remac refresher testing dates - The Regional Emergency Medical ...
remac refresher testing dates - The Regional Emergency Medical ...
remac refresher testing dates - The Regional Emergency Medical ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
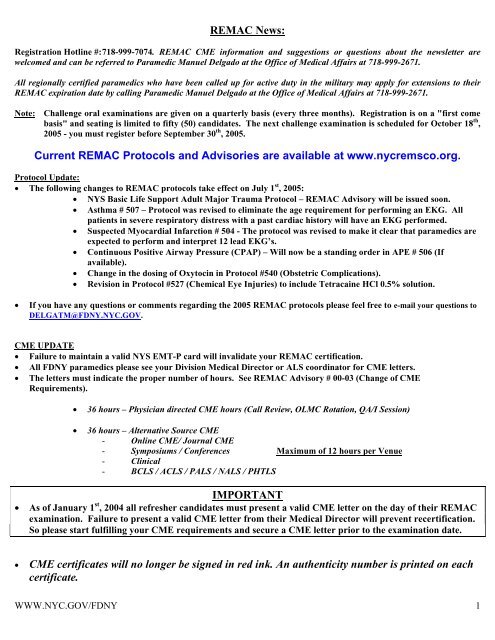
REMAC News:Registration Hotline #: 718-999-7074. REMAC CME information and suggestions or questions about the newsletter arewelcomed and can be referred to Paramedic Manuel Delgado at the Office of <strong>Medical</strong> Affairs at 718-999-2671.All regionally certified paramedics who have been called up for active duty in the military may apply for extensions to theirREMAC expiration date by calling Paramedic Manuel Delgado at the Office of <strong>Medical</strong> Affairs at 718-999-2671.Note: Challenge oral examinations are given on a quarterly basis (every three months). Registration is on a "first comebasis" and seating is limited to fifty (50) candi<strong>dates</strong>. <strong>The</strong> next challenge examination is scheduled for October 18 th ,2005 - you must register before September 30 th , 2005.Current REMAC Protocols and Advisories are available at www.nycremsco.org.Protocol Update:• <strong>The</strong> following changes to REMAC protocols take effect on July 1 st , 2005:• NYS Basic Life Support Adult Major Trauma Protocol – REMAC Advisory will be issued soon.• Asthma # 507 – Protocol was revised to eliminate the age requirement for performing an EKG. Allpatients in severe respiratory distress with a past cardiac history will have an EKG performed.• Suspected Myocardial Infarction # 504 - <strong>The</strong> protocol was revised to make it clear that paramedics areexpected to perform and interpret 12 lead EKG’s.• Continuous Positive Airway Pressure (CPAP) – Will now be a standing order in APE # 506 (Ifavailable).• Change in the dosing of Oxytocin in Protocol #540 (Obstetric Complications).• Revision in Protocol #527 (Chemical Eye Injuries) to include Tetracaine HCl 0.5% solution.• If you have any questions or comments regarding the 2005 REMAC protocols please feel free to e-mail your questions toDELGATM@FDNY.NYC.GOV.CME UPDATE• Failure to maintain a valid NYS EMT-P card will invalidate your REMAC certification.• All FDNY paramedics please see your Division <strong>Medical</strong> Director or ALS coordinator for CME letters.• <strong>The</strong> letters must indicate the proper number of hours. See REMAC Advisory # 00-03 (Change of CMERequirements).• 36 hours – Physician directed CME hours (Call Review, OLMC Rotation, QA/I Session)• 36 hours – Alternative Source CME- Online CME/ Journal CME- Symposiums / Conferences Maximum of 12 hours per Venue- Clinical- BCLS / ACLS / PALS / NALS / PHTLSIMPORTANT• As of January 1 st , 2004 all <strong>refresher</strong> candi<strong>dates</strong> must present a valid CME letter on the day of their REMACexamination. Failure to present a valid CME letter from their <strong>Medical</strong> Director will prevent recertification.So please start fulfilling your CME requirements and secure a CME letter prior to the examination date.• CME certificates will no longer be signed in red ink. An authenticity number is printed on eachcertificate.WWW.NYC.GOV/FDNY 1
If you have any questions please reach out to your ALS borough coordinators (see below) or feel free to call the Office of<strong>Medical</strong> Affairs @ (718) 999-2790 for further clarification.ALS Division Coordinators:• Citywide ALS Coordinator:Paramedic Lt. Esther Coarse (718) 999-1738• Division 1:Paramedic Andrea Katsanakas (212) 964-4518• Division 2:Paramedic Steve Pilla (718) 829-6069• Division 3:Paramedic Gary Simmonds (718) 968-9750Paramedic Al Navarro (718) 968-9750• Division 4:Paramedic Lisa DeSena (718) 883-2150• Division 5:Paramedic Russell Shewchuk (718) 979-7175• Bureau of Training:Paramedic James "Bubba" Fallar (718) 281-8325• EMS Pharmacy:Paramedic Anthony Esposito (718) 571-7620Division <strong>Medical</strong> Directors:• Division 1 and OLMC:Dr. John Freese (718) 999- 0749• Division 2 and BOT:Dr. Dario Gonzalez (718) 999-0748• Division 3 and 5:Dr. Glenn Asaeda (718) 999-2666• Division 4:Dr. Bradley Kauffman (718) 999-1872REMSCO website address:WWW.NYCREMSCO.ORGOnline CME websites: WWW.MEDCOLLEGE.COM WWW.EMS-CE.COMWWW.EMINET.COM WWW.EMCert.COMWWW.MedicEd.comNYS/DOH EMS website address:WWW.Health.State.NY.USCurrent REMAC Protocols and Advisories are available at www.nycremsco.org.WWW.NYC.GOV/FDNY 2
From the Editor:Dario Gonzalez, MD, FACEP, was named <strong>Medical</strong> Director (Acting) for the FDNY/<strong>Emergency</strong> <strong>Medical</strong> ServiceCommand and the Office of <strong>Medical</strong> Affairs. Dr. Gonzalez will continue to serve as the Division Two medicaldirector.ePCR Update: Divisions One and Three are now up and running with Division Two scheduled to be completedby September. Next up are Divisions Four and Five.<strong>The</strong> Bill Shearer BLS and ALS National Competitions were held in Orlando, Fla. on July 7 th . Two teams, oneBLS and one ALS represented the FDNY EMS command at this year’s event. A team from Division Two (thisyears FDNY competition runner-up) also enrolled in the competition but was not part of the EMS Commandofficial contingent. All of our teams performed superbly with the Station 20 BLS team winning the BLScompetition outright. Congratulations to EMT Joe Fortis, EMT Eddy Perez and EMT Erica Serrano forplacing first and winning the competition by a twenty-point margin. <strong>The</strong>y can now boast that they are the“number one BLS team in the country”.Here are the team participants and their final placement:BLS Competition:Station 20 - EMT Joe Fortis, EMT Eddy Perez and EMT Erica Serrano - 1 st out of 58 teams.ALS Competition:Bureau of Training – Paramedics Phillip Lewis, Rolando Gardon and Joseph Esquivias - 36 th out of 58 teams.Station 20 – Paramedic Lieutenants James Bayreuther, John Raftery and Scott Heinze - 8 th out of 58 teams.Have you had an interesting call lately? Submit it to the journal editor and if it’s publishedyou’ll get three hours of Physician Directed CME.All inquires regarding CME certificates should be forwarded to Paramedic Steven Goldstein @(718) 999-0364.WWW.NYC.GOV/FDNY 3
NEW!ePCR TIP OF THE MONTHEach month we will highlight information on the ePCR in this space.Paramedics are reminded to always perform an ALS assessment when appropriate AND to darken the ALS ASSESMENT box onthe ePCR.Paramedics are also reminded to carefully document the correct type of diagnostic EKG used. For example, if only a 3 lead EKGis done be sure 12 lead is not documented unless it was actually performed. Remember, treat your patient appropriately anddocument accordingly. Accurate documentation is your responsibility as a professional.From the OMA StatisticianIn today’s article, the difference between mean and median is discussed as it relates to a statistic called skewness. <strong>The</strong> example that will beused analyzes the time differential between first responders and ambulances as they respond to segment 1 calls for the first quarter of 2005. Inthis example do we want to use the mean or median as the answer. Ambulances arrive almost 37 seconds before (-36.82) first responders, onaverage (mean) but at the 50 th percentile (median) ambulances arrive only 19 seconds ahead (-19) of first responders.Arrival Difference in Seconds (CAD - STARFIRE Times)NValid Arrivals 4325Missing data 663Mean -36.82Std. Error of Mean 3.839Median -19.00Mode -10Std. Deviation 252.449Variance 63730.376Skewness -2.239Std. Error of Skewness .037Kurtosis 24.834Std. Error of Kurtosis .074Maximum 2591Percentiles 25 -123.5050 -19.0075 78.50So the median is above the mean in our example of segment 1 responses. When the median is to the right of the mean the distribution is said tobe negatively skewed, with over 50 percent of the data above the mean. Because the mean is “pulled” toward unbalanced, lower scores, it issaid to be in a negatively skewed distribution, so the median may be a better representation of the arrival difference between ambulances andfirst responders.WWW.NYC.GOV/FDNY 4
<strong>The</strong> median is not affected at all by extreme scores, whether very low differences or very large differences, rather it establishes a rank orderwhere the 50th percent of the cases fall. Notice the skewness statistic has a negative sign.January - M arch, 20051,000,000medianmean1,000Skeweness -2.21.-40 00-30 00-20 00-10 00010002000Arrival Difference in Seconds(C A D - S T A R F IR E Tim es)3000Mean = -36.82Std. Dev. =252.449N = 4,325And the histogram above is ever so slightly negatively skewed with the bubble to the right.Got a stats question? Call Jim Braun @ (718) 999-0331Written by: Jim Braun, MAPPAAFDNY/OMA StatisticianNews & Information from the EMS Bureau of TrainingEMS Training Supervision:Chief of EMS TrainingCommanding Officer EMS AcademyCommanding Officer CFR TrainingALS Program CoordinatorTour 2 BLS Program CoordinatorTour 3 BLS Program CoordinatorTour 3 BLS Program CoordinatorEVOC Program CoordinatorHaz Tac Training Coordinator (detailed)Division Chief James P. MartinCaptain Scott C. HollidayCaptain John QuigleyCaptain William Torres Jr.Lieutenant John J. Scotch IILieutenant Arthur LesterLieutenant David RussellLieutenant Robert RahebLieutenant William MelarangoImportant Contact Numbers for the Bureau of Training:EMS Academy Main Number 718-281-8325EMS Academy Fax 718-352-3954CFR Training 718-281-8405EVOC Training 718-281-8317Haz Tac Training 718-281-8310EMS Training Administration 718-281-8460Training Schedules Coordinator 718-281-8466Registrar 718-281-8467Paramedic Basic Training Update:Paramedic Basic Training Class 4:Academic Schedule – Summer/Fall 2005Sixty members of the service including 5 officers are scheduled to begin this nine-monthtraining program on September 12, 2005. <strong>The</strong>y are scheduled to take the May 2006 NYSexam followed by their REMAC exams.Trainee Orientation Program (TOP):TOP 05-05: Fifty-nine (59) students began the TOP program on Tuesday, July 12, 2005. <strong>The</strong>se 59 EMTs will complete theprogram in early September..WWW.NYC.GOV/FDNY 5
P-TOP 05-01: Ten (10) paramedics began a paramedic TOP program on Tuesday, July 12, 2005. <strong>The</strong>se 10 paramedics arescheduled to complete their Academy training just after Labor Day.Medic Upgrade Program:A paramedic upgrade program is scheduled to begin on September 30, 2005. Any member withcurrent NYS and REMAC certification is urged to contact Lt. Bruce Medjuck at EMS Operationsas soon as possible for information regarding upgrade to paramedic.Refresher Programs:BLS Refreshers:Both a tour 2 and a tour 3 EMT <strong>refresher</strong> will begin on Monday, September 12, 2005. EMT <strong>refresher</strong>s willcontinue on both tours until the next TOP class is scheduled to begin which is tentatively scheduled forNovember 2005.ALS Refreshers: <strong>The</strong> 15-day paramedic <strong>refresher</strong> program begins again on Wednesday, September 7, 2005.Haz Tac Training:Haz Tac training concluded for the summer on July 18, 2005. Several new classes of Haz Tac certifiedpersonnel completed the 10 day training program this last semester while several <strong>refresher</strong> classescompleted their 5 day program.Officer Training:BLEMS: Thirty-five newly promoted EMS Lieutenants began the Basic Leadership for <strong>Emergency</strong> <strong>Medical</strong> Services courseon Monday, July 11, 2005. <strong>The</strong>y are scheduled to complete their training on August 5, 2005.ALEMS:Eight new Captains will begin the nine-day Advanced Leadership for <strong>Emergency</strong> <strong>Medical</strong> Services course onMonday, August 8, 2005.2005 NYS Exam Dates:Thursday, August 18, 2005Thursday, September 29, 2005Thursday, October 27, 2005Thursday, November 17, 2005Thursday, December 15, 2005Frequently Asked Questions (FAQ):1. Can the endotracheal dose of atropine be doubled due to the amount of fluid?Yes, the dose of atropine should be doubled when administered via the endotracheal tube. Currently, the FDNY supplies atropine in vialscontaining 1mg in 10 cc’s. <strong>The</strong> medication inserts are stocked with six of these vials. <strong>The</strong>refore to administer the appropriate dose of atropinevia ET, you must use two vials of atropine. <strong>The</strong> amount of fluid (20cc’s) administered with this atropine dose is not considered to be harmfulto the patient. Even administering the maximum total dose of atropine via the endotracheal tube(total of 60cc’s) is considered to be safe.2. Should all patients with Atrial fibrillation/Atrial flutter be given Cardizem regardless of the heart rate?No, according to the REMAC Atrial fibrillation/Atrial Flutter protocol 505B only patients with heart rates of 150bpm or higher are candi<strong>dates</strong>for treatment. In addition, in order to give Cardizem the complex width must be narrow and the blood pressure must be normal or elevated.Cardizem is a calcium channel blocker used to slow the ventricular response to a rapid A-fib/A-flutter. For example, a rapid atrial fibrillationat a rate of 180 would be slowed to a rate of 110. It is important to remember that stable patients who may have sustained atrialfibrillation/atrial flutter for greater than 48 hours should not be cardioverted, either electrically or chemically (i.e. amiodarone) in theprehospital setting.Answers provided by: Jessica Deresto, EMT-PInstructor - FDNY/BOTWWW.NYC.GOV/FDNY 6
Uncommon SeizuresCharlie Unit Two is dispatched out on a summer evening for a seizure call at a private residence. Upon arrival, family members of a 21 yearoldfemale meet the crew. <strong>The</strong> mother of the patient directs the paramedics to a back room where they find the patient sitting on a chair,complaining of not being able to see.Prehospital Evaluation and TreatmentFrom an interview with the patient, a history of visual disturbances described as on and off episodes of being unable to see anything at all toseeing spots, associated with dizziness, and headache for one day is elicited. Family members state that the patient had 1 seizure episodeaffecting the entire body prompting the call for EMS. <strong>The</strong> mother reports that the seizure lasted about 1 minute.<strong>The</strong> patient denies any past medical history or allergies to medication and reports only taking ibuprofen for the headache. At this time, it isrevealed that the patient is post-partum, just having delivered a healthy infant 6 days prior. <strong>The</strong> child was a normal spontaneous vaginaldelivery with no complications. <strong>The</strong> patient also denies any complications during the entire pregnancy. This was her first and only pregnancy.Physical examination revealed an awake patient, alert and oriented to person, place, and time complaining of the above. Despite the reportedseizure episode, the patient was not post-ictal upon EMS’ arrival and had no evidence of oral trauma or urinary incontinence. Continuedphysical examination showed that there was no evidence of dyspnea or Jugular Venous Distention, lung sounds were clear and equalbilaterally, and the abdomen was soft on palpation with no tenderness. <strong>The</strong>re was also no evidence of pedal edema. Vital signs were a bloodpressure of 180/90, a heart rate of 120, and respirations of 16. An ECG reveals a sinus tachycardia at a rate of 120. No trauma at any time isreported. A 20 gauge IV saline lock is established and secured at the left antecubital area.At this point while getting the patient packaged for transport, the patient suffered a grand mal seizure and was treated according to theappropriate seizure protocol which controlled the tonic/clonic activity. <strong>The</strong> patient was transported to the nearest ED facility.Hospital EvaluationIn the <strong>Emergency</strong> Department, the patient is stabilized and monitored, and admitted to the OB/GYN Services for further management.Case ReviewIt is reported that hypertension during pregnancy can greatly increase the risk to both mother and fetus. 5 to 10% of all pregnancies at sometime during gestation are affected by hypertension, making the disease one of the most common pregnancy related complications.In normally pregnant women, due to physiological changes, blood pressure tends to be lower than during non-pregnant states, particularlyduring the first trimester. <strong>The</strong>refore, the normally accepted values as to the definition of hypertension of 140/90 mm Hg need to be evaluatedwith caution. One study demonstrated that blood pressures only as high as 130/70 mm Hg caused increased fetal risk. Besides the absolutenumber and associated signs and symptoms, the other determination of hypertension in a pregnant patient is an increase in systolic pressure of30 mm Hg or a diastolic rise of 15 mm Hg from baseline levels.Hypertension in pregnancy is divided into three general categories: 1) Pregnancy induced hypertension (PIH) – hypertension induced bypregnancy and resolving postpartum, 2) Pregnancy aggravated hypertension: chronic hypertension superimposed by preeclampsia or eclampsiaoccurring during pregnancy, and 3) Chronic or coincidental hypertension – hypertension present before pregnancy or persisting more than 6weeks postpartum.Pregnancy induced hypertension is a vasospastic disease causing injury to maternal organs, the placenta, and the fetus. <strong>The</strong> extremes of PIHare preeclampsia and eclampsia. Preeclampsia, thought to occur most commonly in young primiparous and older multiparous women, tends toaffect the lower socioeconomic groups more often. <strong>The</strong> progression of preeclampsia begins with gradual edema and hypertension followed byproteinuria. Gradually, symptoms of headache (82.5%), visual disturbance (44.4%), and epigastric to right upper quadrant pain (19%) mayoccur. If these signs and symptoms are associated with seizures or coma, then the patient has progressed into the realm of eclampsia.Although the literature reports that eclampsia has been on the decline in recent years, this disease is still seen in about 1 in every 2,000deliveries and accounts for approximately 12% of fetal mortality.One of the other complications of preeclampsia is the HELLP Syndrome – Hemolysis, Elevated Liver enzymes, and Low Platelets, developingin 5 to 10% of preeclamptic women, further complicating pregnancy induced hypertension.<strong>The</strong> most common cause of death to the mother of severe preeclampsia or eclampsia is ultimately cerebral hemorrhage.WWW.NYC.GOV/FDNY 7
As far as management of these patients, the key is reduction of blood pressure, prevention and control of seizure activity, and early obstetricconsultation. Prehospitally, some EMS protocols allow the use of magnesium sulfate for control of seizures which is thought to act as amembrane stabilizer and vasodilator, reducing cerebral ischemia. <strong>The</strong> control of seizures allows maintenance of uterine and fetal blood flow.While administering magnesium sulfate, patients must be constantly monitored for loss of reflexes and respiratory depression. Magnesiumsulfate is considered first-line medication management in eclampsia. Diazepam may also be considered for seizure control but may cause riskfor the fetus. However, stabilization of the mother is paramount for stabilization of the fetus and the benefits versus risks must be considered.For blood pressure control in the emergency department, hydralazine has been the preferred agent.Ultimately in the eclamptic patient whose seizure activity cannot be controlled or there is evidence of fetal demise, delivery of the infant is thedefinitive treatment.Discussion<strong>The</strong> literature reports that eclampsia can occur up to 10 days or longer postpartum in some cases. One study even identified eclampsia severalweeks after delivery in a patient with a prior history of hypertension. <strong>The</strong> medics in this case were cognizant of the fact that eclampsia canoccur so many days even after delivery and were able to provide the appropriate care. Although most providers are aware that this conditioncan occur after delivery, most do not realize just how far after delivery the disease needs to be considered. Prehospital care providers arereminded through this case to consider this condition even when the infant has already been delivered many days prior.Written by:Glenn Asaeda, MD – Division <strong>Medical</strong> DirectorRay Ferreira, EMT-P – Division ThreeAndre Pierre-Louis, EMT-P – Division ThreeAs previously published in JEMS, February 2005.WWW.NYC.GOV/FDNY 8
Paramedics are encouraged to read the article ("Uncommon Seizures" written by Glenn Asaeda, MD, Ray Ferreira, EMT-Pand Andre Pierre-Louis, EMT-P ) and then answer the following 10 questions on the answer sheet below. Paramedics receivinga minimum grade of 80% will receive (1) one hour of Online/Journal CME. Forward the completed answer sheet by DepartmentMail to theFDNY Office of <strong>Medical</strong> Affairs – ATTN. Paramedic Steven GoldsteinOr FAX (718) 999-0119Or U.S. MAIL 9 MetroTech Center, Brooklyn, N.Y. 11201-3857Participants are strongly advised to keep a copy of their submitted question sheets for their own record.• Please submit the CME answer sheet only once, please DO NOT fax it if you've sent it via e-mail or inter-office mail (pony express).NAME: ___________________________MAC#:_________BATT# / HOSP AFFILIATION: ______________E-MAIL ADDRESS: ______________________________________HOME ADDRESS: ____________________________________________________________________________WWW.NYC.GOV/FDNY 10
This Page wasLeft BlankIntentionallyWWW.NYC.GOV/FDNY 11
NAME: ___________________REMAC# ___________BATT# / HOSP AFFILIATION______________ADDRESS TO FORWARD RESULTS (IF NOT A FDNY EMPLOYEE): ________________________September, 2005 - JOURNAL CME TOPIC - "Uncommon Seizures”1. What percentage of all pregnancies at some time during gestation are affected by hypertension, making the diseaseone of the most common pregnancy related complications?A. 1 to 2%B. 2 to 5%C. 5 to 10%D. 10 to 15%E. > 15%2. In the pregnant woman, the normal physiologic changes of pregnancy ________ the blood pressure, particularlyduring the first trimester.A. elevateB. keeps the sameC. lowerD. none of the aboveE. all of the above3. One study documented that blood pressure measurements only as high as _______ mmHg caused increased fetal risk.A. 90/60B. 100/60C. 110/70D. 120/70E. 130/704. Preeclampsia is thought to occur most commonly in:A. old primiparous and younger multiparous womenB. young primiparous and older multiparous womenC. higher socioeconomic groups more oftenD. none of the above5. All of the following are signs and symptoms of preeclampsia except:A. headacheB. proteinuriaC. hypertensionD. frequent nose bleedsE. all of the aboveWWW.NYC.GOV/FDNY 12
NAME: _______________________REMAC# ___________ BATT# / HOSP AFFILIATION__________________ADDRESS TO FORWARD RESULTS (IF NOT A FDNY EMPLOYEE): ________________________September, 2005 - JOURNAL CME TOPIC – “Uncommon Seizures”6. <strong>The</strong> literature reports that eclampsia accounts for approximately _____% of fetal mortality.A. 5B. 10C. 15D. 20E. 257. Which of the following is not a complication of the HELLP Syndrome of preeclampsia?A. HemolysisB. Elevated Liver enzymesC. Low Protein levelsD. all are complications8. <strong>The</strong> most common cause of death to the mother of severe preeclampsia or eclampsia is ultimately:A. cerebral anoxiaB. cardiac complicationsC. renal complicationsD. cerebral hemorrhageE. electrolyte imbalances9. <strong>The</strong> key to management of preeclamptic/eclamptic patients include all of the following except:A. reduction of blood pressureB. prevention and control of seizure activityC. early obstetric consultationD. early brain CTE. all of the above10. Patients being administered magnesium sulfate must be constantly monitored for all of the following except:A. loss of reflexesB. respiratory depressionC. hypotentsionD. cardiac arrestE. all of the aboveWWW.NYC.GOV/FDNY 13
Citywide CMEQUEENSFDNY - Bureau of Training:Date: September 21 st , 2005 1030 - 1430 hoursHost: John Freese, MDPlace: Fort Totten, Building #325Topic: Call ReviewNew York Hospital of Queens:Date: Last Tuesday of every Month 1800 – 2000 hoursPlace: 2nd Floor Conference RoomTopic: Call ReviewDate: Every Monday 1600 - 1730 hoursPlace: Lang AuditoriumTopic: Trauma RoundsCall George Benedetto @ (718) 670-2929Flushing Hospital:Date: September 19 th , 2005 1700 – 1900 hoursTopic: Geriatric Emergencies/Call ReviewHost: Robert Crupi, MDPlace: Flushing Hospital Board Room<strong>The</strong> Parkway HospitalDate: 3 rd Wednesday of every month 1830 – 2030 hoursTopic: Call ReviewHost: Dr Robert AquinoPlace: Board room (1 st Floor)Contact Robert Collins @ (718) 423-0808 - Food and Beverages ServedElmhurst Hospital:Date: September 7 th , 2005 1600 - 1700 hoursTopic: Grand Rounds/Call ReviewPlace: Auditorium A-122Queens Hospital Center:Date: September 8 th , 2005 1615 - 1815 hoursDate: September 22 nd , 2005 1615 – 1815 hoursTopic: Call reviewHost: Dr. Morgan's office in the EDSVCMC - St. Anthony’s School of Allied Health:Date: August 8 th , 2005 0800 – 1000 hoursAugust 25 th , 20051800 – 2200 hoursTopic: Call reviewHost: Dr. PolitiPlace: 175-05 Horace Harding Expressway, Fresh Meadow, NYContact the Division 4 ALS Coordinator, for more information on CME activities in Queens.WWW.NYC.GOV/FDNY 14
MANHATTANBellevue Hospital Center, Dr. MenloveTopic: Call Review - "Morning Report"Conference room (behind) ER - Bring two forms of IDEvery: Monday, Tuesday, Thursday and Friday0815 - 0900 hoursMetropolitan Hospital:Date: September 29 th , 2005 0800 - 1200 hoursHost: Jay Reich, MD and Joey Smith, MDPlace: Room B-135Topics: Neurological Emergencies, Pediatric Seizures, Call ReviewSt. Luke’s / Roosevelt University Hospital Center:Date: September 20 th , 2005 0800 – 1200 hoursHost: Dr. Philip Hew, MDPlace: St. Luke’s Hospital – Muhlenberg Conference Rm.# D - 4 th Fl.Topic: EMS Prehospital Stroke Evaluation and ManagementTo register call the Stroke Center @ 212 523-3144 – space is limited.Harlem Hospital Center, Dr. TrowersDr. Trower's OfficeTopic: Call ReviewEvery Thursday - <strong>Emergency</strong> Department1600 - 1730 hoursNYU <strong>Medical</strong> Center – 560 First Avenue:Date: September 26 th , 2005 1230 – 1700 hoursTopic: <strong>Emergency</strong> and Disaster Management Symposium:“Lessons learned from Israel”Place: Farkas AuditoriumRegistration is free but space is limited. To reserve a seat please email:George W. Contreras, MPH, MS, EMT-P - george.contreras@nyumc.orgFDNY/EMSC – Station 10:Date: September 23 rd , 2005 1730 – 2030 hoursTopic: Recognition and Management of Shock and Call ReviewHost: John Freese, MD – Division <strong>Medical</strong> DirectorFDNY/EMSC – Station 08:Date: September 27 th , 2005 2200 – 0100 hoursTopic: Recognition and Management of Shock and Call ReviewHost: John Freese, MD – Division <strong>Medical</strong> DirectorFDNY/EMSC – Station 04:Date: September 29 th , 2005 1600 – 1900 hoursTopic: Recognition and Management of Shock and Call ReviewHost: John Freese, MD – Division <strong>Medical</strong> DirectorFDNY/EMSC – Station 13:Date: September 30 th , 2005 0900 – 1200 hoursTopic: Recognition and Management of Shock and Call ReviewHost: John Freese, MD – Division <strong>Medical</strong> DirectorContact the Division 1 ALS coordinator to inquire about CME activities.WWW.NYC.GOV/FDNY 15
BRONXFDNY/EMSC - Station 18:Date: September 14 th , 2005 1600 - 1900 hoursHost: Dario Gonzalez, MD (Division Two <strong>Medical</strong> Director)Topic: Call ReviewCall Paramedic Steve Pilla @ (718) 829-6069 for more informationFDNY/EMSC - Station 55:Date: September 7 th , 2005 1400 - 1600 hoursHost: Dario Gonzalez, MD (Division Two <strong>Medical</strong> Director)Topic: Call reviewCall Paramedic Steve Pilla @ (718) 829-6069 for more informationFDNY/EMSC - Station 20:Date: September 7 th , 2005 1800 - 2000 hoursHost: Dario Gonzalez, MD (Division Two <strong>Medical</strong> Director)Topic: Call ReviewLocation: Jacobi Hospital - Room 1 West 10Call Paramedic Steve Pilla @ (718) 829-6069 for more informationNorth Central Bronx Hospital, Dr. Rajesh Verma:Place: CME Sessions held in the ED Conference RoomSt. Barnabas Hospital:Host: Juan Acosta, DOTopic: Call ReviewPlace: <strong>Emergency</strong> Administrative Office, 1 st FloorCall: (718) 960-5627 for more informationOur Lady of Mercy <strong>Medical</strong> Center:Date: 3 rd Thursday of every monthPlace: Department of Prehospital CareTopic: Call ReviewCall Jamie Dalton @ (718) 920-9962 for more informationContact Division 2 ALS Coordinators for more information on CME activitiesSTATEN ISLANDSt. Vincent's Hospital/ Catholic <strong>Medical</strong> Center-Staten Island:Date: September 14 th , 2005 1500 – 1630 hoursHost: Richard Westfall, MDSVCMC-EMS <strong>Medical</strong> DirectorTopic: Call Review – Mandatory Session for all SVCMC (Staten Island) StaffLocation: Sipp AuditoriumContact Division 5 ALS Coordinator for more information on CME activities.WWW.NYC.GOV/FDNY 16
BROOKLYNFDNY – Headquarters:Date: September 28 th , 2005 1600 – 1900 hoursTopic: Call reviewHost:John Freese, MDDivision One <strong>Medical</strong> DirectorPlace: 9 Metrotech Ctr., 4 th Floor (4W6 conference room)Call Christopher Swanson @ (718) 999-2674 for more informationLong Island College Hospital:Topic: Call ReviewPlace: Othmer Conference RoomCall Edward Caballero @ (718) 780-1859 for more informationMethodist Hospital:Date: Wednesday - Weekly 0830 - 1400 hoursTopic: <strong>Emergency</strong> Medicine Residency ConferenceCall (718) 780-5040 to confirm conference scheduleFlatlands Volunteer Ambulance Corps:Date: September 12 th , 2005 1900 – 2200 hoursTopic: Atypical Cardiac PresentationsHost: Barbara Gatton, MDPlace: Kings Plz. Shopping Mall Community Room (Flatbush Ave. and Avenue U)Wyckoff Heights <strong>Medical</strong> Center:Date: TBATopic: Call ReviewCall Jack Finkelstein @ (718) 386-7778 to confirmConey Island Hospital:Date: Every Wednesday 1000 -1100 hoursTopic: Call ReviewLocation: Dr. Soltani's trailer next to hospital <strong>Emergency</strong> RoomKings County Hospital:Date: Last Tuesday of every odd month 1800 - 2200 hoursHost: Dr. PiusPlace: E.R. Conference RoomCall: (718) 968-9750 for more informationBrookdale University Hospital and <strong>Medical</strong> Center:Department of <strong>Emergency</strong> MedicineCall (718) 240-5570 for more informationContact the Division 3 ALS coordinator to inquire about CME activities in Brooklyn.WWW.NYC.GOV/FDNY 17
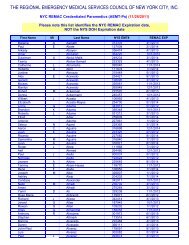
MonthJanuaryFebruaryMarchAprilMayJuneJulyAugustSeptemberOctoberREMAC OralExaminationPart A Part BTuesday Tuesday1/18/05 1/25/05Part A Part BTuesday Tuesday4/19/05 4/26/05Part A Part BTuesday Tuesday7/12/05 7/19/05Part A Part BTuesday Tuesday10/11/05 10/18/052005 REMAC Examination ScheduleREMAC Registration Starts Deadline Date NYS/DOH ExamsRefresher (for <strong>refresher</strong>s only)Wednesday01/26/05 12/1/04 12/31/04 01/2005Wednesday02/23/05 01/1/05 01/31/05Wednesday03/23/05 02/1/05 02/28/05 03/2005Wednesday04/27/05 03/1/05 03/31/05Wednesday05/25/05 04/1/05 04/30/05 05/2005Wednesday06/22/05 05/1/05 05/31/05 06/2005Wednesday07/20/05 06/1/05 06/30/05Thursday08/25/05 07/1/05 07/31/05 08/2005Wednesday09/21/05 08/1/05 08/31/05Wednesday10/19/05 09/1/05 09/30/05NovemberWednesday11/16/05 10/1/05 10/31/05 11/2005DecemberWednesday12/14/05 11/1/05 11/30/05 12/2005Paramedics with current REMAC certification must register for upcoming <strong>refresher</strong> examinations by calling (718)-999-7074 during the respective registration periodslisted above. All <strong>refresher</strong> exams are held at the EMS Division of Training starting at 0700 or 1800 hours. <strong>The</strong> REMAC Challenge Examination is given on a quarterlybasis, seating is limited so register early. <strong>The</strong> challenge exam consists of two parts: Part A is a written exam, Part B are orals. All parties interested in taking achallenge examination should plan accordingly (expired REMAC, inadequate CME) and submit their requests in writing to: FDNY - Office of <strong>Medical</strong> Affairs, 4thFloor, 9 MetroTech Center, Brooklyn, New York 11201 REMAC Protocols are available at www.nycremsco.org.WWW.NYC.GOV/FDNY18