Medco MedicareD Payer Sheet - Catalyst Rx
Medco MedicareD Payer Sheet - Catalyst Rx
Medco MedicareD Payer Sheet - Catalyst Rx
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
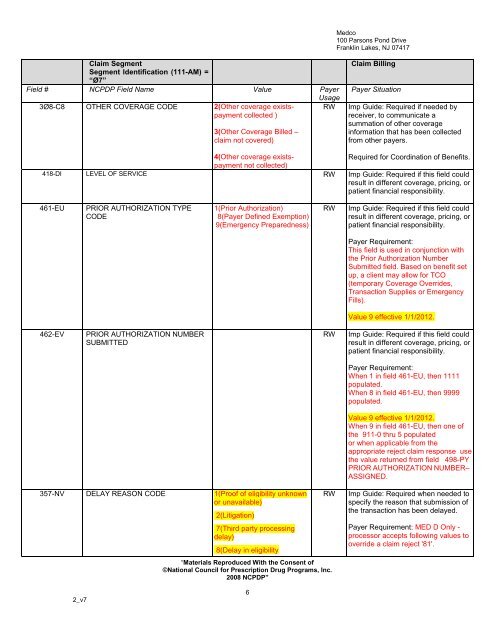
<strong>Medco</strong><br />
100 Parsons Pond Drive<br />
Franklin Lakes, NJ 07417<br />
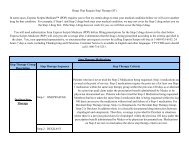
Claim Segment<br />
Segment Identification (111-AM) =<br />
“Ø7”<br />
Field # NCPDP Field Name Value <strong>Payer</strong><br />
3Ø8-C8 OTHER COVERAGE CODE 2(Other coverage existspayment<br />
collected )<br />
3(Other Coverage Billed –<br />
claim not covered)<br />
Usage<br />
RW<br />
Claim Billing<br />
<strong>Payer</strong> Situation<br />
Imp Guide: Required if needed by<br />
receiver, to communicate a<br />
summation of other coverage<br />
information that has been collected<br />
from other payers.<br />
4(Other coverage existspayment<br />
Required for Coordination of Benefits.<br />
not collected)<br />
418-DI LEVEL OF SERVICE RW Imp Guide: Required if this field could<br />
result in different coverage, pricing, or<br />
patient financial responsibility.<br />
461-EU<br />
PRIOR AUTHORIZATION TYPE<br />
CODE<br />
1(Prior Authorization)<br />
8(<strong>Payer</strong> Defined Exemption)<br />
9(Emergency Preparedness)<br />
RW<br />
Imp Guide: Required if this field could<br />
result in different coverage, pricing, or<br />
patient financial responsibility.<br />
<strong>Payer</strong> Requirement:<br />
This field is used in conjunction with<br />
the Prior Authorization Number<br />
Submitted field. Based on benefit set<br />
up, a client may allow for TCO<br />
(temporary Coverage Overrides,<br />
Transaction Supplies or Emergency<br />
Fills).<br />
Value 9 effective 1/1/2012.<br />
462-EV<br />
PRIOR AUTHORIZATION NUMBER<br />
SUBMITTED<br />
RW<br />
Imp Guide: Required if this field could<br />
result in different coverage, pricing, or<br />
patient financial responsibility.<br />
<strong>Payer</strong> Requirement:<br />
When 1 in field 461-EU, then 1111<br />
populated.<br />
When 8 in field 461-EU, then 9999<br />
populated.<br />
Value 9 effective 1/1/2012.<br />
When 9 in field 461-EU, then one of<br />
the 911-0 thru 5 populated<br />
or when applicable from the<br />
appropriate reject claim response use<br />
the value returned from field 498-PY<br />
PRIOR AUTHORIZATION NUMBER–<br />
ASSIGNED.<br />
357-NV DELAY REASON CODE 1(Proof of eligibility unknown<br />
or unavailable)<br />
2(Litigation)<br />
7(Third party processing<br />
delay)<br />
8(Delay in eligibility<br />
RW<br />
“Materials Reproduced With the Consent of<br />
©National Council for Prescription Drug Programs, Inc.<br />
2008 NCPDP”<br />
Imp Guide: Required when needed to<br />
specify the reason that submission of<br />
the transaction has been delayed.<br />
<strong>Payer</strong> Requirement: MED D Only -<br />
processor accepts following values to<br />
override a claim reject '81'.<br />
2_v7<br />
6