Express Scripts, Inc. NCPDP Version D.0 Payer Sheet Emblem Health
Express Scripts, Inc. NCPDP Version D.0 Payer Sheet Emblem Health
Express Scripts, Inc. NCPDP Version D.0 Payer Sheet Emblem Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Express</strong> <strong>Scripts</strong>, <strong>Inc</strong>.<br />
<strong>NCPDP</strong> <strong>Version</strong> <strong>D.0</strong> <strong>Payer</strong> <strong>Sheet</strong><br />
<strong>Emblem</strong> <strong>Health</strong> - Medicare<br />
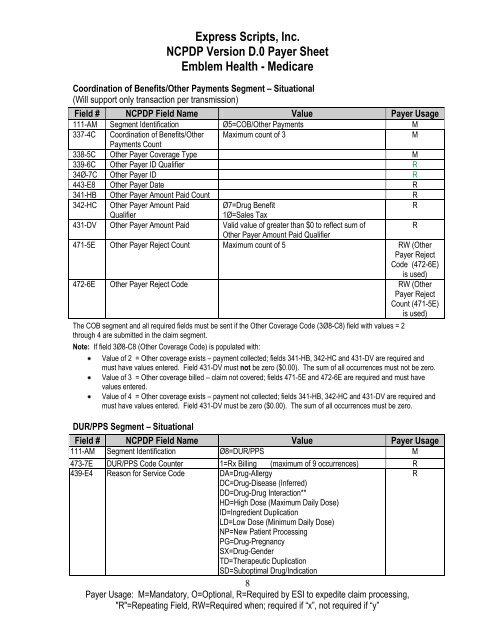
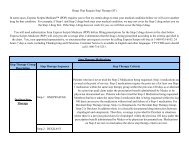
Coordination of Benefits/Other Payments Segment – Situational<br />
(Will support only transaction per transmission)<br />
Field # <strong>NCPDP</strong> Field Name Value <strong>Payer</strong> Usage<br />
111-AM Segment Identification Ø5=COB/Other Payments M<br />
337-4C Coordination of Benefits/Other Maximum count of 3<br />
M<br />
Payments Count<br />
338-5C Other <strong>Payer</strong> Coverage Type M<br />
339-6C Other <strong>Payer</strong> ID Qualifier R<br />
34Ø-7C Other <strong>Payer</strong> ID R<br />
443-E8 Other <strong>Payer</strong> Date R<br />
341-HB Other <strong>Payer</strong> Amount Paid Count R<br />
342-HC Other <strong>Payer</strong> Amount Paid<br />
Ø7=Drug Benefit<br />
R<br />
Qualifier<br />
1Ø=Sales Tax<br />
431-DV Other <strong>Payer</strong> Amount Paid Valid value of greater than $0 to reflect sum of<br />
R<br />
Other <strong>Payer</strong> Amount Paid Qualifier<br />
471-5E Other <strong>Payer</strong> Reject Count Maximum count of 5 RW (Other<br />
<strong>Payer</strong> Reject<br />
Code (472-6E)<br />
is used)<br />
472-6E Other <strong>Payer</strong> Reject Code RW (Other<br />
<strong>Payer</strong> Reject<br />
Count (471-5E)<br />
is used)<br />
The COB segment and all required fields must be sent if the Other Coverage Code (3Ø8-C8) field with values = 2<br />
through 4 are submitted in the claim segment.<br />
Note: If field 3Ø8-C8 (Other Coverage Code) is populated with:<br />
Value of 2 = Other coverage exists – payment collected; fields 341-HB, 342-HC and 431-DV are required and<br />
must have values entered. Field 431-DV must not be zero ($0.00). The sum of all occurrences must not be zero.<br />
Value of 3 = Other coverage billed – claim not covered; fields 471-5E and 472-6E are required and must have<br />
values entered.<br />
Value of 4 = Other coverage exists – payment not collected; fields 341-HB, 342-HC and 431-DV are required and<br />
must have values entered. Field 431-DV must be zero ($0.00). The sum of all occurrences must be zero.<br />
DUR/PPS Segment – Situational<br />
Field # <strong>NCPDP</strong> Field Name Value <strong>Payer</strong> Usage<br />
111-AM Segment Identification Ø8=DUR/PPS M<br />
473-7E DUR/PPS Code Counter 1=Rx Billing (maximum of 9 occurrences) R<br />
439-E4 Reason for Service Code DA=Drug-Allergy<br />
R<br />
DC=Drug-Disease (Inferred)<br />
DD=Drug-Drug Interaction**<br />
HD=High Dose (Maximum Daily Dose)<br />
ID=Ingredient Duplication<br />
LD=Low Dose (Minimum Daily Dose)<br />
NP=New Patient Processing<br />
PG=Drug-Pregnancy<br />
SX=Drug-Gender<br />
TD=Therapeutic Duplication<br />
SD=Suboptimal Drug/Indication<br />
8<br />
<strong>Payer</strong> Usage: M=Mandatory, O=Optional, R=Required by ESI to expedite claim processing,<br />
"R"=Repeating Field, RW=Required when; required if ―x‖, not required if ―y‖