REDEFINING CASE MANAGEMENT - HRSA HIV/AIDS Programs
REDEFINING CASE MANAGEMENT - HRSA HIV/AIDS Programs
REDEFINING CASE MANAGEMENT - HRSA HIV/AIDS Programs
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
NOVEMBER 2008Why Now?The Connecticut ModelNashville, TNIndianapolis, IN<strong>REDEFINING</strong> <strong>CASE</strong> <strong>MANAGEMENT</strong>ONLINE RESOURCESI might only spend 15 minutes with the doctor every 3 months, but my casemanager calls me in between to see how I’m doing, remind me of doctor’sappointments, and to see if I need anything. We have a relationship.DID YOU KNOW?—An <strong>HIV</strong>-positive consumer, Nashville, TNEvery day, the interaction between client and case manager affects whetheran individual or family accesses and remains in primary medical care.Indeed, the relationship mentioned in the quotation above from theNashville consumer exists between people living with <strong>HIV</strong>/<strong>AIDS</strong> and casemanagers in community-based agencies, clinics, hospitals, homes, correctionalfacilities, and even parking lots all across the country.Medical case management is considered a core medical service.In 2006, the Ryan White <strong>HIV</strong>/<strong>AIDS</strong> Program spent approximately $135million on case management. 1Towards a typology of case management:ftp://ftp.hrsa.gov//hab/Typology.pdfApplying elements of the chronic caremodel to <strong>HIV</strong>/<strong>AIDS</strong> clinical care:moving CARE Act clients from intensivecase management toward selfmanagement:www.hab.hrsa.gov/special/ccm/ccm.htmLos Angeles Part A grantee standardsof care: www.hivcommission-la.info/soc.aspOregon Part B grantee standards ofcare: www.puc.state.or.us/dhs/ph/hiv/services/cmstdrds.shtmlOhio Part B grantee case managementoutcomes tool: www.careacttarget.org/library/tools/ohiooutcomemeasures.pdfPlease visit our Web site at www.hrsa.gov
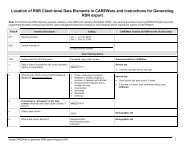
management services were expected to total approximately$83.5 million. These reports were submittedbefore the change in the legislation and may not capturesome types of medical case management previouslyconsidered part of ambulatory outpatient medicalcare. Also, treatment adherence services, now consideredpart of medical case management, were reportedseparately in 2006. In the 2008 program and fiscalreports, it is expected that a higher percentage of dollarswill be reported under the medical case managementcategory. 1The current service definition from the <strong>HIV</strong>/<strong>AIDS</strong>Bureau (HAB) defines the critical services included inmedical case management and the competenciesneeded by medical case managers (see box below). Itdoes not specify or require a terminal degree.The definitiontakes into account the variety of case managementmodels, settings, and difficult system changes that couldoccur with a more stringent definition.Yet, the change is much more than a new name for aset of service activities. To qualify as medical casemanagement, activities must be tied to providing, facilitating,and keeping a client in primary medical care. Therequirements include ensuring that medical case managersare part of clinical care teams to help clients navigatemedical care. They also include a comprehensiveMEDICAL AND NONMEDICAL <strong>CASE</strong> <strong>MANAGEMENT</strong>HAB DEFINES MEDICAL <strong>CASE</strong> <strong>MANAGEMENT</strong> as a range of client-centered services that link clients with healthcare, psychosocial, and other services. Coordination and follow-up of medical treatments are components of medicalcase management. Services ensure timely, coordinated access to medically appropriate levels of health andsupport services and continuity of care through ongoing assessment of clients’ and key family members’ needs andpersonal support systems. Medical case management includes treatment adherence counseling to ensure readinessfor and adherence to complex <strong>HIV</strong>/<strong>AIDS</strong> regimens. Key activities include (1) initial assessment of service needs;(2) development of a comprehensive, individualized service plan; (3) coordination of services required to implementthe plan; (4) client monitoring to assess the efficacy of the plan; and (5) periodic reevaluation and adaptation of theplan as necessary over the life of the client. It includes all types of case management, including face-to-face meetings,phone contact, and any other forms of communication.NONMEDICAL <strong>CASE</strong> <strong>MANAGEMENT</strong> includes advice and assistance in obtaining medical, social, community, legal,financial, and other needed services. Nonmedical case management does not involve coordination and follow-upof medical treatments, as medical case management does.3
clinical assessment of need that is reassessed andreevaluated periodically. The medical case managerneed not be located in the primary care facility, but he orshe must work closely and directly with the primary careprovider.Failure to address this paradigm shift could result incase management activities that are impermissibleunder core medical services, thus jeopardizing the abilityof providers to meet the requirement that 75 percent ofservice dollars be allocated to core medical services.Through the use of future evaluation projects, HABwill work to further define core competencies and identifymeasures to assess the quality of Ryan White casemanagement services.Collaboration Across <strong>Programs</strong>Connecticut and Medical Case Management<strong>HIV</strong> case management in the State of Connecticut isfunded by Ryan White <strong>HIV</strong>/<strong>AIDS</strong> Program Parts A–D.During FY 2007, 39 agencies received more than $4 millionin Ryan White <strong>HIV</strong>/<strong>AIDS</strong> Program funding to providecase management services. 3 Last summer, the Part Bprogram took the lead in convening representativesfrom Parts A–D to discuss the creation of statewidemedical case management standards. With the assistanceof a facilitator, the group began discussing currentmodels of case management and the needs of differentgeographical areas across the State to obtain a statewideperspective on the issue.At the time of the first meeting, the Part B providerhad not made final funding decisions for the year. ThePart B program had had internal discussions about medicalcase management centered on the need to createefficiencies in the model(s) of case management, thepossible use of an acuity scale to assess need, data collection,and the creation of performance indicators.Connecticut had begun a series of training meetings forcase managers entitled “Introduction to Medical CaseManagement.” The goal was to familiarize case managerswith the new medical model.Connecticut has two transitional grant areas (TGAs):Hartford and New Haven. (TGAs are cities with a totalpopulation of at least 50,000 and between 1,000 and1,999 reported <strong>AIDS</strong> cases in the past 5 years.) 2 The Stateincludes several urban, suburban, and rural areas.<strong>HIV</strong> service delivery is always challenging in ruralareas. Stigma, transportation, and a lack of services arejust a few of the major barriers affecting access andretention in care services. To address the need forprimary medical care, a significant portion of the medicalcare in Connecticut’s rural areas is provided byprivate physicians. The State also has a large network ofcommunity-based case managers in rural and urbanareas; many of them already perform some, if not all,service components of medical case management. RyanWhite <strong>HIV</strong>/<strong>AIDS</strong> Program providers across the Stateoften receive funding from more than one Ryan WhiteProgram component.Part A <strong>Programs</strong>Part A TGA programs in New Haven and Hartford hadalready developed service definitions, which wereapproved by their respective Planning Councils whenthis collaboration first began. Both Part A programsacknowledged that service definitions were only a smallpart of the work ahead; other tasks included the developmentof standards, the need for training amongproviders and clients, and discussions of the need to createor enhance linkages of medical case management toother service categories.They welcomed the opportunityto work with others in completing this task and madethe group aware of the role of the Planning Councils andother timeframes and deadlines specific to their localcity procurement and quality management processes.Part C ProvidersSeveral Part C providers discussed their work and therole of medical case managers in their programs.Because of the focus on primary care for the Part C programand its origins in the Bureau of Primary HealthCare, medical case management is the predominantmodel of case management. The processes and procedures,forms, standards, and best practices were alreadyin place, as was the requirement to spend at least 75 percentof funding on core medical services in place. ThePart C representatives agreed to share their knowledgeand expertise in the effort to create statewide standards.Part D <strong>Programs</strong>Part D programs are structured on a family-centeredmodel that allows providers to work with the affectedfamily member. Medical case management for theseprograms involves partnerships between case managementservice providers and nursing or clinical coordination.Some of these partnerships involve other RyanWhite-funded clinics. The close connection betweencase management and clinical care is integral to Part D4
programs and has also allowed them to develop andtrack clinical indicators for their patients.The Part D programs,too, offered to share their experience and knowledgewith the working group.Process and Results in ConnecticutOver the course of several meetings, the group agreedon a uniform definition of medical case managementthat contained all the critical activities as defined byHAB. The collaborative working group developed a setof core standards of care, with indicators and outcomesreflecting the minimum expectations for the delivery ofmedical case management in Connecticut for all Parts.Core standards are applicable in both community andclinic-based case management programs. Each Part wasgiven the option of adding to (but not deleting from)the core standards to meet the needs of its service populations.The standards will also go through an approvalprocess by the Part A planning bodies.The group agreedto reconvene in 6 months to discuss successes andchallenges and make adjustments to the core set ofstandards as needed at that time.Lessons LearnedHaving an outside facilitator help explain HAB’s expectationsprovided everyone with an opportunity to hearthe same message regarding the issue of medical casemanagement and thereby helped unify the grouparound a common understanding. This approachenabled the group to begin its tasks with clear directionand purpose. The process also enabled participants toshare their expectations and then come to a consensuson a set of medical case management standards andoutcomes that could be used statewide and adapted tothe specific needs of each Part and geographic area.The expertise of the Part C and D grantees helpedenrich the process and may have enabled the group tocomplete its tasks in less time than expected.These programsbrought important working knowledge of existingmedical case management practices and assessmenttools to the meetings. The “real-life” perspectivefocused discussions as the group brainstormed on whatto include as part of the core standards.The assistance of staff and program support wasinvaluable to the group in compiling and analyzing dataThe close connection between case management and clinical care is integral to Part D programs.5
from the programs; geomapping case managementservices; and tracking changes and updates as thegroup moved through the process of revising draft standards,outcomes, and indicators. The work group alwaysremained client centered in its approach and gave carefulconsideration to specific actions that might affectclients if those actions were included as standards.With the development of new medical case managementstandards, the State Department of PublicHealth has developed and initiated several trainings toincrease the core competencies of current case managersto provide medical case management services.These trainings (which include a component on the newstandards of care) are now part of a mandatory comprehensivetraining curriculum for all new Part B medicalApril of this year, the grantee hosted a 1-day medicalcase management meeting to help providers of casemanagement services understand the new definitionand discuss the key activities now included in the definitionof medical case management. The grantee wantedto create a welcoming environment where providers feltfree to raise issues and concerns to foster an honestdiscussion of case management services.Process and ResultsA facilitator helped manage the meeting and move thediscussion forward. The meeting was not held at a serviceagency, nor was it held at the grantee’s office. Aconference room at a city-owned golf course was theselected venue. Taking participants out of their officesTwenty percent of [Indianapolis] respondents indicated that case management,including medical case management, was the single service most necessary toensuring good health.case managers. The plan is to provide training for allmedical case managers funded by Part B. Those fundedby Ryan White Parts A, C, and D are invited to attend.Workgroup discussions have included approachingthe <strong>AIDS</strong> Education and Training Centers regardingsome of the training needs.The Part A Planning Councilsin New Haven and Hartford have acknowledged thatthis paradigm shift requires education and training fortheir current case managers and clinicians who may notbe accustomed to working with consumers in this manner.Thework group also acknowledged that consumersneed training on how to use medical case managerseffectively. Many consumers may have to adjust theirassumptions or let go of past experience with case managerswith the change to a chronic disease managementmodel.Medical Case Management and theContinuum of Care in NashvilleThe Nashville TGA program recently completed its firstyear of operations. During FY 2007, everything—includinghiring staff, forming a Planning Council, developingcontracts, and learning the Ryan White <strong>HIV</strong>/<strong>AIDS</strong>Program and legislation—had to happen quickly. Inhelped them focus more on the topics for discussion. Itwas also important that providers not feel that theywere being summoned to the grantee’s office to be reprimanded.Judi Grimes, the clinical quality manager forthe Nashville TGA, said, “I think the neutral territorychanged the climate, and then the timbre of the conversationbecame more acceptable for everyone.”In addition, the meeting opened with a panel ofthree Nashville consumers, who talked about their casemanagers, medical services, and the activities their casemanagers perform to help keep them in care. They presentedtheir impressions of case management andreminded the meeting participants of the importantrole these services play in the lives of clients.The session clarified the difference between medicaland nonmedical case management. Information onHAB’s intent and expectations regarding medical casemanagement was also shared with all participants.There was positive interaction between theproviders and a discussion of tasks that could be doneto move community- and clinic-based case managers inthe direction of HAB’s definition. Several good modelscurrently exist in the TGA, and future meetings will focuson the ability to replicate key components at otheragencies.6
Consumers need training on how to use medical case managers effectively. Many consumers may have to let go of their pastexperiences with case managers with the change to a chronic disease management model.The clinical quality manager shared a process fordeveloping standards of care. In addition, she discussedthe need for providers to assist the Planning Councilwith the development of standards as the granteemoves forward to define minimum expectations for thedelivery of all Ryan White <strong>HIV</strong>/<strong>AIDS</strong> Program Part Aservices.The need to continue meeting and working throughsome of the issues of medical case management, includingmodels for clinic- and non-clinic-based case managers,was clear. How medical case management shouldcoordinate with other <strong>HIV</strong> and non-<strong>HIV</strong> services stillneeds to be decided. Nashville is using the new servicedefinition as a catalyst to examine several of its <strong>HIV</strong> servicesby asking questions and collaboratively developingthe answers.Lessons LearnedThe session answered many questions, but PamSylakowski, Part A program director for the City ofNashville, says, “This is the beginning of a conversationregarding our continuum of care. The session raisedmany questions we have yet to explore—not only definingand understanding medical case management buthow it will coordinate with early intervention servicesand primary care to create a seamless system.”Sylakowski adds,“The answers to many of the questionsare obtainable, but only if we create the opportunitiesand the time to continue asking key questions inorder to distinguish the similarities and differencesbetween each of our providers of medical case management.The answers to the questions may also beaffected by the different populations each of the agenciesserves and whether the setting is urban, suburban,or rural”.Coordination and linkage with other services is animportant activity of medical case management, but theneed and level of coordination and linkage may varyaccording to the populations served by each agencyand locale.Participants agreed that having everyone togetherat the meeting, including consumers, nurses, case7
managers, the Part B grantee, and Planning Councilmembers, helped foster greater appreciation for eachother’s role.Part A and Part C Medical Case Managementin IndianapolisIn the Indianapolis 2002-2005 needs assessment, 20percent of respondents indicated that case management,including medical case management, was thesingle service most necessary to ensuring good health.The need for case management services ranked justslightly lower than dental services in the same series ofneeds assessments.Two different Indianapolis hospitalshistorically provided medical case management in theirclinics.Part A funds will expand the current Part C medicalcase management model to other area clinics that onlyhave had psychosocial case managers. The new medicalcase managers will work to decrease system fragmentationand the number of patients lost to care. One of thenew medical case management positions will focus onthe Hispanic population and will include a medical interpreteras part of the clinical care team to work withnewly diagnosed Spanish-speaking clients.Helen Rominger works as a nurse practitioner at theWishard Memorial Hospital infectious disease clinic,which receives Ryan White <strong>HIV</strong>/<strong>AIDS</strong> Program fundingunder Parts A, B, and C. “I welcome any effort to betterassist clients and am surprised to learn that my work isdefined as medical case management,” she says.Until recent conversations with the Part A programdirector, Rominger thought medical case managerswere social workers with specific clinical skills. She is thenurse who facilitates clinical issues. At Wishard,Rominger is part of a multidisciplinary care team thatincludes dentists and mental health professionals. Socialworkers, or care coordinators, are also part of the team.The care coordinators handle enrollment for third-partypayment programs, such as Medicaid and Medicare.They also facilitate referrals for external services outsidethe Wishard Care system.Sometimes, care coordinators identify medicalissues for the nurses or medical case managers.Rominger does not seem to be worried about servicecategory definitions or funding streams: “My job and myrole [are] to facilitate things for the patient, particularlythose things which are clinically related or affect theirhealth. It might include prescription refills, disabilitypaperwork, assessing the need for specialty care, handlingacute health issues, or just calling and following upafter a doctor’s visit.”Lessons LearnedTraining psychosocial case managers is critical toincrease the number of people who can provide qualitymedical case management services. An assessment ofthe current skill sets is a good starting point.Rominger also mentions that “many nurses and clinicalproviders will need training [because] they understandtheir roles and what they do but may not haveconsidered them in terms of medical case management.”Case management continues to be an essentialservice that enables individuals and families to receivecare. The change in the legislation emphasizes thatmedical case management should be used as an opportunityto examine this vital service. Many grantees arealready engaged in efforts to comply with HAB servicedefinitions and to ensure that medical case management—likeall Ryan White <strong>HIV</strong>/<strong>AIDS</strong> Program services—extends and enhances life for those most in need.REFERENCES1U.S. Department of Health and Human Services. Health Resourcesand Services Administration, 2006 CARE Spending, FY 2006.[Unpublished data].2Ryan White <strong>HIV</strong>/<strong>AIDS</strong> Treatment Modernization Act of 2006.Public Law No. 109-415. December 19, 2006. Accessed June 3,2008 at: ftp://ftp.hrsa.gov/hab/reauth06.pdf3State of Connecticut. Part B 2007 program document on casemanagement services. 2007. [Unpublished data].8