infusion for thrombolysis - StreamlineMD
infusion for thrombolysis - StreamlineMD
infusion for thrombolysis - StreamlineMD
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
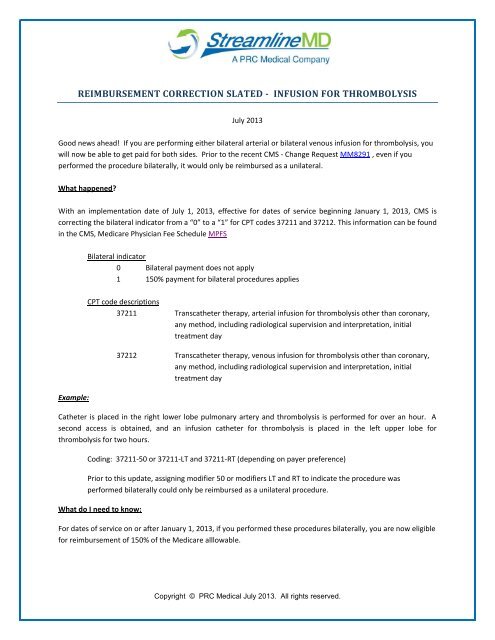
REIMBURSEMENT CORRECTION SLATED - INFUSION FOR THROMBOLYSIS<br />
July 2013<br />
Good news ahead! If you are per<strong>for</strong>ming either bilateral arterial or bilateral venous <strong>infusion</strong> <strong>for</strong> <strong>thrombolysis</strong>, you<br />
will now be able to get paid <strong>for</strong> both sides. Prior to the recent CMS - Change Request MM8291 , even if you<br />
per<strong>for</strong>med the procedure bilaterally, it would only be reimbursed as a unilateral.<br />
What happened?<br />
With an implementation date of July 1, 2013, effective <strong>for</strong> dates of service beginning January 1, 2013, CMS is<br />
correcting the bilateral indicator from a “0” to a “1” <strong>for</strong> CPT codes 37211 and 37212. This in<strong>for</strong>mation can be found<br />
in the CMS, Medicare Physician Fee Schedule MPFS<br />
Bilateral indicator<br />
0 Bilateral payment does not apply<br />
1 150% payment <strong>for</strong> bilateral procedures applies<br />
Example:<br />
CPT code descriptions<br />
37211 Transcatheter therapy, arterial <strong>infusion</strong> <strong>for</strong> <strong>thrombolysis</strong> other than coronary,<br />
any method, including radiological supervision and interpretation, initial<br />
treatment day<br />
37212 Transcatheter therapy, venous <strong>infusion</strong> <strong>for</strong> <strong>thrombolysis</strong> other than coronary,<br />
any method, including radiological supervision and interpretation, initial<br />
treatment day<br />
Catheter is placed in the right lower lobe pulmonary artery and <strong>thrombolysis</strong> is per<strong>for</strong>med <strong>for</strong> over an hour. A<br />
second access is obtained, and an <strong>infusion</strong> catheter <strong>for</strong> <strong>thrombolysis</strong> is placed in the left upper lobe <strong>for</strong><br />
<strong>thrombolysis</strong> <strong>for</strong> two hours.<br />
Coding: 37211-50 or 37211-LT and 37211-RT (depending on payer preference)<br />
Prior to this update, assigning modifier 50 or modifiers LT and RT to indicate the procedure was<br />
per<strong>for</strong>med bilaterally could only be reimbursed as a unilateral procedure.<br />
What do I need to know:<br />
For dates of service on or after January 1, 2013, if you per<strong>for</strong>med these procedures bilaterally, you are now eligible<br />
<strong>for</strong> reimbursement of 150% of the Medicare alllowable.<br />
Copyright © PRC Medical July 2013. All rights reserved.
2013 National Medicare Allowable:<br />
What do I need to do?<br />
37211 Arterial <strong>infusion</strong> $405.57<br />
37212 Venous <strong>infusion</strong> $358.94<br />
Since the correction will not be made until July 1, 2013 but will affect all previous dates of service, you may need to<br />
assign modifier 50 or LT and RT and notify the payer.<br />
Note: Your Medicare contractor will not search their files to either retract payment <strong>for</strong> claims already paid or to<br />
retroactively pay claims. So, if you have in the past per<strong>for</strong>med these procedures bilaterally and want to get<br />
reimbursed appropriately, you would need to bring it to their attention.<br />
In summary:<br />
‣ Past claims:<br />
Be proactive, if you have per<strong>for</strong>med a bilateral <strong>infusion</strong> <strong>for</strong> <strong>thrombolysis</strong> on or after January 1,<br />
2013 but were reimbursed only <strong>for</strong> a unilateral procedure, you must notify the payer. Payers will<br />
not automatically make the correction.<br />
‣ Future claims:<br />
Don’t make the assumption that just because CMS made the correction to the Medicare<br />
Physician Fee Schedule that all other payers will follow suit. Chances are they have not done so.<br />
Be proactive, review your claims to make sure they are properly adjucated.<br />
‣ Documentation is critical:<br />
Due to the fact that many payers are going to require “proof” that the <strong>infusion</strong> <strong>for</strong> <strong>thrombolysis</strong><br />
was truly bilateral, it is imperative that your documentation individually describes each<br />
procedure. For each <strong>infusion</strong>, your documentation must include:<br />
Access site – name the vessel<br />
Laterality – identify the side<br />
Vascular system – arterial or venous<br />
Final catheter placement – name the vessel<br />
Identify the thrombolytic agent<br />
Infusion time<br />
Medical necessity<br />
If there is a topic that you would like to see covered, please contact Wendy Block at wblock@prcmedical or by phone,<br />
330.564.2618.<br />
Copyright © PRC Medical July 2013. All rights reserved.