Total Pancreatectomy - Memorial Sloan-Kettering Cancer Center
Total Pancreatectomy - Memorial Sloan-Kettering Cancer Center
Total Pancreatectomy - Memorial Sloan-Kettering Cancer Center
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
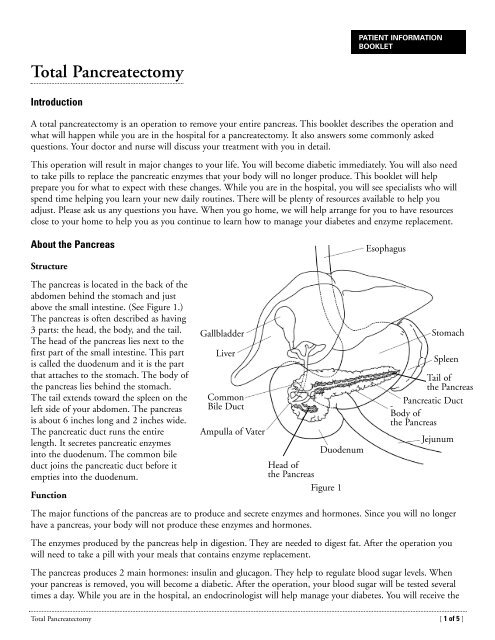
correct dose of insulin to keep your blood sugar levels within a saferange. A diabetes nurse educator will also visit you in the hospital.You and a care partner will slowly learn how to manage yourdiabetes. When you go home, you will need to have a doctor tomanage the diabetes. It can be your internist or an endocrinologist.You can discuss this with your surgeon.The ProcedureMost patients stay in the hospital for 7 to 10 days. Because of thelocation of the pancreas, it may be necessary to remove part of thestomach, the duodenum, the end of the common bile duct, thegallbladder, and the spleen. (See figure 2.)The surgeon will reconnectyour stomach and remaining portion of your common bile duct tothe jejunum. (See figure 3.) The jejunum is the second part of thesmall intestine. This ensures that food and bile flow into your smallintestines. The operation takes 4 to 6 hours.Scheduling your SurgeryOnce you decide to have surgery, it can usually be scheduled to takeplace within 1 or 2 weeks. Your doctor’s office will set up any additionaltests you may need. You will need to have other testing within 45 daysof your surgery. You may be able to have this testing right after you seethe doctor. If not, an appointment will be made for you.Preparing for your SurgeryThe spleen is part of your body’s immune system. If it will be removed,your doctor may want you to have a Pneumovax ® vaccination beforethe surgery. This will help protect you against certain types of infection.You can get it before the operation on a day when you come in to seethe doctor. You can also get it after your operation when you return fora follow-up visit.Your bowels must be clean before surgery. You may have to complete a bowel preparation procedure at home. Yournurse will give you these instructions and review what you must do.You will get a booklet called Getting Ready for Surgery. You will also get a fact card called Common MedicinesContaining Aspirin and Nonsteroidal Anti- Inflammatory Drugs. If you have not received these, please ask your nursefor them. Review them carefully. They explain what you should do before surgery. You must stop taking vitamin Eand any medicine that has aspirin in it 10 days before your surgery. You must stop taking drugs such as asibuprofen (Motrin ® or Advil ® ) 48 hours before surgery. The fact card lists all of the common medicines that havethese drugs. It also lists the medicines that you can take instead.After your SurgeryFigure 2Figure 3After your surgery, you will be taken to the Post Anesthesia Care Unit (PACU). You will spend the first nightthere. When you wake up after the surgery you will most likely have the following:stomachspleenpancreasduodenumremainingportion ofcommonbile ductremainingportion ofstomachjejunum• A tube called a nasogastric or NG tube. It is inserted into your nose and down to your stomach. This tubedrains the fluid that collects in your stomach. You will have the NG tube for one or more days. It may beuncomfortable.<strong>Total</strong> <strong>Pancreatectomy</strong> [ 2 of 5 ]
• A Foley ® catheter (a soft, flexible tube). It is inserted through your urethra into your bladder to drain urine.It is usually taken out on the second or third day after surgery.• An intravenous (IV) line in a vein in your neck or arm. It is used to give you fluids and medicines until youbegin drinking and eating again.• Compression boots on your legs. These boots help maintain blood flow. They gently squeeze your calf andthen relax to help prevent blood from clotting. They will be removed when you are out of bed walkingfrequently.• A small drain or tube in your abdomen. It drains excess fluid from around the surgical site.You will be helped out of bed to a chair soon after you are brought up to your room. You will then be encouragedto walk a short distance with help. Walking soon after surgery helps improve circulation, prevent blood clots, andstimulate bowel function. You will also need to do coughing and deep breathing exercises and use the incentivespirometer. These help to prevent pneumonia.Pain ControlYou will probably have a patient controlled analgesia (PCA) pump. It will be connected to your IV line. It lets yougive yourself prescribed doses of medicine safely when you need it to relieve your pain. The nurses in the PACUwill teach you how to use the PCA pump. Please speak to your nurse, doctor, or both, if you do not have enoughpain relief. It is very important that your pain is controlled. If it is not controlled, you will not want to walk,cough, and deep breathe. Doing these things helps you get better faster.Managing DiabetesThe thought of being diabetic may seem overwhelming. You will be one of millions who live with diabetes. Mostlive normal lives. During your hospital stay, you will see a diabetes nurse educator. This nurse will work closelywith you and your care partner to prepare you for managing your diabetes. You will be taught:• How diabetes affects your body.• What foods to eat and what ones to avoid.• How to check your blood sugar.• How to give yourself an injection of insulin.You must see a doctor close to home who will help you manage your diabetes after you leave the hospital. Anendocrinologist is a doctor who specializes in diabetes. We can help you find a doctor if you do not already haveone.DietYou will have liquids to drink on the first or second day after your operation. Your doctor may not want you tohave solid food until your bowels begin to work again. You will gradually advance to a diabetic diet. At first youwill not be able to eat the same portions of food you did before the surgery. Try to eat 4 to 6 small meals a day. Ifyou find that your appetite is not good at first, you may try a supplement. A dietitian will work closely with you toplan your diet before you are discharged. If you need to reach a dietitian after you go home, you can leave amessage at (212) 639-7312. Someone will return your call as soon as possible.You will be taking pancreatic enzyme replacement pills before every meal and with snacks. They help you digest fats.If you have diarrhea, tell your doctor or nurse. The dose of your enzyme pills may need to be adjusted. Finding theright dose may take weeks or even months.<strong>Total</strong> <strong>Pancreatectomy</strong> [ 3 of 5 ]
Many patients lose weight before the operation. You may keep losing during the first couple of weeks after thesurgery. You may regain the weight slowly as your appetite and capacity for food improves, but not everyone does.Your goal is to maintain your new weight.Going HomeYou will be ready to go home when you:• Can eat a regular diet.• Show no signs of complications.Your doctor will give you discharge instructions and prescriptions for any medicines you need. Your nurse willreview these instructions with you. You will get a printed copy to keep. The case manager will arrange for anyhome care before you leave. Many patients need visiting nurse services at home. In general, your firstpost-operative visit will be 10 to 14 days after you leave the hospital. This will be indicated on your dischargeinstruction sheet. Please call your doctor’s office to schedule the appointment.ExerciseExercise will help you gain strength and feel better. Walking is very good exercise. Check with your doctor or nursebefore resuming any strenuous exercise. Do not lift anything heavier than 10 pounds for 6 weeks. You may resumedriving three weeks after your surgery, as long as you are not taking any pain medicine that could make you drowsy.Special Instructions• A common complaint that patients have after this surgery is lack of appetite. Try to eat small amounts ofyour favorite foods often throughout the day. It is important to eat a balanced diet. It will help your bodyheal faster. It can help you keep your blood sugar levels within your target range. It is important that you donot skip entire meals because this could cause low blood sugar or hypoglycemia. Low blood sugar can be veryserious if it is not treated. The diabetes nurse educator will give you booklet on how to treat it and otherinformation to help you manage your diabetes. Always carry a source of sugar with you. It can be hardcandy or glucose tablets. Take it immediately if you have any symptoms of hypoglycemia.• Feeling tired (fatigue) is common after surgery, and may last for 6 to 8 weeks. This will improve slowly overtime. Try to increase your activity level every day to help manage your fatigue. Get up, get dressed, and walk.You may need a nap during the day, but try to stay out of bed as much as possible so you will sleep at night.Ask your nurse for the booklet, Handling Fatigue During and After <strong>Cancer</strong> Treatment, if you haven’t alreadyreceived it.• When you go home, you may still have some incisional pain that requires pain medicine. Take it as directedwhen you need it. Remember, your pain medicine will let you do the things that will help you gain strengthand recover faster. They are important. However, pain medicines cause constipation. Take extra fluids andfiber, and use a stool softener such as docusate (Colace ® ). As the pain lessens, acetaminophen (Tylenol ® ) maybe enough to control it.Call Your Doctor or Nurse If You Have:• Chills or fever of 101º F (38.3ºC) or higher.• Incisional redness or drainage.• Any sudden increase in pain or new pain.<strong>Total</strong> <strong>Pancreatectomy</strong> [ 4 of 5 ]
• Nausea and vomiting.• Diarrhea.• Constipation that is not relieved in 2 or 3 days.• Difficulty keeping you blood sugar levels within your target range.• Any new or unexplained symptom.ConclusionThe removal of your pancreas will result in some life-altering changes. There are many resources to help you adjust tothese changes. You can work with staff at MSKCC and out in the community. We hope this booklet has helped youunderstand your surgery and recovery. If you have any questions, please call your doctor or nurse.Doctor’s Name ________________________________Telephone ____________________________________Nurse’s Name _________________________________Telephone ____________________________________At night and on weekends, call (212) 639-2000 and ask to speak to the doctor covering your doctor.©2011 <strong>Memorial</strong> <strong>Sloan</strong>-<strong>Kettering</strong> <strong>Cancer</strong> <strong>Center</strong>1275 York Avenue, New York, New York 10065B-209<strong>Total</strong> <strong>Pancreatectomy</strong> [ 5 of 5 ]