Osteoporosis - Hong Kong Physiotherapy Association
Osteoporosis - Hong Kong Physiotherapy Association
Osteoporosis - Hong Kong Physiotherapy Association
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
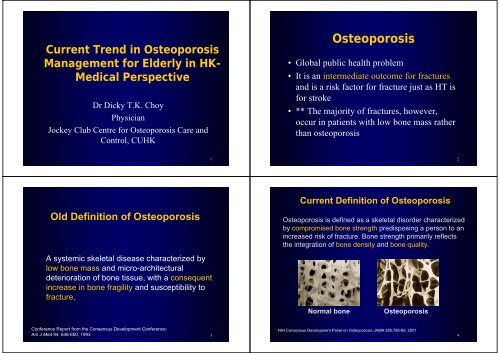
Current Trend in <strong>Osteoporosis</strong>Management for Elderly in HK-Medical PerspectiveDr Dicky T.K. ChoyPhysicianJockey Club Centre for <strong>Osteoporosis</strong> Care andControl, CUHK<strong>Osteoporosis</strong>• Global public health problem•It is an intermediate outcome for fracturesand is a risk factor for fracture just as HT isfor stroke• ** The majority of fractures, however,occur in patients with low bone mass ratherthan osteoporosis12Old Definition of <strong>Osteoporosis</strong>A systemic skeletal disease characterized bylow bone mass and micro-architecturaldeterioration of bone tissue, with a consequentincrease in bone fragility and susceptibility tofracture.Current Definition of <strong>Osteoporosis</strong><strong>Osteoporosis</strong> is defined as a skeletal disorder characterizedby compromised bone strength predisposing a person to anincreased risk of fracture. Bone strength primarily reflectsthe integration of bone density and bone quality.Normal bone<strong>Osteoporosis</strong>Conference Report from the Consensus Development Conference:NIH Consensus Development Panel on <strong>Osteoporosis</strong> JAMA 285:785-95; 2001Am J Med 94: 646-650, 1993 34
A diagram of a cutting cone with osteoclasts resorbingbone followed by osteoblasts depositing new osteoid,which subsequently becomes calcifiedPathophysiology56Bone remodelingVertebral Fracture• Bone loss occurs when this balance isaltered, resulting in greater bone removalthan replacement• This imbalance occurs with menopause andadvancing age.Hip FractureColles Fracture7
EpidemiologyAllHipSpineforearmWomen40%18%16%16%Men13%6%5%3%9(Melton, 1992)10Asia54%Hip fracture for men andwomen in 2050Men(1.8 million)Others8% LatinAmerica6%MiddleEast8%Europe11%NorthAmerica13%Asia51%Others6% LatinAmerica12%Women(4.5 million)MiddleEast6%NorthAmerica12%Europe12%11Adjusted Rates (100,000)Age-adjusted incidencerates in women6005004003002001000535459442269US (White) <strong>Hong</strong> <strong>Kong</strong> Singapore Thailand218Malaysia12
Adjusted Rates (100,000)Age-adjusted incidencerates in men200150100501871801641140US (White) <strong>Hong</strong> <strong>Kong</strong> Singapore Thailand88Malaysia13Age specific incidence rates for hip, vertebral, anddistal forearm fractures in men and womenMenWomenIncidence/100,000 person-yr40003000200010000HipHipVertebralVertebralColles’Colles’35-39 ≥85 ≥85Age group, yr14Incidence of hip fracture in<strong>Hong</strong> <strong>Kong</strong> women250020001995Incidence of hip fracture in<strong>Hong</strong> <strong>Kong</strong> men120019851995Per 100,0001500100050019851966Per 100,0008004001966050-59 60-69 70-79 80+Age15050-59 60-69 70-79 80+Age16
Direct cost for osteoporoticfracturesMortality and morbidity dueto hip fracture is highUSA<strong>Hong</strong> <strong>Kong</strong>(hip fracture)Women11.1 billion2.9 billionMen2.7 billion1.1 billion• 10-20% excess mortalitywithin 1 year• Up to 25% remain inlong term nursing homecare• Only 40% fully regaintheir pre fracture levelof independence1718Mortality and morbidity due tovertebral fracture is also high• Significant complicationsincluding back pain, height lossand kyphosis• Limited activity includingbending and reaching• May result in restrictive lungdisease if multiple thoracicfractures• Lumbar fracture may alterabdominal anatomyApproach to the Diagnosisand Management1920
Comprehensive approach• Detailed history (clinical risk factorsassessment including fall risk assessment )• Bone mineral density (BMD) assessment• Establish fracture risk using WHO 10-yearestimated fracture probabilityRisk factors included in the WHO 10-year Fracture Risk Assessment Model• Age• Gender• Personal history of fracture• Parental history of hip fracture• Low body mass index (BMI)• Use of oral glucocorticoid• Secondary osteoporosis (e.g RA )• Current smoking• Alcohol intake 3 or more drinks/day• Femoral neck BMD2122Risk Factors for Falls1. Environmental2. Medical3. Neuromuscular4. Fear of fallingEnvironmental• Low level lighting• Obstacles in the walking path• Lack of assist devices in bathrooms• Slippery outdoor conditions2324
MedicalNeuromuscular• Age• Arrthymias• Poor vision• Urgent urinary incontinence• Previous fall• Orthostatic hypotension• Medications ( narcotic analgesics, anticonvulsants,psychotropics )• Depression• Anxiety and agitation• Vit D def• Malnutrition• Poor balance• Weak muscles• Kyphosis• Reduced proprioception2526WHO definition of osteoporosisWHO DefinitionBMDT scoreBMDT score>2.5SDat or below-2.51-2.5SDBetween -1and -2.5Below themean peakadultBelow themean peakadult<strong>Osteoporosis</strong>Osteopenia• Although these definition are necessary toestablish the presence of osteoporosis, theyshould not be used as sole determinant oftreatment decisionsBMDT score
Bone Densitometry• Dual x-ray absorptiometry (DXA)• Quantitative computed tomography (QCT) –mainly use in research field• Quantitative ultrasoundDual x-ray absorptiometry(DXA)• Measure the BMD of lumbar spine ( L1-L4)and the hip ( femoral neck and total hip )• Diagnosis based on T-score ( WHOdefinition of osteoporosis )293032
Quantitative Ultrasound(QUS )• Can only used on peripheral bones e.g heel• Advantages of small size, relatively quickand simple measurements, and no radiation33 34Indications for BMD testing( NOF recommendation )• Women > 65 and men > 70, regardless of clinicalrisk factors• Younger postmenopausal women and men age 50-70 about whom you have concern based on theirclinical risk factor profile• Women in the menopausal transition if there is aspecific risk factor associated with increasedfracture risk such as low body weight, prior lowtrauma fracture, or high risk medication36
NOF GuidelineAntiresorptive agents• Low bone mass with secondary causesassociated with high risk of fracture ( suchas steroid use or total immobilization )• Low bone mass and 10-yr probability of hipfracture >3% or a 10-yr probability of anymajor osteoporosis related fracture >20%based on the WHO model45• Bisphosphonates- Alendronate- Risedronate- Ibandronate ( oral and IV )- Zoledronate (IV)• Selective Estrogen Receptor Modulators(SERM)- Raloxifene• Strontium * ( dual action )• Calcitonin• HRT46Anabolic agentBisphosphonate• PTH 1-34 ( Parathyroid hormone )• Inhibitors of osteoclast activity• Strong affinity for calcium ions and arerapidly taken up by bone• Long skeletal half life• ??? Long term side effects – oversuppressed bone turnover4748
Alendronate ( Fosamax )• 70mg oral weekly• New formulation ( fosamax plus ) hadvitamin D3 2800/5600IU• Reduce vertebral fracture by 48% over 3years in patient w/o prior vertebral fracture• Reduce the incidence of vertebral and nonvertebralfracture by around 50% in patientwith prior vertebral fractureIbandronate ( Bonviva )• 150mg oral once a month• 3mg every 3 months by IV injection• Reduces the incidence of vertebral fractureby about 50% over 3 years4950Risedronate ( Actonel )• 35 mg oral weekly• Reduces the incidence of vertebral fractureby 41-49% and non-vertebral fracture by36% over 3 yearsZoledronate ( Aclasta )• 5mg by IV infusion over at least 15 minsonce yearly• Reduces the incidence of vertebral fractureby 70%, hip fracture 41% and non-vertebralfracture by 25% over 3 years5152
Side effects of Bisphosphonates• Similar for all oral bisphosphonates whichinclude GI problems such as dyspepsia,nausea, pain in the bones, muscles andjoints. ( need to be taken on an emptystomach, 1st thing in the morning withplenty of plain water, at least 30-60 minsbefore eating or drinking, remain uprightduring this interval as well )Side effects of Bisphosphonates• Osteonecrosis of the jaw have been reported(very rare in osteoporosis cases)- usually seen in oncology cases with highdose IV bisphosphonate5354Drug Interactions withbisphosphonate• No clinical significant interactions withmost common medicationsSERM(Selective Estrogen Receptor Modulator)• Raloxifene ( Evista )• 60mg oral daily• Reduces the risk of vertebral fracture by 55% inpatients with prior fracture, 30% in patients w/oprior fracture over 3 years• Reduces the risk of breast cancer• Increase risk of DVT• Increase hot flashes5556
Effect of Raloxifene on All Breast Cancer IncidenceMORE Trial - 4 Years% of Randomized Patients2.01.51.00.5RR = 0.38 (95% CI = 0.24-0.58)NNT = 94*0.00 1 2 3 4Years since Randomization62%PlaceboRLX(pooled)Arrow denotes annual mammogram (*optional)Total Cases = 77Adapted from Cauley J et al. Breast Cancer Res Treatment 65:125-34, 200157Strontium Ranelate ( Protos )• Both anti-resorptive and anabolic effects• 1 sachet ( 2 g ) daily to be taken at bedtime• Reduces vertebral fracture risk by 41% in 3years, non-vertebral fracture risk by 16%• Side effects of nausea, diarrhea, headache, skinirritation• Risk of DVT may be increased58Calcitonin• Salmon calcitonin• Single daily intranasal spray / s.c inj• No big RCT data to look at fracture riskreduction• May reduce back pain caused by acutevertebral fracture• S/E of nausea, vomiting, dizziness andflushing may occur59HRT( Hormone Replacement Therapy )• Reduces the risk of clinical vertebral fractureand hip fracture by 34% and other osteoporoticfracture by 23% over 5 years• Increased risks of myocardial infarction, stroke,invasive breast cancer, pulmonary emboli andDVT during the 5 years of treatment• No longer used as 1st line agent to treatosteoporosis60
Anabolic agent• PTH 1-34 ( Forteo )• Daily s.c injection• Reduces the risk of vertebral fracture by 65%and non-vertebral fracture by 53% in patientswith osteoporosis, after an average use of 18monthsPTH 1-34 (Forteo)• Side effects of leg cramps and dizziness• Relatively expensive• Safety and efficacy has not beendemonstrated beyond 2 years of treatment• Common practice to follow PTH treatmentwith an anti-resorptive agent6162Combination therapy??Remaining issues……Not recommended – no good researchevidence to show better fracture outcome6364
• How can we better assess bone strength using non-invasivetechnologies and thus improve identification of patients athigh risk of fracture?• How effective are different drug treatments in preventingfractures in patients with moderately low bone mass?• How long should anti-resorptive therapies be continued,and are there long term side effects as yet unknown?• Are combination therapies useful, and if so, which are theuseful drug combinations and when should they be used?• Can we identify agents that will significantly increase bonemass and return bone structure to normalSummary6566<strong>Osteoporosis</strong>• Global public health problem• Very common condition among elderly( 1 in 2 for women and 1 in 5 in men )• Fracture can KILL• Can be easily diagnosed and have veryeffective drug treatment• Multidisciplinary approach6768