Trust Board Papers - Barts Health NHS Trust
Trust Board Papers - Barts Health NHS Trust
Trust Board Papers - Barts Health NHS Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
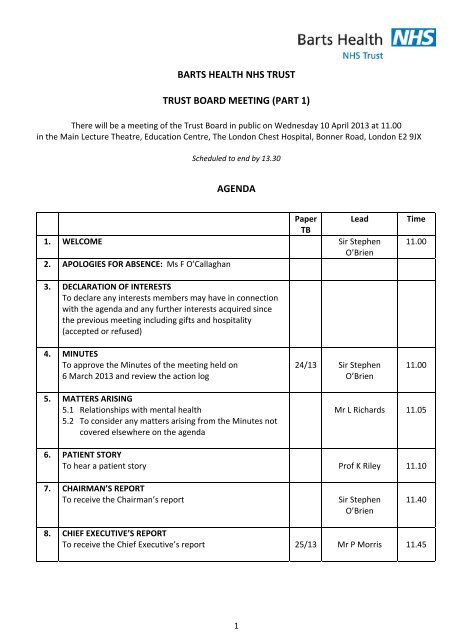
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING (PART 1)<br />
There will be a meeting of the <strong>Trust</strong> <strong>Board</strong> in public on Wednesday 10 April 2013 at 11.00<br />
in the Main Lecture Theatre, Education Centre, The London Chest Hospital, Bonner Road, London E2 9JX<br />
Scheduled to end by 13.30<br />
AGENDA<br />
Paper Lead<br />
TB<br />
1. WELCOME Sir Stephen<br />
O’Brien<br />
2. APOLOGIES FOR ABSENCE: Ms F O’Callaghan<br />
Time<br />
11.00<br />
3. DECLARATION OF INTERESTS<br />
To declare any interests members may have in connection<br />
with the agenda and any further interests acquired since<br />
the previous meeting including gifts and hospitality<br />
(accepted or refused)<br />
4. MINUTES<br />
To approve the Minutes of the meeting held on<br />
6 March 2013 and review the action log<br />
24/13 Sir Stephen<br />
O’Brien<br />
11.00<br />
5. MATTERS ARISING<br />
5.1 Relationships with mental health<br />
5.2 To consider any matters arising from the Minutes not<br />
covered elsewhere on the agenda<br />
Mr L Richards 11.05<br />
6. PATIENT STORY<br />
To hear a patient story Prof K Riley 11.10<br />
7. CHAIRMAN’S REPORT<br />
To receive the Chairman’s report<br />
Sir Stephen<br />
O’Brien<br />
11.40<br />
8. CHIEF EXECUTIVE’S REPORT<br />
To receive the Chief Executive’s report 25/13 Mr P Morris 11.45<br />
1
Paper<br />
TB<br />
Lead<br />
Time<br />
QUALITY, SAFETY AND PERFORMANCE<br />
9. PERFORMANCE – 2012/13 MONTH 11<br />
9.1 Integrated Performance Report<br />
9.2 Quality and Safety performance<br />
9.3 Financial performance<br />
26/13<br />
27/13<br />
28/13<br />
Mr L Readman<br />
Prof K Riley/<br />
Dr S Ryan<br />
Mr M Ogden<br />
12.20<br />
GOVERNANCE AND ASSURANCE<br />
10. ANNUAL PLAN 2013/14<br />
To receive the final version of the annual plan 29/13 Mr P Morris 12.50<br />
11. INFORMATION GOVERNANCE TOOLKIT<br />
To ratify the 2012/13 IG Toolkit scores 30/13 Mr I Walker 13.00<br />
12. BOARD ASSURANCE FRAMEWORK<br />
To receive and approve the BAF 31/13 Mr I Walker 13.05<br />
13. TRUST BOARD MEMBERSHIP<br />
To note the reappointment of a Non Executive Director 32/13 Mr I Walker 13.15<br />
14. STANDING ORDERS AND STANDING FINANCIAL<br />
INSTRUCTIONS<br />
To approve revisions to the SOs and SFIs 33/13 Mr M Ogden 13.15<br />
15. USE OF THE SEAL<br />
To ratify use of the <strong>Trust</strong> Seal 34/13 Mr I Walker 13.20<br />
16. SINGLE OPERATING MODEL<br />
To receive and approve the monthly submission 35/13 Mr L Readman 13.20<br />
17. ORAL REPORTS FROM BOARD COMMITTEES<br />
17.1 Quality Assurance Committee: 13 March 2013<br />
17.2 FT Sub Committee: 13 March 2013<br />
17.3 Finance and Investment Committee: 13 March and<br />
10 April 2013<br />
Ms S James<br />
Sir Stephen<br />
O’Brien<br />
Mr G Dalal<br />
13.25<br />
2
Paper<br />
TB<br />
Lead<br />
Time<br />
ITEMS FOR INFORMATION<br />
18. ANY OTHER BUSINESS<br />
19. QUESTIONS FROM MEMBERS OF THE PUBLIC 13.30<br />
20. DATE OF THE NEXT MEETING<br />
The next meeting of the <strong>Trust</strong> <strong>Board</strong> in public will be held<br />
on Wednesday 1 May 2013 at 11.00 in Room 8, Education<br />
Centre, Burdett House, Mile End Hospital, Bancroft Road,<br />
London E1 4DG.<br />
21. RESOLUTION<br />
That representatives of the press and other members of the<br />
public be excluded from the remainder of this meeting<br />
having regard to the confidential nature of the business to<br />
be transacted, publicity on which would be prejudicial to<br />
the public interest (section (2) Public Bodies (Admissions to<br />
Meetings) Act 1960).<br />
Ian Walker<br />
Director of Corporate Affairs and <strong>Trust</strong> Secretary<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
020 7092 5212<br />
3
TB 24/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING (PART 1)<br />
Minutes of the <strong>Trust</strong> <strong>Board</strong> meeting held in public on Wednesday 6 March 2013 at 11.00<br />
in Rooms 1 and 2, Ground Floor, Pathology and Pharmacy Building, Newark Street,<br />
The Royal London Hospital, London E1 1BB<br />
Present:<br />
In attendance:<br />
Apologies:<br />
Sir Stephen O’Brien (Chairman)<br />
Mr P Wright (Vice Chairman and Senior Independent Director)<br />
Mr P Morris (Chief Executive)<br />
Ms S James (Non Executive Director)<br />
Mr M Ogden (Chief Financial Officer)<br />
Mr L Richards (Chief Operating Officer)<br />
Professor K Riley (Chief Nurse)<br />
Dr S Ryan (Medical Director)<br />
Professor R Trembath (Non Executive Director)<br />
Ms A Whitaker (Non Executive Director)<br />
Mr T Lewis (Deputy Chief Executive and Development Director)<br />
Ms F O’Callaghan (Director of Strategy)<br />
Mr M Pantlin (Director of Human Resources)<br />
Mr L Readman (Chief Information Officer)<br />
Mr I Walker (Director of Corporate Affairs and <strong>Trust</strong> Secretary)<br />
Ms H Shanahan (Deputy Chief Nurse, Patient Experience) – agenda item 6<br />
Ms F Hollwey (Head of Patient Experience and Engagement) – agenda item 6<br />
Ms P Mason (Patient) – agenda item 6<br />
Ms M Mason (Relative) – agenda item 6<br />
Ms M Banerjee (Non Executive Director)<br />
Mr A Camp (Non Executive Director)<br />
Mr G Dalal (Non Executive Director)<br />
21/13 WELCOME AND INTRODUCTION<br />
The Chairman welcomed everyone to the meeting. He explained that Ms Banerjee<br />
would be taking a period of leave of absence for personal reasons.<br />
1
TB 24/13<br />
The Chairman noted that this was the final <strong>Trust</strong> <strong>Board</strong> meeting which Mr Lewis<br />
would be attending before taking up his new role as Chief Executive of Sandwell<br />
and West Birmingham Hospitals <strong>NHS</strong> <strong>Trust</strong>. On behalf of the <strong>Trust</strong> <strong>Board</strong>, the<br />
Chairman expressed his gratitude to Mr Lewis for all he had achieved in his time at<br />
both <strong>Barts</strong> and The London <strong>NHS</strong> <strong>Trust</strong> and <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> and wished him<br />
every success for the future.<br />
22/13 DECLARATIONS OF INTEREST<br />
Attendees were reminded of the need to declare any interests they may have in<br />
connection with the agenda.<br />
No declarations were received.<br />
23/13 MINUTES<br />
The Minutes of the meeting of the <strong>Trust</strong> <strong>Board</strong> held in public on 6 February 2013<br />
were received and approved as a correct record of the proceedings.<br />
The Minutes were duly signed.<br />
The <strong>Board</strong> noted the progress made on closing issues on the action log appended<br />
to the Minutes. The following points were specifically noted:<br />
The Chairman reported that he had discussed the issue of the name of the<br />
Charity with its Chairman and an update would be provided at the next<br />
meeting.<br />
The Chief Operating Officer would provide an update on work with the<br />
mental health trust at the next meeting.<br />
Action: Chief Operating Officer<br />
The Chief Operating Officer confirmed that he had discussed with CAG<br />
leadership teams the importance of monitoring security arrangements and<br />
challenging visitors to wards and clinical areas. The issue was also being<br />
picked up in regular ward conversations.<br />
The Deputy Chief Executive confirmed that a report on Estates and the New<br />
Hospitals Programme would now be produced during the next quarter. The<br />
existing action would be amended accordingly.<br />
On New Hospitals benefits realisation, it was agreed to close the current<br />
action and that the Deputy Chief Executive would discuss with the Chief<br />
Executive how best to monitor benefits realisation for <strong>Barts</strong> Phase 2.<br />
2
TB 24/13<br />
24/13 MATTERS ARISING<br />
There were no matters not covered elsewhere on the agenda.<br />
25/13 PATIENT STORY<br />
The Deputy Chief Nurse for Patient Experience introduced Ms Pam Mason, who<br />
had formally consented to tell her story. She was accompanied by her daughter,<br />
Ms Margaret Mason.<br />
Ms Mason explained that she had been a foster carer for 14 years. She had a son<br />
Philip who she had adopted when he was two years old, two birth daughters and<br />
13 foster children. Her story related to Philip who was 35 and suffered from<br />
Down’s Syndrome and autism. His understanding was very limited and his autism<br />
meant that routine was very important to him.<br />
Philip had started to become more acutely ill around four years ago and was<br />
admitted to a ward via A&E Resus at The Royal London. His dad had wanted to<br />
stay with Philip to provide him with the support he needed but the ward staff had<br />
said that parents could not stay with adult patients. Eventually they had offered<br />
his dad a chair and a mattress on the floor. But no one on the ward had<br />
understood Philip’s needs.<br />
Philip was subsequently admitted to hospital a second time and his dad was again<br />
offered the floor to sleep on. He had then spoken to the bed manager who<br />
managed to organise a bed for him. However, no one offered him anything to eat<br />
or drink despite him not being able to leave Philip alone.<br />
On Philip’s third admission, there was no bed available for parents and they were<br />
not allowed to stay with Philip. They asked the ward staff if they could make a care<br />
plan for Philip but were told that they only did that for children. They also asked if<br />
they could come in the next morning to help care for Philip but were told that they<br />
could not visit until 2.00pm. Philip’s parents then received a call from the ward at<br />
5.30am asking them to come in because Philip needed support.<br />
During that stay they had tried to give the staff a copy of a book about Philip and<br />
his requirements but the staff had told his mum that they did not have time to read<br />
it. Tablets were being left by Philip’s bedside despite him not knowing how to take<br />
them. He was given tea in flexible cups which were not appropriate given his<br />
condition. A request for a yoghurt to take his tablets with was refused as and on<br />
one occasion he was given sandwiches because they had run out of food.<br />
Ms Mason explained that she had contacted PALS, not to make a complaint but in<br />
an attempt to understand what support was available for patients with learning<br />
disabilities. She was particularly concerned about the experience of patients and<br />
carers who were not confident enough to speak up about their problems or who<br />
experienced language or other barriers in doing so.<br />
3
TB 24/13<br />
She felt that there was a particular need to focus on staff awareness and training,<br />
including of the catering staff who had passed Philip’s bed without stopping to ask<br />
him about his choice of food because they had assumed he was not able to make a<br />
choice despite one of his parents being available to help him. It might, for<br />
example, be helpful to identify people who could visit wards to talk to staff and<br />
carers about what would help during the stay.<br />
She also emphasised the need to recognise that it was not appropriate to keep<br />
moving patients with autism. In Philip’s case, he had been moved from one ward<br />
to another without his parents being informed so that they could reassure him.<br />
The Chairman thanked Ms Mason for being willing to tell her story to the <strong>Board</strong><br />
and invited questions and comments from <strong>Board</strong> members. The following points<br />
were made in discussion:<br />
<br />
<br />
<br />
The Chairman noted that this was the second patient story which had<br />
involved the experience of a patient with autism.<br />
The Chief Operating Officer asked about Philip’s experience in A&E. Ms<br />
Mason confirmed that this had not been problematic and the difficulties<br />
had arisen in the ward environment.<br />
The Chief Nurse thanked Ms Mason for telling the story and said that<br />
she was extremely sorry to hear about her family’s experiences. She<br />
was also very grateful to Ms Mason for offering to work with the <strong>Trust</strong><br />
on improving the experience of patients in the future. A learning<br />
disabilities action plan was due to be presented to the Quality<br />
Assurance Committee the following week which would include a focus<br />
on strengthening and better utilising available resources. In addition,<br />
the <strong>Trust</strong> would be launching its Care Campaign later in the week with a<br />
focus on the fundamental, basic standards of nursing care.<br />
Ms James apologised to Ms Mason for this experience. As in the<br />
previous case the <strong>Board</strong> had heard about, it appeared that the <strong>Trust</strong><br />
was failing to make use of the invaluable help and expertise that carers<br />
were able to offer.<br />
<br />
The Chief Nurse asked Ms Mason whether she had raised the issues<br />
with the Senior Sister or Charge Nurse at the time. Ms Mason explained<br />
that some of the responses were coming from staff at that level. The<br />
Chief Nurse felt that some of the flexibility and standard practice of the<br />
past of working with carers had perhaps been lost and Ms Whitaker<br />
encouraged the empowerment of staff to be able to exercise greater<br />
flexibility in response to individual circumstances.<br />
4
TB 24/13<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
The Deputy Chief Executive hoped that the increase in single room<br />
capacity at The Royal London meant that it was now easier to<br />
accommodate carers being able to stay with patients overnight. He also<br />
observed that a common theme from recent patient stories had been a<br />
failure of the organisation to respond when concerns were raised.<br />
Consideration therefore needed to be given as to how issues could be<br />
addressed more rapidly at the time they were identified rather than<br />
waiting to apologise later.<br />
The Chief Operating Officer cited the example of the Virginia Mason<br />
Hospital in the United States which identified ‘stop the line’ events<br />
which could be raised by patients, carers or staff and had to be<br />
responded to by an Executive within half an hour. While there may be<br />
practical challenges in implementing such a system, it provided a clear<br />
focus on the need for effective escalation routes.<br />
The Medical Director expressed his regret and frustration at what Philip<br />
and his family had experienced. He noted that on a paediatric ward it<br />
was normal for parents and carers to be closely involved in the care of<br />
their children and there was therefore no reason why this could and<br />
should not be the same for patients with learning disabilities.<br />
The Medical Director noted that doctors should act as advocates for<br />
patients and asked Ms Mason whether she had felt able to raise her<br />
concerns with the doctors treating Philip. Ms Mason said that the<br />
doctors were aware of some of the issues but had not intervened. She<br />
emphasised that she had been satisfied with the quality of clinical care<br />
provided by the doctors and nurses on the wards.<br />
Ms Whitaker asked how the voices of patients and carers who were not<br />
as confident in raising their concerns were heard. The Chief Nurse<br />
explained that a review was being undertaken of the PALS and<br />
complaints function with a focus on the routes for concerns to be raised<br />
and escalated. There was also a key role for Matrons to play in<br />
intervening rapidly to address problems locally as they arose.<br />
The Chief Information Officer was very sorry to hear about this<br />
experience and said that he would welcome the opportunity to work<br />
with Ms Mason to look at how the care record held by parents and<br />
carers could be integrated into the main patient health record.<br />
Professor Trembath emphasised the importance of learning from the<br />
practice and experience of colleagues in mental health services.<br />
5
TB 24/13<br />
The Chairman concluded that there was a clear sense of outrage among <strong>Board</strong><br />
members at what Philip and his family had experienced and that there was a need<br />
to receive an update on actions taken in the near future, including in relation to<br />
work with the mental health trust. The Chief Nurse proposed further discussion at<br />
the Quality Assurance Committee meeting the following week as part of the item<br />
on learning disabilities, specifically considering whether the issues highlighted in<br />
this story were adequately addressed by the proposed strategy. The outcome of<br />
this discussion would then be reported back to the <strong>Board</strong>.<br />
Action: Chief Nurse<br />
The Chairman thanked Ms Mason and her daughter for attending the meeting and<br />
the Deputy Chief Nurse for Patient Experience and the Head of Patient Experience<br />
and Engagement for supporting Ms Mason in telling the story.<br />
26/13 CHAIRMAN’S REPORT<br />
The Chairman reported on the following matters:<br />
<br />
<br />
The delivery of operational performance standards remained a key priority<br />
for the <strong>Trust</strong> <strong>Board</strong>. Improving performance on those indicators which<br />
were currently tracking below trajectory was essential if the <strong>Trust</strong> was to<br />
drive forward its wider strategic initiatives.<br />
With a strong leadership team in place in the top tiers of the organisation,<br />
there was a need to focus on staff engagement and organisational culture.<br />
27/13 CHIEF EXECUTIVE’S REPORT<br />
The Chief Executive introduced TB 14/13, his report on recent developments, and<br />
highlighted the following:<br />
<br />
<br />
As set out in the report, there was agreement in principle from the <strong>Board</strong>s<br />
of both <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> and University College London Hospitals <strong>NHS</strong><br />
Foundation <strong>Trust</strong> to bring together The London Chest, St Bartholomew’s<br />
and The London Independent Hospitals to create one of the largest and<br />
finest cardiac centres in the world from both a service and research<br />
perspective.<br />
There was now a 24/7 specialist heart rhythm centre on the <strong>Barts</strong> site which<br />
was able to offer direct access via the London Ambulance Service to<br />
patients in north London suffering from three of the most serious acute<br />
heart rhythm problems. The Chief Executive reported that he had visited<br />
the centre the previous week and had been very impressed by it.<br />
6
TB 24/13<br />
<br />
On operational performance, MRSA, emergency care, cancer 62‐day waiting<br />
times and mixed sex accommodation breaches remained off track. There<br />
were encouraging signs on two of these indicators while two required<br />
greater focus:<br />
o On MRSA, the current run rate was significantly below that in the<br />
first half of the year and there had been no bacteraemias at The<br />
Royal London for over 100 days. However, the <strong>Trust</strong> would not be<br />
compliant with its annual threshold for 2012/13.<br />
o There had also been positive progress on cancer 62‐day waits with a<br />
narrowing of the problem in urology. There was an improvement<br />
plan in place which, if achieved, should deliver compliance with the<br />
national standard by the end of April 2013.<br />
o Mixed sex accommodation breaches were being driven substantially<br />
by failures to move patients from critical care to general beds within<br />
six hours when they were clinically fit for step down. Improving<br />
overall patient flow and discharge arrangements should significantly<br />
reduce the number of such breaches.<br />
o On emergency care, The Royal London and Whipps Cross were<br />
concerns. Performance at the former had slipped recently while the<br />
latter had not recovered from a downturn in performance around<br />
November 2012. Significant work was being undertaken to improve<br />
performance but this had not yet translated into the required<br />
improvements in compliance. While the <strong>Trust</strong> remained on track to<br />
meet the 95% All Types standard at year end, there were concerns<br />
that there was not yet a sufficiently robust plan to deliver a run rate<br />
of 95% or above from April 2013. The Chief Executive reported that<br />
he would be reviewing with the Chief Operating Officer the action<br />
plans in place on a site and CAG basis to achieve compliance on a<br />
sustainable basis.<br />
<br />
The publication of the report of Sir Robert Francis’ public inquiry into the<br />
failings of care at Mid Staffordshire <strong>NHS</strong> Foundation <strong>Trust</strong> had been a major<br />
development since the previous <strong>Board</strong> meeting and was the subject of a<br />
separate agenda item and paper. In response to a request from the<br />
Secretary of State for <strong>Health</strong>, the <strong>Trust</strong> was able to confirm that it neither<br />
prevented nor discouraged staff from raising concerns which could be<br />
considered to be in the public interest as part of its contractual<br />
arrangements with them as employees. As reported in the separate <strong>Board</strong><br />
paper, the <strong>Trust</strong> Management <strong>Board</strong> had discussed the Francis report in<br />
detail shortly after its publication. In addition, the Chief Executive was<br />
personally attending each CAG <strong>Board</strong> before the end of March where the<br />
Francis report would form part of the discussion. He was also meeting oneto‐one<br />
with all 38 Group and Clinical Directors.<br />
7
TB 24/13<br />
The following points were raised in discussion:<br />
<br />
The Vice Chairman asked for an update on the work of the Integrated<br />
Cancer System (ICS) for north east and north central London. The Chief<br />
Executive recalled that, at its previous meeting, the <strong>Trust</strong> <strong>Board</strong> had<br />
recognised that the ICS had 12‐14 clinically‐led tumour groups which were<br />
reviewing specialist cancer provision from a patient and population health<br />
perspective and the <strong>Board</strong> had agreed to support this approach. A<br />
proposition on the approach to radiotherapy was still to emerge. Decisions<br />
had already come forward in relation to urology, where there was a clinical<br />
consensus for University College London Hospitals <strong>NHS</strong> Foundation <strong>Trust</strong> to<br />
be the preferred location for bladder and prostate cancers, and in relation<br />
to upper tract renal cancers, where the Royal Free London <strong>NHS</strong> Foundation<br />
<strong>Trust</strong> was the preferred location. Decisions were due shortly on liver and<br />
pancreatic cancers and head and neck cancers, and later in the year on<br />
gynaecological and blood cancers.<br />
Of the five tumour groups where decisions were upcoming, <strong>Barts</strong> <strong>Health</strong><br />
had interests in all of them. It was also important to recognise that<br />
common cancers, such as lung, breast and skin cancer, would always be an<br />
important part of the service provision of <strong>Barts</strong> <strong>Health</strong>, including in terms of<br />
prevention and early detection.<br />
The Vice Chairman noted that it would be important to fully understand the<br />
clinical, operational and financial impacts on other <strong>Trust</strong> services of the<br />
forthcoming decisions on the locations for specialist cancer treatment. The<br />
Chief Executive agreed and explained that the Director of Strategy was<br />
working closely with the CAGs to ensure that such implications were<br />
assessed.<br />
The Director of Strategy emphasised that the activity impact of any changes<br />
in the location of specialist cancer services would be marginal when<br />
compared to the overall level of <strong>Trust</strong> cancer activity. The core of the<br />
<strong>Trust</strong>’s cancer services would remain very significant and span prevention,<br />
diagnosis, secondary care and palliative care.<br />
Professor Trembath informed the <strong>Board</strong> that Queen Mary University of<br />
London and University College London had agreed to commission an<br />
independent review of where there was academic competition and<br />
complementarity in work on cancer to support decisions on how the<br />
academic endeavour could best support future clinical service provision.<br />
The <strong>Trust</strong> <strong>Board</strong> noted these and the other items set out in the Chief Executive’s<br />
report and, as requested, delegated approval of the <strong>Trust</strong>’s 2012/13 Information<br />
Governance Toolkit submission to the Chief Executive. It was noted that a paper<br />
providing details of the Information Governance Toolkit submission would be<br />
presented at the next meeting of the <strong>Trust</strong> <strong>Board</strong>.<br />
Action: Director of Corporate Affairs and <strong>Trust</strong> Secretary<br />
8
TB 24/13<br />
28/13 PERFORMANCE – 2012/13 MONTH 10<br />
(i) Integrated Performance Report<br />
The Deputy Chief Executive introduced TB 15/13, the first Integrated Performance<br />
Report for <strong>Barts</strong> <strong>Health</strong>. He recorded his thanks to all those who had worked on<br />
the development of the new Integrated Performance Framework (IPF), particularly<br />
Ms Susan Murray. Inevitably the IPF remained work in progress and would be<br />
further developed in the months ahead in response to feedback.<br />
The following points were highlighted:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
The IPF reflected the <strong>Board</strong>’s previous decision that there should be a key<br />
focus on the views of the <strong>Trust</strong>’s patients, staff and students, regulators and<br />
partners.<br />
In terms of the RAG status, Red indicated below the line performance,<br />
Green indicated above the line performance, Blue meant that no threshold<br />
had yet been set and Grey meant that data were not yet available.<br />
Little progress had been made to date on integrating the domain relating to<br />
the views of partners and significant work was still required to integrate<br />
financial information into the IPF.<br />
In terms of the views of regulators, the position was as the Chief Executive<br />
had set out earlier in the meeting. The <strong>Trust</strong> was compliant with the<br />
Cooperation and Competition Panel’s indicators for the second successive<br />
quarter and the Deputy Chief Executive agreed to circulate the details of<br />
these following the <strong>Board</strong> meeting.<br />
Action: Deputy Chief Executive<br />
In terms of patient views, the ratings were based on Real Time Feedback<br />
results. It was encouraging that the Cancer CAG was rated Green and this<br />
provided an area for other CAGs to seek to learn from.<br />
On staff and student views, many of the red ratings were currently driven<br />
by surveys of postgraduate medical trainees. However, the results of the<br />
monthly ‘Pulse’ surveys of 2,000 members of staff would soon be available<br />
to feed into the IPF.<br />
Alongside continuing to develop the IPF, a key challenge would be to stand<br />
down other reports and indicators which duplicated or overlapped with<br />
information in the IPF.<br />
9
TB 24/13<br />
The following points were made in discussion:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Ms James welcomed the new IPF and agreed on the need to retire other<br />
reports. She asked who would be leading on this. It was confirmed that the<br />
Chief Information Officer would be leading on this in future, working with<br />
Executive Director colleagues.<br />
The Chief Nurse reported that discussions were continuing about how the<br />
important narrative on quality and safety of care currently contained in the<br />
separate Quality and Safety report could be integrated into the IPF. In the<br />
meantime, it was planned to continue with a separate Quality and Safety<br />
report.<br />
Ms James felt that it would be helpful to review the new report in detail to<br />
ensure that <strong>Board</strong> members fully understood the presentation of the<br />
indicators and the approach to exception reporting. It was agreed that a<br />
separate session would be arranged with the Chief Information Officer to<br />
increase familiarity with the IPF.<br />
Action: Director of Corporate Affairs<br />
Ms Whitaker encouraged the use of exception reporting within the body of<br />
the Integrated Performance Report rather than as separately appended<br />
reports. The Chief Information Officer confirmed that this was the<br />
intention.<br />
Ms James reminded <strong>Board</strong> members that the Quality Assurance Committee<br />
had a role in looking at specific performance issues in greater detail at the<br />
request of the <strong>Trust</strong> <strong>Board</strong>.<br />
The Vice Chairman asked for further details of VTE screening performance<br />
in the context of the chart on page 13 of the report. The Deputy Chief<br />
Executive explained that the <strong>Trust</strong> as a whole was compliant with the 90%<br />
minimum standard in the year to date but performance had deteriorated<br />
sharply since autumn 2012. Actions were in place to recover performance<br />
at The Royal London, Mile End and <strong>Barts</strong> but performance had also recently<br />
deteriorated at Whipps Cross. The Executive Team was discussing what<br />
further action was required to improve performance, including monitoring<br />
compliance by individual consultant.<br />
The Director of Academic <strong>Health</strong> Sciences highlighted continued poor<br />
compliance with statutory and mandatory training requirements. A new<br />
<strong>Trust</strong>‐wide database was providing greater visibility of compliance<br />
information and enabled managers to review individual compliance for<br />
each member of their staff. Managers had been reminded of their<br />
responsibility to drive compliance in their teams and it had been reiterated<br />
that a failure to comply with statutory and mandatory training<br />
requirements constituted a failure of personal objectives.<br />
10
TB 24/13<br />
The Vice Chairman asked how the minimum standard of 95% was set. The<br />
Director of Academic <strong>Health</strong> Sciences explained that this was a standard<br />
identified by the Care Quality Commission and that it reflected an<br />
allowance for the volume of staff turnover in the organisation.<br />
The Director of Human Resources felt that the requirements for statutory<br />
and mandatory training were well defined and it was therefore a cultural<br />
issue of tolerance of non‐compliance that needed to be tackled.<br />
<br />
The Deputy Chief Executive reminded <strong>Board</strong> members that one of the<br />
important principles of the IPF was that the same set of information would<br />
be available at all levels of the organisation. Work was continuing to deliver<br />
this. The Chief Operating Officer supported this approach, giving the<br />
example of VTE screening where the availability of daily data at a local level<br />
had helped to identify recording problems in some areas which were now<br />
being addressed.<br />
The Chairman thanked all those involved in producing the new report and looked<br />
forward to its continued development in the period ahead.<br />
(ii) Clinical quality and safety performance<br />
The Medical Director and Chief Nurse introduced TB 16/13, the Quality and Safety<br />
Report for January 2013, and highlighted the following issues:<br />
<br />
<br />
<br />
<br />
There had been three Care Quality Commission (CQC) inspection visits since<br />
the previous <strong>Trust</strong> <strong>Board</strong> meeting and a meeting with the CQC to discuss<br />
Never Events. Verbal feedback had been received on the inspection visits<br />
and the formal reports were awaited. A visit to Mile End Hospital had<br />
identified some concerns in relation to staffing levels and mealtimes; a<br />
follow‐up visit to the Ainslie Unit had identified some improvement but<br />
more work to be done; and the verbal feedback on a visit to <strong>Barts</strong> which<br />
had focused on cancer services had been positive.<br />
Progress had been made on reducing the number of outstanding legacy<br />
complaints and serious incident reports although this had not been as rapid<br />
as originally planned. The revised target was to reduce these to zero by the<br />
end of March 2013.<br />
A consequence of the focus on closing legacy complaints was that<br />
performance on current complaints had deteriorated.<br />
A discussion of serious incident reporting to the <strong>Board</strong> was scheduled for<br />
the next meeting of the Quality Assurance Committee.<br />
11
TB 24/13<br />
<br />
<br />
The report included benchmarking data on the Standardised Hospital<br />
Mortality Indicator (SHMI) as previously requested by the <strong>Board</strong>. Mortality<br />
data were also increasingly available at specialty level. In response to<br />
reported cases elsewhere in the country, the Medical Director confirmed<br />
that within <strong>Barts</strong> <strong>Health</strong> clinical coding was a matter which was left solely to<br />
the decisions of clinicians and professional coders.<br />
The Deputy Chief Executive felt that it would be helpful to gain a better<br />
understanding of the key drivers of the <strong>Trust</strong>’s low overall mortality rate<br />
and also asked whether mortality data were available for each of the<br />
hospital sites. The Medical Director explained that hospital site data were<br />
not published but to the best of his knowledge none of the legacy trusts had<br />
overall mortality rates in excess of 1.00. In relation to understanding the<br />
reasons for the <strong>Trust</strong>’s low mortality rate, information had been circulated<br />
to CAGs on SHMI by coding group and Dr Foster had been commissioned to<br />
provide the <strong>Trust</strong> with additional information for those groups with a<br />
particularly low SHMI to assist the analysis of the reasons for good<br />
performance. It was agreed that an update on this work should be<br />
provided to the <strong>Trust</strong> <strong>Board</strong> in around three months’ time.<br />
Action: Chief Information Officer and Medical Director<br />
There had been 11 MRSA bacteraemias in the year to date. Despite<br />
exceeding the annual threshold, if this was the end point for <strong>Barts</strong> <strong>Health</strong> in<br />
2012/13 it would represent an improvement of around a third compared<br />
with the 2011/12 position across the legacy trusts. The Medical Director<br />
observed that there had recently been increased medical engagement in<br />
root cause analysis of MRSA and C. difficile cases.<br />
The following points were made in discussion:<br />
<br />
<br />
The Vice Chairman asked about the ambition on pressure ulcers. The Chief<br />
Nurse explained that it was the <strong>Trust</strong>’s aim to eliminate all avoidable<br />
pressure ulcers and that the current trajectory represented a reasonable<br />
step towards this. Some pressure ulcers were unavoidable given the acuity<br />
and dependency of patients being admitted to the <strong>Trust</strong>’s hospitals and the<br />
fact that the community services operated by the <strong>Trust</strong> were often caring<br />
for chronically ill patients and those in the late stages of life.<br />
Ms James asked how the Red rated indicators from the CQC’s Quality and<br />
Risk Profile, as listed on page 17 of the report, were tracked. The Chief<br />
Nurse explained that these were all responses to questions from the<br />
national patient and staff surveys which had been previously reported to<br />
the <strong>Board</strong>. They were therefore part of the survey action plans which were<br />
kept under regular review. The timetable for survey reporting was due to<br />
be discussed at the next Quality Assurance Committee meeting.<br />
The <strong>Trust</strong> <strong>Board</strong> noted the report.<br />
12
TB 24/13<br />
(iii) Financial performance<br />
The Chairman noted that the Finance and Investment Committee was due to meet<br />
in the next week and had therefore not had the usual opportunity to review the<br />
financial position in detail.<br />
The Chief Financial Officer introduced TB 17/13, the finance report for January<br />
2013, and highlighted the following points:<br />
<br />
<br />
<br />
The <strong>Trust</strong> continued to forecast an overall breakeven position for the year<br />
end but the margins within which the <strong>Trust</strong> was currently operating, with a<br />
year to date surplus of just £200,000, meant that it would not be possible to<br />
confirm breakeven until after completion of the annual audit of the<br />
accounts.<br />
There remained a shortfall against the current year’s CIP target which<br />
would add to the following year’s already significant challenge.<br />
PricewaterhouseCoopers LLP had been engaged by the <strong>Trust</strong> to help CAGs<br />
and corporate directorates to identify CIP opportunities for 2013/14 and<br />
beyond. This work included assessing the robustness of CIP plans and<br />
undertaking quality impact assessments. Progress would be reviewed at an<br />
event the following day involving senior clinical leaders and an update<br />
would be provided to the Finance and Investment Committee on 13 March<br />
2013.<br />
The draft capital programme would be presented to the Finance and<br />
Investment Committee in April. From 2013/14, the affordable level of<br />
capital expenditure would be significantly lower than in previous years,<br />
necessitating some difficult decisions on what could and could not be<br />
funded.<br />
The following points were made in discussion:<br />
<br />
<br />
Ms James asked about PricewaterhouseCoopers’ approach to undertaking<br />
benchmarking against other trusts. The Chief Financial Officer explained<br />
that they were adopting a sophisticated approach which took casemix and<br />
volumes at specialty level and compared the specialty to organisations with<br />
a similar casemix and volumes. PwC were also able to access data on the<br />
clinical outcomes delivered by the comparator organisations.<br />
The Chief Operating Officer noted that the meeting with clinical leaders the<br />
following day would spend a significant amount of time reviewing the<br />
benchmarking approach and addressing any concerns in order to gain the<br />
confidence of clinical teams in the benchmarking data.<br />
13
TB 24/13<br />
<br />
<br />
<br />
<br />
<br />
The Chief Executive observed that the initial benchmarking work indicated<br />
that there were significant CIP opportunities. This was positive. However,<br />
it was important not to become overly focused on the detail of the<br />
benchmarking data at the expense of putting efforts into translating the<br />
opportunities into robust and implementable schemes. The challenge of<br />
delivering the scale of CIPs required should not be underestimated,<br />
particularly with new leadership teams.<br />
The Chief Executive also emphasised the importance of combining a focus<br />
on CIP delivery with maintaining a tight control environment. While he<br />
believed that there was an adequate policy framework in place, including<br />
Standing Financial Instructions and a Scheme of Delegation, he was<br />
concerned about compliance. It was essential that managers ensured that<br />
individuals were clear about and complied with their responsibilities within<br />
the control framework.<br />
Ms Whitaker sought confirmation that the year to date financial position<br />
showed an adverse variance of £6.6 million to the original budget. The<br />
Chief Financial Officer confirmed that this was the case. When the original<br />
budget was set, it had been planned to have a cumulative surplus of £6.7<br />
million at Month 10 but the actual figure was now just £0.2 million.<br />
The Vice Chairman questioned whether it was realistic to expect CAGs to<br />
have robust and deliverable CIP plans in place within the next six weeks,<br />
particularly given the current reorganisation of the CAGs. The Chief<br />
Financial Officer noted that the focus of the external support would now<br />
shift from data gathering and analysis to working with CAG teams to<br />
develop detailed plans. He also reminded <strong>Board</strong> members that corporate<br />
directorates needed to lead by example and had to deliver savings as large<br />
as those for the CAGs.<br />
The Vice Chairman asked for further details as to how the proposed CIP<br />
schemes would be reviewed to provide assurance that they would not<br />
adversely impact on the quality and safety of patient care. The Chief<br />
Financial Officer explained that, following CAG review, an independent<br />
panel would review each scheme on behalf of the Medical Director and<br />
Chief Nurse as part of a seven stage process in signing off a scheme as being<br />
Green rated for implementation. The Chief Nurse added that it was also<br />
essential to ensure that there was a robust approach to ongoing monitoring<br />
of the impact on quality and safety of schemes as they were implemented.<br />
The Safety Net tool would provide one element of this although for some<br />
schemes there may be other specific metrics which were identified for<br />
monitoring. Further details of the approach to assessing the quality and<br />
safety impact of CIP schemes would be provided to the Quality Assurance<br />
Committee at its meeting on 13 March 2013.<br />
14
TB 24/13<br />
<br />
The Vice Chairman asked to what extent CAGs had been able to focus on<br />
starting to identify savings opportunities for years 2 and 3. The Chief<br />
Financial Officer said that the current focus was on identifying CIPs for<br />
2013/14 but CAGs would also be asked within the next month to outline<br />
year 2 and 3 opportunities.<br />
The <strong>Trust</strong> <strong>Board</strong> noted the report and agreed that any further points would be<br />
covered at the Finance and Investment Committee meeting the following week.<br />
29/13 FRANCIS INQUIRY<br />
The Chief Nurse introduced TB 18/13, a paper outlining the <strong>Trust</strong>’s initial response<br />
to the report of the Mid Staffordshire <strong>NHS</strong> Foundation <strong>Trust</strong> Public Inquiry, and<br />
highlighted the following points:<br />
<br />
<br />
<br />
<br />
This was likely to be one of the most important reports that any <strong>Board</strong><br />
member would read in their career in the <strong>NHS</strong> and there should be a clear<br />
expectation that the <strong>Board</strong> would return to the key themes and findings of<br />
the public inquiry on a regular basis.<br />
The learning from the failings in care at Mid Staffordshire had begun with<br />
the publication of the first Francis inquiry report in February 2010 and the<br />
<strong>Board</strong> had recently reviewed the actions taken in response, covering the<br />
domains of standards, compliance, culture and compassion.<br />
The key challenge going forward would be to embed the learning<br />
throughout the organisation, from <strong>Board</strong> to ward. While the Executive<br />
Team would be undertaking a review of the individual recommendations<br />
from the public inquiry, the consensus of detailed discussions at the <strong>Trust</strong><br />
Executive and the <strong>Trust</strong> Management <strong>Board</strong> was that the <strong>Trust</strong>’s response<br />
to Francis should focus on the key learning for the organisation rather than<br />
the development of multiple action plans.<br />
The paper outlined a set of proposals developed by the <strong>Trust</strong> Executive and<br />
the <strong>Trust</strong> Management <strong>Board</strong> including holding ‘Learning from Francis’<br />
conversations across the organisation; supporting every team to identify<br />
the top three things they are going to do differently in the light of the<br />
report; reporting back on progress against these commitments; reinforcing<br />
the key messages of Francis through First Fridays, Clinical Fridays and <strong>Board</strong><br />
visits; allocating <strong>Board</strong> Seminar and <strong>Board</strong> Development Programme time<br />
to reflecting on the specific learning for the <strong>Trust</strong> <strong>Board</strong>; strengthening and<br />
triangulating feedback from <strong>Board</strong> ward and department visits and<br />
spending dedicated <strong>Board</strong> time reviewing and discussing visits; and<br />
continuing to embed the <strong>Trust</strong>’s values and behaviours.<br />
The following points were made in discussion:<br />
15
TB 24/13<br />
<br />
<br />
<br />
<br />
The Chairman emphasised the need to maintain the learning from the<br />
Francis report at the top of the <strong>Board</strong> agenda, not least through <strong>Board</strong><br />
members constantly seeking out opportunities to talk directly to patients,<br />
relatives and staff about their experiences and concerns. In doing so, the<br />
Medical Director encouraged the use of simple techniques such as asking<br />
open rather than closed questions.<br />
The Chief Financial Officer felt that the paper provided a very good<br />
summary of the report and fully supported the proposed actions. Thinking<br />
back to the patient story at the beginning of the <strong>Board</strong> meeting, he asked<br />
what changes would be required to ensure that such a story was not<br />
repeated in future. The Chief Nurse felt that the single greatest focus<br />
should be on building teams which felt empowered to address concerns or<br />
problems on the spot and to escalate rapidly if necessary to secure<br />
appropriate resolution. The Medical Director agreed, adding that it would<br />
also be important to hold people to account for failing to raise concerns.<br />
The Chief Executive suggested that the <strong>Board</strong> needed to develop a clear and<br />
consistent message about the key priorities for every member of staff in the<br />
organisation, focused on standards, values, accountability, engagement and<br />
visibility. These should be constantly emphasised by <strong>Board</strong> members and<br />
leaders in the organisation.<br />
Ms Whitaker supported the approach outlined in the paper and suggested<br />
that sharing and celebrating examples of people demonstrating effective<br />
behaviours could be very powerful.<br />
The <strong>Trust</strong> <strong>Board</strong> approved the approach and specific proposals set out in the paper<br />
and agreed that it should review progress against the agreed actions on a regular<br />
basis at both the <strong>Trust</strong> <strong>Board</strong> and the Quality Assurance Committee.<br />
30/13 STAFF SURVEY 2012<br />
The Director of Human Resources introduced TB 19/13, a report on the results of<br />
the 2012 staff survey, and noted the following points:<br />
<br />
<br />
Both the patient story and the paper on the Francis report provided<br />
important and helpful context to discussion of the staff survey results.<br />
The 2012 staff survey was the first to be conducted for <strong>Barts</strong> <strong>Health</strong> and<br />
would therefore act as a baseline for measuring future progress. The <strong>Board</strong><br />
was grateful to the 5,000 members of staff who had taken the time to<br />
complete the survey.<br />
16
TB 24/13<br />
<br />
<br />
<br />
<br />
The overall picture was one of being close to the national average, although<br />
there were a few questions where the <strong>Trust</strong> was a relatively high performer<br />
and a number where the <strong>Trust</strong> was among the lowest performers.<br />
Corporate directorates, with the exception of Corporate Affairs and Nursing<br />
and Governance, had generally poor results. While this might partly reflect<br />
the fact that corporate functions were being restructured at the time of the<br />
survey, it indicated that there was significant work to be undertaken to<br />
build capability and confidence in corporate areas.<br />
The paper sought to map the staff survey results to the four key levers or<br />
enablers of staff engagement which the <strong>Board</strong> had previously discussed. A<br />
potential fifth enabler was team working or ‘teamship’.<br />
The final section of the paper outlined the proposed priority areas for<br />
action. A number of these were already being progressed, such as the <strong>Barts</strong><br />
<strong>Health</strong> Improvement System which was due to be discussed by the <strong>Board</strong> in<br />
April, leadership development work and the development of a new<br />
performance appraisal system. However, there were other areas where<br />
further consideration was needed on how to address the findings of the<br />
survey, for example in relation to workplace stress and bullying, harassment<br />
and discrimination. Of particular concern were the results that showed that<br />
BME staff in the <strong>Trust</strong> were more motivated than other staff groups but felt<br />
less able to progress.<br />
The following points were made in discussion:<br />
<br />
<br />
Ms James asked the Director of Human Resources whether he was<br />
confident that the monthly Pulse surveys would generate a good response<br />
rate. The Director of Human Resources said that he believed that they<br />
would. The first Pulse survey had run for a week and generated 400<br />
responses from a sample of 2,000 members of staff. However, he was<br />
concerned that these surveys were being conducted by email and may<br />
therefore not be effective in reaching certain groups of staff. This would be<br />
given further consideration.<br />
The Chief Executive said that he had found paragraphs 16‐18 of the paper<br />
very powerful in relation to how to maintain the motivation of the already<br />
engaged group of staff. He suggested that consideration should be given to<br />
more frequent opportunities to reward staff and celebrate success,<br />
including at local level. Equally, it was important to have early and frank<br />
conversations with staff who did not want to be engaged.<br />
The <strong>Trust</strong> <strong>Board</strong> noted the survey results, supported the planned actions described<br />
in the paper and invited the Director of Human Resources to propose a process for<br />
regular feedback, including through the Integrated Performance Report.<br />
Action: Director of Human Resources<br />
17
TB 24/13<br />
31/13 MIXED SEX ACCOMMODATION<br />
The Chief Nurse introduced TB 20/13, a paper on mixed sex accommodation<br />
compliance to inform the required annual declaration of compliance.<br />
It had been a difficult assessment to make given the challenges which had been<br />
discussed earlier in the meeting in relation to meeting the critical care step down<br />
requirements of the mixed sex accommodation standards. However, taking the<br />
year as a whole and the fact that all hospital sites were compliant outside critical<br />
care, it was proposed that the <strong>Trust</strong> should declare overall compliance as at 1 April<br />
2013. It was understood that such an approach would be consistent with that of<br />
other London trusts which were also struggling on the critical care step down<br />
element.<br />
The <strong>Trust</strong> <strong>Board</strong> approved making the declaration of compliance as at 1 April 2013<br />
as set out at Appendix 1 of the paper, subject to inclusion of a specific reference to<br />
the challenge in critical care in meeting the step down requirements.<br />
Action: Chief Nurse<br />
32/13 BOARD ASSURANCE FRAMEWORK<br />
The Director of Corporate Affairs and <strong>Trust</strong> Secretary introduced TB 21/13, a paper<br />
describing the approach taken to the development of the <strong>Board</strong> Assurance<br />
Framework (BAF) for <strong>Barts</strong> <strong>Health</strong> and seeking the views of <strong>Board</strong> members on the<br />
proposed risks for inclusion on the BAF.<br />
He explained that the development of the BAF had awaited the completion of the<br />
initial exercise to merge and cleanse the <strong>Trust</strong> risk register. This had enabled a<br />
‘bottom up’ approach to be adopted to derive BAF risks based on the high risks on<br />
the <strong>Trust</strong> risk register as grouped by strategic objective. The outputs had then<br />
been tested in discussions with Executive Directors to introduce a ‘top down’<br />
element. The paper included a proposed shortlist of BAF entries together with<br />
potential longlist entries. The paper also included two examples of worked up BAF<br />
entries.<br />
The following points were made in discussion:<br />
<br />
<br />
The Director of Human Resources questioned whether sufficiency of<br />
staffing should be included as a separate entry on the BAF. The Chief<br />
Executive felt that this was an issue to be managed rather than a risk for the<br />
BAF.<br />
The Deputy Chief Executive noted that the BAF was in many ways as good<br />
as the <strong>Trust</strong> risk register and there was a strong focus on improving the<br />
quality of risk identification and recording via the work of the Risk<br />
Management Committee.<br />
18
TB 24/13<br />
The <strong>Trust</strong> <strong>Board</strong>:<br />
<br />
<br />
Noted the update and approved the approach to the development of the<br />
<strong>Board</strong> Assurance Framework.<br />
Agreed to provide comments on the proposed risk entries to the Director of<br />
Corporate Affairs ahead of the next <strong>Trust</strong> <strong>Board</strong> meeting where a full<br />
version of the BAF would be presented for approval.<br />
Action: All <strong>Board</strong> members<br />
33/13 USE OF THE SEAL<br />
The Director of Corporate Affairs and <strong>Trust</strong> Secretary introduced TB 22/13, a paper<br />
seeking <strong>Trust</strong> <strong>Board</strong> ratification of the use of the Seal on the occasions listed.<br />
The <strong>Trust</strong> <strong>Board</strong> ratified the use of the Seal.<br />
34/13 ORAL REPORTS FROM BOARD COMMITTEES<br />
(i) Audit and Risk Committee<br />
The Vice Chairman reported that the Audit and Risk Committee had met on 20<br />
February 2013. The Committee had discussed salary overpayments,<br />
implementation of the Whistleblowing policy, confirmation that the <strong>Trust</strong> had not<br />
made inappropriate use of confidentiality agreements, the <strong>Board</strong> Assurance<br />
Framework and a number of internal and external audit reports.<br />
(ii) Public <strong>Health</strong> and Equalities Committee<br />
Ms Whitaker reported that the Public <strong>Health</strong> and Equalities Committee had met on<br />
20 February 2013. The Committee had welcomed the <strong>Trust</strong>’s new Director of<br />
Public <strong>Health</strong> and had discussed the north east London convergence programme,<br />
ways of strengthening liaison with the GLA, local authorities and <strong>Health</strong> and<br />
Wellbeing <strong>Board</strong>s, the public health vision, local employment initiatives and ways<br />
of promoting healthy living to staff.<br />
35/13 SINGLE OPERATING MODEL<br />
The <strong>Trust</strong> <strong>Board</strong> reviewed and retrospectively approved the February 2013 Single<br />
Operating Model (SOM) self‐certification return reporting December 2012 data.<br />
36/13 ANY OTHER BUSINESS<br />
There was no other business.<br />
19
TB 24/13<br />
37/13 QUESTIONS FROM MEMBERS OF THE PUBLIC<br />
Questions and comments were received from members of the public and the<br />
questions were duly answered by members of the <strong>Trust</strong> <strong>Board</strong> as follows:<br />
<br />
Concern was expressed that patients and patient groups were not being<br />
adequately consulted by London Cancer on the emerging proposals for<br />
specialist cancer provision in north east and north central London. The<br />
recommendations on urological cancer appeared to involve a diminution of<br />
choice and accessibility and a number of patient groups would be pressing<br />
for a full statutory consultation. It had also been suggested that the <strong>Trust</strong><br />
had been pre‐occupied by the merger and had taken its eye off the ball on<br />
specialist cancer services.<br />
The Chief Executive explained that the decision on whether there would be<br />
formal consultation would be one for specialist commissioners in London.<br />
The London Cancer tumour groups charged with making proposals were<br />
clinically led and their proposals would be reviewed by an independent<br />
body which would present recommendations to commissioners.<br />
<br />
It appeared that a large part of the cancer services at <strong>Barts</strong> were being<br />
given away to competitors. This raised questions as to how the <strong>Trust</strong> would<br />
manage the resulting loss of income, what the impact would be on patient<br />
access, how it would be possible to maintain a seamless care pathway for<br />
cancer patients and what cancer services would ultimately remain on the<br />
<strong>Barts</strong> site.<br />
The Chief Executive noted that the Integrated Cancer System (ICS)<br />
proposals were not expected to impact on the location of the vast majority<br />
of cancer services at <strong>Barts</strong> and there was therefore a clear expectation that<br />
the investment in the <strong>Barts</strong> Cancer Centre would continue to derive strong<br />
value and <strong>Barts</strong> would continue to have a key role to play in providing<br />
cancer care for the ICS population of some 3 million people and the<br />
Academic <strong>Health</strong> Sciences Network population of around 6 million people.<br />
There might be some changes in how income flowed into the system<br />
without a relocation of services. But for any services that did relocate,<br />
there would be a loss of both income and cost and the <strong>Trust</strong> was currently<br />
assessing the potential scale of these for the specialist areas where there<br />
was the potential for relocation. It was also important to recognise that<br />
any changes would take time to implement and there would therefore be<br />
time for provider organisations to manage the impact.<br />
20
TB 24/13<br />
On access, the Chief Executive noted that London Cancer was seeking to<br />
take decisions on the long‐term configuration of services for the benefit of<br />
patients. He believed that The Royal London was well placed<br />
geographically to serve the populations of north east and north central<br />
London and Essex.<br />
In terms of care pathways, the Medical Director explained that the focus<br />
would be on delivering the best possible outcomes for patients by<br />
concentrating the surgical element of the pathway in a smaller number of<br />
centres but providing the rest of the care locally, including working with<br />
GPs on prevention. This had the potential to save a large number of lives.<br />
The Chief Executive added that he saw a clear, long‐term role for the <strong>Barts</strong><br />
site centred around leading edge cardiovascular and cancer services (both<br />
as part of wider systems) and also a strong heritage focus.<br />
<br />
Questions were raised as to why the control weaknesses referred to during<br />
the meeting had not been tackled earlier in the year and whether the <strong>Trust</strong><br />
would be waiting for the outcome of the <strong>NHS</strong> Medical Director’s review of<br />
emergency medicine before redesigning the <strong>Trust</strong>’s own emergency<br />
medicine pathway.<br />
On control issues, the Chief Executive noted that the new clinical<br />
management structure had only been in place for around five months.<br />
Progress was being made on addressing control weaknesses but would take<br />
time as information requirements were addressed.<br />
On service redesign and reconfiguration, the Chief Executive explained that<br />
all such changes would be approached from the perspective of quality of<br />
care. Some changes might be possible in the relatively short term while<br />
others would take longer to deliver. The Medical Director noted that the<br />
review being undertaken by the <strong>NHS</strong> Medical Director was based on the<br />
methodology used for the earlier review of emergency care by the Medical<br />
Director of <strong>NHS</strong> London. Based on the London work, CAGs were reviewing<br />
how they worked together to deliver the best standards of emergency care<br />
in order to achieve the best possible patient outcomes.<br />
38/13 DATE OF NEXT MEETING<br />
The next meeting of the <strong>Trust</strong> <strong>Board</strong> (Part 1) in public would be held on<br />
Wednesday 10 April 2013 at 11.00 in the Main Lecture Theatre, Education Centre,<br />
The London Chest Hospital, Bonner Road, London E2 9JX.<br />
21
TB 24/13<br />
39/13 RESOLUTION<br />
The <strong>Board</strong> resolved that representatives of the press and other members of the<br />
public be excluded from the remainder of this meeting having regard to the<br />
confidential nature of the business to be transacted, publicity on which would be<br />
prejudicial to the public interest (section (2) Public Bodies (Admissions to<br />
Meetings) Act 1960).<br />
Signed ……………........................................<br />
Dated …………………………………<br />
Ian Walker<br />
Director of Corporate Affairs and <strong>Trust</strong> Secretary<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
020 7092 5212<br />
22
TB 24/13<br />
ACTION LOG<br />
<strong>Trust</strong> <strong>Board</strong> meeting (Part 1): 6 March 2013<br />
Page Action Lead Status update<br />
no.<br />
2 Mental health ‐ provide an update on work<br />
with the mental health trust at the next<br />
meeting.<br />
Chief Operating<br />
Officer<br />
Completed – matter<br />
arising on April 2013<br />
<strong>Board</strong> agenda.<br />
6 Patient story – there would be further Chief Nurse<br />
Completed.<br />
discussion at the Quality Assurance<br />
Committee meeting the following week as<br />
part of the item on learning disabilities.<br />
The outcome of this discussion would then<br />
be reported back to the <strong>Board</strong>.<br />
8 Chief Executive’s report ‐ a paper providing<br />
details of the Information Governance<br />
Director of Corporate<br />
Affairs and <strong>Trust</strong><br />
Completed ‐ on April<br />
2013 <strong>Board</strong> agenda.<br />
Toolkit submission would be presented at<br />
the next meeting of the <strong>Trust</strong> <strong>Board</strong>.<br />
Secretary<br />
9 IPF – circulate CCP compliance details<br />
following <strong>Board</strong> meeting.<br />
Deputy Chief<br />
Executive<br />
Completed – circulated<br />
on 11 March 2013.<br />
10 IPF ‐ a separate session would be arranged<br />
with the Chief Information Officer to<br />
increase familiarity with the IPF.<br />
12 SHMI ‐ an update on work to understand<br />
reasons for low SHMIs should be provided<br />
to the <strong>Trust</strong> <strong>Board</strong> in around three months’<br />
time.<br />
17 Staff survey ‐ propose a process for regular<br />
feedback, including through the Integrated<br />
Performance Report.<br />
18 Mixed Sex Accommodation compliance<br />
declaration – include a specific reference to<br />
the challenge in critical care in meeting the<br />
step down requirements.<br />
19 BAF ‐ provide comments on the proposed<br />
risk entries to the Director of Corporate<br />
Affairs ahead of the next <strong>Trust</strong> <strong>Board</strong><br />
meeting<br />
<strong>Trust</strong> <strong>Board</strong> meeting (Part 1): 6 February 2013<br />
23<br />
Director of Corporate<br />
Affairs<br />
Medical Director and<br />
Chief Information<br />
Officer<br />
Director of Human<br />
Resources<br />
Chief Nurse<br />
Completed – arranged<br />
for <strong>Board</strong> Seminar on<br />
10 April 2013.<br />
Scheduled for July<br />
2013 <strong>Trust</strong> <strong>Board</strong><br />
meeting.<br />
Process to be<br />
confirmed.<br />
Completed and<br />
published.<br />
All <strong>Board</strong> members Completed –<br />
comments received<br />
incorporated into BAF<br />
on April 2013 <strong>Board</strong><br />
agenda.<br />
Page Action Lead Status update<br />
no.<br />
4 Patient story ‐ prepare a briefing on the<br />
current arrangements and future plans for<br />
volunteering to be brought back to the<br />
<strong>Board</strong> in three months’ time. Also look at<br />
how staff are encouraged to volunteer<br />
outside the <strong>Trust</strong> in the local community.<br />
Chief Nurse<br />
Scheduled for May<br />
2013 <strong>Board</strong> meeting.
TB 24/13<br />
9 Quality and safety – consider reporting on<br />
complaints per 1,000 beds.<br />
10 Quality and Safety – Quality Assurance<br />
Committee to review ‘Red’ rated survey<br />
indicators from the latest CQC Quality and<br />
Risk Profile.<br />
10 Quality and Safety – provide an update to<br />
the Quality Assurance Committee on the<br />
timetable for reporting on surveys.<br />
13 Royal College of Surgeons – confirm by<br />
when it will be possible to report on<br />
emergency surgery waiting times across the<br />
whole <strong>Trust</strong>.<br />
16 Safeguarding – issue a reminder to all staff<br />
on security arrangements and challenging<br />
visitors to wards and clinical areas.<br />
Chief Nurse<br />
To report back at next<br />
<strong>Board</strong> meeting.<br />
Chief Nurse Completed ‐<br />
considered at March<br />
2013 QAC meeting.<br />
Chief Nurse Completed ‐<br />
considered at March<br />
2013 QAC meeting.<br />
Medical Director Outstanding.<br />
Chief Nurse and Chief<br />
Operating Officer<br />
Completed.<br />
<strong>Trust</strong> <strong>Board</strong> meeting (Part 1): 28 November 2012<br />
Page Action Lead Status update<br />
no.<br />
5 Patient story – draw up an action plan to<br />
address both systemic and behavioural<br />
Chief Operating<br />
Officer and Chief<br />
Scheduled for May<br />
2013 QAC meeting.<br />
issues. Patient to review action plan and<br />
progress to be reviewed by the Quality<br />
Assurance Committee in three to four<br />
months’ time.<br />
Nurse<br />
7 King George Ilford renal satellite unit ‐<br />
provide a report in due course on the<br />
operation of the new unit.<br />
Chief Operating<br />
Officer<br />
Scheduled for summer<br />
2013.<br />
16 Patient food ‐ taste patient food at a future<br />
<strong>Board</strong> meeting.<br />
<strong>Trust</strong> <strong>Board</strong> meeting (Part 1): 31 October 2012<br />
Chief Operating<br />
Officer<br />
Completed – patient<br />
food being served at<br />
April 2013 meeting.<br />
Page Action Lead Status update<br />
no.<br />
7 Chairman’s report – identify ways of sharing<br />
positive news and developments.<br />
Chief Nurse and<br />
Director of<br />
Currently under<br />
review.<br />
Communications and<br />
Engagement<br />
8 Circulate GMC report to <strong>Board</strong> members<br />
when available.<br />
Director of Academic<br />
<strong>Health</strong> Sciences<br />
Awaiting final report.<br />
24
TB 24/13<br />
<strong>Trust</strong> <strong>Board</strong> meeting (Part 1): 26 September 2012<br />
Page Action Lead Status update<br />
no.<br />
6 Governance arrangements with Director of Corporate Will maintain on the<br />
commissioners ‐ this should be included<br />
explicitly on the action log.<br />
Affairs<br />
action log until<br />
resolved.<br />
<strong>Trust</strong> <strong>Board</strong> meeting (Part 1): 25 July 2012<br />
Page Action Lead Status update<br />
no.<br />
3 Patient story ‐ the Chairman proposed that<br />
the <strong>Board</strong> should discuss the <strong>Trust</strong>’s<br />
Chief Operating<br />
Officer and Chief<br />
Completed – feedback<br />
from COO at April 2013<br />
relationship with local mental health Nurse<br />
<strong>Board</strong> meeting.<br />
services during the autumn.<br />
8 Chief Executive’s Report – raise issue of<br />
Charity name with the <strong>Barts</strong> and The<br />
London Charity.<br />
Chairman<br />
Completed – outcome<br />
reported in April 2013<br />
Chief Executive’s<br />
report.<br />
<strong>Trust</strong> <strong>Board</strong> meeting (Part 1): 30 May 2012<br />
Page Action Lead Status update<br />
no.<br />
8 Serious Incidents – consider inviting Chief<br />
Executive of Salford Royal <strong>NHS</strong> Foundation<br />
<strong>Trust</strong> to speak to the <strong>Board</strong> about patient<br />
Chairman In progress –<br />
discussing dates for a<br />
wider <strong>Trust</strong> event.<br />
safety culture.<br />
15 <strong>Trust</strong> objectives – present advice to the<br />
<strong>Board</strong> on a <strong>Trust</strong> improvement system.<br />
<strong>Trust</strong> <strong>Board</strong> meeting (Part 1): 25 April 2012<br />
Chief Executive and<br />
Deputy Chief<br />
Executive<br />
Completed – on April<br />
2013 <strong>Board</strong> Seminar<br />
agenda.<br />
Page Action Lead Status update<br />
no.<br />
15 New Hospitals Programme ‐ the New Deputy Chief Completed.<br />
Hospitals benefits realisation programme<br />
was being refreshed and would be brought<br />
to the <strong>Trust</strong> <strong>Board</strong> in the next two months.<br />
Executive and<br />
Development Director<br />
15 New Hospitals Programme ‐ produce a<br />
consolidated estates report covering all of<br />
<strong>Barts</strong> <strong>Health</strong> from the third quarter of the<br />
year.<br />
Director of Strategy<br />
and Chief Operating<br />
Officer<br />
Now scheduled for<br />
2013/14 Q1.<br />
25
Report to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013 TB 25/13<br />
Title<br />
Sponsoring Director<br />
Author(s)<br />
Purpose<br />
Previously considered by<br />
Chief Executive’s Report<br />
Chief Executive<br />
As above<br />
To report on key issues and developments<br />
Not applicable<br />
Executive summary<br />
The report sets out current key issues for the <strong>Trust</strong> <strong>Board</strong> to note and discuss.<br />
Related <strong>Trust</strong> objectives<br />
All objectives<br />
Sub‐objectives<br />
Risk and Assurance<br />
Related Assurance<br />
Framework entries<br />
Legal implications/<br />
regulatory requirements<br />
n/a<br />
n/a<br />
None identified.<br />
Action required by the <strong>Board</strong><br />
The <strong>Trust</strong> <strong>Board</strong> is asked to note and discuss the issues raised in the report.<br />
1
TB 25/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING: 10 APRIL 2013<br />
CHIEF EXECUTIVE’S REPORT<br />
1. Francis Report<br />
Conversations are continuing across the organisation about how we respond to the<br />
findings and recommendations of the Francis report, with a particular focus on<br />
values, culture and leadership. Since we last met, the Government has published its<br />
initial response to the report. A copy has been circulated to <strong>Board</strong> members.<br />
2. Operational performance<br />
The main areas of concern remain emergency care performance (at The Royal<br />
London and Whipps Cross), mixed sex accommodation breaches at The Royal London<br />
and 62 day cancer pathways (focusing on uro‐ and gynae‐oncology) and VTE<br />
assessment (as the target moves to 95% from 1 April) across most of our sites. We<br />
are on track to deliver the RTT position from Q1 and have maintained the<br />
improvement in MRSA. Whipps Cross recently passed the one year mark with zero<br />
MRSA bacteraemias.<br />
On financial performance, there was a small surplus at the end of Month 11<br />
compared to a target surplus of £5.7 million. We continue to forecast breakeven for<br />
2012/13.<br />
Looking forward, from a forecast £50 million CIP delivery at year end (an undershoot<br />
of £14 million on the 2012/13 target) we face a requirement to increase CIP delivery<br />
by around 50% for 2013/14. We must also further strengthen financial information<br />
and controls in the relatively new CAG management structures.<br />
3. Property Transfers<br />
As part of the <strong>NHS</strong> reforms, a number of properties have been transferred to the<br />
<strong>Trust</strong> from 1 April 2013. These include the majority of the Mile End Hospital site and<br />
a small number of GP surgeries ‐ Steels Lane, Spitalfields <strong>Health</strong> Centre, St Peter’s<br />
Street and Leopold Street.<br />
4. Sir Ludwig Guttmann <strong>Health</strong> and Wellbeing Centre<br />
Following our success in the pre‐qualifying stage, we have submitted our bid to<br />
provide primary care services from the health and wellbeing centre on the Olympic<br />
park site. The shortlisted bidders will be announced in mid April and the final<br />
selection will be made in early May.<br />
2
TB 25/13<br />
5. Newham Urgent Care Centre (UCC)<br />
The Newham UCC, located next to the Newham A&E department, is operated by East<br />
London <strong>NHS</strong> Foundation <strong>Trust</strong>. Commissioners are retendering the service which will<br />
stream patients to appropriate services and reduce pressure on the A&E department.<br />
With the <strong>Board</strong>’s support, we will bid to run this service in partnership with a primary<br />
care team in Newham. The bid will be submitted by 7 June, the preferred bidder will<br />
be selected by 11 July and the service is due to begin operating from 13 November.<br />
6. Baby Friendly accreditation<br />
A partnership between The Royal London Hospital, Tower Hamlets public health and<br />
Tower Hamlets council has become the first in London to be awarded the prestigious<br />
Baby Friendly Initiative accreditation from UNICEF (United Nations Children's Fund)<br />
for implementing recommended standards to promote and sustain breastfeeding in<br />
both hospital and community settings.<br />
7. Royal London Renal team<br />
The Renal Supportive and Palliative Care Team at The Royal London and St Joseph’s<br />
Hospice in Hackney have won an award from The International Journal of Palliative<br />
Nursing and Macmillan Cancer Support for caring for end‐of‐life kidney patients. The<br />
award recognises their work on Symptom Control Guidelines.<br />
8. Maternity services at King George Hospital<br />
The <strong>NHS</strong> North East London and the City <strong>Board</strong> decided last month to move forward<br />
with the planned transfer of maternity birthing services from King George Hospital,<br />
Ilford. <strong>Barts</strong> <strong>Health</strong> has worked closely with commissioners and colleagues at<br />
Barking, Havering and Redbridge University Hospitals <strong>NHS</strong> <strong>Trust</strong> and Homerton<br />
University Hospital <strong>NHS</strong> Foundation <strong>Trust</strong> over the past year to enable the transfer of<br />
antenatal, birth and post natal services for around 1,700 women. For <strong>Barts</strong> <strong>Health</strong>,<br />
this has included increasing capacity at Newham, including opening the Barking<br />
Birthing Centre.<br />
9. National Clinical Director appointments<br />
I am delighted to report that Director of Academic <strong>Health</strong> Sciences, Professor Jo Martin,<br />
has been appointed as the new National Clinical Director of Pathology Services at the<br />
Department of <strong>Health</strong> from April 2013, and Consultant Gastroenterologist and<br />
Hepatologist, Dr Michael Glynn, has been appointed as the new National Clinical Director<br />
for Gastrointestinal and Liver Diseases.<br />
3
TB 25/13<br />
10. <strong>Barts</strong> Charity<br />
The <strong>Barts</strong> and The London Charity has decided to adopt ‘<strong>Barts</strong> Charity’ as its name.<br />
As <strong>Board</strong> members are aware, we are in the process of transferring the Newham and<br />
Whipps Cross charitable funds from the corporate trusteeship of <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong><br />
<strong>Trust</strong> to <strong>Barts</strong> Charity. The target date for the transfer is 1 May.<br />
11. Joint application for British Heart Foundation (BHF) Centre of Excellence<br />
Unfortunately the joint application (<strong>Barts</strong> <strong>Health</strong>/QMUL/UCLH/UCL) for BHF Centre of<br />
Excellence funding was not successful this time, but related grant applications have<br />
been requested in recognition of the potential for major steps forward in<br />
cardiovascular research in the partnership, and this will help pump prime further<br />
research funding and development.<br />
Peter Morris<br />
Chief Executive<br />
April 2013<br />
4
Report to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013<br />
TB 26/13<br />
Title<br />
Sponsoring Director<br />
Author(s)<br />
Purpose<br />
Previously considered by<br />
Integrated Performance Framework (IPF) –<br />
Februaryy 2013<br />
Chief Information Officer<br />
Chief Information Officer and<br />
Deputy Director of Informationn<br />
To summarise the organisation’s in‐month and year to<br />
date performance to<br />
the end of February 2013.<br />
<strong>Trust</strong> Management<br />
<strong>Board</strong>, 9 April 2013<br />
Executive summary<br />
<br />
<br />
<br />
The performance<br />
report is shown in its new format. A parallel report on<br />
Quality and Safety<br />
is also presented.<br />
Regulatory performance remains of concern. The deterioration since s<br />
October 2012 was noted last month. There is a clear plan to grip each off the<br />
indicators and drive improvement.<br />
VTE performance has recovered to meet<br />
the requirement in February.<br />
<br />
A training session<br />
has been set for<br />
understand this report.<br />
members<br />
of the <strong>Board</strong> to further<br />
<br />
Work on the Partners’ View within the report is progressing.<br />
Related <strong>Trust</strong> objectives<br />
All <strong>Trust</strong> objectives.<br />
Legal implications/<br />
regulatory requirements<br />
None<br />
Action required by the <strong>Board</strong><br />
The<br />
<strong>Trust</strong> <strong>Board</strong> is asked to: t<br />
Note performancee for February 2013.<br />
Comment on format, inclusions and exclusions to t support<br />
development of this report.<br />
the continued
TB 26/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING: 10 APRIL 2013<br />
INTEGRATED PERFORMANCE FRAMEWORK<br />
CONTEXT<br />
1. In April 2012 the new organisation’s <strong>Board</strong> committed itself to a series of<br />
principles about performance management. These were evidently intended<br />
to enshrine a different culture within <strong>Barts</strong> <strong>Health</strong>. In particular, we sought<br />
to confirm that information about performance would travel transparently<br />
from ward to boardroom, and that what was meant by performance in the<br />
organisation would include in equal measure safety and quality, workforce,<br />
finance, operational minimum standards, education, research and<br />
development.<br />
2. In December 2012, the <strong>Board</strong>’s Quality Assurance Committee accepted the<br />
recommendation that the Integrated Performance Framework should replace<br />
other forms of data routinely presented to the <strong>Board</strong>. We agreed that our<br />
focus would be in eight areas:<br />
KEY performance<br />
indicators………………<br />
What do our patients think of us?<br />
What do our staff and students think<br />
of us?<br />
What do our regulators think of us?<br />
What do our partners think of us?<br />
Performance indicators<br />
about…………….<br />
Quality, safety and innovation<br />
Workforce information<br />
Efficiency and productivity<br />
Research, education and<br />
communication<br />
3. The task of constructing this approach was never underestimated and a<br />
substantial amount of work remains to be done to complete the promise.<br />
The substantial work is in five key elements:<br />
i. Ensuring that the data is available not less frequently than monthly,<br />
and in some cases weekly, for use by frontline leaders and with<br />
availability to the Executive and the <strong>Board</strong>. Wherever feasible, this<br />
dataflow would be automated.<br />
ii. Ensuring that the data quality of the information is understood, and<br />
is, in time, uniformly of high standard. This task is complicated by the<br />
still merging nature of some indicators’ supporting data systems.<br />
2
TB 26/13<br />
iii. Agreeing what success would be for an indicator, especially in those<br />
areas where no national measure is prescribed. The threshold needs<br />
to be agreed there not later than the end of March for the 2013/14<br />
annual plan, which will be supported by this IPF for measurement.<br />
iv. Creating a rhythm of performance assurance by CAG, by service<br />
group, by ward or department across our new organisation. A system<br />
by CAG has been in place for some months. Looking into 2013/14 it is<br />
important we set a trajectory by which this can deepen, and of course<br />
can be matched by the performance assessment of each corporate<br />
function. Performance management based on managing the opinions<br />
of others – our KPIs – is a new and perhaps different skill to be<br />
mastered.<br />
v. While maintaining data availability and individuals’ capability to query<br />
data sources themselves, beginning the process of ruthlessly retiring<br />
other reports which show information herein either in a different<br />
format or at a different time period.<br />
REPORT<br />
4. The report provides data in a broadly standard format across six of the eight<br />
areas. The exception is the partnering domain where there is a need now to<br />
grip how we plan to track reputation. Where the format is non‐standard it is<br />
because the data is not yet available with the regularity needed to make a<br />
graph over time useful.<br />
5. The data provided takes members to the most recent information – from<br />
February 2013 (month 11). How far back the data displayed goes relates to<br />
availability and a measured view of past data quality. However, it does not<br />
indicate that a full data quality review of the current data has been<br />
completed.<br />
6. The RAG system is deliberately rudimentary. Above the line performance is<br />
green. Below the line performance is red. A future iteration can consider<br />
what portion of green performance should be considered fragile and amber.<br />
Perhaps brutally, where a composite judgement is needed across areas or<br />
indicators, the lowest performing judgment governs the colour shown.<br />
7. The report includes some description of the data. This is provided by the<br />
relevant Executive lead. We need to discuss further (i) how that is assured<br />
across all domains and (ii) how other qualitative information and opinion is<br />
not lost from our reporting. In particular this is a valued part of the Quality<br />
and Safety report.<br />
3
TB 26/13<br />
WHAT DOES THE REPORT TELL US?<br />
8. We have far further to go in systematically collating feedback monthly from<br />
staff, students, patients and partners. Nonetheless we are now able to do<br />
that for staff (through our new monthly pulse survey) and for patients (not<br />
only through RTF but now through the Friends and Family test).<br />
9. We need to set some stretching goals in the workforce, efficiency and quality<br />
performance indicators, which give us all a clear indication of what we are<br />
striving to achieve. Without those expectations, our performance<br />
conversation will focus on whether a data point has gone up or down.<br />
10. While our annual staff survey provided some positive indications of<br />
performance, and whilst we are not an outlier for patient opinion, we need<br />
to actively seek to manage the underlying valence issues if we are to see<br />
these two Key performance indicators move towards green. There is a real<br />
opportunity here for teams to learn from each other: CAG to CAG, service to<br />
service, ward to ward.<br />
11. Our Regulatory performance in February has not yet recovered from the<br />
deterioration reported in quarter 3. After two quarters of Department of<br />
<strong>Health</strong> indicator compliance, we are now in the performance under review<br />
category. Likewise our SOM is not green. We have indicators – cancer waits<br />
and MRSA – which have not been compliant for three successive quarters.<br />
We are, however compliant, with our Cooperation and Competition Panel<br />
(CCP) obligations. VTE has shown recovery in February 2013.<br />
12. A key question for the <strong>Trust</strong> <strong>Board</strong> to consider is the need for any preceding<br />
dialogue in addition to that contained within the report itself.<br />
Luke Readman<br />
Chief Information Officer 5 April 2013<br />
4
BARTS HEALTH <strong>NHS</strong> TRUST<br />
February 2013 Integrated Performance Report<br />
Luke Readman<br />
Chief Information Officer<br />
26 th March 2013
BARTS HEALTH INTEGRATED PERFORMANCE<br />
HOW ARE WE DOING?<br />
2
What do staff & students think?<br />
Workforce<br />
Overall; Permanent staffing is at 89.5%, down from 89.8% in Month 10. In some cases,<br />
vacancies are being held in order to secure a return to budgeted pay spend this. Focus on our<br />
time to hire has led to a median rate of 12.8 weeks at 22 nd March from 17 weeks at end<br />
January. A workforce planning process has been agreed and completed first for ACCU. This<br />
includes advanced recruitment authorisation in high volume areas.<br />
Bank & Agency; Of concern, 26% of filled temporary staffing being via agencies. ECAM<br />
remains the highest spender in temporary staffing, accounting for 17.44% of its pay budget in<br />
month (15.95% YTD). Driven by unfunded beds, reductions will be seen as these beds are<br />
closed. High spend within Surgery also remains and, Trauma and Orthopaedics; driven by<br />
additional clinics inpatient list at RLH.<br />
Turnover; Turnover is stable at 10.8%. Attributed to limited opportunities for career<br />
progression. Turnover of staff appointed within the last 12 months is high in Cardiovascular<br />
at 35.1% and Surgery at 24.9%. Cardiovascular is introducing a 6 month retention survey to<br />
better understand how new staff have settled into their roles. In Surgery within ITU at the<br />
RLH are high levels of vacancies &opportunities for promotion elsewhere and a lack of<br />
support and development.<br />
Sickness Absence; Highest are Women’s <strong>Health</strong> and Ambulatory. Across both, efforts are<br />
being prioritised for management action via the new process. Occupational <strong>Health</strong> capacity<br />
to support this is being increased.<br />
What do our partners think?<br />
Communication, R&D and Education<br />
Work is underway with the Director of Communications to define an approach to<br />
obtaining regular feedback from partners. A number of options are being explored.<br />
Research and development metrics are presented showing overall good<br />
performance, although expenditure and income recovered are down.<br />
Executive Summary – Feb<br />
What do our patients think?<br />
Quality, Safety and Innovation<br />
SHMI is unchanged at 0.84 which is a lower than expected for the <strong>Trust</strong>.<br />
There were 33 SIs raised in the month<br />
There was 1 case of MRSA bacteraemia for a patient at Newham (NUH<br />
There were 8 cases of C. difficile infection across four sites but no severe harm falls<br />
One patient in the community had 3 separate grade 4 pressure ulcers and 2 grade 2<br />
One Never Event was reported but the care episode in which it occurred was in January 2013,<br />
this was a retained swab associated with an obstetric delivery<br />
84 incidents have exceeded their investigation completion dates. These comprise of legacy<br />
incidents (12) and incidents raised since 1/10/12 (72). A plan is in place. While clearing the<br />
oldest incidents more recent SI cases become overdue within the month. The CAGs with<br />
central support are working together to resolve these.<br />
CAS Alert performance indicates there are no alerts currently overdue for action.<br />
34 legacy complaints outstanding. The central and CAG teams are working to resolve these.<br />
The Friends and Family Test (FFT) continues to be rolled out across the organisation and is on<br />
target for all wards/departments to be asking the FFT question by end of February, prior to<br />
national implementation in April 2013. Response rate is currently disappointing<br />
CQC activity in February and early March included 2 new unannounced compliance reviews<br />
one at St Bartholomew Hospital (SBH) and the other Mile End (MEH). The CQC also carried<br />
out a follow up visit to Intercare Services at Whipps Cross (WX) in March.<br />
What do our regulators think?<br />
Efficiency and Productivity<br />
Headline regulatory performance in month reflects the difficult position although VTE has<br />
come back in line in February. Key issues are<br />
Cancer 62 day standard; The backlog of cases to be treated is reducing & we plan to be back<br />
on track in April 13‐we are delivering the recovery plan<br />
18 week treatment standard; On plan to recover the admitted position from April 2013‐We<br />
are delivering the recovery plan<br />
Mixed sex accommodation breaches; We are outliers in terms of performance in London and<br />
have put in place revised controls to improve the April 13 position<br />
4hr emergency access; Now managed through the Emergency Care <strong>Board</strong>, there are several<br />
work streams (Infants and young people, assessment model at Wx, admission, Length of stay<br />
and discharge)<br />
Infection control; Our current rate has improved on the position over the last year however<br />
we remain with challenging targets next year<br />
We are about to report Q3 performance against the CCP standards. We met those standards<br />
overall in Q1 and in Q2. From 2013‐14 the CCP standards start to anticipate performance gains<br />
arising from our merger, around provision of services such as chemotherapy locally, acute<br />
care rotas and workforce distribution in paediatrics and acute oncology, and productivity gains<br />
on length of stay and re‐admission rates where the <strong>Trust</strong> aims to achieve organisation wide<br />
what we achieve in our best performing hospital.<br />
3
What do our regulators think?<br />
BH Level Summary<br />
DH Score<br />
Feb13<br />
1.92<br />
YTD<br />
2.38<br />
Q3<br />
2.42<br />
Year to date<br />
DH Monitoring Framework<br />
DH<br />
Scale 0<br />
1 2 2.4 3<br />
4<br />
5<br />
Q3<br />
3.5<br />
Q3 adjusted<br />
4<br />
GRR Score<br />
GRR<br />
Foundation <strong>Trust</strong> Single<br />
Operating Model<br />
Scale<br />
0<br />
1 2 3<br />
4<br />
5<br />
GRR Score<br />
Q3<br />
2<br />
FRR<br />
Scale 1<br />
2 3<br />
4<br />
5<br />
Co-operation and<br />
Competition Panel<br />
Dashboard<br />
Q1 Q2 Q3<br />
provisional<br />
Care Quality Commission<br />
Compliance<br />
compliant<br />
4
Safety, Quality and Innovation<br />
BH Level Detailed PI Tracking<br />
Patient Experience Real Time Feedback (RTF)<br />
DH Friends and Family Test<br />
A threshold has not yet been set<br />
5
Safety, Quality and Innovation<br />
BH Level Detailed PI Tracking<br />
Incidents, Serious Incidents and Never Events<br />
6
Safety, Quality and Innovation<br />
BH Level Detailed PI Tracking<br />
Saving Lives<br />
7
Safety, Quality and Innovation<br />
BH Level Detailed PI Tracking<br />
Falls (BH Quality Priority)<br />
8
Safety, Quality and Innovation<br />
BH Level Detailed PI Tracking<br />
Pressure Ulcers (BH Quality Priority)<br />
Reference / Benchmark for Total Pressure Ulcers:<br />
TBD per 1,000 OBD<br />
9
Safety, Quality and Innovation<br />
BH Level Detailed PI Tracking<br />
Maternity<br />
*<br />
* Note: validation of February data is not yet complete<br />
10
Safety, Quality and Innovation<br />
BH Level Detailed PI Tracking<br />
Complaints<br />
11
What do our regulators think?<br />
BH Level Detailed KPI Tracking<br />
18 weeks<br />
Accident and Emergency<br />
Cancer Access – Provisional Feb<br />
12
What do our regulators think?<br />
BH Level Detailed KPI Tracking<br />
VTE, DTOC, MSA, Diagnostics<br />
Infection Control<br />
13
Efficiency, Productivity and Finance<br />
BH Level Detailed PI Tracking<br />
Inpatient Activity<br />
Outpatient Activity<br />
14
What do our partners think?<br />
BH Level Detailed KPI Tracking<br />
Work is underway with the Director of Communications to define an approach to<br />
obtaining regular feedback from partners.<br />
The following approaches are being considered:<br />
• GPs – regular temperature checks<br />
• CCG, CSUs and stakeholder groups – annual 360° feedback, regular<br />
temperature check<br />
• General - reputation tracker<br />
15
R&D, Education and Communications<br />
BH Level Detailed PI Tracking<br />
R & D Financial Metrics<br />
R & D Non-Financial Metrics<br />
R & D Project Metrics<br />
Actual YTD<br />
Target<br />
Forecast > target<br />
Note: Only Four data points available in year<br />
16
What do our staff and students think?<br />
BH Level Detailed KPI Tracking<br />
Staff Pulse Survey<br />
NOTE: Baseline represents results from 2012 National Staff Survey engagement questions 17
What do our staff and students think?<br />
BH Level Detailed KPI Tracking<br />
Post Graduate Medical Trainees – 2012 Survey<br />
Overall Mean of survey responses<br />
Overall satisfaction<br />
Access to education resource<br />
Adequate Experience<br />
-1.8%<br />
+0.1%<br />
-2.7%<br />
+1.1%<br />
Clinical Supervision<br />
Education Supervision<br />
Feedback<br />
Handover<br />
-0.5%<br />
-4.3%<br />
-5.0%<br />
+1.9%<br />
Induction<br />
Local Teaching<br />
Regional Teaching<br />
Study Leave<br />
-6.8%<br />
+1.1%<br />
-2.2%<br />
-0.6%<br />
Undermining<br />
Work Load<br />
-0.4% -4.8%<br />
18
Workforce<br />
BH Level Detailed PI Tracking<br />
Statutory and Mandatory Training<br />
19
Workforce<br />
BH Level Detailed PI Tracking<br />
Human Resources<br />
*<br />
* NOTE: Target (represented by------) is equal to 95% of budgeted establishment 20
Workforce<br />
BH Level Detailed PI Tracking<br />
Human Resources<br />
* NOTE: Annualised sickness absence is calculated one month in arrears<br />
21
Report to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013 TB 27/13<br />
Title Quality and safety performance report ‐ Month 11<br />
Sponsoring Director<br />
Chief Nurse<br />
Author(s)<br />
Deputy Chief Nurse Quality Governance, <strong>Barts</strong> <strong>Health</strong><br />
Head of Governance Standards and Risk Management<br />
Head of Patient Safety<br />
Purpose<br />
To report to the <strong>Trust</strong> <strong>Board</strong> on safety and quality indicators<br />
and issues across all sites of <strong>Barts</strong> <strong>Health</strong>.<br />
Previously considered by <strong>Trust</strong> Management <strong>Board</strong>, 9 April 2013<br />
Executive summary:<br />
This report provides a summary of performance against key quality and safety indicators<br />
for SHMI, hospital acquired infections, falls, pressure ulcers, serious incidents, CAS alerts,<br />
CQC assurance and patient feedback for <strong>Barts</strong> <strong>Health</strong> for Month 11, February 2013.<br />
Risk and Assurance<br />
Related Assurance<br />
Framework entries<br />
Legal implications/<br />
regulatory requirements<br />
This report provides assurance of the quality and safety of<br />
services provided ensuring the best outcomes for patients.<br />
This report provides assurance against the following CQC<br />
Essential Standards:<br />
Outcome 4 ‐ care and welfare of people who use the services<br />
Outcome 8 ‐ cleanliness and infection control<br />
Outcome 16 – assessing and monitoring the quality of service<br />
Action required:<br />
The <strong>Trust</strong> <strong>Board</strong> is asked to review and discuss 2012/13 Month 11 quality and safety<br />
performance.<br />
1
TB 27/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING: 10 APRIL 2013<br />
QUALITY AND SAFETY PERFORMANCE REPORT – MONTH 11<br />
INTRODUCTION<br />
1. This report highlights performance against key quality and safety indicators for hospital acquired<br />
infections, falls, pressure ulcers, serious incidents, CAS alerts and patient feedback across all of the<br />
six <strong>Barts</strong> <strong>Health</strong> hospital sites. It also provides an update on recent CQC compliance review activity<br />
and action planning.<br />
Executive Summary for Month 11 (February 2013)<br />
The SHMI is unchanged at 0.84 which is a lower than expected for the <strong>Trust</strong>.<br />
There was 1 case of MRSA bacteraemia for a patient at Newham (NUH).<br />
There were 8 cases of C. difficile infection across four sites.<br />
There were no severe harm falls incidents.<br />
One patient in the community had 3 separate grade 4 pressure ulcers and 2 grade 2 pressure ulcers.<br />
There were 33 SIs raised in the month.<br />
One Never Event was reported but the care episode in which it occurred was in January 2013, this<br />
was a retained swab associated with an obstetric delivery.<br />
There remain a high number of incidents (84) that have exceeded their investigation completion<br />
dates. These comprise of legacy incidents (12) and incidents raised since 1/10/12 (72). A recovery<br />
plan is in place but while clearing the oldest incidents more recent SI cases become overdue within<br />
the month. The CAGs with the support of the central Patient Safety and Governance and Standards<br />
Teams are working together to resolve these.<br />
CAS Alert performance indicates there are no alerts currently overdue for action.<br />
The number of legacy complaints outstanding (34) remains a concern for the organisation. The<br />
central and CAG teams are working to resolve these.<br />
The Friends and Family Test (FFT) continues to be rolled out across the organisation and is on target for all<br />
wards/departments to be asking the FFT question by the middle of February, prior to national<br />
implementation in April 2013.<br />
CQC activity in February and early March included 2 new unannounced compliance reviews one at<br />
St Bartholomew’s Hospital (SBH) and the other Mile End (MEH). The CQC also carried out a follow<br />
up visit to Intercare Services at Whipps Cross (WX) in March.<br />
2
PERFORMANCE AGAINST SELECTED INDICATORS<br />
TB 27/13<br />
Standardised Hospital Mortality Indicator (SHMI)<br />
2. <strong>Barts</strong> <strong>Health</strong>’s SHMI at 0.84 places it 10 th position in a list of relevant healthcare organisations in<br />
England which measure the indicator of deaths associated with hospitalisation. This is derived from<br />
the last quarterly reported SHMI data for hospitals in England published in January 2013 for the<br />
period up to June 2012.<br />
3. Sixteen trusts had a ‘significantly lower than expected’ SHMI (between 0.71 and 0.87) indicating a<br />
13% to 29% lower than expected mortality rate. <strong>Barts</strong> <strong>Health</strong> is in this group and is also the largest<br />
organisation in the sample with 159,820 hospital cases. Given the size of <strong>Barts</strong> <strong>Health</strong>, there were<br />
717 less deaths than expected in comparison for example to 424 at UCH with 64,972 cases.<br />
Infection Control<br />
Table 1: Summary of <strong>Barts</strong> <strong>Health</strong> Infection data at 28 February 2013<br />
February<br />
2013<br />
<strong>Barts</strong> <strong>Health</strong><br />
Targets<br />
Period<br />
April<br />
2012 to<br />
March<br />
2013<br />
Non <strong>Trust</strong><br />
Apportioned<br />
'Pre'<br />
<strong>Trust</strong><br />
Apportioned<br />
'Post'<br />
3<br />
YTD Non<br />
<strong>Trust</strong><br />
Apportioned<br />
'Pre'<br />
YTD <strong>Trust</strong><br />
Apportioned<br />
'Post'<br />
<strong>Trust</strong><br />
Apportioned<br />
'Post'<br />
Date since<br />
last +ve<br />
Specimen<br />
MRSA BC 8 1 1 10 11 06/02/2013 22<br />
C difficile 99 1 8 43 84 18/02/2013 10<br />
The London Chest<br />
MRSA BC 6 * 0 0 0 2 14/07/2012 229<br />
C difficile 59 * 0 0 0 2 17/05/2012 287<br />
Newham<br />
MRSA BC 2 0 1 3 2 06/02/2013 22<br />
C difficile 6 0 1 10 12 11/02/2013 17<br />
The Royal London<br />
MRSA BC 6 * 0 0 4 6 10/11/2012 110<br />
C difficile 59 * 0 3 13 33 18/02/2013 10<br />
St Bartholomew's<br />
MRSA BC 6 * 0 0 1 1 05/12/2012 85<br />
C difficile 59 * 0 2 5 6 04/02/2012 24<br />
Whipps Cross<br />
MRSA BC 0 1 0 2 0 16/03/2012 349<br />
C difficile 34 1 2 15 31 18/02/2013 10<br />
No. of<br />
days<br />
since<br />
last<br />
+ve<br />
Case
TB 27/13<br />
Mile End Hospital is not counted in total for <strong>Barts</strong> <strong>Health</strong> as attributed to Commissioners<br />
MRSA BC 0 0 0 0 ‐ ‐<br />
C difficile 0 1 1 2 27/02/2013 1<br />
Narrative for MRSA bacteraemia and C/diff acquisition after 72 hours<br />
MRSA Bacteraemia<br />
4. One case of MRSA Bacteraemia was attributed to NUH (see Table 1. The MRSA admission screen was<br />
completed on the 21/12/12 but skin wounds present were not screened. The admission screen was<br />
negative. Subsequent screening for MRSA colonisation was positive on the 11/2/13. At this time the<br />
sores on various part of the body were swabbed for MRSA (grade 2 pressure ulcers had also developed<br />
on the heel and sacrum and a leg laceration). The patient also developed C. difficile during the<br />
admission. Decolonisation therapy protocol was prescribed on the 13/2/13.<br />
MRSA RCA findings<br />
5. The skin wounds were not screened on admission but on 07/ 02/13; the results which came back as<br />
MRSA positive. It is therefore difficult to state whether the patient had acquired MRSA whilst an<br />
inpatient or the wound may had been colonised prior to admission. The patient's skin condition made<br />
it difficult for venous access; takes multiple attempts hence possibility of contamination of the blood<br />
culture bottles.<br />
6. Once results for MRSA bacteraemia was confirmed patient’s treatment plan was reviewed and it was<br />
confirmed that patient was not septic therefore antibiotics therapy was not required.<br />
7. The blood culture positive for MRSA was taken from a newly inserted cannula this is not a normal<br />
recommendation. However, considering the patient’s condition this practice was deemed acceptable.<br />
8. Monthly MRSA screening as the <strong>Trust</strong>’s policy recommends was not adhered to, it is possible that a<br />
positive screening result would have prompted protocol and could have prevented this incident.<br />
Clostridium Difficile<br />
9. Nine cases were reported in February: eight post 72 hours and one pre 72 hours of the patient’s<br />
admission (see Table 1). The target for <strong>Barts</strong> <strong>Health</strong> is 99. At the end of February there have been 127<br />
cases: eighty four post 72 hours and forty three pre 72 hours.<br />
The London Chest reported no cases. Total year to date is two post 72 hours.<br />
Newham reported one post 72 hours. Total year to date is twenty two: twelve post 72 hours and<br />
ten pre 72 hours.<br />
Royal London reported three post 72 hours. Total year to date is forty six: thirty three post 72<br />
hours and thirteen pre 72 hours.<br />
St Bartholomew's reported two post 72 hours. Total year to date is eleven: six post 72 hours and<br />
five pre 72 hours.<br />
Whipps Cross reported two post 72 hours and one pre 72 hours. Total year to date is forty six:<br />
thirty one post 72 hours and fifteen pre 72 hours.<br />
Mile End (Community) reported one post 72 hour. Total year to date is three: two post 72 hours<br />
and one pre 72 hours, the case at Mile End is on the Commissioners trajectory.<br />
4
TB 27/13<br />
Newham Hospital<br />
10. There was a single case of C. difficile in a patient admitted to the stroke unit. The patient was<br />
commenced on laxative treatment as well as antibiotics for different infections. The patient developed<br />
diarrhoea 05/02/13 was sampled and it tested positive to C. difficile. Since the patient has been taking<br />
both antibiotics and laxatives since admission it is not clear whether this was medication induced<br />
infection.<br />
11. Action taken: Medical, pharmacist and nursing staff to review/ monitor the use of laxatives and<br />
antibiotics. Staff to be educated, on when to isolate patients and test for c. difficile.<br />
Royal London Hospital<br />
12. Three cases of C. difficile were reported in February the following issues were reviewed:<br />
One patient was a recurrence (CDT positive 11 months earlier)<br />
All three patients were on antibiotics; these were deemed as appropriate despite poor<br />
documentation around reason for medication and duration.<br />
Two of the patients had PPI’s<br />
Hand Hygiene scores were above 95%<br />
One patient was critically ill and died not related to C. Difficile infection.<br />
In ACCU staff were unable to isolate patients when on 4F (HDU) due to staffing<br />
Two of the cases were isolated on 4E, when investigated they were found not to be linked.<br />
Action taken: Medical, pharmacist and Nursing staff to review/ monitor the prescribing of antibiotics.<br />
St Bartholomew’s Hospital<br />
13. Two cases of C. difficile was reported the following were RCA issues were reviewed:<br />
Both patients were oncology patients and received multiple courses of antibiotics. However all<br />
were prescribed in line with the Antibiotic Policy.<br />
Hand Hygiene scores were above 95% in the areas<br />
In ward 4A both patients were initially isolated when symptoms commenced, one was de isolated<br />
to accommodate another known infectious patient. They were re‐isolated on receipt of positive<br />
samples<br />
The two cases did occur on one ward but when investigated they were found not to be linked.<br />
Action taken: Medical and Nursing staff are to review care of patients with diarrhoea, and must not be deisolated<br />
while symptomatic.<br />
Whipps Cross Hospital<br />
14. Two cases of hospital C. difficile were reported during February, the following issues were reviewed<br />
Clinical Infection deemed unlikely in 1 patient as clinically well but treatment was started due to<br />
mild neutrophilia. The second patient admitted to ICU had clinical infection.<br />
Antibiotics were prescribed for uro‐sepsis and LRTI. One case was deemed not to be in line with<br />
WX antibiotic guidelines<br />
Hand hygiene compliance and environment cleaning audit results were good on both wards >97%<br />
Patient was not isolated from the onset of diarrhoea but isolated on receipt of results<br />
One patient was not isolated from the onset of diarrhoea but isolated on receipt of results<br />
Action taken: Where non‐compliance with the antibiotic policy identified this has been addressed during<br />
the RCA. A copy of the RCA form has been sent to the ward manager and matron to identify learning and<br />
to agree actions to improve practice. Isolation of patients remains a challenge at the WX site and the<br />
importance of isolating patients with diarrhoea is being continuously reinforced as a priority<br />
5
TB 27/13<br />
Patient Falls<br />
Table 2: Patient Falls February 2013<br />
Patient Falls<br />
Period<br />
Site<br />
B&L NUH WX<br />
Q1: April‐June 208 96 165<br />
Q2: July‐Sept 232 92 152<br />
No Harm<br />
Low Harm<br />
Moderate Harm<br />
Severe Harm/Death<br />
LCH MEH RLH SBH<br />
Q 3: Oct ‐ Dec 11 20 130 20 88 121<br />
January 2013 9 20 59 8 38 61<br />
February 2013 5 19 55 8 40 68<br />
YTD: 2012‐2013 804 354 567<br />
Inpatient Falls<br />
Period<br />
Site<br />
B&L NUH WX<br />
Q1: April‐June 124 20 62<br />
Q2: July‐Sept 130 22 37<br />
LCH MEH RLH SBH<br />
Q3: Oct ‐ Dec 15 7 61 14 28 74<br />
January 2013 3 6 38 4 4 29<br />
February 2013 3 3 25 5 12 18<br />
YTD: 2012‐2013 438 86 220<br />
Inpatient Falls<br />
Period<br />
Site<br />
B&L NUH WX<br />
Q1: April‐June 7 3 1<br />
Q2: July‐Sept 6 2 2<br />
LCH MEH RLH SBH<br />
Q3: Oct ‐ Dec 0 1 3 4 2 3<br />
January 2013 2 0 0 0 0 0<br />
February 2013 0 0 2 0 0 1 <br />
YTD: 2012‐2013 25 7 7<br />
Inpatient Falls<br />
Period<br />
Site<br />
B&L NUH WX<br />
Q1: April‐June 1 0 0<br />
Q2: July‐Sept 0 2 1<br />
LCH MEH RLH SBH<br />
Q3: Oct ‐ Dec 0 0 0 0 0 0<br />
January 2013 0 0 0 0 0 0<br />
February 2013 0 0 0 0 0 0<br />
YTD: 2012‐2013 1 2 1<br />
All Falls – February 8 22 82 13 52 87<br />
Falls per 1,000 Bed Days (Feb) 1.4 3.8 14.3 2.3 9.1 15.2<br />
/denotes an increase or decrease in number of incidents this month compared to last month<br />
6
TB 27/13<br />
15. As can be seen in Table 2 there were no severe falls Injuries in month 11.<br />
Pressure Ulcers<br />
Table 3: Pressure Ulcers February 2013<br />
Pressure Ulcers<br />
Site<br />
Timescale<br />
B&L<br />
LCH MEH RLH SBH<br />
NUH WX<br />
Q1: April‐June 17 16 9<br />
Q2: July‐Sept 27 7 12<br />
Q3 Oct‐Dec 1 6 21 3 10 16<br />
January 2013 0 0 3 0 8 2<br />
February 2013 1 0 3 2 12 10<br />
YTD: 2012‐1213 84 53 49<br />
Pressure Ulcers<br />
Site<br />
Timescale<br />
B&L<br />
LCH MEH RLH SBH<br />
NUH WX<br />
Q1: April‐June 85 26 50<br />
Q2: July‐Sept 85 21 44<br />
O3: Oct‐Dec 9 8 61 12 45 36<br />
January 2013 6 1 28 4 24 11<br />
February 2013 1 0 18 3 19 25<br />
YTD: 2012‐1213 321 135 166<br />
Pressure Ulcers<br />
Site<br />
Timescale<br />
B&L<br />
LCH MEH RLH SBH<br />
NUH WX<br />
Q1: April‐June 4 3 6<br />
Q2: July‐Sept 9 4 4<br />
O3: Oct‐Dec 0 2 2 0 10 14<br />
January 2013 0 0 2 0 4 4<br />
February 2013 0 0 1 0 2 4<br />
YTD: 2012‐1213 20 23 32<br />
Pressure Ulcers<br />
Site<br />
Timescale<br />
B&L<br />
LCH MEH RLH SBH<br />
NUH WX<br />
Q1: April‐June 9 0 0<br />
Q2: July‐Sept 7 2 0<br />
O3: Oct‐Dec 0 0 1 2 1 2<br />
January 2013 0 0 0 0 0 1<br />
February 2013 0 0 0 0 0 0<br />
YTD: 2012‐1213 19 3 3<br />
All PU February 2 0 22 5 33 39<br />
Rate per 1,000 bed<br />
days (Feb)<br />
0.3 0 3.8 0.9 5.8 6.8<br />
/denotes an increase or decrease in number of incidents this month compared to last month<br />
Grade 1<br />
Grade 2<br />
Grade 3<br />
Grade 4<br />
7
TB 27/13<br />
16. As shown in Table 3 there were no severe harm grade 4 pressure ulcer incidents in February 2013.<br />
Tissue Viability Service led Quality Improvement<br />
The Tissue Viability (TV) nurses are participating in the Patient Safety Forum to facilitate the<br />
champions for the Quality Improvement Collaborative (QIC) in pressure ulcer reduction. This will<br />
ensure ward champions are trained and PU link nurses identified in all areas that will cascade<br />
training re risk assessment, implementing care plans and ensure investigatory pathways for<br />
pressure ulcer incidents.<br />
An e‐learning module on standardised pressure ulcer prevention and management is being<br />
developed and will be made accessible via the Learning and Development intranet.<br />
TV Service has gained assistance from the Education Academy to include pressure ulcer care<br />
pathways as mandatory training for all nurses attending the Induction programme and update days.<br />
The QIC pressure ulcer reduction programme continues. Tayberry (NUH), 5A (SBH), Neonatal<br />
Intensive Care Unit (RLH) all continue to trial different tools/ methods to reduce avoidable pressure<br />
ulcers. Improvements made will be rolled out across BH.<br />
The TV nurses now support the Preceptorship Nurse Facilitators’ training programme for newly<br />
qualified Registered Nurses by teaching them the pressure ulcer prevention care pathway and<br />
processes and wound management.<br />
Table 4: Adult Community Nursing reported pressure ulcers February 2013<br />
Adult Community (District ) Nursing<br />
Grade<br />
Period<br />
Grade 1 Grade 2 Grade 3 Grade 4<br />
Q1: April‐June 3 17 13 5<br />
Q2: July‐Sept 4 20 5 0<br />
Q3: Oct‐Dec 6 9 3 0<br />
January 2013 0 3 1 0<br />
February 2013 0 3 0 3<br />
YTD: 2012‐1213 13 52 22 8<br />
17. One patient had 5 pressure ulcers which consisted of 3 grade 4 pressure ulcers on their foot, 1 x grade<br />
2 also on the foot and a grade 2 on leg. This patient was known to tissue viability team and there was<br />
underlying ischemia with comorbidities. The full RCA investigation is to be completed. The Wound<br />
Care Team continue to work closely with district nurses in providing joint visits and reviewing grade 3<br />
and 4 pressure ulcer patients on a weekly/twice weekly basis.<br />
8
Serious Incidents<br />
TB 27/13<br />
Table 5: Serious Incidents (SI) by category February 2013<br />
SI<br />
Reported<br />
Serious Incidents<br />
Category<br />
Number<br />
in Pressure Ulcers 9<br />
February Delays in Care 7<br />
2013 Obstetrics (includes 1 Never Event) 5<br />
Treatment 3<br />
Safeguarding Adults 2<br />
Equipment 1<br />
IT related 1<br />
Medication 1<br />
Safeguarding Children 1<br />
Tracheostomy 1<br />
Anaesthetics/Theatres/SSD 1<br />
Appointments and Clinics 1<br />
Totals 33<br />
18. There were 33 new SIs reported in February 2013<br />
19. There was one Never Event reported but the incident happened in January 2013. This was a maternity<br />
case where 2 vaginal swabs were not removed after suturing. The Women’s CAG have subsequently<br />
published a ‘hot topic’ memo to all staff to remind them of checking for swabs at the end of all suturing<br />
procedures.<br />
20. As of 15 March 2013, there were 84 overdue SIs. This comprised of 12 legacy incidents (down from 27<br />
last month) and the central Patient Safety and Governance & Standards Teams are working with the<br />
CAG teams to complete the overdue investigations and reports. The aim is try to achieve closure of all<br />
the legacy incidents by 31 March.<br />
21. There are 72 overdue SI reports identified since 1/10/12 and the CAG teams are working hard to<br />
conclude and finalise the investigations.<br />
Moderate severity incidents reported in February<br />
22. In March TMB and QAC discussed a paper which recommended changes to the SI process including<br />
how other non‐SI but potentially ‘of concern’ incidents and complaints are triangulated and reported<br />
going forward (e.g. those of moderate severity and/or resulting in actual harm and/or which identify<br />
omissions in basic care). This recommendation (number 7) was supported and approved by QAC.<br />
23. Table 6 reports moderate severity incidents by category and CAG reported in February and should be<br />
viewed as a precursor to further analysis, reporting and eventual triangulation with moderate/high risk<br />
rated complaints going forward. It does not drill down to sub category level but this is intended and<br />
individual incident reports were reviewed.<br />
24. The most frequently reported (top 3 moderate) incident categories are;<br />
Tissue ulcers (22)<br />
Obstetric incidents (15)<br />
Staff injuries / illness (13)<br />
25. Further work is being undertaken to understand some data anomalies identified from this initial review<br />
of moderate incidents by category and of the individual incidents themselves. Firstly it indicated a high<br />
degree of variability of actual harm to patients even though coded as moderate severity. For example<br />
9
TB 27/13<br />
for pressure ulcers 22 coded as moderate harm should have been recoded as no harm as 10 were<br />
acquired outside of BH care and 1 case was an unavoidable end of life skin change. Four of these had<br />
received final approval without the severity being modified.<br />
26. Seven needle stick injuries in the Staff Injury/Illness category were graded as moderate harm. In no<br />
case was there significant immediate harm to the staff member and in only one case was there a<br />
significant risk of blood borne infection. In some cases high risk situations which had been handled<br />
without harm arising were reported as moderate harm. In others review of the incident had indicated<br />
no <strong>Trust</strong> fault although the patient had suffered harm as a result of ill health.<br />
27. Less than a third of the moderate incidents had received final approval (all of them should have done,<br />
according to the dates). Inappropriate grading seemed as common amongst those with final approval.<br />
as without, indicating that grade is not being picked up either by the incident handlers or at final<br />
approval as it should be.<br />
Table 6: Moderate Severity Incidents in February 2013<br />
Incident Category<br />
Ambulatory<br />
Cancer Services<br />
Cardiovascular<br />
Children’s Services<br />
Clinical Support Services<br />
Corporate<br />
ECAM<br />
Surgery<br />
Women’s <strong>Health</strong><br />
Totals<br />
% all MIs. This incident<br />
type<br />
Anaesthetics/Theatres/SSD 1 3 4 4%<br />
Appointments and Clinics 1 1 1%<br />
Blood Transfusion 1 2 3 3%<br />
Communication Issues 1 1 1%<br />
Delays in Care 2 1 1 2 1 1 8 8%<br />
Equipment 2 1 3 3%<br />
Infection Control 1 1 2 2%<br />
Medication 1 1 1%<br />
Obstetrics 1 14 15 16%<br />
Pathology/Specimen 1 1 1%<br />
Patient Falls 1 2 1 4 4%<br />
Pressure Ulcers 4 14 4 22 23%<br />
Safeguarding Adults 1 1 2 2%<br />
Skin Trauma 1 1 1%<br />
Staff injuries/illness at<br />
work 2 2 1 3 1 2 2 13 14%<br />
Staffing Issues 1 1 2 2%<br />
Tracheostomy 1 1 2 2%<br />
Transport 1 1 1%<br />
Treatment 2 1 1 1 1 3 9 9%<br />
Totals 11 6 3 2 3 3 28 14 25 95 100%<br />
% all MI's, this CAG 12% 6% 3% 2% 3% 3% 29% 15% 26% 100%<br />
Central Alerting System (CAS), Alert Assurance and Performance<br />
28. Table 7 shows that of the six new CAS alerts received in February all have been closed.<br />
10
TB 27/13<br />
29. Regarding the remaining open alerts, actions to ensure compliance with the Estates & Facilities (tamper<br />
free window restrictors) alert are nearing completion and on track to be completed by the target of<br />
23/05/13.<br />
NPSA Safer Intrathecal devices alert Part B<br />
30. The remaining open NPSA alert relates to the introduction of safer intrathecal devices and action by<br />
relevant clinical leads in each CAG, this is currently overseen by the Medical Director (MD) and the<br />
Clinical Procurement Group. The MD has requested that each CAG using intrathecal devices undertakes<br />
a risk assessment. Not all CAGs have responded and the requested risk assessments are outstanding. It<br />
is highly probable that procurement and clinical recommendations regards the selection and<br />
introduction of suitable devices across the <strong>Trust</strong> will not have been completed by the target date of 1<br />
April 2013.<br />
Table 7 Central Alerting System (CAS) Assurance and Performance<br />
CAS Alerts Received February 2013 and (year to date since 1 April 2012)<br />
MDA NPSA Estates & Facilities Total<br />
6 (78) 0 (0) 0 (3) 6 (81)<br />
All open alerts (as at 28 February 2013)<br />
MDA NPSA Estates & Facilities Total<br />
1 1 1 3<br />
Overdue CAS Alerts, <strong>Barts</strong> <strong>Health</strong>, pre & post 1 April 2012<br />
MDA NPSA Estates & Facilities Total<br />
0 0 0 0<br />
Patient Experience<br />
Legacy Complaints<br />
31. In October, the <strong>Trust</strong> had a total of 122 legacy complaints, which progressively exceeded the timescales<br />
negotiated with complainants. A number of contributory factors were identified as the reason for the<br />
delays. Some of these included:<br />
Difficulties accessing ICT systems across different hospital sites post the 1 October<br />
Delays with accessing records across different hospital sites<br />
Limited knowledge of complaints management on the part of a significant number of staff who<br />
were new to their roles<br />
Inadequate handovers due to staff absence pre and post the merger<br />
It was subsequently agreed that:<br />
The CAG Governance Teams would contact all the complainants to give them an update and agree<br />
reasonable deadlines for providing responses to complaints<br />
The Patient Experience Team would support the CAGs with drafting response letters<br />
Al legacy complaints would be responded to and closed by the 31 st of January<br />
The Patient Experience Team would provide specific training for the appropriate staff<br />
32. At the end of February, a total of 88 legacy complaints had been closed and 34 remain open at the time<br />
of reporting, (see Tables 7 and 8). Staff absence due to sickness and a high number of incoming<br />
complaints is cited by the CAGs as some of the reasons why a number of legacy complaints remain<br />
11
TB 27/13<br />
open. In addition to this, difficulties with ICT systems and accessing records across sites remain a<br />
problem.<br />
Training and Developments in Complaints Management<br />
33. Training has been provided to staff that required it and on‐going support from the Patient Experience<br />
Team. This has included additional training, shadowing, drafting response letters and providing advice<br />
about how to manage complex complaints<br />
34. The Patient Experience Team continue to work closely with all the CAG Governance Managers and their<br />
teams and CAGS have provided assurance to the corporate Patient Experience Team that all open<br />
legacy complaints will be closed by the 31 st of March.<br />
35. However The <strong>Trust</strong> board should note that some staff in CAGs with a key role in the management of<br />
complaints remain on leave and further organisational changes might impact on the progress of<br />
meeting the set deadline.<br />
Table 8. Number of legacy complaints currently open<br />
Mile<br />
End Newham<br />
Royal<br />
London <strong>Barts</strong><br />
Multiple<br />
sites<br />
2 2 28 1 1<br />
CAG<br />
No. of legacy<br />
complaints currently<br />
open<br />
Ambulatory 8<br />
Cancer 1<br />
Corporate 3<br />
Clinical Support Services 0<br />
ECAM 7<br />
Surgery 12<br />
Women’s 3<br />
Total 34<br />
Table 9: Complaint Performance Report by Clinical Academic Group<br />
Clinical Academic Group<br />
Number of<br />
complaints<br />
Ack. within 3<br />
working days Percentage<br />
Ambulatory 22 21 95%<br />
Cancer 2 1 50%<br />
Cardiovascular 5 4 80%<br />
Children's 6 6 100%<br />
COO 3 2 67%<br />
CSS 10 8 80%<br />
Nursing & Quality<br />
Governance 1 1 100%<br />
ECAM 44 28 64%<br />
Surgery 23 22 96%<br />
Women's 16 16 100%<br />
Total 132 109 83%<br />
12
TB 27/13<br />
CAG<br />
Number of<br />
complaints<br />
Response<br />
performance Percentage<br />
Ambulatory 22 13 59%<br />
Cancer 2 2 100%<br />
Cardiovascular 5 5 100%<br />
Children's 6 2 33%<br />
CSS 10 8 80%<br />
COO 3 2 67%<br />
Nursing & Quality<br />
Governance 1 0 0%<br />
ECAM 44 38 86%<br />
Surgery 23 18 78%<br />
Women's 16 13 81%<br />
Grand Total 132 101 77%<br />
36. Top areas of complaints for service users are detailed in Table 10.<br />
Consistent with previous months, the top 3 areas of concern for service users have been;<br />
Diagnosis and Treatment ‐ 34% (43) of the total number of complaints closed during the month<br />
Communication ‐ 23% (30) of the total number of complaints closed during the month<br />
Delays in care ‐ 14% (18) of the total number of complaints closed during the month<br />
Table 10: Top areas of concerns by site<br />
Diagnosis /<br />
Treatment<br />
Communication ‐ verbal /<br />
written / electronic Delays in care Total<br />
London Chest 1 0 0 1<br />
Mile End 1 0 1 2<br />
Newham 0 3 4 7<br />
Royal London 25 15 5 45<br />
St. Bartholomew's 1 3 0 4<br />
Whipps Cross 15 9 8 32<br />
Total 43 30 18 91<br />
Parliamentary <strong>Health</strong> Service Ombudsman Cases<br />
37. During the year to date, the PHSO has indicated interest in 61 complaints concerning <strong>Barts</strong> <strong>Health</strong> see<br />
Graph 1. Of the cases concerned:<br />
‐ 30 are currently active (24 at the request for information stage 6 referred back for further local<br />
resolution and are currently being considered by the services)<br />
‐ 31 have been closed with no further action required of the <strong>Trust</strong><br />
‐ 1 complaint (not included in the summary above) from last financial year remains open at the time<br />
of reporting, has been investigated and is currently in the action planning stage.<br />
38. Cases are returned to the <strong>Trust</strong> by the PHSO where it is considered that further dialogue or a local<br />
resolution meeting could resolve the issues a complainant has reported to PHSO. In some case,<br />
complainants go straight to the PHSO before contacting the <strong>Trust</strong> about the response they have<br />
received.<br />
39. Usually the PHSO refer such cases back to the <strong>Trust</strong> and recommend that: a clarification of policies,<br />
providing copies of policies or other relevant documentation or a sum of money for minor<br />
inconveniences would suffice as a form of local resolution<br />
13
Graph 1: Distribution of complaints reported to PHSO<br />
TB 27/13<br />
No. of active PHSO cases by site<br />
1<br />
1<br />
10<br />
5<br />
13<br />
Newham<br />
Whipps Cross<br />
Royal London<br />
Mile End<br />
<strong>Barts</strong><br />
Patient Advice and Liaison Service (PALs)<br />
40. In February, the <strong>Trust</strong> managed 484 contacts, compared with 420 in January and 344 in December. Of<br />
these, 89% (432) came under ‘issues & concerns,’ (see Table 10. As well as outlining the “type” of work<br />
the service has been engaged in, the adjacent chart demonstrates that a high proportion of PALS work<br />
involves supporting people to resolve issues and concerns they have about services across the <strong>Trust</strong>.<br />
This emphasises the important role of PALS as an early warning system, which identifies potential<br />
complaints, and supports service users to resolve these before they escalate any further.<br />
Table 11: Number of PALS Contacts by Site<br />
Site<br />
Total number<br />
Another hospital 14<br />
London Chest 5<br />
Mile End 14<br />
Newham 139<br />
Royal London 161<br />
St. Bartholomew's 16<br />
Whipps Cross 135<br />
41. As indicated in the bar chart on page 15 the <strong>Trust</strong>’s service users contact the PALS service for various<br />
reasons ranging from requests for advice and information about <strong>Trust</strong> services, to concerns about the<br />
care they received.<br />
42. This demonstrates the pivotal role PALS plays in delivering the organisation’s patient experience<br />
agenda. By being available for patients and their families, PALS represent a service which patients and<br />
their relatives can contact independently of their clinical care providers whenever they wish to alert<br />
the <strong>Trust</strong> to issues or if they wish to raise concerns relating their care needs. As indicated below, the<br />
highest area of activity for the PALS has been around providing advice and information.<br />
43. With regard to actual issues and concerns service users presented with during the month, the three<br />
highest areas of concern have been about:<br />
Communication (24%), which is consistent with reportable complaints, where the second highest<br />
reason for complaints was communication<br />
Appointments and clinics (19%)<br />
Diagnosis / Treatment (14%)<br />
14
TB 27/13<br />
Graph 2: PALS contact by Themes<br />
No. of PALS contacts by subject<br />
140<br />
120<br />
122<br />
116<br />
100<br />
93<br />
80<br />
69<br />
60<br />
40<br />
26<br />
18<br />
20<br />
1<br />
2 1 1<br />
0<br />
Diagnosis / Treatment<br />
Advice and Information<br />
Appointments / Clinics<br />
Blood and Blood products<br />
Communication ‐ verbal / written / electronic<br />
Delays in care<br />
Environment<br />
Equipment and supplies<br />
Fire Safety<br />
Medication / Radiation<br />
<strong>Health</strong>care records / X‐rays / Scans<br />
10 12<br />
6<br />
1 1<br />
Obstetrics<br />
Patient falls<br />
Privacy and dignity<br />
Surgical / Invasive procedures<br />
Security and unacceptable behaviour<br />
1 4<br />
Transport<br />
Friends and Family Test (FFT)<br />
44. <strong>Barts</strong> <strong>Health</strong> achieved 100% coverage (asking the Friends and Family question) in all appropriate areas<br />
at the beginning of February. Results for this month show a high percentage of the patients who<br />
responded would be extremely likely (64%) to recommend the ward or area to their friends and family<br />
(Graph 3 and Table 11).<br />
45. Although gradual improvement in uptake is evident from December to February, this is not reflective of<br />
the total number of eligible discharges across Bart’s <strong>Health</strong>. In order to assist in embedding the<br />
process, Patient Experience facilitators under the guidance of the team leaders continue to support the<br />
CAGs by ensuring that they have all the materials to deliver the process successfully.<br />
46. Facilitators are visiting the wards across all the sites on a weekly basis along with a Team leader<br />
attending a number of committees to further raise awareness of FFT.<br />
47. Staff awareness of and engagement in the process at discharge is of paramount importance to the<br />
success of achieving at least the 15% target which will come into place when the FFT goes live<br />
nationally from the 1 April. The Chief Nurse has raised the issue of staff engagement at <strong>Trust</strong><br />
Management <strong>Board</strong> and information has been sent out to staff via the weekly bulletin.<br />
48. The other important element is to raise awareness amongst patients and their families and carers that<br />
they will be asked on their discharge to answer the FFT question. Leaflets for staff and patients along<br />
with posters have been produced by the DH which has just been received by the <strong>Trust</strong>. These are<br />
15
TB 27/13<br />
currently being distributed around the wards and areas carrying out the FFT. The FFT agenda has<br />
CQUIN monies attached and also will provide the trust with valuable feedback from our patients<br />
therefore it is imperative that everyone takes responsibility for its success.<br />
Graph 3 Friends and Family Test Responses for Recommendation of ward to family/friend<br />
<strong>Barts</strong> <strong>Health</strong> overall response<br />
2% 2% 2%<br />
30%<br />
64%<br />
Extremely likely Likely Neither likely nor unlikely Unlikely Extremely unlikely<br />
Table 12: Numbers of Patients Participating in Friends and Family Test<br />
Dec‐12 Jan‐13 Feb‐13 Total<br />
Base 42 114 248 404<br />
49. Snapshot of comments made by patients:<br />
Extremely likely ‐ “Service was first class. All staff were very friendly and kind. Food was very bad”<br />
Extremely likely ‐ “I would recommend the ward due to the care treatment not only of doctors but of<br />
the nurses and staff. Clean caring helpful polite”<br />
Likely ‐ “Discharged takes too long. Have to wait too long for medication. Otherwise good”<br />
Likely ‐ “It was all good but took a while to be attended at the main entrance/reception”<br />
Neither likely nor unlikely ‐ “There is a v marked difference between the quality of nursing during<br />
the week (great) and at the weekends”<br />
Unlikely ‐ “A few good reasons. The nurses have no thought about patients trying to sleep at night;<br />
laughing & talking loud & banging things about. It was a nightmare”<br />
Real Time Feedback (RTF)<br />
50. Real time feedback collected for February is available through the Integrated Performance Framework<br />
by site and CAG and reported to the <strong>Trust</strong> <strong>Board</strong>. CAGs receive a monthly report as part of their<br />
monthly review information.<br />
16
TB 27/13<br />
CARE QUALITY COMMISSION (CQC) ESSENTIAL STANDARDS<br />
Update on the recent CQC inspection visits and reports<br />
51. The Care Quality Commission carried out unannounced compliance reviews at three registered <strong>Trust</strong><br />
locations in February and the beginning of March.<br />
Mile End Hospital<br />
52. On 18 February CQC carried out an unannounced compliance review. The assessors visited two elderly<br />
service wards Gerry Bennet and Jubilee and assessed compliance with eight Outcomes. These were;<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Outcome 1 Respecting and involving people<br />
Outcome 4 Care and welfare of people who use services<br />
Outcome 5 Meeting nutritional needs<br />
Outcome 7 Safeguarding people who use services from abuse<br />
Outcome 13 Staffing<br />
Outcome 14 Supporting Staff<br />
Outcome 16 Assessing and monitoring the quality of service provision<br />
Outcome 21 Records<br />
53. The <strong>Trust</strong> has received the draft report which judged 3 Outcomes as non‐compliant with moderate<br />
impact on patients or safety. These are Outcomes 5, 13 and 21. The ECAM CAG will factual accuracy<br />
checks the report and the <strong>Trust</strong> will respond to the CQC within the specified time of ten working days.<br />
St Bartholomew Hospital<br />
54. A further compliance review was carried out over two days at SBH 27 and 28 February consecutively.<br />
The assessors visited wards 5A, 5B, 4A, Percival Pott and the Macmillan Vicky Clement Jones Cancer<br />
Information Centre.<br />
55. The <strong>Trust</strong> has received a draft report and the positive findings and fully met judgements are consistent<br />
with the verbal feedback given after the visit. The main areas of focus in the Cancer Services visited<br />
were;<br />
<br />
<br />
<br />
<br />
Outcome 1 respect and involvement( fully met)<br />
Outcome 8 infection control (fully met)<br />
Outcome 13 staffing ( fully met)<br />
Outcome 17 complaints management (fully met)<br />
Whipps Cross Hospital<br />
56. On 1 March the CQC inspected the Ainslie and Hingham’s Intercare Unit. This was a follow up visit from<br />
an initial compliance review in August 2012. The following Outcomes were re assessed along with<br />
evidence of progress and the changes introduced by implementation of the action plan developed after<br />
the visit in August when 3 Outcomes were judged non‐compliant. The verbal feedback and draft report<br />
both provided positive assurance and evidence that quality, safety and patient experience have<br />
improved in this service. The CQC judges that three Outcomes previously not met are now compliant.<br />
<br />
<br />
Outcome 4 Care and welfare of people who use services now fully met (noncompliant<br />
in August)<br />
Outcome 5 Meeting nutritional needs fully met<br />
17
TB 27/13<br />
Outcome 13 Staffing now fully met (non‐compliant in August)<br />
Outcome 14 Supporting Staff now fully met (non‐compliant in August)<br />
Outcome 21 Record keeping not met minor concern (Outcome 21 was not assessed<br />
previously)<br />
57. The <strong>Trust</strong> is yet to respond formally with a factual accuracy check and action plan to address the new<br />
issue identified in relation to nursing documentation.<br />
Care Quality Commission Quality Risk Profile (QRP) for <strong>Barts</strong> <strong>Health</strong><br />
58. An updated version of the Quality and Risk Profile (QRP) was issued on 6 March. It highlighted no<br />
significant changes to risk estimates for the 16 Outcomes since the previous version. There are no high<br />
(red or amber) risk estimates.<br />
59. Outcome 13 Staffing (R22) – the risk slightly decreased from “high yellow” to “low yellow” as a result of<br />
a recent inspection visit. The <strong>Trust</strong> was found compliant with this outcome following a visit at London<br />
Chest Hospital in November 12.<br />
60. Outcome 16 Assessing and monitoring the quality service provision (R10) – the risk estimate rating has<br />
slightly increased from “high green” to “low yellow”. There are no significant changes to any<br />
performance indicators except that previous QRP versions still had some indicators separated for the 3<br />
legacy trusts.<br />
61. The <strong>Trust</strong> is still rated “much worse than expected” for an indicator that relates to “Proportion of alerts<br />
acknowledged within deadline out of total number of alerts issued to the organisation for the period<br />
01/02/12 ‐18/02/13”. However, this issue has been addressed by new systems and controls<br />
implemented since 1 October 2012 and all alerts are acknowledged within the expected time frame.<br />
62. Below are the ‘red’ indicators extracted from the latest version of the <strong>Barts</strong> <strong>Health</strong> QRP. These<br />
indicators are a selection which are used to estimate risk with a high number of the 16 Outcomes<br />
18
Table 13: Summary of Red RAG rated items<br />
Indicator information relevant to many Outcomes<br />
Data source Item description Data Value Site<br />
Adult inpatient<br />
survey<br />
Adult inpatient<br />
survey<br />
Adult inpatient<br />
survey<br />
Adult outpatient<br />
survey<br />
2011<br />
Adult outpatient<br />
survey<br />
2011<br />
<strong>NHS</strong> staff<br />
survey2011/12<br />
<strong>NHS</strong> staff<br />
survey<br />
2011/12<br />
<strong>NHS</strong> staff<br />
survey<br />
2011/12<br />
<strong>NHS</strong> staff<br />
survey<br />
2011/12<br />
Respondents stating they waited<br />
more than 5 months to be<br />
admitted from the time they were<br />
first told they needed to be<br />
admitted<br />
Respondents stating they did not<br />
have confidence and trust in the<br />
nurses treating them<br />
Respondents stating that they did<br />
not get enough emotional support<br />
from hospital staff during their stay<br />
Respondents stating they did not<br />
have confidence and trust in the<br />
doctor examining and treating<br />
them<br />
Respondents stating that the main<br />
reason they went to the<br />
Outpatients Department was not<br />
dealt with to their satisfaction<br />
Staff job satisfaction<br />
% of staff experiencing<br />
discrimination at work in the last 12<br />
months<br />
Effective team working<br />
Percentage of staff witnessing<br />
potentially harmful errors, near<br />
misses or incidents in last month<br />
Much worse than<br />
expected<br />
Much worse than<br />
expected<br />
Much worse than<br />
expected<br />
Much worse than<br />
expected<br />
Much worse than<br />
expected<br />
Lowest (worst)<br />
20% when<br />
compared to<br />
other trusts<br />
Highest (worst)<br />
20% when<br />
compared to<br />
other trusts<br />
This trust was in<br />
the lowest<br />
(worst) 20%<br />
when compared<br />
to other trusts<br />
for this key<br />
finding<br />
This trust was in<br />
the highest<br />
(worst) 20%<br />
when compared<br />
to other trusts<br />
for this key<br />
finding<br />
NUH<br />
BLT<br />
NUH<br />
WX<br />
NUH<br />
BLT<br />
NUH<br />
NUH<br />
BLT<br />
NUH<br />
WX<br />
NUH<br />
NUH WX<br />
TB 27/13<br />
19
TB 27/13<br />
RECOMMENDATION<br />
63. The <strong>Trust</strong> <strong>Board</strong> is asked to<br />
Note the contents of the report.<br />
Identify areas that the Quality Assurance Committee should examine further.<br />
Kay Riley<br />
Chief Nurse 26 March 2013<br />
20
Report<br />
to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013<br />
TB 28/13<br />
Title<br />
Sponsoring Director<br />
Author(s)<br />
Purpose<br />
Previously considered by<br />
Finance Report – 2012/13 Monthh 11<br />
Chief Financial Officer<br />
Senior Finance Staff<br />
To providee the <strong>Board</strong><br />
with the <strong>Trust</strong>’s financial performance<br />
report for Month 11 and the key risks to the achievement of<br />
the financial plan for 2012/13.<br />
<strong>Trust</strong> Management <strong>Board</strong>, 9 April 2013<br />
CFO Message<br />
At Month 11 the <strong>Trust</strong> continues to forecast overall breakeven for the year end. This has<br />
been achieved after planned financial support relating to the merger business case and in<br />
year financial support for contract overperformance.<br />
The overall position for patient treatment income shows overperformance on Ambulatory<br />
Care, Paediatrics and Cancerr services, with underperformance on Emergency Care and<br />
Acute Medicine, Cardiovascular, Women’s <strong>Health</strong> and Surgery. The expenditure position<br />
remains<br />
of concern, as all CAGs are overspent against budget. Pay expenditure has<br />
remained largely static acrosss the year, with bank and agency spend s increasing in February<br />
compared to previous months (see tablee 4). The <strong>Trust</strong> is undertaking a specific initiative to<br />
review and improve the controls on variable pay.<br />
The overall CIP achieved in 2012/13 wass in line with the merger FBC, butt below the<br />
more<br />
ambitious target we set ourselves. This is disappointing, and is an unsustainable position<br />
going forward. We<br />
have therefore engaged external consultancy support to help CAGs and<br />
corporate areas to<br />
deliver the<br />
CIPs for 2013/14.<br />
The <strong>Trust</strong>’s capital programme has been revised<br />
down to £41.7m with year‐to‐date<br />
expenditure at £22.6m, £15.6m less than plan. A number of large projects are still at the<br />
pre‐approval stages and the Finance and Investment Committee will bee asked to review r<br />
the capital programme this month aheadd of seeking<br />
<strong>Board</strong> approval in May.<br />
In summary, while<br />
we will achieve ourr overall financial targets for 2012/13, the more<br />
urgent priority is to address the t underlying financial position. This requires a step‐change<br />
in our CIP delivery<br />
and a significant improvement in budgetary control during 2013/ /14, in<br />
order to ensure the <strong>Trust</strong>’s overall strategy and service improvement plans for patients<br />
can be realised.<br />
Mark Ogden, Chief<br />
Financial Officer
TB 28/13<br />
Related <strong>Trust</strong> objectives<br />
6. Deliver the <strong>Trust</strong>’s 2012/13 financial plan, and cost improvement target, and develop a<br />
sustainable long term financial plan (LTFM).<br />
Risk and Assurance<br />
Related Assurance<br />
Framework entries<br />
Legal implications/<br />
regulatory requirements<br />
Key risks to the delivery of the plan<br />
n/a<br />
No direct legal implications identified.<br />
Action required by the <strong>Trust</strong> <strong>Board</strong><br />
The <strong>Trust</strong> <strong>Board</strong> is asked to review and discuss the 2012/13 Month 11 financial<br />
performance, including the key risks identified in this report.<br />
2
TB 28/13<br />
Report Structure<br />
1 Overview of financial Comprehensive Statement of Income. Commentary on income,<br />
performance pay/non‐pay and CAG and corporate performance. Financial risk<br />
rating and summary CIP.<br />
2 Capital expenditure Performance against plan.<br />
3 Cost improvement Performance against plans and commentary on<br />
underachievement.<br />
4 Income Income analysed by sectors (commissioners), point of delivery.<br />
5 Balance sheet Balance sheets since start of the year, aged debt analysis and cash<br />
flows details.<br />
3
TB 28/13<br />
1.0 Overview of Financial Performance<br />
1.1 Comprehensive Statement of Income and Expenditure<br />
Table 1 below summarises the financial position of the <strong>Trust</strong> by income and expenditure<br />
categories and Table 2 shows the position by CAG and Corporate.<br />
Table 1 – Analysis of Income and Expenditure by income/expenditure category<br />
In Month<br />
Year to Date<br />
<strong>Trust</strong> Financial Performance<br />
Year End<br />
February 2013<br />
Budget<br />
£m<br />
Actual<br />
£m<br />
Variance<br />
£m<br />
Budget<br />
£m<br />
Actual<br />
£m<br />
Variance<br />
£m<br />
Budget<br />
£m<br />
Income 104.8 109.8 5.0 1,153.5 1,180.0 26.5 1,264.7<br />
- -<br />
Expenditure<br />
Pay 60.0 61.8 (1.8) 649.9 659.3 (9.3) 715.7<br />
Non-Pay 35.5 41.0 (5.5) 401.9 441.6 (39.7) 439.8<br />
Internal Trading (0.0) 0.0 (0.1) (0.6) (0.4) (0.1) (0.6)<br />
Central Expenditure & Reserves 1.7 (0.0) 1.7 2.5 (0.9) 3.3 6.3<br />
Total Expenditure 97.2 102.8 (5.6) 1,053.8 1,099.6 (45.9) 1,161.2<br />
EBITDA 7.6 6.9 (0.6) 99.7 80.4 (19.3) 103.5<br />
Interest, Tax and Depreciation 8.4 7.7 0.7 92.3 85.1 7.3 101.6<br />
Donated Assets Adjustment 0.2 (0.6) 0.8 1.7 (5.0) 6.7 1.8<br />
Retained Surplus / (Deficit) Before IFRS (1.0) (0.1) 0.9 5.7 0.3 (5.4) 0.0<br />
Included in the non-pay above:<br />
Pass Through Costs - Drugs 3.5 4.8 1.3 40.7 46.9 6.2 44.5<br />
Pass Through Costs - Devices 1.6 1.7 0.1 18.7 18.9 0.2 20.4<br />
CIPs Achieved 6.7 5.1 (1.7) 56.9 42.2 (14.6) 63.3<br />
The <strong>Trust</strong> is showing a small surplus against a year to date target of a £5.7m surplus. There is<br />
a favourable income variance of £26.5m, offset by an adverse operating expenditure<br />
variance of £45.9m. Most of the expenditure variance relates to non‐pay, this is partly on<br />
the costs of drugs, (overspent by £7.1m), clinical supplies (overspent by £8.5m) and an<br />
£8.2m underachievement of non‐pay CIPs.<br />
Interest and depreciation have a favourable variance against budget, mainly due to the<br />
impact on the asset base, of impairments at the Royal London. In addition a donated asset<br />
adjustment is applied, to exclude the impact of donated assets, in the <strong>Trust</strong>’s financial<br />
performance, as required by the Department of <strong>Health</strong>.<br />
4
TB 28/13<br />
Table 2 – Analysis of Income and Expenditure by CAG<br />
I&E by CAG<br />
In Month<br />
Year to Date<br />
Year End<br />
February 2013<br />
Budget<br />
£m<br />
Actual<br />
£m<br />
Variance<br />
£m<br />
Budget<br />
£m<br />
Actual<br />
£m<br />
Variance<br />
£m<br />
Budget<br />
£m<br />
Income<br />
Ambulatory Care 18.9 19.8 0.9 212.0 215.1 3.1 231.5<br />
Cancer Services 4.4 4.9 0.5 50.6 58.0 7.3 55.2<br />
Cardiovascular Services 7.0 6.7 (0.3) 80.8 79.8 (1.0) 88.2<br />
Children's <strong>Health</strong> 4.6 4.7 0.1 54.3 59.0 4.7 59.3<br />
Clinical Support Services 6.4 7.3 0.8 74.8 75.7 0.9 81.6<br />
Emergency Care & Acute Medicine 18.0 18.6 0.5 210.1 207.7 (2.5) 229.3<br />
Surgery 15.3 14.4 (0.9) 175.2 167.9 (7.3) 191.1<br />
Women's <strong>Health</strong> 7.9 7.6 (0.3) 91.8 90.8 (1.0) 100.2<br />
Corporate 5.2 5.6 0.4 52.9 57.5 4.5 57.1<br />
Central Income 17.0 20.3 3.2 150.8 168.7 17.9 171.1<br />
Total Income 104.8 109.8 5.0 1,153.5 1,180.0 26.5 1,264.7<br />
Expenditure<br />
Ambulatory Care 12.8 13.7 (0.9) 142.8 146.6 (3.8) 156.2<br />
Cancer Services 3.6 4.1 (0.5) 38.7 42.9 (4.3) 42.3<br />
Cardiovascular Services 5.3 6.1 (0.8) 58.7 61.8 (3.1) 64.0<br />
Children's <strong>Health</strong> 3.9 4.2 (0.2) 42.9 45.1 (2.2) 46.9<br />
Clinical Support Services 12.0 12.6 (0.6) 134.7 139.6 (4.9) 147.0<br />
Emergency Care & Acute Medicine 13.7 13.8 (0.1) 142.4 148.5 (6.1) 155.3<br />
Surgery 14.1 14.9 (0.9) 142.2 149.9 (7.8) 156.1<br />
Women's <strong>Health</strong> 5.2 5.6 (0.4) 57.4 59.8 (2.4) 62.6<br />
Corporate & Central Expenditure 35.2 35.1 0.1 388.7 386.0 2.8 434.9<br />
Total Expenditure 105.9 109.9 (4.0) 1,148.4 1,180.1 (31.8) 1,265.3<br />
Internal Trading<br />
Ambulatory Care 0.7 0.8 (0.1) 8.5 8.4 0.1 9.3<br />
Cancer Services 0.5 0.7 (0.2) 5.8 6.4 (0.6) 6.3<br />
Cardiovascular Services 0.4 0.3 0.1 4.1 3.9 0.1 4.4<br />
Children's <strong>Health</strong> 0.2 0.2 0.0 1.8 1.7 0.2 2.0<br />
Clinical Support Services (3.4) (3.7) 0.2 (39.8) (39.5) (0.3) (43.6)<br />
Emergency Care & Acute Medicine 0.8 0.9 (0.1) 9.5 9.7 (0.2) 10.4<br />
Surgery 0.6 0.6 (0.0) 6.9 6.7 0.1 7.5<br />
Women's <strong>Health</strong> 0.2 0.2 0.0 2.7 2.2 0.5 3.0<br />
Total Internal Trading (0.0) 0.0 (0.1) (0.6) (0.4) (0.1) (0.6)<br />
Retained Surplus / (Deficit) Before IFRS (1.0) (0.1) 0.9 5.7 0.3 (5.4) 0.0<br />
Table 3 – Analysis of Corporate and Central Expenditure<br />
Corporate & Central Expenditure<br />
In Month<br />
Year to Date<br />
Year End<br />
Budget<br />
£m<br />
Actual<br />
£m<br />
5<br />
Variance<br />
£m<br />
Budget<br />
£m<br />
Actual<br />
£m<br />
Variance<br />
£m<br />
Budget<br />
£m<br />
Chief Executive 0.1 0.2 (0.1) 2.8 3.6 (0.8) 2.9<br />
Development 13.6 14.7 (1.0) 157.1 162.1 (5.0) 176.9<br />
Human Resources 0.6 0.7 (0.2) 6.3 7.5 (1.2) 6.9<br />
Finance 0.8 1.1 (0.3) 9.2 9.8 (0.6) 10.2<br />
Payroll 0.1 0.1 (0.0) 1.1 1.2 (0.1) 1.2<br />
Procurement 0.2 0.2 (0.0) 1.9 2.8 (0.9) 2.1<br />
Strategy 0.2 0.1 0.0 1.6 1.5 0.1 1.8<br />
Medical Director 0.3 0.4 (0.0) 3.6 3.6 0.1 4.1<br />
Chief Nurse 2.5 2.7 (0.2) 29.0 29.6 (0.6) 31.5<br />
Academic <strong>Health</strong> Sciences 4.4 4.4 (0.0) 42.8 42.3 0.5 46.3<br />
Chief Operating Officer 1.5 1.7 (0.2) 20.5 21.4 (1.0) 22.1<br />
Central Income & Expenditure 0.3 -0.2 0.0 2.9 1.1 1.8 3.1<br />
Reserves 1.0 (0.2) 1.3 0.9 (0.2) 1.0 5.5<br />
BLT/NUH/WUH Merger 1.4 1.2 0.2 16.9 14.6 2.2 18.7<br />
Interest 3.0 3.1 (0.1) 32.8 33.3 (0.5) 35.8<br />
Dividends 0.5 0.2 0.4 5.9 2.0 3.9 6.5<br />
Depreciation 4.8 4.4 0.4 53.5 49.7 3.8 59.3<br />
Sub Total 35.2 35.1 0.1 388.7 386.0 2.8 434.9
TB 28/13<br />
In month & YTD performance<br />
Expenditure analysis<br />
Pay expenditure<br />
Actual pay expenditure during month eleven was £61.8m, which is £1.5m higher than<br />
month ten. At month eleven, there was an adverse variance against budget of £1.8m in<br />
month and £9.3m year to date. This was mainly the result of non‐delivery of CIPs, which<br />
continues to demonstrate that pay expenditure is not reducing at a sufficient rate to<br />
deliver the recurrent CIPs. In addition, the Bank and Agency expenditure was at £7m,<br />
which is £1.3m higher than bank and agency spend in the preceding two months.<br />
The run rate of pay expenditure is shown by month in table 4.<br />
Table 4 – Analysis of ‘run rate’ pay expenditure (including bank and agency)<br />
Pay Spend by Month<br />
Apr 2012<br />
£m<br />
May 2012<br />
£m<br />
Jun 2012<br />
£m<br />
Jul 2012<br />
£m<br />
Aug 2012<br />
£m<br />
Sep 2012<br />
£m<br />
Oct 2012<br />
£m<br />
Nov 2012<br />
£m<br />
Dec 2012<br />
£m<br />
Jan 2013<br />
£m<br />
Feb 2013<br />
£m<br />
YTD<br />
Total<br />
£m<br />
Pay Spend<br />
Medical 16.5 15.9 16.4 16.3 16.7 17.0 17.2 17.2 16.7 17.6 17.6 185.2<br />
Nursing & Midwifery 23.5 24.1 23.8 23.5 24.0 24.1 23.7 24.4 23.4 24.6 24.1 263.3<br />
Scientific, Therapeutic & Technical 8.4 8.5 8.2 8.2 8.5 8.2 8.4 8.5 8.8 8.3 8.2 92.2<br />
Directors & Senior Managers 2.8 2.6 2.9 2.7 2.8 2.7 2.8 3.2 3.1 2.8 3.1 31.5<br />
Admin & Clerical 9.3 9.7 6.8 8.4 8.2 6.5 6.5 8.7 7.2 6.9 8.9 87.1<br />
Total Pay Spend 60.5 60.9 58.0 59.1 60.3 58.6 58.6 61.9 59.3 60.3 61.8 659.3<br />
Bank & Agency Spend<br />
Medical 0.5 0.6 0.7 0.8 1.0 0.8 0.9 0.8 0.9 1.1 1.1 9.2<br />
Nursing & Midwifery 3.8 2.9 3.3 2.8 3.4 3.6 3.4 4.3 3.8 3.6 3.6 38.4<br />
Scientific, Therapeutic & Technical 0.3 0.4 0.4 0.3 0.5 0.3 0.3 0.5 0.4 0.3 0.4 4.1<br />
Directors & Senior Managers 0.1 0.1 0.1 0.1 0.1 0.1 (0.0) 0.1 0.1 0.1 0.1 0.9<br />
Admin & Clerical 1.9 3.3 (0.2) 1.3 1.3 (0.4) (0.7) 1.8 0.4 0.6 1.9 11.1<br />
Total Bank & Agency Spend 6.6 7.3 4.2 5.3 6.2 4.3 3.9 7.5 5.7 5.7 7.0 63.8<br />
An analysis of CIP underperformance is included in section 3.<br />
Non‐pay expenditure<br />
In month eleven, expenditure on non‐pay totalled £41m, with an adverse variance against<br />
budget of £5.5m. The spend on drugs and clinical supplies in month was above trend to<br />
date but this reflected the impact of winter pressures activity and working towards<br />
achieving access targets by utilising the private sector for some work. The impact of<br />
unidentified/unachieved CIPs continues to be a factor in continuing non pay overspends.<br />
CAG Expenditure (year to date overspends)<br />
Surgery. The year to date expenditure overspend is mainly on bank and agency, clinical<br />
supplies and non achievement of CIPs.<br />
Ambulatory Care. The year to date expenditure overspend is mainly due to high cost drugs<br />
in Rheumatology and Infection & Immunology.<br />
Cardiovascular. The year to date expenditure overspending is mainly on medical and nursing<br />
staff, clinical supplies and underachieved CIPs.<br />
Clinical Support Services. The year to date overspend is mainly on clinical supplies,<br />
maintenance contracts and the underachievement of CIPs.<br />
ECAM. The year to date expenditure overspend is mainly on nursing and medical staff,<br />
mostly bank and agency and unachieved CIPs.<br />
6
TB 28/13<br />
Women Services. The year to date expenditure overspend is mainly on nursing and medical<br />
staff, and unachieved CIPs<br />
Cancer Services. The year to date expenditure overspend is mainly due to high cost drugs<br />
and unachieved CIPs.<br />
Children’s Services. The year to date overspend is mainly on nursing and medical staff, high<br />
cost drugs and activity related clinical supplies costs.<br />
Control Environment. The controls across the organisation are being improved and in<br />
particular compliance with existing controls and polices. There is a working group<br />
developing and implementing a new approach to the control of variable pay, which has<br />
increased significantly compared to previous years. This is covering:‐<br />
Banning overtime<br />
Improved roster planning and review<br />
Weekly analysis of bank and agency spend<br />
Increasing the bank pool<br />
More senior request and authorisation levels.<br />
There are also a number of unfunded posts, which have been identified at budget setting,<br />
which are being addressed.<br />
In addition, steps are being taken to control non‐pay expenditure. The <strong>Trust</strong> is rationalising<br />
the number of suppliers and driving compliance to ordering from preferred suppliers’ who<br />
have been through a tendering and selection process. Fundamental to this though is the<br />
need to improve the use of the <strong>Trust</strong>’s purchase ordering system.<br />
7
1.2 Key Metrics – By<br />
Month<br />
TB 28/13<br />
The tables below<br />
show the actual income/expenditure per month.<br />
Table 5 ‐ Key Financial Metrics – By Month<br />
Table 6 – Actual Monthly ‘Run Rate’ (£m)<br />
Ref. Category<br />
3. Monthly I& &E<br />
3.1 Incom me<br />
3.2 Pay<br />
3.3 Non Pay - Clinical<br />
3.4 Non Pay - Non Clinical<br />
3.5 Central Support and Reserves<br />
3.6 Interest, Tax and Depreciation<br />
3.7 Surplus / (Deficit)<br />
Type<br />
Apr 20122 May 2012 Jun 20122 Jul 2012<br />
£m £m £m £m<br />
Aug 20122 Sep 2012 Oct 20122 Nov 2012 Dec 20122<br />
£m £m £m £m £m<br />
Jan 2013<br />
£m<br />
Feb 2013<br />
£m<br />
In Month Actual<br />
In Month Actual<br />
In Month Actual<br />
In Month Actual<br />
In Month Actual<br />
In Month Actual<br />
In Month Actual<br />
97.99 60.5<br />
16.9<br />
17.0<br />
(0.3) 8.4<br />
(4.6) 106.1<br />
60.9<br />
19.0<br />
17.8<br />
(0.2)<br />
8.1<br />
0.6<br />
103.4<br />
58.0<br />
18.4<br />
23.4<br />
(0.2) 8.2<br />
(4.4) 108.5<br />
59.1<br />
16.5<br />
23.0<br />
0.7<br />
8.1<br />
1.1<br />
105.6<br />
60.3<br />
17.77 20.9<br />
(0.2) 8.88 (2.0) 101.8<br />
58.6<br />
17.1<br />
18.8<br />
(0.0)<br />
8.3<br />
(1.0)<br />
111.2<br />
58.6<br />
17.77 27.5<br />
(0.6) 8.0<br />
(0.2) 112.9<br />
61.9<br />
20.5<br />
22.2<br />
(0.3)<br />
8.3<br />
(0.3)<br />
106.9<br />
59.3<br />
18.2<br />
19.3<br />
(0.0) (0.3) 10.5<br />
115.8<br />
60.3<br />
19.9<br />
28.6<br />
(0.1)<br />
6.9<br />
0.2<br />
109.8<br />
61.8<br />
18.88 22.22 (0.0) 7.1<br />
(0.1) 1,180.0<br />
659.3<br />
200.8<br />
240.8<br />
(1.3)<br />
80.1<br />
(0.3)<br />
YTD<br />
Total<br />
£m<br />
8
1.3 Financial Risk Rating<br />
TB 28/13<br />
Table 7 – Financial risk rating<br />
Metric<br />
Year End<br />
Plan<br />
Year to<br />
Date<br />
YTD<br />
Rating<br />
Forecast<br />
Outturn<br />
Commentary<br />
EBITDA margin 3 3 ● 3<br />
EBITDA margin is obtained by dividing EBITDA by<br />
total income. The year to date score is in line with the<br />
plan.<br />
EBITDA; % achieved 5 3 ● 5<br />
EBITDA % achieved is calculated by comparing the<br />
actual EBITDA with that planned. The full year<br />
forecast score is in line with the plan.<br />
Return on Assets 2 2 ● 2<br />
Return on Assets is essentially the surplus divided by<br />
average net assets. The year to date score is in line<br />
with the plan.<br />
I&E surplus margin 2 2 ● 2<br />
I&E surplus margin is the <strong>Trust</strong>’s surplus (exclusive of<br />
IFRS IFRIC 12 costs) as a percentage of total<br />
income. The <strong>Trust</strong> would need a 1% surplus in order<br />
to achieve a 3. The current plan is breakeven.<br />
Liquidity 3 2 ● 2<br />
Liquidity is net current assets, excluding inventory,<br />
divided by operating expenses.<br />
Weighted Average 2.8 2.4 ● 2.6<br />
The 5 measures above are subjected to a weighted<br />
average calculation which returns an overall score.<br />
Overall Rating 2 2 ● 2<br />
A score of 3 is mandatory to achieve Foundation <strong>Trust</strong><br />
status.<br />
The financial risk rating provided to our external regulators requires the <strong>Trust</strong> to report all measures on an in year<br />
basis. The <strong>Board</strong> should note that this position is more favourable compared to the underlying situation, which has<br />
required additional non‐recurrent support as part of the merger FBC.<br />
9
TB 28/ /13<br />
2.0<br />
Capital Expenditure<br />
Table 8 – Capital expenditure analysis by site<br />
Table 9 – Capital expenditure analysis by CAG<br />
Capital Plan<br />
The <strong>Trust</strong>’s capital programme has been revised to £41.7m<br />
from the previous plan of £64.6m. This<br />
revised budget represents the outcome of discussions with CAG and Corporate teams to prioritise<br />
schemes for 2012‐13. Year to date spend s is £22.6m, whichh is a £15.6mm underspend against the year to<br />
date plan.<br />
On<br />
a specific scheme basis, the most significant underspends relate to t the following schemes:<br />
Table 10 – Under‐spending capital schemes s<br />
10
Report<br />
to the <strong>Trust</strong> <strong>Board</strong>: 10 Aprill 2013<br />
TB 29/13<br />
Title<br />
Sponsoring Director<br />
Author<br />
Purpose<br />
Previously considered by<br />
<strong>NHS</strong> <strong>Trust</strong> Development Authority 2013/14 Annual Plan<br />
–<br />
Final Submission<br />
Director of Strategy<br />
FT Programme Lead<br />
To note thee final submission of the 2013/14 Annual Plan to the<br />
<strong>NHS</strong> <strong>Trust</strong> Development Authority (NTDA)<br />
FT Project <strong>Board</strong>, 13 March 2013<br />
<strong>Trust</strong> Executive, 2 April 2013<br />
<strong>Trust</strong> Management <strong>Board</strong>, 9 April 2013<br />
Executive summary<br />
This paper sets out<br />
our response to the 2013/14 annual planning requirements in terms of:<br />
1. NTDA requirements.<br />
2. Our 5 April 2013 final submission. s .<br />
3. Key risks.<br />
4. Further work.<br />
Related<br />
<strong>Trust</strong> objectives<br />
Achievement of foundation trust status within agreed timeline. .<br />
Risk and<br />
Assurance<br />
Related<br />
Assurance<br />
Framework entries<br />
Legal implications/<br />
regulatory requirements<br />
See the risks table at paragraph 14. 1<br />
n/a<br />
<strong>Health</strong> and Social Care<br />
Act 2012<br />
Toward High Quality, Sustainable<br />
Services (NTDA), requirement<br />
to submit an annual plan.<br />
Action required:<br />
The <strong>Trust</strong> <strong>Board</strong> is asked to receive the final 2013/ /14 annual plan as submitted to the <strong>NHS</strong><br />
<strong>Trust</strong> Development<br />
Authority on 5 April 2013.
TB 29/13tt TB 29/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING: 10 APRIL 2013<br />
NATIONAL TRUST DEVELOPMENT AGENCY 2013/14 ANNUAL PLAN<br />
INTRODUCTION<br />
1. The ‘Toward High Quality, Sustainable Services’ planning guidance from the <strong>NHS</strong> <strong>Trust</strong><br />
Development Agency (NTDA) sets out the expectations for <strong>NHS</strong> trusts to deliver in the<br />
coming year and how the NTDA will support them to achieve high quality and<br />
sustainable care for the patient and communities they serve. The FT Project <strong>Board</strong><br />
reviewed a detailed second draft submission of the <strong>Trust</strong>’s Annual Plan at their meeting<br />
on 13 March 2013.<br />
2. As was noted during that discussion, the final draft submission was required to be<br />
submitted to the NTDA on 5 April 2013. This submission has been made and this paper<br />
therefore outlines next steps and risk mitigation<br />
3. This planning guidance sets out clear expectations on:<br />
<br />
<br />
<br />
Quality – that agreed CQUIN schemes are delivered in full and the basic<br />
standards on quality are adhered to;<br />
Delivery – that all the core standards are met and that all contracts are<br />
delivered in full;<br />
Sustainability – that all <strong>NHS</strong> trusts show an improvement trajectory for<br />
surpluses and Financial Risk Ratings for 2013/14 linked to their overall medium<br />
to long term financial plans in their Long Term Financial Model.<br />
4. The <strong>Trust</strong> was required to submit a final plan by the 5 April 2013 deadline, responding<br />
to written and verbal NTDA feedback in relation to the 25 January and 7 March draft<br />
submissions. They key components of the plan are:<br />
<br />
<br />
<br />
<br />
Overarching presentation ‐ to capture the narrative on the last year and the<br />
year ahead, set out the key challenges and development needs and the plans<br />
for the year ahead, alongside the areas of variation where improvement is<br />
expected.<br />
Annex A and B – to identify development and improvement priorities for the<br />
coming year.<br />
Annex C, D and E – to present triangulated activity, workforce and finance<br />
plans.<br />
Annex F Planning checklist ‐ to confirm (self‐certify) that we meet key<br />
requirements in relation to quality, financial planning, workforce planning,<br />
CQUINs, QIPP and the FT pipeline. Action plans are required for areas of noncompliance<br />
2
TB 29/13tt TB 29/13<br />
5. Based on the delegated authority provided at the March Foundation <strong>Trust</strong> Project<br />
<strong>Board</strong>, the final submission of the plan was reviewed in detail by the <strong>Trust</strong> Executive on<br />
the 2 April.<br />
6. The <strong>Board</strong> is asked to note that the submitted plan is a final draft and that further<br />
iterations and discussions are expected with the NTDA throughout April. It is<br />
anticipated that a final version, agreed between the <strong>Trust</strong> and the NTDA, will be<br />
available in early May.<br />
7. The robustness of the annual plan will form the basis of the <strong>Trust</strong>’s agreed FT trajectory<br />
with the NTDA, replacing the earlier process of the Tripartite Formal Agreement (TFA).<br />
PROCESS TO DATE<br />
8. <strong>Barts</strong> <strong>Health</strong> submitted an initial annual plan to the NTDA to meet the 25 January 2013<br />
deadline. This plan was still in development, given that our workforce plan (Annex E)<br />
and our improvement and development priorities (Annex A & B) required further work.<br />
9. A second version of the plan was submitted on 7 March including our finance plan<br />
(Annex D) to reflect feedback from the NTDA and to reconcile fully with current<br />
iterations of our CIP plans, workforce and activity plans. We also submitted the<br />
outstanding information from the 25 th January submission (Annex A, B and E).<br />
10. Additional information was also requested from the NTDA on the 28 February and this<br />
was collated and submitted on 7 March 2013. This focussed primarily on<br />
demonstrating improvement plans and trajectories for our key operational<br />
performance targets and clarifying processes for engaging stakeholders in our annual<br />
planning process.<br />
11. A meeting took place between the NTDA and key <strong>Trust</strong> Executives on 19 March and<br />
feedback was provided around the finance and operational performance elements of<br />
the annual plan. Subsequently, additional queries regarding some of the detail behind<br />
quality arrangements have been raised by the NTDA which have been addressed in the<br />
final, submitted version.<br />
12. Significant work has taken place to generate robust and aligned financial, workforce<br />
and activity plans for submission. The 5 April plan incorporated the latest work on the<br />
quantum and phasing of cost improvement plans and all plans have been reviewed by<br />
a small sub‐group to ensure that they read across to each other.<br />
3
TB 29/13tt<br />
TB 29/13<br />
KEY AREAS TO NOTE<br />
13. The <strong>Trust</strong> <strong>Board</strong> is asked<br />
to consider the following:<br />
<br />
<br />
The NTDA has set s out clear expectations on quality, delivery and sustainability<br />
in the planning<br />
guidance. . It needs to be recognised that from itss current<br />
position, <strong>Barts</strong> <strong>Health</strong> has a number of areas where it is challenged in meeting<br />
these expectations.<br />
Specifically the NTDA and commissioners have highlighted:<br />
o The challenging cost improvement<br />
plan for the coming year<br />
o Commissioner supportt and engagement in agreeing a our operating plan is<br />
still at an early stage. At the time of writing, we have not yet agreed our<br />
2013/14 contract. As such, the activity and finance plans which we have<br />
submitted in Annexes C and D remain provisional andd we have not been<br />
able to fully<br />
describe our planning processes for Commissioner QIPPs and<br />
innovation (CQUINs)(<br />
inn the Annex F Planning Checklist.<br />
o Our operational performance, particularly inn relation to A&E waits which<br />
has resulted<br />
in the request for the<br />
submission of improvement trajectories<br />
and action plans to address this area.<br />
We have been prudent inn our responses to thee planning checklist (Annex F).<br />
Where we have<br />
identified actions to ensure compliance in 2013/14 but are not<br />
yet compliant at the timee of submitting our plan, we have recordedd ‘partial<br />
compliance’ and have set out our<br />
planned actions too move towards a<br />
compliant position.<br />
<br />
Our improvement and development<br />
priorities in Annex A & B have been<br />
iterated from the versions seen at the<br />
13 March FT Project <strong>Board</strong> although the<br />
broad themes remain r the same. It is<br />
intended that t these now translate into a<br />
set of formal corporate objectives which the <strong>Board</strong> will review in May<br />
4
TB 29/13tt<br />
TB 29/13<br />
<br />
<br />
<br />
<br />
The <strong>Trust</strong> is planning a £1m<br />
(0.1%) surplus for the financial year 2013/14 on a<br />
turnover of £1,256m. The key financial assumptions are:<br />
Income:<br />
o 1.3% tariff deflator has been applied to all Paymentss by Resultss income.<br />
This is the national standard<br />
o There iss underlying demographic and non‐demographic growth of<br />
£22m which has largely been<br />
recognised in discussions to date along<br />
with decommissioning of activity for £7m.<br />
o We willl agree QIPP (Quality, Innovation, Productivity, Prevention)<br />
deductions where the evidence base is strong andd this is likely to be<br />
around £30m.<br />
o There will be a £7m increasee for counting and coding improvements<br />
and business rules.<br />
o Commissioners will fund £28m tenders and service development<br />
growth in i year.<br />
o Non‐recurrent income will include merger transitional funding of<br />
£23.8m and £18.1m<br />
for PFI and Project Diamond.<br />
Expenditure:<br />
o Inflationn will be 1.8% for pay, 6.5% for drugs, d 2.7% for clinical supplies,<br />
3.1% forr other operating expenses and 5% % PFI inflation.<br />
o We will deliver £77.5m in recurrent CIP savings.<br />
o We will improve itss cost control by £20mm and theree will be no material<br />
unbudgeted expenditure.<br />
o We will have an £32m capital programme.<br />
Delivering the plan will require robust implementation plans, a programme<br />
management approach inn key areas and an unrelentingg focus on<br />
driving<br />
improvement.<br />
5
TB 29/13tt TB 29/13<br />
Wider engagement and communications around the annual plan is still to be<br />
addressed. We need to ensure that the plan is clearly aligned to our other<br />
plans (Integrated Business Plan, clinical strategy work) to ensure that messages<br />
to internal and external stakeholders are consistent). This process will be<br />
supported by the agreement of the set of corporate objectives referred to<br />
earlier.<br />
KEY RISKS<br />
14. The following table summarises the key risks to delivery of the annual plan.<br />
Risk Mitigation Lead<br />
1 Delivery of cost improvement<br />
plan falls short of the financial<br />
challenge.<br />
2 CIP plans require a step<br />
change in delivery on a<br />
monthly basis and failure to<br />
achieve that from month one<br />
will risk the ability to deliver<br />
the financial position.<br />
Focus by executive team. High<br />
quality programme management<br />
and support programme. Early<br />
action on slippage. Short‐term<br />
non‐pay controls to be designed to<br />
reduce spend to ensure the <strong>Trust</strong><br />
remains within the overall budget<br />
within year.<br />
PWC are facilitating discussions<br />
with CAGs to ensure CIP schemes<br />
exist. TX to look at top down<br />
schemes. Additional support posts<br />
from the recovery team to work<br />
with CAGs on design, control and<br />
delivery.<br />
Mark Ogden/<br />
Stephen<br />
Bloomer/ Mark<br />
Cubbon<br />
<strong>Trust</strong> Executive<br />
3 Workforce CIPs will require<br />
lead‐in time to begin realising<br />
savings<br />
4 Delay in agreeing contracts<br />
with commissioners will mean<br />
that activity plans are not set<br />
at the point of submitting the<br />
annual plan.<br />
TX to look at alternative non‐pay<br />
schemes to be brought forward to<br />
keep the integrity of the CIP<br />
profile.<br />
Contracting team are working with<br />
commissioners and working in an<br />
escalated manner. The annual plan<br />
is based on realistic income<br />
assumptions some of which are<br />
already agreed with<br />
commissioners.<br />
Michael Pantlin/<br />
Len Richards<br />
Mark Ogden<br />
6
TB 29/13tt TB 29/13<br />
Risk Mitigation Lead<br />
5 Lack of alignment between the<br />
annual plan and Integrated<br />
Business Plan (IBP) and Long<br />
Term Financial Model (LTFM).<br />
6 Performance improvement not<br />
delivered in line with annual<br />
plan.<br />
7 Annual plan poorly<br />
communicated to and agreed<br />
with key stakeholders and<br />
CAGs.<br />
8 Internal budgetary control<br />
must be improved to ensure<br />
CAGs deliver to budget. This<br />
requires a £20m improvement<br />
across the organisation.<br />
Ongoing reference to annual plan<br />
in IBP and LTFM preparation.<br />
Performance improvement<br />
strategy and underlying processes<br />
to support delivery of identified<br />
priorities and address operational<br />
performance issues.<br />
Communications plan for sharing<br />
annual plan with CAGs and other<br />
stakeholders. Annual plan and<br />
associated activity to be used as<br />
basis for CAG plans.<br />
Control breaches and issues being<br />
highlighted with suggested<br />
solutions. Basic controls at the<br />
front line level being examined<br />
with rectification plans put in<br />
place.<br />
Frances<br />
O’Callaghan/<br />
Stephen<br />
Bloomer<br />
Len Richards<br />
Frances<br />
O’Callaghan/<br />
Adrienne Noon<br />
Len Richards<br />
FUTURE WORK ON THE ANNUAL PLAN<br />
15. The NTDA will review the annual plan with the <strong>Trust</strong> to agree a final plan during April<br />
and that CAG plans support the overall delivery requirements in the <strong>Trust</strong>. Work will<br />
continue on the plan to include:<br />
<br />
<br />
<br />
<br />
Communication of the annual plan to inform CAG plans.<br />
Translation of activity and workforce plans into CAG plans.<br />
Ongoing liaison with commissioners regarding the annual plan and its<br />
implementation.<br />
Alignment of the annual plan to finance, workforce and activity assumptions<br />
underpinning the Integrated Business Plan (IBP) and Long Term Financial Model<br />
(LTFM).<br />
RECOMMENDATION<br />
16. The <strong>Trust</strong> <strong>Board</strong> is asked to receive the final 2013/14 annual plan as submitted to the<br />
<strong>NHS</strong> <strong>Trust</strong> Development Authority on 5 April 2013.<br />
7
TB 29/13tt TB 29/13<br />
Frances O’Callaghan<br />
Director of Strategy 5 April 2013<br />
8
Annual Plan<br />
Overarching presentation<br />
5 April 2013
Purpose<br />
• Stronger together: a reminder why creating <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
was the right decision for the local health and social care economy<br />
• To celebrate our success as <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
• To highlight our progress against our <strong>Trust</strong> objectives<br />
• Demonstrate our approach to our emerging <strong>Trust</strong> strategy and<br />
requirements for FT authorisation<br />
• To ensure a common understanding of the challenges and<br />
developments needs for our journey
Stronger together: our case for change<br />
• The need to sustain performance: health needs are<br />
challenging; people living longer with more complex illnesses, a<br />
diverse and changing population; some of the most deprived and<br />
unhealthiest communities; big health inequalities (17 years’<br />
difference in life expectancy compared to national average).<br />
• Financial challenge: growing population; cost of drugs,<br />
techniques and technology outstripping income; foundation trust<br />
status required; historical deficits; estate investment required; the<br />
need to achieve cost improvement plans to contribute to the <strong>NHS</strong><br />
£20bn efficiency savings over five years.<br />
• The need to improve: patient experience could be much better;<br />
some services are excellent but far too many needed to improve;<br />
the changing face of healthcare. New understanding of best<br />
practice requires a fresh look at services e.g. ensuring senior<br />
doctors are on site for more hours of the day.
Benefits of creating <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
• A healthcare system that is committed to preventing ill-health as<br />
well as providing excellent health care<br />
• Locally accessible, excellent quality, sustainable and<br />
comprehensive health services that are focused on each<br />
individual’s needs<br />
• Better access to high-quality specialist care when it is needed<br />
• Benefits to staff would benefit patients: staff can gain experience<br />
across the whole patient journey; a bigger trust offers more career<br />
progression, retention of staff; being part of the Academic <strong>Health</strong><br />
Sciences Network offers more interesting and rewarding roles for<br />
staff, making recruitment easier e.g. to persistent vacancies
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Changing lives together from 1 April 2012
<strong>Barts</strong> <strong>Health</strong> at a glance<br />
Waltham Forest<br />
Population 270,702<br />
• 1.25 billion turnover<br />
• 15,000 employees<br />
• Serving over one<br />
million people – our<br />
population is growing<br />
faster than London<br />
and national averages<br />
• 15,000 births<br />
• 1,300,000 outpatient<br />
attendances<br />
Hackney<br />
Population<br />
272,906 (includes<br />
City)<br />
City of London<br />
<strong>Barts</strong><br />
Tower<br />
Hamlets<br />
Population 242,618<br />
Whipps Cross<br />
London Chest<br />
Royal London<br />
Mile End<br />
Newham<br />
Newham<br />
Population 333,256
Investing in our community<br />
2012/13 has been an exceptional year of investment across our <strong>Trust</strong>:<br />
• The brand new Royal London hospital became fully operational<br />
• The second phase of the St Bartholomew’s build remains on<br />
schedule with the London Chest hospital services due to move in<br />
2014<br />
• Brand new maternity services opened at Newham Hospital<br />
• Newham Hospital emergency department underwent a £7m<br />
refurbishment ahead of the Olympic and Paralympic Games<br />
• Our merger secured the necessary capital funding for a larger and<br />
refurbished maternity unit at Whipps Cross Hospital and £23m was<br />
invested in a new emergency department<br />
• Newham Hospital received a brand new CT-scanner<br />
• We started offering maternity services from Barking Birth Centre<br />
• <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> was highly commended in the <strong>Health</strong><br />
Service Journal Award in the ‘Workforce’ category for its<br />
Community Works for <strong>Health</strong> programme which aims to boost<br />
local recruitment and retention of key groups of staff
Investing in our people<br />
• Our new structure is based on eight Clinical Academic Groups which<br />
went live on 1 October 2012 alongside the supporting corporate<br />
functions<br />
• A dedicated development programme is underway to ensure we<br />
build our leadership capacity and deliver on the key themes we have<br />
heard from our stakeholders during our merger engagement:<br />
‣ ensuring financial stability for future generations<br />
‣ providing patient choice, bringing care closer to home and<br />
improving patient outcomes<br />
‣ taking our staff on the journey<br />
‣ Improved engagement and communications; and<br />
‣ working in partnership with statutory leaders, public and<br />
private organisations and the wider community
Achievements in our first few months<br />
• Our Clinical Academic Groups went live on schedule<br />
• Our new <strong>Trust</strong> vision to change lives, and our values and<br />
behaviours were developed in partnership with staff, patients and<br />
our partners<br />
• We are investing in our staff with a<br />
new education academy and<br />
dedicated organisational<br />
development team<br />
• Our organisational development<br />
programme has seen us survey all<br />
of our staff to secure a baseline for<br />
improvement, host our first <strong>Barts</strong><br />
<strong>Health</strong> Heroes awards ceremony<br />
reward and develop an emerging<br />
staff reward and recognition<br />
programme
• We have established a Patient and<br />
Public Forum, with members of the<br />
public sitting on our Clinical Academic<br />
Groups from February and a Local<br />
Authority Forum to guide us. Both will<br />
be our base to build our <strong>Board</strong> of<br />
Governors when we attain Foundation<br />
<strong>Trust</strong> status<br />
• We are currently developing our brand<br />
standards to articulate the level of<br />
consistent service that our patients can<br />
expect<br />
• The patient experience is a standing<br />
item in our <strong>Trust</strong> <strong>Board</strong> meetings, with a<br />
patient story shared at each meeting
• We are actively engaged in the Academic<br />
<strong>Health</strong> Sciences and UCL Partners<br />
reviews to improve services to local people<br />
• Our public health strategy was launched in<br />
August and our Community Works for<br />
<strong>Health</strong> employment team were highly<br />
commended at the HSJ awards<br />
• Shortly we will be launching our innovative<br />
Integration Performance Framework based<br />
on four premises: what do our patients,<br />
staff, partners and regulators think of us?<br />
In time we will be able to report this down<br />
to each service we offer
• Recognised as a leading <strong>Trust</strong><br />
nationally in Standardised Hospital<br />
Mortality (SHMI) one of the key<br />
recognised indicators on the quality of<br />
care that hospitals provide<br />
• Hyper Acute and Acute Stroke Unit<br />
recognised as best organised in Royal<br />
College of Physicians national audit<br />
• First London <strong>Trust</strong> to be awarded the<br />
prestigious Baby Friendly Initiative<br />
accreditation by UNICEF to promote<br />
and sustain breastfeeding in both<br />
hospital and community settings
What we have achieved in Year 1<br />
Changing lives
Objective<br />
Our outcomes<br />
Deliver minimum national<br />
standards set out in our<br />
Operating Framework<br />
including A&E, 18 weeks<br />
RTT, cancer access and<br />
MRSA<br />
Lead Executive:<br />
Chief Operating Officer<br />
<strong>Trust</strong> Objectives 12/13<br />
• The <strong>Barts</strong> <strong>Health</strong> Standardised Hospital Mortality (SHMI) continues<br />
to indicate ‘better than expected’ comparative performance and we<br />
are in the top ten in the country.<br />
• MRSA bacteraemia – the <strong>Trust</strong>’s year to date total is 11, three<br />
above the <strong>Barts</strong> <strong>Health</strong> combined target of 8<br />
• Clostridium Difficile – year to date total is 68. Performance remains<br />
within the monthly and end of year trajectories.<br />
• Targeted infection prevention and control training continues as a<br />
key improvement priority objective, e.g. Non Aseptic Non-Touch<br />
Technique training is now being rolled out at both Newham and<br />
Whipps Cross Hospitals.<br />
• Stop and Wash social marketing campaign across the <strong>Trust</strong><br />
• Agreed internal <strong>Barts</strong> <strong>Health</strong> divert process with the London<br />
Ambulance Service<br />
• Recruitment to a full consultant establishment at WX for the first<br />
time in at least three years<br />
• Demonstrable reduction in grade 3 and 4 pressure ulcers<br />
• We continue to miss 62 day cancer wait targets but we have a<br />
clear improvement plan in place.
Objective<br />
Our outcomes<br />
Achieve the three quality<br />
improvement priorities to<br />
keep patients better<br />
informed about their care,<br />
to improve feedback given<br />
to staff whey they raise<br />
quality and safety<br />
concerns, and to improve<br />
our patient administration<br />
systems<br />
Lead Executive:<br />
Chief Nurse / Medical<br />
Director / Chief Operating<br />
Officer<br />
• The Outpatient Transformation <strong>Board</strong> is reviewing patient letters<br />
and information<br />
• All <strong>Barts</strong> <strong>Health</strong> staff (15,000) have been invited to participate in<br />
the staff survey<br />
• CRS upgrade at three of our six hospitals<br />
• Working with primary care to integrate some of our electronic<br />
patient records<br />
• Patient literature review underway<br />
• Revised interpreting and advocacy arrangements<br />
• Friends and Family Test phased roll out from December 2012<br />
• We are launching our Caring and Compassionate Campaign on 8<br />
March 2013<br />
• We have a Quality Collaborative underway across the <strong>Trust</strong><br />
• Our <strong>Trust</strong> <strong>Board</strong> dedicates the first hour of its business every<br />
month to hear a patient story<br />
• Since the establishment of our CAG structure our senior nurses<br />
have undertaken Clinical Friday where they are all in uniform and<br />
working on the wards across the <strong>Trust</strong>. This is complemented by<br />
the First Friday of the month when all <strong>Barts</strong> <strong>Health</strong> leaders are<br />
visible throughout our hospitals.
Objective<br />
Our outcomes<br />
Implement a plan to improve<br />
patient experience and<br />
satisfaction, including a focus on<br />
outpatients appointments<br />
Lead Executive:<br />
Chief Nurse /Chief Operating<br />
Officer<br />
• The Outpatient Transformation <strong>Board</strong> led by a CAG Group<br />
director is reviewing all patient letters and literature<br />
• A Patient Forum has been established to represent patient<br />
views, reporting directly to the <strong>Trust</strong> Management <strong>Board</strong>.<br />
• Patient representatives are sitting on each of our CAG<br />
<strong>Board</strong>s<br />
• We have built closer relationships with the local BME media<br />
to promote health messages and we are now producing<br />
bilingual press releases<br />
• We have created a new Bilingual <strong>Health</strong> Advocacy and<br />
Interpreting Service (BHAIS) to provide patients, relatives<br />
and carers with easy access to translators, sign language<br />
interpreters and support those with learning disabilities<br />
• Newham Language Shop provides us with a 24/7<br />
interpreting telephone service<br />
• We work closely with all of our Local Involvement Networks<br />
and look forward to working with <strong>Health</strong>watch
Objective<br />
Our outcomes<br />
Implement a plan for improved<br />
communication and joint working<br />
with GPs<br />
Lead Executive:<br />
Medical Director<br />
• <strong>Barts</strong> <strong>Health</strong> has a director of primary care and two<br />
associate directors, all of which are GPs in our local area to<br />
act as a link with primary care<br />
• Monthly quality review meetings are undertaken in each of<br />
our boroughs<br />
• Quarterly general meetings are coordinated in every<br />
borough and used as networking events<br />
• We have hosted two GP / consultant dinners to build<br />
relationships<br />
• We attend CCG and LMC meetings regularly throughout the<br />
year<br />
• CCGs and <strong>Barts</strong> <strong>Health</strong> are actively engaged in the<br />
Integrated Care agenda with local authority partners<br />
• We are working on a joint ICT system to share patient<br />
records<br />
• A GP specific section has been developed for our new <strong>Trust</strong><br />
website and we have a monthly GP News publication<br />
• <strong>Barts</strong> <strong>Health</strong> also has a public health team who regularly<br />
engage with primary care.
Objective<br />
Our outcomes<br />
Deliver Transforming Community<br />
Services objectives for three<br />
improvement areas in Tower<br />
Hamlets<br />
Lead Executive:<br />
Chief Operating Officer<br />
• Improving care for children with long-term conditions at<br />
home following discharge and improving the coordination of<br />
care for children<br />
• Continuing to reduce unnecessary referrals where care can<br />
be provided in the community and in primary care<br />
• Improving pathways in specific care pathways such as<br />
obesity and incontinence<br />
• Complex children’s community services will be moved into<br />
the Children’s CAG from April 2013<br />
• Launched consultation with staff and stakeholders in<br />
February 2013 into a delivery model for the integrated care<br />
programme for frail elderly<br />
• Developing how we share patient information across the<br />
care pathway through improved informatics<br />
• Establishing a strategic partnership group to agree a joint<br />
vision, system objectives and support joint working on end<br />
of life care.<br />
• Taking part in "Communicate My Care" - a system which<br />
allows clinicians ease of access to care plans and patient<br />
preferences
Objective<br />
Our outcomes<br />
Provide an environment that<br />
supports staff to embed the<br />
<strong>Trust</strong>’s values<br />
Lead Executive:<br />
Development Director<br />
• All of our 15,000 staff were surveyed in order to have a<br />
benchmark results for our first year; this information can be<br />
cut by professional group, CAG and hospital etc<br />
• Our staff developed our vision and values, with 1500 taking<br />
part in shaping these and our behaviours<br />
• We hosted our first <strong>Barts</strong> <strong>Health</strong> Heroes Awards in January<br />
2013 after a campaign across the <strong>Trust</strong> celebrating individuals<br />
and teams that embody our <strong>Trust</strong> values and behaviours<br />
• Our OD team is developing a leadership development<br />
programme (360 appraisals have commenced for our top<br />
250); we have a new <strong>Trust</strong> wide appraisal process launching<br />
in April 2013 – this will include a talent management<br />
approach; and we have a ‘you said, we did’ campaign in the<br />
making, matching our staff and patient survey results<br />
• We have a full embedding programme for our OD<br />
programme, working with leaders throughout the organisation<br />
to empower their staff.
Objective<br />
Our outcomes<br />
Deliver the <strong>Trust</strong>s 2012/13<br />
financial plan, and cost<br />
improvement target, and<br />
develop a sustainable long term<br />
financial plan (LTFM)<br />
Lead Executive:<br />
Chief Financial Officer / Chief<br />
Operating Officer<br />
• Our new finance team is now completely in place after a<br />
lengthy recruitment process to find the very best staff<br />
• We have integrated our legacy <strong>Trust</strong> financial teams and<br />
reconciled the <strong>Trust</strong> budgets into a single <strong>Barts</strong> <strong>Health</strong> ledger<br />
• We have leveraged major non-pay savings e.g. £1m on<br />
cardiac implants, £750k on hip and knee joints.<br />
• £50m in efficiency savings have been made in 2012/12<br />
• We are forecasting to breakeven for 2012/13<br />
• 120 management and administrative posts have been made<br />
redundant in this year<br />
• Our efficiency savings target for 2013/14 is £77.5m with<br />
similar annual requirements going forward<br />
• The <strong>Trust</strong> is current going through a robust challenge session<br />
with our CAGs to ensure we have CIP schemes that will<br />
deliver in 13/14, including Independent Assurance Panels,<br />
consisting of peers.
Objective<br />
Our outcomes<br />
Develop service line<br />
management, ownership and<br />
capability through Clinical<br />
Academic Group (CAG)<br />
structures<br />
Lead Executive:<br />
Chief Operating Officer / Chief<br />
Financial Officer<br />
• We have an established Clinical Academic Group (CAG<br />
structure) which went live on 1 October 2012.<br />
• Each CAG is led by a Group Director, Operations Director<br />
and a Director of Nursing and Governance<br />
• Clinical Directors have been appointed across all specialties<br />
• Our teams work across <strong>Barts</strong> <strong>Health</strong> and the six hospitals that<br />
we operate.<br />
• Each of the CAGs has a central location within one of our<br />
hospitals who also provide leadership alongside their<br />
deputy/associate chief operating officer and deputy/associate<br />
chief nurse colleagues<br />
• Service line reporting is being rolled out across the <strong>Trust</strong><br />
• We have developed an Integrated Performance Framework<br />
based on four quadrants: What our patients, staff, partners<br />
and regulators think of us. Each speciality will have a monthly<br />
report but can review the information on a daily basis if<br />
necessary.<br />
• Each CAG is subject to a monthly performance review.
Objective<br />
Our outcomes<br />
Deliver the post-merger<br />
integration plan including the<br />
clinical due diligence action plan<br />
and corporate and clinical<br />
services management<br />
integration<br />
Lead Executive:<br />
Development Director<br />
• Our integration plans are complete at the end of 31 March<br />
2013 when we move into our service improvement phase.<br />
• The actions from our merger clinical due diligence review<br />
have now all been closed or are being taken forward in our<br />
service improvement programme, care quality collaborative or<br />
are now part of our mainstream priorities.<br />
• We are also working with all staff to implement the Francis<br />
Review recommendations and to engage with our 15,000<br />
strong workforce<br />
Prepare a growth plan for<br />
clinical trial take-up and an<br />
ambitious but realistic growth<br />
plan for R&D income<br />
Lead Executive:<br />
Director of Academic <strong>Health</strong><br />
Sciences<br />
• We have increased the numbers of patients participating in<br />
NIHR adopted research by 10%<br />
• We have increased the numbers of active researchers by<br />
over 10%<br />
• We have increased externally funded research project<br />
expenditure by over 5%<br />
• Strong commercial clinical trial activity has been developed to<br />
support local and national wealth creation<br />
• We are founder members of UCL Partners Academic <strong>Health</strong><br />
Sciences Centre and have helped shape the new network.<br />
• We have been working hard with our local communities since<br />
October 2012 to demystify and explain the importance of<br />
clinical trials, and to get patient input into trial design.
Objective<br />
Our outcomes<br />
Agree a Foundation <strong>Trust</strong><br />
authorisation trajectory and<br />
achieve all milestones<br />
Lead Executive:<br />
Director of Strategy<br />
• We have just appointed to our FT programme Lead who will<br />
join <strong>Barts</strong> <strong>Health</strong> in April 2013<br />
• We intend to enter the formal FT progress in October 2013<br />
with a view to authorisation in April 2016, if not before<br />
• We are in active discussions with the NTDA about our<br />
timescale for authorisation and milestones<br />
• We are already making good progress against many of the<br />
elements required to achieve FT status<br />
Develop a comprehensive<br />
strategy for <strong>Barts</strong> <strong>Health</strong><br />
Lead Executive:<br />
Director of Strategy<br />
• The <strong>Barts</strong> <strong>Health</strong> <strong>Board</strong> reviewed our emerging strategy at<br />
our <strong>Board</strong> meeting in February<br />
• All of our CAGs have engaged in this process: fact,<br />
judgement, choice. We have completed phase one of our<br />
process and our clinical leaders are now making their<br />
judgement on their strategic directions. Our <strong>Trust</strong> <strong>Board</strong><br />
receives monthly updates through out FT Project <strong>Board</strong> and<br />
we have an established FT Executive committee and an FT<br />
Working Group to support our journey
Objective<br />
Our outcomes<br />
Agree a commercial strategy<br />
and property development<br />
programme<br />
Lead Executive:<br />
Development Director<br />
• An appointment has just been made to the position of director<br />
of redevelopment<br />
• Progress on our property development programme requires<br />
our <strong>Trust</strong> strategy to be defined<br />
• This portfolio will now be led by the Executive Director of<br />
Strategy<br />
• We have started conversations with the London Borough of<br />
Tower Hamlets over our joint vision for the Whitechapel area,<br />
where the Royal London is located.<br />
• The St Bartholomew’s phase two development is progressing<br />
well and we have an agreement in principle with UCLH to<br />
move the Heart Hospital to be located with the London Chest<br />
on this site in 2014 (subject to consultation and regulatory<br />
approvals)<br />
• We have a maternity capital investment programme underway<br />
at Whipps Cross Hospital, which will also support the<br />
implementation of <strong>Health</strong> for north east London
Quality Objectives 12/13<br />
Quality Objectives<br />
1. To keep patients (and their carers) better informed about their care and treatment,<br />
so that they feel safe and involved before and after they leave the hospital, and<br />
able to make informed choices.<br />
2. To improve the feedback given to staff when they report and raise quality and<br />
safety concerns.<br />
3. To improve our patient administration systems, with a focus on the quality<br />
standard and timeliness of letters and discharge summaries that we send to GPs.<br />
We will continue to work in partnership with GPs to deliver a high quality clinical<br />
service with the best possible outcome for every patient
Quality Objective One 2012/13<br />
To keep patients (and their carers) better informed about their care and treatment, so that they<br />
feel safe and involved before and after they leave the hospital, and able to make informed<br />
choices.<br />
Outcomes to date<br />
• Patient literature review underway<br />
• Revised interpreting and advocacy arrangements<br />
• Friends and family test phased roll out from December 2012<br />
• We are launching our Caring and Compassionate Campaign on 8 March 2013<br />
• We have a Quality Collaborative underway across the <strong>Trust</strong><br />
• Our <strong>Trust</strong> <strong>Board</strong> dedicates the first hour of its business every month to hear a patient story<br />
• Since the establishment of our CAG structure our senior nurses have undertaken Clinical<br />
Friday where they are all in uniform and working on the wards across the <strong>Trust</strong>. This is<br />
complemented by the First Friday of the month when all <strong>Barts</strong> <strong>Health</strong> leaders are visible<br />
throughout our hospitals.<br />
• Intentional rounding – a check of the basic care needs of every patient every one to two<br />
hours. We are delivering this already across all of our wards – but we need to ensure that<br />
we do this consistently and to the same standards
Quality Objective Two 2012/13<br />
To improve the feedback given to staff when they report and raise quality and safety concerns.<br />
Outcomes to date<br />
• Since the establishment of our CAG structure our senior nurses have undertaken Clinical<br />
Friday where they are all in uniform and working on the wards across the <strong>Trust</strong>. This is<br />
complemented by the First Friday of the month when all <strong>Barts</strong> <strong>Health</strong> leaders are visible<br />
throughout our hospitals.<br />
• Clinical Safety Net – this measurement tool supports our senior sisters and charge nurses<br />
to see how issues such as changes to staffing levels affect quality indicators (e.g. pressure<br />
ulcers, falls, and needle stick injuries). This information allows senior staff to gauge how<br />
safe their environment is and to escalate concerns.<br />
• All <strong>Barts</strong> <strong>Health</strong> staff (15,000) have been invited to participate in the staff survey and local<br />
teams are being empowered to question behaviours which are not in line with those<br />
agreed for <strong>Barts</strong> <strong>Health</strong> as well as supporting them to improve our engagement throughout<br />
the organisation
Quality Objective Three 2012/13<br />
To improve our patient administration systems, with a focus on the quality standard and<br />
timeliness of letters and discharge summaries that we send to GPs. We will continue to work<br />
in partnership with GPs to deliver a high quality clinical service with the best possible outcome<br />
for every patient<br />
Outcomes to date<br />
• The Outpatient Transformation <strong>Board</strong> is reviewing patient letters and information<br />
• We have had a major CRS upgrade at three of our six hospitals, with further upgrades<br />
planned across <strong>Barts</strong> <strong>Health</strong> in the next year<br />
• We are working with primary care to integrate some of our electronic patient records<br />
• We meet primary care colleague on a monthly basis to discuss issues and we have a<br />
dedicated primary care team who liaise with our partners on a daily basis.
Our plans for the future<br />
Changing lives
<strong>Trust</strong> objectives 13/14<br />
Our <strong>Trust</strong> objectives for 13/14 are currently being considered but have<br />
not yet received <strong>Board</strong> approval.
Quality Priorities 13/14<br />
Our <strong>Trust</strong> objectives for 13/14 are currently being considered and are awaiting <strong>Board</strong><br />
approval.<br />
It is expected that these will build on our 12/13 priorities in the following areas:<br />
Have Free Care within all our wards and departments<br />
A quality improvement intervention via a single methodology – The Care Quality<br />
Improvement Collaborative (QIC). The areas this will cover are:<br />
• Falls Improvement<br />
• Pressure Ulcer Improvement<br />
• Acutely Ill (deteriorating patients)<br />
• MRSA/C Diff<br />
• Surgical safety Improvement to reduce the incidence of surgical related never<br />
events<br />
To ensure the patients gets to the right place, first time (lost patient)<br />
• Reviewing the length of stay, via the <strong>Health</strong> Care Program . Defined metrics will<br />
be agreed, aligned to best practice, benchmarking data and monitored.
Quality Priorities 13/14 continued…<br />
Executive use of the SHMI<br />
• To establish effective mortality review systems, to ensure learning is shared<br />
and practice is evidence based.<br />
Improving Standards of Care for older people via the Older Peoples Program<br />
• This program is to encompass mental <strong>Health</strong> Care and Learning Disabilities<br />
Improvement.<br />
Patient experience<br />
• To improve patient experience, enhance communication to families and carers<br />
about their care. To enhance the actual giving of care to our patients, providing<br />
care with dignity and compassion via the Care Campaign<br />
Staff engagement<br />
• To improve staff engagement and develop a culture whereby every individual<br />
is valued and understands how they can improve quality of care, and that<br />
when staff do raise concerns about quality and safety they are listened to and<br />
we are open and transparent in the lessons that are learnt
How we will deliver a <strong>Barts</strong> <strong>Health</strong> Strategy<br />
• It is acknowledged that a <strong>Trust</strong> wide strategy needs to be<br />
embedded in our operational model, and it has been agreed that<br />
all service lines will need to engage in the strategy process over<br />
the next 12 months. To enable this, numerous conversations have<br />
taken place with clinical leaders and will continue over the coming<br />
months.<br />
• All service lines are being asked to commit to brand standards of<br />
excellence: all services have an opportunity to be involved in their<br />
development through their clinical and CAG leaders.<br />
• A first draft of our emerging strategy was shared with our <strong>Board</strong> in<br />
February 2013. We will shortly be writing to our partners to ask for<br />
their input.
How we are approaching our strategy development<br />
Changing lives<br />
An academically based health system<br />
delivering excellent clinical outcomes and health improvement<br />
Values<br />
▪ Caring and Compassionate<br />
▪ Listening and understanding<br />
▪ Working together to achieve<br />
ambitious results<br />
▪ Improving and Innovating<br />
▪ Valuing every member of staff<br />
Strategic<br />
initiatives<br />
3<br />
Selected clinical<br />
distinctiveness<br />
4 5 6 7<br />
Integrated care Population<br />
health<br />
Research<br />
excellence<br />
Teaching and<br />
training<br />
excellence<br />
Foundations<br />
to become a<br />
successful FT<br />
1 Brand standards: Consistently excellent quality and delivery<br />
2<br />
Clinical and financial sustainability, enabled by SLR (achieved via basic cost<br />
management & CIPs, commercial and partnership opportunities, service redesign)<br />
Strategic enablers<br />
a. <strong>Board</strong> and quality governance<br />
b. Clinical Leadership<br />
c. Informatics and Systems<br />
d. HR, OD & Workforce<br />
e. Performance management<br />
f. Estates optimisation
Introduction to selected distinctiveness: <strong>Barts</strong> <strong>Health</strong> thinks<br />
about its portfolio of services as falling into three broad categories<br />
All services need to meet<br />
brand standards on<br />
▪ Quality, Safety and Patient Experience<br />
▪ Delivery and Operational efficiency,<br />
including finances<br />
▪ Basic research and teaching<br />
▪ Staff and patient engagement<br />
Brand standard<br />
performers<br />
One or two globally<br />
acknowledged truly<br />
distinctive service lines, that<br />
bring International renown<br />
and acclaim for <strong>Barts</strong> <strong>Health</strong><br />
along the dimensions of<br />
▪ Reputation and Recognition<br />
▪ Research power<br />
▪ Excellence in Teaching and<br />
Training<br />
▪ World class infrastructure and<br />
investment levels<br />
Deep local<br />
impact, nationally<br />
acclaimed, world<br />
class<br />
World<br />
leading<br />
A subset of services<br />
which excel on all the brand<br />
standards and also<br />
▪ Are critical to addressing<br />
local population needs<br />
▪ Have significant<br />
opportunity to develop a<br />
nationally distinctive<br />
profile within <strong>Barts</strong><br />
<strong>Health</strong>, through<br />
partnerships<br />
▪ Have healthy current<br />
and future scale and<br />
margins
Service improvement programme approach<br />
Our service improvement approach is currently being refined and has<br />
not yet received <strong>Board</strong> approval.
Our approach to Cost Improvement<br />
• We have a clear approach established to ensure that we deliver on<br />
our cost improvement programme for 2013/14<br />
• We need to achieve a CIP of 6.5%, equating to £77.5m next year<br />
and going forward<br />
• Our CAG teams are working on the detail of our programmes with<br />
support of our corporate services<br />
• We will have a detailed programme management approach to<br />
enable delivery<br />
• Our control systems are also being firmed up to ensure that we<br />
have a firm grip across the organisation to ensure CIP delivery and<br />
efficiency whilst maintaining high quality levels of care.
The challenge ahead<br />
• Our merger was only one step in the right direction and we knew<br />
we would still need to work hard to improve services, reduce<br />
health inequalities and would have to find the same efficiencies<br />
over the next five years or attract more income or funding.<br />
• We are almost through the first year of our roadmap: integration<br />
and we have delivered on our ambitions.<br />
• In our merger full business case we outlined year two as a focus<br />
on service improvement, and delivery of our clinical and patient<br />
experience improvements and financial benefits of our merger. To<br />
enable this we have an established leaders forum, clear<br />
expectations regarding cost improvement plans and an emerging<br />
<strong>Trust</strong> strategy.<br />
• Year three and beyond will be our transformation stage including<br />
larger scale pathway redesign information by our finalised <strong>Trust</strong><br />
strategy.
Our merger five year plan…<br />
In our merger full business case we outlined the following outcomes<br />
that we intend to achieve within five years:<br />
• Achieving among the lowest rates of hospital mortality<br />
• Achieving among the lowest rates of defects and hospital<br />
associated harm in the <strong>NHS</strong><br />
• Being a quality leader among <strong>NHS</strong> <strong>Trust</strong>s – consistently among<br />
the highest ranking in national quality indicators and top<br />
performers in national patient surveys<br />
• Being the employer of choice for staff, supporting their health and<br />
wellbeing and helping them to thrive in their work<br />
• Achieving authorisation as a <strong>NHS</strong> Foundation <strong>Trust</strong><br />
…these remain our focus.
Annex A – Improvement priorities<br />
Annex A – improvement priorities<br />
Deliver a reliable Patient Administration System<br />
Engage staff in the pursuit of high quality, compassionate services, as demonstrated by an improvement in the staff<br />
survey results<br />
Enhance the patient experience, as demonstrated by a significant improvement in the patient survey results<br />
Drive consistency of clinical practice across the sites levelling up to the “best in <strong>Barts</strong> <strong>Health</strong>”<br />
Achieve all the performance and quality standards set out by our regulators, commissioners and set out in our<br />
annual Quality Priorities<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> – Annex A – Improvement priorities v3.2 draft 5 April 2013
Annex B – Development priorities<br />
Annex B – development priorities<br />
Develop joined up informatics systems<br />
Strengthen capacity and capability at all levels within the organisation<br />
Working with partners to improve population health and reduce inequalities<br />
Develop an innovative Integrated Care model to improve care for the local population<br />
Develop a <strong>Barts</strong> <strong>Health</strong> improvement system<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> – Annex B Development priorities – v3.2 draft 4 April 2013
Financial Briefing<br />
2013/14 Annual Plan<br />
<strong>Trust</strong> <strong>Board</strong><br />
10 th April 2013
Purpose of the Briefing<br />
The briefing is based on a briefing given to the <strong>Trust</strong><br />
Development Agency and explains the annual plan moving from<br />
the outturn of 2012/13 to the submitted plan covering the key<br />
financial assumptions and areas of risk.<br />
2
2012/13 forecast outturn to underlying position<br />
The trust 2012/13 outturn<br />
The <strong>Trust</strong> will achieve a break-even position<br />
The trust will have an underlying<br />
deficit of £46m at the end of<br />
2012/13 (3.9% of income)<br />
The 2012/13 underlying position<br />
excludes £101.7m non-recurrent<br />
income and £50.5m nonrecurrent<br />
expenditure<br />
The <strong>Trust</strong>’s underlying deficit has deteriorated from £11m to £46m during<br />
2012/13 (a £35m deterioration) mainly due to:<br />
1) Changes in SLA activity levels. Our lead commissioners have recently<br />
agreed to a higher recurrent activity and income baseline in 2012/13 mainly<br />
due to failed commissioner QIPP and increased non-elective activity.<br />
Although this income has not been fully paid for in 2012/13 due to our block<br />
contract arrangements, this is the revised income and activity starting<br />
position for 2013/14 SLA negotiations.<br />
2) Changes in planning assumptions, e.g. 1% coding benefit not achieved<br />
3) Material reliance on transitional funding to deliver the in-year position<br />
4) The trust set a challenging CIP program for 2012/13 to mitigate cost<br />
pressures and changes in planning assumptions. The actual forecast<br />
c£40m recurrent CIP delivery is marginally less than the £45m (3.9%)<br />
recurrent CIP assumed in the FBC LTFM<br />
The £101.7m non-recurrent income comprises of:<br />
£10.5m Agreed additional commissioner support<br />
£49.4m FBC merger funding<br />
£18.8m <strong>NHS</strong> Bank PFI transitional funding<br />
£ 9.2m Project Diamond (excluding MFF)<br />
£ 8.3m Additional income related to the cost of PDC cash support<br />
£ 5.5m Financial support to cover one-off year end expenditure pressures<br />
The £50.5m non-recurrent expenditure comprises of:<br />
£16.9m Merger costs<br />
£18.6m <strong>NHS</strong> Bank PFI transitional costs<br />
£10.5m Excessive use of bank and agency<br />
£ 4.5m Additional asbestos provision<br />
The underlying position has also been adjusted for the £7.8m CIP delivered<br />
non-recurrently in 2012/13 and an £8.7m full year effect benefit generated by<br />
the pay spend reduction program.<br />
3
Bridge 3: 2012/13 forecast outturn to underlying position<br />
4
4: 2013/14 Income and Expenditure plan<br />
5
4: 2013/14 Income and Expenditure plan –<br />
Income Assumptions<br />
Key income assumptions • 1.3% national tariff deflator<br />
• £22m SLA growth (demographic and nondemographic)<br />
• (£30m) commissioner led QUIPP and productivity<br />
schemes<br />
• (£7m) commissioner decommissioning deduction<br />
• £7m counting and coding improvements and business<br />
rules impact<br />
• £28m other growth (tenders and service<br />
developments)<br />
• There will not be a material PbR gain or loss from the<br />
2013/14 tariff or grouper<br />
• Non-recurrent merger transitional funding of £23.8m<br />
• Non-recurrent other income of £18.1m (PFI and Project<br />
Diamond)<br />
Total income includes £42m of nonrecurrent<br />
income<br />
SLA growth and coding gains are<br />
necessary to keep the cost savings target<br />
at 6.5%<br />
The £42m non-recurrent income comprises of £23.8m<br />
merger funding and £9.2m <strong>NHS</strong> Bank PFI support, both in<br />
line with the merger FBC and Project Diamond income of<br />
£9.0m (2012/13: £9.2m).<br />
SLA growth includes income for additional activity from<br />
demographic growth, service developments in renal and<br />
additional pass-through drugs income.<br />
6
4: 2013/14 Income and Expenditure Plan –<br />
Income Assumptions<br />
There are significant risks in our plan due<br />
to uncertainty around commissioner QIPP<br />
(demand management and<br />
decommissioning)<br />
Our lead commissioners have indicated an annual SLA<br />
QIPP/demand management pressure of £100m which is<br />
20% reduction. Our 2013/14 draft plan assumes total SLA<br />
demand management and decommissioning of £37m.<br />
This is broadly in line with the £36m planned<br />
commissioner QIPP in 2012/13. Further work is required<br />
with commissioners to understand the reasonableness<br />
and robustness of their proposed £100m QIPP target for<br />
2013/14. The trust cannot accept any demand<br />
management plans without robust evidence and<br />
milestones for delivery. Evidence in 2012/13 is that<br />
demand is not being managed, particularly at Whipps<br />
Cross and The Royal London sites. SLA discussions with<br />
commissioners are on-going and may require arbitration if<br />
a satisfactory agreement cannot be reached.<br />
7
4: 2013/14 Income and Expenditure Plan -<br />
Expenditure Assumptions<br />
Key expenditure assumptions • 1.8% pay inflation (incremental drift and wage<br />
inflation)<br />
• 6.5% drug inflation<br />
• 2.7% clinical supplies inflation<br />
• 3.1% other operating expenses inflation<br />
• 5% PFI inflation<br />
• £77.5m CIP savings requirement<br />
• No material unbudgeted expenditure<br />
• £25m capital expenditure<br />
Total expenditure includes £16.1m of nonrecurrent<br />
spend<br />
The overall expenditure decrease of £4.9m<br />
includes increases for inflation in line with<br />
<strong>NHS</strong> national planning guidance, offset by<br />
planned cost savings target of £77.5m<br />
The plan assumes £16.1m non-recurrent<br />
expenditure comprising of £10.1m FBC merger<br />
transition costs and £6.0m <strong>NHS</strong> Bank PFI transition<br />
costs, both in line with the FBC.<br />
Identification and implementation of CIPs is being<br />
led by the trust PMO supported by PwC. Work to<br />
date has identified around £100m of savings<br />
opportunities. The trust will embed CIP schemes<br />
directly into agreed budgets and workforce planning.<br />
The trust has been playing ‘catch up’ during 2012/13<br />
because of the lack of identified schemes at the start<br />
of 2012/13. Clinical engagement through the CAGs<br />
has been strengthened and will be much stronger<br />
than in 2012/13.<br />
8
4: 2013/14 Income and Expenditure plan –<br />
Cost Improvement Programme<br />
Total Total<br />
Q1 Q2 Q3 Q4 2013/14 2014/15<br />
£000s £000s £000s £000s £000s £000s<br />
Pay<br />
Headcount recovery programme 2,356 2,356 2,356 2,357 9,425 10,800<br />
Medical productivty 501 501 501 501 2,004 2,000<br />
Other workforce productivity 465 465 465 465 1,860 2,000<br />
Outpatient productivity 2,135 2,135 2,135 2,135 8,540 3,500<br />
Pathways & service development 1,111 1,111 1,111 1,112 4,445 3,000<br />
Reduction in LOS schemes 1,148 1,148 1,148 1,148 4,592 2,000<br />
Skill mix/ structure 2,088 2,088 2,088 2,086 8,350 3,000<br />
Theatre Efficiency 750 750 750 750 3,000 3,600<br />
Unidentified CIPS 2,946 2,946 2,946 2,946 11,784 20,000<br />
Pay Total 13,500 13,500 13,500 13,500 54,000 49,900<br />
Non-Pay<br />
Corporate (Estates) efficiencies 1,203 1,203 1,203 1,201 4,810 3,000<br />
Diagnostics 2,544 2,544 2,544 2,544 10,176 4,000<br />
<strong>Trust</strong>wide procurement savings 1,625 1,625 1,625 1,626 6,501 8,000<br />
Unidentified CIPS 504 504 504 504 2,016 12,300<br />
Non-Pay Total 5,876 5,876 5,876 5,875 23,503 27,300<br />
Total 19,376 19,376 19,376 19,375 77,503 77,200<br />
*The current submission to the TDA shows a backloaded CIP, but this will be changed to 1/12ths for the final submission<br />
9
2013/14 Cost Improvement Programme<br />
by CAG<br />
Analysis of Targets<br />
By Scheme Category<br />
CAG - Existing Structure<br />
Annual<br />
Target<br />
2012/13<br />
Shortfall<br />
FYE of<br />
2012/13<br />
New<br />
Schemes Total<br />
£m £m £m £m £m<br />
Ambulatory Care 10.1 3.3 0.5 6.4 10.1<br />
Cancer 4.1 1.8 0.0 2.2 4.1<br />
Cardiovascular 4.8 1.6 0.6 2.6 4.8<br />
Childrens Serivces 3.2 0.6 0.0 2.6 3.2<br />
Clinical Support Services 10.3 2.4 0.5 7.5 10.3<br />
ECAM 9.6 1.6 0.4 7.6 9.6<br />
Surgery 12.2 3.4 0.4 8.4 12.2<br />
Womens Services 5.9 2.2 0.0 3.7 5.9<br />
Corporate 17.3 5.9 0.1 11.4 17.3<br />
Total 77.5 22.7 2.5 52.3 77.5
4: 2013/14 income and expenditure plan –<br />
key risks<br />
SLA with our lead commissioners has not<br />
been agreed<br />
Development of the 2013/14 cost savings<br />
program is behind schedule<br />
Tighter cost control and budget monitoring<br />
will be required in 2013/14<br />
The main contracts for 2013/14 have not been<br />
agreed with either our local or specialist<br />
commissioners. The ability of the CAG’s to release<br />
full costs in response to downward contract changes,<br />
is limited in the short-term.<br />
The finalisation and delivery of the <strong>Trust</strong>’s CIP plans<br />
presents a key risk to delivery of the trust’s plan<br />
surplus of £1m. The planned target at 6.5% of<br />
income represents a significant challenge to the<br />
CAGs, particularly bearing in mind performance on<br />
the 2012/13 CIPs. Plans are being finalised under<br />
the <strong>Trust</strong>’s Recovery Plan, which will be reported<br />
separately.<br />
Internal budget variances have been identified as<br />
part of the budget setting process. However, further<br />
work is required to determine the extent to which<br />
these are attributable to poor budgetary control, or to<br />
genuinely unavoidable cost pressures. The<br />
assumption within the provisional budgets that have<br />
been set is that internal cost pressures will be dealt<br />
with by the CAGs and Corporate, as part of their<br />
business planning process, rather than to increase<br />
the CIP above £77.5m.<br />
11
Statement of Financial Position
Statement of Financial Position Key<br />
Assumptions<br />
Key balance sheet and cash flow<br />
assumptions<br />
The plan assumes cash funding of £64.7m in<br />
Q1<br />
• £79m PFI addition for Royal London (Phase 2)<br />
• £28m estimated PFI impairment<br />
• £32m other capital expenditure<br />
• £65m PDC cash funding receipts (see below)<br />
• £62m pay down of loans and creditors to improve<br />
liquidity position<br />
• £88m closing cash balance target by 31 March<br />
2014<br />
The merger FBC outlined the need for cash funding.<br />
The trust is seeking to draw-down the full entitlement<br />
to funding as set out in the FBC. This comprises of:<br />
• £26.7m funding that was due in 12/13<br />
• £14.0m funding for the capital program<br />
• £24.0m additional funding to improve liquidity
Report to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013 TB 30/13<br />
Title<br />
Information Governance (IG) Toolkit<br />
Sponsoring Director Director of Corporate Affairs and <strong>Trust</strong> Secretary<br />
Author(s)<br />
Information Governance Manager<br />
Purpose To ratify the IG Toolkit submission for 2012/13.<br />
Previously considered by <strong>Trust</strong> Management <strong>Board</strong>, 9 April 2013<br />
Executive summary<br />
2012/13 has been a year of transition for the IG function. While we are confident that<br />
standards of IG within <strong>Barts</strong> <strong>Health</strong> are as high as, and in some cases higher than, in the<br />
pre‐merger legacy trusts, a single IG Team for the new organisation did not come into<br />
place until 1 October 2012 and work is continuing to develop and implement unified IG<br />
policies, procedures and systems across all our sites. A key consequence of this for an<br />
assessment such as the IG Toolkit, which relies heavily on having evidence of embedded<br />
systems and processes, is that the scores for the first year of the new <strong>Trust</strong> are lower<br />
than those in the legacy organisations. Good progress has been made in many cases on<br />
implementing a <strong>Barts</strong> <strong>Health</strong> wide approach but this is not yet universal. Moreover, we<br />
need time to build up evidence that staff are aware of the new arrangements and they<br />
are working effectively. A deliberately cautious approach has therefore been taken to<br />
scoring this year. Compliance with 32 of the 45 IG Toolkit requirements has been<br />
assessed at the required Level 2 or above. 11 requirements have been assessed at Level<br />
1 and 2 requirements have been assessed at Level 0. This gives an overall rating for<br />
2012/13 of ‘Not Satisfactory’ (with a corresponding percentage of 57%).<br />
Related <strong>Trust</strong> objectives<br />
9. Deliver the post‐merger integration plan including the clinical due diligence action<br />
plan and corporate and clinical services management integration.<br />
Risk and Assurance<br />
Related Assurance<br />
Framework entries<br />
Key information governance risks are monitored by the<br />
Information Governance Committee, which is chaired by the<br />
<strong>Trust</strong>’s Senior Information Risk Owner.<br />
n/a<br />
Legal implications/<br />
regulatory requirements<br />
The <strong>Trust</strong> is required to make an annual submission to the<br />
Department of <strong>Health</strong> by 31 March 2013.<br />
Action required by the <strong>Board</strong><br />
The <strong>Trust</strong> <strong>Board</strong> is asked to:<br />
Ratify the <strong>Trust</strong>’s 2012/13 Information Governance Toolkit submission.<br />
Note the proposed key Information Governance priorities for 2013/14.<br />
1
TB 30/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING: 10 APRIL 2013<br />
INFORMATION GOVERNANCE TOOLKIT<br />
INTRODUCTION<br />
1. Information Governance covers the way in which the <strong>NHS</strong> manages all types of<br />
information, in particular the personal and sensitive information of patients and<br />
employees. Fundamentally, an effective Information Governance framework<br />
gives organisations and individuals the confidence that personal information is<br />
being dealt with legally, securely, efficiently and effectively, in support of<br />
delivering the best possible standards of clinical care.<br />
INFORMATION GOVERNANCE TOOLKIT<br />
2. The Department of <strong>Health</strong>’s Information Governance Toolkit (IGT) is an annual<br />
mandatory self‐assessment of how <strong>NHS</strong> acute trusts are performing against a<br />
range of 45 separate requirements spanning the six initiatives of Information<br />
Governance. Each standard must be rated on a scale of 0 to 3:<br />
0 No compliance<br />
1 Weak compliance<br />
2 Adequate compliance<br />
3 Full compliance<br />
<strong>Trust</strong>s are required to meet a minimum of Level 2 for all 45 requirements in<br />
order to achieve an overall ‘Satisfactory’ level of compliance on the Toolkit.<br />
3. <strong>NHS</strong> organisations have had to make three toolkit submissions during 2012/13: a<br />
July 2012 baseline assessment, an October 2012 performance update and the<br />
final submission by 31 March 2013. At its meeting on 6 March 2013, the <strong>Trust</strong><br />
<strong>Board</strong> delegated authority to the Chief Executive to sign off the <strong>Barts</strong> <strong>Health</strong> final<br />
submission. This was completed on 28 March 2013.<br />
4. <strong>Trust</strong>s’ submissions are subsequently used by other organisations such as the<br />
Care Quality Commission, the <strong>NHS</strong> Litigation Authority and the Information<br />
Commissioner’s Office, to support the wider <strong>NHS</strong> compliance and information<br />
management framework. For example, the CQC uses a number of the IG Toolkit<br />
standards as indicators of potential non‐compliance for the Records Outcome<br />
(Outcome 21) of the Essential Standards of Quality and Safety.<br />
2012/13 PERFORMANCE<br />
5. As in many other areas of <strong>Barts</strong> <strong>Health</strong>, 2012/13 has been a year of transition for<br />
the information governance function. While we are confident that standards of<br />
2
TB 30/13<br />
information governance within <strong>Barts</strong> <strong>Health</strong> are as high as, and in some cases<br />
higher than, in the pre‐merger legacy trusts, a single IG Team for the new<br />
organisation did not come into place until 1 October 2012 and work is continuing<br />
to develop and implement unified IG policies, procedures and systems across all<br />
our sites.<br />
6. A key consequence of this for an assessment such as the IG Toolkit, which relies<br />
heavily on having evidence of embedded systems and processes, is that the<br />
scores for the first year of the new <strong>Trust</strong> are lower than those in each of the<br />
legacy organisations. Good progress has been made in many cases on<br />
implementing a <strong>Barts</strong> <strong>Health</strong> wide approach but this is not yet universal.<br />
Moreover, we need time to build up evidence that staff are aware of the new<br />
arrangements and they are working effectively. A deliberately cautious<br />
approach has been taken to scoring this year.<br />
7. Each IG requirement has an assigned lead and a senior manager, generally at<br />
Director level, who is responsible for signing off the proposed score and<br />
confirming that it is supported by appropriate evidence. Their reviews of<br />
compliance have been supported by the findings of an Internal Audit of a sample<br />
of the IG Toolkit requirements, particularly in relation to information security.<br />
The Internal Audit work to date has confirmed the IG Team’s own assessment of<br />
the need to build a stronger evidence base for a number of the requirements as<br />
further integration and embedding of systems and processes is completed.<br />
8. Table 1 below sets out the 2012/13 IG Toolkit scores for <strong>Barts</strong> <strong>Health</strong>, as<br />
endorsed by the <strong>Trust</strong>’s Information Governance Committee:<br />
Total number of requirements<br />
Level 0 Level 1 Level 2 Level 3 Total<br />
Overall<br />
Score<br />
IG Management 0 2 3 0 5 53%<br />
Confidentiality and<br />
Data Protection<br />
0 2 6 1 9 62%<br />
Information Security 2 2 11 0 15 53%<br />
Clinical Information 0 2 3 0 5 53%<br />
Secondary Use 0 3 5 0 8 54%<br />
Overall<br />
Grade<br />
Not<br />
Satisfactory<br />
Not<br />
Satisfactory<br />
Not<br />
Satisfactory<br />
Not<br />
Satisfactory<br />
Not<br />
Satisfactory<br />
Corporate Information 0 0 2 1 3 77% Satisfactory<br />
Overall 2 11 30 2 45 57%<br />
Not<br />
Satisfactory<br />
Key:<br />
Satisfactory:<br />
Not Satisfactory:<br />
Achieved attainment Level 2 or above on all requirements<br />
Not achieved attainment Level 2 or above on all requirements<br />
3
TB 30/13<br />
9. In summary, compliance with 32 of the 45 requirements has been assessed at<br />
the required Level 2 or above. 11 requirements have been assessed at Level 1<br />
and 2 requirements have been assessed at Level 0. This gives an overall rating<br />
for 2012/13 of ‘Not Satisfactory’ (with a corresponding percentage of 57%).<br />
10. For information, each of the three legacy trusts also scored ‘Not Satisfactory’ in<br />
their 2011/12 submissions, albeit with a lower number of Level 1 and no Level 0<br />
scores.<br />
11. The main areas of non‐compliance are as follows:<br />
<br />
<br />
<br />
<br />
<br />
IG Management: all staff to have undertaken annual mandatory IG<br />
training and passed a test of comprehension (currently the figure is<br />
under 50%); and all contracts to include robust IG requirements.<br />
Confidentiality and Data Protection: consolidation of data flow<br />
mapping work; and embedding a single Subject Access Request<br />
process.<br />
Information Security: all information assets are risk assessed and<br />
managed, with up‐to‐date and tested business continuity plans; and<br />
appropriate use of pseudonymisation and anonymisation techniques.<br />
Clinical Information: monitoring, auditing and tracing clinical records<br />
across all specialties.<br />
Secondary Use: comprehensive data quality completeness and<br />
validity checks.<br />
2013/14 INFORMATION GOVERNANCE WORK PROGRAMME<br />
12. A key priority for the 2013/14 Information Governance work programme will be<br />
to raise the Level 0 and Level 1 scores to Level 2 and the IG Team will work with<br />
the requirement leads to ensure that an appropriate evidence base is in place.<br />
An action plan will be developed, informed by the final Internal Audit report, and<br />
its implementation will be monitored by the Information Governance<br />
Committee. Issues will be reported to the <strong>Trust</strong> Management <strong>Board</strong> by<br />
exception.<br />
13. Other key IG priorities for 2013/14 will be as follows:<br />
<br />
<br />
Identifying and mitigating information governance risks by raising<br />
awareness and undertaking spot checks across all sites.<br />
Continuing to drive compliance with annual mandatory Information<br />
Governance training, ensuring a flexible supply of both face‐to‐face and<br />
e‐learning opportunities to undertake training.<br />
4
TB 30/13<br />
<br />
<br />
<br />
<br />
Initiating and completing the de‐identification project for all secondary<br />
uses of patient information.<br />
Preparing the <strong>Trust</strong> for the adoption of the European General Data<br />
Protection Regulation which will supersede the current Data Protection<br />
Directive in 2014.<br />
Establishing a unified register of data flows and information assets across<br />
<strong>Barts</strong> <strong>Health</strong>.<br />
Providing specialist IG advice and support on a range of informatics<br />
projects.<br />
OTHER IG ISSUES<br />
Information Governance Assurance Statement<br />
14. The Information Governance Assurance Statement is the agreement between<br />
<strong>NHS</strong> Connecting for <strong>Health</strong> and Approved Service Recipients that sets out the<br />
terms and conditions for the use of <strong>NHS</strong> Connecting for <strong>Health</strong> services,<br />
including the <strong>NHS</strong> N3 network, in order to preserve the integrity of those<br />
services. The Information Governance Assurance Statement is supported by the<br />
annual submission of the IG Toolkit and <strong>NHS</strong> organisations are required to attain<br />
Level 2 for all the IGT requirements that feed into the Information Governance<br />
Assurance Statement.<br />
15. On the basis of the proposed 2012/13 IG Toolkit scores above, the <strong>Trust</strong> will not<br />
meet all of these requirements at Level 2 or above. This requires the Chief<br />
Executive to sign an action plan detailing how and when Level 2 or above will be<br />
achieved. The action plan will be draw up and tabled at the next Information<br />
Governance Committee meeting in May 2013 prior to being signed off by the<br />
Chief Executive.<br />
Freedom of Information<br />
16. The volume of Freedom of Information requests received by the <strong>Trust</strong> continues<br />
to remain high and to consume significant resources both centrally and across<br />
the organisation. During this reporting period, the <strong>Trust</strong> has dealt with over 500<br />
requests for information under the Act.<br />
IG incidents and risks<br />
17. During 2012/13, the <strong>Trust</strong> reported three IG‐related incidents to the Information<br />
Commissioner’s Office. These were investigated as Serious Incidents and will be<br />
disclosed in the Annual Report as required by Department of <strong>Health</strong> guidance.<br />
The <strong>Trust</strong> and has not been subject to any Information Commissioner Data<br />
Protection monetary penalties, enforcement notices or Freedom of Information<br />
notices. The Information Governance team continues to work with colleagues<br />
across the <strong>Trust</strong> to learn from these incidents and the Information Governance<br />
Committee reviews all IG incidents and key risks at each of its meetings.<br />
5
TB 30/13<br />
RECOMMENDATIONS<br />
18. The <strong>Trust</strong> <strong>Board</strong> is asked to:<br />
Ratify the <strong>Trust</strong>’s 2012/13 Information Governance Toolkit submission.<br />
Note the proposed key Information Governance priorities for 2013/14.<br />
Remi Ogbe<br />
Information Governance Manager<br />
Ian Walker<br />
Director of Corporate Affairs and Senior Information Risk Owner 28 March 2013<br />
6
Report to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013 TB 31/13<br />
Title<br />
Sponsoring Director<br />
<strong>Board</strong> Assurance Framework<br />
Director of Corporate Affairs and <strong>Trust</strong> Secretary<br />
Author(s)<br />
Deputy <strong>Trust</strong> Secretary<br />
Interim Risk Manager<br />
Purpose<br />
The <strong>Board</strong> Assurance Framework (BAF):<br />
Provides an assessment of the principal risks to the<br />
<strong>Trust</strong>’s strategic annual objectives.<br />
Is used to assist the commissioning of assurances and<br />
the development of work plans for the <strong>Board</strong>’s<br />
assurance committees.<br />
Is an essential requirement for trusts to produce,<br />
demonstrating the <strong>Board</strong>’s oversight of the<br />
organisation’s systems of control.<br />
Previously considered by Audit and Risk Committee, 20 February 2013<br />
<strong>Trust</strong> Management <strong>Board</strong>, 5 March 2013<br />
Risk Management Committee, 4 April 2013<br />
Related <strong>Trust</strong> objectives<br />
All <strong>Trust</strong> objectives<br />
Risk and Assurance<br />
Related Assurance<br />
Framework entries<br />
Legal implications/<br />
regulatory requirements<br />
This report highlights proposed principal risks to the delivery of<br />
the <strong>Trust</strong>’s annual objectives for 2012/13.<br />
All<br />
It is a requirement as part of the <strong>Trust</strong>’s Annual Governance<br />
Statement (an element of the <strong>Trust</strong>’s annual report and<br />
accounts) that the <strong>Trust</strong> evidences its systems of control, most<br />
commonly through the development of a BAF. Its development<br />
and use is reported on in the related Head of Internal Audit<br />
Opinion.<br />
Action required by the <strong>Board</strong><br />
The <strong>Trust</strong> <strong>Board</strong> is asked to:<br />
Receive and approve the <strong>Board</strong> Assurance Framework for 2012/13 Q4.<br />
Note and comment on the methodology used to develop the <strong>Board</strong> Assurance<br />
Framework and proposed steps to refine this during 2013/14.<br />
1
TB 31/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
REPORT TO THE TRUST BOARD: 10 APRIL 2013<br />
BOARD ASSURANCE FRAMEWORK<br />
INTRODUCTION AND BACKGROUND<br />
1. The <strong>Trust</strong> <strong>Board</strong> receives the <strong>Board</strong> Assurance Framework (BAF) on a regular basis to note<br />
and discuss principal risks to the delivery of the <strong>Trust</strong>’s annual objectives. It is proposed that,<br />
following its development, the <strong>Board</strong> Assurance Framework is presented to the <strong>Board</strong> at<br />
least three times during 2013/14 following review by the Risk Management Committee.<br />
2. The terms of reference for the <strong>Board</strong>’s principal assurance committees (the Quality<br />
Assurance Committee and Audit and Risk Committee) establish that the respective<br />
Committee will receive and review at each meeting the BAF entries allocated to it for<br />
oversight. The BAF is intended to inform the development of annual work plans for these<br />
committees and their role in commissioning assurances.<br />
3. Immediate <strong>Barts</strong> <strong>Health</strong> priorities for risk management were identified by the <strong>Trust</strong><br />
Management <strong>Board</strong> and the Risk Management Committee following the merger on 1 April<br />
2012 and during the transition from legacy site‐based units to the establishment of a Clinical<br />
Academic Group (CAG) structure on 1 October 2012. These priorities included the<br />
completion of clinical and financial due diligence exercises, the development of a risk<br />
management strategy and policy and steps to consolidate and validate the <strong>Trust</strong>’s risk<br />
register (taking into account the letters of representation exercises).<br />
4. The development of a <strong>Barts</strong> <strong>Health</strong> BAF has followed on from the above steps and builds on<br />
this work. The BAF entries set out in Appendix 2 have been developed based on the<br />
approach outlined at the last meeting of the <strong>Trust</strong> <strong>Board</strong> on 6 March 2013. These seek to<br />
take account of key national and local drivers, such as the Francis Report on events at Mid<br />
Staffordshire <strong>NHS</strong> Foundation <strong>Trust</strong>, the <strong>Trust</strong>’s Foundation <strong>Trust</strong> aspirations and the<br />
current financial environment.<br />
BAF FORMAT<br />
5. At an early stage, the proposed approach to developing the <strong>Board</strong> Assurance Framework<br />
entries indicated an emphasis on the high risks identified in the risk register. It was felt that<br />
a purely ‘top‐down’ assessment of principal risks to the <strong>Trust</strong>’s objectives (by the <strong>Board</strong>,<br />
executive team or others) could result in gaps, given the size and scale of the new<br />
organisation. There was also an important opportunity to build on other risk identification<br />
work outlined in paragraph 3. It was also felt that previous BAF formats had proved weak in<br />
terms of providing an established link between high risks on the risk register and BAF<br />
entries. This is addressed in the new BAF format by explicitly referencing the related high<br />
risks that appear on the risk register.<br />
2
TB 31/13<br />
6. The format of the current BAF (as at Appendix 2) reflects the decision taken to focus initially<br />
on identifying the principal risks. A link to performance will be re‐established in later<br />
iterations of the <strong>Board</strong> Assurance Framework – with the intention of reflecting the evolving<br />
changes to performance reporting in the <strong>Trust</strong>. Other planned improvements in 2013/14<br />
include a focus on revising the BAF in line with new 2013/14 objectives, mapping assurances<br />
more systematically (with the involvement of Internal Audit and reflecting their forward<br />
plan – the Internal Audit plan 2013/14) and establishing target risk scores which reflect what<br />
the <strong>Board</strong> may consider to be an acceptable level of residual risk (risk appetite).<br />
BAF DEVELOPMENT<br />
7. Since the last meeting, steps have been taken to review the ‘shortlist’ and ‘long list’ of<br />
possible BAF entries with lead executives (in meetings held jointly with Risk Management<br />
and <strong>Trust</strong> Offices staff) and the Risk Management Committee to identify risk scores,<br />
controls, assurances and gaps in controls and assurances. This iterative process of BAF<br />
review will continue throughout 2013/14, with the continued advice and assistance of<br />
colleagues from Risk Management and Internal Audit functions.<br />
8. The BAF risks highlighted in this version reflect changes to the scores of related risk register<br />
entries and progress against some risks previously appearing on the ‘shortlist’. Steps will be<br />
taken to ensure that those risks identified on the ‘long list’ are reflected in the risk register<br />
(if this is not already the case). The BAF risks have been assigned to lead executives who will<br />
be responsible for reporting to the <strong>Board</strong> on progress against these entries. The BAF risks<br />
have also been tentatively assigned to <strong>Board</strong> assurance committees to assist with planned<br />
discussions on committee work plans for 2013/14 (the final committee allocation will be<br />
discussed at scheduled planning meetings and committees during May).<br />
9. The BAF was discussed and endorsed by the Risk Management Committee on 4 April 2013.<br />
The Risk Management Committee agreed some changes, including the addition of risk 6<br />
(relating to assessing team effectiveness). Other proposals for further developing the BAF<br />
included an assessment of the risks relating to broader academic developments and to<br />
signpost where BAF entries relate to recommendations in the Francis Report.<br />
RECOMMENDATION<br />
10. The <strong>Trust</strong> <strong>Board</strong> is asked to:<br />
Receive and approve the <strong>Board</strong> Assurance Framework (BAF) for 2012/14 Q4.<br />
<br />
Note and comment on the methodology used to develop the <strong>Board</strong> Assurance<br />
Framework and proposed steps to refine this during 2013/14.<br />
Sean Collins<br />
Deputy <strong>Trust</strong> Secretary<br />
Mark Rogers<br />
Interim Risk Manager 4 April 2013<br />
3
RISK HEATMAP<br />
<strong>Board</strong> Assurance Framework (heatmap)<br />
<strong>Trust</strong> <strong>Board</strong> meeting<br />
10 April 2013<br />
Current Score (consequence x likelihood, arrow indicates movement in<br />
quarter)<br />
Risk entry Page Outset Score =20 Target Score<br />
1. Failure to identify or address safeguarding concerns impacts on the quality of services, safety of patients and the<br />
<strong>Trust</strong>’s reputation. 1 5x4=20 5x4 tbc<br />
2. As a result of skills and capacity constraints, a failure to manage acutely ill patients in a consistent way at all sites<br />
and all times, could result in isolated incidents of delayed responses to deteriorating patients Insufficient emergency<br />
care capacity and failure to address patient flow issues impacts on patient safety and experience and meeting<br />
national targets. 2 5x3=15 5x3 4x4 tbc<br />
3. Insufficient emergency care capacity and failure to address patient flow issues impacts on patient safety and<br />
experience and meeting national standards. 3 4x4=16 4x4 tbc<br />
4. Lack of a robust infection prevention framework for eliminating avoidable health care associated infections<br />
impacts on patient safety and experience. 4 4x4=16 4x4 tbc<br />
5. Absence of an integrated informatics infrastructure to ensure that the ‘right information at the right time’ is<br />
available adversely impacts on patient treatment or flagging safety issues. 5 5x3=15 5x3 tbc<br />
6. A failure to systematically assess the health of teams, in particular team cultures, and the effectiveness of<br />
individual services adversely impacts on quality of care. 6 5x3=15 5x3 tbc<br />
7. Underachievement of CIPs and other expenditure controls leads to increased challenge to LTFM in subsequent<br />
years and to ongoing financial sustainability. 7 4x5=20 4x5 tbc<br />
8. Cost improvement plans involve workforce changes and temporary staffing controls that adversely impact on<br />
quality and safety. 8 5x3=15 5x3 tbc<br />
9. The lack of sufficiently robust workforce information impairs decision‐making and the optimal use of workforce<br />
resources to deliver safe patient care efficiently. 9 5x3=15 5x3 tbc<br />
10. Non‐compliance with mandatory systems and policies and a failure to engage staff on its importance adversely<br />
impacts on safety and efficiency. 10 5x4=20 5x4 tbc<br />
11. A failure to develop a Clinical Strategy consistent with the LTFM and delivery of merger full business case<br />
benefits impacts on the organisation’s Foundation <strong>Trust</strong> trajectory. 11 5x3=15 5x3 tbc<br />
TB 31/13a<br />
Period covered: 2012/13 Quarter‐4<br />
12. Statutory and mandatory training non‐compliance results in patient safety risks and impairs quality of care. 12 3x4=12 3x4 tbc<br />
Highlights by exception: (Going forward to highlight changes to the previous version)<br />
Addition of new risk 1a(v) above. Deletion of previous risk 8(i) which stated 'Failure to satisfactorily resolve issues relating to non‐recurrent funding to support the PFI and support for <strong>Barts</strong> site costs has an adverse impact on the<br />
Addition of new risk 1a(v) above. Deletion of previous risk 8(i) which stated 'Failure to satisfactorily resolve issues relating to non‐recurrent funding to support the PFI and support for <strong>Barts</strong> site costs has an adverse impact on the<br />
<strong>Trust</strong>’s financial outlook'.<br />
Notes: Shading indicates risks for which a <strong>Board</strong> committee has an assurance role: ARC QAC FIC FT Project <strong>Board</strong>
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: A. Service Quality and Development<br />
Sub Objective: n/a<br />
PRINCIPAL RISKS<br />
Description of risk<br />
1. Failure to identify or<br />
address safeguarding<br />
concerns impacts on the<br />
quality of services, safety of<br />
patients and the <strong>Trust</strong>’s<br />
reputation.<br />
Executive lead: Chief Nurse<br />
Subcommittee role: Quality<br />
Assurance Committee<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (5x4=20)<br />
Outset risk: Mar<br />
13 (5x4=20)<br />
Essential<br />
Standard:<br />
Outcomes 4, 7,<br />
13, 20<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
Unified <strong>Barts</strong> <strong>Health</strong> safeguarding adults and children team in<br />
place. Safeguarding policies and processes in place (risk 162).<br />
Focus on safeguarding adults at risk:<br />
Joint working group with 5 Local Authorities to agree<br />
standard processes for alerts , referrals and Mental<br />
Capacity Act implementation<br />
Learning disabilities strategy to address risks of<br />
inequality of access or treatment. Additional resources<br />
for this strategy supported by the <strong>Board</strong>.<br />
Older People’s Services improvement programme with<br />
well integrated support from safeguarding.<br />
Statutory and mandatory training programme in place and<br />
staff must attend appropriate level of safeguarding children's<br />
training for their role. Training for level 1 and 2 is provided on<br />
a monthly basis and Level 3 on bi monthly basis (risk 162 and<br />
931).<br />
Safeguarding adults training programme in place with focus in<br />
April/May 2013 on increasing training take‐up and provision.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
Reporting to <strong>Trust</strong> <strong>Board</strong> twice yearly on safeguarding<br />
children.<br />
Safeguarding <strong>Board</strong> monitors performance information.<br />
External assurance:<br />
Clinical Due Diligence phase 2 reviews.<br />
Pan‐London Local Safeguarding Children’s <strong>Board</strong> monitors<br />
serious case reviews and key data.<br />
Management assurance:<br />
Reporting to <strong>Trust</strong> <strong>Board</strong> on Mental <strong>Health</strong> Act compliance.<br />
Progress against learning disabilities strategy objectives<br />
monitored regularly.<br />
Older People’s Services improvement programme<br />
governance mechanisms.<br />
External assurance:<br />
Clinical Due Diligence phase 2 reviews.<br />
External reviews of Older People’s Service (MEH/RLH) in<br />
2011 and 2012.<br />
CQC reviews of Ainslie and Highams; Beech Ward<br />
arrangements.<br />
Pan‐London Safeguarding Adults <strong>Board</strong> group monitors<br />
serious case reviews and key data.<br />
External membership on Older People’s Services<br />
independent assurance panel.<br />
Management assurance:<br />
Reporting through the Integrated Performance Framework<br />
and focus at Performance Reviews<br />
External assurance:<br />
RED<br />
RD<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Incidents in Older peoples’ services and<br />
findings from external reviews indicates the<br />
need for further review of controls.<br />
Action: QAC agreed <strong>Health</strong> Check review<br />
process for Older People’s Services<br />
Detail: Lack of a consistent and integrated<br />
approach with social care to managing patients<br />
with mental health issues or learning disabilities<br />
Action: Regular liaison with social care partners<br />
Detail: Absence of a systematic <strong>Barts</strong> <strong>Health</strong>wide<br />
approach to flagging patients with<br />
learning disabilities to identify needs and target<br />
resources.<br />
Action: Steps to improve and harmonise<br />
patient administration systems across <strong>Barts</strong><br />
<strong>Health</strong><br />
Detail: As a result of non‐compliance as<br />
stipulated by <strong>NHS</strong>LA, CQC to achieve a rate of<br />
95% compliance in Safeguarding particularly,<br />
the <strong>Trust</strong> could face a negative report and an<br />
improvement notice (risk 931)<br />
Action: Additional training sessions being<br />
provided based on training needs analysis.<br />
Communicating with CAGs re compliance<br />
requirements and the need to release staff to<br />
attend training (risk 931)<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
98 ‐ Assessment, treatment & discharge of under 16s in ED with urgent primary care needs (risk score ‐ 16, lead ‐ ECAM CAG)<br />
162 – Management and compliance with regional and national policy and legislation for safeguarding children (risk score – 16, lead Children’s CAG)<br />
931 – Statutory and Mandatory <strong>Trust</strong> wide safeguarding children training coverage below commissioners requirements (current risk score 9 [was 15] – lead Director of AHS)<br />
1
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: A. Service Quality and Development<br />
Sub Objective: n/a<br />
PRINCIPAL RISKS<br />
Description of risk<br />
2. As a result of skills and<br />
capacity constraints, a failure<br />
to manage acutely ill patients<br />
in a consistent way at all sites<br />
and all times, could result in<br />
isolated incidents of delayed<br />
responses to deteriorating<br />
patients.<br />
Executive lead: Medical<br />
Director<br />
Subcommittee role: Quality<br />
Assurance Committee<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (5x3=15)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 4, 16<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
Role of matrons in routine ward reviews and identifying issues<br />
particularly the systematic use of Early Warning Scores.<br />
Managing acutely ill patients policies and dedicated critical<br />
care outreach team in place to assist frontline staff.<br />
Mortality and Morbidity reviews by clinical teams.<br />
Serious Incident reporting mechanisms.<br />
Root cause analysis and staggered audits (through the Global<br />
Trigger Tool) provides management information.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
Resus team carries out frequent audits.<br />
Risk Management Committee tracks risks and issues<br />
escalated to TMB as required<br />
External assurance:<br />
Management assurance:<br />
A <strong>Trust</strong>‐wide Critical Care <strong>Board</strong>, with cross‐CAG<br />
representation, which has a Managing the Acutely‐Ill<br />
Patient workstream.<br />
RED<br />
RD<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Quality Assurance Committee agreed in<br />
March plans for further focused work at The<br />
Royal London.<br />
Action: Increased multidisciplinary team<br />
meetings and education sessions.<br />
Detail: No natural forum where cross‐CAG<br />
themes in failures of care are discussed. No<br />
obvious early trigger‐point when episodes of<br />
harm are on the rise.<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
99 Management of the Acutely ill patient (risk score – 15, lead – ECAM CAG)<br />
B<br />
2
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: A. Service Quality and Development<br />
Sub Objective: A1.Deliver minimum national service standards set out in the Operating Framework including A&E, 18 weeks RTT, cancer access and MRSA<br />
PRINCIPAL RISKS<br />
Description of risk<br />
3. Insufficient emergency<br />
care capacity and failure to<br />
address patient flow issues<br />
impacts on patient safety and<br />
experience and meeting<br />
national standards.<br />
Executive lead: Chief<br />
Operating Officer<br />
Subcommittee role: Quality<br />
Assurance Committee<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (4x4=16)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 4, 13,<br />
16<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
A&E and site management teams in place. Bed management<br />
protocols identified for admissions and discharge with<br />
escalation plans.<br />
Introduction of additional measures at Whipps Cross to<br />
improve throughflow and reduce length of stay including,<br />
weekend consultant‐led discharge and escalation<br />
arrangements (risk 9).<br />
Emergency Department facilities: move to an integrated<br />
ED/Urgent Care Centre on a new site with a single point of<br />
access at RLH. Similar improvements at Whipps (risk 98).<br />
Introduction of Patient At Risk (PAR) scoring, revised<br />
escalation and security arrangements to reflect changes to<br />
ways of working. (risk 100)<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance: Daily operational team reviews of<br />
performance and weekly reviews by <strong>Trust</strong> Executive. Chief<br />
Executive more directly involved from March 2013 in A&E<br />
performance monitoring. TMB and <strong>Board</strong> monthly<br />
reporting via the Integrated Performance Framework.<br />
External assurance: TX commissioned an independent<br />
review of A&E flows at all sites to identify variances in<br />
attendances and admissions rates. Initial results fed back in<br />
March 2013 and further work now being undertaken.<br />
Management assurance: Daily and weekly operational<br />
team reviews of performance. TMB and <strong>Board</strong> monthly<br />
reporting.<br />
External assurance:<br />
Management assurance:<br />
New Hospital planning group for A&E developed flow<br />
models. CAG <strong>Board</strong> oversight (risk 100).<br />
External assurance:<br />
RED<br />
RD<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Failure to satisfactorily address issues<br />
with managing within existing bed capacity,<br />
responding to higher attendances and greater<br />
acuity (risk 83).<br />
Action: Ongoing performance monitoring.<br />
Detail: Greater Information and analysis<br />
required to minimise readmissions (risk 938).<br />
Action: Readmissions data reviewed at PRs.<br />
Detail: Issues with psychiatry team’s timeliness<br />
of responses to complete joint assessments<br />
(risk 120)<br />
Action: Agreements identified with ELMHT and<br />
steps to review consistency of application.<br />
Detail: Insufficient resources to support<br />
preferred levels of medical cover (risk 9, 98)<br />
Action: Appointment of additional emergency<br />
care consultants.<br />
Detail: Changed layout and size of emergency<br />
departments requires changes to ways of<br />
working (risk 100).<br />
Action: New controls implemented to respond<br />
to new arrangements and the impact assessed.<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
9 ‐ Failure to achieve reduction in Length of Stay at Whipps Cross site (risk score ‐ 16, lead – ECAM CAG)<br />
83 ‐ Failure to achieve A & E 4 hour wait indicator (risk score 25, lead Len Richards/ECAM CAG)<br />
98 ‐ Assessment, treatment & discharge of under 16s in ED with urgent primary care needs (risk score ‐ 16, lead ‐ ECAM CAG)<br />
938 ‐ Cost of Readmissions (risk score – 16, lead Len Richards)<br />
100 ‐ Introduction of new format of emergency care department – visibility / management (risk score – 20, lead – ECAM CAG)<br />
120 ‐ Psychiatry liaison issues (risk score 16, lead – ECAM CAG)<br />
3
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: A. Service Quality and Development<br />
Sub Objective: A1. Deliver minimum national service standards set out in the Operating Framework including A&E, 18 weeks RTT, cancer access and MRSA<br />
PRINCIPAL RISKS<br />
Description of risk<br />
4. Lack of a robust infection<br />
prevention framework for<br />
eliminating avoidable health<br />
care associated infections<br />
impacts on patient safety and<br />
experience.<br />
Executive lead: Medical<br />
Director<br />
Subcommittee role: Quality<br />
Assurance Committee<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (4x4=16)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 4, 8, 9,<br />
10<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
A dedicated infection control team is in place with leadership<br />
of Director of Infection Prevention and Control and Deputy<br />
DIPC. Occupational <strong>Health</strong> department provides leadership on<br />
workforce health and flu immunisation programmes.<br />
CAGs have designated clinical directors as leads for infection<br />
control. CAG‐level targets and dashboards for infection<br />
control.<br />
Interventions to support zero tolerance infection control<br />
culture include infection control training, launch of IC<br />
campaigns (including infection control day in May); post<br />
infection reviews for C diff and MRSA cases. Targeted<br />
executive walkrounds where MRSA bacteraemias occur<br />
(Executive and lead consultant attend all MRSA case reviews)<br />
meetings); and inclusion of infection control requirements in<br />
all job descriptions.<br />
Infrastructure improvements through construction of new<br />
hospitals at The Royal London and <strong>Barts</strong> (designed to reduce<br />
infections, with increased single room availability) and<br />
refurbishment programmes at Whipps Cross.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance: Infection Control work plan RED<br />
monitored regularly by Infection Control Committee.<br />
CAG <strong>Board</strong>s monitor CAG‐level performance and<br />
Performance Reviews.<br />
External assurance:<br />
CQC visits with focus on Outcome 8 (cleanliness and<br />
infection control)<br />
Management assurance:<br />
Staff survey and other patient survey data.<br />
Management assurance: Daily and weekly operational<br />
team reviews of performance. TMB and <strong>Board</strong> monthly<br />
reporting.<br />
RD<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Interim arrangements in place pending<br />
standardisation of nursing resources and<br />
appointment of a <strong>Trust</strong> decontamination lead.<br />
Action: Completion of recruitment processes.<br />
Detail: Centralisation of laboratory systems<br />
identified as a possible cause of reporting<br />
delays.<br />
Action: Monitoring to ensure predicted benefits<br />
of centralisation are realised.<br />
Detail: Isolation facilities and older wards,<br />
including 9 at Whipps Cross, increases risk<br />
profile (risk 3).<br />
Action: Ongoing performance monitoring and<br />
capital developments.<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
3 Acacia Ward isolation ward facilities (risk score 15 – lead ECAM CAG)<br />
35 Insufficient data on Surgical Site Infection (SSI) rates (risk score 16 – lead Surgery CAG)<br />
77, 89, 165 Failure to implement effective infection control framework (risk score 20 – lead Medical Director)<br />
119 Facilities for cystic fibrosis patients (risk score 16 – lead Medical Director)<br />
131 Pseudomonas (ACCU) (risk score 16 – lead ECAM CAG)<br />
4
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: A. Service Quality and Development<br />
Sub Objective: A2. Achieve the three quality improvement priorities: to keep patients better informed about their care, to improve feedback given to staff when they raise quality and safety concerns, and to improve our patient<br />
administration systems.<br />
PRINCIPAL RISKS<br />
Description of risk<br />
5. Absence of an integrated<br />
informatics infrastructure to<br />
ensure that the ‘right<br />
information at the right time’<br />
is available adversely impacts<br />
on patient treatment or<br />
flagging safety issues.<br />
Executive lead: Chief<br />
Information Officer<br />
Subcommittee role: Audit<br />
and Risk Committee for data<br />
quality and systems / Quality<br />
Assurance Committee for<br />
patient safety aspects<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (5x3=15)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 9, 16<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
ICT infrastructure in place and key Patient Administration<br />
Systems (PAS) supported by a central team. Business case to<br />
procure a single Electronic Patient Record system to replace<br />
contracts expiring in next 18‐36 months endorsed by FIC in<br />
March 2013. Whipps Cross to move across to Cerner CRS<br />
system in 2013/14.<br />
Information Governance and Information security teams in<br />
place.<br />
Upgrade of Millennium Cerner at former <strong>Barts</strong> and The<br />
London sites in Dec 2012 to enhance functionality.<br />
Work being piloted to join up CRS and EMIS.<br />
Key policies including information governance, information<br />
security, disaster recovery and Major Incident Plans in place.<br />
<strong>Health</strong> records management with dedicated team.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
Reports to TMB and the Finance and Investment<br />
Committee on the informatics strategy and CRS route map.<br />
Management assurance:<br />
Information Governance Committee with oversight of IG<br />
issues and escalation to TMB as required. <strong>Health</strong> Records<br />
Committee being established.<br />
External assurance:<br />
IG Toolkit submitted and assessment processes reviewed<br />
by Internal Audit.<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Limitations on flagging in existing PAS<br />
systems (risk 12).<br />
Action:<br />
Detail: PACs/RIS interface / reporting issues.<br />
Action: Contract agreed for new PACs system.<br />
Detail: Steps required to finalise single policy<br />
and lack of a coordinated health records<br />
management system.<br />
Action: Policy drafted and in consultation.<br />
Electronic Document Management project to<br />
deliver improved health records access and<br />
quality with intent to roll out beyond former<br />
<strong>Barts</strong> and The London sites.<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
12 Lack of ‘Target’ Flag on PAS (risk score ‐ 16, lead ‐ Cancer CAG)<br />
66,121 Failure to capture all maternity clinical data and activity at point of care electronically (risk scores – 15, 16, lead – Women and Children’s CAG)<br />
84 Diagnosis recording in Cerner Millennium (risk score – 15, lead – ICT Directorate)<br />
105 EPR replacement (risk score – 15, lead – ICT Directorate)<br />
111 ICT infrastructure (risk score – 15, lead – ICT Directorate)<br />
129 CRS issues with consultant names (risk score – 16, lead – Surgery CAG)<br />
1332 Delays in accessing patient letters on DMS system (risk score – 15, lead – Cancer CAG)<br />
144,155 <strong>Health</strong> records management system (risk scores – 15, lead – ICT Directorate)<br />
5
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: A. Service Quality and Development<br />
Sub Objective: A3. Develop and deliver a plan to improve patient experience and satisfaction, including a focus on Outpatients appointments<br />
PRINCIPAL RISKS<br />
Description of risk<br />
6. A failure to systematically<br />
assess the health of teams, in<br />
particular team cultures, and<br />
the effectiveness of<br />
individual services adversely<br />
impacts on quality of care.<br />
Executive lead: Chief<br />
Executive<br />
Subcommittee role:<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (5x3=15)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 4, 6,<br />
10<br />
Datix ref: tbc<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
Incident reporting rates, staff survey results and complaints<br />
data used at CAG, site and organisational level to identify<br />
exemplars and areas of concern.<br />
<strong>Health</strong> Check tool designed to look at different aspects within<br />
wards /departments such as observation of practice, staff<br />
behaviour, patient experience, SI’s alongside other metrics to<br />
get a rounded picture of themes within an area /speciality.<br />
Safety thermometer tool to asses harm free care within the<br />
ward in patient areas and community services. A monthly<br />
audit is undertaken looking at 6 areas and output forms part<br />
of CAG Dashboards.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
Risk Management Committee tracks key risks and issues<br />
escalated to TMB as required.<br />
RMC rolling programme of drill down reviews for CAGs and<br />
Directorates.<br />
QAC rolling programme of drill down reviews for CAGs.<br />
Triangulation through Clinical Fridays, NED walkrounds.<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: A lack of transparency regarding<br />
possible team working arrangements or<br />
working in silos.<br />
Action: Focus at QAC and RMC on higher risk<br />
areas (e.g. smaller, niche services such as<br />
screening services)<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
Ward accreditation process to asses harm free care within the<br />
ward in patient areas and community services. A monthly<br />
audit is undertaken looking at 6 areas and output forms part<br />
of CAG Dashboards.<br />
Integrated Performance Framework with increased focus on<br />
staff, stakeholder and patient perception of performance.<br />
Staff engagement led by Chief Executive with support from<br />
Human Resources, OD, Communications and Governance<br />
functions. Professional leadership arrangements led by Chief<br />
Nurse and Medical Director.<br />
OD and leadership work to develop capability, team working<br />
and succession planning arrangements<br />
HR processes to support staff raising concerns<br />
(whistleblowing).<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
137, 138 Failure to improve the organisational culture (Risk scores – 16,20, lead – Director of HR)<br />
981, 988 Staff engagement (Risk scores – 15, 15, lead – Director of HR)<br />
6
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: B. Financial management<br />
Sub Objective: B6. Deliver the <strong>Trust</strong>’s 2012/13 financial plan, and cost improvement target, and develop a sustainable long term financial plan (LTFM).<br />
PRINCIPAL RISKS<br />
Description of risk<br />
7. Underachievement of CIPs<br />
and other expenditure<br />
controls leads to increased<br />
challenge to LTFM in<br />
subsequent years and to<br />
ongoing financial<br />
sustainability<br />
Executive lead: Chief<br />
Financial Officer<br />
Subcommittee role: Finance<br />
and Investment Committee<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (4x5=20)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcome 26<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
CIP challenge identified in 3 year LTFM. Dedicated resources<br />
including Director of Recovery post and PMO team in place to<br />
support CAGs and Departments to identify and deliver CIPs.<br />
Procurement of additional external support for identifying<br />
and validating 2013/14 CIPs schemes.<br />
CIPs risk assessment process to identify any efficiency, quality<br />
or safety issues and to identify cross‐cutting themes.<br />
Budgetary management controls supported by Finance and<br />
embedded finance managers.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
<strong>Trust</strong> Management <strong>Board</strong> and Finance and Investment<br />
Committee oversight of CIPs and LTFM.<br />
CIPs tracker tool.<br />
Strategic Cost Improvement <strong>Board</strong> meets monthly chaired<br />
by the Chief Executive.<br />
External assurance:<br />
Management assurance:<br />
Framework being developed to quality assure CIPs<br />
schemes<br />
Management assurance:<br />
Financial position and run rate monitored at performance<br />
reviews.<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Identification of 2013/14 CIPs<br />
significantly behind schedule at Month 11,<br />
2012/13.<br />
Action: Steps being taken to identify additional<br />
schemes and strengthen existing schemes RAG<br />
rated as red or amber.<br />
Detail: Framework not yet gone live for quality<br />
assuring schemes<br />
Action: Launch details to be confirmed.<br />
Detail: Inconsistent application of budgetary<br />
controls.<br />
Action:<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
143, 157, 217 QIPP/CIP Plans delivery for 2012/13 (Risk Scores ‐ 16, 15, 16, lead – Chief Financial Officer)<br />
164 Deliver the planned run rate as per the agreed plan for 2012/13 (Risk Score ‐ 15, lead – Chief Financial Officer)<br />
7
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: B. Financial management<br />
Sub Objective: B6. Deliver the <strong>Trust</strong>’s 2012/13 financial plan, and cost improvement target, and develop a sustainable long term financial plan (LTFM).<br />
PRINCIPAL RISKS<br />
Description of risk<br />
8. Cost improvement plans<br />
involve workforce changes<br />
and temporary staffing<br />
controls that adversely<br />
impact on quality and safety<br />
Executive lead: Medical<br />
Director and Chief Nurse<br />
Subcommittee role: Quality<br />
Assurance Committee<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (5x3=15)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 12, 13,<br />
16<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
Dedicated resources including Director of Recovery post and<br />
team in place to support CAGs and Departments to identify<br />
and deliver CIPs (with additional external support for<br />
identifying the 2013/14 CIPs schemes).<br />
CIPs risk assessment process to identify any efficiency, quality<br />
or safety issues and to identify cross‐cutting themes. Process<br />
includes clinical sign‐off on schemes (with escalation<br />
arrangements in place). Identified arrangements to capture<br />
any unintended consequences of schemes and revisit risk<br />
profile of CIPs programme.<br />
Embedded processes to capture staff and patient feedback<br />
regarding suitability of staffing and experience.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
<strong>Trust</strong> Management <strong>Board</strong> and Finance and Investment<br />
Committee oversight of CIPs and LTFM<br />
External assurance:<br />
Deloitte review of quality governance framework.<br />
Management assurance:<br />
<strong>Trust</strong> Management <strong>Board</strong> and Finance and Investment<br />
Committee oversight of CIPs and LTFM.<br />
Framework being developed to quality assure CIPs<br />
schemes<br />
External assurance:<br />
CQC inspections covering Outcome 12<br />
Management assurance:<br />
Clinical Fridays and NED walkrounds using 15 Steps tool<br />
help to triangulate formal feedback mechanisms.<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Framework not yet gone live for quality<br />
assuring schemes<br />
Action: Launch details to be confirmed.<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
143, 157, 217 QIPP/CIP Plans delivery for 2012/13 (Risk Scores ‐ 16, 15, 16, lead – Chief Financial Officer)<br />
142 Workforce reduction and service changes (Risk Score ‐ 15, lead – Chief Operating Officer)<br />
145, 147 Bank and agency staff spend (Risk scores – 16, 20, lead – ECAM CAG, Chief Financial Officer)<br />
8
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: C. Achieving FT status/post‐merger integration<br />
Sub Objective: C.8 Deliver the post‐merger integration plan including the clinical due diligence action plan and corporate and clinical services management integration<br />
PRINCIPAL RISKS<br />
Description of risk<br />
9. The lack of sufficiently<br />
robust workforce information<br />
impairs decision‐making and<br />
the optimal use of workforce<br />
resources to deliver safe<br />
patient care efficiently.<br />
Executive lead: Director of<br />
Human Resources<br />
Subcommittee role: Audit<br />
and Risk Committee<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (5x3=15)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 12, 13,<br />
14, 16<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
Development of the Electronic Staff Record as the key<br />
resource for workforce information. Reconciliations to the<br />
financial ledger carried out and exercises to capture<br />
organisational structure changes to ensure accuracy of ledger<br />
and ESR. Work to develop ESR’s OLM training functionality<br />
and interim solutions in place to record statutory and<br />
mandatory training.<br />
Pre and post employment checks, policies and procedures in<br />
place to ensure a safe workforce. Action plan in place<br />
following look back exercise to address gaps on CRB checks.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
<strong>Trust</strong> Management <strong>Board</strong> and Finance and Investment<br />
Committee oversight of CIPs and LTFM<br />
External assurance:<br />
CRB external review (of <strong>Barts</strong> and The London sites).<br />
Management assurance:<br />
Workforce Resourcing Assurance Group established to<br />
oversee delivery of action plan.<br />
Audit and Risk Committee and Quality Assurance<br />
Committee receives regular assurance reports on<br />
workforce<br />
Independent assurance:<br />
Internal Audit reviews of employment checks<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Further work required to assess and<br />
evidence completion of all pre‐employment<br />
checks from legacy sites<br />
Action: Manual checks of personnel files and<br />
additional CRB processes implemented<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
1032 CRB checks (Risk score – 15, Lead – Director of HR)<br />
926 Retention of key talent (Risk score – 20, Lead – Director of HR)<br />
1034 Right to Work in UK (Risk score – 15, Lead – Director of HR)<br />
1035 Safe Practice Assurance/Professional Registration Checks (Risk score – 15, Lead – Director of HR)<br />
1036 Honorary contracts (Risk score – 15, Lead – Director of HR)<br />
1037 Clinical observers (Risk score – 15, Lead – Director of HR)<br />
1041 Overpayments (Risk score – 16, Lead – Director of HR)<br />
i<br />
9
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: C. Achieving FT status/post‐merger integration<br />
Sub Objective: C.8 Deliver the post‐merger integration plan including the clinical due diligence action plan and corporate and clinical services management integration<br />
PRINCIPAL RISKS<br />
Description of risk<br />
10. Non‐compliance with<br />
mandatory systems and<br />
policies and a failure to<br />
engage staff on its<br />
importance adversely<br />
impacts on safety and<br />
efficiency.<br />
Executive lead: Chief<br />
Executive<br />
Subcommittee role: ‐<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (5x4=20)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 12, 14<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
Performance management framework supported by policies<br />
and procedures, OD and leadership development and<br />
performance reporting (identifying objectives, quality<br />
priorities and staff, patient and stakeholder perceptions).<br />
Increasing focus of TMB, QAC and ARC on holding individuals<br />
to account (for example on salary overpayments).<br />
Development of brand standards for CAGs and Directorates<br />
identifying service imperatives, expectations of staff and<br />
escalation arrangements.<br />
<strong>Barts</strong> <strong>Health</strong> Improvement System to develop culture of<br />
continuous improvement and maximise resources.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
<strong>Trust</strong> <strong>Board</strong> and assurance committee workplans prioritise<br />
development of an effective <strong>Trust</strong> strategy and culture that<br />
supports the vision and values of the organisation.<br />
Management assurance:<br />
<strong>Trust</strong> Management <strong>Board</strong> to receive regular updates and<br />
drive delivery.<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Lack of a comprehensive and consistent<br />
approach to holding to account for noncompliance.<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
137, 138 Failure to improve the organisational culture (Risk scores – 16,20, lead – Director of HR)<br />
981, 988 Staff engagement (Risk scores – 15, 15, lead – Director of HR)<br />
146, 1372 Failure to comply with statutory and mandatory training targets (risk score – 15, 16, lead ‐ Director of Corporate Affairs, Director of AHS)<br />
77 Failure to implement effective infection control framework (risk score – 25, lead – Medical Director)<br />
1099 Effective management of senior medical staff, supporting revalidation (risk score – 16, lead – Medical Director)<br />
10
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: D. Strategy<br />
Sub Objective: n/a.<br />
PRINCIPAL RISKS<br />
Description of risk<br />
11. A failure to develop a<br />
Clinical Strategy consistent<br />
with the LTFM and delivery<br />
of merger full business case<br />
benefits impacts on the<br />
organisation’s Foundation<br />
<strong>Trust</strong> trajectory.<br />
Executive lead: Director of<br />
Strategy<br />
Subcommittee role: <strong>Trust</strong><br />
<strong>Board</strong> (in capacity as FT<br />
Project <strong>Board</strong>)<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (5x3=15)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 6, 10,<br />
26<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
Dedicated Strategy team led by Director of Strategy working with<br />
CAGs to develop a Clinical Strategy for <strong>Barts</strong> <strong>Health</strong>.<br />
FT programme structure and governance mechanisms to address<br />
key workstreams.<br />
Clinical engagement in development of the clinical strategy to<br />
ensure that this is viable and patient‐focused.<br />
Development of CAG strategies and brand standards for CAGs and<br />
Directorates identifying strategic aspirations, service imperatives,<br />
expectations of staff and escalation arrangements.<br />
Regular updates of the LTFM to ensure clarity on the financial<br />
envelope for developing clinical services.<br />
Estates options appraisals being developed to inform commercial<br />
plans.<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
<strong>Trust</strong> <strong>Board</strong> and assurance committee workplans prioritise<br />
development of an effective <strong>Trust</strong> strategy and culture that<br />
supports the vision and values of the organisation.<br />
<strong>Trust</strong> <strong>Board</strong> away day and challenge from McKinseys on<br />
proposed approach.<br />
External assurance:<br />
External support for development of Clinical Strategy.<br />
Management assurance:<br />
Close involvement of clinical leaders in strategy<br />
development through the Leadership Group and Strategic<br />
Advisory Group.<br />
Management assurance:<br />
Staff survey<br />
Management assurance:<br />
Finance and Investment Committee oversight of LTFM and<br />
commercial strategy. WDS Advisory Group led by NEDs<br />
provides advice to the <strong>Board</strong> on estates options.<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Potential for external reconfiguration/<br />
designations to impact on the development of a<br />
clinical strategy.<br />
Action: Horizon scanning and development of<br />
key partnerships including UCLP, AHS structures<br />
and academic links.<br />
Detail: Steps required to understand the cost<br />
implications of CAG strategies and fit against<br />
Service Line Management profitability analyses.<br />
Action: Development of matrix to assess CAG<br />
strategies, including costs and risks.<br />
Detail: Potential for external factors to limit the<br />
available options for the clinical strategy.<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
932 Medical workforce – failure to realise benefits of economies of scale on 24/7 cover (Risk score – 16, lead – Medical Director)<br />
976 Non‐delivery of Full Business Case deliverables (Risk score – 16, lead – Development Director)<br />
993 Public <strong>Health</strong> – lack of focus on health improvement (Risk score – 16, lead Medical Director)<br />
11
APPENDIX 2 – BOARD ASSURANCE FRAMEWORK – QUARTER 4 2012/13 TB 31/13b<br />
Objective Heading: E. Academic <strong>Health</strong> Sciences<br />
Sub Objective: n/a<br />
PRINCIPAL RISKS<br />
Description of risk<br />
12. Statutory and mandatory<br />
training non‐compliance<br />
results in patient safety risks<br />
and impairs quality of care.<br />
Executive lead: Director of<br />
Academic <strong>Health</strong> Sciences<br />
Subcommittee role: ‐<br />
CURRENT RISK<br />
SCORE<br />
[CxL]<br />
Current risk score,<br />
and relevant CQC<br />
Outcome;<br />
Current risk –<br />
Quarter 4 risk<br />
score: (3x4=12)<br />
Outset risk: As<br />
above<br />
Essential<br />
Standard:<br />
Outcomes 12, 14<br />
KEY CONTROLS<br />
(numbers in brackets indicate controls relating to<br />
Identified related high risks)<br />
Most significant controls/systems in place to assist in securing<br />
delivery of objective and managing principal risks:<br />
Capacity and delivery analysis.<br />
Training Needs Analyses for all staff groups.<br />
Monthly compliance report to CAGs and Directorates.<br />
Changes made in terms of training delivery (more e‐learning).<br />
Steps taken to identify particular areas of non‐compliance to<br />
flag for priority notification to CAGs<br />
ASSURANCES ON CONTROLS<br />
Does the available assurance [process outlined below] provide<br />
evidence that controls/systems, on which we are placing reliance,<br />
are effective? (Indicate if management, internal audit or<br />
independent assurance)<br />
Management assurance:<br />
Education and Training <strong>Board</strong> monitors progress.<br />
Training compliance reported in Integrated Performance<br />
Framework and reviewed at performance reviews.<br />
Regular updates to QAC on<br />
Internal Audit review provided significant assurance on<br />
processes for training provision.<br />
GAPS IN CONTROL / ASSURANCE<br />
Where are we failing to a) put effective controls/systems<br />
in place? b) gain evidence that controls are effective<br />
Detail: Lack of a comprehensive and consistent<br />
approach to holding to account for noncompliance.<br />
Action: Monitoring at PRs. Links to appraisal<br />
and individual performance assessments<br />
established.<br />
TARGET RISK<br />
SCORE<br />
Target (by Q4<br />
unless stated)<br />
Q4 2013/14<br />
target to be<br />
confirmed<br />
Datix ref: tbc<br />
Related high<br />
risks >15 on the<br />
risk register –<br />
Datix refs:<br />
(See table below)<br />
Related high risks (>15 at outset) on the risk register – Datix refs:<br />
56, 852 Statutory & Mandatory training ‐ access to & provision of training (Risk Score 16, Lead – Director of AHS)<br />
931 Safeguarding children training coverage below commissioners requirements<br />
146, 1372 Failure to comply with statutory and mandatory training targets (risk score – 15, 16, lead ‐ Director of Corporate Affairs, Director of AHS)<br />
12
Report to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013 TB 32/13<br />
Title<br />
Sponsoring Director<br />
Author(s)<br />
Purpose<br />
Previously considered by<br />
<strong>Trust</strong> <strong>Board</strong> membership<br />
Director of Corporate Affairs and <strong>Trust</strong> Secretary<br />
As above<br />
To note the reappointments of a Non Executive Director of<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong>.<br />
n/a<br />
Executive summary<br />
The previous term of office of Professor Richard Trembath as University Nominated Non<br />
Executive Director of <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> ended on 31 March 2013.<br />
The <strong>NHS</strong> <strong>Trust</strong> Development Authority has confirmed Professor Trembath’s<br />
reappointment to this position for a further term from 1 April 2013 to 31 March 2015.<br />
Related <strong>Trust</strong> objectives<br />
n/a<br />
Risk and Assurance<br />
Related Assurance<br />
Framework entries<br />
Legal<br />
implications/regulatory<br />
requirements<br />
Sub‐objectives<br />
The appointments have been made in accordance with the<br />
Commissioner for Public Appointments Code of Practice.<br />
n/a<br />
See ‘Risk and Assurance’ above.<br />
Action required by the <strong>Board</strong><br />
The <strong>Trust</strong> <strong>Board</strong> is asked to note the reappointment of Professor Richard Trembath as a<br />
Non Executive Director of <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong>.<br />
1
Report to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013 TB 33/13<br />
Title<br />
Sponsoring Director<br />
Author(s)<br />
Purpose<br />
Previously<br />
considered by<br />
Amendment to the <strong>Trust</strong>’s Standing Orders, Standing Financial<br />
Instructions and Reservation and Delegation of Powers<br />
Chief Financial Officer<br />
Associate Director of Finance<br />
Deputy <strong>Trust</strong> Secretary<br />
The purpose of this paper is to seek <strong>Board</strong> approval to make minor<br />
amendments to the <strong>Trust</strong>’s Standing Orders (SOs), Standing Financial<br />
Instructions (SFIs) and Reservations and Delegation of Powers.<br />
Audit and Risk Committee, 20 February 2013<br />
Executive summary<br />
The Standing Orders, Standing Financial Instructions and Reservations and Delegation of<br />
Powers set out the delegated responsibilities of both individuals and/or Committees. The<br />
paper sets out proposed changes to limits, thresholds and processes relating to<br />
procurement within the <strong>Trust</strong>’s current Standing Financial Instructions (SFIs). A wider<br />
review of the Standing Orders and Standing Financial Instructions will be conducted during<br />
2013/14 to address any further improvements that may be required.<br />
Related <strong>Trust</strong> objectives<br />
6. Deliver the <strong>Trust</strong>’s 2012/13 financial plan, and cost improvement target, and develop a<br />
sustainable long term financial plan (LTFM).<br />
Risk and Assurance<br />
Related Assurance<br />
Framework entries<br />
Legal implications/<br />
regulatory requirements<br />
n/a<br />
n/a<br />
The SOs and SFIs incorporate key legal and statutory<br />
requirements in relation to corporate and financial<br />
governance.<br />
Action required by the <strong>Board</strong><br />
The <strong>Trust</strong> <strong>Board</strong> is asked to approve the amendments to the <strong>Trust</strong>’s Standing Orders,<br />
Standing Financial Instructions and Reservations and Delegation of Powers.<br />
1
TB 33/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING: 10 APRIL 2013<br />
AMENDMENTS TO THE TRUST’S STANDING FINANCIAL INSTRUCTIONS<br />
INTRODUCTION<br />
1. The limits and thresholds relating to procurement within the <strong>Trust</strong>’s current<br />
Standing Financial Instructions (SFIs) have been reviewed and this paper details<br />
some proposed changes. A wider review of the Standing Orders and Standing<br />
Financial Instructions will be conducted during 2013/14 to address any further<br />
improvements that may be required.<br />
2. The Audit and Risk Committee endorsed the proposed changes at its meeting on<br />
20 February 2013. It was agreed that further review of e‐tendering arrangements<br />
would be undertaken by Internal Audit during 2013/14 to provide additional<br />
assurance.<br />
Proposed amendment to section 16.5: Obtaining quotations and tenders.<br />
3. The current limits are:<br />
Goods & Services (including Capital)*<br />
Less than £10,000 2 quotes<br />
Between £10,000 and £50,000 obtain<br />
minimum 4 quotes<br />
Between £50,000 and £100,000 obtain<br />
minimum 4 tenders<br />
Between £100,000 and OJEU obtain<br />
minimum 6 tenders<br />
Above OJEU threshold use EU tender<br />
Works (including Capital)*<br />
Less than £50,000 3 quotes<br />
Between £50,000 and £100,000 obtain<br />
minimum 4 tenders<br />
Between £100,000 and OJEU obtain<br />
minimum 6 tenders<br />
Above OJEU threshold: EU tender rules apply<br />
4. The proposed limits are:<br />
Goods and services (including capital)<br />
Up to £5,000: 1 verbal quotation<br />
(minimum)<br />
Between £5,000 and £50,000: 2 written<br />
quotations (minimum)<br />
Between £50,000 and OJEU Limit: 3<br />
written quotations (minimum)<br />
Over OJEU Limit: EU directive applies<br />
Works (including capital)<br />
Up to £50,000: 3 written quotations<br />
(minimum)<br />
Between £50,000 and £100,000: 4 written<br />
quotations (minimum)<br />
Between £100,000 to OJEU Limit: 4 tenders<br />
(minimum)<br />
Over OJEU Limit: EU directives apply<br />
2
TB 33/13<br />
5. The OJEU limits are currently £113k for Goods and Services and £4,348k for<br />
works.<br />
6. For all quotations and tenders over £50,000, all employees involved in evaluating<br />
and concluding contracts will continue to be obliged to complete a declaration of<br />
interest form.<br />
7. The rationale for the change is as follows:<br />
<br />
<br />
<br />
<br />
The current procedures for quotations and tenders are too cumbersome<br />
to ensure the timely delivery of contracts, which has resulted in a high<br />
number of waivers being produced.<br />
The reduction in the written quotations up to the OJEU limits is more<br />
practicable whilst ensuring effective competition of all high value orders.<br />
The majority of the contracts following merger have exceeded the OJEU<br />
limit.<br />
The proposed procedures have been benchmarked against similar <strong>Trust</strong>s<br />
(UCL Hospitals <strong>NHS</strong> Foundation <strong>Trust</strong>, Great Ormond Street Hospital for<br />
Children <strong>NHS</strong> Foundation <strong>Trust</strong> and Guy’s and Thomas’s <strong>NHS</strong> Foundation<br />
<strong>Trust</strong>).<br />
8. Guidance on commercial awareness will be issued to ensure that the <strong>Trust</strong> is<br />
competitive with its requests for pricing.<br />
Proposed amendments to section 16.6: E Tendering<br />
9. As part of the e tendering regime the proposal is to amend the requirements on<br />
opening of tenders, which is currently managed by the <strong>Trust</strong> Offices.<br />
10. Currently the requirement is that a minimum of two <strong>Trust</strong> directors (or one<br />
director plus the Deputy <strong>Trust</strong> Secretary) must be present for the opening of<br />
tenders.<br />
11. The proposal is that all <strong>Trust</strong> tenders conducted via the procurement e‐<br />
tendering portal may be unlocked by procurement, with procurement<br />
maintaining the tendering numbering system. For manual tenders, it is proposed<br />
to add the Associate <strong>Trust</strong> Secretary to the list of those authorised to open<br />
tenders.<br />
3
TB 33/13<br />
12. The rationale for the change and increased emphasis on e‐tendering is:<br />
a. The current paper based system is an inefficient process.<br />
b. All electronic tenders are locked by the system until the closing date and<br />
time has lapsed.<br />
c. The electronic system has a full audit trail with the forms being in PDF<br />
format.<br />
d. The Bravo e‐tendering system was audited by the internal auditors at<br />
Whipps Cross University Hospital before the merger.<br />
RECOMMENDATION<br />
13. The <strong>Trust</strong> <strong>Board</strong> is asked to approve the above amendments to the <strong>Trust</strong>’s<br />
Standing Orders and Standing Financial Instructions.<br />
Tracey Leforte<br />
Deputy Director of Procurement<br />
Martin Botterill<br />
Associate Director of Finance 5 April 2013<br />
4
Report to the <strong>Trust</strong> <strong>Board</strong>: 10 April 2013 TB 34/13<br />
Title<br />
Sponsoring Director<br />
Author(s)<br />
Purpose<br />
Previously considered by<br />
Use of the <strong>Trust</strong> Seal<br />
Director of Corporate Affairs and <strong>Trust</strong> Secretary<br />
As above<br />
To seek <strong>Trust</strong> <strong>Board</strong> ratification of use of the Seal, pursuant<br />
to Standing Order 21.2<br />
n/a<br />
Executive summary<br />
This paper documents the use of the <strong>Trust</strong> Seal on the following occasions:<br />
27 March 2013<br />
A Licence to Underlet relating to First floor, 51‐53 Bartholomew Close, London<br />
EC1A 7HP between <strong>Barts</strong> Two Investment Property Limited, <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong><br />
<strong>Trust</strong> and The Secretary of State for <strong>Health</strong>. (3 copies)<br />
A Sublease of Part of First floor, 51‐53 Bartholomew Close, London EC1A 7HP<br />
between <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> and The Secretary of State for <strong>Health</strong>.<br />
Related <strong>Trust</strong> objectives<br />
n/a<br />
Risk and Assurance<br />
Related Assurance Framework entries<br />
n/a<br />
n/a<br />
Legal implications/<br />
regulatory requirements<br />
The <strong>Trust</strong>’s lawyers were involved in drawing up the<br />
documents requiring sealing.<br />
Action required by the <strong>Board</strong><br />
The <strong>Trust</strong> <strong>Board</strong> is asked to ratify the use of the Seal on the occasions listed above.<br />
1
SELF-CERTIFICATION RETURNS<br />
Organisation Name:<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Monitoring Period:<br />
February 2013<br />
<strong>NHS</strong> <strong>Trust</strong> Oversight self certification template<br />
Returns to som@london.nhs.uk by noon on<br />
15th April 2013
<strong>NHS</strong> <strong>Trust</strong> Governance Declarations :<br />
2012/13 In-Year Reporting<br />
Name of Organisation: <strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Period: February 2013<br />
Organisational risk rating<br />
Each organisation is required to calculate their risk score and RAG rate their current performance, in addition to providing comment with regard to any<br />
contractual issues and compliance with CQC essential standards:<br />
Governance Risk Rating (RAG as per SOM guidance)<br />
Key Area for rating / comment by Provider<br />
Score / RAG rating*<br />
R<br />
Normalised YTD Financial Risk Rating (Assign number as per SOM guidance) 2<br />
* Please type in R, AR, AG or G and assign a number for the FRR<br />
Governance Declarations<br />
Declaration 1 or declaration 2 reflects whether the <strong>Board</strong> believes the <strong>Trust</strong> is currently performing at a level compatible with FT authorisation.<br />
Supporting detail is required where compliance cannot be confirmed.<br />
Please complete one of the two declarations below. If you sign declaration 2, provide supporting detail using the form below. Signature may be either hand<br />
written or electronic, you are required to print your name.<br />
Governance declaration 1<br />
The <strong>Board</strong> is sufficiently assured in its ability to declare conformity with all of the Clinical Quality, Finance and Governance elements of the <strong>Board</strong><br />
Statements.<br />
Signed by : Print Name :<br />
on behalf of the <strong>Trust</strong> <strong>Board</strong><br />
Acting in capacity as:<br />
Signed by:<br />
Print Name:<br />
on behalf of the <strong>Trust</strong> <strong>Board</strong><br />
Acting in capacity as:<br />
Governance declaration 2<br />
At the current time, the board is yet to gain sufficient assurance to declare conformity with all of the Clinical Quality, Finance and Governance elements of<br />
the <strong>Board</strong> Statements.<br />
Signed by : Print Name :<br />
Stephen O'Brien<br />
on behalf of the <strong>Trust</strong> <strong>Board</strong><br />
Acting in capacity as:<br />
Chairman<br />
Signed by:<br />
Print Name:<br />
Peter Morris<br />
on behalf of the <strong>Trust</strong> <strong>Board</strong><br />
Acting in capacity as:<br />
Chief Executive<br />
If Declaration 2 has been signed:<br />
For each target/standard, where the board is declaring insufficient assurance please state the reason for being unable to sign the declaration, and explain<br />
briefly what steps are being taken to resolve the issue. Please provide an appropriate level of detail. (Only 5 can be accommodated on this template - see<br />
attached for full exception report)<br />
Target/Standard:<br />
The Issue :<br />
Action :<br />
Target/Standard:<br />
The Issue :<br />
Action :<br />
Target/Standard:<br />
The Issue :<br />
Action :<br />
Target/Standard:<br />
The Issue :<br />
Action :<br />
Target/Standard:<br />
The Issue :<br />
Action :<br />
3. All medical practitioners have met the relevant requirements.<br />
The responsible officer and revalidation statute was enacted on 3rd December 2012 and all trusts are on a<br />
The <strong>Trust</strong> is compliant with the relevant responsible officer legislation as of December 2012 and had<br />
4. The trust will maintain a FRR ≥ 3 over the next 12 months.<br />
The <strong>Trust</strong>'s FRR is 2 in October 2012.<br />
The <strong>Trust</strong>'s FRR is currently at 2 due to the in year deficit. This position will improve to an FRR of 3 when<br />
7. All current key risks have been identified and addressed.<br />
Not currently possible to provide full assurance.<br />
Currently, there is robust evidence, knowledge and quantification of current risks but insufficient<br />
8. The board has considered all likely future risks.<br />
Not currently possible to provide full assurance.<br />
Our latest review of risk management integration as <strong>Barts</strong> <strong>Health</strong> re-confirmed our trajectory to have both<br />
9. The necessary planning, management and mitigation plans are in place to deliver the annual plan.<br />
Not currently possible to provide full assurance.<br />
New arrangements currently being developed for implementation following planned go live of new
<strong>Board</strong> Statements<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
February 2013<br />
For each statement, the <strong>Board</strong> is asked to confirm the following:<br />
For CLINICAL QUALITY, that:<br />
Response<br />
The <strong>Board</strong> is satisfied that, to the best of its knowledge and using its own processes and having had regard to the SOM's<br />
1<br />
Oversight Regime (supported by Care Quality Commission information, its own information on serious incidents, patterns<br />
of complaints, and including any further metrics it chooses to adopt), the trust has, and will keep in place, effective<br />
Yes<br />
arrangements for the purpose of monitoring and continually improving the quality of healthcare provided to its patients.<br />
The board is satisfied that plans in place are sufficient to ensure ongoing compliance with the Care Quality Commission’s<br />
2 Yes<br />
registration requirements.<br />
The board is satisfied that processes and procedures are in place to ensure all medical practitioners providing care on<br />
3 No<br />
behalf of the trust have met the relevant registration and revalidation requirements.<br />
For FINANCE, that:<br />
Response<br />
4 The board anticipates that the trust will continue to maintain a financial risk rating of at least 3 over the next 12 months.<br />
No<br />
5<br />
The board is satisfied that the trust shall at all times remain a going concern, as defined by relevant accounting standards<br />
in force from time to time.<br />
Yes<br />
For GOVERNANCE, that:<br />
Response<br />
6 The board will ensure that the trust at all times has regard to the <strong>NHS</strong> Constitution.<br />
Yes<br />
All current key risks have been identified (raised either internally or by external audit and assessment bodies) and<br />
7 No<br />
addressed – or there are appropriate action plans in place to address the issues – in a timely manner<br />
The board has considered all likely future risks and has reviewed appropriate evidence regarding the level of severity,<br />
8 No<br />
likelihood of occurrence and the plans for mitigation of these risks.<br />
The necessary planning, performance management and corporate and clinical risk management processes and<br />
9 mitigation plans are in place to deliver the annual plan, including that all audit committee recommendations accepted by No<br />
the board are implemented satisfactorily.<br />
An Annual Governance Statement is in place, and the trust is compliant with the risk management and assurance<br />
10 framework requirements that support the Statement pursuant to the most up to date guidance from HM Treasury<br />
No<br />
(www.hm-treasury.gov.uk).<br />
The board is satisfied that plans in place are sufficient to ensure ongoing compliance with all existing targets (after the<br />
11 application of thresholds) as set out in the Governance Risk Rating; and a commitment to comply with all commissioned No<br />
targets going forward.<br />
The trust has achieved a minimum of Level 2 performance against the requirements of the Information Governance<br />
12 No<br />
Toolkit.<br />
The board will ensure that the trust will at all times operate effectively. This includes maintaining its register of interests,<br />
13<br />
ensuring that there are no material conflicts of interest in the board of directors; and that all board positions are filled, or<br />
plans are in place to fill any vacancies, and that any elections to the shadow board of governors are held in accordance<br />
Yes<br />
with the election rules.<br />
The board is satisfied that all executive and non-executive directors have the appropriate qualifications, experience and<br />
14 skills to discharge their functions effectively, including setting strategy, monitoring and managing performance and risks, Yes<br />
and ensuring management capacity and capability.<br />
The board is satisfied that: the management team has the capacity, capability and experience necessary to deliver the<br />
15 Yes<br />
annual plan; and the management structure in place is adequate to deliver the annual plan.<br />
Signed on behalf of the <strong>Trust</strong>: Print name Date<br />
CEO Peter Morris Peter Morris 10-Apr-13<br />
Chair Stephen O'Brien Stephen O'Brien 10-Apr-13
QUALITY<br />
Information to inform discussion meeting<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Insert Performance in Month<br />
Criteria<br />
Unit Mar-12 Apr-12 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 <strong>Board</strong> Action<br />
1 SHMI - latest data Score 0.8 0.8 0.8 0.8 0.8 0.8 0.8 0.8 0.8 0.8 0.8<br />
This indicator remains consistent and positive for the whole trust. This figure is taken from<br />
the <strong>NHS</strong> Information Centre (<strong>NHS</strong>IC) publication in January 2013 for the period up to June<br />
2012. <strong>Barts</strong> <strong>Health</strong>’s SHMI at 0.84 places it 10th position in a list of relevant healthcare<br />
organisations in England which measure the indicator of deaths associated with<br />
hospitalisation.<br />
Sixteen trusts had a ‘significantly lower than expected’ SHMI (between 0.71 and 0.87)<br />
indicating a 13% to 29% lower than expected mortality rate. <strong>Barts</strong> <strong>Health</strong> is in this group<br />
and is also the largest organisation in the sample with 159,820 hospital cases. Given the<br />
size of <strong>Barts</strong> <strong>Health</strong>, there were 717 less deaths than expected.<br />
2<br />
Venous Thromboembolism (VTE)<br />
Screening<br />
% 90.31 91.06 91.04 91.13 91.13 92.09 90.65 89.83 87.56 88.58 90.25<br />
Recording of VTE assessment has recovered to above the 90% level this month due to a<br />
widespread daily focus on delivery and is on an upward trajectory for March. Recording at<br />
Whipps Cross Hospital remains a problem, where we still rely on paper systems to record<br />
VTE assessment. Our IT strategy aims to deal with this by implementing Cerner Millenium<br />
Care records service as quickly as possible – though this will be at least 18-24 months away.<br />
In the interim the Clinical Academic Groups (CAGs) are receiving the VTE data now by site<br />
as well as by CAG. This data is now presented for each working date and can drill down to<br />
ward level. The data is subject to monthly scrutiny at executive led performance reviews<br />
and the accountability framework has been re-emphasised to support delivery . The cohort<br />
basis for low risk patients is well established. A VTE <strong>Board</strong> to cover the whole <strong>Trust</strong> (taking<br />
over from the separate arrangements prior to 1st October) has been established, chaired<br />
by the Medical Director with a focus on all 3 aspects of the future CQUIN.<br />
3a Elective MRSA Screening % 121 103 99 91 93 94.17 92.5 100.1 137.8 92.8 To follow<br />
Significant work has been undertaken to develop a report that is based on combined<br />
laboratory and admissions data in order to match at a patient level. The old report used to<br />
take unmatched tests and admissions and it was therefore possible to get performance in<br />
excess of 100% (due to multiple tests being undertaken on some patients).<br />
<strong>Barts</strong> <strong>Health</strong> is co-locating its laboratory services at the Royal London site and<br />
consolidating its admissions data on to a single platform which are a prerequisites to<br />
proving accurate reporting.<br />
3b Non Elective MRSA Screening % 128 99 94 112 96 111.35 101.8 100.9 78.4 89.5 To follow<br />
Significant work has been undertaken to develop a report that is based on combined<br />
laboratory and admissions data in order to match at a patient level. The old report used to<br />
take unmatched tests and admissions and it was therefore possible to get performance in<br />
excess of 100% (due to multiple tests being undertaken on some patients).<br />
<strong>Barts</strong> <strong>Health</strong> is co-locating its laboratory services at the Royal London site and<br />
consolidating its admissions data on to a single platform which are a prerequisites to<br />
proving accurate reporting.<br />
4 Single Sex Accommodation Breaches Number 3 31 29 3 1 0 0 24 129 125 124<br />
5<br />
Open Serious Incidents Requiring<br />
Investigation (SIRI)<br />
Number 31 37 26 40 41 25 24 39 27 21 33<br />
6 "Never Events" occurring in month Number 1 3 1 1 2 0 0 0 3 0 1<br />
7 CQC Conditions or Warning Notices Number 0 0 0 0 0 0 0 0 0 0 0<br />
Increases in reported figures over the past few months reflects a reporting system within<br />
critical care that was not as robust as it could have been. As a result of this, an increase in<br />
reporting has been seen. Work is underway to address the causes of these breaches.<br />
Pressures on critical care beds/ lack of step-down beds, including an increase in<br />
tracheostomy patients has had a significant impact. Remedial action is in place to address<br />
the causal factors.<br />
There were 33 new SIs reported in February 2013. As of 1 March 2013, there were 81<br />
overdue SIs. This comprised of 19 legacy incidents (down from 27 last month) and the<br />
central Patient Safety and Governance & Standards Teams are working with the CAG teams<br />
to complete the overdue investigations and reports in line with our recovery plan. The aim<br />
is try to achieve closure of all the legacy incidents by 31 March.<br />
There are 62 overdue SI reports identified since 1/10/12 and the CAG teams are working<br />
We have undertaken a review of all never events in the last year, we have focused work on<br />
the retention of foreign object never event on all sites. There was one Never Event<br />
reported but the incident happened in January 2013, relating to a maternity case. The<br />
Women’s CAG have subsequently published a ‘hot topic’ memo to all staff to avoid future<br />
incidents.<br />
A draft QCQ compliance report for the Whipps Cross Q&E and Older Person's Services<br />
review in November, indicated one area of minor non-compliance in respect of outcome<br />
14, supporting staff.<br />
On 18 February CQC carried out an unannounced compliance review at Mile End Hospital,<br />
visiting two elderly service wards and a further compliance review at St <strong>Barts</strong> Hospital<br />
(cancer services). The <strong>Trust</strong> has received a draft report with positive findings and fully met<br />
judgements.<br />
8<br />
Open Central Alert System (CAS)<br />
Alerts<br />
Number 38 43 50 30 19 20 23 27 3 1 0<br />
Since end Oct, we made a concerted effort to get all overdue alerts actioned/closed off and<br />
managed to acheive our target of zero overdue alerts.<br />
Six new CAS alerts received in February all have been closed.<br />
The remaining open alerts, and actions to ensure compliance with the Estates & Facilities<br />
(tamper free window restrictors) alert are nearing completion and on track to be<br />
completed by the target of 23/05/13.<br />
9<br />
RED rated areas on your maternity<br />
dashboard?<br />
Number 1 0 0 0 0 0 0 0 0 0 0<br />
Maternity dashboard in development across all BH sites however this work is not yet<br />
complete.<br />
10<br />
Falls resulting in severe injury or<br />
death<br />
Number 0 0 2 1 0 0 0 0 0 0 0 Reducing falls is a BH 2012 quality improvement priority<br />
11 Grade 3 or 4 pressure ulcers Number 7 16 9 8 13 14 9 8 16 11 7<br />
This is a BH 2012 quality priority, focus on reducing all grades, particularly grade 4, working<br />
to a zero tolerance approach<br />
12<br />
100% compliance with WHO surgical<br />
checklist<br />
Y/N N N N Y Y N N N N N N<br />
A report considering never events at BH and legacy organisations, has recommendationed<br />
a review of the WHO checklist approaches adopted so far and work to identify a new coordinated<br />
programme of action to promote consistent practice.<br />
The medical Direcotr has circulated a joint communication with the President of the Royal<br />
Colelge of Surgeons to all surgeons and procedure leads. The Chief Nurse has likewise<br />
emphasised the importance to all other staff groups.<br />
13 Formal complaints received Number 115 182 155 191 150 111 89 184 144 178 132 The reduction in formal complaints received has continued.<br />
14<br />
Agency as a % of Employee Benefit<br />
Expenditure<br />
% 5.10% 4.47% 4.81% 4.43% 4.54% 5.28% 4.58% 5.00% 5.10% 5.58% 4.99%<br />
Controls to manage agency use continue and authorisation for agency posts is held at<br />
senior levels within CAGs. Assurance is required that controls are being fully implemented.<br />
A recruitment drive for posts which require temporary cover commenced across <strong>Barts</strong><br />
<strong>Health</strong> in December. Augmenting the Bank pool and improving the “time to hire” period<br />
are also core objectives to reduce agency spend.<br />
15 Sickness absence rate % 3.24% 3.24% 3.20% 3.14% 3.10% 3.09% 3.09% 3.11% 3.45% 3.45% To follow<br />
Current reporting is being improved and this will increase reported sickness levels.<br />
Capacity issues in Occupational <strong>Health</strong> are being addressed and this will help augment<br />
management action where appropriate.<br />
16<br />
Consultants which, at their last<br />
appraisal, had fully completed their<br />
previous years PDP<br />
% - - - - - - - - 85% 85% To follow<br />
Although there is an agreed process and policy for appraisals in place which includes<br />
review of previous years PDP objectives and whether they have been achived, this is not<br />
systematically monitored currently. We are putting in place a new computer system<br />
across <strong>Barts</strong> <strong>Health</strong> (e-portfoliio) to record PDPs and we will develop a system for recording<br />
an opinion by the appraiser on satisfactory completion of the PDP and a means of gaining<br />
assuranceThis system has been mandatory from 1 April.<br />
Audit taken from Staffing list on 13/02/2013. <strong>NHS</strong> Consultant, Locum <strong>NHS</strong> Consultant and<br />
Academic Clinicans staffing groups selected to provide figures for this return:<br />
Data Source : 2011-12 individual consultant appraisal documentation.
FINANCIAL RISK RATING<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Risk Ratings<br />
Insert the Score (1-5) Achieved for each<br />
Criteria Per Month<br />
Reported<br />
Position<br />
Normalised<br />
Position*<br />
Criteria Indicator Weight 5 4 3 2 1<br />
Year to<br />
Date<br />
Forecast<br />
Outturn<br />
Year to<br />
Date<br />
Forecast<br />
Outturn<br />
<strong>Board</strong> Action<br />
Underlying<br />
performance<br />
EBITDA margin % 25% 11 9 5 1
FINANCIAL RISK TRIGGERS<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Insert "Yes" / "No" Assessment for the Month<br />
Historic Data<br />
Current Data<br />
Criteria<br />
Qtr to<br />
Jun-12<br />
Qtr to<br />
Sep-12<br />
Qtr to<br />
Dec-12<br />
Jan-13 Feb-13 Mar-13<br />
Qtr to<br />
Mar-13<br />
<strong>Board</strong> Action<br />
1<br />
Unplanned decrease in EBITDA margin in two consecutive<br />
quarters<br />
No Yes No No No<br />
2<br />
Quarterly self-certification by trust that the normalised<br />
financial risk rating (FRR) may be less than 3 in the next<br />
12 months<br />
Yes Yes Yes Yes Yes<br />
Increased planned and actual I&E surpluses will improve the<br />
FRR to 3 (currently an I&E deficit).<br />
3<br />
Working capital facility (WCF) agreement includes default<br />
clause<br />
N/a N/a N/a N/a N/a N/a N/a<br />
4<br />
Debtors > 90 days past due account for more than 5% of<br />
total debtor balances<br />
Yes Yes Yes Yes Yes<br />
The <strong>Trust</strong> is continuing to pursue all debts vigorously and debt<br />
write off is a last resort.<br />
5<br />
Creditors > 90 days past due account for more than 5% of<br />
total creditor balances<br />
Yes Yes Yes Yes Yes<br />
Payments have been slower than plan as <strong>Trust</strong>-wide<br />
compliance with purchase ordering remains an issue. An<br />
executive led purchase to pay project has been launched.<br />
6<br />
Two or more changes in Finance Director in a twelve<br />
month period<br />
No No No No No<br />
7<br />
Interim Finance Director in place over more than one<br />
quarter end<br />
Yes No No No No<br />
8 Quarter end cash balance
Quality<br />
Patient Experience<br />
Effectiveness<br />
GOVERNANCE RISK RATINGS<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Insert YES, NO or N/A (as appropriate)<br />
See 'Notes' for further detail of each of the below indicators<br />
Area Ref Indicator Sub Sections<br />
Threshold<br />
Weighting<br />
Historic Data<br />
Qtr to Jun- Qtr to<br />
12 Sep-12<br />
Qtr to<br />
Dec-12<br />
Current Data<br />
Jan-13 Feb-13 Mar-13<br />
Qtr to<br />
Mar-13<br />
<strong>Board</strong> Action<br />
Referral to treatment information 50%<br />
1a<br />
Data completeness: Community services<br />
comprising:<br />
Referral information 50%<br />
Treatment activity information 50%<br />
1.0<br />
No<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
This metric applies to those services<br />
currently on an electronic system. While the<br />
majority of the community services are now<br />
on some form of electronic system, there are<br />
some areas where implementation of the<br />
EMIS Web system is still in progress or still<br />
to happen. T. We are now getting a regular<br />
CIDS data extract, which we have begun to<br />
test and are on track to begin reporting for<br />
April13<br />
1b<br />
Data completeness, community services:<br />
(may be introduced later)<br />
Patient identifier information 50% No No No No No See above<br />
Patients dying at home / care<br />
home<br />
50% No No No No No<br />
See above<br />
1c Data completeness: identifiers MHMDS 97% 0.5 N/a N/a N/a N/a N/a<br />
1c<br />
2a<br />
Data completeness: outcomes for patients<br />
on CPA<br />
From point of referral to treatment in<br />
aggregate (RTT) – admitted<br />
50% 0.5 N/a N/a N/a N/a N/a<br />
Maximum time of 18 weeks 90% 1.0 Yes Yes Yes No No<br />
2b<br />
From point of referral to treatment in<br />
aggregate (RTT) – non-admitted<br />
Maximum time of 18 weeks 95% 1.0 Yes Yes Yes Yes Yes<br />
2c<br />
From point of referral to treatment in<br />
aggregate (RTT) – patients on an<br />
incomplete pathway<br />
Maximum time of 18 weeks 92% 1.0 Yes Yes Yes Yes Yes<br />
2d<br />
Certification against compliance with<br />
requirements regarding access to<br />
healthcare for people with a learning<br />
disability<br />
N/A 0.5 No No No No No<br />
Working on policies and protocols across<br />
<strong>Barts</strong> <strong>Health</strong>.<br />
3a<br />
All cancers: 31-day wait for second or<br />
subsequent treatment, comprising :<br />
Surgery 94%<br />
Anti cancer drug treatments 98%<br />
Radiotherapy 94%<br />
1.0<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
3b<br />
All cancers: 62-day wait for first treatment:<br />
From urgent GP referral for<br />
suspected cancer<br />
From <strong>NHS</strong> Cancer Screening<br />
Service referral<br />
85%<br />
90%<br />
1.0<br />
No<br />
No<br />
No<br />
No<br />
No<br />
The IST have supported the organisation to<br />
develop a comprehensive Action Plan to<br />
remedy this indication during Q2. The Action<br />
Plan has been shared with Commissioners<br />
and is being monitored through our<br />
Performance Reviews. Q2 compliance was<br />
achieved for the 62 day target across <strong>Barts</strong><br />
<strong>Health</strong> as a whole (85.53%).<br />
3c<br />
All Cancers: 31-day wait from diagnosis to<br />
first treatment<br />
96% 0.5 Yes Yes Yes Yes Yes<br />
The IST have supported the organisation to<br />
develop a comprehensive Action Plan to<br />
remedy this indication during Q2. The Action<br />
Plan has been shared with Commissioners<br />
and is being monitored through our<br />
Performance Reviews. Q2 compliance was<br />
achieved for the 62 day target across <strong>Barts</strong><br />
<strong>Health</strong> as a whole (85.53%).<br />
3d<br />
Cancer: 2 week wait from referral to date<br />
first seen, comprising:<br />
all urgent referrals 93%<br />
for symptomatic breast patients<br />
(cancer not initially suspected)<br />
93%<br />
0.5 Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
3e<br />
A&E: From arrival to<br />
admission/transfer/discharge<br />
Maximum waiting time of four<br />
hours<br />
95% 1.0 Yes Yes Yes No No<br />
3f<br />
Care Programme Approach (CPA) patients,<br />
comprising:<br />
Receiving follow-up contact within<br />
7 days of discharge<br />
Having formal review<br />
within 12 months<br />
95%<br />
95%<br />
1.0<br />
N/a N/a N/a<br />
N/a<br />
N/a<br />
3g<br />
Minimising mental health delayed transfers<br />
of care<br />
≤7.5% 1.0 N/a N/a N/a N/a N/a<br />
3h<br />
Admissions to inpatients services had<br />
access to Crisis Resolution/Home<br />
Treatment teams<br />
95% 1.0 N/a N/a N/a N/a N/a<br />
3i<br />
Meeting commitment to serve new<br />
psychosis cases by early intervention<br />
teams<br />
95% 0.5 N/a N/a N/a N/a N/a<br />
3j<br />
Category A call – emergency response<br />
within 8 minutes<br />
Red 1 80% 0.5 N/a N/a N/a N/a N/a<br />
Red 2 75% 0.5 N/a N/a N/a N/a N/a<br />
3k<br />
Category A call – ambulance vehicle<br />
arrives within 19 minutes<br />
95% 1.0 N/a N/a N/a N/a N/a
Effectiveness<br />
Safety<br />
GOVERNANCE RISK RATINGS<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Insert YES, NO or N/A (as appropriate)<br />
See 'Notes' for further detail of each of the below indicators<br />
Area Ref Indicator Sub Sections<br />
1a<br />
Data completeness: Community services<br />
comprising:<br />
Threshold<br />
Weighting<br />
1.0<br />
Historic Data<br />
Qtr to Jun- Qtr to<br />
12 Sep-12<br />
No<br />
No<br />
Qtr to<br />
Dec-12<br />
Yes<br />
Current Data<br />
Jan-13 Feb-13 Mar-13<br />
Is the <strong>Trust</strong> below the de minimus 12 No No No No No<br />
4a Clostridium Difficile 1.0<br />
Is the <strong>Trust</strong> below the YTD ceiling 99 Yes Yes Yes Yes Yes<br />
Yes<br />
Yes<br />
Qtr to<br />
Mar-13<br />
<strong>Board</strong> Action<br />
The <strong>Trust</strong> is below the YTD trajectory, but<br />
with little margin for error. The <strong>Trust</strong> is above<br />
the de minimis level of course. From a first<br />
This metric applies to those services<br />
cut analysis undertaken by the deputy DIPC<br />
currently on an electronic system. While the<br />
we were able to detect avoidable cases of<br />
majority of the community services are now<br />
cross infection. 2 patients were<br />
on some form of electronic system, there are<br />
inappropriately sampled. All patients were on<br />
some areas where implementation of the<br />
antibiotics – but these were within formulary<br />
EMIS Web system is still in progress or still<br />
and properly indicated. Future RCAs will<br />
to happen. T. We are now getting a regular<br />
focus on detailed pharmacist analysis and<br />
CIDS data extract, which we have begun to<br />
the chief pharmacist will consolidate<br />
test and are on track to begin reporting for<br />
oversight of antibiotic husbandry reporting<br />
April13<br />
across the full trust Additional measures to<br />
improvse HCAI performance include more<br />
intensive local peer review led by CAGs with<br />
immediate actions, enhanced scrutiny of<br />
RCAs for MRSA and CDiff, with targeted<br />
actions to improve device management and<br />
adopt BH approach to antibiotic surveillance.<br />
4b<br />
MRSA<br />
Is the <strong>Trust</strong> below the de minimus 6 Yes No No No No<br />
1.0<br />
Is the <strong>Trust</strong> below the YTD ceiling 8 Yes Yes No No No<br />
Additional measures to improvse HCAI<br />
performance include more intensive local<br />
peer review led by CAGs with immediate<br />
actions, enhanced scrutiny of RCAs for<br />
MRSA and CDiff, with targeted actions to<br />
improve device management and adopt BH<br />
approach to antibiotic surveillance.<br />
A<br />
CQC Registration<br />
Non-Compliance with CQC Essential<br />
Standards resulting in a Major Impact on<br />
Patients<br />
0 2.0 No No No No No<br />
B<br />
Non-Compliance with CQC Essential<br />
Standards resulting in Enforcement Action<br />
0 4.0 No No No No No<br />
C<br />
<strong>NHS</strong> Litigation Authority – Failure to<br />
maintain, or certify a minimum published<br />
CNST level of 1.0 or have in place<br />
appropriate alternative arrangements<br />
0 2.0 No No No No No<br />
TOTAL 3.5 4.5 3.5 5.5 5.5 0.0 0.0<br />
RAG RATING : AR R AR R R G G<br />
GREEN = Score less than 1<br />
AMBER/GREEN = Score greater than or equal to 1, but less than 2<br />
AMBER / RED = Score greater than or equal to 2, but less than 4<br />
RED = Score greater than or equal to 4<br />
Overriding Rules - Nature and Duration of Override at SHA's Discretion<br />
Greater than six cases in the year to date, and breaches the<br />
i) Meeting the MRSA Objective cumulative year-to-date trajectory for three successive<br />
No No Yes Yes Yes<br />
quarters<br />
ii)<br />
Meeting the C-Diff Objective<br />
Greater than 12 cases in the year to date, and either:<br />
Breaches the cumulative year-to-date trajectory for three<br />
successive quarters<br />
Reports important or signficant outbreaks of C.difficile, as<br />
defined by the <strong>Health</strong> Protection Agency.<br />
No No No<br />
No<br />
No<br />
iii)<br />
RTT Waiting Times<br />
Breaches:<br />
The admitted patients 18 weeks waiting time measure for a<br />
third successive quarter<br />
The non-admitted patients 18 weeks waiting time measure<br />
for a third successive quarter<br />
The incomplete pathway 18 weeks waiting time measure for<br />
a third successive quarter<br />
No<br />
No<br />
No<br />
No<br />
No<br />
Fails to meet the A&E target twice in any two quarters over<br />
iv) A&E Clinical Quality Indicator a 12-month period and fails the indicator in a quarter during No No No No No<br />
the subsequent nine-month period or the full year.<br />
Breaches either:<br />
v) Cancer Wait Times<br />
the 31-day cancer waiting time target for a third successive<br />
quarter<br />
No<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
the 62-day cancer waiting time target for a third successive<br />
quarter<br />
vi)<br />
Ambulance Response Times<br />
Breaches:<br />
the category A 8-minute response time target for a third<br />
successive quarter<br />
the category A 19-minute response time target for a third<br />
successive quarter<br />
N/a<br />
N/a<br />
N/a<br />
N/a<br />
N/a<br />
either Red 1 or Red 2 targets for a third successive quarter<br />
Fails to maintain the threshold for data completeness for:<br />
vii) Community Services data completeness<br />
referral to treatment information for a third successive<br />
quarter;<br />
service referral information for a third successive quarter,<br />
or;<br />
No No No<br />
treatment activity information for a third successive quarter<br />
No<br />
No<br />
viii) Any other Indicator weighted 1.0 Breaches the indicator for three successive quarters.<br />
N/a N/a N/a No No<br />
Adjusted Governance Risk Rating 3.5 4.5 4.0 5.5 5.5 0.0 0.0<br />
AR R R R R G G
CONTRACTUAL DATA<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Information to inform discussion meeting<br />
Insert "Yes" / "No" Assessment for the Month<br />
Historic Data<br />
Current Data<br />
Criteria<br />
Qtr to<br />
Jun-12<br />
Qtr to<br />
Sep-12<br />
Qtr to<br />
Dec-12 Jan-13 Feb-13 Mar-13 Qtr to<br />
Mar-13<br />
<strong>Board</strong> Action<br />
1 Are the prior year contracts* closed? Yes Yes Yes Yes Yes<br />
2<br />
3<br />
Are all current year contracts* agreed and<br />
signed?<br />
Has the <strong>Trust</strong> received income support outside<br />
of the <strong>NHS</strong> standard contract e.g.<br />
transformational support?<br />
Yes Yes Yes Yes Yes<br />
Yes Yes Yes Yes Yes<br />
Main contracts signed on 14th September<br />
2012<br />
The <strong>Trust</strong> has received additional funding<br />
to support the transition as detailed the<br />
merger FBC and agreed by all relevant<br />
stakeholders.<br />
4<br />
5<br />
6<br />
Are both the <strong>NHS</strong> <strong>Trust</strong> and commissioner<br />
fulfilling the terms of the contract?<br />
Are there any disputes over the terms of the<br />
contract?<br />
Might the dispute require third party intervention<br />
or arbitration?<br />
Yes Yes Yes Yes Yes<br />
No No No No No<br />
N/a N/a N/a N/a No<br />
7 Are the parties already in arbitration? No No No No No<br />
8 Have any performance notices been issued? No No No No No<br />
9 Have any penalties been applied? No No No No No<br />
*All contracts which represent more than 25% of the <strong>Trust</strong>'s operating revenue.
TFA Progress<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Apr-13<br />
Select the Performance from the drop-down list<br />
TFA Milestone (All including those delivered)<br />
Milestone<br />
Date<br />
Performance<br />
<strong>Board</strong> Action<br />
1<br />
TFA - <strong>Board</strong> approval of BELH Merger OBC and support to moving to FBC<br />
stage<br />
Jul-11<br />
Fully achieved in time<br />
2 TFA - <strong>NHS</strong> L CIC consideration of OBC Aug-11 Fully achieved in time<br />
3<br />
TFA - Liquidity - complete assessment of cash/liquidity issues and scale of<br />
merger funding requirement together with identification of potential solutions<br />
Sep-11<br />
Fully achieved but late<br />
Confirmation of near-term transaction-related financing and longer-term<br />
transition costing required finalisation, including agreement from all<br />
stakeholders; status of business case funding (as specified in OBC);<br />
continuing challenge on aspects of financial/ performance position of<br />
merger partners.<br />
4 TFA - CCP response expected Nov-11 Fully achieved but late<br />
5 TFA - FBC to be finalised and taken to <strong>Trust</strong> board Nov-11 Fully achieved in time<br />
6 TFA - <strong>Trust</strong> <strong>Board</strong> approval of FBC Dec-11 Fully achieved in time<br />
7 TFA - <strong>NHS</strong> L Main <strong>Board</strong> approval of FBC Dec-11 Fully achieved in time<br />
8 TFA - Initial DH Transaction <strong>Board</strong> consideration of FBC Jan-12 Fully achieved in time<br />
9 TFA - Final DH Transaction <strong>Board</strong> consideration of FBC Feb-12 Fully achieved in time<br />
10 TFA - <strong>NHS</strong> Co-operation and Competition Panel (CCP) recommendation Feb-12 Fully achieved in time<br />
CCP Stage 2 review was extended (announced 14 November)<br />
FBC finalised on 25th November and taken to <strong>Trust</strong> <strong>Board</strong>s in early<br />
December .<br />
FBC, including transaction financing, approved by the <strong>Board</strong>s of BLT,<br />
Newham, Whipps Cross INEL and ONEL.<br />
FBC, including transaction financing, approved by <strong>NHS</strong> London <strong>Board</strong> on<br />
13 December.<br />
Informal consideration and feedback received 'no substantive concerns'<br />
DH Transaction <strong>Board</strong> considered merger on 9 February and submitted<br />
to the Secretary of State for Ministerial approval.<br />
CCP announced w/c 6 February that they would recommend to the<br />
Secretary of State for <strong>Health</strong> that the proposed merger goes ahead<br />
11 TFA - Complete commissioning of phase 1 of Royal London Hospital Mar-12 Fully achieved in time<br />
All services intended to move into the new Royal London Hospital<br />
transferred and the hospital opened on 1 March.<br />
12 TFA - Secretary of State approval Mar-12 Fully achieved in time<br />
13 TFA - <strong>Trust</strong> dissolved, <strong>Barts</strong> <strong>Health</strong> established Apr-12 Fully achieved in time<br />
14 TFA - 18 months trading (April 2012 - September 2013) Sep-13 On track to deliver<br />
15 TFA - Develop IBP / LTFM (April 2012 - September 2013) Sep-13 On track to deliver<br />
<strong>Barts</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> successfully established on the 1st April 2012.<br />
Quarter 1 and Quarter 2 trading arrangements based on post merger<br />
implementation plan. The eight Clinical Academic Groups (CAGs) went<br />
live in Quarter 3 2012/13<br />
Strategic and annual planning processes with CAGs commenced in<br />
Quarter 3 2012/13<br />
16 TFA - Public Consultation (July - September 2013) Jul-13<br />
17 TFA - HDD1 Jul-13<br />
18 TFA - HDD1 Actions *(August - September 2013) Aug-13<br />
19 TFA - HDD2 (October - November 2013) Oct-13<br />
20 TFA - HDD2 Actions (November - December 2013) Nov-13<br />
21 TFA - FT Application submission to DH Dec-13<br />
22 TFA - Secretary of State Approval Apr-14<br />
23 TFA - Submission to Monitor May-14<br />
24 TFA - Monitor Assessment Process (June - September 2014) Jun-14<br />
25 TFA - Working Capital Review Oct-14<br />
26 TFA - Target Authorisation Date Dec-14<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
Will not be delivered on<br />
time<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation was<br />
submitted to <strong>NHS</strong> London at the end of November and is currently being<br />
agreed. This will change the future milestones.<br />
27<br />
28<br />
29<br />
30<br />
31<br />
32<br />
33<br />
34<br />
35<br />
36<br />
37<br />
38<br />
39<br />
40
Notes<br />
Ref Indicator Details<br />
Thresholds<br />
1a<br />
1b<br />
1c<br />
The SHA will not utilise a general rounding principle when considering compliance with these targets and standards, e.g. a performance of 94.5% will be considered as failing to<br />
achieve a 95% target. However, exceptional cases may be considered on an individual basis, taking into account issues such as low activity or thresholds that have little or no<br />
tolerance against the target, e.g. those set between 99-100%.<br />
Data<br />
Completeness:<br />
Community<br />
Services<br />
Data<br />
Completeness<br />
Community<br />
Services (further<br />
data):<br />
Mental <strong>Health</strong><br />
MDS<br />
Data completeness levels for trusts commissioned to provide community services, using Community Information Data Set (CIDS) definitions, to<br />
consist of:<br />
- Referral to treatment times – consultant-led treatment in hospitals and Allied <strong>Health</strong>care Professional-led treatments in the community;<br />
- Community treatment activity – referrals; and<br />
- Community treatment activity – care contact activity.<br />
While failure against any threshold will score 1.0, the overall impact will be capped at 1.0. Failure of the same measure for three quarters will<br />
result in a red-rating.<br />
Numerator:<br />
all data in the denominator actually captured by the trust electronically (not solely CIDS-specified systems).<br />
Denominator:<br />
all activity data required by CIDS.<br />
The inclusion of this data collection in addition to Monitor's indicators (until the Compliance Framework is changed) is in order for the SHA to<br />
track the <strong>Trust</strong>'s action plan to produce such data.<br />
This data excludes a weighting, and therefore does not currently impact on the <strong>Trust</strong>'s governance risk rating.<br />
Patient identity data completeness metrics (from MHMDS) to consist of:<br />
- <strong>NHS</strong> number;<br />
- Date of birth;<br />
- Postcode (normal residence);<br />
- Current gender;<br />
- Registered General Medical Practice organisation code; and<br />
- Commissioner organisation code.<br />
1d<br />
Mental <strong>Health</strong>:<br />
CPA<br />
Numerator:<br />
count of valid entries for each data item above.<br />
(For details of how data items are classified as VALID please refer to the data quality constructions available on the Information Centre’s<br />
website: www.ic.nhs.uk/services/mhmds/dq)<br />
Denominator:<br />
total number of entries.<br />
Outcomes for patients on Care Programme Approach:<br />
• Employment status:<br />
Numerator:<br />
the number of adults in the denominator whose employment status is known at the time of their most recent assessment, formal review or other<br />
multi-disciplinary care planning meeting, in a financial year. Include only those whose assessments or reviews were carried out during the<br />
reference period. The reference period is the last 12 months working back from the end of the reported month.<br />
Denominator:<br />
the total number of adults (aged 18-69) who have received secondary mental health services and who were on the CPA at any point during the<br />
reported month.<br />
• Accommodation status:<br />
Numerator:<br />
the number of adults in the denominator whose accommodation status (i.e. settled or non-settled accommodation) is known at the time of their<br />
most recent assessment, formal review or other multi-disciplinary care planning meeting. Include only those whose assessments or reviews were<br />
carried out during the reference period. The reference period is the last 12 months working back from the end of the reported month.<br />
Denominator:<br />
the total number of adults (aged 18-69) who have received secondary mental health services and who were on the CPA at any point during the<br />
reported month.<br />
• Having a <strong>Health</strong> of the Nation Outcome Scales (HoNOS) assessment in the past 12 months:<br />
Numerator:<br />
The number of adults in the denominator who have had at least one HoNOS assessment in the past 12 months.<br />
Denominator:<br />
The total number of adults who have received secondary mental health services and who were on the CPA during the reference period.<br />
2a-c<br />
2d<br />
3a<br />
3b<br />
3c<br />
3d<br />
RTT<br />
Learning<br />
Disabilities:<br />
Access to<br />
healthcare<br />
Cancer:<br />
31 day wait<br />
Cancer:<br />
62 day wait<br />
Cancer<br />
Cancer<br />
Performance is measured on an aggregate (rather than specialty) basis and trusts are required to meet the threshold on a monthly basis.<br />
Consequently, any failure in one month is considered to be a quarterly failure. Failure in any month of a quarter following two quarters’ failure of<br />
the same measure represents a third successive quarter failure and should be reported via the exception reporting process.<br />
Will apply to consultant-led admitted, non-admitted and incomplete pathways provided. While failure against any threshold will score 1.0, the<br />
overall impact will be capped at 2.0. The measures apply to acute patients whether in an acute or community setting. Where a trust with existing<br />
acute facilities acquires a community hospital, performance will be assessed on a combined basis.<br />
The SHA will take account of breaches of the referral to treatment target in 2011/12 when considering consecutive failures of the referral to<br />
treatment target in 2012/13. For example, if a trust fails the 2011/12 admitted patients target at quarter 4 and the 2012/13 admitted patients<br />
target in quarters 1 and 2, it will be considered to have breached for three quarters in a row.<br />
Meeting the six criteria for meeting the needs of people with a learning disability, based on recommendations set out in <strong>Health</strong>care for All (DH,<br />
2008):<br />
a) Does the trust have a mechanism in place to identify and flag patients with learning disabilities and protocols that ensure that pathways of<br />
care are reasonably adjusted to meet the health needs of these patients?<br />
b) Does the trust provide readily available and comprehensible information to patients with learning disabilities about the following criteria:<br />
- treatment options;<br />
- complaints procedures; and<br />
- appointments?<br />
c) Does the trust have protocols in place to provide suitable support for family carers who support patients with learning disabilities?<br />
d) Does the trust have protocols in place to routinely include training on providing healthcare to patients with learning disabilities for all staff?<br />
e) Does the trust have protocols in place to encourage representation of people with learning disabilities and their family carers?<br />
f) Does the trust have protocols in place to regularly audit its practices for patients with learning disabilities and to demonstrate the findings in<br />
routine public reports?<br />
Note: trust boards are required to certify that their trusts meet requirements a) to f) above at the annual plan stage and in each month. Failure to<br />
do so will result in the application of the service performance score for this indicator.<br />
31-day wait: measured from cancer treatment period start date to treatment start date. Failure against any threshold represents a failure against<br />
the overall target. The target will not apply to trusts having five cases or less in a quarter. The SHA will not score trusts failing individual cancer<br />
thresholds but only reporting a single patient breach over the quarter.. Will apply to any community providers providing the specific cancer<br />
treatment pathways<br />
62-day wait: measured from day of receipt of referral to treatment start date. This includes referrals from screening service and other consultants.<br />
Failure against either threshold represents a failure against the overall target. The target will not apply to trusts having five cases or less in a<br />
quarter. The SHA will not score trusts failing individual cancer thresholds but only reporting a single patient breach over the quarter. Will apply to<br />
any community providers providing the specific cancer treatment pathways.<br />
National guidance states that for patients referred from one provider to another, breaches of this target are automatically shared and treated on a<br />
50:50 basis. These breaches may be reallocated in full back to the referring organisation(s) provided the SHA receive evidence of written<br />
agreement to do so between the relevant providers (signed by both Chief Executives) in place at the time the trust makes its monthly declaration<br />
to the SHA.<br />
In the absence of any locally-agreed contractual arrangements, the SHA encourages trusts to work with other providers to reach a local systemwide<br />
agreement on the allocation of cancer target breaches to ensure that patients are treated in a timely manner. Once an agreement of this<br />
nature has been reached, the SHA will consider applying the terms of the agreement to trusts party to the arrangement.<br />
Measured from decision to treat to first definitive treatment. The target will not apply to trusts having five cases or fewer in a quarter. The SHA<br />
will not score trusts failing individual cancer thresholds but only reporting a single patient breach over the quarter. Will apply to any community<br />
providers providing the specific cancer treatment pathways.<br />
Measured from day of receipt of referral – existing standard (includes referrals from general dental practitioners and any primary care<br />
professional).Failure against either threshold represents a failure against the overall target. The target will not apply to trusts having five cases or<br />
fewer in a quarter. The SHA will not score trusts failing individual cancer thresholds but only reporting a single patient breach over the quarter.<br />
Will apply to any community providers providing the specific cancer treatment pathways.<br />
Specific guidance and documentation concerning cancer waiting targets can be found at:<br />
http://nww.connectingforhealth.nhs.uk/nhais/cancerwaiting/documentation
Notes<br />
Ref Indicator Details<br />
3e<br />
A&E<br />
Waiting time is assessed on a site basis: no activity from off-site partner organisations should be included. The 4-hour waiting time indicator will<br />
apply to minor injury units/walk in centres.<br />
3f Mental 7-day follow up:<br />
Numerator:<br />
the number of people under adult mental illness specialties on CPA who were followed up (either by face-to-face contact or by phone discussion)<br />
within seven days of discharge from psychiatric inpatient care.<br />
Denominator:<br />
the total number of people under adult mental illness specialties on CPA who were discharged from psychiatric inpatient care.<br />
All patients discharged to their place of residence, care home, residential accommodation, or to non-psychiatric care must be followed up within<br />
seven days of discharge. Where a patient has been transferred to prison, contact should be made via the prison in-reach team.<br />
Exemptions from both the numerator and the denominator of the indicator include:<br />
- patients who die within seven days of discharge;<br />
- where legal precedence has forced the removal of a patient from the country; or<br />
- patients discharged to another <strong>NHS</strong> psychiatric inpatient ward.<br />
For 12 month review (from Mental <strong>Health</strong> Minimum Data Set):<br />
Numerator:<br />
the number of adults in the denominator who have had at least one formal review in the last 12 months.<br />
Denominator:<br />
the total number of adults who have received secondary mental health services during the reporting period (month) who had spent at least 12<br />
months on CPA (by the end of the reporting period OR when their time on CPA ended).<br />
3g<br />
Mental <strong>Health</strong>:<br />
DTOC<br />
For full details of the changes to the CPA process, please see the implementation guidance Refocusing the Care Programme Approach on the<br />
Department of <strong>Health</strong>’s website.<br />
Numerator:<br />
the number of non-acute patients (aged 18 and over on admission) per day under consultant and non-consultant-led care whose transfer of care<br />
was delayed during the month. For example, one patient delayed for five days counts as five.<br />
Denominator:<br />
the total number of occupied bed days (consultant-led and non-consultant-led) during the month.<br />
3h<br />
Mental <strong>Health</strong>: I/P<br />
and CRHT<br />
Delayed transfers of care attributable to social care services are included.<br />
This indicator applies only to admissions to the foundation trust’s mental health psychiatric inpatient care. The following cases can be excluded:<br />
- planned admissions for psychiatric care from specialist units;<br />
- internal transfers of service users between wards in a trust and transfers from other trusts;<br />
- patients recalled on Community Treatment Orders; or<br />
- patients on leave under Section 17 of the Mental <strong>Health</strong> Act 1983.<br />
3i<br />
3j-k<br />
Mental <strong>Health</strong><br />
Ambulance<br />
Cat A<br />
The indicator applies to users of working age (16-65) only, unless otherwise contracted. An admission has been gate-kept by a crisis resolution<br />
team if they have assessed the service user before admission and if they were involved in the decision-making process, which resulted in<br />
admission.<br />
For full details of the features of gate-keeping, please see Guidance Statement on Fidelity and Best Practice for Crisis Services on the<br />
Department of <strong>Health</strong>’s website. As set out in this guidance, the crisis resolution home treatment team should:<br />
a) provide a mobile 24 hour, seven days a week response to requests for assessments;<br />
b) be actively involved in all requests for admission: for the avoidance of doubt, ‘actively involved’ requires face-to-face contact unless it can be<br />
demonstrated that face-to-face contact was not appropriate or possible. For each case where face-to-face contact is deemed inappropriate, a<br />
declaration that the face-to-face contact was not the most appropriate action from a clinical perspective will be required;<br />
c) be notified of all pending Mental <strong>Health</strong> Act assessments;<br />
d) be assessing all these cases before admission happens; and<br />
e) be central to the decision making process in conjunction with the rest of the multidisciplinary team.<br />
Monthly performance against commissioner contract. Threshold represents a minimum level of performance against contract performance,<br />
rounded down.<br />
For patients with immediately life-threatening conditions.<br />
The Operating Framework for 2012-13 requires all Ambulance <strong>Trust</strong>s to reach 75 per cent of urgent cases, Category A patients, within 8 minutes.<br />
From 1 June 2012, Category A cases will be split into Red 1 and Red 2 calls:<br />
• Red 1 calls are patients who are suffering cardiac arrest, are unconscious or who have stopped breathing.<br />
• Red 2 calls are serious cases, but are not ones where up to 60 additional seconds will affect a patient’s outcome, for example diabetic<br />
episodes and fits.<br />
Ambulance <strong>Trust</strong>s will be required to improve their performance to show they can reach 80 per cent of Red 1 calls within 8 minutes by April 2013.<br />
4a<br />
4b<br />
C.Diff<br />
MRSA<br />
Will apply to any inpatient facility with a centrally set C. difficile objective. Where a trust with existing acute facilities acquires a community<br />
hospital, the combined objective will be an aggregate of the two organisations’ separate objectives. Both avoidable and unavoidable cases of C.<br />
difficile will be taken into account for regulatory purposes.<br />
Where there is no objective (i.e. if a mental health trust without a C. difficile objective acquires a community provider without an allocated C.<br />
difficile objective) we will not apply a C. difficile score to the trust’s governance risk rating.<br />
Monitor’s annual de minimis limit for cases of C. difficile is set at 12. However, Monitor may consider scoring cases of
Report<br />
to the <strong>Trust</strong> <strong>Board</strong>: 10 Aprill 2013<br />
TB 35/13<br />
Title<br />
Sponsoring Director<br />
Author( (s)<br />
Purpose<br />
Previously considered by<br />
Single Operating Model (SOM) – April A Self Certification<br />
Submissionn<br />
Director of Informatics<br />
and Chief Information Officer<br />
Director of Informatics<br />
and Chief Information Officer<br />
To seek <strong>Trust</strong> <strong>Board</strong> approval of the t April 2013 self‐certification<br />
return of the Single Operating Model, reporting February 2013<br />
data (to bee submitted to the <strong>NHS</strong>S <strong>Trust</strong> Development Authority<br />
on 15 April 2013).<br />
<strong>Trust</strong> Executive, 2 April 2013<br />
Executive summary<br />
The ratings for this<br />
month’s self‐certification return are:<br />
Key area for rating<br />
Governance Risk Rating (GRR)<br />
Score<br />
5.5<br />
RAG rating<br />
Red<br />
Financial Risk Rating (FRR)<br />
2<br />
Red<br />
Related<br />
<strong>Trust</strong> objectives<br />
10. Agree a foundation trust authorisatio<br />
on trajectory<br />
and achieve all milestones.<br />
Risk and<br />
Assurance<br />
Related<br />
Assurance<br />
Framework entries<br />
Legal implications/<br />
regulatory requirements<br />
The report provides assurance in relation to <strong>Trust</strong> objective 10.<br />
n/a<br />
As an aspirant <strong>NHS</strong> foundation trust, <strong>Barts</strong> <strong>Health</strong> is required to<br />
submit a monthly SOM<br />
return.<br />
Action required:<br />
The <strong>Trust</strong> <strong>Board</strong> is asked to<br />
review and approve<br />
the April<br />
(reporting February<br />
2013 data).<br />
2013 self‐certification<br />
return
TB 35/13<br />
BARTS HEALTH <strong>NHS</strong> TRUST<br />
TRUST BOARD MEETING: 10 APRIL 2013<br />
SINGLE OPERATING MODEL (SOM) –<br />
APRIL 2013 SELF CERTIFICATION SUBMISSION<br />
SUMMARY OF KEY POINTS<br />
1. The purpose of this report is to inform the <strong>Trust</strong> <strong>Board</strong> of the content of the April<br />
2013 self‐certification return of the Single Operating Model, reporting February 2013<br />
data, and present the templates which will be submitted to the <strong>NHS</strong> <strong>Trust</strong><br />
Development Authority on 15 April 2013. The ratings for this month’s selfcertification<br />
return are:<br />
Key area for rating Score RAG rating<br />
Governance Risk Rating (GRR) 5.5 Red<br />
Financial Risk Rating (FRR) 2 Red<br />
INTRODUCTION<br />
2. On 3 August 2012 the Department of <strong>Health</strong> (DH) launched part 2 of the Single<br />
Operating Model (SOM), focusing on SHA oversight of <strong>NHS</strong> <strong>Trust</strong>s. Oversight includes<br />
clinical quality, finance, service performance, governance and the delivery of the<br />
Tripartite Formal Agreement (TFA). The SOM aims to ensure a consistent approach to<br />
FT development across the country and to prepare for the establishment of the <strong>NHS</strong><br />
<strong>Trust</strong> Development Authority (NTDA).<br />
PRINCIPLES UNDERPINNING THE SINGLE OPERATING MODEL<br />
3. The model is designed around Monitor’s criteria and assessment methodology and<br />
the eight domains of assurance against which the DH considers FT applications for<br />
Secretary of State. As such, the oversight approach aims to develop the skills which<br />
will be tested in detail as part of the assessment for FT status and will be required<br />
once authorised. The model aims to remove duplication of activity across all stages of<br />
the applications process and promote integrated performance management of<br />
actions and milestones in Tripartite Formal Agreements (TFA).<br />
2
TB 35/13<br />
4. Monthly self‐certification returns are expected to be submitted on time and in full.<br />
Late, incomplete or inaccurate submissions will automatically be overridden to a red<br />
governance risk rating. The SOM framework comprises:<br />
<strong>NHS</strong> <strong>Trust</strong> Governance Declarations<br />
<strong>Board</strong> Statements<br />
Quality Return<br />
Financial Risk Rating<br />
Governance Risk Rating<br />
Contract status<br />
TFA Progress<br />
SUMMARY OF APRIL 2013 SELF‐CERTIFICATION RETURN (FEBRUARY 2013 POSITION)<br />
a. <strong>Board</strong> Statements<br />
5. The latest position is that 7 of the 15 <strong>Board</strong> Statements can be confirmed and 8<br />
cannot. The 8 exceptions are:<br />
The board is satisfied that processes and procedures are in place to ensure all<br />
medical practitioners providing care on behalf of the trust have met the relevant<br />
registration and revalidation requirements.<br />
The board anticipates that the trust will continue to maintain a financial risk<br />
rating of at least 3 over the next 12 months.<br />
All current key risks have been identified (raised either internally or by external<br />
audit and assessment bodies) and addressed – or there are appropriate action<br />
plans in place to address the issues – in a timely manner.<br />
The board has considered all likely future risks and has reviewed appropriate<br />
evidence regarding the level of severity, likelihood of it occurring and the plans<br />
for mitigation of these risks.<br />
The necessary planning, performance management and corporate and clinical<br />
risk management processes and mitigation plans are in place to deliver the<br />
annual plan, including that all audit committee recommendations accepted by<br />
the board are implemented satisfactorily.<br />
An Annual Governance Statement is in place, and the trust is compliant with the<br />
risk management and assurance framework requirements that support the<br />
Statement pursuant to the most up to date guidance from HM Treasury<br />
(www.hm‐treasury.gov.uk).<br />
The board is satisfied that plans in place are sufficient to ensure ongoing<br />
compliance with all existing targets (after the application of thresholds) as set out<br />
in the Governance Risk Rating; and a commitment to comply with all<br />
commissioned targets going forwards.<br />
The trust has achieved a minimum of Level 2 performance against the<br />
requirements of the Information Governance Toolkit.<br />
3
TB 35/13<br />
6. The full return and the <strong>Board</strong> Statement Exception Report includes a brief summary<br />
of the issues and actions relating to each of these statements.<br />
b. Quality Return<br />
7. This section is not risk rated but the indicators are used to inform clinical quality<br />
discussions between the <strong>Trust</strong> and the SHA. Key areas to highlight are:<br />
HMSR – 2011 data (the latest published) indicates a positive position for the<br />
<strong>Trust</strong> (0.8 against a national average of 1) as a whole and for each of the three<br />
legacy <strong>Trust</strong>s.<br />
VTE Screening ‐ performance has improved from prior month (90.25 compared<br />
to 88.58 in January 2013).<br />
MRSA screening ‐ data is still being collated.<br />
Open Serious Incidents Requiring Investigation – incidents have increased to 33<br />
from 21 in January 2013. A recovery plan is in place to address the high number<br />
of legacy and current Sis.<br />
Single Sex Accommodation Breaches – Remedial action is in place to address the<br />
causal factors<br />
Formal Complaints Received – there has been a decrease in the number of<br />
complaints from previous months.<br />
Sickness absence rate ‐ data is still being collated.<br />
Consultant PDPs – data is still being collated.<br />
Agency spend – decreased from 5.58 to 4.99% due to implementation of controls<br />
around spend.<br />
c. Financial Risk Rating (FRR)<br />
8. Financial Risk Ratings remain at 2 (red) due to the current in year deficit position.<br />
d. Governance Risk Rating (GRR)<br />
9. The GRR is based on Monitor’s latest compliance framework. For April 2013 the <strong>Trust</strong><br />
is RAG rated red with a score of 5.5. The following indicators contributed to this<br />
position:<br />
Certification against compliance with requirements regarding access to<br />
healthcare for people with a learning disability (weighting 0.5)<br />
18 week Referral to Treatment (RTT) waits – admitted (weighting 1.0)<br />
All cancers – 62 day wait for first treatment (weighting 1.0)<br />
A&E – 4 hour waits (weighting 1.0)<br />
Clostridium Difficile ‐ above the de minimis threshold (weighting 1.0)<br />
MRSA ‐ above the de minimis threshold and above the year to date ceiling<br />
(weighting 1.0)<br />
4
TB 35/13<br />
10. Additionally, the overriding rules around cancer wait times and meeting the MRSA<br />
objective have been triggered. The position remains static from the March position<br />
(red, with a score of 5.5).<br />
e. Contract Status<br />
11. All main contracts were signed on 14 September 2012 and there are no issues or<br />
disputes.<br />
f. TFA Progress<br />
12. This section outlines progress with the milestones and actions in the tripartite formal<br />
agreement. For November, an amber/red rating was agreed for TFA progress, with<br />
the comment “A <strong>Barts</strong> <strong>Health</strong> TFA including a revised trajectory for FT authorisation<br />
was submitted to <strong>NHS</strong> London at the end of November 2012 and is currently being<br />
agreed. This will change the future milestones”.<br />
RECOMMENDATION<br />
13. The <strong>Trust</strong> <strong>Board</strong> is asked to review and approve the April 2013 self‐certification return<br />
(reporting February 2013 data).<br />
5