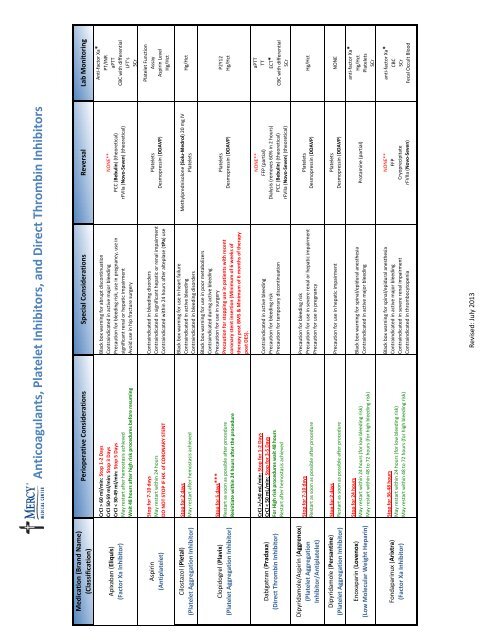
Anticoagulants Platelet Inhibitors and Direct Thrombin Inhibitors.xlsx
Anticoagulants Platelet Inhibitors and Direct Thrombin Inhibitors.xlsx
Anticoagulants Platelet Inhibitors and Direct Thrombin Inhibitors.xlsx
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
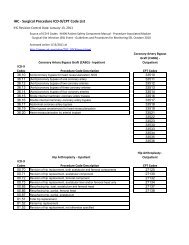
Medication (Br<strong>and</strong> Name)<br />
(Classification)<br />
Apixaban (Eliquis)<br />
(Factor Xa Inhibitor)<br />
Aspirin<br />
(Antiplatelet)<br />
Cilostazol (Pletal)<br />
(<strong>Platelet</strong> Aggregation Inhibitor)<br />
Clopidogrel (Plavix)<br />
(<strong>Platelet</strong> Aggregation Inhibitor)<br />
Dabigatran (Pradaxa)<br />
(<strong>Direct</strong> <strong>Thrombin</strong> Inhibitor)<br />
Dipyridamole/Aspirin (Aggrenox)<br />
(<strong>Platelet</strong> Aggregation<br />
Inhibitor/Antiplatelet)<br />
Dipyridamole (Persantine)<br />
(<strong>Platelet</strong> Aggregation Inhibitor)<br />
Enoxaparin (Lovenox)<br />
(Low Molecular Weight Heparin)<br />
Fondaparinux (Arixtra)<br />
(Factor Xa Inhibitor)<br />
<strong>Anticoagulants</strong>, <strong>Platelet</strong> <strong>Inhibitors</strong>, <strong>and</strong> <strong>Direct</strong> <strong>Thrombin</strong> <strong>Inhibitors</strong><br />
Perioperative Considerations Special Considerations Reversal Lab Monitoring<br />
CrCl > 60 ml/min: Stop 1‐2 Days<br />
CrCl 50‐59 ml/min: Stop 3 Days<br />
CrCl < 30‐49 ml/min: Stop 5 Days<br />
May restart after hemostasis achieved<br />
Wait 48 hours after high risk procedures before resuming<br />
Black box warning for abrupt discontinuation<br />
Contraindicated in active major bleeding<br />
Precaution for bleeding risk, use in pregnancy, use in<br />
significant renal or hepatic impairment<br />
Avoid use in hip fracture surgery<br />
NONE**<br />
PCC (Bebulin) (theoretical)<br />
rFVIIa (Novo‐Seven) (theoretical)<br />
Anti‐factor Xa*<br />
PT/INR<br />
aPTT<br />
CBC with differential<br />
LFT's<br />
SCr<br />
Stop for 7‐10 days<br />
May restart within 24 hours<br />
DO NOT STOP IF HX. of CORONARY STENT<br />
Contraindicated in bleeding disorders<br />
Contraindicated in significant hepatic or renal impairment<br />
Contraindicated within 24 hours after alteplase (tPa) use<br />
<strong>Platelet</strong>s<br />
Desmopressin (DDAVP)<br />
<strong>Platelet</strong> Function<br />
Assay<br />
Aspirin Level<br />
Hg/Hct<br />
Stop for 2 days<br />
May restart after hemostasis achieved<br />
Stop for 5 days***<br />
Restart as soon as possible after procedure<br />
Reinitiate within 24 hours after the procedure<br />
CrCl >/=50 mL/min: Stop for 1‐2 Days<br />
CrCl < 50 mL/min: Stop for 3‐5 Days<br />
For High risk procedures wait 48 hours<br />
Restart after hemostasis achieved<br />
Black box warning for use in heart failure<br />
Contraindicated in active bleeding<br />
Contraindicated in bleeding disorders<br />
Black box warning for use in poor metabolizers<br />
Contraindicated during active bleeding<br />
Precaution for use in surgery<br />
Precaution for stopping use in patients with recent<br />
coronary stent insertion (Minimum of 6 weeks of<br />
therapy post BMS & Minimum of 6 months of therapy<br />
post DES).<br />
Contraindicated in active bleeding<br />
Precaution for bleeding risk<br />
Precaution for temporary discontinuation<br />
Methylprednisolone (Solu‐Medrol) 20 mg IV<br />
<strong>Platelet</strong>s<br />
<strong>Platelet</strong>s<br />
Desmopressin (DDAVP)<br />
NONE**<br />
FFP (partial)<br />
Dialysis (removes 60% in 2 hours)<br />
PCC (Bebulin) (theoretical)<br />
rFVIIa (Novo‐Seven) (theoretical)<br />
Hg/Hct<br />
P2Y12<br />
Hg/Hct<br />
aPTT<br />
TT<br />
ECT*<br />
CBC with differential<br />
SCr<br />
Stop for 7‐10 days<br />
Restart as soon as possible after procedure<br />
Precaution for bleeding risk<br />
Precaution for use in severe renal or hepatic impairment<br />
Precaution for use in pregnancy<br />
<strong>Platelet</strong>s<br />
Desmopressin (DDAVP)<br />
Hg/Hct<br />
Stop for 2 days<br />
Restart as soon as possible after procedure<br />
Precaution for use in hepatic impairment<br />
<strong>Platelet</strong>s<br />
Desmopressin (DDAVP)<br />
NONE<br />
Stop for 24 hours<br />
May restart within 24 hours (for low bleeding risk)<br />
May restart within 48 to 72 hours (for high bleeding risk)<br />
Black box warning for spinal/epidural anesthesia<br />
Contraindicated in active major bleeding<br />
Protamine (partial)<br />
anti‐factor Xa*<br />
Hg/Hct<br />
<strong>Platelet</strong>s<br />
SCr<br />
Stop for 36‐48 hours<br />
May restart within 24 hours (for low bleeding risk)<br />
May restart within 48 to 72 hours (for high bleeding risk)<br />
Black box warning for spinal/epidural anesthesia<br />
Contraindicated in active major bleeding<br />
Contraindicated in severe renal impairment<br />
Contraindicated in thrombocytopenia<br />
NONE**<br />
FFP<br />
Cryoprecipitate<br />
rFVIIa (Novo‐Seven)<br />
anti‐factor Xa*<br />
CBC<br />
SCr<br />
Fecal Occult Blood<br />
Revised: July 2013
<strong>Anticoagulants</strong>, <strong>Platelet</strong> <strong>Inhibitors</strong>, <strong>and</strong> <strong>Direct</strong> <strong>Thrombin</strong> <strong>Inhibitors</strong><br />
Medication (Br<strong>and</strong> Name)<br />
(Classification)<br />
Heparin<br />
(Anticoagulant)<br />
Herbal Supplements<br />
Perioperative Considerations Special Considerations Reversal Lab Monitoring<br />
IV: Stop for 2‐6 hours depending on the dose<br />
Subq: Stop for 12‐24 hours depending on the dose<br />
May restart within 24 hours (for low bleeding risk)<br />
May restart within 48 to 72 hours (for high bleeding risk)<br />
Stop for 7 days<br />
Black box warning for use of benzyl alcohol preserved<br />
product in neonates<br />
Contraindicated in severe thrombocytopenia<br />
Contraindicated in uncontrolled, active bleeding (except<br />
DIC)<br />
Contraindicated in patients with history of HIT<br />
Protamine<br />
aPTT<br />
anti‐factor Xa*<br />
ACT<br />
Hg/Hct<br />
<strong>Platelet</strong>s<br />
Fecal Occult Blood<br />
Various supplements increase the risk for bleeding N/A N/A<br />
NSAID's Stop for 1‐3 days<br />
All NSAID's (other than aspirin) may cause reversible<br />
inhibition of platelet function <strong>and</strong> should be stopped<br />
perioperatively to reduce the risk of bleeding associated<br />
with reduced platelet function<br />
N/A N/A<br />
Prasugrel (Effient)<br />
(<strong>Platelet</strong> Aggregation Inhibitor)<br />
Stop for 7 days***<br />
Restart as soon as possible after procedure<br />
Black box warning for bleeding risk<br />
Black box warning for use in active bleeding<br />
Black box warning for use in patients 75 <strong>and</strong> older or<br />
weighing less than 60 kg<br />
Contraindicated if history of TIA or stroke<br />
Precaution for stopping use in patients with recent<br />
coronary stent insertion (Minimum of 6 weeks of<br />
therapy post BMS & Minimum of 6 months of therapy<br />
post DES).<br />
<strong>Platelet</strong>s<br />
Desmopressin (DDAVP)<br />
P2Y12<br />
Hg/Hct<br />
Rivaroxiban (Xarelto)<br />
(Factor Xa Inhibitor)<br />
Stop for 1 Day when renal function is WNL<br />
Stop for 2 Days with CrCL 60‐90 mL/min<br />
Stop for 3 Days with Cr. CL of 30‐59 mL/min<br />
Stop for 4 Days with Cr.CL 15‐29 mL/min<br />
May restart within 6 hours<br />
For High risk procedures: wait 48 hours before resuming<br />
Black box warning for spinal/epidural anesthesia<br />
Contraindicated in active major bleeding<br />
Precaution for bleeding risk, use in pregnancy, use in<br />
significant renal or hepatic impairment<br />
NONE**<br />
PCC (Bebulin) (theoretical)<br />
rFVIIa (Novo‐Seven) (theoretical)<br />
Anti‐factor Xa*<br />
PT/INR<br />
aPTT<br />
CBC with differential<br />
LFT's<br />
SCr<br />
Ticagrelor (Brilinta)<br />
(<strong>Platelet</strong> Aggregation Inhibitor)<br />
Stop for 5 days***<br />
Restart as soon as possible after procedure<br />
Black box warning for bleeding risk<br />
Black box warning for stopping use<br />
Precaution for use with aspirin doses above 100 mg<br />
<strong>Platelet</strong>s<br />
Desmopressin (DDAVP)<br />
P2Y12<br />
Hg/Hct<br />
SCr<br />
Uric Acid level<br />
Ticlopidine (Ticlid)<br />
(<strong>Platelet</strong> Aggregation Inhibitor)<br />
Stop for 10‐14 days***<br />
Restart as soon as possible after procedure<br />
Black box warning for blood dyscrasias (TTP, neutropenia,<br />
or aplastic anemia)<br />
Precaution for bleeding risk<br />
Precaution use in sig renal/hepatic impairment<br />
<strong>Platelet</strong>s<br />
Desmopressin (DDAVP)<br />
P2Y12<br />
CBC with differential<br />
LFT's<br />
Warfarin (Coumadin)<br />
(Coumadin Anticoagulant)<br />
Stop for 1‐8 days depending on the INR<br />
INR decreases to
<strong>Anticoagulants</strong>, <strong>Platelet</strong> <strong>Inhibitors</strong>, <strong>and</strong> <strong>Direct</strong> <strong>Thrombin</strong> <strong>Inhibitors</strong><br />
Approach to Bridging Therapy<br />
Condition: Bridging Therapy Required: No Bridging Therapy: Comments:<br />
Mechanical Heart Valve Mitral‐value replacement, two or more mechanical<br />
valuves, nonbileaflet aortic‐valves, replacement, or<br />
aortic‐value replacement with other risk factors.<br />
Aortic‐valve replacement, bileaflet<br />
prosthesis, <strong>and</strong> no additional risk factors.<br />
Other risk factors include prior<br />
stroke, TIA, intracardiac thrombus,<br />
or cardioembolic event.<br />
Nonvalvular Atrial Fibrillation Prior stroke or embolic event, cardiac thrombus, No prior stroke or embolic event, Prior stroke, TIA, intracardiac<br />
or CHADS score >/= 4. absence of thrombus, or CHADS score thrombus, or cardioembolic<br />
of < 4. event increases risk.<br />
Venous Thromboembolism Venous thromboembolism within previous 3 Venous thromboembolism > 3 months Consider inferior vena cava<br />
months or severe thrombophilia. previously or no additional risk factors filter if venous thromboembolism<br />
(e.g. active cancer <strong>and</strong> nonsevere<br />
thrombophilia). occurred < 1 month previously, if<br />
urgent or emergent surgery is<br />
required, or if there is a<br />
contraindication to anticoagulation<br />
therapy.<br />
Medications High risk patients with CrCL < 30 mL/min: Use Heparin<br />
Mechanical Heart Valve or Afib: Lovenox 1 mg/kg<br />
every 12 hours.<br />
Hx VTE: Lovenox 1.5 mg/kg daily<br />
Source: The New Engl<strong>and</strong> Journal of Medicine 368;22. May 30, 2013<br />
Revised: July 2013