2009 Drug Trend Insights - Prime Therapeutics
2009 Drug Trend Insights - Prime Therapeutics
2009 Drug Trend Insights - Prime Therapeutics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
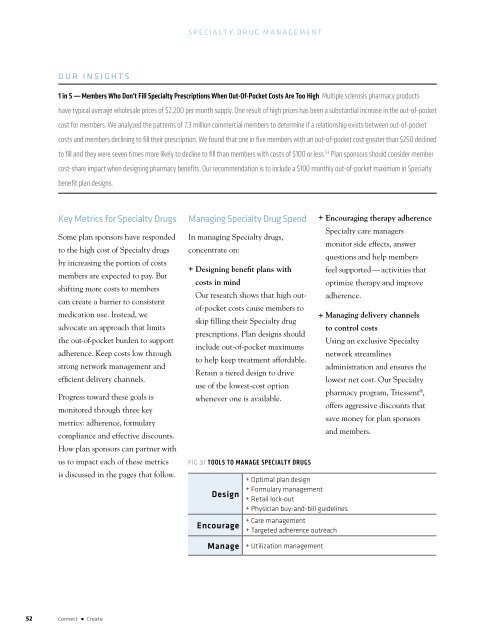
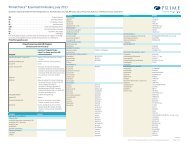
Specialty <strong>Drug</strong> ManagementOUR INSIGHTS1 in 5 — Members Who Don’t Fill Specialty Prescriptions When Out-Of-Pocket Costs Are Too High Multiple sclerosis pharmacy productshave typical average wholesale prices of $2,200 per month supply. One result of high prices has been a substantial increase in the out-of-pocketcost for members. We analyzed the patterns of 7.3 million commercial members to determine if a relationship exists between out-of-pocketcosts and members declining to fill their prescription. We found that one in five members with an out-of-pocket cost greater than $250 declinedto fill and they were seven times more likely to decline to fill than members with costs of $100 or less. 53 Plan sponsors should consider membercost-share impact when designing pharmacy benefits. Our recommendation is to include a $100 monthly out-of-pocket maximum in Specialtybenefit plan designs.Key Metrics for Specialty <strong>Drug</strong>sSome plan sponsors have respondedto the high cost of Specialty drugsby increasing the portion of costsmembers are expected to pay. Butshifting more costs to memberscan create a barrier to consistentmedication use. Instead, weadvocate an approach that limitsthe out-of-pocket burden to supportadherence. Keep costs low throughstrong network management andefficient delivery channels.Progress toward these goals ismonitored through three keymetrics: adherence, formularycompliance and effective discounts.How plan sponsors can partner withus to impact each of these metricsis discussed in the pages that follow.Managing Specialty <strong>Drug</strong> SpendIn managing Specialty drugs,concentrate on:+ Designing benefit plans withcosts in mindOur research shows that high outof-pocketcosts cause members toskip filling their Specialty drugprescriptions. Plan designs shouldinclude out-of-pocket maximumsto help keep treatment affordable.Retain a tiered design to driveuse of the lowest-cost optionwhenever one is available.Fig 31 Tools to manage specialty drugsDesignEncourage+ Optimal plan design+ Formulary management+ Retail lock-out+ Physician buy-and-bill guidelines+ Care management+ Targeted adherence outreach+ Encouraging therapy adherenceSpecialty care managersmonitor side effects, answerquestions and help membersfeel supported — activities thatoptimize therapy and improveadherence.+ Managing delivery channelsto control costsUsing an exclusive Specialtynetwork streamlinesadministration and ensures thelowest net cost. Our Specialtypharmacy program, Triessent ® ,offers aggressive discounts thatsave money for plan sponsorsand members.Manage+ Utilization management52 Connect ● Create