Express Scripts, Inc. NCPDP Version D.0 Payer Sheet WellPoint ...
Express Scripts, Inc. NCPDP Version D.0 Payer Sheet WellPoint ...
Express Scripts, Inc. NCPDP Version D.0 Payer Sheet WellPoint ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
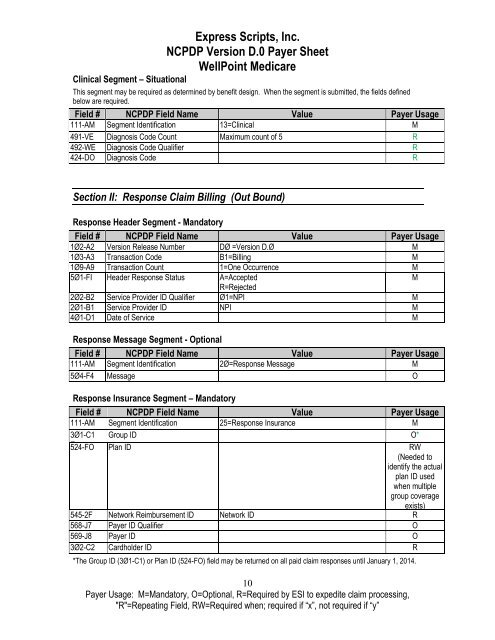
Clinical Segment – Situational<br />
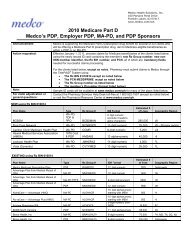
<strong>Express</strong> <strong>Scripts</strong>, <strong>Inc</strong>.<br />
<strong>NCPDP</strong> <strong>Version</strong> <strong>D.0</strong> <strong>Payer</strong> <strong>Sheet</strong><br />
<strong>WellPoint</strong> Medicare<br />
This segment may be required as determined by benefit design. When the segment is submitted, the fields defined<br />
below are required.<br />
Field # <strong>NCPDP</strong> Field Name Value <strong>Payer</strong> Usage<br />
111-AM Segment Identification 13=Clinical M<br />
491-VE Diagnosis Code Count Maximum count of 5 R<br />
492-WE Diagnosis Code Qualifier R<br />
424-DO Diagnosis Code R<br />
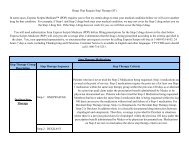
Section II: Response Claim Billing (Out Bound)<br />
Response Header Segment - Mandatory<br />
Field # <strong>NCPDP</strong> Field Name Value <strong>Payer</strong> Usage<br />
1Ø2-A2 <strong>Version</strong> Release Number DØ =<strong>Version</strong> D.Ø M<br />
1Ø3-A3 Transaction Code B1=Billing M<br />
1Ø9-A9 Transaction Count 1=One Occurrence M<br />
5Ø1-FI Header Response Status A=Accepted<br />
M<br />
R=Rejected<br />
2Ø2-B2 Service Provider ID Qualifier Ø1=NPI M<br />
2Ø1-B1 Service Provider ID NPI M<br />
4Ø1-D1 Date of Service M<br />
Response Message Segment - Optional<br />
Field # <strong>NCPDP</strong> Field Name Value <strong>Payer</strong> Usage<br />
111-AM Segment Identification 2Ø=Response Message M<br />
5Ø4-F4 Message O<br />
Response Insurance Segment – Mandatory<br />
Field # <strong>NCPDP</strong> Field Name Value <strong>Payer</strong> Usage<br />
111-AM Segment Identification 25=Response Insurance M<br />
3Ø1-C1 Group ID O*<br />
Respons<br />
524-FO<br />
e<br />
Message<br />
Segment<br />
-<br />
Mandato<br />
ry 545-2F<br />
Plan ID<br />
Network Reimbursement ID Network ID<br />
RW<br />
R<br />
568-J7 Field # <strong>Payer</strong> ID <strong>NCPDP</strong> Qualifier Field Name Value <strong>Payer</strong> O Usage<br />
569-J8 111-AM <strong>Payer</strong> Segment ID Identification 2Ø=Response Message O M<br />
3Ø2-C2 5Ø4-F4 Cardholder Message ID R O<br />
1-C1 *The Group ID (3Ø1-C1) or Plan ID (524-FO) field may be returned on all paid claim responses until January 1, 2014.<br />
10<br />
<strong>Payer</strong> Usage: M=Mandatory, O=Optional, R=Required by ESI to expedite claim processing,<br />
"R"=Repeating Field, RW=Required when; required if ―x‖, not required if ―y‖<br />
(Needed to<br />
identify the actual<br />
plan ID used<br />
when multiple<br />
group coverage<br />
exists)