Sample Test Report - Rocky Mountain Analytical
Sample Test Report - Rocky Mountain Analytical
Sample Test Report - Rocky Mountain Analytical
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
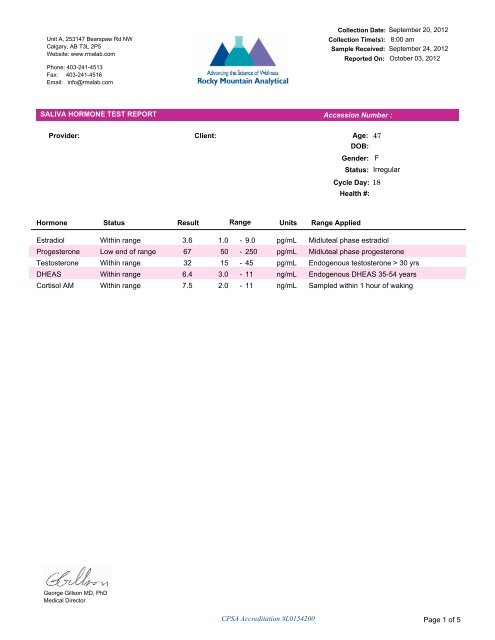
Unit A, 253147 Bearspaw Rd NWCalgary, AB T3L 2P5Website: www.rmalab.comPhone: 403-241-4513Fax: 403-241-4516Email: info@rmalab.comCollection Date: September 20, 2012Collection Time(s): 8:00 am<strong>Sample</strong> Received: September 24, 2012<strong>Report</strong>ed On: October 03, 2012SALIVA HORMONE TEST REPORT Accession Number :Provider: Client:Age: 47DOB:Gender: FStatus: IrregularCycle Day: 18Health #:Hormone Status Result Range Units Range AppliedEstradiol Within range 3.6 1.0 - 9.0 pg/mL Midluteal phase estradiolProgesterone Low end of range 67 50 - 250 pg/mL Midluteal phase progesterone<strong>Test</strong>osterone Within range 32 15 - 45 pg/mL Endogenous testosterone > 30 yrsDHEAS Within range 6.4 3.0 - 11 ng/mL Endogenous DHEAS 35-54 yearsCortisol AM Within range 7.5 2.0 - 11 ng/mL <strong>Sample</strong>d within 1 hour of wakingGeorge Gillson MD, PhDMedical DirectorCPSA Accreditation #L0154200 Page 1 of 5
Interpretation Accession Number :SymptomAllergiesAnxietyBleeding ChangesBone LossBreast SwellingBreast TendernessCaffeine ConsumptionCold Body TempDecreased Muscle MassDepressionDrowsinessExcess Facial/Body HairFatigueFeel 'Burned Out'Feel 'Pressed for Time'Feel 'Tired But Wired'Fibrocystic BreastsFoggy ThinkingHeadachesHeart PalpitationsHot FlashesIncontinenceIncreased AcneIrritabilityLoss of Scalp HairLow Blood SugarLow Sex DriveMemory LapsesMood SwingsMorning SluggishnessMuscle Aches/StiffnessNauseaNight SweatsOily SkinPoor Exercise ToleranceSleep DisturbancesTearfulnessUnable to CopeUterine FibroidsVaginal DrynessWater RetentionWeight Gain-HipsWeight Gain-Waist* Indicates symptom left blank.0 1 2 3RankPage 2 of 5
Interpretation Accession Number :The patient indicates some problems with sleep. Recognize that there is an optimum range for bedtime cortisol. Ifbedtime cortisol is too low, there is some evidence that normal sleep architecture is not established (insufficientREM sleep). Conversely, high bedtime cortisol is suppressive for melatonin, and may result in difficulty initiatingand sustaining sleep. It may be worth looking at the cortisol profile via saliva, depending on the severity of thesituation.Strictly speaking, vasomotor symptoms including hot flashes and night sweats reflect sympathetic nervous system(SNS) instability. Hence these symptoms are dependent on many factors such as stress, brain chemical levels(T3, serotonin, norepinephrine, melatonin, GABA, progesterone, estradiol and cortisol), and HPA axis function.They are not "pure" symptoms of estrogen deficiency (Prior J. Endocrine Rev 1998;19:397-428), and in fact, thesesymptoms may co-exist with symptoms of estrogen dominance. Vasomotor symptoms can be seen with manydifferent patterns of hormone imbalance, such as low progesterone, low testosterone, low or high DHEAS, highestradiol, high cortisol. (Note: A one year trial of progesterone cream demonstrated efficacy compared to placebo,for the control of vasomotor symptoms (Leonetti HB, Longo S, Anasti JN. Transdermal progesterone cream forvasomotor symptoms and postmenopausal bone loss. Obstet Gynecol. 1999 Aug;94(2):225-228).) Excessive useof progesterone (higher dose or unbroken daily usage) can also result in vasomotor symptoms by downregulationof estradiol receptors.Breast tenderness is listed as a complaint for this patient. Diffuse breast tenderness usually indicates anestrogen-progesterone imbalance, with high estradiol or low progesterone. Breast tenderness in the upper outerquadrants, toward the axillae, can be caused by too much progesterone relative to estrogen. For example , breasttenderness is often seen in women who have low salivary estradiol. When both estradiol and progesterone arelow, the mechanism for breast tenderness is not well understood. Caffeine and cortisol play a role. Lowtestosterone may also be a factor; research indicates that testosterone plays a role in balancing theproliferation-inducing effect of estradiol. (<strong>Test</strong>osterone inhibits estrogen/progestogen-induced breast cellproliferation in postmenopausal women. Hofling et al. Menopause 2007; 14:1-8.)October 2009 results of analysis of the Women's Health Initiative Study (whose participants received oral equineestrogen and oral medroxyprogesterone acetate) indicate that the women on this combination of therapies whohad breast tenderness were more likely to develop breast cancer over the course of the study. (New-Onset BreastTenderness After Initiation of Estrogen Plus Progestin Therapy and Breast Cancer Risk. Crandall CJ, et al. ArchIntern Med 2009;169(18):1684-1691. ) We do not know if this association can be extrapolated to women usinghuman identical hormone combinations, nor do we know whether breast tenderness in the absence of hormonetherapy has any negative connotation.*Symptoms commonly associated with hypothyroidism are present. These may include cold intolerance/feelingcold all the time, depression, weight gain, fatigue, headaches, thinning hair, and aching muscles, although not allthese symptoms will be present in every individual. Other symptoms (not inventoried here) can includeconstipation, dry skin and muscle cramps. (Baiser W, Hertoghe J, Eeckhaut W. J Nutritional Env Med2000;10:105-113.)Note that these symptoms may be present in the face of normal thyroid studies including TSH. This is known as afunctional deficiency state in which the blood level of a hormone is normal, but the action of the hormone at thetissue level is being blocked by other hormone imbalances. For example, unopposed/insufficiently opposedestrogen replacement (especially oral estrogen) and excessive estrogen dosing are common causes ofhypothyroid symptoms. High cortisol can oppose the action of T3 at the tissue level, whereas low cortisol can failto potentiate the tissue action of T3, even if there is sufficient T3. Many individuals with low cortisol complain ofhypothyroid symptoms.Note also that hypothyroid symptoms may persist despite supplementation with T4 (Synthroid, Eltroxin, L-throxine).In this situation, conversion of T4 to T3 (the more active form) may be blocked by high cortisol, heavy metal toxicityor deficiencies of nutrients including selenium, chromium and zinc.Some insight into hypothyroid symptoms in the face of normal serum thyroid testing might be had by assessing T3,T4 and selenium in a 24 hour urine specimen. For more information on this test, please contact the laboratory atPage 3 of 5
Interpretation Accession Number :866 370 5227.Symptoms of suboptimal estradiol usually include hot flushes, night sweats, depression, "brain fog", vaginaldryness (commented on elsewhere), low sex drive and bone loss, although not all these symptoms will be presentin every individual. If these symptoms are prominent, regardless of the estradiol level, it may be worthwhile thinkingabout zinc status in this patient. Zinc is an essential trace element necessary for the proper structure of estradiolbinding sites.The patient gave the sample before day 18 of her cycle. Progesterone might be low because she has not yetstarted the luteal surge.Low/low normal progesterone may result in diminished response to endogenous or supplemental estradiol, andmay impair tissue action of thyroid hormone. Symptoms which can accompany low progesterone include breasttenderness, weight gain, fluid retention, vasomotor symptoms, poor sleep, decreased libido, irritability and anxiety.A one year, placebo-controlled, randomized trial has demonstrated that topical progesterone is effective for relief ofvasomotor symptoms in early menopause. (Leonetti HB, Longo S, Anasti JN. Transdermal progesterone cream forvasomotor symptoms and postmenopausal bone loss. Obstet Gynecol. 1999 Aug;94(2):225-228)All other considerations aside, the ratio Pg/E2 is 18 for this patient. Regularly cycling women sampled in themidluteal phase generally have a ratio between 23 and 57. A lower ratio may indicate a relative deficiency ofprogesterone, even if the progesterone level is normal or higher than normal. If the sample was taken in thefollicular phase, this comment is not applicable.<strong>Test</strong>osterone is normal but the patient has complaints consistent with low testosterone. There is increasingawareness that symptoms are often related to the balance between many factors, as opposed to being directlydependent on one hormone level. For example, some symptoms may depend more on local conversion of DHEAto testosterone in target tissues such as the brain, in which case the measured DHEAS level may correlate betterto symptoms. Please do not hesitate to call the Medical Director at 866 370 5227 to discuss situations where thereis a mismatch between hormone levels and symptom patterns.Hair loss is a prominent symptom. Hair loss is often associated with high androgens, but there are other causes.Hair loss may also associated with decreased delivery of T3 to tissue. If the testosterone and DHEAS levels insaliva are low or normal in the face of hair loss, questioning about other signs and symptoms of decreased deliveryof T3 to tissue should be undertaken. Chronic hair loss is also associated with iron deficiency. One of the firstblood tests to become abnormal when iron is deficient is serum ferritin. Low ferritin-associated hair loss is wellrecognized. Some toxic or potentially toxic metals (arsenic, selenium, thallium) can also cause hair loss. A traceelement analysis of hair can be helpful to detect metal toxicity.DHEAS is within the normal range for the patient's age, but this may not be an optimal level for this patient. Bearin mind that for reference, in healthy individuals less than 25 years of age, the normal range for DHEAS is 6 to 18ng/ml for women, and slightly higher than this for men. Note that some some women less than 35 years of age,whose DHEAS is toward the upper end of their normal range might have complaints such as oily skin or facial hairgrowth.RMA database analysis (February 2008) indicates that a normal first morning cortisol sample is not predictive ofnormal cortisol levels throughout the rest of the day. The morning point is, in a sense, "disconnected" from the restof the day in this case, and symptoms will tend to correlate much better to the noon, suppertime and bedtimecortisol levels.It is still worthwhile measuring the morning point as a screen, because in contrast to a normal finding first thing inthe morning, a low morning cortisol is usually predictive of low cortisols throughout the rest of the day. Also, theratio of morning cortisol to morning DHEAS, C/DS, has been well characterized in saliva as a function of age, so itis sometimes helpful to compare the patient's ratio to age-appropriate norms.Morning cortisol is normal and symptoms which might suggest any significant problems with cortisol throughout therest of the day are not prominent.Page 4 of 5
Interpretation Accession Number :The ratio C/DHEAS is 1.2. This ratio normally increases with age. Based on a large in-house analysis of morethan 15,000 samples at ZRT Laboratory in Portland, the ratio at age 20 is approximately 0.6; at age 45 it is 1.0; atage 60 it is 1.5 and at age 75 it is 2.3. This is because DHEAS declines with age whereas morning cortisol staysthe same or increases slightly. If the ratio is higher than expected, based on the patient's age, this may beindicative of unbalanced adrenal function (cortisol too high or DHEAS too low). Factors which can contribute toimbalance include acute or chronic stress, obesity, metabolic syndrome/diabetes, and hypothyroidism. If the ratiois lower than expected for age, and DHEAS is within normal limits, this may simply be an indicator of healthy aging(i.e. preservation of DHEA output with age); however, a lower-than-expected ratio for age may also be due to lowcortisol, high DHEAS, or both.George Gillson MD, PhDMedical DirectorNote: The College of Physicians and Surgeons of Alberta considers saliva hormone testing andsome forms of bio-identical hormone replacement to be complementary medicine. Theinterpretation comments have not been evaluated or approved by any regulatory body. Commentaryis provided to clinicians for educational purposes and should not be interpreted as diagnostic ortreatment recommendations. *General treatment suggestions can be found in the <strong>Rocky</strong> <strong>Mountain</strong><strong>Analytical</strong> Resource Binder.Page 5 of 5