December 2011 - Prime Therapeutics
December 2011 - Prime Therapeutics
December 2011 - Prime Therapeutics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Prime</strong> Perspective | November <strong>2011</strong>Medicare News cont'dDispensing the Accurate Medication is EssentialCMS guidance establishes many requirements with respectto medication errors. The following are common types ofbilling errors:→ → Incorrect drug dispensed→ → Incorrect strength of drug dispensed→ → Drug dispensed to incorrect Covered Persons→ → Incorrect information on the prescription labelBilling errors can result in harm to Covered Persons as well asadditional hardship at the Participating Pharmacy. These errorscan cause confusion for Covered Persons when dispensingprescriptions at Participating Pharmacies.When dispensing prescriptions, <strong>Prime</strong> requires all ParticipatingPharmacies and staff to double check the Covered Person’sname, ID number, date of birth (DOB), phone number(s),address(es) and medication(s).This will help to improve the accuracy of dispensed prescriptions,reduce medication errors, adverse drug interactions, and helpimprove overall medication use.Uniform Exceptions and AppealsEffective January 1, 2012, CMS requires all Medicare Part Dbenefit sponsors to use a single uniform exceptions and appealsprocess with respect to the determination of prescription drugcoverage for a Covered Person under the plan. <strong>Prime</strong> will beimplementing the following reject messages to the ParticipatingPharmacy to comply with the final rule:→ → NCPDP Reject Code 569: “Notice of Appeal Rights”→ → Secondary messaging: “Provide Beneficiary withCMS Notice of Appeal Rights”CMS Notice of Appeal Rights will be posted on <strong>Prime</strong>’s websiteat <strong>Prime</strong><strong>Therapeutics</strong>.com > Pharmacists > Medicare Part D> Medicare Resources > More > Additional Links > MedicareCoverage & RightsCMS Prescription Drug Event ChangesFor Medicare Part D claims that are processed or reprocessed,a record is sent to CMS. This record is called a Prescription DrugEvent (PDE). CMS will no longer accept PDE records that are sentfor dates of service between 2006 and 2007. <strong>Prime</strong> will also nolonger reprocess any claims for dates of service between 2006and 2007.CMS has established a 37-month window for submitting PDErecords; the window begins each year on January 31. EffectiveJanuary 31, 2012, CMS will reject PDE records with dates ofservice before 2008. <strong>Prime</strong> will also no longer reprocess anyclaims for dates of service before 2008 effective January 31, 2012.© <strong>Prime</strong> <strong>Therapeutics</strong> LLC5
<strong>Prime</strong> Perspective | November <strong>2011</strong>Kansas News cont'dEffective January 1, 2012, brand doxycycline and minocycline drugswill be excluded from coverage. The PA process is not available forcoverage of these products:Adoxa (doxycycline monohydrate tablet, capsule)Alodox (doxycycline hyclate tablet plus cleanser)Avidoxy (doxycycline monohydrate tablet)Avidoxy DK (doxycycline monohydrate tablet plus wash,sunscreen)Doryx (doxycycline hyclate delayed-release tablet)Monodox (doxycycline monohydrate capsule)Morgidox Kit (doxycycline hyclate capsule plus cleanser)Ocudox Kit (doxycycline hyclate capsule plus cleanser, spray)Oracea (doxycycline monohydrate delayed-release capsule)Oraxyl (doxycycline hyclate capsule)Periostat (doxycycline hyclate tablet)Vibramycin (doxycycline capsule, suspension, syrup)Vibra-Tab (doxycycline hyclate tablet)Dynacin (minocycline capsule, tablet)Minocin (minocycline capsule)Minocin Kit (minocycline capsule plus acne care products)Solodyn (minocycline extended-release tablet)Texas NewsBlue Cross and Blue Shield of Texas UtilizationManagement ProgramsBlue Cross and Blue Shield of TexasNew Generics Plus FormularyEffective January 1, 2012, Blue Cross and Blue Shield of Texas willbe offering an additional formulary. The new formulary, GenericsPlus (Preferred Drug List 2), emphasizes the use of generic drugsthrough inclusion of all clinically approved generic drugs, plusa select number of brand-name drugs. The Generics Plus druglist can be viewed at www. bcbstx.com. Covered Persons withquestions about the new drug list should be instructed to callthe number on the back of their ID card for further information.Blue Cross and Blue Shield of Texas to Exclude Coveragefor Repackager NDC’sEffective January 1, 2012, Blue Cross and Blue Shield of Texas willno longer cover repackager NDC numbers under the pharmacybenefit. Participating Pharmacies submitting claims for repackagerNDC numbers should resubmit and dispense the Original ProductManufacturer’s NDC on all claims.If a repackager claim is submitted, it will reject with the followingpoint-of-sale rejection messages:→→NCPDP Reject Code 70: “Prod/Service Not Covered”→→Secondary Message: “Repackager Not CoveredEffective January 1, 2012, Blue Cross and Blue Shield of Texas willimplement the following utilization management programs for fullyinsured Covered Persons and self-insured groups:→→Prior authorization: Doxycycline/Minocycline, AndrogenAnabolic Steroid, Antifungal, Erectile Dysfunction, OralFentanyl, Pradaxa, Provigil/Nuvigil, Adcirca/Revatio, Ampyra,Arcalyst/Ilaris, ESA, Forteo, Growth Hormone, Egrifta, HepB&C, ITP, Kuvan, Oral Oncology, Xenazine, Xolair, and Xyrem→→Step therapy: Byetta/Victoza, Lipid Management,COX-2/Vimovo, Depression, Glucose Test Strips, ProtonPump Inhibitors, Infertility, Letairis, Multiple Sclerosis,and Rheumatoid Arthritis/Psoriasis→→Several new quantity limits will be added, pay extra attentionto the point-of-sale messaging for adjustments to day-supplyneeded or refill too soon rejection.© <strong>Prime</strong> <strong>Therapeutics</strong> LLC7
New Plan AnnouncementHormel FoodsEffective January 1, 2012Effective January 1, 2012, <strong>Prime</strong> <strong>Therapeutics</strong> will begin processingCommercial claims for approximately 22,000 Covered Persons forHormel Foods. Covered Persons will use the <strong>Prime</strong> <strong>Therapeutics</strong>Select Network and <strong>Prime</strong> Choice Plus Formulary.Processing RequirementsTo ensure uninterrupted service to Participating Pharmacies andCovered Persons, please use the following information to set upyour system prior to January 1, 2012, for processing all new andrefill claims for Covered Persons of Hormel Foods.BIN:........................................610455PCN:.......................................HORMEL (new)Covered Person ID Number(Covered Persons will receive new ID card)For all <strong>2011</strong> Outstanding Claims Reversals and Processing→→Participating Pharmacies should complete all Commercialclaims reversals and processing by close of business<strong>December</strong> 31, <strong>2011</strong>→→For assistance with claims that have a date of fill prior toJanuary 1, 2012, please contact Innoviant at 877.559.2955For More Information→→<strong>Prime</strong>’s payer specification sheets may be found at:<strong>Prime</strong><strong>Therapeutics</strong>.com > Pharmacists > D.0/Version 5010Pharmacy Information > D.0 Payer Sheets→→Effective January 1, 2012, if you have questions regardingclaims processing, please contact <strong>Prime</strong>’s Contact Centerat 855.457.0002Date of BirthGenderPerson CodeU&CDays SupplyPharmacy NPIPrescriber ID (NPI or DEA)Featured below are examples of the new ID cards for CoveredPersons of Hormel Foods:8 © <strong>Prime</strong> <strong>Therapeutics</strong> LLC
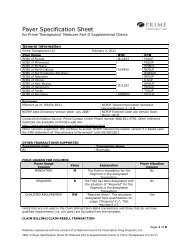
New Plan AnnouncementBlue Cross Blue Shield of Arizona Medicare Part DEffective January 1, 2012Effective January 1, 2012, <strong>Prime</strong> <strong>Therapeutics</strong> will begin processingMedicare Part D claims for Covered Persons of Blue CrossBlue Shield of Arizona (BCBSAZ) Blue MedicareRx (PDP).Processing RequirementsTo ensure uninterrupted service to Participating Pharmacies andCovered Persons, please use the following information to set upsystems prior to January 1, 2012.BCBSAZ PDP IndividualBIN:........................................610455PCN:.......................................PDPAZBCBSAZ PDP Employer GroupBIN:........................................610455PCN:.......................................PDGAZCovered Person ID Number<strong>2011</strong> Outstanding Claims Reversals and Processing→→Participating Pharmacies should complete all claims processingand reversals by close of business <strong>December</strong> 31, <strong>2011</strong>→→Medicare Part D claims with a fill date after January 1, 2012must be submitted with the BIN/PCN outlined aboveFor More Information→→For <strong>Prime</strong>’s helpful resources for Medicare Part D coverageand issues, please visit: <strong>Prime</strong><strong>Therapeutics</strong>.com > Pharmacists> Medicare Part D > Medicare Resources > Helpful Resources→→<strong>Prime</strong>’s Medicare Part D PDP and MA-PD payer specificationsheet is available at: <strong>Prime</strong><strong>Therapeutics</strong>.com > Pharmacists >D.0/Version 5010 Pharmacy Information > D.0 Payer Sheets→→If you have questions regarding claims processing,please contact <strong>Prime</strong>’s Contact Center at 877.878.8668Date of BirthGenderGroup NumberPerson CodeU&CDays SupplyPharmacy NPIPrescriber ID (NPI or DEA only; UPIN when allowed)Date Rx WrittenPrescription Origin CodeFeatured below are examples of the most common ID cardsused for BCBSAZ Individual Blue MedicareRx:10 © <strong>Prime</strong> <strong>Therapeutics</strong> LLC
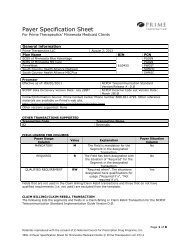
<strong>Prime</strong> Perspective | November <strong>2011</strong><strong>Prime</strong> NewsNCPDP Version D.0 Claim Submission RequirementsEffective January 1, 2012 pharmacies are required to submit claimsto <strong>Prime</strong> in the D.0 format. <strong>Prime</strong> recommends ParticipatingPharmacies convert to the D.0 format before January 1, 2012.In order for <strong>Prime</strong> to assess the networks’ readiness, Pharmaciesmust attest to their ability to submit D.0 claims beginningJanuary 1, 2012. Effective March 31, 2012 <strong>Prime</strong> will only acceptclaims submitted in the D.0 format.For more information regarding the CMS statement released onNovember 17, <strong>2011</strong> go to the following link: https://www.cms.gov/ICD10/Downloads/CMSStatement5010EnforcementDiscretion111711.pdfConvert to the D.0 Format to Prevent Covered Person DisruptionTo prevent disruption for the Covered Person, if a ParticipatingPharmacy is not compliant with the D.0 format by March 31, 2012,<strong>Prime</strong> will send a communication to Covered Persons advising theutilization of alternate Participating Pharmacies.→→Payer Sheet Information <strong>Prime</strong>’s D.0 payer specificationsheets may be found at <strong>Prime</strong><strong>Therapeutics</strong>.com >Pharmacists > D.0/Version 5010 Pharmacy Information> D.0 Payer Sheet ASC X12/005010X221A1→→<strong>Prime</strong> is ready to convert 835 ERA files from the 4010 to5010 version. To request to be converted from the 4010to 5010 version or to request a test 5010 ERA file, pleasecontact pharmacyops@primetherapeutics.com.→→For D.0 or version 5010 related questions, please contactpharmacyops@primetherapeutics.comD.0 Changes Impacting Multiple Ingredient CompoundsIn September <strong>2011</strong>, <strong>Prime</strong> began accepting claims in both theNCPDP 5.1 and D.0 formats. In conjunction with accepting dualstandard claims, <strong>Prime</strong> started accepting multiple ingredientcompound submissions.See guidelines below to assist in submitting a multiple ingredientcompound claim to <strong>Prime</strong>:→ → <strong>Prime</strong> will accept a multiple ingredient compound submissionutilizing NCPDP’s Compound Segment for up to 25 ingredients.→ → Prior authorizations previously issued for processing acompound may no longer apply.→ → Dynamic prior authorizations for processing compounds whichcontain situational Medicare Part B versus Medicare Part Ddrugs will no longer apply, even if the compound meets thecriteria for inclusion as a Medicare Part D covered drug.A one-time prior authorization will be issued if the claimmeets the criteria for coverage under Medicare Part D.→ → Submission clarification codes will be supported for both<strong>Prime</strong>’s Commercial and Medicare Programs business.In the situation where an ingredient within the compoundis not covered, the Participating Pharmacy can submit thesubmission clarification code of “08” and the previouslyrejected claim will process to allow payment of all coveredingredients.→→Compounds containing a Medicare Part B ingredient must beprocessed under Medicare Part B.If you have questions regarding claims processing, please contact<strong>Prime</strong>’s Contact Center at 800.821.4795© <strong>Prime</strong> <strong>Therapeutics</strong> LLC11
<strong>Prime</strong> Perspective | November <strong>2011</strong>MAC List UpdatesClinical format Effective Date Description of Changeacyclovir tabs, 400 mg (ZOVIRAX) 8/15/11 Additionclotrimazole crm, 1% 8/1/11 Additiondesmopressin acetate nasal spray soln (refrigerated), 0.01% (DDAVP) 7/1/11 Additiondiflorasone oint, 0.05% 8/1/11 Additionestradiol transdermal weekly patch, 0.025 mg/24 hr (CLIMARA) 7/1/11 Additionimipramin pamoate caps, 125 mg (TOFRANIL-PM) 8/1/11 Additionletrozole tabs, 2.5 mg (FEMARA) 7/1/11 Additionlevofloxacin tabs, 250 mg, 500 mg, 750 mg (LEVAQUIN) 8/1/11 Additionnisoldipine ext-release 24 hour tabs, 17 mg (SULAR) 8/1/11 Additionvancomycin for inj, 1000 mg 8/1/11 Additionvenlafaxine ext-release 24 hour caps, 37.5 mg, 75 mg, 150 mg (EFFEXOR XR) 7/1/11 Additionvenlafaxine ext-release 24 hour tabs, 37.5 mg, 75 mg, 150 mg (VENLAFAXINE ER) 7/1/11 Additionzolpidem ext-release tabs, 6.25 mg, 12.5 mg (AMBIEN CR) 7/15/11 Additionamphetamine/dextroamphetamine mixed salts tabs, 7.5 mg, 15 mg (ADDERALL) 9/1/11 Removalaugmented betamethasone dipropionate lotn, 0.05% (DIPROLENE) 7/1/11 Removalcarbamazepine susp, 100 mg/5 mL (TEGRETOL) 8/1/11 Removalchlorpropamide tabs, 100 mg, 250 mg 7/1/11 Removalclarithromycin tabs, 250 mg, 500 mg (BIAXIN) 9/15/11 Removalclotrimazole crm, 1% 7/15/11 Removalclotrimazole/betamethasone lotn, 1-0.05% (LOTRISONE) 8/1/11 Removaldesoximetasone gel, 0.05% (TOPICORT) 7/1/11 Removaldexamethasone sodium phosphate ophth soln, 0.1% 7/15/11 Removaldexmethylphenidate tabs, 5 mg (FOCALIN) 8/1/11 Removaldrospirenone/ethinyl estradiol tabs, 3-0.02 mg (YAZ) 9/15/11 Removalfentanyl transdermal patch 72 hour, 12.5 mcg/hr (DURAGESIC) 8/15/11 RemovalFLUNISOLIDE nasal soln, 0.025% 8/15/11 Removalfluocinonide oint, 0.05% 9/1/11 Removalfluocinonide soln, 0.05% 8/15/11 Removallansoprazole delayed-release orally disintegrating tabs, 15 mg (PREVACID SOLUTAB) 7/1/11 Removalmethotrexate sodium preservative-free inj, 25 mg/mL 8/1/11 RemovalNYSTATIN/TRIAMCINOLONE crm, 100000 units - 1 mg/g 8/15/11 Removaloxcarbazepine susp, 300 mg/5 mL (TRILEPTAL) 8/15/11 Removalpermethrin crm, 5% 9/15/11 Removalpolyethylene glycol 3350 oral packets 8/1/11 Removalsulfacetamide sodium/sulfur emul, 10-5% (PLEXION CLEANSER) 9/15/11 Removal12 © <strong>Prime</strong> <strong>Therapeutics</strong> LLC
<strong>Prime</strong> Perspective | November <strong>2011</strong>How to Reach <strong>Prime</strong> <strong>Therapeutics</strong>As a service to Participating Pharmacies, <strong>Prime</strong> <strong>Therapeutics</strong>(<strong>Prime</strong>) publishes <strong>Prime</strong> Perspective quarterly to provide importantinformation for claims processing. We value your opinion and yourparticipation in our network. If you have comments or questions,you can reach us:By phone: <strong>Prime</strong> Pharmacy Contact Center 800.821.4795(24 hours a day, seven days a week)By email: pharmacyops@primetherapeutics.comLooking for Formularies?For Commercial formularies go to either the Blue Cross Blue Shieldplan website or <strong>Prime</strong><strong>Therapeutics</strong>.com > Pharmacists > FormularySearchFor Medicare Part D formularies go to <strong>Prime</strong><strong>Therapeutics</strong>.com >Medicare Part D > Medicare Resources > <strong>2011</strong> Medicare FormulariesKeep your Pharmacy Information Current<strong>Prime</strong> uses the National Council for Prescription Drug Programs(NCPDP) database to obtain addresses for network pharmacymailings. To update your pharmacy information go towww.ncpdp.org > NCPDP Provider ID (on the left side).Report Fraud, Waste and AbuseIf you suspect fraud, waste or abuse, by a Covered Person,Prescribing Provider, Participating Pharmacy or anyone else,notify <strong>Prime</strong> at 800.731.3269 or send the information to:<strong>Prime</strong> <strong>Therapeutics</strong> LLCAttn: Compliance OfficerP.O. Box 64812St. Paul, MN 55164-0812By email: reportfraud@primetherapeutics.comIf you would like an FWA Report to be anonymous, pleasecontact <strong>Prime</strong>'s 24-hour anonymous compliance hotline.Contact the hotline:By phone: 800.474.8651By email: atreports@lighthouse-services.comBy third party vendor’s website:www.lighthouse-services.com/primeDisclaimer: Product names listed are the property of their respective owners.© <strong>Prime</strong> <strong>Therapeutics</strong> LLC13
<strong>Prime</strong> Perspective | November <strong>2011</strong>Notes14 © <strong>Prime</strong> <strong>Therapeutics</strong> LLC
<strong>Prime</strong> Perspective | November <strong>2011</strong>Notes© <strong>Prime</strong> <strong>Therapeutics</strong> LLC15
<strong>Prime</strong> <strong>Therapeutics</strong> llcP.O. Box 64812St. Paul, MN 55164-0812PRESORTEDSTANDARD MAILU.S. POSTAGE PAIDPRIME THERAPEUTICS LLCTime SensitiveInformation from <strong>Prime</strong> <strong>Therapeutics</strong>→ Claims processing instructions→ Utilization management updates from Blue Cross and Blue Shield plans→ <strong>Prime</strong> audit requirements