9261 HEPATITIS C REPORT GALLEY - North West Public Health ...
9261 HEPATITIS C REPORT GALLEY - North West Public Health ...
9261 HEPATITIS C REPORT GALLEY - North West Public Health ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
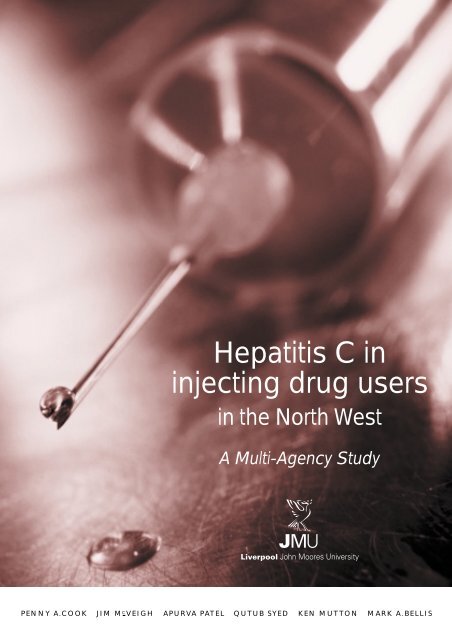
Hepatitis C in<br />
injecting drug users<br />
in the <strong>North</strong> <strong>West</strong><br />
A Multi-Agency Study<br />
Penny A.Cook Jim M C Veigh Apurva Patel Qutub Syed Ken Mutton Mark A.Bellis
Hepatitis C in<br />
injecting drug users<br />
in the <strong>North</strong> <strong>West</strong><br />
A Multi-Agency Study<br />
Penny A. Cook, Jim McVeigh, Apurva Patel, Qutub Syed, Ken Mutton and Mark A. Bellis<br />
Published by<br />
<strong>Public</strong> <strong>Health</strong> Sector<br />
School of <strong>Health</strong> and Human Sciences<br />
Liverpool John Moores University<br />
70 Great Crosshall Street<br />
Liverpool L3 2AB<br />
Tel: +44 (0151) 231 4316<br />
Fax: +44 (0151) 231 4320<br />
e-mail: p.a.cook@livjm.ac.uk<br />
August 2000<br />
ISBN 1-902051-19-X<br />
British Library Cataloguing in <strong>Public</strong>ation Data<br />
A Catalogue record for this book is available from the British Library<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
S UMMARY<br />
Viruses such as HIV, hepatitis C and hepatitis B that are transmitted in the blood pose<br />
a major health threat for people who inject drugs. Hepatitis C is a particular cause for<br />
concern for several reasons. Firstly, its prevalence is extremely high among injecting<br />
drug users (IDUs) (reported levels range between 60 - 80%). Secondly, no vaccine is as<br />
yet available, and the rapid mutation rate of the virus makes the imminent<br />
development of one unlikely. Thirdly, treatment is often ineffective, with even the most<br />
advanced treatment available clearing the infection on only 40% of occasions. Finally,<br />
a high proportion of cases (around 80%) become chronically infected, and of these,<br />
around 20% go on to develop serious liver damage, such as cirrhosis or hepatic<br />
carcinomas. Because individuals can have many years of asymptomatic infection before<br />
presenting to health services with chronic disease, the scale of the problem is hard to<br />
assess. Moreover, in IDUs infection with multiple strains of hepatitis C or co-infection<br />
with hepatitis B or HIV is common, and this exacerbates damage to the liver.<br />
In the wake of the HIV crisis and the provision of needle exchange schemes, IDUs<br />
reduced the levels of high risk sharing behaviour. However, hepatitis C is much more<br />
efficiently transmitted in small amounts of blood, and infections occur via indirect<br />
sharing of other injecting paraphernalia. At present there is no national strategy for<br />
the screening and treatment of IDUs. Treatment requires a high level of compliance,<br />
and has unpleasant side effects such as depression. Since IDUs often display chaotic<br />
behaviour, they are generally not considered suitable for treatment. However, taking a<br />
hepatitis C test and the counselling that accompanies it may represent an opportunity<br />
for addressing risk behaviours and possibly stabilising drug use.<br />
Aims<br />
Reviewing current knowledge about hepatitis C epidemiology reveals a number of<br />
factors that are at present unmeasured but necessary to implement effective and<br />
economic policies for hepatitis C prevention and treatment. Key amongst these is the<br />
level of infection in wider drug injecting communities in the <strong>North</strong> <strong>West</strong> (not just those<br />
requesting a test or in treatment at specialist drug agencies). Equally however,<br />
additional data are needed on the risk behaviours associated with infection and<br />
information is required on whether and how individuals change such behaviour once<br />
aware of their hepatitis C serostatus. Consequently, a group of IDUs in the <strong>North</strong> <strong>West</strong><br />
were recruited in order to:<br />
1. compare the prevalence of hepatitis C among drug users accessing different types<br />
of service, and among drug users not accessing services<br />
2<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
2. establish the extent of co-infection of hepatitis C and hepatitis B<br />
3. elucidate risk factors for hepatitis C infection<br />
4. explore the effect of knowledge of previous hepatitis test results on behaviour<br />
5. identify factors that predict sharing of equipment<br />
6. establish a cohort for follow up and establish feasibility of monitoring hepatitis C<br />
infection among drug using populations using saliva samples (results not covered<br />
in this report).<br />
Key Findings and Recommendations<br />
This study has identified the following key findings and recommendations:<br />
• Among the 341 injecting drug users in this study, the prevalence of hepatitis C<br />
was 53.1% (181 people), hepatitis B 26.6% (89 people) and 19.0% (65 people)<br />
were co-infected with hepatitis C and B (Section 4.1). Although the study was<br />
relatively small, different areas of study recruitment provided different levels of<br />
hepatitis C infection, with those presenting to drugs services requesting a test or<br />
those in treatment with community drugs teams having the highest prevalence.<br />
Those who had been for a hepatitis C test before this study were 1.68 times more<br />
likely to be hepatitis C positive in this study, again suggesting that people<br />
presenting for tests are more likely to be hepatitis C positive (Section 4.4).<br />
Models of health impact of hepatitis C should consider potential variations in<br />
prevalence rates between settings and recognise that most studies to date have<br />
assessed those most at risk of infection.<br />
• We crudely estimate that there are around 30,200 drug users currently in contact<br />
with services in the <strong>North</strong> <strong>West</strong>. Using estimates of the proportion of these injecting<br />
drugs, and applying the hepatitis C prevalence of 53% found in this study, we<br />
estimate that there are 12,800 people currently chronically infected with hepatitis C.<br />
Of these, 2,600 will go on to develop serious liver damage (cirrhosis or hepatic<br />
carcinoma) (Section 5.1). This figure does not include the hidden population of drug<br />
users, previous or new users entering the drug-using population.<br />
<strong>Health</strong> Authorities should anticipate the increase in treatment costs associated with<br />
treating this high number of patients with liver damage over the next twenty years.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
3
• Those who are infected with hepatitis C are four times more likely to also be<br />
infected with hepatitis B (Section 4.1). Co-infection increases the risk of<br />
progression to serious disease.<br />
Current hepatitis B vaccination programmes should attempt to protect people<br />
early in their drug injecting career before exposure to hepatitis C.<br />
• Having ever visited prison, and the number of prison stays, were both strong<br />
predictors of hepatitis C infection (Figure 1). Prison represents a potential injecting<br />
and non-injecting risk for hepatitis C. For example sharing of personal items such<br />
as razors may lead to infection, and those few study participants infected but not<br />
identified as injectors were more likely to have been in prison.<br />
More awareness of these other, albeit low risk, activities is needed generally but in<br />
particular in prisons.<br />
• Chaotic behaviours such as polydrug use (Figure 3), use of less commonly misused<br />
drugs (Section 4.3) and a longer history of injecting (Figure 2) all predicted hepatitis<br />
C infection.<br />
Harm reduction measures can be targeted at such high risk groups and predictors<br />
identified in this study can be used as indicators as to which populations or<br />
individuals are at most risk of infection or most likely to be infected.<br />
• Significant levels of sharing were revealed. Almost 40% had shared some form of<br />
injecting equipment over the previous four weeks, and 7% had shared needles<br />
(Table 4). Consistent with more chaotic behaviour, sharing injecting equipment is<br />
more likely to occur in those with polydrug use (Section 4.5). Also, sharing injecting<br />
equipment is most common in new injectors (those who have been injecting for up<br />
to five years) (Figure 5).<br />
Work is urgently needed to reach young vulnerable groups of drug users who<br />
have recently begun injecting or may progress to injecting drugs. Such work<br />
requires education on the risks of injecting to reduce high risk behaviours or<br />
ideally prevent them even before they begin.<br />
4<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
• A previous positive result for hepatitis C did not appear to result in a change in<br />
sharing behaviour (Section 4.4). However, those who had presented for previous<br />
tests were more likely to be reformed sharers (i.e. not currently sharing). This may<br />
be because counselling received at the time of the test was successful in reducing<br />
subsequent risk behaviour regardless of the actual results of the test. However, it<br />
may relate to those asking for a test already having decided to protect their health.<br />
Further work should examine in more detail the links between hepatitis C testing<br />
and the identified reduction in sharing behaviour.<br />
• Sharing injecting equipment is more likely to occur in smaller groups of fellow<br />
users (Figure 4), possibly because the user feels safe among friends or with a<br />
partner. The high prevalence of hepatitis C in drug users in the <strong>North</strong> <strong>West</strong> means<br />
sharing with anyone carries a high risk of hepatitis C infection.<br />
Information about the risks of sharing should stress this includes close friends and<br />
sexual partners. <strong>Health</strong> information should also help users address the problems<br />
around refusing to share with a partner.<br />
A CKNOWLEDGMENTS<br />
We would like to thank staff at each drug unit for recruiting subjects and<br />
administering questionnaires and the drug unit clients for taking part in the survey. We<br />
thank Rod Thomson and the <strong>North</strong> <strong>West</strong> health authorities for supporting this study,<br />
Gerry Hale for his help in co-ordinating the project, and Nick Beeching (Infectious<br />
Disease Unit, University Hospital Aintree) and Diana Leighton (<strong>Public</strong> <strong>Health</strong> Sector,<br />
Liverpool John Moores University) for comments on the manuscript. Andrew Weild<br />
(PHLS Communicable Disease Surveillance Centre) and David Hillier (Prison <strong>Health</strong><br />
Policy Unit) provided helpful information on current policy on hepatitis C education for<br />
prisoners. Finally, we thank Colin Heron for assistance with the production of this report.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
5
C ONTENTS<br />
Summary 2<br />
Aims 2<br />
Key Findings and Recommendations 3<br />
Acknowledgments 5<br />
1 Introduction 8<br />
1.1 Background 8<br />
1.2 Transmission 8<br />
1.3 Prisons 10<br />
1.4 Drug use in the <strong>North</strong> <strong>West</strong> 11<br />
1.5 Harm reduction policies 13<br />
1.6 Screening 13<br />
1.7 Tests for hepatitis C 14<br />
1.8 Disease course and treatment 14<br />
2 Aims and Objectives 16<br />
3 Methods 17<br />
3.1 Subjects 17<br />
3.2 Questionnaire 17<br />
3.3 Testing 18<br />
3.4 Statistics 18<br />
4 Results 19<br />
4.1 Comparison of injectors and non injectors 19<br />
4.2 Contact groups 21<br />
4.3 Predictors of hepatitis C and hepatitis B infection 23<br />
4.4 Previous hepatitis C test history 29<br />
4.5 Predicting sharing behaviour 30<br />
4.6 Blood donation 32<br />
5 Discussion 33<br />
5.1 Contact Groups 33<br />
5.2 Co-infection between hepatitis B and hepatitis C 34<br />
5.3 Risk factors 34<br />
5.4 Effects of testing on risk behaviour 35<br />
5.5 Sharing behaviour 36<br />
5.6 Blood Donation 37<br />
5.7 Further research 37<br />
5.8 Conclusions and Recommendations 38<br />
References 40<br />
6<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
List of tables<br />
Table 1 Basic results 19<br />
Table 2 Hepatitis C and B status as determined during this study 22<br />
and recall of testing history in relation to contact type<br />
Table 3 Effects of risk factors on the prevalence of hepatitis C and 24<br />
hepatitis B infection<br />
Table 4 Percentage of individuals sharing injecting equipment 27<br />
(ever and in the previous four weeks) by current<br />
serostatus and test history<br />
Table 5 Percentage (number) of subjects using and injecting 28<br />
each type of drug<br />
List of figures<br />
Figure 1 Percentage of injecting drug users with hepatitis C and B 23<br />
infection against number of times individuals have been<br />
in prison<br />
Figure 2 Percentage of drug users infected with hepatitis C and B 25<br />
against length of history of injecting drug use<br />
Figure 3 Percentage of injecting drug users with hepatitis C and B 26<br />
infection against number of different drugs injected<br />
during lifetime<br />
Figure 4 Percentage of injecting drug users sharing injecting 30<br />
equipment stratified by size of the group of fellow drug<br />
takers present when last injecting<br />
Figure 5 The percentage of injecting drug users sharing any 31<br />
form of injecting equipment in the previous four weeks<br />
(needles, syringes or other paraphernalia), categorised<br />
by time since first injected<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
7
1. INTRODUCTION<br />
1.1 Background<br />
Viruses such as the human immunodeficiency virus (HIV), hepatitis C and hepatitis B<br />
that are transmitted through blood pose a major health threat particularly for people<br />
who inject drugs. Amongst these viruses, hepatitis C represents a growing concern for<br />
several reasons. Firstly, previous studies in the UK and Ireland suggest that its<br />
prevalence is extremely high among injecting drug users (IDUs) (between 60% and<br />
90%: Smythe et al.1998; Goldberg et al. 1998; Lamden et al. 1998; Best et al. 1999).<br />
Secondly, unlike for hepatitis A and B, no vaccine is as yet available, and the rapid<br />
mutation rate of the hepatitis C virus makes the imminent development of one<br />
unlikely (Liang et al. 2000). Thirdly, a high proportion of cases (around 80%) become<br />
chronically infected, and of these, around 20% go on to develop serious liver damage,<br />
such as cirrhosis or hepatic carcinoma (Theodore & Fried 2000). Finally, current<br />
treatment is often ineffective, with even the most advanced treatment available<br />
clearing the infection on only 40% of occasions (Liang et al. 2000).<br />
Key objectives in the Government's ten year drug strategy Tackling Drugs to Build a<br />
Better Britain (1998) include increasing the number of users entering treatment<br />
programmes, reducing the number of young people using drugs and reducing the<br />
levels of injecting and sharing of equipment. If these targets are met, the number of<br />
new hepatitis C infections would decrease. However, currently there are large numbers<br />
of users in the <strong>North</strong> <strong>West</strong> who share equipment who are either infected with hepatitis<br />
C or at risk of infection (see Section 1.4). The exact scale of the problem is difficult to<br />
assess as individuals typically have many years of asymptomatic infection before<br />
presenting to health services with chronic disease. What is clear though, is that the<br />
high prevalence among IDUs currently accessing drug treatment services suggests<br />
considerable future health care costs in treating the expected associated rise in liver<br />
failure and associated morbidity (Leal et al. 1999), as well as the health and social costs<br />
of prolonged morbidity and disability to those infected with hepatitis C (Dolan 1997).<br />
1.2 Transmission<br />
Hepatitis C is primarily transmitted through blood. Prior to screening of blood<br />
donations, recipients of blood transfusions or blood products were at risk of infection.<br />
As a result, an estimated 4000 haemophiliacs in the UK have been infected through<br />
blood products (The Haemophilia Society 1999) and the total number of people<br />
infected through blood or blood product transfusion and organ donation is estimated<br />
to be around 7500 (Syed & Snee 1997; CDSC <strong>North</strong> <strong>West</strong> 1999). The risk of infection<br />
through this route dropped dramatically with the introduction of effective heat<br />
treatment in 1986 (1987 in Scotland) (The Haemophilia Society 1999). The risk then<br />
dropped further with the introduction of hepatitis C antibody screening in 1991.<br />
The group now at the highest risk is IDUs.<br />
8<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
The high prevalence of infection among IDUs means that, when sharing needles or<br />
other injecting equipment occurs, the probability of sharing with an infected individual<br />
is very high. Furthermore, infection among IDUs occurs very quickly; the risk of infection<br />
for each year of injecting has been estimated at between 15% and 30% (Rezza et al.<br />
1996; Hagan et al. 1999), but results of a recent Australian study suggest that the risk<br />
may be as high as 80% per year injecting in younger users (van Beek et al. 1998).<br />
Compared to HIV, hepatitis C is transmitted in blood relatively easily. For example, the<br />
probability of becoming hepatitis C positive following a needlestick injury (3% to 9%)<br />
is ten times higher than with needlesticks involving HIV (0.3%) (Coutinho 1998). Thus,<br />
although the length of time since onset of injecting behaviour is a strong predictor of<br />
hepatitis C infection, a large proportion of users get infected within a year or two of<br />
beginning injecting (e.g. Smythe et al. 1998; Lamden et al. 1998). Furthermore,<br />
because of its infectivity, it is not only sharing needles that poses a risk, but also<br />
syringes, spoons, filters, water; in other words any material used for the preparation of<br />
the drug and potentially shared between users (collectively called paraphernalia)<br />
(Renton & Main 1996). This ease of transmission and persistence of infective particles<br />
increases the probability that those injecting in the presence of other injectors will come<br />
into contact with the virus even if the user is taking fairly stringent precautions.<br />
There has been a degree of behaviour change (such as not sharing needles) among IDUs<br />
towards adopting safer injecting practice in order to avoid HIV infection (Stimson 1995).<br />
However, the same awareness and behavioural change is yet to be realised for other<br />
injecting equipment. Thus, many studies report a high prevalence of sharing injecting<br />
equipment: for example 94% of IDUs in Berlin had shared syringes more than one<br />
hundred times (Stark et al. 1996) and among British IDUs, 80% had shared some form of<br />
injecting equipment in the last month (Hunter & Stimson 1998). Even if the probability of<br />
contracting hepatitis C after a single occasion of sharing paraphernalia is relatively low,<br />
the likelihood of infection can become high if such sharing behaviour is frequent.<br />
Seventy percent of people currently living with hepatitis C have had their infections<br />
attributed to injecting drug use, 10% to blood products, 2% to occupational exposure<br />
(i.e. needlestick injuries), up to 2% to household contact, 1-2% to tattooing and related<br />
procedures and up to 1% to sexual contact, with many of the remaining cases having an<br />
unknown route of transmission (Dolan 1997). This high proportion of unattributed cases<br />
remains an enigma in the study of the epidemiology of hepatitis C. Unlike HIV and<br />
Hepatitis B, transmission of hepatitis C through sex appears to be relatively rare<br />
(Zylberberg et al. 1999). For example, spouses of haemophiliacs infected with hepatitis C<br />
do not appear to be infected at a higher rate than the general population (Brackmann et<br />
al. 1993; Thomas 2000). Hepatitis C virus particles have been isolated from the semen of<br />
infected men in some studies but not others (Semprini et al. 1998; Zylberberg et al.<br />
1999). Although case studies suggest that sexual transmission is possible, the actual risk<br />
appears too low to be accurately quantified (Renton & Main 1996). In the rare cases<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
9
where sexual partners do get infected, it is hard to rule out the possibility that they<br />
were infected via other forms of contact, for example by regularly sharing toothbrushes<br />
or razors, or via unacknowledged injecting drug use (Zylberberg et al. 1999; Thomas<br />
2000). Population studies also indicate the relatively unimportant role of sexual<br />
transmission. In Thailand, where the prevalence of hepatitis C among IDUs is high<br />
(85%), the prevalence among high class sex workers is relatively low at 2% (Suganuma<br />
et al. 1998), although in part this low prevalence may be due to successful efforts to<br />
promote condom use. Studies in the USA (Osella et al. 1998) and Australia (Bodsworth<br />
et al. 1996) support the view that sexual behaviour is also not an important<br />
transmission route among homosexual men.<br />
For pregnant IDUs who are infected with hepatitis C, there is a 3-10% risk of passing<br />
on the infection to the child, with risk of infection increasing with increasing viral load<br />
of the mother (Resti et al. 1998; Garland et al. 1998) and with co-infection with HIV<br />
(Resti 1999). Mother to child infection may represent the fastest growing category of<br />
infection route (Dolan 1997). There may also be a risk of transmitting hepatitis C via<br />
breast feeding if the mother has a high viral load, either due to infected breast milk or<br />
traces of blood from cracked nipples (Kumar & Shahul 1998). Other factors that are<br />
known to damage the liver may be linked to the probability of contracting hepatitis C<br />
infection when exposed to the virus (e.g. excessive alcohol and drug use even in the<br />
absence of injecting) (Strugo et al. 1998; Rodriguez et al. 1998). Overall, however, now<br />
that blood products are routinely screened for the hepatitis C virus, forms of<br />
transmission other than the use of contaminated injecting equipment are comparatively<br />
rare. Consequently, extremely efficient transmission through blood and relatively low<br />
rates of transmission via sexual contact and other routes has led to a pool of infection<br />
being built up amongst injecting drug users. While generally this may pose a relatively<br />
small risk to other populations, in particular settings where incidental exposure to<br />
infected blood may occur, risks may be significant. One such setting is prisons.<br />
1.3 Prisons<br />
Previous studies have found that having been to prison is a significant risk factor for<br />
hepatitis C infection (Crofts et al. 1993; McBride et al. 1994; De Mercato et al. 1995;<br />
Stark et al. 1996; Weild et al. 2000). Many individuals who are dependent on drugs<br />
spend periods of time in prison because they commit crimes to support their habit<br />
(Eaton et al. 1998). Moreover, a considerable proportion of drug users entering prison<br />
have not previously been in contact with drugs treatment services and are therefore not<br />
in receipt of treatment for their drug addiction or information on harm minimisation<br />
(Birtles et al. 1998; Weild et al. 2000). In one prison in Merseyside, over a quarter of all<br />
new prisoners reported ever having injected drugs (Bellis et al. 1997). Of those who had<br />
been imprisoned previously, 16% had injected drugs in prison, and over half of those<br />
had shared equipment in prison (Bellis et al. 1997). In a recent survey of prisons in<br />
10<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
England and Wales, over a quarter of inmates were found to have previously injected<br />
drugs, 31% of whom had injected in prison, and of those, three quarters had shared<br />
injecting equipment (Weild et al. 2000). In Scottish prisons, over a third of prisoners had<br />
a history of injecting drug use (Gore et al. 1999). Correspondingly, the prevalence of<br />
hepatitis C in prisons is high. In England and Wales, 9% of all adult prisoners (20% of<br />
adult males on remand) were hepatitis C positive (Weild et al. 2000). In Scotland, 20%<br />
of all prisoners were hepatitis C positive (Gore et al. 1999). Once in prison, evidence<br />
suggests that half of drug users continue to use and injecting equipment, when<br />
available, is likely to be shared by a lot of people (Eaton et al. 1998).<br />
Prisons are confined environments where the prevalence of hepatitis C is likely to be<br />
high (Gore et al. 1999; Weild et al. 2000). Even in the absence of sharing injecting<br />
equipment, occurrences of blood to blood contact, such as sharing of razors and other<br />
personal items, or involvement in fights, are likely to be frequent. Although in isolation<br />
each individual event may present a relatively low risk of hepatitis C exposure, several<br />
such events over time may account for additional cases of infection. Thus, in Scottish<br />
prisons 3% (Gore et al. 1999) and in English and Welsh prisons 2% (Weild et al. 2000)<br />
of the non-injectors were positive, a higher prevalence than that estimated for the<br />
general population, at less than 1% (Renton & Main 1996; Dolan 1997).<br />
1.4 Drug use in the <strong>North</strong> <strong>West</strong><br />
The <strong>North</strong> <strong>West</strong> has the second highest rate of problematic drug users accessing drug<br />
treatment services in the UK at 73 per 100,000 according to the national monitoring<br />
system, the Drugs Misuse Database (DMD) (Birtles et al. 1999). This provides a national<br />
comparison of drug use, but hugely underestimates the number of individuals even in<br />
treatment, let alone those using other services, such as agency based syringe exchange<br />
schemes (SES), pharmacy-based SES and outreach. More injectors again will not be in<br />
contact with any service at all (Hardi & Bellis 1999) and are thus ommitted from<br />
monitoring. In those areas of the <strong>North</strong> <strong>West</strong> (i.e. Merseyside and Cheshire) for which<br />
the actual numbers of users attending drugs agencies has been ascertained, the<br />
numbers of individuals reported to the DMD each year underestimates actual<br />
attendance by around one third (Birtles & Bellis 2000). In fact, approximately 9,000<br />
drug users attend Specialist Drugs Agencies each year with 3,500 attending agency<br />
based SES and 4,500 attending pharmacy based SES in Merseyside and Cheshire.<br />
Some people use more than one agency type, giving a total of 14,670 individuals<br />
accessing some form of treatment in Merseyside and Cheshire alone (Birtles & Bellis<br />
2000). If this rate of drug use is assumed to apply to the rest of the <strong>North</strong> <strong>West</strong><br />
(although DMD data suggest that rates in the rest of the <strong>North</strong> <strong>West</strong> are higher), then a<br />
crude extrapolation on a population basis gives a conservative estimate of 40,200 drug<br />
users in contact with services in the <strong>North</strong> <strong>West</strong>. Not all of these will have injected<br />
drugs: around three quarters of users reporting to the DMD have disclosed injecting<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
11
ehaviour at some stage in their drug using career (although the rates of injecting<br />
among those attending SES and pharmacy SES are likely to be higher), giving a<br />
conservative estimate of 30,200 IDUs. However, statistical estimations of the hidden<br />
population of drug users in Merseyside (based on the overlap between the number of<br />
people contacting drugs agencies and those arrested by the police for drug crime)<br />
suggest that only about half of problematic heroin users are in contact with services<br />
(Hardi & Bellis 1999). Although this would suggest that there may be twice as many<br />
problematic drug users in the <strong>North</strong> <strong>West</strong> than we have estimated, the proportion of<br />
the hidden population of drug users who are injectors cannot be determined.<br />
In the <strong>North</strong> <strong>West</strong> of England, 67% of IDUs requesting a hepatitis test tested positive<br />
for hepatitis C (Lamden et al. 1998). Since the sample was drawn from those requesting<br />
a test, only a subset of the total population of IDUs was included. Little is known about<br />
potential differences in patterns of injecting and sharing between groups attending<br />
different agencies or none at all. A Scottish survey found little difference between<br />
prevalence of hepatitis C among IDUs recruited from SES, treatment centres and on the<br />
street (Taylor et al 2000). However, a survey of HIV prevalence among female IDUs in<br />
London found a higher prevalence in those recruited from the community than in those<br />
attending treatment agencies (Judd et al. 1999). Therefore, the assessment of the levels<br />
of hepatitis C in the wider drug using communities requires sampling individuals<br />
attending different services as well as those not in contact with services at all (Aim 1 of<br />
this study).<br />
Of the new agency episodes reported to the DMD, 73% were clients who reported<br />
having injected at some stage previously, and of those, 48% reported ever having<br />
shared injecting equipment (Birtles et al. 1999). A high proportion of those using drugs<br />
have periods of imprisonment, where continued drug use and levels of sharing are<br />
high (Eaton et al. 1998; section 1.3). However, estimations of sharing behaviour often<br />
rely on a single question on sharing behaviour that may not measure the extent of<br />
sharing (Hunter & Stimson 1998). In depth questions on sharing behaviour of IDUs in<br />
the <strong>North</strong> <strong>West</strong> revealed that around 80% of IDUs had shared injecting equipment in<br />
the previous four weeks (Speed & Bennet 1997). Moreover, there was a lack of<br />
knowledge among IDUs as to the risks of sharing injecting paraphernalia compared to<br />
the more well known risks of sharing needles and syringes (Speed & Bennett 1997).<br />
The number of people in contact with services who share injecting equipment in the<br />
<strong>North</strong> <strong>West</strong> can be estimated, assuming 80% of the estimated 30,200 IDUs share.<br />
This leads to the prediction that there are around 24,100 current drug users who have<br />
shared injecting equipment. Conservatively, this ignores those that have used drugs in<br />
the past but now abstain from drugs and do not use drugs services.<br />
12<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
1.5 Harm reduction policies<br />
Compared to the high prevalence of hepatitis C, the prevalence of HIV among IDUs in<br />
the UK has remained low at under 1% (Unlinked Anonymous Surveys Steering Group<br />
1999). This low prevalence has often been attributed to the prompt introduction in the<br />
UK of harm reduction strategies such as syringe exchange schemes (SES) (Stimson<br />
1995). In contrast, in the USA, where such schemes were not adopted very rapidly,<br />
there is a large pool of IDUs infected with HIV (Stimson 1995). However, the high<br />
prevalence of hepatitis C infection suggests that this pragmatic approach to decreasing<br />
the spread of blood borne infections has been less successful at preventing hepatitis C.<br />
Several studies report no decline in incidence or prevalence of hepatitis C after<br />
adoption of harm reduction policies such as methadone treatment and SES (Lamden et<br />
al. 1998; Hagan et al. 1999; Crofts et al. 1997) and where effects are reported the<br />
reduction is rather small (Rezza et al. 1996). However, the decline in hepatitis C<br />
prevalence among IDUs in Scotland has been attributed to the introduction of SES<br />
(Goldberg et al. 1998; Taylor et al. 2000). Similarly, in Switzerland, Broers et al. (1998)<br />
found a decrease in prevalence from 91% to 30%. These mixed findings on the effect<br />
of harm reduction measures are difficult to interpret.<br />
Studies evaluating harm reduction policies need to take into account many factors<br />
such as the advice given and the desire of the clients to change their behaviour as well<br />
as established trends prior to the intervention. Relevant to this study however, factors<br />
that could lead to harm reducing behaviour need to be identified in order to measure<br />
any effect they may have on hepatitis C infection. One potential factor still in need of<br />
study is whether having a hepatitis C test, and consequently knowledge of serostatus,<br />
has an effect on behaviour (Aim 4 of this study).<br />
1.6 Screening<br />
Due to the limited success of treatment, the benefits of screening or even offering<br />
tests for hepatitis C have been questioned from a clinical perspective. At present<br />
treatment is not offered routinely to anyone with hepatitis C, and there are no<br />
nationally agreed guidelines for managing hepatitis C infections and no screening<br />
programmes for drug users, leaving health authorities to respond individually (Syed &<br />
Snee 1997; CDSC <strong>North</strong> <strong>West</strong> 1999). Calculations show that, despite the high cost of<br />
treatment, screening and treatment may be cost effective in the long term (Leal et al.<br />
1999; Dusheiko & Roberts 1995). In addition, a screening programme would allow<br />
monitoring and counselling of infected individuals. Such counselling may also<br />
discourage other risk behaviours that may aggravate hepatitis C infection, for example<br />
alcohol use (Datz et al. 1999; Theodore & Fried 2000). Moreover, individuals'<br />
knowledge of hepatitis C status may encourage safer injecting behaviour, either to<br />
avoid infection or to avoid infecting others ('the altruistic response'). In a study of IDUs<br />
infected with HIV in several European countries, those knowing their status were more<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
13
likely to use a condom and less likely to pass on used injecting equipment to others<br />
(Schlumberger et al. 1999). However, this response is only likely if individuals who have<br />
been tested perceive and understand their result correctly. In a study of IDUs in<br />
London, over half of people who had previously been for a hepatitis C test either did<br />
not know their status or incorrectly thought themselves to be negative (Best et al.<br />
1999), although some of these could have had correct recall of their test result and<br />
subsequently become infected. To understand the potential impact of wider screening<br />
it is necessary to determine whether correct perceptions of test results are related to<br />
risk taking behaviour IDUs (Aim 4 of this study).<br />
1.7 Tests for hepatitis C<br />
A hepatitis C infection can be detected through the identification of specific<br />
antibodies. However, this does not distinguish past from present infection: the 20%<br />
who have naturally removed the infection, or those who have had successful<br />
treatment, will still test positive. Current infection is confirmed by the presence of the<br />
virus in the blood (by detecting viral RNA) using polymerase chain reaction (PCR) tests.<br />
As the disease progresses, the virus and / or the cellular immune response to hepatitis<br />
C virus damages the liver cells and liver enzymes are released into the blood.<br />
Measurement of the level of enzymes in the blood can provide information on the<br />
course of the disease and the effectiveness of treatment. However, the most accurate<br />
way to measure the progression of damage to the liver is to take a biopsy of the liver<br />
and perform microscopic investigation of its structure (Dusheiko et al. 1996).<br />
1.8 Disease course and treatment<br />
The outcome of infection by hepatitis C is very variable (Theodore & Fried 2000). Initial<br />
acute infection with hepatitis C may be accompanied by transient flu-like symptoms,<br />
but in many cases the infection passes unnoticed. Calculations based on those infected<br />
with the virus via blood transfusions indicate that of those with acute infection, the<br />
majority (around 80%) develop chronic hepatitis C infection and remain infectious to<br />
others, with 20% of those progressing to cirrhosis over a 20 year period (Theodore &<br />
Fried 2000). After development of cirrhosis, approximately 1% per year go on to<br />
develop liver cancer (Tong et al. 1995). When severe liver damage occurs, a liver<br />
transplant can be given but the new liver will eventually become infected. However,<br />
progression to severe disease is very variable and is influenced by gender (males are<br />
more susceptible), alcohol use, the genotype of the virus and the genes of the host's<br />
immune system (Datz et al. 1999; Theodore & Fried 2000). The consequences for<br />
those acquiring the infection via injecting drug use are even less well known.<br />
Because IDUs tend to contract the infection at a younger age (on average), and may<br />
be exposed on more than one occasion to different strains of the virus, the risk of<br />
serious liver disease may be higher (Renton & Main 1996; Dolan 1997).<br />
14<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
A course of treatment usually comprises injections of interferon alpha three times a<br />
week for a year. This treatment successfully clears the virus in only 20% of cases<br />
(Liang et al. 2000), with some individuals simply not responding and some relapsing<br />
after treatment finishes. Failed treatment may increase the severity of the eventual liver<br />
disease (Dusheiko et al. 1996). However, the latest treatment, combination therapy<br />
with interferon and ribavirin, increases the success rate to 40% (Liang et al. 2000).<br />
Combination therapy is expensive, at around £6,000 per patient (but the cost of this<br />
may be considerably less than the social and medical costs of letting the disease<br />
progress untreated: Leal et al. 1999). Treatment is associated with unpleasant side<br />
effects such as nausea and depression and requires a high level of compliance<br />
(Liang et al. 2000). In contrast, the behavioural characteristics of IDUs can be chaotic<br />
and consequently the demands of the treatment regime have been considered by<br />
some to make it unsuitable for this group of patients (Renton & Main 1996).<br />
Furthermore, since the risk of re-infection is high (immunity is not obtained even if the<br />
infection is cleared from the body: Liang et al. 2000), it is generally only recommended<br />
for individuals who are definitely drug free.<br />
Although there is no evidence that continued drug use increases progression to severe<br />
liver disease, alcohol use and co-infection with other viral infections such as HIV and<br />
hepatitis B do appear to increase the risk of serious disease (Pol et al. 1998; Tagger et<br />
al. 1999; Allory et al. 2000). Conversely, hepatitis C infection appears not to accelerate<br />
the course of HIV disease (Haydon et al. 1998; Staples et al. 1999), although this may<br />
depend on the genotype of the hepatitis C virus (Dieterich 1999). The management of<br />
treatment in cases of co-infection with HIV is complex (Dusheiko et al. 1996) and there<br />
is an increased risk of transmission of hepatitis C from mother to child (Resti 1999).<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
15
2. AIMS AND O BJECTIVES<br />
Reviewing current knowledge about hepatitis C epidemiology reveals a number of<br />
factors that are at present unmeasured but necessary to implement effective and<br />
economic policies for hepatitis C prevention and treatment. Key amongst these is the<br />
level of infection in wider drug injecting communities in the <strong>North</strong> <strong>West</strong> (not just those<br />
requesting a test or in treatment at specialist drug agencies). Equally however,<br />
additional data are needed on the risk behaviours associated with infection and<br />
information is required on whether and how individuals change such behaviour once<br />
aware of their hepatitis C serostatus. Consequently, a group of IDUs in the <strong>North</strong> <strong>West</strong><br />
were recruited in order to:<br />
1. compare the prevalence of hepatitis C among drug users accessing different types<br />
of service, and among drug users not accessing services<br />
2. establish the extent of co-infection of hepatitis C and hepatitis B<br />
3. elucidate risk factors for hepatitis C infection<br />
4. explore the effect of knowledge of previous hepatitis test results on behaviour<br />
5. identify factors that predict sharing of equipment<br />
6. establish a cohort for follow up and establish feasibility of monitoring hepatitis C<br />
infection among drug using populations using saliva samples (results not covered<br />
in this report).<br />
16<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
3. METHODS<br />
3.1 Subjects<br />
Study participants were recruited and laboratory analyses of samples undertaken<br />
between 1997 and 1999 for the Wirral sample and between 1998 and 1999 for the<br />
Manchester sample. The aims of the study necessitated drawing drug users from a<br />
wide variety of services as well as attracting groups of users not currently in contact<br />
with services. Consequently, subjects were either in contact with treatment agencies in<br />
Drugs <strong>North</strong> <strong>West</strong> and Wirral Drugs Service or not in contact with any drugs services.<br />
There were 110 people recruited through community drug teams, 112 from syringe<br />
exchange schemes and 23 through outreach. Forty five people were recruited on their<br />
first ever visit to a drugs agency, and 60, who were not in contact with treatment<br />
agencies, were recruited via a snowballing technique through the existing service<br />
users. Forty eight people presented at Wirral Drugs service specifically to request either<br />
an HIV, hepatitis B or C test and were invited to join the study (referred to as 'self<br />
presenters'). Nine further drug users were recruited through other sources (for<br />
example, some were resident in an in-patient facility).<br />
3.2 Questionnaire<br />
Subjects completed a questionnaire ascertaining drug taking, sharing of needles and<br />
other equipment, previous hepatitis B and C test history and sexual behaviour. Drug<br />
taking history elicited information on whether the subject had ever used or injected<br />
each of 14 named drugs, and whether they had used or injected these same drugs in<br />
the previous four weeks. Participants were also given the opportunity to identify any<br />
drug other than those on the list that they had used or injected. Sharing questions<br />
identified whether the subject had ever, or in the previous four weeks, shared needles,<br />
spoons, syringes, filters or other injecting equipment (such as water used in the<br />
preparation of drugs). The age of first use of drugs, the age of first injecting behaviour<br />
and the size of the group of fellow users on the previous occasion that the subject had<br />
injected was determined. Subjects were also asked if they had ever been to prison, and<br />
if so, on how many occasions. Sexual behaviour questions determined how many male<br />
and female partners the subjects had ever had, and had in the previous four weeks,<br />
and what their usual method of contraception had been. Questions on previous test<br />
history asked whether subjects had ever taken tests for hepatitis C or hepatitis B, and<br />
if so, what their results had been.<br />
Questionnaires were self-administered, but a drug worker was present if any clarification<br />
of questions was needed. Participants had a choice of named or anonymous participation.<br />
Those who were named were notified of their test result and consequently formed part of<br />
a cohort for follow up (see Aim 6). Two hundred and fifty nine (64%) volunteered to be<br />
part of the follow up group and therefore provided identifying details.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
17
3.3 Testing<br />
Subjects gave blood and saliva samples 1 . Blood samples were tested by the Liverpool<br />
and Manchester Laboratories of <strong>Public</strong> <strong>Health</strong> Laboratory <strong>North</strong> <strong>West</strong> for hepatitis B<br />
core antibodies and antibodies to hepatitis C. These measures give an indication of<br />
infection at some point (previous or current) with the hepatitis viruses. In the case of<br />
hepatitis B, only around 5% become chronic carriers of the virus, so many of the<br />
positives will be the result of previous infection. For hepatitis C, around 80% of the<br />
positive results are likely to be people with chronic infection. In this study, having ever<br />
been infected was used as the best measure of risk factors for infection. Consequently<br />
all analyses refer to whether hepatitis C or B antibodies were detected in samples.<br />
All samples testing positive for hepatitis C antibody were re-tested with a second enzyme<br />
linked immunosorbent assay (ELISA) test in order to confirm the positive hepatitis C<br />
antibody test. Samples remaining inconclusive were analysed using recombinant<br />
immunoblot assay (RIBA-III) and polymerase chain reaction (PCR). Individuals testing<br />
positive for hepatitis C were referred to local clinical services for full clinical examination<br />
and appropriate assessment for treatment, counselling and monitoring.<br />
3.4 Statistics<br />
Comparisons were made using chi-square tests and t tests between those who had<br />
ever been or never been hepatitis B and C positive, between sharers of equipment and<br />
non-sharers, and between those taking previous hepatitis B and C tests and those not.<br />
Univariate results are presented as means and odds ratios (OR) with 95% confidence<br />
intervals (CI). Then, significant variables were entered into multivariate logistic<br />
regression models to identify which were independent predictors of hepatitis B and C<br />
infection, sharing injecting equipment and taking a hepatitis B or C test. Results of<br />
multivariate analyses are presented as adjusted OR and 95% CI.<br />
1 The saliva samples were retained for comparison with the blood test results to ascertain the potential of saliva<br />
testing as a method of detecting hepatitis C infection in this type of survey. Results will be presented elsewhere.<br />
18<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
4. RESULTS<br />
A basic breakdown of results, split by those who had injected at some stage during<br />
their life and those who claimed never to have injected, is given in Table 1.<br />
4.1 Comparison of injectors and non injectors<br />
There were 407 completed questionnaires, 21 of which were excluded because their<br />
matching hepatitis C results were equivocal or there was insufficient blood sample for<br />
analysis (5 and 17 respectively). Of the remaining 386, 45 claimed never to have<br />
injected. A comparison of those who have never injected with those who have is<br />
shown in Table 1a. Injectors were more likely to be male, were more likely to have<br />
been in prison, had been to prison on more occasions, and were more likely to have<br />
taken a prior hepatitis C test. Injectors were over four times more likely to be infected<br />
with hepatitis C (odds ratio and confidence intervals, OR = 4.45, CI 1.73-11.4).<br />
Table 1a: Basic results: characteristics of injecting & non-injecting drug users<br />
Injectors Non injectors P<br />
Number 341 45<br />
Mean Age (years) 29.5 27.9 NS 1<br />
Percent (number) male 72.3% (245) 42.2% (19) 3 sexual partners<br />
in previous 12 months<br />
4.1% (14) 13.3% (6) 0.009 2<br />
15.0% (51) 31.1% (14) 0.023 2<br />
NS non significant, 1 t test, 2 chi-square test, 3 of those who had been to prison at least once,<br />
4 other than HIV, hepatitis B or C<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST<br />
19
Table 1b: Basic results: behaviours of injecting drug users<br />
Sharing in previous 4 weeks<br />
Needles 7.3% (25)<br />
Syringes 7.3% (25)<br />
Spoons 34.6% (118)<br />
Filters 27.6% (94)<br />
Other 5.0% (17)<br />
Any 37.8% (129)<br />
Sharing ever<br />
Needles 53.7% (183)<br />
Syringes 53.1% (181)<br />
Spoons 82.1% (280)<br />
Filters 71.6% (244)<br />
Other 23.2% (79)<br />
Any 85.0% (290)<br />
Size of group when injecting<br />
Alone 24.6% (82)<br />
One other 40.5% (135)<br />
2 - 5 others 30.9% (103)<br />
More than 5 others 3.9% (13)<br />
Age at first injection<br />
Of the 45 who claimed never to have injected, eight had been or were currently<br />
infected with hepatitis C. These infected non-injectors were nearly 20 times more likely<br />
to have been in prison than non infected non-injectors (seven out of eight compared<br />
to nine out of 25: odds ratio OR = 19.4, CI 2.1-180.7, X 2 = 10.23, P = 0.001), and<br />
were over twenty times as likely to have taken heroin in the previous four weeks<br />
(seven out of eight compared to nine out of 28; OR = 21.8, CI 2.4-201.7; X 2 = 11.46,<br />
P = 0.001). However, two of the individuals were recruited through SES which could<br />
suggest that some of these eight did not identify their real injecting status (although<br />
attendance at SES to access other services or accompany an injecting friend could not<br />
be ruled out).<br />
Subsequent analysis was limited to the 341 who claimed to have injected a drug at<br />
some stage in their life. Among this group, the prevalence of hepatitis C was 53.1%<br />
(181 people), 26.6% (89 people) had been infected with hepatitis B and 19.0%<br />
(65 people) had been infected with both hepatitis C and B. People who were positive<br />
for antibodies to one virus were over four times as likely to also be positive for the<br />
other (OR = 4.25, CI 2.42-7.46; P
Table 2: Hepatitis C and B status as determined during this study and recall of<br />
testing history in relation to contact type<br />
Hepatitis C<br />
SES Outreach CDT Self New Not in Other p 2<br />
presenting 1 (first contact) contact<br />
Number 104 17 88 42 41 40 9<br />
% hepatitis C antibody<br />
positive (this study)<br />
48.1 58.8 61.4 61.9 48.8 45.0 33.0 0.255<br />
% previously taken test 28.3 29.4 24.0 25.6 33.3 23.3 55.6 0.488<br />
% not previously taken test 65.1 64.7 63.0 67.4 50.0 65.1 44.4<br />
% do not know 6.6 5.9 13.0 7.0 16.7 11.6 0.0<br />
Number having taken a<br />
test previously<br />
30 5 24 11 14 10 5<br />
% positive (previous test) 36.7 40.0 37.5 45.5 21.4 50.0 20.0 0.782<br />
% negative (previous test) 46.7 40.0 50.0 27.3 50.0 50.0 40.0<br />
% don’t know (previous test) 16.7 20.0 12.5 27.3 28.6 0.0 40.0<br />
Hepatitis B<br />
Number 106 17 100 43 42 43 9<br />
% hepatitis B positive<br />
(this study) 24.0 6.7 33.0 41.0 20.0 22.5 11.1 0.067<br />
% previously taken test 42.5 41.2 42.0 39.5 42.9 34.9 55.6 0.066<br />
% not previously taken test 53.8 58.8 40.0 55.8 47.6 58.1 33.3<br />
% do not know 3.8 0.0 18.0 4.7 9.5 7.0 11.1<br />
Number having taken a<br />
test previously<br />
45 7 42 17 18 15 5<br />
% positive (previous test) 24.4 0.0 23.8 17.6 16.7 13.3 0.0 0.145<br />
% negative (previous test) 68.9 85.7 59.5 64.7 44.4 80.0 60.0<br />
% don’t know (previous test) 6.7 14.3 16.7 17.6 38.9 6.7 40.0<br />
1 People presenting at Wirral Drugs Service specifically to request either an HIV, hepatitis B or C test who were<br />
invited to join the study, 2 chi-square P values<br />
22<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
4.3 Predictors of hepatitis C and hepatitis B infection<br />
Using basic univariate analyses similar risk factors were found to predict both hepatitis<br />
B and C infections, as shown in Table 3. The most important factors were being in<br />
prison (and the number of occasions in prison: Figure 1), the length of time since the<br />
onset of injecting behaviour (Figure 2) and polydrug use (i.e. ever having injected more<br />
than one type of drug: Figure 3).<br />
Figure 1: Percentage of injecting drug users with hepatitis C and B infection<br />
against number of times individuals have been in prison<br />
% INFECTED<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
<strong>HEPATITIS</strong> C + <strong>HEPATITIS</strong> B +<br />
Never 1 2-5 6-9 10+<br />
NUMBER OF TIMES IN PRISON<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 23
Table 3: Effects of risk factors on the prevalence of hepatitis C and hepatitis B<br />
infection<br />
CHARACTERISTIC Hepatitis C Hepatitis B<br />
+ ve (n=181) -ve (n=160) P 1 +ve (n=89) -ve (n=245) P 1<br />
Being male 72.9% (132) 71.5% (113) NS 80.9% (72) 70.4% (171) *<br />
Being from Wirral 69.6% (126) 65.0% (124) NS 69.7% (62) 64.5% (158) NS<br />
Been in prison 72.4% (131) 51.3% (82) **** 77.5% (69) 56.7% (139) ****<br />
Lived abroad 14.4% (26) 12.5% (20) NS 13.5% (12) 13.9% (34) NS<br />
Shared equipment abroad 4.4% (8) 1.3% (2) * 3.4% (3) 2.9% (7) NS<br />
Length of injecting career **** ****<br />
Up to 5 years 9.4% (17) 20.6% (43) 8.0% (9) 17.9% (43)<br />
6-10 years 24.3% (44) 39.4% (90) 21.6% (19) 37.5% (90)<br />
11-15 years 27.1% (49) 23.1% (59) 27.3% (24) 24.6% (59)<br />
16-20 years 19.9% (36) 11.3% (34) 21.6% (19) 14.2% (34)<br />
21-25 years 13.3% (24) 1.9% (10) 15.9% (14) 4.2% (10)<br />
26+ years 4.4% (8) 1.9% (4) 5.7% (5) 1.7% (4)<br />
Number of drugs<br />
ever injected<br />
**** ****<br />
One 7.9% (14) 21.5% (34) 5.7% (5) 18.2% (44)<br />
2-5 44.4% (79) 60.1% (95) 49.4% (43) 54.1% (131)<br />
More than 5 48.8% (85) 18.4% (29) 44.8% (39) 27.7% (67)<br />
Sexual Behaviour<br />
More than 2 partners<br />
in 4 weeks 2<br />
3.9% (7) 4.4% (7) NS 4.5% (4) 3.7% (9) NS<br />
Number of partners<br />
in year 2<br />
* NS<br />
One 64.6% (117) 56.3% (90) 57.3% (51) 61.2% (150)<br />
2-3 24.3% (44) 24.4% (39) 29.2% (26) 23.3% (57)<br />
More than 3 11.0% (20) 19.4% (31) 13.5% (12) 15.5% (38)<br />
Sex with non UK resident 23.8% (43) 19.4% (31) NS 23.6% (21) 19.2% (47) NS<br />
Using contraception 49.7% (90) 50.6% (81) NS 50.6% (45) 49.0% (120) NS<br />
Using a condom 42.0% (72) 42.5% (68) NS 44.9% (40) 58.8% (144) NS<br />
Using pill 6.1% (11) 12.5% (20) ** 10.1% (9) 8.6% (21) NS<br />
1 univariate chi-square analysis, 2 analysis repeated on females only (because some females in this sample may<br />
use prostitution to support their drug use); however, there was no significant effect of multiple partners on<br />
hepatitis C or B infection. NS is non significant, * P
When non-injectors are included in the analysis (see Figure 2), the increase in infection<br />
occurs near to the onset of injecting, with those with five or fewer years of injecting<br />
having a prevalence of 34%. The prevalence of hepatitis C rose to 84% for those who<br />
had injected for over 20 years.<br />
Imprisonment, length of injecting career and polydrug use all remained independently<br />
significant in logistic regression analysis to predict hepatitis C infection: having been in<br />
prison corresponded with a 70% increase in risk (OR =1.71, CI 1.02-2.86, p = 0.041);<br />
injecting for 21 to 25 years corresponded with a seven-fold increase in risk compared with<br />
those who had injected for up to five years (OR =7.59, CI 1.91-30.17 p = 0.0376); and a<br />
history of injecting multiple types of drugs (compared with having injected only one drug)<br />
quadrupled the risk (OR = 4.16, CI 1.81-9.54, p25yr<br />
TIME SINCE ONSET OF INJECTING<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 25
Figure 3: Percentage of injecting drug users with hepatitis C and B infection<br />
against number of different drugs injected during lifetime<br />
% INFECTED<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
<strong>HEPATITIS</strong> C + <strong>HEPATITIS</strong> B +<br />
1 2-5 >5<br />
NUMBER OF DIFFERENT DRUGS EVER INJECTED<br />
The proportion of IDUs sharing injecting equipment ever and in the last four weeks is<br />
shown in Table 1b. Whether the subject had ever shared needles or syringes was<br />
associated with hepatitis C infection in the univariate analyses (Table 4). However, sharing<br />
variables did not remain significant after multivariate adjustment for imprisonment,<br />
length of injecting history and polydrug use. This is discussed further in Section 5.<br />
For hepatitis B, sharing needles and syringes was associated with infection (Table 4).<br />
However, after multivariate adjustment, only sharing spoons (a two-fold increase in risk<br />
of infection) remained significant (OR = 2.13, CI 1.01-4.52, p = 0.048). In addition,<br />
having used (without injecting) or injected most of the named drugs, except Temgesic<br />
(buprenorphine) and crack, was related to hepatitis C infection (Table 5). However, in the<br />
case of heroin and anabolic steroids there was too little variation to use in statistical<br />
analyses, with too many subjects using heroin and too few using steroids (Table 5).<br />
26<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
Use of any particular drug is likely to be related to use of the other drugs. Therefore, a<br />
backwards stepwise logistic regression was carried out to identify which drugs were<br />
independently related to hepatitis C infection. Compared to not having used the drug at<br />
all, having injected methadone (OR = 3.62, CI 1.38 - 9.48), DF 118 (dihydrocodeine<br />
tartrate) (OR = 3.92, CI 1.12 - 13.75), Diconal (dipipanone hydrochloride) (OR = 3.09, CI<br />
1.42 - 6.69) and morphine (OR = 3.48, CI 1.71 - 7.08) all resulted in higher risk of<br />
hepatitis C infection. Compared to not using the drug, those who used (but not injected)<br />
amphetamines and those who had used or injected Temgesic were at lower risk of<br />
infection (using amphetamine: OR = 0.33, CI 0.14 - 0.78; using Temgesic OR = 0.32, CI<br />
0.14 - 0.75, injecting Temgesic OR = 0.32 CI 0.13-0.75). For hepatitis B, having used or<br />
injected Diconal tripled the risk (compared to not using: OR = 3.76, CI 1.32-10.71 and<br />
OR = 3.34, CI 1.74-6.42 respectively) while those using (but not injecting) amphetamines<br />
were about a third as likely to be infected (OR = 0.3, CI 0.1-0.82). These patterns of drug<br />
use, as measures of chaotic behaviour, are examined further in the discussion.<br />
Table 4: Percentage of individuals sharing injecting equipment (ever and in the<br />
previous four weeks) by current serostatus and test history<br />
Hepititis C<br />
Needle Syringe Spoon Filter Paraphernalia 1 Any<br />
n ever last 4 ever last 4 ever last 4 ever last 4 ever last 4 ever last 4<br />
weeks weeks weeks weeks weeks weeks<br />
Current +ve 181 61.3** 5.5 59.7* 6.1 81.8 32.6 74.0 29.3 82.9 35.4 86.2 37.6<br />
Serostatus -ve 160 45.0 9.4 46.6 8.8 82.5 36.9 68.8 25.6 83.1 37.6 83.8 38.1<br />
Previously yes 99 64.6* 5.1 61.6* 5.1 87.9 28.3 81.8* 28.3 84.6 32.3 90.9 33.3<br />
Tested no 225 49.3 8.4 46.7 7.1 80.4 38.7 68.9 29.8 82.1 40.4 82.7 41.3<br />
Previous +ve 36 69.4 5.6 58.3 2.8 86.1 33.3 83.3 36.1 88.9 38.9 94.4 41.7<br />
Test Result -ve 45 55.6 6.7 60.0 8.9 88.9 28.9 77.8 22.2 88.9 28.9 88.9 28.9<br />
Hepititis B<br />
Current +ve 89 64.0* 4.5 61.8* 5.6 87.6 33.7 77.5 27.0 87.6 34.8 91.0 36.0<br />
Serostatus -ve 245 49.4 8.6 48.2 7.8 79.2 35.1 69.0 28.2 80.8 37.6 82.9 39.2<br />
Previously yes 149 58.4 6.0 55.0 5.4 86.6 30.9 77.9 26.8 87.9* 33.6 88.6 34.2<br />
Tested no 179 47.5 7.8 46.9 7.3 78.8 38.5 68.2 30.7 79.3 40.8 81.6 41.3<br />
Previous +ve 29 58.6 3.4 51.7 3.4 89.7 34.5 79.3 24.1 89.7 34.5 89.7 34.5<br />
Test Result -ve 96 56.3 6.3 55.2 5.2 86.5 31.3 79.2 30.2 87.5 35.4 88.5 35.4<br />
1 Injecting equipment other than needles or syringes. *p
Table 5: Percentage (number) of subjects using 1 and injecting each type of drug<br />
Hepatitis C<br />
Hepatitis B<br />
+ ve (n=181) -ve (n=160) P 2 +ve (n=89) -ve (n=245) P 2<br />
Heroin NS 3<br />
Used 4.4% (8) 5.0% (8) 5.6% (5) 4.5% (11)<br />
Injected 93.9% (170) 92.5% (148) 94.4% (84) 92.7% (227)<br />
Methadone **** **<br />
Used 43.1% (78) 58.1% (93) 42.7% (38) 53.9% (132)<br />
Injected 52.5% (95) 28.1% (45) 51.7% (46) 35.9% (88)<br />
Cocaine **** NS<br />
Used 13.8% (25) 23.1% (37) 11.2% (10) 21.2% (52)<br />
Injected 74.6% (135) 57.5% (92) 73.0% (65) 63.3% (155)<br />
Amphetamine **** **<br />
Used 9.9% (18) 25.6% (41) 9.0% (8) 22.4% (55)<br />
Injected 72.4% (131) 56.3% (90) 73.0% (65) 59.6% (146)<br />
Temgesic NS NS<br />
Used 12.7% (23) 15.6% (25) 13.5% (12) 13.9% (34)<br />
Injected 18.2% (33) 11.9% (19) 20.2% (18) 12.2% (30)<br />
Temazepam **** ****<br />
Used 26.0% (47) 40.0% (64) 19.1% (17) 38.0% (93)<br />
Injected 52.5% (95) 29.4% (47) 56.2% (50) 34.7% (85)<br />
DF118 **** ***<br />
Used 51.4% (93) 51.3% (82) 47.2% (42) 51.8% (127)<br />
Injected 13.8% (25) 3.1% (5) 15.7% (14) 4.9% (12)<br />
Dicanol **** ****<br />
Used 4.4% (8) 8.8% (14) 9.0% (8) 5.3% (13)<br />
Injected 34.3% (62) 9.4% (15) 37.1% (33) 15.1% (37)<br />
Cyclizine **** ***<br />
Used 2.8% (5) 6.3% (10) 5.6% (5) 3.7% (9)<br />
Injected 25.4% (46) 6.3% (10) 24.7% (22) 10.2% (25)<br />
Diazepam *** *<br />
Used 55.8% (101) 61.3% (98) 50.6% (45) 60.4% (148)<br />
Injected 22.1% (40) 8.8% (14) 22.5% (20) 12.2% (30)<br />
Morphine **** ****<br />
Used 9.4% (17) 14.4% (23) 7.9% (7) 12.7% (31)<br />
Injected 42.5% (77) 13.8% (22) 42.7% (38) 22.4% (55)<br />
Crack NS NS<br />
Used 32.0% (58) 41.9% (67) 33.7% (30) 37.6% (92)<br />
Injected 31.5% (57) 23.8% (38) 23.6% (21) 29.8% (73)<br />
Dalmane *** NS<br />
Used 8.3% (15) 6.3% (10) 6.7% (6) 6.1% (15)<br />
Injected 5.5% (10) 0.0% (0) 3.4% (3) 1.6% (4)<br />
Steroids 4 4<br />
Used 1.7% (3) 3.1% (5) 1.1% (1) 2.9% (7)<br />
Injected 2.8% (5) 2.5% (4) 0.0% (0) 2.9% (7)<br />
1 Used refers to taking but not injecting. 2 Numbers using (but not injecting), numbers injecting and numbers not<br />
using each drug (percentages of those not using are not shown) are compared by infection status (chi-square<br />
analysis). NS is non significant, * P
4.4 Previous hepatitis C test history<br />
People who had been for previous hepatitis C tests were nearly three times more<br />
likely to have shared needles or other equipment at some point in their lives<br />
(adjusted OR = 2.63, CI 1.23-6.17) and were twice as likely to have been in prison<br />
(adjusted OR = 1.94, CI 1.23-3.31). Since these are both risk factors for hepatitis C<br />
infection itself (see Section 4.3), it follows that those presenting for previous tests<br />
were about 70% more likely to be hepatitis C positive (OR =1.68, CI 1.03-2.75,<br />
chi square p = 0.01).<br />
Table 4 shows that those who have ever shared needles or any item of injecting<br />
paraphernalia were more likely to have presented for a hepatitis C test. Thus, over<br />
90% of those previously tested for hepatitis C had shared at least some item of<br />
injecting equipment (needles or paraphernalia) at some time compared to 83% of<br />
those who had not been tested. However, when examining recent sharing behaviour<br />
(last four weeks), importantly this trend was reversed. Here, of those having taken a<br />
hepatitis C test only 33% had shared in the past four weeks compared with 41% of<br />
those who had not previously been tested.<br />
This was examined further by dividing the study sample into those who had shared in<br />
the past but not in the four weeks prior to taking part in the study ('reformed sharers')<br />
and those who disclosed sharing in the previous four weeks ('current sharers').<br />
Analyses indicate that those having previously taken a hepatitis C tests were 1.69<br />
times more likely than previously untested individuals to be reformed sharers (i.e. no<br />
longer sharing; CI 1.01-2.85, p = 0.045). In other words, taking a test was associated<br />
with a small but significant change in sharing behaviour.<br />
Length of time being an injector was not related to having taken a hepatitis C test.<br />
Of the people who had been tested previously, 63 (66%) knew their correct status<br />
(32 positive, 31 negative). For fifteen (16%), their present test result was not the same<br />
as that recalled from the previous test: 14 stated that they had tested negative but<br />
were found to be positive during this study. Either these individuals were in fact<br />
negative at the time of their previous test and have been infected subsequently,<br />
or their recall of their test result was incorrect. The remaining person mistakenly<br />
thought himself or herself to be positive. Seventeen people did not know their<br />
status following their previous test, of those, over half (11, 65%) were positive at the<br />
current test.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 29
4.5 Predicting sharing behaviour<br />
People who believed themselves to be positive (by a previous test) did not differ<br />
significantly in their recent (previous four weeks) sharing behaviour from those who<br />
believed themselves to be negative, with around 6% having shared needles and<br />
about a third having shared any paraphernalia (Table 4). However, the size of the<br />
group within which the individual most recently injected their drugs was an important<br />
predictor of recent sharing behaviour (Figure 4). Of those whose previous injecting<br />
occasion was with one other person, 54% had shared some form of injecting<br />
equipment in the previous four weeks, whereas only 35% of those who injected<br />
with a larger group (two to five others) had recently shared. Compared to those<br />
who injected alone on their most recent injecting occasion, people who injected<br />
with one other person were nearly five times more likely to have shared equipment<br />
in the previous four weeks (p
A history of polydrug use was another significant predictor of recent sharing of<br />
equipment (p = 0.019) with those having used five or more drugs being over three<br />
times more likely to share (adjusted OR = 3.31, CI 1.40-7.79). Importantly,<br />
sharing was also more likely among those who had started injecting drugs within the<br />
previous 5 years (Figure 5, p = 0.014), with people who took up the habit recently<br />
being between two and seven times more likely to share equipment than those with<br />
longer histories of injecting behaviour (6-10 years, adjusted OR = 0.41, CI 0.2-0.85;<br />
11-15 years, adjusted OR = 0.30, CI 0.14-0.67; 16-20 years, adjusted OR = 0.26,<br />
CI 0.11-0.61; 21-25 years, adjusted OR = 0.14, CI 0.04-0.42; and over 25 years,<br />
adjusted OR = 0.21, CI 0.05-0.92).<br />
Figure 5: The percentage of injecting drug users sharing any form of injecting<br />
equipment in the previous four weeks (needles, syringes or other<br />
paraphernalia), categorised by time since first injected<br />
60<br />
% SHARING ANY EQUIPMENT<br />
IN PREVIOUS 4 WEEKS<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
0-5yr 6-10yr 11-15yr 16-20yr 21-25yr >25yr<br />
YEARS SINCE FIRST INJECTING<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 31
4.6 Blood donation<br />
Of those who had ever injected drugs, 15% had donated blood at some stage<br />
(Table 1a). Although we did not ascertain when blood donation had occurred, at least<br />
five individuals gave blood after commencing injecting, since they first injected before<br />
the age of 17 (the permitted age for blood donation is 17 years). Three of these five<br />
were hepatitis C positive in this study. A further 23 blood-donating individuals (13 of<br />
whom were hepatitis C positive) had commenced injecting before the age of 20;<br />
around the same time as they would be permitted to give blood. For the remaining<br />
27 individuals, the relative timing of blood donation and onset of injecting behaviour<br />
could not be ascertained.<br />
32<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
5. DISCUSSION<br />
5.1 Contact Groups<br />
Across the whole sample the prevalence of hepatitis C (current or previous infection)<br />
was 49% rising to 53% (with 95% confidence intervals of 47% to 58%) when<br />
considering injectors alone. Those approaching services specifically for tests (here called<br />
self-presenters) and those in treatment through community drugs teams had higher<br />
levels of hepatitis C (see Table 2) than those contacted through other settings. However,<br />
these differences failed to reach significance (see Section 4.2). A previous study to<br />
determine the hepatitis C prevalence in the <strong>North</strong> <strong>West</strong> found a higher prevalence of<br />
67% (with 95% confidence intervals of 63% to 70%) based on a sample of 545 IDUs<br />
presenting for hepatitis C testing (Lamden et al. 1998). Perhaps not surprisingly, this<br />
figure (67%) was closest to the prevalence found in CDT recruited participants for this<br />
study (61.4%) and those again presenting to services to request a test (61.9%). In our<br />
study, those who came forward for a previous test are those who are more likely to<br />
have shared, more likely to have been in prison (both risk factors for hepatitis C) and<br />
more likely to be hepatitis C positive. Similarly, Best et al. (1999), in their study of IDUs<br />
in London, found that those attending for previous tests were more likely to be hepatitis<br />
C positive. Combined therefore, these studies suggest caution should be used when<br />
interpreting prevalence of hepatitis C infection in studies where people have come<br />
forward for testing, since these prevalence estimations cannot necessarily be<br />
meaningfully extrapolated to the general population of injecting drug users.<br />
Based on the crude estimations of the number of current injecting drug users in<br />
contact with services in the <strong>North</strong> <strong>West</strong> (30,200: section 1.4) and the prevalence of<br />
hepatitis C found in this study (53%), we would expect 16,000 current drug users to<br />
be infected with hepatitis C. Studies on the disease progression (Section 1.8) suggest<br />
that 80% of these will go on to develop chronic hepatitis (i.e. 12,800), 20% of whom<br />
will go on to develop cirrhosis of the liver after a period of around 20 years (around<br />
2,600 cases). Having developed cirrhosis, the risk of developing hepatic carcinoma is<br />
estimated to be 1% per year (Tong et al. 1995), leading to around 26 cases per year.<br />
However, the prognosis of individuals infected by injecting drug use may be worse<br />
than that for transfusion patients (on whom the calculations of disease progression<br />
have been made), because IDUs may be exposed to multiple strains of the virus on<br />
more than one occasion (Renton & Main 1996). These numbers are based on estimates<br />
of the current drug using population assessing services. However, statistical estimates<br />
of the hidden population of drug users suggest that half of drug users may not be in<br />
contact with services. Also there are unknown numbers of former users exposed to the<br />
virus, and the addition of new users to the drug using population will increase the<br />
number of people with hepatitis C. This underlines the importance of the Government<br />
drug strategies to reduce the number of young people starting to use drugs, and<br />
reduce levels of injecting and equipment sharing.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 33
5.2 Co-infection between hepatitis B and hepatitis C<br />
Nineteen percent of the IDUs in this study were co-infected with hepatitis B and hepatitis<br />
C. People who had been infected with one virus were over four times as likely to also<br />
have been infected with the other. Results suggest that similar risk factors are associated<br />
with both infections such as prison, length of time since starting injecting and polydrug<br />
use (see Section 4.3). Co-infection represents a serious problem: the outcomes of the<br />
disease are more severe (Pol et al. 1998; Tagger et al. 1999); treatment is more difficult to<br />
manage (Dusheiko et al. 1996) and the risk of mother to child transmission of hepatitis C<br />
is increased (Resti 1999). Moreover, those infected with both viruses appear to be more<br />
infectious, possibly because they have higher viral loads in their body fluids (Dolan 1997).<br />
In this sense, continued pressures to increase levels of hepatitis B immunisation are<br />
essential both to reduce hepatitis B but also to potentially reduce the morbidity<br />
associated with hepatitis C and the levels of hepatitis C transmission.<br />
5.3 Risk factors<br />
In common with many other studies (e.g Garfein et al. 1998; Smythe et al. 1998;<br />
Lamden et al. 1998), a major risk factor for hepatitis C infection among IDUs was time<br />
since onset of injecting behaviour. In this study, prevalence increases from 18% among<br />
those who claim never to have injected to 34% in those injecting for up to five years,<br />
and 89% in those injecting for 21 to 25 years (Figure 2). The consequences for<br />
prevention programmes of the increase in hepatitis C infection that begins early in<br />
injectors’ careers are discussed in section 5.5.<br />
Having been in prison and the number of prison stays (Figure 1) were also important<br />
predictors of hepatitis C. The prison environment is one in which drug use is prevalent<br />
and, because clean equipment is difficult to obtain, when injecting occurs sharing is<br />
likely to happen (Bellis et al. 1997). Because such a large number of drug users find<br />
themselves in prison, the prevalence of hepatitis C among all prisoners is much higher<br />
than in the general population (for example, estimated as 20% in Scottish prisons:<br />
Gore et al. 1999). Moreover, within the confined environment of a prison, individuals<br />
may frequently be exposed to less common routes of transmission, for example, by<br />
sharing razors and other personal items or by being involved in fights that draw blood<br />
(De Mercato et al. 1995). Although transmission of infection is unlikely from a single<br />
such event, a high number could add up to a significant risk. Eight individuals in this<br />
study were infected with hepatitis C despite claiming never to have injected. Around<br />
15% of hepatitis C infections cannot be attributed to any cause and these may fall into<br />
this category but, of the eight, a disproportionate number (88%) had been in prison<br />
(P
azors should not be shared and should be made aware of the risk to both staff and<br />
prisoners posed by blood shed in the environment. At present, there is no centrally<br />
co-ordinated education programme on hepatitis C for prisoners although individual<br />
prisons may have arrangements with local services, for example drugs agencies.<br />
Type of drug injected had a strong statistical relationship with probability of ever<br />
having been hepatitis C infected. It is probable that the injecting or illegal use of<br />
certain drugs acts as a proxy for chaotic behaviour and that chaotic behaviour rather<br />
than a specific drug of use is directly related to increased chances of infection.<br />
Thus, having injected methadone, DF 118, Diconal and morphine all resulted in a<br />
higher risk of hepatitis C infection. The greater the number of different drugs used or<br />
injected, the more likely the individual was to be positive. Despite the probability of<br />
only an indirect link, polydrug use can still be used as a risk factor for hepatitis C and a<br />
marker for those most at risk. Other studies find a relationship between types and<br />
combinations of drugs used and infection: for example, the use of cocaine in addition<br />
to heroin increases the risk of hepatitis C infection (Garfein et al. 1998). In contrast,<br />
steroid injectors have been found to have a very low prevalence of hepatitis B and HIV<br />
compared to heroin users, which has been attributed to steroid users’ injecting<br />
practices being more hygienic and less likely to share (Crampin et al. 1998). Steroid<br />
users are also likely to inject relatively infrequently (Lenehan & McVeigh 1998).<br />
5.4 Effects of testing on risk behaviour<br />
In this study, subjects' perception of their hepatitis C status was not directly<br />
ascertained; instead, their history of previous tests was recorded. Thus, the 17<br />
individuals who were hepatitis C positive but claimed that their previous test was<br />
negative may have had an incorrect recollection of their status or could have become<br />
infected (or passed through the incubation period) since their previous test. However,<br />
both alternatives are causes for concern. Either individuals had forgotten or not<br />
understood their result in which case the value of the test was reduced or they have<br />
continued with risk behaviour despite a negative test result. In fact, in our sample an<br />
individuals' previous test result did not affect current sharing behaviour: regardless of<br />
whether a previous test was negative or positive, around 6% had shared needles in<br />
the previous four weeks, and up to 40% had shared some form of injecting<br />
equipment over the same time period (Table 4). Importantly however, there was some<br />
indication that individuals who had taken a test (regardless of the result) may be less<br />
likely to be currently sharing. Table 4 shows that, although those who took a previous<br />
test were more likely to have shared all forms of equipment in the past (i.e. ever<br />
shared), they were less likely to have shared in the previous four weeks (although this<br />
just failed to reach significance). Furthermore, when the data were grouped into<br />
current (those who admitted sharing in the previous four weeks) and reformed sharers<br />
(those who had shared in the past but not in the previous four weeks), reformed<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 35
sharers were significantly more likely to be people who had taken a test (P = 0.045).<br />
Therefore, taking a test per se but not the result of the test appears to have some<br />
relationship with changing behaviour. In the case of sero-negative individuals this may<br />
be to retain their negative status. For sero-positives it may act to prevent infection of<br />
fellow users, or to prevent multiple infection with different strains or co-infection with<br />
hepatitis B or HIV.<br />
It is difficult to distinguish cause and effect. Presenting for the test in the first place<br />
may mean individuals have already made a decision to improve and protect their<br />
health or the test may allow intervention by a drugs worker to encourage behaviour<br />
change. Certainly, the test procedure presents an opportunity for the drugs worker to<br />
provide holistic appraisal of risk behaviour, for example to counsel about safer injecting<br />
behaviour, and encourage uptake of the hepatitis B vaccine and abstinence from<br />
alcohol abuse. Further research should address whether changes in risk behaviour<br />
identified in the study occur just prior to or just after testing.<br />
5.5 Sharing behaviour<br />
This study identified an important link between the size of the group within which an<br />
individual injects and sharing behaviour. Sharing of needles and all types of<br />
paraphernalia was much more likely to happen if the user was injecting with just one<br />
other person present (Figure 4). Of those whose previous injecting occasion was with<br />
one other person, 54% had shared some form of injecting equipment in the previous<br />
four weeks, compared with 35% of those who injected with a larger group (two or<br />
more others). Many of the occasions of sharing with just one other person may be<br />
between sexual partners, in which case, sharing equipment may be seen as a sign of<br />
trust and intimacy (Rhodes & Quirk 1998). Harm reduction messages already explain<br />
the dangers of sharing but such messages on safer injecting practices should reiterate<br />
the fact that sharing with anybody else who injects drugs, be it friends or sexual<br />
partners, is a high risk activity for hepatitis C infection and other blood borne viruses.<br />
Of equal importance was the finding that sharing is more likely among those who<br />
have taken up injecting recently (i.e. within previous five years; Figure 5). This supports<br />
the importance of intercepting young users at the beginning of their drug taking<br />
careers to educate them in safer injecting behaviour. Harm minimisation policies<br />
should consider whether those not injecting, but who are progressing towards such<br />
drug use, need safer injecting information in order to reduce the increase in hepatitis C<br />
that occurs soon after injecting begins (Figure 2; Smythe et al. 1998; Lamden et al.<br />
1998). Consequently, it is especially important that efforts are made to reach<br />
vulnerable groups of young drug users.<br />
Overall, it appears that while IDUs may have changed their behaviour regarding<br />
sharing of needles (in response to the HIV crisis), messages about the danger of other<br />
36<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
forms of sharing have not necessarily been received. Around 40% of this study sample<br />
had either shared spoons, filters or other paraphernalia in the previous four weeks<br />
(Table 4) possibly because sharing paraphernalia is still not viewed as risky by many<br />
users. Speed & Bennett (1997), in an audit of sharing behaviour in the <strong>North</strong> <strong>West</strong>,<br />
reported a low awareness among IDUs of the risk of such indirect sharing: only around<br />
a third knew that such behaviour could lead to infections. Clearly, attempts to educate<br />
users that all forms of sharing are dangerous should be continued and the debate<br />
around whether syringe exchange schemes could also provide other clean equipment<br />
in addition to needles and syringes needs to be re-addressed.<br />
5.6 Blood donation<br />
In countries where donors are paid for giving blood there is an increased probability of<br />
blood being infected because drug users may give blood to supplement their income.<br />
Studies of infected blood donors in the USA show that having injected drugs is by far<br />
the largest single risk factor for being hepatitis C positive (Murphy et al. 2000). In fact,<br />
many Canadian haemophiliacs are infected with hepatitis C from blood collected in US<br />
prisons, even after the high risk nature of the prison setting was known (The Hepatitis<br />
Information Network 2000). Blood donors in the UK are not paid (and therefore not<br />
financially motivated), and the introduction of effective heat treatment of blood in<br />
1986 has made infection through transfusions or blood products very rare. However,<br />
no screening procedure can be 100% effective and hepatitis C (and HIV) cannot be<br />
detected in the 'window period' before antibodies are made. To further minimise the<br />
risk, potential donors are asked not to give blood if they have a history of injecting<br />
drugs. It is important to know to what extent injecting drug users donate blood.<br />
The results of this study show that 15% of those who had ever injected drugs had<br />
donated blood at some stage. Although we did not ascertain when blood donation<br />
had occurred, at least five individuals gave blood after commencing injecting, since<br />
they first injected before the age of 17 (the permitted age for blood donation is 17<br />
years). New blood borne infections emerge periodically, with IDUs always being a key<br />
risk group. The screening process should therefore place more emphasis on identifying<br />
drug users prior to donation, since tests for potential pathogens can only identify<br />
known disease organisms. The proportion of IDUs (or ex-IDUs) that currently donate<br />
blood is unknown, and this should be a topic for future research.<br />
5.7 Further research<br />
Sixty four percent of the individuals recruited to this study volunteered to be included<br />
as part of the cohort for follow up. This group provides the opportunity for a<br />
controlled study of test results on behavioural change. Levels of treatment uptake and<br />
the effects of such treatment could also be effectively monitored using this group.<br />
Such information is essential in order to inform policy around the costs and benefits of<br />
screening, counselling and treatment.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 37
5.8 Conclusions and Recommendations<br />
This study has identified the following key findings and recommendations:<br />
• Among the 341 injecting drug users in this study, the prevalence of hepatitis C<br />
was 53.1% (181 people), hepatitis B 26.6% (89 people) and 19.0% (65 people)<br />
were co-infected with hepatitis C and B (Section 4.1). Although the study was<br />
relatively small, different areas of study recruitment provided different levels of<br />
hepatitis C infection, with those presenting to drugs services requesting a test or<br />
those in treatment with community drugs teams having the highest prevalence.<br />
Those who had been for a hepatitis C test before this study were 1.68 times more<br />
likely to be hepatitis C positive in this study, again suggesting that people<br />
presenting for tests are more likely to be hepatitis C positive (Section 4.4).<br />
Models of health impact of hepatitis C should consider potential variations in<br />
prevalence rates between settings and recognise that most studies to date have<br />
assessed those most at risk of infection.<br />
• We crudely estimate that there are around 30,200 drug users currently in contact<br />
with services in the <strong>North</strong> <strong>West</strong>. Using estimates of the proportion of these<br />
injecting drugs and applying the hepatitis C prevalence of 53% found in this study,<br />
we estimate that there are 12,800 people currently chronically infected with<br />
hepatitis C. Of these, 2,600 will go on to develop serious liver damage (cirrhosis or<br />
hepatic carcinoma) (Section 5.1). This figure does not include the hidden<br />
population of drug users, previous or new users entering the drug-using population.<br />
<strong>Health</strong> Authorities should anticipate the increase in treatment costs associated with<br />
treating this high number of patients with liver damage over the next twenty years.<br />
• Those who are infected with hepatitis C are four times more likely to also be infected<br />
with hepatitis B (Section 4.1). Co-infection increases the risk of progression to serious<br />
disease.<br />
Current hepatitis B vaccination programmes should attempt to protect people<br />
early in their drug injecting career before exposure to hepatitis C.<br />
• Having ever visited prison, and the number of prison stays, were both strong<br />
predictors of hepatitis C infection (Figure 1). Prison represents a potential injecting<br />
and non-injecting risk for hepatitis C. For example sharing of personal items such<br />
as razors may lead to infection, and those few study participants infected but not<br />
identified as injectors were more likely to have been in prison.<br />
More awareness of these other, albeit low risk, activities is needed generally but in<br />
particular in prisons.<br />
38<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
• Chaotic behaviours such as polydrug use (Figure 3), use of less commonly misused<br />
drugs (Section 4.3) and a longer history of injecting (Figure 2) all predicted hepatitis<br />
C infection.<br />
Harm reduction measures can be targeted at such high risk groups and predictors<br />
identified in this study can be used as indicators as to which populations or<br />
individuals are at most risk of infection or most likely to be infected.<br />
• Significant levels of sharing were revealed. Almost 40% had shared some form of<br />
injecting equipment over the previous four weeks, and 7% had shared needles<br />
(Table 4). Consistent with more chaotic behaviour, sharing injecting equipment is<br />
more likely to occur in those with polydrug use (Section 4.5). Also, sharing injecting<br />
equipment is most common in new injectors (those who have been injecting for up<br />
to five years) (Figure 5).<br />
Work is urgently needed to reach young vulnerable groups of drug users who<br />
have recently begun injecting or may progress to injecting drugs. Such work<br />
requires education on the risks of injecting to reduce high risk behaviours or<br />
ideally prevent them even before they begin.<br />
• A previous positive result for hepatitis C did not appear to result in a change in<br />
sharing behaviour (Section 4.4). However, those who had presented for previous<br />
tests were more likely to be reformed sharers (i.e. not currently sharing). This may<br />
be because counselling received at the time of the test was successful in reducing<br />
subsequent risk behaviour regardless of the actual results of the test. However, it<br />
may relate to those asking for a test already having decided to protect their<br />
health.<br />
Further work should examine in more detail the links between hepatitis C testing<br />
and the identified reduction in sharing behaviour.<br />
• Sharing injecting equipment is more likely to occur in smaller groups of fellow<br />
users (Figure 4), possibly because the user feels safe among friends or with a<br />
partner. The high prevalence of hepatitis C in drug users in the <strong>North</strong> <strong>West</strong> means<br />
sharing with anyone carries a high risk of hepatitis C infection.<br />
Information about the risks of sharing should stress this includes close friends and<br />
sexual partners. <strong>Health</strong> information should also help users address the problems<br />
around refusing to share with a partner.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 39
R EFERENCES<br />
Allory Y, Charlotte F, Benhamou Y, Opolon P, Le Charpentier Y, Poynard T (2000) Impact of human<br />
immunodeficiency virus infection on the histological features of chronic hepatitis C: a case-control<br />
study. Human Pathology 31: 69-74.<br />
van Beek I, Dwyer R, Dore GJ, Luo K, Kaldor JM (1998) Infection with HIV and hepatitis C virus<br />
among injecting drug users in a prevention setting: retrospective cohort study.<br />
British Medical Journal 317: 433-437.<br />
Bellis MA, Weild AR, Beeching NJ, Mutton KJ, Syed Q (1997) Prevalence of HIV and injecting drug<br />
use in men entering a Liverpool Prison. British Medical Journal 315: 30-31<br />
Best D, Noble A, Finch E, Gossop M, Sidwell C, Strang J (1999) Accuracy of perceptions of<br />
hepatitis B and C status: cross sectional investigation of opiate addicts in treatment.<br />
British Medical Journal 319: 290-291.<br />
Birtles R, Bellis MA (2000) Drug services in Merseyside and Cheshire 1999: prevalence and<br />
outcomes. Liverpool John Moores University.<br />
Birtles R, Bellis MA, Millar T, Domnall M (1998) Drug misuse and the criminal justice system in the<br />
<strong>North</strong> <strong>West</strong> of England 1996. <strong>North</strong> <strong>West</strong> Drug Misuse occasional paper, issue number 1/98,<br />
University of Liverpool and University of Manchester.<br />
Birtles R, Bellis MA, Millar T, Domnall M (1999) Drug misuse in the <strong>North</strong> <strong>West</strong> of England 1998.<br />
Liverpool John Moores University and Manchester University.<br />
Bodsworth NJ, Cunningham P, Kaldor J, Donovan B (1996) Hepatitis C virus infection in a large<br />
cohort of homosexually active men: independent associations between HIV-1 infection and<br />
injecting drug use but not sexual behaviour. Genitourinary Medicine 72: 118-122.<br />
Brackmann SA, Gerritzen A, Oldenburg J, Brackmann HH, Schneweis KE (1993) Search for<br />
intrafamilial transmission of hepatitis C virus in haemophiliac patients. Blood 81: 1077-1082.<br />
Broers B, Junet C, Bourquin M, Déglon J-J, Perrin L, Hirschel B (1998) Prevalence and incidence<br />
rate of HIV, hepatitis B and C among drug users on methadone maintenance treatment in Geneva<br />
between 1988 and 1995. AIDS 12: 2059-2066.<br />
CDSC <strong>North</strong> <strong>West</strong> (1999) Policy Directory of the <strong>North</strong> <strong>West</strong> Communicable Disease and<br />
Environment Group (NWCDEG). Chapter 18, Hepatitis C.<br />
Coutinho (1998) HIV and hepatitis C among injecting drug users. British Medical Journal 317:<br />
424-425.<br />
Crampin AC, Lamagni TL, Hope VD, Newham JA, Lewis KM, Parry JV, Gill ON. (1998) The risk of<br />
infection with HIV and hepatitis B in individuals who inject steroids in England and Wales.<br />
Epidemiology and Infection 121: 381-386.<br />
Crofts N, Hopper JL, Bowden DS, Breshkin AM, Milner R, Locarnini SA (1993) Hepatitis C virus<br />
infection among a cohort of Victorian injecting drug users.<br />
Medical Journal of Australia 159: 237-241.<br />
40<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
Crofts N, Nigro L, Oman K, Stevenson E, Sherman J (1997) Methadone maintenance and hepatitis<br />
C virus infection among injecting drug users. Addiction 92: 999-1005.<br />
Datz C, Cramp M, Haas T, Dietze O, Nitschko H, Froesner G, Muss N, Sandhofer F, Vogel W<br />
(1999) The natural course of hepatitis C virus infection 18 years after an epidemic outbreak of<br />
non-A, non-B hepatitis in a plasmapheresis centre. Gut 44: 563-567.<br />
De Mercato R, Cantiello JP, Celentano U, Giani U, Romano A, Guarnaccia D, DAntonio A (1995)<br />
Hepatitis C virus in prisoners. Minerva Medicine 86: 89-91.<br />
Dieterich DT (1999) Hepatitis C virus and human immunodeficiency virus: clinical issues in<br />
coinfection. American Journal of Medicine 107: 79S-84S.<br />
Dolan M (1997) The hepatitis C handbook. Catalyst press. (London).<br />
Dusheiko GM, Khakoo S, Soni P, Grellier L (1996) A rational approach to management of<br />
hepatitis C infection. British Medical Journal 312: 357-64.<br />
Dusheiko GM, Roberts JA (1995) Treatment of chronic type B and C hepatitis with interferon<br />
alpha: an economic appraisal. Hepatology 22: 1863-1873.<br />
Eaton GG, Eaton RM, Bellis MA (1998) Drugs and drug users in <strong>North</strong> <strong>West</strong> prisons.<br />
<strong>Public</strong> <strong>Health</strong> Sector, Liverpool John Moores University.<br />
Garfein RS, Doherty MC, Monterroso ER, Thomas DL, Nelson KE, Vlahov D (1998) Prevalence and<br />
incidence of hepatitis C virus infection among young adult injection drug users.<br />
Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology 18, (Suppl 1): 11-19.<br />
Garland SM, Tabrizi S, Robinson P, Hughes C, Markman L, Devenish W, Kliman L (1998)<br />
Hepatitis C - role of perinatal transmission. Australian and New Zealand Journal of Obstetrics &<br />
Gynaecology 38: 424-427.<br />
Goldberg D, Cameron S, McMenamin J (1998) Hepatitis C virus antibody prevalence among<br />
injecting drug users in Glasgow has fallen but remains high. Communicable Diseases and <strong>Public</strong><br />
<strong>Health</strong> 1: 95-97.<br />
Gore SM, Bird SO, Cameron SO, Hutchinson SJ, Burns SM, Goldberg DJ (1999) Prevalence of<br />
hepatitis C in prisons: WASH-C surveillance linked to self-reported risk behaviours.<br />
Quarterly Journal of Medicine 92: 25-32.<br />
The Haemophilia Society (1999) Alive and kicking: a guide for young adults living with hepatitis C.<br />
Booklet. November 1999.<br />
Hagan H, McGough JP, Thiede H, Weiss NS, Hopkins S, Alexander ER (1999) Syringe exchange and<br />
risk of infection with hepatitis B and C viruses. American Journal of Epidemiology 149: 203-213.<br />
Hardi LV, Bellis MA (1999) Merseyside inter agency drug misuse database: a unified approach to<br />
drug misuse data. First annual report: 1 July - 30 June 1998. Liverpool John Moores University.<br />
Haydon GH, Flegg PJ, Blair CS, Brettle RP, Burns SM, Hayes PC (1998) The impact of chronic<br />
hepatitis C virus infection on HIV disease and progression in intravenous drug users.<br />
European Journal of Gastroenterology and Hepatology 10: 485-489.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 41
Hepatitis Information Network (2000) U.S. authorities did not alert Canadian broker that prison<br />
blood unsafe: federal memo. Press Release February 23, 2000<br />
[World Wide Web] http://www.hepnet.com/hepc/news022300.html.<br />
Hunter G, Stimson GV (1998) Survey of prevalence of sharing by injecting drug users not in<br />
contact with services. An independent study carried out on behalf of the Department of <strong>Health</strong>.<br />
The Centre for Research on Drugs and <strong>Health</strong> Behaviour, Imperial College School of Medicine.<br />
Judd A, Hunter GM, Maconochie N, Hickman M, Parry JV, Renton AM, Stimson GV (1999) HIV<br />
prevalence and risk behaviour among female injecting drug users in London, 1990 to 1996.<br />
AIDS 13: 833-837.<br />
Kumar RM, Shahul S (1998) Role of breast-feeding in transmission of hepatitis C virus to infants<br />
of HIV-infected mothers. Journal of Hepatology 29: 191-197.<br />
Lamden KH, Kennedy N, Beeching NJ, Lowe D, Morrison CL, Mallinson H, Mutton KJ, Syed Q<br />
(1998) Hepatitis B and hepatitis C virus infections: risk factors among drug users in <strong>North</strong> <strong>West</strong><br />
England. Journal of Infection 37: 260-269.<br />
Leal P, Stein K, Rosenberg W (1999) What is the cost utility of screening for hepatitis C virus<br />
(HCV) in intravenous drug users? Journal of Medical Screening 6: 124-131.<br />
Lenehan P, McViegh J (1998) Anabolic steroids: a guide for professionals. University of Liverpool.<br />
Liang TJ, Rehermann B, Seeff MD, Hoofnagle JH (2000) Pathogenesis, natural history, treatment,<br />
and prevention of hepatitis C. Annals of Internal Medicine 132: 296-305.<br />
McBride AJ, Ali IM, Clee W (1994) Hepatitis C and injecting drug use in prisons.<br />
British Medical Journal 309: 876.<br />
Murphy EL, Bryzman SM, Glynn SA, Ameti DI, Thomson RA, Williams AE, Nass CC, Ownby GH,<br />
Schreiber GB, Kong F, Neal KR, Nemo GJ (2000) Risk factors for hepatitis C virus infection in<br />
United States blood donors: NHLBI retrovirus epidemiology donor study. Hepatology 31: 756-762.<br />
Osella AR, Massa MA, Joekes S, Blanch N, Yacci MR Centonze S, Sileoni S (1998) Hepatitis B and<br />
C virus sexual transmission among homosexual men.<br />
American Journal of Gastroenterology 93: 49-52.<br />
Pol S, Lamorthe B, Thi NT, Thiers V, Carnot F, Zylbergerg H, Berthelot P, Brechot C, Nalpas B.<br />
(1998) Retrospective analysis of the impact of HIV infection and alcohol use on chronic hepatitis C<br />
in a large cohort of drug users. Journal of Hepatology 28: 945-950.<br />
Renton A, Main J (1996) Hepatitis C among injecting drug users (ed. Quirk A) The Centre for<br />
Research on Drugs and <strong>Health</strong> Behaviour, Executive Summary Number 50.<br />
Resti M (1999) Mother-to-infant transmission of hepatitis C virus.<br />
Italian Journal of Gastroenterology and Hepatology 31: 489-493.<br />
Resti M, Azzari C, Mannelli F, Moriondo M, Novembre E, de Martino M, Vierucci A (1998) Mother<br />
to child transmission of hepatitis C virus: prospective study of risk factors and timing of infection<br />
in children born to women seronegative for HIV-1. British Medical Journal 317: 437-441.<br />
42<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
Rezza G, Sagliocca L, Zaccarelli M, Nespoli M, Siconolfi M, Baldassarre C (1996) Incidence rate<br />
and risk factors for HCV seroconversion among injecting drug users in an area with low HIV<br />
seroprevalence. Scandinavian Journal of Infectious Disease 28: 27-29.<br />
Rhodes T, Quirk A (1998) Drug users sexual relationships and the social organisation of risk:<br />
The sexual relationship as a site of risk management. Social Science & Medicine 46: 157-169.<br />
Rodriguez OES, Gil MLM, Santana JFH, Liminana JFH, Sanchez AMM (1998) Prevalence of<br />
serologic markers of HBV, HDV, HCV and HIV in non-injecting drug users compared to injecting<br />
drug users. European Journal of Epidemiology 14: 555-561.<br />
Schlumberger MG, Desenclos J-C, Papaevangelou G, Richardson SC, Ancelle-Park R (1999)<br />
Knowledge of HIV serostatus and preventive behaviour among European injecting drug users:<br />
second study. European Journal of Epidemiology 15: 207-215.<br />
Semprini AE, Persico T, Thiers V, Oneta M, Tuveri R, Serafini P, Boschini A, Giuntelli S, Pardi G,<br />
Brechot C (1998) Absence of hepatitis C virus and detection of hepatitis G virus/GB virus C RNA<br />
sequences in the semen of infected men. Journal of Infectious Disease 177: 848-854<br />
Smythe BP, Keenan E, O’Connor J. (1998) Bloodborne viral infection in Irish injecting drug users.<br />
Addiction 93: 1649-1656.<br />
Speed S, Bennett A (1997) Sharing injecting paraphernalia: an audit of risk taking among<br />
attenders at syringe exchange schemes in <strong>North</strong> <strong>West</strong> England. University of Central Lancashire<br />
and HIT.<br />
Staples CT Jr, Rimland D, Dudas D (1999) Hepatitis C in the HIV (human immunodeficiency virus)<br />
Atlanta VA (Veterans Affairs Medical Center) Cohort study (HAVACS): the effect of coinfection on<br />
survival. Clinical Infectious Diseases 29: 150-154.<br />
Stark K, Müller R, Bienzle U, Guggenmoos-Holzmann I (1996) Frontloading: a risk factor for HIV<br />
and hepatitis C virus infection among injecting drug users in Berlin. AIDS 10: 311-317.<br />
Stimson GV (1995) AIDS and injecting drug use in the UK, 1988-1993: The policy response and<br />
the prevention of an epidemic. Social Science & Medicine 41: 699-716.<br />
Strugo I, Shinar E, Bar-Shany S, Amos L (1998) Hepatitis B and C markers among alcoholics in<br />
Israel: high incidence of HCV infection. European Journal of Epidemiology 14: 333-337.<br />
Suganuma N, Ikeda S, Taketa K, Wang DH, Yamamoto H, Phornphukutkul K, Peerakome S,<br />
Sitvacharanum K, Jittiwutikarn J. (1998) Risk analysis of the exposure to GB virus C / hepatitis G<br />
virus among populations of intravenous drug users, commercial sex workers and male outpatients<br />
at an STD clinic in Chiang Mai, Thailand: a cross-sectional case-control study.<br />
Acta Medica Okayama 52: 161-167.<br />
Syed Q, Snee K (1997) Hepatitis C - Advice for purchasers in the <strong>North</strong> <strong>West</strong> Region. Draft.<br />
Communicable Disease Surveillance Centre <strong>North</strong> <strong>West</strong>.<br />
Tackling Drugs to Build a Better Britain (1998) The Government's ten year strategy for tackling<br />
drugs misuse. White Paper. The Stationery Office.<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST 43
Tagger A, Donato F, Ribero ML, Chiesa R, Portera G, Gelatti U, Albertini A, Fasola M, Boffetta P,<br />
Nardi G (1999) Case-control study on hepatitis C virus (HCV) as a risk factor for hepatocellular<br />
carcinoma: the role of HCV genotypes and the synergism with hepatitis B virus and alcohol.<br />
International Journal of Cancer 81: 695-699.<br />
Taylor A, Goldberg D, Hutchinson S, Cameron S, Gore SM, McMenamin J, Green S, Pithie A,<br />
Fox R (2000) Prevalence of hepatitis C virus infection among injecting drug users in Glasgow<br />
1990-1996: are current harm reduction strategies working? Journal of Infection 40: 176-183.<br />
Theodore D, Fried MW (2000) Natural history and disease manifestations of hepatitis C infection.<br />
Current Topics in Microbiology and Immunology 242: 43-54.<br />
Thomas DL (2000) Hepatitis C epidemiology: injecting new tools in the field. Hepatology 31: 790-<br />
791.<br />
Tong MJ, el-Farra NS, Reikes AR, Co RL (1995) Clinical outcomes after transfusion-associated<br />
hepatitis C. New England Journal of Medicine 332: 1463-1466.<br />
Unlinked Anonymous Surveys Steering Group (1999) Prevalence of HIV in the United Kingdom:<br />
summary of data to the end of 1998. Department of <strong>Health</strong>.<br />
Weild AR, Gill ON, Bennett D, Livingstone SJM, Parry JV, Curran L (2000) Prevalence of HIV,<br />
hepatitis B, and hepatitis C antibodies in prisoners in England and Wales: a national survey.<br />
Communicable Diseases and <strong>Public</strong> <strong>Health</strong> 3: 121-126.<br />
Zylberberg H, Thiers V, Lagorce D, Squadrito G, Leone F, Berthelot P, Brechot C, Pol S (1999)<br />
Epidemiological and virological analysis of couples infected with hepatitis C virus. Gut 45: 112-116.<br />
44<br />
H EPATITIS C IN INJECTING DRUG USERS IN THE N ORTH W EST
Hepatitis C in<br />
injecting drug users<br />
in the <strong>North</strong> <strong>West</strong><br />
A Multi-Agency Study<br />
Penny A. Cook, Jim McVeigh, Apurva Patel, Qutub Syed, Ken Mutton and Mark A. Bellis<br />
Published by<br />
<strong>Public</strong> <strong>Health</strong> Sector<br />
School of <strong>Health</strong> and Human Sciences<br />
Liverpool John Moores University<br />
70 Great Crosshall Street<br />
Liverpool L3 2AB<br />
Tel: +44 (0151) 231 4301<br />
Fax: +44 (0151) 231 4320<br />
e-mail: p.a.cook@livjm.ac.uk<br />
© JULY 2000 ISBN 1-902051-19-X