Proficiency Testing
Proficiency Testing
Proficiency Testing
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
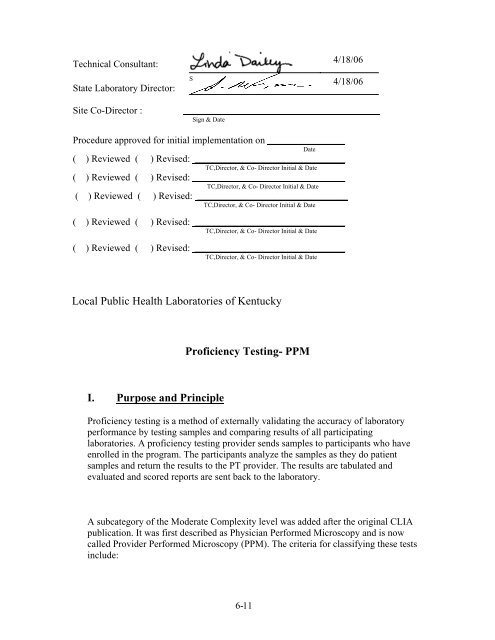
Technical Consultant:<br />
State Laboratory Director:<br />
S<br />
4/18/06<br />
4/18/06<br />
Site Co-Director :<br />
________________________________________<br />
Sign & Date<br />
Procedure approved for initial implementation on ________________<br />
Date<br />
( ) Reviewed ( ) Revised: _______________________________<br />
TC,Director, & Co- Director Initial & Date<br />
( ) Reviewed ( ) Revised: _______________________________<br />
TC,Director, & Co- Director Initial & Date<br />
( ) Reviewed ( ) Revised: _______________________________<br />
TC,Director, & Co- Director Initial & Date<br />
( ) Reviewed ( ) Revised: _______________________________<br />
TC,Director, & Co- Director Initial & Date<br />
( ) Reviewed ( ) Revised: _______________________________<br />
TC,Director, & Co- Director Initial & Date<br />
Local Public Health Laboratories of Kentucky<br />
<strong>Proficiency</strong> <strong>Testing</strong>- PPM<br />
I. Purpose and Principle<br />
<strong>Proficiency</strong> testing is a method of externally validating the accuracy of laboratory<br />
performance by testing samples and comparing results of all participating<br />
laboratories. A proficiency testing provider sends samples to participants who have<br />
enrolled in the program. The participants analyze the samples as they do patient<br />
samples and return the results to the PT provider. The results are tabulated and<br />
evaluated and scored reports are sent back to the laboratory.<br />
A subcategory of the Moderate Complexity level was added after the original CLIA<br />
publication. It was first described as Physician Performed Microscopy and is now<br />
called Provider Performed Microscopy (PPM). The criteria for classifying these tests<br />
include:<br />
6- 11
• The examination must be performed by a physician or a mid-level practitioner<br />
(i.e., nurse practitioners, nurse midwives and physician assistants) during the<br />
patient visit on a specimen obtained from the provider's patient or a patient of the<br />
group practice.<br />
• The procedure must be in the moderately complex category.<br />
• The primary instrument for the test must be a microscope.<br />
• The specimen must be labile or a delay in testing could compromise the accuracy<br />
of the test.<br />
• Control materials are not available to monitor the entire testing process.<br />
• Limited specimen handling is required.<br />
The 42 CFR 493 - October 2001 indicates that PPM laboratories are subject to<br />
Subparts H (<strong>Proficiency</strong> <strong>Testing</strong>), J (Patient test Management), K (Quality Control),<br />
M (Personnel), and P (Quality Assurance). Because the PPM tests are considered<br />
"non-regulated," proficiency testing is not specifically required, but a laboratory is<br />
responsible for documenting quality assurance. In other words, at a minimum, two<br />
split samples for each PPM test should be done yearly. Since split sampling would<br />
not be feasible for most sites, the Local PHLOK is directed to perform proficiency<br />
testing sent twice a year from the State Public Health Laboratory Technical<br />
Consultant.<br />
II.<br />
Procedural Instructions<br />
<strong>Proficiency</strong> <strong>Testing</strong> Procedure<br />
1. Each site performing PPM testing will receive twice a year, proficiency testing<br />
material from the State Technical Consultant. This material is in the form of<br />
photomicrographs obtained from the Wisconsin State Laboratory of Hygiene<br />
<strong>Proficiency</strong> <strong>Testing</strong>.<br />
2. View the images and identify the structures that the arrows are pointing to.<br />
Beginning April 2006, the State Laboratory will begin sending 5 challenges with<br />
each mailing instead of 4 for KOH/Wet Preps. Use the information provided in<br />
the case histories to aid identification.<br />
3. Record your test results on the Provider Performed Microscopy (PM) Result<br />
Form. Use the “Microscopic Glossary” provide on the Provider Performed<br />
Microscopy (PM)/Urine Sediment (SU) Instructions form to obtain code numbers<br />
for the urine sediment and wet prep challenges. Select the appropriate response<br />
codes from the glossary and enter them on the result form. For all other<br />
microscopic procedures, mark an appropriate response circle on the result form. If<br />
you do not perform a particular procedure, fill in the “Test not performed” circle.<br />
4. Sites performing any of the Microscopic Procedures listed on the Provider<br />
Performed Microscopy (PM) Result Form need to complete the <strong>Proficiency</strong><br />
<strong>Testing</strong> for those tests.<br />
6- 12
5. Obtain signature of Co-Director and testing personnel and complete the<br />
Attestation Statement Form.<br />
6. Mail results back to the State Public Health Laboratory within 5 days in the<br />
provided envelope.<br />
7. The State Technical Consultant will mail back to your site a copy of your results<br />
and the expected results along with an event specific information data form<br />
complied by Wisconsin State Hygiene Laboratory from all sites that submit<br />
testing results.<br />
8. If your site receives a score less than 80%, remedial action must be taken,<br />
documented and documentation sent to the State Lab Technical Consultant.<br />
CLIA Regulations to Support <strong>Proficiency</strong> testing<br />
493.801<br />
Subpart H<br />
<strong>Testing</strong> of <strong>Proficiency</strong> Specimen<br />
1. The laboratory must examine or test, as applicable, the proficiency testing<br />
samples it receives from the proficiency testing program in the same manner as<br />
it tests patient specimens.<br />
2. The samples must be examined or tested with the laboratory's<br />
regular patient workload by personnel who routinely perform the testing in the<br />
laboratory, using the laboratory's routine methods. The individual testing or<br />
examining the samples and the laboratory director must attest to the routine<br />
integration of the samples into the patient workload using the laboratory's routine<br />
methods.<br />
3. Laboratories that perform tests on proficiency testing samples must not engage in<br />
any inter-laboratory communications pertaining to the results of proficiency<br />
testing sample(s) until after the date by which the laboratory must report<br />
proficiency testing results to the program for the testing event in which the<br />
samples were sent. Laboratories with multiple testing sites or separate locations<br />
must not participate in any communications or discussions across sites/locations<br />
concerning proficiency testing sample results until after the date by which<br />
the laboratory must report proficiency testing results to the program.<br />
4. The laboratory must document the handling, preparation, processing,<br />
examination, and each step in the testing and reporting of results for all<br />
proficiency testing samples. The laboratory must maintain a copy of all records,<br />
including a copy of the proficiency testing program report forms used by the<br />
laboratory to record proficiency testing results including the attestation statement<br />
provided by the PT program, signed by the analyst and the laboratory<br />
director, documenting that proficiency testing samples were tested in the<br />
6- 13
same manner as patient specimens, for a minimum of two years from the date<br />
of the proficiency testing event.<br />
493.803<br />
Subpart H<br />
Failure to Participate<br />
1. Each laboratory performing nonwaived testing must successfully participate in a<br />
proficiency testing program approved by CMS, if applicable, as described in subpart I<br />
of this part for each specialty, subspecialty, and analyte or test in which the laboratory<br />
is certified under CLIA. Except as specified in paragraph (c) of this section, if<br />
a laboratory fails to participate successfully in proficiency testing for a given<br />
specialty, subspecialty, analyte or test, as defined in this section, or fails to take<br />
remedial action when an individual fails gynecologic cytology, CMS imposes<br />
sanctions, as specified in subpart R of this part.<br />
2. If a laboratory fails to perform successfully in a CMS-approved proficiency testing<br />
program, for the initial unsuccessful performance, CMS may direct the laboratory to<br />
undertake training of its personnel or to obtain technical assistance, or both, rather<br />
than imposing alternative or principle sanctions except when one or more of<br />
the following conditions exists:<br />
(1) There is immediate jeopardy to patient health and safety.<br />
(2) The laboratory fails to provide CMS or a CMS agent with<br />
satisfactory evidence that it has taken steps to correct the<br />
problem identified by the unsuccessful proficiency testing performance.<br />
(3) The laboratory has a poor compliance history.<br />
493.825<br />
Subpart H<br />
Unsatisfactory performance and remedial actions<br />
1. Failure to attain an overall testing event score of at least 80 percent is<br />
unsatisfactory performance.<br />
2. Failure to participate in a testing event is unsatisfactory performance and results<br />
in a score of 0 for the testing event.<br />
3. Failure to return proficiency testing results to the proficiency testing program<br />
within the time frame specified by the program is unsatisfactory performance and<br />
results in a score of 0 for the testing event.<br />
6- 14
4. For any unsatisfactory testing event for reasons other than a failure to participate,<br />
the laboratory must undertake appropriate training and employ the technical<br />
assistance necessary to correct problems associated with a proficiency testing<br />
failure.<br />
5. Remedial action must be taken and documented, and the documentation must be<br />
maintained by the laboratory for two years from the date of participation in the<br />
proficiency testing event.<br />
6. Failure to achieve an overall testing event score of satisfactory performance for<br />
two consecutive testing events or two out of three consecutive testing events is<br />
unsuccessful performance. The site must then demonstrate sustained satisfactory<br />
performance on two consecutive proficiency testing events, one of which may be<br />
on site. Failure to resolve remedial action will be under special review by the<br />
Director.<br />
Investigating an Unacceptable PT Result<br />
1. All documentation should be reviewed.<br />
2. Personnel who processed or tested the specimen, and who transcribed results<br />
should be interviewed. The investigation should include:<br />
• Checks for clerical errors<br />
• Review of records of quality control, calibration status and instrument<br />
function checks<br />
• Repeat analysis and calculations when possible<br />
• Evaluation of the laboratory’s historical performance for that analyte<br />
3. The laboratory should review patient data from the time of the unacceptable PT<br />
result, to determine whether the problem could have affected patient care. If so,<br />
appropriate follow-up action should be documented.<br />
4. The laboratory should make every effort to find the cause(s) of an unacceptable<br />
result. In instances where the laboratory can identify an underlying system<br />
problem that contributed to the unacceptable result, actions to improve laboratory<br />
systems will minimize the risk of recurrence and potentially improve the quality<br />
of patient results.<br />
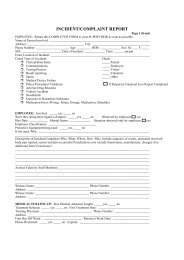
5. The investigation, conclusions, and corrective action should be thoroughly<br />
documented. For standardized form for reporting the results of every unacceptable<br />
PT investigation, use the Corrective Action/Incident Reporting form found in<br />
Section 7.<br />
III. References<br />
Appendix C, Survey Procedures and Interpretive Guidelines for Laboratories and<br />
Laboratory Services, CMS Website, http://www.phppo.cdc.gov/clia/regs/toc.aspx,<br />
accessed April 2006<br />
6- 15
Using <strong>Proficiency</strong> <strong>Testing</strong> (PT) to Improve the Clinical Laboratory; Approved Guideline,<br />
NCCLS GP27-A, Vol. 19, No, 15, 940 West Valley Road, Wayne, PA, 19087, 1999<br />
Provider-Performed Microscopy <strong>Testing</strong>; Approved Guideline, NCCLS HS2-A, Vol. 20<br />
No.3, 940 West Valley Road, Wayne, PA, 19087, 2003<br />
Wisconsin State Hygiene Laboratory <strong>Proficiency</strong> <strong>Testing</strong> Program,<br />
http://www.slh.wisc.edu/pt/, 465 Henry Mall: Room 402,<br />
Madison WI 53706-1578, accessed April 2006<br />
American Academy of Family Physicians <strong>Proficiency</strong> <strong>Testing</strong>, P.O. Box 11210<br />
Shawnee Mission, KS 66207-1210, http://www.aafp.org/x2255.xml, accessed April 2006<br />
IV. Author<br />
Linda Dailey, MT (ASCP) April 2006<br />
V. Procedure Policy, Approval and Review Process<br />
1. The official copy of each procedure will be placed in the Technical and<br />
Administrative Branch Manager’s copy of the Local Public Health Laboratory of<br />
Kentucky Standard Operating Procedures Manual. A copy of the procedure to be<br />
placed in the SOPM at each PHLOK approved site.<br />
2. Each procedure will be initially reviewed and approved with signature by the<br />
Technical Consultant, State Director and Co-Director prior to implementation.<br />
3. Each procedure will be reviewed annually and as needed for necessary revision. Any<br />
modification will be reviewed and approved as stated in #2 above.<br />
4. Implementation of new or revised procedures must be communicated to all testing<br />
personnel prior to the implementation date. The Co-Director must document that<br />
each of the testing personnel (by individual name) have been made aware of the<br />
procedure changes, revision implementation date and been trained as necessary.<br />
5. Any associated logs, specimen collection instructions or other documents related to<br />
the procedure change must be initiated.<br />
6. Each procedure must have a master file, stored at the State Lab, that contains the<br />
current and all previous versions. The master file serves as the documented history of<br />
the procedure, showing all revisions and the dates used and discontinued or retired.<br />
The master file must be maintained for a least two (2) years from last date used.<br />
VI. Appendix<br />
Copy of Provider Performed Microscopy (PM)/ Urine Sediment (SU) Instructions<br />
Copy of Provider Performed Microscopy (PM) Result Form<br />
Copy of Urinalysis & Microscopy Attestation/Comments Page<br />
Copy of Provider Performed Microscopy (PM) photomicrographs<br />
Copy of Performance Evaluation by Site<br />
6- 16