Form 1: Modified Resident's Verbal Pain Inventory (M ... - CareSearch
Form 1: Modified Resident's Verbal Pain Inventory (M ... - CareSearch
Form 1: Modified Resident's Verbal Pain Inventory (M ... - CareSearch
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
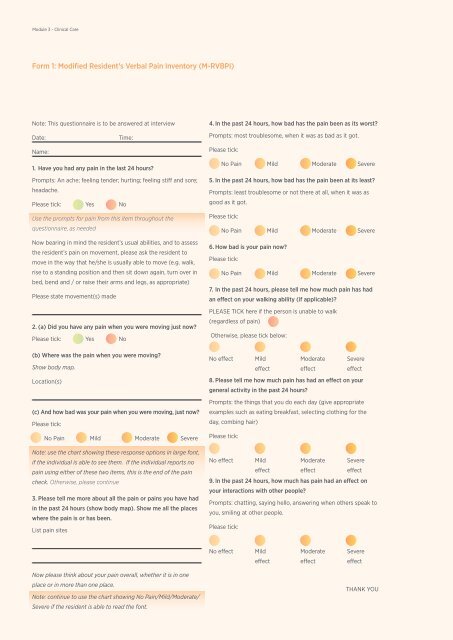
Module 3 - Clinical Care<br />
<strong>Form</strong> 1: <strong>Modified</strong> Resident’s <strong>Verbal</strong> <strong>Pain</strong> <strong>Inventory</strong> (M-RVBPI)<br />
Note: This questionnaire is to be answered at interview<br />
Date:<br />
Time:<br />
Name:<br />
1. Have you had any pain in the last 24 hours?<br />
Prompts: An ache; feeling tender; hurting; feeling stiff and sore;<br />
headache.<br />
Please tick: Yes No<br />
Use the prompts for pain from this item throughout the<br />
questionnaire, as needed<br />
Now bearing in mind the resident’s usual abilities, and to assess<br />
the resident’s pain on movement, please ask the resident to<br />
move in the way that he/she is usually able to move (e.g. walk,<br />
rise to a standing position and then sit down again, turn over in<br />
bed, bend and / or raise their arms and legs, as appropriate)<br />
Please state movement(s) made<br />
2. (a) Did you have any pain when you were moving just now?<br />
Please tick: Yes No<br />
(b) Where was the pain when you were moving?<br />
Show body map.<br />
Location(s)<br />
(c) And how bad was your pain when you were moving, just now?<br />
Please tick:<br />
No <strong>Pain</strong> Mild Moderate Severe<br />
Note: use the chart showing these response options in large font,<br />
if the individual is able to see them. If the individual reports no<br />
pain using either of these two items, this is the end of the pain<br />
check. Otherwise, please continue<br />
3. Please tell me more about all the pain or pains you have had<br />
in the past 24 hours (show body map). Show me all the places<br />
where the pain is or has been.<br />
List pain sites<br />
4. In the past 24 hours, how bad has the pain been as its worst?<br />
Prompts: most troublesome, when it was as bad as it got.<br />
Please tick:<br />
No <strong>Pain</strong> Mild Moderate Severe<br />
5. In the past 24 hours, how bad has the pain been at its least?<br />
Prompts: least troublesome or not there at all, when it was as<br />
good as it got.<br />
Please tick:<br />
No <strong>Pain</strong> Mild Moderate Severe<br />
6. How bad is your pain now?<br />
Please tick:<br />
No <strong>Pain</strong> Mild Moderate Severe<br />
7. In the past 24 hours, please tell me how much pain has had<br />
an effect on your walking ability (if applicable)?<br />
PLEASE TICK here if the person is unable to walk<br />
(regardless of pain)<br />
Otherwise, please tick below:<br />
No effect Mild<br />
Moderate Severe<br />
effect effect<br />
effect<br />
8. Please tell me how much pain has had an effect on your<br />
general activity in the past 24 hours?<br />
Prompts: the things that you do each day (give appropriate<br />
examples such as eating breakfast, selecting clothing for the<br />
day, combing hair)<br />
Please tick:<br />
No effect Mild<br />
Moderate Severe<br />
effect effect<br />
effect<br />
9. In the past 24 hours, how much has pain had an effect on<br />
your interactions with other people?<br />
Prompts: chatting, saying hello, answering when others speak to<br />
you, smiling at other people.<br />
Please tick:<br />
No effect<br />
Mild<br />
effect<br />
Moderate<br />
effect<br />
Severe<br />
effect<br />
Now please think about your pain overall, whether it is in one<br />
place or in more than one place.<br />
Note: continue to use the chart showing No <strong>Pain</strong>/Mild/Moderate/<br />
Severe if the resident is able to read the font.<br />
THANK YOU
Module 3 - Clinical Care<br />
<strong>Form</strong> 1: <strong>Modified</strong> Resident’s <strong>Verbal</strong> <strong>Pain</strong> <strong>Inventory</strong> (M-RVBPI) (continued)<br />
Scoring the M-RVBPI<br />
Items 2c, 4, 5, and 6 assess the intensity of pain as reported by<br />
the resident. These items are best used to obtain a picture of the<br />
level of the resident’s pain experience that can be summarised in<br />
the <strong>Pain</strong> Intensity Summary.<br />
<strong>Pain</strong> Intensity Summary<br />
Item <strong>Pain</strong> Feature<br />
1. <strong>Pain</strong> initially recalled in past 24 hours<br />
Please tick: Yes No<br />
2c. <strong>Pain</strong> on movement<br />
No <strong>Pain</strong> Mild Moderate Severe<br />
4. <strong>Pain</strong> worst in past 24 hours<br />
No <strong>Pain</strong> Mild Moderate Severe<br />
5. <strong>Pain</strong> least in past 24 hours<br />
No <strong>Pain</strong> Mild Moderate Severe<br />
6. <strong>Pain</strong> now<br />
No <strong>Pain</strong> Mild Moderate Severe<br />
Responses to items 7, 8 and 9 can be scored using the scale of<br />
0 (no pain) to 3 (severe pain) and these scores can be summed<br />
to give an overall score for pain interference. This score can be<br />
documented in the <strong>Pain</strong> Interference Summary.<br />
<strong>Pain</strong> Interference Summary<br />
Item Area of interference Circle and transfer score to total.<br />
7. Walking<br />
0 No <strong>Pain</strong> 1 Mild 2 Moderate 3 Severe<br />
Not Applicable<br />
Recommended Uses of Scores<br />
Obviously, responses for pain intensity and scores for pain<br />
interference can be used for comparison purposes. This is<br />
especially important when trialling an intervention to reduce<br />
pain. However, responses and scores should also serve to alert<br />
staff to the need to implement such an intervention.<br />
Some key principles are that:<br />
• <strong>Pain</strong> of moderate or severe intensity that cannot be<br />
controlled by existing measures needs urgent review.<br />
• Scores of 6 and over for pain interference, or four and over<br />
when the resident cannot walk, also mean that urgent<br />
review is required.<br />
• <strong>Pain</strong> of any level of intensity that recurs, lasts for long<br />
periods, and/or causes interference with walking, general<br />
activity, or interactions must prompt the implementation<br />
or review of pain management strategies.<br />
8. General activity<br />
0 No <strong>Pain</strong> 1 Mild 2 Moderate 3 Severe<br />
Not Applicable<br />
9. Interactions<br />
0 No <strong>Pain</strong> 1 Mild 2 Moderate 3 Severe<br />
Not Applicable<br />
TOTAL PAIN SCORE /9
Module 3 - Clinical Care<br />
<strong>Form</strong> 2: Abbey <strong>Pain</strong> Scale<br />
For measurement of pain in people with dementia who<br />
cannot verbalise.<br />
Name of Resident:<br />
Name and designation of person completing the scale:<br />
Date:<br />
Time:<br />
Latest pain relief given was:<br />
at<br />
hours<br />
How to use scale:<br />
While observing the resident, score questions 1 to 6<br />
1. Vocalisation<br />
e.g. whimpering, groaning, crying<br />
0 Absent 1 Mild 2 Moderate 3 Severe<br />
2. Facial Expression<br />
e.g. looking tense, frowning, grimacing, looking frightened<br />
0 Absent 1 Mild 2 Moderate 3 Severe<br />
3. Change in Body Language<br />
e.g. fidgeting, rocking, guarding part of the body, withdrawn<br />
0 Absent 1 Mild 2 Moderate 3 Severe<br />
4. Behavioural Change<br />
e.g. increased confusion, refusing to eat, alteration in<br />
usual patterns<br />
0 Absent 1 Mild 2 Moderate 3 Severe<br />
5. Physiological Change<br />
e.g. temperature, pulse or blood pressure outside normal limits,<br />
perspiring, flushing or pallor<br />
0 Absent 1 Mild 2 Moderate 3 Severe<br />
6. Physical Changes<br />
e.g. skin tears, pressure areas, arthritis, contractures,<br />
previous injuries<br />
0 Absent 1 Mild 2 Moderate 3 Severe<br />
Now tick the circle that matches the Total <strong>Pain</strong> Score<br />
0-2<br />
No <strong>Pain</strong><br />
3-7<br />
Mild<br />
8-13<br />
Moderate<br />
Finally, tick the circle which matches the type of pain<br />
Chronic<br />
Acute<br />
Acute on<br />
Chronic<br />
14+<br />
Severe<br />
TOTAL PAIN SCORE /18
Module 3 - Clinical Care<br />
<strong>Form</strong> 3: Oral Health Assessment Tool<br />
Name of Resident: Completed by: Date:<br />
Resident: is independent needs reminding needs supervision needs full assistance<br />
Will not open mouth Grinding or chewing Head faces down Refuses treatment<br />
Is aggressive Bites Excessive head movement Cannot swallow well<br />
Cannot rinse and spit<br />
Will not take dentures out at night<br />
Healthy Changes Unhealthy<br />
Dental<br />
Referral<br />
Healthy Changes Unhealthy<br />
Dental<br />
Referral<br />
Lips<br />
Natural Teeth<br />
Smooth, pink,<br />
moist<br />
Dry, chapped or<br />
red at corners<br />
Swelling or<br />
lump, red/<br />
white/ulcerated<br />
bleeding/<br />
ulcerated<br />
at corners *<br />
Yes<br />
No<br />
No decayed<br />
or broken teeth<br />
or roots<br />
1- 3 decayed<br />
or broken teeth/<br />
roots, or teeth<br />
very worn down<br />
4 or more<br />
decayed or<br />
broken teeth/<br />
roots or fewer<br />
than 4 teeth, or<br />
very worn down<br />
teeth *<br />
Yes<br />
No<br />
Tongue<br />
Dentures<br />
Normal moist,<br />
roughness, pink<br />
Patchy, fissured,<br />
red, coated<br />
Patch that is<br />
red and/or<br />
white/ulcerated,<br />
swollen *<br />
Yes<br />
No<br />
No broken areas<br />
or teeth, worn<br />
regularly, and<br />
named<br />
1 broken area or<br />
tooth, or worn<br />
1-2 hours per<br />
day only or not<br />
named<br />
1 or more broken<br />
areas or teeth,<br />
denture missing /<br />
not worn, need<br />
adhesive, or not<br />
named *<br />
Yes<br />
No<br />
Gums and Oral Tissue<br />
Oral Cleanliness<br />
Moist, pink,<br />
smooth,<br />
no bleeding<br />
Dry, shiny,<br />
rough, red,<br />
swollen, sore,<br />
one ulcer/sore<br />
spot, sore under<br />
dentures<br />
Swollen, bleeding,<br />
ulcers, white/red<br />
patches,<br />
generalised<br />
redness under<br />
dentures *<br />
Yes<br />
No<br />
Clean and no<br />
food particles or<br />
tartar in mouth<br />
or on dentures<br />
Food, tartar,<br />
plaque 1-2 areas<br />
of mouth, or on<br />
small area of<br />
dentures<br />
Food particles,<br />
tartar, plaque<br />
most areas of<br />
mouth, or on<br />
most of dentures<br />
*<br />
Yes<br />
No<br />
Saliva<br />
Dental <strong>Pain</strong><br />
Moist tissues<br />
watery and<br />
free flowing<br />
Dry, sticky<br />
tissues, little<br />
saliva present,<br />
resident thinks<br />
they have a dry<br />
mouth<br />
Tissues parched<br />
and red, very<br />
little/no saliva<br />
present, saliva<br />
is thick, resident<br />
thinks they have a<br />
dry mouth *<br />
Yes<br />
No<br />
No behavioural,<br />
verbal or<br />
physical signs<br />
of dental pain<br />
<strong>Verbal</strong> &/or<br />
behavioural<br />
signs of pain<br />
such as pulling<br />
at face, chewing<br />
lips, not eating,<br />
changed<br />
behaviour.<br />
Physical pain signs<br />
(swelling of cheek<br />
or gum, broken<br />
teeth, ulcers), as<br />
well as verbal &/or<br />
behavioural signs<br />
(pulling at face, not<br />
eating, changed<br />
behaviour) *<br />
Yes<br />
No<br />
* Unhealthy signs usually indicate referral to a dentist is necessary<br />
Assessor Comments
Module 3 - Clinical Care<br />
<strong>Form</strong> 4: Oral Health Care Plan<br />
Last Oral Health Assessment (OHA) Date:<br />
(OHA) Review Due Date<br />
Oral Health Care Considerations<br />
Problems:<br />
difficulty swallowing difficulty moving head difficulty opening mouth fear of being touched<br />
Interventions:<br />
bridging chaining hand over hand distraction (activity board/toy) rescue other<br />
Daily Activities of Oral Hygiene<br />
Morning<br />
Natural Teeth<br />
Yes No<br />
clean teeth, gums,<br />
tongue<br />
Cleaned by:<br />
Self Supervise Assist<br />
After Lunch<br />
rinse mouth with water<br />
antibacterial product<br />
(teeth & gums)<br />
Night<br />
clean teeth, gums,<br />
tongue<br />
Replace toothbrush (3 monthly) Date:<br />
Denture<br />
Full Partial<br />
Upper Lower<br />
Inserted/ removed by:<br />
Self Staff<br />
clean teeth, gums,<br />
tongue<br />
brush denture<br />
rinse mouth with water<br />
rinse denture<br />
antibacterial product<br />
(gums)<br />
clean teeth, gums, tongue<br />
brush denture with<br />
mild soap<br />
leave dentures out<br />
overnight<br />
Cleaned by:<br />
Self Supervise Assist<br />
soak denture in cold<br />
water<br />
Disinfect dentures (weekly) Specify day:<br />
Oral Hygiene Aids<br />
soft toothbrush modified toothbrush toothbrush grip denture brush spray bottle (labelled)<br />
Oral Health Care Products<br />
mild soap (denture)<br />
antibacterial product<br />
saliva substitute<br />
lip moisturiser<br />
high fluoride (5000 ppm) toothpaste<br />
Additional Oral Care Instruction<br />
antifungal gel<br />
denture adhesive<br />
interproximal brush<br />
tongue scraper<br />
normal saline mouth toilet<br />
Check daily, document and report to RN if:<br />
bad breath bleeding gums lip blisters/sores/cracks tongue for any coating/<br />
change in colour<br />
sore mouth or gums mouth ulcer swelling of face/mouth broken/lost denture<br />
difficulty eating refusal of oral care denture not named excessive food left in mouth<br />
broken teeth<br />
Signed RN:<br />
Date:
Module 3 - Clinical Care<br />
<strong>Form</strong> 5: Confusion Assessment Method (CAM) - Shortened version<br />
Name of resident:<br />
Date of Birth:<br />
Date: / / Time:<br />
I. ACUTE ONSET AND FLUCTUATING COURSE<br />
a) Is there evidence of an acute change in mental status from<br />
the patient’s baseline?<br />
b) Did the (abnormal) behaviour fluctuate during the day, that is<br />
tend to come and go or increase and decrease in severity?<br />
II. INATTENTION<br />
Did the patient have difficulty focusing attention, for example, being easily<br />
distractible or having difficulty keeping track of what was being said?<br />
No<br />
No<br />
No<br />
BOX 1<br />
Yes<br />
Yes<br />
Yes<br />
III. DISORGANISED THINKING<br />
Was the patient’s thinking disorganised or incoherent, such as rambling or<br />
irrelevant conversation, unclear or illogical flow of ideas, or unpredictable<br />
switching from subject to subject?<br />
IV. ALTERED LEVEL OF CONSCIOUSNESS<br />
Overall, how would you rate the patient’s level of consciousness?<br />
Alert (normal)<br />
BOX 3<br />
Vigilant (hyperalert)<br />
Lethargic (drowsy, easily aroused)<br />
Stupor (difficult to arouse)<br />
Coma (unarousable)<br />
Do any checks appear in box 3?<br />
No<br />
No<br />
BOX 2<br />
Yes<br />
Yes<br />
If all items in Box 1 are ticked and at least<br />
one item in Box 2 is ticked a diagnosis of<br />
delirium is suggested.<br />
Adapted from: Inouye SK, vanDyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI.<br />
Clarifying confusion: The Confusion Assessment Method. A new method for detection<br />
of delirium. Ann Intern Med. 1990; 113: 941-948. Confusion Assessment Method: Training<br />
Manual and Coding Guide, Copyright 2003, Sharon K. Inouye, M.D., MPH