suspected anaphylactic reactions associated with anaesthesia - aagbi
suspected anaphylactic reactions associated with anaesthesia - aagbi
suspected anaphylactic reactions associated with anaesthesia - aagbi
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
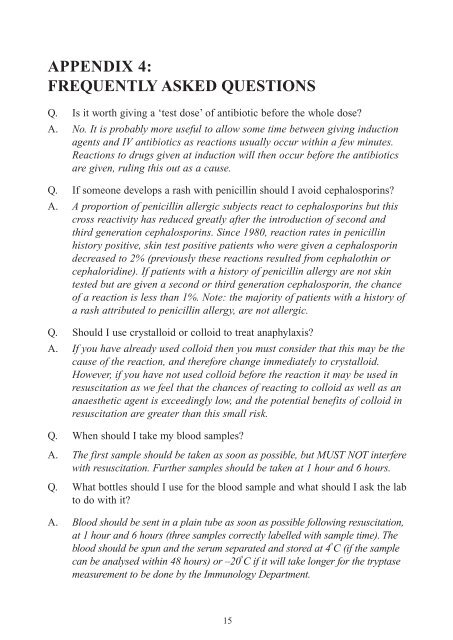
APPENDIX 4:FREQUENTLY ASKED QUESTIONSQ. Is it worth giving a ‘test dose’ of antibiotic before the whole dose?A. No. It is probably more useful to allow some time between giving inductionagents and IV antibiotics as <strong>reactions</strong> usually occur <strong>with</strong>in a few minutes.Reactions to drugs given at induction will then occur before the antibioticsare given, ruling this out as a cause.Q. If someone develops a rash <strong>with</strong> penicillin should I avoid cephalosporins?A. A proportion of penicillin allergic subjects react to cephalosporins but thiscross reactivity has reduced greatly after the introduction of second andthird generation cephalosporins. Since 1980, reaction rates in penicillinhistory positive, skin test positive patients who were given a cephalosporindecreased to 2% (previously these <strong>reactions</strong> resulted from cephalothin orcephaloridine). If patients <strong>with</strong> a history of penicillin allergy are not skintested but are given a second or third generation cephalosporin, the chanceof a reaction is less than 1%. Note: the majority of patients <strong>with</strong> a history ofa rash attributed to penicillin allergy, are not allergic.Q. Should I use crystalloid or colloid to treat anaphylaxis?A. If you have already used colloid then you must consider that this may be thecause of the reaction, and therefore change immediately to crystalloid.However, if you have not used colloid before the reaction it may be used inresuscitation as we feel that the chances of reacting to colloid as well as ananaesthetic agent is exceedingly low, and the potential benefits of colloid inresuscitation are greater than this small risk.Q. When should I take my blood samples?A. The first sample should be taken as soon as possible, but MUST NOT interfere<strong>with</strong> resuscitation. Further samples should be taken at 1 hour and 6 hours.Q. What bottles should I use for the blood sample and what should I ask the labto do <strong>with</strong> it?A. Blood should be sent in a plain tube as soon as possible following resuscitation,at 1 hour and 6 hours (three samples correctly labelled <strong>with</strong> sample time). Theblood should be spun and the serum separated and stored at 4 o C (if the samplecan be analysed <strong>with</strong>in 48 hours) or –20 o C if it will take longer for the tryptasemeasurement to be done by the Immunology Department.15