Please click here (1.5MB) - Hong Kong Society of Palliative Medicine
Please click here (1.5MB) - Hong Kong Society of Palliative Medicine
Please click here (1.5MB) - Hong Kong Society of Palliative Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
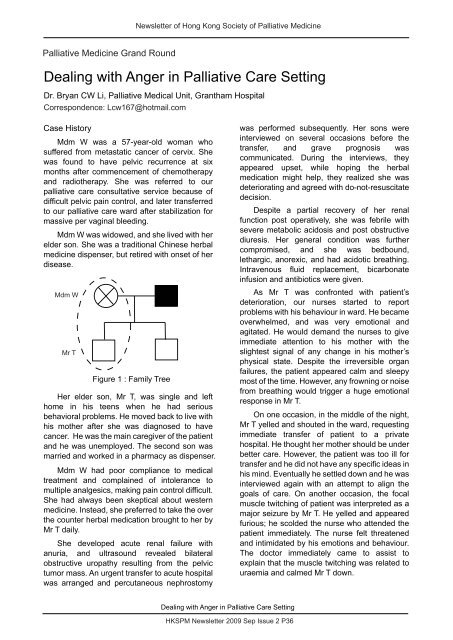
Newsletter <strong>of</strong> <strong>Hong</strong> <strong>Kong</strong> <strong>Society</strong> <strong>of</strong> <strong>Palliative</strong> <strong>Medicine</strong><strong>Palliative</strong> <strong>Medicine</strong> Grand RoundDealing with Anger in <strong>Palliative</strong> Care SettingDr. Bryan CW Li, <strong>Palliative</strong> Medical Unit, Grantham HospitalCorrespondence: Lcw167@hotmail.comCase HistoryMdm W was a 57-year-old woman whosuffered from metastatic cancer <strong>of</strong> cervix. Shewas found to have pelvic recurrence at sixmonths after commencement <strong>of</strong> chemotherapyand radiotherapy. She was referred to ourpalliative care consultative service because <strong>of</strong>difficult pelvic pain control, and later transferredto our palliative care ward after stabilization formassive per vaginal bleeding.Mdm W was widowed, and she lived with <strong>here</strong>lder son. She was a traditional Chinese herbalmedicine dispenser, but retired with onset <strong>of</strong> herdisease.Mdm WMr TFigure 1 : Family TreeHer elder son, Mr T, was single and lefthome in his teens when he had seriousbehavioral problems. He moved back to live withhis mother after she was diagnosed to havecancer. He was the main caregiver <strong>of</strong> the patientand he was unemployed. The second son wasmarried and worked in a pharmacy as dispenser.Mdm W had poor compliance to medicaltreatment and complained <strong>of</strong> intolerance tomultiple analgesics, making pain control difficult.She had always been skeptical about westernmedicine. Instead, she preferred to take the overthe counter herbal medication brought to her byMr T daily.She developed acute renal failure withanuria, and ultrasound revealed bilateralobstructive uropathy resulting from the pelvictumor mass. An urgent transfer to acute hospitalwas arranged and percutaneous nephrostomywas performed subsequently. Her sons wereinterviewed on several occasions before thetransfer, and grave prognosis wascommunicated. During the interviews, theyappeared upset, while hoping the herbalmedication might help, they realized she wasdeteriorating and agreed with do-not-resuscitatedecision.Despite a partial recovery <strong>of</strong> her renalfunction post operatively, she was febrile withsevere metabolic acidosis and post obstructivediuresis. Her general condition was furthercompromised, and she was bedbound,lethargic, anorexic, and had acidotic breathing.Intravenous fluid replacement, bicarbonateinfusion and antibiotics were given.As Mr T was confronted with patient’sdeterioration, our nurses started to reportproblems with his behaviour in ward. He becameoverwhelmed, and was very emotional andagitated. He would demand the nurses to giveimmediate attention to his mother with theslightest signal <strong>of</strong> any change in his mother’sphysical state. Despite the irreversible organfailures, the patient appeared calm and sleepymost <strong>of</strong> the time. However, any frowning or noisefrom breathing would trigger a huge emotionalresponse in Mr T.On one occasion, in the middle <strong>of</strong> the night,Mr T yelled and shouted in the ward, requestingimmediate transfer <strong>of</strong> patient to a privatehospital. He thought her mother should be underbetter care. However, the patient was too ill fortransfer and he did not have any specific ideas inhis mind. Eventually he settled down and he wasinterviewed again with an attempt to align thegoals <strong>of</strong> care. On another occasion, the focalmuscle twitching <strong>of</strong> patient was interpreted as amajor seizure by Mr T. He yelled and appearedfurious; he scolded the nurse who attended thepatient immediately. The nurse felt threatenedand intimidated by his emotions and behaviour.The doctor immediately came to assist toexplain that the muscle twitching was related touraemia and calmed Mr T down.Dealing with Anger in <strong>Palliative</strong> Care SettingHKSPM Newsletter 2009 Sep Issue 2 P36