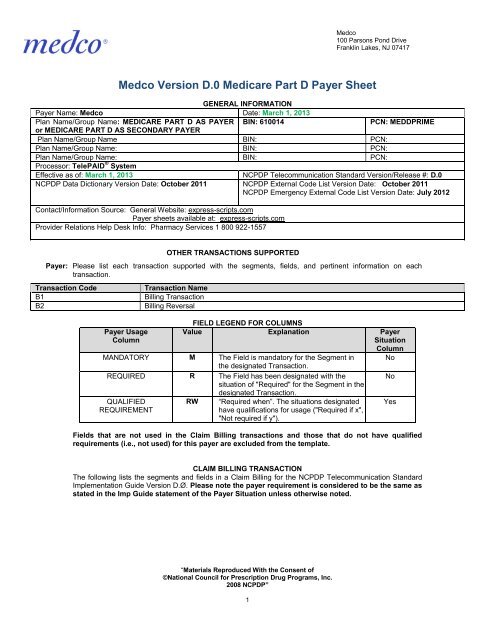
Medco Version D.0 Medicare Part D Payer Sheet - Express Scripts
Medco Version D.0 Medicare Part D Payer Sheet - Express Scripts
Medco Version D.0 Medicare Part D Payer Sheet - Express Scripts
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
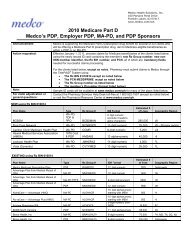
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Insurance SegmentSegment Identification (111-AM) =“Ø4”Field # NCPDP Field Name Value <strong>Payer</strong>UsageClaim Billing<strong>Payer</strong> Situation<strong>Payer</strong> Requirement: May be submittedby Long Term Care Pharmacies.Patient Segment Questions Check Claim BillingIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXThis Segment is situationalPatient SegmentClaim BillingSegment Identification (111-AM) =“Ø1”Field # NCPDP Field Name Value <strong>Payer</strong> <strong>Payer</strong> SituationUsage3Ø4-C4 DATE OF BIRTH R3Ø5-C5 PATIENT GENDER CODE R31Ø-CA PATIENT FIRST NAME R Imp Guide: Required when the patienthas a first name.311-CB PATIENT LAST NAME R325-CP PATIENT ZIP/POSTAL ZONE RW Imp Guide: Optional.<strong>Payer</strong> Requirement: Emergency/DisasterSituations; Patient Zip Code of theemergency should be entered.3Ø7-C7 PLACE OF SERVICE 01(Pharmacy) RW Imp Guide: Required if this field couldresult in different coverage, pricing, orpatient financial responsibility.<strong>Payer</strong> Requirement: Valid valuesrequired for Patient Residence andPharmacy Type. Values entered shouldbe consistent with your contract384-4X PATIENT RESIDENCE RW Imp Guide: Required if this field couldresult in different coverage, pricing, orpatient financial responsibility.<strong>Payer</strong> Requirement: Valid valuesrequired for Patient Residence andPharmacy Type. Values entered shouldbe consistent with your contractClaim Segment Questions Check Claim BillingIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXThis payer does support partial fillsThis payer does not support partial fillsX“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”3
Claim SegmentSegment Identification (111-AM) =“Ø7”Field # NCPDP Field Name Value <strong>Payer</strong>Usage455-EMPRESCRIPTION/SERVICEREFERENCE NUMBER QUALIFIER<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim Billing<strong>Payer</strong> Situation1(Rx Billing) M Imp Guide: For Transaction Code of“B1”, in the Claim Segment, thePrescription/Service ReferenceNumber Qualifier (455-EM) is “1”(Rx Billing).M4Ø2-D2 PRESCRIPTION/SERVICEREFERENCE NUMBER436-E1 PRODUCT/SERVICE ID QUALIFIER ØØ (Not Specified)M Use 00 for Multi- ingredientØ3(NDC)compound claim.4Ø7-D7 PRODUCT/SERVICE ID M Use 0 for Multi- ingredientcompound claim.442-E7 QUANTITY DISPENSED R4Ø3-D3 FILL NUMBER R4Ø5-D5 DAYS SUPPLY R4Ø6-D6 COMPOUND CODE 1(Not a Compound)2 (Compound)RSee Compound Segment forsupport of multi-ingredientcompounds when compound = 2.4Ø8-D8 DISPENSE AS WRITTENR(DAW)/PRODUCT SELECTIONCODE414-DE DATE PRESCRIPTION WRITTEN R419-DJ PRESCRIPTION ORIGIN CODE R Imp Guide: Required if necessary forplan benefit administration.354-NXSUBMISSION CLARIFICATIONCODE COUNTMaximum count of 3 RW Imp Guide: Required if SubmissionClarification Code (42Ø-DK) is used.42Ø-DKSUBMISSION CLARIFICATIONCODERWImp Guide: Required if clarification isneeded and value submitted isgreater than zero (Ø).If the Date of Service (4Ø1-D1)contains the subsequent payercoverage date, the SubmissionClarification Code (42Ø-DK) isrequired with value of “19” (SplitBilling – indicates the quantitydispensed is the remainder billed to asubsequent payer when <strong>Medicare</strong><strong>Part</strong> A expires. Used only in long-termcare settings) for individual unit of usemedications.3Ø8-C8 OTHER COVERAGE CODE 2(Other coverage existspaymentcollected )3(Other Coverage Billed –claim not covered)4(Other coverage existspaymentnot collected)RW<strong>Payer</strong> Requirement: The value of 2 isused to respond to a Max DailyDose/High Dose Reject.Imp Guide: Required if needed byreceiver, to communicate asummation of other coverageinformation that has been collectedfrom other payers.Required for Coordination of Benefits.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”4
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim SegmentClaim BillingSegment Identification (111-AM) =“Ø7”Field # NCPDP Field Name Value <strong>Payer</strong> <strong>Payer</strong> SituationUsage995-E2 ROUTE OF ADMINISTRATION RW Imp Guide: Required if specified intrading partner agreement.147-U7 PHARMACY SERVICE TYPE 1 (Community/RetailPharmacy Services)3( Home Infusion TherapyServices)5( Long Term Care PharmacyServices)RW<strong>Payer</strong> Requirement: Required whenCompound Code (4Ø6-D6) = 2(compound).Imp Guide: Required when thesubmitter must clarify the type ofservices being performed as acondition for proper reimbursement bythe payer.<strong>Payer</strong> Requirement: Valid values arerequired for Patient Residence andPharmacy Service Type. Valuesentered should be consistent withyour contract.Pricing Segment Questions Check Claim BillingIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXPricing SegmentClaim BillingSegment Identification (111-AM) =“11”Field # NCPDP Field Name Value <strong>Payer</strong> <strong>Payer</strong> SituationUsage4Ø9-D9 INGREDIENT COST SUBMITTED R412-DC DISPENSING FEE SUBMITTED RW Imp Guide: Required if its value hasan effect on the Gross Amount Due(43Ø-DU) calculation.<strong>Payer</strong> Requirement: DispensingFee Submitted is required whenSubmission Clarification Code=19(Split Billing). Pharmacy shouldprovide appropriate dispensing feefor the transaction.438-E3 INCENTIVE AMOUNT SUBMITTED RW Imp Guide: Required if its value hasan effect on the Gross Amount Due(43Ø-DU) calculation.<strong>Payer</strong> Requirement: Required whensubmitting a claim for a vaccine drugand administrative fee together.481-HAFLAT SALES TAX AMOUNTSUBMITTEDRWImp Guide: Required if its value hasan effect on the Gross Amount Due(43Ø-DU) calculation.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”6
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Pricing SegmentSegment Identification (111-AM) =“11”Field # NCPDP Field Name Value <strong>Payer</strong>Usage482-GE PERCENTAGE SALES TAX AMOUNTRWSUBMITTEDClaim Billing<strong>Payer</strong> SituationImp Guide: Required if its value hasan effect on the Gross Amount Due(43Ø-DU) calculation.483-HEPERCENTAGE SALES TAX RATESUBMITTEDRWImp Guide: Required if PercentageSales Tax Amount Submitted (482-GE) and Percentage Sales Tax BasisSubmitted (484-JE) are used.Required if this field could result indifferent pricing.Required if needed to calculatePercentage Sales Tax Amount Paid(559-AX).484-JEPERCENTAGE SALES TAX BASISSUBMITTEDRWImp Guide: Required if PercentageSales Tax Amount Submitted (482-GE) and Percentage Sales Tax RateSubmitted (483-HE) are used.Required if this field could result indifferent pricing.Required if needed to calculatePercentage Sales Tax Amount Paid(559-AX).426-DQ USUAL AND CUSTOMARY CHARGE R Imp Guide: Required if needed pertrading partner agreement.43Ø-DU GROSS AMOUNT DUE R423-DN BASIS OF COST DETERMINATION R Imp Guide: Required if needed forreceiver claim/encounter adjudication.<strong>Payer</strong> Requirement: Basis of CostDetermination not required for MultiIngredient Compound claims.Prescriber Segment Questions Check Claim BillingIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXThis Segment is situational“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”7
Prescriber SegmentSegment Identification (111-AM) =“Ø3”Field # NCPDP Field Name Value <strong>Payer</strong>Usage466-EZ PRESCRIBER ID QUALIFIER Ø1 = NPIRØ8 = State License12 = DEA<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim Billing<strong>Payer</strong> SituationImp Guide: Required if Prescriber ID(411-DB) is used.411-DB PRESCRIBER ID NPI, State License or DEA R Imp Guide: Required if this field couldresult in different coverage or patientfinancial responsibility.Required if necessary forstate/federal/regulatory agencyprograms.<strong>Payer</strong> Requirement: NPI, DEA orState License Number. For vaccines,an individual NPI is required. It may bethe prescriber who wrote the prescriptionor alternate care provider (pharmacist,nurse practitioner, etc.) who administeredthe vaccine.427-DR PRESCRIBER LAST NAME RW Imp Guide: Required when thePrescriber ID (411-DB) is not known.Required if needed for Prescriber ID(411-DB) validation/clarification.367-2N PRESCRIBER STATE/PROVINCEADDRESSRW<strong>Payer</strong> Requirement: Required whenPrescriber Id Qualifier =08 (StateLicense) is submitted.Imp Guide: Required if needed toassist in identifying the prescriber.Required if necessary forstate/federal/regulatory agencyprograms.<strong>Payer</strong> Requirement: Required whensubmitting Prescriber Id Qualifier = 8(State License) or Prescriber IdQualifier = 12 (DEA) is submitted.Coordination of Benefits/Other Payments Segment Check Claim BillingQuestionsIf Situational, <strong>Payer</strong> SituationThis Segment is situational X Required only for secondary, tertiary, etc claims.Scenario 1 - Other <strong>Payer</strong> Amount Paid Repetitions OnlyXScenario 2 - Other <strong>Payer</strong>-Patient Responsibility AmountRepetitions and Benefit Stage Repetitions OnlyScenario 3 - Other <strong>Payer</strong> Amount Paid, Other <strong>Payer</strong>-Patient Responsibility Amount, and Benefit StageRepetitions Present (Government Programs)“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”8
Coordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) =“Ø5”Field # NCPDP Field Name Value <strong>Payer</strong>Usage337-4C COORDINATION OFMaximum count of 9. MBENEFITS/OTHER PAYMENTSCOUNT<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingScenario 1- Other <strong>Payer</strong> AmountPaid Repetitions Only<strong>Payer</strong> Situation338-5C OTHER PAYER COVERAGE TYPE M339-6C OTHER PAYER ID QUALIFIER Ø3(BIN) M Imp Guide: Required if Other <strong>Payer</strong> ID(34Ø-7C) is used.34Ø-7C OTHER PAYER ID M Imp Guide: Required if identification ofthe Other <strong>Payer</strong> is necessary forclaim/encounter adjudication.443-E8 OTHER PAYER DATE RW Imp Guide: Required if identification ofthe Other <strong>Payer</strong> Date is necessary forclaim/encounter adjudication.341-HB342-HCOTHER PAYER AMOUNT PAIDCOUNTOTHER PAYER AMOUNT PAIDQUALIFIERMaximum count of 9 RW Imp Guide: Required if Other <strong>Payer</strong>Amount Paid Qualifier (342-HC) isused07 = Drug Benefit10 = Sales TaxRWImp Guide: Required if Other <strong>Payer</strong>Amount Paid (431-DV) is used.431-DV OTHER PAYER AMOUNT PAID RW Imp Guide: Required if Other <strong>Payer</strong>has approved payment for some/all ofthe billing.471-5E OTHER PAYER REJECT COUNT Maximum count of 5 RW Imp Guide: Required if Other <strong>Payer</strong>Reject Code (472-6E) is used.472-6E OTHER PAYER REJECT CODE RW Imp Guide: Required when the otherpayer has denied the payment for thebilling.DUR/PPS Segment Questions Check Claim BillingIf Situational, <strong>Payer</strong> SituationThis Segment is always sentThis Segment is situational X Based on pharmacy determination for clinical or vaccineprocessing. When submitting a claim for a vaccine andadministration fee, only the 440-E5 (Professional Service Code)field is required in this segment.When submitting a compound claim, Field 474-8E (DUR/PPSLevel of Effort) is required; using the values consistent with yourcontract.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”9
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417CLAIM BILLING RESPONSEGENERAL INFORMATION<strong>Payer</strong> Name: <strong>Medco</strong> Date: March 1, 2013Plan Name/Group Name: MEDICARE PART D AS PAYER or BIN: 610014PCN:MEDDPRIMEMEDICARE PART D AS A SECONDARY PAYERPlan Name/Group Name: Plan Name/Group Name: BIN: PCN:Plan Name/Group Name: Plan Name/Group Name BIN: PCN:CLAIM BILLING PAID (OR DUPLICATE OF PAID) RESPONSEThe following lists the segments and fields in a Claim Billing response (Paid or Duplicate of Paid) Transaction for theNCPDP Telecommunication Standard Implementation Guide <strong>Version</strong> D.Ø. Please note the payer requirement isconsidered to be the same as stated in the Imp Guide statement of the <strong>Payer</strong> Situation unless otherwisenoted.Response Transaction Header Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Transaction HeaderSegmentField # NCPDP Field Name Value <strong>Payer</strong>Usage1Ø2-A2 VERSION/RELEASE NUMBER DØ M1Ø3-A3 TRANSACTION CODE B1 M1Ø9-A9 TRANSACTION COUNT Same value as in request M5Ø1-F1 HEADER RESPONSE STATUS A M2Ø2-B2 SERVICE PROVIDER ID QUALIFIER Same value as in request M2Ø1-B1 SERVICE PROVIDER ID Same value as in request M4Ø1-D1 DATE OF SERVICE Same value as in request MClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> SituationResponse Message Header Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, <strong>Payer</strong> SituationThis Segment is always sentThis Segment is situational X Provided when additional message text is necessaryResponse Message SegmentSegment Identification (111-AM) =“2Ø”Field # NCPDP Field Name Value <strong>Payer</strong>UsageClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation5Ø4-F4 MESSAGE RW Imp Guide: Required if text is neededfor clarification or detail.Response Insurance Header Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, <strong>Payer</strong> SituationThis Segment is always sentX“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”12
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Response Insurance SegmentSegment Identification (111-AM) =“25”Claim BillingAccepted/Paid (or Duplicate ofPaid)Field # NCPDP Field Name Value <strong>Payer</strong> <strong>Payer</strong> SituationUsage3Ø1-C1 GROUP ID R Imp Guide: Required if needed toidentify the actual cardholder oremployer group, to identifyappropriate group number, whenavailable.Required to identify the actual groupthat was used when multiple groupcoverage exists.545-2F NETWORK REIMBURSEMENT ID R Imp Guide: Required if needed toidentify the network for the coveredmember.Required if needed to identify theactual Network Reimbursement ID,when applicable and/or available.Required to identify the actualNetwork Reimbursement ID that wasused when multiple NetworkReimbursement IDs exist.3Ø2-C2 CARDHOLDER ID RW Imp Guide: Required if theidentification to be used in futuretransactions is different than whatwas submitted on the request.Response Status Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value <strong>Payer</strong>Usage112-AN TRANSACTION RESPONSEP, D MSTATUSClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation5Ø3-F3 AUTHORIZATION NUMBER R Imp Guide: Required if needed toidentify the transaction.547-5F APPROVED MESSAGE CODECOUNTMaximum count of 5. RW Imp Guide: Required if ApprovedMessage Code (548-6F) is used.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”13
Response Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation548-6F APPROVED MESSAGE CODE RW Imp Guide: Required if ApprovedMessage Code Count (547-5F) isused and the sender needs tocommunicate additional follow up fora potential opportunity.13Ø-UFADDITIONAL MESSAGEINFORMATION COUNTMaximum count of 9. RW Imp Guide: Required if AdditionalMessage Information (526-FQ) isused.132-UHADDITIONAL MESSAGEINFORMATION QUALIFIERØ1-Ø9 = Free Form Text1Ø = Next Available FillDate (CCYYMMDDRWImp Guide: Required if AdditionalMessage Information (526-FQ) isused.526-FQADDITIONAL MESSAGEINFORMATIONRWImp Guide: Required when additionaltext is needed for clarification ordetail.131-UGADDITIONAL MESSAGEINFORMATION CONTINUITYRWImp Guide: Required if and only ifcurrent repetition of AdditionalMessage Information (526-FQ) isused, another populated repetition ofAdditional Message Information (526-FQ) follows it, and the text of thefollowing message is a continuation ofthe current.549-7F HELP DESK PHONE NUMBERQUALIFIERRWImp Guide: Required if Help DeskPhone Number (55Ø-8F) is used.55Ø-8F HELP DESK PHONE NUMBER RW Imp Guide: Required if needed toprovide a support telephone numberto the receiver.Response Claim Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Claim SegmentSegment Identification (111-AM) =“22”Field # NCPDP Field Name Value <strong>Payer</strong>Usage455-EM PRESCRIPTION/SERVICEMREFERENCE NUMBER QUALIFIER4Ø2-D2PRESCRIPTION/SERVICEREFERENCE NUMBERM“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”Claim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> SituationImp Guide: For Transaction Code of“B1”, in the Response ClaimSegment, the Prescription/ServiceReference Number Qualifier (455-EM)is “1” (Rx Billing).14
Response Claim SegmentSegment Identification (111-AM) =“22”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation551-9F PREFERRED PRODUCT COUNT Maximum count of 6. RW Imp Guide: Required if PreferredProduct ID (553-AR) is used.<strong>Payer</strong> Requirement: Based on benefitand when preferred alternative areavailable for the submitted productservice ID.552-APPREFERRED PRODUCT IDQUALIFIERRWImp Guide: Required if PreferredProduct ID (553-AR) is used.553-AR PREFERRED PRODUCT ID RW Imp Guide: Required if a productpreference exists that needs to becommunicated to the receiver via anID.556-AUPREFERRED PRODUCTDESCRIPTIONRWImp Guide: Required if a productpreference exists that either cannotbe communicated by the PreferredProduct ID (553-AR) or to clarify thePreferred Product ID (553-AR).Response Pricing Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Pricing SegmentSegment Identification (111-AM)= “23”Field # NCPDP Field Name Value <strong>Payer</strong>UsageClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation5Ø5-F5 PATIENT PAY AMOUNT R5Ø6-F6 INGREDIENT COST PAID R5Ø7-F7 DISPENSING FEE PAID R Imp Guide: Required if this value isused to arrive at the finalreimbursement.557-AV TAX EXEMPT INDICATOR R Imp Guide: Required if the sender(health plan) and/or patient is taxexempt and exemption applies tothis billing.558-AW FLAT SALES TAX AMOUNT PAID RW Imp Guide: Required if Flat SalesTax Amount Submitted (481-HA) isgreater than zero (Ø) or if Flat SalesTax Amount Paid (558-AW) is usedto arrive at the final reimbursement.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”15
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Response Pricing SegmentSegment Identification (111-AM)= “23”Field # NCPDP Field Name Value <strong>Payer</strong>Usage559-AX PERCENTAGE SALES TAXRWAMOUNT PAIDClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> SituationImp Guide: Required if this value isused to arrive at the finalreimbursement.Required if Percentage Sales TaxAmount Submitted (482-GE) isgreater than zero (Ø).Required if Percentage Sales TaxRate Paid (56Ø-AY) and PercentageSales Tax Basis Paid (561-AZ) areused.56Ø-AYPERCENTAGE SALES TAX RATEPAIDRWImp Guide: Required if PercentageSales Tax Amount Paid (559-AX) isgreater than zero (Ø).561-AZPERCENTAGE SALES TAX BASISPAIDRWImp Guide: Required if PercentageSales Tax Amount Paid (559-AX) isgreater than zero (Ø).521-FL INCENTIVE AMOUNT PAID RW Imp Guide: Required if this value isused to arrive at the finalreimbursement.Required if Incentive AmountSubmitted (438-E3) is greater thanzero (Ø).5Ø9-F9 TOTAL AMOUNT PAID R522-FM BASIS OF REIMBURSEMENTRDETERMINATIONImp Guide: Required if IngredientCost Paid (5Ø6-F6) is greater thanzero (Ø).523-FNAMOUNT ATTRIBUTED TOSALES TAXRWRequired if Basis of CostDetermination (432-DN) is submittedon billing.Imp Guide: Required if Patient PayAmount (5Ø5-F5) includes sales taxthat is the financial responsibility ofthe member but is not also includedin any of the other fields that add upto Patient Pay Amount.Imp Guide: Provided forinformational purposes only.Imp Guide: Provided forinformational purposes only.512-FC ACCUMULATED DEDUCTIBLEAMOUNTRW513-FD REMAINING DEDUCTIBLERWAMOUNT514-FE REMAINING BENEFIT AMOUNT RW Imp Guide: Provided forinformational purposes only.517-FH AMOUNT APPLIED TO PERIODICRWDEDUCTIBLEImp Guide: Required if Patient PayAmount (5Ø5-F5) includesdeductible.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”16
Response Pricing SegmentSegment Identification (111-AM)= “23”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation518-FI AMOUNT OF COPAY RW Imp Guide: Required if Patient PayAmount (5Ø5-F5) includes co-payas patient financial responsibility.52Ø-FK571-NZAMOUNT EXCEEDING PERIODICBENEFIT MAXIMUMAMOUNT ATTRIBUTED TOPROCESSOR FEERWImp Guide: Required if Patient PayAmount (5Ø5-F5) includes amountexceeding periodic benefitmaximum.Imp Guide: Required if the customeris responsible for 1ØØ% of theprescription payment and when theprovider net sale is less than theamount the customer is expected topay.575-EQ PATIENT SALES TAX AMOUNT RW Imp Guide: Used when necessary toidentify the Patient’s portion of theSales Tax.574-2Y PLAN SALES TAX AMOUNT RW Imp Guide: Used when necessary toidentify the Plan’s portion of theSales Tax.572-4U AMOUNT OF COINSURANCE RW Imp Guide: Required if Patient PayAmount (5Ø5-F5) includescoinsurance as patient financialresponsibility.392-MU BENEFIT STAGE COUNT Maximum count of 4. R Imp Guide: Required if BenefitStage Amount (394-MW) is used.RW“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”17
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Response Pricing SegmentSegment Identification (111-AM)= “23”Field # NCPDP Field Name Value <strong>Payer</strong>393-MV BENEFIT STAGE QUALIFIER Blank = Not specifiedØ1 = DeductibleØ2 = Initial BenefitØ3 = Coverage Gap (donuthole)Ø4 = Catastrophic Coverage5Ø = Not paid under <strong>Part</strong> D,Paid Under <strong>Part</strong> C benefit (forMA-PD plan)6Ø = Not paid under <strong>Part</strong> D,paid as or under asupplemental benefit only.*61 = <strong>Part</strong> D drug not paid by<strong>Part</strong> D plan benefit. Paid as orunder a co-administeredbenefit only.**62 = Non-<strong>Part</strong> D/non-qualifieddrug not paid by <strong>Part</strong> D planbenefit. Paid as or under a coadministeredbenefit only.**7Ø = <strong>Part</strong> D drug not paid by<strong>Part</strong> D plan benefit, paid by thebeneficiary under plansponsorednegotiated pricing8Ø = Non-<strong>Part</strong> D/non-qualifieddrug not paid by <strong>Part</strong> D planbenefit, hospice benefit or anyother component of <strong>Medicare</strong>;paid by the beneficiary underplan-sponsored negotiatedpricing9Ø = Enhance or OTC drug(PDE value of E/O) notapplicable to <strong>Part</strong> D drugspend, but covered by <strong>Part</strong> Dplan***(Occurs up to 4 times)UsageRClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> SituationImp Guide: Required if BenefitStage Amount (394-MW) is used.<strong>Payer</strong> Requirement: See values“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”18
Response Pricing SegmentSegment Identification (111-AM)= “23”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation394-MW BENEFIT STAGE AMOUNT R Imp Guide: Required when a<strong>Medicare</strong> <strong>Part</strong> D payer appliesfinancial amounts to <strong>Medicare</strong> <strong>Part</strong>D beneficiary benefit stages. Thisfield is required when the plan is aparticipant in a <strong>Medicare</strong> <strong>Part</strong> Dprogram that requires reporting ofbenefit stage specific financialamounts.Required if necessary forstate/federal/regulatory agencyprograms.<strong>Payer</strong> Requirement: Amount willbe returned as appropriate for thecorresponding Benefit StageQualifiers (393-MV).577-G3 ESTIMATED GENERIC SAVINGS RW Imp Guide: This information shouldbe provided when a patient selectedthe brand drug and a generic form ofthe drug was available. It will containan estimate of the differencebetween the cost of the brand drugand the generic drug, when thebrand drug is more expensive thanthe generic.128-UCSPENDING ACCOUNT AMOUNTREMAININGRWImp Guide: This dollar amount willbe provided, if known, to thereceiver when the transaction hadspending account dollars reportedas part of the patient pay amount.129-UDHEALTH PLAN-FUNDEDASSISTANCE AMOUNTRWImp Guide: Required when thepatient meets the plan-fundedassistance criteria, to reduce PatientPay Amount (5Ø5-F5). The resultingPatient Pay Amount (5Ø5-F5) mustbe greater than or equal to zero.133-UJAMOUNT ATTRIBUTED TOPROVIDER NETWORKSELECTIONRWImp Guide: Required if Patient PayAmount (5Ø5-F5) includes anamount that is attributable to a costshare differential due to theselection of one pharmacy overanother.134-UKAMOUNT ATTRIBUTED TOPRODUCT SELECTION/BRANDDRUGRWImp Guide: Required if Patient PayAmount (5Ø5-F5) includes anamount that is attributable to apatient’s selection of a Brand drug.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”19
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Response Pricing SegmentSegment Identification (111-AM)= “23”Field # NCPDP Field Name Value <strong>Payer</strong>Usage135-UM AMOUNT ATTRIBUTED TORWPRODUCT SELECTION/NON-PREFERRED FORMULARYSELECTIONClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> SituationImp Guide: Required if Patient PayAmount (5Ø5-F5) includes anamount that is attributable to apatient’s selection of a non-preferredformulary product.136-UNAMOUNT ATTRIBUTED TOPRODUCT SELECTION/BRANDNON-PREFERRED FORMULARYSELECTIONRWImp Guide: Required if Patient PayAmount (5Ø5-F5) includes anamount that is attributable to apatient’s selection of a Brand nonpreferredformulary product.137-UPAMOUNT ATTRIBUTED TOCOVERAGE GAPRWImp Guide: Required when thepatient’s financial responsibility isdue to the coverage gap.566-J5 OTHER PAYER AMOUNTRECOGNIZEDImp Guide: Required if this value isused to arrive at the finalreimbursement.Required if Other <strong>Payer</strong> AmountPaid (431-DV) is greater than zero(Ø) and Coordination ofBenefits/Other Payments Segmentis supported.*Only available for use on claims with fill dates of 12/31/2012 and prior.**Benefit Stage Qualifier (393-MV) values 61 or 62 replace value of 6Ø. Available for use as of 1/1/13.*** Available for use as of 1/1/13.Check Claim BillingResponse DUR/PPS Segment QuestionsAccepted/Paid (or Duplicate of Paid)If Situational, <strong>Payer</strong> SituationThis Segment is always sentThis Segment is situational X When DUR Information to be providedResponse DUR/PPS SegmentSegment Identification (111-AM) =“24”Field # NCPDP Field Name Value <strong>Payer</strong>Usage567-J6 DUR/PPS RESPONSE CODECOUNTERMaximum 9 occurrencessupported.RWClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> SituationImp Guide: Required if ReasonFor Service Code (439-E4) isused.439-E4 REASON FOR SERVICE CODE RW Imp Guide: Required if utilizationconflict is detected.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”20
Response DUR/PPS SegmentSegment Identification (111-AM) =“24”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation528-FS CLINICAL SIGNIFICANCE CODE RW Imp Guide: Required if needed tosupply additional information forthe utilization conflict.529-FT OTHER PHARMACY INDICATOR RW Imp Guide: Required if needed tosupply additional information forthe utilization conflict.53Ø-FU PREVIOUS DATE OF FILL RW Imp Guide: Required if needed tosupply additional information forthe utilization conflict.Required if Quantity of PreviousFill (531-FV) is used.531-FV QUANTITY OF PREVIOUS FILL RW Imp Guide: Required if needed tosupply additional information forthe utilization conflict.Required if Previous Date Of Fill(53Ø-FU) is used.532-FW DATABASE INDICATOR RW Imp Guide: Required if needed tosupply additional information forthe utilization conflict.533-FX OTHER PRESCRIBER INDICATOR RW Imp Guide: Required if needed tosupply additional information forthe utilization conflict.544-FY DUR FREE TEXT MESSAGE RW Imp Guide: Required if needed tosupply additional information forthe utilization conflict.57Ø-NS DUR ADDITIONAL TEXT RW Imp Guide: Required if needed tosupply additional information forthe utilization conflict.Response Coordination of Benefits/Other <strong>Payer</strong>sSegment QuestionsCheck Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, <strong>Payer</strong> SituationThis Segment is situational X When available 4Rx or <strong>Medicare</strong> D OHI DATA to be returned.Response Coordination ofBenefits/Other <strong>Payer</strong>s SegmentSegment Identification (111-AM) =“28”Field # NCPDP Field Name Value <strong>Payer</strong>Usage355-NT OTHER PAYER ID COUNT Maximum count of 3 M338-5C OTHER PAYER COVERAGE TYPE MClaim BillingAccepted/Paid (or Duplicate of Paid)<strong>Payer</strong> Situation“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”21
Response Coordination ofBenefits/Other <strong>Payer</strong>s SegmentSegment Identification (111-AM) =“28”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate of Paid)<strong>Payer</strong> Situation339-6C OTHER PAYER ID QUALIFIER RW Imp Guide: Required if Other <strong>Payer</strong> ID(34Ø-7C) is used.<strong>Payer</strong> Requirement: When availableand required, 4Rx (Primary) or<strong>Medicare</strong> D OHI Data may be returnedon a claim response.34Ø-7C OTHER PAYER ID RW Imp Guide: Required if other insuranceinformation is available for coordinationof benefits.991-MHOTHER PAYER PROCESSORCONTROL NUMBERRW<strong>Payer</strong> Requirement: When availableand required, 4Rx (Primary) or<strong>Medicare</strong> D OHI Data may be returnedon a claim response.Imp Guide: Required if other insuranceinformation is available for coordinationof benefits.<strong>Payer</strong> Requirement: When availableand required, 4Rx (Primary) or<strong>Medicare</strong> D OHI Data may be returnedon a claim response.356-NU OTHER PAYER CARDHOLDER ID RW Imp Guide: Required if other insuranceinformation is available for coordinationof benefits.<strong>Payer</strong> Requirement: When availableand required, 4Rx (Primary) or<strong>Medicare</strong> D OHI Data may be returnedon a claim response.992-MJ OTHER PAYER GROUP ID RW Imp Guide: Required if other insuranceinformation is available for coordinationof benefits.<strong>Payer</strong> Requirement: When availableand required, 4Rx (Primary) or<strong>Medicare</strong> D OHI Data may be returnedon a claim response.142-UV OTHER PAYER PERSON CODE RW Imp Guide: Required if needed touniquely identify the family memberswithin the Cardholder ID, as assignedby the other payer.<strong>Payer</strong> Requirement: When availableand required, 4Rx (Primary) or<strong>Medicare</strong> D OHI Data may be returnedon a claim response.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”22
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Response Coordination ofBenefits/Other <strong>Payer</strong>s SegmentSegment Identification (111-AM) =“28”Field # NCPDP Field Name Value <strong>Payer</strong>Usage127-UB OTHER PAYER HELP DESKRWPHONE NUMBERClaim BillingAccepted/Paid (or Duplicate of Paid)<strong>Payer</strong> SituationImp Guide: Required if needed toprovide a support telephone number ofthe other payer to the receiver.<strong>Payer</strong> Requirement: When availableand required, 4Rx (Primary) or<strong>Medicare</strong> D OHI Data may be returnedon a claim response.CLAIM BILLING/ACCEPTED/REJECTED RESPONSEResponse Transaction Header Segment Questions Check Claim Billing/Claim Rebill Accepted/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Transaction HeaderSegmentField # NCPDP Field Name Value <strong>Payer</strong>Usage1Ø2-A2 VERSION/RELEASE NUMBER DØ M1Ø3-A3 TRANSACTION CODE B1 M1Ø9-A9 TRANSACTION COUNT Same value as in request M5Ø1-F1 HEADER RESPONSE STATUS A M2Ø2-B2 SERVICE PROVIDER ID QUALIFIER Same value as in request M2Ø1-B1 SERVICE PROVIDER ID Same value as in request M4Ø1-D1 DATE OF SERVICE Same value as in request MClaim BillingAccepted/Rejected<strong>Payer</strong> SituationResponse Message Segment Questions Check Claim Billing/Claim Rebill Accepted/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentThis Segment is situational X Provided when additional message textResponse Message SegmentSegment Identification (111-AM) =“2Ø”Field # NCPDP Field Name Value <strong>Payer</strong>UsageClaim BillingAccepted/Rejected<strong>Payer</strong> Situation5Ø4-F4 MESSAGE Imp Guide: Required if text isneeded for clarification or detail.Response Insurance Segment Questions Check Claim Billing Accepted/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXThis Segment is situational“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”23
Response Insurance SegmentSegment Identification (111-AM) =“25”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Rejected<strong>Payer</strong> Situation3Ø1-C1 GROUP ID RW Imp Guide: Required if needed toidentify the actual cardholder oremployer group, to identifyappropriate group number, whenavailable.Required to identify the actual groupthat was used when multiple groupcoverage exist.545-2F NETWORK REIMBURSEMENT ID RW Imp Guide: Required if needed toidentify the network for the coveredmember.Required if needed to identify theactual Network Reimbursement ID,when applicable and/or available.Required to identify the actualNetwork Reimbursement ID thatwas used when multiple NetworkReimbursement IDs exist.3Ø2-C2 CARDHOLDER ID RW Imp Guide: Required if theidentification to be used in futuretransactions is different than whatwas submitted on the request.Response Status Segment Questions Check Claim BillingAccepted/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value <strong>Payer</strong>Usage112-AN TRANSACTION RESPONSER = RejectMSTATUS51Ø-FA REJECT COUNT Maximum count of 5 R511-FB REJECT CODE R546-4F REJECT FIELD OCCURRENCERWINDICATOR13Ø-UFADDITIONAL MESSAGEINFORMATION COUNTClaim Billing Accepted/Rejected<strong>Payer</strong> SituationImp Guide: Required if a repeatingfield is in error, to identify repeatingfield occurrenceMaximum count of 9 RW Imp Guide: Required if AdditionalMessage Information (526-FQ) isused.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”24
Response Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value <strong>Payer</strong>Usage132-UH526-FQ131-UGADDITIONAL MESSAGEINFORMATION QUALIFIERADDITIONAL MESSAGEINFORMATIONADDITIONAL MESSAGEINFORMATION CONTINUITY549-7F HELP DESK PHONE NUMBERQUALIFIERØ1- Ø9 = Free-Form Text1Ø = Next Available FillDate (CCYYMMDD)RWRWRWRW<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim Billing Accepted/Rejected<strong>Payer</strong> SituationImp Guide: Required if AdditionalMessage Information (526-FQ) isused.Imp Guide: Required whenadditional text is needed forclarification or detail.Imp Guide: Required if and only ifcurrent repetition of AdditionalMessage Information (526-FQ) isused, another populated repetitionof Additional Message Information(526-FQ) follows it, and the text ofthe following message is acontinuation of the current.Imp Guide: Required if Help DeskPhone Number (55Ø-8F) is used.55Ø-8F HELP DESK PHONE NUMBER RW Imp Guide: Required if needed toprovide a support telephonenumber.987-MA URL RW Imp Guide: Provided forinformational purposes only to relayhealthcare communications via theInternet.<strong>Payer</strong> Requirement: Will returnhttp://www.expressscripts.com/services/pharmacistsResponse Claim Segment Questions Check Claim Billing Accepted/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Claim SegmentSegment Identification (111-AM) =“22”Field # NCPDP Field Name Value <strong>Payer</strong>Usage455-EMPRESCRIPTION/SERVICEREFERENCE NUMBER QUALIFIERClaim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation1 M Imp Guide: For Transaction Codeof “B1”, in the Response ClaimSegment, the Prescription/ServiceReference Number Qualifier (455-EM) is “1” (Rx Billing).M4Ø2-D2 PRESCRIPTION/SERVICEREFERENCE NUMBER551-9F PREFERRED PRODUCT COUNT Maximum count of 6. RW Imp Guide: Required if PreferredProduct ID (553-AR) is used.552-APPREFERRED PRODUCT IDQUALIFIERRWImp Guide: Required if PreferredProduct ID (553-AR) is used.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”25
Response Claim SegmentSegment Identification (111-AM) =“22”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)<strong>Payer</strong> Situation553-AR PREFERRED PRODUCT ID RW Imp Guide: Required if a productpreference exists that needs to becommunicated to the receiver viaan ID.556-AUPREFERRED PRODUCTDESCRIPTIONRWImp Guide: Required if a productpreference exists that either cannotbe communicated by the PreferredProduct ID (553-AR) or to clarifythe Preferred Product ID (553-AR).Response DUR/PPS Segment Questions Check Claim Billing Accepted/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentThis Segment is situational X When DUR has additional information to be returnedResponse DUR/PPS SegmentSegment Identification (111-AM) =“24”Field # NCPDP Field Name Value <strong>Payer</strong>Usage567-J6 DUR/PPS RESPONSE CODECOUNTERMaximum 9 occurrencessupported.RWClaim Billing/Accepted/Rejected<strong>Payer</strong> SituationImp Guide: Required if and only ifcurrent repetition of AdditionalMessage Information (526-FQ) isused, another populated repetitionof Additional Message Information(526-FQ) follows it, and the text ofthe following message is acontinuation of the current.439-E4 REASON FOR SERVICE CODE RW Imp Guide: Required if utilizationconflict is detected.528-FS CLINICAL SIGNIFICANCE CODE RW Imp Guide: Required if needed tosupply additional information for theutilization conflict.529-FT OTHER PHARMACY INDICATOR RW Imp Guide: Required if needed tosupply additional information for theutilization conflict.53Ø-FU PREVIOUS DATE OF FILL RW Imp Guide: Required if needed tosupply additional information for theutilization conflict.Required if Quantity of Previous Fill(531-FV) is used.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”26
Response DUR/PPS SegmentSegment Identification (111-AM) =“24”<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim Billing/Accepted/Rejected531-FV QUANTITY OF PREVIOUS FILL RW Imp Guide: Required if needed tosupply additional information for theutilization conflict.Required if Previous Date Of Fill(53Ø-FU) is used.532-FW DATABASE INDICATOR RW Imp Guide: Required if needed tosupply additional information for theutilization conflict.533-FX OTHER PRESCRIBER INDICATOR RW Imp Guide: Required if needed tosupply additional information for theutilization conflict.544-FY DUR FREE TEXT MESSAGE RW Imp Guide: Required if needed tosupply additional information for theutilization conflict.57Ø-NS DUR ADDITIONAL TEXT RW Imp Guide: Required if needed tosupply additional information for theutilization conflict.Response Prior Authorization Segment Questions Check Claim Billing Accepted/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentThis Segment is situational X Provided when the receiver has the opportunity to reprocessthe claim with using a Prior Authorization Number.Response Prior AuthorizationSegmentSegment Identification (111-AM) =“26”Field # NCPDP Field Name Value <strong>Payer</strong>Usage498-PY PRIOR AUTHORIZATIONRWNUMBER–ASSIGNEDClaim BillingAccepted/Rejected<strong>Payer</strong> SituationImp Guide: Required whenthe receiver must submit this PriorAuthorization Number in order toreceive payment for the claim.<strong>Payer</strong> Requirement: The valuereturned in this field will provide thevalue that may be submitted in PriorAuthorization Number Submitted,field 462-EV. This value must besubmitted with appropriatecorresponding Prior AuthorizationType Code, field 461-EU.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”27
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Response Coordination of Benefits/Other <strong>Payer</strong>s Check Claim Billing Accepted/RejectedSegment QuestionsIf Situational, <strong>Payer</strong> SituationThis Segment is situational X When 4Rx or <strong>Medicare</strong> OHI data availableResponse Coordination ofBenefits/Other <strong>Payer</strong>s SegmentSegment Identification (111-AM) =“28”Field # NCPDP Field Name Value <strong>Payer</strong>UsageClaim Billing/Accepted/Rejected<strong>Payer</strong> Situation355-NT OTHER PAYER ID COUNT Maximum count of 3. M338-5C OTHER PAYER COVERAGE TYPE M339-6C OTHER PAYER ID QUALIFIER 03 (BIN Number) RW Imp Guide: Required if Other <strong>Payer</strong> ID(34Ø-7C) is used.<strong>Payer</strong> Requirement: The 4Rx datasubmitted on the claim must beupdated this field maybe returned orwhen available <strong>Medicare</strong> D OHI Datamay be returned.34Ø-7C OTHER PAYER ID RW Imp Guide: Required if other insuranceinformation is available for coordinationof benefits.991-MHOTHER PAYER PROCESSORCONTROL NUMBERRW<strong>Payer</strong> Requirement: The 4Rx datasubmitted on the claim must beupdated this field maybe returned orwhen available <strong>Medicare</strong> D OHI Datamay be returned.Imp Guide: Required if other insuranceinformation is available for coordinationof benefits.<strong>Payer</strong> Requirement: The 4Rx datasubmitted on the claim must beupdated this field maybe returned orwhen available <strong>Medicare</strong> D OHI Datamay be returned.356-NU OTHER PAYER CARDHOLDER ID RW Imp Guide: Required if other insuranceinformation is available for coordinationof benefits.<strong>Payer</strong> Requirement: The 4Rx datasubmitted on the claim must beupdated this field maybe returned orwhen available <strong>Medicare</strong> D OHI Datamay be returned.992-MJ OTHER PAYER GROUP ID RW Imp Guide: Required if other insuranceinformation is available for coordinationof benefits.<strong>Payer</strong> Requirement: The 4Rx datasubmitted on the claim must beupdated this field maybe returned orwhen available <strong>Medicare</strong> D OHI Datamay be returned.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”28
Response Coordination ofBenefits/Other <strong>Payer</strong>s SegmentSegment Identification (111-AM) =“28”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim Billing/Accepted/Rejected<strong>Payer</strong> Situation142-UV OTHER PAYER PERSON CODE RW Imp Guide: Required if needed touniquely identify the family memberswithin the Cardholder ID, as assignedby the other payer.127-UBOTHER PAYER HELP DESKPHONE NUMBERRW<strong>Payer</strong> Requirement: The 4Rx datasubmitted on the claim must beupdated this field maybe returned orwhen available <strong>Medicare</strong> D OHI Datamay be returned.Imp Guide: Required if needed toprovide a support telephone number ofthe other payer to the receiver.<strong>Payer</strong> Requirement: The 4Rx datasubmitted on the claim must beupdated this field maybe returned orwhen available <strong>Medicare</strong> D OHI Datamay be returned.CLAIM BILLING REJECTED/REJECTED RESPONSEResponse Transaction Header Segment Questions Check Claim BillingRejected/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Transaction HeaderSegmentField # NCPDP Field Name Value <strong>Payer</strong>Usage1Ø2-A2 VERSION/RELEASE NUMBER DØ M1Ø3-A3 TRANSACTION CODE B1 M1Ø9-A9 TRANSACTION COUNT Same value as in request M5Ø1-F1 HEADER RESPONSE STATUS R M2Ø2-B2 SERVICE PROVIDER IDSame value as in request MQUALIFIER2Ø1-B1 SERVICE PROVIDER ID Same value as in request M4Ø1-D1 DATE OF SERVICE Same value as in request MClaim BillingRejected/Rejected<strong>Payer</strong> SituationResponse Message Segment Questions Check Claim BillingRejected/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentThis Segment is situationalX“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”29
Response Message SegmentSegment Identification (111-AM) =“2Ø”Field # NCPDP Field Name Value <strong>Payer</strong>Usage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingRejected/Rejected<strong>Payer</strong> Situation5Ø4-F4 MESSAGE Imp Guide: Required if text is neededfor clarification or detail.Response Status Segment Questions Check Claim Billing/Rejected/RejectedIf Situational, <strong>Payer</strong> SituationThis Segment is always sentXResponse Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value <strong>Payer</strong>Usage112-AN TRANSACTION RESPONSERMClaim BillingRejected/Rejected<strong>Payer</strong> SituationSTATUS5Ø3-F3 AUTHORIZATION NUMBER RW Imp Guide: Required if needed toidentify the transaction.51Ø-FA REJECT COUNT Maximum count of 5 R511-FB REJECT CODE R546-4F REJECT FIELD OCCURRENCEINDICATORRWImp Guide: Required if a repeatingfield is in error, to identify repeatingfield occurrence.13Ø-UF132-UHADDITIONAL MESSAGEINFORMATION COUNTADDITIONAL MESSAGEINFORMATION QUALIFIERMaximum count of 9 RW Imp Guide: Required if AdditionalMessage Information (526-FQ) isused.RWImp Guide: Required if AdditionalMessage Information (526-FQ) isused.526-FQ131-UGADDITIONAL MESSAGEINFORMATIONADDITIONAL MESSAGEINFORMATION CONTINUITY549-7F HELP DESK PHONE NUMBERQUALIFIERRWRWRWImp Guide: Required when additionaltext is needed for clarification ordetail.Imp Guide: Required if and only ifcurrent repetition of AdditionalMessage Information (526-FQ) isused, another populated repetition ofAdditional Message Information (526-FQ) follows it, and the text of thefollowing message is a continuation ofthe current.Imp Guide: Required if Help DeskPhone Number (55Ø-8F) is used.55Ø-8F HELP DESK PHONE NUMBER RW Imp Guide: Required if needed toprovide a support telephone numberto the receiver.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”30