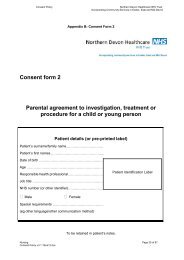
Consent form 1 Patient agreement to investigation, treatment or ...
Consent form 1 Patient agreement to investigation, treatment or ...
Consent form 1 Patient agreement to investigation, treatment or ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Consent</strong> PolicyN<strong>or</strong>thern Devon Healthcare NHS TrustInc<strong>or</strong>p<strong>or</strong>ating Community Services in Exeter, East and Mid DevonGuidance <strong>to</strong> health professionals (<strong>to</strong> be read in conjunction with <strong>Consent</strong> policy)What a consent <strong>f<strong>or</strong>m</strong> is f<strong>or</strong>This <strong>f<strong>or</strong>m</strong> documents the patient’s <strong>agreement</strong> <strong>to</strong> go ahead with the <strong>investigation</strong> <strong>or</strong> <strong>treatment</strong>you have proposed. It is not a legal waiver – if patients, f<strong>or</strong> example, do not receive enoughin<strong>f<strong>or</strong>m</strong>ation on which <strong>to</strong> base their decision, then the consent may not be valid, even thoughthe <strong>f<strong>or</strong>m</strong> has been signed. <strong>Patient</strong>s are also entitled <strong>to</strong> change their mind after signing the<strong>f<strong>or</strong>m</strong>, if they retain capacity <strong>to</strong> do so. The <strong>f<strong>or</strong>m</strong> should act as an aide-memoire <strong>to</strong> healthprofessionals and patients, by providing a check-list of the kind of in<strong>f<strong>or</strong>m</strong>ation patients shouldbe offered, and by enabling the patient <strong>to</strong> have a written rec<strong>or</strong>d of the main points discussed.In no way, however, should the written in<strong>f<strong>or</strong>m</strong>ation provided f<strong>or</strong> the patient be regarded as asubstitute f<strong>or</strong> face-<strong>to</strong>-face discussions with the patient.The law on consentSee the Department of Health’s Reference guide <strong>to</strong> consent f<strong>or</strong> examination <strong>or</strong> <strong>treatment</strong> f<strong>or</strong> acomprehensive summary of the law on consent (also available at www.doh.gov.uk/consent).Who can give consentEveryone aged 16 <strong>or</strong> m<strong>or</strong>e is presumed <strong>to</strong> be competent <strong>to</strong> give consent f<strong>or</strong> themselves,unless the opposite is demonstrated. If a child under the age of 16 has “sufficientunderstanding and intelligence <strong>to</strong> enable him <strong>or</strong> her <strong>to</strong> understand fully what is proposed”, thenhe <strong>or</strong> she will be competent <strong>to</strong> give consent f<strong>or</strong> himself <strong>or</strong> herself. Young people aged 16 and17, and legally ‘competent’ younger children, may theref<strong>or</strong>e sign this <strong>f<strong>or</strong>m</strong> f<strong>or</strong> themselves, butmay like a parent <strong>to</strong> countersign as well. If the child is not able <strong>to</strong> give consent f<strong>or</strong> himself <strong>or</strong>herself, some-one with parental responsibility may do so on their behalf and a separate <strong>f<strong>or</strong>m</strong> isavailable f<strong>or</strong> this purpose. Even where a child is able <strong>to</strong> give consent f<strong>or</strong> himself <strong>or</strong> herself, youshould always involve those with parental responsibility in the child’s care, unless the childspecifically asks you not <strong>to</strong> do so. If a patient is mentally competent <strong>to</strong> give consent but isphysically unable <strong>to</strong> sign a <strong>f<strong>or</strong>m</strong>, you should complete this <strong>f<strong>or</strong>m</strong> as usual, and ask anindependent witness <strong>to</strong> confirm that the patient has given consent <strong>or</strong>ally <strong>or</strong> non-verbally.When NOT <strong>to</strong> use this <strong>f<strong>or</strong>m</strong>If the patient is 18 <strong>or</strong> over and is not legally competent <strong>to</strong> give consent, you should use <strong>f<strong>or</strong>m</strong> 4(<strong>f<strong>or</strong>m</strong> f<strong>or</strong> adults who are unable <strong>to</strong> consent <strong>to</strong> <strong>investigation</strong> <strong>or</strong> <strong>treatment</strong>) instead of this <strong>f<strong>or</strong>m</strong>. Apatient will not be legally competent <strong>to</strong> give consent if: they are unable <strong>to</strong> comprehend and retain in<strong>f<strong>or</strong>m</strong>ation material <strong>to</strong> the decision and/<strong>or</strong> they are unable <strong>to</strong> weigh and use this in<strong>f<strong>or</strong>m</strong>ation in coming <strong>to</strong> a decision.You should always take all reasonable steps (f<strong>or</strong> example involving m<strong>or</strong>e specialistcolleagues) <strong>to</strong> supp<strong>or</strong>t a patient in making their own decision, bef<strong>or</strong>e concluding that they areunable <strong>to</strong> do so.Relatives cannot be asked <strong>to</strong> sign this <strong>f<strong>or</strong>m</strong> on behalf of an adult who is not legally competent<strong>to</strong> consent f<strong>or</strong> himself <strong>or</strong> herself.In<strong>f<strong>or</strong>m</strong>ationIn<strong>f<strong>or</strong>m</strong>ation about what the <strong>treatment</strong> will involve, its benefits and risks (including side-effectsand complications) and the alternatives <strong>to</strong> the particular procedure proposed, is crucial f<strong>or</strong>patients when making up their minds. The courts have stated that patients should be <strong>to</strong>ldabout ‘significant risks which would affect the judgement of a reasonable patient’. ‘Significant’has not been legally defined, but the GMC requires doc<strong>to</strong>rs <strong>to</strong> tell patients about ‘serious <strong>or</strong>frequently occurring’ risks. In addition if patients make clear they have particular concernsabout certain kinds of risk, you should make sure they are in<strong>f<strong>or</strong>m</strong>ed about these risks, even ifthey are very small <strong>or</strong> rare. You should always answer questions honestly. Sometimes,Nursing Page 33 of 57<strong>Consent</strong> Policy v3.1 19Jul12.doc