Restorative Procedure - Kerr Hawe
Restorative Procedure - Kerr Hawe
Restorative Procedure - Kerr Hawe
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Clinical Guide for <strong>Restorative</strong> <strong>Procedure</strong><br />
Adhesives | Composites | Finishing and Polishing<br />
Your practice is our inspiration. <br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Clinical Guide
All you need is <strong>Kerr</strong><br />
Introduction<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
INDEX<br />
<strong>Restorative</strong> procedure steps and products overview 3-6<br />
Bonding:<br />
Bonding & Adhesion, Prof. David Watts, Dr. Nick Silikas 7-8<br />
OptiBond Family 9-10<br />
OptiBond FL 11-12<br />
OptiBond Solo Plus 13-14<br />
OptiBond All-In-One 15-16<br />
Composites:<br />
Aesthetics and composite, Prof. Angelo Putignano 17-20<br />
Herculite XRV Ultra 21-22<br />
Clinical case: Class IV 23-24<br />
Clinical case: Class V 25-26<br />
Clinical case: Class II 27-28<br />
Clinical case: Class I 29<br />
Finishing and Polishing:<br />
Finishing and polishing of composite restorations, Prof. Martin Jung 31-33<br />
Surface treatment of composite filling overview 34-36<br />
OptiDisc 37-38<br />
HiLuster Plus Polishing System 39-40<br />
OptiShine 41<br />
Herculite XRV, OptiBond FL References 42<br />
Authors Biographies 43<br />
1
Everyday challenge in restorative procedure is<br />
to achieve aesthetic results in a simple, fast and<br />
reliable way. <strong>Kerr</strong>’s competence in composites<br />
and adhesive systems accompanied with smart<br />
<strong>Hawe</strong> restorative tools offer solutions for<br />
predictable and faster results in each clinical<br />
situation.<br />
This guide for restorative procedure summarizes<br />
different materials, tools and techniques which<br />
are essential to achieve high quality restorations<br />
with long term clinical success.<br />
2<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Introduction<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
STEP PRODUCT KERR PRODUCTS<br />
Caries<br />
diagnostic<br />
X-rays<br />
Film and Sensor Holder Line<br />
Kwik-Bite SuperBite Anterior SuperBite Posterior<br />
Cavity<br />
preparation<br />
Burs<br />
Beavers Carbide Jet Burs<br />
BlueWhite Diamond Burs<br />
Beavers Carbide Jet Bur<br />
BlueWhite Diamond Bur<br />
Accessories<br />
OptiDam <br />
SoftClamp <br />
Fixafloss <br />
OptiDam<br />
OptiView <br />
SoftClamp<br />
OptiView<br />
Fixafloss<br />
3
STEP PRODUCT KERR PRODUCTS<br />
Adhesion<br />
Total-Etch<br />
OptiBond FL<br />
OptiBond Solo Plus <br />
Self-Etch<br />
OptiBond All-In-One<br />
Composite<br />
Filling<br />
Nanohybrid<br />
Microhybrid<br />
Premise <br />
Premise Packable<br />
Herculite ® XRV Ultra <br />
Herculite ® XRV <br />
Point 4 <br />
Flowable<br />
Premise Flowable<br />
Premise<br />
Premise Packable<br />
Herculite XRV Ultra<br />
Revolution Formula 2<br />
Premise Flowable<br />
4<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Introduction<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
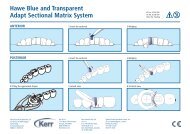
STEP PRODUCT KERRHAWE PRODUCTS<br />
Application<br />
methods<br />
Matrices<br />
SuperMat ® System<br />
<strong>Hawe</strong> Adapt ® Matrices<br />
Lucifix ® Matrices<br />
Adapt SuperCap<br />
Steel and Transparent Matrices<br />
Lucifix Matrice<br />
SuperMat System<br />
<strong>Hawe</strong> Adapt ® Sectional Matrices<br />
<strong>Hawe</strong> Transparent Cervical Matrices<br />
Wedges<br />
<strong>Hawe</strong> Sycamore Wedges<br />
Sectional Matrice<br />
Cervical Matrices<br />
Wedge Dispenser<br />
Hand shaping<br />
instruments<br />
CompoRoller <br />
CompoRoller<br />
Polymerization<br />
Halogen curing lights<br />
LED lamps<br />
OptiLux 501, Demetron LC<br />
Demetron A1 and A2<br />
LEDemetron II<br />
DEMI<br />
Demetron A1 and A2<br />
Demi<br />
5
Finishing and<br />
polishing<br />
Flexible disc<br />
Abrasive strips<br />
OptiDisc ®<br />
OptiStrip <br />
OptiDisc<br />
OptiStrip<br />
Abrasive brushes<br />
Occlubrush ®<br />
OptiShine <br />
Occlubrush<br />
OptiShine<br />
Polishers<br />
HiLuster Polishing System<br />
Gloss Plus Polishers<br />
HiLuster Plus Polishers<br />
Professional cleaning<br />
Cleanic ®<br />
CleanPolish and SuperPolish<br />
Pro-Cup ®<br />
Brushes<br />
Cleanic Mint, Apple and Bubble Gum<br />
Pro-Cup<br />
6<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Adhesives<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Adhesives<br />
Bonding & Adhesion<br />
Prof. David Watts, Dr. Nick Silikas, University of Manchester, UK<br />
The mechanism of enamel bonding is based on a<br />
micro-mechanical bond between the resin and the<br />
phosphoric acid conditioned rough surface of the<br />
enamel.Enamel conditioning remains the most<br />
commonly used method to bond resin-composites<br />
to enamel surface. It provides strong bonds.<br />
Enamel conditioning may be regained by re-etching<br />
the surface and applying the resin, thus recovering<br />
the required shear bond strength at the enamel-resin<br />
interface, and allowing the resin to mechanically<br />
bond onto its surface.<br />
Dentine however has a much more complex<br />
structure than enamel. Prior to dentine-bonding,<br />
the removal or modification of the smear layer is<br />
indicated to clear the openings of the dentine<br />
tubules by conditioning the surface of the dentine.<br />
A fluid adhesive is then applied over the dentine<br />
and cured, ensuring that optimum wetting of the<br />
surface and absorption into the dentinal tubules<br />
is achieved; thus creating an inter-penetrating<br />
network with the demineralised collagen in the<br />
dentinal tubules, hence forming the hybrid layer.<br />
Preservation of the hybrid layer prior to the<br />
application of the hydrophobic resin restoration<br />
is imperative for an efficient bond to form between<br />
the resin and dentine. Therefore, any contamination<br />
of any region of the adhesive system would<br />
evidently jeopardise the integrity of the bond.<br />
The mechanism proposed for this material was<br />
to bond to the organic component of the dentine,<br />
namely the collagen. The first work to investigate<br />
the mechanism of bonding to the dentine was by<br />
Nakabayashi (1). He first identified a layer between<br />
the resin and dentine substrate referred to as<br />
“hybrid” dentine, in that it was the organic components<br />
of the dentine that had been permeated by<br />
resin.<br />
The term “hybrid layer” has now become synonymous<br />
with bonding of resins to etched dentine.<br />
There has been a tremendous amount of research<br />
done on the hybrid layer, its structure, formation<br />
and how it can be improved. This layer has also<br />
been referred to as the “resin-dentine interdiffusion<br />
zone” (2).<br />
Classification<br />
Numerous dentine bonding agents have been<br />
commercially introduced. These changes have<br />
been referred by some people as “generations”,<br />
implying that there was a chronological development.<br />
This can be very confusing. A more consistent<br />
and logical approach is to classify bonding<br />
agents by the number of steps needed to complete<br />
the bonding process.<br />
“Three-step” or “Conventional” systems<br />
This group typically consists of three separate<br />
application steps: etching, priming and adhesive<br />
resin. They are also known as “etch-and-rinse”<br />
7
systems. Although they were the first ones<br />
introduced, they are still widely used and have<br />
been shown to provide reliable bonding. Their<br />
main drawback seems to be technique sensitivity,<br />
since any deviation from the recommended<br />
procedure will result in inferior bonding.<br />
“Two-step” systems<br />
This group can be subdivided into two subgroups:<br />
i) they have a separate etch and have combined<br />
the priming and bonding steps. These systems<br />
are often referred to as “Single-bottle” systems.<br />
Similar problems found with the “Three-step”<br />
system can also be seen here.<br />
ii) etching and priming steps are combined together<br />
and bonding is separate. This is referred to as<br />
“Self-etching primers”. An acidic resin etches and<br />
infiltrates the dentine simultaneously. The tooth<br />
does not need to be rinsed which decreases<br />
the clinical application time and also reduces<br />
technique sensitivity by eliminating the need to<br />
maintain the dentine in a moist state.<br />
“One-bottle” or “All-in-one” systems<br />
This is when all steps are combined into one<br />
process. Their mode of action is similar to that of<br />
the “self-etching primers”, but the bonding resin is<br />
also incorporated. It is considered that these do<br />
not etch as effectively as the previous ones. They<br />
are the most recently introduced so limited clinical<br />
data is available.<br />
Bonding mechanism<br />
This micromechanical coupling of restorative<br />
materials to dentine, via an intermediate adhesive<br />
layer, is referred to as dentine bonding (3). The<br />
resin in the primer and bonding step penetrates<br />
the collapsed collagen fibrils (after demineralisation),<br />
and forms an interpenetrating network. This<br />
layer had been described extensively and in great<br />
detail (4, 5). The thickness of the hybrid layer<br />
ranges from less than 1 µm for the all-in-one<br />
systems to up to 5 µm for the conventional systems.<br />
The bond strength is not dependent on the<br />
thickness of the hybrid layer, as the self-etching<br />
priming materials have shown bond strengths<br />
greater than many other systems but exhibit a<br />
thin hybrid layer. The etching, rinsing and drying<br />
process cause the dentine to collapse due to the<br />
loss of the supporting hydroxyapatite structure.<br />
The collapsed state of collagen fibrils was hindering<br />
the successful diffusion of the resin monomers.<br />
To overcome this problem, two approaches were<br />
introduced. The first one is called “dry-bonding<br />
technique” and involves air-drying of dentine after<br />
etching and subsequent application of a waterbased<br />
primer that can re-expand the collapsed<br />
collagen (6, 7). The second one is the “wet bonding<br />
technique” in which the demineralized collagen is<br />
supported by residual water after washing (8). This<br />
allows the priming solution to diffuse throughout<br />
the collagen fibre network more successfully.<br />
However, when it comes to clinical practice, it is<br />
very difficult to find the correct balance of residual<br />
moisture. Excess water can be detrimental to<br />
bonding and these problems have been described<br />
as “overwetting phenomena” (9). Since the<br />
“dry-bonding technique” is considered to be<br />
significantly less technique sensitive, it should<br />
be preferred over the most difficult to standardize<br />
“wet bonding technique” (2).<br />
Relevant in-vitro bond strength studies can provide<br />
a useful indication of the prospective clinical<br />
success of a system. However, the highest level of<br />
evidence for comparing the efficiency of a bonding<br />
system is obtained from randomised clinical trials.<br />
Randomised clinical trials with elongated the<br />
treatment periods will be very useful in assessing<br />
both the effectiveness of a particular group and<br />
a particular method of application.<br />
References<br />
1. Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by<br />
the infiltration of monomers into tooth substrates. J Biomed Mater Res<br />
1982;16:265-273.<br />
2. Van Landuyt K, De Munck J, Coutinho E, Peumans M, Lambrechts P,<br />
Van Meerbeek B. Bonding to Dentin: Smear Layer and the Process of<br />
Hybridization. In: Eliades G, Watts DC, Eliades T, editors. Dental Hard<br />
Tissues and Bonding Interfacial Phenomena and Related Properties Berlin:<br />
Springer; 2005. p. 89-122.<br />
3. Eick JD, Gwinnett AJ, Pashley DH, Robinson SJ. Current concepts on<br />
adhesion to dentin. Crit Rev Oral Biol Med 1997;8:306-335.<br />
4. Van Meerbeek B, Braem M, Lambrechts P, Vanherle G. Morphological<br />
characterization of the interface between resin and sclerotic dentine.<br />
J Dent Res 1994;22:141-146.<br />
5. Van Meerbeek B, Inokoshi S, Braem M, Lambrechts P, Vanherle G.<br />
Morphological aspects of the resin-dentin interdiffusion zone with<br />
different dentin adhesive systems. J Dent Res 1992;71:1530-1540.<br />
6. Finger WJ, Balkenhol M. Rewetting strategies for bonding to dry dentin<br />
with an acetone-based adhesive. J Adhes Dent 2000;2:51-56.<br />
7. Frankenberger R, Krämer N, Petschelt A. Technique sensitivity of dentin<br />
bonding: effect of application mistakes on bond strength and marginal<br />
adaptation. Oper Dent 2000;25:324-330.<br />
8. Kanca JI. Effect of resin primer solvents and surface wetness on resin<br />
composite bond strength to dentin. Am J Dent 1992;5:213-215.<br />
9. Tay FR, Gwinnett JA, Wei SH. Micromorphological spectrum from<br />
overdrying to overwetting acid-conditioned dentin in water-free acetonebased,<br />
single-bottle primer/adhesives. Dent Mater 1996;12:236-244.<br />
8<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Adhesives<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
OptiBond <br />
Respected by leading opinion leaders, perceived as the gold<br />
standard of the adhesive technology OptiBond family provides<br />
performance, versatility and predictable results.<br />
... the name that stands<br />
for adhesive brilliance...<br />
OptiBond Family<br />
Total-etch<br />
Self-etch<br />
Chemistry Behind<br />
GPDM Adhesive Monomer<br />
No. of steps 3 2 1<br />
Gel Etchant<br />
All OptiBond adhesives comprise the unique<br />
proprietary chemistry which made OptiBond TM<br />
FL the gold standard among bonding agents.<br />
Proven GPDM adhesive monomers are effective<br />
in creating a superb bond with minimized risk of<br />
microleakage and post-operative sensitivity.<br />
Primer<br />
Adhesive<br />
4 th generation 5 th generation 7 th generation<br />
GPDM = Glycero-Phosphate-1.3 Dimethacrylate<br />
9
OptiBond OptiBond OptiBond <br />
FL Solo Plus All-In-One<br />
Years in market 15 years 10 years 3 years<br />
Application<br />
Direct procedure • • •<br />
Indirect procedure - • •<br />
Etching Yes Yes No<br />
Application time 1:30 min. 1:10 min. 0:55 min.<br />
Bond strength Mpa<br />
To dentine 32 MPa 31 MPa 36 MPa<br />
To enamel 33 MPa 34 MPa 26 MPa<br />
Properties<br />
Filler load 48% 15% 7%<br />
Works on wet or dry dentine • • •<br />
Film thickness ~60 µ ~10 µ ~5 µ<br />
Radiopacity 267% Al - -<br />
Solvent Water Ethanol Water, Ethanol,<br />
Ethanol<br />
Acetone<br />
Packaging<br />
Storage conditions Ambient Ambient Refrigeration<br />
temperature temperature 2 °C to 8 °C<br />
Bottle content<br />
Primer Bottle 8 ml<br />
Adhesive Bottle 8 ml<br />
5 ml 5 ml<br />
Unidose content 0.1 ml 0.1 ml 0.18 ml<br />
Filled adhesive technology<br />
The technology of filled adhesives was first<br />
time ever introduced by <strong>Kerr</strong> in its OptiBond FL<br />
adhesive.<br />
Glass Filler in OptiBond Adhesive:<br />
• Reinforces the dentin tubules for high bond<br />
strengths and protection against microleakage<br />
• Releases fluoride over the long-term<br />
• Decreases polymerization shrinkage<br />
• Works as a shock absorber and thermal barrier<br />
between the restorative material and the tooth<br />
• Virtually eliminates post-operative sensitivity<br />
• Works well in dry, moist or wet environment<br />
10<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Adhesives<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
OptiBond FL<br />
Two-bottle total-etch adhesive system<br />
OptiBond FL launched in 1995 established from<br />
the beginning the standard in the adhesive<br />
technology. Over 15 years it has been successful<br />
worldwide, proven in long-term clinical studies<br />
and recommended as the gold standard by<br />
leading dental universities worldwide.<br />
After applying OptiBond FL I can achieve a<br />
reliable bonding without any post-operative<br />
sensitivity. Also I can use successfuly<br />
OptiBond FL in any bonding procedure.<br />
Prof. Marco Ferrari<br />
Features<br />
• Unique structural bond. 48% filler load<br />
delivers superior bond strength.<br />
• Efficient application flow. One coat primer.<br />
One coat adhesive. Wet or dry prep.<br />
• Highly radiopaque. 267% radiopacity makes<br />
X-ray detection easy.<br />
• Delivery options. The only two-bottle<br />
adhesive available in bottle and Unidose delivery.<br />
• Proven long-term performance.<br />
The legend among<br />
the adhesives<br />
11
OptiBond FL<br />
Application Guide<br />
OptiBond FL wins<br />
REALITY’S 20 th<br />
Anniversary Legacy<br />
Award, emblematic of<br />
extraordinary long-term<br />
clinical performance.<br />
Technique<br />
Technique<br />
Summary<br />
Summary<br />
Clinical Success<br />
13-year Clinical Study<br />
Clinical Evaluation of a Dentin Adhesive<br />
System: 13 Year Results, A. A. Boghosian<br />
and J.L. Drummond and E. P. Lautenschlager,<br />
Northwestern University Feinberg School of<br />
Medicine<br />
1. Etch enamel with <strong>Kerr</strong><br />
Gel Etchant<br />
(35% phosphoric acid)<br />
for 15 seconds.<br />
2. Rinse thoroughly for<br />
15 seconds.<br />
3. Air dry for 3 seconds.<br />
Do not dessicate.<br />
4. Apply Primer (yellow<br />
rocket for Unidose delivery)<br />
with light brushing motion<br />
for 15 secs.<br />
Conclusion: At thirteen years, the OptiBond<br />
adhesive system has demonstrated outstanding<br />
performance in both retention and sealing of<br />
the tooth. OptiBond has further demonstrated<br />
effectiveness, in conjunction with composite,<br />
eliminating sensitivity resulting from abfraction<br />
lesions.<br />
Over 10 years<br />
posttreament with<br />
OptiBond FL.<br />
5. Air dry for 5 seconds. 6. Using second applicator,<br />
apply Adhesive (black<br />
rocket for Unidose<br />
delivery) with light<br />
brushing motion for<br />
15 secs.<br />
7. Air thin for 3 seconds. 8. Light cure for<br />
20 seconds*. Surface<br />
is ready for composite<br />
placement.<br />
Over 13 years<br />
posttreatment with<br />
OptiBond FL<br />
Cases courtesy of Dr. Alan Boghosian<br />
* Recommended Cure Times: Demi 5 sec., L.E.Demetron II 5 sec., L.E.Demetron I, 10 sec. or Optilux 501 in Boost mode 10 sec.<br />
12<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Adhesives<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
OptiBond Solo Plus<br />
Single component total-etch adhesive<br />
OptiBond Solo Plus is a single component<br />
adhesive that combines primer and adhesive<br />
in one step. Combining primer and adhesive<br />
in one bottle answered the need for a simplerto-use<br />
bonding agent that maintained total-etch<br />
strength and durability.<br />
Case courtesy of Prof. Angelo Putignano<br />
Features<br />
• Strong bond. Proven performance achieved<br />
with simplified application procedure.<br />
The durable chemical and micro-mechanical<br />
bonds protect against microleakage to ensure<br />
superior marginal integrity.<br />
• Filled technology. OptiBond Solo Plus is<br />
15%-filled with the same 0.4 micron filler<br />
found in <strong>Kerr</strong>'s industry-recognized composites.<br />
• Ethanol based. The adhesion promoters are<br />
carried in an ethanol solvent, diminishing both<br />
the tedious need for multiple coats and constant<br />
reapplication commonly found with acetone<br />
adhesives.<br />
• Versatile. Effective in use for all direct<br />
and indirect indications. Use in moist or<br />
dry environment.<br />
• Unidose delivery. Available in bottle and<br />
Unidose delivery.<br />
High performance easy-touse<br />
total-etch adhesive<br />
13
OptiBond Solo Plus<br />
Application Guide<br />
Clinical Research<br />
Dentin Shear Bond Strength (MPa)<br />
of 5th-Generation Adhesives<br />
35<br />
30<br />
25<br />
31<br />
20<br />
15<br />
10<br />
5<br />
20 21 22<br />
Table missing<br />
23 23<br />
0<br />
Excite ® XP Bond Adper Prime ® & One Step ® OptiBond ®<br />
Single Bond Bond NT Plus Solo Plus <br />
Published by H. Lu*, H. Bui, X. Qian, D. Tobia, <strong>Kerr</strong> Corporation,<br />
IADR 2008, #401<br />
1. Etch enamel and dentine<br />
for 15 seconds.<br />
2. Rinse thoroughly<br />
for 15 seconds.<br />
3. Air dry for 3 seconds.<br />
Do not dessicate.<br />
4. Shake unidose before<br />
dispensing.<br />
5. Twist open the<br />
unidose.<br />
6. Dip brush. Apply<br />
OptiBond Solo Plus<br />
for 15 seconds using<br />
light brushing motion.<br />
7. Air thin for 3 seconds. 8. Light cure for 20<br />
seconds*. Surface is<br />
ready for composite<br />
placement.<br />
STRONG DURABLE BOND. SEM Image<br />
shows excellent penetration of OptiBond<br />
Solo Plus into demineralized dentin,<br />
forming long resin tags and a well-defined<br />
hybrid layer, which results in superior bond<br />
strength.<br />
* Recommended Cure Times: Demi 5 sec., L.E.Demetron II 5 sec., L.E.Demetron I, 10 sec. or Optilux 501 in Boost mode 10 sec.<br />
14<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Adhesives<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
OptiBond All-In-One<br />
Single step, self-etch adhesive<br />
OptiBond All·In·One Self-Etch Adhesive delivers excellent penetration<br />
of dentin tubules, providing exceptional bond strength and protection<br />
against microleakage and post-op sensitivity. Its unique nano-etching<br />
capability enables the most effective enamel etching of any existing<br />
single-component adhesive, creating a deeper etched surface for higher<br />
mechanical retention and chemical bonding. In addition its low film<br />
thickness creates an effective, single-phase adhesive interface for easier<br />
seating and better fit of your final restoration.<br />
Effective enamel nano-etching<br />
SEM image shows clearly<br />
exposed nanoscale enamel<br />
hydroxyapatite crystals,<br />
which present greater<br />
rough surface area<br />
for micromechanical<br />
retention and chemical<br />
bonding.<br />
Well defined adhesive layer<br />
Dentin Interface and<br />
Superb Sealing Ability<br />
Provides a Well Defined<br />
Adhesive.<br />
SEM shows the composite,<br />
OptiBond All-In-One<br />
adhesive layer and dentin<br />
bonding interface.<br />
Effective bonding<br />
in a simple way<br />
15
OptiBond All-In-One<br />
Application Guide<br />
Clinical Research<br />
Shear Bond Strength of Single-Component<br />
Self-Etch Adhesive Systems to Human Dentine<br />
(24 hr)*<br />
20 seconds<br />
Shear Bond Strength (MPa)<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
30,4<br />
10,3<br />
20,2<br />
32,2<br />
35,0<br />
Clearfil ® GBond iBond Xeno ® IV OptiBond ®<br />
S 3 Bond<br />
All•In•One<br />
1. Shake.<br />
2. Twist open. 3. Dip brush. 4. Apply first application<br />
with scrubbing motion.<br />
Shear Bond Strength of Single-Component<br />
Self-Etch Adhesive Systems to Bovine<br />
Enamel (24 hr)*<br />
20 seconds<br />
5. Dip brush. 4. Apply second<br />
application with<br />
scrubbing motion.<br />
7. Gently air dry, then<br />
use medium force<br />
to air dry for at least<br />
5 seconds.<br />
8. Light cure for<br />
10 seconds*.<br />
Shear Bond Strength (MPa)<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
21,7<br />
23,0<br />
11,3<br />
21,6<br />
28,2<br />
Clearfil ® GBond iBond Xeno ® IV OptiBond ®<br />
S 3 Bond<br />
All•In•One<br />
* Study conducted by Dr. James Dunn of Loma Linda University.<br />
Trademarks are property of their respective owners.<br />
* Recommended Cure Times: Demi 5 sec., L.E.Demetron II 5 sec., L.E.Demetron I, 10 sec. or Optilux 501 in Boost mode 10 sec.<br />
16<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Composites<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
COMPOSITES<br />
Aesthetics and composite<br />
Prof. Angelo Putignano, University of Marche, Ancona, Italy<br />
Since the ancient Greeks great philosophers, such<br />
as Plato, Baumgarten, Kant, Hegel, Vico and Croce,<br />
have sought to place the concept of aesthetics and<br />
beauty on a rational and “scientific” basis.The triad<br />
of beauty, goodness and truth represents the ideal<br />
to which individuals should aspire in the attainment<br />
of what is called “perfection”, which perhaps does<br />
not exist. Most widely shared concepts on<br />
perceived beauty arise from interaction between<br />
“sensibility” emotional and instinctive influence,<br />
and “intellect” or rational factors. Hutchinson and<br />
Shaftesbury defined felicitously aesthetics as the<br />
aptitude for perceiving harmony (Inquiry into the<br />
origin of our ideas of beauty 1725).<br />
Cosmetics tend to be distinguished from aesthetics,<br />
which is searching for a stereotype of beauty<br />
regardless of the natural context in which the<br />
subject is placed. Aesthetics, on the other hand,<br />
would be an expression of a natural archetype<br />
in accordance with mathematical theorem, with<br />
clear and translatable principles of beauty.<br />
In this respect, an ethical inner sense of aesthetics<br />
has been theorized, defined as the passive ability<br />
to receive ideas of beauty from all objects in which<br />
there is uniformity in variety ("harmony") (1). These<br />
objective factors, which accept an interaction<br />
between the object and the “mental categories” of<br />
the observer, provide the rational basis of beauty.<br />
Numerous rules of beauty have been applied to<br />
anatomy in formulating dentofacial proportions<br />
coherent with the “golden section” (Leonardo), or<br />
in accordance with anthropometric (cephalometric)<br />
parameters adopted from epidemiological studies.<br />
However, there are a series of subjective factors<br />
peculiar to instinctive emotional and psychological<br />
context of the observer, which can significantly<br />
condition the sensitivity to beauty. Also to assimilate<br />
to “taste” and perception of beauty correlated with<br />
the epoch and specific historical, cultural and social<br />
context in which the observer inhabits. Pilkington<br />
defined dental aesthetics in 1936 as “the science of<br />
copying, harmonising our work with that of nature,<br />
seeking to minimise it as much as possible”.<br />
A few decades ago, the majority of dentists working<br />
in the field of restoration concentrated on long-term<br />
solutions and the appearance of the restorations<br />
was of secondary importance (2). Thus, in ordinary<br />
practice, restorations made of amalgam and crowns<br />
made of gold alloy were utilised as the main and<br />
most lasting solutions and patients accepted these<br />
dental restorations despite their unpleasant<br />
appearance. The evolution of preventive and<br />
conservative dentistry has had a great impact on<br />
the development of restorative aesthetic dentistry.<br />
The success of preventive dentistry has resulted<br />
in teeth without caries and therefore white and not<br />
restored, with a resulting increase in the demand<br />
for aesthetic restorations.<br />
Good appearance, together with good overall health,<br />
with adequate restoration of function, and an<br />
attractive smile play an important role in modern<br />
society. In general, a smile is beautiful when the<br />
teeth are well characterised in respect to their<br />
shape, contour, colour, surface texture and detail,<br />
emergence profile, angle and position, and incisal<br />
occlusion. The aim of every aesthetic restoration is<br />
to be credible and natural with regards to function<br />
with maximum preservation of dentition and<br />
periodontal tissues, in achieving this objective the<br />
clinician must select the most suitable materials<br />
17
for resistance, biocompatibility, and of course<br />
aesthetic appearance. Composite resins have now<br />
been in use for over three decades and in recent<br />
years have become a solution that is adopted<br />
more often, because of their excellent aesthetics<br />
and their ever better mechanical properties (3).<br />
The term composite refers to a combination of at<br />
least two chemically diverse materials, with a distinct<br />
interface to separate the two components. Superior<br />
properties are exhibited when in combination,<br />
opposed to when used separately.<br />
When formulating a composite resin, we identify<br />
three different components:<br />
• Organic matrix;<br />
• Inorganic filler;<br />
• Binding agent.<br />
The organic matrix of the most modern composite<br />
resins consists mainly of the monomer developed<br />
by Bowen in 1957, through a reaction between<br />
one molecule of bisphenol A and two molecules<br />
of glycidyl methacrylate (GMA), yields a viscous<br />
monomer of high molecular weight which is called<br />
BISGMA. In the formulation of the matrix of<br />
composite resins we then find other monomers of<br />
lower molecular weight in lower percentages such<br />
as TEDGMA (triethylene glycol dimethacrylate, the<br />
most used), UEDMA (diurethane dimethacrylate,<br />
sometimes used as the sole component of the<br />
matrix), MMA (methyl methacrylate) and others of<br />
less importance and little used.<br />
The second component of a composite resin is<br />
the inorganic filler, which is added to the matrix<br />
to increase its resistance characteristics, which<br />
are otherwise insufficient, such as hardness,<br />
resistance to compression, resistance to wear<br />
and impermeable.<br />
The fillers can be classified on the basis of their<br />
chemical nature into fillers based on silicon dioxide<br />
or colloidal silica, quartz, vitreous materials, other<br />
metals or zirconium.<br />
On the other hand, Bayne in 1994 suggested the<br />
following subdivision based on the diameter of<br />
the particles:<br />
• mega fillers (from 2 to 0.5 mm)<br />
• macro fillers (from 100 to 10 µm)<br />
• medium fillers (from 10 to 1 µm)<br />
• mini fillers (from 1 to 0.1 µm)<br />
• micro fillers (from 0.1 to 0.01 µm)<br />
• nano fillers (from 0.01 to 0.005 µm)<br />
Based on production techniques, conventional or<br />
traditional fillers are produced by trituration of the<br />
inorganic substances listed above, obtaining a<br />
macro filler with particles of irregular shape and<br />
size, which require little monomer to become wet,<br />
therefore conferring less viscosity, but they make<br />
the restoration difficult to finish and polish and<br />
also favour the formation of micro fractures.<br />
Fillers obtained by precipitation of pyrogenic silica<br />
at high temperatures, introduced successively,<br />
18<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Composites<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
consist of spherical particles of microfiller<br />
(between 0.04 and 0.06 µm). One of the most<br />
innovative products in this family of materials is<br />
the micro filler composite with prepolymerised<br />
spherical particles. The micro fillers in general are<br />
able to provide a significant advance in the qualities<br />
of the composite; in addition, this particular type<br />
of micro filler confers further advantages due to<br />
the spherical shape of the filler:<br />
• Better matrix-filler bond;<br />
• Less internal matrix-filler tension as there are<br />
prepolymerised spheres loaded with evenly<br />
distributed SiO 2 ;<br />
• Consequent improvement in wear and fatigue<br />
characteristics.<br />
However, this class of materials does not represent<br />
the solution to all the conditions required by a<br />
dental restoration, as even they are affected by<br />
technical gaps: the micro fillers are not capable of<br />
supporting high occlusal loads, especially because<br />
of the lower resistance of the pyrogenic silica when<br />
compared with fillers based on glass and above all<br />
quartz. Moreover, contraction due to polymerisation<br />
represents one of the major weak points of the<br />
micro fillers; this can compromise the tooth-obturation<br />
interface, the most critical zone of a restorative<br />
treatment (4,5).<br />
The experience obtained with traditional macro<br />
composites (TC) and micro fillers, both homogeneous<br />
and non-homogeneous (HMC e IMC), has<br />
provided the producers with the knowledge base<br />
needed for achieving a material that can now be<br />
used in all classes of dental cavities, as it has both<br />
the physical characteristics of the former and the<br />
19<br />
aesthetic characteristics of the latter: the hybrid<br />
composites. Hybrid composites are highly loaded<br />
materials (over 70% in volume).<br />
The technology of the hybrids is based on the<br />
presence of a double dispersed phase, consisting<br />
of ceramic-vitreous macro particles similar to the<br />
macro fillers, though of more limited dimensions<br />
(for the most part between 10 and 50 µm), as well<br />
as micro particles consisting of pyrogenic silica,<br />
which are typical of the micro fillers (approximate<br />
dimensions 0.04-0.06 µm) (6). The mixed filler<br />
provides a clear improvement in the material on<br />
both fronts: the physical characteristics and the<br />
aesthetic benefit. The macro particles are responsible<br />
for the increased mechanical resistance of the<br />
material because they have a higher elasticity<br />
modulus compared to that of the matrix with which<br />
they form a single body; in this way, an applied force<br />
should induce flexion of the particles before it can<br />
act on the resin, which is the real weak point during<br />
the application of loads; furthermore, the high<br />
filling value reduces the percentage of resin<br />
employed, in consequence reducing the contraction<br />
on polymerisation for which this is responsible. The<br />
improved aesthetic benefit, on the other hand, is a<br />
function of the presence of the micro filler, which<br />
guarantees greater surface polishing and an<br />
extremely wide range of shades (7, 8).<br />
The third component of composite is a silane<br />
binding agent, a bifunctional molecule capable of<br />
binding two different materials. Silane is an organic<br />
silicon glue which has two functional groups, one<br />
of which binds to the methacrylate groups of the<br />
resin, the other to the silicon dioxide of the filler.<br />
Hardening of the composite resins is linked to a<br />
process of polymerisation in which the monomers<br />
form macromolecular complexes known as polymers.<br />
In addition, there is a primer in the resin, a<br />
molecule that, when activated, provides the free<br />
radicals necessary for polymerisation to progress;<br />
the most commonly used primers employ visible<br />
light or UV rays to become activated in turn (9).<br />
Those belonging to the second group, now fallen<br />
into disuse, are basically represented by benzoinodimethyl<br />
ether, whereas a diketone is the most<br />
widely used molecule in the most common and<br />
recent composites: camphoroquinone together<br />
with NN-dimethylaminoethylmethacrylate.<br />
Activation of the latter primer is by a lamp using<br />
visible light with a wavelength between 430 and<br />
480 nm. These molecules initiate polymerisation<br />
by forming a three-dimensional network with<br />
many cross-links; while the reticulation process<br />
is proceeding, the levels of free radicals and the<br />
dimethacrylate molecules not involved in the<br />
process tend to drop drastically, preventing<br />
complete conversion of the double bonds of<br />
the dimethacrylate.<br />
When the composite hardens, the degree of<br />
conversion (DC), which is the percentage of<br />
monomers that undergo polymerisation, hardly<br />
exceeds 75% under standard conditions. The<br />
degree of conversion is a determinant for a<br />
series of physical properties of the composite,<br />
such as hardness and resistance to wear.
When two monomers combine the molecular<br />
structure is shortened, and it can be concluded<br />
that the greater degree of conversion will increase<br />
the percentage of contraction, because the overall<br />
length of a polymer is less than that of the individual<br />
monomers. In fact, the monomers combine with<br />
covalent bonds, assuming a distance between one<br />
another that is three times lower than that of the<br />
Van der Waals bonds that exist between one<br />
monomer and another. For this reason, a composite<br />
will contract more when used in a single mass than<br />
with minimal successive increments.<br />
The direction of contraction depends on the shape<br />
of the cavity and the strength of adhesion. In fact,<br />
adhesive placed on the walls of the cavity opposes<br />
the contraction of the composite, so that the<br />
surface of the material that contracts in contact<br />
with a wall of the cavity cannot contract because<br />
of the prevailing effect of the adhesive. Therefore,<br />
if the composite is in contact with one wall only,<br />
the contraction takes place towards it and involves<br />
all the other free surfaces. If there are two walls,<br />
the remaining unsupported surface will be left free<br />
to contract; if all the walls of a cavity are present,<br />
the composite adheres to them and the only wall<br />
free to contract is the occlusal one. Therefore, the<br />
greater the number of walls to which the composite<br />
adheres, the greater is the C-factor, that is, the<br />
relationship between the adhesive surface and<br />
the free surface and thus the greater is the stress<br />
to which the material will be subjected when<br />
contracting, as Feilzer stated in 1987. The stress<br />
within the tooth-composite interface has been<br />
measured at about 4 MPa for each surface.<br />
During polymerisation, there are two phases, one<br />
called the pre-gel phase in which contraction of<br />
the composite is compensated by the intrinsic<br />
flowing of the material, so as to diminish the<br />
contraction and reduce stress; the second is called<br />
the post-gel phase, separated from the former by a<br />
gel point, in which the material is no longer able to<br />
run to compensate the contraction so that stress<br />
is produced. A rigid composite will have a higher<br />
modulus of elasticity or Young’s modulus, and<br />
will develop more stress during polymerisation,<br />
having a shorter pre-gel phase; conversely, a<br />
fluid composite will have a lower modulus of<br />
elasticity with a longer pre-gel phase.<br />
Although the composites are regarded as optimal<br />
materials, they certainly have certain limits that<br />
may potentially frustrate the aims of a restoration.<br />
The main deficiency, and this applies for all classes<br />
of composite including the hybrids, is contraction<br />
on polymerisation, that is, the reduction in volume<br />
that the resin undergoes during the polyaddition<br />
phase, once the reaction has begun. It can be<br />
concluded that at the end of the restoration a<br />
marginal fissure will form between the tooth and<br />
obturation caused by the contraction; on the other<br />
hand, absence of the formation of a fissure introduces<br />
tensile forces into the reconstituted element<br />
that will be discharge either on the residual tooth<br />
walls, with the risk of fracturing them, or on the<br />
body of the obturation; the result will be the same<br />
for the three analysed outcomes that should be<br />
considered, however unlikely they may be: failure<br />
of the restoration. To avoid this, cases that may<br />
undergo direct restorative treatment with composite<br />
resins should be assessed carefully, following the<br />
instructions for use and observing the limitations<br />
that are still present, albeit reduced, especially in<br />
the case of the hybrids.<br />
Even if the evolution of the composites has probably<br />
approached its technological limit, there is certainly<br />
scope for improvement and it is permissible to<br />
expect that in the near future there will yet be a<br />
composite resin, even self-adhesive, that will be<br />
the material of choice in aesthetic reconstructions.<br />
It may also be considered that the hybrids come<br />
closest to the ideal material from the aesthetic<br />
aspect, although, like all composites, they are<br />
affected by technical problems that have not yet<br />
been fully resolved.<br />
References<br />
1. Ceruti A, Mangani F, Putignano A. Odontoiatria estetica adesiva – Didattica<br />
Multimediale. Ed. Quintessence. 2008 Cap.1; p:18-20.<br />
2. Christensen GJ. Longevity versus Esthetics. The Great <strong>Restorative</strong> Debate.<br />
JADA 2007, 138, 1013-1015.<br />
3. Raj V, Macedo GV, Ritter AV. Longevity of Posterior Composite Restorations.<br />
Journal Compilation 2007, 19(1), 3-5.<br />
4. Abe Y, Lambrechts P, Inoue S, et al. Dynamic elastic modulus of “packable”<br />
composites. Dent Mater 2001;17:520-5.<br />
5. Burgess JO, Walker R, Davidson JM. Posterior resin-based composite:<br />
review of the literature. Pediatr Dent 2002;24:465-79. Review.<br />
6. Dino R, Cerutti A, Mangani F, Putignano A. Restauri estetico-adesivi indiretti<br />
parziali nei settori posteriori. Ed.U.T.E.T. 2007 Cap. 2; p: 18-22.<br />
7. Christensen GJ. Preventing postoperative tooth sensitivity in class I, II and<br />
V restorations. J Am Dent Assoc 2002;133:229-31.<br />
8. Fabianelli A, Goracci C, Ferrari M. Sealing ability of packable resin<br />
composites in class II restorations. J Adhes Dent 2003 Fall; 5:217-23<br />
9. Lee IB, Son HH, Um CM. Rheologic properties of flowable, conventional<br />
hybrid, and condensable composite resins. Dent Mater 2003;19:298-307.<br />
20<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Composites<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Herculite ® XRV Ultra <br />
The legacy of Herculite<br />
For 25 years Herculite XRV has been the<br />
industry standard for composite restoratives.<br />
Herculite XRV Ultra is a nanohybrid version of<br />
Herculite XRV (microhybrid), that incorporates<br />
more biomimetic, “tooth-like” features into a<br />
restoration. Based on the latest nanofiller<br />
technology, in addition to offering improved<br />
handling, polishability and wear resistance,<br />
Herculite XRV Ultra delivers an improved lifelike<br />
appearance to final restorations by replicating<br />
the opalescence and fluorescence of the natural<br />
tooth.<br />
Herculite restoration after 13 years<br />
Case courtesy of A. A. Boghosian, J. L. Drummond and<br />
E.P. Lautenschlager – Study conducted by Northwestern University<br />
The Advantages of Nanotechnology<br />
Herculite Ultra’s advanced nanotechnology<br />
delivers additional benefits that can’t be<br />
found in traditional microhybrid composites.<br />
As a nanohybrid composite, Herculite XRV<br />
Ultra combines conventional hybrid fillers with<br />
smaller filler particles in size of about 50 nm.<br />
These smaller particles enable Herculite XRV<br />
Ultra to deliver improved polish and clinical<br />
gloss, better aesthetics and superior<br />
mechanical strength.<br />
Compared to Other Composites<br />
Plucking, or natural wear over time, tends to<br />
occur faster in restorations with larger particles,<br />
decreasing the overall life and esthetics of<br />
the restoration. When polymerized, the large<br />
prepolymerized particles virtually disappear<br />
and the surface is easily polishable. The<br />
polished surface consists only of nanohybrid<br />
particles below the wavelength of visible light.<br />
Nanohybrid composite<br />
21
Improved Handling<br />
Handling Comparison Map<br />
Creamy<br />
TPH3<br />
Z100<br />
Venus<br />
Gradia Direct<br />
Filtek Supreme Plus<br />
Map was created with input from<br />
various clinicians and <strong>Kerr</strong> R&D.<br />
Grandio<br />
Point 4<br />
Sticky<br />
Non-Sticky<br />
Herculite Ultra<br />
Esthet X<br />
Herculite XRV <br />
Premise <br />
Here’s what clinicians are saying about<br />
Herculite Ultra<br />
Filtek Z250<br />
90% of focus group attendees said they would purchase Herculite<br />
Ultra over their current composite.<br />
“Adapts really well, not sticky at all, really sculptable”.<br />
“Superb for a nanohybrid. Best composite ever”.<br />
Best<br />
5<br />
4<br />
3<br />
4,85<br />
4,54 4,69 4,77 4,77 4,69<br />
Stiff<br />
4,92<br />
Clinical Research<br />
Gloss Retention<br />
Over time, resin in a composite restoration wears off,<br />
exposing glass fillers and creating a rough surface.<br />
If the filler size is smaller than the average wavelength of light<br />
(as in the case of Herculite Ultra, Premise, and Point 4),<br />
light will be diffused uniformly and the surface will appear<br />
glossy, resulting in superior gloss retention over time despite<br />
resin wear.<br />
Toothbrush test, University of Leeds<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Before<br />
73<br />
Herculite ® Ultra<br />
<strong>Kerr</strong><br />
69.1<br />
Venus ®<br />
Heraeus Kulzer<br />
65.2<br />
Tetric EvoCeram ®<br />
Ivoclar<br />
62.3<br />
Miris <br />
Coltene Whaledent<br />
51.1<br />
Filtek Z250<br />
3M<br />
Gloss meter readings were taken using a gloss meter at 600 minutes<br />
after the initial reading.<br />
Herculite<br />
Ultra<br />
Venus<br />
Tetric<br />
Evoceram<br />
2<br />
1<br />
After<br />
Worst<br />
0<br />
Handling Stickiness/ Thickness Adaptability Compression Adherence Resistance<br />
Tackiness w/ Instrument to Instrument to Slumping<br />
Photographs courtesy of University of Leeds<br />
22<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Composites<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Herculite XRV Ultra in Clinical Cases<br />
Class IV<br />
Case courtesy of Prof. Angelo Putignano.<br />
1) Initial case. 2) Teeth prints taken for diagnostic wax-up. 3) Mask based on diagnostic wax-up.<br />
4) Mask test. 5) The case with applied OptiDam. 6) Mask test with OptiDam.<br />
23
7) Etching for 15 seconds with<br />
Gel Etchant.<br />
8) Palatinal wall A2 Enamel mass, small<br />
amount of A3 dentin on the most<br />
coronal part of the injury was placed.<br />
9) A2 dentin mass was applied to cover<br />
the former layer and sculpted with<br />
grooves.<br />
10) The incisal mass is used both around and<br />
between the grooves to create a translucent<br />
effect and to highlight the grooves.<br />
11) The most coronal part is then slightly<br />
pigmented with orange, while whitish<br />
areas are designed with Kolor + Plus ® White.<br />
12) Vestibular A2 enamel mass applied<br />
in a very fine layer.<br />
13) The case after fininishing and<br />
polishing.<br />
14) The completed case after the<br />
10-day follow-up.<br />
24<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Composites<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Class V<br />
Case courtesy of Prof. Angelo Putignano.<br />
The present case concerns a 30 year old patient with multiple erosions<br />
from particular alimentary habits and inadequate oral hygiene:<br />
1) Initial situation, erosions on 1.1<br />
and 2.1.<br />
2) Rubber Dum isolation. 3) Gentle roughening of sclerotic dentin<br />
with rounded carbide bur.<br />
4) Finishing line with 20 micron<br />
diamond bur.<br />
5) Etching with 37% phosphoric acid. 6) OptiBond Solo Plus adhesive applied<br />
with scrubbing motion for 15 seconds;<br />
light cured for 10 sec with Demi.<br />
25
7) Application of a thin layer of Premise<br />
Flow A3.5; light cure for 20 sec with<br />
Demi.<br />
8) First layer of Herculite XRV Ultra,<br />
A3 Enamel, on cervical part;<br />
light cure for 20 sec.<br />
9) Second and last layer of<br />
Herculite XRV Ultra, A3 Enamel;<br />
light cure for 20 sec.<br />
10) Finishing with OptiDisc<br />
Coarse/Medium, small size.<br />
11) Polishing with GlossPlus Polisher<br />
Minipoint.<br />
12) High gloss polishing with HiLuster Dia<br />
Polisher Minipoint.<br />
13) Final case after RubberDum removal.<br />
26<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Composites<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Class II<br />
Case courtesy of Prof. Angelo Putignano.<br />
1) Initial case. 2) Preliminary preparation.<br />
3) Cavity smoothing with Pasteless<br />
prophy without fluoride.<br />
4) Cavity preparation after caries removal<br />
revealing sclerotic dentin.<br />
5) Etching with Gel Etchant 15 sec.<br />
6) Bonding with OptiBond Solo Plus.<br />
Apply for 15 seconds and light cure<br />
for 10 seconds.<br />
7) A thin layer of Premise Flow. 8) Build-up of interproximal wall.<br />
27
9) First layer of Herculite XRV Ultra,<br />
Dentin A3,5, light cured for 20<br />
seconds.<br />
10) Vestibular dentin masses A3,<br />
light cured for 10 seconds.<br />
11) Lingual dentin masses A3,<br />
light cured for 10 seconds.<br />
12) A thin layer of Enamel A3 under<br />
glycerin to avoid air inhibition.<br />
13) Interproximal emergency profile<br />
of restoration.<br />
14) Finishing procedure with multi-blade<br />
bur.<br />
15) Occlusal check.<br />
16) Polishing with OptiShine.<br />
17) Final result.<br />
28<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Composites<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Class I<br />
Case courtesy of Prof. Angelo Putignano.<br />
1) Initial case. 2) Prepared cavity. 3) Etching with Gel Etchant<br />
15 seconds.<br />
4) Bonding with OptiBond Solo Plus,<br />
apply for 15 seconds and light cure<br />
for 10 seconds.<br />
5) Dentin layer A3, light cured for<br />
20 seconds.<br />
6) Final result.<br />
29
30<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Finishing and Polishing<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Finishing and Polishing<br />
Finishing and polishing of composite restorations<br />
Prof. Martin Jung, Justus-Liebig-University, Giessen, Germany<br />
Aesthetic superiority is one of the key features of<br />
dental composite restorations. Shading, optical<br />
appearance and surface texture of a tooth<br />
coloured restoration is crucial not only with<br />
respect to patient’s satisfaction and comfort<br />
[Jones et al., 2004]. The behaviour of composites<br />
in the biological environment of the oral cavity<br />
and composite material properties are strongly<br />
influenced by surface quality. Surface irregularities<br />
enhance plaque accumulation [Ikeda et al., 2007],<br />
which in turn can lead to secondary caries and<br />
inflammation of the adjacent gingival tissues.<br />
Especially in case of restorations that are exposed<br />
to strong occlusal load and antagonistic activity,<br />
surface roughness affects the wear resistance and<br />
the abrasivity of dental composites [Willems et al.,<br />
1991; Mandikos et al., 2001]. Rough composite<br />
surfaces are liable to discoloration and staining<br />
[Patel et al., 2004; Lu et al., 2005]. Moreover,<br />
material properties such as mechanical and<br />
flexural strength as well as microhardness of resin<br />
based composites are improved by minimizing<br />
surface roughness [Gordan et al., 2003; Venturini<br />
et al., 2006; Lohbauer et al., 2008]. Thus accomplishing<br />
a superior surface finish is a prerequisite<br />
for patient’s satisfaction and for the longevity of a<br />
composite restoration.<br />
Composite surfaces, which are cured against a<br />
mylar matrix, show minimum surface roughness<br />
[Yap et al., 1997; Ergücü and Türkün, 2007; Üctasli<br />
et al., 2007; Korkmaz et al., 2008] Clinically, most<br />
composite restorations require further finishing and<br />
polishing after placement. Finishing includes elimination<br />
of excessive material, adjustment of surface<br />
morphology and removal of occlusal interferences.<br />
Case courtesy of Prof. Angelo Putignano<br />
This causes a roughening of surfaces, which must<br />
be eliminated by subsequent polishing. Rotary<br />
instruments which are used for these purposes<br />
face a lot of requirements. They must be equally<br />
effective when exposed to hard filler particles and<br />
soft resin matrix, without having detrimental<br />
effects on the composite surface. Instruments for<br />
finishing require cutting efficiency to some degree<br />
without leaving the surfaces in a rough state.<br />
Finally, rotary instruments for finishing and polishing<br />
must work on different types of surface morphology<br />
(even and convex vs. structured and concave<br />
surfaces).<br />
With respect to initial finishing of composite<br />
restorations, there are mainly two types of burs<br />
which are recommended for this purpose: finishing<br />
diamonds and tungsten carbide finishing instruments.<br />
Finishing diamonds are characterized by a<br />
comparatively high cutting efficiency, depending<br />
on the size of the abrasive diamond particles<br />
[Jung, 1997]. Due to the aggressive effect of the<br />
diamond particles, finishing diamonds leave<br />
composite surfaces in a more or less rough state<br />
[Jung et al., 2007b].<br />
31
Tungsten carbide finishing burs vary with respect<br />
to the number and orientation of the cutting flutes.<br />
These instruments are characterized by a limited<br />
cutting efficiency and achieve a smooth composite<br />
surface with only little remaining roughness [Jung,<br />
1997; Barbosa et al., 2005; Turssi et al., 2005].<br />
There is some controversy in literature, whether<br />
there are significant differences between different<br />
types of tungsten carbide finishing burs with<br />
respect to the resultant surface quality [Jung,<br />
1997; Radlanski and Best, 2007].<br />
After pre-treatment, the composite surfaces are in<br />
a variably rough state, depending on the extent<br />
and amount of corrective work and on the number<br />
and type of burs used. In order to accomplish a<br />
superior aesthetic result, maximum reduction of<br />
remaining roughness is necessary by subsequent<br />
polishing.<br />
There is a great number of polishing techniques<br />
available for application on composite restorations.<br />
Polishing systems vary with respect to shape and<br />
size of the individual instruments, number of working<br />
steps, matrix and abrasive particle composition as<br />
well as consistency.<br />
Flexible discs generally yield well smoothened<br />
composite surfaces and permit an effective<br />
reduction of remaining roughness. For this<br />
reason, flexible discs were regarded as some<br />
kind of clinical polishing standard for composite<br />
surfaces [Tjan and Clayton, 1989; Wilson et al.,<br />
1990; Hoelscher et al., 1998; Setcos et al., 1999;<br />
Roeder et al., 2000; Üctasli et al., 2007]. Because<br />
of their shape, flexible discs are efficient on even<br />
or convex surfaces; they are not recommended for<br />
application on concave or structured surfaces<br />
[Chen et al., 1988; Tjan and Clayton, 1989]. By<br />
variation of disc diameter and thickness, their<br />
application can be adapted to several clinical situations.<br />
Most disc systems are available in three or<br />
even four working steps, thus permitting a high<br />
cutting efficiency and effective roughness reduction.<br />
For this reason, flexible discs represent the<br />
only technique which can be used both for finishing<br />
and polishing.<br />
Case courtesy of Dr. Joseph Sabbagh<br />
Rubber polishers comprise a great and heterogeneous<br />
group of polishing devices. Variations in size<br />
and shape enable the application of rubber<br />
polishers both on convex and on structured or<br />
concave composite restoration surfaces. Most of<br />
the products out of this group are characterized<br />
by a rubber-like silicon matrix. The abrasive<br />
particles which are integrated into the matrix<br />
are mostly made of silicon carbide or dioxide,<br />
aluminium oxide or diamond particles in different<br />
grain sizes. The clinical application mode for the<br />
various products differs considerably. It reaches<br />
from a single-step application to two, three or four<br />
working steps. Owing to these great variations,<br />
the polishing efficiency depends strongly on the<br />
individual products used. Many systems achieved<br />
a good composite surface quality, comparable or<br />
even better than flexible discs [Jung et al., 2003;<br />
Jung et al., 2007a]. Other products caused less<br />
favourable polishing results [Ergücü and Türkün,<br />
2007; Cenci et al., 2008]. The efficiency of onestep<br />
vs. multi-step systems is still discussed in<br />
literature [Da Costa et al., 2007; Jung et al., 2007a].<br />
Polishing brushes represent a different approach<br />
towards minimizing composite roughness. Silicon<br />
carbide abrasive particles are integrated into the<br />
matrix of special synthetic filaments. This enables<br />
a universal application of polishing brushes on<br />
different types of composite surface morphology.<br />
Polishing brushes are one-step systems; their<br />
polishing efficiency is favourable, but depends<br />
on the quality of initial finishing [Krejci et al., 1999;<br />
Jung et al., 2007a].<br />
32<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Finishing and Polishing<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Felt wheels are another one-step polishing system,<br />
with abrasive diamond particles attached to a felt<br />
matrix with the help of wax. Because of the soft<br />
matrix, felt wheels can be used on various types<br />
of composite surfaces. Due to its nature, felt<br />
wheels must be discarded after a single use. The<br />
polishing results depend strongly on the kind of<br />
pre-treatment [Jung et al., 1997; Jung et al., 2003;<br />
Scheibe et al., 2009].<br />
Finally, gels are an alternative for polishing composites.<br />
Their application in a single or few steps<br />
is possible on all types of surfaces. Polishing<br />
gels are used on discs, plastic tips or brushes.<br />
A diamond based polishing paste achieved<br />
favourable results on a hybrid composite<br />
[Jung, 2002]. Polishing pastes based on diamond<br />
particles achieved lower roughness compared to<br />
aluminium-oxide gels [Kaplan et al., 1996].<br />
The use of gels as a final polishing step is<br />
recommended [Turssi et al., 2000; Radlanski<br />
and Best, 2007].<br />
For rotary instruments there is only limited access<br />
to proximal surfaces. This special situation requires<br />
the use of manual finishing and polishing strips,<br />
although their polishing efficiency seems to be<br />
limited [Whitehead et al., 1990]. Alternatively<br />
diamond-coated oscillating finishing files may be<br />
used in cases with greater amounts of excess<br />
composite material in the proximal-cervical area<br />
of composite restorations. Oscillating diamond<br />
files caused rough areas after application to cervical<br />
margins of composite-inlays. A subsequent use of<br />
polishing paste on plastic files achieved a reduction<br />
of remaining surface roughness [Small et al., 1992].<br />
The choice of an appropriate system for finishing<br />
and polishing of composite restorations depends<br />
on a several factors; there is no universal system<br />
for all clinical indications. The accessibility and<br />
morphology (convex or structured) of surfaces and<br />
the need and extent for initial finishing is of great<br />
importance. Finally the choice of a certain polishing<br />
system should be made with respect to texture<br />
and roughness of the surfaces after initial finishing.<br />
The success of one-step polishing systems generally<br />
strongly depends on the surface condition and<br />
its remaining roughness after finishing. Polishing<br />
systems with two or more working steps are less<br />
sensitive to the kind of pre-treatment.<br />
All references are available upon request.<br />
33
Surface treatment of composite filling<br />
Occlusal / Concave Surfaces<br />
Surface<br />
Roughness<br />
CONTOURING<br />
Adjust primary<br />
geometric form.<br />
Carbide Bur 12 Blades<br />
Diamond 40 µm<br />
Dia: sRa=1.25 µm<br />
FINISHING<br />
Remove composite excesses.<br />
Shape Occlusal anatomy,<br />
lingual fissures,<br />
secondary anatomy.<br />
Carbide Bur 30 Blades<br />
Diamond 20 µm<br />
Dia: sRa=0.56 µm<br />
POLISHING<br />
Eliminate surface scratches.<br />
Reduce surface<br />
roughness below<br />
Ra = 0.35 µm.<br />
Occlubrush and<br />
OptiShine is<br />
universal polishing<br />
tool for all occlusal<br />
and concave<br />
posterior surfaces<br />
Occlubrush<br />
OptiShine<br />
Gloss<br />
GlossP: sRa=0.26 µm<br />
HIGH GLOSS POLISHING<br />
Reduce surface roughness till to<br />
high gloss below<br />
Ra = 0.2 µm.<br />
HiLuster<br />
HiLust: sRa=0.10 µm<br />
34<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Finishing and Polishing<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
Convex / Flat Surfaces<br />
Surface<br />
Roughness<br />
CONTOURING<br />
Adjust primary<br />
geometric form.<br />
Carbide Bur 12 Blades<br />
Diamond 40 µm<br />
OptiDisc Extra-Coarse<br />
Disc: sRa=1.20 µm<br />
FINISHING<br />
Remove composite excesses.<br />
Shape Occlusal anatomy,<br />
lingual fissures,<br />
secondary anatomy.<br />
Carbide Bur 30 Blades<br />
Diamond 20 µm<br />
OptiDisc Coarse-Medium<br />
Disc: sRa=0.63 µm<br />
POLISHING<br />
Eliminate surface scratches.<br />
Reduce surface<br />
roughness below<br />
Ra = 0.35 µm.<br />
OptiDisc Fine<br />
OptiShine<br />
Gloss Polisher<br />
Disc: sRa=0.33 µm<br />
HIGH GLOSS POLISHING<br />
Reduce surface roughness till to<br />
high gloss below<br />
Ra = 0.2 µm.<br />
OptiDisc Extra-Fine<br />
HiLuster Polisher<br />
Disc: sRa=0.12 µm<br />
35
Interproximal Surfaces<br />
Surface<br />
Roughness<br />
CONTOURING<br />
Adjust primary<br />
geometric form.<br />
Diamond strip not<br />
recommended for<br />
anterior application<br />
Diamond 40 µm<br />
Diamond Strip<br />
Strip: sRa=0.90 µm<br />
FINISHING<br />
Remove composite excesses.<br />
Shape Occlusal anatomy,<br />
lingual fissures,<br />
secondary anatomy.<br />
Diamond 20 µm<br />
Finishing OptiStrip<br />
Strip: sRa=0.58 µm<br />
POLISHING<br />
Eliminate surface scratches.<br />
Reduce surface<br />
roughness below<br />
Ra = 0.35 µm.<br />
OptiDisc can<br />
also be used<br />
interproximally<br />
Polishing OptiStrip<br />
OptiShine<br />
OptiDisc<br />
OShine: sRa=0.25 µm<br />
HIGH GLOSS POLISHING<br />
Reduce surface roughness till to<br />
high gloss below<br />
Ra = 0.2 µm.<br />
HiLuster<br />
HiLust: sRa=0.10 µm<br />
36<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Finishing and Polishing<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
OptiDisc ®<br />
OptiDisc<br />
Sof-Lex XT<br />
The first translucent finishing and polishing disc, which is both gentle and more efficient. The flexible discs<br />
are used for finishing and polishing of composites, glassionomers, amalgams, semiprecious and precious<br />
metals. The use of the complete system gives the restoration a final polish equal to the natural dentition.<br />
Features<br />
• Unique fixation between disc and mandrel. Optimal torque transmission to disc,<br />
no sliding and no rpm sensitive.<br />
• Optimized disc flexibility. For excellent adaptation on tooth anatomy.<br />
• Translucent discs. Good view of the working area.<br />
• Colour coded stages of abrasivity. Easy recognition of grit size.<br />
• Green coding of abrasive side. Easy distinction between abrasive and non-abrasive side.<br />
• Ready to use abrasive layer. High efficiency. Uncoated cutting edges for high efficiency from the start.<br />
15.9mm 12.6mm 9.6mm<br />
Extra-Coarse<br />
80 µm<br />
Coarse/Medium<br />
40 µm<br />
Green active side<br />
Disc: sRa=1.20 µm<br />
Disc: sRa=0.63 µm<br />
The Mandrel<br />
• Metal mandrel<br />
• Patented mandrel design. Mandrel is placed<br />
below the surface of the disc to avoid<br />
contact with the tooth.<br />
• Special coating of the mandrel. Protection<br />
against scarring.<br />
Fine<br />
20 µm<br />
Disc: sRa=0.33 µm<br />
Extra-Fine<br />
10 µm<br />
Disc: sRa=0.12 µm<br />
37
Abrasive coating<br />
OptiDisc <strong>Kerr</strong><br />
200 µm<br />
< ><br />
Extra-Coarse<br />
Coarse-Medium<br />
Fine<br />
Extra-Fine<br />
200 µm<br />
< ><br />
OptiDisc can be turned<br />
on the mandrel in order<br />
to have an easy access<br />
of active side on mesial<br />
and distal surface of<br />
the tooth.<br />
Coarse Medium Fine<br />
Sof-Lex XT 3M Espe<br />
Super Fine<br />
SEM pictures show comparison of abrasive<br />
coating of 2 competitive materials.<br />
SEM pictures courtesy of Dr. Jean-Pierre Salomon, France<br />
0.0160<br />
0.0140<br />
Mass removal after each application<br />
of 20 sec. on Point4<br />
3M Soft-Lex<br />
OptiDisc<br />
Abrasive<br />
Glue<br />
Polyester<br />
OptiDisc<br />
Sof-Lex XT 3M Espe<br />
OptiDisc has a ready to use abrasive layer - uncoated cutting edges for<br />
high efficiency from the start.<br />
Glue<br />
Abrasive<br />
Foil<br />
Mass removal (g)<br />
0.0120<br />
0.0100<br />
0.0080<br />
0.0060<br />
0.0040<br />
0.0020<br />
0.0000<br />
3M Coarse 3M Medium Fine Super Fine<br />
<strong>Hawe</strong> Extra coarse <strong>Hawe</strong> Medium/Coarse<br />
38<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Finishing and Polishing<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
HiLuster Plus Polishing system<br />
2-step polishing system for composites<br />
Features<br />
• High-gloss results in only 2 steps. Smooth surface and high gloss in two steps.<br />
• Efficient. Pre- and gloss polishing in one single step by efficient Gloss PLUS polishers,<br />
final roughness after first step around sRa 0.25 µm.<br />
• Diamond particles. Outstanding final result thanks to diamond particles integrated in the HiLuster PLUS<br />
polisher, final roughness around sRa 0.10 µm is achieved after second step.<br />
• Optimum flexibility. The flexibility of the polishers was optimized for excellent adaptation to the tooth<br />
anatomy.<br />
• Good adhesion between the mandrel and the polisher. Avoids that the abrasive parts come off.<br />
• Hygienic. Possibility to sterilize before first use in order to preserve the hygienic – can be autoclaved<br />
at 134 °C.<br />
Material of Polisher:<br />
Gloss PLUS Polishers<br />
Flame<br />
Part. No. 2651<br />
Minipoint<br />
Part. No. 2652<br />
Cup<br />
Part. No. 2653<br />
Cup<br />
Part. No. 2654<br />
GlossP: sRa=0.26 µm<br />
Gloss Plus Polisher:<br />
HiLuster Plus Dia Polisher:<br />
Aluminium oxide particles embedded into a silicone elastomer.<br />
(mean particle size: 20 microns)<br />
Silicone carbide and diamond particles (5 microns)<br />
embedded into a silicon elastomer.<br />
HiLuster PLUS Dia Polishers<br />
Flame<br />
Part. No. 2651<br />
Minipoint<br />
Part. No. 2652<br />
Material of Mandrel:<br />
Golden coated mandrel<br />
Cup<br />
Part. No. 2653<br />
Cup<br />
Part. No. 2654<br />
HiLust: sRa=0.10 µm<br />
39
Usage on different surfaces<br />
Comparison HiLuster Polishing System and Enhance+PoGo<br />
polishing system used on Herculite XRV Ultra<br />
Gloss Plus Polisher<br />
1: Reference surface<br />
OptiDisc coarse/medium<br />
OptiDisc sRa: 0.56 µm<br />
2: Polishing Enhance + PoGo HiLuster PLUS Polishing<br />
system<br />
Flame Minipoint Minipoint Cup<br />
Enhance sRa: 0.6 µm<br />
Gloss PLUS sRa: 0.27 µm<br />
HiLuster Plus Dia Polisher<br />
2: High Gloss PoGo HiLuster PLUS<br />
Polishing<br />
Polishing system<br />
Enhance sRa: 0.32 µm<br />
HiLuster PLUS Dia sRa: 0.14 µm<br />
Enhance is a very aggressive polisher, leaving high surface<br />
roughness. PoGo polisher has the ability to smooth the<br />
surface after Enhance but the final surface roughness<br />
sRa = 0.32 µm is not considered as high gloss surface.<br />
A much smoother and high gloss surface of sRa = 0.14 µm<br />
is achieved with 2-step HiLuster Polishing system.<br />
Flame Minipoint Minipoint Cup<br />
40<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Finishing and Polishing<br />
<strong>Restorative</strong> <strong>Procedure</strong><br />
OptiShine<br />
The first concave-shaped polishing brush<br />
Features<br />
• Efficient in practice. The concave shape of the brush is efficient on all tooth surfaces,<br />
also on less accessible surfaces like interproximal and occlusal fissures.<br />
• Universal use. Always produces excellent polishing results for all restorations due<br />
to the concave shape of the brush.<br />
Reduce the surface roughness without changing the anatomical shape and the micro surface texture.<br />
• Excellent polish. The polishing effect is created by polishing particles embedded in the bristles<br />
(silicone carbide), therefore no paste is necessary.<br />
• Durable for multiple use. Autoclavable at 134 °C, at least 3 min.<br />
No effect on the polishing performance.<br />
Good accessibility<br />
due to concave shape<br />
of OptiShine.<br />
Each bristle<br />
is a polishing<br />
instrument.<br />
Specialfibres with<br />
in-built silicon-carbide<br />
abrasive particles.<br />
OShine: sRa=0.25 µm<br />
Not liable to confusion.<br />
Easily recognisable<br />
by the golden shaft.<br />
Good accesses to the fissures and occlusal surfaces.<br />
41
Herculite XRV References<br />
1. Effect of delivering light in specific narrow bandwidths from 394 to 515nm on the micro-hardness of resin<br />
composites. Price RB, Felix CA. Dent Mater. 2009 Feb 23.<br />
2. Shear strength evaluation of composite-composite resin associations. Ribeiro JC, Gomes PN, Moysés MR,<br />
Dias SC, Pereira LJ, Ribeiro JG. J Dent. 2008 May;36(5):326-30. Epub 2008 Mar 11.<br />
3. Polymerization stress of resin composites as a function of system compliance. Gonçalves F, Pfeifer CS,<br />
Meira JB, Ballester RY, Lima RG, Braga RR. Dent Mater. 2008 May;24(5):645-52. Epub 2007 Aug 24.<br />
4. Cytotoxicity of resin composites as a function of interface area. Franz A, König F, Skolka A, Sperr W, Bauer<br />
P, Lucas T, Watts DC, Schedle A. Dent Mater. 2007 Nov;23(11):1438-46. Epub 2007 Aug 3.<br />
5. The evaluation of direct composite restorations for the worn mandibular anterior dentition - clinical performance<br />
and patient satisfaction. Poyser NJ, Briggs PF, Chana HS, Kelleher MG, Porter RW, Patel MM. J Oral<br />
Rehabil. 2007 May;34(5):361-76.<br />
6. Surface texture of four nanofilled and one hybrid composite after finishing. Jung M, Sehr K, Klimek J. Oper<br />
Dent. 2007 Jan-Feb;32(1):45-52.<br />
7. Residual stress in composites with the thin-ring-slitting approach. Park JW, Ferracane JL. J Dent Res. 2006<br />
Oct;85(10):945-9.<br />
8. Effect of light-curing method on marginal adaptation, microleakage, and microhardness of composite<br />
restorations. Ritter AV, Cavalcante LM, Swift EJ Jr, Thompson JY, Pimenta LA. J Biomed Mater Res B Appl<br />
Biomater. 2006 Aug;78(2):302-11.<br />
9. The effects of thermocycling on the flexural strength and flexural modulus of modern resin-based filling<br />
materials. Janda R, Roulet JF, Latta M, Rüttermann S. Dent Mater. 2006 Dec;22(12):1103-8. Epub 2006 Jan<br />
10.<br />
10. A clinical evaluation of posterior composite restorations: 17-year findings. da Rosa Rodolpho PA, Cenci MS,<br />
Donassollo TA, Loguércio AD, Demarco FF. J Dent. 2006 Aug;34(7):427-35. Epub 2005 Nov 28.<br />
11. Polishing occlusal surfaces of direct Class II composite restorations in vivo. Jung M, Hornung K, Klimek J.<br />
Oper Dent. 2005 Mar-Apr;30(2):139-46.<br />
12. The survival and clinical performance of resin-based composite restorations used to treat localised anterior<br />
tooth wear. Redman CD, Hemmings KW, Good JA. Br Dent J. 2003 May 24;194(10):566-72; discussion 559.<br />
13. In vivo comparison of a microfilled and a hybrid minifilled composite resin in Class III restorations: 2-year<br />
follow-up. Reusens B, D'hoore W, Vreven J. Clin Oral Investig. 1999 Jun;3(2):62-9.<br />
14. Tooth wear treated with direct composite restorations at an increased vertical dimension: results at 30<br />
months. Hemmings KW, Darbar UR, Vaughan S. J Prosthet Dent. 2000 Mar;83(3):287-93.<br />
15. A 4-year retrospective clinical study of Class I and Class II composite restorations. Geurtsen W, Schoeler U.<br />
J Dent. 1997 May-Jul;25(3-4):229-32.<br />
16. Stratification of composite restorations: systematic and durable replication of natural aesthetics. Magne P,<br />
Holz J. Pract Periodontics Aesthet Dent. 1996 Jan-Feb;8(1):61-8; quiz 70.<br />
17. A clinical evaluation of posterior composite resin restorations. Bryant RW, Hodge KL. Aust Dent J. 1994<br />
Apr;39(2):77-81.<br />
18. Clinical evaluation of a highly wear resistant composite. Dickinson GL, Gerbo LR, Leinfelder KF. Am J Dent.<br />
1993 Apr;6(2):85-7.<br />
19. Two-year evaluation in vivo and in vitro of Class 2 composites. Fuks AB, Chosack A, Eidelman E. Oper<br />
Dent. 1990 Nov-Dec;15(6):219-23.<br />
20. Cuspal deformation and fracture resistance of teeth with dentin adhesives and composites. Sheth JJ, Fuller<br />
JL, Jensen ME. J Prosthet Dent. 1988 Nov;60(5):560-9.<br />
OptiBond FL References<br />
1. A randomized controlled clinical trial of a HEMA-free all-in-one adhesive in non-carious cervical<br />
lesions at 1 year. Van Landuyt KL, Peumans M, Fieuws S, De Munck J, Cardoso MV, Ermis RB, Lambrechts<br />
P, Van Meerbeek B. J Dent. 2008 Oct;36(10):847-55.<br />
2. In vitro cytotoxicity of different desensitizers under simulated pulpal flow conditions. Wiegand A, Buchholz<br />
K, Werner C, Attin T. J Adhes Dent. 2008 Jun;10(3):227-32.<br />
3. Bonding effectiveness and interfacial characterization of a HEMA/TEGDMA-free three-step etch&rinse<br />
adhesive. Mine A, De Munck J, Van Landuyt KL, Poitevin A, Kuboki T, Yoshida Y, Suzuki K, Lambrechts P,<br />
Van Meerbeek B. J Dent. 2008 Oct;36(10):767-73.<br />
4. Direct dentin bonding technique sensitivity when using air/suction drying steps. Magne P, Mahallati R,<br />
Bazos P, So WS. J Esthet Restor Dent. 2008;20(2):130-8<br />
5. Micropermeability of current self-etching and etch-and-rinse adhesives bonded to deep dentine: a comparison<br />
study using a double-staining/confocal microscopy technique. Sauro S, Pashley DH, Mannocci F, Tay<br />
FR, Pilecki P, Sherriff M, Watson TF. Eur J Oral Sci. 2008 Apr;116(2):184-93.<br />
6. Marginal integrity: is the clinical performance of bonded restorations predictable in vitro? Frankenberger R,<br />
Krämer N, Lohbauer U, Nikolaenko SA, Reich SM. J Adhes Dent. 2007;9 Suppl 1:107-16. Erratum in: J<br />
Adhes Dent. 2007 Dec;9(6):546.<br />
7. Bond strength of self-etch adhesives to dentin prepared with three different diamond burs. Ermis RB, De<br />
Munck J, Cardoso MV, Coutinho E, Van Landuyt KL, Poitevin A, Lambrechts P, Van Meerbeek B. Dent<br />
Mater. 2008 Jul;24(7):978-85.<br />
8. Bonding BisGMA to dentin--a proof of concept for hydrophobic dentin bonding. Tay FR, Pashley DH, Kapur<br />
RR, Carrilho MR, Hur YB, Garrett LV, Tay KC. J Dent Res. 2007 Nov;86(11):1034-9.<br />
9. Immediate dentin sealing supports delayed restoration placement. Magne P, So WS, Cascione D. J Prosthet<br />
Dent. 2007 Sep;98(3):166-74.<br />
10. Influence of dentin cavity surface finishing on micro-tensile bond strength of adhesives. Cardoso MV,<br />
Coutinho E, Ermis RB, Poitevin A, Van Landuyt K, De Munck J, Carvalho RC, Van Meerbeek B. Dent Mater.<br />
2008 Apr;24(4):492-501.<br />
11. Marginal integrity of class V restorations: SEM versus dye penetration. Ernst CP, Galler P, Willershausen B,<br />
Haller B. Dent Mater. 2008 Mar;24(3):319-27.<br />
12. Bonding to ground versus unground enamel in fluorosed teeth. Ermis RB, De Munck J, Cardoso MV,<br />
Coutinho E, Van Landuyt KL, Poitevin A, Lambrechts P, Van Meerbeek B. Dent Mater. 2007<br />
Oct;23(10):1250-5.<br />
13. Polymerization kinetics of dental adhesives cured with LED: correlation between extent of conversion and<br />
permeability. Breschi L, Cadenaro M, Antoniolli F, Sauro S, Biasotto M, Prati C, Tay FR, Di Lenarda R. Dent<br />
Mater. 2007 Sep;23(9):1066-72.<br />
14. Restoring cervical lesions with flexible composites. Peumans M, De Munck J, Van Landuyt KL, Kanumilli P,<br />
Yoshida Y, Inoue S, Lambrechts P, Van Meerbeek B. Dent Mater. 2007 Jun;23(6):749-54.<br />
15. Effect of water storage on the bonding effectiveness of 6 adhesives to Class I cavity dentin. De Munck J,<br />
Shirai K, Yoshida Y, Inoue S, Van Landuyt K, Lambrechts P, Suzuki K, Shintani H, Van Meerbeek B. Oper<br />
Dent. 2006 Jul-Aug;31(4):456-65.<br />
16. Immediate dentin sealing of onlay preparations: thickness of pre-cured Dentin Bonding Agent and effect of<br />
surface cleaning. Stavridakis MM, Krejci I, Magne P. Oper Dent. 2005 Nov-Dec;30(6):747-57.<br />
17. Degree of conversion and permeability of dental adhesives. Cadenaro M, Antoniolli F, Sauro S, Tay FR, Di<br />
Lenarda R, Prati C, Biasotto M, Contardo L, Breschi L. Eur J Oral Sci. 2005 Dec;113(6):525-30.<br />
18. Self-etch vs etch-and-rinse adhesives: effect of thermo-mechanical fatigue loading on marginal quality of<br />
bonded resin composite restorations. Frankenberger R, Tay FR. Dent Mater. 2005 May;21(5):397-412.<br />
19. Influence of c-factor and layering technique on microtensile bond strength to dentin. Nikolaenko SA,<br />
Lohbauer U, Roggendorf M, Petschelt A, Dasch W, Frankenberger R. Dent Mater. 2004 Jul;20(6):579-85.<br />
42<br />
Your practice is our inspiration.
All you need is <strong>Kerr</strong><br />
Authors Biographies<br />
in alphabetic order<br />
Prof. Martin Jung, DDS<br />
Policlinic for Conservative and Preventive Dentistry<br />
Faculty of Dentistry, Justus-Liebig University, Giessen, Germany<br />
martin.jung@dentist.med.uni-giessen.de<br />
Study of Dentistry at the Justus-Liebig-University, Giessen, Germany, 1979-1984.<br />
Approbation for Dentistry, 1984.<br />
Scientific Assistant in the Policlinic for Conservative and Preventive Dentistry at the Faculty<br />
of Dentistry, Justus-Liebig-University in Giessen, Germany, 1985.<br />
Promovation (thesis: “effects of rotary instrumentation on surface of human teeth”) 1989.<br />
Assistant Medical Director in the Policlinic for Conservative and Preventive Dentistry, 1992.<br />
Habilitation (“Finishing and polishing of indirect ceramic- and composite-inlays in-vitro and<br />
in-vivo”) at the Faculty of Dentistry, Justus-Liebig-University, 1999.<br />
Professor for Conservative Dentistry, 2005.<br />
Specialist for Clinical endodontics, 2006.<br />
Main scientific activities: dental materials, surface quality of restorative materials, oral<br />
hygiene products, endodontics.<br />
Dr. Nick Silikas, BSc, MPhil, PhD, FADM<br />
Lecturer in Dental Biomaterials Science<br />
University of Manchester, UK<br />
nick.silikas@manchester.ac.uk<br />
Dr. Nick Silikas is currently a Lecturer in Dental Biomaterials Science in the School of<br />
Dentistry at The University of Manchester. He was born in Greece but has completed all<br />
his Higher Education studies in Manchester where he obtained a BSc (Hons) in Chemistry,<br />
an MPhil in Pharmacy, and a PhD in Dental Biomaterials.<br />
He is an Editorial Advisor of Dental Materials-Journal for Oral and Craniofacial Biomaterials<br />
Sciences [Elsevier Science]. He is a Fellow of the Academy of Dental Materials (FADM) and<br />
a member of the International Association of Dental Research (IADR).<br />
His research interests lie in surface Imaging & Analysis. His expertises are in characterizing<br />
interfaces using several techniques like Atomic Force Microscopy (AFM), X-ray<br />
Photoelctron Spectroscopy (XPS), FEG-SEM, Fourier Transform Infra-Red Spectroscopy<br />
(FTIR) etc. He is also involved in studying mechanical properties of materials using nanoindentation<br />
and traditional mechanical testing (3-point bending, compression, flexure etc.).<br />
Prof. Angelo Putignano, MD, DDS<br />
Professor of <strong>Restorative</strong> Dentistry, Head of Endodontic and Operative Dentistry Dept.,<br />
Dean School of Dental Hygienist<br />
Polytechnic University of Marche, Ancona, Italy<br />
aputi@tin.it; a.putignano@univpm.it<br />
M.D. degree and D.D.S. post graduate certificate from the University of Ancona, Italy.<br />
Full professor in <strong>Restorative</strong> Dentistry at School of Dentistry Polytechnic University of<br />
Marche, Ancona.<br />
Head of the Operative Dentistry and Endodontic department at School of Dentistry<br />
Polytechnic University of Marche, Ancona.<br />
Dean School of Dental Hygienist Polytechnic University of Marche, Ancona.<br />
Active Member of the Italian Society of Operative Dentistry (SIDOC), as well as of the<br />
European Academy of Esthetic Dentistry (EAED).<br />
Founding Member of the Academy of Minimally Invasive Dentistry (ACAMID).<br />
Private practice in <strong>Restorative</strong> Dentistry, in Ancona.<br />
Co-author of the book “Adhesive Dentistry: the Key to success” edited by Quintessence<br />
International.<br />
Prof. David Watts, DSc, PhD, FInstP, FRSC, FADM<br />
Head of Biomaterials/Biomechanics Research Group<br />
University of Manchester, UK<br />
david.watts@man.ac.uk<br />
Professor David Watts, PhD leads the internationally-reputed Biomaterials/Biomechanics<br />
Research Group in the University of Manchester, School of Dentistry, investigating basic<br />
hard-tissue structure/properties, biomimetic-composites, new scientific instruments,<br />
photon science and developments with dental/orthopaedic industries. He has successfully<br />
supervised 40 PhD Theses and has 250+ peer-reviewed research papers. Professor Watts<br />
holds Fellowships of the Royal Society of Chemistry, the Institute of Physics and the<br />
Academy of Dental Materials and is also Research Professor at Oregon Health and<br />
Sciences University, USA. He received a Doctorate of Science from the University of<br />
Athens and the 2003 IADR Distinguished Scientist [Souder] Award for research in dental<br />
biomaterials. He became Editor-in-Chief of Dental Materials – Journal for Oral and<br />
Craniofacial Biomaterials Sciences [Elsevier] in 1998. Since 1986 he has served as UK<br />
Principal Expert to International Standards Organization TC 106 (Dentistry), on ceramics,<br />
resin-composites and photo-polymerization.<br />
I wish to thank sincerely our eminent authors, Prof. Martin Jung, Prof. Angelo Putignano,<br />
Dr. Nick Silikas and Prof. David Watts for the valuable support, scientific contribution and<br />
guidance to the realization of the <strong>Kerr</strong> <strong>Restorative</strong> Clinical Booklet.<br />
Heartfelt thanks also to the <strong>Kerr</strong> Innovation and Product Management Teams for the<br />
significant input and collaboration.<br />
Manuela Brusoni<br />
Clinical Affairs Manager Europe<br />
manuela.brusoni@kerrhawe.com<br />
43
<strong>Kerr</strong><strong>Hawe</strong> SA | Via Strecce 4 | P.O.Box 268 | CH-6934 Bioggio | Phone ++41 91 610 05 05 | Fax ++41 91 610 05 14 | www.<strong>Kerr</strong><strong>Hawe</strong>.com<br />
© 2009 <strong>Kerr</strong><strong>Hawe</strong> SA - V.01-06-’09