FAILURE TO THRIVE - Flourish Paediatrics
FAILURE TO THRIVE - Flourish Paediatrics
FAILURE TO THRIVE - Flourish Paediatrics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
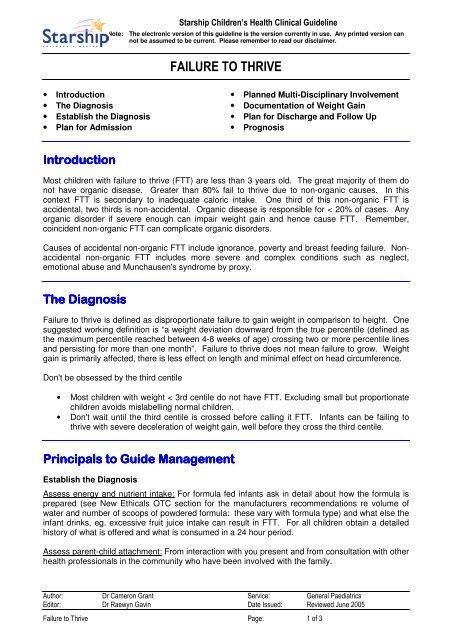
Starship Children’s Health Clinical Guideline<br />
Note: The electronic version of this guideline is the version currently in use. Any printed version can<br />
not be assumed to be current. Please remember to read our disclaimer.<br />
<strong>FAILURE</strong> <strong>TO</strong> <strong>THRIVE</strong><br />
• Introduction<br />
• The Diagnosis<br />
• Establish the Diagnosis<br />
• Plan for Admission<br />
• Planned Multi-Disciplinary Involvement<br />
• Documentation of Weight Gain<br />
• Plan for Discharge and Follow Up<br />
• Prognosis<br />
Introduction<br />
Most children with failure to thrive (FTT) are less than 3 years old. The great majority of them do<br />
not have organic disease. Greater than 80% fail to thrive due to non-organic causes. In this<br />
context FTT is secondary to inadequate caloric intake. One third of this non-organic FTT is<br />
accidental, two thirds is non-accidental. Organic disease is responsible for < 20% of cases. Any<br />
organic disorder if severe enough can impair weight gain and hence cause FTT. Remember,<br />
coincident non-organic FTT can complicate organic disorders.<br />
Causes of accidental non-organic FTT include ignorance, poverty and breast feeding failure. Nonaccidental<br />
non-organic FTT includes more severe and complex conditions such as neglect,<br />
emotional abuse and Munchausen's syndrome by proxy.<br />
The Diagnosis<br />
Failure to thrive is defined as disproportionate failure to gain weight in comparison to height. One<br />
suggested working definition is “a weight deviation downward from the true percentile (defined as<br />
the maximum percentile reached between 4-8 weeks of age) crossing two or more percentile lines<br />
and persisting for more than one month”. Failure to thrive does not mean failure to grow. Weight<br />
gain is primarily affected, there is less effect on length and minimal effect on head circumference.<br />
Don't be obsessed by the third centile<br />
• Most children with weight < 3rd centile do not have FTT. Excluding small but proportionate<br />
children avoids mislabelling normal children.<br />
• Don't wait until the third centile is crossed before calling it FTT. Infants can be failing to<br />
thrive with severe deceleration of weight gain, well before they cross the third centile.<br />
Principals to Guide Management<br />
Establish the Diagnosis<br />
Assess energy and nutrient intake: For formula fed infants ask in detail about how the formula is<br />
prepared (see New Ethicals OTC section for the manufacturers recommendations re volume of<br />
water and number of scoops of powdered formula: these vary with formula type) and what else the<br />
infant drinks, eg. excessive fruit juice intake can result in FTT. For all children obtain a detailed<br />
history of what is offered and what is consumed in a 24 hour period.<br />
Assess parent-child attachment: From interaction with you present and from consultation with other<br />
health professionals in the community who have been involved with the family.<br />
Author: Dr Cameron Grant Service: General <strong>Paediatrics</strong><br />
Editor: Dr Raewyn Gavin Date Issued: Reviewed June 2005<br />
Failure to Thrive Page: 1 of 3
Starship Children’s Health Clinical Guideline<br />
Note: The electronic version of this guideline is the version currently in use. Any printed version can<br />
not be assumed to be current. Please remember to read our disclaimer.<br />
<strong>FAILURE</strong> <strong>TO</strong> <strong>THRIVE</strong><br />
Developmental assessment is crucial: With non-organic failure to thrive all milestones are usually<br />
delayed by the time the infant reaches 4 months of age. Areas dependent upon environmental<br />
interactions, such as language development and social adaptation, are often disproportionately<br />
delayed.<br />
Common physical examination findings in non-organic failure to thrive:<br />
• Signs of failure to gain weight<br />
e.g. loss of fat, prominence of<br />
ribs, muscle wasting<br />
especially of large groups e.g.<br />
gluteals<br />
• Signs of poor hygiene<br />
• Infant very watchful and alert<br />
• Infant dislikes being touched or held<br />
• Lack of stranger anxiety<br />
• Toddler may indiscriminately seek<br />
affection<br />
• Developmental delay • Mild hepatomegaly<br />
• Apathetic and withdrawn<br />
behaviour<br />
• Minimal smiling and<br />
decreased vocalisation<br />
• Infant rarely cries but is<br />
hyperirritable<br />
• Hypertonia<br />
• Diminished muscle strength<br />
• Retention of tonic posturing<br />
Exclude organic disease: This requires a detailed history and examination. Laboratory<br />
investigations will add very little unless there are significant findings in the history and examination.<br />
Investigations that should be considered include: urinalysis (pH, osmolality, cellular elements,<br />
glucose, ketones), urine culture, stool for ova and parasites, full blood count, erythrocyte<br />
sedimentation rate, serum urea, creatinine, electrolytes, calcium and phosphorus, total protein,<br />
albumin, and liver enzymes and coeliac screening.<br />
Plan for Admission<br />
Children should be hospitalised for FTT when it persists despite maximisation of community<br />
support (community nurse, community dietician, social worker, whanau, church, etc.) or because<br />
characteristics of the child, care giver or family make such outpatient management inappropriate or<br />
place the child at risk of neglect or injury.<br />
The three aims of hospitalisation of children with FTT are:<br />
To observe the child's feeding behaviour and the mother-child interaction<br />
To see whether the infant's weight gain returns to normal when s/he is provided with adequate<br />
caloric intake and/or is removed from the family<br />
To decide whether further laboratory testing is indicated<br />
Planned Feeding Regimen<br />
The feeding regimen must be accurately charted and nutritional intake accurately recorded on a 24<br />
hour fluid balance sheet. The majority of children with FTT will consume > 130 kcal/kg/day. They<br />
should be offered a caloric intake 50% greater than required for normal growth by a child of the<br />
same height and of average weight. Average energy requirements are 110 kcal/kg/day for first 6<br />
months, 100 kcal/kg/day for second 6 months and subsequently to age 3.<br />
Severity of malnutrition can be determined by calculating the actual weight as a percentage of ideal<br />
weight for height. Normal is 90 to 110 percent<br />
Author: Dr Cameron Grant Service: General <strong>Paediatrics</strong><br />
Editor: Dr Raewyn Gavin Date Issued: Reviewed June 2005<br />
Failure to Thrive Page: 2 of 3
Starship Children’s Health Clinical Guideline<br />
Note: The electronic version of this guideline is the version currently in use. Any printed version can<br />
not be assumed to be current. Please remember to read our disclaimer.<br />
<strong>FAILURE</strong> <strong>TO</strong> <strong>THRIVE</strong><br />
Malnutrition:<br />
Mild = 85 to 90 % of ideal weight for actual height<br />
Moderate = 75 to 85 percent<br />
Severe is = < 75 percent<br />
With non-organic FTT consistent weight gain usually occurs within 2 weeks, occasionally it may<br />
take up to 3-4 weeks. Usually it will reach 50 g per day.<br />
Planned Multi-Disciplinary Involvement<br />
Consultation with the dietician will be helpful in determining severity of malnutrition, estimating<br />
caloric intake and ensuring appropriate, high calorie diet. FTT in the infant can be a symptom of<br />
much broader dysfunction affecting the family. Assessment of the family will require consultation<br />
with the community agencies listed above. During hospitalisation assessment of the mother's and<br />
the family's emotional and psychiatric health may be necessary. The child and family unit may<br />
need to be consulted. Social work involvement may be required. Input from other disciplines such<br />
as Kaitiaki, Pacific family support, lactation specialists, speech therapy and developmental therapy<br />
will be helpful in some situations.<br />
Documentation of weight gain<br />
Weight, length, head circumference and weight-for-height should be plotted on admission. The<br />
infant should be weighed daily and this weight recorded on daily weight plot. All parameters<br />
should be documented again prior to discharge.<br />
Plan for Discharge and Follow Up<br />
Multi-disciplinary community management is required<br />
If child not admitted plan follow up with community nurse ± dietician, GP, and CED or outpatient<br />
clinic.<br />
If admitted multidisciplinary community co-ordination with discharge planning is essential. Ensure<br />
communication and follow up between all hospital services and related community agencies has<br />
occurred.<br />
eg. Medical staff ↔ general practitioner<br />
Hospital ↔ community nursing.<br />
Occupational therapy ↔ visiting developmental therapy<br />
Kaitiaki ↔ community Maori health services<br />
Pacific family support ↔ community Pacific health providers<br />
Prognosis<br />
There is an increased risk of continued growth retardation. Many children remain small.<br />
Furthermore, severely impaired growth during the first 6 months of life (controlling for SES and iron<br />
deficiency) is associated with impaired mental and psychomotor development during the second<br />
year. The earlier the onset and the greater its severity the worse the outcome. Whether or not<br />
these changes persist, and how much this persistence is due to adverse social circumstances is<br />
still uncertain.<br />
Author: Dr Cameron Grant Service: General <strong>Paediatrics</strong><br />
Editor: Dr Raewyn Gavin Date Issued: Reviewed June 2005<br />
Failure to Thrive Page: 3 of 3