Menopausal hormones and risk of ovarian cancer - ResearchGate
Menopausal hormones and risk of ovarian cancer - ResearchGate
Menopausal hormones and risk of ovarian cancer - ResearchGate
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
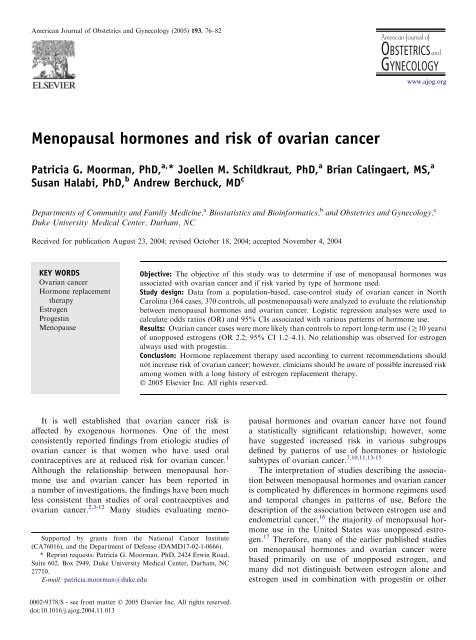
American Journal <strong>of</strong> Obstetrics <strong>and</strong> Gynecology (2005) 193, 76–82<br />
www.ajog.org<br />
<strong>Menopausal</strong> <strong>hormones</strong> <strong>and</strong> <strong>risk</strong> <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong><br />
Patricia G. Moorman, PhD, a, * Joellen M. Schildkraut, PhD, a Brian Calingaert, MS, a<br />
Susan Halabi, PhD, b Andrew Berchuck, MD c<br />
Departments <strong>of</strong> Community <strong>and</strong> Family Medicine, a Biostatistics <strong>and</strong> Bioinformatics, b <strong>and</strong> Obstetrics <strong>and</strong> Gynecology, c<br />
Duke University Medical Center, Durham, NC<br />
Received for publication August 23, 2004; revised October 18, 2004; accepted November 4, 2004<br />
KEY WORDS<br />
Ovarian <strong>cancer</strong><br />
Hormone replacement<br />
therapy<br />
Estrogen<br />
Progestin<br />
Menopause<br />
Objective: The objective <strong>of</strong> this study was to determine if use <strong>of</strong> menopausal <strong>hormones</strong> was<br />
associated with <strong>ovarian</strong> <strong>cancer</strong> <strong>and</strong> if <strong>risk</strong> varied by type <strong>of</strong> hormone used.<br />
Study design: Data from a population-based, case-control study <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong> in North<br />
Carolina (364 cases, 370 controls, all postmenopausal) were analyzed to evaluate the relationship<br />
between menopausal <strong>hormones</strong> <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong>. Logistic regression analyses were used to<br />
calculate odds ratios (OR) <strong>and</strong> 95% CIs associated with various patterns <strong>of</strong> hormone use.<br />
Results: Ovarian <strong>cancer</strong> cases were more likely than controls to report long-term use (R10 years)<br />
<strong>of</strong> unopposed estrogens (OR 2.2; 95% CI 1.2–4.1). No relationship was observed for estrogen<br />
always used with progestin.<br />
Conclusion: Hormone replacement therapy used according to current recommendations should<br />
not increase <strong>risk</strong> <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong>; however, clinicians should be aware <strong>of</strong> possible increased <strong>risk</strong><br />
among women with a long history <strong>of</strong> estrogen replacement therapy.<br />
Ó 2005 Elsevier Inc. All rights reserved.<br />
Supported by grants from the National Cancer Institute<br />
(CA76016), <strong>and</strong> the Department <strong>of</strong> Defense (DAMD17-02-1-0666).<br />
* Reprint requests: Patricia G. Moorman, PhD, 2424 Erwin Road,<br />
Suite 602, Box 2949, Duke University Medical Center, Durham, NC<br />
27710.<br />
E-mail: patricia.moorman@duke.edu<br />
It is well established that <strong>ovarian</strong> <strong>cancer</strong> <strong>risk</strong> is<br />
affected by exogenous <strong>hormones</strong>. One <strong>of</strong> the most<br />
consistently reported findings from etiologic studies <strong>of</strong><br />
<strong>ovarian</strong> <strong>cancer</strong> is that women who have used oral<br />
contraceptives are at reduced <strong>risk</strong> for <strong>ovarian</strong> <strong>cancer</strong>. 1<br />
Although the relationship between menopausal hormone<br />
use <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> has been reported in<br />
a number <strong>of</strong> investigations, the findings have been much<br />
less consistent than studies <strong>of</strong> oral contraceptives <strong>and</strong><br />
<strong>ovarian</strong> <strong>cancer</strong>. 2,3-12 Many studies evaluating menopausal<br />
<strong>hormones</strong> <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> have not found<br />
a statistically significant relationship; however, some<br />
have suggested increased <strong>risk</strong> in various subgroups<br />
defined by patterns <strong>of</strong> use <strong>of</strong> <strong>hormones</strong> or histologic<br />
subtypes <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong>. 7,10,11,13-15<br />
The interpretation <strong>of</strong> studies describing the association<br />
between menopausal <strong>hormones</strong> <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong><br />
is complicated by differences in hormone regimens used<br />
<strong>and</strong> temporal changes in patterns <strong>of</strong> use. Before the<br />
description <strong>of</strong> the association between estrogen use <strong>and</strong><br />
endometrial <strong>cancer</strong>, 16 the majority <strong>of</strong> menopausal hormone<br />
use in the United States was unopposed estrogen.<br />
17 Therefore, many <strong>of</strong> the earlier published studies<br />
on menopausal <strong>hormones</strong> <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> were<br />
based primarily on use <strong>of</strong> unopposed estrogen, <strong>and</strong><br />
many did not distinguish between estrogen alone <strong>and</strong><br />
estrogen used in combination with progestin or other<br />
0002-9378/$ - see front matter Ó 2005 Elsevier Inc. All rights reserved.<br />
doi:10.1016/j.ajog.2004.11.013
Moorman et al 77<br />
<strong>hormones</strong>. Since the late 1970s, physicians have tended<br />
to prescribe lower dose estrogens, <strong>and</strong> a much larger<br />
proportion <strong>of</strong> women have used menopausal <strong>hormones</strong><br />
consisting <strong>of</strong> both an estrogen <strong>and</strong> progestin. 17,18 Given<br />
that the effects <strong>of</strong> progestins on the ovaries may be very<br />
different from that <strong>of</strong> estrogens, with some investigators<br />
hypothesizing a protective effect <strong>of</strong> progestins, 19,20 the use<br />
<strong>of</strong> combination therapy could have very different effects<br />
on <strong>ovarian</strong> <strong>cancer</strong> <strong>risk</strong> than estrogen alone. However,<br />
relatively few studies have assessed the association<br />
between different hormone regimens <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong>.<br />
In addition to the possibility that the effect <strong>of</strong><br />
menopausal <strong>hormones</strong> depends on the specific regimen<br />
used, some studies have suggested that the <strong>risk</strong> may vary<br />
between histologic subtypes <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong>. Several<br />
studies have reported larger increases in <strong>risk</strong>s for serous<br />
<strong>and</strong>/or endometrioid than for other subtypes. 13-15<br />
In this report we describe the associations between<br />
menopausal hormone use <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> using data<br />
from a population-based, case-control study <strong>of</strong> <strong>ovarian</strong><br />
<strong>cancer</strong> conducted in North Carolina between 1999 <strong>and</strong><br />
2003. The analyses focus on the effects <strong>of</strong> different<br />
hormone regimens on epithelial <strong>ovarian</strong> <strong>cancer</strong> overall,<br />
<strong>and</strong> on different histologic subtypes <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong>.<br />
Material <strong>and</strong> methods<br />
We analyzed data from Phase I <strong>of</strong> the North Carolina<br />
Ovarian Cancer Study, a population-based case-control<br />
study <strong>of</strong> newly diagnosed epithelial <strong>ovarian</strong> <strong>cancer</strong> cases<br />
in a 48-county area <strong>of</strong> North Carolina. Cases were<br />
identified using a rapid case ascertainment system<br />
developed by the North Carolina Central Cancer<br />
Registry, a statewide population-based tumor registry.<br />
Pathology reports for all <strong>ovarian</strong> <strong>cancer</strong>s diagnosed in<br />
the hospitals in the study area were forwarded to the<br />
Central Cancer Registry, <strong>and</strong> then to the study <strong>of</strong>fice<br />
within 2 months <strong>of</strong> diagnosis. Of the 53 hospitals in the<br />
study area that treat <strong>ovarian</strong> <strong>cancer</strong> patients, 52 agreed<br />
to participate in the study. Eligible cases were women<br />
aged 20 to 74 years who were diagnosed with primary<br />
epithelial <strong>ovarian</strong> <strong>cancer</strong> between January 1, 1999 <strong>and</strong><br />
March 31, 2003, <strong>and</strong> resided in the 48-county study area.<br />
Both invasive tumors <strong>and</strong> those with low malignant<br />
potential (borderline tumors) were included. Permission<br />
to contact the <strong>ovarian</strong> <strong>cancer</strong> cases was requested from<br />
the physician <strong>of</strong> record on the pathology report. All<br />
participants were English-speaking, mentally competent<br />
to complete an interview, <strong>and</strong> able to give informed<br />
consent. All cases underwent st<strong>and</strong>ardized pathologic<br />
<strong>and</strong> histologic review to confirm the diagnosis. Of 883<br />
cases <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong> identified through the hospitals,<br />
784 were eligible for the study. Reasons for ineligibility<br />
included diagnosis other than epithelial <strong>ovarian</strong> <strong>cancer</strong><br />
(n = 55), date <strong>of</strong> diagnosis before initiation <strong>of</strong> study<br />
(n = 11), inability to complete an interview in English<br />
due to language or cognitive issues (n = 16), age greater<br />
than 74 years (n = 12), residence outside <strong>of</strong> the study<br />
area (n = 4), <strong>and</strong> institutionalized patient (n = 1). The<br />
overall response rate among eligible cases was 76%,<br />
although 86% <strong>of</strong> women who were contacted were<br />
successfully recruited into the study. Reasons that cases<br />
were not interviewed included death (4%), debilitating<br />
illness (2%), patient refusal (7%), physician refusal<br />
(3%), <strong>and</strong> inability to locate the woman (8%). A total<br />
<strong>of</strong> 594 cases were enrolled in the study.<br />
Controls were identified from the same 48-county<br />
area that generated the cases using r<strong>and</strong>om digit dialing<br />
methodology. Controls were frequency matched to cases<br />
by race <strong>and</strong> age (within 5 years). Race was based on selfreport<br />
by the participant. Health Care Financing <strong>and</strong><br />
Administration tapes were initially used to identify<br />
controls aged 65 to 74 years; however, this strategy<br />
was ab<strong>and</strong>oned due to the difficulty in contacting<br />
potential controls because <strong>of</strong> the absence <strong>of</strong> telephone<br />
numbers on these tapes. Eligible controls resided in the<br />
same 48-county area as the cases, had no history <strong>of</strong><br />
<strong>cancer</strong>, <strong>and</strong> had to have at least 1 ovary intact. As was<br />
required for the cases, controls had to be Englishspeaking,<br />
mentally competent to complete an interview,<br />
<strong>and</strong> able to give informed consent. Seventy-one percent<br />
<strong>of</strong> controls (n = 628) identified by r<strong>and</strong>om digit dialing<br />
who met the eligibility criteria were successfully enrolled<br />
into the study. The study protocol was approved by<br />
institutional review boards at Duke University Medical<br />
Center <strong>and</strong> all hospitals that participated in the study.<br />
The analyses presented here are restricted to postmenopausal<br />
cases (n = 364) <strong>and</strong> controls (n = 370). We<br />
included: (1) women who reported their menstrual<br />
periods had stopped naturally; (2) women who reported<br />
they began hormone replacement therapy before their<br />
periods stopped completely; (3) women who had a hysterectomy<br />
without bilateral oophorectomy <strong>and</strong> were at<br />
least 51 years <strong>of</strong> age; <strong>and</strong> (4) women whose periods<br />
stopped due to chemotherapy unrelated to <strong>ovarian</strong><br />
<strong>cancer</strong>. To be eligible for the study, controls were<br />
required to have at least 1 ovary; therefore, none were<br />
postmenopausal due to bilateral oophorectomy. Four <strong>of</strong><br />
the cases were postmenopausal due to bilateral oophorectomy<br />
(but still were subsequently diagnosed with<br />
<strong>ovarian</strong> <strong>cancer</strong>).<br />
Cases <strong>and</strong> controls were interviewed in person by<br />
trained nurse interviewers in the home <strong>of</strong> the study<br />
participant or at another convenient location. A 90-<br />
minute questionnaire was administered to obtain information<br />
on known <strong>and</strong> suspected <strong>risk</strong> factors for<br />
<strong>ovarian</strong> <strong>cancer</strong>, including family history <strong>of</strong> <strong>cancer</strong> in first<strong>and</strong><br />
second-degree relatives, menstrual characteristics,<br />
pregnancy <strong>and</strong> breastfeeding history, hormone use, <strong>and</strong><br />
lifestyle factors such as smoking history, alcohol consumption,<br />
physical activity, <strong>and</strong> occupational history.
78 Moorman et al<br />
A life-event calendar on which major events in the<br />
woman’s life, such as pregnancies <strong>and</strong> marriages, were<br />
recorded was used to aid recall. Body mass index (BMI)<br />
was calculated based on measured height <strong>and</strong> selfreported<br />
weight from 1 year ago (kg/m 2 ). BMI from 1<br />
year ago was used because many cases reported recent<br />
weight changes related to the <strong>cancer</strong> or its treatment.<br />
In regard to hormone use, women were asked if they<br />
had used PremarinÒ or conjugated estrogens, other estrogen<br />
pills, or estrogen patches. If they responded affirmatively<br />
to use <strong>of</strong> any <strong>of</strong> these types <strong>of</strong> estrogen, they were<br />
asked if they had used progestin along with the estrogen.<br />
The women also were asked about use <strong>of</strong> progestin alone,<br />
testosterone, or any other hormone pills. For each<br />
hormone used, we obtained the name <strong>of</strong> the hormone,<br />
ages at first <strong>and</strong> last use, total duration <strong>of</strong> use, <strong>and</strong> dosing<br />
regimen (every day, R21 days/month, or !21 days/<br />
month). We examined the type <strong>of</strong> hormone used (estrogen<br />
only; progestin only; estrogen always taken with progestin;<br />
estrogen taken sometimes with progestin, sometimes<br />
alone; testosterone with estrogen <strong>and</strong>/or<br />
progestin), the total duration <strong>of</strong> use, <strong>and</strong> the time since<br />
last use.<br />
Statistical analyses<br />
Cases <strong>and</strong> controls were compared in regard to demographic<br />
characteristics <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> <strong>risk</strong> factors<br />
using t tests for continuous variables <strong>and</strong> chi-square<br />
tests for categorical variables. Unconditional logistic<br />
regression analyses were used to calculate odds ratios<br />
(ORs) <strong>and</strong> 95% CIs for the association between<br />
hormone use <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong>, taking into account<br />
potential confounders. Variables considered as potential<br />
confounders in the multivariable models included age<br />
(continuous), race (black/non-black), parity (continuous),<br />
tubal ligation (yes/no), oral contraceptive use (yes/<br />
no), history <strong>of</strong> breastfeeding (yes/no), hysterectomy<br />
(yes/no), history <strong>of</strong> breast or <strong>ovarian</strong> <strong>cancer</strong> in a firstdegree<br />
relative (yes/no), BMI 1 year before interview<br />
(continuous), <strong>and</strong> educational level (less than high<br />
school, high school graduate, or greater than high<br />
school). To test for trend across categories <strong>of</strong> duration,<br />
we created an ordinal variable by assigning nonusers<br />
a value <strong>of</strong> 0, users in the shortest duration category<br />
a value <strong>of</strong> 1, the next highest duration category a value<br />
<strong>of</strong> 2, etc. We then included this ordinal term in our<br />
logistic regression model, <strong>and</strong> took the P value corresponding<br />
to this variable as our test <strong>of</strong> trend. All<br />
analyses were performed using SAS 8.0 (SAS Institute,<br />
Inc, Cary, NC).<br />
Results<br />
Table I presents selected characteristics <strong>of</strong> the cases <strong>and</strong><br />
controls. Although not all differences were statistically<br />
Table I Selected characteristics <strong>of</strong> cases <strong>and</strong> controls, the<br />
North Carolina Ovarian Cancer Study<br />
Cases<br />
(n = 364)<br />
Controls<br />
(n = 370)<br />
n (%) n (%) P value*<br />
Age (y)<br />
!40 0 (0) 1 (0) .006<br />
40-49 12 (3) 8 (2)<br />
50-59 145 (40) 116 (31)<br />
60-69 148 (41) 158 (43)<br />
O70 59 (16) 87 (24)<br />
Race<br />
White 312 (86) 308 (83) .56<br />
African American 47 (13) 54 (15)<br />
Other 5 (1) 8 (2)<br />
Type <strong>of</strong> menopause<br />
Natural 191 (52) 194 (52) .40<br />
Began <strong>hormones</strong> before 51 (14) 65 (18)<br />
periods stopped<br />
Surgical 119 (33) 110 (30)<br />
Chemotherapy 3 (1) 1 (0)<br />
Months <strong>of</strong> pregnancy<br />
None 47 (13) 30 (8) .006<br />
!9 13 (4) 8 (2)<br />
9-18 125 (34) 135 (36)<br />
19-36 140 (39) 141 (38)<br />
O36 38 (10) 56 (15)<br />
Missing 1 0<br />
Months <strong>of</strong> breastfeeding<br />
None 260 (72) 247 (67) .68<br />
!6 37 (10) 48 (13)<br />
6-12 36 (10) 35 (9)<br />
O12 29 (8) 39 (11)<br />
Missing 2 1<br />
Oral contraceptive use (m)<br />
None 158 (43) 175 (47) .22<br />
!12 38 (10) 30 (8)<br />
12-36 62 (17) 66 (18)<br />
O36 96 (26) 92 (25)<br />
Unknown duration <strong>of</strong> use 10 (3) 7 (2)<br />
Tubal ligation<br />
No 281 (77) 259 (70) .027<br />
Yes 83 (23) 111 (30)<br />
1st degree family history <strong>of</strong><br />
<strong>ovarian</strong> <strong>cancer</strong><br />
No 344 (95) 357 (96) .18<br />
Yes 19 (5) 12 (3)<br />
Missing 1 1<br />
Body mass index (kg/m 2 )<br />
Quartile 1 82 (23) 90 (25) .16<br />
Quartile 2 94 (26) 91 (25)<br />
Quartile 3 75 (21) 90 (25)<br />
Quartile 4 104 (29) 91 (25)<br />
Missing 9 8<br />
Education<br />
!High school 36 (10) 62 (17) .062<br />
High school graduate 122 (34) 99 (27)<br />
OHigh school 206 (57) 209 (56)<br />
* P values based on t tests for continuous variables (age, months<br />
<strong>of</strong> pregnancy, months <strong>of</strong> breastfeeding, months <strong>of</strong> oral contraceptive<br />
use, body mass index) <strong>and</strong> chi-square tests for categorical variables.
Moorman et al 79<br />
Table II Odds ratios for <strong>ovarian</strong> <strong>cancer</strong> associated with hormone use<br />
Cases<br />
(n = 364)<br />
Controls<br />
(n = 370)<br />
n n OR* 95% CI OR y 95% CI<br />
Never users 129 152 1.0 (Reference) 1.0 (Reference)<br />
Ever user 235 218 1.2 (0.9-1.6) 1.2 (0.8-1.6)<br />
Duration <strong>of</strong> use<br />
!12 months 11 14 0.8 (0.4-1.9) 0.8 (0.3-1.9)<br />
12-59 months 68 64 1.1 (0.7-1.6) 1.2 (0.7-1.9)<br />
60-119 months 42 42 1.0 (0.6-1.7) 1.0 (0.6-1.6)<br />
O119 months 96 78 1.5 (1.0-2.2) 1.5 (1.0-2.3)<br />
Missing 18 20<br />
Time since last use<br />
!12 months 147 145 1.1 (0.8-1.5) 1.1 (0.7-1.5)<br />
12-59 months 41 31 1.4 (0.8-2.4) 1.6 (0.9-2.8)<br />
60-119 months 15 7 2.4 (0.9-6.1) 2.6 (1.0-7.0)<br />
O119 months 11 12 1.1 (0.5-2.7) 1.2 (0.5-2.8)<br />
Missing 21 23<br />
* ORs (odds ratios) adjusted for age <strong>and</strong> race using logistic regression modeling.<br />
y ORs adjusted for age, race, parity, tubal ligation, hysterectomy, BMI 1 year before interview, 1st degree family history <strong>of</strong> breast or <strong>ovarian</strong> <strong>cancer</strong>,<br />
breastfeeding (yes/no), oral contraceptive use (yes/no), <strong>and</strong> educational level using logistic regression modeling.<br />
Table III Odds ratios for <strong>ovarian</strong> <strong>cancer</strong> by hormone regimen used <strong>and</strong> duration <strong>of</strong> use<br />
Cases<br />
(n = 364)<br />
Controls<br />
(n = 370)<br />
n n OR* 95% CI OR y 95% CI<br />
Never use 129 152 Referent Referent<br />
Estrogen only<br />
Ever use 105 79 1.2 (0.7-2.0) 1.5 (0.9-2.3)<br />
!12 months 5 6 0.8 (0.2-2.9) 0.9 (0.3-3.2)<br />
12-59 months 23 24 1.0 (0.5-1.8) 1.2 (0.6-2.3)<br />
60-119 months 17 11 1.7 (0.7-3.7) 1.5 (0.6-3.5)<br />
O119 months 52 32 2.1 (1.2-3.4) 2.2 (1.2-4.1)<br />
Missing duration 8 6<br />
Estrogen always with progestin<br />
Ever use 70 87 0.8 (0.6-1.3) 0.9 (0.6-1.4)<br />
!12 months 3 7 0.5 (0.1-1.8) 0.5 (0.1-2.0)<br />
12-59 months 29 31 0.9 (0.5-1.7) 1.0 (0.6-1.9)<br />
60-119 months 14 14 1.0 (0.4-2.2) 1.1 (0.5-2.6)<br />
O119 months 20 28 0.9 (0.5-1.7) 1.0 (0.5-2.0)<br />
Missing duration 4 7<br />
Estrogen <strong>and</strong> progestin, not always<br />
used together<br />
Ever use 44 38 1.2 (0.7-2.0) 1.3 (0.8-2.2)<br />
!12 months 0 1 - -<br />
12-59 months 9 4 1.8 (0.5-6.3) 2.2 (0.6-7.9)<br />
60-119 months 10 14 0.7 (0.3-1.6) 0.7 (0.3-1.9)<br />
O119 months 22 14 1.9 (0.9-4.0) 2.4 (1.1-5.3)<br />
Missing duration 3 5<br />
Progestin only<br />
Ever use 7 1 6.9 (0.8-57.3) 6.7 (0.8-57.9)<br />
Testosterone<br />
Ever use 9 13 0.7 (0.3-1.6) 0.6 (0.3-1.6)<br />
* ORs (odds ratios) adjusted for age <strong>and</strong> race using logistic regression modeling.<br />
y ORs adjusted for age, race, parity, tubal ligation, hysterectomy, BMI 1 year before interview, 1st degree family history <strong>of</strong> breast or <strong>ovarian</strong> <strong>cancer</strong>,<br />
breastfeeding (yes/no), oral contraceptive use (yes/no), <strong>and</strong> educational level using logistic regression modeling.
80 Moorman et al<br />
Table IV Odds ratios* for <strong>ovarian</strong> <strong>cancer</strong> associated with hormone use by type <strong>of</strong> hormone <strong>and</strong> histologic subtype <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong><br />
Controls<br />
Serous Endometrioid or clear cell Mucinous Other<br />
n n OR 95% CI n OR 95% CI n OR 95% CI n OR 95% CI<br />
Never user 152 68 1.0 (reference) 31 1.0 (reference) 13 1.0 (reference) 17 1.0 (reference)<br />
Estrogen only 79 73 2.0 (1.3-3.1) 17 1.0 (0.5-2.0) 6 0.9 (0.3-2.5) 9 1.1 (0.5-2.7)<br />
Estrogen always with 87 48 1.1 (0.7-1.8) 9 0.4 (0.2-0.9) 5 0.4 (0.1-1.3) 8 1.0 (0.4-2.4)<br />
progestin<br />
Estrogen <strong>and</strong> progestin,<br />
not always used together<br />
38 27 1.4 (0.8-2.5) 8 0.9 (0.4-2.1) 2 0.4 (0.1-2.0) 7 2.0 (0.7-5.4)<br />
* All ORs adjusted for age <strong>and</strong> race using logistic regression modeling.<br />
significant, the characteristics <strong>of</strong> the cases <strong>and</strong> controls<br />
were generally consistent with established <strong>risk</strong> factors<br />
for <strong>ovarian</strong> <strong>cancer</strong>. Cases tended to have fewer months<br />
<strong>of</strong> pregnancy, were less likely to have had a tubal<br />
ligation, were more likely to have a family history <strong>of</strong><br />
<strong>ovarian</strong> <strong>cancer</strong>, <strong>and</strong> had higher educational levels. In<br />
contrast to many studies, we observed little difference in<br />
oral contraceptive use between cases <strong>and</strong> controls.<br />
When comparing characteristics <strong>of</strong> hormone users<br />
<strong>and</strong> nonusers among the control women, we found few<br />
significant differences (data not shown). However, the<br />
trends were consistent with published data, suggesting<br />
that hormone users are more likely to be nulliparous,<br />
have used oral contraceptives, have lower BMI, have<br />
higher educational level, <strong>and</strong> drink alcohol.<br />
Table II shows the ORs for <strong>ovarian</strong> <strong>cancer</strong> associated<br />
with use <strong>of</strong> any type <strong>of</strong> menopausal <strong>hormones</strong>. There<br />
was not a statistically significant relationship between<br />
ever use <strong>of</strong> menopausal <strong>hormones</strong> <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong>.<br />
There was a suggestion <strong>of</strong> a modestly increased <strong>risk</strong> for<br />
women who reported long-term use, but no clear<br />
relationship with time since last use. Because we<br />
hypothesized that the effects <strong>of</strong> <strong>hormones</strong> on <strong>ovarian</strong><br />
<strong>cancer</strong> could vary by the specific regimen used, we<br />
examined various categories <strong>of</strong> hormone use separately<br />
(Table III). The OR associated with ever use <strong>of</strong> estrogen<br />
only was only slightly elevated; however, analyses by<br />
duration <strong>of</strong> use showed significantly increased ORs with<br />
longer duration <strong>of</strong> use (P for trend = .03). Ovarian<br />
<strong>cancer</strong> cases were twice as likely to report 10 years or<br />
more <strong>of</strong> unopposed estrogen use as the control women.<br />
There was no suggestion <strong>of</strong> increased <strong>risk</strong> for women<br />
who had taken estrogen <strong>and</strong> progestin always in<br />
combination, whether considering ever use or duration<br />
<strong>of</strong> use. Among women who had taken both estrogen <strong>and</strong><br />
progestin but not always at the same time, there was no<br />
clear trend with duration <strong>of</strong> use. This was a diverse<br />
exposure category in which some <strong>of</strong> the women took<br />
a progestin for nearly all <strong>of</strong> the time when they took<br />
estrogen, whereas other women took progestins for<br />
relatively short periods <strong>of</strong> time <strong>and</strong> were mostly exposed<br />
to unopposed estrogen. There were no significant<br />
associations with use <strong>of</strong> progestin alone (which was<br />
taken by only 7 cases <strong>and</strong> 1 control) or with testosterone<br />
(which was taken by 9 cases <strong>and</strong> 13 controls <strong>and</strong> was<br />
always taken in combination with estrogen <strong>and</strong>/or<br />
progestin).<br />
Table IV shows associations between the hormone<br />
regimens <strong>and</strong> histologic subtypes <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong>.<br />
Among users <strong>of</strong> estrogen only, the elevated <strong>risk</strong> was<br />
confined to the serous subtype, with no indication <strong>of</strong><br />
increased <strong>risk</strong> in other histologic types. There was not<br />
a strong indication <strong>of</strong> increased <strong>risk</strong> within any histologic<br />
subtype among users <strong>of</strong> estrogen <strong>and</strong> progestin. It<br />
must be noted that with the exception <strong>of</strong> the serous<br />
subtype there was a small number <strong>of</strong> cases within any<br />
given category defined by histology <strong>and</strong> hormone use.<br />
Therefore, it is difficult to say whether some <strong>of</strong> the<br />
observed differences in the ORs by histologic type were<br />
true differences or chance variation due to the small<br />
numbers.<br />
Comment<br />
Analyses from this population-based, case-control study<br />
showed no association between <strong>ovarian</strong> <strong>cancer</strong> <strong>and</strong><br />
menopausal hormone use overall, but suggested that<br />
long-term users <strong>of</strong> unopposed estrogen may be at increased<br />
<strong>risk</strong>. Although these findings are consistent with<br />
some studies reporting increased <strong>risk</strong> for long-term<br />
users, 7,11,21 the overall picture <strong>of</strong> the relationship between<br />
estrogen use <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> is far from consistent,<br />
with a number <strong>of</strong> studies finding no increased <strong>risk</strong> for<br />
hormone users. At a biological level, the relationship<br />
between estrogens <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> is similarly unclear.<br />
It has been shown that both normal <strong>and</strong> malignant<br />
<strong>ovarian</strong> epithelial cells have estrogen receptors; however,<br />
in vitro studies have not consistently found that estradiol<br />
increases proliferation <strong>of</strong> the <strong>ovarian</strong> epithelium. 9 Our<br />
findings suggested that any increased <strong>risk</strong> related to<br />
estrogen use was confined to the serous histologic subtype.<br />
Some investigators have reported a similar increase<br />
in <strong>risk</strong> for the serous subtype, 7,13,14 but they tended to report<br />
increased <strong>risk</strong> for endometrioid tumors as well. 7,13-15<br />
We saw no indication <strong>of</strong> increased <strong>risk</strong> for endometrioid
Moorman et al 81<br />
or clear cell tumors; however, we had few women with<br />
these histologic subtypes.<br />
Women who reported taking estrogen always with<br />
progestin did not appear to be at increased <strong>risk</strong>. The<br />
overall lack <strong>of</strong> association with combination estrogenprogestin<br />
therapy is consistent with the hypothesis that<br />
progestin protects against <strong>ovarian</strong> <strong>cancer</strong>. 19,20 The wellestablished<br />
protective effects <strong>of</strong> pregnancy or oral<br />
contraceptive use are beyond what can be explained<br />
simply through suppression <strong>of</strong> ovulation, <strong>and</strong> it has<br />
been suggested that high progesterone levels during<br />
pregnancy <strong>and</strong> the progestin component <strong>of</strong> oral contraceptives<br />
contribute significantly to reducing <strong>ovarian</strong><br />
<strong>cancer</strong> <strong>risk</strong>. 19,22 A possible mechanism for the protective<br />
effect <strong>of</strong> progestins was demonstrated in an in vivo study<br />
that showed that the progestin component <strong>of</strong> oral<br />
contraceptives has a potent apoptotic effect on the<br />
<strong>ovarian</strong> epithelium. 20 It must be noted, however, that<br />
the lack <strong>of</strong> association between <strong>ovarian</strong> <strong>cancer</strong> <strong>and</strong><br />
estrogen-progestin therapy that we observed contrasts<br />
with recently published findings from the Women’s<br />
Health Initiative r<strong>and</strong>omized clinical trial in which there<br />
was a suggestion <strong>of</strong> increased <strong>risk</strong> associated with<br />
estrogen plus progestin use (hazard ratio 1.58; 95% CI<br />
0.77–3.24) based on a total <strong>of</strong> 32 cases <strong>of</strong> invasive<br />
<strong>ovarian</strong> <strong>cancer</strong>. 12<br />
The overall findings from the Women’s Health<br />
Initiative, in which the <strong>risk</strong>s for coronary heart disease,<br />
stroke, pulmonary embolism, <strong>and</strong> breast <strong>cancer</strong> were all<br />
statistically significantly elevated among estrogen plus<br />
progestin users, 23 have resulted in changes in recommendations<br />
for use <strong>of</strong> menopausal <strong>hormones</strong>. Given the<br />
observed lack <strong>of</strong> benefit for cardiovascular conditions,<br />
there is no longer a strong justification for long-term use<br />
<strong>of</strong> menopausal <strong>hormones</strong> for prevention <strong>of</strong> chronic<br />
diseases, <strong>and</strong> many women discontinued them after<br />
publication <strong>of</strong> the Women’s Health Initiative findings.<br />
Current recommendations for use <strong>of</strong> estrogen <strong>and</strong>/or<br />
progestin limited to short-term treatment <strong>of</strong> menopausal<br />
symptoms with the lowest effective dose 24 would not be<br />
expected to have an important effect on <strong>ovarian</strong> <strong>cancer</strong><br />
<strong>risk</strong> based on our findings <strong>and</strong> the findings <strong>of</strong> most other<br />
studies, in which any increased <strong>risk</strong> <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong><br />
seemed to be most pronounced among long-term users.<br />
An important strength <strong>of</strong> this study was that we were<br />
able to examine different hormone regimens in relation<br />
to <strong>ovarian</strong> <strong>cancer</strong> <strong>risk</strong>. However, our analyses were<br />
somewhat limited by the number <strong>of</strong> women who had<br />
taken any specific regimen, which prevented us from<br />
more thoroughly considering issues <strong>of</strong> latency, recency,<br />
<strong>and</strong> duration <strong>of</strong> use with any given hormone regimen.<br />
Another limitation was in our ability to do race-specific<br />
analyses. Although our study population was closer to<br />
the US population in terms <strong>of</strong> representation <strong>of</strong> African<br />
Americans (approximately 14%) than many other<br />
studies that have addressed this question, the number<br />
<strong>of</strong> African Americans was still too low to do meaningful<br />
analyses.<br />
Although it would be expected that in the future there<br />
should be relatively few women who would have exposure<br />
to the patterns <strong>of</strong> menopausal hormone use that would<br />
likely increase their <strong>risk</strong> for <strong>ovarian</strong> <strong>cancer</strong>, clinicians<br />
should be aware <strong>of</strong> the past histories <strong>of</strong> hormone use<br />
among their patients. Based on data suggesting both<br />
a latency effect <strong>of</strong> 10 or more years <strong>and</strong> a persistence <strong>of</strong><br />
effect such that users continue to be at increased <strong>risk</strong> for<br />
some years after stopping <strong>hormones</strong>, 25 it is important that<br />
women <strong>and</strong> their physicians be alert to possible <strong>risk</strong>s for<br />
<strong>cancer</strong> among long-term users <strong>of</strong> menopausal <strong>hormones</strong>,<br />
particularly among women who used unopposed estrogens.<br />
References<br />
1. Weiss NS, Cook LS, Farrow DC, Rosenblatt KA. Ovarian <strong>cancer</strong>.<br />
In: Schottenfeld D, Fraumeni JF Jr, editors. Cancer epidemiology<br />
<strong>and</strong> prevention, 2nd ed. New York: Oxford University Press; 1996.<br />
p. 1040-57.<br />
2. Riman T, Persson I, Nilsson S. Hormonal aspects <strong>of</strong> epithelial<br />
<strong>ovarian</strong> <strong>cancer</strong>: review <strong>of</strong> epidemiological evidence. Clin Endocrinol<br />
1998;49:695-707.<br />
3. Hempling RE, Wong C, Piver MS, Natarajan N, Mettlin CJ.<br />
Hormone replacement therapy as a <strong>risk</strong> factor for epithelial<br />
<strong>ovarian</strong> <strong>cancer</strong>: results <strong>of</strong> a case-control study. Obstet Gynecol<br />
1997;89:1012-6.<br />
4. Negri E, Tzonou A, Beral V, Lagiou P, Trichopoulos D, Parazzini<br />
F, et al. Hormonal therapy for menopause <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> in<br />
a collaborative re-analysis <strong>of</strong> European studies. Int J Cancer<br />
1999;80:848-51.<br />
5. Chiaffarino F, Pelucchi C, Parazzini F, Negri E, Franceschi S,<br />
Talamini R, et al. Reproductive <strong>and</strong> hormonal factors <strong>and</strong> <strong>ovarian</strong><br />
<strong>cancer</strong>. Ann Oncol 2001;12:337-41.<br />
6. Tavani A, Ricci E, LaVecchia C, Surace M, Benzi G, Parazzini F,<br />
et al. Influence <strong>of</strong> menstrual <strong>and</strong> reproductive factors on <strong>ovarian</strong><br />
<strong>cancer</strong> <strong>risk</strong> in women with <strong>and</strong> without family history <strong>of</strong> breast or<br />
<strong>ovarian</strong> <strong>cancer</strong>. Int J Epidemiol 2000;29:799-802.<br />
7. Riman T, Dickman PW, Nilsson S, Correia N, Nordlinder H,<br />
Magnusson CM, et al. Hormone replacement therapy <strong>and</strong> the <strong>risk</strong><br />
<strong>of</strong> invasive epithelial <strong>ovarian</strong> <strong>cancer</strong> in Swedish women. J Natl<br />
Cancer Inst 2002;94:497-504.<br />
8. Bosetti C, Negri E, Franceschi S, Trichopoulos D, Beral V,<br />
LaVecchia C. Relationship between postmenopausal hormone<br />
replacement therapy <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong>. JAMA 2001;285:3089-90.<br />
9. Sit ASY, Modugno F, Weissfeld JL, Berga SL, Ness RB. Hormone<br />
replacement therapy formulations <strong>and</strong> <strong>risk</strong> <strong>of</strong> epithelial <strong>ovarian</strong><br />
carcinoma. Gynecol Oncol 2002;86:118-23.<br />
10. Lacey JV Jr, Mink PJ, Lubin JH, Sherman ME, Troisi R, Hartge<br />
P, et al. <strong>Menopausal</strong> hormone replacement therapy <strong>and</strong> <strong>risk</strong> <strong>of</strong><br />
<strong>ovarian</strong> <strong>cancer</strong>. JAMA 2002;288:334-41.<br />
11. Rodriguez C, Patel AV, Calle EE, Jacob EJ, Thun MJ. Estrogen<br />
replacement therapy <strong>and</strong> <strong>ovarian</strong> <strong>cancer</strong> mortality in a large<br />
prospective study <strong>of</strong> US women. JAMA 2001;285:1460-5.<br />
12. Anderson GL, Judd HL, Kaunitz AM, Barad DH, Beresford SAA,<br />
Pettinger M, et al, for the Women’s Health Initiative Investigators.<br />
Effects <strong>of</strong> estrogen plus progestin on gynecologic <strong>cancer</strong>s <strong>and</strong><br />
associated diagnostic procedures. JAMA 2003;290:1739-48.<br />
13. Risch HA, Marrett LD, Jain M, Howe GR. Differences in <strong>risk</strong><br />
factors for epithelial <strong>ovarian</strong> <strong>cancer</strong> by histologic type. Am J<br />
Epidemiol 1996;144:363-72.
82 Moorman et al<br />
14. Weiss NS, Lyon JL, Krishnamurthy S, Dietert SE, Liff JM, Daling<br />
JR. Noncontraceptive estrogen use <strong>and</strong> the occurrence <strong>of</strong> <strong>ovarian</strong><br />
<strong>cancer</strong>. J Natl Cancer Inst 1982;68:95-8.<br />
15. LaVecchia C, Liberati A, Franceschi S. Noncontraceptive estrogen<br />
use <strong>and</strong> the occurrence <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong>. J Natl Cancer Inst<br />
1982;69:1207.<br />
16. Smith DC, Prentice R, Thompson DJ, Herrmann WL. Association<br />
<strong>of</strong> exogenous estrogen <strong>and</strong> endometrial carcinoma. N Engl J Med<br />
1975;293:1164-7.<br />
17. Kennedy DL, Baum C, Forbes MB. Noncontraceptive estrogens <strong>and</strong><br />
progestins: use patterns over time. Obstet Gynecol 1985;65:441-6.<br />
18. Wysowski DK, Golden L, Burke L. Use <strong>of</strong> menopausal estrogens<br />
<strong>and</strong> medroxyprogesterone in the United States, 1982-1992. Obstet<br />
Gynecol 1995;85:6-10.<br />
19. Risch HA. Hormonal etiology <strong>of</strong> epithelial <strong>ovarian</strong> <strong>cancer</strong>, with<br />
a hypothesis concerning the role <strong>of</strong> <strong>and</strong>rogens <strong>and</strong> progesterone. J<br />
Natl Cancer Inst 1998;90:1774-86.<br />
20. Rodriguez GC, Walmer DK, Cline M, Krigman H, Lessey BA,<br />
Whitaker RS, et al. Effect <strong>of</strong> progestin on the <strong>ovarian</strong> epithelium <strong>of</strong><br />
macaques: <strong>cancer</strong> prevention through apoptosis? J Soc Gynecol<br />
Investig 1998;5:271-6.<br />
21. Cramer DW, Hutchison GB, Welch WR, Scully RE, Ryan KJ.<br />
Determinants <strong>of</strong> <strong>ovarian</strong> <strong>cancer</strong> <strong>risk</strong>. I. Reproductive experiences<br />
<strong>and</strong> family history. J Natl Cancer Inst 1983;71:711-6.<br />
22. Schildkraut JM, Calingaert B, Marchbanks PA, Moorman PG,<br />
Rodriguez GC. Impact <strong>of</strong> progestin <strong>and</strong> estrogen<br />
potency in oral contraceptives on <strong>ovarian</strong> <strong>cancer</strong> <strong>risk</strong>. J Natl<br />
Cancer Inst 2002;94:32-8.<br />
23. Writing Group for the Women’s Health Initiative Investigators.<br />
Risks <strong>and</strong> benefits <strong>of</strong> estrogen plus progestin in healthy postmenopausal<br />
women. Principal results from the Women’s Health<br />
Initiative R<strong>and</strong>omized Clinical Trial. JAMA 2002;288:321-33.<br />
24. US Food <strong>and</strong> Drug Administration FDA Talk Paper. FDA plans<br />
to evaluate results <strong>of</strong> Women’s Health Initiative study for<br />
estrogen-alone therapy. Accessed: August 15, 2004. http://www.<br />
fda.gov/bbs/topics/ANSWERS/2004/ANS01281.html<br />
25. Risch HA. Hormone replacement therapy <strong>and</strong> the <strong>risk</strong> <strong>of</strong> <strong>ovarian</strong><br />
<strong>cancer</strong>. Gynecol Oncol 2002;86:115-7.