 32<br />
of hepatotropic drugs, forced diuresis, repeated<br />
haemodialyses, peritoneal dialysis and in patients in liver<br />
coma we used exchange transfusions and later<br />
plasmaphereses (2,8). Occurrence of acute tetrachloride<br />
poisoning is very rare in the last years, because it was due to<br />
prohibition to use of carbon tetrachloride in fireextinguishers,<br />
in industry and in various chemical<br />
laboratories.<br />
In the second group of 81 patients, who were poisoned by<br />
mushroom (Amanita phalloides), acute toxic hepatitis<br />
developed rapidly until to liver insufficiency and coma. From<br />
this group of patients 24 patients (29,6%) died in liver coma.<br />
Damage of the kidneys after Amanita phalloides poisoning<br />
was less frequent, despite that in 16 patients acute tubular<br />
necrosis with kidney failure developed. No one patient died<br />
caused by acute renal failure. That dissociation of liver and<br />
kidney damage is characteristic for hepatotoxic type of acute<br />
mushroom poisoning. Conservative treatment including of<br />
hepatic drugs and of forced diuresis and especially of<br />
extracorporeal elimination therapy we used relatively late for<br />
the late admission of the patients to our renal unit (in average<br />
53 hours after poisoning).<br />
During many years we tried to use early haemodialysis,<br />
charcoal haemoperfusion, Amberlite XAD-2 and XAD-4<br />
haemoperfusions and in the last years plasmapheresis which<br />
is the bridge to liver transplantation. Haemodialysis was used<br />
on the influence of uremic syndrome (3,5,9,10,13,14).<br />
In the third group of patients with acute ethylene glycol<br />
poisoning dominated severe metabolic acidosis, leucocytosis,<br />
oxaluria and various neurological symptoms. Leucocytosis<br />
was present from the onset of acute poisoning caused by<br />
ethylene glycol irritation of the bone marrow and duration of<br />
that laboratory sign was in average 7 days. Damage of the<br />
kidneys with relatively slow development of acute renal<br />
failure showed for the important disturbances of renal<br />
functions. Damage of the liver with hepatomegaly and<br />
increase of serum activity of alanine aminotransferase were<br />
less important and occurred in 16 patients (11,12).<br />
Dissociation of the liver and kidney damage was present after<br />
ethylene glycol poisoning in disadvantage for the kidney<br />
damage. In the medical treatment of ethylene glycol<br />
poisoning were applicated hepatic drugs including of the<br />
group of vitamin B. The therapeutic method of choice in<br />
ethylene glycol poisoning was in the last years bicarbonate<br />
haemodialysis using 100 mg% ethylalcohol in dialysis<br />
solution. Ethylalcohol was used as a blocker of<br />
alcoholdehydrogenase in metabolic transformation from<br />
ethylene glycol to glycol aldehyde. Two patients died after<br />
ethylene glycol poisoning before the possibility to use<br />
bicarbonate haemodialysis and one patient died for the late<br />
admission to our dialysis unit (11,12).<br />
At the end of this retrospective study it is neccessary to say,<br />
that the review of simultaneous damage of the liver and<br />
kidneys after carbon tetrachloride poisoning, mushroom<br />
poisoning (Amanita phalloides) and ethylene glycol<br />
poisoning contributed to diagnosis, differential diagnosis and<br />
also to the use of various forms of extracorporeal elimination<br />
therapy. In the near future several new forms of<br />
extracorporeal elimination therapy will be used in the<br />
treatment of acute poisoning i.e. albumin dialysis and the use<br />
of new sorbents for toxins removal mainly for toxins with<br />
high albumin and other proteins binding in plasma (29-31).<br />
References<br />
1. Jaros F. Practical toxicology. 1st eds. Martin: Osveta, 1988;<br />
200 p.<br />
2. Mydlik M, Takac M, Melnicak P et al. Diagnosis and therapy<br />
of carbon tetrachloride poisonong. Vnitr Lek 25, 1979; 7: 672-9<br />
3. Mydlik M, Derzsiova K. Use of hemoperfusion in acute<br />
poisoning: Clinical analysis of 229 patients. In: D.<br />
Falkenhagen, H. Klinkmann, E. Piskin, K. Opatrny, Jr. (eds):<br />
Blood-Material Interaction. A basic guide from polymer<br />
science to clinical application. S 149- S 153. INFA 1998,<br />
Glasgow, Krems, 156 p.<br />
4. Mydlik M, Derzsiova K, Mizla P. Use of plasmapheresis in<br />
dialysis centre - - analysis of 105 patients. Akt Nefrol 8, 2002;<br />
1: 9-13<br />
5. Seyfart G. Poison Index. The treatment of acute intoxication.<br />
1st ed. Pubst Science Publisher, Lengerich, Berlin, Düsseldorf<br />
et al. 1997; 664 p.<br />
6. Sevcik M. Practical toxicology. IIIrd ed. Státní zdravotnické<br />
nakladatelství, Prague 1968; 350 p.<br />
7. Mydlik M, Halko N. Use of exchange transfusion in acute<br />
poisonings. Prakt Lék 59, 1979; 22: 846-9<br />
8. Mydlik M, Derzsiova K, Mizla P. Diagnosis and treatment of<br />
carbon tetrachloride poisoning – analysis of 60 patients.<br />
Abstract of the XIIth International Congress of Nephrology, p.<br />
286. Jerusalem, Israel, 1993; 13-18<br />
9. Mydlik M, Derzsiova K, Mizla P et al. Use of haemoperfusion<br />
in acute mushroom poisoning. Clinical analysis of 58 patients.<br />
Cas Lek Ces 132, 1993; 15: 464-7<br />
10. Mydlik M, Derzsiova K, Klan J et al. Haemoperfusion with<br />
alpha-amanitin – an in vitro study. Int J Artif Organs 20, 1997;<br />
2: 105-7<br />
11. Mydlik M, Melnicak P, Derzsiova K et al. Dialysis therapy of<br />
acute renal failure. Analysis of 230 patients. Cas Lek Ces 118,<br />
1979; 18: 559-63<br />
12. Mydlík M, Derzsiová K, Mizla P et al. Diagnosis and therapy<br />
of acute ethylene glycol poisoning – analysis of 20 patients.<br />
Vnit Lék 48, 2002; 11: 1054-9<br />
13. Enjabert F, Rapior S, Nouguier-Soule J et al. Treatment of<br />
amatoxin poisoning: 20–-year retrospective analysis. J Toxicol<br />
Clin Toxicol 40, 2002; 6: 715-57<br />
14. Galmarini D, Tarenzi L, Cantaluppi P et al. Acute hepatic<br />
failure and renal damage. Experimental and clinical studies.<br />
Minerva Med 30, 1978; 69: 1417-26<br />
15. Markiewicz K, Trznadel K, Szeszko A. Acute carbon<br />
tetrachloride poisoning. Med Pr 28, 1977; 1: 15-20<br />
16. Svendsen B S, Gjellestrand A, Eivindson G et al. Serious<br />
mushroom poisoning by Cortinarius and Amanita virosa.<br />
Tidsskr Nor Laegeforen 122, 2002; 8: 777-80<br />
17. Burkhart K K, Hall A H, Gerace R et al. Hyperbaric oxygen<br />
treatment for carbon tetrachloride poisoning. Drug Saf 6, 1991;<br />
5: 332-8<br />
18. Nehoda H, Wieser C Koller J et al. Recurrent liver failure with<br />
severe rhabdomyolysis after liver transplantation for carbon<br />
tetrachloride intoxication. Hepatogastroenterology 45, 1998;<br />
19: 191-5<br />
19. Fernandez P, Bermejo A M, Lopez-Rivandulla M et al. A fatal<br />
case of parenteral paraquat poisoning. Forensic Sci Int 49,<br />
1991; 2:215-24<br />
20. Melnicak P, Mydlik M. Poisoning by Gramoxon (paraquat).<br />
Proceedings of the „Industrial toxicology 78“, Bratislava 21.-<br />
24. VI. 1978, p. 147-57, Zilina, House of Technique SVTS<br />
Žilina – 55/78, 308 p.<br />
21. Labadie H, Stoessel P, Callard P et al. Hepatic venoocclusive<br />
disease and perisinusoidal fibrosis secondary to arsenic<br />
poisoning. Gastroenterology 99, 1990; 4: 1140-43<br />
22. Lin J M, Jiang CQ. Clinical manifestation and ultrasonic<br />
characteristic of five patients with acute arsenic poisoning.<br />
Zhonguhua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 21, 2003;<br />
6: 420-2
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 33<br />
23. Mathieu D, Mathieu-Nolf M, Germain-Alonso M et al.<br />
Massive-arsenic poisoning--effect of hemodialysis and<br />
dimercaprol on arsenic kinetics. Intensive Care Med 18, 1992;<br />
1: 47-50<br />
24. David NJ, Wolman R, Milne FJ et al. Acute renal failure due to<br />
trichlorethylene poisoning. Brit J Ind Med 46, 1989; 5:347-9<br />
25. Derzsiová K, Mydlík M, Petríková V et al. Haemoperfusion of<br />
paracetamol – an in vitro study. Akt Nefrol 8, 2002; 4: 129 –32<br />
26. Herrero J L, Castellano I, Gomez-Martino J R. Acute kidney<br />
failure caused by paracemol poisoning. Nefrologia 21, 2001; 6:<br />
592-5<br />
27. Jones A F, Vale J A. Paracetamol poisoning and the kidney. J<br />
Clin Pharm Ther 18, 1993; 1: 5-8<br />
28. Hopen G, Nesthus I, Laerum OD. Fatal carbamazepinassociated<br />
hepatitis. Report of two cases. Acta Med Scand 210,<br />
1981; 4: 333-5<br />
29. Sen S, Ytrebo LM, Rose C et al. Albumin dialysis: a new<br />
therapeutic strategy for intoxication from protein-bound drugs.<br />
Intensive Care Med 30, 2000; 3: 496-501<br />
30. Senf R, Klingel R, Kurz S et al. Bilirubin-adsorption in 33<br />
critically ill patients with liver failure. Int J Artif Organs 27,<br />
2004; 8: 717-22<br />
31. Wu BF, Wang MM. Molecular adsorbent recirculating system<br />
in dealing with maternal Amanita poisoning during the second<br />
pregnancy trimester: a case report. Hepatobiliary Pancreat Dis<br />
Int 3, 2004; 1: 152-4
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 34<br />
Vascular calcifications in patients on hemodialysis<br />
T. Damjanovic¹, N. Markovic², S. Djorovic³, T. Djordjevic¹ and N. Dimkovic¹<br />
¹Center for Renal Diseases, ²Cardiology Department, ³Radiology Department,<br />
Zvezdara University Hospital, Belgrade, Serbia and Montenegro<br />
Abstract<br />
Vascular calcifications (VC) in ESRD patients are strongly<br />
associated with cardiovascular morbidity and mortality.<br />
There are two different types of VC: arterial media<br />
calcifications (AMC), a non occlusive condition, related to a<br />
mineral metabolism disturbances, and atherosclerosis with<br />
intima calcifications (AIC) of atherosclerotic plaques. The<br />
aim of this study was to evaluate arterial and intima<br />
calcifications by plain radiography and B-mode<br />
ultrasonography in HD patients, and to analyze potential risk<br />
factors on their appearance. Study included 73 HD patients<br />
(33 males), mean (±SD) age 54,30±8,52 years, and HD<br />
duration of 115,56±60,32 months. AMC were detected by<br />
plain radiography of pelvis, hands and region of vascular<br />
access. AIC were detected by B-mode ultrasonography of<br />
common carotid arteries. The influence of potential risk<br />
factors (age, gender, HD duration, diabetes, Ca, P product,<br />
plasma phosphorous, total cholesterol and albumen) on the<br />
appearance of overall AMC, AMC in different regions and<br />
AIC was also analyzed.<br />
AMC were detected in 41(56,2%) patients: in pelvis<br />
26(35,3%), hands 7(9,6%), and in region of vascular access<br />
28(38,4%). In group of patients with overall VC detected by<br />
plain radiography, there was a strong association with male<br />
gender (p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 35<br />
Results<br />
The frequency of owerall arterial media calcifications<br />
evaluated by plain radiography was in 56% of HD patients<br />
(Figure 1).<br />
Fig 1. Frequency of arterial media calcifications evaluated by plain<br />
radiography<br />
w/o AMC<br />
44%<br />
AMC<br />
56%<br />
access were significantly younger (51,68±8,71 vs.<br />
55,82±8,07; p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 36<br />
Is there a seasonal variation in mortality in hemodialysis patients?<br />
J. Popovic, N. Dimkovic, Z. Djuric, G. Popovic and N. Lazic<br />
Centre for Renal Diseases, Zvezdara University Hospital, Belgrade, Serbia and Montenegro<br />
Abstract<br />
Mortality rates among hemodialysis (HD) patients differ<br />
considerably between and within countries.<br />
The aim of this study was to analyze overall and specific<br />
mortality in patients on regular hemodialysis during the last 8<br />
years (1997-2004) and to investigate possible monthly and<br />
seasonal fluctuations in deaths.<br />
Baseline demographic characteristics together with primary<br />
renal disease, previous treatment with peritoneal dialysis,<br />
cause as well as month and season of death were observed.<br />
Seasons were divided into four periods: December-February<br />
(winter), March-May (spring), June-August (summer) and<br />
September-November (autumn).<br />
Total of 254 HD patients (59 % males) who died from 1997<br />
to 2004 were included; overall mean age was 62.1 ± 11.2<br />
years (range 27-88), with 47.6% aged over 65 (60% in 2004);<br />
age significantly increased from 59.4 ± 13.1 years in 1997 to<br />
66.0 ± 7.5 years in 2004 (p< 0.05). Even so, mortality rate<br />
decreased from 17.2% in 1997 to 9.2% in 2004. The mean<br />
HD duration was 72.6 ± 68.9 months; 18.9% of patients were<br />
previously on peritoneal dialysis (highest distribution in 2004<br />
i.e. 25%). The difference in seasonal mortality throughout the<br />
whole observation period was statistically insignificant. Still,<br />
higher frequency was observed in summer and winter periods<br />
(28.3% and 27.2% respectively) with mortality peaks in June<br />
and December (11% each). The leading cause of death in<br />
both months was cardiac disease (50% and 46.4%).<br />
Throughout the whole period cardiac diseases were the main<br />
cause of death (46.1%, X²=230.08; p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 37<br />
Table 1. Baseline demographic characteristics by the year<br />
PATIENTS 1997<br />
N=39<br />
1998<br />
N=30<br />
1999<br />
N=33<br />
2000<br />
N=32<br />
2001<br />
N=37<br />
2002<br />
N=26<br />
2003<br />
N=37<br />
2004<br />
N=20<br />
TOTAL<br />
N=254<br />
Age (years ± SD) 59.4 ±<br />
13.1<br />
62.9 ±<br />
11.7<br />
62.7 ±<br />
11.6<br />
62.5 ±<br />
12.8<br />
60.5 ±<br />
12.2<br />
63.0 ±<br />
7.7<br />
62.5 ±<br />
9.8<br />
66.0 ±<br />
7.5*<br />
62.1 ±<br />
11.2<br />
Age (range) 32- 88 43– 87 44– 79 27– 81 29– 79 48– 81 36– 78 49– 77 27 – 88<br />
% 65 + 38.5 50 51.5 50 46 38.5 51.4 60 47.6<br />
Sex (M/F) 18/21 19/11 20/13 15/17 26/11 16/10 22/15 14/6 150/104<br />
Months on HD ±<br />
SD<br />
56.4 ±<br />
61.6<br />
64.7 ±<br />
73.6<br />
66.8 ±<br />
69.1<br />
98.9 ±<br />
78.5<br />
85.0 ±<br />
86.1<br />
65.3 ±<br />
39.0<br />
84.6 ±<br />
65.3<br />
47.8 ±<br />
45.3<br />
72.6 ±<br />
68.9<br />
Range 3-267 4-281 4-250 4-344 4-328 5-146 6-258 4-165 3-344<br />
% prior on PD 17.9 13.3 24.2 15.6 21.6 11.5 21.6 25 18.9<br />
* t = 2.049 ; p< 0.05<br />
Results<br />
Demographic characteristics<br />
Baseline demographic characteristics of 254 deceased HD<br />
patients observed in the period from 1997 to 2004 are listed<br />
in Table 1.<br />
HD patients that died in 1997 were younger than in following<br />
years (significantly so in comparison to 2004, p< 0.05).<br />
Despite that mortality rate decreased from 17.2% in 1997 to<br />
9.2% in 2004. Highest percentage of patients aged over 65<br />
was also observed in 2004 (60%; overall for the whole period<br />
47.6%). Patients deceased in 2004 were also older at the<br />
initiation of HD. The frequency of patients previously treated<br />
with peritoneal dialysis (PD) varied from 13.3% to 25%<br />
(overall 18.9%). Higher proportion of males for the whole<br />
period was observed (59%).<br />
Fig 1. Percentage of deceased by seasons<br />
Number of deaths<br />
%<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
Seasonal mortality<br />
p=ns<br />
Seasonal analysis of deaths<br />
The seasonal peaks of deaths for the whole 8-year period<br />
were found in summer and winter months (28.3% and 27.2%<br />
respectively). The difference between seasons was<br />
statistically insignificant (X²= 4.075; p=ns).<br />
The frequency of deaths by seasons is shown on Figure 1.<br />
Analysis of causes of death for the whole observed period<br />
revealed cardiac causes as the main cause of death in HD<br />
population (46.1% of deaths), followed by cerebrovascular<br />
(11%) and infection-sepsis accounting for 9.8% of deaths.<br />
The difference is highly significant (X²=230.08; p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 38<br />
April (lowest, i.e. 5.1%), followed by the increase to the<br />
highest percentage in June (11%) with the drop in summer<br />
and autumn months characterized by narrow variations, and a<br />
peak again in December (11% -equal to the one in June).<br />
(Figure 3).<br />
Fig 3. Monthly deaths in HD population<br />
Percentage of death in HD patients<br />
per month<br />
12<br />
10<br />
%<br />
8<br />
6<br />
4<br />
2<br />
0<br />
1 2 3 4 5 6 7 8 9 10 11 12<br />
Month<br />
Leading cause of death in both peak months was cardiac<br />
(50% in June and 46.4% in December, slightly above the<br />
overall percentage for this cause). The occurrence of<br />
cerebrovascular deaths was more prominent in June (17.9%),<br />
much more than overall, and especially so than in December<br />
(3.6%). Infection was equally distributed in both peak months<br />
(10.7%), i.e. slightly above the overall frequency.<br />
The analysis of sex difference in seasonal mortality revealed<br />
higher proportion of males in summer months (65.3%) in<br />
comparison to overall Figure, almost equal gender<br />
distribution in spring (52% male, 48% female) and similar<br />
frequency in gender distribution as in the whole observed<br />
period for winter and autumn months (55.1% and 61.9%<br />
respectively). Statistically, difference in gender mortality by<br />
seasons was insignificant (X² = 2.994; p > 0.05).<br />
Deceased in winter and autumn months (64.0 and 63.1) were<br />
older than in spring and summer (both 60.6), but without<br />
significance (F=1.46; p > 0.05).<br />
Patients who died in autumn had been receiving hemodialysis<br />
longer (82.5 months) than the ones deceased in winter (66.6),<br />
spring (75.0) and summer (68.1).The difference was not<br />
significant (H=1.990; p > 0.05).<br />
Deceased patients with hypertensive nephrosclerosis as the<br />
primary renal disease represented the highest proportion for<br />
the whole observed period (38.6%), followed by diabetes<br />
(18.9%), pyelonephritis (14.2%), glomerulonephritis (10.2%)<br />
and polycystic kidney disease (7.5%). The difference is<br />
highly significant (X² = 216.029 ; p< 0.01). Analysis of renal<br />
diagnoses in relation to seasonal variations of deaths did not<br />
show significant difference for none of the primary etiologies<br />
of ESRD.<br />
Discussion<br />
Mortality rate among our HD population in the first year<br />
analyzed (1997) was somewhat higher than reported by<br />
European DOPPS and ERA-EDTA for the similar period<br />
(1,2) and lower than the rate in Yugoslavia (5). Although<br />
mortality rate varies across countries this speaks more in<br />
favor of the variations across facilities, even more so for the<br />
following years.<br />
Mortality rate in our HD population dropped to 9.2% in 2004<br />
despite significant increase in age from 1997 to 2004. Also,<br />
60% of patients died in 2004 were aged over 65 years.<br />
Numerous studies showed the association between older age<br />
and increased risk of mortality (1,3,6,7), with the risk of<br />
death increasing by 3% to 4% per year (1). USRDS (12)<br />
reported expected remaining life span for dialysis patients<br />
from 7 to 10 years in aged 40 to 44, and 4 to 5 years for those<br />
60 to 64 years of age. As for the analysis by the seasons,<br />
patients that died in autumn and winter were older, but<br />
insignificantly.<br />
Our results did not show significant difference in mortality<br />
between males and females. In DOPPS (1) gender also did<br />
not predict survival, contrary to the findings of Marcelli et al<br />
(7) where women had better survival rate.<br />
We observed significant difference in mortality when<br />
analysing primary etiologies of ESRD, leading diagnosis<br />
being hypertensive nephrosclerosis (38.6%). This is almost<br />
identical to the prevalence of hypertensive nephrosclerosis in<br />
our HD population (constantly between 30% and 38.8%) (8).<br />
Diabetes as the cause of renal failure represented the second<br />
largest proportion of deceased (18.9%) which is in contrast to<br />
their prevalence in our Centre in observed period (despite its<br />
steadily increase from 7.9% to 11.7%) (9). DOPPS (1)<br />
identified diabetes as one of co-morbid factors significantly<br />
associated with mortality. Five-year survival in patients with<br />
diabetic nephropathy as an underlying renal disease is only<br />
20% (13,14). Ten-year survival is less likely for diabetics in<br />
comparison to nondiabetics (4% vs. 11-14%) (12). Lower<br />
percentage in deaths than its prevalence in our HD population<br />
was observed for following diagnoses: glomerulonephritis<br />
(10.2% vs. 16.8%) and polycystic kidney disease (7.5% vs.<br />
10.7%). Studies reported the best five-year survival in<br />
dialysis patients with respect to underlying renal disease in<br />
glomerular diseases and polycystic kidney disease,<br />
intermediate with hypertension-induced renal disease, and<br />
worst with diabetic nephropathy (12,13). There was no<br />
seasonal variation in deaths with respect to primary etiologies<br />
of ESRD in our patient group.<br />
Association between longer dialysis duration and enhanced<br />
risk of death is well established. Each year on dialysis<br />
increases the risk of death by approximately 6% (19). Our<br />
data showed insignificant difference between seasons with<br />
respect to length of HD.<br />
Higher percentage of deaths occurred in winter and summer<br />
but seasonal variations in deaths were insignificant. The<br />
analysis of monthly deaths revealed two peaks - June and<br />
December. Similar results were reported for HD patients by<br />
UK survey with the peak only in December (11). It was<br />
concluded that the earlier peak in deaths on dialysis<br />
compared to the general population was probably due to a<br />
cardiac peak as the main cause of death in the dialysis<br />
population. Studies (12,15-18) have identified major causes<br />
of death in dialysis population as: cardiovascular disease,<br />
infection, and withdrawal from dialysis. Cardiac cause was<br />
also the leading cause of death in our HD population<br />
(46.1%), somewhat more so than overall in both peak<br />
months. USRDS (12) reported that cardiovascular disease<br />
accounts for approximately 50% of deaths, without the<br />
tendency to decline. Cerebrovascular death, as the second<br />
overall single cause in our population, occurred more<br />
frequently in June. Infection, mostly related to vascular<br />
access, is responsible for 9.8% of deaths in our group, less<br />
common than 15-20% reported elsewhere (15,17). It was<br />
equally represented in both peak months. Withdrawal from<br />
dialysis is by no means feature in our HD population.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 39<br />
Analysis of seasonal fluctuations of deaths by cause did not<br />
show significant difference.<br />
Conclusions<br />
Mortality rate in our Centre decreased considerably in<br />
observed period despite the increase in patients` age.<br />
Insignificant seasonal variations were observed for sex,<br />
primary renal disease, age and HD duration.<br />
This mortality analysis in our HD center revealed different<br />
percentage of deaths between the seasons with higher<br />
occurrence in summer and winter. Two months were<br />
especially pinpointed- June and December. The reasons for<br />
this have yet to be elicited.<br />
It is advisable to keep elderly patients with cardiovascular<br />
diseases in focus during autumn and winter, at least in our<br />
region.<br />
References<br />
1. Goodkin DA, Bragg-Gresham JL, Koenig KG, Wolfe RA,<br />
Akiba T, Andreucci VE, Saito A, Rayner HC, Kurokawa K,<br />
Port FK, Held PJ, Young EW. Association of co morbid<br />
conditions and mortality in hemodialysis patients in Europe,<br />
Japan, and United States: The Dialysis Outcomes and Practice<br />
Patterns Study (DOPPS). J Am Soc Nephrol 2003; 14: 3270-7<br />
2. Berthoux F, Jones E, Gellert R, Mendel S, Saker L, Briggs D.<br />
Epidemiological data of treated end-stage renal failure in the<br />
European Union (EU) during the year 1995: Report of the<br />
European Renal Association Registry and the National<br />
Registries. Nephrol Dial Transplant 1999; 14: 2332-42<br />
3. U.S.Renal Data System: USRDS 2000 Annual Data Report:<br />
Atlas of End-Stage Renal Disease in the United States.<br />
Bethesda, MD, National Institutes of Health, National Institute<br />
of Diabetes and Digestive and Kidney Disease, 2000.<br />
4. Shinzato T, Nakai S, Akiba T, Yamagami S, Yamazaki C,<br />
Kitaoka T, Kubo K, Maeda K, Morii H. Report on the annual<br />
statistical survey of the Japanese Society for Dialysis Therapy<br />
in 1996. Kidney Int 1999; 55: 700-12<br />
5. Djukanovic LJ, Hadzi-Djokic J, Djordjevic V, Radovic M.<br />
Yearly Report on Renal Replacement Therapy in Yugoslavia,<br />
1997. Belgrade 1998.<br />
6. Lowrie EG, Huang WH, Lew JL, Liu Y. The relative<br />
contribution of measured variables to death risk among<br />
hemodialysis patients. In: Death on Hemodialysis. Ed.<br />
Friedman EA, Kluwer Academic publishers, 1994, pp 121-41<br />
7. Marcelli D, Stannard D, Conte F, Held PJ, Locatelli F, Port FK.<br />
ESRD patient mortality with adjustment for co morbid<br />
conditions in Lombardy (Italy) versus the United States. Kidney<br />
Int 1996; 50: 1013-18<br />
8. Popovic J, Damjanovic T, Djordjevic T, Stankovic N, Djuric Z,<br />
Dimkovic N. Vascular access in our hemodialysis population.<br />
<strong>BANTAO</strong> <strong>Journal</strong> 2003; 1: 217-18<br />
9. Popovic J, Dimkovic N. Analysis of vascular access in our<br />
diabetic hemodialysis population. XVII Danube Symposium of<br />
Nephrology. Sofia 2004. Abstracts 104.<br />
10. Djukanovic LJ, Radovic M. Annual report on regular dialysis<br />
and kidney transplantation in Yugoslavia, 2001. Belgrade 2003.<br />
11. Ansell D, van Schalkwyk D, Roderick P, Burden R, Feest T.<br />
UK seasonal variation in deaths on renal replacement therapy<br />
by modality and cause. XLI Congress of the European Renal<br />
Association European Dialysis and Transplant Association,<br />
Lisbon 2004; Abstracts 123.<br />
12. United States Renal Data System. USRDS 1998 Annual Data<br />
Report. U.S. Department of Health and Human Services. The<br />
National Institutes of Health, National Institute of Diabetes and<br />
Digestive and Kidney Diseases, Bethesda, MD, 1998.<br />
13. Mailloux LU, Bellucci AG, Napolitano B, et al. Survival<br />
estimates for 683 patients starting dialysis from 1970 through<br />
1989: Identification of risk factors for survival. Clin Nephrol<br />
1994; 42: 127<br />
14. United States Renal Data System. Excerpts from the USRDS<br />
2000 annual data report: Atlas of end-stage renal disease in the<br />
United States. Am J Kidney Dis 2000; 36 (2): S127<br />
15. Bloembergen WE, Port FK, Mauger EA, Wolfe RA. Causes of<br />
death in dialysis patients: Racial and gender differences. J Am<br />
Soc Nephrol 1994; 5: 1231<br />
16. Cohen LM, McCue JD, Germain M, et al. Dialysis<br />
discontinuation: A »good« death? Arch Intern Med<br />
1995;155:42<br />
17. United States Renal Data System. USRDS 1999 Annual Data<br />
Report. U.S. Department of Health and Human Services. The<br />
National Institutes of Health, National Institute of Diabetes and<br />
Digestive and Kidney Diseases, Bethesda, MD, 1999.<br />
18. Wallen MD, Radhakrishnan J, Appel G, et al. An analysis of<br />
cardiac mortality in patients with new-onset end-stage renal<br />
disease in New York State. Clin Nephrol 2001; 55: 101<br />
19. Chertow GM, Johansen KL, Lew N, et al. Vintage, nutritional<br />
status, and survival in hemodialysis patients. Kidney Int 2000;<br />
57: 1176
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 40<br />
Propyl gallate-induced platelet aggregation in patients with end stage renal<br />
disease – The influence of the hemodialysis procedure<br />
T. Eleftheriadis 1 , G. Antoniadi 1 , V. Liakopoulos 2 , A. Tsiandoulas 1 , K. Barboutis 1 and I. Stefanidis 2<br />
1 Department of Nephrology, General Hospital of Serres, Serres; 2 Department of Nephrology, University of Thessaly,<br />
Larissa, Greece<br />
Abstract<br />
Platelet dysfunction is a well-established disturbance in<br />
hemodialysis (HD) patients. Propyl gallate is a synthetic<br />
platelet activator with the property to stimulate platelet<br />
aggregation. The aim of this study was to evaluate the<br />
influence of a single hemodialysis session on propyl gallateinduced<br />
platelet aggregation.<br />
Thirty-nine HD patients were enrolled in the study and 20<br />
healthy volunteers were used as controls. Cellulose diacetate<br />
(CD) dialysers were used in 20 patients and polysulfone (PS)<br />
dialysers in 19. HD was performed via an A-V fistula in 27<br />
patients and via an intravenous catheter in 12. Erythropoietin<br />
was administered in 37 patients (epoietin-alpha in 24 and<br />
darbepoietin in 13). Thirty-four were receiving the low<br />
molecular weight heparin tinzaparin. Propyl gallate slide<br />
aggregometry was used for evaluating platelet aggregation.<br />
In HD patients, platelet aggregation was impaired before as<br />
well as after the HD session. No effect of the HD procedure,<br />
type of vascular access, adequacy of HD or type of<br />
erythropoietin on the propyl gallate-induced platelet<br />
aggregation was detected. Platelet aggregation was higher<br />
when CD dialyser was used. A negative correlation between<br />
the time needed for platelet aggregation to occur and<br />
tinzaparin dose was found.<br />
Propyl-gallate induced platelet aggregation in HD patients is<br />
impaired. Platelet aggregation was higher in patients dialyzed<br />
with CD membrane than in those dialyzed with PS<br />
membrane. The higher was the dose of tinzaparin, the higher<br />
the platelet aggregation. The clinical significance of the<br />
above results needs further evaluation.<br />
Keywords: hemodialysis, platelet aggregation, propylgallate,<br />
erythropoietin, low molecular weight heparin<br />
Introduction<br />
Chronic hemodialysis (HD) treatment improves uremia<br />
induced bleeding diathesis but only partially (1,2). The<br />
bleeding diathesis observed in HD patients is of<br />
multifactorial origin but platelet dysfunction induced by<br />
uremia seems to play a central role. Uremic<br />
thrombocytopathy is attributed to acquired defects in specific<br />
receptors that impair platelet binding to fibrinogen and von<br />
Willebrand factor (3,4), lower than normal content of ADP<br />
and serotonin in platelet -granules (5) and impaired<br />
arachidonate metabolism (6). Guanidinosuccinic acid, a low<br />
molecular weight uremic toxin related with an increase in NO<br />
production by uremic vessels, is implicated in platelet<br />
dysfunction (7).<br />
Recombinant human erythropoietin (rHuEPO) administration<br />
in HD patients improves bleeding diathesis because it<br />
increases red cells blood count and ameliorates blood<br />
rheology abnormalities (8,9). On the other hand, there is<br />
controversy regarding the effect of rHuEPO administration<br />
on platelet aggregation (9-16).<br />
Heparin, the commonly used anticoagulant in HD procedure,<br />
activates platelets and increases platelet aggregation (18,19).<br />
A few studies have evaluated the effect of the more recently<br />
used low molecular weight heparins (LMWH) on platelet<br />
aggregation in HD patients (20,21). In non-uremic subjects<br />
LMWH seems to increase platelet aggregation, although to a<br />
lesser extend than unfractionated heparin (22-25).<br />
Some authors have found out that HD procedure per se<br />
enhances (3,26) platelet activation and aggregation, while<br />
others reached different conclusions (27,28). Finally, the type<br />
of the dialysis membrane used seems to play an important<br />
role in platelet activation or aggregation during the dialysis<br />
session. However, the results of different studies are<br />
controversial (27, 29-31).<br />
The aim of our study was to evaluate the impact of HD<br />
procedure and its different aspects on platelet aggregation.<br />
The impact of the medications commonly used in HD<br />
patients, i.e. rHuEPO and LMWH, on platelet aggregation,<br />
was also assessed. For this purpose the simple and<br />
inexpensive propyl gallate (PG) slide aggregometry test was<br />
used. This test has been shown to be more sensitive in<br />
detecting most of the abnormal platelet aggregation<br />
conditions than the commonly used platelet aggregating<br />
reagents (32). In addition, this procedure shows strong<br />
correlation with the bleeding time test (33). To our<br />
knowledge this is the first time that PG was used as platelet<br />
aggregation agonist in order to evaluate platelet aggregation<br />
in HD patients. Impairment in arachidonate metabolism,<br />
adenosine phosphate receptors or ADP and glycoprotein<br />
IIb/IIIa (GpIIb/IIIa) receptor availability can contribute to<br />
platelet dysfunction in HD patients (3-6). Propyl gallate can<br />
concurrently detect disorders in all these factors (34). This<br />
fact makes it probably the most suitable reagent for an overall<br />
evaluation of platelet aggregation in HD patients, in contrast<br />
with other commonly used platelet aggregation agonists like<br />
arachidonate, ADP, epinephrine, fibrinogen and others,<br />
which evaluate only specific platelet aggregation pathways<br />
(35).<br />
______________________<br />
Correspodence to: T. Eleftheriadis, Department of Nephrology, General Hospital of Serres, Serres, Greece
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 41<br />
Patients and methods<br />
Patients<br />
Thirty-nine patients (19 males, 20 females, mean age 62±11<br />
years) with end stage renal disease undergoing chronic HD<br />
(mean HD duration 63±61 months) were studied. The cause<br />
of end-stage renal disease was primary glomerulonephritis in<br />
13 patients, diabetes mellitus in 5 patients, hypertension in 4<br />
patients, polycystic kidney disease in 3 patients, Alport’s<br />
syndrome in 2 patients, analgesic nephropathy in 1 patient,<br />
primary amyloidosis in 1 patient, and unknown in 10<br />
patients. Patients underwent regular HD with a bicarbonate<br />
buffer for 4 hours each day, 3 days a week. Vascular access<br />
was A-V fistula in 27 patients and a permanent double central<br />
venous catheter in 12 patients. Thirty-seven patients were<br />
receiving i.v. erythropoietin (rHuEPO), 24 epoietin-alpha<br />
(Eprex ® ; Johnson & Johnson, Manati, PR) and 13<br />
darbepoietin-alpha (Aranesp ® ; Amgen, Thousand Oaks, CA).<br />
During treatment the LMWH tinzaparin sodium (Innohep ® ;<br />
Leo Pharmaceuticals, Ballerup, Denmark) was used for<br />
anticoagulation in 34 patients, unfractionated heparin<br />
(Heparin ® , Leo Pharmaceuticals, Ballerup, Denmark) in 2<br />
patients, while 3 patients did not receive anticoagulation.<br />
Cellulose diacetate (CD) dialysers (FB-T series ® ; Nipro<br />
Corporation, Osaka, Japan) were used in 20 patients and<br />
polysulfone (PS) dialysers (F low-flux series ® ; Fresenius<br />
Medical Care, Bad Homburg, Germany) in the other 19<br />
patients.<br />
Twenty healthy volunteers (9 males, 11 females, mean age<br />
54±16 years) were studied as a control group. Except heparin<br />
during HD none of the patients or the healthy volunteers was<br />
receiving coagulation related medication. In particular none<br />
received antiplatelet agents or had been taking non-steroidal<br />
anti-inflammatory drugs for at least 20 days prior to the<br />
study. An informed consent was obtained from each<br />
individual enrolled into the study and the hospital ethics<br />
committee gave its approval to the study protocol.<br />
Methods<br />
Blood samples for the assessment of platelet aggregation<br />
were drawn from the dialysis access site immediately before<br />
and shortly after the 2 nd HD session of the week. Blood was<br />
then collected with citrate (1 part sodium citrate 3.8 %, 9<br />
parts blood) in a polypropylene tube and centrifuged for 5<br />
minutes at 500RCF in order to obtain platelet rich plasma<br />
(cPRP). The supernatant was transferred with a plastic pipette<br />
in a plastic test tube.<br />
Platelet aggregation was evaluated by means of a slide<br />
platelet aggregation test kit (SPAT ® ; Analytical Control<br />
Systems, Fishers, IN, USA), which includes PG as platelet<br />
aggregation agonist. On a plastic microscope slide 100l<br />
cPRP were mixed with 100 l SPAT reagent (Analytical<br />
Control Systems, Fishers, IN, USA). A stopwatch was started<br />
and the slide was rocked continuously until aggregation, in<br />
the form of many visible white clumps of platelets, occurred.<br />
The time needed for platelet aggregation to occur (platelet<br />
aggregation time) is as measure of platelet aggregability. All<br />
tests were done in duplicate at room temperature, and the<br />
mean value was obtained. One of the authors, blinded<br />
regarding the subjects’ identity, performed all the tests in the<br />
same laboratory environment.<br />
Concurrently, platelet count, hemoglobin (Hb), international<br />
normalized ratio (INR) and activated partial thromboplastin<br />
time (aPTT) were examined in blood samples obtained before<br />
the start of HD. Blood urea was assessed before the start and<br />
after the end of HD in order to estimate KT/V according to<br />
the second generation natural logarithmic formula, developed<br />
by Daugirdas based on the single pool urea kinetic model<br />
(36). The weekly dose of rHuEPO (units per Kg of patient’s<br />
dry body weight) was registered for epoietin-alpha (Epoa/bw)<br />
and darbepoietin-alpha (Dar-a/bw) and for both<br />
together (Epo/bw). Multiplying the dose of darbepoietinalpha<br />
in micrograms by a factor of 200 gave its equivalent in<br />
weekly epoietin-alpha dose. Finally, the dose of tinzaparin<br />
per Kg of patient’s dry body weight given in the examined<br />
hemodialysis session (LMWH/bw) was registered (Table 1).<br />
Table 1. The values of factors that are evaluated for effect on<br />
platelet aggregation, expressed as mean±SD<br />
platelet count (platelets/l) 249871±66976<br />
Hb (g/dl) 10.9±1.15<br />
INR 0.91±0.09<br />
aPTT (patient/control sec) 1.22±0.75<br />
KT/V 1.18±0.44<br />
Epo/bw (units/Kg) 189.64±148.43<br />
Epo-a/bw (units/Kg) 208.61±139.88<br />
Dar-a/bw (g/Kg) 0.948±0.802<br />
LMWH/bw (units/Kg) 40.48±19.47<br />
Statistical analysis<br />
Results are expressed as a mean value and standard deviation<br />
(SD). Normality of the evaluated variables was assessed with<br />
the single sample Kolmogorov-Smirnov test. Unpaired t-test,<br />
paired t-test and Pearson correlation test were used where<br />
appropriate. P-values < 0.05 were considered as statistically<br />
significant.<br />
Results<br />
Propyl gallate-induced platelet aggregation time, as it is<br />
assesses by the time needed for aggregation to occur, before<br />
the start of the HD session (PLA1) was significantly impaired<br />
in comparison with the control group (PLAc). PLA1 was<br />
62.74±15.80sec while PLAc was 43.66±11.25sec (p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 42<br />
Platelet aggregation, as it is assesses by the time needed for<br />
aggregation to occur, before the start of the HD session<br />
(PLA1) was significantly impaired in comparison with the<br />
control group (PLAc). PLA1 was 62.74±15.80sec while<br />
PLAc was 43.66±11.25sec (p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 43<br />
arachidonate metabolism is incriminated for defective platelet<br />
aggregation in HD patients. Recently, Xiao et al<br />
demonstrated that PG-induced platelet aggregation and<br />
tyrosine phosphorylation of multiple proteins were<br />
substantially abolished by aspirin, apyrase, and abciximab,<br />
suggesting that PG is associated with activation of platelet<br />
cyclooxygenase 1, adenosine phosphate receptors, and<br />
GpIIb/IIIa, respectively (34). Abnormal function of all these<br />
factors has been implicated in platelet dysfunction in HD<br />
patients (3-6). Propyl-gallate is possibly a suitable reagent for<br />
a global evaluation of platelet aggregation in HD patients, in<br />
contrast with other commonly used aggregation reagents like<br />
arachidonate, ADP, epinephrine, fibrinogen and others,<br />
which are proper for specific, but only partial evaluation of<br />
platelet aggregation (35).<br />
As expected, impaired platelet aggregation was detected in<br />
HD patients. Interestingly, platelet aggregation impairment<br />
did not show any improvement after the HD procedure. This<br />
is in contrast with other studies that detected enhancement of<br />
platelet aggregation after the HD procedure (3,26). On the<br />
other hand, there are studies, which indicated that HD<br />
procedure reduces platelet aggregation (27,28). The<br />
difference among these studies could be attributed to the<br />
different HD conditions (i.e. HD membrane composition or<br />
type of anticoagulant) or to the different platelet aggregation<br />
agonists used. In our study PG was used for the first time in<br />
order to evaluate platelet aggregation in HD patients. As<br />
already noted, PG is a platelet agonist that can detect<br />
impairments in many pathways leading to platelet<br />
aggregation. Consequently, our study assessed platelet<br />
aggregation more globally than others, which used more<br />
specific platelet aggregation agonists that are capable for<br />
evaluating only one pathway of platelet aggregation each<br />
(35).<br />
Regarding the HD procedure per se, we failed to detect any<br />
difference. Type of dialysis access (A-V fistula or central<br />
intravenous catheter) did not affect platelet aggregation. Two<br />
kinds of dialysis membranes were used in our study, CD and<br />
PS. There are many studies that evaluate the effect of<br />
membrane composition on platelet activation or aggregation.<br />
Most of them evaluated the fibrinogen binding to GpIIb/IIIa<br />
receptor but the results are contradicting. In one study the<br />
level of bound GPIIb/IIIa fibrinogen receptor was increased<br />
when PS membrane was used but there was no significant<br />
change with cellulose triacetate membrane (29). In contrast,<br />
another study indicated that the degree of GPIIb/IIIa<br />
activation was greater during hemodialysis with regenerated<br />
cellulose than PS membrane (30). In a paper comparing the<br />
influence of cuprophan, hemophan, and PS on fibrinogen<br />
binding on platelets, Gawaz et al concluded that it is<br />
increased only when cuprophan membrane was used (31).<br />
Finally, another study comparing polymethylmethacrylate,<br />
cuprophan, and PS membranes did not demonstrate any effect<br />
of the type of dialysis membrane on platelet aggregation (27).<br />
In our study, we detected that PG induced platelet<br />
aggregation time before HD session was higher when PS<br />
membrane was used in comparison with CD membrane. That<br />
was a long-term effect since there was not difference in the<br />
change in platelet aggregation time before and after HD if PS<br />
or CD dialysers were used. The fact that PG induced platelet<br />
aggregation is totally abolished by the GpIIb/IIIa inhibitor<br />
abciximab in relatively low concentrations (34), in<br />
combination with the results of the above studies, raises the<br />
possibility that PS membrane induces less GpIIb/IIIa<br />
activation than CD membrane.<br />
Dialysis adequacy (as expressed by KT/V) did not have any<br />
effect on platelet aggregation either. This means that the<br />
clearance of the low molecular weight toxins by HD does not<br />
influence platelet aggregation. On the other hand, the role of<br />
some low molecular weight toxins, especially of<br />
guanidinosuccinic acid, in uremic platelet dysfunction is well<br />
established (7). It is possible that the difference in urea<br />
clearances, among our patients was not big enough in order to<br />
induce difference in platelet aggregation. Standard HD, 3<br />
times a week, 4 hours per session, seems adequate in<br />
removing enough guanidinosuccinic acid or other low<br />
molecular weight uremic toxins, responsible for platelet<br />
dysfunction.<br />
Nowadays rHuEPO is administered in most HD patients. The<br />
beneficial effect of rHuEPO on hemostasis is well<br />
established. One certain mechanism is improvement in blood<br />
rheology due to correction of anemia (9). Many studies, using<br />
various platelet agonists, have evaluated the effects of<br />
rHuEPO on platelet aggregation in HD patients. Again the<br />
results were conflicted, as some authors detected an increase<br />
in platelet aggregation after rHuEPO administration (10-14),<br />
while others failed to do so (9,15-17). In our study we did not<br />
detect any correlation between platelet aggregation time and<br />
the weekly dose of rHuEPO per Kg of dry body weight<br />
(Epo/bw). There was no statistically significant difference in<br />
platelet aggregation if epoietin-alpha or darbepoietin-alpha<br />
was administered. It is notable that in another study platelet<br />
aggregation responses to thrombin did not differ between the<br />
two treatments (39).<br />
In most HD patients, extracorporeal blood circulation is<br />
maintained with the administration of unfractionated heparin,<br />
or more recently with the administration of LMWH. Studies<br />
in non-uremic subjects indicated that unfractionated heparin<br />
activates platelets and increases platelet aggregation. In nonuremic<br />
subjects LMWH also seems to increase platelet<br />
aggregation, although to a lesser extend than unfractionated<br />
heparin (22-25). There are some studies in HD patients that<br />
confirm the platelet aggregation enhancement by<br />
unfractionated heparin (18,19). On the other hand, there are<br />
quite a few studies that evaluate the effect of the more<br />
recently used LMWH on platelet aggregation in HD patients.<br />
In one study LMWH did not alter ADP or collagen induced<br />
platelet aggregation during dialysis (20), and in another one<br />
no differences between unfractionated heparin and LMWH<br />
were observed regarding the platelet aggregation in HD<br />
patients (21). In our unit the major anticoagulant used was the<br />
LMWH tinzaparin sodium. Platelet aggregation before HD<br />
was positively, although weakly, correlated with the dose of<br />
tinzaparin sodium (units/kg of dry body weight). This<br />
positive correlation became much stronger after HD, i.e. near<br />
tinzaparin administration, indicating a short-term effect of<br />
that LMWH on platelet aggregation. The positive impact of<br />
LMWH on platelet aggregation could be the result of the less<br />
microthrombus formation and consequently of the less<br />
fibrinolytic mechanism activation and fibrinogen fragments<br />
production during HD procedure. Accoring to a study by<br />
Sreedhara et al, platelet dysfunction in chronic HD patients<br />
results from decreased GpIIb/IIIa availability due to receptor<br />
occupancy by fibrinogen fragments (40). Additionally, Sobel<br />
et al have detected that unfractionated heparin directly binds
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 44<br />
to GpIIb/IIIa modulating its function (41). This aspect has not<br />
been evaluated yet for LMWH.<br />
Finally, no correlation was detected in our study among<br />
platelet aggregation and Hb, INR or aPTT, indicating, as<br />
expected, that PG induced platelet aggregation is independent<br />
of other factors that are correlated with blood rheology or<br />
coagulation. In contrast, also as expected, PG induced platelet<br />
aggregation was positively correlated with the whole blood<br />
platelet count.<br />
Conclusions<br />
In conclusion, our study demonstrates that PG induced<br />
platelet aggregation in chronic HD patients is decreased in<br />
comparison with non-uremic subjects. The HD procedure<br />
does not influence platelet aggregation neither does the<br />
dialysis access type (A-V fistula or central intravenous<br />
catheter) or the low molecular weight uremic toxins<br />
clearance. Different types of dialysis membranes have<br />
different effects on platelet aggregation. Polysulfone dialyser<br />
prolongs the PG-induced platelet aggregation time in<br />
comparison to CD dialyser. Finally, from the medications<br />
usually administered in HD patients, only LMWH had a<br />
positive effect on PG-induced platelet aggregation. The<br />
clinical significance of the above results, in relation with the<br />
bleeding or thrombotic episodes in HD patients, needs further<br />
evaluation.<br />
References<br />
1. Weigert AL, Schafer AI. Uremic bleeding: pathogenesis and<br />
therapy. Am J Med Sci 1998; 316(2): 94-104<br />
2. Malyszko J, Malyszko JS, Mysliwiec M. Comparison of<br />
hemostatic disturbances between patients on CAPD and<br />
patients on hemodialysis. Perit Dial Int 2001; 21(2): 158-165<br />
3. Gawaz MP, Dobos G, Spath M, Schollmeyer P, Gurland HJ,<br />
Mujais SK. Impaired function of platelet membrane<br />
glycoprotein IIb-IIIa in end-stage renal disease. J Am Soc<br />
Nephrol 1994; 5(1): 36-46<br />
4. Moal V, Brunet P, Dou L, Morange S, Sampol J, Berland Y.<br />
Impaired expression of glycoproteins on resting and stimulated<br />
platelets in uraemic patients. Nephrol Dial Transplant 2003;<br />
18(9): 1834-1841<br />
5. Eknoyan G, Brown CH. Biochemical abnormalities of platelets<br />
in renal failure. Evidence for decreased platelet serotonin,<br />
adenosine diphosphate and Mg-dependent adenosine<br />
triphosphatase. Am J Nephrol 1981; 1(1): 17-23<br />
6. Pietrzak I, Komarnicki M, Zaremba-Drobnik D. Platelet<br />
aggregation and prostaglandin metabolism in uremic patients.<br />
Am J Kid Dis 2001; 38(4): S111-S114<br />
7. Noris M, Remuzzi G. Uremic Bleeding: Closing the Circle<br />
After 30 Years of Controversies? Blood 1999; 94(8): 2569-<br />
2574<br />
8. Maurin N, Fitzner S, Fritz H, Gladziwa U, H„gel J, Stefanidis<br />
I. Influence of recombinant human erythropoietin on<br />
hematological and hemostatic parameters with special reference<br />
to microhemolysis. Clin Nephrol 1995; 43: 196-200<br />
9. Gordge MP, Leaker B, Patel A, Oviasu E, Cameron JS, Neild<br />
GH. Recombinant human erythropoietin shortens the uraemic<br />
bleeding time without causing intravascular haemostatic<br />
activation. Thromb Res 1990; 57(2): 171-182<br />
10. Van Geet C, Hauglustaine D, Verresen L, Vanrusselt M,<br />
Vermylen J. Haemostatic effects of recombinant human<br />
erythropoietin in chronic haemodialysis patients. Thromb<br />
Haemost 1989; 61(1): 117-121<br />
11. Huraib S, al-Momen AK, Gader AM, Mitwalli A, Sulimani F,<br />
Abu-Aisha H. Effect of recombinant human erythropoietin<br />
(rHuEPO) on the hemostatic system inchronic hemodialysis<br />
patients. Clin Nephrol 1991; 36(5): 252-257<br />
12. Zwaginga JJ, Ijsseldijk MJ, de Groot PG, Kooistra M, Vos J,<br />
van Es A, Koomans, H.A. Struyvenberg, A.; Sixma, J.J.<br />
Treatment of uremic anemia with recombinant erythropoietin<br />
also reduces the defects in platelet adhesion and aggregation<br />
caused by uremic plasma. Thromb Haemost 1991; 66(6): 638-<br />
647<br />
13. Cases A, Escolar G, Reverter JC, Ordinas A, Lopez-Pedret J,<br />
Revert L, Castillo R. Recombinant human erythropoietin<br />
treatment improves platelet function in uremic patients. Kidney<br />
Int 1992; 42(3): 668-672<br />
14. El-Shahawy MA, Francis R, Akmal M, Massry SG:<br />
Recombinant human erythropoietin shortens the bleeding time<br />
and corrects the abnormal platelet aggregation in hemodialysis<br />
patients. Clin Nephrol 1994; 41(5): 308-313<br />
15. Akizawa T, Kinugasa E, Kitaoka T, Koshikawa S: Effects of<br />
recombinant human erythropoietin and correction of anemia on<br />
platelet function in hemodialysis patients. Nephron 1991; 58(4):<br />
400-406<br />
16. Zirkman DM, Zeigler ZR, Fraley DS, Bruns FJ, Adler S:<br />
Evaluation of platelet hyperfunction in hemodialysis patients<br />
receivingrecombinant human erythropoietin. Am J Kidney Dis<br />
1993; 21(1): 31-37<br />
17. Stenver D, Jeppesen L, Nielsen B, Dalsgaard Nielsen J,<br />
Haedersdal C, Mehlsen J, Winther K. The effect of<br />
erythropoietin on platelet function and fibrinolysis in chronic<br />
renal failure. Int J Artif Organs 1994; 17(3): 141-145<br />
18. Matsuo T, Matsuo M, Kario K, Suzuki S. Characteristics of<br />
heparin-induced platelet aggregates in chronic hemodialysis<br />
with long-term heparin use. Haemostasis 2000; 30(5): 249-257<br />
19. Charvat J, Konig J, Blaha J. Is heparin responsible for<br />
enhanced platelet aggregation after haemodialysis? Nephron<br />
1986; 44(2): 89-91<br />
20. Suzuki T, Ota K, Naganuma S, Koshikawa S, Hirasawa Y,<br />
Nakagawa S, Otsubo O, Akizawa T. Clinical application of<br />
Fragmin (FR-860) in hemodialysis: multicenter cooperative<br />
study in Japan. Semin Thromb Hemost. 1990; 16(S1): 46-54<br />
21. Borm JJ, Krediet R, Sturk A, ten Cate JW. Heparin versus low<br />
molecular weight heparin K 2165 in chronic hemodialysis<br />
patients: a randomized cross-over study. Haemostasis 1986;<br />
16(S2): 59-68<br />
22. Ljungberg B, Beving H, Egberg N, Johnsson H, Vesterqvist O.<br />
Immediate effects of heparin and LMW heparin on some<br />
platelet and endothelial derived factors. Thromb Res 1988;<br />
51(2): 209-217<br />
23. Sakuragawa N, Takahashi K. Comparative studies on<br />
properties of unfractionated and low molecular weight heparin.<br />
Semin Thromb Hemost 1990; 16(Sl): 5-11<br />
24. Kawano K, Ikeda Y, Handa M, Kamata T, Anbo H, Araki Y,<br />
Kawai Y, Watanabe K, Itagaki I, Kawakami K. Enhancing<br />
effect by heparin on shear-induced platelet aggregation. Semin<br />
Thromb Hemost 1990; 16( Sl): 60-65<br />
25. Burgess JK, Chong BH. The platelet proaggregating and<br />
potentiating effects of unfractionated heparin, low molecular<br />
weight heparin and heparinoid in intensive care patients and<br />
healthy controls. Eur J Haematol 1997; 58(4): 279-285<br />
26. Winter M, Frampton G, Bennett A, Machin SJ, Cameron JS.<br />
Synthesis of thromboxane B2 in uraemia and the effects of<br />
dialysis. Thromb Res 1983; 30(3): 265-272<br />
27. Sreedhara R, Itagaki I, Lynn B, Hakim RM. Defective platelet<br />
aggregation in uremia is transiently worsened by hemodialysis.<br />
Am J Kidney Dis 1995; 25(4): 555-563<br />
28. Sloand JA, Sloand EM. Studies on platelet membrane<br />
glycoproteins and platelet function during hemodialysis. J Am<br />
Soc Nephrol 1997; 8(5): 799-803<br />
29. Kuragano T, Kuno T, Takahashi Y, Yamamoto C, Nagura Y,<br />
Takahashi S, Kanmatsuse K. Comparison of the effects of<br />
cellulose triacetate and polysulfone membrane onGPIIb/IIIa<br />
and platelet activation. Blood Purif 2003; 21(2): 176-182
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 45<br />
30. Kawabata K, Nakai S, Miwa M, Sugiura T, Otsuka Y, Shinzato<br />
T, Hiki Y, Tomimatsu I, Ushida Y, Hosono F, Maeda K.<br />
Platelet GPIIb/IIIa is activated and platelet-leukocyte<br />
coaggregates formed in vivo during hemodialysis. Nephron<br />
2002; 90(4): 391-400<br />
31. Gawaz MP, Mujais SK, Schmidt B, Blumenstein M, Gurland<br />
HJ. Platelet-leukocyte aggregates during hemodialysis: effect of<br />
membrane type. Artif Organs 1999; 23(1): 29-36<br />
32. Speck RE. Comparison of slide platelet aggregation reagents.<br />
Am Clin Lab 1994; 13(9): 22-23<br />
33. Speck RE, Melvin JR. A Comparison of the slide platelet<br />
aggregation procedure with the bleeding time test. Am Clin Lab<br />
1994; 13(1): 12-13<br />
34. Xiao H, Kovics R, Jackson V, Remick DG. Effects of platelet<br />
inhibitors on propyl gallate-induced platelet aggregation,<br />
protein tyrosine phosphorylation, and platelet factor 3<br />
activation. Blood Coagul Fibrinolysis 2004; 15(3): 199-206<br />
35. Van Cott EM, Laposata M. "Coagulation." In: Jacobs DS, De<br />
Mott WR, Oxlay DK ed. The Laboratory Test Handbook, 5th<br />
Edition. Lexi-Comp, Cleveland, 2001; 327-358<br />
36. Daugirdas JT. Second generation logarithmic estimates of<br />
single-pool variable volume Kt/V: an analysis of error. J Am<br />
Soc Nephrol 1993; 4: 1205-1213<br />
37. Stejskal D, Proskova J, Petrzelova A, Bartek J, Oral I, Lacnak<br />
B, Horalik D, Sekaninova S. Application of cationic propyl<br />
gallate as inducer of thrombocyte aggregation for evaluation of<br />
effectiveness of antiaggregation therapy. Biomed Pap Med Fac<br />
Univ Palacky Olomouc Czech Repub 2001; 145(2): 69-74<br />
38. Schwartz KA, Schwartz DE, Pittsley RA, Mantz SL, Ens, G<br />
Sami A, Davis GM. A new method for measuring inhibition of<br />
platelet function by nonsteroidal antiinflammatory drugs. J Lab<br />
Clin Med 2002; 139: 227-233<br />
39. Fuste B, Escolar G, Cases A, Lopez-Pedret J, Ordinas A, Diaz-<br />
Ricart M. Novel erythropoiesis stimulating protein exerts an<br />
effect on platelet function in uremia equivalent to that exerted<br />
by recombinant human erythropoietin. Haematologica 2002;<br />
87(5): 551-553<br />
40. Sreedhara R, Itagaki I, Hakim RM. Uremic patients have<br />
decreased shear-induced platelet aggregation mediated by<br />
decreased availability of glycoprotein IIb-IIIa receptors. Am J<br />
Kidney Dis 1996; 27(3): 355-364<br />
41. Sobel M, Fish WR, Toma N, Luo S, Bird K, Mori K,<br />
Kusumoto S, Blystone SD, Suda Y. Heparin modulates integrin<br />
function in human platelets. J Vasc Surg 2001; 33(3): 587-594
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 46<br />
Serum cystatin C as an endogenous marker of kidney function in elderly<br />
with chronic kidney failure<br />
H. Resic 1 and A. Mataradzija 2<br />
1 Center for Haemodialysis, 2 Nephrology Institute, Clinical Center, Sarajevo, Bosnia and Herzegovina<br />
Abstract<br />
Concentration of serum cystatine C primarly dependes on the<br />
glomerular filtration rate (GFR), and cystatin C concentration<br />
in serum can be used as an endogenous marker of kidney<br />
function. Use of cystatin C in the assesment of GFR in<br />
elderely, childern and pre - dialysis patients could be usful.<br />
The aim of the study was to evaluate the use of cystatin C as<br />
a renal marker of the glomerular filtration rate (GFR) in<br />
patients with various degrees of kidney failure.<br />
The study icluded the total of 104 patients (various etiology<br />
of kidney disease) with different degrees of kidney failure.<br />
All of them were on conservative tretmant and 10 healtly<br />
patients will comprised the control group. Mean values of<br />
cystatin C and creatinine in serum hes been measured and<br />
compared to endogeneus cretainine clearense.<br />
There were 104 patients testid in total with various etiology<br />
of kidney disease. Mean age of patients receiving<br />
conservative treatment was 68, 4 ± 5, 06 years and controls<br />
69 ± 3, 66 years. Significant correlation have established<br />
between creatinine clearence and creatinine r = 0, 663 p < 0,<br />
001, and between creatinine clearence and cystatin C r = 0,<br />
765, p < 0, 001 in patients will different degrees of chronic<br />
kidney failure (CKF). Correlation between creatinine<br />
clearence and cystatin C was significantly better than<br />
between serum creatinine p < 0, 05.<br />
According to results from our study the level of cystatin C in<br />
serum is better marker of kidney function than the level of<br />
creatinine in serum.<br />
Hering in mind that this is faster and cheaper method it could<br />
find wider application in every day clinical practtise,<br />
especially in elderly where is often impossible to accurately<br />
collect 24 - hour - urine (inconontinence)<br />
Key words: serum cystatin C, chronic kidney failure,<br />
clearence creatinin<br />
Introduction<br />
In clinical practice the glomerular filtration rate (GFR) is<br />
assessed with various methods. The most accurate method is<br />
the radioisotopic measurement of inulin clearance (1).<br />
However, in everyday clinical practice radioisotopic methods<br />
are expensive, time-consuming and they expose patients to<br />
radiation, the reason of their substitution with cheaper and<br />
quicker methods such as the measurement of creatinine and<br />
creatinine clearance levels in serum (2). As of recent many<br />
studies have evaluated the use of cystatin C in the assessment<br />
of GFR in elderly and children, especially in group of predialysis<br />
patients because the cystatin C value does not depend<br />
on age, gender of muscle weight.<br />
Cystatin C is a cystatin protease inhibitor and is a part of<br />
intracellular protein catabolism. It is non-glycolysed, lowmolecular<br />
protein (133kD) which comprises 120 amino acids.<br />
Protein is created in each nucleus, freely passes glomerular<br />
membrane and almost completely is reabsorbed and<br />
catabolised in proximal tubular cells (3). Due to these facts<br />
concentration of serum cystatine C primarily depends on the<br />
glomerular filtration rate (GFR), and cystatin C concentration<br />
in serum can be used as an endogenous marker of kidney<br />
function (4). Many authors, (Schuck O, Teplan V et al.,<br />
2003) agree that cystatin C, as a new endogenous marker, can<br />
have advantages in early recognition of damaged kidney<br />
function (5-7).<br />
The aim of this study was to compare both serum markers:<br />
creatinine and cystatin C with creatinine clearance in elderly,<br />
and to evaluate the use of cystain C as a renal marker of the<br />
glomerular filtration rate (GFS) in patients with various<br />
degrees of kidney failure.<br />
Patients and methods<br />
The study included the total of 104 patients (various etiology<br />
of kidney disease), with different degrees of kidney failure.<br />
All of them were on conservative treatment (I degree of<br />
creatinine clearance – mean value 72.48 ± 17.62 ml/min – 42<br />
patients, II degree – creatinine clearance 34.53 ± 9.92 ml/min<br />
– 44 patients, III degree 11.63 ± 3.71ml/min – 18 patients)<br />
and 10 healthy patients which comprised the control group.<br />
Mean values of cystatin C and creatinine in serum had been<br />
measured and compared to endogenous creatinine clearance.<br />
Dade Behring nephelometer has been used for cystatin C<br />
measurement by immunonephelometric method, urea with<br />
uresis method, creatinine with kinetic method on the same<br />
machine, and creatinine clearance had been calculated using<br />
formula: urine creatinine x diuresis / serum creatinine x f (f =<br />
84.400).<br />
Patients were divided according to the values of creatinine<br />
clearance in three groups. During the study they were under<br />
the standard treatment of a kidney disease: antihypertensives,<br />
drugs lowering fat, vitamins, and Fe preparations.<br />
Manuel statistical data processing has been used:<br />
percentages, arithmetic mean, standard deviation, Chi-square<br />
test, t-test, differentiation and correlation coefficients.<br />
Results<br />
There were 104 patients tested in total with various etiology<br />
of kidney disease: 46 patients – Chronic Pyelonephritis (CP);<br />
______________________<br />
Correspodence to: H. Resic, Center for Haemodialysis, Clinical Center, Sarajevo, Bosnia and Herzegovina
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 47<br />
25 patients – Obstructive nephropathy (ON); 27 patients –<br />
Polycystic kidneys (PK); 6 patients – Other etiology:<br />
Nephrectomy, unknown etiology (Other).<br />
Discussion<br />
Accurate measurement of kidney function on daily basis in<br />
clinical practice is essential in order to be able to continually<br />
follow up differential treatments aimed to maintain or<br />
improve kidney function, and in time set to begin with kidney<br />
function replacement therapy in pre-dialysis patients (1).<br />
Accurate methods such as inulin clearance, radioisotopic<br />
contrast techniques are often expensive, time-consuming and<br />
inaccessible, therefore in routine clinical practice more<br />
suitable are measurement of creatinine concentration in<br />
serum and creatinine clearance (2). These methods have their<br />
disadvantages in pre-dialysis patients and in elderly because<br />
they are not absolute indicators of the GFR (4,5). The<br />
creatinine level is actually lower because a part of creatinine<br />
is eliminated by intestinal degradation, then in uremia with<br />
lower ingestion of proteins occur muscle degradation, which<br />
in turn lowers the production of creatinine and its level in<br />
serum. Many substances such as keto acids, glucose, and<br />
bilirubin can interfere with measurement of creatinine in<br />
serum (6). Thus the serum level of creatinine is lower than it<br />
is expected according to the decrease of the GFR. On the<br />
other hand, the creatinine clearance measurement depends on<br />
muscle weight of a patient, on the feasibility of adequate 24-<br />
hour urine collection and tubular secretion which makes the<br />
method deficient (7).<br />
As of recent cystatin C has proven to be not only better, but<br />
ideal, endogenous marker of kidney function since it is a<br />
constant value that does not depend on gender, patient’s<br />
muscle weight, accompanying infections or malignancies (3-<br />
6). It is produced in every nucleus as a constant value, freely<br />
passes glomerular membrane and it is reabsorbed and<br />
completely metabolized in proximal tubules. Its plasma level<br />
linearly correlates with the GFR, i.e. its plasma level<br />
increases proportionally to the decrease of the GFR which<br />
makes it more sensitive marker than creatinine (6-10).<br />
Besides, it does not take long time to prepare 24-hour urine<br />
for the cystatin C measurement. It is believed to show the<br />
kidney function damage much earlier than creatinine.<br />
Serum cystatin C has been measured with immunoassay<br />
technique which is fast, accurate and suitable for use in<br />
clinical practice (3,10-12). There are not any drugs yet known<br />
to affect the serum level of cystatin C in clinical settings, as<br />
the available literature suggests (11-14).<br />
In our study we have established significant correlation<br />
between creatinine clearance and creatinine r = - 0,663,<br />
p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 48<br />
Fig 2a Control group – distribution according to gender<br />
CONTROL GROUP – DISTRIBUTION<br />
ACCORDING TO GENDER<br />
Females<br />
60%<br />
Males<br />
40%<br />
Fig 2b Conservative treatment according to gender<br />
Females<br />
50%<br />
Conservative treatment<br />
according to gender<br />
Males<br />
50%<br />
Table 3. Mean cystatin C values (mg/l)<br />
Number of<br />
patients (n)<br />
CONSERVATIVE TREATMENT<br />
Arithmetic<br />
mean x<br />
Standard<br />
deviation SD<br />
I DEGREE 42 1,015 0,279<br />
II DEGREE 44 1,898 0,677<br />
III DEGREE 18 3,931 0,897<br />
TOTAL 104 1,893 1,181<br />
CONTROL GROUP 10 0,648 0,131<br />
Test results of significant differencies in mean creatinine values,<br />
according to the type of treatment compared to control group<br />
I DEGREE II DEGREE III DEGREE<br />
CONTROL GROUP 5,495 11,351 15,239<br />
SIGNIFICANCE p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 49<br />
Table 5. Coefficients of linear correlation between creatinine and<br />
creatinine clearance<br />
COEFIFCENT OF LINEAR<br />
CORREALATION (r)<br />
SIGNIFICAN<br />
CE<br />
CONSERVATIVE TREATMENT<br />
I DEGREE r= -0,302 p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 50<br />
Thyroid disfunction and ultrasonographic abnormalities in uremic patients<br />
undergoing conservative management and haemodialysis<br />
A. Mataradzija 1 , H. Resic 2 and E. Kucukalic-Selimovic 3<br />
1 Nephrology Department, 2 Center for Haemodialysis, 3 Nuclear Medicine Department, Clinical Center, University of Sarajevo<br />
Abstract<br />
Morphologic abnormalities of thyroid gland are ordinary in a<br />
form of thyroid nodules, goiter or thyroid carcinoma in<br />
patients with chronic renal failure (CRF). The aim of our<br />
study was to examine the prevalence of morphologic and<br />
functional abnormalities of patients with CRF at conservative<br />
management and haemodialysis.<br />
The study was conducted in 81 patients (40 with CRF, 31<br />
haemodialaysis patients and 10 healthy controls. All patients<br />
were evaluated by ultrasonography of the thyroid gland and<br />
blood sample was drawn for a various biochemical<br />
parameters of thyroid function. The duration of the study was<br />
12 months.<br />
The study cohort with mean age 56,20±11,80 years, was<br />
predominated by female patients (61.7%), on a conservative<br />
treatment (72.5%). Disease duration at conservative<br />
management was significantly longer in comparison with<br />
patients on haemodialysis (11.3±6.46 vs. 8.45±5.61 years).<br />
Ultrasound revealed an irregular assessment of thyroid gland<br />
in 52.1% of the patients. Significantly lower mean values of<br />
thyroid hormones was obtained in the evaluated groups as<br />
compared with the controls.<br />
A substantial number of our patients have been presented<br />
with changes of one or both lobules of thyroid gland. The<br />
mean values of serum thyroid hormones were significantly<br />
lower in patients with CRF at conservative management and<br />
haemodialysis treatment in compare with patients of control<br />
group.<br />
Key words: thyroid disfunction, dialysis, ultrasonography<br />
Results<br />
All results are presented within the following tables and<br />
figures.<br />
Introduction<br />
Many authors have agreed that morphologic abnormalities of<br />
thyroid gland are ordinary in a form of thyroid nodules, goiter<br />
or thyroid carcinoma in patients with chronic renal failure<br />
than in the general population (1-5). In the same time, we<br />
found out lower serum thyroid hormone values, and these<br />
patients were clinically euthyroid. Modern literature<br />
describes these phenomena as “Sick euthyroid syndrome”<br />
(12,13).<br />
The aim of the study was to examine the prevalence of<br />
morphologic and functional abnormalities of patients with<br />
chronic renal failure (CRF) at conservative management and<br />
haemodialysis.<br />
Patients and methods<br />
Patients<br />
This study totally involves 81 patients. 40 patients with CRF<br />
at conservative management, (with clearence creatinine in a<br />
range of 80-10 ml/min), 31 patients at haemodialaysis<br />
treatment (clearence creatinine underlying 10 ml/min), and<br />
10 healthy patients with regular kidney and thyroid function<br />
used as control group.<br />
Methods<br />
All patients were evaluated by ultrasonography of the thyroid<br />
gland (Siemens ultrasonograph with linear sonde of 70<br />
MHz). Free and total serum thyroid hormone values have<br />
been calculated using Radioimmunoassay methods, and FT3,<br />
FT4 by Chemiluminescent technique. Duration of study has<br />
been 12 months, using standard statistical methods for<br />
manually elaboration of information, with no use of<br />
computer.<br />
Table 1. Gender distribution<br />
Number of<br />
Therapy type<br />
males<br />
Number of<br />
females<br />
Males in<br />
percentages<br />
Females in<br />
percentages<br />
Total<br />
number<br />
p-values<br />
Conservative management<br />
I degree 1 8 11,10% 88,90% 9 n.s.<br />
II degree 2 5 28,60% 71,40% 7 n.s.<br />
III degree 8 16 33,30% 66,70% 24 n.s.<br />
Total 11 29 27,50% 72,50% 40 n.s.<br />
Haemodialysis 15 16 48,40% 51,60% 31 n.s.<br />
Control group 5 5 50% 50% 10 n.s.<br />
Total 31 50 38,30% 61,70% 81 p< 0,001<br />
Demographic data (61,7% patients were females and 38,3% were males out of total 81 patients)<br />
______________________<br />
Correspodence to: A. Mataradzija, Nephrology Department, Clinical Center, University of Sarajevo,<br />
Bosnia and Hercegovina
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 51<br />
Fig 1a In a group of patients at conservative management, female population was predominant<br />
Conservative management<br />
27,50 %<br />
72,50 %<br />
Males<br />
Females<br />
1 2<br />
Fig 1b. The same pattern of female predominance was observed also in haemodialysis treatment<br />
Haemodilaysis<br />
51,60%<br />
Female<br />
48,40%<br />
Males<br />
1 2<br />
Table 2. Average age<br />
Number of<br />
Therapy type<br />
patients<br />
Conservative management<br />
Mean age in years<br />
Standard<br />
deviation<br />
Standard<br />
omission<br />
p-values<br />
I degree 9 62,44 9,96 3,32 n.s.<br />
II degree 7 57,57 12,37 4,68 n.s.<br />
III degree 24 58,71 9,00 1,84 n.s.<br />
Total 40 59,35 10,03 1,59 n.s.<br />
Haemodialysis 31 51,55 11,78 2,12 p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 52<br />
Table 4. Ultrasonic assessment of thyroid gland<br />
Regular<br />
assessment of %<br />
thyroid gland<br />
Conservative<br />
management<br />
Irregular<br />
assessment of<br />
thyroid gland<br />
%<br />
Total number<br />
of patients<br />
I degree 2 22,2 7 78,8 9 100<br />
II degree 3 42,9 4 57,1 7 100<br />
III degree 10 29,4 24 70,6 34 100<br />
Total 15 37,5 25 62,5 40 100<br />
Haemodialysis 19 61,3 12 38,7 31 100<br />
Total 34 47,9 37 52,1 71 100<br />
%<br />
Ultrasonic assessment of thyroid<br />
gland (conservative management)<br />
Ultrasonic assessment of thyroid<br />
gland (haemodialysis treatment)<br />
Regular<br />
assessment<br />
38%<br />
Irregular<br />
assessmnet<br />
Irregular<br />
assessment<br />
39%<br />
Regular<br />
assessment<br />
62%<br />
61%<br />
Fig 2a<br />
Fig 2b<br />
Ultrasonic assessment was irregular in 62% of patients at conservative management (Figure 2a), and in 39% patients<br />
at haemodialysis treatment (Figure 2b)<br />
Table 5. Average values of thyroid hormone in different groups of patients<br />
TT4 nmol/l TT3 nmol/l FT4 pmol/l FT3 pmol/l TSH mlU/l TBG mg/l<br />
Total<br />
proteins<br />
I degree 128,00±38,59 2,18±0,82 15,43±3,49 4,43±1,02 2,48±1,32 26,87±2,3 70,22±3,91<br />
II degree 123,40±57,23 2,33±0,93 15,40±2,65 4,62±1,43 1,96±0,90 23,51±3,5 72,14±5,59<br />
III degree 99,42±28,62 2,09±0,47 13,43±2,36 4,23±0,84 3,03±1,67 20,58±7,8 73,71±4,48<br />
Total 110,10±26,86 2,15±0,67 14,25±2,76 4,28±1,01 2,72±1,54 22,51±6,8 72,65±4,79<br />
Hemodialysis 93,13±23,94 2,11±0,76 11,86±2,29 4,35±1,02 2,13±1,45 22,55±7,6 72,32±4,95<br />
Control group 123,09±3,51 2,94±0,14 17,72±1,59 5,66±0,21 2,54±0,87 23,22±3,4 75,70±4,24<br />
p values P
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 53<br />
Average values of TT4<br />
in groups of patients<br />
Conservative<br />
ti<br />
Haemodialysis<br />
Control<br />
1 2 3<br />
110,10 93,13 123,09<br />
Fig 3. Significantly lower average values of hormones TT4 in evaluated groups of patients at conservative<br />
management and haemodialysis in comparison with the control group<br />
Average values of TT3<br />
in groups of patients<br />
2,94<br />
3,00<br />
2,15 2,11<br />
2,00<br />
1,00<br />
0,00<br />
Total conservative<br />
Haemodialysis<br />
Control group<br />
Fig 4. Significantly lower average values of TT3 in evaluated groups of patients in comparison with the control group<br />
FT4 average values in groups of patients<br />
20,00<br />
10,00<br />
0,00<br />
14,25<br />
11,86<br />
17,72<br />
Conservative management<br />
Haemodialysis<br />
Control group<br />
Fig 5. Significantly lower value of serum hormone FT4 in evaluated groups in comparison with the control group
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 54<br />
Average values of FT3 in groups of patients<br />
6 4,28<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
Total conservative management<br />
Haemodialysis<br />
5,66<br />
4,35<br />
Control group<br />
Fig 6. Significantly lower values of serum hormone FT3 in patients at conservative management<br />
and haemodialyis treatment in comparison with the control group<br />
Average values of TSH in groups of patients<br />
3,00<br />
2,50<br />
2,00<br />
1,50<br />
1,00<br />
0,50<br />
0,00<br />
2,72 2,13 2,54<br />
Total conservative management Haemodialysis Control group<br />
Fig 7. TSH value was not significantly lower in evaluated groups in comparison with the controls<br />
Average values of TBG in groups of patients<br />
22,51 22,55<br />
23,22<br />
1 2 3<br />
Fig 8. There are no significant differences between TBG values in evaluated groups of patients in comparison with controls<br />
Discussion<br />
Higher rates of goiter, hypothyroidism, thyroid nodules and<br />
thyroid carcinoma could be more typical at CRF patients than<br />
at general population (1-5). In our study 62,5% patients of<br />
conservative management and 38,7% of haemodialysis<br />
treatment had thyroid nodules in one or both thyroid lobes.<br />
All patients of evaluated groups had lower serum values of<br />
total proteins in compare with control group (6-11),<br />
confirming theory of malnutrition (6,7). Patients were<br />
clinically euthyroid, which correspons to the ”Sick euthyroid<br />
syndrome”, according to available literature (12,13). Average<br />
ages of patients in evaluated groups correspond to world<br />
information and its amount is 59 yrs.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 55<br />
Conclusions<br />
Ultrasonic nodules changes one or both lobules of thyroid<br />
gland were recorded at 52,1% of examined patients. Average<br />
values of serum concentrations TT4, TT3, FT4, and FT3<br />
were significantly lower in patients with CRF at conservative<br />
management and haemodialysis treatment in compare with<br />
patients of control group. Duration of haemodialysis<br />
treatment is inversely proportionally serum value TT3 in<br />
evaluated patients. Serum concentrations TSH and TBG were<br />
same in patients of evaluated groups in compare with control<br />
group. Serum value of total proteins was significantly lower<br />
of tested patients in compare with control group. 3% out of<br />
total number of 71 patients with CRF had clinically<br />
hypotiroidsm, and required substitutive therapy. 97% were<br />
clinically euthyroid (“Sick Euthyroid syndrome”).<br />
References<br />
1. Miki H, Oshimo K, Inque H, Kawano M, Tanaka K, Komaki<br />
K, Uyama T, Kawauchi M, Minakuchi J, Kawashima S,<br />
Monden Y. Thyroid nodules in female uremic patients on<br />
maintenance hemodialysis. J Surg Oncol 1993; 54: 216-218<br />
2. Prinz RA, Barbato AL, Lawrance AM, Paloyan E. Simultaneus<br />
primary hyperparathyroidism and nodular thyroid disease.<br />
Surgery 1982; 92: 454-458<br />
3. Kantor AF, Hoover RN, Kinlen LJ, McMullan R, Fraumeni JF.<br />
Cancer in patients receiving long-term dialysis treatment. Am J<br />
Epidemiol 1987; 126: 370-376<br />
4. Penn I. The effect of immunosuppresion on pre-exiting cancers.<br />
Transplantation 1993; 55: 742-747<br />
5. Brunner FP, Landais P, Selwood NH. Malignancies after renal<br />
transplantation: the EDTA-ERA registry experience. Nephrol<br />
Dial Transpl 1995; 10(suppl.): 74-80<br />
6. Owens WF, Lew NL, Liu Y, Lowrie EG, Lazarus JM.The urea<br />
reduction ratio and serum albumin concentration as predictors<br />
of mortality in patients undergoing hemodialysis. N Engl J Med<br />
1993; 329: 1001-1006<br />
7. Lim VS, Fang VS, Katz Al, Refetoff S. Thyroid disfunction in<br />
chronic renal failure: A study of the pituitary-thyroid axis and<br />
peripheral turnover kinetics of thyroxine and triiodthyronine. J<br />
Clin Invest 1977; 60: 522-534<br />
8. Oppenheimer JH, Schwartz HL, Mariash CN, and Kaiser FE.<br />
Evidence for a factor in the sera of patients with non-thyroidal<br />
disease which inhibitsiodothyronine binding by solid matrices,<br />
serum proteins, and rat hepatocites. J Clin Endocrinol Metab.<br />
1982; 54: 757-766<br />
9. Chopra IJ, Van Herle AJ, Chua Teco GN, Nguyen AH. Serum<br />
free thyroxine in thyroidal and nonhyroidal illnesses: A<br />
comparison of measurement by radioimmunoassay, equilibrium<br />
dialysis, and freethyroxine index. J Clin Endocrinol Metab.<br />
1980; 51: 135-143<br />
10. Nelson JC, Wilcox RB, Pandian MR. Dependence of free<br />
thyroxine estimates obtained with equilibrium tracer dialysis on<br />
the concentration of thyroxine- binding globulin. Clin Chem<br />
1992; 38: 1294-1300<br />
11. Robey C, Shreedhar K, Batuman V. Effect of chronic<br />
peritoneal dialysis on thyroid function tests. Am J Kidney Dis<br />
1989; 13: 99-103<br />
12. Lim VS, Henriwuez C, Seo H, Refetof S, Martino E. Thyroid<br />
function in a uremic rat model: Evidence suggesting tissue<br />
hypothyroidism. J Clin Invest 1980; 66: 946-954<br />
13. Lim VS, Flanigan MJ, Zavala DC, Freeman RM. Protective<br />
adaptation of low serum triiodothyronine in patients with<br />
chronic renal failure. Kidney Int 1985; 28: 541-549<br />
14. Owen WF Jr, Lew NL, Liu Y, Lowrie EG, Lazarus JM. The<br />
urea reduction ratio and serum albumin concentration as<br />
predictors of mortality in patients undergoing hemodialysis. N<br />
Engl J Med 1993; 329: 1001-1006
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 56<br />
Prednisone/Cyclophosphamide treatment in adult-onset autosomal<br />
dominant familial focal segmental glomerulosclerosis (FSGS 1)<br />
L. Grcevska 1 , S. Dzikova 1 , V. Ristovska 1 , M. Milovanceva Popovska 1 , G. Petrusevska 2<br />
and M. Polenakovic 1<br />
1 Department of Nephrology, Clinical Center Skopje, 2 Institute of Pathology, Faculty of Medicine Skopje, Republic of Macedonia<br />
Abstract<br />
Familial FSGS is a heterogeneous disease characterized by<br />
proteinuria and an unremitting deterioration of the excretory<br />
function. FSGS 1 is a less severe form of familial FSGS with<br />
autosomal-dominant inheritance, adult onset and slow<br />
progression to end-stage renal failure. Previous studies<br />
showed steroid unresponsiveness or variable response to<br />
steroids, cyclophosphamide and ACE inhibitors, and low rate<br />
of recurrence after transplantation.<br />
We treated with steroids/cyclophosphamide 8 patients (3<br />
families) with FSGS1 (aged 24±3,11) and compared the<br />
results to 20 patients with idiopathic FSGS (aged 35±2), and<br />
6 untreated patients with familial form. The treatment<br />
included prednisone 0,5mg/kg/daily for 4 months with slow<br />
tapping over to 20mg daily for further 6 months and<br />
cyclophosphamide 50mg daily 6 months, alternate use after.<br />
The follow-up period was two years.<br />
None of the patients with idiopathic FSGS experienced endstage<br />
renal failure during follow-up (serum creatinine<br />
115±10, to 183,4±65 mol/l) and proteinuria decreased<br />
(5,42±0,84 to 4,68±1,2g/d). One FSGS 1 patient died because<br />
of intracranial hemorrhage, 2/8 started dialysis within two<br />
years, but 5/8 presented similar results as control group: slow<br />
increase of creatinine form 130,62±15,91 to 215,78±63,62<br />
mol/l and slight decrease of proteinuria from 4,69±0,81 to<br />
3,28±0,24g/d. All untreated patients with FSGS1 experienced<br />
end-stage renal failure within two years.<br />
Both forms of adult-onset FSGS, idiopathic and familial<br />
presented slow deterioration of the renal function under<br />
immunosuppression, but we can not say that they are good<br />
responders: complete or partial remission was not noted. The<br />
number of treated patients is small to make exact<br />
conclusions.<br />
Key words: familial focal segmental glomerulosclerosis,<br />
prednisone, cyclophosphamide<br />
Introduction<br />
The discovery of molecular effects of podocyte components<br />
causing familial forms of nephrotic syndrome suggested the<br />
role of podocytes as the site of permselectivity in the kidney<br />
(1). Since then, knockout models of podocyte components<br />
and further molecular genetic screenings definitely<br />
consolidated this concept (1,2). Nephrin (NPHS1) was the<br />
first podocyte protein to be found mutated in association with<br />
a rare form of congenital nephrotic syndrome with autosomal<br />
recessive inheritance. Podocin (NPHS2) was the second<br />
recognized protein to cause proteinuria in familial cases with<br />
recessive inheritance and in sporadic patients (1,2,3). The<br />
clinical picture of nephrotic syndrome caused by podocin<br />
mutations ranges from an early onset, resembling congenital<br />
nephrotic syndrome to a late onset in the second decade of<br />
life, resembling idiopathic focal segmental<br />
glomerulosclerosis (1,5). Finally, -actinin 4 was the most<br />
recognized structural component of the podocyte causing<br />
proteinuria in rare cases of dominant nephrotic syndrome in<br />
adults. So, the familial forms of FSGS are caused by<br />
mutations in genes at (1,6):<br />
- 1q25-31 for NPHS2, autosomal recessive form, and<br />
- 11q21-22, and 19q13 for -actinin 4, autosomal<br />
dominant form of FSGS (FSGS1)<br />
Patients with autosomal recessive form do not respond to<br />
standard steroid treatment of nephrotic syndrome and exhibit<br />
a decreased risk of FSGS recurrence after kidney<br />
transplantation (7-9).<br />
The aim of our study was to analyze the responsiveness to<br />
prednisone/cyclophosphamide treatment in two groups of<br />
patients: (I) patients with adult-onset autosomal dominant<br />
familial FSGS (1) and (II) patients with idiopathic FSGS.<br />
Patients and methods<br />
Selection of the patients<br />
3 groups of patients were included in the study.<br />
1. 8 patients (3 families) with FSGS1 aged 24±3,11, treated.<br />
2. 20 treated patients with idiopathic FSGS aged 35±2<br />
3. 6 untreated patients with FSGS 1 (treated only with<br />
supportive treatment), aged 26±4,2.<br />
Treatment and follow-up<br />
Prednisone 0,5mg/kg/daily was performed for 4 months with<br />
slow tapping over to 20mg daily for the further 6 months,<br />
then continuing with this dosage to the end of the study. The<br />
daily dosage of cyclophosphamide for the first 6 months was<br />
50mg, alternate day use was performed later. The whole<br />
follow-up period was two years. Laboratory investigations<br />
were performed monthly.<br />
______________________<br />
Correspodence to: L. Grcevska, Department of Nephrology, Clinical Center Skopje Vodnjanska 17, Skopje,<br />
Republic of Macedonia; Phone: +389 23 123 334; E-mail: maknefpo@mt.net.mk
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 57<br />
Results<br />
Idiopathic FSGS<br />
None of the patients experienced end-stage renal failure<br />
during follow-up. Serum creatinine presented slight, non<br />
significant increase, from 115±10, to 183,4±65 mol/l,<br />
p>0,05. Proteinuria decreased, but also non-significantly,<br />
from 5,42±0,84 to 4,68±1,2g/daily, p>0,05. So we did not<br />
noted partial or complete remission of the nephrotic<br />
syndrome.<br />
FSGS1 patients – treated<br />
One of the patients, 20-year old, female, died because of<br />
intracranial hemorrhage due to severe form of hypertension.<br />
2/8 patients started dialysis within two years, one after 18<br />
months, the other after 6 months. The second patient (male,<br />
18 years) was transplanted after two months dialysis<br />
treatment without evidence of recurrence during the followup.<br />
5/8 patients presented similar results as idiopathic form.<br />
Slight, but significant increase of serum creatinine was noted<br />
in this group of patients, from 130,62±15,91 to 215,78±63,62<br />
mol/l, p0,05), from 4,69±0,81 to 3,28±0,24g/daily, so it was still<br />
in nephrotic ranges.<br />
FSGS1 patients – untreated<br />
The results at the end of the study were catastrophic. At start,<br />
their mean value of serum creatinine was not significantly<br />
different comparing to previous two groups: 167,92±45,21<br />
mol/l. All six patients experienced end-stage renal failure<br />
within two years.<br />
Discussion<br />
There are many studies on genetic disorders in familial forms<br />
of FSGS (1-3,10-13), but the experience with the treatment of<br />
these cases is poor, so it is very difficult for us to compare<br />
our results. It was accepted that nephrotic syndrome in<br />
familial forms of FSGS is steroid resistant (2,7,11,13).<br />
Patients with homozygous or compound heterozygous<br />
mutations in NPHS2 exhibit primary steroid resistance and a<br />
decreased risk of FSGS recurrence after kidney<br />
transplantation (7). There was published a study in 2004<br />
which tested this hypothesis comparing the results between<br />
two groups of patients: 1)190 patients with familial FSGS<br />
and 2) 124 patients with idiopathic FSGS (7). Recurrence of<br />
the disease was noted in only 8% of familial form, but in<br />
35% of idiopathic form. Because of steroid unresponsiveness<br />
of familial form, the patients in this study were treated with<br />
cyclosporine A and cyclophosphamide with partial response.<br />
Besides small number of patients we noted some encouraging<br />
results: 5/8 treated patients did not develop end stage renal<br />
failure after two years and all untreated ones did.<br />
Conclusions<br />
The small number of patients did not allow us to perform<br />
standard statistic methods in order to make exact conclusions.<br />
It is also unclear what can be the mechanism of the drug<br />
acting in the patients who responded and did not worsen their<br />
renal function.<br />
References<br />
1. Caridi G et al. Broadening the spectrum of diseases related to<br />
podocin mutations. J am Soc Nephrol 2003; 14: 1278-1286<br />
2. Pollak MR. The genetic basis of FSGS and steroid-resistant<br />
nephrosis. Semin Nephrol 2003; 23: 141-146<br />
3. Winn MP. Approach to the evaluation of heritable diseases and<br />
update of familial focal segmental glomerulosclerosis. Nephrol<br />
Dial Transplant 2003; 6: vi14-20<br />
4. D’agati V. Pathologic classification of focal segmental<br />
glomerulosclerosis. Semin Nephrol 2003; 23: 117-134<br />
5. Winn MP et al. Clinical and genetic heterogeneity in familial<br />
focal segmental glomerulosclerosis. International collaborative<br />
group for therapy of familial focal segmental<br />
glomerulosclerosis. Kidney Int 1999; 55: 1241-1246<br />
6. Rana K et al. Clinical, histopathologic, and genetic studies in<br />
nine families with focal segmental glomerulosclerosis. Am J<br />
Kidney Dis 2003; 41: 1170-1178<br />
7. Ruf RG et al. Patients with mutations in NPHS2 (podocin) do<br />
not respond to standard steroid treatment of nephrotic<br />
syndrome. J Am Soc Nephrol 2004; 15: 722-732<br />
8. Weber S et al. NPHS2 mutation analysis shows genetic<br />
heterogeneity of steroid resistant nephrotic syndrome and low<br />
post-transplant recurrence. Kidney Int 2004; 66: 571-579<br />
9. Yorgin PD, Belson A, Higgins J, Alexander SR. Pulse<br />
methylprednisolone, cyclosporine, and ace inhibitor therapy<br />
decreases proteinuria in two siblings with familial focal<br />
segmental glomerulosclerosis. Am J Kidney Dis 2001; 37: E44<br />
10. Conlon PJ et al. Spectrum of disease in familial focal and<br />
segmental glomerulosclerosis. Kidney Int 1999; 56: 1863-1871<br />
11. Ekim M et al. Three siblings with steroid-resistant nephritic<br />
syndrome: new NPHS2 mutations in a Turkish family. Am J<br />
Kidney Dis 2004; 44: 10-12<br />
12. Koziell A et al. Genotype/phenotype correlations of NPHS1<br />
and NPHS2 mutations in nephrotic syndrome advocate a<br />
functional inter-relationship in glomerular filtration. Human<br />
Molecular genetics 2002; 11: 379-388<br />
13. Karle SM et al. Novel mutations in NPHS2 detected in both<br />
familial and sporadic steroid-resistant nephritic syndrome. J Am<br />
Soc Nephrol 2002; 13: 388-393
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 58<br />
Microalbuminuria – The new marker for Balkan Endemic Nephropathy?<br />
G. Imamovic 1 , S. Trnacevic 1 , M. Tabakovic 1 , E. Mesic 1 , M. Uzeirbegovic 2 , M. Malohodzic 3 ,<br />
A. Halilbasic 1 , V. Habul 1 , D. Tulumovic 1 , E. Hodzic 1 , M. Atic 1 , S. Lekic 1 M. Dugonjic 1 ,<br />
A. Becirovic 1 and E. Hasanovic<br />
1 Clinic for nephrology, urology, dialysis and renal transplantation, 2 Central laboratory, 3 Nuclear medicine department, University<br />
medical center Tuzla, Bosnia and Herzegovina<br />
Abstract<br />
Several criteria are necessary to meet in order to have the<br />
diagnosis of Balkan endemic nephropathy established. One of<br />
them is tubular proteinuria type that may be found, but not in<br />
the early stage of the disease. Beta 2 microglobulin may be<br />
found in the early stage, but its determination is rather<br />
cumbersome and not suitable for a daily routine. Therefore,<br />
urinary albumin/creatinine ratio was determined in 8 patients<br />
(all females, aged 58,37±4,37 years) from the town of Šamac<br />
region (Bosnia and Herzegovina) as a measure of albumin<br />
excretion in order to establish useful marker in the early stage<br />
of the disease. Increased urinary albumin/creatinine ratio, was<br />
found in 50% of BEN patients. According to these<br />
preliminary results, microalbuminuria could be used as the<br />
reliable marker for the early detection of BEN.<br />
Key words: Balkan endemic nephropathy, microalbuminuria,<br />
urinary albumin/creatinine ratio<br />
Introduction<br />
Balkan endemic nephropathy (BEN) is an unknown disease<br />
that ultimately leads to terminal uremia. It affects rural<br />
population of Croatia, Bosnia and Herzegovina, Serbia,<br />
Romania and Bulgaria. It is characterized primarily with<br />
tubulo-interstitial changes (1) and predominant tubular<br />
proteinuria type has been reported by now (2). Beta 2<br />
microglobulin (B2M) has been used as a marker for early<br />
detection of the disease, but its use is rather complicated and<br />
not applicable for a daily routine. Quantitative measurement<br />
of urinary albumin as a marker of an early tubular changes<br />
has not been done by now. Therefore, we tested nonproteinuric<br />
urine samples of patients suffering from early<br />
stages of BEN for microalbuminuria in order to suggest<br />
possible new reliable BEN marker.<br />
Patients and methods<br />
Urinary albumin to creatinine ratio was determined in<br />
random urine samples in eight patients suffering from the<br />
early stage of BEN (all females, aged 58,37±4,37 years,<br />
range 51-63) from the town of Šamac region, Bosnia and<br />
Herzegovina<br />
Patients were selected on the basis of established criteria.<br />
Half of them had biopsy-proven lesions compatible with<br />
BEN in a study done 17 years ago (1). Hypertension, diabetes<br />
mellitus, heart failure and urinary tract infection have been<br />
ruled out because those conditions give rise to<br />
microalbuminuria themselves.<br />
Random urine samples were first tested on proteinuria with<br />
20% sulfosalycilic acid (SSA) test. The SSA test is<br />
performed by mixing one part urine supernatant (e.g., 2.5<br />
mL) with three parts 3 percent sulfosalicylic acid, and<br />
grading the resultant turbidity according to the following<br />
schema (the numbers in parentheses represent the<br />
approximate protein concentration): 0 = no turbidity (0<br />
mg/dL), trace = slight turbidity (1 to 10 mg/dL), 1+ =<br />
turbidity through which print can be read (15 to 30 mg/dL),<br />
2+ = white cloud without precipitate through which heavy<br />
black lines on a white background can be seen (40 to 100<br />
mg/dL), 3+ = white cloud with fine precipitate through<br />
which heavy black lines cannot be seen (150 to 350 mg/dL),<br />
4+ = flocculent precipitate (>500 mg/dL). Only those who<br />
proved non-proteinuric were tested on microalbuminuria<br />
using urinary albumin/creatinine ratio.<br />
Albumin was determined by immunonephelometric method<br />
using BN System (Dade Behring) on the basis of scattered<br />
light that has passed through immune complexes made up of<br />
albumin and specific antibodies. Intensity of scattered light<br />
was proportional to the quantity of the albumin in a sample.<br />
Results were evaluated by comparing them with the standard<br />
of known concentration.<br />
Creatinine in serum and urine was determined using autoanalyzer<br />
Dimension RxK (Dade Behring) with kinetic<br />
method by Jaffe, modified by Larsen (3).<br />
Albumin to creatinine ratio was then calculated. The cutpoint<br />
for females is > or = 2,7 mg/mmol (25 mcg/mg) (4)<br />
Diethylen Threeamino Penta Acetate (DTPA) clearance rate<br />
was determined by computerized method after the patients<br />
had been overloaded with fluid (1 L two hours prior to the<br />
test) and after they had voided. Tc99m DTPA was then<br />
applied in a dose of 185 MBq. Radioactivity was measured,<br />
memorized in a computer and clearance rate calculated.<br />
The statistical analysis was done using chi square test.<br />
P
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 59<br />
microalbuminuric range in US (5,6) and between 5% and 7%<br />
in Europe (7,8).<br />
Results<br />
Urinary albumin/creatinine ratios in individual samples are<br />
shown in Table 1. Increased urinary albumin/creatinine ratio<br />
was found in 50% of BEN patients, what was statistically<br />
significant result (p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 60<br />
Lymphatic neoangiogenesis in human neoplasia and transplantation as<br />
experiments of nature<br />
D. Kerjaschki<br />
Department of Pathology, Medical University of Vienna, Austria<br />
Introduction<br />
A plexus of lymphatic vessels guides interstitial fluid,<br />
passenger leukocytes, and tumor cells towards regional<br />
lymph nodes. Microvascular endothelial cells of lymph<br />
channels (LECs) are difficult to distinguish from those of<br />
blood vessels (BECs) because both express a similar set of<br />
markers, such as CD31, CD34, podocalyxin, von Willebrand<br />
factor (vWF), etc. Analysis of the specific properties of LECs<br />
was hampered so far by lack of tools to isolate LECs.<br />
Recently, the 38 kD mucoprotein podoplanin was found to be<br />
expressed by microvascular LECs but not BECs in vivo. Here<br />
we isolated for the first time podoplanin + LECs and<br />
podoplanin - BECs from dermal cell suspensions by<br />
multicolor flow cytometry. Both EC types were propagated<br />
and stably expressed VE-cadherin, CD31, and vWF.<br />
Molecules selectively displayed by LECs in vivo, i.e.,<br />
podoplanin, the hyaluronate receptor LYVE-1, and the<br />
vascular endothelial cell growth factor (VEGF)-C receptor,<br />
Flt-4/VEGFR-3, were strongly expressed by expanded LECs,<br />
but not BECs. Conversely, BECs but not LECs expressed<br />
VEGF-C. LECs as well as BECs formed junctional contacts<br />
with similar molecular composition and ultrastructural<br />
features. Nevertheless, the two EC types assembled in<br />
vascular tubes in a strictly homotypic fashion. This EC<br />
specialization extends to the secretion of biologically relevant<br />
chemotactic factors: LECs, but not BECs, constitutively<br />
secrete the CCR7 ligand SLC/CCL21 at their basal side,<br />
while both subsets, upon activation, release MIP-3a/CCL20<br />
apically. These results demonstrate that LECs and BECs<br />
constitute stable and specialized EC lineages equipped with<br />
the potential to navigate leukocytes and, perhaps also, tumor<br />
cells into and out of the tissues.<br />
Lymphatic Neoangiogenesis in Human Cancer.<br />
Formation of lymphatic metastasis is the initial step of<br />
generalized spreading of tumor cells, and predicts poor<br />
clinical prognosis. Lymphatic vessels generally arise within<br />
the peritumoral stroma, although the lymphangiopoetic<br />
vascular endothelial growth factors (VEGF)–C and -D are<br />
secreted in apparently small amounts by tumor cells. In a<br />
carefully selected collective of human cervical cancers (stage<br />
pT1b1) we demonstrate by quantitative<br />
immunohistochemistry and in situ hybridization that density<br />
of lymphatic microvessels is significantly increased in<br />
peritumoral stroma, and that a subset of stromal cells express<br />
large amounts of VEGF-C and -D. The density of cells<br />
producing these vascular growth factors correlates with<br />
peritumoral inflammatory stroma reaction, lymphatic<br />
microvessel density, peritumoral carcinomatous<br />
lymphangiosis, and with the frequency of lymph node<br />
metastasis. The VEGF-C and -D producing stroma cells were<br />
identified in situ as a subset of activated tumor associated<br />
macrophages (TAMs) by expression of a panel of<br />
macrophage specific markers, including CD68, CD23, CD14<br />
and others, in double-immunofluorescence confocal<br />
microscopy. These group of TAMs also expressed the<br />
VEGF-C and -D specific tyrosine kinase receptor flt-4. As<br />
TAMs are derived from monocytes in the circulation, a<br />
search in peripheral blood for candidate precursors of flt-4<br />
expressing TAMs revealed a subfraction of flt-4 expressing,<br />
CD14-positive monocytes, that, however, failed to express<br />
VEGF-C and -D. Only after in vitro incubation with TNFα,<br />
LPS or VEGF-D these naive monocytes started to synthesise<br />
VEGF-C de novo. In conclusion VEGF-C expressing TAMs<br />
play a novel role in peritumoral lymphangiogenesis, and<br />
subsequent dissemination in human cancer.<br />
Lymphatic Neoangiogenesis in Human Renal Transplants.<br />
Renal transplant rejection is caused by a lymphocyte rich<br />
inflammatory infiltrate that attacks cortical tubules and<br />
endothelial cells. Immunosupressive therapy reduces the<br />
number of infiltrating cells, however, their exit routes are not<br />
known. Here we demonstrate by immunohistochemistry on<br />
human renal transplant biopsies, a > 100 fold increase of<br />
lymphatic vessel density over normal kidneys in grafts with<br />
nodular mononuclear infiltrates, using antibodies to the<br />
lymphatic endothelial marker protein podoplanin. Nodular<br />
infiltrates are constantly associated with newly formed, Ki-67<br />
expressing lymphatic vessels and contain the entire repertoire<br />
of T- and B-lymphocytes to provide specific cellular and<br />
humoral alloantigenic immune responses, including Ki-67 +<br />
CD4 + and CD8 + T-lymphocytes, S100 + dendritic cells, as<br />
well as Ki-67 + CD20 + B-lymphocytes and l- and k-chainexpressing<br />
plasmacytoid cells. Numerous chemokine receptor<br />
CCR7 + cells within the nodular infiltrates are apparently<br />
attracted by secondary lymphatic chemokine (SLC/CCL21)<br />
that is produced and released by lymphatic endothelial cells<br />
in a complex with podoplanin. Thus, lymphatic<br />
neoangiogenesis contributes not only to the export of the<br />
rejection infiltrate, but is also involved in the maintainance of<br />
a potentially detrimental alloreactive immune response in<br />
renal transplants, and provides a novel therapeutic target.<br />
______________________<br />
Correspodence to: D. Kerjaschki, Department of Pathology, Medical University of Vienna, Austria
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 61<br />
A Novel Role for Podoplanin in Lymphangiogenesis.<br />
In order to analyze podoplanin function in the development<br />
of the lymphatic vasculature, we generated podoplanin -/- mice<br />
in 129S/v : Swiss background.<br />
The lack of podoplanin resulted in loss of about 30 % of the<br />
embryos. Within the first week, approximately 55% of born<br />
podoplanin -/- mice died, but 20% of born mice survived till<br />
adulthood. With respect to the lymphatic vasculature, young<br />
podoplanin -/- mice showed enlarged and tortuous lymphatic<br />
vessels, while the lymphatic network was impaired.<br />
Additionally, throughout the small intestine a network of<br />
dilated, tortuous and leaky lymphatic vessels resulting in the<br />
chylous ascitis and hyperemic Peyer´s patches were found.<br />
Lymphatic fluid transport, as revealed by intradermal<br />
injection of Chicago sky blue dye, was impaired in the<br />
knockouts. These data indicate that formation of the<br />
lymphatic vessel system is erroneous in lymphoid and nonlymphoid<br />
tissues in podoplanin -/- mice. The most impressive<br />
alkteration of the lymphatic vessels in Podoplanin -/- mice,<br />
however, was their lack of separtion from the blood<br />
vasculature during their entire life span. We have<br />
demonstrated that this separation defect is due to the platelet<br />
aggregating effect of podoplanin on LEC surfaces. Thus,<br />
platelets that come in contact with LECs in the embryonic<br />
lymphatic saccules aggregate and degranulate, and induce<br />
constriction of the blood vascular-lymphatic anastomosis<br />
(10).<br />
References<br />
1. Kerjaschki D, Regele HM, Moosberger I, Nagy-Bojarski K,<br />
Watschinger B, Soleiman A, Birner P, Krieger S, Hovorka A,<br />
Silberhumer G, Laakkonen P, Petrova, T, Langer B, Raab I.<br />
Lymphatic neoangiogenesis in human kidney transplants is<br />
associated with immunologically active lymphocytic infiltrates.<br />
J Am Soc Nephrol 2004; 15: 603-12<br />
2. Schoppmann SF, Birner P, Stockl J, Kalt R, Ullrich R, Caucig<br />
C, Kriehuber E, Nagy K, Alitalo K, Kerjaschki D. Tumorassociated<br />
macrophages express lymphatic endothelial growth<br />
factors and are related to peritumoral lymphangiogenesis. Am J<br />
Pathol 2002; 161: 947-56<br />
3. Petrova TV, Makinen T, Makela TP, Saarela J, Virtanen I,<br />
Ferrell RE, Finegold DN, Kerjaschki D, Yla-Herttuala S,<br />
Alitalo K. Lymphatic endothelial reprogramming of vascular<br />
endothelial cells by the Prox-1 homeobox transcription factor.<br />
EMBO J 2002; 21: 4593-9<br />
4. Saaristo A, Veikkola T, Enholm B, Hytonen M, Arola J,<br />
Pajusola K, Turunen P, Jeltsch M, Karkkainen MJ, Kerjaschki<br />
D, Bueler H, Yla-Herttuala S, Alitalo K. Adenoviral VEGF-C<br />
overexpression induces blood vessel enlargement, tortuosity,<br />
and leakiness but no sprouting angiogenesis in the skin or<br />
mucous membranes. FASEB J 2002; 16: 1041-9<br />
5. Kang DH, Kanellis J, Hugo C, Truong L, Anderson S,<br />
Kerjaschki D, Schreiner GF, Johnson RJ. Role of the<br />
microvascular endothelium in progressive renal disease. J Am<br />
Soc Nephrol 2002; 13: 806-16<br />
6. Kriehuber E, Breiteneder-Geleff S, Groeger M, Soleiman A,<br />
Schoppmann SF, Stingl G, Kerjaschki D, Maurer D. Isolation<br />
and characterization of dermal lymphatic and blood endothelial<br />
cells reveal stable and functionally specialized cell lineages. J<br />
Exp Med 2001; 194: 797-808<br />
7. Breiteneder-Geleff S, Soleiman A, Kowalski H, Horvat R,<br />
Amann G, Kriehuber E, Diem K, Weninger W, Tschachler E,<br />
Alitalo K, Kerjaschki D. Angiosarcomas express mixed<br />
endothelial phenotypes of blood and lymphatic capillaries:<br />
podoplanin as a specific marker for lymphatic endothelium. Am<br />
J Pathol 1999; 154: 385-94<br />
8. Matsui K, Breiteneder-Geleff S, Kerjaschki D. Epitope-specific<br />
antibodies to the 43-kD glomerular membrane protein<br />
podoplanin cause proteinuria and rapid flattening of podocytes.<br />
J Am Soc Nephrol 1998; 9: 2013-26<br />
9. Breiteneder-Geleff S, Matsui K, Soleiman A, Meraner P,<br />
Poczewski H, Kalt R, Schaffner G, Kerjaschki D. Podoplanin, a<br />
novel 43-kd membrane protein of glomerular epithelial cells, is<br />
down-regulated in puromycin nephrosis. Am J Pathol 1997;<br />
151: 1141-52<br />
10. Uhrin P, Zaujec J, Bauer M, Hilpert M, Kowalski H, Furtbauer<br />
E, Hannes Stockinger H, Kerjaschki D, Binder B R. Podoplanin<br />
induced platelet aggregation mediates separation of blood and<br />
lymphtic vessels. "submitted"
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 62<br />
Cytokines and acute renal failure<br />
K. Cakalaroski<br />
University Clinic for Nephrology, Clinical Centre, Skopje, Republic of Macedonia<br />
Introduction<br />
The crucial question in the settings of acute renal failure<br />
(ARF) is to elucidate the role of cytokines in the acute and<br />
chronic issue of the disease: death or survival with normal<br />
kidney function or inevitable evolution to chronic kidney<br />
disease (CKD) and terminal renal insufficiency.<br />
Topics for Discussion – Field of controversy<br />
Many years ago the relation between ischemic (mainly<br />
septic) ARF in the clinical settings and serum level of<br />
pro/anti inflammatory cytokines (IFNγ, TNFα, IL-1β, IL-<br />
6,IL-8,IL-10,ICAM –1,VCAM), is the field of controversy.<br />
Intrinsic ARF, as a special form of acute renal insufficiency<br />
is also associated with the cytokines production (their blood<br />
levels, kidney tissue and urine concentrations). The evolution<br />
of obstructive type of ARF may be related with the serum and<br />
tissue presence of anti and pro-inflammatory cytokines. ARF<br />
after kidney grafting is a differential diagnostic problem<br />
between s.c. initial tubulopathy and toxic effects of drugs<br />
used in the first few days after kidney transplantation.<br />
Plasma levels of pro and anti-inflammatory cytokines and<br />
adequate conservative measures on the one hand, and the<br />
mortality ratio in ARF on the other, may be strongly related.<br />
Elimination of cytokines from the blood and tissues<br />
compartments via extracorporeal procedures may have a<br />
beneficial effect on clinical evolution of ARF.<br />
Chronically elevated levels of pro-inflammatory cytokines<br />
once the ARF is over, are the signs of inflammation and<br />
progression to CKD. The limitations of the cytokines plasma<br />
dosing may compromise theirs clinical benefit.<br />
Sepsis related ischemic ARF<br />
The endotoxins (bacterial corporal lipopolysacharids, LPS s )<br />
via CD-14, activate and deliver cytokines (TNFα, IL-1β,IL-<br />
6) from polymorphonuclear cells (PMNC s ) in ARF patients,<br />
via the process named “cytokines deliberation” with<br />
consecutive higher plasma concentration of all measured<br />
cytokines when compared to CKD patients (1). The impaired<br />
monocyte’s cytokines production in critically ill patients with<br />
ARF is presented with a dip fall of the blood levels of TNFα<br />
and IL-6 (84% vs 45% respectively) (2). The elevated serum<br />
concentrations of sTNFα R I, II are predictive for septic<br />
shock induced ARF (3). The IL-6 enhances the renal injury,<br />
organs dysfunction and inflammation (producing T-cells<br />
activation and elevation of CRP plasma levels) caused by the<br />
whole body ischemia-reperfusion in patients with ARF due to<br />
______________________<br />
Correspodence to: K. Cakalaroski, University Clinic for Nephrology, Clinical Centre,<br />
Skopje, Republic of Macedonia<br />
systemic shock or cardiac arrest. The lesions correlate with<br />
the plasma level of IL-6: for each 100 pg/ml increase for IL-<br />
6, patients are 2.8 times likely to develop organ dysfunction<br />
(4). Endotoxemic ARF is caused by direct action of TNFα on<br />
TNFαR-1 in the kidney (proximal tubular epithelial cells,<br />
PTEC s ). In this case the urinary elimination of TNFα is<br />
increased (5). The Fas, FaSL and caspase mediated<br />
apoptopsis of PTEC s by inflammatory cytokines or LPS s , can<br />
be possible mechanism of endotoxic renal dysfunction (6).<br />
The cytokines stimulate PMNC s attraction, aggregations,<br />
adhaezion (via ICAM-1 and VCAM), activation and<br />
degranulation with lysosims liberation (7). The endothelial<br />
lesions, disseminated intravascular coagulation (DIC) via<br />
sepsis induced TF, fibrinolysis and prolonged<br />
vasoconstriction (because ET-1 production) – lead to tissue<br />
hypoxia, inflammation, Tc-mediated injury and ARF (8).<br />
Intrinsic ARF<br />
Many factors are included in the genesis of intrinsic ARF<br />
beginning with the obstetric shock and finishing with the<br />
acute tubulointerstitial nephritis. The obstetric shock is<br />
related to PAI-1 activation, renal DIC and a possible<br />
successive partial or total cortical necrosis of the kidney (9).<br />
Necrotic vasculitis mainly presented by a glomerulitis or<br />
pneumonitis is due to the activation of Th 1 and mediators of<br />
tissue injury like leucotriens, TxA 2 , PAF, reactive oxygen<br />
and nitrogenous metabolites (ROM, RNO), complement,<br />
intravascular activation of coagulation and secondary<br />
fibrinolysis. Interleukins (especially IL-2,IL-6,IL-8 and<br />
IFNγ), via nature killers cells (NK) and macrophages (M<br />
induce vascular (mainly capillary) leak syndrome because<br />
elevated plasma concentration of nitrogen oxide (NO). The<br />
consequences of capillary wall lesion are extension of<br />
interstitial volume, depletion of effective arterial blood<br />
volume, arterial hypotension and DIC with effective<br />
thrombocytopenia (under 60 000/cmm) and ARF (namely,<br />
acute tubular necrosis, ATN) (10). The acute tubulointerstitial<br />
nephritis is mediated by elevated plasma levels of<br />
interleukins (from IL-1 to IL-7), IFN s (α,β,γ), platelet derived<br />
growth factor –A, B, epithelial growth factor, fibrocyte<br />
growth facror-2, TNFα,β and TGFα,β generated by<br />
infiltrating and somatic renal cells (11,12).<br />
Tubular obstruction and ARF<br />
The endotoxins and the same cited pro-inflammatory<br />
cytokines provoke direct vasoconstrictive effects in the<br />
kidney, enhancement of tubular damage and delay of
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 63<br />
recovery phase. This type of ARF in the clinical practice is<br />
known as “nephrohydrosis” (13).<br />
Acute renal failure after kidney grafting<br />
The persistent urinary excretion of IL-6 and IL-8 means<br />
organic sustained ARF. Urinary TNFα and LDH are reduced<br />
in severe and increased in mild ARF (14). Severe ARF<br />
correlates with increased plasma concentration of TNFα,s<br />
TNFαR s 55,75. If the plasma levels of s TNFα R s diminish,<br />
the renal function improves explicating the better urinary<br />
excretion of TNFα R s (7). Uromodulin decreases in urine in<br />
the case of ARF and augments if acute rejection is no longer<br />
questionable (15).<br />
Plasma levels of pro and anti-inflammatory cytokines and<br />
mortality in ARF<br />
Many plasma cytokines (IFNγ, TNFα, IL-1β, IL-6,IL-8,IL-<br />
10) may predict mortality and correlate with the lethality rate<br />
in patients with ARF (2). Proinflammatopry cytokines<br />
(especially IFNγ, TNFα, IL-1β, IL-6, IL-8) lead to systemic<br />
inflammatory response syndrome (SIRS) and contrary antiinflammatory<br />
response syndrome (CARS) precipitating the<br />
lethal issue of ARF (following the results of PICARD study<br />
group). The plasma levels of IL-6 (not-survivors: survivors =<br />
235:114, pg/ml), IL-8 (not-survivors : survivors = 36:21,<br />
pg/ml) and IL-10 (not-survivors : survivors = 3.1 : 2.4, p/ml)<br />
are more increased in patients with ARF not-survivors when<br />
compared to survivors (16).<br />
Chronically elevated levels of pro-inflammatory cytokines<br />
as a sign of inflammation and progression to CKD<br />
The perpetual production of cytokines (IL-1, IL-6, IL-7,<br />
TNFα) is a central event in the patophysiology of cell<br />
mediated damage by resident mesangial, interstitial or<br />
infiltrating cells (17). The vascular endothelial dysfunction<br />
and accelerated atherosclerosis are related to acute phase<br />
proteins (CRP, SAP) and plasma cytokines demonstrating a<br />
chronic inflammatory state after ARF (18). Proteinuria<br />
transcripts the genes of pro-inflammatory cytokines (mainly<br />
TNFα gene) (19). The plasma levels of IL-1, TNFα and IFNγ<br />
directly correlate with ICAM-1 and VCAM-1 expression<br />
(20). The IFNγ / IL-10 ratio is greater in patients with severe<br />
nephrosclerosis due to lupus nephritis (21). The Th 1 /Th 2 renal<br />
parenchymal predominance support cell-mediated immune<br />
response and produce pro-inflammatory cytokines (IFNγ,<br />
TNFα, IL-12) as a mediators responsible for progression of<br />
renal lesions (22).<br />
Conservative therapeutic anti-cytokines options<br />
Many conservative therapeutic anti-cytokines procedures are<br />
trailed in the ARF patients with variable, mainly nonsatisfactory<br />
results. In the following text will be presented the<br />
most acceptable anti-cytokines conservative treatment.<br />
The inhibition of LPS activity is a theoretically very<br />
attractive therapeutic modality of septic induced ARF. The<br />
use of anti LPS monoclonal (E-5 murine, human anti lipid A<br />
region and HA-1A) and polyclonal antibodies (J5) in<br />
combination with the anti CD 14 Ra on the Mis effective<br />
in the experimental setting, but without efficacy in clinical<br />
medicine (23).<br />
The inhibition of IL-1 with r hu IL1Ra blocks the basic signal<br />
transduction and reduces interstitial cells infiltration (24).<br />
The inhibition of TNFα with murine anti TNFα monoclonal<br />
antibodies (afelimomab) in i.v continuous infusion, prevents<br />
endothelial lesions and reduce mortality in experimental and<br />
clinical cases (25).<br />
The inhibition of IL-6 with IL-6 monoclonal antibodies<br />
reduces the renal injury, kidney dysfunction and<br />
inflammation caused by ischemia-reperfusion via reduction<br />
of immuno-histochemical markers (ICAM-1, P-selectin,<br />
nitrothyrosin, ROM and RNM) (4). LPS may induce renal IL-<br />
6 m RNA synthesis that may be inhibited by a single dose of<br />
ACE inhibitors (like enalaprilate) and in this way, to prevent<br />
cytokines-induced renal damage during endotoxemia (31).<br />
There are other therapeutic conservative modalities used<br />
more or less successfully in patients with ARF like thyroid<br />
hormones (26), growth factors (EGF, HGF, IGF-1) (27),<br />
soluble P-selectin GP ligand –1 (28) and R hu PAF Ra (29).<br />
The blockade of sepsis induced tissue factor (TF) with site<br />
inactivated F VIIa (s.c.TF-F VIIa-complex) is a mode to<br />
attenuate kidney injury in septic shock (32). With Zn-bis DL-<br />
OH aspartat may be stimulated the production of heat shock<br />
proteins (mainly HSP-70) and the regeneration of necrotic<br />
tubular cells (33). The BMP-7 reduces the harmful effects of<br />
pro-inflammatory cytokines (IL-1β, IL-6, IL-8, TNFα, MCP-<br />
1) on kidney proximal tubular cells after inflammation related<br />
to ischemic injury and stimulates a tubular cells proliferation<br />
(42). The monomethyl arginin (L-NMMA) as a NO synthase<br />
(NOS) – blocker (34), vasodilative atrial natriuretic peptides<br />
(ANP s ) (35), anti-endothelin – 1 monoclonal antibodies and<br />
receptor antagonists (Anti ET-1 Mo abs; ET-1 Ras) (36,37),<br />
anti ICAM-1 monoclonal antibodies (38) and Arg-Gly-Asp<br />
(RGD) peptides (39) - are also trailed in clinical studies.<br />
Active therapeutic anti-cytokines options<br />
The aim of active therapeutic procedures is to eliminate or<br />
diminish the production of pro-inflammatory cytokines<br />
related to different haemodialysis membranes or to promote<br />
the elimination of active reactants from the blood, via extracorporeal<br />
devices (membranes, adsorbens).<br />
Today it is largely accepted that the cuprophan membrane<br />
enhances activation of various pathways of tubular cells<br />
injury during the haemodialysis procedure like ROM, RNM,<br />
cytokines, eicosanoides, complement production and PMNC s<br />
activation, as compared to synthetic membranes (40).<br />
The hydrophobic biocompatible high flux dialyzers<br />
membranes (PAN, PS, PA, PMMA, PAES) do not activate<br />
the M PMNC s and do not deliberate cytokines and other<br />
active chemical reactants (41).<br />
Elimination of active reactants via extracorporeal devices<br />
(membranes, adsorbens) today is accepted as an attractive<br />
therapeutic modality. Classical haemodialysis (HD) not<br />
influence the plasma levels of many cytokines (IL-1β, IL-2R,<br />
IL-6, TNFα), but reduces the blood levels of hemokine IL-8<br />
for 50% (43). CVVH ± HD improve hemodinamics in septic<br />
shock related ARF with or without modifying plasma<br />
concentration of cytokines (IL1β, TNFα) except IL-6,<br />
although the clearances for two basic pro-inflammatory<br />
cytokines is about the same (Clearance for TNFα = 21<br />
ml/min; clearance for IL-6 = 25 ml/min) (44).
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 64<br />
High permeability hemofiltration (HPHF) using polyflux<br />
hemofiltres with nominal cut-off point of 60 kD and<br />
intermittent hemoperfusion – hemofiltration (HP-HF),<br />
eliminate TNFα (Clearance = 15-28 ml/min), IL-6 (Clearance<br />
= 23-42 ml/min) and IL-1 Ra (Clearance = 25-54 ml/min) in<br />
septic patients with ARF (45). Plasmaferesis eliminates<br />
endotoxins (LPS s ), cytokines (IL-1β, IL-6, TNFα) soluble<br />
cytokines-binding proteins, C 3 and Ca ++ (30).<br />
The molecular adsorbens recycling system (MARS)<br />
eliminates albumin-binding toxins.water soluble toxins, NO,<br />
IFNγ, TNFα, IL-6 and IL-8 in sever liver failure and Multi<br />
Organs Dysfunction Syndrome (MODS) with marked<br />
decrease of sequential organ failure assessment (Sequential<br />
Organ Failure Assessment, SOFA score reduction from 9.7 to<br />
7.0). MARS may increase the serum levels of IL-6 by<br />
unknown mechanism (47).<br />
Limitations of cytokines plasma dosage<br />
The soluble receptors have almost all pro- inflammatory<br />
cytokines (IL-1, IL-2, IL-6, TNFα, IFNγ); that’s the active<br />
interleukins fraction is difficult to know. The cytokines<br />
retention may be due to reduced renal clearance a blood<br />
accumulation. The tissue (namely effective) cytokine<br />
concentration differs from the plasma levels for the same<br />
cytokine and the conclusion about his efficiency following<br />
the blood cytokines presence is inconclusive. Finally, the<br />
cytokines network is interrelated and may compensate for<br />
each other.<br />
References<br />
1. Casey LC, Balk RA, Bone RC. Plasma cytokine and endotoxin<br />
levels correlate with survival in patients with sepsis<br />
syndrome.Ann Intern Med 1993; 119: 771-78<br />
2. Himmelfarb J, Le P, Klenzak J, Freedman S, McMenamin ME,<br />
Ikizler TA. Impaired monocyre cytokine production in<br />
critically ill patients with acute renal failure. Kidney Int 2004;<br />
66(6): 2354-60<br />
3. Iglesias J, Marik PE, Levine JS. Elevated serum levels of type I<br />
and type II receptors for TNFα as predictive factors for acute<br />
renal failure in patients with septic shock. Am J Kidney Dis<br />
2003; 41: 62-75<br />
4. Patel NS, Chatterjee PK, Di Paola R, Mazzon E, Britti D, De<br />
Saro A, Guzzocrea S, Thiemermann.Endogenous IL-6<br />
enhances the renal injury,dysfunction and inflam-mation<br />
caused by ischemia-reperfusion. J Phrarmacol Exp Ther 2005;<br />
312: 1170-78<br />
5. Cunningham PN, Dyanov HM, Park P, Wang J, Newell KA,<br />
Quigg RJ. Acute renal failure in endotoxemia is caused by TNF<br />
acting directly on TNF receptor-1 in kidney. J Immunol 2002;<br />
168: 5817-23<br />
6. Jo SK, Cha DR, Cho WY, Kim HK, Chang KH, Yun SY, Won<br />
NH. Inflammatory cytokines and lipopolysacharide induce fasmediated<br />
apoptosis in renal tubular cells. Nephron 2002; 91(3):<br />
406-15<br />
7. Hoffman JN, Hartl WH, Deppisch R, Faist E, Jochum M,<br />
Inthorn D. Hemofiltration in human sepsis: evidence for<br />
elimination of immunomodulatory substances. Kidney Int<br />
1995; 48(5): 1563-70<br />
8. Kohan DE. Role of endothelin and TNF in the renal response to<br />
sepsis. Nephrol Dial Transplant 1994; 9 Suppl 4: 73-77<br />
9. Chugh KS, Jha V, Sakhuja v, Joshi K. Acute renal cortical<br />
necrosis-a study of 113 patients. Ren Fail 1994; 16: 37-47<br />
10. Rasche FM et al. Thrombocytopenia and acute renal failure in<br />
Puumala Hantaan infections.emerg infect dis 2004; 10(8):<br />
1069-78<br />
11. Floege J, Rees A. Growth factors and cytokines. In<br />
Immunologic Renal Diseases (ed.EG Neilson&WG Couser),<br />
pp. 417-588. Philadelphia PA: Lippincott-Raven, 1997<br />
12. Webb NJ, Brnechley PE. Cytokines and cell adhesion<br />
molecules in the inflammatory response during acute<br />
pyelonephritis. Nephron Experim Nephrol 2004; 96(1): 1-6<br />
13. Maillet PJ, Pelle-Franzos D, Laville M, Gay F, Pinet A. Non<br />
dilated obstructive acute renal failure: diagnostic procedures<br />
and therapeutic management. Radiology 1986; 160: 659-62<br />
14. Kwon O, Molitoris BA, Pescowitz M, Kelly KJ. Urinary actin,<br />
interleukin-6 and interleukin-8,may predict sustained ARF after<br />
ischemic injury in renal allografts. Am J Kidney Dis 2003;<br />
41(5): 1074-87<br />
15. McLaughlin PJ, Aikawa A, Davies HM, Ward RG, Bakran A,<br />
Sells RA, Johnson PM. Uromodulin levels are decreased in<br />
urine during acute tubular necrosis but not during immune<br />
rejection after renal transplantation. Clin Sci 1993; 84(2): 243-<br />
46<br />
16. Simmons EM, Himmelfarb J, Sezer MT, Chertow GM, Mehta<br />
RL, Paganini EP, Soroko S et al. Plasma cytokines levels<br />
predict mortality in patients with acute renal failure. Kidney Int<br />
2004; 65(4): 1357-1365<br />
17. Rodriguez-Iturbe B, Pons H, Herrera-Acosta J, Johnson RJ.<br />
Role of immunocompetent cells in non-immune renal diseases.<br />
Kidney Int 2001; 59: 1626-1640<br />
18. Borazan A, Ustun H, Ustundag J, Aydemir S, Bayraktaroglu T,<br />
Sert M, Yilmaz A. The effects of peritoneal dialysis and<br />
haemodialysis on serum TNFα, IL-6, IL-10 and CRP levels.<br />
Mediators Inflamm 2004; 13(3): 201-204<br />
19. Lim CS et al. Th1/Th2 predominance and proinflammatory<br />
cytokines determine the clinicopathological severity of IgA<br />
nephropathy. Nephrol Dial Transplant 2001; 16: 269-275<br />
20. Albelda SM, Smith CV, Ward PA. Adhesion molecules and<br />
inflammatory injury. FASEB J 1994; 8: 504-512<br />
21. Lauwerys BR, Houssiau FA. Cytokines: clues to the<br />
pathogenesis of SLE. Lupus 1998; 7: 211-213<br />
22. Kym JS et al. Differential expression of various cytokine and<br />
chemokine genes between proliferative and nonproliferativeglomerulonephritides.<br />
Clin Nephrol 2001; 56: 199-<br />
206<br />
23. Schor N. Acute renal failure and sepsis syndrome. Kidney Int<br />
2002; 61: 764-771<br />
24. Opal SM, Cross AS. Clinical trials for severe sepsis: past<br />
failures and future hopes. Infect Dis Clin North Am 1999; 13:<br />
285-297<br />
25. Reinhart K, Karzai W. Anti tumor necrosis factor therapy in<br />
sepsis: Update on clinical trials and lessons learned. Crit Care<br />
Med 2001; 29: Supp 121-125<br />
26. Rogers SA, Miller SB, Hammerman MR. Triiodthyronine<br />
stimulates renal EGF expression in adult rat. Am j Physiol<br />
1995; 268 F 128-F134
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 65<br />
27. Hammerman MR, Miller SB. Therapeutic use of growth factors<br />
in renal failure. J Am Soc Nephrol 1994; 5: 1-11<br />
28. De Sa HM, Freitas La, Alves VC, Garcao MF, Rosa MA,<br />
Marques AA. Leuko-cyte, platelet and endothelial sctivation in<br />
patients with acute renal failure trated by intermittent<br />
haemodialysis. Am J.Nephrol 2001; 21(4): 264-273<br />
29. Grino JM. A plateler activating factor antagonist for preventing<br />
post-transplant renal failure: a double blind randomized study.<br />
Ann Intern Med 1994; 121: 345-347<br />
30. Stegmayr BG, Banga R, Berggren R, Norda R, Rydvall A,<br />
Vikerforst T. Plasma exchange as rescue therapy in multiple<br />
organ failure including acute renal failure. Crit Care Med 2003;<br />
31: 1730-36<br />
31. Niimi R, Nakamura A, Yamagawa Y. Suppression of<br />
endotoxin induced TNFα and IL-6 mRNA by renninangiotensin<br />
system inhibitors. Jpn J Pharmacol 2002; 88: 139-<br />
145<br />
32. Seifert JK, France MP, Zhao J, Bolton EJ, Finlay I, Juninger T,<br />
Marris DL. Large volume hepatic freezing: association with<br />
significant release of the cytokines IL-6 and TNFα in a rat<br />
model. World J Surg 2002; 26(11): 1333-1341<br />
33. Van Why SK, Siegel NJ. Heat shock proteins: role in<br />
prevention and recovery from acute renal failure. In Acute<br />
renal failure: A companion to Brenner&Rectors The Kidney<br />
(ed. BA Molitoris and WF Finn), pp 143-155. Philadelphia:<br />
WB Saunders, 2001<br />
34. Lopez A, Lorente JA, Steingrun GJ et al. Multiple-center,<br />
randomized, placebo-controlled, double blind study of the<br />
nitric oxide synthase inhibitor (546C88) effect on survival in<br />
patients with septic shock. Crit Care Med 2004; 32: 21-30<br />
35. Rahman SN, Kim GE, Mathew AS et al. Effects of atrial<br />
natriuretic peptide in clinical acute renal failure. Kidney Int<br />
1994; 45: 1731-38<br />
36. Kon V, Yoshioka T, Fogo A, Ichikawa I. Glomerular action of<br />
endothelin in vitro, J Clin Invest 1989; 83: 1762-67<br />
37. Chan L, Chittinanandana A, Shapiro JI, Shanley PF, Schrier<br />
RW. Effect of an endothelin receptor antagonist on ischemic<br />
acute renal failure. Am J Physiol 1994; 266: F135-F138<br />
38. Haug CE, Colvin RB, Delmonico El et al. A phase I trial<br />
immunosuppression with anti-ICAM I (CD 54) mAb in renal<br />
allograft recipients. Transplantation 1993; 55: 766-72<br />
39. Goligorsky MS, di Bona GF. Pathogenetic role of Arg-Gly-<br />
Asp-recognizing integrins in acute renal failure. Proc Natl<br />
Acad Sci USA 1993; 90: 5700-5704<br />
40. Schulman G, Fogo A, Gung A, Bodr K, Hakim<br />
RM.Complement activation retards resolution of acute<br />
ischemic renal failure in the rat. Kidney Int 1991; 40: 1069-<br />
1074<br />
41. Schiffl H, Lang SM, Konig A, Strasser T, Haider MC, Held E.<br />
Biocompatible membranes in acute renal failure: prospectivenon<br />
controlled study. Lancet 1994; 344: 570-72<br />
42. Burney-Taney MJ, Kofler J, Yokota N, Weisfeldt M,<br />
Traystman RJ, Ralb H. Acute renal failure after whole body<br />
ischemia is characterized by inflammation and T-cell-mediated<br />
injury. Am J Physiol Renal Physiol 2003; 285 (1): F 87-94<br />
43. Zwolinska D, Medynska A, Szprynger K, Szczepanska M.<br />
Serum concentration of IL-2, IL-6, TNFα and their soluble<br />
receptors in children on maintenance haemodialysis. Nephron<br />
2000; 86(1): 441-46<br />
44. Klouche K, Cavadere P, Portales P, Clot J, Canaud B, Beraud<br />
JJ. Continuous VVHF improves hemodinamics in septic shock<br />
with acute renal failure without modifying TNFα and IL-6<br />
plasma concentration. J Nephrol 2002; 15(2): 150-57<br />
45. Morgera S, Klonower D, Rocktaschel J, Haase M, Priem F,<br />
Ziemer S et al. TNFα elimination with high cut-off<br />
hemofilters: a feasible clinical modality for septic patients?<br />
Nephrol Dial Transplant 2003; 18(7): 1361-69<br />
46. Bellomo R, Tipping P, Boyce N. Interleukine-6 and<br />
interleukine-8 extraction during CVVHF in septic acute renal<br />
failure. Ren Fail 1995; 17: 457-66<br />
47. Dagher L, Moore K. The hepatorenal syndrome. Gut 2001; 49:<br />
729-737
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 66<br />
Amyloidosis<br />
M. Tunca<br />
Dokuz Eylül University School of Medicine, Department of Internal Medicine, Izmir, Turkey<br />
Abstract<br />
Amyloidosis is a group of diseases due to pathologic<br />
deposition of various insoluble fibrilllar proteins having an<br />
identical secondary structure (ß-pleated sheet) in the<br />
extracellular compartments of the body. When diabetes<br />
mellitus type II and Alzheimer’s disease are taken into<br />
account, the prevalence of amyloidosis is obviously quite<br />
high. There are four types of amyloidosis: AL (light chain)<br />
amyloidosis, AA amyloidosis (secondary to chronic<br />
inflammation), Aß 2 M amyloidosis (secondary to long-term<br />
hemodialysis) and heredofamilial (ATTR and other)<br />
amyloidoses. The process may be focal, local or generalized<br />
whose clinical consequences are reflections of the involved<br />
organ(s). Some clinical features such as macroglossia (AL),<br />
nephrotic syndrome (AA), arthropathy (Aß 2 M ) or familial<br />
peripheral neuropathy (ATTR) may imply the type of deposit<br />
to a certain extend. A definitive diagnosis requires not only<br />
tissue confirmation (Congo Red staining with green<br />
birefringence under polarized light) but also genomic DNA<br />
and protein analyses and immunohistochemistry. Suitable<br />
tissue samples can be obtained from subcutaneous fat pad<br />
aspiration, rectal mucosa or renal biopsy. Neural or<br />
myocardial biopsies are rarely necessary. Serum amyloid P<br />
component (SAP) scintigraphy can visualise and demonstrate<br />
the amyolid burden of the patient; this procedure may also be<br />
useful to measure the response to treatment.<br />
Amyloidosis is not regarded as an irreversible pathology<br />
anymore. Detection of the precursor protein such as SAA or<br />
mutated transthyretin is an important step in therapeutic<br />
decision making since further progression of the deposits can<br />
thus be halted. There are several treatment options available<br />
to the clinicians, while the efficacy of some of these<br />
modalities has not yet been definitely established.<br />
Keywords: amyloidosis, pathogenesis, treatment, familial<br />
mediterranean fever<br />
Introduction<br />
Amyloidosis is a heterogeneous group of diseases.<br />
Misfolding and deposition of certain soluble proteins as<br />
insoluble fibrils in the extracellular compartments of the body<br />
cause variety of organ dysfunctions. They have an identical<br />
secondary structure (ß-pleated sheet) but there are 21<br />
different proteins causing amyloidosis. The majority of<br />
amyloid cases are due to acquired pathologic processes but a<br />
substantial minority is hereditary.<br />
Historically, the term “amyloid” (starch-like) was first used<br />
by Schleiden, a German botanist, in 1838. Virchow<br />
introduced it to medical jargon in 1858 for the autopsy<br />
findings which were later demonstrated that they had nothing<br />
to do with starch but were proteinaceous in nature. Congo<br />
Red staining was first used by Divry in 1927 and the<br />
ultrastructure of amyloid fibrils was identified by Cohen and<br />
Calkins in 1959 (1).<br />
Types of amyloidosis and their prevalence<br />
Amyloidosis may be localized or systemic. There are four<br />
types of systemic amyloidosis:<br />
1. AL amyloidosis is due to plasma cell dyscrasia<br />
related to multiple myeloma where the precursor<br />
protein is either or immunoglobulin.<br />
2. AA amyloidosis is secondary to chronic<br />
inflammation and the precursor protein is serum<br />
amyloid A protein.<br />
3. Aß 2 M amyloidosis is secondary to long-term<br />
hemodialysis and the precursor protein is ß 2<br />
microglobulin.<br />
4. ATTR and other heredofamilial amyloidoses where<br />
the precursor protein is usually abnormal<br />
transthyretin (previously called prealbumin). The<br />
precursor of other rarer forms may be apolipoprotein<br />
A-I, lysozyme, or fibrinogen A -chain.<br />
It is estimated that amyloidosis is the cause of death of about<br />
6,6/10,000 people in the United Kingdom annually (2) and<br />
age-adjusted incidence of AL amyloidosis is around 8 per<br />
million person-years in USA where the ratio of ATTR<br />
amyloidosis rate is 10-20 percent of AL cases (3). AA type is<br />
relatively more prevalent in under-developed countries since<br />
untreated chronic infections such as tuberculosis are still not<br />
exceptional; other chronic inflammatory diseases<br />
(rheumatoid arthritis etc) are outstanding sources of new<br />
cases universally. Familial Mediterranean fever (FMF) needs<br />
mentioning since it is quite prevalent in Turkey (0,1 percent)<br />
and in Greece and may be encountered in other Balkan<br />
countries to a certain extend. Migration of populations from<br />
the Middle East in the twentieth century has transformed<br />
FMF into a universal disease. It was recently observed that<br />
about 13 percent of nearly 3000 FMF patients had AA<br />
amyloidosis in Turkey and it is the most frequent cause of<br />
amyloidosis in that country (4, 5). Aß 2 M amyloidosis is<br />
potentially important source because there are approximately<br />
1 million people on dialysis programs worldwide and the<br />
development of amyloidosis approaches to 100 percent after<br />
20 years (6).<br />
______________________<br />
Correspodence to: M. Tunca, Dokuz Eylül University School of Medicine, Department of Internal Medicine,<br />
Balcova, 35350 Izmir Turkey; E-mail: mehmet.tunca@deu.edu.tr
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 67<br />
When diabetes mellitus type II and Alzheimer’s disease are<br />
taken into account, the prevalence of amyloidosis is<br />
obviously quite high. Amyloidosis is not systemic but<br />
localized to pancreatic islet cells and cerebrum in these<br />
diseases and their pathogenetic implications are not well<br />
established.<br />
Pathogenesis<br />
The newly synthesized polypeptides enter a funnel-like<br />
pathway of conformational modification in the cytoplasm<br />
under physiological conditions. Some polypeptides may<br />
however misfold and aggregate as insoluble fibrils, which is a<br />
pathologic process leading to amyloidosis. The first step in<br />
amyloidogenesis is the change in the precursor protein that<br />
starts the process of fibrillar autoaggregation. Production of<br />
the precursor protein is quantitatively and/or qualitatively<br />
pathologic. There are specific amino acid substitutions in the<br />
precursor light chain in AL amyloidosis or transthyretin in<br />
ATTR and it is thought that such changes destabilize the<br />
molecule and facilitate fibrillogenesis. A third mechanism is<br />
proteolytic remodelling of the precursor protein.<br />
Since not every person with the same mutation develops<br />
amyloidosis and there is a very wide time range in AA<br />
amyloidosis, other genetic and macro and<br />
microenvironmental factors may be operational. Certain<br />
genotypes such as being M694V homozygote and SAA1<br />
alpha/alpha and a positive family history for amyloidosis<br />
have significantly higher risk of amyloidosis in FMF (7). The<br />
concentration of urea in the inner renal medulla or the pH<br />
level of the tissues may enhance fibrillogenesis. It is also well<br />
recognized that once amyloid deposition starts, progression is<br />
easier (“amyloid begets amyloid”). This may explain the<br />
concentration of amyloid in certain organs but the tissue<br />
specificity of each protein (joints, peripheral nerves etc.) is<br />
not well understood (1, 3, 8).<br />
Diagnosis<br />
Every patient must be evaluated for extend of organ<br />
involvement and family history and the type of precursor<br />
protein must be determined. A definitive diagnosis requires<br />
not only tissue confirmation (Congo Red staining with green<br />
birefringence under polarized light) but also genomic DNA<br />
and protein analyses and immunohistochemistry, otherwise<br />
some hereditary forms may be misdiagnosed as AL type (2,<br />
9). Suitable tissue samples can be obtained from<br />
subcutaneous fat pad aspiration, rectal mucosa or renal<br />
biopsy. Neural biopsy is not very reliable because of the focal<br />
distribution of amyloid. Myocardial biopsy is rarely<br />
necessary. Serum amyloid P component (SAP) scintigraphy<br />
can visualise and demonstrate the amyolid burden of the<br />
patient; this procedure may also be useful to diagnose subclinical<br />
disease in progress or measure the response to<br />
treatment (1, 10).<br />
Clinical aspects<br />
Some clinical features such as macroglossia (AL), nephrotic<br />
syndrome (AA), arthropathy (Aß 2 M) or familial peripheral<br />
neuropathy (ATTR) may imply the type of deposit to a<br />
certain extend but the clinical picture is rarely conclusive.<br />
AL type is the most diverse in clinical picture but the central<br />
nervous system is spared. Kidney and heart are frequently<br />
involved and the absence of hypertension despite severe renal<br />
failure should alert the physician. Heart failure is particularly<br />
an ominous sign. Easy bruising and spontaneous periorbital<br />
purpura (“racoon eyes”), hard hepatomegaly with elevated<br />
alkaline phosphatase and macroglossia (about 20 percent of<br />
the patients) are prominent features (3).<br />
AA amyloidosis almost always presents with proteinuria<br />
which may be intermittent initially. Other organ<br />
involvements such as hepatomegaly, splenomegaly,<br />
malabsorption, thyroid or heart failure are exceptional<br />
features of the average patient.<br />
Aß 2 M amyloidosis is always secondary to prolonged dialysis<br />
and the commonest complaint is severe joint pain in the<br />
absence of radiological changes of arthritis, the shoulders<br />
usually being the most affected. Carpal tunnel syndrome<br />
(usually bilateral) is also frequently encountered (5).<br />
Heredeofamilial amyloidosis is probably more frequent than<br />
perceived (2). Peripheral and autonomous nervous system<br />
involvements are outstanding features while renal failure is<br />
rare and macroglossia has not been reported. The most<br />
frequent mutation of ATTR causes cardiac conduction<br />
disturbances while other mutations may cause cardiac failure<br />
indistinguishable from AL type. Generally heart failure is<br />
less common and more benign in ATTR type (3).<br />
Treatment<br />
Amyloidosis is not regarded as an irreversible pathology<br />
anymore. Detection of the precursor protein such as SAA or<br />
mutated transthyretin is an important step in therapeutic<br />
decision making since further progression of the deposits can<br />
thus be halted. Another main objective is to support the<br />
failing organ while transplantation may be the definitive<br />
therapy (11, 12).<br />
AL amyloidosis may respond to oral melphalan and<br />
prednisone but high dose IV melphalan with autologous stem<br />
cell transplantation is more effective. The trials with IDOX<br />
(4’-iodo-4’-deoxydoxorubicin) have been disappointing.<br />
AA amyloidosis can respond favourably to specific treatment<br />
of the primary disease. SAA determinations with aim of<br />
values lower than 10 mg/L would be appropriate. It has been<br />
shown that colchicine can slow the progression of<br />
amyloidosis and regress the proteinuria in FMF (13, 14),<br />
where drug dosage must be escalated to tolerated maximum<br />
which is usually 2-2.5 mg/day. Patients with amyloidosis<br />
secondary to inflammatory arthritides may respond to anti-<br />
TNF treatment (infliximab or etanercept) particularly when<br />
combined with methotrexate (15). CPHPC is a promising<br />
drug which removes SAP from the circulation and amyloid<br />
deposits (9, 11). Sodium-I,3-propane-disulfonate (Fibrillex)<br />
is an investigational drug whose phase II/III results will soon<br />
be available.<br />
Liver transplantation is the definitive therapy of ATTR<br />
amyloidosis. If the liver of the affected patient is transplanted<br />
to another patient (so-called “domino liver transplantation”)<br />
systemic ATTR amyloidosis may sometimes develop in the<br />
recipient. Renal transplantation is the only effective treatment<br />
of Aß 2 M amyloidosis.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 68<br />
References<br />
1. Hawkins PN. The diagnosis, natural history and treatment of<br />
amyloidosis. The Goulstonian Lecture 1995. J R Coll<br />
Physicians Lond 1997; 31: 552-560<br />
2. Lachmann HJ, Booth DR, Booth SE, Bybee A, Gilbertson JA,<br />
Gillmore JD, Pepys MB, Hawkins PN. Misdiagnosis of<br />
hereditary amyloidosis as AL (primary) amyloidosis. N Engl J<br />
Med 2002; 346: 1786-1791<br />
3. Falk RH, Comenzo RL, Skinner M. Medical Progress: The<br />
Systemic Amyloidoses. N Engl J Med 1997; 337: 898-909<br />
4. Turkish FMF Study Group. Familial Mediterranean fever<br />
(FMF) in Turkey: results of a nationwide multicenter study.<br />
Medicine (Baltimore) 2005; 84: 1-11<br />
5. Tuglular S, Yalcinkaya F, Paydas S, et al. A retrospective<br />
analysis for aetiology and clinical findings of 287 secondary<br />
amyloidosis cases in Turkey. Nephrol Dial Transplant 2002;<br />
17: 2003-2005<br />
6. Kurer MH, Baillod RA, Madgwick JC. Musculoskeletal<br />
manifestations of amyloidosis. A review of 83 patients on<br />
haemodialysis for at least 10 years. J Bone Joint Surg Br 1991;<br />
73: 271-276<br />
7. Delibas A, Oner A, Balci B, et al. Genetic risk factors of<br />
amyloidogenesis in familial Mediterranean fever. Am J Nephrol<br />
2005; 25: 434-440<br />
8. Merlini G, Bellotti V. Mechanisms of disease: Molecular<br />
mechanisms of amyloidosis. N Engl J Med 2003; 349: 583-596<br />
9. Hazenberg BP, van Gameren II, Bijzet J, Jager PL, van<br />
Rijswijk MH. Diagnostic and therapeutic approach of systemic<br />
amyloidosis. Neth J Med 2004; 62: 121-128<br />
10. Hawkins PN, Aprile C, Capri G, Vigano L, Munzone E, Gianni<br />
L, Pepys MB, Merlini G. Scintigraphic imaging and turnover<br />
studies with iodine-131 labelled serum amyloid P component in<br />
systemic amyloidosis. Eur J Nucl Med 1998; 25: 701-708<br />
11. Hirschfield GM, Hawkins PN. Amyloidosis: new strategies for<br />
treatment. Int J Biochem Cell Biol 2003; 35: 1608-1613<br />
12. Grateau G, Jeru I, Rouaghe S, et al. Amyloidosis and autoinflammatory<br />
syndromes. Curr Drug Targets Inflamm Allergy<br />
2005; 4: 57-65<br />
13. Oner A, Erdogan O, Demircin G, Bulbul M, Memis L. Efficacy<br />
of colchicine therapy in amyloid nephropathy of familial<br />
Mediterranean fever. Pediatr Nephrol 2003; 18: 521-526<br />
14. Livneh A, Zemer D, Langevitz P, Laor A, Sohar E, Pras M.<br />
Colchicine treatment of AA amyloidosis of familial<br />
Mediterranean fever. An analysis of factors affecting outcome.<br />
Arthritis Rheum 1994; 37: 1804-1811<br />
15. Gottenberg JE, Merle-Vincent F, Bentaberry F, et al. Antitumor<br />
necrosis factor alpha therapy in fifteen patients with AA<br />
amyloidosis secondary to inflammatory arthritides: a followup<br />
report of tolerability and efficacy. Arthritis Rheum 2003; 48:<br />
2019-2024
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 69<br />
Oxidative stress evaluation in uraemic patients undergoing continuous<br />
ambulatory peritoneal dialysis<br />
G. Mircescu 1 , C. Capusa 1 , I. Stoian 2 , D. Lixandru 2 , E. Rus 3 , L. Coltan 2 and L. Gaman 2<br />
1 “Dr Carol Davila” University Hospital of Nephrology, Bucharest, Romania<br />
2 Biochemistry Dept. “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania<br />
3 NephroCare “Dr Carol Davila” Dialysis Centre, Bucharest, Romania<br />
Abstract<br />
Since the great bulk of evidences regarding oxidative stress<br />
associated with chronic renal failure (CRF) came from<br />
haemodialysis patients and only scant data is available<br />
concerning peritoneal dialysis, we investigated the oxidative<br />
status in CRF patients on continuous ambulatory peritoneal<br />
dialysis (CAPD).<br />
Plasma lipid peroxidation assayed as thiobarbituric acid<br />
reactive substances (TBARS; nmol/g protein), plasma total<br />
free thiols (Pt-SH; mcmol/g protein) as marker of<br />
extracellular antioxidant status and parameters of<br />
enzymatic/non-enzymatic intracellular antioxidant defence<br />
(erythrocyte superoxide dismutase (SOD; U/g haemoglobin),<br />
glutathione peroxidase (EGPx; U/g haemoglobin) and nonprotein<br />
thiols (E-SH; mcmol/g haemoglobin)] were measured<br />
by spectrophotometry in 18 CAPD patients, 16 non-dialysed<br />
CRF patients and 12 healthy subjects.<br />
Increased TBARS were found only in CAPD patients versus<br />
Controls (58.3±19.8 vs. 42.7±12.4, p= 0.01). Also, they had<br />
lower activity of erythrocyte SOD (164.2±47.5 vs.<br />
463.2±77.5 in CRF group, p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 70<br />
median volume of ultrafiltration per day was 1000mL<br />
(between 300-1800mL).<br />
Sixteen age- and gender-matched non-dialysed CRF patients<br />
(mean serum creatinine 4.5±2.7mg/dL) were randomly<br />
selected from those attending the Nephrology Clinic for<br />
routine periodical examination over a period of six months<br />
and composed the control patients group. They were not<br />
considered candidates for RRT in the near future.<br />
The CRF groups had a similar distribution according to<br />
primary renal disease, with primary chronic<br />
glomerulonephritis being the main cause of CRF (Table I).<br />
There were no patients with diabetic nephropathy.<br />
Exclusion criteria for the patients were inflammatory and<br />
infectious disorders (including exit or tunnel infections and/or<br />
peritonitis two months before enrolment), malignancies,<br />
diabetes mellitus, active liver diseases, severe anaemia, and<br />
medications with antioxidative potentialities (vitamin C or E,<br />
folic acid, allopurinolum). None of the patients required<br />
blood transfusions in the preceding two months.<br />
Normal control group consisted of twelve matched healthy<br />
volunteers with normal routine biochemistry and urine<br />
analyses. They did not take any medication or nutritive<br />
supplements.<br />
An informed consent was obtained from all participants.<br />
Methods<br />
Blood samples were drawn after overnight fasting into<br />
standard vacuum tubes with lithium heparin, were transported<br />
on ice, in the dark, and were processed within 30 minutes of<br />
collection by centrifugation (3000 g for 10 minutes at room<br />
temperature).<br />
The plasma aliquots were stored at -70°C until analysed for<br />
oxidative stress determinations or used immediately for<br />
routine laboratory parameters. Erythrocytes were washed<br />
three times with isotonic saline solution and lysed in cold<br />
ultrapure water. The red cell stroma was removed by<br />
centrifugation (10000 g for 15 minutes at 4°C) and the clear<br />
supernatant was stored at -70°C until erythrocytes antioxidant<br />
parameters were assayed. Reagents and ultra pure water were<br />
treated with Chelex 100 in order to bind transitional metals.<br />
Usual biochemistry parameters, C-reactive protein included,<br />
were determined by means of routine automated procedures<br />
on multiparameter analyser and haemoglobin concentrations<br />
were measured by automated spectrophotometric method.<br />
All the oxidative stress parameters were determined by<br />
spectrophotometry and the measurements were carried out on<br />
triplicate samples.<br />
Plasma thiobarbituric acid reactive substances (TBARS),<br />
measured according to the method described by Esterbauer<br />
(4), were used to assess plasma lipid peroxidation. Plasma<br />
aliquots were treated with butylated hydroxytoluene in order<br />
to prevent artifactual oxidation during the assay procedure<br />
and mixed with 0.67% thiobarbituric acid (TBA) and 20%<br />
trichloroacetic acid. Blank samples from distilled water and<br />
the same reagents were prepared. The reaction mixture was<br />
heated at 100°C for one hour and then cooled with tap water.<br />
The pink TBA-reacting substances adduct was extracted in n-<br />
butanol and the absorbance of the organic layer was read at<br />
532nm, after centrifugation. The concentration of lipid<br />
peroxidation products was calculated as malondialdehyde<br />
(MDA) equivalents using the extinction coefficient for the<br />
MDA-TBA complex of 153000 M -1 cm -1 and expressed as<br />
nmol/g protein.<br />
Plasma total free thiols (Pt-SH) assayed by the Ellman’s<br />
method (5), served as marker of extracellular antioxidant<br />
status. Briefly, aliquots of plasma were mixed with 5mM<br />
phosphate buffer (pH=8) and 10% sodium dodecil sulphate.<br />
Then Ellman’s reagent was added and samples were<br />
incubated at 37˚C for one hour. The absorbance was read at<br />
412nm against a reagent blank. Results were calculated using<br />
a calibration curve with glutathione as standard, and<br />
expressed as mcmol/g protein.<br />
Erythrocyte superoxide dismutase activity (SOD) was<br />
assessed by analysing the rate of inhibition of pyrogallol<br />
auto-oxidation, according to Marklund and Marklund (6).<br />
The erythrocyte lysate was treated with a mixture of<br />
ethanol/chloroform and was centrifuged for 20 minutes at<br />
6000 g. The supernatant fluid was mixed with 0.2mM<br />
pyrogallol and TRIS buffer (pH = 8.2), in the presence of<br />
oxygen. The rate of change in the absorbance at 420nm was<br />
monitored for 3 minutes against the blank sample. SOD<br />
activity was expressed as U/g haemoglobin.<br />
Erythrocyte glutathione peroxidase activity (EGPx) was<br />
determined indirectly by measuring the rate of consumption<br />
of NADPH during the regeneration of reduced glutathione<br />
from the oxidised glutathione produced by EGPx in the<br />
presence of oxidising substrate (7). The erythrocyte lysate<br />
was mixed with TRIS buffer and the enzymatic reaction was<br />
initiated by adding 1mM tert-butyl hydroperoxide. The<br />
conversion of NADPH to NADPH + was followed by<br />
recording the decrease in the absorbance at 340nm for 3<br />
minutes. The enzyme activity was calculated using the molar<br />
extinction coefficient for NADPH of 6220 M -1 cm -1 and was<br />
expressed as U/g haemoglobin.<br />
Erythrocyte non-protein thiols (E-SH), which consist mainly<br />
of reduced glutathione (GSH), were measured according to<br />
the method of Beutler et al (8). The erythrocyte lysate was<br />
mixed with a protein precipitating solution (1.67 g<br />
metaphosphoric acid, 0.2 g disodium ethylenediaminetetraacetic<br />
acid and 30 g sodium chloride in 100 ml distilled<br />
water). After 5 minutes, the mixture was filtered and 0.3M<br />
sodium phosphate and Ellman’s reagent were added. The<br />
absorbance was read at 412nm against a reagent blank. The<br />
results were calculated using the molar extinction coefficient<br />
for GSH of 13600 M -1 cm -1 and were expressed as mcmol/g<br />
haemoglobin.<br />
Statistical analysis<br />
Results were expressed as mean ± standard deviation and<br />
were compared using Student’s t test or ANOVA (for<br />
normally distributed variables). Median and interquartile<br />
range wase used to express the non-parametric variables.<br />
Standard regression analysis and Pearson r correlation<br />
coefficient were used to evaluate the relationship between<br />
pairs of variables.<br />
A p value < 0.05 was considered significant.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 71<br />
Results<br />
Table 1. Main characteristics of the subjects<br />
Parameter CAPD Group CRF non-D group Controls<br />
Number 18 16 12<br />
Main causes of CRF:<br />
primary chronic<br />
glomerulonephritis (%)<br />
44 38 -<br />
tubulo-interstitial nephritis (%) 28 25 -<br />
vascular nephropathies (%) 22 25 -<br />
polycystic kidney disease (%) 0 12 -<br />
other (%) 6 0 -<br />
Mean age (years) 55.6±16.9 55±15.7 45.5±12.1<br />
Gender ratio (M/F) 8/10 10/6 5/7<br />
Smokers in (%)] 3 (16.7) 3 (18.8) 1 (8.3)<br />
Body mass index (kg/m 2 )<br />
‡ 26.2±3.7<br />
† 22.8±3.1 25.6±3.0<br />
Serum iron (mcg/dL) 58.6±28.4 54.8±24.7 73.1±24.7<br />
Serum cholesterol (mg/dL) 225.8±57.0 191.9±55.8 229.5±48.1<br />
Serum albumin (g/dL)<br />
† 3.7±0.4<br />
† 3.9±0.6 4.6±0.3<br />
Haemoglobin (g/dL)<br />
† 9.7±2.3<br />
† 9.6±2.3 14.1±1.3<br />
Serum creatinine (mg/dL)<br />
†‡ 9.4±2.9<br />
† 4.5±2.7 0.9±0.1<br />
Serum uric acid (mg/dL)<br />
† 6.1±0.8<br />
† 6.8±1.5 4.7±1.5<br />
p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 72<br />
renal replacement therapy, but more probably it is related to<br />
the low sensibility and specificity of the used assay.<br />
Alternatively, the serum levels of TBARS might be kept in<br />
the normal range by some protective mechanisms like hepatic<br />
microsomes that are capable of both TBARS generation and<br />
degradation, as supported by the study of Gotoh et al (12).<br />
Previously, Malgorzewicz et al also discovered higher plasma<br />
content of MDA in peritoneal dialysis compared to healthy<br />
group, especially in severely malnourished patients and<br />
supposed that the increase in oxidative stress may be related<br />
to a degree of malnutrition (13). Our findings support the<br />
presence of oxidative stress in uraemic patients on CAPD<br />
with no apparent deficiency of the nutritional status, at least<br />
as reflected by the BMI and serum cholesterol (that did not<br />
differ from Controls), or serum albumin (that was similar to<br />
CRF group). Furthermore, the CRF group who had lower<br />
BMI and serum albumin than normal controls showed no<br />
differences in TBARS levels compared to healthy subjects.<br />
However, the present study does not provide enough data to<br />
sustain or deny the role of malnutrition in augmenting<br />
oxidative stress because the evaluation of nutritional status<br />
was not a primary objective and its casual assessment relied<br />
on few, unspecific parameters.<br />
Indirect evidences of oxidative stress can also be obtained<br />
from the investigation of antioxidant parameters. The<br />
decrease of plasma total free thiols levels observed in all<br />
studied CRF patients compared to healthy individuals, which<br />
reflects a deficiency of the extracellular antioxidant defence,<br />
could be speculated in favour of an increased consumption<br />
for counteracting the potential oxidative burden associated<br />
with chronic renal failure. The presumable contribution of<br />
hypoalbuminaemia to the lower plasma thiols appears<br />
implausible in our patients since no significant correlation<br />
was found between serum albumin and Pt-SH in either CRF<br />
groups (r = 0.27, confidence interval 95% = -0.3 ÷ +0.7; p =<br />
0.4 in CRF non-dialysed group, and r = -0.13, confidence<br />
interval 95% = -0.47 ÷ +0.32; p = 0.5 in CAPD group,<br />
respectively). Therefore, we interpreted the reduced plasma<br />
thiols as an indirect proof of augmented oxidative stress in<br />
CRF patients, dialysed or not. Similar results have been<br />
reported by Tarng et al, who demonstrated the decrease of the<br />
whole-blood reduced glutathione as well as of the plasma<br />
ascorbate and alfa-tocopherol in chronic peritoneal dialysis<br />
patients and in non-dialysed patients with advanced renal<br />
failure (mean creatinine clearance 11.8±4.6mL/min) (3).<br />
The deficiency of antioxidant systems in peritoneal dialysis<br />
patients is further sustained in our results by the marked<br />
decline of erythrocyte SOD activity. Therefore, one can<br />
assume that both extracellular and enzymatic intracellular<br />
defence against oxidative stress are defective in uraemic<br />
patients undergoing CAPD. These findings are in agreement<br />
with some other studies that reported reduced enzymatic<br />
erythrocyte defence (superoxide dismutase and catalase) in<br />
CAPD group (14,15), although discrepant results were also<br />
obtained. For example, Bonnefont-Rousselot et al did not<br />
detect any abnormalities in erythrocyte SOD activity in<br />
CAPD-treated patients in comparison with age-matched<br />
control group (16). However, they included older subjects<br />
than ours and this might allow to speculate the lack of<br />
difference on the account of advanced age, which impairs the<br />
antioxidant systems by itself and, possible, uraemia or<br />
dialysis procedure were not able to add further deterioration<br />
in this distinctive age group.<br />
Concerning the other two studied erythrocyte antioxidant<br />
parameters, contrary to previous published data that<br />
described unchanged EGPx and reduced erythrocyte<br />
glutathione (11), significantly higher values were noticed in<br />
both CRF groups. We hypothesised that an enzymatic<br />
induction occurs in response to oxidative stress and accounts<br />
for the increased EGPx activity and the regeneration of the<br />
intracellular pool of reduced glutathione (GSH). Indeed, the<br />
ability of glutathione peroxidase to adapt its activity<br />
according to oxidative stress was demonstrated in chronic<br />
haemodialysis children (17) and was supposed by Canestrari<br />
et al in order to explain the increased EGPx found in CAPD<br />
subjects (cited by (16)). Also, it was stated that the oxidantsinduced<br />
up-regulation of glucose-6-phosphate dehydrogenase<br />
(G6PD) might play a role in the increase of intracellular<br />
GSH. In experimental setting, on culture of human cells, the<br />
authors showed that G6PD expression is rapidly enhanced in<br />
response to oxidative stress and it controls intracellular<br />
reduced glutathione without interfering with the activity of<br />
the other enzymes involved in the peroxide/hydroperoxidedetoxifying<br />
pathway (18). As a result, cells overexpressing<br />
G6PD had an overall reduced state, although the precise<br />
biochemical mechanism underlying the enzyme’s antioxidant<br />
properties is still debated. Until now, two alternative<br />
explanations were proposed: either G6PD influences the<br />
output of GSH and thus contribute to the maintaining of an<br />
intracellular redox potential, or it is implicated in a<br />
mechanism that promotes glutathione storage (18). Anyway,<br />
these experimental inferences support our interpretation of<br />
the increased EGPx and E-SH in uraemic patients as an<br />
adaptive reaction to enhanced oxidative stress.<br />
Conclusions<br />
We concluded that peritoneal dialysis patients are exposed to<br />
oxidative stress, evidenced by both an increase in plasma<br />
lipid peroxidation (TBARS) and a suppressed activity of<br />
antioxidants (erythrocyte SOD). Also, the impairment of<br />
extracellular antioxidant system expressed by the lower levels<br />
of plasma free thiols, probably accounted for by the enhanced<br />
consumption in order to offset the oxidative burden, plead for<br />
an imbalance between reactive species production and<br />
antioxidant defence mechanisms in CAPD patients. The<br />
enhancement of erythrocyte glutathione-dependent<br />
antioxidants might reflect rather an adaptive response to<br />
oxidative processes and, therefore, indirectly argues in favour<br />
of oxidative stress occurring before initiation of dialysis and<br />
augmented thereafter.<br />
References<br />
1. Ward RA, McLeish KR. Oxidant stress in hemodialysis<br />
patients: What are the determining factors? Artif Organs 2003;<br />
27(3): 230-236<br />
2. Agalou S, Ahmed N, Dawnay A, Thornalley PJ. Removal of<br />
advanced glycation end products in clinical renal failure by<br />
peritoneal dialysis and haemodialysis. Biochem Soc<br />
Transactions 2003; 31(6): 1394-1396<br />
3. Tarng DC, Chen TW, Huang T-P et al. Increased oxidative<br />
damage to peripheral blood leukocyte DNA in chronic<br />
peritoneal dialysis patients. J Am Soc Nephrol 2002; 13: 1321-<br />
1330<br />
4. Esterbauer H, Cheeseman KH. Determination of aldehydic<br />
lipid peroxidation products: malonaldehyde and 4-<br />
hydroxynonenal. Methods Enzymol 1990; 186: 407-421
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 73<br />
5. Rice-Evans CA, Diplock AT, Symons MCR. Techniques In<br />
Free Radicals Research. Elsevier, Amsterdam 1991; 207-234<br />
6. Marklund S, Marklund G. Involvement of the superoxide anion<br />
radical in the autoxidation of pyrogallol and a convenient assay<br />
for superoxide dismutase. Eur J Biochem 1974; 47(3): 469-474<br />
7. Ursini F, Maiorino M, Brigelius-Flohe R et al. Diversity of<br />
glutathione peroxidases. Methods Enzymol 1995; 252: 38-53<br />
8. Beutler E, Duron O, Kelly BM. Improved method for the<br />
determination of blood glutathione. J Lab Clin Med 1963; 61:<br />
882-888<br />
9. Himmelfarb J, Hakim RM. Oxidative stress in uraemia. Curr<br />
Opin Nephrol Hypertens 2003; 12(6): 593-598<br />
10. Kim SB, Yang WS, Min WK, Lee SK, Park JS. Reduced<br />
oxidative stress in hypoalbuminemic CAPD patients. Perit Dial<br />
Int 2000; 20(3): 290-294<br />
11. Ozden M, Maral H, Akaydin D et al. Erythrocyte glutathione<br />
peroxidase activity, plasma malondialdehyde and erythrocyte<br />
glutathione levels in hemodialysis and CAPD patients. Clin<br />
Biochem 2002; 35(4): 269-273<br />
12. Gotoh M, Nagase S, Aoyagi K et al. Thiobarbituric acid<br />
reactive substances are increased in the subcutaneous fat tissue<br />
of patients with end-stage renal disease. Nephrol Dial<br />
Transplant 1997; 12: 713-717<br />
13. Malgorzewicz S, Lichodziejewska-Niemierko M, Rutkowski B,<br />
Lysiak-Szydlowska W. Nutritional status and oxidative<br />
processes in diabetic and nondiabetic peritoneal dialysis<br />
patients. J Renal Nutr 2004; 14(4): 242-247<br />
14. Durak I, Akyol O, Baeme E, Canbolat O, Kavatcu M.<br />
Reduced erythrocyte defense mechanisms against free radical<br />
toxicity in patients with chronic renal failure. Nephron 1994;<br />
66: 76-80<br />
15. Taylor JE, Scott N, Bridges A, Henderson IS, Stewart WK,<br />
Belch JJF. Lipid peroxidation and antioxidants in continuous<br />
ambulatory dialysis patients. Perit Dial Int 1992; 12: 252-256<br />
(medline)<br />
16. Bonnefont-Rousselot D, Jaudon MC, Issad B et al. Antioxidant<br />
status of elderly chronic renal patients treated by continuous<br />
ambulatory peritoneal dialysis. Nephrol Dial Transplant 1997;<br />
12: 1399-1405<br />
17. Sommerburg O, Grune T, Ehrich JHH, Siems WG. Adaptation<br />
of glutathione-peroxidase activity to oxidative stress occurs in<br />
children but not in adult patients with end-stage renal failure<br />
undergoing hemodialysis. Clin Nephrol 2002; 58(suppl 1):<br />
S31-S36<br />
18. Salvemini F, Franze A, Iervolino A et al. Enhanced glutathione<br />
levels and oxidoresistance mediated by increased glucose-6-<br />
phosphate dehydrogenase expression. J Biol Chem 1999;<br />
274(5): 2750-2757
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 74<br />
Hyperhomocysteinemia in ESRD<br />
A. F. Perna 1 , C. Lombardi 1 , R. Capasso 1 , F. Acanfora 1 , E. Satta 1 , D. Ingrosso 2 , M. G. Luciano 1<br />
and N. G. De Santo 1<br />
1 First Division of Nephrology/Department of Pediatrics, 2 Department of Biochemistry and Biophysics “F. Cedrangolo”,<br />
Cardiovascular Research Center, School of Medicine, Second University of Naples, Naples, Italy<br />
Abstract<br />
In chronic renal failure and in uremia, the role of uremic<br />
toxins and in particular of protein-bound molecules, such as<br />
AGEs, phenols, and homocysteine, is attracting much<br />
attention from scientists interested in understanding the<br />
mechanisms leading to the dramatic increase in<br />
cardiovascular risk and mortality typical of the condition.<br />
Homocysteine is a cardiovascular risk factor in the general<br />
population and in uremia. It displays several effects at the<br />
genomic level and on protein function, and it represents an<br />
interesting candidate in the study of the pathogenesis of the<br />
cardiovascular disease specific of uremia. Several aspects of<br />
hyperhomocysteinemia, such as clinical epidemiology,<br />
therapeutic aspects, and malnutrition, will be discussed.<br />
Key words: homocysteine, folate receptors, uremia, chronic<br />
renal failure, hypomethylation, uremic toxins<br />
Homocysteine metabolism<br />
Homocysteine is a sulfur amino acid whose metabolism is<br />
related to methionine, an essential amino acid, contained<br />
either in the normal diet or originating from protein<br />
breakdown. Methionine, when it is not employed in protein<br />
biosynthesis, is condensed with ATP to form S-<br />
adenosylmethionine (AdoMet), a sulfonium compound.<br />
AdoMet in turn donates, after decarboxylation, the propyl<br />
amino moiety in polyamine synthesis, while its methyl group<br />
is utilized in the transmethylation pathway to methylate<br />
various methyl acceptors (proteins, DNA, and small<br />
molecules, such as guanidino acetate, in creatine<br />
biosynthesis). AdoMet demethylated product is S-<br />
adenosylhomocysteine (AdoHcy). AdoHcy is hydrolyzed to<br />
adenosine and homocysteine in a reversible reaction, which is<br />
inhibited by AdoHcy itself (in a competitive product type of<br />
inhibition). Homocysteine is then metabolized to<br />
cystathionine in the transsulfuration pathway, where CBS is<br />
the rate-limiting enzyme. The remethylation pathway leads to<br />
methionine formation from homocysteine, which receives a<br />
methyl group from methyltetrahydrofolate (MTHF), in a<br />
reaction catalyzed by methionine synthase. MTHF reductase<br />
is the enzyme which catalyzes the reduction of<br />
methylenetetrahydrofolate to MTHF, thereby irreversibly<br />
committing one carbon units to MTHF. This represents a<br />
“folate trap”, because MTHF can be used in this and only this<br />
remethylation reaction, while folates in less reduced forms<br />
can be used in other reactions and in particular by thymidilate<br />
synthase in the synthesis of this DNA precursor.<br />
Hyperhomocysteinemia and the cardiovascular disease in<br />
uremia<br />
An increase in plasma homocysteine levels is associated with<br />
an elevation of cardiovascular risk (1). The inherited<br />
enzymatic defect of CBS represents the most common form<br />
of homocystinuria, in which affected patients, who display<br />
high homocysteine levels in blood, used to die of premature<br />
cardiovascular disease (2, 3). In the general population, even<br />
a mild or moderate increase in blood homocysteine levels is<br />
associated with an increase in cardiovascular risk (4-7). In<br />
uremic patients, both those under conservative treatment and<br />
undergoing dialysis, there is an increase in cardiovascular<br />
risk, and actually uremia represents a model of generalized<br />
atherosclerosis. In addition, traditional risk factors or those<br />
typical of uremia can hardly explain this increase.<br />
Hyperhomocysteinemia is highly prevalent in this population.<br />
Recent studies show that hyperhomocysteinemia predicts<br />
mortality and cardiovascular events in uremic patients on<br />
hemodialysis (8-12). However, it has been recently proposed<br />
that low levels of homocysteine are linked to an increase in<br />
cardiovascular risk, so called reverse epidemiology (13-14).<br />
A recent study by Ducloux et al (15) clarifies once and for all<br />
this controversy. In this work, 459 patients, stratified in<br />
relation to the presence or absence of a chronic malnutritioninflammation<br />
state (CISM), were followed prospectically.<br />
Homocysteine levels > 30 micromolar were associated with a<br />
significantly higher risk of global mortality (Hazard ratio<br />
1.55, CI 1.12-4.72) in patients without CISM, and not in<br />
patients with CISM. Also taking into exam cardiovascular<br />
mortality, homocysteine levels > 30 micromolar were kinked<br />
to an increase in risk (Hazard ratio 1.91, CI 1.23-3.23) in<br />
patients without CISM, and not in those with this<br />
confounding factor. The conclusion is that<br />
hyperhomocysteinemia is a strong risk factor in patients<br />
without CISM, while in those with CISM, the association is<br />
masked by the combination of malnutrition-inflammation. In<br />
this case, in fact, homocysteine levels are lower, an<br />
expression of a reduced amino acid pool, and of<br />
hypoalbuminemia. Reverse epidemiology is so explained in<br />
patients with CISM, while in patients without CISM, the<br />
direct relation between homocysteine and mortality is<br />
confirmed.<br />
______________________<br />
Correspodence to: A. F. Perna, MD, PhD, Division of Nephrology/Department of Pediatrics, Second University<br />
of Naples, Via Pansini 5, Ed. 17, Naples, Italy 80131; Phone: +39-081-5666651;<br />
Fax +39-081-5666655; E-mail: alessandra.perna@unina2.it
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 75<br />
Causes of hyperhomocysteinemia<br />
As for the cause, this could be theoretically linked to<br />
increased production, reduced removal, or reduced excretion.<br />
The latter can be ruled out because urinary homocysteine<br />
excretion is negligible (16). Considering the possibility of an<br />
increase in homocysteine production: homocysteine comes<br />
from the hydrolysis of AdoHcy, the demethylated product of<br />
AdoMet, the methyl donor in transmethylations. However,<br />
the accumulation of homocysteine leads to an increase of its<br />
precursor AdoHcy, due to the slowing down of the hydrolysis<br />
reaction, and this in turn leads to transmethylation inhibition,<br />
and in particular of certain methyltransferases. We have<br />
shown, and findings were then confirmed by Loeher et al.<br />
and van Guldener et al. (17-19), that this is the case in CRF<br />
and uremia. At the high concentrations of AdoHcy present in<br />
uremia, and considering the Km and Ki of the various<br />
methyltransferases, several methyltransferases are affected,<br />
such as DNA methyltransferase, or the protein L-isoaspartate<br />
methyltransferase, a repair enzyme of damaged L-isoaspartyl<br />
residues, while others are not, such as the quantitatively most<br />
important one, guanidinoacetate methyltransferase. This<br />
methyltransferase leads to the formation of creatine, and then<br />
creatinine forms spontaneously from creatine.<br />
In 1980, Mitch and coworkers administered radiolabeled<br />
creatinine intravenously to subjects with severe CRF, and<br />
were able to show that the average rate of creatinine<br />
production was 150 micromoles/kg/day, similar to the<br />
production present in normal subjects (20). Guttormsen et al<br />
(21) showed that the average net influx of homocysteine into<br />
plasma was the same in controls and renal failure patients.<br />
Stam and coworkers (22) using stable isotope techniques<br />
have shown that transmethylations are reduced, as well as<br />
homocysteine clearance, in the whole body of CRF patients.<br />
All in all, it can be said that in uremia some<br />
methyltranferases are inhibited by AdoHcy, while some are<br />
relatively affected, and continue to produce AdoHcy and<br />
homocysteine, which will lead to AdoHcy accumulation, thus<br />
producing a vicious cycle. So, at present current evidence is<br />
in favor of the idea that no increased production of<br />
homocysteine is present in uremia.<br />
The most likely possibility, at this point of studies, is:<br />
decreased metabolic removal, either from the kidney, or from<br />
an extrarenal source. Studies from independent groups have<br />
shown that there is no difference in homocysteine<br />
concentration between the renal artery and the renal vein in<br />
humans (23, 24). However, this does not rule out the<br />
possibility that the kidney metabolizes homocysteine,<br />
because limitations of the measurement, expressing<br />
themselves in a relatively high coefficient of variation, could<br />
be an issue, that is small differences could still be important,<br />
and also we don’t know what happens in the fed state.<br />
Glomerular filtration of homocysteine is restricted because of<br />
protein binding, however, homocysteine could still be<br />
removed through peritubular uptake. Peritubular uptake refers<br />
to the transport of aminoacids, peptides and proteins which<br />
are taken up from the arterial capillaries coming from the<br />
efferent arteriole, surrounding the proximal tubules, and go<br />
into tubular cells, where they are either secreted into the<br />
tubular lumen, or remain into cells and are metabolized. This<br />
concept is supported by findings by Garibotto et al (25). In<br />
this paper, they show that the fractional extraction of<br />
homocysteine is positively linked to renal plasma flow, with<br />
a net uptake occurring when renal plasma flow is above 500<br />
ml/min. In addition, they show that homocysteine renal<br />
clearance is linked to renal plasma flow, that is, in these<br />
subjects, homocysteine clearance goes down to 0 when renal<br />
plasma flow is reduced. So at this point, we know that a<br />
reduction in homocysteine removal is found in CRF, but little<br />
more than that, and the matter is still controversial.<br />
Metabolic consequences of hyperhomocysteinemia<br />
Recently, some unforeseen consequences of<br />
hyperhomocysteinemia, coming from other laboratories, and<br />
ours, have been explored, which can ultimately affect<br />
mortality. We have proposed and explored the “unbalanced<br />
methylation” hypothesis in uremia. The accumulation of the<br />
homocysteine precursor AdoHcy, occurring when<br />
homocysteine levels are high, leads to an inhibition of those<br />
methyltransferases which are more sensitive to the inhibitor<br />
AdoHcy (high-sensitive methyltransferases, HS-Mtases). The<br />
low-sensitive methyltransferases (LS-Mtases) will continue<br />
to consume AdoMet and produce AdoHcy to an almost<br />
normal extent, thus further maintaining inhibition of the HS-<br />
MTases.<br />
For example, we have shown some years ago that<br />
methylation-dependent membrane protein repair, a process in<br />
which a methylation reaction is involved, is inhibited in<br />
erythrocytes of uremic patients (17).<br />
In addition, we have shown that total DNA methylation is<br />
reduced in dialysis patients and levels of decrease correlate<br />
significantly with plasma homocysteine levels (26).<br />
DNA methylation is viewed as a mechanism for gene<br />
silencing and regulation, as, for example, in the case of<br />
“imprinted genes”. Considering the way through which genes<br />
are passed from one generation to another, the allele coming<br />
from one of the parents is generally shut off through<br />
methylation. Under normal conditions, gene expression is<br />
therefore termed monoallelic for these genes (the gene<br />
coming from either the mother or the father is expressed, the<br />
other is silenced in a non-random manner). SYBL1 (a<br />
pseudoautosomal gene, X or Y inactivated) and H19 (an<br />
imprinted gene with maternal expression) are regulated in the<br />
way we just described. The allelic expression of these genes<br />
was used to test the "functional" outcome of DNA<br />
hypomethylation in uremic patients. Results show that, for<br />
SYBL1, gene expression in patients is biallelic, that is both<br />
alleles are expressed. For H19, only in patients with high<br />
homocysteine levels (approximately above 60 M) gene<br />
expression is biallelic.<br />
After folate therapy, gene expression returns monoallelic and<br />
total DNA methylation improves in parallel with a decrease<br />
of homocysteine levels, thus testifying that homocysteine<br />
modifies DNA methylation in a reversible fashion. So, we<br />
can state that, in patients with higher homocysteine, there is a<br />
transcriptional activation of the normally repressed allele, due<br />
to DNA hypomethylation. Folate treatment is able to revert<br />
the biallelic expression into monoallelic in the patients who<br />
had biallelic expression.<br />
Coming to plasma proteins, plasma proteins in hemodialysis<br />
patients display a significant increase in the content of L-<br />
isoaspartyl residues, so they are significantly altered, or<br />
damaged (27).<br />
This alteration under normal conditions can be repaired by a<br />
mechanism depending on a specific methyl transfer reaction.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 76<br />
This particular methyltransferase has been shown to be<br />
inhibited in uremia and, therefore, this kind of protein<br />
damage is increased. This inhibition depends partially on<br />
high homocysteine levels, and therefore methylation<br />
inhibition, because folate therapy is able to reduce damage<br />
levels.<br />
However, the pathogenesis of this alteration, when<br />
considering the plasma protein compartment, depends mostly<br />
on uremic toxicity. Several uremic toxins, from different<br />
chemical groups, can induce protein damage. However, we<br />
found that guanidine in particular is able to elicit this protein<br />
damage in a dose-dependent manner. Deamidated albumin,<br />
that is in vitro damaged albumin, was prepared with a<br />
standard protocol, and the binding capacity of various<br />
substances to this damaged albumin was tested. A reduced<br />
binding of homocysteine to serum albumin was found. We<br />
can conclude that increased protein damage, due to the<br />
uremic milieu and hypomethylation, induces protein damage,<br />
with reduced homocysteine binding to proteins, and possible<br />
increase in free homocysteine levels.<br />
Among the possible consequences of hyperhomocysteinemia,<br />
there is protein homocysteinylation, that is the binding of<br />
homocysteine to proteins, which occurs basically as a postbiosynthetic<br />
acylation of free amino groups (protein-Nhomocysteinylation,<br />
mediated by homocysteine thiolactone).<br />
This protein modification in in vitro experiments leads to<br />
functional derangements, such as a loss of enzymatic activity.<br />
Another type of protein homocysteinylation is through the<br />
formation of a covalent disulfide bond found primarily with<br />
cysteine residues (protein-S-homocysteinylation). We have<br />
been able to demonstrate the presence of a significant<br />
increase of homocysteinylated proteins in uremia (28). We<br />
obtained, with a new method combining gel filtration,<br />
hydrolysis, and HPLC chromatography, data for both protein-<br />
S-Hcy and protein-N-Hcy, which were significantly increased<br />
in the plasma of uremic patients on hemodialysis. This type<br />
of protein alteration occurs in uremia, because of the high<br />
homocysteine levels present in this condition, thus<br />
representing another example of a widespread presence of a<br />
derangement of the peptide link in uremia. Protein<br />
homocysteinylation could be one of the principal mediators<br />
of homocysteine toxicity, contributing to determine structural<br />
and functional alterations at the molecular and cellular level.<br />
Therefore, it can be stated that in chronic renal failure and<br />
end stage renal disease, both altered gene expression and the<br />
alterations in protein structure, dependent on<br />
hyperhomocysteinemia and acting through an increase of a<br />
homocysteine-related metabolite, may play a crucial role in<br />
terms of macromolecule functional derangement.<br />
Therapy<br />
In view of the epidemiological data and the high frequency of<br />
cardiovascular disease in chronic renal failure patients,<br />
numerous attempts have been made to lower plasma total<br />
homocysteine concentrations in these patients. In the general<br />
population, it is possible to reduce homocysteine levels by<br />
means of dietary intervention or with small folate<br />
supplementation. In chronic renal failure patients, possible<br />
tools conducive to a reduction of homocysteine levels are<br />
folate therapy, therapy with betaine, serine, N-acetylcysteine,<br />
or B vitamins (vitamin B 6 , B 12 , B 2 ), and improved dialysis.<br />
Betaine, serine, and B vitamins are either not effective, or can<br />
add only a modest additive effect. The mainstay of therapy is<br />
represented by folic acid, or folic acid in its active,<br />
circulating form, MTHF (29-30 for review).<br />
Folic acid therapy in chronic renal failure patients have been<br />
shown to reduce, albeit not to normalize, plasma total<br />
homocysteine concentrations, particularly in dialysis patients,<br />
who express therefore a resistance to folates. Folic acid<br />
supplementation of 1 mg daily, in contrast to what is usually<br />
observed in the general population, does not have any effect<br />
on plasma total homocysteine concentration in chronic failure<br />
failure patients, despite the induction of supernormal plasma<br />
folate levels. Oral supplementation with high doses of folic<br />
acid (up to 15 mg daily), which leads to a 20 to 50-fold<br />
increase of plasma folate concentrations, is only partially<br />
effective in reducing plasma total homocysteine. This relative<br />
resistance to folate action does not appear to be caused by<br />
defects in folate absorption or impairment in folic acid<br />
conversion in the plasma to the active metabolite MTHF.<br />
Moreover, active reduced forms of folic acid did not lead to a<br />
greater decrease in plasma total homocysteine levels than<br />
those observed with native folic acid supplementation in<br />
hemodialysis patients. However, MTHF provides a moiety<br />
which does not need to be further metabolized. This is<br />
important because a polymorphism, the C677T transition of<br />
MTHF reductase, is very common in the population (20 % in<br />
the homozygous, 30-40 % in the heterozygous). Providing<br />
the active form circumvents the possibility that the specific<br />
patient genetic pattern could affect folate utilization.<br />
Other abnormalities in homocysteine metabolism, as for<br />
instance a relative resistance to vitamin B12 action, have<br />
been observed in chronic renal failure patients. Theses<br />
abnormalities may also participate to the genesis of<br />
hyperhomocysteinemia in these patients. However, as<br />
mentioned previously, the correction of these abnormalities<br />
in folate-replete patients has only a partial additional effect<br />
on fasting total homocysteine in chronic renal failure patients.<br />
For the sake of completeness, it has to be mentioned that<br />
more efficient dialysis procedures could allow an improved<br />
removal of uremic toxins and/or homocysteine. The main<br />
reason for the genesis of hyperhomocysteinemia, and the<br />
reduced efficacy of folate therapy in dialysis chronic renal<br />
failure patients, as mentioned previously, is unclear at<br />
present. The accumulation of uremic toxins and the decrease<br />
in homocysteine clearance and metabolism owing to a<br />
decreased functioning renal mass are the two most probable<br />
explanations. Standard dialysis procedures using low-flux<br />
dialysers or high-flux dialysis are unable to remove sufficient<br />
amounts of homocysteine to maintain total homocysteine<br />
within the normal range. In contrast, dialysis in super-flux<br />
mode significantly lowered total homocysteine concentrations,<br />
possibly due to a greater reduction in uremic toxin concentration.<br />
This may also be partially due to albumin removal,<br />
since the major part of circulating homocysteine is protein-bound.<br />
Recently, it has been also demonstrated that total<br />
homocysteine levels were significantly lower among patients<br />
undergoing daily nocturnal HD.<br />
A displacement of homocysteine from protein-binding sites,<br />
allowing increased free homocysteine availability for plasma<br />
clearance by dialysis procedures could be an interesting alternative<br />
strategy to reduce total homocysteine concentrations.<br />
It has been reported by Scholze et al (31) that the acute<br />
intravenous administration of N-acetylcysteine (5 g in 5%<br />
glucose for 4 hours) during a hemodialysis session, which
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 77<br />
presumably can displace homocysteine from protein-binding<br />
sites, was able to completely normalize total homocysteine<br />
concentrations at the end of the session, with residual<br />
efficacy for the next two days. The acute decrease of total<br />
homocysteine concentrations induced by N-acetylcysteine<br />
supplementation during the dialysis session has been also<br />
shown to improve pulse pressure and endothelial function in<br />
hemodialysis patients. In a previous study, the same group<br />
has also shown that acetylcysteine reduces cardiovascular<br />
events, when given 600 mg per os, for two years (32).<br />
Friedman et al (33) have shown that long-term oral N-<br />
acetylcysteine administration (1.2 g twice a day) total<br />
homocysteine levels were reduced by 19 % in hemodialysis<br />
patients, compared with an 8 % reduction in patients treated<br />
with placebo (p = 0.07). Patients were vitamin-replete.<br />
Possibly, this study was underpowered to detect a statistically<br />
significant difference, and also acetylcysteine was<br />
administered orally.<br />
Although these results are promising, the efficacy and safety<br />
of intravenous administration of N-acetylcysteine needs,<br />
however, to be evaluated before drawing a definite<br />
conclusion. In any case, these data suggest that maneuvers<br />
aimed to displace homocysteine from protein-binding sites<br />
may represent a valuable strategy to normalize total<br />
homocysteine in dialysis patients.<br />
References<br />
1. Homocysteine studies collaboration. Homocysteine and risk of<br />
ischemic heart disease and stroke. JAMA 2002; 288(16): 2015-<br />
22<br />
2. McCully KS. Vascular pathology of homocysteinemia:<br />
implications for the pathogenesis of atherosclerosis. Am J<br />
Pathol 1969; 56: 111-128<br />
3. Wilcken DEL, Wilcken B. The natural history of vascular<br />
disease in homocystinuria and the effects of treatment. J Inherit<br />
Metab Dis 1997; 20: 295-300<br />
4. Wilcken DEL, Wilcken B. The pathogenesis of coronary artery<br />
disease. A possible role for methionine metabolism. J Clin<br />
Invest 1976; 57: 1079-1082<br />
5. Clarke R, Daly L, Robinson K et al. Hyperhomocysteinemia:<br />
an independent risk factor for vascular disease. N Engl J Med<br />
1991; 324: 1149-1155<br />
6. Ueland PM, Refsum H, Beresford SAA et al. The controversy<br />
over homocysteine and cardiovascular risk. Am J Clin Nutr<br />
2000; 72: 324-332<br />
7. Refsum H, Ueland PM. Recent data are not in conflict with<br />
homocysteine as a cardiovascular risk factor. Curr Opin<br />
Lipidol 1998; 9: 533-539<br />
8. Jungers P, Massy ZA, Khoa TN et al. Incidence and risk<br />
factors of atherosclerotic cardiovascular accidents in<br />
predialysis chronic renal failure patients: a prospective study.<br />
Nephrol Dial Transplant 1997; 12: 2597-2602<br />
9. Bostom AG, Shemin D, Verhoef P et al. Elevated fasting total<br />
plasma homocysteine levels and cardiovascular disease<br />
outcomes in maintenance dialysis patients. A prospective<br />
study. Arterioscler Thromb Vasc Biol 1997; 17: 2554-2558<br />
10. Moustapha A, Naso A, Nahlawi M et al. Prospective study of<br />
hyperhomocysteinemia as an adverse cardiovascular risk factor<br />
in end-stage renal disease. Circulation 1998; 97: 138-141<br />
11. Massy ZA, Chadefaux-Vekemans B, Chevalier A et al.<br />
Hyperhomocysteinemia: a significant risk factor for<br />
cardiovascular disease in renal transplant recipients. Nephrol<br />
Dial Transplant 1994; 9: 1103-1108<br />
12. Mallamaci F, Zoccali C, Tripepi G et al, on behalf of the<br />
CREED Investigators. Hyperhomocysteinemia predicts cardio-<br />
Kalantar-Zadeh K, Block G, Humphreys MH et al. A low,<br />
rather than a high, total plasma homocysteine is an indicator of<br />
poor outcome in hemodialysis patients. J Am Soc Nephrol<br />
2004; 15: 442-453<br />
13. Wrone EM, Hornberger JM, Zehnder JL et al. Randomized<br />
trial of folic acid for prevention of cardiovascular events in<br />
end-stage renal disease. J Am Soc Nephrol 2004; 15: 420-426<br />
14. Ducloux D, Klein A, Kazory A, Devillard N, Chalopin J-M.<br />
Impact of malnutrition-inflammation on the association between<br />
homocysteine and mortality. Kidney Int 2006;69:331-335<br />
15. Refsum H, Helland S, Ueland PM. Radioenzymic<br />
determination of homocysteine in plasma and urine. Clin<br />
Chem 1985; 31: 624-628<br />
16. Perna AF, Ingrosso D, Galletti P, Galletti P, Capasso G, De<br />
Santo NG. Enzymatic methyl esterification of erythrocyte<br />
membrane proteins is impaired in chronic renal failure.<br />
Evidence for high levels of the natural inhibitor S-<br />
adenosylhomocysteine. J Clin Invest 1993; 91: 2497-2503<br />
17. Loehrer FMT, Angst CP, Brunner FP, Haefeli WE, Fowler B.<br />
Evidence for disturbed S-adenosylmethionine: S-<br />
adenosylhomocysteine ratio in patients with end-stage renal<br />
failure: a cause for disturbed methylation reactions? Nephrol<br />
Dial Transplant 1998; 13: 656-661<br />
18. Van Guldener C, Kulik W, Berger R et al. Homocysteine and<br />
methionine metabolism in ESRD: A stable isotope study.<br />
Kidney Int 1999; 56: 1064-71<br />
19. Mitch WE, Collier VU, Walser M. Creatinine metabolism in<br />
chronic renal failure. Clin Sci 1980; 58: 327-335<br />
20. Guttormsen AB, Ueland PM, Svarstad E, Refsum H. Kinetic<br />
basis of hyperhomocysteinemia in patients with chronic renal<br />
failure. Kidney Int 1997; 52: 495-502<br />
21. Stam F, et a.l Am J Physiol 2004; 287: F215 van Guldener C,<br />
Donker AJM, Jacobs C, Teerlink T, De Meer K, Stehouwer C<br />
D A. No net renal extraction of homocysteine in fasting<br />
humans. Kidney Int 1998; 54: 166-169<br />
22. Bostom A G, Brosnan J T, Hall B et al. Net uptake of plasma<br />
homocysteine by the rat kidney in vivo. Atherosclerosis 1995;<br />
116: 59-62<br />
23. Garibotto G, Sofia A, Saffioti S et al. Inter-organ exchange of<br />
aminothiols in humans. Am J Physiol Endocrinol Metab 2003;<br />
284: E757-763<br />
24. Ingrosso D, Cimmino A, Perna AF et al. Folate treatment and<br />
unbalanced methylation and changes of allelic expression<br />
induced by hyperhomocysteinaemia in patients with uremia.<br />
Lancet 2003; 361: 1693-1699<br />
25. Perna AF, Ingrosso D, Satta E, Lombardi C, Galletti P,<br />
D’Aniello A, De Santo NG. Plasma protein aspartyl damage is<br />
increased in hemodialysis patients: studies on causes and<br />
consequences. J Am Soc Nephrol 2004; 15: 2747-2754<br />
26. Perna AF, Satta E, Acanfora F, Lombardi C, Ingrosso D, De<br />
Santo NG. Increased plasma protein homocysteinylation in<br />
hemodialysis patients. Kidney Int, 2006, epub ahead of print.<br />
27. Gonin JM. Folic acid supplementation to prevent adverse<br />
events in individuals with chronic kidney disease and end stage<br />
renal disease. Curr Opin Nephrol Hypertens 2005; 14: 277-261<br />
28. Massy ZA. Potential strategies to normalize the levels of<br />
homocysteine in chronic renal failure patients. Kidney Int 2003;<br />
63: S134-S136<br />
29. Scholtze A, Ringer C, Beige J et al. Acetylcysteine reduces<br />
plasma homocysteine concentration and improves pulse and<br />
endothelial function in patients with endstage renal failure.<br />
Circulation 2004; 1009(3): 369-74<br />
30. Tepel M, van der Giet M, Statz M, Jankowski J, Zidek W. The<br />
antioxidant acetylcysteine reduces cardiovascular events in patients<br />
with end-stage renal failure. Circulation 2003;107:992-<br />
995<br />
31. Friedman AN, Bostom AG, Laliberty P et al. The effects of N-<br />
acetylcysteine on plasma total homocysteine levels in<br />
hemodialysis: a randomised, controlled study. Am J Kidney Dis<br />
2003; 41(2): 442-6
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 77<br />
C.E.R.A. (Continuous Erythropoietin Receptor Activator):<br />
A new perspective in anaemia management<br />
W. Sulowicz<br />
Jagiellonian University, Krakow, Poland<br />
Abstract<br />
Challenges in anaemia management<br />
Continuous Erythropoietin Receptor Activator (C.E.R.A.), an<br />
innovative agent with unique receptor activity and a<br />
prolonged half-life, is currently in development to provide<br />
correction of anaemia and stable control of haemoglobin (Hb)<br />
levels at extended administration intervals in patients with<br />
chronic kidney disease (CKD) on dialysis and not on dialysis.<br />
Phase II studies suggest that C.E.R.A. can correct anaemia<br />
and maintain Hb levels when administered intravenously or<br />
subcutaneously at extended intervals of up to once monthly.<br />
C.E.R.A. is currently undergoing evaluation for the control of<br />
anaemia in patients with CKD in a large-scale Phase III<br />
programme.<br />
Keywords: anaemia, chronic kidney disease, haemoglobin<br />
Introduction<br />
Chronic kidney disease (CKD) is highly prevalent, with<br />
increasing numbers of patients affected by the disease<br />
worldwide (1). The progressive nature of CKD and ensuing<br />
end-stage renal disease is associated with high and increasing<br />
treatment costs that are creating a significant burden on<br />
global healthcare resources (2). Forecasts indicate that the<br />
incidence of CKD is expected to continue rising (3,4),<br />
reflecting the growing incidence of diabetes and the ageing<br />
population (1).<br />
Anaemia is already highly prevalent in the early stages of<br />
CKD (5–7) and is associated with increased mortality and<br />
morbidity (8–10). Evidence suggests that patients with CKD<br />
and anaemia progress more rapidly to dialysis than patients<br />
without anaemia (11,12). In addition, anaemia negatively<br />
impacts on cardiovascular disease (13,14), cognitive function<br />
(15) and quality of life (16,17).<br />
National and international clinical guidelines exist to<br />
facilitate the management of anaemia in patients with CKD<br />
(18–21). A number of studies demonstrate that maintaining<br />
haemoglobin (Hb) levels within recommended targets is<br />
associated with positive clinical outcomes (10,22–25).<br />
Extrapolation of data from the Dialysis Outcomes and<br />
Practice Patterns Study estimated a potential gain of 23 910<br />
patient-years in the US haemodialysis population over a 5-<br />
year period if patients were brought within Hb targets (≥11<br />
g/dL) (24).<br />
Despite the proven benefits, management of renal anaemia<br />
remains suboptimal; anaemia is often under-recognised and<br />
under-treated (5,26). The use of erythropoiesis-stimulating<br />
agents (ESAs) before the initiation of dialysis is still<br />
uncommon in most countries (27,28) with many CKD<br />
patients only receiving treatment once anaemia is advanced.<br />
Furthermore, with current treatment, approximately twothirds<br />
of patients with CKD have Hb levels outside guideline<br />
targets (29,30). In addition, substantial variability in Hb<br />
values over short periods of time has been demonstrated in<br />
many patients with CKD treated with ESAs (29,31–34). This<br />
variability in ESA response may be due to a range of factors,<br />
such as dialysis effects, intercurrent illness and iron therapy.<br />
Effective management of anaemia is already time consuming,<br />
and the burden on healthcare providers can only increase as<br />
the prevalence of CKD continues to rise. Currently most<br />
available ESAs require frequent administration (up to three<br />
times per week) (19,20). Furthermore, frequent monitoring<br />
and dose adjustment is required to maintain Hb levels within<br />
guideline targets with current treatment. New agents that<br />
offer more effective anaemia management by providing<br />
stable Hb levels at extended administration intervals may<br />
reduce the burden on healthcare professionals.<br />
C.E.R.A.<br />
Continuous Erythropoietin Receptor Activator (C.E.R.A.), an<br />
innovative agent with unique receptor activity and a<br />
prolonged half-life, is currently in development to provide<br />
correction of anaemia and stable control of Hb levels at<br />
extended administration intervals in patients with CKD on<br />
dialysis and not on dialysis. C.E.R.A. is chemically<br />
synthesised, and differs from erythropoietin through the<br />
integration of amide bonds between amino groups and<br />
methoxy polyethylene glycol-succinimidyl butanoic acid<br />
(35).<br />
Evidence is accumulating that C.E.R.A. has unique receptor<br />
properties, acting differently to epoetin at the receptor level<br />
(36). Data suggest that C.E.R.A. has a much lower affinity<br />
for the erythropoietin receptor compared with epoetin beta,<br />
leading to a reduced specific activity in vitro. However, since<br />
the elimination half-life is so prolonged, C.E.R.A. has<br />
increased erythropoietic activity in vivo (37).<br />
Phase I studies in healthy subjects<br />
Four Phase I studies have been conducted in healthy subjects<br />
to investigate the pharmacokinetic and pharmacodynamic<br />
properties of C.E.R.A. In two single ascending dose studies,<br />
subjects were randomised to receive single intravenous (IV)<br />
doses of C.E.R.A. (0.4–3.2 µg/kg) or placebo (n=38) or<br />
______________________<br />
Correspodence to: W. Sulowicz, Department of Nephrology, Jagiellonian University, 31-501 Krakow,<br />
ul. Kopernika 15 c, Poland; Email: wladsul@mp.pl
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 78<br />
single subcutaneous (SC) doses of C.E.R.A. (0.1–3.2 µg/kg)<br />
or placebo (n=70) (38). In two multiple ascending dose<br />
studies, subjects were randomised to receive three IV doses<br />
of C.E.R.A. (0.4–3.2 µg/kg) or placebo (n=61) once every 3<br />
weeks or four SC doses of C.E.R.A. (0.4–3.2 µg/kg) or<br />
placebo (n=48) once every 2 weeks (38). In the single<br />
ascending dose studies, a dose-dependent erythropoietic<br />
response was seen with both IV and SC C.E.R.A.<br />
administration. C.E.R.A. induced an increase in reticulocyte<br />
counts that peaked within 10 days and returned to baseline<br />
after 20 days. Consistent results were obtained in the multiple<br />
ascending dose studies: a dose-dependent erythropoietic<br />
response was observed with both routes of administration.<br />
The half-life for C.E.R.A. was observed to be considerably<br />
longer than those reported for currently available ESAs<br />
(Table 1) (39–42). In the multiple ascending dose studies, the<br />
clearance of both IV and SC C.E.R.A. was low (IV 27.6–44.6<br />
ml/h; SC 97–347 ml/h) (41). The prolonged half-life and low<br />
clearance observed with C.E.R.A., together with its unique<br />
receptor activity, give rise to a different pharmacological<br />
profile compared with currently available ESAs and suggest<br />
that extended administration intervals are possible.<br />
Table 1. Half-lives of C.E.R.A. and currently available<br />
erythropoietic stimulating agents in healthy volunteers<br />
(39–42)<br />
Mean half-life (h)<br />
IV SC<br />
C.E.R.A. 133 137<br />
Epoetin alfa 6.8 19.4<br />
Epoetin beta 8.8 24.2<br />
Darbepoetin alfa 25.3 48.8<br />
IV, intravenous; SC, subcutaneous.<br />
Phase II studies in patients with CKD and anaemia<br />
Four Phase II dose-finding studies have investigated the<br />
feasibility of C.E.R.A. for the correction of anaemia and<br />
maintenance of Hb levels at extended administration intervals<br />
in more than 350 patients with CKD.<br />
Fig 1. Mean (±SEM) haemoglobin (Hb) change from baseline after<br />
6 weeks’ treatment with C.E.R.A. in A) patients with chronic kidney<br />
disease receiving dialysis and B) patients with chronic kidney<br />
disease not receiving dialysis (35).<br />
A)<br />
Mean Hb change (g/dL)<br />
2.0<br />
1.5<br />
1.0<br />
0.5<br />
0.0<br />
1x/wk 1x/2wk 1x/3wk<br />
Administration schedule<br />
B)<br />
Mean Hb change (g/dL)<br />
2.0<br />
1.5<br />
1.0<br />
0.5<br />
0.0<br />
1x/wk 1x/2wk 1x/3wk<br />
Administration schedule<br />
In two studies, one in CKD patients receiving dialysis (n=61)<br />
(43) and one in CKD patients not yet receiving dialysis<br />
(n=65) (44), SC C.E.R.A. was administered for the correction<br />
of anaemia. All patients were aged 18 years, with Hb 8–11<br />
g/dL and were ESA-naïve. These studies examined escalating<br />
doses of C.E.R.A., with once-weekly, once every 2 weeks,<br />
and once every 3 weeks schedules being assessed in each<br />
dose group. Mean increases in Hb are shown in Figure 1.<br />
There was a significant dose response to C.E.R.A. and the Hb<br />
response was independent of the frequency of administration<br />
(43,44). These results suggest that C.E.R.A. is capable of<br />
correcting anaemia to guideline targets within the<br />
recommended timeframe when administered to ESA-naïve<br />
CKD patients at extended administration intervals.<br />
Two Phase II, multicentre, dose-finding studies have been<br />
conducted to determine the efficacy of C.E.R.A. for the<br />
maintenance of Hb levels in adult patients with renal anaemia<br />
(Hb 10–13 g/dL) on dialysis. In one study, 91 haemodialysis<br />
patients previously maintained on three-times weekly IV<br />
epoetin alfa were switched to IV C.E.R.A. (45). After a 2-<br />
week run-in period, patients were randomised to one of three<br />
C.E.R.A. doses based on their previous epoetin dose and data<br />
on exposure to C.E.R.A. from healthy subjects; once-weekly<br />
and once every 2 weeks administration schedules were<br />
assessed in each dose group for 19 weeks. A significant<br />
(P
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 79<br />
month period (Figure 2); mean Hb levels over time were<br />
11.51 g/dL (95% confidence interval (CI): 11.31, 11.71),<br />
11.18 g/dL (95% CI: 10.91, 11.46) and 11.15 g/dL (95% CI:<br />
10.91, 11.39) for once every 2 weeks, once every 3 weeks<br />
and once monthly administration schedules, respectively<br />
(47,48). Data from these long-term extension studies indicate<br />
that C.E.R.A. can control anaemia when administered at<br />
extended intervals, maintaining sustained and stable Hb<br />
levels in dialysis patients.<br />
A large-scale Phase III programme is underway evaluating<br />
the efficacy and safety of C.E.R.A. in approximately 2400<br />
patients with CKD on dialysis and not on dialysis from 29<br />
countries.<br />
Fig 2. Mean (±SD) haemoglobin (Hb) over time following once<br />
monthly subcutaneous administration of C.E.R.A.<br />
Reproduced with permission from Curr Hematol Rep (35).<br />
Copyright 2005, Current Science Group<br />
16<br />
Hb (mean ± SD, g/dL)<br />
15<br />
14<br />
13<br />
12<br />
11<br />
10<br />
9<br />
8<br />
7<br />
Tolerability<br />
1 2 3 4 5 6 7 8 9 10 11 12<br />
Months of treatment (extension period)<br />
C.E.R.A. was generally well tolerated in healthy volunteers<br />
(38,49). Similarly, in patients with CKD, C.E.R.A. was<br />
generally well tolerated with no unexpected safety concerns.<br />
Available information indicates that the incidence of adverse<br />
events (AEs) was in accordance with that expected for this<br />
study population (50). The most frequent AEs in the two 12-<br />
month maintenance study extension periods (n=109) were<br />
hypotension and muscle cramp (8.05% and 4.39% of all AE<br />
episodes, respectively) (50). The most common serious AEs<br />
were hypotension (five events), myocardial infarction (five<br />
events), cellulitis (four events) and pancreatitis (four events).<br />
In all studies conducted to date (healthy volunteers and<br />
patients with CKD), there has been no evidence of antibody<br />
development in any patient treated with C.E.R.A.<br />
Conclusions<br />
C.E.R.A.’s pharmacokinetic properties, including a prolonged<br />
half-life and low clearance, together with its unique receptor<br />
binding properties, result in a different pharmacological<br />
profile compared with currently available ESAs and suggest<br />
that extended administration intervals are feasible. Phase II<br />
studies in patients with CKD suggest that C.E.R.A. can<br />
correct anaemia and maintain Hb levels at extended intervals<br />
of up to once monthly. C.E.R.A. is currently undergoing<br />
evaluation for the management of anaemia in patients with<br />
CKD in a large-scale Phase III programme, with preliminary<br />
results expected soon. The potential for C.E.R.A. to be<br />
administered at extended administration intervals may<br />
simplify anaemia management, reducing the burden for<br />
patients and healthcare professionals.<br />
Acknowledgements<br />
Medical writing support was provided by Emma Marshman at<br />
Prime Medica Ltd during the preparation of this paper, supported<br />
by F. Hoffmann-La Roche. Responsibility for opinions, conclusions<br />
and interpretation of data lies with the authors.<br />
References<br />
1. El Nahas AM, Bello AK. Chronic kidney disease: the global<br />
challenge. Lancet 2005; 365: 331–340<br />
2. U.S. Renal Data System, USRDS 2005 Annual Data Report:<br />
Atlas of End-Stage Renal Disease in the United States, National<br />
Institutes of Health, National Institute of Diabetes and<br />
Digestive and Kidney Diseases, Bethesda, MD, 2005<br />
3. Xue JL, Ma JZ, Louis TA, Collins AJ. Forecast of the number<br />
of patients with end-stage renal disease in the United States to<br />
the Year 2010. J Am Soc Nephrol 2001; 12: 2753–2758<br />
4. Roderick P, Davies R, Jones C, Feest T, Smith S, Farrington K.<br />
Simulation model of renal replacement therapy: predicting<br />
future demand in England. Nephrol Dial Transplant 2004; 19:<br />
692–701<br />
5. Kazmi WH, Kausz AT, Khan S et al. Anemia: an early<br />
complication of chronic renal insufficiency. Am J Kidney Dis<br />
2001; 38: 803–812<br />
6. Astor BC, Muntner P, Levin A, Eustace JA, Coresh J.<br />
Association of kidney function with anemia: the third national<br />
health and nutrition examination survey (1988-1992). Arch<br />
Intern Med 2002; 162: 1401–1408<br />
7. McClellan W, Aronoff SL, Bolton WK et al. The prevalence of<br />
anemia in patients with chronic kidney disease. Curr Med Res<br />
Opin 2004; 20: 1501–1510<br />
8. Collins AJ, Li S, St Peter W et al. Death, hospitalization, and<br />
economic associations among incident hemodialysis patients<br />
with hematocrit values of 36 to 39%. J Am Soc Nephrol 2001;<br />
12: 2465–2473<br />
9. Ofsthun N, LaBrecque J, Lacson E, Keen M, Lazarus JM. The<br />
effects of higher hemoglobin levels on mortality and<br />
hospitalization in hemodialysis patients. Kidney Int 2003; 63:<br />
1908–1914<br />
10. Li S, Collins AJ. Association of hematocrit value with<br />
cardiovascular morbidity and mortality in incident<br />
hemodialysis patients. Kidney Int 2004; 65: 626–633<br />
11. Gilbertson DT, Li S, Murray A, Herzog C, Collins A. The<br />
competing risks of death vs. ESRD in Medicare beneficiaries<br />
65+ with chronic kidney disease, CHF and anemia (abstract). J<br />
Am Soc Nephrol 2002; 13: 439A<br />
12. Silverberg D. Outcomes of anaemia management in renal<br />
insufficiency and cardiac disease. Nephrol Dial Transplant<br />
2003; 18 (Suppl 2): ii7–ii12<br />
13. Foley RN, Parfrey PS, Morgan J et al. Effect of hemoglobin<br />
levels in hemodialysis patients with asymptomatic<br />
cardiomyopathy. Kidney Int 2000; 58: 1325–1335<br />
14. McClellan WM, Flanders WD, Langston RF, Jurkovitz C,<br />
Presley R. Anemia and renal insufficiency are independent risk<br />
factors for death among patients with congestive heart failure<br />
admitted to community hospitals: a population-based study. J<br />
Am Soc Nephrol 2002; 13: 1928–1936<br />
15. Pickett JL, Theberge DC, Brown WS, Schweitzer SU,<br />
Nissenson AR. Normalizing hematocrit in dialysis patients<br />
improves brain function. Am J Kidney Dis 1999; 33: 1122–<br />
1130<br />
16. Perlman RL, Finkelstein FO, Liu L et al. Quality of life in<br />
chronic kidney disease (CKD): a cross-sectional analysis in the<br />
Renal Research Institute-CKD study. Am J Kidney Dis 2005;<br />
45: 658–666
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 80<br />
17. Gerson A, Hwang W, Fiorenza J et al. Anemia and healthrelated<br />
quality of life in adolescents with chronic kidney<br />
disease. Am J Kidney Dis 2004; 44: 1017–1023<br />
18. Barrett BJ, Fenton SS, Ferguson B et al. Clinical practice<br />
guidelines for the management of anemia coexistent with<br />
chronic renal failure. Canadian Society of Nephrology. J Am<br />
Soc Nephrol 1999; 10 (Suppl 13): S292–S296<br />
19. National Kidney Foundation: K/DOQI Clinical practice<br />
guidelines: 2000 update. Am J Kidney Dis 2001; 37 (Suppl 1):<br />
S1–S238<br />
20. Locatelli F, Aljama P, Barany P et al. European Best Practice<br />
Guidelines Working Group: Revised European best practice<br />
guidelines for the management of anaemia in patients with<br />
chronic renal failure. Nephrol Dial Transplant 2004; 19 (Suppl<br />
2): ii1–ii47<br />
21. Pollock C, McMahon L. Haemoglobin. Nephrology 2005; 10<br />
(Suppl 4): S108–S115<br />
22. Ma JZ, Ebben J, Xia H, Collins AJ. Hematocrit level and<br />
associated mortality in hemodialysis patients. J Am Soc<br />
Nephrol 1999; 10: 610–619<br />
23. Xia H, Ebben J, Ma JZ, Collins AJ. Hematocrit levels and<br />
hospitalization risks in hemodialysis patients. J Am Soc<br />
Nephrol 1999; 10: 1309–1316<br />
24. Port FK, Pisoni RL, Bragg-Gresham JL et al. DOPPS estimates<br />
of patient life years attributable to modifiable hemodialysis<br />
practices in the United States. Blood Purif 2004; 22: 175–180<br />
25. Ofsthun NJ, LaBrecque J, Keen M, Im Youngson H, Krishnan<br />
M, Lazarus M. The association of mortality and hospitalization<br />
with hemoglobin (Hb) and missed dialysis treatments in stage 5<br />
chronic kidney disease (CKD) patients with and without<br />
cardiac morbidities (abstract). Nephrol Dial Transplant 2005;<br />
20(Suppl 5): v268<br />
26. Obrador GT, Pereira BJ. Anaemia of chronic kidney disease: an<br />
under-recognized and under-treated problem. Nephrol Dial<br />
Transplant 2002; 17(Suppl 11): 44–46<br />
27. Hörl WH, Macdougall IC, Rossert J et al. Predialysis Survey<br />
on Anemia Management: patient referral. Am J Kidney Dis<br />
2003; 41: 49–61<br />
28. Valderrábano F, Hörl WH, Macdougall IC, Rossert J,<br />
Rutkowski B, Wauters JP. PRE-dialysis survey on anemia<br />
management. Nephrol Dial Transplant 2003; 18: 89–100<br />
29. Lacson E Jr, Ofsthun N, Lazarus JM. Effect of variability in<br />
anemia management on hemoglobin outcomes in ESRD. Am J<br />
Kidney Dis 2003; 41: 111–124<br />
30. Centers for Medicare & Medicaid Services. 2004 Annual<br />
Report, End Stage Renal Disease Clinical Performance<br />
Measures Project. Department of Health and Human Services,<br />
Centers for Medicare & Medicaid Services, Office of Clinical<br />
Standards & Quality, Baltimore, Maryland, December 2004<br />
31. Berns JS, Elzein H, Lynn RI, Fishbane S, Meisels IS, DeOreo<br />
PB. Hemoglobin variability in epoetin-treated hemodialysis<br />
patients. Kidney Int 2003; 64: 1514–1521<br />
32. Collins AJ, Brenner RM, Ofman JJ et al. Epoetin alfa use in patients<br />
with ESRD: an analysis of recent US prescribing patterns<br />
and hemoglobin outcomes. Am J Kidney Dis 2005;46: 481–488<br />
33. Fishbane S, Berns JS. Hemoglobin cycling in hemodialysis<br />
patients treated with recombinant human erythropoietin. Kidney<br />
Int 2005; 68: 1337–1343<br />
34. Macdougall IC, Wilson P, Roche A. Impact of Haemoglobin<br />
Variability in Haemodialysis Patient Receiving Erythropoiesis-<br />
Stimulating Agents for the Management of Renal Anemia<br />
(abstract). J Am Soc Nephrol 2005; 16: 899A<br />
35. Macdougall IC. CERA (Continuous Erythropoietin Receptor<br />
Activator): A New Erythropoiesis-Stimulating Agent for the<br />
Treatment of Anemia. Curr Hematol Rep 2005; 4: 436–440<br />
36. Bailon P, Pahlke W, Brandt M, Haselbeck A. CERA<br />
(Continuous Erythropoiesis Receptor Activator) for the<br />
treatment of renal anemia: a new agent with an innovative<br />
mechanism of action (abstract). Nephrol Dial Transplant 2003;<br />
18 (Suppl 4): 166<br />
37. Macdougall IC, Bailon P, Tare N, Pahlke W, Pill J. CERA<br />
(Continuous Erythropoietin Receptor Activator) for the<br />
treatment of renal anemia: an innovative agent with unique<br />
receptor binding characteristics and prolonged serum half-life<br />
(abstract). J Am Soc Nephrol 2003; 14: 769A<br />
38. Reigner B, Jordan P, Pannier A, Glaspy J. Phase I studies with<br />
CERA (Continuous Erythropoiesis Receptor Activator), an<br />
innovative erythropoietic agent (abstract). Eur J Cancer 2003;<br />
1(Suppl 5): S172<br />
39. Halstenson CE, Macres M, Katz SA et al. Comparative<br />
pharmacokinetics and pharmacodynamics of epoetin alfa and<br />
epoetin beta. Clin Pharmacol Ther 1991; 50: 702–712<br />
40. Macdougall IC, Gray SJ, Elston O et al. Pharmacokinetics of<br />
novel erythropoiesis stimulating protein compared with epoetin<br />
alfa in dialysis patients. J Am Soc Nephrol 1999;10: 2392–2395<br />
41. Dougherty FC, Reigner B, Jordan P, Pannier A. CERA<br />
(Continuous Erythropoietin Receptor Activator): doseresponse,<br />
pharmacokinetics and tolerability in phase I multiple<br />
ascending dose studies (abstract). J Clin Oncol 2004; 22: 14S<br />
42. Macdougall IC, Reigner B, Dougherty FC. Consistent<br />
pharmacologic properties of C.E.R.A. (Continuous<br />
Erythropoietin Receptor Activator) in healthy volunteers and in<br />
patients with CKD (abstract). Am JKidney Dis 2006;47:In Press<br />
43. de Francisco AL, Sulowicz W, Dougherty FC. Subcutaneous<br />
CERA (Continuous Erythropoiesis Receptor Activator) has<br />
potent erythropoietic activity in dialysis patients with chronic<br />
renal anemia: an exploratory multiple-dose study (abstract). J<br />
Am Soc Nephrol 2003; 14: 27A-28A<br />
44. Provenzano R, Besarab A, Macdougall IC, Dougherty FC,<br />
Beyer U on behalf of the BA16528 study group. CERA<br />
(Continuous Erythropoietin Receptor Activator) administered<br />
up to once every 3 weeks corrects anemia in patients with<br />
chronic kidney disease not on dialysis (abstract). J Am Soc<br />
Nephrol 2004; 15: 544A<br />
45. Besarab A, Bansal V, Fishbane S et al, on behalf of the<br />
BA16285 study group: Intravenous CERA (Continuous<br />
Erythropoiesis Receptor activator) administered once weekly or<br />
once every 2 weeks maintain haemoglobin levels in haemodialysis<br />
patients with chronic renal anaemia (abstract). Abstract<br />
Book of the XLI Congress of the ERA-EDTA. 2004; p230<br />
46. Locatelli F, Villa G, Arias M, Marchesi D, Dougherty FC,<br />
Beyer U on behalf of the BA16286 study group. CERA<br />
(Continuous Erythropoietin Receptor Activator) maintains<br />
hemoglobin levels in dialysis patients when administered<br />
subcutaneously up to once every 4 weeks (abstract). J Am Soc<br />
Nephrol 2004; 15: 543A<br />
47. Locatelli F, Villa G, Beyer U, Dougherty FC, on behalf of the<br />
BA16286 extension study group. Subcutaneous CERA<br />
(Continuous Erythropoietin Receptor Activator) maintains<br />
haemoglobin concentrations with dosing intervals up to 4<br />
weeks in dialysis patients (abstract). Nephrol Dial Transplant<br />
2005; 20(Suppl 5): v261<br />
48. Besarab A, Beyer U, Dougherty FC. Long-term intravenous<br />
CERA (Continuous Erythropoietin Receptor Activator)<br />
maintains haemoglobin concentrations in hemodialysis patients<br />
(abstract). Nephrology 2005; 10 (Suppl): A312<br />
49. Reigner B, Jordan P, Pannier A, Dougherty FC. Phase I studies<br />
of the new erythropoietic agent, CERA (Continuous<br />
Erythropoiesis Receptor Activator): demonstration of a dosedependent<br />
response (abstract). Nephrol Dial Transplant 2003;<br />
18(Suppl 3): 167<br />
50. Dougherty FC, Beyer U. Safety and tolerability profile of<br />
Continuous Erythropoietin Receptor Activator (CERA) with<br />
extended dosing intervals in patients with chronic kidney:<br />
disease on dialysis (abstract). Nephrology 2005;<br />
10(Suppl)A313
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 82<br />
Diagnosis and treatment of renal bone disease<br />
G. B. Spasovski<br />
Department of Nephrology, University Clinical Center, University of Skopje, Republic of Macedonia<br />
Abstract<br />
The abnormalities in bone histology in patients with chronic<br />
renal failure (CRF), known as renal osteodystrophy (ROD),<br />
can be observed early in the course of the disease. Patients<br />
with mild to moderate degrees of CRF rarely experience<br />
symptoms, although skeletal changes may occur years before<br />
the symptoms arise. In end stage renal failure (ESRF) when<br />
patients require chronic maintenance dialysis, nearly all of<br />
them have abnormal bone histology. Moreover, survival rates<br />
of patients on dialysis have increased because of therapeutic<br />
improvement and the resultant increase in duration of dialysis<br />
has led to a further rise in renal osteodystrophy. Because<br />
metabolic bone disease can produce fractures, bone pain, and<br />
deformities late in the course of the disease, diagnosis,<br />
prevention and early treatment are essential.<br />
To date, bone biopsy is the most powerful and informative<br />
diagnostic tool to provide precise information on the type and<br />
severity of renal osteodystrophy and also useful in research to<br />
assess the effects of therapies on bone. Alternatives to the<br />
bone biopsy continue to be searching for, but the noninvasive<br />
bone markers have not been proven to hold<br />
sufficient diagnostic performance. Hence, transiliac bone<br />
biopsy remains the golden standard for the diagnosis of renal<br />
osteodystrophy.<br />
The therapy of renal bone disease depends on the particular<br />
type of ROD. However, some therapies (aluminum hydroxide<br />
and calcium carbonate) can exacerbate mineral balance and<br />
lead to the development of low-turnover bone diseases<br />
(osteomalacia or adynamic bone) and increased levels of<br />
vascular calcifications. Nowadays, phosphate control has<br />
been achieved with alternative phosphate binders that are not<br />
associated with these side effects (Sevelamer hydrochloride -<br />
RenaGel and Lanthanum carbonat - Fosrenol ).<br />
Key words: renal failure, renal osteodystrophy, bone biopsy,<br />
bone markers, calcium carbonate, lanthanum carbonate.<br />
Bone biopsy<br />
Double tetracycline labelling is the first prerequisite for an<br />
informative bone biopsy with an interval of 8 to 12 days (1).<br />
Phosphate binding treatment is stopped at the time of labeling<br />
and transiliac bone biopsy is then performed 2 to 6 days after<br />
the second label, under local anesthesia.<br />
The possible complications from bone biopsies can include<br />
pain, haematoma, wound infection, and rarely neuropathy.<br />
However, studies show that the biopsies of the anterior iliac<br />
result of procedure (2-4). The operator's experience is<br />
important in minimizing morbidity and in obtaining an<br />
adequate specimen. Based on histomorphometric findings,<br />
two main groups of renal bone disease can be classified: low<br />
(LTO) and high bone turnover (HTO) (3,5). Adynamic bone<br />
disease is characterized by a decreased number of osteoblasts<br />
and osteoclasts with a low bone formation rate (BFR). The<br />
second type of LTO, osteomalacia (OM), has a superimposed<br />
mineralization defect producing a great amount of<br />
unmineralized osteoid. HTO bone disease includes mild and<br />
severe hyperparathyroid bone disease (HPTH) or osteitis<br />
fibrosa, characterized by an excessive number of osteoclasts<br />
and osteoblasts and a high rate of bone formation and<br />
resorption. Mixed uremic osteodystrophy (Mx) possesses the<br />
combined features of both HPTH and OM.<br />
Alternatives to the bone biopsy continue to be searching for,<br />
but the non-invasive bone markers have not been proven to<br />
hold sufficient diagnostic performance (6). Hence, transiliac<br />
bone biopsy remains the golden standard for the diagnosis of<br />
renal osteodystrophy.<br />
Clinical application - Because bone biopsies more accurately<br />
determine the type of renal osteodystrophy and can indicate<br />
potential aluminum, strontium and lanthanum accumulation<br />
in dialyzed patients, they also allow tailoring of therapeutic<br />
measures. Additionally, bone biopsies could be performed at<br />
an interval of 6-12 months, sufficient for recognition of the<br />
specific changes of bone remodeling and mineral<br />
metabolism.<br />
The biopsy shows the degree of bone turnover helping the<br />
practitioner to determine the route, aggressiveness, and length<br />
of phosphate binding and calcitriol therapy. Severe<br />
hyperparathyroidism with marked bone marrow fibrosis is an<br />
indication for high doses of calcitriol if the calciumphosphorus<br />
product can be controlled. In patients with mild<br />
to moderate increase in bone turnover with or without<br />
mineralization defect, doses of intravenous or preoperative<br />
calcitriol and duration of therapy may be adjusted to avoid<br />
the development of ABD.<br />
In case of ABD, calcitriol therapy is not desirable because of<br />
the risk of inducing hypercalcemia, extraosseous<br />
calcifications and further suppression of parathyroid glands'<br />
activity. Moreover, the use of a low calcium dialysate is<br />
recommended, as well as a lesser daily intake of calcium in<br />
the diet, ommiting the treatment with calcium containing<br />
phosphate binding agents.<br />
Clinical experience<br />
Our bone biopsy study in 84 ESRD patients revealed that<br />
crest result in very small morbidity and no mortality as a<br />
______________________<br />
Correspodence to: G. B. Spasovski, Department of Nephrology, University Clinical Center,<br />
Vodnjanska 17, 1000 Skopje, Macedonia; Telephone: + 389 70 268 232; Fax: + 389 2 3231 501;<br />
E-mail: gspas@sonet.com.mk
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 83<br />
62% of a predialysis population had abnormal bone histology<br />
(3). ABD was found to be the most frequent bone lesion<br />
observed in 23%, while HPTH (mild form) was diagnosed in<br />
only 9% of the patients. The majority of patients (38%) in our<br />
study presented with a normal bone histology. Hence, this<br />
finding differs considerably from the ROD spectra reported<br />
previously in non-dialysed renal failure patients where none<br />
of the patients was reported to have normal bone histology<br />
(7,8). Furthermore, our study revealed that serum calcium<br />
levels in 15 out of 19 (79%) patients with ABD appeared to<br />
be > 2.1 mmol/l; 4 of them were hypercalcemic >2.5 mmol/l<br />
and 12 (63%) presented with calcium x phosphorus product ><br />
4.4 mmol/l (55 mg 2 /dl 2 ). These findings were in agreement<br />
with the afore-mentioned treatment for ABD patients.<br />
A recent study with lanthanum carbonate (LC) as a new<br />
phosphate binder, has shown its safety and effectiveness in<br />
phosphate binding (9). Additionally, we evaluated plasma<br />
and bone lanthanum levels in 20 incident dialysis patients at<br />
baseline, after 1 year of LC (n=10) and calcium carbonate<br />
treatment (CC=10) and after a 2-year of follow-up period<br />
during which the lanthanum treatment was replaced by CC<br />
(n=19) (4).<br />
Baseline plasma lanthanum levels were below 0.03 ng/ml in<br />
most of the patients of both groups. During lanthanum<br />
carbonate treatment lanthanum levels increased reaching a<br />
maximal level of 1.26 ± 1.24 ng/ml at 24 weeks, after which<br />
they stabilized at a value varying around 0.60 ng/ml.<br />
Compared to the values noted at cessation of lanthanum<br />
treatment a significant decline of plasma lanthanum levels<br />
was noted at 6 weeks of follow-up (0.59 ± 0.52 vs. 0.17 ±<br />
0.12 ng/ml; P < 0.05). There was no further significant<br />
decrease in mean plasma lanthanum concentration during the<br />
further 2-year follow-up (0.09 ± 0.03 ng/ml).<br />
The mean bone concentration in patients receiving LC<br />
increased substantially from 0.05±0.03 to 2.3±1.6 mg/g<br />
(P
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 83<br />
Efficiency of mycophenolate-mofetil in resistant nephrotic syndrome – case<br />
reports<br />
B. Milic, T. Ilic, I. Mitic, I. Budosan and S. Curic<br />
Clinic of Nephrology, Institute of Internal Diseases, Clinical Centre, Novi Sad, Serbia and Montenegro<br />
Abstract<br />
Patients with nephrotic syndrome (NS) in the primary<br />
glomerulonephritis are usually treated with standard<br />
immunosuppressive treatment including steroids and<br />
cyclophosphamide. This is a case report of two patients<br />
resistant to standard therapy who showed remarkable<br />
improvement in their NS when using mycophenolate-mofetil<br />
(MMF). First patient, (male, 54-year old) was admitted to our<br />
hospital with a 1-month clinical and laboratory history of NS.<br />
He was diagnosed with membranoproliferative glomerulonephritis<br />
after renal biopsy. After three months of standard<br />
steroid therapy (methylprednisolone 1-2 mg/kg BW) he did<br />
not achieve remission. Because of that we continued the<br />
treatment with pulse doses of methylprednisolone, followed<br />
with cyclophosphamide pulses. During the following two<br />
years of therapy patient continued to have frequent relapses.<br />
Proven to be steroid and cyclophosphamide resistant he was<br />
shifted to MMF therapy (dose of 2g/day). One month after<br />
starting therapy patient achieved complete remission with no<br />
side effects. The other patient (male, aged 62) was diagnosed<br />
with NS (membranous nephropathy) two months before<br />
admitting in our hospital. Standard therapeutic procedure<br />
included pulse doses of methylprednisolone during one<br />
month and then cyclophosphamide per os (2 mg/kg BW) for<br />
one year but with no respond in decreasing of proteinuria. In<br />
order to achieve remission, Cyclosporin A (2-5 mg/kg BW)<br />
was given. Finally, after one month of no response, we<br />
administered mycophenolate-mofetil when patient promptly<br />
entered partial remission of nephrotic syndrome. We<br />
concluded that MMF was found to be effective and beneficial<br />
drug in cases of resistant primary nephrotic syndrome.<br />
Key words: resistant nephrotic syndrome, mycophenolatemofetil<br />
Introduction<br />
down regulates the expression of cell-surface adhesion<br />
molecules, has been used successfully for the prevention of<br />
acute rejection of renal allografts (1,2). Preliminary studies<br />
suggest that it may also be effective in treatment of the<br />
resistant NS in the primary glomerulonephritis.<br />
Patients and methods<br />
We report data on two patients with NS who were diagnosed<br />
with primary glomerulonephritis. First patient, (male, 54-<br />
year old) was admitted to our hospital with a 1-month clinical<br />
and laboratory history of NS. He had nephrotic range<br />
proteinuria (mean proteinuria 8,5 g/24h) and stable serum<br />
creatinine level and creatinine clearance. Biopsy documented<br />
membranoproliferative glomerulonephritis by light<br />
microscopy and immunofluorescence was showed. After<br />
three months of standard steroid therapy (methylprednisolone<br />
1-2 mg/kg BW) he did not achieve remission. Because of that<br />
we continued the treatment with pulse doses of<br />
methylprednisolone, followed with cyclophosphamide pulses.<br />
During the following two years of therapy patient continued<br />
to have frequent relapses (proteinuria range 0,4-15 g/ 24h).<br />
Proven to be steroid and cyclophosphamide resistant he was<br />
shifted to MMF therapy (dose of 2g/day). The other patient<br />
(male, aged 62) was diagnosed with NS (membranous<br />
nephropathy) two months before admitting in our hospital<br />
(mean proteinuria of 10 g/24h) with stable serum creatinine<br />
level and halved creatinine clearance. Standard therapeutic<br />
procedure included pulse doses of methylprednisolone during<br />
one month and then cyclophosphamide per os (2 mg/kg BW)<br />
for one year but with no respond in decreasing of proteinuria.<br />
In order to achieve remission, Cyclosporin A (2-5 mg/kg<br />
BW) was given but with no response. Finally MMF was<br />
administered in standard dose of 2g/day along with<br />
Cyclosporine A. Both patients received steroids along with<br />
MMF (median dose was 20 mg/kg/day). Baseline evaluations<br />
on enrolment consisted of physical examination; serum<br />
albumin, serum cholesterol, and serum creatinine levels; and<br />
a 24-hour urine collection for protein and creatinine<br />
clearance. Patients were followed up for 6 months, and<br />
evaluated at 1- to 2-month intervals for these parameters. A<br />
partial remission was defined as at least a 50% reduction of<br />
proteinuria with a stable serum creatinine level (3). A<br />
complete remission was defined as proteinuria less than 0,3<br />
g/24 h with a stable serum creatinine level. Side effects of<br />
MMF were also observed.<br />
Patients with nephrotic syndrome (NS) in the primary<br />
glomerulonephritis are usually treated with standard<br />
immunosuppressive treatment including steroids and<br />
cyclophosphamide. However, a small proportion of patients<br />
run a multiply relapsing course despite treatment. Some go<br />
into remission with cyclosporine but are dependent on this<br />
drug, with which prolonged usage can lead to nephrotoxicity.<br />
Mycophenolate-mofetil (MMF) is a specific inhibitor of<br />
inosine monophosphate dehydrogenase which is involved in<br />
de novo purine synthesis. MMF, an immunosuppressive<br />
agent that preferentially inhibits stimulated lymphocytes and<br />
______________________<br />
Correspodence to: B. Milic, Clinic of Nephrology, Institute of Internal Diseases, Clinical Centre,<br />
Novi Sad, Serbia and Montenegro
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 84<br />
Results<br />
Both patients experienced remissions following MMF<br />
therapy. First patient, only one month after starting therapy,<br />
achieved complete remission (mean proteinuria 0,07 g/24h),<br />
with stable serum creatinine and increased serum albumin<br />
level, while the serum cholesterol levels were reduced<br />
significantly. Other patient promptly entered partial remission<br />
of NS (mean proteinuria 4 g/24 h), with stable serum<br />
creatinine and increased serum albumin level while serum<br />
cholesterol level decreased. There was no improvement in<br />
creatinine clearance level. In both cases, there was no side<br />
effect of MMF.<br />
Conclusions<br />
MMF is a relatively new immunosuppressive drug now being<br />
used in the prevention of allograft rejection. Preliminary<br />
studies have shown that MMF is effective in treatment in<br />
several types of primary glomerular diseases when<br />
conventional therapy has failed (4,5). In the majority of<br />
patients it was well tolerated and achieve the goals of<br />
improvement of nephrotic syndrome and stabilisation of renal<br />
function. Although being usually given with variable doses of<br />
steroid, results demonstrate that MMF has major steroidsparing<br />
effects and can be even effective as monotherapy. We<br />
concluded that MMF was found to be effective and beneficial<br />
drug in cases of resistant primary nephrotic syndrome.<br />
References<br />
1. Eugui EM, Mirkovitch A, Allison AC. Lymphocyte-selective<br />
antiproliferative and immunosuppressive effects of<br />
mycophenolic acid in mice. Scand J Immunol 1991; 33: 175-<br />
183<br />
2. Sintchak M, Fleming MA, Futer O et al. Structure and<br />
mechanisms of inosine monophosphate dehydrogenase in<br />
complex with the immunosuppressant mycophenolic acid. Cell<br />
1996; 85: 921-930<br />
3. Cattran DC, Greenwood C, Ritchie S, Bernstein K, Churchill<br />
DN, Clark WF, Morrin PA, Lavoie S. A controlled trial of<br />
cyclosporine in patients with progressive membranous<br />
nephropathy. Canadian Glomerulonephritis Study Group.<br />
Kidney Int 1995; 47:1130-1135<br />
4. Choi MJ, Eustace JA, Gimenez LF et al. Mycophenolate<br />
mofetil treatment for primary glomerular diseases. Kidney Int<br />
2002; 61: 1098-1114<br />
5. Badid C, Desmouliere A, Laville M. Mycophenolate<br />
implications for the treatment of glomerular disease. Nephrol<br />
Dial Transplant 2001; 16: 1752-1756
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 85<br />
Bacterial infections associated with double lumen central venous catheters<br />
M. S. Simin, M. Milosevic, S. Vodopivec, I. Mitic and S. Curic<br />
Institute for Internal diseases, Clinic for Nephrology and Clinical Immunology, Novi Sad, Serbia and Montenegro<br />
Abstract<br />
Central venous catheters were a major advance in end-stage<br />
renal disease patient care until the burden of catheter related<br />
complications became obvious.<br />
A retrospective study on infections complications of the<br />
double lumen catheterisation of central veins for<br />
haemodialysis and PD was done in 2004 year. In period from<br />
January to December 2004, 60 catheters were placed. 55<br />
patients had double lumen, one for plasmapheresis and 54 for<br />
haemodialysis. The mean duration of catheters remaining in<br />
situ was 36.67 days (range 7 - 145 days). There were 7<br />
double lumen catheters placed with coffs and tunelisation,<br />
and the other 48 patients had catheters of a short duration.<br />
Routine smears were taken from the top of catheters after<br />
extraction, and from the skin surrounding the place of<br />
catheter insertion. Hemocultures were also taken, and smears<br />
from periphery (smears from pharynx, nose and<br />
urinoculture). Reasons for placing catheters were acute renal<br />
failure in 19.65%, end stage renal disease in 35.71%, and<br />
complications of permanent vascular access in 44.64%.<br />
In 2|55 patients, Staphylococcus aureus and Enterococcus<br />
species were isolated from the top of dialysis catheter, after<br />
extraction, and without positive blood bacterial cultures. In a<br />
few patients micro-organisms were isolated from periphery<br />
on skin changes 2|55, urine 2|55, pharynx 1|55. Prophylaxis<br />
with antibiotics was administered in 18|55 patients, with<br />
antibiotics from group of cephalosporin and chinolone over<br />
next 7 to 14 days. Mortality during the period of observation<br />
was 7|55 patients.<br />
The conclusion based on the aforementioned parameters is<br />
that duration of placed catheters did not correlated with the<br />
frequency of infections. The respect of the surgical principles<br />
of asepsis and desinfection has contributed to a decreased<br />
frequency of catheter infections for dialysis.<br />
Key words: central venous catheter, bacterial infection,<br />
hemoculture, urinoculture<br />
Introduction<br />
Central venous catheters were a major advance in end-stage<br />
renal disease (ESRD) patient care until the burden of catheter<br />
related complications became obvious. Catheter-related<br />
infection is one of the major causes of morbidity, with<br />
potential lethal hazards in haemodialysis patients. Today, the<br />
incidence of bacteraemia ranges from 0, 5 to 13 per 1000<br />
patient - days with haemodialysis catheters (1). According to<br />
data from the last register of dialysis treatment and<br />
transplantation of kidneys in Serbia and Montenegro, an<br />
increase of hospitalised patients with vascular problems was<br />
noticed. More precisely, every fifth haemodialysis patient<br />
was hospitalised due to a vascular problems (A-V fistula<br />
thrombosis, malfunction, infection or moving from CAPD to<br />
HD) (2). Haemodialysis catheters are indicated in two types<br />
of situation: first, short term solution to permit creation,<br />
maturation or revision of arteriovenous fistula or graft,<br />
second, long term solution for patients with exhausted<br />
vascular access sites and with contraindications for<br />
arteriovenous access due to medical reasons such as heart<br />
failure, severe limb ischaemia or to provide comfort in<br />
elderly patients with poor prognosis. Today, an estimatation<br />
is that 13% of patients with end-stage renal disease are<br />
regularly treated with permanent or temporary central<br />
catheters. The catheter insertion site plays a significant role<br />
in the magnitude of the infectious risk. The femoral route is<br />
apparently less favourable then subclavian or jugular route,<br />
(1-3).<br />
Patients and methods<br />
A retrospective study of complications caused by infections<br />
of central venous catheters for haemodialysis was done in<br />
University Hospital in Novi Sad, Department of Nephrology<br />
in 2004. In the period from January to December 2004, 60<br />
catheters were placed. 55 patients had central venous<br />
catheter, one of them because of plasmapheresis and 54<br />
because of haemodialysis. The duration of catheter placement<br />
averaged 36,67 days (shortest 7 days, longest 145 days).<br />
There were 7 patients with long term cuffed tunnelled<br />
catheters and 49 patients had short duration catheters.<br />
Insertion site of short time catheters was: v. jugularis 28, v.<br />
subclavia 19, and v. femoralis 2. During the treatment 39<br />
patients had 1 catheter, in 2 patients 3 catheters were changed<br />
and in 1 patient 4 catheters were changed.<br />
Results<br />
Smears were taken from catheter tips after extraction, and<br />
from the skin surrounding catheter insertion place. Blood<br />
cultures and smears were also taken from periphery (smears<br />
from pharynx, nose and urinoculture). Indications for placing<br />
catheters were acute renal failure in 19.65%, ESRD in<br />
35.71%, and complications of permanent vascular access in<br />
44.64%. In 2/55 patients, Staphylococcus aureus and<br />
Enterococcus species were isolated, from catheter tips after<br />
extraction, but without positive blood cultures. In a few<br />
patients Staphylococcus aureus, Pseudomonas aeruginosa,<br />
Escherichia coli, and Klebsiella pneumoniae, were isolated<br />
from periphery (skin changes 2|55, urine 2|55, pharynx 1|55).<br />
______________________<br />
Correspodence to:<br />
M. S. Simin, Institut for Internal diseases, Clinic for Nephrology and Clinical Immunology,<br />
Novi Sad, Serbia and Montenegro
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 86<br />
Prophylaxis with antibiotics of cephalosporin and chinolone<br />
groups lasting 7 to 14 days was administered in 18 (32,2%)<br />
patients. 8/55 patients (14,5%) were treated with antibiotics<br />
according to antibiogram. 29 patients were left without<br />
antibiotic therapy. Mortality during this period of<br />
observation was 7|56 patients.<br />
Conclusions<br />
According to presented data, the conclusion is that duration<br />
of catheterisation period did not correlate with increase of the<br />
infection frequency. The number of patients dialysed with<br />
catheters is increased in the last few years, together with<br />
catheter related complications, especially bacteraemia, that<br />
became leading cause of morbidity and mortality. Obedience<br />
of surgical principles of asepsis and desinfection (sterile<br />
gloves, masks, galoshes, skin preparation for catheter<br />
insertion, appliance of desinfection means when<br />
disconnecting and connecting the catheters) evidently<br />
contribute to reduction of frequency of haemodialysis<br />
infections.<br />
References<br />
1. Bernard C. Haemodialysis catheter-related infection; time for<br />
action. Nephrol Dial Transplant 1999; 14: 2288-2290<br />
2. Radovic M, Nesic V. Godisnji izvestaj o lecenju dijalizama i<br />
transplantacijom bubrega u Srbiji i Crnoj Gori 2002 g.<br />
3. Hoen B, Paul-Dauphin A, Hestin D, Kessler M. Epibacdial: a<br />
multicenter prospective study of risk factor for bacteraemia in<br />
chronic hemodialysis patients. J Am Soc Nephrol 1998; 9(5):<br />
869-876<br />
4. Hung KY, Tsai TJ, Yen CJ, Yen TS. Infection associated with<br />
double-lumen catheterisation for temporary haemodialysis;<br />
experience of 168 cases. Nephrol Dial Transplant 1995; 10-<br />
247-251<br />
5. Tokaras JI, Miller ER, Alter MJ, ArudinoMJ, National<br />
surveillance of dialysis associated diseases in the UNITED<br />
states. 1995 ASAIO J 1998; 44(1): 98-107
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 87<br />
Early renal protocol biopsies: beneficial effects of treatment of borderline<br />
changes and subclinical rejections on the histological changes for chronic<br />
allograft nephropathy<br />
J. Masin-Spasovska 1 , N. Ivanovski 1 , S. Dzikova 1 , G. Petrusevska 2 , B. Dimova 2 , Lj. Lekovski 3 ,<br />
Z. Popov 3 and G. Spasovski 1<br />
1 Department of Nephrology, 2 Department of Pathology, 3 Department of Urology, Faculty of Medicine, Skopje,<br />
Republic of Macedonia<br />
Abstract<br />
Protocol biopsies in the early course after renal<br />
transplantation revealed that chronic allograft nephropathy<br />
(CAN) starts early. Our study aimed to identify borderline<br />
changes (BC), subclinical rejections (SR) and histological<br />
markers of chronic allograft nephropathy (CAN) in protocol<br />
biopsies at 1 and 6 months after living related kidney<br />
transplantation, and to determine whether treatment of BC<br />
and SR at the 1-month postransplant has a beneficial effect<br />
on graft histology and function at 6 months.<br />
Forty paired allograft biopsies were evaluated according to<br />
the Banff scoring schema.<br />
BC was found in 13/40 (32.5%) and 12/40 (30%), and SR in<br />
15/40 (37.5%) and 21/40 (52.2%) of patients, on 1 and 6-<br />
month biopsies, respectively. The mean HI (histological<br />
index/ sum of scores for acute/chronic changes) and CAN<br />
score (sum of histological markers for chronicity) increased<br />
significantly at 6-month biopsy 5.3±2.9 vs. 7.8±3.6 (p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 88<br />
Seron et al. reported a prevalence of CAN in about 42% of<br />
protocol biopsies at 3 months after transplantation (11,12).<br />
Recent reports provide evidence in favor of treating biopsyproven<br />
BC and SR, and that timely therapeutic intervention<br />
improves clinical outcomes, thereby preventing development<br />
of CAN. This raises the issue of early protocol biopsies of<br />
stable allografts and the clinically useful information they<br />
provide.<br />
Patients and methods<br />
The cohort of forty consecutive living related (LR) transplant<br />
patients with their first allograft received induction therapy<br />
with methylprednisolone (500 mg) and Daclizumab<br />
(Zenapax; 1 mg/kg BW at implantation and thereafter every 2<br />
weeks x five doses). The post-transplant standard triple<br />
immunosuppression therapy consisted of: cyclosporine<br />
(Neoral; 4 to 6 mg/kg/day) to reach target C2 levels (blood<br />
concentration 2 hours after administration of the drug),<br />
prednisolone (1 mg/kg/day tapered to 0.1 mg/kg/day after 4<br />
weeks) and mycophenolate mofetil (Cellcept 1 g bid.).<br />
During the first postoperative month patients with delayed<br />
graft function (DGF) who suffered post-transplant acute<br />
tubular necrosis or experienced a clinical episode of acute<br />
rejection (AR) were treated with hemodialysis or pulse<br />
corticosteroids, respectively, whenever an increase in serum<br />
creatinine >20% or decrease in urine output for 2 consecutive<br />
days was observed. These cases were included if their graft<br />
function had been stable (no change in serum creatinine ><br />
20%) for at least 2 weeks before the first biopsy. Patients<br />
with histology at 1 month biopsy of BC or AR type I or IIA<br />
and an increase in serum creatinine between 10 and 20 %<br />
from baseline (serum creatinine 2 weeks prior the biopsy)<br />
were assessed as SR and consequently treated with pulse<br />
corticoid therapy. The patients with histology of BC or AR<br />
followed by rise in serum creatinine < 10% from baseline<br />
were not treated.<br />
Protocol biopsies were performed using ultrasound-guided<br />
automated biopsy "gun". The formalin fixed biopsies were<br />
embedded in paraffin, serially sectioned at 3 to 5 µm<br />
thickness and stained with hematoxylin-eosin (HE), periodic<br />
acid-Schiff (PAS), Masson's trichrome as well as<br />
methenamine silver. Biopsies were considered adequate when<br />
they contained ≥7 glomeruli and at least one artery. The same<br />
pathologist blindly reviewed the renal lesions for evidence of<br />
acute and chronic changes by using descriptive morphologic<br />
criteria according to the Banff 97 scoring schema on a scale<br />
from 0 to 3 (13). CAN score was calculated as a sum of<br />
scores for the individual histological markers for chronicity:<br />
interstitial fibrosis, tubular atrophy, vascular fibrous intimal<br />
thickening, arterial hyalinosis and chronic glomerulopathy.<br />
The histological index (HI) was calculated as total sum of<br />
scores for acute and chronic changes.<br />
The clinical and biochemical data were recorded at<br />
the time of transplantation as well as at 1 and 6 months after<br />
transplantation. Results were expressed as mean values ± SD.<br />
An unpaired two-tailed Student t test was used to examine<br />
differences in mean values between the groups. Chi square<br />
analysis was used to compare the categorical variables.<br />
Results<br />
Donors and recipients mean age was 59.3 13 and 34.3 9.8<br />
years, respectively. Only 7.5% (6/80) of the biopsies showed<br />
no histopathological lesions. BC was found in 13/40 (32.5%)<br />
and 12/40 (30%), and SR in 15/40 (37.5%) and 21/40<br />
(52.2%) of patients, on 1 and 6 months biopsies, respectively.<br />
The mean HI and CAN score increased significantly at 6-<br />
month biopsy, 5.3 ± 2.9 vs. 7.8 ± 3.6 (p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 84<br />
first month after transplantation sCr was significantly higher<br />
in the group with high HI, 134 ± 35.9 vs.113 ± 27.5 (p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 90<br />
Table 4: Comparison of biochemical, clinical data and histological findings and scores at 1 and 6 months post-transplantation<br />
between the groups according to the treatment of borderline changes (BC) and subclinical rejections (SR)<br />
CLASSIFICATIONS MEAN SD MEAN SD P value<br />
1 month 6 months<br />
TREATMENT OF BC/SR Treatment (Tx) group Non-treatment (NTx)<br />
Number of patients (n = 9) (n = 19)<br />
sCr 1 month 130.56 33.09 122.26 29.24 n.s.<br />
sCr 6 months 151.44 38.36 136.11 44.23 n.s.<br />
Crcl 1 month 62.15 15.15 66.38 18.34 n.s.<br />
Crcl 6 months 58.11 21.50 63.35 18.31 n.s.<br />
DGF 1/9 (11.113%) 5/19 (26.32%) < 0.05<br />
AR (before 1 month biopsy) 1/9 (11.113%) 3/19 (15.79 %) n.s.<br />
AR 1 month / /<br />
BC 1 month 2/9 (22.22%) 11/19 (54.89%) < 0.05<br />
SR 1 month 7/9 (77.78%) 8/19 (42.11%) < 0.05<br />
BC 6 months 4/9 (44.44%) 5/19 (26.32%) < 0.05<br />
SR 6 months 4/9 (44.44%) 12/19 (63.16%) < 0.05<br />
HI 1 month 7.11 ± 1.90 4.95 ± 1.99 0.013<br />
HI 6 month 7.11 ± 2.32 8.16 ± 4.30 n.s.<br />
CAN score 1 month 2.33 ± 1.41 1.89 ± 1.37 n.s.<br />
CAN score 6 months 4.33 ± 1.73 8.16 ± 4.30 n.s.<br />
Discussion<br />
Chronic allograft nephropathy (CAN) causes most kidney<br />
allograft losses and despite improvements in<br />
immunosuppression, remains the central clinical challenge<br />
(14). In protocol biopsy studies, allograft damage is common,<br />
time-dependent, progressive and underestimated by<br />
measurement of serum creatinine. Rejection leads to<br />
allograft damage but the expression depends on its type,<br />
timing, severity and persistence. Subclinical rejection (SR) is<br />
defined as histologically-proven acute rejection without<br />
concurrent renal dysfunction (15), and is influenced by the<br />
time after transplantation, prior acute rejections, HLA<br />
mismatches, and immunosuppression (9,15). Untreated SR<br />
inflicts permanent tubulointerstitial damage and fibrosis (9).<br />
There is an evidence that protocol biopsy of stable renal<br />
allografts may be valuable tool to uncover early clinically<br />
invisible acute histological lesion, such as BC and SR (16).<br />
Previous reports show the prevalence of SR approximately in<br />
30-50% of protocol biopsies in the first 3 months after<br />
transplantation (9). The principal finding of our study is the<br />
histological evidence of BC and SR in relatively high<br />
percentage (33 and 38%) at first month, being even higher at<br />
6-month biopsies (30 and 52%), respectively. A comparable<br />
experience have been reported by Rush et al. (21 and 33-<br />
50%), and by Schweitzer et al. (23 and 33%), for the<br />
prevalence of BC and SR, respectively (4, 9, 17).<br />
Our study demonstrates that corticosteroid treatment of early<br />
BC and SR found at 1-month biopsies, is associated with<br />
improved histology of acute and chronic lesions at 6 months<br />
biopsies. Additionally, 4 patients in Tx group initially<br />
diagnosed as SR (classified as type IIA), showed an<br />
improvement in histology towards type I A, while 7 patients<br />
in NTx group diagnosed as BC at 1-month biopsies,<br />
worsened their histology towards SR type IA, at 6-month<br />
biopsies. Despite the progression of renal scarring in NTx<br />
group (significant increase of mean CAN and HI at 6-month<br />
biopsies), both groups presented with similar serum<br />
creatinine at the same time point. However, treatment of BC<br />
and SR did not result in improved allograft function at 6<br />
months. In contrast, Rush et al. reported that the treatment of<br />
early SR decreases chronic pathology (CAN), late clinical<br />
rejection episodes and improves long-term graft function (9).<br />
In addition, Shweitzer et al. reported a complete therapeutic<br />
response to steroid tretament in 58%, and Gaber et al. in<br />
100% of patients with BC (17,18).<br />
Conclusions<br />
A protocol 1-month biopsy may uncover a high prevalence of<br />
BC or SR in stable allografts. The presence of untreated BC<br />
or SR showed a greater susceptibility for histological acute<br />
and chronic deterioration on 6-month biopsy, accelerating the<br />
process of CAN. The beneficial effect of the treatment of<br />
BC/SR should be confirmed at follow-up of the graft function<br />
at 1 and 2 years.<br />
Our preliminary data support the hypothesis that treatment of<br />
the subclinical conditions (BC and SR) may counteract the<br />
development of CAN, aiming to provide a strong impetus to<br />
incorporate early allograft protocol biopsies into a standard<br />
clinical practice. Understanding the causes and the<br />
mechanisms of chronic allograft nephropathy may suggest<br />
targeted therapies to prevent the initiation or progression of<br />
CAN.<br />
References<br />
1. Paul LC. Chronic renal transplant loss. Kidney Int 1995; 47:<br />
1491-1499<br />
2. Isoniemi HM, Krogerus L, von Willebrand E, Taskienen E et<br />
al. Histological findings in well-functioning, long term renal<br />
allografts. Kidney Int 1992; 41: 155-160<br />
3. Rush DN, Henry SH, Jeffery JR, Schroeder TJ, Gough J.<br />
Histological findings in early routine biopsies of stable renal<br />
allograft recipients. Transplatation 1994; 57: 208-211<br />
4. Rush D, Nickerson P, Gough J et al. Beneficial effects of<br />
treatment of early subclinical rejection: a randomized study. J<br />
Am Soc Nephrol 1998; 9: 2129-2134<br />
5. Nickerson P, Jeffery JR, Gough J et al. Effect of increasing<br />
baseline immunosuppression on the prevalence of clinical and<br />
subclinical rejection: a pilot study. J Am Soc Nephrol 1999;<br />
10: 1801-1805<br />
6. Shapiro R, Randhawa P, Jordan M et al. An analysis of early<br />
renal transplant protocol biopsies- the high incidence of<br />
subclinical tubulitis. Am J Transpl 2001; 1: 47-50
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 91<br />
7. Morath C, Ritz E and Zeier M. Protocol biopsy: what is the<br />
rationale and what is the evidence? Nephrol Dial Transplant<br />
2003; 18: 644-647<br />
8. Rush D, Karpinski M, Nickerson P, Dancea S et al. Does<br />
subclinical rejection contribute to chronic rejection in renal<br />
transplant patients? Clin Transplant 1999; 13: 441-446<br />
9. Rush DN, Jeffery J, Trpkov K et al. Effect of subclinical<br />
rejection on renal allograft histology and function at 6 months.<br />
Transpl Proc 1996; 28: 494-495<br />
10. Shapiro R, Randhawa P, Jordan ML et al. An analysis of early<br />
renal transplant protocol biopsies-the high incidence of<br />
subclinical tubilitis. Am J Transplant 2001; 1: 47-50<br />
11. Nankivell BJ, Fenton-Lee CA, Kuypers DJ et al. Effect of<br />
histological damage on long-term kidney transplant outcome.<br />
Transplantation 2001; 71: 515-523<br />
12. Seron D, Moreso F, Bover J, Condom E et al. Early protocol<br />
renal allograft biopsies and graft outcome. Kidney Int 1997;<br />
51: 310-316<br />
13. Racusen LC, Solez K, Colvin RB et al. The Banff 97 working<br />
classification of renal allograft pathology. Kidney Int 1999; 55:<br />
713-723<br />
14. Meier-Kriesche HU, Schold JD, Kaplan B. Long-term renal<br />
allograft survival: have we made significant progress or is it<br />
time to rethink out analytic and therapeutic strategies? Am J<br />
Transplant 2004; 4: 1289-1295<br />
15. Kuypers DR, Chapman JR, O`Connell PJ et al. Predictors of<br />
renal transplant histology at three months. Transplantation<br />
1999; 75: 1222-1230<br />
16. Gough J, Rush D, Jeffery J et al. Reproducibility of the Banff<br />
schema in reporting protocol biopsies of stable renal allografts.<br />
Nephrol Dial Transplant 2002; 17: 1081-1084<br />
17. Schweitzer EJ, Drachenberg CB, Anderson L, Papadimerou<br />
HC et al. Significance of the Banff borderline biopsy. Am J<br />
Kidney Dis 1996; 28: 585-588<br />
18. Gaber LW, Moore LW, Alloway RR, Flax S, gaber AO.<br />
Correlation between Banff classification, acute renal rejection<br />
scores, and reversal of rejection. Transplant Proc 1995; 27:<br />
1019
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 92<br />
Factors associated with carotid and femoral atherosclerosis in non-diabetic<br />
hemodialysis patients<br />
S. Gelev, S. Dzikova, A. Sikole, Gj. Selim, P. Dzekova, V. Amitov and G. Spasovski<br />
Department of Nephrology, University of Skopje, Skopje, Republic of Macedonia<br />
Abstract<br />
Information on different stages of atherosclerotic changes has<br />
been obtained by combining information from B-mode<br />
ultrasonography recordings of the common carotid (CCA)<br />
and femoral arteries (FA). The aim of our study was to<br />
analyze the potential risk factors associated with different B-<br />
mode ultrasonography measurements on CCA and FA in<br />
non-diabetic hemodialysis (HD) patients.<br />
In a cross-sectional study we examined 67 non-diabetic,<br />
asymptomatic HD patients. All patients underwent high<br />
resolution B-mode ultrasonography of the CCA and FA. We<br />
compared the ultrasonographic findings in patients stratified<br />
according to various cut off levels for each clinical and<br />
biochemical parameter (mean value of one year laboratory<br />
data).<br />
The intima media thickness (IMT) exceeded the upper limit<br />
of normal range in 97.5% on CCA and in 100% of patients<br />
on FA. Atherosclerotic plaques (AP) were detected in 43.3<br />
and 55.2%, and were calcified in 20.9 and 13.4% of the<br />
patients on CCA and FA, respectively. An increased CCA-<br />
IMT was found in older patients (> 50 years and > 45 years at<br />
start of HD), with lower (< 1.2) kt/V, higher (> 1.5 mmol/L)<br />
phosphate and LDL (> 2,8 mmol/L) levels. An increased FA-<br />
IMT was only associated with HD duration > 72 months.<br />
Male gender, kt/V < 1.2, systolic blood pressure (SBP) > 150<br />
mmHg and pulse pressure (PP) > 70 mmHg were associated<br />
with increased CCA and FA internal diameter (ID). An<br />
increased CCA-ID was revealed in older patients (>50 years<br />
and > 45 years at the start of HD) and those with body mass<br />
index (BMI) > 23 kg/m 2 . Mean arterial pressure (MAP) ><br />
100 mmHg was associated with an increased FA-ID.<br />
Higher frequency of CCA and FA-AP were detected in older<br />
patients (> 50 years and > 45 years at start of HD), and higher<br />
total serum calcium (Ca) > 2,4 mmol/L. The finding of CCA-<br />
AP was associated with male gender and lower (< 150 pg/ml)<br />
serum intact parathyroid hormone (iPTH), while the presence<br />
of FA-AP was associated with higher (> 70 mmHg) PP and<br />
serum C-reactive protein (CRP) levels (> 3 mg/L). The<br />
gender, age (> 50 years and > 45 years at start of HD), PP ><br />
70 mmHg and iPTH < 150 pg/ml were associated with higher<br />
presence of calcified CCA and FA-AP. The calcified CCA<br />
and FA-AP were associated with lower (< 0.9 mmol/L) HDL<br />
and higher (> 3.5 mmol/L) Ca x phosphate product,<br />
respectively.<br />
The atherosclerotic changes on CCA and FA were frequently<br />
found in our cohort of asymptomatic, non-diabetic HD<br />
risk for cardiovascular disease. Age, gender, blood pressure,<br />
dialysis adequacy, bone markers and serum lipid disorders<br />
were associated with the atherosclerotic lesions in our<br />
patients. Timely management of the associated factors may<br />
be beneficial in preventing of atherosclerosis.<br />
Key words: dialysis, atherosclerosis, ultrasonography<br />
Introduction<br />
The association between uremia and increased risk of<br />
atherosclerotic disease has been documented in many<br />
investigations (1). Atherosclerotic damage of large arteries is<br />
major contributory factor to the high cardiovascular<br />
morbidity and mortality of hemodialysis (HD) patients (2).<br />
Since cardiovascular complications are a common cause of<br />
death in HD patients, the early detection and prevention of<br />
atherosclerosis are desirable. Arterial intima calcification<br />
represents an advanced stage of atherosclerosis and is<br />
associated with development of plaques and occlusive lesions<br />
(3). Moreover, the vascular calcification in advanced<br />
atherosclerosis is a common feature in HD patients (4).<br />
It is assumed that the atherosclerotic changes in carotid artery<br />
may reflect the general atherosclerosis (5). High resolution B-<br />
mode carotid ultrasonography is a fundamental technique for<br />
the noninvasive investigation of atherosclerosis in HD<br />
patients, combining the data from measurements of the<br />
carotid and femoral arteries (5,6). The investigation of the<br />
carotid artery with this technique is important not only for the<br />
assessment of its structural alterations but also because the<br />
extent of atherosclerosis of this vessel reflects the severity of<br />
arterial damage in other districts (6). Increased common<br />
carotid artery intima-media thickness (IMT) is a marker of<br />
early atherosclerosis (7).<br />
Traditional risk factors for atherosclerotic disease can not<br />
completely explain the excess of cardiovascular disease<br />
(CVD) in HD patients (5). Among a variety of<br />
pathophysiological conditions, age, gender, HD duration (5),<br />
hypertension (8,9), diabetes (10), chronic inflammation<br />
(11,12), malnutrition (13), abnormalities in lipid composition<br />
(14), serum calcium (Ca), hyperphosphatemia, calciumphosphorus<br />
product (Ca x P) (15-17) and intact parathyroid<br />
hormone (iPTH) concentrations (18), have been closely<br />
associated with atherosclerotic changes in HD populations.<br />
However, further information about the possible factors<br />
associated with atherosclerosis is needed in order to better<br />
prevent and control development of CVD.<br />
patients, implying the need for examination of this group at<br />
______________________<br />
Correspodence to: G. B. Spasovski, Department of Nephrology, University Clinical Center,<br />
Vodnjanska 17, 1000 Skopje, Macedonia; Telephone: + 389 70 268 232; Fax: + 389 2 3231 501;<br />
E-mail: gspas@sonet.com.mk
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 93<br />
The primary endpoint of present study was to analyze the<br />
association between B-mode ultrasonography findings in the<br />
carotid and femoral arteries and the possible risk factors for<br />
atherosclerosis in our non-diabetic HD population. Secondary<br />
endpoint was to assess the presence of atherosclerotic<br />
changes in the carotid and femoral arteries in our nondiabetic,<br />
asymptomatic HD patients.<br />
Patients and methods<br />
Patients<br />
In a cross-sectional study we examined 67 patients (at least<br />
12 months on HD), with no records and symptoms of CVD<br />
(19), infection or diabetes. The patients were dialyzed with<br />
low-flux synthetic membranes, bicarbonate dialysate (1,75<br />
mmol/l calcium), on erythropoietin therapy to maintain predialysis<br />
hemoglobin between 100 and 120 g/l, regular<br />
supplementation with iron, and calcium carbonate (CaCO 3 )<br />
use to maintain pre-dialysis serum phosphate levels < 1,8<br />
mmol/l. The duration of HD was individualized (4-5 hours,<br />
thrice weekly) to control body fluids and blood chemistries.<br />
Systolic (SBP) and diastolic blood pressure (DBP) was<br />
recorded monthly before HD, at the same day for blood<br />
sampling, and averaged for the last 12 months prior to the B-<br />
mode ultrasonography for statistical analysis. Brachial pulse<br />
pressure (PP) and mean arterial pressure (MAP) were<br />
calculated by the formula PP = SBP-DBP; MAP = DBP +<br />
(SBP-DBP) / 3. Body mass index (BMI), prescription for<br />
vitamin D (µg/weekly) and CaCO 3 (g of elemental Ca/day)<br />
prescribed to each patient were recorded from the patients'<br />
files. The demographic data on age at inclusion and start of<br />
HD, gender, HD duration, smoking, and dialysis adequacy<br />
were also recorded in the database.<br />
Blood chemistries<br />
Pre-dialysis hemoglobin, leukocyte, serum Ca, phosphate,<br />
albumin, triglycerids, total, HDL and LDL cholesterol and C-<br />
reactive protein (CRP) were determined once monthly.<br />
Serum iPTH and ferritin were measured every 4 months. The<br />
values of biochemical data considered in the study were<br />
averaged over the last 12 months preceding the B-mode<br />
ultrasonography measurements.<br />
Ultrasonography<br />
All patients underwent bilateral B-mode ultrasonography<br />
(Toshiba HDI 3000 with 7,5 MHz transducer) of the common<br />
carotid arteries (CCA) and femoral arteries (FA) for the<br />
evaluation of IMT, internal diameter (ID), atherosclerotic<br />
plaque (AP) detection and the presence of calcified AP. CCA<br />
measurements were made 2 cm beneath the bifurcation (20)<br />
and included approximately 4 cm of the CCA, and FA was<br />
examined approximately 4 cm below the inguinal ligament at<br />
the site where the artery divides into the superficial and the<br />
profound FA (5). IMT measurements were made on the far<br />
walls at the same level as the ID measurements (20). IMT<br />
was defined as the distance between the leading edge of the<br />
lumen-intima interface to the leading edge of the mediaadventitia<br />
interface of the far walls (5). Abnormal IMT is<br />
defined as IMT > 0,8 mm (6). A localized echo-structure<br />
encroaching into the vessel lumen was considered to be AP if<br />
the IMT was > 50% thicker than neighboring sites (20).<br />
Measurements of IMT and ID were always made in AP-free<br />
arterial segments (20).<br />
Statistical analysis<br />
Variables were expressed as frequencies, percentages for<br />
assessed factors and mean values ± SD for normally<br />
distributed continuous parameters.<br />
Patients were divided into 2 groups as a result of different cut<br />
off levels of each parametric variable and different code of<br />
nonparametric variables, respectively. Fifty years at<br />
inclusion, 45 years at the start of HD, 72 months HD<br />
duration, Kt/V ≥ 1.2, SBP ≥ 150mmHg, DBP ≥ 90mmHg,<br />
MAP ≥ 100mmHg, PP ≥ 70mmHg, BMI ≥ 23 kg/m2, CaCO 3<br />
≥ 3g Ca/day, hemoglobin ≥ 110g/L, leukocyte ≥ 6x10 9 /L,<br />
serum albumin ≤ 40 g/L, total serum Ca ≥ 2.4mmol/L, serum<br />
PO 4 ≥ 1.5mmol/L, Ca x P product ≥ 3.5mmol/L, iPTH ≥ 150<br />
pg/ml, TG ≥ 1.9 mmol/L, cholesterol ≥ 4.8mmol/L, HDL ≥<br />
0.9mmol/L, LDL ≥ 2.8mmol/L, ferritin ≥ 500mg/L and CRP<br />
≥ 3.0mg/L were determined for cut off values. Gender (0-<br />
male, 1-female), vitamin D treatment, smoking, AP detection<br />
and presence of calcified AP (0-no, 1-yes) were used as<br />
categorical variables. Ultrasonography findings (IMT, ID,<br />
plaque detection and presence of calcified plaques) were<br />
compared among the groups.<br />
Statistical comparison between the groups was performed<br />
with Student t-test for continuous variables, and chi-square<br />
analysis for the categorical variables.<br />
Statistical analysis was performed with standard statistical<br />
package (SPSS for Windows version 9.0). For all<br />
comparisons, a P-value < 0.05 was considered statistically<br />
significant.<br />
Results<br />
This is the first study performed in our dialysis patients using<br />
high-resolution B-mode ultrasound for evaluation of the<br />
atherosclerotic changes in CCA and FA.<br />
The intima media thickness (IMT) exceeded the upper limit<br />
of normal range in 66 (97.5%) on CCA and in 100% of<br />
patients on FA. Atherosclerotic plaques (AP) were detected<br />
in 29 (43.3) and 37 (55.2%), and were calcified in 14 (20.9)<br />
and 9 (13.4%) of the patients on CCA and FA, respectively.<br />
Ultrasonographic findings on CCA and FA of the whole<br />
study group are presented in Table 1.<br />
Table 1. Ultrasonograpic characteristics of all patients<br />
CCA-IMT (mm) 1.46±0.29 FA-IMT (mm) 1.43±0.23<br />
frequency of CCA-AP (%) 43,28 Frequency of FA-AP (%) 55.22<br />
Freq. of calcified CCA-AP (%) 20.9 freq. of calcified FA-AP (%) 13.43<br />
CCA-ID (mm) 7.36±0.99 FA-ID (mm) 7.43±1.05<br />
Age: When divided according to age (>50< years) the older<br />
patients (n=37) had mean age of 60.9±7.2 years (range 51-74)<br />
as compared with 41.4±6.3 years (range 26-49) in the<br />
younger group, while patients (> 45 years) at start of HD
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 84<br />
(n=35) had mean age of 55.3±7.0 years (range 45-67) as<br />
compared with 33.7±7.7 years (range 19-44) in the younger<br />
patients. Both older groups of patients showed significantly<br />
increased CCA-IMT, CCA-ID, higher frequency of CCA and<br />
FA-AP, calcified CCA and FA-AP (the last being at<br />
borderline of significance for age at start of HD) (Table 2).<br />
Table 2. Ultrasonograpic characteristics of patients divided according to age (>50< years)<br />
age at inclusion > 50 years < 50 years P<br />
CCA-IMT (mm) 1.53±0.27 1.37±0.29 0.02<br />
CCA-ID (mm) 7.62±1.02 7.04±0.88 0.01<br />
frequency of CCA-AP (%) 22/37 (59.46) 7/30 (23.33) 0.000<br />
freq. of calcified CCA-AP (%) 13/37 (35.13) 1/30 (3.33) 0.000<br />
frequency of FA-AP (%) 25/37 (67.57) 12/30 (40.0) 0.03<br />
freq. of calcified FA-AP (%) 8/37 (21.62) 1/30 (3.33) 0.04<br />
age at start of HD 45 years < 45 years P<br />
CCA-IMT (mm) 1.55±0.27 1.37±0.28 0.009<br />
CCA-ID (mm) 7.68±1.01 7.01±0.87 0.005<br />
frequency of CCA-AP (%) 20/35 (57.14) 9/32 (28.12) 0.001<br />
freq. of calcified CCA-AP (%) 13/35 (37.14) 1/32 (3.12) 0.000<br />
frequency of FA-AP (%) 23/35 (65.71) 14/32 (43.75) 0.04<br />
freq. of calcified FA-AP (%) 7/35 (20.0) 2/32 (6.25) 0.07<br />
Gender: Male patients (n=43) had significantly increased<br />
CCA-ID, FA-ID, higher frequency of CCA-AP, calcified<br />
CCA-AP and calcified FA-AP when compared with female<br />
patients (n=24) (Table 3).<br />
Table 3. Ultrasonograpic characteristics of patients divided according to the gender<br />
Gender Male Female P<br />
CCA-ID (mm) 7.60±0.96 6.92±0.93 0.006<br />
FA-ID (mm) 7.84±0.98 6.69±0.72 0.000<br />
frequency of CCA-AP (%) 24/43 (55.81) 5/24 (20.83) 0.005<br />
freq. of calcified CCA-AP (%) 12/43 (27.91) 2/24 (8.33) 0.04<br />
freq. of calcified FA-AP (%) 9/43 (20.93) 0/24 (0.0) 0.02<br />
Dialysis adequacy and HD duration: CCA-IMT, CCA-ID and<br />
FA-ID were significantly lower in patients (n=37) with<br />
higher (> 1.2) kt/V (mean 1.37±0.14, range 1.21-1.76) as<br />
compared to the patients with kt/V 1.2 (mean 1.08±0.1,<br />
range 0.81-1.2). Patients (n=33) with longer (> 72 months)<br />
HD treatment (mean 130±47, range 72-236) in comparison<br />
with patients being shorter on HD (mean 47±15, range 14-68)<br />
showed significantly increased FA-IMT (Table 4).<br />
Table 4. Ultrasonograpic characteristics of patients according to dialysis adequacy and HD duration<br />
dialysis adequacy kt/V 1.2 kt/V > 1.2 P<br />
CCA-IMT (mm) 1.54±0.26 1.39±0.29 0.03<br />
CCA-ID (mm) 7.74±0.87 7.04±0.99 0.003<br />
FA-ID (mm) 7.91±0.96 7.05±0.97 0.000<br />
HD duration 72 months < 72 months P<br />
FA-IMT (mm) 1.49±0.19 1.37±0.24 0.028<br />
Blood pressure: The patients (n=33) with higher<br />
(150mmHg) SBP (mean 162±11, range 151-190) presented<br />
with significantly increased CCA and FA-ID as compared<br />
with patients with lower SBP (mean 124±14, range 91-145).<br />
Significantly higher FA-ID<br />
Table 5. Ultrasonograpic characteristics of patients divided according to the blood pressure<br />
SBP 150 mmHg < 150 mmHg P<br />
CCA-ID (mm) 7.60±1.03 7.12±0.92 0.049<br />
FA-ID (mm) 7.74±1.06 7.13±0.96 0.01<br />
MAP > 100 mmHg < 100 mmHg P<br />
FA-ID (mm) 7.69±1.08 7.18±0.98 0.049<br />
PP 70 mmHg < 70 mmHg P<br />
CCA-ID (mm) 7.65±0.92 7.19±1.01 0.06<br />
freq. of calcified CCA-AP (%) 8/24 (33.33) 6/43 (13.95) 0.018<br />
FA-ID (mm) 7.85±0.98 7.19±1.03 0.012<br />
frequency of FA-AP (%) 18/24 (75.0) 19/43 (44.19) 0.016<br />
freq. of calcified FA-AP (%) 6/24 (25.0) 3/43 (6.98) 0.028
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 83<br />
measurements were found in patients (n=33) with MAP ><br />
100mmHg (mean 115±7, range 103-130) as compared with<br />
those with lower MAP (mean 89±9, range 63-100). Patients<br />
(n=24) with higher ( 70 mmHg) PP (mean 77±8, range 70-<br />
100) tended to have increased CCA-ID, while FA-ID, FA-<br />
AP, calcified CCA and FA-AP were significantly higher<br />
when compared to the patients with lower PP (mean 52±9,<br />
range 31-61) (Table 5).<br />
BMI: Significantly higher CCA-ID was shown in patients<br />
(n=33) with an increased (> 23 kg/m 2 ) BMI (mean 27.1±3.5,<br />
range 23.0-35.7) as compared with patients having lower<br />
BMI (mean 20.5±1.5, range 16.4-22.7) (Table 6).<br />
Table 6. Ultrasonograpic characteristics of patients divided according to BMI<br />
BMI > 23 kg/m 2 < 23 kg/m 2 P<br />
CCA-ID (mm) 7.69±1.11 7.17±1.11 0.04<br />
Bone mineral metabolism parameters: Patients (n=31) with<br />
an increased ( 2.4 mmol/L) serum Ca (mean 2.49±0.08,<br />
range 2.4-2.8) had significantly higher frequency of CCA-AP<br />
and FA-AP being at borderline of significance in comparison<br />
with patients with lower Ca (mean 2.25±0.12, range 1.84-<br />
2.39). CCA-IMT was significantly increased in patients<br />
(n=34) with serum phosphate 1.5 mmol/L (mean 1.8±0.22,<br />
range 1.5-2.32) when compared with patients with lower<br />
phosphate levels (mean 1.23±0.18, range 0.86-1.47).<br />
Calcified FA-AP tended to be more frequent in patients<br />
(n=35) with serum Ca x P > 3.5 mmol/L (mean 4.27±0.62,<br />
range 3.51-5.84) as compared with patients with lower Ca x P<br />
product (mean 2.89±0.49, range 1.71-3.46). Patients (n=36)<br />
with lower serum iPTH < 150 pg/ml (mean 64.5±33.2, range<br />
11.5-140) showed significantly higher frequency of CCA-AP,<br />
calcified CCA and FA-AP in comparison with patients with<br />
higher iPTH (mean 298.1±130, range 150-599) (Table 7).<br />
Table 7. Ultrasonograpic characteristics of patients divided according to the bone mineral metabolism parameters<br />
total serum Ca 2.4 mmol/L < 2.4 mmol/L P<br />
frequency of CCA-AP (%) 16/31 (51.62) 10/36 (27.78) 0.04<br />
frequency of FA-AP (%) 21/31 (67.74) 16/36 (44.44) 0.07<br />
serum phosphate 1.5 mmol/L < 1.5 mmol/L P<br />
CCA-IMT (mm) 1.53±0.29 1.39±0.27 0.04<br />
Ca x P product > 3.5 mmol/L < 3.5 mmol/L P<br />
freq. of calcified FA-AP (%) 7/35 (20.0) 2/32 (6.25) 0.06<br />
serum iPTH > 150 pg/ml < 150 pg/ml P<br />
frequency of CCA-AP (%) 11/31 (35.48) 18/36 (50.0) 0.05<br />
freq. of calcified CCA-AP (%) 2/31 (6.45) 12/36 (33.33) 0.019<br />
frequency of calcified FA-AP (%) 1/31 (3.23) 8/36 (22.22) 0.03<br />
Serum HDL and LDL cholesterol: Significantly lower<br />
frequency of calcified CCA-AP was observed in patients<br />
(n=36) with higher (> 0.9mmol/L) HDL cholesterol (mean<br />
1.17±0.25, range 0.92-1.94) as compared with patients lower<br />
HDL (mean 0.77±0.08, range 0.57-0.88); while significantly<br />
increased CCA-IMT was found in patients (n=33) with<br />
higher ( 2.8mmol/L) serum LDL cholesterol (mean<br />
3.42±0.57, range 2.8-4.92) in comparison with patients with<br />
lower LDL (mean 2.11±0.38, range 1.43-2.77) (Table 8).<br />
Table 8. Ultrasonograpic characteristics of patients divided according to the lipid parameters<br />
serum HDL cholesterol < 0.9 mmol/L > 0.9 mmol/L P<br />
frequency of calcified CCA-AP (%) 11/31 (35.48) 3/36 (8.33) 0.04<br />
serum LDL cholesterol 2.8 mmol/L < 2.8 mmol/L P<br />
CCA-IMT (mm) 1.56±0.34 1.39±0.32 0.04<br />
Serum CRP: Patients (n=33) with low ( 3.0 mg/L) serum<br />
CRP (mean 1.63±0.84, range 0.25-3.0) had significantly<br />
lower frequency of calcified FA-AP as compared with<br />
patients with high CRP (mean 7.02±4.89, range 3.07-30.0)<br />
(Table 9).<br />
Table 9. Ultrasonograpic characteristics of patients divided according to CRP levels<br />
serum CRP > 3 mg/L 3.0 mg/L P<br />
frequency of FA-AP (%) 19/34 ( 55.88 ) 10/33 ( 30.3 ) 0.03<br />
Other variables: When divided according to various cut off<br />
levels of parameters like DBP, daily dose of CaCO 3, blood<br />
hemoglobin and leukocyte, serum albumin, ferritin,<br />
triglycerides and total cholesterol, there was no significant<br />
difference between the groups of patients, neither for<br />
comparison of the use of vitamin D or smoking.<br />
Discussion<br />
The results of this study confirm that atherosclerotic changes<br />
on CCA and FA in asymptomatic, non-diabetic HD patients<br />
are rather frequent, implying the need for examination of
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 96<br />
systemic atherosclerosis in HD patients even they are free of<br />
symptoms. Moreover, the higher risk of cardiovascular<br />
mortality was reported to be associated with IMT of CCA<br />
obtained by ultrasonographic measurement (6). The present<br />
data has confirmed previous reports that age, gender, blood<br />
pressure, dialysis adequacy, bone mineral markers and serum<br />
HDL/LDL cholesterol disorders in HD patients are<br />
predominantly associated with their atherosclerotic lesions<br />
(8,9,14-17).<br />
Increased CCA-IMT in our patients was associated with<br />
traditional risk factors such as older (> 50 years) age at<br />
inclusion, and (> 45 years) at start of HD, worse dialysis<br />
adequacy (kt/V levels < 1.2), higher (> 1.5 mmol/L)<br />
phosphate and LDL (> 2.8 mmol/L) levels. In many studies<br />
no relationship was found between CCA and FA-IMT and<br />
the duration of HD (5). However, we found that increased<br />
FA-IMT was associated with longer (> 72 months) HD<br />
duration, although for better explanation we need a further<br />
statistical evaluation with multiple regression analysis. Male<br />
gender, lower kt/V (< 1.2), higher (> 150 mmHg) SBP and<br />
PP (> 70 mmHg) were associated with increased CCA and<br />
FA-ID. Increased CCA-ID was also associated with an older<br />
age at inclusion and at start of HD, and increased (> 23<br />
kg/m 2 ) BMI. Higher (> 100 mmHg) MAP was also<br />
associated with an increased FA-ID.<br />
Higher frequency of CCA and FA-AP in our patients was<br />
associated with an older age at inclusion and at start of HD,<br />
as well as an increased total serum Ca levels (> 2.4 mmol/L).<br />
The last could be possibly explained by the high (1.75<br />
mmol/L) concentration of calcium in the dialysis fluid, and<br />
calcium influx during each of the sessions. In addition, a<br />
higher frequency of CCA-AP was also associated with male<br />
gender and lower (< 150 pg/ml) iPTH, and a higher presence<br />
of FA-AP was found in patients with higher (> 70 mmHg) PP<br />
and serum CRP levels (> 3 mg/L). Calcified CCA and FA-<br />
AP were most frequently observed in males, older patients,<br />
with higher PP and lower iPTH levels. A recent<br />
epidemiological survey on bone markers in our HD<br />
population has shown adynamic bone disease (ABD) as most<br />
frequent renal bone disease (21). It was concluded that the<br />
use of high (1.75 mM) dialysate Ca concentration, calcium<br />
carbonate and vitamin D treatment might be associated with<br />
development of ABD. Hence, the over-suppression of PTH<br />
and ABD as predominant type of renal osteodystrophy<br />
(ROD) contribute to high levels of calcium and phosphorus<br />
in the blood, which are strongly associated with<br />
cardiovascular disease, a major cause of mortality and<br />
morbidity (22). This is also in line with our study data that<br />
higher presence of calcified CCA and FA-AP was associated<br />
with lower HDL and an increased Ca x P product,<br />
respectively.<br />
DBP, serum albumin, ferritin, triglycerides, cholesterol and<br />
the amount of ingested CaCO 3, vitamin D intake and smoking<br />
did not show significant associations with CCA and FA<br />
ultrasonographic findings in our patients. Here, the possible<br />
explanation could be a regular supplementation with<br />
parenteral iron therapy if needed, prescription of<br />
hypolipemics upon strict indication and precautious treatment<br />
with CaCO 3 and vitamin D.<br />
In line with the previous reports that IMT is a strong<br />
predictor for cardiovascular events in the HD population (23),<br />
and that CCA-ID, but not CCA-IMT predict overall mortality<br />
and cardiovascular outcomes in HD patients (6), we need<br />
further keep trying to get under control the atherogenic<br />
factors like disorders of mineral metabolism (abnormalities in<br />
plasma Ca, phosphorus and iPTH concentration), blood<br />
pressure, HDL/LDL cholesterol, inflammation (CRP), and to<br />
improve the dialysis adequacy. The case if we can't establish<br />
any association between ultrasonographic findings and other<br />
atherogenic factors do not release us to keep up controlling<br />
further nutritional and inflammation markers, serum<br />
triglycerides and cholesterol, and the amount of ingested Ca<br />
from CaCO 3, vitamin D intake and smoking.<br />
Conclusions<br />
The measurement of IMT on CCA and FA in the present<br />
study demonstrated that atherosclerosis in asymptomatic nondiabetic<br />
HD patients is frequent. Our results suggest a few<br />
emerging risk factors for atherosclerosis such as older age,<br />
male gender, impaired dialysis adequacy, longer HD<br />
duration, increased BMI, SBP, MAP and PP, increased serum<br />
Ca, phosphate and Ca x P product, lower iPTH and HDL and<br />
higher LDL. We need to examine atherosclerotic conditions<br />
of CCA and FA in HD patients even if they are<br />
asymptomatic. The management of these associated factors<br />
may be beneficial in preventing of atherosclerosis and CVD<br />
development in this population at risk.<br />
References<br />
1. Ma KW, Greene EL, Raij L. Cardiovascular risk factors<br />
in chronic renal failure and hemodialysis populations.<br />
Am J Kidney Dis 1992; (19): 505-513<br />
2. US Renal Data system. USRDS Annual report. Am J<br />
Kidney Dis 1998; 32 (Suppl 1): S81-S88<br />
3. London GM, Guerin AP, Marchais SJ, Metivier F,<br />
Pannier B, Adda H. Arterial media calcification in endstage<br />
renal disease: impact on all-cause and<br />
cardiovascular mortality. Nephrol Dial Transplant 2003;<br />
18: 1731-1740<br />
4. Guerin AP, London GM, Marchais SJ, Metivier F.<br />
Arterial stiffening and vascular calcifications in endstage<br />
renal disease. Nephrol Dial Transplant 2000; 15:<br />
1014-1021<br />
5. Kawagishi T, Nishizawa Y, Konishi T, Kawasaki K,<br />
Emoto M, Shoji T, Tabata T, Inoue T, Morii H. Highresolution<br />
B-mode ultrasonography in evaluation of<br />
atherosclerosis in uremia. Kidney Int 1995; 48 (3): 820-<br />
826<br />
6. Benedetto FA, Mallamaci F, Tripepi G, Zoccali C.<br />
Prognostic Value of Ultrasonographic Measurement of<br />
Carotid Intima Media Thickness in Dialysis patients. J<br />
Am Soc Nephrol 2001; 12: 2458-2464<br />
7. Drueke T, Witko-Sarsat V, Massy Z, Descamps-Latscha<br />
B, Guerin AP, Marchais SJ, Gausson V, London GM.<br />
Iron therapy, advanced oxidation protein products, and<br />
carotid artery intima-media thickness in end-stage renal<br />
disease. Circulation 2002; 106 (17): 2212-2217<br />
8. Mailloux LU, Haley WE. Hypertension in ESRD<br />
patients: pathophysiology, therapy, outcomes, and future<br />
directions. Am J Kidney Dis 1998; 32: 705-719<br />
9. Tozava M, Iseki C, Takishita S. Pulse pressure and risk<br />
of total mortality and cardiovascular events in patients<br />
on chronic hemodijalysis. Kidney Int 2002; 61: 717-726.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 97<br />
10. Krane V, Wanner Ch. The metabolic burden of diabetes<br />
and dyslipidaemia in chronic kidney disease. Nephrol<br />
Dial Transplant 2002; 17(Suppl.11): 23-27<br />
11. Wanner Ch, Zimmermann J, Schwedler S, Metzger T.<br />
Inflammation and cardiovasular risk in dialysis patients.<br />
Kidney Int 2002; 61(Suppl.80): S99-S102<br />
12. Brancaccio D, Tetta C, Gallieni M, Panichi V.<br />
Inflammation, CRP, calcium overload and high calciumphosphate<br />
product: a ‘liaison dangereuse’. Nephrol Dial<br />
Transplant 2002; 17: 201-203<br />
13. Marcen R, Teruel JL, de la Cal MA, Gamez C. The<br />
impact of malnutrition in morbidity and mortality in<br />
stable hemodialysis patients. Nephrol Dial Transplant<br />
1997; 12: 2324-2331<br />
14. Quaschning T, Krane V, Metzger T, Wanner Ch.<br />
Abnormalities in Uremic Lipoprotein Metabolism and<br />
Its Impact on Cardiovascular Disease. Am J Kidney Dis<br />
2001; 38(Suppl.1): S14-S19<br />
15. Block GA, Hulbert-Shearon TE, Levin NW, Port FK.<br />
Association of serum phosphorus and calcium x<br />
phosphate product with mortality risk in chronic<br />
hemodialysis patients: a national study. Am J Kidney Dis<br />
1998; 31: 607-617<br />
16. Rostand SG, Drueke TB. Parathyroid hormone, vitamin<br />
D, and cardiovascular disease in chronic renal failure.<br />
Kidney Int 1999; 56: 383-392<br />
17. Fournier A. CaCO3 dose and risk of arterial<br />
calcification. Nephrol Dial Transplant 2001; 16: 1075-<br />
1076<br />
18. Yamauchi T, Kuno T, Takada H, Nagura Y, Kanmatsuse<br />
K, Takahashi S. The impact of visceral fat on multiple<br />
risk factors and carotid atherosclerosis an chronic<br />
haemodialysis patients. Nephrol Dial Transplant 2003;<br />
18: 1842-1847<br />
19. Savage T, Clarke AL, Giles M, Tomson CRV, Raine<br />
AEG. Calcified plaque is common in the carotid and<br />
femoral arteries of dialysis patients without clinical<br />
vascular disease. Nephrol Dial Transplant 1998; 13:<br />
2004-2012<br />
20. London GM, Guerin AP, Marchhias SJ, et al. Cardiac<br />
and arterial interactions an end-stage renal disease.<br />
Kidney Int 1996; 50: 600-608<br />
21. Spasovski G, Gelev S, Zdravkovska V, Tomanovski V,<br />
Trpenovski L, Ivanovski K, Bajraktarova T, Janakievska<br />
P, Damjanovski M, Neskovski J, Karceva-Sarajlia E,<br />
Petrovska T, Filkovska K, Matovic S, Luseva V,<br />
Jordanovski D, Zafirovska M. Epidemiology of renal<br />
osteodystrophy in R. Macedonia. Bantao <strong>Journal</strong> 2005;<br />
3(2): 160-161<br />
22. Goodman WG, Goldin J, Kuizon BD. Coronary-artery<br />
calcification in young adults with end-stage renal<br />
disease who are undergoing dialysis. N Engl J Med<br />
2000; 342: 1478-1483<br />
23. Ekart R, Hojs R, Hojs-Fabjan T, Balon BP. Predictive<br />
value of carotid intima media thickness in hemodialysis<br />
patients. Artif Organs 2005; 29 (8): 615-619
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 98<br />
Acid-base disorders in patients with hypoproteinemia<br />
P. Mavromatidou 1 , N. Sotirakopoulos 2 , T. Tsitsios 2 , I. Skandalos 3 , M. Peiou 2 , and K. Mavromatidis 2<br />
1 Evosmos, Thessaloniki, 2 Renal Unit of Gen. Hosp. of Komotini, 3 Second Surgical Department, Gen. Hosp. Papageorgiou,<br />
Thessaloniki, Greece<br />
Abstract<br />
Hypoproteinemia is a common disturbance in patients<br />
suffering from various diseases. It can be accompanied by<br />
hypovolemia and hypotension that influences the volume<br />
space of drugs in the body as well as the acid-base balance.<br />
In the present study, 22 patients with hypoproteinemia (8F,<br />
14M) constituted group A. In this group the acid-base<br />
disorders as well as their importance were evaluated. From<br />
group A, 10 patients suffered from nephrotic syndrome,<br />
while 17/22 from chronic renal failure (CRF). The level of<br />
serum proteins varied from 46 gr/L to 64 gr/L, while the<br />
levels of albumin ranged from 13 to 32 gr/L. Furthermore, 15<br />
normal individuals were used as controls (group B) aging<br />
from 24 to 72 years old with normal levels of serum proteins.<br />
The results suggested that in group A, 21/22 patients had<br />
acid-base disorders. Moreover, 11/22 patients had a mixed<br />
disturbance (metabolic alkalosis combined with respiratory<br />
alkalosis). Only 4/22 patients had metabolic alkalosis, 4/22<br />
had metabolic acidosis (mixed) and 2/22 respiratory<br />
alkalosis. In particular, the blood’s pH appeared to be slightly<br />
alkaline.<br />
In group A the patients’ anion gap ranged from 5,7 to 18,5<br />
mmol/L. Based on this fact, group A patients were divided in<br />
two sub-groups. The first one (sub-group A1) consisted of 12<br />
patients measuring an anion gap higher than 10 mmol/L,<br />
while the second group (sub-group A2) consisted of 10<br />
patients with an anion gap lower than 10 mmol/L. The<br />
comparison of the pH between the two sub-groups suggested<br />
that A1 had respiratory alkalosis, while A2 had metabolic<br />
alkalosis.<br />
It can be concluded, that patients with hypoproteinemia<br />
appear to have disturbances of acid-base balance (mainly<br />
metabolic alkalosis), because of the reduction in serum<br />
proteins, which improves the pH levels in patients with CRF.<br />
The second most common acid-base disorder that appears in<br />
hypoproteinemic patients is respiratory alkalosis.<br />
Key words: hypoproteinemia, acid-base disorders, metabolic<br />
alkalosis, respiratory alkalosis, anion gap<br />
Introduction<br />
The electrochemical balance that exists in the body’s fluid<br />
compartments (also in plasma) suggests that the anions are<br />
equal to the cations. Nevertheless, it is not possible, in routine<br />
blood tests, to estimate most of the anions (non-counted<br />
anions) in comparison to the cations. For this reason, an<br />
anion gap appears which is expressed by a number that<br />
represents the non-counted negative ions (which, when added<br />
to the negatives’ ions sum, result to a number that is a equal<br />
to the positives ions sum).<br />
The anions, that are included usually to the anion gap, are<br />
serum proteins as well as organic acid, phosphate and sulfate<br />
ions (1). The acidosis with normal anion gap is caused by<br />
either bicarbonate loss or addition of chloride salts to the<br />
body. Greater than normal anion gap suggests the presence of<br />
retained acid anions other than chloride.<br />
The anion gap is actually low in the conditions stated, where<br />
an increase to the non-counted cations is present (acute<br />
toxicity from lithium, paraproteinemias-such as multiple<br />
myeloma, because of their positive charge-hypercalcaemia,<br />
hypermagnesemia). Extremely low anion gap occurs because<br />
of the reduction of the counted anions in hypoproteinemia<br />
and, in addition, in this case the anion gap is technically<br />
reduced (1). Understanding the anion gap in the above<br />
situations is very important since all these are life-threatening<br />
(2).<br />
The protein contributes to the anion gap approximately 2-2,8<br />
mmol/L for every 10 gr/L protein that exists in the serum (3).<br />
Since the human proteins are non-volative acids, their<br />
increase causes acidosis and their reduction causes alkalosis<br />
(4,5) and for this reason their estimation is necessary for the<br />
evaluation of the patients’ acid-base balance. In conclusion, it<br />
is estimated that normally about 8 mmol/L of the anion gap is<br />
due to serum proteins (2x4=8) and this is the reason<br />
responsible for the reduction of the anion gap in<br />
hypoproteinemia. In the present study the influence of<br />
hypoproteinemia in the acid-base balance of patients was<br />
evaluated.<br />
Patients and methods<br />
In the study were included patients with hypoproteinemia<br />
(serum albumin10 mmol/L) as well as those with hyperlipidemia<br />
(serum total cholesterol>3,4 mmol/L or triglycerides>3,4<br />
mmol/L). Furthermore, patients with hypernatremia,<br />
hypomagnesemia, hyperkalemia, paraproteinemia and<br />
bromism were excluded. Patients who received diuretics were<br />
also excluded. The study included 22 patients (8F, 14M),<br />
aging from 37 to 88 years old (median=63 years old). The<br />
control group (group B), consisted of 15 healthy individuals<br />
______________________<br />
Correspodence to:<br />
K. Mavromatidis, Ant. Rossidi 11 – 69100 , N. Mosinoupoli, Komotini – Greece;<br />
Tel. (+30) 25310 57149; Fax (+30) 25310 30706; E-mail: mavromatidis_k@yahoo.com
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 99<br />
(7F, 8M), aging from 24 to 72 years old (median =40 years<br />
old) with normal levels of serum proteins.<br />
Blood for the gas determination was taken from the radical<br />
artery, while for the determination of serum electrolytes was<br />
taken from a peripheral vein. Blood gases were determined as<br />
well as haematocrite, creatinine and serum electrolytes<br />
(potassium, sodium, calcium, chloride), while the anion gap<br />
was calculated by using the formula: anion gap= (sodium) –<br />
(chloride + bicarbonate). The cause responsible for<br />
hypoproteinemia was marked as well as the presence or<br />
absence of nephrotic syndrome.<br />
The existence or not of hypovolemia in our patients was<br />
estimated based on medical history, clinical findings (arterial<br />
pressure in sitting and trendelenburg position, pulse wave,<br />
jugular vein condition) and laboratory findings (proportional<br />
increase of ratio Na + /CI - ). The diagnosis of acid-base<br />
disorders was based on medical history, clinical findings,<br />
blood gases, serum electrolytes and lactates, urine<br />
examination and serum anion gap.<br />
Serum electrolyte levels were determined by the use of an<br />
iontoepilectic analyzer (Dimension A.R., Acsess, USA) and<br />
blood gases were determined by the use of an automatic<br />
analyzer (GemPrimer 3000, USA). The statistical analysis<br />
was carried out by an unpaired student t-test. Changes with a<br />
level of significance p
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 100<br />
(normal values for the serum total proteins: 65-80 gr/L and<br />
for albumin: 35-50 gr/L) (Table 1).<br />
It was found that, in group A, 21 patients showed<br />
disturbances of the acid-base balance. Specifically, 11<br />
patients appeared to have a mixed disturbance (metabolic<br />
alkalosis with respiratory alkalosis), 4 had metabolic<br />
alkalosis, 4 had metabolic acidosis (mixed), two had<br />
respiratory alkalosis and one had normal values. The mean<br />
average of the blood pH was slightly alkaline (7,44±0,06).<br />
Bicarbonates appeared to be at a mean average increased<br />
(24,1±5,2) and were ranging from 10,6 to 35,3 mmol/L.<br />
The comparison of the results of group A to those of group B<br />
(Table 1, 2) revealed a significant difference to the serum<br />
proteins and albumin (p=0,00001 in both cases), while in<br />
group B no acid-base disturbance was noted.<br />
n (7F, age pH PaC2 HCO3- Hct Cr Pro Alb + a+ CI- Ca++ AG<br />
8M)<br />
1 35 7.413 33.8 21.1 42.5 0.9 7.9 5 4.2 143 110 10.2 12.1<br />
2 60 7.434 36.7 24 41.5 0.9 7.4 4.3 4.4 142 108 10.8 10<br />
3 43 7.427 35.5 22.9 48.3 1 9.1 5.6 4.6 141 105 10.5 13.1<br />
4 24 7.423 36.9 23.6 38 1 8.9 5.4 4.2 141 104 10.7 9<br />
5 45 7.438 34.2 22.6 38.2 0.7 8.3 5.2 4.3 139 106 10.9 10.4<br />
6 30 7.414 41.3 25.8 38.2 0.8 8.3 5.2 4.4 140 102 10.8 12.2<br />
7 37 7.441 32.8 21.9 38.7 0.7 8.7 5.1 3.9 145 109 10.2 14.1<br />
8 67 7.42 38 24.1 39.5 0.8 8.7 6.7 4.2 141 105 9.9 11<br />
9 35 7.41 33.7 20.9 40 0.7 8 5.3 4.3 142 104 10.3 17.1<br />
10 40 7.446 32.1 21.6 38.2 0.7 7 4.4 4.4 142 106 9.8 14.4<br />
11 72 7.364 40.4 22.5 36.8 1.1 7.1 4.5 4.6 148 104 10 11.5<br />
12 50 7.437 39.3 25.9 43.5 0.9 7.3 4.5 4.7 143 103 9.6 14.1<br />
13 26 7.407 40.9 25.2 41.5 1.1 7.4 4.9 4.1 144 104 9.6 14.8<br />
14 30 7.419 40.2 25.2 36.8 0.9 6.8 4.2 4.5 139 102 9.7 11.8<br />
15 54 7.376 41.6 23.9 38.6 0.8 7.3 4.3 4.3 141 106 8.3 11.1<br />
Table 2: Blood gases, serum electrolytes, creatinine, proteins and haematocrite of normal individuals<br />
(Hct=haematocrite, Cr=creatinine, Pro=proteins, Alb=albulin, K+=potassium, Na+=sodium, CI-<br />
=chloride, Ca++=calcium, AG=anion gap)<br />
mean+/-<br />
sd<br />
43,2+/<br />
-14,7<br />
7,42+/-<br />
0,02<br />
range 24-72 7,36-<br />
7,475<br />
37,2+/-<br />
3,3<br />
32,1-<br />
41,6<br />
23,4+/-<br />
0,4<br />
20,9-<br />
25,9<br />
40+/-<br />
3,1<br />
36,8-<br />
48,3<br />
0,9+/-<br />
0,1<br />
0,7-<br />
1,1<br />
7,9+/-<br />
0.8<br />
6,8-<br />
9,1<br />
4,8+/-<br />
0,7<br />
4,2-<br />
6,7<br />
4,3+/-<br />
0,2<br />
3,9-<br />
4,7<br />
142+/-<br />
2,3<br />
139-<br />
148<br />
105+/-<br />
2,4<br />
102-<br />
110<br />
10,1+/<br />
-0,7<br />
8,3-<br />
10,9<br />
12,8+/<br />
-1,9<br />
10-<br />
17,1<br />
The anion gap in group A was ranging from 5,7 to 18,5<br />
mmol/L (11,5±3,7). Because of this wide range, the patients<br />
were divided in two further sub-groups (Table 3). These were<br />
sub-group A1 with 12 patients that had an anion gap higher<br />
than 10 mmol/L and sub-group A2 with 10 patients that had<br />
an anion gap lower than 10 mmol/L. Evaluating the pH of the<br />
two sub-groups revealed the first (A1) had respiratory<br />
alkalosis (mean±SD, pH=7,42±0,06, PaCO 2 =32,0±4,2 and<br />
HCO 3 - =21,6±4,6), while the second (A2) had metabolic<br />
alkalosis (mean±SD, pH=7,46±0,04, HCO 3 - =27,3±5,2 and<br />
PaCO 2 =38,3±7,5).<br />
Seven patients in sub-group A2 suffered from CRF, while 3<br />
of these patients had a serum creatinine greater than 264<br />
mmol/L (advanced stage) (Table 3). In total, 6/22 patients<br />
had serum creatinine>264 mmol/L and from these patients, 3<br />
had clearly metabolic acidosis combined with some other<br />
disturbance (metabolic or respiratory alkalosis).<br />
Discussion<br />
In the extracellular fluids, the total concentration of weak<br />
acids cannot be regulated in order to achieve acid-base<br />
balance. However, since the total concentration of weak acids<br />
is an independent variable, a change to their levels would<br />
cause a change to the acid-base balance. Proteins are weak<br />
acids, and when they are reduced in the plasma, the<br />
concentration of bicarbonates is increased (causing metabolic<br />
alkalosis), in order to retain electric balance, a fact that was<br />
noted in most of the patients in this study (21/22). The<br />
metabolic alkalosis in 15/22 patients was caused by<br />
hypoproteinemia. If alkalosis was due to an acid deficiency,<br />
the serum chloride levels would be much more reduced,<br />
while the calculated bicarbonates would be increased (over<br />
42 mmol/L). However, in the patients of this study, the mean<br />
value of serum bicarbonates and chloride was approximately<br />
in the normal limits (small increase of bicarbonates), as it<br />
happens in the case of a primary hypoproteinemic alkalosis.<br />
The above information is of particular importance<br />
considering that 6/22 patients suffered from CRF with serum<br />
creatinine over 264 mmol/L. While this situation is<br />
accompanied by metabolic acidosis (usually with an<br />
increased anion gap), this was a fact only in 3 of our patients.
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 101<br />
n age pH PaC2 HCO3- Hct Cr Pro Alb + a+ CI- Ca++ AG<br />
Subgroup<br />
A2<br />
1 60 7.48 35 27 34 2.8 5 2.1 3.5 142 101 7.2 14<br />
2 65 7.426 40.3 25.8 37.3 1.3 6 3.1 4.1 135 100 9.4 9.2<br />
3 74 7.427 38.7 24.9 27.6 2.2 6 3.2 4 132 98 9.5 9.1<br />
4 68 7.5 35.2 25.5 35 3 6 2.6 4.3 138 95 8.8 18.5<br />
5 50 7.4 32.2 23.3 30.8 0.6 4.6 2.5 4.5 143 108 8.5 11.7<br />
6 45 7.44 30.7 21.2 27.1 2.9 5.1 2.2 3.2 145 107 8.1 17<br />
7 88 7.4 34 22.1 40.7 1.1 5.3 2.5 4.7 148 112 9 10.9<br />
8 62 7.465 36.4 25.6 34.5 2.9 5.7 2.5 3.7 134 97 8 11<br />
9 37 7.5 33.6 28.3 43.4 0.7 6 2.5 3.8 144 104 11.7 9.7<br />
10 76 7.43 36.5 24 28 5.2 5 1.8 3.6 142 102 6.5 16<br />
11 59 7.289 22.6 10.6 25.1 6.9 4.9 1.9 3.8 140 116 8.4 13.4<br />
12 54 7.4 25.5 18.9 30.3 2.8 5 1.7 6.2 150 119 8.2 12<br />
13 64 7.304 32.4 15.7 29.7 4.7 6 3.2 4.5 139 108 8.3 15.3<br />
14 65 7.484 31.8 23.4 39 2.6 6.4 2.9 4.3 139 103 8.5 12<br />
15 74 7.459 32.1 22.3 28.5 2.4 6.1 2 5.1 136 96 8.1 17.7<br />
(mean+/-sd)<br />
62,7+/-<br />
12,9<br />
7,43+/-<br />
0,06 33,1+/-4,6 22,6+/-4,6<br />
range 37-88 7,29-7,5 22,6-40,3 10,6-28,3<br />
13,2+/-<br />
3,1<br />
9,1-<br />
18,5<br />
32,7+/-<br />
5,5<br />
2,8+/-<br />
1,7<br />
5,5+/-<br />
0,6<br />
2,5+/-<br />
0,5<br />
4,2+/-<br />
0,7<br />
140+/-<br />
4,9<br />
104,4+/-<br />
7,2<br />
8,6+/-<br />
1,2<br />
25,1-<br />
43,4 0,6-6,9 4,6-6,4 1,7-3,2 3,2-6,2 132-150 95-119 6,5-11,7<br />
Subgroup<br />
A1<br />
1 58 7.455 46.7 32 34 1.7 5.4 2.3 4.4 143 103 8 8<br />
2 70 7.491 34.9 25.4 34.8 2.9 5.8 2.5 2.9 138 94 8.1 8.6<br />
3 62 7.489 34.8 25.9 33.4 3.1 4.7 1.9 4 139 107 7.3 6.1<br />
4 38 7.397 41.5 25 37.5 3.2 6.2 3.2 4.7 135 103 9.1 7<br />
5 73 7.529 43.3 35.3 31.6 3.1 6.2 2.4 2.4 131 86 8.3 9<br />
6 53 7.433 44.2 28 44.4 0.8 5.7 1.3 3.7 137 100 8.1 9<br />
7 84 7.493 25 19.3 31.7 0.9 6.1 2.7 4 137 112 9 5.7<br />
(mean+/-sd)<br />
62,6+/-<br />
14,9<br />
7,47+/-<br />
0,04 38,6+/-7,5 27,3+/-5,2<br />
range 38-84 7,4-7,53 25-46,7 19,3-35,3<br />
35,3+/-<br />
4,5<br />
2,2+/-<br />
1,1<br />
5,6+/-<br />
0,5<br />
2,3+/-<br />
0,6<br />
3,7+/-<br />
0,8<br />
137+/-<br />
3,7<br />
100,7+/-<br />
8,6<br />
8,3+/-<br />
0,6<br />
7,6+/-<br />
1,4<br />
31,6-<br />
44,4 0,8-3,2 4,7-6,2 1,3-3,2 2,4-4,7 31-143 86-112 7,3-9,1 5,7-9<br />
Table 3: Patients with hypoproteinemia in subgroups depends on their anion gap (AG)<br />
(Hct=haematocrite, Cr=creatinine, Pro=proteins, Alb=albumin, K+=potassium, Na+=sodium,<br />
CI-=chloride, Ca++=calcium)<br />
Normal serum proteins are polyanionic molecules and their<br />
contribution to the electrochemical balance cannot be easily<br />
specified with accuracy. They contribute to the change of the<br />
charge, a change that depends on the kind of proteins, their<br />
concentration as well as the serum pH. In particular, albumin<br />
contributes at 2,0-2,8 mmol/L for every 10 gr/L of change in<br />
the serum level, while the globulins 1,3-1,9 mmol/L for every<br />
10 gr/L of change. Hence, this explanation constitutes the<br />
possible mechanism according to which the reduced anion<br />
gap in patients with nephrotic syndrome or severe stage of<br />
liver cirrhosis may arise (2). In sub-groups A1 and A2 it is<br />
obvious that at a mean average in the first one (A1) there was<br />
respiratory alkalosis due to tachypnea because they were<br />
hypovolemic, while in the second one (A2), there was at a<br />
mean average metabolic alkalosis, apparently due to the<br />
relative hypoproteinemia.<br />
In addition, patients of group A showed to have at a mean<br />
average a mild increase of the pH (7,44±0,06), approximately<br />
normal bicarbonates (24,1±5,2) and reduced PaCO 2<br />
(34,9±6,1), all suggesting the presence of respiratory<br />
alkalosis, apparently due tachypnea because the presence of<br />
hypovolemia. Rossing et al., studied 23 patients with<br />
hypoproteinemia due to liver cirrhosis or other diseases and<br />
ascertained that alkalemia (metabolic alkalosis of<br />
hypoproteinemia) was accompanied by hypocapnea<br />
(compensatory hypercapnea would be expected) for which<br />
hypoxemia was not responsible. In addition, the PaCO 2 levels<br />
were proportional to the reduction of albumin as well as the<br />
total serum proteins (6). All these facts were established in<br />
the present study in most of the patients, as mentioned above.<br />
Taking in consideration that 12 patients of sub-group A2 had<br />
CRF, while in 3 of these patients serum creatinine was over<br />
264 mmol/L, it is obvious that the importance of the reduced<br />
gap is greater, since in cases of an advanced stage of CRF an<br />
increased anion gap is expected (Table 3). Furthermore, the<br />
fact that 6/22 patients had serum creatinine>264 mmol/L
<strong>BANTAO</strong> <strong>Journal</strong> 2006: 4 (1): 102<br />
suggests that there should be, at least, an evident metabolic<br />
acidosis, with some patients showing an increased anion gap.<br />
Indeed, 3 of these patients had metabolic acidosis combined<br />
with some other disturbance (metabolic or respiratory<br />
alkalosis). These facts clearly show the influences of<br />
hypoproteinemia in the acid-base balance of those patients.<br />
Conclusions<br />
It can be concluded that: a) patients with hypoproteinemia<br />
have disturbances of the acid-base balance (mainly metabolic<br />
and respiratory alkalosis), which are due to the reduction of<br />
the serum proteins and b) the influence of hypoproteinemia in<br />
patients with CRF contributes to the improvement of the<br />
blood’s pH level.<br />
References<br />
1. Gabow PA. Disorders associated with an altered anion gap.<br />
Kidney Int 1985; 27: 472-83<br />
2. Emmett M & Narins RG. Clinical use of the anion gap. N Engl<br />
J Med 1977; 56: 38-54<br />
3. McAuliffe JJ, Lind LJ, Leith DE, Fenci V. Hypoproteinemic<br />
alkalosis. Am J Med 1986; 8: 86-90<br />
4. Rossing TH, Maffeo N, Fenci V. Acid-base effects of altering<br />
plasma protein concentration in human blood in vitro. J Appl<br />
Physiol 1986; 61: 2260-5<br />
5. Schlichtig R. Base excess vs strong ion difference. Which is<br />
more helpful? Adv. Exp Med Biol 1997; 411: 91-5<br />
6. Rossing TH, Boixeda D, Maffeo N, Fenci V. Hyperventilation<br />
with hypopropteinemia. J Lab Clin Med 1988; 112: 553-9
INSTRUCTIONS TO AUTHORS<br />
ALL ARTICLES MUST BE SUBMITTED ONLINE. Once you have prepared your<br />
manuscript according to the Instructions below, please send it as an attachment to the<br />
deputy editor Goce Spasovski (gspas@sonet.com.mk).<br />
AUTHORS: PLEASE PAY PARTICULAR ATTENTION TO THE SECTIONS ON<br />
CONFLICT OF INTEREST DECLARATION AND FIGURE PREPARATION<br />
AIMS AND SCOPE<br />
<strong>BANTAO</strong> <strong>Journal</strong> is the official publication of the Balkan Cities Association of Nephrology,<br />
Dialysis, Transplantation and Artificial Organs. It publishes original articles relating to clinical<br />
or laboratory investigations of relevance to nephrology, dialysis or transplantation. Papers<br />
relating to basic immunology, anatomy and physiology are welcomed if these relate to the<br />
kidney. Rapid communications, case reports, technical reports and letters to the Editor are also<br />
considered. Letters to the Editor do not necessarily express the views of the Editor, and may or<br />
may not be peer-reviewed. All material is assumed to be submitted exclusively unless otherwise<br />
stated, and must not have been published previously except in abstract form. Manuscripts related<br />
to the topic of the submitted manuscript which are in preparation or submitted to other journals,<br />
must be sent in together with the manuscript destined for <strong>BANTAO</strong> <strong>Journal</strong>.<br />
Only papers in UK/USA English will be considered for publication. The text should be typed<br />
double spaced on A4 sized (30 x 21 cm) paper. A 2 cm margin should be left at both sides of the<br />
text, 3 cm wide margins at top and bottom of page.<br />
If any tables, illustrations or photomicrographs have been published elsewhere, written consent<br />
to re-publication (in print and online) must be obtained by the author from the copyright holder<br />
and the authors, such permission being detailed in the cover letter.<br />
Manuscripts should bear the full name and address, with telephone, fax, and email of the author<br />
to whom the proofs and correspondence should be sent (corresponding author). For all authors<br />
first name and surname should be written in full. In the covering letter the individual<br />
contribution of each co-author must be detailed. This letter must contain the statement:'the<br />
results presented in this paper have not been published previously in whole or part, except in<br />
abstract form'.Should your manuscript be accepted for publication, you will be required to give<br />
signed consent for publication.<br />
On acceptance the corresponding author will be advised of the approximate date of receipt of<br />
proofs. Proofs must be returned by the author within 48 hours of receipt.<br />
To accelerate publication only one set of PDF proofs is sent to the corresponding author by<br />
email. This shows the layout of the paper as it will appear in the <strong>Journal</strong>. It is, therefore, essential<br />
that manuscripts are submitted in their final form, ready for the printer. Proof-reading must be<br />
limited to the correction of typographical errors. Any other changes involve time-consuming and<br />
expensive work. If additions are necessary, these may be made at the end of the paper in a Note<br />
in Proof.<br />
Authors are referred to the statement on uniform requirements for manuscripts submitted to<br />
biomedical journals prepared by an international committee of medical journal editors. (Br Med<br />
J 1982; 284: 1766-1770, Ann Intern Med 1982; 96: 766-771.)<br />
CONFLICT OF INTEREST DECLARATION<br />
All authors must make a formal statement at the time of submission indicating any potential<br />
conflict of interest that might constitute an embarrassment to any of the authors if it were not to<br />
be declared and were to emerge after publication. Such conflicts might include, but are not<br />
limited to, shareholding in or receipt of a grant or consultancy fee from a company whose<br />
product features in the submitted manuscript or which manufactures a competing product.
The corresponding author must inlcuded a Conflict of Interest Statement on behalf of all<br />
the authors at the end of their article. If no Conflict of Interest is declared this must be<br />
stated also.<br />
It is a condition of publication that a statement declaring any conflict of interest is included at the<br />
end of the manuscript on first submission. Failure to insert a statement for all authors will delay<br />
the review process.<br />
PAGE CHARGES<br />
There will be no charges for the printed 5 pages for an Original Article, 3 pages for a Case<br />
Report, Technical Report or Brief Report, and 1 page for a Letter. Excess page charges will be<br />
charged 10 EURO per page.<br />
Case Reports must be 3 pages or less, and the standard length of a Letter to the Editor is 200<br />
words. A printed page is ~850 words, but pro rata reductions in the length of the text must be<br />
made for Tables, Figures and illustrations.<br />
In the proof email there is a reminder of the excess page charges levied on manuscripts that are<br />
over length. It is the authors responsibility to check their proof page extent and act according if<br />
they are do not wish to be charge for excess pages.<br />
AUTHORS<br />
Each author should have participated sufficiently in the work to take public responsibility for the<br />
content. This participation must include:<br />
Conception or design, or analysis and interpretation of data, or both.<br />
Drafting the article or revising it for critically important intellectual content.<br />
Final approval of the version to be published. (See Br Med J 1985; 291: 722-723.)<br />
TEXT<br />
NB - Please include your abstract and title page in the main body of your manuscript, as<br />
well as submitting it separately.<br />
The order of original articles should be as follows:<br />
Title page giving details of all authors, including first or given name (see above).<br />
On a separate page an abstract of ~250 words. It should consist of four paragraphs labelled,<br />
`Background', `Methods', `Results'and `Conclusions'. They should briefly describe, respectively,<br />
the problems being addressed in this study, how the study was performed, the salient results and<br />
what the authors conclude from the results.<br />
Keywords not more than 6, in alphabetical order, characterizing the scope of the paper, the<br />
principal materials, and main subject of work. Authors are requested to supply an additional 10-<br />
15 keywords for electronic publication purposes.<br />
Running title of not more than 75 letters and spaces.<br />
On a new page: Introduction, Subjects and Methods, Results, Discussion, Acknowledgements,<br />
References (see below), Tables, Legends to Figures and Figures. All pages should be numbered<br />
consecutively commencing with the title page. Headings (Introduction; Subjects and Methods,<br />
etc) should be placed on separate lines. It is most important that authors number their pages<br />
prior to submission as reviewers will refer to particular pages when providing their<br />
comments on the manuscript.<br />
Please ensure that your abstract and title page are inlcuded in the main body of your manuscript,<br />
as well as submitting it separately.
Any statistical method must be detailed in the Subjects and methods section, and any not in<br />
common use should be described fully or supported by references.<br />
Authors should not use abbreviations in headings, and Figure legends should be comprehensive<br />
without extensive perusal of the Subjects and methods section. Authors are advised to refrain<br />
from excessive use of uncommon abbreviations, particularly to describe groups of patients or<br />
experimental animals.<br />
Images in Nephrology aims to publish 1 or 2 high quality pictures of great clinical interest<br />
accompanying by a minimal amount of text and 2-3 references. The piece can not exceed 2<br />
printed pages.<br />
TABLES<br />
Tables must be typed on separate pages and should follow the reference list. All Tables must be<br />
numbered consecutively and each must have a brief heading describing its contents. Any<br />
footnotes to Tables should be indicated by superscript characters. Tables must be referred to in<br />
the main text in order. All Tables must be simple and not duplicate information given in the text.<br />
FIGURE PREPARATION<br />
Please be aware that the requirements for online submission and for reproduction in the journal<br />
are different: (i) for online submission and peer review, please upload your Figures either<br />
embedded in the word processing file or separately as low-resolution images (.jpg, .tif, .gif or.<br />
eps); (ii) for reproduction in the journal, you will be required after acceptance to supply highresolution<br />
.tif files (1200 d.p.i. for line drawings and 300 d.p.i. for colour and half-tone artwork)<br />
or high-quality printouts on glossy paper. We advise that you create your high-resolution images<br />
first as these can be easily converted into low-resolution images for online submission.<br />
For useful information on preparing your Figures for publication, go to<br />
http://cpc.cadmus.com/da. Figures will not be relettered by the publisher. The journal reserves<br />
the right to reduce the size of illustrative material. All micrographs must carry a magnification<br />
bar. Any photomicrographs, electron micrographs or radiographs must be of high quality.<br />
Wherever possible photographs should fit within the print area of 169 x 235 mm (full page) or<br />
within the column width of 82 mm. Photomicrographs should provide details of staining<br />
technique and a scale bar. Patients shown in photographs should have their identity concealed or<br />
should have given their written consent to publication. Normally no more than six illustrations<br />
will be accepted without charge.<br />
TRADE NAMES<br />
Non-proprietary (generic) names of products should be used. If a brand name for a drug is used,<br />
the British or International non-proprietary (approved) name should be given. The source of any<br />
new or experimental preparation should also be given.<br />
REFERENCES<br />
The references should be numbered in the order in which they appear in the text. At the end of<br />
the article the full list of references should give the name and initials of all authors unless there<br />
are more than six, when only the first three should be given followed by et al. The authors'<br />
names should be followed by the title of the article, the title of the <strong>Journal</strong> abbreviated according<br />
to the style of Index Medicus, the year of publication, the volume number and the first and last<br />
page numbers. References to books should give the title of the book, which should be followed<br />
by the place of publication, the publisher, the year and the relevant pages.
EXAMPLES<br />
1. Madaio MP. Renal biopsy. Kidney Int 1990; 38: 529-543<br />
Books:<br />
2. Roberts NK. The cardiac conducting system and the His bundle electrogram. Appleton-<br />
Century-Crofts, New York, NY: 1981; 49-56<br />
Chapters:<br />
3. Rycroft RJG, Calnan CD. Facial rashes among visual display unit (VDU) operators. In: Pearce<br />
BG, ed. Health hazards of VDUs. Wiley, London, UK: 1984; 13-15<br />
References should be limited to those relating directly to the content of the paper and should not<br />
exceed 20. Case Reports should contain no more than 10 references, and letters to the editor no<br />
more than five.<br />
Note: It is the responsibility of the author to ensure the accuracy of the references in the<br />
submitted article. Downloading references direct from Medline is highly recommended.<br />
COPYRIGHT<br />
It is a condition of publication in the <strong>Journal</strong> that authors grant an exclusive licence to the<br />
<strong>Journal</strong>.<br />
EDITORIAL ENQUIRIES:<br />
A Basci<br />
Ege University Medical School Nephrology Dept.<br />
Bornova, Universite Caddesi<br />
IZMIR, 35100<br />
TURKEY<br />
Tel/Fax: + 90 232 388 9231<br />
E-mail: alibasci@med.ege.edu.tr<br />
Deputy editor: Clinical Nephrology Goce Spasovski<br />
Email: gspas@sonet.com.mk (for original articles - clinical research)<br />
Deputy editor: Basic research Adrian Covic<br />
Email: acovic@xnet.ro (for original articles - basic research)<br />
COLOUR ILLUSTRATIONS<br />
Colour illustrations are accepted, but the authors will be required to contribute to the cost of the<br />
reproduction. Colour figures will incur a printing charge of 50 euros. Illustrations for which<br />
colour is not essential can be reproduced as black and white images in the print journal.<br />
<strong>BANTAO</strong> <strong>Journal</strong><br />
Published on behalf of<br />
Balkan Cities Association<br />
of Nephrology, Dialysis,<br />
Transplantation and Artificial Organs