EQUINE CLINICAL PATHOLOGY - Rossdale & Partners
EQUINE CLINICAL PATHOLOGY - Rossdale & Partners
EQUINE CLINICAL PATHOLOGY - Rossdale & Partners
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
the<br />
beaufort cottage laboratories Guide to<br />
equine clinical<br />
pathology
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Welcome to the Beaufort Cottage Laboratories<br />
Guide to Equine Clinical Pathology.<br />
We hope this Guide will provide practical help to<br />
busy veterinary clinicians, nurses and students in<br />
need of a reference source in the course of their<br />
daily work or studies. It is not intended to be a<br />
textbook, nor do we pretend it is complete.<br />
For further advice on pathology issues raised in this<br />
Guide, please call Beaufort Cottage Laboratories<br />
on +44 (0)1638 663017 (office hours). In case of<br />
emergency, please call <strong>Rossdale</strong> & <strong>Partners</strong> on<br />
+44 (0)1638 663150 (24 hours).
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Contents<br />
Introduction 4<br />
Using clinical pathological aids to diagnosis 6<br />
Clinical disease, preventive medicine, laboratory profiles, management aids<br />
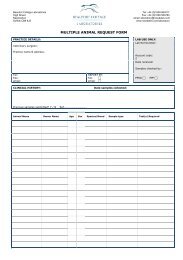
Sampling requirements 8<br />
Labelling and request forms, dispatch, post & packaging, sampling equipment<br />
Reference ranges 11<br />
Haematology 12<br />
Erythrocytes 12, Leucocytes 14, Platelets 17<br />
Clinical chemistry 19<br />
Proteins 19, IGG 21, plasma fibrinogen, SAA, AST, 22, CK, LD 24, cardiac troponin 25, SDH,<br />
GLDH, GGT 27, SAP, IAP, bilirubin, bile acids 28, amylase, glucose, oral glucose absorption<br />
test, cholesterol & triglycerides, urea 29, creatinine, urine fractional clearance ratios 30,<br />
calcium, potassium & chloride, calcium, phosphate & magnesium 31, plasma lactate 32<br />
Blood gas analysis 33<br />
Endocrinology 33<br />
Pregnancy tests, progestagens 33, granulosa cell tumour 34, cryptorchidism,<br />
thyroid function, pituitary function, glucose, cortisol, insulin, overnight dexamethasone<br />
suppression test 35, TRH stimulation test, combined DXM suppression/TRH stim. test 36<br />
Urine collection and analysis 37<br />
Parasitology 38<br />
Faeces collection, faecal worm egg counts, faecal lungworm larval counts<br />
Microbiology 39<br />
Bacterialogy, skin scrapings, virology 40<br />
Cytology 42<br />
Fluid samples - peritoneal, pleural 43, synovial, tracheal washes, bronchoalveolar lavage 44,<br />
cerebrospinal fluid, bone marrow 45, semen samples, endometrial smears 46<br />
Histology 47<br />
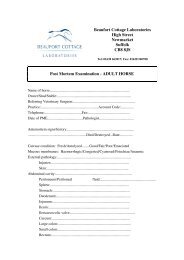
Necropsy (postmortem) examinations 48<br />
Adult horses 48, CMSNG sampling, neonatal foals, foeti and placentae 50<br />
Biopsy sampling 52<br />
Skin, lump, liver, lung 52, kidney, endometrial 53, testicular, ileal 54, rectal 55<br />
Tables of reference ranges 56
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
introduction<br />
In all aspects of veterinary medicine, an<br />
accurate diagnosis is a pre-requisite for<br />
specific treatment and appropriate case<br />
management. Making a diagnosis involves<br />
a challenging combination of art and science and, if<br />
used correctly, laboratory investigations may be helpful.<br />
Following a definitive diagnosis, follow-up clinical<br />
and laboratory examinations can assess the effects of<br />
treatment. Where progress is unsatisfactory, more detailed<br />
investigations are often indicated as directed by the<br />
characteristics of the individual case.<br />
Making a diagnosis can be likened to ‘jigsaw puzzling’.<br />
The more pieces become available, the easier it becomes<br />
to solve the puzzle. Historical information and clinical<br />
examination results remain the first steps in the diagnostic<br />
pathway, sometimes allowing a definitive diagnosis to<br />
be made immediately, e.g. for a mid-shaft cannon bone<br />
fracture. More often, a differential diagnosis needs to be<br />
refined by clinical pathological aids and further clinical<br />
diagnostic procedures, e.g. recurrent laminitis and<br />
hepatopathy associated with equine Cushing’s syndrome.<br />
These aids must be applied appropriately, accurately and<br />
efficiently, to best effect.<br />
Incorrect results or incorrectly interpreted results may<br />
confuse the diagnostic pathway, leading to incorrect<br />
treatment and case management. In-house quality control
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
and external quality assurance are important for all<br />
veterinary laboratories to ensure reliability of results and<br />
to give confidence both to laboratory staff and to their<br />
clients.<br />
Veterinary surgeons have a duty to relieve suffering<br />
in animals as quickly and efficiently as possible. Ideally,<br />
to achieve this, they should provide their patients with<br />
the most accurate diagnosis possible, as early as possible,<br />
using whatever aids are available and appropriate so that<br />
early treatment is successful. This may appear costly in the<br />
short term, but can sometimes save expense in the longer<br />
term by avoiding delays in starting appropriate treatments<br />
or by avoiding the use of inappropriate treatments and<br />
thereby shortening time to recovery. In addition to welfare<br />
considerations, early accurate diagnoses and treatments<br />
bring significant benefits for performance horses and aid<br />
profitability to their owners.<br />
Clinicopathological aids may be applied in cases of<br />
clinical disease and for the assessment of their treatment,<br />
in preventive medicine programmes, and as management<br />
aids. The tables on the next two pages are presented as<br />
broad guides to the use of laboratory aids to diagnosis<br />
in specific clinical, preventive medicine and managerial<br />
indications.<br />
August 2006
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Using Clinical Pathological aids to diagnosis<br />
Clinical disease<br />
Clinical condition<br />
Infection<br />
Intestinal parasitism<br />
Liver disease<br />
Kidney disease<br />
Pancreatic disease<br />
Skin disease<br />
Bone metabolic/parathyroid<br />
abnormality<br />
Weight loss/diarrhoea<br />
Pulmonary abnormality<br />
Fluid/electrolyte balance<br />
Stallion genital abnormality<br />
Mare genital abnormality<br />
Potentially useful tests<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
protein electrophoresis, bacteriology, mycology, virology,<br />
serology.<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
albumin and protein electrophoresis, tapeworm ELISA, faecal<br />
worm egg count, rectal biopsy.<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
protein electrophoresis, AST, LD and isoenzymes, GGT, GLDH,<br />
SAP, bile acids, liver scan and biopsy.<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
proteins, urea, creatinine, urine analysis and electrolytes,<br />
fractional electrolyte clearance ratios, bacteriology, kidney scan<br />
and biopsy.<br />
Serum GGT, amylase and lipase.<br />
Skin scrapings, biopsy, bacteriology, mycology, feed allergen<br />
tests.<br />
SAP, calcium and phosphate, urine phosphate<br />
clearance ratios.<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
albumin and protein electrophoresis, SAP, IAP, glucose<br />
absorption test, peritoneal fluid cytology, faecal Rotavirus assay,<br />
serum electrolytes, feed allergen tests. Faecal occult blood.<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
proteins, blood gas analysis, faecal lungworm examination,<br />
tracheal wash/BAL cytology, bacteriology.<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
albumin and proteins, electrolytes, urine analysis and fractional<br />
electrolyte clearances, blood gas analysis.<br />
Endocrinology, bacteriology, semen analysis, testicular biopsy.<br />
Endocrinology, bacteriology, endometrial cytology and biopsy.
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Preventive medicine<br />
Clinical condition<br />
Intestinal parasitism<br />
Venereal disease<br />
Diarrhoea<br />
Nasal discharge<br />
Skin lesions<br />
Useful tests<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
albumin and protein electrophoresis, tapeworm ELISA, faecal<br />
worm egg count.<br />
Penile and preputial, clitoral and endometrial aerobic and<br />
microaerophilic bacteriology.<br />
Rectal/faecal bacteriology for Salmonella spp. and<br />
Campylobacter spp. and fluid faeces for Rotavirus test. Faecal<br />
occult blood test.<br />
Nasopharyngeal, guttural pouch and tracheal washes for<br />
Streptococcus equi and Rhodococcus equi bacteriology.<br />
Scrapings for dermatophytes, skin biopsy.<br />
Laboratory Profiles<br />
Age/type/condition<br />
Useful tests<br />
12-36 hours Haematology, serum amyloid A, plasma fibrinogen, serum<br />
proteins, IgG.<br />
Weanling and yearling<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
proteins, SAP, calcium, phosphate, urinary phosphate fractional<br />
clearance ratios.<br />
Inflammatory disease<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
proteins and electrophoresis.<br />
Horses in training<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
proteins, AST, CK.<br />
Mature horse complete profile Haematology, serum amyloid A, plasma fibrinogen, serum<br />
proteins and electrophoresis, AST, CK, LD and isoenzymes, GGT,<br />
GLDH, SAP, IAP, urea, creatinine.<br />
Management Aids<br />
Management requirement<br />
‘Unfitness’ (horses in training)<br />
Mare pregnancy tests<br />
Mare luteal function<br />
Anthelmintic programme efficacy<br />
Useful tests<br />
Haematology, serum amyloid A, plasma fibrinogen, serum<br />
proteins, AST, CK.<br />
45-95 days – serum eCG.<br />
>120 days – serum oestrone sulphate.<br />
>150 days – urinary oestrogens.<br />
Plasma progesterone.<br />
WEC, tapeworm ELISA
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
sampling requirements<br />
Laboratory results are only as good as the samples submitted<br />
allow them to be. Samples should be taken by the correct<br />
techniques, with suitable equipment, into suitable containers<br />
and media/preservatives and securely dispatched to the<br />
laboratory in the shortest possible time.<br />
<br />
Labelling and request forms<br />
All specimens should be labelled legibly<br />
with the name of the horse, date and<br />
time of sampling and site of collection,<br />
if appropriate, to enable proper reporting<br />
and certification of results. A concise<br />
case history should always be included,<br />
to help the laboratory make sure that<br />
the appropriate tests are performed and<br />
reported quickly and efficiently and in order<br />
to allow the clinical pathologist to help the<br />
clinician interpret the results.<br />
Dispatch<br />
Avoid sending perishable specimens over<br />
the weekend, where they may be held<br />
up and deteriorate in the post. Where<br />
possible it is sensible to centrifuge or to<br />
allow clotted blood samples to stand until<br />
it is possible to pour or pipette off the<br />
serum, in order to avoid haemolysis. Do<br />
not refrigerate EDTA samples or haemolysis<br />
will render the results useless. Do not send<br />
frozen or unfixed tissues for histological<br />
examinations as they will undergo natural<br />
autolysis and arrive in a less than suitable<br />
or even useless condition for satisfactory<br />
examination.<br />
For urgent samples and for dead foals,<br />
foeti and placentae for postmortem<br />
examinations, we strongly recommend<br />
personal delivery, e.g. by owner or private<br />
courier service.<br />
Post and Packaging<br />
Please instruct your secretarial staff<br />
in the proper packaging of specimens<br />
so that disappointments do not occur.<br />
Sound packaging is essential to avoid<br />
the breakage of containers in the post<br />
and the loss of, or damage to samples.<br />
Internal and external packing is essential<br />
('Jiffy bags' alone cannot be relied upon).<br />
The leakage of pathological specimens<br />
can present public health hazards and<br />
the Royal Mail may refuse to handle<br />
soiled packages. The following notice was<br />
published and circulated by the Royal<br />
College of Veterinary Surgeons in August<br />
1988:-<br />
1. In general, the despatch of deleterious<br />
substances by post is banned by the<br />
Post Office. There are however special<br />
exemptions for pathological material sent<br />
to and from laboratories by veterinary
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Sampling Equipment<br />
Test Sample Container/anticoagulant/preservative<br />
Haematology Whole blood EDTA (lilac Vacutainer or blue Monovette)<br />
Plasma fibrinogen Whole blood Sodium citrate (blue Vacutainer or green<br />
Monovette)<br />
Clinical chemistry,<br />
serology, minerals Serum Empty tube (red Vacutainer or brown Monovette)<br />
and electrolytes<br />
Plasma glucose Whole blood Fluoride/oxalate (grey Vacutainer or yellow<br />
Monovette)<br />
Plasma progesterone Plasma or serum Lithium heparin (green Vacutainer or orange<br />
Monovette)<br />
Mare pregnancy Serum or plasma Empty tube (red Vacutainer or brown Monovette)<br />
Urinalysis Urine Sterile, empty, leak-proof container<br />
Blood selenium or<br />
Lithium heparin (green Vacutainer or orange<br />
glutathione peroxidase Erythrocytes Monovette)<br />
Bacteriology Swabs<br />
Amies charcoal transport medium<br />
Fluids<br />
Blood grow medium<br />
Faeces<br />
Sterile, leak-proof container<br />
Blood<br />
Blood grow medium<br />
Virology Rotavirus Liquid faeces in sterile leak-proof container<br />
Swabs<br />
Viral transport medium<br />
Parasitology Faeces<br />
Sterile, leak-proof container<br />
Dermatology Skin scrapings Sterile, leak-proof container<br />
Cytology Endometrial and Rolled onto sterile gelatine-coated slides and<br />
other smears fixed with ‘smear fix’ or carbowax<br />
Peritoneal, pleural, One sample preserved in EDTA, another diluted<br />
CSF, synovial fluids, 50:50 in cytospin centrifuge fluid and another<br />
tracheal washes undiluted in a sterile leak-proof container<br />
and BALs<br />
(synovial fluid also in blood grow medium for<br />
bacterial culture)<br />
Histology General tissue Thin, representative samples fixed in an ample<br />
samples<br />
volume (at least 10 x) of 10% formol saline<br />
Endometrial and Bouin’s fluid<br />
testicular biopsies<br />
Semen analysis Semen One sample diluted 50:50 in formol citrate and<br />
another in an empty, sterile, leak-proof container.
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
surgeons and some others. Very highly<br />
infected materials such as that containing<br />
foot and mouth disease virus or some<br />
especially dangerous human pathogens are<br />
excluded from this exemption.<br />
2. Members of the public may send<br />
specimens through the post only at the<br />
express request of a registered laboratory<br />
or veterinary surgeon.<br />
3. Only first-class letter post or data post<br />
may be used. Parcel post must not be<br />
used.<br />
4. The Post Office requires that all samples<br />
be packed in a particular way. These rules<br />
must be followed otherwise the Post Office<br />
may remove and destroy the specimen.<br />
a. Every specimen must be enclosed in<br />
a primary container, which is securely<br />
sealed. This container must not exceed<br />
50ml (although special multi-specimen<br />
packs may be approved).<br />
b. The primary container must be wrapped<br />
in sufficient absorbent material to absorb all<br />
possible leakage in the event of damage.<br />
c. The container and absorbent material<br />
must be sealed in a leak proof plastic bag.<br />
d. This package must then be placed in<br />
either:<br />
i. A polypropylene clip down container.<br />
ii. A cylindrical light metal container.<br />
iii. A strong cardboard box with full<br />
depth lid.<br />
iv. A specially grooved two-piece<br />
polystyrene box.<br />
5. It is recommended that this completed<br />
package should be placed in a padded<br />
bag.<br />
6. Multi-specimen packs may be used<br />
provided that each primary container is<br />
separated from the next by absorbent<br />
packing.<br />
7. Any other packaging systems must have<br />
the prior approval of the Post Office.<br />
8. Labelling: The outer cover must be<br />
labelled ‘Pathological Specimen Fragile.<br />
With Care’. It must show the name and<br />
address of the sender to be contacted in<br />
case of leakage.<br />
9. Therapeutic and diagnostic substances,<br />
such as blood, serum, vaccines etc. are<br />
classified as pathological specimens.<br />
Ensure that anything you send by post<br />
complies with the regulations otherwise<br />
it may be removed from the mail and<br />
destroyed, and you will lose a valuable<br />
specimen. You may be prosecuted by<br />
the Royal Mail. You may cause injury or<br />
disease to someone handling the package<br />
either during its transit through the mails,<br />
or at the receiving laboratory.<br />
10
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
reference ranges<br />
Clinicians and clinical pathologists must rely upon so-called<br />
‘normal’ reference ranges to interpret laboratory results.<br />
Unfortunately it is not possible to produce one set of ‘normals’<br />
to suit all equine animals, as horses and ponies of different<br />
ages, types, uses and stages of training all have significant<br />
variations in some parameters.<br />
Another problem is that individual horses<br />
vary considerably not only in their own<br />
‘normal’ reference results but also by the<br />
effects that variations from reference range<br />
and even clinical abnormality will have<br />
on their clinically-apparent health and<br />
performance. Sub-clinical disease, e.g.<br />
low-grade anaemia, viral ‘challenges’,<br />
low-grade myopathy, hepatopathy and<br />
nephropathy will all produce effects on<br />
the appropriate laboratory results although<br />
the horse is considered clinically ‘normal’.<br />
The owner, rider, trainer or manager’s<br />
assessment of each horse as an individual<br />
remains essential and laboratory results<br />
should never be used to 'train' performance<br />
horses. Experienced interpretations are<br />
required for different types of horses used<br />
for different purposes.<br />
The ‘classical’ method of producing<br />
reference ranges for laboratory tests was to<br />
use the ‘bell-shaped curve’ of two standard<br />
deviations either side of the mean of large<br />
numbers of clinically normal horses. This<br />
requires the measured parameter to have a<br />
mathematically normal distribution within<br />
the horse population to be applicable and<br />
this is rarely the case. Alternatives are to<br />
work with percentiles (the range within<br />
which the results of 90% of clinically<br />
normal horses fall). Even then clinically<br />
normal horses will have significant subclinical<br />
changes and individual horses will<br />
have idiosyncratic ranges different to the<br />
population range. Clinicians and clinical<br />
pathologists must use reference ranges that<br />
they are comfortable with.<br />
Reference ranges for the more commonly<br />
used haematological and clinical chemical<br />
parameters, for adult non-Thoroughbred<br />
horses, neonatal and older Thoroughbred<br />
foals, Thoroughbred yearlings and two<br />
and three-year-old Thoroughbred horses in<br />
training can be found on pages 56-71.<br />
11
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Haematology<br />
In the presence of clinical signs of disease, haematological<br />
examinations, performed on sequestrated (EDTA)<br />
blood samples, may reveal abnormalities suggesting<br />
haemoconcentration, anaemia, bacterial or viral infections,<br />
parasitic or allergic conditions.<br />
12<br />
These examinations may also be valuable<br />
as part of a preventive medicine programme<br />
for groups of horses, when examined on a<br />
regular and routine basis, and interpreted<br />
carefully. Such a sampling programme may<br />
provide useful information that can be used<br />
as a basis for advice to trainers of race and<br />
performance horses.<br />
Most clinical pathology laboratories now use<br />
automated or semi-automated cytochemical<br />
or particle counting haematology analysers.<br />
These provide much more accurate and<br />
repeatable results than the older manual<br />
counting technologies if the analysers are<br />
correctly calibrated for equine samples.<br />
It is important to remember that results<br />
from analysers that provide granulocyte/<br />
non-granulocyte differential leucocyte<br />
counts must be interpreted differently from<br />
those that produce cytochemically stained<br />
and laser scanned differential leucocyte<br />
counts. The latter, if calibrated correctly,<br />
can be indistinguishable from traditional<br />
manual counts performed on stained<br />
films. Automated differentials are highly<br />
repeatable and are more accurate than<br />
manual cell counts as some analysers<br />
differentiate and count 10,000 rather<br />
than 100 leucocytes. Beaufort Cottage<br />
Laboratories currently use a Bayer Advia<br />
120 automated cytochemical haematology<br />
analyser.<br />
Samples for haematological examinations<br />
should be taken from horses at rest with<br />
minimal excitement, otherwise splenic<br />
contraction can make the interpretation of<br />
erythrocyte parameters impossible.<br />
Erythrocytes<br />
(RBC, PCV, Hb, MCV, McHc, McH)<br />
Haemoconcentration/dehydration (raised<br />
total erythrocyte count, haematocrit and<br />
haemoglobin concentration) can only be<br />
interpreted in samples taken from resting<br />
horses that are relaxed at collection and<br />
this can be very difficult to achieve in<br />
some excitable individuals. Reflex splenic<br />
contraction occurs in horses in response to<br />
fright, excitement and exercise, increasing<br />
numbers of young macrocytic erythrocytes<br />
in the circulating pool. Routine sampling<br />
sessions in performance horse stables are<br />
therefore often conducted at standard times
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
after a period of rest and quiet, e.g. early<br />
morning or late afternoon, before mucking<br />
out and feeding, in order to avoid sampling<br />
excited horses and to add a degree of<br />
standardisation.<br />
Haemoconcentration is sometimes a<br />
feature of so-called ‘over-trained’ horses<br />
that perform poorly, appear stressed, and<br />
have dry scurfy skin coats, lose condition<br />
and drink inadequately. They usually<br />
respond well to fluid and electrolyte therapy<br />
administered by nasogastric tube followed<br />
by a period of rest. Chronic anhidrosis can<br />
produce a similar picture. Dehydration is a<br />
feature of horses who are clinically ill with<br />
acute enteritis or colitis, requiring intensive<br />
fluid, electrolyte, acid-base and supportive<br />
therapy to replace losses. Haemoconcentration<br />
and dehydration are features<br />
of exercise and heat exhaustion in horses<br />
performing in hot dry climates and over<br />
long distances (typically endurance races),<br />
requiring timely diagnosis and appropriate<br />
treatment/management. The interesting<br />
condition of acute anhidrosis, i.e. failure<br />
of normal sweating, occurs in some horses<br />
who are raised in temperate climates and<br />
then perform in hot, dry climates when<br />
they have failed to acclimatise, resulting<br />
in respiratory distress, laboured breathing,<br />
pyrexia, collapse and even death.<br />
Attempts have been made to interpret<br />
the significance of results of post-exercise<br />
blood samples in terms of fitness. In terms<br />
of haematologic tests, variable degrees<br />
of haemoconcentration and leucocytosis<br />
are always a feature and without rigid<br />
standard exercise test regimes, which are<br />
almost impossible to organise within most<br />
performance horse training environments,<br />
results are usually uninterpretable. Specific<br />
muscle enzyme tests (see page 16)<br />
performed on serum samples collected<br />
before and after exercise, can help with the<br />
diagnosis of exercise-induced myopathy.<br />
There has been considerable interest in<br />
lactate assays before, during and after<br />
exercise to determine aerobic/anaerobic<br />
metabolic capacity, with still considerable<br />
debate and differences of opinion.<br />
Anaemia (low total erythrocyte count,<br />
haematocrit and haemoglobin concentration)<br />
in horses is less commonly a primary<br />
condition and more often occurs secondary<br />
to some other primary condition, e.g.<br />
infection (bacterial or viral), parasitism (endo<br />
or ectoparasitism) or metabolic abnormality<br />
(e.g. hepatopathy, nephropathy), which<br />
require specific diagnosis and treatment.<br />
Malnutrition is rarely seen in performance<br />
horse stables but mineral and vitamin<br />
imbalances (involving deficiency or excess)<br />
may occur.<br />
Acute haemorrhage can cause acute primary<br />
blood loss anaemia following accidental<br />
injury involving a major blood vessel. The<br />
haemorrhage may sometimes be visible<br />
externally but more often occurs internally<br />
within a body cavity, i.e. intraperitoneal,<br />
intrapleural or intrapericardial haemorrhage.<br />
13
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Chronic haemorrhage, e.g. following<br />
castration, may cause an anaemia and selfperpetuating<br />
thrombocytopenia. Platelet<br />
transfusion may result in haemostasis<br />
without further surgical interference.<br />
Guttural pouch mycosis may cause<br />
internal carotid artery ulceration, resulting<br />
in profound acute and sometimes fatal<br />
epistaxis and blood-loss anaemia. Gastric<br />
ulceration, not uncommonly seen in<br />
performance horses, can cause anaemia<br />
from chronic haemorrhage. Examination<br />
of faecal samples for the presence of<br />
occult blood can be performed but results<br />
are frequently positive, most commonly<br />
because of activity of intestinal parasites,<br />
even in well-managed horses, and are<br />
therefore not reliably diagnostic of gastric<br />
ulceration. Unfortunately, serum pepsinogen<br />
assays are not reliably diagnostic of gastric<br />
ulceration in horses. Where suspected,<br />
the diagnosis must be made and the<br />
significance assessed by gastroscopic<br />
examinations.<br />
Intravascular haemolysis, i.e. erythrocyte<br />
destruction resulting in haemolytic<br />
anaemia, has a variety of different<br />
causes, which require specific diagnostic<br />
testing. Equine Infectious Anaemia<br />
(Coggins’ agar gel immunodiffusion<br />
test), autoimmune haemolytic anaemia<br />
(Coombs’ antiglobulin test), Piroplasmosis<br />
(Babesiosis) (complement fixation test),<br />
disseminated intravascular coagulopathy<br />
(DIC) (prolonged prothrombin and activated<br />
partial thromboplastin times) and a variety<br />
of plant and environmental toxins are some<br />
causes of intravascular haemolysis.<br />
Equine anaemia is most commonly<br />
macrocytic (raised McV), reflecting splenic<br />
replacement with juvenile erythrocytes,<br />
as seen with blood loss, infections and<br />
parasitism. Reticulocytes are not commonly<br />
seen in equine blood samples and so<br />
their presence or absence is not a reliable<br />
means of determining regeneration or<br />
non-regeneration, as in other species.<br />
Normocytic (McV within normal range)<br />
anaemia is sometimes seen in horses who<br />
are being challenged by respiratory viruses<br />
but who show no clinical signs. Microcytic<br />
anaemia (low McV) is uncommon but is<br />
sometimes seen in immature individuals<br />
and has been reported in horses with iron/<br />
folate deficiency.<br />
Leucocytes<br />
(WBC & Differential leucocyte count)<br />
Leucocytosis (raised total leucocyte count)<br />
and neutrophilia (raised segmented<br />
neutrophil count) most commonly occurs<br />
in performance horses in association<br />
with septic and non-septic inflammatory<br />
conditions. Septic inflammation is most<br />
commonly associated with bacterial<br />
infection. In performance horses this<br />
may occur following an injury, e.g.<br />
penetrating wounds followed by cellulitis,<br />
septic arthritis or tenosynovitis, upper<br />
respiratory infections and less commonly<br />
14
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
in systemic bacterial infections. Non-septic<br />
inflammation can occur following nonpenetrating<br />
injury, e.g. bruising of soft<br />
tissues, tendons, ligaments or periosteum<br />
and traumatic arthritis or tenosynovitis,<br />
sometimes associated with degenerative<br />
joint disease. Marked leucocytosis is seen<br />
in foals responding to bacterial infections,<br />
notably Rhodococcus equi (‘summer<br />
pneumonia’) and Streptococcus equi<br />
(‘strangles’) infections.<br />
Neutrophilic ‘shifts to the left’ (appearance of<br />
juvenile neutrophils or ‘band’ neutrophils),<br />
while diagnostically helpful in foal-hood<br />
infections, are seldom seen in adult horses<br />
unless severely and acutely infected<br />
with conditions such as acute cellulitis<br />
or lymphangitis. Some cases of acute<br />
salmonellosis, endotoxaemia, peracute<br />
enterocolitis, peritonitis and pleuritis<br />
have neutrophilic shifts to the left, more<br />
commonly associated with leucopenia and<br />
neutropenia.<br />
Leucopenia (low total leucocyte count) and<br />
neutropenia (low segmented neutrophil<br />
count) is most commonly seen in adult<br />
performance horses during the acute phase<br />
of a viral challenge, when there may or<br />
may not be clinical signs. These may<br />
include lethargy, pyrexia, nasal discharge,<br />
coughing and oedematous legs. Leucocytic<br />
changes seen with infection very much<br />
depend upon sampling time in relation<br />
to the stage of the disease process (see<br />
Fig.1).<br />
If the early acute infectious phase has<br />
passed then the leucopenic phase will be<br />
missed and haematologic examinations<br />
will reflect repair and sometimes-secondary<br />
bacterial involvement with leucocytosis and<br />
neutrophilia (see page 14). Therefore, blood<br />
samples should be taken from symptomless<br />
stablemates where viral infections are<br />
suspected, in order to help with diagnosis,<br />
epidemiology and assessment of recovery.<br />
Unfortunately, unless Equine Influenza,<br />
Fig.1: equine blood leucocyte response to viral challenge<br />
14<br />
Circulating blood leucocytes x<br />
10^9/l<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
1 2 3 4 5 6 7 8<br />
Days – Viral challenge starts on day1. Basal leucocyte count is 8 x 10 9 /l<br />
15
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
16<br />
Herpesvirus, Rhinovirus or Adenovirus<br />
infections are involved (for which specific<br />
serologic assays are available), virological<br />
‘screening’ investigations are seldom<br />
rewarding.<br />
Profound leucopenia is seen in neonatal<br />
foals with either bacterial (most commonly<br />
Escherichia coli) or viral (most commonly<br />
Equine Herpesvirus-1) septicaemia and<br />
is an indication for urgent intensive care.<br />
A blood culture should be performed<br />
immediately prior to starting broadspectrum<br />
antibiotic therapy in order to<br />
try to identify the pathogen and clarify<br />
antibiotic sensitivity.<br />
Occasionally, profound leucopenia with<br />
neutropenia and neutrophilic shifts to the<br />
left are seen in adult performance horses<br />
suffering from acute salmonellosis, peracute<br />
enterocolitis, peritonitis and pleuritis or<br />
pleuropneumonia and in newly foaled<br />
mares with toxic metritis/laminitis, most<br />
commonly following placental retention.<br />
Profound leucopenia is always a sign of<br />
severe illness, indicating the need for<br />
intensive care and suggesting a guarded<br />
prognosis.<br />
Lymphocytosis (raised lymphocyte<br />
count) is seen in horses in response<br />
to endogenous catecholamine release<br />
during excitement or exercise. Otherwise,<br />
it is most commonly seen in response to<br />
some chronic viral infections and in more<br />
rarely seen autoimmune diseases. Massive<br />
leucocytosis (sometimes greater than 100<br />
x 10 9 /l) with lymphocytosis is a feature of<br />
generalised lymphoma, in which neoplastic<br />
lymphocytes can be demonstrated in<br />
peripheral blood and sometimes in body<br />
cavity fluid samples and tissue biopsy<br />
samples.<br />
Lymphopenia (low lymphocyte count) is<br />
seen in horses in response to endogenous<br />
glucocorticoid release and in response to<br />
exogenous corticosteroid administration.<br />
Otherwise, it may be seen in acute viral<br />
infections, severe bacterial infections,<br />
septicaemia, endotoxaemia and immune<br />
deficiency conditions. Profound, persistent<br />
leucopenia always carries a poor<br />
prognosis.<br />
Monocytosis (raised monocyte count)<br />
reflects increased phagocytic demand<br />
as may occur with chronic suppurative<br />
conditions with tissue necrosis. In<br />
performance horses, monocytosis is most<br />
commonly seen during the post-acute or<br />
recovery phases following upper respiratory<br />
viral infections.<br />
Eosinophilia (raised eosinophil count)<br />
occurs with antigen-antibody response<br />
in tissues rich in mast cells, e.g. skin,<br />
lung, gastrointestinal tract and uterus<br />
and in parasitically sensitised horses. In<br />
performance horses, low-grade eosinophilia<br />
is most commonly seen in association<br />
with leucopenia or lymphocytosis in<br />
the acute-phase of responses to viral<br />
infections. In horses at pasture, the first<br />
differential diagnosis for eosinophilia is
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
intestinal parasitism and warrants further<br />
investigations with protein electrophoresis<br />
and faecal worm egg counts. Rare cases<br />
of eosinophilic leukaemia have been seen<br />
with eosinophil counts as high as 2.5<br />
x 10 9 /l (25% of differential leucocyte<br />
count).<br />
Basophilia (raised basophil count) is very<br />
uncommon in horses, as are the presence<br />
of basophils themselves. Basophils have<br />
been a feature in cases of hyperlipidaemia<br />
and in some horses that were recovering<br />
from colic.<br />
Platelets<br />
Thrombocytosis (raised platelet count) is<br />
seen uncommonly in adult horses but may<br />
occur in bacterial infections. It may occur<br />
with bacterial infections in foals and has<br />
been associated with Rh. equi infections.<br />
Thrombocytopenia (low platelet count)<br />
may be a reflection of decreased<br />
production, increased usage or from various<br />
spurious factors, e.g. drug administration,<br />
the presence of cold agglutinins in the<br />
sample or platelet clumping in EDTA).<br />
Thrombocytopenia is sometimes seen<br />
in horses with viral infections. Where<br />
pseudothrombocytopenia is suspected,<br />
platelet counts should be measured on two<br />
blood samples collected at the same time,<br />
one into EDTA and the other into sodium<br />
citrate anticoagulants. If the sodium citrate<br />
sample, after correction for dilution, is<br />
considerably higher than the EDTA sample,<br />
EDTA-induced pseudo-thrombocytopenia is<br />
the likely answer. Decreased production<br />
may occur with neoplasia or a toxic insult<br />
to the bone marrow, the latter is diagnosed<br />
by biopsy. Idiopathic thrombocytopenia<br />
is probably an immune-mediated<br />
condition and thrombocytopenia is seen<br />
in horses with disseminated intravascular<br />
coagulopathy (DIC) most commonly a<br />
serious complication of acute enterocolitis.<br />
Haematologic examinations are often used<br />
routinely to screen horses in training for<br />
subclinical disease and can be helpful<br />
when examined on a regular routine basis,<br />
and interpreted carefully. Haematologic<br />
signs of viral infection (leucopenia and<br />
neutropenia or relative lymphocytosis,<br />
depending on stage of sampling), in<br />
a clinically normal horse may suggest<br />
‘challenge’, i.e. the horse’s immune system<br />
is responding but not succumbing to the<br />
infection. In this condition, many horses<br />
do not perform to their best athletic<br />
potential, their recovery after exertion may<br />
be prolonged and they may be more<br />
likely to suffer secondary complications<br />
such as pneumonia, lung abscess, skeletal<br />
and/or cardiac myopathy and/or exerciseinduced<br />
pulmonary haemorrhage<br />
Haematologic examinations, in combination<br />
with inflammatory protein measurements<br />
(see later) are often used to help screen<br />
and monitor the progress of foals and<br />
older horses at studfarms when Rh. equi<br />
infections or Strep. equi epidemics occur.<br />
17
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
In cases of clinical disease, haematologic<br />
variations from 'normality' are often marked<br />
and obvious, but more sophisticated<br />
analytical equipment is required when<br />
screening for less obvious variations and<br />
trends. Modern automated cytochemical<br />
haematology analysers (e.g. Bayer Advia<br />
120) provide accurate differential cell<br />
counts that correlate closely with traditional<br />
manual differential counting techniques.<br />
Their automated differentials are highly<br />
repeatable and are likely to be more<br />
accurate than manual cell counts as they<br />
are performed on 10,000 rather than 100<br />
leucocytes. These analysers provide results<br />
that are more accurate, repeatable and<br />
therefore reliable for the routine monitoring<br />
of performance horses. However, when<br />
required by clinical history or results<br />
obtained, a traditional stained smear is<br />
still required to demonstrate erythrocyte<br />
or leucocyte abnormalities. Red cell<br />
abnormailities include Howell-Jolly bodies<br />
and nucleation, fragmentation, oxidative<br />
damage, spherocytes, basophilic stippling<br />
or Babesia spp. parasites in piroplasmosis.<br />
White cell changes include left shifts, toxic<br />
degeneration, hypersegmentation, neoplastic<br />
change or cytoplasmic inclusions as seen<br />
for example in ehrlichiosis.<br />
NOTES<br />
18
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
clinical chemistry<br />
Proteins<br />
Total protein, albumin and globulin<br />
estimations are useful in the assessment<br />
of general bodily condition and nutritional<br />
status and the response to infectious or<br />
parasitic disease. Electrophoresis helps<br />
determine the significance of raised total<br />
globulin levels. Specific tapeworm ELISA<br />
assays are now available commercially. Low<br />
serum albumin and/or rising globulin levels<br />
are a ‘red flag’ warning, most commonly seen<br />
with cyathostomiasis (hypoalbuminaemia),<br />
large strongylosis (raised beta 1 globulin),<br />
mixed helminthiasis (hypoalbuminaemia<br />
and raised beta 1 globulin), hepatopathy<br />
(hypoalbuminaemia and raised beta 2<br />
globulin), antibody response to infection<br />
(raised gamma globulin) or abscess<br />
formation (raised alpha 2 and gamma<br />
globulins). Globulins can be differentiated<br />
by electrophoresis (Fig.2).<br />
Protein Electrophoresis<br />
Strep. equi infections) will often show<br />
characteristic alpha 2 and gamma globulin<br />
responses. Serum samples should be<br />
used for protein electrophoresis, as raised<br />
fibrinogen levels in heparinised plasma<br />
samples will cause confusing rises in beta<br />
2 globulins (Fig.7).<br />
Occasionally, horses with generalised<br />
lymphosarcoma or plasma call myeloma<br />
have massively increased total protein<br />
and globulin levels, for which protein<br />
electrophoresis shows a massively raised,<br />
discrete, ‘skyrocket’ peak, usually in the<br />
beta 2 globulin range (Fig.8) suggesting<br />
monoclonal lymphoma protein production.<br />
Fig.2: serum protein electrophoresis<br />
normal horse serum<br />
Test : ELECTR Gel 1 – 8 03/01/2002<br />
This identifies elevations in specific globulin<br />
fractions:-<br />
1. Alpha 2 globulin - acute-phase<br />
inflammatory protein responses (Fig.3).<br />
2. Beta 1 globulin - Strongylus vulgaris<br />
and mixed strongyle larval activity (Fig.4).<br />
3. Beta 2 globulin – hepatopathy (Fig.5).<br />
4. Gamma globulin - antibody responses<br />
to bacterial or viral infections (Fig.6).<br />
Horses with abscesses (e.g. Rh. equi and<br />
Fraction Rel% G/L<br />
1 5.0 1.10<br />
2 26.1 5.74<br />
3 20.6 4.53<br />
4 24.9 5.48<br />
5 23.5 5.17<br />
Total G/L 22.00<br />
19
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Fig.3: serum protein electrophoresis<br />
raised alpha 2 globulin<br />
Test : ELECTR Gel 2 – 9 10/01/2002<br />
Fig.3: serum protein electrophoresis<br />
raised alpha 2 globulin<br />
Test : ELECTR Gel 2 – 9 10/01/2002<br />
Fig.4: serum protein electrophoresis<br />
raised alpha 2 and beta 1 globulins<br />
Test : ELECTR Gel 1 – 3 08/02/2002<br />
Fig.4: serum protein electrophoresis<br />
raised alpha 2 and beta 1 globulins<br />
Test : ELECTR Gel 1 – 3 08/02/2002<br />
Fraction Rel% G/L<br />
1 2.8 0.78<br />
2 33.7 13.14<br />
3 16.4 6.40<br />
4 24.5 9.56<br />
Fraction 5 Rel% 23.4 9.13 G/L<br />
Total 1 G/L 39.00 2.8 0.78<br />
2 33.7 13.14<br />
3 16.4 6.40<br />
4 24.5 9.56<br />
5 23.4 9.13<br />
Fig.5: Total G/L serum protein 39.00 electrophoresis<br />
raised beta 2 globulin<br />
Test : ELECTR Gel 1 – 1 01/02/2002<br />
Fig.5: serum protein electrophoresis<br />
raised beta 2 globulin<br />
Test : ELECTR Gel 1 – 1 01/02/2002<br />
Fraction Rel% G/L<br />
1 1.3 0.62<br />
2 24.0 11.52<br />
3 48.2 23.14<br />
4 10.4 4.99<br />
Fraction 5 Rel% 16.2 7.78 G/L<br />
Total 1 G/L 48.00 1.3 0.62<br />
2 24.0 11.52<br />
3 48.2 23.14<br />
4 10.4 4.99<br />
5 16.2 7.78<br />
Fig.6: Total G/L serum protein 48.00 electrophoresis<br />
raised gamma globulin<br />
Test : ELECTR Gel 1 – 2 04/01/2002<br />
Fig.6: serum protein electrophoresis<br />
raised gamma globulin<br />
Test : ELECTR Gel 1 – 2 04/01/2002<br />
Fraction Rel% G/L<br />
1 0.9 0.49<br />
2 17.0 9.18<br />
3 15.2 8.21<br />
4 39.3 21.22<br />
Fraction 5 Rel% 27.6 14.90 G/L<br />
Total 1 G/L 54.00 0.9 0.49<br />
2 17.0 9.18<br />
3 15.2 8.21<br />
4 39.3 21.22<br />
5 27.6 14.90<br />
Total G/L 54.00<br />
Fraction Rel% G/L<br />
1 2.1 0.76<br />
2 18.3 6.59<br />
3 17.5 6.30<br />
4 17.1 6.16<br />
Fraction 5 Rel% 45.1 16.24 G/L<br />
Total 1 G/L 36.00 2.1 0.76<br />
2 18.3 6.59<br />
3 17.5 6.30<br />
4 17.1 6.16<br />
5 45.1 16.24<br />
Total G/L 36.00<br />
20
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Fig.7: serum protein electrophoresis<br />
fibrinogen spike in heparinised plasma<br />
Test : ELECTR Gel 2 – 5 16/05/2002<br />
Fig.8: serum protein electrophoresis<br />
monoclonal beta 2 globulin 'sky rocket'<br />
Test : ELECTR Gel 1 – 8 30/05/2002<br />
Fraction Rel% G/L<br />
1 5.4 2.48<br />
2 19.8 9.11<br />
3 17.5 8.05<br />
4 36.0 16.56<br />
5 21.3 9.8<br />
Total G/L 46.00<br />
Serum Immunoglobulin G (IgG)<br />
As there is no transplacental transfer of<br />
IgG before birth, foals are born essentially<br />
agammaglobulinaemic. During the last few<br />
months of gestation, mares concentrate<br />
IgG in their colostrum. Foals’ intestines are<br />
capable of absorbing IgG for their first 12<br />
hours of life. Providing the mare makes<br />
colostrum of good quality in terms of IgG<br />
concentration, she does not ‘run milk’<br />
before foaling and the foal sucks sufficient<br />
colostrum within the first 12 hours, the foal<br />
acquires good circulating IgG levels and<br />
therefore adequate passive immunity.<br />
Foals should have their serum IgG levels<br />
checked as a routine preventive medicine<br />
policy. Serum samples collected from foals<br />
after 12 hours of age should have IgG<br />
levels of more than 4 g/l and ideally more<br />
than 6 g/l. Levels of less than 2 g/l indicate<br />
failure of transfer of colostral immunity and<br />
levels of 2-4 g/l indicate partial failure.<br />
Fraction Rel% G/L<br />
1 2.1 1.91<br />
2 9.5 8.65<br />
3 9.5 8.65<br />
4 71.2 64.79<br />
5 7.6 6.92<br />
Total G/L 91.00<br />
Foals with levels below 4 g/l are considered<br />
at risk for neonatal infections and should be<br />
transfused with hyperimmune plasma and<br />
their serum IgG levels re-checked 24 hours<br />
later to make sure that IgG levels have risen<br />
to acceptable levels.<br />
Our experience suggests that none of the<br />
currently available ‘stable-side’ foal serum<br />
IgG tests are reliably accurate at the 0-4 g/l<br />
end of the scale and we measure IgG by an<br />
immunospectrophotometric method run on<br />
our autoanalyser.<br />
IgG can be measured in colostrum<br />
immediately after parturition semiquantitatively,<br />
using a refractometer<br />
(Colostrometer) (see table on page 22). If<br />
readings suggest an IgG level of less than<br />
45 g/l, the foal should be considered for<br />
donor colostrum supplementation by bottle<br />
or stomach tube.<br />
21
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Colostrometer reading Concentration IgG g/l Colostrum quality<br />
30% >80 Excellent<br />
Plasma Fibrinogen<br />
This is an acute-phase reactive protein,<br />
which increases in response to inflammation.<br />
Elevations are found in the presence of<br />
tissue damage and this assay may help<br />
with diagnosis and prognosis in cases of<br />
internal abscessation, chronic infectious or<br />
parasitic disease and in cases of exercise<br />
induced pulmonary haemorrhage (EIPH).<br />
The test can be performed on fresh, paired,<br />
non-haemolysed EDTA and serum samples<br />
by subtraction of total serum protein from<br />
plasma protein results, but more accurate<br />
results are obtained from samples collected<br />
into sodium citrate anticoagulant to<br />
measure fibrinogen by direct coagulometric<br />
assay. When measured serially with<br />
serum amyloid A (see right) the kinetics<br />
of the inflammatory response can often<br />
be determined (Fig.9) and this can be<br />
very helpful when monitoring response to<br />
treatment. Fibrinogen is a very useful test<br />
to help diagnose and monitor the response<br />
to treatment for a number of pyogenic<br />
conditions in foals and yearlings, e.g.<br />
Rh. equi and Strep. equi.<br />
Serum Amyloid A (SAA)<br />
This is a highly sensitive, rapidly reacting<br />
inflammatory protein, which can be very<br />
helpful in monitoring early responses to<br />
infection and their response to treatment.<br />
Most normal horses have zero measurable<br />
levels and in the face of acute, particularly<br />
septic inflammation, levels increase quickly<br />
(within 24 hours) to over 20 mg/l and<br />
often more than 100 mg/l. Levels peak<br />
and fall similarly quickly with subsidence<br />
of inflammation when the infection is<br />
controlled (Fig.9). SAA is a very useful<br />
addition to routine neonatal foal ‘profiles’<br />
to help identify those who may have or<br />
may be developing septicaemia and require<br />
antibiotic therapy.<br />
Aspartate Aminotransferase<br />
(AST, AAT, SGOT)<br />
Elevations are seen in the presence of acute<br />
myopathy or hepatopathy. After myopathy,<br />
levels peak at 24-48 hours and return to<br />
baseline by 10-21 days, assuming that no<br />
further damage occurs. This test, taken<br />
with CK at first visit and then 10-14 days<br />
later, can therefore be a useful guide to<br />
recovery from acute myopathy (Fig.10).<br />
22
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Fig.9: schematic diagram showing equine inflammatory protein dynamics<br />
following an inflammatory challenge<br />
Magnitude Magnitude of response of (%) response (%)<br />
100<br />
80<br />
100<br />
60<br />
80<br />
40<br />
60<br />
20<br />
40<br />
20<br />
Fig.9: schematic diagram showing equine inflammatory protein dynamics<br />
following an inflammatory challenge<br />
SAA<br />
Pfib<br />
SAA<br />
Pfib<br />
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21<br />
Days<br />
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21<br />
Days<br />
Fig.10: schematic diagram showing equine serum muscle enzyme levels during<br />
a relatively mild episode of exertional rhabdomyolysis<br />
iu/i<br />
iu/i<br />
3500<br />
3500<br />
2500 3500<br />
2000 3500<br />
1500 2500<br />
1000 2000<br />
1500<br />
Fig.10: schematic diagram showing equine serum muscle enzyme levels during<br />
a relatively mild episode of exertional rhabdomyolysis<br />
CK<br />
AST<br />
CK<br />
AST<br />
1000 0<br />
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15<br />
500<br />
Days<br />
0<br />
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15<br />
Days<br />
23
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Creatine Kinase (CK, CPK)<br />
Elevations are specifically seen in the<br />
presence of acute myopathy. CK isoenzyme<br />
analysis was used in human medicine<br />
to help differentiate cardiac and skeletal<br />
myopathy from brain pathology, but has<br />
never become routinely established in<br />
equine sports medicine. Cardiac troponin<br />
(see page 25) assays are now used to<br />
differentiate skeletal from cardiac myopathy<br />
in horses.<br />
CK levels peak at 6-12 hours and return<br />
to baseline by 3-4 days, assuming that no<br />
further myopathy occurs. When measured<br />
alongside AST (see page 22), which takes<br />
longer to rise, peak and return to normal,<br />
the timing and response to treatment<br />
of myopathy in horses can be usefully<br />
monitored (Fig.10). Paired CK assays<br />
taken before and 2-3 hours after strenuous<br />
exercise, can form a useful diagnostic test<br />
for exercise-induced myopathy, in horses<br />
where the diagnosis may be in doubt. Some<br />
respiratory virus infections, notably Equine<br />
Herpesvirus-1, appear to increase muscle<br />
cell membrane fragility and predispose<br />
to exercise-induced myopathy in horses<br />
in training. This condition is sometimes<br />
associated with clinical signs of fatigue and<br />
stiffness in performance horses.<br />
Significant myopathy, demonstrable by<br />
higher serum CK and AST levels, occurs<br />
more often after exercise in unfit rather<br />
than in fit horses. The conditioning process<br />
protects equine muscle cells from exerciseinduced<br />
injury.<br />
Very high CK levels are seen in young foals<br />
with nutritionally associated myopathy<br />
(‘white muscle disease’) associated with<br />
selenium deficiency.<br />
Lactate Dehydrogenase (LD)<br />
A variety of disease conditions can cause<br />
elevations in total LD and more useful<br />
differentiation can sometimes be provided<br />
by isoenzyme analysis (Fig.11):-<br />
■ LD isoenzyme 1 - most dramatically<br />
increased by intravascular haemolysis<br />
(Fig.12).<br />
Fig.11: serum ld isoenzymes<br />
normal horse<br />
Test : LD Gel 2 – 5 16/01/2002<br />
Fraction Rel% IU/L<br />
LD 1 9.2 46<br />
LD 2 26.6 133<br />
LD 3 41.6 208<br />
LD 4 18.4 92<br />
LD 5 4.2 21<br />
Total IU/L 500 LD1/LD2: 0.35<br />
24
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
■ LD isoenzyme 2 - elevated in some<br />
cases of cardiac pathology, an indication<br />
for cardiac troponin assay (see below)<br />
(Fig.13).<br />
■ LD isoenzyme 3 – no known disease<br />
association in the horse.<br />
■ LD isoenzyme 4 - most commonly<br />
elevated by intestinal pathology (Fig.14).<br />
■ LD isoenzyme 5 - rises seen with<br />
skeletal myopathy and hepatopathy,<br />
requiring further differentiation with CK<br />
(see page 24) and liver enzyme (see<br />
pages 24-28) assays (Fig.15).<br />
Total LD levels are age-dependent to<br />
maturity and reference ranges must be<br />
consulted when interpreting results for<br />
young horses (see pages 56-69).<br />
Cardiac Troponin (cTnI)<br />
Two proteins (tropomyosin and troponin)<br />
working in concert with calcium, regulate<br />
muscle contraction. Troponin is a globular<br />
protein complex composed of three<br />
single chain polypeptide subunits: TnI<br />
(troponin inhibitory component), which<br />
prevents muscle contractions in the<br />
absence of calcium; TnT (tropomyosinbinding<br />
component), which connects<br />
the troponin complex with tropomyosin;<br />
and TnC (calcium binding component),<br />
which binds calcium. The cardiac musclespecific<br />
isoform cTnI (24 kDa) exhibits<br />
approximately 60% homology with the<br />
skeletal isoforms (sTnI) and has a unique<br />
31 amino acid extension of the N-terminus.<br />
Experience in human medicine has shown<br />
that after acute myocardial infarction<br />
(AMI), elevated cTnI levels appear in the<br />
circulation within 3-6 hours. Serum levels<br />
peak within 14-20 hours and return to<br />
normal after 5-7 days. The measurement<br />
of cTnI can therefore be a useful diagnostic<br />
aid for AMI and an aid for the monitoring<br />
of recovery.<br />
Myocardial infarction is rarely diagnosed in<br />
the horse but myocardial necrosis is seen in<br />
conditions such as atypical myoglobinuria.<br />
Myocarditis is sometimes suspected on the<br />
basis of arrhythmias, echocardiographic<br />
abnormalities and/or raised serum lactate<br />
dehydrogenase isoenzyme 2 levels. This<br />
can follow upper respiratory viral infections.<br />
Horses who have suffered in this way will<br />
need more rest and supportive treatment<br />
followed by follow-up to normality before<br />
return to strenuous exercise if potentially<br />
serious complications are to be avoided.<br />
Raised cTnI levels are an indication for<br />
cardiac ultrasound examinations and<br />
ambulatory ECG monitoring.<br />
25
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Fig.12: serum ld isoenzymes<br />
raised ld1<br />
Test : LD Gel 2 – 5 16/01/2002<br />
Fig.12: serum ld isoenzymes<br />
raised ld1<br />
Test : LD Gel 2 – 5 16/01/2002<br />
Fig.13: serum ld isoenzymes<br />
raised ld2<br />
Test : LD Gel 2 – 10 29/06/2002<br />
Fig.13: serum ld isoenzymes<br />
raised ld2<br />
Test : LD Gel 2 – 10 29/06/2002<br />
Fraction Rel% IU/L<br />
LD 1 44.4 316<br />
LD 2 34.1 243<br />
LD 3 16.7 119<br />
Fraction LD 4 Rel% 3.3 IU/L 23<br />
LD 51 44.4 1.5 316 11<br />
Total LD IU/L 2 712 34.1 LD1/LD2: 1.3 243<br />
LD 3 16.7 119<br />
LD 4 3.3 23<br />
LD 5 1.5 11<br />
Total IU/L 712 LD1/LD2: 1.3<br />
Fig.14: serum ld isoenzymes<br />
raised ld<br />
Test : LD Gel 1 – 3 31/07/2002<br />
Fig.14: serum ld isoenzymes<br />
raised ld<br />
Test : LD Gel 1 – 3 31/07/2002<br />
Fraction Rel% IU/L<br />
LD 1 22.0 180<br />
LD 2 39.6 324<br />
LD 3 27.1 221<br />
Fraction LD 4 Rel% 7.6 IU/L 62<br />
LD 51 22.0 3.6 180 29<br />
Total LD IU/L 2 817 39.6 LD1/LD2: 0.56 324<br />
LD 3 27.1 221<br />
LD 4 7.6 62<br />
LD 5 3.6 29<br />
Total IU/L 817 LD1/LD2: 0.56<br />
Fig.15: serum ld isoenzymes<br />
raised ld<br />
Test : LD Gel 1 – 3 10/05/2002<br />
Fig.15: serum ld isoenzymes<br />
raised ld<br />
Test : LD Gel 1 – 3 10/05/2002<br />
Fraction Rel% IU/L<br />
LD 1 4.9 39<br />
LD 2 12.1 96<br />
LD 3 29.4 233<br />
Fraction LD 4 41.4 Rel% 328 IU/L<br />
LD 51 12.2 4.9 97 39<br />
Total LD IU/L 2 792 12.1 LD1/LD2: 0.40 96<br />
LD 3 29.4 233<br />
LD 4 41.4 328<br />
LD 5 12.2 97<br />
Total IU/L 792 LD1/LD2: 0.40<br />
Fraction Rel% IU/L<br />
LD 1 9.3 205<br />
LD 2 12.7 280<br />
LD 3 15.8 348<br />
Fraction LD 4 Rel% 7.3 161 IU/L<br />
LD 51 54.8 9.3 1207 205<br />
Total LD IU/L 2 220312.7 LD1/LD2: 0.73 280<br />
LD 3 15.8 348<br />
LD 4 7.3 161<br />
LD 5 54.8 1207<br />
Total IU/L 2203 LD1/LD2: 0.73<br />
26
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Cardiac troponin (cTnI) levels are measured<br />
in serum samples (lower results may be<br />
found in plasma samples). Clinically<br />
normal horses have serum cTnI levels<br />
of less than 0.2 ng/ml. Experience so<br />
far suggests that greater than 0.3 ng/<br />
ml is abnormal, i.e. suggests myocardial<br />
pathology and 0.2-0.3 ng/ml is currently<br />
a ‘grey’ zone. Levels of 0.9-5.4 ng/ml<br />
have been measured in horses with<br />
ultrasound-confirmed cardiomyopathy.<br />
Nevertheless, results greater than 0.2 ng/<br />
ml are considered ‘red flags’ for expert<br />
cardiological appraisals.<br />
Sorbitol Dehydrogenase (SDH)<br />
This is an enzyme found in the cytoplasm<br />
of hepatocytes and is therefore virtually<br />
liver-specific, although rises are sometimes<br />
seen in horses with skin conditions and<br />
enteropathy. It is useful for the identification<br />
of acute hepatocellular damage for in-house<br />
laboratory conditions, but the enzyme is<br />
highly labile. Therefore, samples must be<br />
handled with care and assays must be<br />
performed within 8-12 hours of sampling<br />
thus SDH assays are unsatisfactory for<br />
transported samples. SDH is not assayed at<br />
our laboratories - the more stable GLDH assay<br />
is now used more frequently than SDH.<br />
Glutamate Dehydrogenase (GLDH)<br />
Elevations are seen in the presence of<br />
acute hepatocellular damage. This is a<br />
mitochondrial enzyme found mainly in<br />
liver, heart muscle and kidney. It is a<br />
relatively stable enzyme and is a suitable<br />
replacement for sorbitol dehydrogenase<br />
(SDH) (see left) in transported samples.<br />
GLDH rises are sometimes seen in horses<br />
with skin conditions and enteropathy.<br />
L-Gamma<br />
Glutamyltransferase (GGT)<br />
GGT is found in cell membranes of<br />
hepatocytes and biliary epithelial cells,<br />
but the enzyme is also found in the<br />
pancreas and kidney. Elevations in serum<br />
levels are seen in the presence of acute<br />
hepatitis, chronic liver cirrhosis and in very<br />
rare cases of pancreatitis. Nephropathy<br />
does not usually result in significantly<br />
raised serum GGT levels so high levels<br />
measured in the horse are usually a sign<br />
of biliary or cholestatic disease. Chronic<br />
pyrrolizidine alkaloid toxicity (ragwort, i.e.<br />
Senecio jacobea poisoning) causes bile<br />
duct hyperplasia and biliary stasis and<br />
therefore typically results in raised serum<br />
GGT and SAP (see below) levels. This<br />
remains an important cause of hepatopathy<br />
in horses and ponies in UK, who ingest<br />
the plant unknowingly in poor-quality hay.<br />
Toxicity is uncommon in well-managed<br />
horses.<br />
Idiopathic GGT elevations are sometimes<br />
seen in horses in training that appear<br />
otherwise healthy, but perform poorly. The<br />
cause of these GGT rises has not yet been<br />
satisfactorily defined although plant and<br />
fungal hepatotoxins have been suspected.<br />
In most cases, other liver enzymes are<br />
27
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
28<br />
within normal range as are urea and<br />
creatinine levels, and liver biopsy reveals<br />
insignificant histopathological findings.<br />
It is therefore not certain that primary<br />
hepatopathy or nephropathy is involved.<br />
Some cases have raised muscle enzyme<br />
levels suggesting an association with<br />
myopathy, either directly or secondarily,<br />
again perhaps via respiratory virus-induced<br />
increased muscle cell membrane fragility.<br />
Most cases respond (GGT levels return<br />
to normal) to a period of reduction in the<br />
training programme.<br />
Urine GGT:creatinine ratios are elevated<br />
(>4.0) in renal tubular pathology.<br />
Alkaline Phosphatase (SAP)<br />
Elevations in this brush border enzyme are<br />
most commonly seen in the presence of<br />
chronic biliary obstructive liver pathology<br />
(e.g. chronic pyrrolizidine alkaloid toxicity).<br />
High levels are also seen with abnormalities<br />
of bone metabolism and intestinal<br />
malfunction, a useful assay in growing<br />
foals and yearlings with clinical signs of<br />
developmental orthopaedic disease, where<br />
SAP results may be very high and will<br />
respond to restricted exercise and mineral,<br />
vitamin and trace element supplementation.<br />
SAP levels are age-dependent to maturity<br />
and appropriate reference ranges must<br />
be consulted when interpreting results for<br />
young horses (see pages 56-69).<br />
Intestinal Phosphatase (IAP)<br />
Elevations in IAP relative to total SAP<br />
are seen in the presence of intestinal<br />
pathology.<br />
References ranges for serum SAP and IAP<br />
levels are very age-related and apparently<br />
high results must be interpreted carefully in<br />
foals, yearlings and immature performance<br />
horses.<br />
Bilirubin<br />
The analysis of bilirubin levels is seldom<br />
useful in the horse but may aid the<br />
classification of anaemia and jaundice<br />
in some cases. Owing to the horse's<br />
unusual biliary excretion system, indirect<br />
(unconjugated) bilirubin levels, may be<br />
higher than those in other species, without<br />
clinical disease, and the significance of<br />
elevations without other abnormalities may<br />
therefore be difficult to interpret. A period of<br />
anorexia, inanition or intestinal malfunction<br />
typically increases indirect bilirubin levels<br />
spuriously.<br />
Bile acids<br />
This is a much better guide to hepatobiliary<br />
status than bilirubin assays. High bile acid<br />
levels occur with embarrassed hepatic<br />
function and are a useful diagnostic and<br />
prognostic liver function and prognostic<br />
guide in horses.<br />
It is important to remember that none<br />
of the liver enzymes, measured singly<br />
or in a profile, give useful information
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
about liver function. The liver has a large<br />
functional reserve and compensatory<br />
capacity. Liver enzyme rises suggest<br />
hepatopathy which can be differentiated<br />
to a degree into acute, chronic, biliary<br />
obstructive or mixed pathology, but bile<br />
acid assays and bromsulphalein clearance<br />
test results reveal either adequate (normal<br />
levels) or impaired (high levels) functional<br />
compensation. Impaired hepatic function<br />
suggests a guarded prognosis. Liver biopsy<br />
and ultrasound examinations are required<br />
to confirm an etiologic diagnosis and to<br />
refine prognosis.<br />
Amylase<br />
Elevations occur in the presence of<br />
pancreatitis, but this condition is rarely<br />
diagnosed in the horse.<br />
Glucose<br />
Other than for oral glucose and xylose<br />
absorption tests, useful for the diagnosis<br />
and evaluation of intestinal malabsorption<br />
cases, the value of this assay in adult<br />
horses is limited to cases of pituitary<br />
pars intermedia dysfunction (equine<br />
Cushing’s syndrome) which are frequently<br />
hyperglycaemic. Measurement of blood<br />
glucose is invaluable in the management of<br />
critically ill foals as profound hypoglycaemia<br />
is often seen in neonatal septicaemia.<br />
Samples for glucose assay must be taken<br />
into fluoride anticoagulant or must reach<br />
the laboratory within hours of collection.<br />
Oral Glucose Absorption Test<br />
The horse to be tested should be fasted<br />
for 18-24 hours. 1 g glucose per kg body<br />
weight is administered by stomach tube.<br />
Blood samples are collected into fluoride<br />
anticoagulant at times 0, 30, 60, 90, 120,<br />
150, 180, 210 and 240 mins. Glucose<br />
levels should peak at double resting (0<br />
mins) levels at 60-120 mins and return to<br />
resting levels by 240 mins.<br />
Cholesterol and Triglycerides<br />
Elevations are seen in the presence<br />
of abnormal lipid metabolism and<br />
hyperlipidaemia. These conditions are<br />
typically seen in the Shetland and other<br />
small ponies, donkeys and occasionally as<br />
a secondary complication in horses that<br />
are anorexic or unable to eat. Pregnant<br />
Shetland pony mares appear particularly<br />
susceptible following a managemental and<br />
nutritional change/challenge.<br />
Urea<br />
Urea is produced in the liver from the<br />
metabolism of ammonia. Elevations are<br />
seen in the presence of abnormal renal<br />
function. Urea levels may also rise in<br />
the haemoconcentrated and ‘over-trained’<br />
horse, associated with fluid balance shifts<br />
rather than renal disease. Many cases<br />
of equine dysautonomia (‘grass sickness’)<br />
have a degree of uraemia but this is<br />
usually caused by catabolism. A period<br />
of anorexia can have a similar result.<br />
29
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
30<br />
Nephrosis and nephritis are important<br />
conditions in neonatal and older foals and<br />
are occasionally seen in other age groups.<br />
Creatinine<br />
Creatinine is formed in muscles from<br />
creatine breakdown and is excreted via<br />
the kidneys. In normal horses, daily<br />
production and excretion are remarkably<br />
constant, leading to its use as an arithmetic<br />
constant for use with urinary fractional<br />
excretion rates (see below). Therefore<br />
serum elevations reflect renal malfunction<br />
(reduced glomerular filtration), levels being<br />
controlled by excretion rate. This may occur<br />
in horses with pre-renal (e.g. circulatory<br />
disturbances, dehydration or shock), renal<br />
(insufficiency) or post-renal conditions.<br />
Measurement of urine specific gravity and<br />
fractional excretion of electrolytes may<br />
help to differentiate pre-renal and renal<br />
azotaemia. When uroperitoneum (postrenal<br />
azotaemia) is suspected it can be<br />
useful to compare peritoneal fluid and<br />
serum creatinine concentrations as a ratio<br />
of greater than 3:1 confirms uroperitoneum.<br />
For both renal and post-renal azotaemia,<br />
ultrasonography can be very helpful.<br />
Urinary Fractional Electrolyte<br />
and Mineral Clearance Ratios<br />
In horses with normal renal tubular<br />
function, urinary excretion rate of creatinine<br />
is almost constant. It can therefore be<br />
used as an arithmetic constant to produce<br />
a measure of the fractional excretion of<br />
electrolytes and minerals in equine urine.<br />
Concentrations of electrolytes or minerals<br />
are measured in serum and urine samples<br />
collected at the same time or at least within<br />
1 hour of one another. Diuretics must not<br />
be used to stimulate urination or spurious<br />
results will be obtained.<br />
The percentage excretion of an electrolyte<br />
is calculated from the following equation:-<br />
Where:<br />
(E)u = Concentration of electrolyte in urine<br />
(E)u (Cr)s<br />
Fractional urinary<br />
X X 100 =<br />
(E)s (Cr)u<br />
excretion (%)<br />
(E)s = Concentration of electrolyte in serum<br />
(Cr)u = Concentration of creatinine in urine<br />
(Cr)s = Concentration of creatinine in serum<br />
Fractional excretion rates for sodium,<br />
potassium, chloride, magnesium, calcium<br />
and phosphate are most commonly<br />
measured. The result provides an<br />
assessment of the horse’s homeostatic<br />
regulatory status for that electrolyte or<br />
mineral, e.g. sodium and chloride may be<br />
selectively excreted at an increased rate<br />
because of excessive dietary salt intake.<br />
Phosphate may be excreted at an increased<br />
rate to try to maintain a normal serum<br />
calcium:phosphate ratio in the face of<br />
inadequate calcium intake. The use of this<br />
method applies only to horses with normal<br />
renal function. Impaired renal tubular<br />
function results in high urine excretion<br />
rates for all the electrolytes and minerals,
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
from failure of retention - in such cases,<br />
creatinine is not a valid arithmetic constant.<br />
Electrolyte imbalance may predispose<br />
exercise-induced myopathy in horses<br />
in training and so fractional clearance<br />
ratios may sometimes be helpful in the<br />
investigation and management of recurrent<br />
cases. Dietary deficiencies, excesses or<br />
imbalances can be corrected and return<br />
to normal excretion rates monitored,<br />
sometimes with useful results in terms of<br />
resolution of myopathy.<br />
In secondary nutritional hyperparathyroidism,<br />
which occurs in horses on a<br />
high phosphate diet, phosphate excretion<br />
rate is high, indicating the need for oral<br />
calcium supplementation and phosphate<br />
reduction, to restore balance. Experience<br />
has shown that in UK, many healthy,<br />
fit, stabled and well performing horses,<br />
receiving high cereal training rations, have<br />
urinary fractional phosphate excretion rates<br />
in excess of 9%, emphasising the need for<br />
calcium supplementation. Higher excretion<br />
rates are seen in horses with clinical<br />
manifestations of secondary nutritional<br />
hyperparathyroidism, which include shifting<br />
lameness, periosteal thickening, facial and<br />
mandibular swelling.<br />
Urinary phosphate clearance ratios are useful<br />
measures of calcium:phosphate balance in<br />
weanlings and yearlings, important for<br />
bone growth and development. Calcium:<br />
phosphate imbalance can predispose to<br />
physitis.<br />
Calcium, Potassium and Chloride<br />
Electrolyte imbalance and fluid loss may<br />
occur with diarrhoea, endotoxaemia,<br />
intestinal crises and exertional exhaustion.<br />
The latter is of particular importance for<br />
endurance horses and for other horses<br />
performing in hot and humid weather<br />
conditions. Serial assays are helpful with<br />
intensive care cases. In other cases,<br />
fractional urinary electrolyte excretion<br />
rates (see page 30) are a much better<br />
assessment than single serum assays.<br />
Electrolyte assays are very important to<br />
the assessment of neonatal foals under<br />
critical care, with specific supplementation,<br />
where indicated and monitoring of return<br />
to normality.<br />
Calcium, Phosphate and Magnesium<br />
Mineral analysis may be helpful in young<br />
horses, i.e. yearlings and two-year-olds<br />
coming into training, with signs suggesting<br />
abnormalities of bone metabolism. As<br />
homeostatic mechanisms are efficient,<br />
serum levels are often normal even in the<br />
face of whole body abnormality, and thus<br />
urinary fractional excretion rates (see page<br />
30) are of greater value.<br />
Hypocalcaemia is a cause of synchronous<br />
diaphragmatic flutter in performance horses<br />
and of uterine inertia in pregnant mares<br />
at full term, requiring cautious corrective<br />
therapy.<br />
31
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
32<br />
Plasma Lactate<br />
A number of hand-held and bench top blood<br />
lactate analysers have been used in horses.<br />
Most have been designed to help assess<br />
the human response to exercise. Results<br />
have been used to describe and predict<br />
aerobic endurance capacity in horses and<br />
it has been suggested that the rate of<br />
decline in blood lactate concentration,<br />
which occurs after exercise, may be a<br />
useful index of fitness. Persistent high<br />
blood lactate concentrations may suggest<br />
metabolic fatigue. Anaerobic capacity is<br />
essential for sprinters and so increases in<br />
blood lactate concentrations for fast, short<br />
distance Thoroughbred flat racehorses may<br />
be an advantage. Successful long distance<br />
endurance racehorses need to be able to<br />
maintain mainly aerobic metabolism (low<br />
blood lactate levels) rather than switching<br />
to increased dependence on anaerobic<br />
metabolism (high blood lactate levels) for<br />
prolonged periods of time.<br />
In horses, high circulating erythrocyte<br />
counts, particularly in response to exercise,<br />
makes measurement of whole blood<br />
lactate levels less accurate, repeatable<br />
and meaningful than plasma lactate levels.<br />
This necessitates deproteinisation and<br />
centrifugation before analysis of plasma<br />
samples, which is much less convenient<br />
than whole blood analyses, which can be<br />
performed for human athletes with instantreading<br />
hand-held machines.<br />
For racehorses, results are uninterpretable<br />
without carefully controlled standard exercise<br />
testing conditions, which are often difficult<br />
to organise, especially under Thoroughbred<br />
racehorse training conditions.<br />
Plasma lactate is also used for monitoring<br />
cardiovascular status in horses receiving<br />
critical care. It has been shown to be a useful<br />
prognostic tool in surgical colic patients<br />
and is particularly helpful in monitoring<br />
circulatory support in compromised foals.<br />
If you wish to assay plasma lactate, please<br />
contact Beaufort Cottage Laboratories for<br />
sample handling guidance.<br />
Therapeutic drug monitoring<br />
Therapeutic drug monitoring (TDM) is<br />
increasingly used in equine medicine and<br />
cardiology and is an invaluable guide to<br />
treatment regimens. The aminoglycosides,<br />
gentimicin and amikacin, have the potential<br />
to cause nephrotoxicity in horses while<br />
under-dosing can lead to treatment failure.<br />
Serum samples are drawn 30 minutes and<br />
8, 12 or 24 (amikacin only) hours later to<br />
identify the peak and trough levels. Peak<br />
levels should be at least 8 times the MIC of<br />
the organism in question (up to 4 for some<br />
gentimicin-sensitive equine pathogens)<br />
whereas a delay in excretion is indicative<br />
of renal tubular dysfunction and should<br />
prompt discontinuation of aminoglycoside<br />
therapy. Several of the drugs that are useful<br />
in equine cardiac patients have a low<br />
therapeutic index. Assays for phenytoin and<br />
digoxin are available for close monitoring for<br />
potential drug toxicity in patients receiving<br />
these drugs.
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
blood gas analysis<br />
Analyses are essential for monitoring<br />
respiratory function under anaesthesia<br />
in cases of neonatal septicaemia or<br />
maladjustment under critical care and<br />
for older horses with respiratory and<br />
intestinal abnormality, where acidosis or<br />
alkalosis are suspected, prior to therapeutic<br />
correction. Analyses are helpful, alongside<br />
fluid and electrolyte balance assessments,<br />
for enterotoxaemia and other criticallyill<br />
horses under intensive care and for<br />
endurance horses and others performing in<br />
hot, humid conditions, suffering exertional<br />
exhaustion and/or heat stress.<br />
Samples must be taken in heparinised,<br />
airtight syringes (preferably glass), and<br />
transported on ice to the laboratory<br />
within an hour or two of collection, so are<br />
practically limited to immediate in-house<br />
testing.<br />
Endocrinology<br />
Pregnancy Tests<br />
Serum gonadotrophins (eCG) may<br />
be detected in mares where functional<br />
endometrial cups are present. For accurate<br />
results, serum samples should be collected<br />
between 45 and 95 days since the last<br />
date of mating. False negative results are<br />
unusual inside this period, but can occur<br />
in rare cases where eCG levels are below<br />
test 'threshold'. False positive tests are more<br />
common and may occur when early foetal<br />
death has left residual functional cups. In<br />
such cases the mare’s serum may remain<br />
eCG positive for the functional life of the<br />
cups, sometimes up to 100 days.<br />
Oestrone sulphate may be detected in the<br />
serum/plasma of mares over 120 days<br />
pregnant. At that time, levels of >100<br />
ng/ml are usually found (0-25 ng/ml in<br />
non-pregnant mares). Most of the oestrone<br />
sulphate peak originates from the foetal<br />
gonads so this may be a useful test of<br />
foetal viability as well as a pregnancy test.<br />
Levels fall during the last few weeks of<br />
pregnancy.<br />
Urinary oestrogens, of placental origin,<br />
may be detected in mares after 150 days<br />
of gestation. Urine samples are required.<br />
In some mares the required fluorescent<br />
response may be unreliable to detect and<br />
the serum oestrone sulphate test is now a<br />
much more reliable test.<br />
Progestagens<br />
The analysis of plasma progesterone levels<br />
is a useful guide to diagnosis and treatment<br />
in the acyclic or irregularly cyclic mare. In<br />
the non-pregnant mare, levels >2 ng/l (6.3<br />
nmol/l) indicate functional luteal tissue<br />
33
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Oestrone sulphate rig test<br />
Normal male Cryptorchid ‘False rig’<br />
Oestrone sulphate 10-50 ng/ml 0.1-10 ng/ml 0-0.02 ng/ml<br />
hCG/testosterone rig test<br />
Testosterone stimulation test should be used for all donkeys and in horses under 3 years old.<br />
Testosterone levels are measured in serum (clotted) or heparinised plasma samples taken before<br />
and then 30-120 minutes after the intravenous injection of 6000 iu hCG.<br />
Normal male Cryptorchid ‘False rig’<br />
Testosterone (1) 5-30 nmol/l 0.3-4.3 nmol/l 0.03-0.15 nmol/l<br />
Testosterone (2) 5-30 nmol/l 1.0-12.9 nmol/l 0.05-0.19 nmol/l<br />
and suggest that prostaglandin treatment<br />
should induce luteolysis, providing that the<br />
corpus luteum is more than 4 days old.<br />
In the pregnant mare, there is no proven<br />
relationship between progesterone levels<br />
and the integrity of pregnancy. Mares with<br />
levels 4 ng/ml but there is considerable daily<br />
and individual variation. The progesterone<br />
assay is in no way an accurate pregnancy<br />
test but may be helpful, or reassuring to<br />
managers, in monitoring individual mares<br />
with histories of repeated pregnancy failure.<br />
Granulosa Cell Tumour (GCT)<br />
The most common ovarian tumour in the<br />
mare is the granulosa cell tumour (GCT).<br />
GCT’s produce steroid hormones which<br />
can be detected in elevated quantities<br />
in the peripheral blood. In cases where<br />
the tumour has a significant theca cell<br />
component (approximately 54% of cases),<br />
serum testosterone is elevated. These<br />
mares are more likely to be aggressive<br />
and stallion like. GCT mares showing<br />
anoestrus or persistent oestrus may have<br />
normal testosterone concentrations. Inhibin<br />
concentrations have been found to be<br />
elevated above normal in approximately<br />
87% of mares with GCT’s, and therefore<br />
inhibin appears to be a more accurate<br />
indicator of the presence of a GCT than<br />
testosterone alone. We recommend<br />
measurement of serum testosterone and<br />
inhibin to support an ultrasonographic<br />
diagnosis of GCT, or in cases in which<br />
rectal palpation is undesirable.<br />
34
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Cryptorchidism<br />
Oestrone sulphate assay may be used as<br />
a cryptorchid or 'rig' test for horses (not<br />
for donkeys) that are over 3 years old (see<br />
table on left).<br />
Thyroid function<br />
Thyroid hormones, i.e. thyroxine (T4) and<br />
tri-iodothyronine (T3) are measured in<br />
equine serum samples. As diurnal rhythms<br />
are involved, two samples should be<br />
collected ideally early in the morning and<br />
late in the afternoon. Low levels (T4 240 nmol/l) in classical cases<br />
(aged, hirsute, polydipsic, polyuric,<br />
glucosuric). However, basal levels are<br />
often within normal range for younger,<br />
developing cases and so TRH stimulation<br />
test, overnight dexamethasone suppression<br />
test or combinations of such tests are<br />
needed to help define pituitary normality<br />
or abnormality.<br />
Insulin<br />
Serum insulin is sometimes a useful<br />
‘screening’ test for equine Cushing’s<br />
syndrome. Results 1000 miu/ml.<br />
Overnight dexamethasone<br />
suppression test<br />
This test is based upon the fact that<br />
dexamethasone administration suppresses<br />
plasma cortisol in normal horses because of<br />
feedback on ACTH release. A resting serum<br />
sample is collected at 5 pm and 40 µg/kg<br />
DXM (Azium, Gist-Brocades, 20 mg/500<br />
kg horse) is injected im. A follow-up serum<br />
sample is collected at 12 pm the following<br />
day. Normal horses show a suppression of<br />
serum cortisol levels to
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
TRH stimulation test<br />
This is considered the safest of the dynamic<br />
cortisol tests with the least risk of inducing<br />
laminitis. Protocol is to collect a baseline<br />
serum sample, inject 1 mg Thyroid Releasing<br />
Hormone (TRH; Roche) iv and then collect<br />
further serum samples at 15 and 60<br />
minutes thereafter. Typical Cushing’s cases<br />
show an increase in cortisol of greater<br />
than 20% (up to 90%) above baseline<br />
at 15 minutes, compared to a rise of<br />
approximately 17% in the normal horse.<br />
Cortisol concentrations return to baseline<br />
values at 60 minutes in the normal horse,<br />
but may remain at around 55% above<br />
baseline in Cushing’s cases.<br />
Combined DXM suppression,<br />
TRH stimulation test<br />
This test has been recently recommended,<br />
although there is dispute about whether<br />
it is more helpful than the overnight<br />
DXM suppression described above. It is<br />
indicated when the results of overnight<br />
DXM suppression or TRH stimulation tests<br />
are inconclusive. A protocol is to collect<br />
a baseline serum sample and then inject<br />
40g/kg DXM iv. A follow-up serum sample<br />
is collected 3 hours later and then 1.0<br />
mg TRH is injected iv. A follow-up serum<br />
sample is collected 30 minutes later and<br />
a final serum sample is collected 24 hours<br />
after the DXM injection. Cushingoid horses<br />
show suppression of serum cortisol level by<br />
3 hours after DXM injection and return to<br />
baseline by 30 minutes after TRH injection<br />
and by 24 hours after DXM injection.<br />
Conclusions are that while typical aged cases<br />
of equine Cushing’s syndrome are easy to<br />
diagnose, often on grounds of clinical signs,<br />
hyperglycaemia and glucosuria, younger,<br />
early and atypical cases are often extremely<br />
difficult to confirm, with marginal clinical<br />
abnormality and often conflicting insulin<br />
and dynamic cortisol testing results. Basal<br />
cortisol and insulin is a useful screening<br />
test in horses grazing at pasture and in<br />
stabled horses providing their samples<br />
are not collected after a feed. The most<br />
practical and probably reliable dynamic test<br />
is currently considered to be the overnight<br />
dexamethasone suppression test.<br />
ACTH stimulation test<br />
This test is primarily used to identify<br />
adrenal insufficiency. In human critical care<br />
it is recognised that many patients with<br />
Systemic Inflammatory Response Syndrome<br />
(SIRS) have adrenal insufficiency and may<br />
benefit from appropriate treatment. Adrenal<br />
insufficiency occurs commonly in premature<br />
foals but its prevalence in adult horses is<br />
unknown. The ACTH stimulation test is NOT<br />
recommended for the diagnosis of equine<br />
pituitary pars intermedia dysfunction where<br />
the combined dexamethasone suppression-<br />
TRH stimulation test is currently considered<br />
the gold standard.<br />
36
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
urine collection & analysis<br />
Urine analysis is useful to help detect renal<br />
or bladder pathology and to investigate<br />
cases of septic nephritis, cystitis or urethritis.<br />
Mid-stream samples should be collected<br />
without the use of diuretics (which alter<br />
urine composition) into a sterile, empty<br />
universal container. Beware of owners<br />
collecting samples into used jam jars or<br />
milk bottles before pouring the urine into<br />
the provided universal container, resulting<br />
in spurious glucosuria and bacterial culture<br />
results. For fractional urinary electrolyte<br />
and mineral clearance ratio measurements<br />
(see page 30), paired urine (not following<br />
diuretic administration) and serum samples<br />
should be collected simultaneously (ideally)<br />
or within one hour of each other.<br />
Urine samples should be examined grossly<br />
for colour and consistency, the presence<br />
of blood (either fresh or changed), pus<br />
or excessive crystalline material. Horse<br />
urine is highly variable in colour from<br />
near colourless to golden or brownish<br />
and in its density, turbidity and mucinous<br />
content. Specific gravity (1.008-1.040<br />
in adult horses, 1.001-1.025 in foals)<br />
should be measured with a refractometer.<br />
Dipsticks are commonly used to measure<br />
pH (normally 7.5-8.5 in adult horses,<br />
5.5-8.0 in foals) and to detect other<br />
abnormalities. Urine pH reflects diet and<br />
horses grazing pasture will normally have<br />
alkaline urine whereas those on a cerealbased<br />
performance-type diet will normally<br />
have slightly acidic urine. Proteinuria<br />
may occur with renal tubular pathology.<br />
Glucosuria may be seen in classical<br />
cushingoid horses and ponies. Haematuria<br />
and sometimes haemoglobinuria may<br />
occur following traumatic injury, or<br />
with renal or cystic calculus formation.<br />
Haemoglobinuria may occur with<br />
haemolytic conditions.Myoglobinuria is<br />
seen with myopathies. Bilirubinuria may<br />
occur with choleliths or other causes of<br />
bile duct obstruction. Ketonuria is rarely<br />
seen in horses. Microscopic examinations<br />
should be used to detect casts (protein<br />
and cellular masses), which suggest renal<br />
tubular pathology, leucocytes, which<br />
suggest inflammation/infection, bacteria,<br />
which if seen following Gram’s stain in<br />
association with leucocytes may indicate<br />
infection and erythrocytes, which indicate<br />
haemorrhage and crystals. Horse urine is<br />
fundamentally a supersaturated solution of<br />
calcium carbonate and will normally contain<br />
variable amounts of predominantly calcium<br />
carbonate crystals. Urolithiasis cases usually<br />
have a degree of proteinuria and haematuria<br />
and may exhibit dysuria. Large amounts<br />
of sabulous material are not necessarily<br />
an indication of abnormality. Further<br />
investigations include bladder and kidney<br />
palpation, ultrasound scan and cystoscopic<br />
examinations, looking for sabulous (bladder)<br />
or discrete calculus formation.<br />
Fractional urinary electrolyte and mineral<br />
clearance ratios (see p30) are significantly<br />
increased in horses with nephropathy, in<br />
particular with renal tubular malfunction.<br />
37
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
parasitology<br />
38<br />
Faeces Collection<br />
Faecal analysis is helpful in providing worm<br />
egg counts to help monitor parasite control<br />
programmes and to investigate cases or<br />
diarrhoea and septic enterocolitis. Freshly<br />
produced or rectal faecal samples should<br />
be collected into an inverted clean rectal<br />
sleeve so that environmental contamination<br />
and alteration is minimised and there is<br />
no doubt about the identity of the horse<br />
that produced the sample. Fluid diarrhoea<br />
samples should be submitted in sterile<br />
universal containers and on sterile swabs<br />
immersed in Amies’ charcoal transport<br />
medium. It is often difficult to collect<br />
diarrhoea samples from foals but digital<br />
stimulation of the rectum sometimes<br />
precipitates production of a sample.<br />
Faecal Worm Egg Counts<br />
These remain the basis of equine intestinal<br />
parasitic surveillance and monitoring of<br />
worm control programmes. They are not<br />
always a reliable means of assessing an<br />
individual horse, for which haematological<br />
and serum protein (albumin and protein<br />
electrophoresis) investigations are more<br />
reliable (see page 19).<br />
Testing methods vary between laboratories.<br />
Our worm egg counts are performed using<br />
the ‘Ovassay’ method, a flotation method<br />
which is particularly suitable for use in<br />
horse samples as it is extremely sensitive<br />
at detecting low numbers of strongyle<br />
and related species eggs. Ascarid and<br />
Strongyloides spp. eggs are also detected.<br />
We believe that other methods (Stoll and<br />
McMaster) are more suitable for counting<br />
worm eggs in samples where high counts<br />
are expected (e.g. farm animals) as these<br />
methods involve dilution rather than<br />
concentration of the eggs into the counting<br />
area. Our experience is that well-managed<br />
horses under good endoparasite control<br />
regimes consistently have zero strongyle<br />
eggs/g of faeces, using the Ovassay<br />
technique. For example, the presence, of<br />
egg laying strongyles in the intestinal lumen<br />
represents the final stage of the protracted<br />
migration of the developing larvae through<br />
the horse’s tissues. Using this method, a<br />
positive worm egg count of any magnitude<br />
in the faeces is a significant finding and<br />
indicates that the horse needs anthelmintic<br />
treatment, the parasite control programme<br />
requires review and the horse would benefit<br />
from a more in-depth haematological and<br />
serum protein appraisal.<br />
Tapeworm segments may sometimes be<br />
seen in the faeces by gross examination<br />
and are often seen in the caecal content<br />
of tapeworm-related intussusception cases<br />
at surgical correction. A serological (ELISA)<br />
test is available for detecting tapeworm<br />
infestations in horses. Titres of 0.6 are considered negative or<br />
low-intensity, moderate and high intensity<br />
infestations, respectively.<br />
Faecal Lungworm Larval Counts<br />
Dictyocaulus arnfieldi larvae may be<br />
detected in fresh rectal-collected faeces<br />
of infested horses using the modified<br />
Baermann funnel gravitation method. A<br />
severe eosinophilic bronchitis may be<br />
detected by cytological examination of<br />
tracheal washes (see page 44).
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
microbiology<br />
Bacteriology<br />
Swabs from any site should be taken into<br />
Amies charcoal transport medium before<br />
transport to the laboratory where they may<br />
be cultured under aerobic, microaerophilic<br />
and/or anaerobic conditions.<br />
Where potential pathogens are isolated,<br />
antibiotic sensitivity tests should be<br />
performed. In acute septicaemias, before<br />
antibiotic treatment has been started,<br />
jugular venous blood samples may be<br />
taken, using sterile techniques, and<br />
inoculated into blood culture media, before<br />
transport to the laboratory.<br />
All genital swabs should be cultured,<br />
unless specifically requested otherwise,<br />
aerobically and microaerophilically.<br />
Aerobic results are available after 24/48<br />
hours culture. Contagious Equine Metritis<br />
(Taylorella equigenitalis) microaerophilic<br />
culture results are available after 7<br />
days incubation, but most specifically<br />
experienced laboratories are able to<br />
culture positive isolates by 3/4 days.<br />
Klebsiella pneumoniae and Pseudomonas<br />
aeruginosa isolates should be confirmed<br />
by biochemical tests and K. pneumoniae<br />
isolates capsule typed for the recognised<br />
K1, K2 or K5 types using the 'Quellung'<br />
or counter current immunoelectrophoretic<br />
methods.<br />
Anaerobic culture may be performed where<br />
indicated, using standard techniques.<br />
Endometrial swabs should be accompanied<br />
by a concurrently sampled endometrial<br />
smear to aid the interpretation of culture<br />
results (see page 46).<br />
In addition to routine aerobic culture,<br />
special methods should be used routinely<br />
to screen rectal swabs and biopsies (in<br />
transport media) and faeces for Salmonella<br />
spp. and Campylobacter spp.<br />
Nasal and pharyngeal swabs,<br />
submandibular and parotid abscess<br />
swabs should be routinely screened<br />
for Streptococcus equi and, in foals,<br />
Rhodococcus equi.<br />
Tracheal wash and bronchoalveolar<br />
lavage (BAL) samples, when submitted<br />
for bacteriological examinations, should<br />
be routinely screened for Streptococcus<br />
pneumoniae, Bordetella bronchiseptica<br />
and Pasteurella spp.<br />
Blood culture medium should be used for,<br />
in addition to blood samples, other body<br />
fluid samples, e.g. peritoneal and pleural<br />
fluids and especially for synovial fluid and<br />
cerebrospinal fluid (CSF) from which it is<br />
often difficult to isolate pathogens.<br />
Skin scrapings<br />
Skin scraping samples are collected from<br />
horses and ponies for the confirmation<br />
of suspected dermatophyte infections or<br />
ectoparasite infestations. Samples should<br />
be collected from fresh skin lesions, from<br />
the edges of the lesions if extensive, using<br />
39
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
a fresh sterile scalpel blade. The hairs<br />
and the scraped skin layers, down to<br />
haemorrhage, should be collected into a<br />
sterile universal container and submitted<br />
for laboratory examination without delay.<br />
The hairs and scraped skin layers should<br />
be incubated for 15 minutes in warm<br />
40% potassium hydroxide (KOH) and then<br />
examined for clear ringworm spores in<br />
broken hair shafts and free whole or<br />
fragmented ectoparasitic mites, including<br />
Sarcoptes, Psoroptes, Chorioptes and<br />
Demodex spp. (differentiated on the basis<br />
of their anatomical appearance).<br />
If negative for dermatophyte spores after<br />
KOH incubation, skin scrapings are<br />
incubated overnight in blue/black ink<br />
and then examined for blue/black stained<br />
spores in clear broken hairs.<br />
Skin scraping samples should be incubated<br />
for bacterial and fungal growth. The latter<br />
(taking up to 3 weeks) will differentiate the<br />
different ringworm-causing dermatophytes,<br />
including Trichophyton and Microsporum<br />
spp.<br />
Microscopic and fungal culture results for<br />
dermatophytes do not always correlate.<br />
Positive microscopic findings but negative<br />
culture results may suggest that the spores<br />
were not viable at the time of scraping.<br />
Negative microscopic findings but positive<br />
culture results may suggest that too few<br />
spores were present in the sample to be<br />
detected in spite of careful examination.<br />
If Dermatophilus congolensis (‘rain scald’<br />
or ‘mud fever’) infection is suspected on<br />
clinical grounds, moist lesions should be<br />
collected and submitted for impression<br />
smear stained with methylene blue to look<br />
for characteristic chains (‘piles of pennies’)<br />
of flattened spores, sometimes in branched<br />
conformation.<br />
clostridial toxin tests<br />
ELISAs to detect the toxins produced<br />
by pathogenic forms of Clostridium<br />
perfringens and Clostridium difficile are<br />
indicated in horses and foals with acute<br />
diarrhoea, particularly where the problem<br />
may be associated with antimicrobial<br />
administration. Faecal samples should be<br />
taken before the drug metronidazole is<br />
given and should be chilled if delivery to<br />
the laboratory is likely to take more than<br />
an hour or two.<br />
Virology<br />
Fluid diarrhoea samples may be examined<br />
by latex particle agglutination for the<br />
presence of Rotavirus antigen.<br />
Specialist virology laboratory facilities and<br />
expertise are required for testing for the<br />
following equine viruses:-<br />
Equine Influenza: paired serum samples<br />
(acute and convalescent phases, collected<br />
14 days apart) are examined for signs<br />
of seroconversion (a four-fold or greater<br />
rise in titres between the acute and<br />
convalescent samples). Nasal discharge or<br />
40
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
nasopharyngeal swabs collected during the<br />
acute phase into viral transport medium are<br />
cultured specifically for the virus. A direct<br />
ELISA test is available for the rapid detection<br />
of the virus in acute-phase nasal discharge<br />
or nasopharyngeal swab samples.<br />
Equine Herpesviruses (EHV-1, EHV-3,<br />
EHV-4): paired serum samples (acute<br />
and convalescent phases, collected 14<br />
days apart) are examined for signs of<br />
seroconversion (significant rise in titres<br />
between the acute and convalescent<br />
samples). Nasal discharge or<br />
nasopharyngeal swabs collected during the<br />
acute phase into viral transport medium are<br />
cultured specifically for EHV-1 and EHV-4.<br />
Aborted foetal, placental and neurological<br />
tissues may be examined for EHV-1 and<br />
EHV-4 DNA by specific polymerase chain<br />
reaction (PCR) test.<br />
Equine Viral Arteritis (EVA): paired serum<br />
samples (acute and convalescent phases,<br />
collected 14 days apart) are examined<br />
for signs of seroconversion (significant<br />
rise in titres between the acute and<br />
convalescent samples). Nasal discharge or<br />
nasopharyngeal swabs collected during the<br />
acute phase into viral transport medium<br />
are cultured specifically for the virus.<br />
Aborted foetal and placental tissues may<br />
be examined for the virus DNA by specific<br />
PCR test.<br />
For the screening of equine aborted foeti<br />
for EHV and EVA infections, please see<br />
postmortem examinations (see page 48).<br />
NOTES<br />
41
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
cytology<br />
Diagnostic cytological examinations are valuable diagnostic<br />
tools following the collection of appropriate and good quality<br />
samples. Safe, reliable and appropriate techniques should be<br />
used to collect either fluid or smear samples.<br />
Fluid samples<br />
These should, in general, be submitted in<br />
sequestrene (EDTA) for a nucleated cell<br />
count, and fixed with a suitable fixative<br />
(e.g. cytospin fixation fluid) for specific<br />
cytological processing. Another undiluted<br />
and unfixed sample should be submitted<br />
in a sterile container or on a sterile swab<br />
in transport medium or ideally in blood<br />
culture medium (particularly for synovial<br />
fluid samples) for concurrent bacterial<br />
culture.<br />
Fluid samples with low total nucleated<br />
cell counts (
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Peritoneal fluid<br />
Analysis of peritoneal fluid is particularly<br />
useful as a diagnostic aid in cases of colic,<br />
weight loss and other suspected abdominal<br />
disease. It may be of particular value in<br />
helping to make the decision for surgical<br />
intervention.<br />
To perform a peritoneal tap, the skin over<br />
the site of puncture should be clipped<br />
and prepared as for surgical intervention.<br />
With the horse restrained in the standing<br />
position, a 19 gauge, 1.5 or 2.0 inch<br />
needle or following local anaesthesia and a<br />
stab incision, a 7.5 cm. blunt teat cannula<br />
(operator preference) is carefully advanced<br />
through the skin at the lowest part of the<br />
abdomen and then through the linea alba.<br />
If fluid is not immediately forthcoming, the<br />
needle may be rotated or the tap may be<br />
repeated at other sites.<br />
In foals, prior ultrasound scan examination<br />
of the abdomen is recommended to<br />
help visualise abnormalities and prevent<br />
inadvertent penetration of the intestine.<br />
Examination of the ventral midline will help<br />
to locate the spleen and to find a ‘pocket’ of<br />
peritoneal fluid to guide productive needle<br />
puncture. Similarly, if fluid is not obtained<br />
in adult horses using the blind technique<br />
described above, ultrasonic guidance may<br />
be helpful.<br />
A turbid and homogeneously blood stained<br />
sample may indicate abdominal vascular<br />
embarrassment. A white, turbid fluid may<br />
suggest peritonitis. A brown, foul smelling<br />
fluid may indicate intestinal rupture or an<br />
intestinal tap. A thick and heavily blood<br />
stained sample suggests a splenic tap.<br />
Total nucleated cell counts
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Synovial fluid<br />
Analysis of Synovial Fluid is useful for the<br />
diagnosis of reactive or septic arthritis in<br />
horses after injury, when a joint becomes<br />
distended, with or without lameness, and to<br />
differentiate septic ('joint-ill') from traumatic<br />
arthritis in foals.<br />
To perform a joint tap, septic techniques<br />
for needle puncture should be used. The<br />
joint to be sampled and its anatomical<br />
relationships govern the site of puncture<br />
and to a degree the techniques used. Total<br />
nucleated cell counts 10 x 10 9 /l, with degenerative and toxic<br />
cytopathological changes.<br />
Tracheal washes or aspirations<br />
These samples can be extremely useful<br />
in confirming and characterising airway<br />
inflammation (leucocytes) in cases of<br />
septic tracheobronchitis and in reactive and<br />
obstructive small airway disease.<br />
Samples can be collected via a suitablelength<br />
sterile endoscope. The endoscope<br />
is passed through the pharynx, larynx and<br />
into the trachea. A long sterile polyethylene<br />
tube is passed down the instrument<br />
channel and accumulated secretions may<br />
be aspirated directly. Alternatively, and<br />
more usually, 50 ml sterile saline may be<br />
injected as quickly as possible and then<br />
aspirated while withdrawing the tube. If<br />
a suitable endoscope is not available, a<br />
sterile polyethylene tube may be passed<br />
down a trochar inserted surgically between<br />
two tracheal rings at the mid lower third<br />
of the cervical trachea. This is clearly a<br />
more invasive technique that may lead<br />
to local wound complications but has the<br />
advantage that there is less likelihood<br />
of contamination of the sample with<br />
commensal bacteria from the oropharynx.<br />
Trans-tracheal aspirates, collected by this<br />
method, are particularly useful in cases<br />
of pleuropneumonia where causative<br />
organisms must be specifically identified to<br />
direct antimicrobial therapy.<br />
Bronchoalveolar lavage<br />
(BAL) samples<br />
BAL samples can be helpful in the<br />
diagnosis of small airway disease. One<br />
must remember that the technique samples<br />
a focal area only and does not help with<br />
the diagnosis of tracheobronchitis. It is<br />
therefore more commonly used in older<br />
horses for the characterisation of reactive<br />
airway obstruction.<br />
Cytological examinations of tracheal<br />
wash or BAL samples may help in the<br />
characterisation of mucous production and<br />
acute and chronic, septic and reactive<br />
(non-septic) inflammatory responses. The<br />
demonstration of significant numbers of<br />
eosinophils in association with signs of septic<br />
bronchitis/bronchiolitis may be a useful<br />
44
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
diagnostic aid for lungworm (Dictyocaulus<br />
arnfieldi) infestation, in horses and ponies<br />
coughing at pasture. Bacterial culture can<br />
be useful in identifying specific pathogens<br />
and guiding antimicrobial therapy.<br />
Cerebrospinal (CSF) samples<br />
CSF samples are most commonly collected<br />
in horses showing neurological signs<br />
for the diagnosis and differentiation of<br />
meningitis or traumatic injury. In horses<br />
imported from countries where equine<br />
protozoal myeloencephalitis occurs and<br />
who develop neurological signs, CSF<br />
analysis is indicated.<br />
For a CSF tap, samples are collected from<br />
the atlanto-occipital space with the horse<br />
restrained in lateral recumbency with the<br />
poll flexed. In foals it may be possible to<br />
perform this under heavy sedation whereas<br />
in adults, general anaesthesia is mandatory.<br />
The skin is clipped and prepared as if for<br />
surgical intervention and a bleb of local<br />
anaesthetic is placed in the midline of the<br />
dorsal neck at a level defined by a line<br />
joining the cranial borders or the atlas,<br />
which may be clearly palpated. A sterile<br />
18 gauge 2 inch needle is then inserted<br />
through the skin at 90° and advanced<br />
until it ‘pops’ through the meninges and<br />
CSF drips or pours from the needle into a<br />
sterile container or is aspirated into a sterile<br />
syringe.<br />
Alternatively, in adult horses, CSF may<br />
be collected via the lumbosacral (LS)<br />
space, by lumbosacral tap. The horse is<br />
restrained, sedated, in stocks. The skin<br />
between the tuber coxae is clipped and<br />
prepared as if for surgical intervention. A<br />
sizeable (3-4 ml) bleb of local anaesthetic<br />
is placed in and under the skin in the<br />
midline at a line bisecting the caudal<br />
borders of the tuber coxae. With the<br />
horse standing ’square’ with weight evenly<br />
distributed on both hind legs, a sterile 18<br />
gauge 6 inch spinal needle with stylette in<br />
place is then inserted though the skin in<br />
the midline at the line bisecting the tuber<br />
coxae and down through the palpable<br />
depression just caudal to the sixth lumbar<br />
spinous process. The horse will often flinch<br />
when the subarachnoid space is penetrated<br />
and this is an indication to start aspiration<br />
into a sterile syringe for a fluid sample.<br />
Gross examination of CSF reveals a clear<br />
almost colourless fluid in normality and<br />
a turbid and/or bloodstained fluid with<br />
meningitis or following traumatic injury.<br />
Laboratory examinations of CSF need to be<br />
able to measure very low total nucleated<br />
cell counts (
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
46<br />
Bone marrow aspirates<br />
These are not commonly collected from<br />
horses - only in cases that may have severe,<br />
undefined anaemia, severe persistent<br />
leucopenia or thrombo-cytopenia and in<br />
some cases of leukaemia.<br />
Samples are most commonly collected<br />
from the wing of the ilium, the ribs or the<br />
sternum. Sternal tap is recommended<br />
because it is most reliably productive.<br />
The ventral midline, under the sternum<br />
is clipped and prepared as if for surgical<br />
intervention. Local anaesthetic is infused<br />
into and under the skin of the ventral<br />
midline, just caudal to the olecranon, with<br />
the horse standing normally, restrained,<br />
sedated, in stocks. A bone marrow<br />
collection needle or an 18 gauge 3.5 inch<br />
spinal needle is introduced through a stab<br />
incision in the skin upwards to contact<br />
the sternum. The needle is then rotated<br />
with upward pressure until it enters the<br />
sternum, the stylette is removed and firm<br />
suction is used to aspirate a sample into a<br />
sterile 10 or 20 ml syringe, pre-treated with<br />
a few drops of 15% tripotassium EDTA to<br />
prevent clotting.<br />
The sample is transferred to EDTA tubes<br />
and labelled for laboratory examination,<br />
without delay. If delay is inevitable, smears<br />
should be made and fixed, to be sent<br />
alongside the wet samples, in case they<br />
are needed.<br />
The cytopathological examination of bone<br />
marrow smears requires specific experience.<br />
Normal and abnormal cell types are classified<br />
and their relative proportions assessed. The<br />
normal equine myeloid:erythroid (M:E) ratio<br />
should be 0.5-1.5.<br />
Semen samples<br />
Semen samples should be collected into<br />
an artificial vagina to allow a meaningful<br />
interpretation. In addition to a full case<br />
history, details of methods of collection, the<br />
colour, consistency, volume and motility of<br />
the ejaculate should be submitted with the<br />
sample. An undiluted semen sample should<br />
be sent in a sterile container for sperm<br />
density and bacteriological examinations,<br />
and a sample diluted immediately 1:1 with<br />
formol citrate solution for sperm live:dead<br />
and morphology examinations.<br />
Smear Samples<br />
Smear samples should, in general, be<br />
submitted already rolled onto a gelatincoated<br />
slide and fixed (‘Smear-fix’, carbowax<br />
or even hair spray) for specific cytological<br />
processing. Another undiluted and unfixed<br />
sample should be submitted in a sterile<br />
container or on a sterile swab in transport<br />
medium for concurrent bacterial culture.<br />
Endometrial smears<br />
Endometrial Smears are simple and quick to<br />
perform and provide a much more accurate<br />
and direct test for the diagnosis of acute<br />
endometritis in mares, pre-coitus than with<br />
swab examinations alone. When used in<br />
conjunction with endometrial swabs for<br />
bacteriological examinations, results are<br />
infinitely more meaningful, interpretable<br />
and therefore valuable. The presence of
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
endometrial epithelial cells is used as a<br />
test of smear quality and the presence or<br />
absence of polymorphonuclear leucocytes<br />
is used as the diagnostic test for acute<br />
endometritis.<br />
Smears may be collected during oestrus<br />
by a variety of methods, but we favour<br />
a simple non-guarded technique. An<br />
extended, sterile, large tipped swab is<br />
passed via a sterile speculum, through<br />
the relaxed cervix and rotated onto the<br />
endometrial lining. The swab is withdrawn<br />
and should be rolled onto gelatine-coated<br />
slides immediately and fixed with 'Smearfix',<br />
carbowax or even hair spray prior to<br />
transport to the laboratory for staining.<br />
Excellent results have been obtained by<br />
rolling smears onto 'Testsimplets' (Boehringer<br />
Mannheim UK Ltd.) pre-stained slides,<br />
then after two to three minutes at room<br />
temperature, washing off the background<br />
blue colour, drying and cover slipping. This<br />
technique provides an excellent permanent<br />
smear sample for immediate reading and/or<br />
for sending for a second opinion.<br />
Histology<br />
Using our state-of-the-art microwave<br />
processing system, same day results can be<br />
provided for most fixed tissue specimens.<br />
In general terms, equine lesions are best<br />
sampled, if possible and appropriate,<br />
by total removal and submission<br />
for histopathological processing and<br />
examination. If total removal is not possible,<br />
samples of representative size and location<br />
should be collected by wedge resection.<br />
Fine needle aspirates should only be<br />
collected if it is not possible to collect<br />
larger samples. Experience suggests that<br />
they often result in a traumatised lesion<br />
without a conclusive diagnosis and with<br />
a recommendation for the collection of a<br />
larger and more representative sample,<br />
delaying resolution. Total lesion removal is<br />
always preferable, if possible.<br />
Removed lesions or biopsies should be<br />
placed immediately into an adequate<br />
volume (10 x sample volume) of 10%<br />
formol saline. Reproductive tissues are<br />
best fixed in Bouin’s fluid because of their<br />
higher water content. Large lesions should<br />
be sectioned before submersion to allow<br />
adequate penetration of fixative. Sectioning<br />
should be performed with a thought to how<br />
the sample will need to be trimmed and<br />
orientated for histopathological processing<br />
to allow the pathologist to make a complete<br />
and meaningful appraisal. When sampling<br />
organs and tissues, we recommend that<br />
samples are taken from adjacent, grossly<br />
normal sites as well as from lesional<br />
sites. Notes of your own postmortem<br />
examination findings should be sent to aid<br />
histopathological interpretations. Samples<br />
should be carefully packed for transport to<br />
avoid leakages and breakages.<br />
47
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
necropsy (postmortem) examinations<br />
48<br />
Full necropsy examinations should be<br />
performed on all adult and younger horses<br />
who die unexpectedly, those who may pose<br />
a risk to in-contact horses, or for whom<br />
confirmation of pathology is required,<br />
and those who are the subject of an<br />
insurance claim. Ideally, the examination<br />
should be performed, without delay, under<br />
conditions of adequate facilities, by suitably<br />
qualified and experienced pathologists,<br />
so that the end result is satisfactory in<br />
terms of answering the questions posed.<br />
Nevertheless, for a variety of reasons, it<br />
may not always be possible for dead horses<br />
to be transported to a specialised equine<br />
pathology facility and examinations may<br />
need to be performed ‘in the field’. Faced<br />
with this need, those responsible should<br />
consider what conditions are required<br />
to enable a productive examination to<br />
be performed. Also, waste and carcase<br />
disposal, prevention of environmental<br />
contamination and spread of infectious<br />
agents to humans and other animals must<br />
be considered. Occasionally, it may be<br />
possible to refer part of a carcase for<br />
specific necropsy investigations, e.g. a foot<br />
or a leg only for orthopaedic examinations<br />
or the head and neck to thoracic vertebra<br />
3 in cases of ataxia for cervical cord<br />
compression examination.<br />
Adult horses<br />
Where full post-mortem facilities, including<br />
hoists and tables are not available,<br />
experience suggests that the horse should<br />
be positioned on the ground in right lateral<br />
recumbency. If an incline is available, the<br />
horse’s back should be positioned up the<br />
hill. The horse should be identified and<br />
an external examination performed and<br />
findings recorded.<br />
The first cut is made deeply under the left<br />
axilla to lay the left front leg upward and<br />
flat back over the horse’s withers. The<br />
second cut is made deeply under the left<br />
groin, aiming caudally towards the anus,<br />
through the left hip joint, to lay the left hind<br />
leg upwards and flat back over the horse’s<br />
pelvis. The abdomen is then opened along<br />
the midline, from xiphisternum to pubis and<br />
the left abdominal wall is laid back over the<br />
horse’s back by cutting up adjacent to the<br />
last rib and up into the groin. The caecum,<br />
large colon and small intestines are then<br />
removed from the abdomen while looking<br />
for signs of displacement or gross pathology.<br />
The small intestines are removed carefully,<br />
examining the cranial mesenteric root for<br />
verminous pathology and the pancreas,<br />
and taking care not to remove the kidneys<br />
and adrenal glands from their attachments<br />
below the spine. The spleen, stomach and<br />
liver are then removed and examined. The<br />
kidneys are then carefully removed for<br />
examination to leave the adrenal glands<br />
attached either side of the aorta. A block
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
of tissue is then removed to include both<br />
adrenal glands and the adjacent aorta,<br />
for overnight fixation, prior to dissecting<br />
out the coeliaco-mesenteric sympathetic<br />
nerve ganglia, which lie between the<br />
adrenal glands and the aorta, but which<br />
are less easy to find in fresh condition.<br />
The bladder and internal genitalia are then<br />
removed and examined. The diaphragm<br />
is then examined and opened to reveal the<br />
thoracic viscera. The ribs are separated<br />
through their costochondral junctions,<br />
the intercostal muscles are cut and the<br />
ribs are broken back over the horse’s<br />
back. The ‘pluck’ including the trachea,<br />
heart and lungs are then removed for<br />
examination. The thymus is examined and<br />
removed in immature horses. The head<br />
is removed through the atlanto-occipital<br />
joint and ideally sectioned longitudinally<br />
with a band saw. The brain, meninges,<br />
guttural pouches, paranasal sinuses, teeth,<br />
pharynx and larynx are then examined<br />
thoroughly. The limb joints are opened<br />
for examination of the synovial fluid and<br />
surfaces. If indicated by the clinical signs,<br />
the neck and back vertebrae are dissected<br />
out and opened for examination of their<br />
articulations and the spinal cord. It is clear<br />
that a satisfactory examination of the head<br />
and spine of an adult horse is difficult to<br />
achieve under field conditions.<br />
Samples for bacterial or viral examination<br />
should be collected from abscesses, areas<br />
of inflammation, body cavities or seared<br />
viscera, using sterile swabs and placed<br />
without delay into Amies’ charcoal or<br />
specific viral transport media.<br />
Fluid samples from abscesses, cysts or<br />
body cavity fluids should be aspirated<br />
with a sterile syringe and then submitted<br />
in sequestrene (EDTA) for a nucleated cell<br />
count, and fixed with a suitable fixative<br />
(e.g. cytospin fixation fluid) for specific<br />
cytological processing. Another undiluted<br />
and unfixed sample should be submitted<br />
in a sterile container or on a sterile swab<br />
in transport medium or ideally into blood<br />
culture medium for concurrent bacterial<br />
culture.<br />
Samples for histopathological processing<br />
and examination should be carefully<br />
selected to provide thin and small, but<br />
representative tissue wedges, and totally<br />
immersed in 10% formol saline. Large<br />
thick samples fail to fix adequately and<br />
histopathological examinations are then<br />
unnecessarily complicated by autolytic<br />
changes, abused tissues may be ruined by<br />
artefactual damage and unrepresentative<br />
samples may not include the primary<br />
pathological changes.<br />
It is often wise to retain appropriate samples,<br />
e.g. gastric and intestinal content, urine and<br />
cubes of liver and kidney, carefully labelled,<br />
frozen, in case toxicological studies are<br />
required at a later date.<br />
49
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
50<br />
Coelioacomesenteric sympathetic<br />
nerve ganglion (CMSNG) sampling<br />
These tissues are specifically required for<br />
the diagnosis of equine dysautonomia<br />
(‘grass sickness’).<br />
In addition to performing a full necropsy<br />
examination (see above) to investigate<br />
other pathological conditions, the CMSNG<br />
require a specific approach to sampling.<br />
With the horse in right lateral recumbency<br />
and the left front and left hind legs cut<br />
back, the abdomen is opened along the<br />
midline, from xiphisternum to pubis and<br />
the left abdominal wall is laid back over the<br />
horse’s back. The caecum, large colon and<br />
small intestines are then removed from the<br />
abdomen. The small intestines are removed<br />
carefully, sectioning the cranial mesenteric<br />
root and taking care not to remove the<br />
kidneys and adrenal glands from their<br />
attachments below the spine. The spleen,<br />
stomach and liver are then removed. The<br />
kidneys are then removed carefully for<br />
examination to leave the adrenal glands<br />
attached either side of the aorta. A block<br />
of tissue is then removed to include both<br />
adrenal glands and the adjacent aorta, for<br />
overnight fixation in an adequate volume of<br />
10% formol saline.<br />
The following day, the tissues are examined<br />
and oriented to identify the two adrenal<br />
glands on the section of aorta. The adrenal<br />
glands are then carefully dissected off<br />
the aorta and the CMSNG are identified,<br />
removed and sectioned transversely and<br />
longitudinally for further fixation prior to<br />
processing. When fixed they appear greycoloured,<br />
solid and clearly neurological,<br />
rather than vascular (tubular on transverse<br />
section) or lymph node-like.<br />
They are<br />
much less easy to find and identify in fresh<br />
unfixed condition.<br />
After further fixation and processing, the<br />
ganglia are examined for the specific<br />
neuronal histopathological degenerative<br />
changes that appear characteristic of<br />
equine dysautonomia.<br />
Neonatal Foals, Foeti and<br />
Placentae<br />
These should be examined to determine<br />
the cause of foetal death and abortion,<br />
specifically looking for signs of EHV or EVA<br />
infections, important infectious causes of<br />
potential epidemic abortion in mares, as<br />
specifically recommended by the Horserace<br />
Betting Levy Board’s Code of Practice.<br />
The carcase and placental membranes<br />
should be examined together to find signs<br />
of foetal/foal, placental and maternal<br />
pathology. The foetus or foal may be<br />
opened in right lateral recumbency in a<br />
manner similar to that described above<br />
for adult horses. Although they may not<br />
be clearly seen in all cases and although<br />
combinations differ in different cases, the<br />
important gross pathological abnormalities<br />
of EHV infection to look for are:-
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
1. A freshly aborted foetus enclosed in<br />
its placental membranes, suggesting<br />
‘explosive’ abortion or a septicaemic<br />
neonate.<br />
2. Jaundiced hooves, mucous membranes<br />
and/or subcutaneous tissues.<br />
3. Excess, jaundiced peritoneal, pleural<br />
and/or pericardial fluids.<br />
4. Jaundiced visceral serosae and gelatinous<br />
jaundiced peri-renal fat.<br />
5. Pleural oedema and pneumonia.<br />
6. Multiple, pale, pinpoint foci visible on<br />
the liver capsule.<br />
The foetus should be weighed, the<br />
crown rump length and the umbilical<br />
cord length measured and recorded. The<br />
placenta should be spread out, checked for<br />
completeness and abnormalities recorded.<br />
Samples for laboratory investigation should<br />
include:-<br />
1. Small but representative slices of liver,<br />
lung, thymus, spleen, adrenal gland and<br />
chorioallantois (horns and posterior pole),<br />
plus any other interesting abnormality,<br />
in carefully packed leak-proof sealed<br />
containers, in an adequate volume<br />
of 10% formol saline for histological<br />
examinations.<br />
3. Swab samples of peritoneal fluid, liver,<br />
lung, heart blood, gastric contents,<br />
the cervical pole of the chorioallantois<br />
and areas of possible placentitis in<br />
Amies charcoal transport medium for<br />
bacteriological examinations.<br />
4. We recommend that small fresh foetal<br />
liver and lung samples are stored at –<br />
20°C (deep-freeze), in case viral isolation<br />
studies are required at a later stage.<br />
In addition, the carcase should be thoroughly<br />
examined for other abnormalities in case an<br />
infectious cause is not involved. Maternal<br />
uterine and placental incompetence often<br />
results in a grossly impoverished foetus.<br />
Umbilical cord vascular embarrassment (an<br />
important cause of equine foetal death and<br />
abortion, often associated with excessive,<br />
i.e. more than 90 cm, cord length) may<br />
be grossly obvious and, if significant, will<br />
be accompanied by signs of foetal vascular<br />
engorgement, haemorrhagic peritoneal and<br />
pleural fluids, congested and autolysed<br />
viscera and meconium staining/foetal<br />
diarrhoea.<br />
Whole carcases and whole placentae to be<br />
referred for necropsy investigations should<br />
be sent to a laboratory that is specifically<br />
experienced with equine neonatal<br />
pathology.<br />
2. Small (0.5 cm) cubes of liver,<br />
lung, thymus, spleen and pieces of<br />
chorioallantois in viral transport medium<br />
for EHV and EVA DNA (PCR) tests.<br />
51
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
biopsy sampling<br />
Skin Biopsy<br />
These are best obtained by full-thickness<br />
wedge incision. While skin punch biopsy<br />
techniques may be simpler to obtain,<br />
they are seldom as rewarding to examine.<br />
Tissues obtained should be fixed<br />
immediately in 10% formol saline.<br />
Lump biopsy<br />
Biopsy is recommended for masses that<br />
appear in or under the skin and sometimes<br />
for deeper masses that may be palpated<br />
or imaged by ultrasound or laparoscopic<br />
examination. If a total lesion resection is<br />
not possible, as is the case for many skin<br />
and subcutaneous masses, representative<br />
biopsies are best obtained by full-thickness<br />
wedge incision, and fixed immediately in<br />
10% formol saline.<br />
Liver Biopsy<br />
Liver biopsy is recommended where serum<br />
biochemical examinations have suggested<br />
hepatic pathology. With the horse restrained<br />
standing, ideally in stocks, the liver on the<br />
right side of the horse is examined with<br />
ultrasound to determine the ideal site<br />
for puncture and to detect signs of gross<br />
pathology, e.g. choleliths or Echinococcus<br />
spp. cysts.<br />
Biopsies are best obtained with a 6' 'Trucut'<br />
biopsy needle inserted between the<br />
14th and 15th ribs, on the right side of the<br />
horse, along a straight line drawn between<br />
the point of the hip and the shoulder,<br />
or elsewhere, if suggested by ultrasound<br />
examination. Specific lesion biopsies are<br />
best obtained by ultrasound guidance. The<br />
tissue sample should be carefully removed<br />
from the needle and fixed in 10% formol<br />
saline. The needle channel should then be<br />
carefully swabbed for bacterial culture.<br />
Lung Biopsy<br />
Lung biopsy may be indicated where there<br />
is clear ultrasonic evidence of pulmonary<br />
pathology. As biopsy of a lung abscess<br />
or focus of infection is contraindicated,<br />
evidence should suggest neoplasia or<br />
focal non-septic pathology before biopsy<br />
is attempted. Pulmonary neoplasia is very<br />
rare in horses so lung biopsy is seldom<br />
indicated.<br />
Needles specifically designed for lung<br />
biopsy should be used and the specific<br />
lesion to be biopsied should be imaged by<br />
ultrasound scan examination. The overlying<br />
intercostal skin site identified, infiltrated<br />
with local anaesthetic and clipped and<br />
prepared as for surgical intervention. With<br />
the transducer coupled in a sterile surgical<br />
glove and sterile coupling gel on its surface,<br />
the lung lesion is imaged and a lung biopsy<br />
device is introduced through the skin and<br />
into the lesion to collect the biopsy.<br />
The tissue sample is fixed in 10% formol<br />
saline without delay and the needle channel<br />
may, if required, be swabbed immediately<br />
for bacterial culture.<br />
52
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Kidney Biopsy<br />
Renal biopsy may be indicated where<br />
there is clinicopathological and ultrasonic<br />
evidence of kidney pathology. The<br />
technique is not without risk of injury<br />
to the horse and therefore should only<br />
be contemplated if clearly indicated and<br />
should only be performed with great care,<br />
using an ultrasound-guided technique.<br />
The right kidney is more easily accessible.<br />
Ultrasound scan examination is used to<br />
identify a suitable site, free from large blood<br />
vessels, in the posterior poles. The horse<br />
should be restrained, sedated in stocks.<br />
The skin over the kidney is clipped for<br />
imaging to identify the site for penetration,<br />
local anaesthesia is induced and the skin is<br />
then prepared as for surgical intervention.<br />
With the transducer coupled in a sterile<br />
surgical glove and sterile coupling gel on<br />
its surface, the kidney is imaged to find the<br />
ideal site for puncture. The biopsy needle is<br />
then introduced through the skin and into<br />
the renal parenchyma, sampling specific<br />
pathological features if visible.<br />
If biopsy of the left kidney is to be<br />
attempted, it is helpful for an assistant to<br />
palpate the kidney per rectum in order to<br />
stabilise it against the body wall, facilitating<br />
the ultrasound-guided biopsy technique.<br />
The tissue sample is fixed in 10% formol<br />
saline without delay and the needle channel<br />
may be swabbed immediately for bacterial<br />
culture.<br />
The horse should be stable-rested for at<br />
least 48 hours after biopsy and should be<br />
monitored for signs of ill health, particularly<br />
associated with renal haemorrhage.<br />
Endometrial Biopsy<br />
Endometrial biopsies are indicated for the<br />
routine investigation of barren mares and<br />
for the investigation of specific endometrial<br />
pathology. Ideally, they are more easily<br />
obtained and interpreted when the mare<br />
is in mid-dioestrus, but samples may be<br />
safely obtained at any stage of the oestrous<br />
cycle from any non-pregnant mare.<br />
Biopsies are obtained with special forceps<br />
(Kruuse UK or Rocket of London Ltd.),<br />
via the vagina and cervix. The mare is<br />
restrained as for routine gynaecological<br />
examinations with her tail bandaged,<br />
rectum evacuated of faeces, tail bandaged<br />
and perineum hygienically prepared. The<br />
mare is re-confirmed not pregnant. The<br />
sterile biopsy forceps are introduced into<br />
the mare’s vagina with a gloved hand, the<br />
cervix is identified (making sure that the<br />
urethral opening has not been accidentally<br />
entered) and the index finger is placed<br />
through the mare’s cervix into the uterine<br />
body. The forceps are then advanced along<br />
the index finger, as a guide, through the<br />
cervix and into the uterine body. The finger<br />
is then ‘hooked’ in the cervix, which may<br />
then be retracted caudally. This straightens<br />
the cervix and the uterine body, allows the<br />
biopsy forceps to fully enter the uterine<br />
body in a cranial direction and prevents<br />
53
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
accidental cervical injury. With the hand<br />
holding the forceps held against the mare’s<br />
buttocks (to avoid injury to the uterus if<br />
the mare moves suddenly) maintaining<br />
the forceps in the uterus, the manipulating<br />
hand and arm are then withdrawn from<br />
the vagina and placed in the rectum. The<br />
forceps are then palpated and advanced<br />
into one or other of the uterine horns. The<br />
jaws of the forceps are then opened and<br />
a fold of endometrium is gently pushed<br />
into the jaws, which are then closed, the<br />
biopsy is completed and the forceps are<br />
withdrawn from the uterus and vagina.<br />
Tissues are carefully removed from the<br />
forceps with fine forceps to avoid artefactual<br />
damage and are fixed immediately in<br />
Bouin's fluid. A fine-tipped sterile swab may<br />
be used to sample the inside of the jaws of<br />
the biopsy instrument for bacterial culture.<br />
Sometimes more than one endometrial<br />
fold is removed and then the smaller one<br />
may be placed into transport medium for<br />
bacterial culture.<br />
Endometrial biopsy samples should be<br />
referred to a laboratory that is specifically<br />
experienced in both equine endometrial<br />
histopathology and equine gynaecology,<br />
in order to receive a meaningful<br />
interpretation.<br />
Testicular Biopsy<br />
Testicular biopsies are best obtained by<br />
conventional wedge resection with the<br />
horse under general anaesthesia in order<br />
to provide adequately interpretable tissues<br />
and to avoid accidental injury to the<br />
testicular artery, by blind needle biopsy,<br />
which may have fatal consequences. The<br />
testicle is examined by ultrasound scan for<br />
visible pathology and best site for sampling<br />
and the scrotum is prepared as for surgical<br />
intervention. Automated punch biopsy and<br />
ultrasound guided techniques are available<br />
but the relatively small tissue samples<br />
are better suited to specific research<br />
requirements. Great care must be taken to<br />
avoid injuring the testicular artery.<br />
Testicular tissues should be fixed<br />
immediately in Bouin's fluid.<br />
Ileal biopsy<br />
Using our state-of-the-art microwave<br />
processing system, same day results can<br />
be provided for fixed tissue specimens.<br />
Ileal biopsies may be indicated to attempt<br />
to confirm or deny a clinical diagnosis of<br />
equine dysautonomia (‘grass sickness’),<br />
where exploratory laparotomy is indicated.<br />
At exploratory laparotomy, a transmural,<br />
i.e. full-thickness, longitudinal ellipse of<br />
ileum, approximately 15mm by up to<br />
10mm is excised at the proximal end of<br />
the ileocaecal fold, midway between the<br />
mesenteric and antimesenteric borders.<br />
The tissue is placed immediately into<br />
10% formol saline and processed for<br />
histopathological examination. The ganglia<br />
in the myenteric plexus between the<br />
54
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
muscular layers are examined for normal<br />
and abnormal neurones. In ‘typical’ cases<br />
of equine dysautonomia, these ganglia are<br />
devoid of normal neurones and appear<br />
‘skeletal’. The occasional degenerate<br />
neurone, with nuclear degeneration and<br />
cytoplasmic vacuolar degenerative changes<br />
are seen in some cases. Also, clusters<br />
or normal neurones are seldom seen in<br />
the submucosal layers and again, the<br />
occasional degenerate neurone, with<br />
nuclear degeneration and cytoplasmic<br />
vacuolar degenerative changes are seen in<br />
some cases.<br />
Ileal biopsies should be referred to a<br />
laboratory that is specifically experienced<br />
with examining these tissues.<br />
Rectal biopsy<br />
Rectal biopsies are useful for the<br />
investigation of weight loss and diarrhoea<br />
cases or where haematological and serum<br />
biochemical results suggest enteropathy.<br />
Samples are best obtained with mare<br />
endometrial biopsy forceps (Yeoman's<br />
basket-jawed), inserted just a hand's length<br />
through the anus. A rectal fold (mucosa<br />
and submucosa only) is removed laterally<br />
on either side (dorsal or ventral biopsies are<br />
more prone to puncture blood vessels and<br />
result in worrying haemorrhage).<br />
One sample is fixed in 10% formol saline<br />
and the other placed into Amies’ charcoal<br />
transport medium for bacteriological<br />
examinations.<br />
NOTES<br />
55
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
reFerence range tables<br />
The data in the following tables are from Beaufort Cottage<br />
Laboratories (www.rossdales.com/laboratory) for:<br />
adult non-Thoroughbred horses<br />
neonatal Thoroughbred foals (24-48 hours old)<br />
older Thoroughbred foals (approximately three weeks old)<br />
yearling Thoroughbred horses<br />
two-year-old Thoroughbred horses in training<br />
three-year-old Thoroughbred horses in training and<br />
adult Thoroughbred horses at stud.<br />
Adult Non-Thoroughbred Horses<br />
56<br />
Test Abbrev. Units Mean Range<br />
Total erythrocytes RBC x10 12 /l 8.2 6.2-10.2<br />
Packed cell volume pcV l/l 0.37 0.31-0.43<br />
Haemoglobin Hb g/dl 13.5 11.1-15.9<br />
Mean cell volume MCV fl 46.0 40.0-50.0<br />
Mean cell haemoglobin. conc. McHc g/dl 36.1 33.5-38.7<br />
Mean cell haemoglobin McH pg 16.6 15.2-19.0<br />
Total leucocytes WBC x10 9 /l 7.5 6.0-10.0<br />
Segmented neutrophils Segs x10 9 /l 4.4 3.4-5.4<br />
Segs % 58 51-65<br />
Lymphocytes Lymphs x10 9 /l 2.6 2.0-3.2<br />
Lymphs % 35 29-41<br />
Monocytes Monos x10 9 /l 0.3 0.2-0.4<br />
Monos % 4 2-6<br />
Eosinophils Eos x10 9 /l 0.2 0-0.4<br />
Eos % 2 1-3<br />
Platelets plts x10 9 /l 156 100-250<br />
Total Protein TSP g/l 63 53-73<br />
Albumin alb g/l 35 29-41<br />
Globulin glob g/l 28 18-38<br />
Alpha 1 globulin α1 glob g/l 1.2 0.4-2.0<br />
Alpha 2 globulin α2 glob g/l 5.8 3.2-8.4<br />
Beta 1 globulin β1 glob g/l 7.4 4.0-10.8<br />
Beta 2 globulin β2 glob g/l 5.3 1.7-8.9<br />
Gamma globulin γ glob g/l 9.0 4.6-13.4<br />
Plasma fibrinogen Fib g/l 2.1 0.3-3.9
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Test Abbrev. Units Mean Range<br />
Serum amyloid A SAA mg/l 1.3 0-20<br />
Aspartate amino transferase AST iu/l 263 102-350<br />
Creatinine kinase ck iu/l 186 110-250<br />
Lactate dehydrogenase LD iu/l 525 225-700<br />
LD isoenzyme 1 LD1 % total LD 14 10-18<br />
LD isoenzyme 2 LD2 % total LD 26 22-30<br />
LD isoenzyme 3 LD3 % total LD 38 34-42<br />
LD isoenzyme 4 LD4 % total LD 18 13-23<br />
LD isoenzyme 5 LD5 % total LD 4 1-7<br />
Gamma glutamyl transferase GGT iu/l 16 1-40<br />
Glutamate dehydrogenase gLDH iu/l 3 1-10<br />
Serum alkaline phosphatase SAP iu/l 204 147-261<br />
Intestinal alk. phosphatase IAP iu/l 47 13-87<br />
iap % total SAP 22.6 10-34<br />
Urea Urea mmol/l 5.2 2.5-10.0<br />
Creatinine creat mmol/l 125 85-165<br />
Glucose glu mmol/l 4.9 4.3-5.5<br />
Total bilirubin TBili mmol/l 20 13-34<br />
Direct bilirubin DBili mmol/l 9 4-16<br />
Bile acids BAcids mmol/l 5.1 1-8.5<br />
Cholesterol chol mmol/l 2.45 2.0-3.3<br />
Triglycerides Trigs mmol/l 0.7 0.2-1.2<br />
Lipase Lip mmol/l 30 8-50<br />
Amylase amyl iu/l 9 3-15<br />
Calcium ca mmol/l 3.1 2.9-3.3<br />
Fractional urinary clearance Ca % 6.2 2.6-15.5<br />
Phosphate pO4 mmol/l 1.4 0.9-1.9<br />
Fractional urinary clearance PO4 % 0.3 0.02-0.53<br />
Magnesium Mg mmol/l 0.8 0.6-1.0<br />
Fractional urinary clearance Mg % 11.7 3.8-21.9<br />
Copper (serum) cu mmol/l 18.2 14.0-22.0<br />
Copper (plasma) cu mmol/l 23.0 18.0-28.0<br />
Zinc Zn mmol/l 12.7 10.0-15.0<br />
Sodium na mmol/l 138 134-142<br />
Fractional urinary clearance Na % 0.09 0.02-1.0<br />
Potassium k mmol/l 4.0 3.0-5.0<br />
Fractional urinary clearance K % 32.8 15-65<br />
Chloride cl mmol/l 99 95-103<br />
Fractional urinary clearance Cl % 0.72 0.04-1.6<br />
Cortisol cort nmol/l 136 71-240<br />
Fasting Insulin ins miu/ml 25.5 8.0-47.5<br />
Tri-iodothyronine T3 nmol/l 1.0 0.48-1.46<br />
Thyroxine T4 nmol/l 22.7 7.7-42.8<br />
Cardiac Troponin cTnI ng/ml 0.1 0.05-0.2<br />
Selenium Se mmol/l 3.0 0.7-8.4<br />
57
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Neonatal Thoroughbred Foals (24-48 hrs old)<br />
58<br />
Test Abbrev. Units Mean Range<br />
Total erythrocytes rBC x10 12 /l 9.4 6.9-11.8<br />
Packed cell volume pcV l/l 0.36 0.30-0.44<br />
Haemoglobin Hb g/dl 13.2 10.2-15.4<br />
Mean cell volume MCV fl 38.8 31.7-44.9<br />
Mean cell haemoglobin. conc. McHc g/dl 36.1 31.7-39.4<br />
Mean cell haemoglobin McH pg 14.0 11.2-16.4<br />
Total leucocytes WBC x10 9 /l 8.8 6.2-12.4<br />
Segmented neutrophils Segs x10 9 /l 6.7 4.1-9.5<br />
Segs % 75 58-85<br />
Lymphocytes Lymphs x10 9 /l 1.8 1.0-3.1<br />
Lymphs % 21 14-37<br />
Monocytes Monos x10 9 /l 0.19 0.1-0.5<br />
Monos % 2 0.5-5<br />
Eosinophils Eos x10 9 /l 0.1 0.1-0.2<br />
Eos % 1 1-2<br />
Platelets plts x10 9 /l 220 140-315<br />
Total Protein TSP g/l 54 41-66<br />
Albumin alb g/l 31 25-35<br />
Globulin glob g/l 24 15-36<br />
Alpha 1 globulin α1 glob g/l 0.9 0.5-1.5<br />
Alpha 2 globulin α2 glob g/l 5.0 4.0-5.6<br />
Beta 1 globulin β1 glob g/l 5.1 3.1-7.2<br />
Beta 2 globulin β2 glob g/l 3.3 1.3-6.0<br />
Gamma globulin γ glob g/l 6.5 4.8-10.1<br />
Immunoglobulin g igG g/l 11.7 6.9-18.6<br />
Plasma fibrinogen Fib g/l 1.9 0.5-3.9<br />
Serum amyloid A SAA mg/l 2.2 0-26<br />
Aspartate amino transferase AST iu/l 157 111-206<br />
Creatinine kinase ck iu/l 414 165-761<br />
Lactate dehydrogenase LD iu/l 860 615-1110<br />
LD isoenzyme 1 LD1 % total LD 5 2-7<br />
LD isoenzyme 2 LD2 % total LD 20 17-24<br />
LD isoenzyme 3 LD3 % total LD 42 36-46<br />
LD isoenzyme 4 LD4 % total LD 28 21-34<br />
LD isoenzyme 5 LD5 % total LD 5 2-10<br />
Gamma glutamyl transferase GGT iu/l 21 10-32
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Test Abbrev. Units Mean Range<br />
Glutamate dehydrogenase gLDH iu/l 25 8-43<br />
Serum alkaline phosphatase SAP iu/l 3341 2424-4544<br />
Intestinal alk. phosphatase IAP iu/l 824 528-1200<br />
iap % total SAP 23.7
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Older Thoroughbred Foals (approx. 3 weeks old)<br />
60<br />
Test Abbrev. Units Mean Range<br />
Total erythrocytes rBC x10 12 /l 10.1 8.8-11.8<br />
Packed cell volume pcV l/l 0.34 0.30-0.38<br />
Haemoglobin Hb g/dl 12.4 10.6-13.6<br />
Mean cell volume MCV fl 34.3 30.6-39.3<br />
Mean cell haemoglobin. conc. McHc g/dl 36.1 34.4-38.9<br />
Mean cell haemoglobin McH pg 12.4 11.1-14.5<br />
Total leucocytes WBC x10 9 /l 9.3 6.9-15.2<br />
Segmented neutrophils Segs x10 9 /l 5.4 4.1-9.1<br />
Segs % 58 42-88<br />
Lymphocytes Lymphs x10 9 /l 3.3 0.9-5.9<br />
Lymphs % 38 22-54<br />
Monocytes Monos x10 9 /l 0.31 0.2-0.6<br />
Monos % 3 1-7<br />
Eosinophils Eos x10 9 /l 0.1 0.1-0.3<br />
Eos % 1 1-3<br />
Platelets plts x10 9 /l 228 133-325<br />
Total Protein TSP g/l 55 42-66<br />
Albumin alb g/l 31 26-37<br />
Globulin glob g/l 24 15-33<br />
Alpha 1 globulin α1 glob g/l 1.1 0.9-1.6<br />
Alpha 2 globulin α2 glob g/l 6.3 4.1-8.9<br />
Beta 1 globulin β1 glob g/l 6.1 4.4-7.3<br />
Beta 2 globulin β2 glob g/l 4.0 2.8-5.8<br />
Gamma globulin γ glob g/l 5.3 4.1-6.8<br />
Plasma fibrinogen Fib g/l 3.0 1.5-4.2<br />
Serum amyloid A SAA mg/l 1.2 0-5.4<br />
Aspartate amino transferase AST iu/l 333 329-337<br />
Creatinine kinase ck iu/l 233 204-263<br />
Lactate dehydrogenase LD iu/l 920 631-1199<br />
LD isoenzyme 1 LD1 % total LD 12 11-13<br />
LD isoenzyme 2 LD2 % total LD 29 27-33<br />
LD isoenzyme 3 LD3 % total LD 40 38-41<br />
LD isoenzyme 4 LD4 % total LD 16 13-18<br />
LD isoenzyme 5 LD5 % total LD 3 2-4
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Test Abbrev. Units Mean Range<br />
Gamma glutamyl transferase GGT iu/l 22 13-30<br />
Glutamate dehydrogenase gLDH iu/l 19 8-31<br />
Serum alkaline phosphatase SAP iu/l 1840 1195-2513<br />
Intestinal alk. phosphatase IAP iu/l 366 260-471<br />
iap % total SAP 20.3 18.7-22.2<br />
Urea Urea mmol/l 3.4 2.8-4.1<br />
Creatinine creat mmol/l 123 97-138<br />
Glucose glu mmol/l 4.2 3.2-6.2<br />
Total bilirubin TBili mmol/l 38 22-54<br />
Direct bilirubin DBili mmol/l 12 5-18<br />
Bile acids BAcids mmol/l 0-8.0<br />
Cholesterol chol mmol/l<br />
Triglycerides Trigs mmol/l<br />
Lipase Lip mmol/l<br />
Amylase amyl iu/l<br />
Calcium ca mmol/l 3.0 2.9-3.1<br />
Fractional urinary clearance Ca %<br />
Phosphate pO4 mmol/l 2.4 2.2-2.7<br />
Fractional urinary clearance PO4 % 0.3 0.02-0.53<br />
Magnesium Mg mmol/l 0.8 0.7-1.0<br />
Fractional urinary clearance Mg %<br />
Copper (serum) cu mmol/l<br />
Copper (plasma) cu mmol/l<br />
Zinc Zn mmol/l<br />
Sodium na mmol/l 141 135-145<br />
Fractional urinary clearance Na %<br />
Potassium k mmol/l 4.8 4.1-5.5<br />
Fractional urinary clearance K %<br />
Chloride cl mmol/l 99 96-102<br />
Fractional urinary clearance Cl %<br />
Cortisol cort nmol/l<br />
Fasting Insulin ins miu/ml<br />
Tri-iodothyronine T3 nmol/l 12.7 0.5-4.2<br />
Thyroxine T4 nmol/l 130 60-320<br />
Cardiac Troponin cTnI ng/ml<br />
Selenium Se mmol/l<br />
61
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Yearling Thoroughbred Horses<br />
62<br />
Test Abbrev. Units Mean Range<br />
Total erythrocytes rBC x10 12 /l 9.5 7.5-11.5<br />
Packed cell volume pcV l/l 0.35 0.30-0.41<br />
Haemoglobin Hb g/dl 12.9 10.0-14.3<br />
Mean cell volume MCV fl 37.0 33.6-40.0<br />
Mean cell haemoglobin. conc. McHc g/dl 36.6 34.5-40.0<br />
Mean cell haemoglobin McH pg 13.5 12.6-15.0<br />
Total leucocytes WBC x10 9 /l 9.5 6.0-15.0<br />
Segmented neutrophils Segs x10 9 /l 4.9 3.7-5.4<br />
Segs % 51 40-53<br />
Lymphocytes Lymphs x10 9 /l 3.9 3.5-4.9<br />
Lymphs % 41 35-49<br />
Monocytes Monos x10 9 /l 0.3 0.2-0.5<br />
Monos % 3 2-5<br />
Eosinophils Eos x10 9 /l 0.2 0.1-1.0<br />
Eos % 2 1-5<br />
Platelets plts x10 9 /l 174 118-243<br />
Total Protein TSP g/l 59 50-70<br />
Albumin alb g/l 32 20-40<br />
Globulin glob g/l 27 20-50<br />
Alpha 1 globulin α1 glob g/l 1.3 0.7-2.0<br />
Alpha 2 globulin α2 glob g/l 7.6 6.0-9.3<br />
Beta 1 globulin β1 glob g/l 6.7 4.8-8.3<br />
Beta 2 globulin β2 glob g/l 5.0 4.3-5.9<br />
Gamma globulin γ glob g/l 7.1 4.6-8.4<br />
Plasma fibrinogen Fib g/l 3.3 2.7-4.4<br />
Serum amyloid A SAA mg/l 1.2 0-10<br />
Aspartate amino transferase AST iu/l 381 323-441<br />
Creatinine kinase ck iu/l 267 190-370<br />
Lactate dehydrogenase LD iu/l 874 476-1200<br />
LD isoenzyme 1 LD1 % total LD 11 5-15<br />
LD isoenzyme 2 LD2 % total LD 25 20-30<br />
LD isoenzyme 3 LD3 % total LD 36 30-44<br />
LD isoenzyme 4 LD4 % total LD 20 12-30<br />
LD isoenzyme 5 LD5 % total LD 5 2-6<br />
Gamma glutamyl transferase GGT iu/l 23 10-30
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Test Abbrev. Units Mean Range<br />
Glutamate dehydrogenase gLDH iu/l 9 7-18<br />
Serum alkaline phosphatase SAP iu/l 611 500-1200<br />
Intestinal alk. phosphatase IAP iu/l 140 100-250<br />
iap % total SAP 23
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Two-Year-Old Thoroughbred Horses in Training<br />
64<br />
Test Abbrev. Units Mean Range<br />
Total erythrocytes rBC x10 12 /l 10.2 8.7-11.7<br />
Packed cell volume pcV l/l 0.40 0.34-0.45<br />
Haemoglobin Hb g/dl 15.0 12.8-16.6<br />
Mean cell volume MCV fl 39.9 37.0-42.1<br />
Mean cell haemoglobin. conc. McHc g/dl 36.8 35.9-37.9<br />
Mean cell haemoglobin McH pg 14.7 13.7-15.7<br />
Total leucocytes WBC x10 9 /l 9.6 7.3-12.7<br />
Segmented neutrophils Segs x10 9 /l 5.1 4.0-6.0<br />
Segs % 53 42-63<br />
Lymphocytes Lymphs x10 9 /l 3.6 2.7-4.4<br />
Lymphs % 38 28-46<br />
Monocytes Monos x10 9 /l 0.4 0.26-0.56<br />
Monos % 4 2-6<br />
Eosinophils Eos x10 9 /l 0.2 0-0.3<br />
Eos % 2 1-3<br />
Platelets plts x10 9 /l 170 127-206<br />
Total Protein TSP g/l 62 59-66<br />
Albumin alb g/l 37 35-39<br />
Globulin glob g/l 25 21-28<br />
Alpha 1 globulin α1 glob g/l 1.1 0.6-1.4<br />
Alpha 2 globulin α2 glob g/l 6.6 5.4-7.8<br />
Beta 1 globulin β1 glob g/l 6.9 5.7-8.5<br />
Beta 2 globulin β2 glob g/l 4.2 1.8-6.8<br />
Gamma globulin γ glob g/l 5.6 3.7-8.2<br />
Plasma fibrinogen Fib g/l 1.9 1.5-2.3<br />
Serum amyloid A SAA mg/l 1.3 0-20<br />
Aspartate amino transferase AST iu/l 545 308-820<br />
Creatinine kinase ck iu/l 354 166-572<br />
Lactate dehydrogenase LD iu/l 793 569-917<br />
LD isoenzyme 1 LD1 % total LD 10 7-12<br />
LD isoenzyme 2 LD2 % total LD 28 24-34<br />
LD isoenzyme 3 LD3 % total LD 40 35-44<br />
LD isoenzyme 4 LD4 % total LD 17 11-23<br />
LD isoenzyme 5 LD5 % total LD 5 1-10<br />
Gamma glutamyl transferase GGT iu/l 24 12-40
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Test Abbrev. Units Mean Range<br />
Glutamate dehydrogenase gLDH iu/l 10 4-11<br />
Serum alkaline phosphatase SAP iu/l 452 293-672<br />
Intestinal alk. phosphatase IAP iu/l 109 64-171<br />
iap % total SAP 23.2
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Three-Year-Old Thoroughbred Horses in Training<br />
66<br />
Test Abbrev. Units Mean Range<br />
Total erythrocytes rBC x10 12 /l 9.7 8.6-10.5<br />
Packed cell volume pcV l/l 0.40 0.35-0.43<br />
Haemoglobin Hb g/dl 14.9 13.0-16.1<br />
Mean cell volume MCV fl 40.7 39.5-43.0<br />
Mean cell haemoglobin. conc. McHc g/dl 37.8 36.6-38.8<br />
Mean cell haemoglobin McH pg 15.4 14.9-16.2<br />
Total leucocytes WBC x10 9 /l 8.2 6.9-9.8<br />
Segmented neutrophils Segs x10 9 /l 4.6 3.9-5.2<br />
Segs % 56 48-64<br />
Lymphocytes Lymphs x10 9 /l 2.8 2.3-3.4<br />
Lymphs % 35 28-42<br />
Monocytes Monos x10 9 /l 0.36 0.2-0.56<br />
Monos % 4 2-6<br />
Eosinophils Eos x10 9 /l 0.1 0-0.2<br />
Eos % 1 1-2<br />
Platelets plts x10 9 /l 170 127-206<br />
Total Protein TSP g/l 62 58-67<br />
Albumin alb g/l 38 35-40<br />
Globulin glob g/l 25 22-29<br />
Alpha 1 globulin α1 glob g/l 1.3 0.9-1.7<br />
Alpha 2 globulin α2 glob g/l 6.3 5.1-7.8<br />
Beta 1 globulin β1 glob g/l 6.7 4.5-8.0<br />
Beta 2 globulin β2 glob g/l 3.3 2.5-5.1<br />
Gamma globulin γ glob g/l 7.0 5.4-9.6<br />
Plasma fibrinogen Fib g/l 1.8 14-2.3<br />
Serum amyloid A SAA mg/l 1.3 0-20<br />
Aspartate amino transferase AST iu/l 467 289-630<br />
Creatinine kinase ck iu/l 390 156-875<br />
Lactate dehydrogenase LD iu/l 638 430-883<br />
LD isoenzyme 1 LD1 % total LD 11 6-17<br />
LD isoenzyme 2 LD2 % total LD 24 19-27<br />
LD isoenzyme 3 LD3 % total LD 39 33-43<br />
LD isoenzyme 4 LD4 % total LD 20 16-23<br />
LD isoenzyme 5 LD5 % total LD 6 1-18
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Test Abbrev. Units Mean Range<br />
Gamma glutamyl transferase GGT iu/l 27 13-47<br />
Glutamate dehydrogenase gLDH iu/l 7 3-12<br />
Serum alkaline phosphatase SAP iu/l 375 277-451<br />
Intestinal alk. phosphatase IAP iu/l 89 65-107<br />
iap % total SAP 22.8
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
Adult Thoroughbred Horses at Stud<br />
68<br />
Test Abbrev. Units Mean Range<br />
Total erythrocytes rBC x10 12 /l 11.5 9.0-14.0<br />
Packed cell volume pcV l/l 0.41 0.35-0.47<br />
Haemoglobin Hb g/dl 14.0 11.1-16.9<br />
Mean cell volume MCV fl 36.0 31.0-41.0<br />
Mean cell haemoglobin. conc. McHc g/dl 34.0 32.0-36.0<br />
Mean cell haemoglobin McH pg 12.1 10.0-14.2<br />
Total leucocytes WBC x10 9 /l 7.1 4.1-10.1<br />
Segmented neutrophils Segs x10 9 /l 3.6 1.4-5.8<br />
Segs % 52 36-68<br />
Lymphocytes Lymphs x10 9 /l 3.0 1.4-4.7<br />
Lymphs % 45 39-61<br />
Monocytes Monos x10 9 /l 0.4 0.36-0.56<br />
Monos % 4 2-6<br />
Eosinophils Eos x10 9 /l 0.2 0-0.5<br />
Eos % 3 0-5<br />
Platelets plts x10 9 /l 170 127-206<br />
Total Protein TSP g/l 70 65-75<br />
Albumin alb g/l 36 34-38<br />
Globulin glob g/l 34 29-39<br />
Alpha 1 globulin α1 glob g/l 1.6 1.1-2.1<br />
Alpha 2 globulin α2 glob g/l 6.9 5.5-7.9<br />
Beta 1 globulin β1 glob g/l 9.2 6.8-11.4<br />
Beta 2 globulin β2 glob g/l 5.5 3.5-7.2<br />
Gamma globulin γ glob g/l 11.3 8.3-14.4<br />
Plasma fibrinogen Fib g/l 2.2 1.5-3.3<br />
Serum amyloid A SAA mg/l 1.3 0-20<br />
Aspartate amino transferase AST iu/l 309 256-369<br />
Creatinine kinase ck iu/l 216 154-270<br />
Lactate dehydrogenase LD iu/l 525 383-664<br />
LD isoenzyme 1 LD1 % total LD 13 10-17<br />
LD isoenzyme 2 LD2 % total LD 30 24-37<br />
LD isoenzyme 3 LD3 % total LD 43 38-49<br />
LD isoenzyme 4 LD4 % total LD 13 9-18<br />
LD isoenzyme 5 LD5 % total LD 2 1-3
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
Test Abbrev. Units Mean Range<br />
Gamma glutamyl transferase GGT iu/l 20 14-28<br />
Glutamate dehydrogenase gLDH iu/l 8 4-14<br />
Serum alkaline phosphatase SAP iu/l 403 286-571<br />
Intestinal alk. phosphatase IAP iu/l 103 77-157<br />
iap % total SAP 24.3
T h e B e a u f o r t c o t t a g e l a b o r a t o r i e s<br />
NOTES<br />
Copies of the Reference Range Tables can be downloaded (as pdf files) from our website:<br />
www.rossdales.com/laboratory<br />
While we have made every endeavor to ensure the accuracy of information in this Guide, <strong>Rossdale</strong> &<br />
<strong>Partners</strong> cannot be held liable for any inaccuries which may inadvertently occur.<br />
70
G u i d e t o e q u i n e c l i n i c a l p a t h o l o g y<br />
The aim of this Guide is to help equine practitioners use<br />
clinical pathological aids to diagnosis to good effect, to provide<br />
‘normal’ reference ranges for horses of different ages and<br />
types, and to give advice for the safe and satisfactory collection<br />
and handling of samples for laboratory investigation.<br />
The Guide was produced by Sidney W. Ricketts, LVO, BSc,BVSc,<br />
DESM, DipECEIM, FRCPath, FRCVS<br />
with the help of<br />
Annalisa Barrelet, BVetMed, MS, CertESM, MRCVS<br />
Celia M.Marr, BVMS, MVM, PhD, DEIM, DipECEIM, MRCVS<br />
Sarah S.Stoneham, BVSc, CertESM, MRCVS<br />
Katherine E. Whitwell, BVSc, DiplECVP, FRCVS<br />
Robert S.G.Cash BSc, FIBiol<br />
Mary Ashpole.<br />
© 2006 <strong>Rossdale</strong> & <strong>Partners</strong><br />
Sidney Ricketts
Beaufort Cottage laboratories<br />
High Street, Newmarket, Suffolk CB8 8JS<br />
Tel +44 (0)1638 663017 Fax +44 (0)1638 560780<br />
Email bcl@rossdales.com<br />
www.rossdales.com