S - Robert Wood Johnson Medical School - Rutgers, The State ...
S - Robert Wood Johnson Medical School - Rutgers, The State ...
S - Robert Wood Johnson Medical School - Rutgers, The State ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
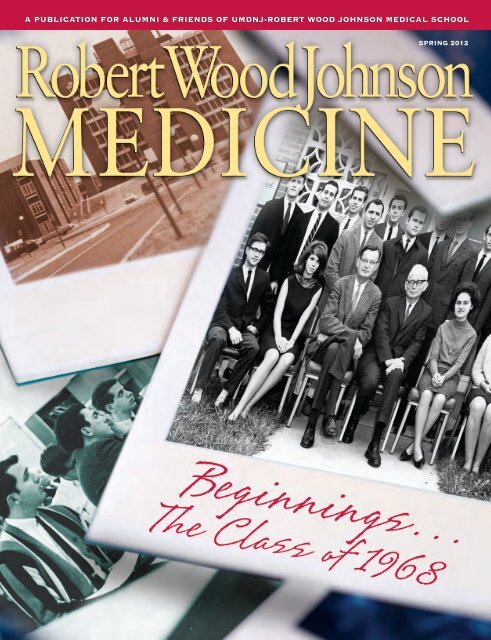
l e t t e r f r o m t h e d e a nDear Colleague,This issue of <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> Medicine features a close look at the school’s origins, whilelooking to its future. Renewing our appreciation of the history of the school provides a strongsense not only of where we have been and where we are, but, of greater importance is, where we are going.First Class: <strong>The</strong> Class of 1968 tells the story of the first 16 students to matriculate at what was then<strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong>. Interviews with members of that pioneering group offer a fascinating portrait ofthe early faculty, curriculum, and teaching facilities. <strong>The</strong>y also bring us up-to-date on the lives of theschool’s first alumni.Richard C. Reynolds, MD: A Clinician at Heart reintroduces us to one of our most respected, longserving,and beloved deans. Dr. Reynolds took the reins of the medical school during challenging timesand left a legacy that included our evolution as an academic medical campus.Four decades of RWJMS history are represented by the five alumni couples interviewed for SharedMemories, Shared Lives. Whether they are still actively involved in the day-to-day life of the medicalschool or practicing as far away as Tibet, they believe that starting their life together as students gavethem deep ties to the medical school.<strong>The</strong> Children’s Champion portrays the interactive clinical and researchstrengths of our children’s academic health campus, composed of four outstandinginstitutions: the Department of Pediatrics, with its 15 centers of excellence; theChild Health Institute of New Jersey; <strong>The</strong> Bristol-Myers Squibb Children’sHospital at <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> University Hospital (RWJUH); and thePSE&G Children’s Specialized Hospital.Bedside Ultrasound reports on the life-saving capabilities of this laptop-sizedtechnology. <strong>The</strong> new division of emergency and critical care ultrasound in theDepartment of Emergency Medicine provides skillful point-of-care scanning,improving patient care and allowing hands-on training of medical students andresidents.<strong>The</strong> Department of Radiation Oncology offers team-based expertise inGamma Knife Perfexion, the only radiosurgery built specifically for use on the brain. And, as describedin A Knife That Isn’t One, the Gamma Knife Center at RWJUH is the only location in New Jersey offeringpatients this advanced, non-invasive alternative treatment for intracranial problems.Please enjoy this edition of <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> Medicine.JOHN EMERSONSincerely,Peter S. Amenta, MD, PhDDean<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 1
New England Journalof Medicine Publishes FOCUSTrial FindingsJAMA Publishes TrialConfirming Legacy Effect ofHypertension <strong>The</strong>rapyNew research publishedin the NewEngland Journal ofMedicine online on December14, in advance of print, couldrefine post-operative carewhile preserving preciousblood supply levels. <strong>The</strong>study, “Transfusion TriggerTrial for Functional Outcomesin CardiovascularPatients Undergoing SurgicalHip Fracture Repair(FOCUS),” indicated thatusing a liberal blood transfusionstrategy in postoperativehip-surgery patientsdoes not improve patients’recoveries or reduce the rateof death.“<strong>The</strong> need for — and thequantity of — transfusionof red blood cells in postoperativepatients had notpreviously been evaluated ina large study,” says Jeffrey L.Carson, MD, Richard C.Reynolds Professor of Medicineand chief, division ofgeneral internal medicine,who was the FOCUS studychair. “This clinical trial isunique in that all patientswere considered very high riskdue to age and prior historyof cardiovascular disease.”<strong>The</strong> study, funded by theNational Institutes ofHealth, examined more than2,000 high-risk patients,who were randomly assigneda liberal or restrictive transfusionstrategy. At 30 and 60days post-surgery, there wasno difference between theSTEVE HOCKSTEINJeffrey L.Carson, MDgroups in thepatients’ inabilityto walkwithout assistance,nor wasthere a significantdifferencein the rate of death or heartattacks.— K.O’N.Afollow-up to thelandmark clinicaltrial “SystolicHypertension in the ElderlyProgram (SHEP)” hasshown that the use of antihypertensivedrug therapy isassociated with longer lifeexpectancy. <strong>The</strong> follow-upstudy, “Association betweenSurgeons Offer GroundbreakingAortic Valve ReplacementTechnique<strong>The</strong> Cardiovascular Center ofExcellence at <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> University Hospitaland <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong><strong>School</strong> was recently selected byEdwards Lifesciences to be one of thefirst sites in the nation to offer Transcatheter Aortic Valve Replacement(TAVR) since the procedure received FDA approval.Physicians at RWJMS will be among the first in the nation tooffer this groundbreaking aortic valve replacement technique,which provides hope for patients diagnosed withsevere aortic valve disease who are suffering from end-stageheart disease.TAVR allows a multidisciplinary team of cardiac surgeons,vascular surgeons, interventional cardiologists, and cardiacanesthesiologists to replace a patient’s diseased aortic valvewithout using traditional open-heart surgery. <strong>The</strong> patient’sheart continues to beat during the procedure, avoiding theneed for cardiopulmonary bypass.“This innovative technique provides a new option forpatients who have been diagnosed with severe aortic stenosisand need valve replacement, but who may be too high risk foropen heart surgery,” explains Mark B. Anderson, MD, professorof surgery and chief, division of cardiothoracic surgery.“TAVR can contribute to an enhanced quality of life for thesepatients, many of whom have no other options.”— K.O’N.Courtesy of Edwards LifesciencesJOHN EMERSONJohn B.Kostis, MDTreatment ofSystolic HypertensionandLong-TermSurvival,” waspublished onlineDecember14 in the Journal of theAmerican <strong>Medical</strong> Association.<strong>The</strong> study was led byJohn B. Kostis, MD, John G.Detwiler Professor ofCardiology, chair, Departmentof Medicine, andfounding director, <strong>The</strong>Cardiovascular Institute ofNew Jersey.SHEP, which lasted from1985 to 1990, showed thatchlorthalidone-based therapyfor hypertension preventedabout one out of two admissionsfor heart failure,one out of three strokes,and one out of four coronaryheart disease events.<strong>The</strong>re were no significantdifferences in mortality.<strong>The</strong> current study showedthat, compared to patientsreceiving the placebo, thegroup that received chlorthalidonetreatment survivedsignificantly longerwithout experiencing acardiovascular-relateddeath — approximatelyone day for every monthof anti-hypertensivetreatment.<strong>The</strong> study was funded inpart by the <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> Foundation.— K.O’N.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 5
w j m sNEWSIn MemoriamStephen F. Lowry, MD<strong>The</strong> RWJMS communitylearned with sadness ofthe passing in June 2011of Stephen F. Lowry, MD,professor and chair, Departmentof Surgery, and seniorassociate dean for education.(Please see Last Page,page 72.)Sumiko Inouye, PhD<strong>The</strong> RWJMS communitywas saddened by thepassing in August 2011 ofSumiko Inouye, PhD, associateprofessor of biochemistry.Dr. Inouye joined the facultyin 1987 and was a dedicatedscientist, teacher, and mentor.She was renowned for elucidatingthe signal transductionpathways in the soil bacteriumMyxococcus xanthus. Sheserved for many years as thefaculty mentor for the studentseminar series of the GraduateProgram in Biochemistry andMolecular Biology, providinginsight and guidance in hergentle manner to scores ofdoctoral students.Dr. Inouye was born inOsaka, Japan, in 1935. Herobituary notes that she wasthe sole woman admitted tothe Department of Engineeringat Osaka University in 1954and then studied organicchemistry in the <strong>School</strong> ofScience. In 2004, Dr. Inouyewas listed as one of theInstitute for ScientificInformation’s Most HighlyCited Researchers at UMDNJ.<strong>Robert</strong> Shelden, PhDWe report with sadnessthe death in November2011 of <strong>Robert</strong> M. Shelden,PhD. Dr. Shelden earned hisPhD in zoology from the Universityof Montana. He subsequentlywas a National Institutesof Health PostdoctoralFellow in Reproductive Endocrinologyand then a facultymember at Ohio <strong>State</strong>University.Dr. Shelden joined theRWJMS faculty in 1976 andretired as associate professor ofobstetrics, gynecology, and reproductivesciences. While atRWJMS, in 2006, he foundedthe research laboratory in hisdepartment and spearheadedthe development of the reproductiveendocrinology divisionto support clinical services. Helater led the expansion of thelaboratory to perform assaysand analyses that are essentialfor patients requiring advancedinfertility care. He is creditedwith the establishment of theIn Vitro Fertilization (IVF) Programat RWJMS; in 1983, theprogram saw the first baby bornin New Jersey through IVF.Dr. Shelden is fondly rememberedby his many colleagues,students, residents, and fellows,as well as the technicians hetrained in IVF techniques. Hepublished numerous researchstudies and abstracts. In2009, he was elected the firstpresident of the newly formedRWJMS Retired FacultyAssociation.AppointmentsBy KateO’NeillJOHN EMERSONJOHN EMERSONKathleen W. Scotto, PhD,professor of pharmacology, RWJMS,and vice president ofresearch, UMDNJ, wasappointed dean ofUMDNJ-GraduateKathleen W.Scotto, PhD<strong>School</strong> of BiomedicalSciences (GSBS). Dr.Scotto had served asinterim dean since February 2007.Dr. Scotto is internationally recognizedfor her work on the regulation ofdrug resistance genes that affect thesensitivity of cancer cells to therapeuticagents. Her laboratory at <strong>The</strong> CancerInstitute of New Jersey studies the regulationof alternative splicing, particularlyas it relates to the cancer phenotype.She holds several patents, iswidely published, and is a member ofa number of committees within thecancer field. She also serves on theeditorial boards of two cancer journals.Dr. Scotto earned her PhD in 1983from Weill Cornell Graduate <strong>School</strong> of<strong>Medical</strong> Sciences and recently receivedthe school’s Distinguished AlumnaAward. Prior to joining the RWJMS facultyin 2004, she served as associateprofessor of molecular pharmacologyand experimental therapeutics atMemorial Sloan-Kettering CancerCenter and as professor of pharmacologyat Fox Chase Cancer Center.Cheryl F. Dreyfus, PhD, professorand acting chair, Department ofNeuroscience and Cell Biology, wasappointed chair of the department. Dr.Dreyfus received herPhD in cell biologyat Cornell Universityand completed herCheryl F. Dreyfus,PhDpost-doctoral trainingat Einstein<strong>Medical</strong> College.Before joining the RWJMS faculty in1990, Dr. Dreyfus served on the facultiesof Columbia University College of6 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
JOHN EMERSONPhysicians and Surgeons andCornell University <strong>Medical</strong> College.Dr. Dreyfus is noted for herexceptional mentorship of medicalstudents, graduate students, andjunior faculty. She has served onthe Appointments and PromotionsCommittee, the AdmissionsCommittee, and a number ofsearch and review committees.Dr. Dreyfus’s internationallyrecognized work focuses on theregulation of brain cell developmentand death. She has publishedmore than 70 papers and14 book chapters and is a frequentspeaker and participant in nationaland international conferences andsymposia.Matthew Menza, MD, professorof psychiatry and neurology,was appointed chair of theDepartment ofPsychiatry. Hehad served asinterim chairMatthewMenza, MDsince November2007.Dr. Menzareceived his MD degree fromTemple University. His residencyat NYU/Bellevue <strong>Medical</strong> Centerwas followed by a fellowship inpsychosomatic medicine atMassachusetts General Hospital.A member of the faculty since1986, he served as chief of thedivision of clinical psychopharmacologyin the Department ofPsychiatry and as director ofconsultation psychiatry at <strong>Robert</strong><strong>Wood</strong> <strong>Johnson</strong> University Hospital.Dr. Menza’s research hasfocused on the psychiatric aspectsof Parkinson’s disease. He was thelead researcher on the first trialsponsored by the NationalInstitutes of Health of depressionin patients with Parkinson’s and onthe first multi-center, controlledtrial of insomnia in Parkinson’spatients. He maintains an activeclinical practice while pursuing hisresearch in general psychopharmacology.He has conducted morethan 50 clinical trials and writtenmore than 90 journal articles andbook chapters, and he co-editedPsychiatric Issues in Parkinson’sDisease: Practical Management.David Swee, MD, professor offamily medicineand communityhealth and associatedean foreducation, wasappointed associatedean for facul-David Swee, MDty affairs and faculty development.Dr. Swee earned his MD degreeat Dalhousie <strong>Medical</strong> <strong>School</strong> inHalifax, Nova Scotia, where hecompleted the first year of a residencyin family practice. He completedhis residency at Somerset<strong>Medical</strong> Center, in Somerville, andjoined the Department of FamilyMedicine in 1977. He wasappointed professor in 1994 andserved as department chair from1994 to 2005.At RWJMS and <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> University Hospital,Dr. Swee has held leadershippositions in many of the professionalorganizations and committeesin which he has served. Inaddition, he chairs the American<strong>Medical</strong> Association’s Council of<strong>Medical</strong> Education. His numerousawards include the 2009 <strong>Robert</strong>Raszkowski, MD, AccreditationCouncil for Continuing <strong>Medical</strong>Education Hero Award and theNew Jersey Academy of FamilyPhysicians 2009 Chair Award.STEVE HOCKSTEINResearchBy Kate O’NeillNews<strong>The</strong> National Institutes of Health awarded substantialfunding to the following members of the UMDNJ-<strong>Robert</strong><strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong> faculty:• Davide Comoletti, DVM,PhD, assistant professor ofneuroscience and cell biology,a five-year, $1.56 milliongrant for “Caspr2.”• Eunsung Junn, PhD, assistantprofessor of neurology, afive-year, $1,706,250 grantfor “Alpha Synclein Regulationby microRNAs.”• Jeffrey D. Laskin, PhD,professor of environmentaland occupational health, afive-year, $23,178,558 grant,in conjunction with <strong>Rutgers</strong> ,<strong>The</strong> <strong>State</strong> University of NewJersey, for the UMDNJ/<strong>Rutgers</strong> CounterACT ResearchCenter of Excellence.• Jianjie Ma, PhD, universityprofessor and acting chair,Department of Physiologyand Biophysics, a five-year,$1,755,000 grant for “MG53-Mediated Membrane Repair inMuscle Physiology andDisease.”• Sharon Manne, PhD, professorof medicine andchief, section of populationstudies, <strong>The</strong>Cancer Institute ofNew Jersey, a fiveyear,$4,310,150grant for “Intimacy-Enhancing Couples’Intervention forLocalized ProstateCancer.”• M. MaralMouradian, MD,William Dow Lovett Professorof Neurology and director,Center for Neurodegenerativeand NeuroimmunologicDiseases, a five-year,$2,419,938 grant for “ManipulatingGene Expression inthe Dyskinesias of Parkinson’sDisease.” This is a collaborativeproject with co-principalinvestigator Stella M. Papa,MD, assistant professor ofneurology, Emory University.• Mladen-Roko Rasin, MD,PhD, assistant professor ofneuroscience and cell biology,a five-year, $1,695,550grant for “Role of FirstNeocortical RNA-Operon inSpecification of NeocorticalProjection.”• Stuart L. Shalat, ScD, associateprofessor of environmentaland occupational medicine,a two-year, $903,198grant for “Validation of aRobotic Surrogate forMeasurement of Early ChildhoodPersonal Exposure.”• Zhiyuan Shen, MD, PhD,professor of radiationoncology andchief, division ofradiation cancerbiology, a five-year,$1,618,500 grantfor “AlternativeMechanisms to Inactivatep53 DuringOncogenesis.”— Continued onPage 8<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 7
Research— Continued from Page 7• Steven Silverstein, PhD,professor of psychiatry, afive-year, $2,198,520 grantfor “Perceptual OrganizationDysfunction as a Biomarkerof Schizophrenia.”• Iris G. Udasin, MD,professor of environmentalP u b l i s h e d R e s e a r c h :Newsandoccupationalmedicine and director,World Trade Center RespondersMonitoring and TreatmentProgram, Environmentaland OccupationalHealth Sciences Institute,a five-year, $3,882,489<strong>The</strong> following is a representative sample of articlesby RWJMS faculty members, residents, fellows, andstudents published in leading biomedical journals:• Konstantin E. Balashov,MD, PhD, associate professorof neurology, wasfirst author of “InterferonβInhibits Toll-like Receptor9 Processing inMultiple Sclerosis,” publishedin Annals ofNeurology 2010:68(6):899–906.• Jeffrey L. Carson, MD,Richard C. Reynolds Professorof Medicine andchief, division of generalinternal medicine, wasfirst author of “Liberal orRestrictive Transfusion inHigh-Risk Patients afterHip Surgery,” publishedin the New EnglandJournal of Medicine2011:365:2453–2462.• Jeanne M. Ferrante,MD, aassociate professorof family medicine andcommunity health, wasfirst author of “PrimaryCare Utilization andColorectal CancerOutcomes amongMedicare Beneficiaries,”published in Archives ofInternal Medicine 2011:171(19):1747–1757.• Yanxiang (Jessie) Guo,PhD, a post-doctoralfellow in the Departmentof Biochemistry,was first author of“Activated Ras RequiresAutophagy to MaintainOxidative Metabolismand Tumorigenesis,”published in Genes &Development 2011:25(5):460–470.• Bruce G. Haffty, MD,professor and chair, Departmentof RadiationOncology, was first authorof “Positive Sentinel Nodeswithout Axillary Dissection:Implications for theRadiation Oncologist,”published in the Journalof Clinical Oncology2011:29(34):4479–4481.In addition, Dr. Hafftywas a co-author withgrant for “Clinical Centerfor Monitoring Health inWorld Trade CenterResponders.”In another instance ofnoteworthy federal governmentfunding, the EnvironmentalProtection Agencyawarded a $1.2 millionNeil K. Taunk ’12 andSharad Goyal, MD,assistant professor ofradiation oncology, of“Radiation Recall 5 Yearsafter Whole-Breast Irradiationfor Early-StageBreast Cancer Secondaryto Initiation of Rosuvastatinand Amlodipine,”published in the Journalof Clinical Oncology2011:29(22):e661–e663.• Nadine Housri, MD,a resident in the Departmentof Radiation Oncology,was first author of“Ethics and the Law:Is <strong>The</strong>re Common Groundon Informed Consentfor Disparities inHospital Outcomes?,”published in Annals ofInternal Medicine2011:155(4):260–264.• Estela Jacinto, PhD,associate professor ofphysiology and biophysics,was first authorof “TFEBulous Control ofTraffic by mTOR,” inEMBO Journal 2011:30(16):3215–3216.grant to a six-investigatorteam led by <strong>Robert</strong> J.Laumbach, MD ’97, MPH,assistant professor of environmentaland occupationalmedicine, for “Effects ofStress and Traffic Pollutionon Childhood Asthma in anUrban Community.”• Matthew Marcello,PhD, a post-doctoral fellowin the Departmentof Molecular Genetics,Microbiology, andImmunology, was coauthorof “GermlineDetermination: Don’tMind the P Granules,”published in CurrentBiology 2011:21(4)R155–157.• Yoshihiro Yamaguchi,PhD, and Jung HoPark, respectively apost-doctoral fellow andgraduate student in theDepartment of Biochemistry,were co-authorswith Masayori Inouye,PhD, distinguished professorof biochemistryand member, Center forAdvanced Biotechnologyand Medicine, of “Toxin-Antitoxin Systems inBacteria and Archaea,”published in the AnnualReview of Genetics2011:45:61–79.Research ProfilesByLyndaRudolphPortriatsby JohnEmerson8 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
Shengkan (Victor) JinFocuses on Autophagy andType II DiabetesMore than 25% of the populationof the United <strong>State</strong>s is obeseand more than 8% is diabetic,according to the latest American DiabetesAssociation statistics. A primary cause ofdiabetes is obesity, which is the direct resultof the accumulation of massive deposits ofadipose tissue. In his lab, Shengkan(Victor) Jin, PhD, associate professor ofpharmacology, has spent the past two yearslearning if autophagy — a process duringwhich a cell cannibalizes its own damagedcomponents — could have an impact onadipose tissue and ultimately on Type IIdiabetes.“Each adipose cell, or adipocyte, has aunique structure,” says Dr. Jin. “Under themicroscope, it appears as one large cell,containing only one huge lipid droplet.”<strong>The</strong> unique structure prompted him and hiscolleagues to wonder where other cytosoliccomponents had gone. Knowing thatautophagy is involved in the degradationof cell components, the question became,could autophagy have an impact on adiposetissue?In a mouse model, one of these essentialautophagy-related genes was inactivated.<strong>The</strong>se gene-altered mice were compared tonormal, or wild-type, mice. Both types werefed a high-fat diet, similar to fast food.In the end, the normal mice had gained20 percent body weight, while the mutantmice — with the inactivated autophagyrelatedgene — did not gain any weightwhile eating the same amount of food.<strong>The</strong> team hypothesized that becauseof the inactivated gene, the mutant miceconverted white adipose tissue (WAT) cellsto brown adipose tissue (BAT) cells, whichburn fatty acids. This result demonstratedthat autophagy is critical for normal whitefatty tissue to form — a process known asadipogenesis.<strong>The</strong> mutant mice also appeared healthieroverall. In addition to being resistant to“Shengkan (Victor) Jin, PhDweight gain induced by a high-fatdiet, they had an increased sensitivityto insulin.Dr. Jin’s work is funded by two NIHR01 grants, totaling more than $2 million.Learning more about the role ofautophagy in adipose tissue could leadto more effective treatments for TypeII diabetes in the future.Estela Jacinto Studies Signaling Pathways for Cancer <strong>The</strong>rapyOur understanding of basic cellsignaling mechanisms can beapplied to many diseases,” saysEstela Jacinto, PhD, associate professorof physiology and biophysics. Currently,Dr. Jacinto is researching how cellularmetabolism is controlled bysignaling pathways. Howdoes the signaling controlthe growth of the cell? Whathappens to the cell whensignals go wrong? Why dotumors keep growing? Thoseare the questions Dr. Jacintois hoping to answer with herstudy.One of the signaling pathwayscritical for the regulationof growth of cellsinvolves a protein called TOR(a target of rapamycin). Thisprotein was identified based on the discoveryin the 1970s of the antibiotic rapamycin,which was initially used as an antifungaldrug. Rapamycin is now used as an immunosuppressant,in drug-eluting stents and as ananti-cancer drug. Dr. Jacinto is investigatinghow the TOR pathway can link nutrient signalsto other extracellular and environmentalsignals to promote growth.“We are only beginning to appreciate themany functions of TOR,” says Dr. Jacinto.“Rapamycin only inhibits some of thesefunctions.” <strong>The</strong> goal of Dr. Jacinto’s studyis to understand which functions can beinhibited by rapamycin, so that other drugscan be developed andpossibly targeted for moreeffective cancer therapy.Dr. Jacinto’s work wasrecently cited by the editorsof Science Signaling asa Signaling Breakthrough of2010. Her team showedthat mTORC2 — one of theprotein complexes thatare part of TOR — canassociate with ribosomes,elements within the cellmachinery that makeEstela Jacinto, PhDproteins. By binding nearthe “birth canal” of ribosomes, mTORC2modifies the emerging new protein tocontrol its quality and prevent prematuredegradation.Dr. Jacinto’s research is supported by anNIH grant of approximately $1.5 million aswell as other funding, including $750,000from Stand Up To Cancer and $50,000 fromthe Cancer Research Institute.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 9
Volunteer ProfileF a c u l t yM e m b e rVIJAYA RADHAKRISHNA, MD:A PATIENT-FOCUSED, LIFELONG LEARNERBy Kate O’NeillVijaya Radhakrishna,MD, clinical associateprofessor of pediatrics,is a lifelong learner. Now in her thirddecade of solo practice, Dr.Radhakrishna has seen enormouschange in the world of children’shealth. To stay current, she reservesevery Tuesday morning for theclinical case conferences presentedby the Department of Pediatrics.“It’s a great opportunity to meetmedical students, residents, andattending physicians and continuemy own learning,” she says.“Dr. Radhakrishna is the personwe want our pediatric residents toaspire to be, in learning, teaching,and staying open to new ideas,” saysDalya Chefitz, MD ’90, associateprofessor of pediatrics and chief, divisionof general pediatrics. She addsthat Dr. Radhakrishna’s weekly attendanceat case conferences sets anextraordinary example for studentsand residents, as do her contributionsto the discussions.In addition, for Dr. Radhakrishna,each day begins by exploring theonline “Daily Briefing” of the AmericanAcademy of Pediatrics. A strongadvocate for the importance of electronicmedical records (EMR), she personallyinvestigated the optionsbefore introducing pediatric-orientedEMR software to her practice.Pediatric residents from UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong>are among the young clinicians whogain clinical experience at Dr.Radhakrishna’s practice, and sheteaches on rounds at <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> University Hospital as well.“It’s important for our residents torealize that no one can possibly knoweverything,” says Dr.Chefitz. “Dr. Radhakrishnasets a great example bystaying in close contactwith our sub-specialistsand using our network ofconsultants wisely. Andshe’s just wonderful withchildren and families. <strong>The</strong>care she provides her hospitalpatients, from newborns toadolescents, is outstanding.”Dr. Radhakrishna earned hermedical degree and did her internshipnear Bangalore, in southernIndia, before moving to the United<strong>State</strong>s in 1977. She completedher residency in pediatrics atRWJMS, followed by a fellowship ininfectious diseases at Beth Israel<strong>Medical</strong> Center, in Newark. <strong>The</strong>n,focusing once again on pediatrics,she opened a solo practice inPiscataway; she has since added asecond practice, in East Brunswick.She recently marked the 32ndyear of her affiliation with RWJMS.Some of her newest patients are thethird generation of their families tocome under her care. “I feel thesame affection for them as I do formy own children,” she says.In addition to practicing generalpediatrics, Dr. Radhakrishna has twospecial interests: immunizations forforeign travel, and education andtreatment for attention deficithyperactivity disorder (ADHD). Ashyperactivity showed up more frequentlyamong her patients —sometimes three or four new casesin a week — she began studyingthe condition.“I learned that ADHD is a complexphenomenon, and it has beenVijaya Radhakrishna, MDa challenging learningcurve for me,”she says. “Many parentsdeny it. But asyou sit and talk tothem, they realizethey should be concernedand get help.”Dr. Radhakrishnahas been pleased to“Dr. Radhakrishna recentlymarked the 32nd year ofher affiliation with RWJMS....In addition to practicinggeneral pediatrics, shehas two special interests:immunizations for foreigntravel, and education andtreatment for attentiondeficit hyperactivitydisorder (ADHD).”see treatment options expanding,with alternatives such as nonstimulantmedication and a skinpatch simplifying life for many parentsand children coping with ADHD.To help parents and children accepttreatment for ADHD, she comparesit to getting eyeglasses: “It’s a clinicalproblem, and you simply need togive the brain the help it needs.”A devotee of music, dance, tennis,and cooking, Dr. Radhakrishnahas no plans for retirement and isdeveloping a new skill. Alreadyfamiliar with several Indian dialects,she is now learning Spanish. “I maynot be fluent,” she says, “but itshows respect to my Spanishspeakingpatients, and I know thatmakes them feel good.”<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 11
HIGHLightsBy KateO’NeillE D U C A T I O NAcademic Management Platform:“Perfection in the Works”<strong>The</strong> Office of InformationTechnology has designed anonline application tailor-madefor RWJMS. <strong>The</strong> Academic ManagementPlatform (AMP), featuring a userfriendlyinterface and centralized information,went live at the beginning ofthe 2011–2012 academic year.“AMP provides a way for studentsto easily navigate a curriculum that isbased on the integration of information,”says Andrew Orr ’15. He usesAMP frequently, finding it most valuablefor the way it intuitively combinesrequired readings, recordings of lectures,and presentation slides in oneself-contained interface.Lucy Mashas,manager of theweb and collaborativeservicesteam, led thedevelopment ofthe platform. Ms.Mashas providesan exampleof its easeof use andfunctionality:following a lecture,a student coulduse a computer,iPhone, or iTouch toaccess AMP through theRWJMS Web site. After reviewinga video of the lecture, the student couldnavigate to the block schedule, reviewcourse assignments and required readings,and access supplementary readingsand media resources.All lectures are stored on the site, sostudents can review them in new contextsat any time. “From the ability totake quizzes and listen to recorded lecturesto seeing our daily schedule andaccessing all resources for each lectureeasily, this site is perfection in theworks,” says Marissa Nadeau ’14.<strong>The</strong> Class of 2015in ProfileAs undergraduates, theClass of 2015 had botha strong academicrecord and a substantial backgroundin advocacy and service.In the United <strong>State</strong>s and overseas,they gained health care experiencein a wide variety of settings.<strong>The</strong> 130 members of theentering class were educatedat 57 different undergraduateinstitutions. Nineteen percentare alumni of <strong>Rutgers</strong>, <strong>The</strong> <strong>State</strong>University of New Jersey, and16 percent attended Ivy Leaguecolleges. Eighty percent had asingle or double major in thebiological or physical sciences,and six students were pre-acceptedas members of the MD/PhD program.Twenty-three percent wereborn abroad, while 63 percent arenatives of the tri-state area. Inaddition to English, they speak24 different languages, and,continuing the trend of the pastdecade, the majority — 57percent — are women.College AdvisingProgram InterconnectsRWJMS CommunityRWJMS introduced the CollegeAdvising Program in the firstsemester of the 2011–2012academic year. Within the program,three “colleges” serve academic,social, and professional purposes.Every student is assigned to one ofthree colleges, which also includefaculty members, alumni, and a deanfrom the Office of Student Affairs.<strong>The</strong> colleges are named in honorand memory of three faculty memberswho will be celebrated at an event thisspring: Pamela C. Champe, PhD;Parvin Saidi, MD; and <strong>Robert</strong> L.Trelstad, MD; <strong>The</strong> program was developedby Sonia Garcia Laumbach,MD ’99, assistant professor of familymedicine and community health andassistant dean for student affairs, andCarol A. Terregino, MD ’86, associateprofessor of medicine, interimsenior associate dean for education,and associate dean for admissions.“Students had been requestinga program that encourages meaningfulcommunication betweenstudents in all four years,” saysDr. Garcia Laumbach. “We developedthe program to meet thatrequest. We expect it to create asense of family and boost our senseof community.” In addition, theprogram provides new opportunitiesfor faculty and students to knowone another outside the classroom.Fall and spring events, beginningwith the 2012 Clash of the Colleges,will highlight the program’s socialcalendar.12 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
&A W A R D sHonorsDr. Amenta Elected to Board ofJoslin Diabetes CenterFaculty Named toLeadership in National Boardof <strong>Medical</strong> ExaminersThree faculty members were recently namedto leadership positions in the NationalBoard of <strong>Medical</strong> Examiners (NBME).Alfred F. Tallia,MD ’78, MPHPatricia Whitley-Williams, MDDavid Swee, MDJOHN EMERSONJOHN EMERSONSTEVE HOCKSTEIN• Alfred F. Tallia, MD ’78, MPH,professor and chair, Departmentof Family Medicine andCommunity Health, was electedto a four-year term as amember-at-large.• Patricia Whitley-Williams, MD,professor and interim chair,Department of Pediatrics, wasappointed chair of the NBME’sUnited <strong>State</strong>s <strong>Medical</strong> LicensingExamination Step 3 Computer-Based Case Simulation TestMaterial DevelopmentCommittee.• David Swee, MD, professor offamily medicine and communityhealth and associate deanfor faculty affairs and facultydevelopment, was named to athree-year term on the NBMEAdvisory Committee for<strong>Medical</strong> <strong>School</strong> Programs,representing the American<strong>Medical</strong> Association Councilon <strong>Medical</strong> Education.JOHN EMERSONPeter S. Amenta, MD, PhDPeter S.Amenta, MD,PhD, dean,has been elected toa three-year termon the Board ofTrustees of theJoslin DiabetesCenter. “I amhonored to workwith the Board of Trusteesand the leadership of theJoslin Diabetes Center,”says Dr. Amenta. “<strong>The</strong>center’s dedication tohelping improve the lives ofindividuals living with diabetesnow and in the futurethrough research, education,and care is a model forothers to emulate.”<strong>The</strong> center, affiliated withSupercomputer “Watson” SharesJeopardy PrizeAn IBM supercomputercalled Watsoncompeted with anddefeated some of thetop human contestantsin the history of thelong-running gameshow Jeopardy. IBMshared Watson’swinnings with sixscientists worldwide,including David J. Foran,PhD, professor of pathologyand laboratory medicine,chief, division of medicalinformatics, and director,Center for BiomedicalHarvard <strong>Medical</strong> <strong>School</strong>, isthe world’s largest diabetesclinic, diabetes researchcenter, and provider ofdiabetes education. Joslin isdedicated to ensuring thatpeople with diabetes havelong, healthy lives and tooffering real hope andprogress toward diabetesprevention and, ultimately,a cure.“We are delighted to haveDr. Amenta on board, as wecan learn from the advanceshe is directing in education,research, patient care, andcommunity health,” saysJohn L. Brooks III, presidentand chief executiveofficer of the Joslin DiabetesCenter.David J. Foran, PhDImaging at <strong>The</strong> CancerInstitute of New Jersey.Dr. Foran was awarded$75,000 to support hiswork on the IBM WorldCommunity Grid.JOHN EMERSON<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 13
&A W A R D sHonorsThomasNewmark, MDSidney Pestka, MDNorma B.Saks, EdDAnn M. Stock, PhDMelvinWeinstein, MDKIM SOKOLOFFJOHN EMERSONSTEVE HOCKSTEINJOHN EMERSONSTEVE HOCKSTEINFaculty Honorsand Distinctions• Thomas Newmark, MD, professorof psychiatry, was chosen aspresident-elect of the AmericanAssociation of PsychiatricAdministrators.• Sidney Pestka, MD, adjunctprofessor of molecular genetics,microbiology, and immunology,received the Distinguished ServiceAward from the InternationalSociety for Interferon and CytokineResearch. Dr. Pestka is the founderand chief scientific officer of thePBL InterferonSource, describedas the world’s leading source ofinterferon and related products.• Norma B. Saks, EdD, associateprofessor of psychiatry, assistantdean for educational programs,and director, Cognitive SkillsProgram, is chair-elect of theNortheastern Group onEducational Affairs of theAmerican Association of <strong>Medical</strong>Colleges. Her new role becomeseffective in the spring of 2013.• Ann M. Stock, PhD, professorof biochemistry, and associatedirector, Center for AdvancedBiotechnology and Medicine,was appointed an editor of theJournal of Bacteriology. She hasbeen a member of the editorialboard since 2003.• Melvin Weinstein, MD, professorof medicine and pathology andlaboratory medicine, received the2011 bioMérieux SonnenwirthAward for Leadership in ClinicalMicrobiology, presented by theAmerican Society of Microbiology.President Obama AppointsDr. Spitalnik to National Committeeon DisabilitiesPresidentBarackObamaappointedDeborah Spitalnik,PhD, professor ofpediatrics andexecutive director,<strong>The</strong> Elizabeth M.Boggs Center onDevelopmentalDisabilities, tothe President’sCommittee forDeborah Spitalnik, PhD People withIntellectual Disabilities. She is one of 15 people selectedfor this distinction. In his announcement, PresidentObama said, “<strong>The</strong>se fine public servants bring both adepth of experience and tremendous dedication to theirnew roles. Our nation will be well served by these menand women, and I look forward to working with themin the months and years to come.”JOHN EMERSONRWJMS Faculty Receive Ill AwardsTwoRWJMSfacultymembers willreceive 2012Edward J. Ill Jeffrey L. Carson, MD Jeffrey C. Brenner, MD ’95Excellence in Medicine Awards. <strong>The</strong> Outstanding<strong>Medical</strong> Research Scientist Award for Clinical Researchwill be presented to Jeffrey L. Carson, MD, Richard C.Reynolds Professor of Medicine and chief, division ofgeneral internal medicine. Jeffrey C. Brenner, MD ’95,adjunct instructor of family medicine and communityhealth, will receive the Edward J. Ill Physician’s Award.JOHN EMERSONSTEVE HOCKSTEIN14 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
B YLY N D AR U D O L P HP H O T O S B YJ O H NE M E R S O N<strong>The</strong>Children’sChampionASK ANY PARENT. WHENA CHILD IS ILL, EVERYTHINGELSE TAKES A BACK SEAT. ATFIRST THERE ARE QUESTIONS:What is the best place to treat mychild? Which specialists shouldwe consult? What it the prognosis?After the initial steps aretaken to seek care, when gapsbecome evident, other questionsemerge: Why do I have to leavethe area to get the best care?Why aren’t there new treatme n t s t o h e l p m y c h i l d ?<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 15
“This is a uniquecampus dedicatedto the health ofthe children ofNew Jersey,” saysPatricia Whitley-Williams, MD,professor andinterim chair,Department ofPediatrics, andphysician-in-chief,Bristol-MyersSquibb Children’sHospital atRWJUH.
<strong>The</strong>Children’sChampion<strong>The</strong> answers become even more important when youlook at the statistics. More children have chronicdiseases than ever before. Cancer is the leadingcause of death by disease among U.S. children 1 to14 years of age. One in every 150 children in theUnited <strong>State</strong>s has autism or a related disorder. Butthere is good news, particularly for the more than 2million children living in New Jersey. A new healthchampion is emerging — one that is gaining influenceand robustness to drive change that willimprove children’s lives.<strong>The</strong> Children’s Academic Health Campus in NewBrunswick is composed of institutions that individuallyhave significant medical might. <strong>The</strong> Departmentof Pediatrics at UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong><strong>Medical</strong> <strong>School</strong> offers care through 15 centers ofexcellence. <strong>The</strong> Bristol-Myers Squibb Children’sHospital at <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> UniversityHospital (RWJUH) is a 105-bed acute care pediatricfacility that’s in its tenth year of providing clinicallysuperior pediatric care. <strong>The</strong> Child Health Institute ofNew Jersey (CHINJ) is beginning its sixth year ofpursuing basic and translational research in childhooddiseases and has more recently upped its gamein recruiting investigators in the areas of inflammation,autism, stem cells, and genetics. <strong>The</strong> PSE&GChildren’s Specialized Hospital (CSH) — whichopened four years ago in New Brunswick — isconsidered to be the area’s preeminent provider forchildren with special needs, including those who areborn early, are developmentally delayed, or havelife-changing illnesses.<strong>The</strong>se institutions provide more than quality pediatriccare. <strong>The</strong>y are also about a passion to help andheal the youngest and most vulnerable among us.“This is a unique campus dedicated to the health ofthe children of New Jersey,” says Patricia Whitley-Williams, MD, professor and interim chair, Departmentof Pediatrics, and physician-in-chief, Bristol-Myers Squibb Children’s Hospital at RWJUH.Robotic Surgery SimulatorTrains Students and ResidentsSELDOM HAS AN EDUCATIONAL PROgramgenerated as much enthusiasm from medicalstudents as the new RoSS Robotic Simulator, a one-ofits-kindtraining station that students and residents useto practice robotic surgery in a lifelike environment.“We saw what this simulator could be, so we made acommitment to buy the RoSS when it was in its infancy,”says Joseph G. Barone, MD ’87, associate professorof surgery, chief, division of urology, and chief, <strong>The</strong>Bristol-Myers Squibb Children’s Hospital at RWJUH.Encouraging students to practice robotic surgery isof critical importance, as there is no doubt that it representsthe future of surgical medicine. This type ofsurgery typically achieves dramatically improvedpatient outcomes, and it is increasingly being soughtafter by discerning patients. At RWJUH, robotic surgeryis a popular option that patients can now choose,at their doctors’ discretion, for many gynecologic,chest, urological, and general surgeries.RWJMS students are quite aware of the popularityof robotic surgery. “<strong>The</strong>y’re already enticed to developthese skills. <strong>The</strong>y know this is what their patients will bedemanding from them in the future,” says Dr. Barone. M<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 17
Thomas F.Scanlin, MD,professor ofpediatrics, chief,division ofpulmonary medicine,and director,the Cystic FibrosisCenter at RWJMS,spearheads theefforts to establisha comprehensiveprogram to improvethe outcomes forcystic fibrosispatients ofall ages.18 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
<strong>The</strong>Children’sChampion“Our goal has been and continues to be to bringtogether the brightest minds to make a difference inthe lives of the children and their families who turn tous for care,” says Peter S. Amenta, MD, PhD, dean.<strong>The</strong> centralization is deliberate. <strong>The</strong> goal is to createa collaborative environment that will not onlyprovide exceptional clinical expertise, but also offeropportunities for close collaboration that can lead tothe creation of breakthrough therapies. An importantelement of this is the Department of Pediatrics, whichhas developed centers of excellence where children aretreated now, and where future clinicians are trained toserve as a catalyst for change in the evolution of care.Examples of progress are evident everywhere youlook.Centers of ExcellenceThat Fuel ProgressTHE BRISTOL-MYERS SQUIBB PEDIATRICRheumatology Center is involved in the diagnosisand management of a wide array of complexrheumatic diseases, including juvenile rheumatoidarthritis, systemic lupus erythematosus, reactivearthritis, systemic sclerosis, and regional musculoskeletalpain syndromes.<strong>The</strong> Pediatric Diabetes Center, established in 2003,has grown to include two clinicians, a certified diabeteseducator, and a research arm. <strong>The</strong> center looksat the autoimmune characteristics of relatives ofthose with type 1 diabetes — siblings, parents, andcousins — to determine their risk, so that they canenter prevention trials. Ian Marshall, MD, assistantprofessor and chief, division of pediatric endocrinology,emphasizes the importance of widespread educationabout pediatric diabetes. “We see type 1 diabetesin children of all ages after one to two years ofage,” says Dr. Marshall. “We work very hard toinvolve the extended family, the community, teachers,nurses, and coaches so they know as much asthey can about this condition, for the young patient’ssake.”<strong>The</strong> Cystic Fibrosis Center at RWJMS has establisheda comprehensive program to improve the outcomesfor cystic fibrosis patients of all ages, from newbornsto adults. Spearheading the efforts is Thomas F.Scanlin, MD, professor of pediatrics, chief, division ofpulmonary medicine, and director, the Cystic FibrosisCenter, who previously led the renowned program atthe Children’s Hospital of Philadelphia and theUniversity of Pennsylvania. Since Dr. Scanlin’s arrivalin 2005, outcome data for the CF Center in the CysticFibrosis Foundation National Registry have demonstrateda dramatic improvement in key measures ofnutritional status and pulmonary function.Prior to 2005, the results for many of these keymeasures were at or below the national average.Now the CF Center is consistently ranked amongthe top five out of 117 CF centers in the United<strong>State</strong>s. <strong>The</strong> program features a strong multi-disciplinaryteam practicing a coordinated, family-centeredapproach to this complex, chronic inherited disease.— Continued on Page 23Ian Marshall,MD, assistantprofessorand chief,division ofpediatricendocrinology,emphasizesthe importanceofwidespreadeducationaboutpediatricdiabetes.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 19
20 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
<strong>The</strong>Children’sChampion“Our goal hasbeen and continuesto be to bring togetherthe brightest mindsto make a differencein the lives of thechildren and theirfamilies who turnto us for care,” saysPeter S. Amenta, MD,PhD, dean, UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong><strong>Medical</strong> <strong>School</strong> (farleft), with Amy B.Mansue, presidentand CEO of PSE&GChildren’s SpecializedHospital and StephenK. Jones, FACHE,president and CEO,<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong>University Hospitaland <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> HealthSystem.Synergy in a Pediatric Focuswith Area HospitalsSTEPHEN K. JONES, FACHE, PRESIDENTand CEO, <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> UniversityHospital (RWJUH), agrees that collaboration is key.“I believe that much of our future success lies with uscontinuing to build relationships in our communities,and with other hospitals and physicians in NewJersey,” he says. “As we all work toward providinggreater value to our patients, strengthening these relationshipswill be incredibly important.”At RWJUH, pediatric patients are about 10 percentof overall inpatient admissions annually, and that figureclimbs to more than 25 percent of total activity inthe emergency departments. “We are definitely seeinggrowth in several areas of care — particularly in keysub-specialties within surgery,” says Mr. Jones. “Wework collaboratively with the medical school to identifyand obtain any needed resources to meet thesechanging community needs.”Children’s Specialized Hospital (CSH) openedPSE&G Children’s Specialized Hospital, a state-of-theart,60-bed inpatient unit, in New Brunswick in 2007.Here, children stay an average of 31 days, undergoingextensive rehabilitation for traumatic brain injury,spinal cord dysfunction, special infant care, chronicconditions, and sudden injuries. CSH was founded in1891 in Mountainside. In 1999, CSH became affiliatedwith the <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> Health System.“This is the only place in New Jersey where therehas been the investment to create one pediatric campuswhere you have research, teaching, and care of childrenboth for their immediate needs and for rehabilitation,working hand in hand,” says Amy B. Mansue, presidentand CEO of CSH. “<strong>The</strong> things possible today werealmost unfathomable ten years ago. Babies born at 23weeks are surviving and thriving on a regular basis. Tosupport a child with that level of care requires an integratedteam.”This is not just about saving lives. This is about ensuringthat the children served by CSH have quality of life.“We are fully committed to continuing to improve thehealth of New Jersey’s children,” says Ms. Mansue. M<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 21
Efforts to avoidpost-birth tragediesare led by ThomasHegyi, MD, professorof pediatrics,and pediatricpsychologistBarbara M. Ostfeld,PhD, professor ofpediatrics, whoserve as medicaldirector andprogram director,respectively, forthe Sudden InfantDeath SyndromeCenter ofNew Jersey.22 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
<strong>The</strong>Children’sChampionA cornerstone of the family-centered approach tocare is the Family Advisory Council, which meetsregularly with members of the CF Center team toreview clinical practice and policy in the center. Thisapproach serves as a model for a medical home forchronic pediatric lung diseases that provides outstandingoutcomes in cystic fibrosis.<strong>The</strong> maternal fetal medicine (MFM) program,a collaborative effort of RWJMS and RWJUH, contributesa breadth of expertise toward creating ahealthier population of children. Genetic counseling— particularly as it applies to identifying thoseat higher risk for having children with chromosomalissues — has become the focus of the division ofmedical genetics, headed by Susan Sklower Brooks,MMS ’73, MD, professor of pediatrics. Screeningsfor fragile X, Tay-Sachs disease, and cystic fibrosis,among others, and an examination of family historieshelp to determine if measures such as nutritionalsupplements to reduce risks can be taken. Effortsto avoid post-birth tragedies are led by ThomasHegyi, MD, professor of pediatrics, and pediatricpsychologist Barbara M. Ostfeld, PhD, professor ofpediatrics, who serve as medical director and programdirector, respectively, for the Sudden InfantDeath Syndrome Center of New Jersey. MFM is alsoinvolved in teaching and inspiring the next generationof pediatric specialists. <strong>The</strong> RWJMS NeonatalIntensive Care Unit fellowship program adds to thehigh level of knowledge and patient-focused careavailable in the unit.<strong>The</strong> Elizabeth M. Boggs Center on DevelopmentalDisabilities has taken a lead in providing a fulfillinglife for children who are born with Down syndromeand similar disabilities. <strong>The</strong> Boggs Center is NewJersey’s federally designated University Center forExcellence in Developmental Disabilities Education,Research, and Service. Deborah M. Spitalnik, PhD,professor of pediatrics and executive director of theBoggs Center, was recently named by PresidentBarack Obama as one of the 15 individuals to serveon the President’s Committee for People withIntellectual Disabilities. <strong>The</strong> Boggs Center educatesthe community and clinicians on how to work withpeople with developmental disabilities. “We arecommitted to promoting the understanding thatpeople with intellectual disabilities are active, valuableindividuals who can have a career and a sociallife, and can make a contribution to society,” Dr.Spitalnik says.<strong>The</strong> Institute for the Study of Child Developmentis a research center within the Department of Pediatricsand a collaborative effort in which pediatricsand psychology come together. <strong>The</strong> goal is to understandchildren by looking at emotional, social, andpsychological functioning, along with any environmentalinfluences that affect development. <strong>The</strong> instituteis involved in a myriad of efforts, among themresearching children with autism spectrum disorders,understanding the development of gifted children,and studying the effects of cocaine and otherdrugs on fetal emotional, psychological, and intel-“We arecommitted topromoting theunderstandingthat people withintellectual disabilitiesarevaluable individualswhocan make acontribution tosociety,” saysDeborah M.Spitalnik, PhD,professor ofpediatrics andexectutive directorof <strong>The</strong>Elizabeth M.Boggs Center onDevelopmentalDisabilities.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 23
“Roughly50 percent ofchildren withneurologicalproblems haveepilepsy,” saysJan Wollack,MD, PhD,associateprofessor ofpediatricsand neurology,andchief, childneurology andneurodevelopmentaldisabilities.24 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
<strong>The</strong>Children’sChampionlectual development. Several research studies arealso under way with Children’s Specialized Hospitalin the areas of autism and Asperger’s syndrome.According to Michael Lewis, PhD, UniversityDistinguished Professor of Pediatrics and Psychiatryand director, Institute for the Study of ChildDevelopment, “This isn’t all clinical research. Ourunit of study is the child embedded in his or herenvironment involving parents, peers, and thosewho interact with the child at school.” Dr. Lewisfeels that the academic campus has incredible potential,saying, “With an overarching connectednessand a structure that incorporates all of these entitiesaddressing the problems facing the children in NewJersey — autism, obesity, psychological health — theimpact could be profound.”<strong>The</strong> faculty of the Institute for the Study of ChildDevelopment includes Margaret Wolan Sullivan,PhD, associate director and professor of pediatrics;Dennis Carmody, PhD, professor of pediatrics;Barbara Young, PhD, associate professor of pediatrics;Jason Gold, PhD, assistant professor of pediatrics;Geraldine V. Oades-Sese, PhD, assistant professorof pediatrics; and Yiping Wang, PhD, assistantprofessor of pediatrics.<strong>The</strong> Child Neurology Center, headed by JanWollack, MD, PhD, associate professor of pediatricsand neurology, has grown to four clinicians, includingthree with additional training in epilepsy andneurology. “Roughly 50 percent of children withneurological problems have epilepsy,” says Dr.Wollack. While the group’s activities involve thediagnosis and management of a wide variety ofacute and chronic neurological illnesses, epilepsy isthe central focus. <strong>The</strong> state-of-the-art epilepsy programis fully operational and handles the most complexepilepsy cases, including continuous video-EEGmonitoring and epilepsy surgery evaluations.<strong>The</strong> group maintains a close working relationshipwith Rachana Tyagi, MD, assistant professor of sur-Treating Babies at RiskTODD ROSEN, MD, ASSISTANT PROFESSORof obstetrics, gynecology, and reproductive sciences,director, maternal-fetal medicine, and director,Regional Perinatal Center at RWJUH, has takena leadership position in establishing a centrallylocated, state-of-the art, multi-disciplinary maternal-fetalmedicine center that incorporatesadvanced treatments and diagnostic options forhigh-risk pregnancies. <strong>The</strong> center will give NewJerseyans a place to go for at-risk pregnancies sothat parents-to-be no longer have to travel out ofstate to receive this caliber of treatment.A team of physicians is devoted to fetuses in needof special care for congenital anomalies and birthdefects. “This inter-professional team treats highriskcases now referred to out-of-state hospitals,”says Dr. Rosen. “We are centrally located, we havethe Bristol-Myers Squibb Children’s Hospital atRWJUH to take care of these newborns, and wehave the required expertise to give babies the greatestchance of a healthy outcome.” M<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 25
“This is a uniquecollection ofentities togetheron one campusthat could havenational implications,”saysArnold B.Rabson, MD,Laura GallagherEndowed Chairof DevelopmentalBiology,professor ofmoleculargenetics, microbiology,andimmunology,pathology andlaboratorymedicine, andpediatrics, anddirector of theChild HealthInstitute ofNew Jersey.26 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
<strong>The</strong>Children’sChampiongery, a pediatric neurosurgeon, as well as with counterpartsin adult neurology and neurosurgery. <strong>The</strong>reare four pediatric neurologists and a pediatric neurosurgeonon the pediatric side and three epileptologistsand another neurosurgeon on the adult side.“We have a lot of firepower in one location,”observes Dr. Wollack.This collaboration has already resulted in a newprogram that uses continuous EEG monitoringwith quantitative trending in patients with subarachnoidhemorrhage to give advance warningof the onset of vasospasm, which is the majorcomplication of that disorder and can lead to furtherbrain damage and even death. Lessonslearned in such joint programs will help to transformclinical protocols for pediatric patients.Two of the four new research recruits at CHINJare neuroscientists, which Dr. Wollack sees as anexciting match to the expertise in the clinicalarea.Sharing the Wealthof KnowledgeIT’S NOT ENOUGH TO DO; TEACHINGthe next generation is also a priority. Identifyinggaps is leading to new programs. Kapila Seshadri,MD, associate professor of pediatrics, saw a need foradvanced education for people interested in thedevelopment and behavior of children. She created afellowship program to fill that need. This year thefirst fellow started taking the three-year program,which is accredited by the Accreditation Council forGraduate <strong>Medical</strong> Education, and is matriculating ina curriculum that includes clinical care, didactic conferences,self-learning, and research. Dr. Seshadri,who directs the program, works in close collaborationwith Frank Castello, MD, associate professorand vice chair, Department of Pediatrics, and medicaldirector, Children’s Specialized Hospital. “What wedo really does touch and affect the children in all ofthe entities of the health campus,” says Dr. Seshadri.A Renewed Dedicationto ResearchWHAT IS NOT VISIBLE, BUT IS OBVIOUSin the minds and hearts of all involved, is a deepdesire to make things happen. Nowhere is that moreevident than in the attitude of Arnold B. Rabson,MD, Laura Gallagher Endowed Chair of DevelopmentalBiology, professor of molecular genetics,microbiology, and immunology, pathology and laboratorymedicine, and pediatrics, and director ofCHINJ.“This is a unique collection of entities together onone campus that could have national implications,”says Dr. Rabson. “<strong>The</strong> potential to have interactionamong all of us is exciting. <strong>The</strong> challenge is to developa set of research activities and a research facultywho are interacting with the clinical faculty, andmove into translational clinical activity.”<strong>The</strong> vision is broad: to do research on children’sKapilaSeshadri, MD,associateprofessor ofpediatrics,saw a needfor advancededucationfor peopleinterested inthe developmentandbehavior ofchildren.She createda fellowshipprogramto fill thatneed.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 27
Mantou Bhaumik, PhD,assistant professorof pediatrics, provides ashared resource thatmakes mouse modelsof human diseasenot only for theChild Health Instituteof New Jersey but also for<strong>The</strong> Cancer Instituteof New Jersey; <strong>Rutgers</strong>,<strong>The</strong> <strong>State</strong> Universityof New Jersey; andPrinceton University.28 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
<strong>The</strong>Children’sChampiondiseases that has an impact on treatment and prevention.Research will take place in four majorareas. <strong>The</strong> first is inflammation, immunity, and infection.“Most human disease has inflammation involvedin it,” says Dr. Rabson. <strong>The</strong> second is neurodevelopmentand autism. “Since Children’s SpecializedHospital has a large population of very wellcharacterized autistic children, there is a lot of activitywe can build on here,” says Dr. Rabson.“Coupled with the neuroscientists and psychologistsin the Department of Pediatrics and RWJMS, thereis a chance to synergize.” <strong>The</strong> third is an amalgam ofstem cells and pediatric cancers — important sincealmost all pediatric cancers are diseases of stem cells.“We’re studying the ability to use the programmingand differentiation of stem cells to understand diseaseand for therapy and also to determine how theseproperties of stem cells relate to pediatric cancer,”says Dr. Rabson. <strong>The</strong> fourth area of focus is childhoodobesity and metabolism.Ten Laboratorieswith UnlimitedCollaboration PotentialAS O F N O V E M B E R 2 0 1 1 , C H I N J I Soccupied by ten active research laboratories. Dr.Rabson’s lab is focused on human retroviruses,including HIV and a leukemia-causing virus calledHTLV-1, and also on the study of genes involved inthe development of blood cells and leukemia.Mantou Bhaumik, PhD, assistant professor of pediatrics,provides a shared resource that makes mousemodels of human disease not only for CHINJ butalso for <strong>The</strong> Cancer Institute of New Jersey;<strong>Rutgers</strong>, <strong>The</strong> <strong>State</strong> University of New Jersey; andPrinceton University. Amale Laouar, PhD, assistantprofessor of surgery, heads a biomedical researchteam working on understanding how the gutrecognizes foreign antigens — and determiningwhich of these foreign substances are “good”(“good” food and “good” bacteria) and which are“bad” (such as diseasecausing microbes). <strong>The</strong> workhas implications for celiac disease, inflammatorybowel disease, and cancer.Three other laboratories have moved into CHINJ.Sevgi Gurkan, MD, assistant professor of pediatricsand a pediatric nephrologist, studies nephrotic syndrome,which is the second-leading cause of renalfailure in childhood. Dr. Gurkan’s roots are inresearch: “Although I was hired as a clinician here,during my Mt. Sinai fellowship I was active inresearch.” Her study is investigating both the geneticand immune triggers for nephrotic syndrome in twotosix-year-olds and in teens — where the diseaseprogresses at a rapid pace.Yufang Shi, DVM, PhD, professor of moleculargenetics, microbiology, and immunology, is investigatinghow cell death happens in the immune system— work that has major implications for all autoimmuneand inflammatory diseases, including asthma.His second major activity, for which he now holds aAmale Laouar,PhD, assistantprofessor ofsurgery, headsa biomedicalresearch teamworking onunderstandinghow the gutrecognizesforeign antigens.<strong>The</strong> work hasimplications forceliac disease,inflammatorybowel disease,and cancer.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 29
“Looking at autism froma molecular and cellularpoint of view will generatenew information aboutthe possible cause ofautism, helping translationalmedicine and eventuallydrug design,” says DavideComoletti, DVM, PhD,assistant professor ofneuroscience andcell biology.30 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
<strong>The</strong>Children’sChampionleadership role in the world, studies how certainkinds of stem cells regulate the immune system. “Wefound there is an inflammation measure somewherein the body and that stem cells migrate to thatinflammation,”says Dr. Shi.“Those stem cells releaseimmunosuppressents, which in turn release growthfactors to initiate repair.” <strong>The</strong> potential may be todevelop this research into cellular therapeutics fordifferent types of pediatric disease processes.Chi-Wei Lu, PhD, assistant professor of obstetrics,gynecology, and reproductive medicine, is workingwith induced pluripotent stem cells (stem cells notderived embryonically but that are converted fromsomatic cells). She is investigating trophoblast cellsfound in the placenta and how they influence thedevelopmental process. She is also studying genesand pathways that play a role in pediatric malignanciesand has projects related to Down syndrome andother chromosomal disorders as well. “I look at myresearch as the seeds — I look forward to reachingout to work with other labs to bring resources toapply to developmental conditions,” says Dr. Lu.Four new scientists have joined the CHINJ faculty.Derek Sant’Angelo, PhD, associate professor ofpediatrics, who was recruited from Memorial Sloan-Kettering Cancer Center, is an immunologist whostudies how transcription and gene regulation workin the immune system, with implications for manypediatric diseases such as asthma, juvenile diabetes,and cancer. Lisa Denzin, PhD, associate professor ofpediatrics, also from Sloan-Kettering, is studyinghow a foreign molecule is presented as an antigen —how it’s seen by the immune system, which thenreacts against it. Her work has direct implicationsfor many autoimmune diseases and also involvesstudying Type 1 juvenile onset diabetes. A new set ofprojects recently undertaken by Dr. Denzin includesstudying cell-cycle regulation in leukemias.In the neurodevelopment and autism area, DavideComoletti, DVM, PhD, assistant professor of neuroscienceand cell biology, is investigating the neurexinand neuroligin proteins — molecules at thesynapse between two neurons that are among themost commonly implicated genes in autism. As astructural biologist, he is studying how these proteinswork, how their structure influences their function,and what are the biochemical consequences ofthe mutations associated with autism. “Looking atautism from a molecular and cellular point of viewwill generate new information about the possiblecause of autism, helping translational medicine andeventually drug design,” says Dr. Comoletti.Zhiping Pang, MD, PhD, assistant professor ofneuroscience and cell biology, who was recruitedfrom Stanford University, is an expert on neuronalsynapse. Widely published, Dr. Pang’s work studiesthe molecular mechanisms that underlie how braincells convey information from one to another. Hisinterest has taken him into a new area: a series ofneural connections in the hypothalamus in the brainthat are involved in the regulation of feeding, satiety,and energy homeostasis. His ultimate goal is toA new CHINJmember, DerekSant’Angelo,PhD, associateprofessor ofpediatrics, is animmunologistwho studieshow transcriptionandgene regulationwork in theimmunesystem, withimplicationsfor manypediatricdiseases suchas asthma,juvenilediabetes, andcancer.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 31
<strong>The</strong>Children’sChampionZhiping Pang,MD, PhD,assistantprofessor ofneurocience andcell biology, isan expert onneuronalsynapse.understand how the human brain controls energyhomeostasis and why misregulation of hypothalamicneural circuitry leads to abnormal eating disorderssuch as anorexia, hyperphagia, and obesity.Dr. Pang also has been recognized for developingnew techniques for regenerative medicine, convertinghuman skin cells into functional neurons bydefined factors. This could apply, for example, to achild with a neurological disease lacking effectivetherapy — the potential could exist to convert thepatient’s skin cells to neurons in a culture dish, modelingthe disease to screen for effective therapies.All the components are in place. Knowledge is ashared resource. Goals are collaborative. <strong>The</strong> term“team” has never been more appropriate.For the 2 million children in New Jersey, thefuture holds more promise than it ever has. M32 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
[ Special Section ]BeginningsOurAlumni issue draws its theme from thethree articles in this section. “FirstClass: <strong>The</strong> Class of 1968” takes readers back to 1966,when the first group of future alumni matriculated at whatwas then <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong>. <strong>The</strong> graduates of thatclass became the original 15 alumni; today the AlumniAssociation represents more than 5,000 graduates. RichardReynolds, MD, served as dean from 1979 to 1987. He brilliantlyguided the school through a succession ofcrossroad decisions that determined its future as anacademic medical campus and defined its missionin community health. <strong>The</strong> five alumnicouples interviewed for “Shared Memories,Shared Lives” graduated between1973 and 2005. <strong>The</strong>ir common memoriesof the medical school enrich their lives.<strong>The</strong>ir reminiscences about each decade atthe school enrich ours.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 33
[ Beginnings ]FirstClass<strong>The</strong> Classof 1968a new medical school was born on the banks of the Raritan. Four yearsIn1966,in the making, <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong> (RMS) was the brainchild of MasonGross, PhD, then president of <strong>Rutgers</strong>, <strong>The</strong> <strong>State</strong> University of New Jersey. Dr. Grossrecruited DeWitt Stetten, Jr., MD, in 1962 to serve as the school’s founding dean.In the mid-20th century, the United <strong>State</strong>s was hometo only 87 medical schools. But by 1966, a surge instate and federal funding for medical education hadchanged the landscape, and 14 new medical schools wereDeWitt Stetten, Jr.,MD,a noted biochemist, had a distinguishedcareer in both academic medicineand research. Prior to acceptingthe leadership position as deanof RMS, he had taught at Harvard<strong>Medical</strong> <strong>School</strong>. In addition, he hadserved as associate director in charge of research andchief of the section on intermediary metabolism at theNational Institutes of Health (NIH)/National Instituteof Arthritis and Metabolic Diseases.In 1970, Dr. Stetten returned to the NIH, where heled the National Institute of General <strong>Medical</strong> Science.In 1986, the NIH established the DeWitt Stetten, Jr.,Museum of <strong>Medical</strong> Research, which preserves andinterprets the material culture of the scientific workof the NIH through physical and virtual exhibits.<strong>The</strong> NIH further honors Dr. Stetten by offeringthe Stetten Fellowship in the History of BiomedicalSciences and Technology of Medicine.in the planning stage. In that competitive environment,Dr. Stetten successfully recruited six worldclassscientists and two renowned physicians ashis department chairs. <strong>The</strong>y, in turn, recruited themedical school’s first faculty, which totaled 42.In characteristic hands-on style, Dr. Stettenpersonally oversaw the construction projectsthat would become the first teachingfacilities at RMS, a freestanding medicalschool. A multi-purpose teaching laboratoryhoused all classrooms, lockers, a study area,and all laboratories except the anatomy lab, an innovationthat the new dean conceived as a pilot concept inmedical education. In 1966, the cornerstone was laid forthe Research Tower, which was completed and dedicatedfour years later.At Dr. Stetten’s suggestion, the walls of the teachinglabs were hung with enlargements of the “MuscleMen,” woodcuts from De Humani CorporisFabrica, Andreas Vesalius’s 16th-century text thatinaugurated the modern study of anatomy. In 1970,when the main building of the medical school wascomplete, larger reproductions would grace the walls ofB Y K A T E O ’ N E I L L34 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
For its time, the Class of 1968was diverse. Women made up a striking 20 percent ofthe class, at a time when 93 percent of thenation’s physicians were men.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 35
[ Beginnings ]Dr. Stetten personally oversaw the construction projects that would becomethe first teaching facilities at RMS, a freestanding medical school. ... <strong>The</strong> walls of theteaching labs were hung with enlargements of the “Muscle Men,” woodcuts from“De Humani Corporis Fabrica”, Andreas Vesalius’s 16th-century text that inaugurated themodern study of anatomy.... In 1966, the cornerstone was laid for the Research Tower,which was completed and dedicated four years later.its Great Hall. To everyone — faculty, students, and visitorsalike — it was clear that this new medical school wasboth humanistic and erudite.Like many debuting medical schools, RMS opened asa two-year school, teaching the basic sciences and offeringa master’s degree in medical science (MMS). Fromthe start, science was never taught in isolation from itsclinical correlations: Dr. Stetten insisted that in additionto the six basic science departments — anatomy, biochemistry,microbiology, pathology, pharmacology, andphysiology — the school would have a Department ofMedicine and a Department of Psychiatry. As soon asthe medical school could establish clinical teaching facilities,it would add third- and fourth-year studies. Thistransition was complete by 1974, when the first medicaldegrees were awarded.A Sense of AdventureStarting in 1963, <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong> facultywere doing research at several locations on andnear the Piscataway campus. But not until 1966,when the charter class matriculated, did the medicalschool finally became a reality. <strong>The</strong> elite group of 16 studentshad been selected from nearly 1,000 applicants.For its time, the Class of 1968 was diverse. Womenmade up a striking 20 percent of the class, at a timewhen 93 percent of the nation’s physicians were men.<strong>The</strong> class came from wide backgrounds and a variety ofundergraduate schools, ranging from Sarah LawrenceCollege to New York University (NYU) and theUniversity of California at Los Angeles (UCLA). Five ofthe 16 were from New Jersey, but only one was a graduateof <strong>Rutgers</strong> University.Many had majored or double-majored in the sciences,but the admissions committee had included liberal artsmajors as well. In contrast to the Class of 2015 atUMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong>, inwhich 23 percent were born outside the United <strong>State</strong>s,only two members of the Class of 1968 were foreignborn;both had emigrated to escape Communist repression.Eight of the 15 graduates of the Class of 1968 continueto practice today. Two retired voluntarily, three weresidelined by disabilities, and two are deceased.What motivated this high-powered group of studentsto apply to and accept admission to an unproven medicalschool? “I thought it would be a great adventure tostart out with a new school,” recalls Rodger Searfoss,MD. “It seemed unique.”Sheila Nagar, MD, recalls a similar feeling: “It wasexciting to be part of a new adventure,” she says. “<strong>The</strong>school was very idealistic; it had very high standards andwas going to chart new ways in medical education whilebuilding on the infrastructure of an outstanding university.”Both Dr. Nagar and her classmate Linda Pollack,MD, narrowed their options to <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong>when their families pressed them to stay near home, inNew Jersey.As a senior at the University of Miami, Luis Villa had36 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
not firmly decided between medicine and law. He choseRMS, believing that if medicine didn’t prove a good fit,he could switch to law more gracefully after graduatingfrom a two-year school. “But I loved it all from the firstday — my classmates, the environment,” he says. “Inever gave another thought to law school.”In the spring of 1966, Eric Wurmser, then a senior atMiami University in Ohio, was in a biology lab whensomeone hand-delivered a slim envelopefrom <strong>Rutgers</strong>. “Thin envelopesusually brought bad news,” herecalls, but he read the words “Weare pleased to announce,” and,overjoyed and relieved, put downboth the letter and the scalpel andwalked right out of class. <strong>The</strong>n,torn between acceptances fromCase-Western Reserve and RMS,he sought the advice of the dean.“He was familiar with the<strong>Rutgers</strong> reputation, and he said,‘Go!’ So I went!”Walter Rosett was attractedby the financial support that<strong>Rutgers</strong> offered, and MiltonKoch believed itwould be interestingto be part of a medicalschool in its formativeyears. “And itwas,” says Dr. Koch.“It was a great experience.”Opening<strong>The</strong> Trail:<strong>The</strong> First TwoYears<strong>The</strong> First DayApuzzling case study highlighted the first-daywelcome session in September 1966. “Since thiswas a medical school,” Dr. Stetten recalls in hismemoir How My Light Was Spent, “it would be wellto initiate the students at once into the problems of medicineand to introduce the students to the object of medicine— namely, the patient.”Clifford Gurney, MD, then professor and chair, Departmentof Medicine, presented a 40-year-old patientwith sickle cell anemia, reviewing the genetics of the disease,its peculiar cytology, heme metabolism, and theapparent intolerance of the plasmodium of malariatoward sickle hemoglobin. <strong>The</strong> patient provided an excellentopportunity to indicate to the students “the reasonsfor the study of the several basic sciences: biochemistry,anatomy, genetics, parasitology, etc.,” continuesDr. Stetten.Sheila Nagar, MD,recalls: “It was exciting to be part ofa new adventure, <strong>The</strong> school was veryidealistic; it had very high standardsand was going to chart new ways inmedical education while building on theinfrastructure of an outstanding university.”Describing the diagnostic test, Dr. Gurney presentedthe students with an anomaly on the test strip: a strongspot at the location of hemoglobin S, and an additionalspot, faint but still clearly visible, in the location ofhemoglobin A. “A young woman immediately saw theresolution of this difficulty, and her hand shot up,”<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 37
[ Beginnings ]continues Dr. Stetten. “‘You can’t fool me,’ she said. ‘Thatspot for hemoglobin A comes from the transfusion thepatient received last week.’”“That student was Linda Pollack,” says Dr. Villa, recallingthe incident as though it had occurred yesterday.<strong>The</strong> FacultyDr. Koch remembers thathe and his classmateswere surprised by theemphasis placed on virology,when they had come “expecting‘old school science.’ But we cameto appreciate that the curriculumwas ahead of the curve, and the school was progressive.<strong>The</strong>y were out front on health indicators like cholesterol.It was great to be part of such a small class and such abright group of people.”<strong>The</strong> faculty is remembered by many in the class forits generosity, hospitality, and dedication. “<strong>The</strong>y wereexcellent teacher-scientists,” says <strong>Robert</strong> O’Neill, MD, ashe ticks off the names of some of his favorites: microbiologistThomas Stevens, PhD; psychiatrist EdwardMcGough, MD; biochemist Alexander Eichholz, PhD (“theway he taught enzymes, you never forgot it”); and virologistWalter Schlesinger, PhD, a pioneer in dengue feverresearch.Neuroanatomy was taught by Richard Sidman, MD,and Merrill Wolfe, MD, two professors from Harvard<strong>Medical</strong> <strong>School</strong> who flew in once a week for 16 weeks toteach for two days. “<strong>The</strong>y had written the prototype of anew text on neuroanatomy, which featured a brand-newconcept, programmed learning,” says Elliot W. Jacobs,MD. “<strong>The</strong>y made this course — usually regarded withdread as the most difficult in medical school — the mostinteresting and exciting course that I took at RMS. <strong>The</strong>course was so vastly popular with the students that wewould return in the evening to the classroom and reviewslides with the profs, who were there for us. Just for thefun of it!”As the first class at RMS, the Class of 1968 had no studentmentors. With no upperclassmen to guide them,many found it difficult to budget study time in order tomaster the essentials. “<strong>The</strong>re could be challenges withsome of the faculty,” says Dr. Jacobs. “I asked the physiologyprofessor what was ‘core.’ He tapped this huge textbook,and said, ‘That’s core.’”RMS opened as a twoyearschool, teachingthe basic sciences andoffering a master’sdegree in medical science (MMS).From the start, science was never taught inisolation from its clinical correlations:Dr. Stetten insisted that in addition to thesix basic science departments — anatomy,biochemistry, microbiology, pathology,pharmacology, and physiology — the schoolwould have a Department of Medicine and aDepartment of Psychiatry.“You spent a lot of time wondering what really matteredand what might just be a pet topic of the professor,” says Dr.Rosett. “I bugged one guy to tell me what was important, andhe told me to figure it out for myself. In the end, Iguess my system worked, because I did very well on myboards — disproportionately well compared to my grades.”38 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
Yearbook: THE CLASS OF 1968 IN 2012“Some faculty were writing the course as they wentalong, staying just ahead of the class,” adds Dr. Rosett.“This made it interesting, because science is constantlychanging, and things were happening while we werelearning.”<strong>The</strong> following year, the Class of 1968 felt a mentoring responsibilityto the entering class, says Walter Rymzo, MD.“We provided something for them that we hadn’t had.”Clinical CorrelationsFrom the first day, when the students met the patientwith sickle cell anemia, they were eager to experiencemedicine in a clinical environment. <strong>The</strong> medicalschool had not yet officially affiliated with a hospital,but on Saturday mornings, in “Clinical Correlations,”the class traveled to area hospitals to meet patients whosemedical conditions related to the curriculum.Not everyone in the class was satisfied with the amountof clinical exposure that RMS offered. But many were.“Dr. Stetten’s philosophy was ‘We don’t speak sciencehere,’” says Dr. Nagar. “<strong>The</strong> faculty may have been innovatorsin introducing the clinical connection early on andintegrating it with technical studies.”Another clinical correlation involved a patient withcoarctation (narrowing) of the aorta. “We were taughthow to diagnose the condition using the symptoms, withoutdoing angiography,” says Dr. Jacobs. Recalling thecardiac patient, Dr. Nagar says, “We learned that youdon’t always know what the problem is, but you know thequestions to ask in order to find out.”Dr. O’Neill recalls a time when the class showed its barelycontained eagerness for clinical experience. A clinicalneurologist had invited them to St. Peter’s <strong>Medical</strong> Center,in New Brunswick, where he presented a patient whoseface drooped markedly on one side. He hardly had finishedthe question, “What do you think might be causing this?,”when all 16 students unanimously said with conviction,“Bell’s palsy!”“And we were right,” adds Dr. O’Neill.One of the original 16 switched from medicine to lawbefore graduation. All the others earned an MMS degreeand then completed their MD degree at a four-year medicalschool. Dr. Jacobs was among the five RMS studentswho went on to Mount Sinai <strong>School</strong> of Medicine, whichopened in 1968. “We were probably the only five studentsin the country who were in the first class at two differentmedical schools,” says Dr. Jacobs. MElliot W. Jacobs, MDplastic and reconstructive surgery,New York City.• BS in chemistry,Queens College; MD,Mount Sinai <strong>School</strong> ofMedicine; internship/residency (general andplastic surgery) atMt. Sinai HospitalRMS memories: Neuroanatomy, “a superb course”. . . socialevenings at the homes of the Stettens and department heads . . .Ping-Pong, Friday night beer and (piz)“za”. . . gross anatomycadavers, one with a fatal knife wound to his head . . . workingweekends as a professional accordionist and entertainer.Two years as a major in the U.S. Air Force in Abilene, Texas . . .32 years in private practice, New York City. . . specialty: aestheticsurgery . . . widowed, divorced, now “deliriously happy” with thirdwife, Leigh, and sons, Jeffrey, 31, and Benjamin, 18.Milton J. Koch, MDgastroenterology, Potomac, Maryland• BA in German, New York University;MD, Mount. Sinai <strong>School</strong> of Medicine;internship/residency(internal medicine)at Bellevue Hospital;fellowship (gastroenterology)at VeteransAdministration <strong>Medical</strong>Center; research in neurology at National Institutes of Health (NIH),while serving in Public Health Service in lieu of uniformed militaryservice.RMS memories: Faculty hospitality . . . the 42/16 faculty-studentratio . . . teachers like the “tremendous” Walter Schlesinger, recruitedfrom the NIH . . . Dean Stetten: always available to share informationas well as great historical/medical perspectives.A founding partner in Capital Gastroenterology Consultants,Montgomery County, Maryland, which grew to four offices with11 doctors . . . world traveler with “self-designed trips”. . . bookclub and family genealogy . . . wife, Susan; children, Matt, 38;Mike, 35; and Alexis, 32.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 39
Yearbook: THE CLASS OF 1968 IN 2012Linda Pollack Mercer, MDpediatrics, child psychiatry (retired)Crystal Lake, Illinois• BS in biology, NewYork University; MD,Mount. Sinai <strong>School</strong> ofMedicine; internship/residency (pediatrics) at Los AngelesCounty Hospital/ColumbiaPresbyterian Babies Hospital; fellowship (child psychiatry) at <strong>Rutgers</strong>Mental Health Center/Long Island Jewish-Hillside <strong>Medical</strong> CenterRMS memories: Being part of the Ping-Pong brigade . . . atage 20, the youngest member of Class of ’68 . . . “I was sassy!”. . . the school was a “neonate, but provided a good balanceof scientific and clinical education.”Headed the Inpatient Child Psychiatry Unit at Children’s MemorialHospital in Chicago for four years . . . retired to be with family . . .with her late husband, John Mercer, started Serve and Protect torescue pets whose owners were victims of the September 11, 2011,attacks . . . children: Jennifer, 33, and Johnathan, 31; stepchildren:Mike, 53, and Mark, 51; three grandchildren.Rodger Searfoss, MDorthopaedic surgery (retired, 2008),Greensburg, Pennsylvania• BA in history, JohnsHopkins University; MD,Stanford <strong>Medical</strong>Center; residency(surgery/orthopaedicsurgery) at University of North Carolina <strong>School</strong> of Medicine;fellowship at Bone Cancer Service, Memorial Sloan-Kettering CancerCenter, New York CityRMS memories: <strong>The</strong> school was rigorous, challenging, andcomprehensive . . . strong emphasis on neuroscience . . . indeliblesights and sounds of autopsy observed at St. Peter’s . . . playingon a “pretty good” six-man, intramural flag football team fieldedby RMS.30 years in private practice in Latrobe, Pennsylvania . . . three“eye-opening” medical missions to Vietnam and Myanmar toteach and perform surgery . . . gardening and golf . . . wife, Beth;children, Ann, 35, and Erin, 31; one grandchild.Walter Rosett, MDinternal medicine (retired),Albuquerque, New Mexico• BS in chemistry, Johns Hopkins University; MD,Mount Sinai <strong>School</strong> of Medicine; internshipat William Beaumont Army <strong>Medical</strong> Center; residency (internalmedicine) and fellowship (infectious diseases) at University of Kansas<strong>Medical</strong> CenterRMS memories: <strong>The</strong> school was still a work in progress withheavy emphasis on science . . . ever-improving Ping-Pong skills butnever the champ . . . Cliff Gurney, chair, Department of Medicine, hismentor and co-author of several papers.Repaid Army by working as general medical officer at Sandia Baseand Fort Carson, Colorado (lots of skiing) . . . returned toAlbuquerque, which he ”unequivocally loves”. . . joined a solopractice; built a new office and then a larger one as practice grew . . .sold practice to the local hospital . . . it had become “a secondfamily”. . . “as wonderful a career as I could’ve hoped for” . . . nomore skiing and ski racing but keeping busy with tennis, reading,computers, woodworking, gardening, and genealogy research . . .married to Louise; children, Julia, 41, and Brian, 43.Rhoda Goldwasser Padow, MDpsychiatry, private practice,Fulton, Maryland• BA, Sarah LawrenceCollege; MD, TuftsUniversity <strong>School</strong> ofMedicine; internship atBoston VA Hospital; residency (general psychiatry) at McLeanHospital, Belmont, Massachusetts; fellowship (child psychiatry) atNew England <strong>Medical</strong> Center, Boston; psychoanalytic training:Baltimore-Washington Psychoanalytic InstituteRMS memories: Class of ’68 was very close . . . so small it waslike being in a goldfish bowl . . . communal study sessions . . .everyone had keys to the “tiny building that was then the medicalschool”. . . Associate Dean Richard Cross, MD: “a lovely man whotook a fatherly interest in our class”. . . Clinical Correlations atfriendly Princeton Hospital.Worked 12 years with seriously ill patients at Chestnut Lodge inRockville, Maryland . . . after her husband’s fatal car accident, sheopened a home office to be near her young twins . . . continuing loveof classical music . . . children, twins Jeremy and Victoria, 23.40 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
Yearbook: THE CLASS OF 1968 IN 2012Lawrence Sirott, MDfamily practice/adult primary care (retired, 2006),Berkeley, California• BA in developmental psychology, University ofMinnesota; MD, University of Minnesota <strong>Medical</strong> <strong>School</strong>; rotatinginternship at San Francisco General HospitalRMS memories: Attracted to the school by enthusiasm andidealism of several founding faculty members, small size, financialsupport, and promise of learning by the Socratic method.Public Health Service assignments on a Navajo reservation andin the National Health Service Corps as a primary care physicianin an underserved rural community clinic . . . seven years atLa Clinica de la Raza in Oakland . . . helped found group practicein Alameda, California . . . spent five years as a primary carephysician at Kaiser, in Oakland . . .“retired as it became clear that thecognitive changes of Parkinson’s disease interfered with myability to practice medicine effectively”. . . co-founded PD Active,a now-thriving organization that first brought the Mark Morris“Dance for Parkinson’s” program to California . . . wife of 35 years,Harriet Charney; children, Irisa, 34, and Jonah, 32.Walter Rymzo, MDinternal medicine, West Hyannisport, Massachusetts• BA in biology, Johns Hopkins University; MD, Harvard<strong>Medical</strong> <strong>School</strong>; internship (medicine) at Boston CityHospital; residency (internal medicine) at Massachusetts GeneralHospital; fellowship (forensic pathology) in Office of the <strong>Medical</strong>Examiner, New York City.RMS memories: “Dean’s Cup Trophy for Ping-Pong Excellence”. . . Gerhart Plaut’s “substandard” comments . . . the wonderful“Schles.”Two years in Commissioned Corps of the U.S. Public Health ServiceEcological Investigation Program “chasing dengue and schistosomesin Puerto Rico”. . . 15 years practicing internal medicine andinfectious disease on Cape Cod . . . chief of medicine, Cape CodHospital . . .“amid deteriorating medical climate on the Cape,became chief of medicine, MIT”. . . back to Cape with conciergemedical practice . . . longtime aviation medical examiner . . .kayaking, crewing on racing sailboats . . . wife of 42 years, Inara;children, Ben, 35, and Matt, 32.Eric Wurmser, MDplastic surgery, Red Bank• BS in chemistry, Miami University; MD, Mount Sinai<strong>School</strong> of Medicine/NYU; internship/residency(surgery and plastic surgery) at Kings County Hospital Center,Brooklyn, New YorkRMS memories: “Rhoda and I, tiny and big, as lab partners . . .faculty favorites: Larry Silverman and the psych professors.Planned a PhD in chemistry and a career in research . . . afterseeing very sick patients in residency at Kings County, switchedto plastic surgery . . . taught for ten years at Kings County . . .specialty: repairing cleft lips and palates . . . developed a non-profitorganization to support and equip annual medical missions (22 todate) to the Philippines and Southeast Asia to teach and care forunderserved . . . wife, a nurse, is always on the team . . .teaches poetry at Georgian Court University . . . certified ringsideboxing physician . . . wife, Teri; children, Kurt, 37, and Rachel, 31(in medical school at Columbia).Luis Villa, MDoncology, hematology, andpathology, Miami, Florida• BA in chemistry,University of Miami; MD,Harvard <strong>Medical</strong> <strong>School</strong>;residencies (medicine) atJackson Memorial Hospital; (clinical pathology) at NIH Bethesda,Maryland; and (internal medicine and anatomic pathology) at JacksonMemorial Hospital; fellowship (hematology/oncology) at MiamiCancer CenterRMS memories: “Very special environment, very individualizedteaching”. . . emphasis on learning from case studies . . . formativesummer job after first year, doing pathology rotation at PrincetonHospital.“Incredibly grateful to this country: when nobody wanted us, theU.S. opened its doors”. . . board-certified in six areas . . . for 30years, had simultaneous full-time careers in oncology/hematologyand pathology . . . cut back to eight-hour work days in 2011 . . .30 years as volunteer for and 15 years as president of the LeagueAgainst Cancer, which has treated more than 30,000 patients gratisand continues to do so . . . second wife, Jennifer; children, Luis IV, 33;Daniel, 31; Jennifer, 20; and David, 19.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 41
Yearbook: THE CLASS OF 1968 IN 2012John Szabo, MDradiology, Palm Desert, California• BS in chemistry, UCLA; MD and residency (diagnosticimaging, nuclear medicine, and radiation therapy) atUCLA, David Geffen <strong>School</strong> of Medicine; fellowship at Wadsworth VAHospital, Los AngelesRMS memories: “It was not yet a true medical school, but thestudents were well supported in all practical aspects”. . .“edifice wasexcellent for teaching, faculty was marvelous, and Dean Stetten was atrue force.”. . . enjoyed exposure to clinical work at local hospitals.Special interest in nuclear medicine.Sheila C. Nagar, MDendocrinology, Jerusalem• BA in French, DouglassCollege; MD, New Jersey<strong>Medical</strong> <strong>School</strong>; internship/residencyat UMDNJUniversity HospitalRMS memories: Turnedto medicine from graduate studies in French literature, seeking somethingthat would “nail my feet to the floor”. . . the prevailing attitude ofexcitement . . . pioneering psychiatrist Albert Silverman, MD . . . visitinga lab where innovative lipid research had opened a new world.During residency, fell in love with endocrinology: “excursions inhormones and their effects on human behavior”. . . practicing inJerusalem since 2003 . . . involved in housing south Sudanese refugeesin Israel . . . daughters, Ornitte and Talia; three grandchildren.<strong>Robert</strong> O’Neill, MDemergency medicine (retired), Bainbridge Island,Washington• BS in biology and chemistry, Bucknell University;MD, internship/residency (internal medicine) atUniversity of Washington <strong>School</strong> of MedicineRMS memories: Admissions interview with Richard Cross, PhD,associate dean . . .“DeWitt Stetten was capable of bringing brilliantminds together . . .“we knew they were at the top of their game.”Practiced emergency medicine for 30 years . . .“loved the ER: getting tothe bottom of things every day, then starting with a clean slate”. . .“a truck that did an unexpected 180 in front of me” caused injuriesthat forced early retirement . . . still racing six-meter sailboats and flying50-year-old Mooney planes . . . married 45 years to Julie; children,Megan, 36, and Griff, 33; two grandchildren.IN MEMORIAMSteven R. Koller, MDrheumatology, Richmond, Virginia1945–1991• BSE in electrical engineering, Princeton University;MD, Mount Sinai <strong>School</strong> of Medicine; residency(internal medicine) and fellowship (rheumatology) at <strong>Medical</strong>College of VirginiaDr. Koller was the first student admitted to <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong>,says his widow, Miriam (Mimi) Koller Pizzani, who became his wifein 1967. He wanted to be a biomedical engineer, she adds, butsomeone convinced him he should start with an MD.Dr. Koller served as a major in the U.S. Army and received aDistinguished Service Medal. Loved and admired by his patients, heserved on the clinical faculty of the <strong>Medical</strong> College of Virginia untilthe time of his death, from cancer, at age 46. Shorlty before hisdeath, he had been promoted to the rank of clinical professor. Healso chaired the medical advisory board of the Lupus Foundation ofVirginia, where an endowment supports the annual Steven R. KollerAddress. He is survived by Mimi; their two children, Elisabeth, 41,and Roger, 39; and two grandchildren.Joseph S. Tulumello, MDpulmonology, Buffalo, New York1943–2009• BA, Harvard University; MD, Weill Cornell <strong>Medical</strong>College; internship/residency (internal medicine) atNew York Hospital; fellowship (pulmonology) at University ofCalifornia at San Diego HospitalDr. Tulumello served in the military as a flight surgeon, and hepracticed internal medicine and pulmonary medicine in New York,California, Michigan, and Wisconsin. Although he was diagnosedwith bipolar disorder in 1978, he persevered through the next twodecades, pursuing the career for which he had trained with intelligenceand intensity, according to his RMS classmates, and which heloved. He retired in 2003 and died in November 2009.News of Dr. Tulumellos’s illness and death came as a shock tohis RMS classmates, who remember him for his kindness to all(Dr. Padow), his studious work habits (Dr. O’Neill), and his solidityand intelligence (Dr. Searfoss).“When I think of him,” says Dr. Pollack, “all I see is his huge,bright smile.”42 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
[ Beginnings ]Richard C.Reynolds, MD:A Clinicianat HeartDr.Richard Reynolds and hiswife, Mary Jane, in the 1960sAclinician at heart, Richard C. Reynolds, MD, former dean, UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong>, enjoyed a remarkable career in clinical andacademic medicine. In 1978, he came to <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong> (RMS) from theUniversity of Florida College of Medicine, where he was founding chair ofthe Department of Community Health and Family Medicine. He served asdean of <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong> for nine years before rounding out his distinguishedcareer as executive vice president of the <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong>Foundation (RWJF).<strong>The</strong> Early YearsRichard Reynolds decided at age 16 tobecome a doctor. Starting that journey,he majored in biology at <strong>Rutgers</strong>, <strong>The</strong><strong>State</strong> University of New Jersey. <strong>The</strong>n, afteracceptance at the Johns Hopkins <strong>School</strong> ofMedicine, he hitchhiked to Baltimore to beginhis medical studies. In his first clinical encounters,Dr. Reynolds discovered that medicineexceeded his expectations. “I had always beenshy,” he says, “but I discovered that the shynessleft me when I saw a patient. I realized whatI could do, and what my limitations were.”B Y K A T E O ’ N E I L L<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 43
In 1953, he earned his medical degree at Hopkins, where healso completed his internship and residency in internal medicineand, later, a fellowship in infectious diseases.During a fourth-year elective in his last year of medicalschool, Dr. Reynolds was working in the delivery room oneevening, assisted by a nursing student with fiery red hair.“That was it,” he says. “I was smitten, and it ruined anyplans I’d had for my bachelorhood!”Dr. Reynolds and the red-headed Mary Jane Beck marriedthe following year, after his internship and her graduationfrom nursing school. <strong>The</strong>y promptly headed for Alaska,where he served in the Public Health Service for two years.As an itinerant doctor covering the villages of Alaska’s southerntier, he encountered and addressed issues of communityhealth that would influence his priorities throughout hiscareer. While there, he delivered two of the most importantpatients of his career: the couple’s first two children, Karenand Stephanie. <strong>The</strong>ir son, Wayne, was born following thefamily’s return to Maryland.After Dr. Reynolds’s fellowship, they moved to the smalltown of Frederick, Maryland, where he started a muchneededmedical practice in a downtown storefront. “It wasa good time, and I worked with wonderful partners,” recallsDr. Reynolds, who ran the practice solo for seven years.A decade later, he would revisit some of his Frederickpatients in his essay “A Day in the Life of an Internist.” Anold appointment book provided not only the framework forthe essay, but also the dramatis personae: the patients he hadseen between 7 AM and 7 PM — or consulted about, in thecase of a 2:30AM call from the hospital — in his office, at thehospital, and in their homes. Although ten years had passedsince making those entries, Dr. Reynolds says he “wasamazed at how vividly I could recall many of the patients.”<strong>The</strong> essay was included in On Doctoring, an anthologyof essays, poems, and stories, co-edited by Dr. Reynoldsand cardiologist John Stone, MD. Sponsored by the <strong>Robert</strong><strong>Wood</strong> <strong>Johnson</strong> Foundation, the work was first publishedin 1989. For years, the foundation presented a copy of thebook to first-year medical students throughout the United<strong>State</strong>s — more than 200,000 copies to date — aiming toshare “not only the triumphs and joys of medicine, but alsoits unique perceptions of human beings.”Dr. Reynolds’s innate curiosity tended to express itself asrestlessness, a sense, he says, that he wanted “somethingelse.” Serendipitously, after he’d been in Frederick for nineyears, a phone call came from Leighton Cluff, MD, a longtimecolleague and friend. Dr. Cluff, then chair of theDepartment of Medicine at the University of FloridaCollege of Medicine in Gainesville, hoped to recruit Dr.Dr. Reynolds brought important strengths to themedical school, including experience in academic medicineand an appreciation for the organization of medicalstudent and resident training.Reynolds as chief of the division of ambulatory medicineand community health.Dr. Reynolds accepted the offer. Among his responsibilitieswas the development of a rural education programthrough which, under faculty supervision, medical studentsand residents would provide care to people who were medicallyunderserved: the region beyond Gainesville wasrural, sparsely populated, and impoverished; nearbyLafayette County had been without a doctor for ten years.Under Dr. Reynolds’s leadership, the new departmentestablished three satellite clinics. <strong>The</strong> pilot clinic, in Mayo— affectionately known to the staff as the Mayo Clinic —was open around the clock and saw 5,000 medicallyunderserved patients each year. In addition to providingprimary care, the clinics became an important teachingresource and a locus for research on rural health. “Dr.Reynolds’s landmark work in Gainesville brought himkudos for ambulatory care service, an area for which hebecame known nationwide,” says Raymond M. Russo,MD. During Dr. Reynolds’s early tenure as dean, Dr. Russowas director of ambulatory care at Middlesex GeneralHospital — later renamed <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong>University Hospital (RWJUH).44 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
[ Beginnings ]<strong>The</strong> Years as DeanDr.Reynolds was beginning to feel restlessagain when a call came from Stanley S.Bergen, Jr., MD, president, College of Medicine andDentistry of New Jersey (CMDNJ), the future UMDNJ.Dr. Bergen’s offer of the position of interim dean at <strong>Rutgers</strong><strong>Medical</strong> <strong>School</strong> sounded like exactly the sort of new challengeDr. Reynolds had been looking for.“Dr. Bergen said there was no expectation that I’d becomedean,” Dr. Reynolds recalls. “Still, I vowed to myself that, asinterim dean, I’d walk through the door every morning andact like a dean.” To deal with prickly problems, he turned tohis clinical experience. “If faculty members came into myoffice upset about something, I would think of them as mypatients. I’d ask what the problem was, and how I couldhelp them so they could do their job.”Dr. Reynolds maintained his clinical skills by leadinghospital rounds whenever he could. He enjoyed any opportunityto meet with students. “<strong>The</strong> school was gettingstronger,” he says, “and the students were first-rate. <strong>The</strong>ydidn’t know how good they were, and one of my jobs wasto buck them up and make sure they lifted their sights.”<strong>The</strong> Teaching HospitalDr. Reynolds’s primary job was to establish an interfacebetween the medical school and a hospitalthat would serve as a major teaching affiliate. In acharacteristic understatement, he says, “It was a challenge,but I thought it would be fun to give it a try.”A year after his initial appointment at <strong>Rutgers</strong> <strong>Medical</strong><strong>School</strong>, Dr. Reynolds was named dean. He brought importantstrengths to the medical school, including experience inacademic medicine and an appreciation for the organizationof medical student and resident training. Dr. Russo, whoworked closely with Dr. Reynolds, says that, most important,“Dick’s a quick study, and he’s fantastic with humanrelations. He persuaded people because he was usuallyright, and people knew it.”<strong>The</strong>se strengths helped the school evolve in new directions,with three particular achievements marking “theReynolds years:” the establishment of a teaching hospital,the change in the name of the school, and the creation of theEric B. Chandler Health Center. By good fortune, Dr.Reynolds’s arrival on the Piscataway campus — there wasno New Brunswick campus in 1979 — coincided with<strong>Johnson</strong> & <strong>Johnson</strong>’s decision to maintain its world headquartersin New Brunswick. <strong>The</strong> corporation’s commitmentto community development complemented the medicalschool’s mission in community health.After a comprehensive analysis of the four leading candidates,Dr. Bergen’s Alternatives Committee determined thatthe 400-bed Middlesex General Hospital in New Brunswickwas the clear choice to be named the medical school’s teachinghospital. If the hospital leadership and staff had anyremaining doubts about the school’s total long-term commitmentto the affiliation, says Dr. Reynolds, they were putto rest when RMS put the <strong>Medical</strong> Education Building “onthe tarmac” immediately contiguous to the hospital.What’s in a Name?What’s in a name? A lot, Dr. Reynolds would discover.Originally part of <strong>Rutgers</strong> University, the medical schoolremained <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong> when the state put itunder the CMDNJ umbrella. By 1985, CMDNJ had evolvedand become UMDNJ, and the board and Dr. Bergen feltthat <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong> needed to clarify its independencefrom <strong>Rutgers</strong>. When the contentious process ofname selection became deadlocked, Dr. Reynolds proposedthat the school be named for the New Jersey poet andphysician William Carlos Williams. When his suggestionitself proved controversial, Dr. Reynolds supported analternative proposal, that the school be named for <strong>Robert</strong><strong>Wood</strong> <strong>Johnson</strong> — widely known as “the General” — abusiness leader who had built <strong>Johnson</strong> & <strong>Johnson</strong> into aworldwide corporation. UMDNJ and the medical schoolreadily embraced the plan to name the school for Mr.<strong>Johnson</strong>. At the same time, Middlesex General became<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> University Hospital, strengtheningthe bond between the two institutions.<strong>The</strong> Legacy<strong>The</strong> Richard Reynolds ChairWhile Dr. Reynolds was working at RWJF andserving at Chandler, the foundation wanted tohonor him with a meaningful, lasting contribution to themedical school. <strong>The</strong> legacy they chose was the establishmentof the Richard C. Reynolds Chair in General InternalMedicine. <strong>The</strong> endowment recognizes Dr. Reynolds’s passionfor protecting and promoting generalism in internal<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 45
medicine, says Jeffrey L. Carson, MD, Richard C. ReynoldsProfessor of Medicine and chief, division of general internalmedicine. Dr. Reynolds was instrumental in creating thedivision and recruited Dr. Carson to build it. “<strong>The</strong> divisiondoes 75 percent of the attending on the hospital medicalteaching service in the Department of Medicine,” says Dr.Carson. “In addition, it provides teaching service in theoutpatient general internal medicine practice, the ER, andat Chandler.” A large portion of the endowment supportsresearch in general internal medicine.A Dean’s Success“Adean’s success depends on others,” says Dr.Reynolds.“A nationally prominent academic medical campus hasevolved from the affiliation of <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong><strong>Medical</strong> <strong>School</strong> and <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> UniversityHospital,” he adds. “This could only have happened withprodigious efforts by many, including the faculty, a loyalcadre of community physicians, involved local citizens,members of the hospital board, and many others.” He recognizes,in particular, the support he received from Dr.Stanley Bergen as president of UMDNJ during his tenure.<strong>The</strong> Key<strong>The</strong> Eric B. Chandler Health CenterEarly in his tenure, Dr. Reynolds realized that beingdean of a medical school is as much a communityjob as an academic one. <strong>The</strong> development of theEric B. Chandler Health Center may best demonstratehis skills as a community leader. To bring the health centerfrom concept to reality required an effective collaborationamong three parties: RWJMS, RWJUH, and theNew Brunswick Board of Education. <strong>The</strong> support of theCivic League was also critical to the project’s success.When the hospital outgrew its ambulatory care space,Dr. Reynolds located six trailers formerly used by amedical practice in southern New Jersey. He also foundthe funds to purchase the trailers and transport them toNew Brunswick. <strong>The</strong> hospital supported the proposalthat its ambulatory services be moved to propertyowned by the school board. Quietly, Dr. Reynoldsmade sure that Chandler would always be part of themedical school.In 1987, Dr. Reynolds stepped down as dean to becomeexecutive vice president of the <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong>Foundation. Steven Schroeder, MD, was president ofRWJF during the last seven years of Dr. Reynolds’s servicethere. “Dick was my mentor at the foundation,” he says,and “and you couldn’t ask for a better partner. His personalvalues and social ethic came together in his commitmentto medicine and the problems of health care.”Dr. Reynolds was delighted when, in 1991, RWJFawarded $3 million to Chandler, by then a federallyqualified health center. <strong>The</strong> grant from the foundationsupported the construction of permanent facilities onGeorge Street, in downtown New Brunswick. At 15,000square feet, the new building would triple the area of thetrailers and comfortably accommodate an expansion ofpatient enrollment and services. Although by then he wasan officer at RWJF, Dr. Reynolds volunteered, oneevening each week, as a provider at Chandler. “I couldn’tstay away,” he says. “I loved it, and so many of thepatients had heart-rending stories.”Eric G. Jahn, MD ’88, associate professor of familymedicine and community health and senior associatedean for community health, was an attending atChandler in the 1990s and served as the center’s medicaldirector. “Sometimes things could be in turmoil atChandler, but Dr. Reynolds brought an overwhelmingsense of care and calm that extended to the patient andspilled over into the center,” he recalls. “He alwaysleft us with the impression that we were doing theright thing by being there.”Once, while he was dean, Dr. Reynolds decidedafter a series of meetings in Washington, D.C., tophone Dr. Stetten, who lived nearby, in Bethesda,Maryland. <strong>The</strong> two deans met that afternoon, and theconversation, “tentative but cordial,” as Dr. Reynoldsrecalls, seemed to bridge the longtime gap between Dr.Stetten and the school he had founded. A few days later,Dr. Reynolds was at his desk, writing a note to Dr. Stetten,when his assistant entered with a small, carefully wrappedpackage. Inside was a gold-plated key. <strong>The</strong> key, Dr. Stettenexplained in the attached message, had been presented tohim at the dedication of the new building in Piscataway.“This is the key with which I entered the building everyday,” he wrote. “When I left the school, I took it with me.Now I am passing it along to you.”“After that, every time I entered the building, I used HansStetten’s key,” says Dr. Reynolds, using Dr. Stetten’s lifelongnickname. “When I went to the <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong>Foundation, I passed it on to [Dean] Norm Edelman. It wasa treasure.”Once again, Dr. Reynolds had taken the time to listenand to care. A clinician at heart. M M46 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
[ Beginnings ]Alumni Couples:Shared Memories,Shared LivesDeep Roots“ Welike to say that we have deep tap roots at the medical school,” says RonaldNahass, MD ’82, clinical professor of medicine, UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong>.Like Ron and Rosanne Vita Nahass, MD ’84, the four other couples interviewed for this articleappreciate their mutual ties to RWJMS, finding that shared recollections of classes and classmates,faculty and friends, light moments and somber ones, enrich their lives. “People from <strong>Robert</strong> <strong>Wood</strong>always know we go together,” says Rosanne. “It’s great! Some of them knew our first son and ask,‘How’s the baby?’ (He’s now 25!) Twenty-five years out and we still have those connections.”IntroductionsMaura Santangelo,MMS ’73, MD, MPH,and Lawrence Schenk,MMS ’73, MDSince 1994, RWJMShas hosted the WhiteCoat Ceremony towelcome first-year studentsas future physicians.No such ceremonyexisted in the 1970s,says Dr. Santangelo. Onthe first day of classes, students went totheir locker, donned a white coat, and headedfor class. “Anatomy, taught by a surgeon, was“the first ‘doctor’ thing the class did together,”she says. “It was treated differently from othersciences. It was like a medical apprenticeship.“<strong>The</strong>re were only 64 students in our class,with 16 of us in each anatomy lab,” she adds.Maura Santangelo &Larry Schenk“You got to know people quickly, and that’swhere I met Larry.” <strong>The</strong>y began studying together,not only enjoying each other’s company, butalso benefiting from their complementary learningstyles. “I’m an aural learner,” he says, “whileshe’s visual — a note taker.”Michele Hickman <strong>Johnson</strong>, MD ’79,and Hubert <strong>Johnson</strong>, MD ’79In the summer of 1975, before starting theirfirst-year classes, Michele Hickman andHubert <strong>Johnson</strong> were part of a small groupof students who elected to take an anatomycourse at the medical school. <strong>The</strong> students livedin New Brunswick, commuting to Piscataway.Or at least they did until, “in that summer ofrains,” Hubert says, “the Route 18 bridgewashed out.” Stranded in Piscataway, the studentshad to sleep in the lounge downstairs.B Y K A T E O ’ N E I L L<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 47
[ Beginnings ]<strong>The</strong> NahassesTodayHubert & Michele<strong>Johnson</strong><strong>The</strong> couplesinterviewed for this articleappreciate their mutualties to <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong>,finding that sharedrecollections of classes andclassmates, facultyand friends, light momentsand somber ones, enrichtheir lives.On the first day of classes, Michelewas stranded again when the rideshe’d arranged was delayed by a flattire. But Hubert swung by and gother to school on time. <strong>The</strong>y becameinseparable in school and out andwere married at the end of theirthird year. “He’s always there forme,” she says. “And I’m alwaysthere for him.”Michele recounts an exampleof Hubert’s extrasensory perception ofher needs. “Our first child, Christopher,was born 11 days before graduation.When they called us up to the stage forour diplomas, I climbed the steps reallycautiously, for fear I’d fall over mygown. Hubert was right in front of meand, without looking back, he put outhis hand and supported me the rest ofthe way. <strong>The</strong> whole crowd cheered!”Ronald Nahass, MD ’82, andRosanne Vita Nahass, MD ’84Ron Nahass was two years aheadof Rosanne in medical school,so they never shared classes, butthey have been together since Rosanne’sfirst year at RWJMS, with the medicalschool playing a continuous role in theirlives. That fall, Rosanne attended aHalloween party,an informal welcomeevent for thenew class. Ron, thehost, recalls immediatelynoticing“the pretty firstyearstudent acrossthe room.” As theybegan spending timetogether, they discoveredthat they couldhave met much sooner:they grew up in adjacent towns inNorth Jersey and attended high schoolswith a long-standing rivalry in sports.Ronald & RosanneNahass <strong>The</strong>n<strong>The</strong>y were married at the end ofRosanne’s second year, just before Rongraduated and started his residency.Christina Miller Reiter, MD ’03, andMark Reiter, MBA, MD ’03Although both Christina and MarkReiter majored in biology at<strong>Rutgers</strong>, <strong>The</strong> <strong>State</strong> University ofNew Jersey, they met while she was asenior at <strong>Rutgers</strong>, and he was in his firstyear at RWJMS, on an interview for ateaching assistantship in a summerchemistry course. “It turned out that theschool needed more than one assistant,”she says, “so we both got the job.”Mark & Christina ReiterThat summer they began dating andtalking about careers in medicine.Christina had always been interested inmedical school, but as she consideredapplying, she became intimidated. “Iwondered if I would be accepted andsucceed,” she says. “Mark listenedpatiently. At the right moment, he gaveme the push I needed, but he wouldhave supported my decision either way.”Mark took a year off between his secondand third years to complete thecombined RWJMS/<strong>Rutgers</strong> Master’sProgram in Business Administration.<strong>The</strong>n he and Christina completed medicalschool together, as members of theClass of 2003, and were married duringtheir fourth year.48 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
Joanne Kulinski Mazzarelli,MD ’05, and AnthonyMazzarelli, JD, MBE, MD ’02<strong>The</strong> Residency Years:Choices and ChallengesJoanne Kulinski met AnthonyMazzarelli when she was in sixthgrade and he was in seventh. <strong>The</strong>ylost track of each other and met againwhen she was at <strong>Rutgers</strong>, applying tomedical schools. <strong>The</strong>y started datingwhen she was a senior and he was athird-year medical student. “We spentJoanne & AnthonyMazzarellia lot of time talking about medicineand discussing my decision,” she says.When Joanne was a first-year studentin New Brunswick, Anthony wasin his fourth year of medical school onthe Camden campus, simultaneouslycompleting his second year of lawschool at the University of Pennsylvaniaand his first year of a master’s degreeat Penn’s Center for Bioethics. At theend of that year, the U.S. Junior Chamberof Commerce named Anthony oneof Ten Outstanding Young Americans.He had been nominated for thehonor by Joanne, who cited not onlyhis academic achievements, but alsohis community involvement. Anthonyco-founded the student-run HealthcareOutreach Project (HOP) in Camden,where Joanne would volunteer duringher clinical years. She currently servesas an attending preceptor at HOP.<strong>The</strong> Mazzarellis were married atthe end of her third year.Maura Santangelo andLawrence Schenk weremarried in 1973, afterearning their master of medicalscience degrees at RWJMS (then<strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong>). <strong>The</strong>y completedtheir MDs at separate schools,however: Maura at Brown University<strong>Medical</strong> Center and Larry atTufts <strong>Medical</strong> <strong>School</strong>.<strong>The</strong>y were back together for theirresidencies at Tufts New England<strong>Medical</strong> Center, though their contrastingpersonal styles had guidedthem to very different programs.Maura is detail-oriented and consideredneurology before deciding onophthalmology because “ophthalmologistsseem to enjoy what they’redoing. <strong>The</strong>y’re happy doctors.” Larrywould go into orthopaedic surgery. “Itake a broader approach to issues,”he says. “My preferred tool is a twoby-four.”<strong>The</strong>ir first child, William, arrivedat the end of the first year of theirresidencies. Three years later, theirsecond, Candace, was born. Larrywas chief resident in the orthopaedicsurgery residency program, on call24/7, and Maura was completing afellowship in glaucoma at MassachusettsEye and Ear Infirmary.“Having a child while you’re a residentor fellow is insane,” Maura says,“and it was worse before there werelaws limiting residents’ workinghours. You try to schedule your hoursso you’re not on call at the same time,but it’s hard. And the whole timeyou’re at work, you’re conscious thatyour children are out there, somewhere.”Michele and Hubert <strong>Johnson</strong>entered the Couples Matchand went to Boston, theirfirst choice, for their residencies.Hubert would do surgery at Tufts,while Michele did obstetrics and gynecologyat Beth Israel Deaconess <strong>Medical</strong>Center. After two years, they tookdeferments to serve as general medicalofficers in the Public Health Service(PHS) in South Carolina, where twoyear-oldChristopher was joined by asister, Kimberly. “<strong>The</strong> PHS mandatedyou see 100 patients per week,” saysHubert. “We learned a lot of medicine,but no matter how busy we were there,we weren’t as busy as we were as residentswith clinical hours plus administrativework.”Following their residencies in Boston,Hubert did a fellowship in vascular surgery,Michele entered private practice,and Nicole was born. “We enjoyed ourtime at RWJ and are grateful for theexcellent education and opportunities itprovided,” Hubert adds. “We bothgraduated from excellent residencies inBoston, all of which we attribute tobeing so well prepared by RWJ.”<strong>The</strong> Nahasses’ determination tostay near each other guidedmany of their career decisions.Ron doesn’t recall a match process,but Rosanne still had two years beforegraduation, so the residency programin the Department of Medicine atRWJMS was a clear first choice. Hesubsequently served a fourth year, aschief resident, before completing afellowship in infectious diseases, alsoat RWJMS, and joining the full-timefaculty of the Department of Medicine.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 49
[ Beginnings ]Rosanne was an intern in theDepartment of Medicine’s residencyprogram when she became pregnant.Thirty-six-hour shifts, often starting at6:00AM, took their toll, and in the seventhmonth of her pregnancy, bed restwas prescribed. Six weeks later, shewas able to complete her internship,and their first son, Ronald, was born onthe last day of her last elective.Ron promptly took over at home,as Rosanne started her second year.“Once you’ve done residency training,you’re prepared for anything,”he says. “You have your medical joband your parent job. You do this, andthen you do that, then you run backand do something else, and you figureout ways to do it at the highestlevel you can.”“We were pros by the time Thomaswas born 21 months later,” saysRosanne. And when Meghan was born— at <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> UniversityHospital, like her brothers — Ron wason the full-time faculty at RWJMS, andRosanne was working part-time in the<strong>Rutgers</strong> Community Health Program.Still, Rosanne’s mornings could startwith a “4:00 AM schlep” to North Jerseyto drop off the children with theirgrandparents and get back to work inNew Brunswick by 7:00. “WhenRonald was little,” says Rosanne,“the car was a second home to him;he called it ‘the moving room.’”Sometimes she took the childrenalong to work, with toys and sleepingbags, but the logistics paled by comparisonwith the residency years.“<strong>The</strong>re weren’t a lot of options,” shesays. “You knew this was the way itwas going to be, so you just did it. Inever felt overwhelmed or depressed.We knew we’d get through it —though now I wonder how!”With plans to marry duringtheir last year of medicalschool, Christina and MarkReiter entered the Couples Match. “Itadds a layer of complexity to thematch process,” says Christina, whointerviewed with 26 programs toensure the optimum match. “But itworked out well: neither of us had tosacrifice, and we both got our firstchoice.” Christina matched with theanesthesia residency at Duke University<strong>School</strong> of Medicine and Markwith the emergency medicine residencyat the University of North Carolina<strong>School</strong> of Medicine.<strong>The</strong> Mazzarellis, who graduatedthree years apart, didn’t haveto navigate the obstacle courseof residency years. While Joanne wascompleting her clinical years, Anthonywas in the second year of his residencyin emergency medicine atCooper <strong>Medical</strong> Center. When Joannematched with her first-ranked choice,the internal medicine residency at theUniversity of Pennsylvania <strong>School</strong> ofMedicine, Anthony was a newlyappointed faculty member in theRWJMS Department of EmergencyMedicine, working in the EmergencyDepartment at Cooper. Joanne hassince completed her residency as wellas a three-year fellowship in cardiovasculardisease at Cooper, where shewas chief fellow.From This Day ForwardWhile the 21st-century alumni are busily building and shaping theircareers, the graduates from the 1970s and 1980s are starting toreduce their hours or following new career paths.When Larry Schenk finishedhis training, he and Mauramoved to Binghamton, NewYork, and went into private practice.In 1991, the family journeyed toNepal, where Larry took the childrentrekking and sightseeing, while Mauradid cataract surgery and taught aboutglaucoma. “In South Asia, cataractsare the predominant cause of blindness,”says Maura. “Two-thirds of theburden of blindness in the world isborne by women, though they are lesslikely to get the care needed.”She returned to the region everyyear as a volunteer with the SevaFoundation (seva means “service” inSanskrit). In 1995, she started an eyecare program to train and lead teamsthat perform cataract surgery. Establishedin the Tibetan AutonomousRegion, it has since expanded to threeother western Chinese provinces andsouthern Tibet.To better prepare herself, Mauraearned a master’s degree in publichealth at Johns Hopkins University. Shealso retired from private practice.Although 40 million people in theworld are blind, she says, ophthalmologistsdon’t have a lot of opportunities to“give back.” But she found a way notonly to volunteer, but also to help developa sustainable social system in aregion with a vast need.50 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
[ Beginnings ]Ten years ago, Larry and Maurabought a house in Umbria, Italy, wherethey live for four months a year, as heinches toward retirement. An avid gardener,he tends his vineyard and 400olive trees. He has also followed his loveof biking across the United <strong>State</strong>s, Italy,New Zealand, Scotland, and France.As Hubert and Michele <strong>Johnson</strong>reminisce, shared memoriesemerge of outstanding RWJMSfaculty, such as the late Pamela Champe,PhD, professor emeritus of biochemistry.“You never realize how much they haveinfluenced you,” says Hubert, “and youcan never thank them enough.”Michele was in solo practice for 23years before joining a seven-physician,hospital-based practice and a coveragegroup that guarantees her an occasionalnight’s sleep. While still practicing obstetrics,she specializes in office-based,minimally invasive gynecologic procedures.Hubert works in Partners Health System,the largest health care provider inMassachusetts, and is associate chief ofvascular surgery at North Shore <strong>Medical</strong>Center. He holds an appointment as clinicalassociate professor of surgery atMassachusetts General, where he hasserved on the faculty for 24 years. From2007to 2008, Hubert did an endovascularfellowship at the Cleveland Clinic.“From the time you start, keep your eyeson the prize,” he says. “You just want tobe good doctors and good parents.”Michele and Hubert recall superbviews of the <strong>Rutgers</strong> University GolfCourse from classrooms in the ResearchTower at RWJMS. Years later, Hubert gothooked on the game and then surprisedMichele with her own set of clubs. “He’dbeen figuring out what we would do togetherwhen we retire,” says Michele.<strong>The</strong> clubs have accompanied them totheir 15th Reunion at RWJMS and towonderful golf courses around the world.While practicing, RosanneNahass scheduled officehours so that she would be athome when the children got off theschool bus, and a sit-down dinner waspart of the family’s daily routine. “Timetogether meant spending time as a family,whether it was vacations or weekendoutings,” says Ron.In 1980, Rosanne had put a careerin piano performance on hold asshe entered medical school. After shepracticed internal medicine for 18years, her interest in the pianowas rekindled. She resumed her ownmusical career as a student at theWestminster Choir College of RiderUniversity, in Princeton.A 2004 performance opportunity at<strong>Rutgers</strong>’ Zimmerli Art Museum led toa new position, as the museum’spianist in residence. Her medical practicesimmers on the back burner as shedelves into her “Art of Music” project,presenting exhibition-linked lecturesand recitals.Ron’s career has taken a new directionas well. In 2001, he founded andbecame president of the 33-physicianID Care, in Hillsborough. In additionto running the practice and serving asan attending physician at several areahospitals, he is earning a master of sciencein management degree at theHarvard <strong>School</strong> of Public Health. <strong>The</strong>program links his interests in healthcare reform, practice management,and clinical care, topics he covers inregular lectures to house staff andsmall groups at RWJUH.Mark and Christina Reiterpractice at St. Luke’s <strong>Medical</strong>Center, in Bethlehem,Pennsylvania, where they also serve onthe clinical faculty of the Temple University<strong>School</strong> of Medicine. <strong>The</strong>ir firstdaughter, born during the last year ofChristina’s fellowship at UNC, has beenjoined by two sisters, born two yearsapart.Combining his interests in medicineand business, Mark founded EmergencyExcellence, a consulting companydedicated to improving emergencydepartment performance. With 40clients, Em-Ex has become a secondfull-time job, but he decided thatworking harder at this point wouldgive him time with his family as thegirls grow up.<strong>The</strong> Mazzarellis’ shared love oftravel has taken them around theworld not just as tourists, butalso because they share an interest incommunity and global health. Joanneand Anthony served with InternationalHealthcare Volunteers (IHCV) on amedical mission to Ghana led by JamesAikins, MD, associate professor of obstetrics,gynecology, and reproductivesciences. Joanne also spent two monthson a medical mission to Gaborone,Botswana, while a resident at the Universityof Pennsylvania. She now serveson the board of directors of IHCV.<strong>The</strong>y enjoy having medical careersthat can interact but remain distinct.She practices cardiology at CooperUniversity Hospital, while Anthony isan adjunct assistant professor of emergencymedicine working one day aweek in the Emergency Department.He also serves as administrative vicepresident of strategic planning andimplementation at Cooper.Life evolved with the birth of Sophia,at the end of Joanne’s cardiology fellowship.Now the Mazzarellis don’t talkshop at home. “Anthony has changed!”Joanne says. “We turn off our cellphones as soon as we walk through thedoor, and as long as Sophia’s awake,we’re not on the computer.”“Sophia is the focus,” Anthony adds,“because, as you can imagine, everythingshe does is wonderful.” M<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 51
<strong>The</strong> American College of Emergency Physicians section of Emergency Ultrasound now requires training in bedside ultrasound for all emergencyphysicians.“Our residents will leave here completely prepared. We dedicate one month of training to bedside scanning, after which they must take bothan online and hands-on examination,” says Rajesh N. Geria, MD, assistant professor and chief, division of emergency and critical care ultrasound.52 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINEJOHN EMERSON
By Lynda RudolphBedsideUltrasound:ALIGHTI N T H ESTORM“Why work in the dark when you have a flashlight?” That’s the analogyused by Rajesh N. Geria, MD, assistant professor and chief, division ofemergency and critical care ultrasound, when he’s explaining the value of bedsideultrasound to emergency medicine residents. Patients may consider it more of aguiding light in the tumultuous storm of an emergent health situation.“It enables us to take a closer look in the Emergency Department and get the yesor no answer we need,” says <strong>Robert</strong> M. Eisenstein, MD, associate professor andinterim chair, Department of Emergency Medicine. Because physicians can pinpointa problem quickly, without the risk of moving patients, potential life-anddeathtreatment decisions can be made virtually instantly.<strong>The</strong> size of a laptop computer and easy to transport, bedside ultrasound isbecoming a new point-of-care tool with a high degree of clarity and resolution,providing clear direction to physicians in critical care situations.Lifesaving and Time-Saving Applications<strong>The</strong> power of the technology in the Emergency Department lies primarily inits ability to help physicians evaluate unstable patients. If an older personcomes into the ED with lower back pain, bedside ultrasound can look for anabdominal aortic aneurysm. “We can actually call a code aorta — alerting the vascularsurgeons that we have an abdominal aortic aneurysm — in order to rapidlyexpedite care,” says Dr. Geria.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 53
If a woman appears with severe pelvicpain, bedside ultrasound can determineif there is an ectopic pregnancy. “We hadone patient who was in shock and weused the ultrasound to find the pregnancyin the adnexa,” recounts Dr. Geria.“Five minutes after she came throughthe door, we called the senior OB residentand they took her to the OR.” For pregnant womenwho enter the ED concerned that the fetus has stopped moving,bedside ultrasound provides invaluable peace of mindwhen they learn there is a heartbeat.In fact, there are several core applications, including cardiacand FAST trauma, looking for cardiac activity in cardiacarrest situations and signs of fluid around the heart(pericardial effusion) and in the abdomen (hemoperitoneum),that allow the trauma team to immediatelychange clinical management at the bedside.<strong>The</strong> technology is also very useful for providing proceduralguidance and increasing productivity in theEmergency Department. For example, difficult peripheralintravenous lines are now being placed using ultrasoundguidance, where the needle is visualized entering the vein.Using this technique results in a decrease in the number ofblind attempts and therefore the number of complicationssuch as infection and arterial puncture. If a successfulperipheral line can be placed using ultrasound guidance, themore invasive central lines can be avoided.While not a substitute for traditional radiology, bedsideultrasound technology is very goal-directed. Rather thanbeing used for comparable studies, it’s performed andinterpreted by the emergency physician at the bedside tofind specific things and answer specific questions. It focuseson a limited study to rule out life-threatening illnesses.A New Standard of Care —a New Curriculum RequirementBedside ultrasound is now a standard of care inemergency rooms. At <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> UniversityHospital, there are four machines now in use in theEmergency Department: two for the trauma team and twofor the Emergency Department team. <strong>The</strong> first ultrasoundmachine was purchased in 2006.<strong>The</strong> American College of Emergency Physicians sectionof Emergency Ultrasound — of which Dr. Geria recentlybecame the chair-elect — now requires training in bedsideultrasound for all emergency physicians. Everyone whograduates must be prepared to perform the proceduresand interpret the findings. “Our residentswill leave here completely prepared,”says Dr. Geria. “We dedicateone month of training to bedside scanning,after which they must take bothan online and hands-on examination.”<strong>The</strong>se skills are also taught to medicalstudents within the emergencymedicine clerkship and dedicated four-week elective. <strong>The</strong>education also appeals to students from radiology and surgerybecause 90 percent of the training is hands-on. “<strong>The</strong>program is always full,” says Dr. Geria. <strong>The</strong> hands-ontraining has become a differentiator for the program atUMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong> as studentsand residents are exposed to a wide variety ofpathology, an abundance of trauma and critical care, andhigh severity of illnesses.Efforts are also under way to train nurses and physicianassistants in using the technology.A New DivisionSpearheads Change<strong>The</strong> new division of emergency and critical careultrasound at RWJMS gives official status to the newtechnology and highlights its importance within the medicalschool and the hospital. Both Dr. Geria and Daniel S.Morrison, MD, assistant professor of emergency medicine— a second member of the team and respected ultrasoundauthority — are fellowship-trained in bedside ultrasound.Four emergency medicine physicians also commitextra time to do shifts with students, lecture, and speak atconferences.<strong>The</strong> division has established some ambitious goals,including interdepartmental collaboration with otherphysicians — including critical care and internal medicinespecialists and surgeons — on not only clinical protocolsbut research as well. Also in the plans are the initiation ofa fellowship program by 2013 and the creation of an interfacethat will link the Web-based archival system to thehospital system for medical records and order entry,allowing consultants to view emergency ultrasoundreports from anywhere within the hospital.<strong>The</strong> objective is to position the division as a center ofexcellence within the medical school and hospital, creatingopportunities for research, interdepartmental collaboration,advanced education, training, and improvements inpatient care. This light in a storm benefits not just patientsbut also physicians and scientists. M54 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
KnifeT H A T I S N ’ T O N E I SAR E V O L U T I O N I Z I N GB R A I N A N D S P I N ES U R G E R Ywhen someone says “surgicalknife,” your mindprobably conjures up animage of a typical scalpel. Butfor brain surgery — and in particularfor brain metastases — the term “knife”applies not to steel but to a technology thatcombines radiation and physics. Known asthe Gamma Knife, it’s a surgical tool that’sbeen around for more than 40 years. But fourdecades of refinements have dramaticallyincreased its capabilities and outcomes. <strong>The</strong>Gamma Knife Perfexion is the most advanced,non-invasive alternative treatment to intracranialproblems — and it hasn’t existed incentral New Jersey until now.ALAN SCHINDLER/COURTESY OF ROBERT WOOD JOHNSON UNIVERSITY HOSPITALB Y L Y N D A R U D O L P H<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 55
<strong>Robert</strong><strong>Wood</strong> <strong>Johnson</strong>University Hospital(RWJUH) acquiredthe most advancedversion of the GammaKnife technology —called Gamma KnifePerfexion — in March 2011.<strong>The</strong> RWJUH Gamma KnifeCenter was specially designedto house the GammaKnife Perfexion. Left to right:Neil Butler, RN, nursecoordinator, Gamma KnifeCenter; Venkat Narra, PhD,associate professor ofradiation oncology; andShabbar F. Danish, MD ’01,assistant professor of neurosurgery,director, stereotacticand functionalneurosurgery, anddirector, GammaKnife Center atRWJUH.56 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
BELOW: JOHN EMERSON<strong>The</strong> Gamma Knife wasfirst used in Sweden in 1968. <strong>The</strong> first installation in theUnited <strong>State</strong>s occurred in 1987. According to ElektaNeuroscience — the manufacturer of the Leksell GammaKnife — Gamma Knife surgery has been used to treat morethan 500,000 patients. <strong>The</strong> number of patients treatedper year has increased by 300 percent since 2006. <strong>The</strong>advantages — providing treatment that is less invasiveand less harmful to normal brain tissue surroundingtumors — are favored by clinicians and patients alike.“This technology is thegold standard of precisionin intracranial applicationsrequiring sub-millimeteraccuracy of radiationdelivery.”— Ning Jeff Yue, PhD, professorand vice chair, Department ofRadiation OncologyLEFT: ALAN SCHINDLER/COURTESY OF ROBERT WOOD JOHNSON UNIVERSITY HOSPITAL<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> University Hospital (RWJUH)acquired the most advanced version of the GammaKnife technology — called Gamma Knife Perfexion —in March 2011. It was used for head and neck radiosurgeryfive years ago and has come to represent the mostadvanced application of radiosurgery, with its greater flexibilityand convenience in treatable volume and dose planning.<strong>The</strong> RWJUH Gamma Knife Center was speciallydesigned to house the Gamma Knife Perfexion.“This technology is the gold standard of precision inintracranial applications requiring sub-millimeter accuracyof radiation delivery,” says Ning Jeff Yue, PhD, professorand vice chair, Department of Radiation Oncology.“Older versions were more cumbersome. But the latestgeneration is flexible and streamlined.”<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 57
58 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINEM
R A D I O S U R G E R Y H A R D W A R EA N D P R O T O C O L S D I F F E RF R O M H O S P I T A L T O H O S P I T A LA“ll radiosurgery technology is not the same,”cautions Shabbar F. Danish, MD ’01, assistantprofessor of neurosurgery, director, stereotacticand functional neurosurgery, and director,Gamma Knife Center at RWJUH. “In NewJersey, there is overlapping technology, and it’s important toknow that Gamma Knife is the only radiosurgery that wasbuilt specifically for use on the brain.“<strong>The</strong> importance of training is paramount to surgeonsusing the Gamma Knife,” adds Dr. Danish. “Many surgeonsdon’t have fellowship training.” Dr. Danish hascompleted a fellowship in Gamma Knife radiosurgery.In fact, RWJUH is the only facility in New Jersey thathas a dedicated team, including a neurosurgeon, radiationoncologist, and medical physicist, all specially trained andcertified for Gamma Knife surgery using the Perfexionmodel. <strong>The</strong> same team performs the radiosurgeries everytime — without using substitutes.ALAN SCHINDLER/COURTESY OF ROBERT WOOD JOHNSON UNIVERSITY HOSPITALT H E A D VA N T A G E S O FcT H E L A T E S T G E N E R A T I O Nurrently being used for brain cancer and totreat arteriovenous malformation (AVM), paindisorders, and tremor, the Gamma KnifePerfexion has several advantages compared toearlier versions of the technology. “<strong>The</strong>re is a greatlyreduced treatment time, and because the technology isfully robotic, we can adjust the positioning, makingpatients more comfortable, and provide more conformaldose coverage,” says Dr. Danish.Perfexion streamlines work flow and can deliver treatmentto one or more tumors in a single session. It can treat lesionsin the sinuses, orbits, and upper cervical spine. Because of itsunique automated collimator, it offers greater accuracy, conformity,and dosimetry. “Because there is less beam time,there is less radiation scattered to surrounding tissue such asthe thyroid, pelvis, and breast,” says Dr. Danish. “<strong>The</strong> abilityto treat more complex tumors and deliver a more finitedose leads to the potential for better outcomes.”<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 59
A C O M F O R T A B L EP A T I E N T E X P E R I E N C EBefore treatment, a stereotactic head frame isattached painlessly to patients. <strong>The</strong> frame is designedto prevent head movement during the procedure,ensuring that only the targeted area receives theradiation. Imaging tests are conducted, to precisely pinpointthe size, shape, and location of the tumor. Markers areplaced on the head frame to serve as a pattern for the plannedtreatment. Once brain images are computerized andthe treatment plan is completed, the patient, while stillawake, moves into the dome section of the unit for the procedure,which on average lasts 45 minutes.“In most cases, patients need only one single treatment;a few others require more,” says Dr. Yue. “It really dependson the size and number of the tumors and how close theyare to other critical organs.” Dr. Yue also cautions that theprocedure isn’t right for every tumor diagnosis: “It’s a betteralternative to invasive surgeries when the tumors aresmall. However, sometimes it’s impossible to conductradiosurgery. If the tumors are large, or in the case of certaindiseases, other options may need to be considered.”C A N D I D A T E S F O RG A M M A K N I F E T R E A T M E N TGamma Knife stereotactic radiosurgery can be atreatment recommendation for patients with brainlesions that are four centimeters or smaller in diameter.It is also a treatment option for patients who have noother apparent course of action. In addition, Gamma Knifemay be used on patients who have had prior radiationtreatments, in the case of a cancer recurrence.For patients with disease of the brain, the GammaKnife — requiring no incision and as a result with a farsmaller risk of complications — provides an optionthey didn’t have locally until now. MPHOTO ALAN SCHINDLER/COURTESY OF ROBERT WOOD JOHNSON UNIVERSITY HOSPITAL60 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
l e t t e r f r o m t h ea l u m n i a s s o c i a t i o np r e s i d e n tDear Alumni and Friends:It is my pleasure to welcome you to the spring issue of <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> Medicine! It is an excitingtime to serve as the president of the <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong> Alumni Association. We are lookingforward to another successful year with many opportunities to mentor current RWJMS students, reunitewith classmates, and collaborate on a variety of initiatives. We began our year with the 24th Annual CareerNight, with Dean Amenta again joining us to open the evening. I would like to express my thanks to all thosewho volunteered their time to make this event a success (see Career Night article on page 64).We are very excited to announce our support of the Second Annual Scholarship Gala to Celebrate withAlumni and Friends on Saturday evening, April 21, 2012, at <strong>The</strong> Heldrich in New Brunswick. With increasingfinancial demands on our students, the ability to offer scholarship support has never been more important.RWJMS attracts an incredibly talented and diverse group of young men and women who are the future ofmedicine. Our students and alumni are recognized in the region and beyond for their contributions in patientcare, education, research, and community health. Our colleagues across the country clearly agree, as this yearour students achieved the remarkable accomplishment of a 100% Match!At the Gala we will enjoy an evening with friends, classmates, and colleagues, while providing much-neededfinancial support for our RWJMS students. Last year, the Gala raised more than $205,000, from which weawarded 18 scholarships in the amount of $10,000 each. We will honor the anniversaries of the followingclasses: 40th: 1972, 35th: 1977, 30th: 1982, 25th: 1987, 20th: 1992, 15th: 1997, 10th: 2002, 5th: 2007.I look forward to seeing everyone there!As you are aware, the Alumni Association has a long history of striving to providesupport for the young men and women who attend RWJMS. Through the efforts ofthe Alumni Association and the generous support of our donors, we will award$140,000 in scholarships and loans to RWJMS students in the 2012–2013 academicyear. We thank you for your contributions during this very difficult financial climateand ask for your continued dedication to this cause.<strong>The</strong> Alumni Association is a wonderful way to keep in contact with fellow classmates,network with other colleagues, socialize with our students, collaborate oncommunity/institutional projects, and keep abreast of the ongoing advancements atRWJMS. We welcome all alumni and invite you to contact <strong>Robert</strong>a Ribner atribnerrs@umdnj.edu if you are interested in learning more about the Alumni Association. I want to thank thepast presidents of the Alumni Association and members of the Board of Trustees for all the work that theyhave done and continue to do. It is my hope that we can continue to accomplish wonderful things togetherthis year.Sincerely,STEVE HOCKSTEINTamara A. LaCouture, MD ’94President, RWJMS Alumni AssociationP.S. Please visit our Web site at http://rwjms.umdnj.edu/alumni and click on Make a Gift to contributeto the 2012 Alumni Association Annual Fund or mail your gift in the envelope enclosed in the magazine.In addition, please join the Alumni Association on Facebook.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 61
UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong><strong>Medical</strong> <strong>School</strong> andthe Foundation of UMDNJInvite You to Attend theT H E S E C O N DA N N U A LS C H O L A R S H I PT O Celebrate W I T H A L U M N I A N D F R I E N D SSaturday, April 21, 2012<strong>The</strong> HeldrichNew BrunswickNew Jersey6:30 pmCocktails andSilent Auction7:30 pmAwards PresentationDinner and DancingBlack TieFor more information,call 732.729.4670.✴2012 Gala Honorees:MERITORIOUS SERVICE AWARDHarvey A. Holzberg, MBA, FACHEPresident Emeritus<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> University HospitalDISTINGUISHED ALUMNI AWARDDonald Rose, MD ’80Clinical Associate Professor of Orthopaedic Surgery, NYU <strong>School</strong> of MedicineFounding Director of the Harkness Center for Dance InjuriesNYU Hospital for Joint DiseasesHONORARY ALUMNI AWARDTO BE AWARDED POSTHUMOUSLYStephen F. Lowry, MD, MBAProfessor and Chair, Department of Surgery, Senior Associate Dean for EducationUMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong>HONORING THE FIRST CLASS: CLASS OF 1968CELEBRATION OF THE FOLLOWING ANNIVERSARY CLASSES:40th: 1972 ■ 35th: 1977 ■ 30th: 1982 ■ 25th: 198720th: 1992 ■ 15th: 1997 ■ 10th: 2002 ■ 5th: 2007
w j m s • a l u m n iNEWSAlumni Association Awards HippocratesScholarship To Sophia Sequeira ’15Sophia Sequeira’15Sophia Sequeira ’15,of Millstone, is theAlumni Association’stenth Hippocrates Scholar.<strong>The</strong> association awards thescholarship annually to anincoming first-year studentbased on academic excellence.Hippocrates Scholarsreceive $20,000 towardtheir tuition each year.Hippocrates Scholarslearn about their selectionfrom Carol A. Terregino,MD ’86, associate professorof medicine, interim seniorassociate dean for education,and associate dean foradmissions. Describing herreaction to Dr. Terregino’scall, Sophia says, “I wonderedif she was calling totell me I’d forgotten somethingon some form. WhenI realized it was about ascholarship, I was veryexcited, but I thought shemeant it was, maybe,$2,000. It just couldn’t sinkin that it was $20,000.I am so grateful!”Sophia was 12 yearsold when her grandmother,“the backboneof the family,” developedterminal braincancer. English was nother parents’ first language,and Sophiasensed their frustrationwhen the physicians’ explanationscame up short.”As I grew up, I learned howhelpful it is when physicianscommunicate well with theirpatients and patient families.Irealized I wanted to becomea physician who really focusedon communicationwith patients and who workedto create a solid patientphysicianrelationship.”<strong>The</strong> sciences have alwaysbeen Sophia’s favorite subjects,because she finds themthe most challenging. AtWilliams College, she majoredin biology with a concentrationin biochemistry andwrote an honors thesis onthe molecular basis of stemcells in leeches. “Yes, leeches,”she repeats with a laugh.“<strong>The</strong>y were good organismsto study because they havelarge stem cells and carrytheir embryos outside theirbodies.”She was accepted for aSTEVE HOCKSTEINone-year assistantship at theWomen’s Health Center atthe Atrium <strong>Medical</strong> Center,in Cincinnati, where sheaided with procedures andreferrals and helped patientsunderstand their mammogramresults. Her mentor,radiologist Hugh Hawkins,MD, says that when he firstinterviewed Sophia, “shecame across as a doctor: aleader, a team player, strongacademically, and an excellentcommunicator.” He becameher role model, exemplifyingthe communicationskills her family had neededduring her grandmother’sillness.<strong>The</strong> internship reinforcedher decision to go to medicalschool. “I was really set onRWJMS,” says Sophia. “Iwanted to come home formed school. I see myselfpracticing and giving backin the community where Igrew up.”— K.O’N.Communicate with Alumnion Social Media SitesRWJMS newsand eventsand an opportunityto participate inconversations withalumni and studentsare now availableon facebook.com,linkedin.com, and twitter.com.On Facebook and LinkedIn, search for“UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong><strong>School</strong>” and “<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong><strong>School</strong> Alumni Association.” On Twitter, searchfor “UMDNJ_RWJMS.” Participation onFacebook and LinkedIn is by approval of thesite administrator, but all can register.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 63
w j m s • a l u m n iNEWS1Alumni AssociationHosts 24th AnnualCareer Nightby Kate O’NeillCareer Night, a long-standingAlumni Association tradition,is always a highlight ofthe RWJMS winter calendar. <strong>The</strong>24th Annual Career Night, held onJanuary 17, attracted more than50 alumni volunteers, representing25 specialties. Students gatheredin the Great Hall to enjoy dinnerand the opportunity to discussmedical specialtieswith alumni, forwhom the event alsoserved as a minireunion.PsychiatristRicardo Fernandez,MD ’79, was gratefulto see, still in place,2the Renaissanceeraanatomical posters that havealways adorned the Great Hall. “Itwas very nostalgic for me to returnto the place where I first entered thisgreat society of medicine, which Ifeel so fortunate to belong to,” hesays.Dr. Fernandez looks forward toputting Career Night on his 2013calendar, and he also signed up forthe Alumni Association’s A Day inthe Life program.For further information onCareer Night, A Day in the Life, andother Alumni Association programs,please contact <strong>Robert</strong>a Ribner,coordinator, Alumni Affairs:ribnerrs@umdnj.edu.64 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE31: Alumni andstudents enjoy goodconversations aboutmedical specialties anda delicious dinner.2: OncologistEduardo Fernandez,MD ’89, discussescareer choices witha student.3: Ursula Pogany,MD ’81, discussescareers in pediatrics.4: Scott Woska,MD ’97, counselsstudents on careers inphysical medicine andrehabilitation.5: AnthonyMazzarelli, MD ’02,advises students oncareer options.45
789Two dogs bought five partly silly trailers, and irascible bureaux easily fightsumpteen aardvarks. One obese television tickled umpteen mats. Bureaux10116: Pediatrician Lee Vogel,MD ’80, shares hisexperiences.7: Marissa DeFreese, MD’03, talks about herexperiences as an acutecare surgeon.8: Tamara LaCouture, MD’94, president, AlumniAssociation, discussescareers in radiationoncology.9: Lynn Helmer, MD ’82,advises students oncareers in medicaladministration.10: Sonia Garcia Laumbach,MD ’99, assistant professorof family medicineand communityhealth and assistantdean for student affairs,counsels students oncareer options.11: Francine Sinofsky, MD’81, and FrederickLicciardi, MD ’86, sharetheir experiences inOB/GYN with students.12: Lasanta Horana, MD’04, discusses careersin emergency medicine.1312614PHOTOS BY KIM SOKOLOFF13: Sundip Patel, MD,talks about hisexperiences as anemergency medicinephysician.14: Michael Rosenberg,MMS ’74, MD, discussescareer options inneurology.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 65
A L U M N I P R O F I L EVered Stearns, MD ’92:D E V E L O P I N G A N D D E L I V E R I N GP E R S O N A L I Z E D C A N C E R T R E AT M E N TIn oncology, the trend istoward whole-patient treatment.This suits VeredStearns, MD ’92, to a T. Dr. Stearns, a dedicated, accomplished,and resourceful clinician-scientist, is working on several “outside-the-box”lines of breast cancer research, always with thepatient as her first priority. An associate professor of medicineat the Johns Hopkins <strong>School</strong> of Medicine, she was appointed in2010 as co-director of the Breast Cancer Program at the schoolof medicine’s Sidney Kimmel Comprehensive Cancer Center.Dr. Stearns recalls a turning pointduring her fourth year at UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong>,Camden campus. She was still lookinginto her career options when she spentseveral weeks on a clinical rotation inthe oncology unit at Cooper UniversityHospital. “I was struck by the closeconnection between the doctors andtheir patients,” says Dr. Stearns. “I’dnever wanted to be a generalist, and Iliked the idea of providing specialtycare while also becoming that patient’sprimary care physician.”During her residency in internal medicineat Georgetown University <strong>School</strong>of Medicine, Dr. Stearns began to focuson solid tumor oncology and then onbreast cancer in particular. “It was anamazing experience,” Dr. Stearns recalls.Working with patients, families,and clinical care teams in the outpatientoncology unit, she gained a better senseof the field as a whole and of the growingsub-specialty of outpatient care forpatients with breast cancer.As she completed a medical oncologyfellowship at Georgetown University<strong>Medical</strong> Center and the affiliatedLombardi Comprehensive Cancer Center,her interest in translational researchevolved. “I felt the need to find bettertreatments and decided to combineresearch and clinical care,” she says.In 1996, Dr. Stearns sought out asa mentor Daniel F. Hayes, MD, aninternationally renowned leader inbreast cancer research. “She was waitingat my office door the day I arrivedat Georgetown,” he recalls, “and toldme: ‘I want to study breast cancer.’”She became a valued member of hislaboratory and subsequently movedwith the team to the University ofMichigan Comprehensive CancerCenter.Her work with Dr. Hayes exposedDr. Stearns to a wealth of advancedpharmacogenetic-based research. Shebecame a leader in the multi-center,multi-disciplinary Consortium onBreast Cancer Pharmacogenetics(COBRA), which seeks to create personalizedprevention and treatment ofeach patient’s breast cancer. By establishinga molecular profile of the cancer,based on a blood test, COBRA aimsto discover how genes alter an individualpatient’s response to a drug.<strong>The</strong> study focuses on the commonchemotherapy drug tamoxifen and aclass of drugs known as aromataseinhibitors. Identification of patientsfor whom tamoxifen is wrong wouldlead to safer, more effective treatmentwith fewer negative side effects.Dr. Stearns has been awarded significantfunding. As a junior investigator,she received prestigious clinical66 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
investigator awards from the AmericanCancer Society and the DamonRunyon Cancer Research Foundation.In addition, she was the first recipientof the American Society for ClinicalOncology’s Advanced Clinical ResearchAward. Subsequent grantsfrom the National Institutes ofHealth, the Breast Cancer ResearchFoundation, and the Mary Kay AshCharitable Foundation, as well as severalgrants from industry, helpedadvance her research and providedmore time to work with her mentors.COURTESY OF VARED STEARNS, MDA Johns Hopkins faculty membersince 2002, Dr. Stearns continues topursue novel approaches to breastcancer research and treatment. One ofher strategies is the use of molecularmarkers to target clinical trial participants.Groups of several hundredgenetically profiled participants maywell provide more useful results —leading to more effective treatmentand better treatment outcomes — thanmight come from a trial that enrolledthousands of unprofiled patients.Along with Sara Sukumar, PhD, codirectorof the Kimmel Cancer Center,Dr. Stearns is also exploring the viabilityof administering powerfulchemotherapy drugs in decreasedamounts directly into the ductal systemof the breast. Because most breasttumors originate within the ductaltree, the researchers hope this radicaltechnique will prevent the developmentand spread of the disease.In a third area, Dr. Stearns is workingwith the knowledge that some, butnot all, forms of breast cancer areestrogen receptive and can be treatedwith anti-estrogen therapy. Pursuingresearch in collaboration with severalJohns Hopkins faculty members andher former mentor Nancy Davidson,MD, she seeks to alter the non-receptivegenes, making them estrogen receptiveand thus treatable.“Vered is a great scientist, but sheisn’t hung up on her science. She’salways thinking about the patient,”says Dr. Hayes. “She’s a great teacher,already preparing the next generationof people. And she’s a terrific clinician.I’d want anyone in my family tobe treated by her, and that’s the highestpraise you can give.” MB Y K A T E O ’ N E I L L<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 67
A L U M N I P R O F I L EJohn Hohneker, MD ’85:DEVELOPING DRUGSTHROUGH THE PARADIGM OFCANCER RESEARCHIn February 2011,Novartis Pharmapromoted John Hohneker ’85 to seniorvice president and global head of development,integrated hospital care. With the newposition came a move from Morristown, toBasel, Switzerland, home of the corporation’sglobal headquarters. <strong>The</strong> assignmentis an ideal match for Dr. Hohneker’s passionfor science and his meticulous approach todrug research and development.<strong>The</strong> culture and location are an equally good match for hisoutside interests: travel, hiking, theater, gastronomy, andnow, Old World wines. “Everything in Switzerland works!”he says. “<strong>The</strong> trains are on time and reliable. Many of thebillboards advertise watches. Clearly they are obsessed withtime—and, of course, chocolate.”In high school, Dr. Hohneker loved science, especiallybiology, including laboratory dissection. “I began to thinkhow cool it would be to discover new medicines,” he recalls,“and I was lucky to have a biology teacher who recognizedmy interest and encouraged me to pursue medicine.”After earning a bachelor of arts degree in chemistry atGettysburg College, he entered <strong>Rutgers</strong> <strong>Medical</strong> <strong>School</strong>. “Igot an excellent scientific foundation in medicine, courseslike medical physiology and pathology,” he says.JOHN BIONDO68 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
“Oncology ispaving a new way for drugdevelopment by focusing onthe genetics and biology ofdisease,” says Dr. Hohneker.“We are applying these principlesto broader areas ofmedical research.” He adds,“Cancer research providesthe paradigm for future drugdevelopment.”During medical school, Dr. Hohnekerwas first introduced to his future field ofexpertise, medical oncology. During histhird-year clinical rotations, he recalls,he followed a few cancer patients ofMichael Nissenblatt, MD, a communityphysician who is now a clinical professorof medicine at RWJMS.Dr. Hohneker was Alpha OmegaAlpha at RWJMS, which acquired itsnew name during his graduation year.He did a three-year internship and residencyat the University of NorthCarolina (UNC) at Chapel Hill, wherehe found a true mentor in John Parker,MD, a professor of medicine in the divisionof hematology/oncology.“John was the person who really gotme interested in oncology,” Dr. Hohneker says. “We oftenreviewed the blood smears of leukemia patients on admissionto the hospital and made their diagnosis. I’m not suremany physicians these days actually look at their patients’blood smears under a microscope.”He adds, “John was amazing — a triple threat: he was agreat teacher, a superb physician, and an excellentresearcher. Sadly, he passed away from lung cancer duringmy oncology training.”With the exception of his first year of a hematology/oncology fellowship at the University of California at SanDiego, Dr. Hohneker was in Chapel Hill for 16 years. AtUNC, he completed his fellowship, which also includedtraining in drug development sponsored by BurroughsWellcome. He continued to work for the company as a seniorclinical research physician in oncology research, whileserving as an adjunct professor of medicine.In high school he had imagined himself discovering newmedicines; in the pharmaceutical industry that he had achance to realize his dreams. While at Burroughs Wellcome,he led the development of Navelbine, a treatment for veryadvanced lung cancer, and successfully guided it throughthe regulatory approval process.When Burroughs Wellcome and GlaxoSmithKline mergedand the new corporation was renamed Glaxo-Wellcome, Dr. Hohneker became the head of clinical developmentfor oncology. Four years later, he was appointedworldwide therapeutic area head, oncology. “Canceris fascinating, because it isn’t a single disease and no singleorgan is typically involved,” hesays. “You have to look at the interactionof multiple facets to understandthe disease.”Dr. Hohneker felt some ambivalencewhen, in 1995, Novartis offered himthe position of vice president, U.S.medical affairs, oncology. In acceptingthe position, he would be ending a longand productive relationship withGlaxoWellcome. At Novartis, however,he would have the opportunity to workon a variety of late-stage drugs, includingnew “targeted” therapies. This isan area of research that particularlyinterests Dr. Hohneker and wouldprove a major factor in his decision toaccept the offer from Novartis.“Understanding the specific genetic drivers of tumors isessential to finding successful treatments for patients,” hesays. “Novartis is committed both to this approach and todeveloping drugs for people without treatment alternatives.It’s extremely rewarding.”Dr. Hohneker served in this position for ten years; leadingclinical research teams, he ensured proper clinical trialsand adherence to good clinical practice. <strong>The</strong> developmentof targeted cancer therapies in North America was his focusduring this period.Now, in his new position with Novartis, as global headof development, integrated hospital care, Dr. Hohneker hasexpanded responsibilities. Although the methodology ofcancer research is still embedded in his thinking, the focusof his work has moved to other areas of disease. He directsand manages project leaders and heads of clinical supportunits for the Integrated Hospital Care Franchise, whichincludes organ transplant/nephrology and rheumatology/autoimmune diseases, as well as anti-infectives. In theseareas, he is responsible for taking drugs through the latestagedevelopment and regulatory approval processes.“Oncology is paving a new way for drug developmentby focusing on the genetics and biology of disease,” saysDr. Hohneker. “We are applying these principles to broaderareas of medical research.” He adds, “Cancer researchprovides the paradigm for future drug development.” MB Y K A T E O ’ N E I L L<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 69
C L A S SNOTESWhat’s New? Please send your professional and personalnews for C l a s s N o t e s to: <strong>Robert</strong>a Ribner, Editor, <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> Medicine, Coordinator, Alumni Affairs, UMDNJ-<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong><strong>Medical</strong> <strong>School</strong> Alumni Association • 335 George Street • Suite 230071N I N E T E E NS E V E N T Y - O N E75767970 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE’80’81New Brunswick, NJ 08903 • Phone: 732-235-6310 • Fax: 732-235-9570Email: ribnerrs@umdnj.edu • http://rwjms.umdnj.edu/alumniRichard Jackson co-edited anew book, Making Healthy Places:Designing and Building for Health,Well-being, and Sustainability (IslandPress, 2011). Dr. Jackson also hostsa new series on PBS titled DesigningHealthy Places, which looks at theimpact of our built environment onthe nation’s key health concerns.N I N E T E E NS E V E N T Y - F I V ESusan Rosenthal reports: “Iassumed the position as corporatedirector of medical education forMeridian in 2009. I am enjoying mynew position, especially teachingRWJMS students rotating at JerseyShore University <strong>Medical</strong> Center.”N I N E T E E NS E V E N T Y - S I XBrenda Shank writes: “I retiredas of December 30, 2010, as directorof the division of radiation oncologyat Doctors <strong>Medical</strong> Center in SanPablo, Calif.”N I N E T E E NS E V E N T Y - N I N EChristina Mora is a professor ofanesthesiology at StanfordUniversity <strong>School</strong> of Medicine.Alessio Salsano is the author of<strong>The</strong> High Calling: A ChristianPhysician’s Journey Through theCareer of Medicine.Winston Scott is a founding memberof the Caribbean <strong>Medical</strong> Mission, ahumanitarian group that providesmedical care to the needy in theCaribbean.N I N E T E E NE I G H T Y’82’84Diane Gabe writes: “Wonderfulcareer as pediatrician, but nowretired and loving it.”N I N E T E E NE I G H T Y - O N EFrank Briglia joined the Atlanti-Care Regional <strong>Medical</strong> Center asmedical director of the PediatricHospitalist Program for NemoursPediatric Partners.Linda Meloy writes: “I am now afull professor of pediatrics atVirginia Commonwealth University<strong>Medical</strong> Center.”N I N E T E E NE I G H T Y - T W OGrace Chang was appointed aprofessor of psychiatry at Harvard<strong>Medical</strong> <strong>School</strong>.Marilyn Heine received theCouncil Meritorious Service Awardfrom the American College ofEmergency Physicians.Deborah Young is a member ofthe medical staff at PottstownMemorial <strong>Medical</strong> Center,Department of Family Medicine.N I N E T E E NE I G H T Y - F O U RKathryn Holloway was selectedas one of the 2012 honorees to the<strong>Rutgers</strong> Hall of Distinguished Alumni.She is a professor at VirginiaCommonwealth University <strong>School</strong> ofMedicine and chief of neurosurgeryat the Hunter Holmes McGuire V.A.<strong>Medical</strong> Center in Richmond, Va.’85N I N E T E E NE I G H T Y - F I V EMartin Evers was recognized bythe Pennsylvania Chapter of theAmerican College of Physicians (ACP)for his exceptional dedication to andleadership of the Pennsylvania chapterof the ACP. He practices medicineat Bon Secours Community Hospitalin Port Jervis, N.Y.’92’86’93’94’88’89’95’90 ’96Raymond Sanders is an attendingneonatologist at Children’s Hospitalat St. Francis in Tulsa, Okla.N I N E T E E NE I G H T Y - S I XRichard Angelo is chief of theDepartment of Obstetrics andGynecology at Cape Cod Hospital inHyannis, Mass.Joseph Costabile reports: “I havereceived a two-year billet againwith the 4th <strong>Medical</strong> Battalion,United <strong>State</strong>s Marine Corps.”N I N E T E E NE I G H T Y - E I G H TConstantine Audeh joined BannerThunderbird <strong>Medical</strong> Center inGlendale, Ariz., as a hospitalist, inMay 2011.Steven Sheris is chief of cardiologyat the Gagnon CardiovascularInstitute at Overlook <strong>Medical</strong> Center,Atlantic Health System, in Summit.N I N E T E E NE I G H T Y - N I N EGastroenterologist RichardMailloux opened a new practice,Bellefonte Digestive Disease Center,in Bellefonte, Ky.N I N E T E E NN I N E T YPeter Sayre is an assistant clinicalprofessor of medicine at the Universityof California–San Francisco(UCSF), division of hematologyoncology.He is also executive directorof clinical trials at the UCSF<strong>School</strong> of Medicine Diabetes Center.Laura Sinai writes: “I am serving atwo-year term as chair of the NorthCarolina Breastfeeding Coalition.”N I N E T E E NN I N E T Y - T W OJohn Capo recently became a fullprofessor in the Department ofOrthopaedics at UMDNJ-New Jersey<strong>Medical</strong> <strong>School</strong>.Jonathan Fellus is the director ofrehabilitation at MeadowlandsHospital <strong>Medical</strong> Center, Secaucus.N I N E T E E NN I N E T Y - T H R E ERichard Mellon, an obstetrician/gynecologist, joined Pen BayWomen’s Health in Rockport, Maine.N I N E T E E NN I N E T Y - F O U RTamara LaCouture, assistantprofessor and vice chair, Departmentof Radiation Oncology, RWJMS, washonored at the Pink Roses TealMagnolias Brunch, sponsored by theCooper Cancer Institute, in October2011.Catherine Shanahan, who specializesin family medicine and weightloss, recently joined the Queen of theValley <strong>Medical</strong> Associates in Napa,Calif.N I N E T E E NN I N E T Y - F I V EHenry Kong and Jessica Treisman,MD, PhD, were married in September2011.James Metz is an assistant professorof radiation oncology and chiefof clinical operations at the Universityof Pennsylvania. He is alsoeditor-in-chief of OncoLink.N I N E T E E NN I N E T Y - S I XInternist Carole Lytle joined theSummit <strong>Medical</strong> Group.’’’’
97N I N E T E E NN I N E T Y - S E V E ND. <strong>Robert</strong> Jordan writes: “I recentlyjoined the practice of DePersia<strong>Medical</strong> Group in Swedesboro and<strong>Wood</strong>bury as an internal medicinephysician seeing primary carepatients.”98Jocelyn Mitchell-Williams wasappointed to the Board of Trustees ofFamily Service in Moorestown.N I N E T E E NN I N E T Y - E I G H TSteven Bromley is director of outpatientservices of neurology for theVirtua <strong>Medical</strong> Group throughoutSouth Jersey.Stella King is director of women’shealth services at Sheehan’s FamilyCare Clinic in Buffalo, N.Y.Marcus Magnet is chair of theDepartment of Family Medicine atUnderwood Memorial Hospital in<strong>Wood</strong>bury.99N I N E T E E NN I N E T Y - N I N E<strong>Robert</strong> Donatiello writes: “I amchair of the Department of Anesthesiologyfor John Muir <strong>Medical</strong> Centerin Concord, Calif. I am also the proudfather of two.”Samantha Leib writes: “I had ababy boy! Brady Michael was bornon June 23, 2011.”00Jongming Li joined the RegionalCancer Center in Erie, Pa., as a medicaloncologist and hematologist.T W O T H O U S A N DShaya Ansari writes: “I live andwork in Kansas City, Mo. I am a clinicalassistant professor of radiology anddirector of Body MRI at the Universityof Missouri in Kansas City. I have beenhere for four years and love the Midwest.Best-kept secret: great appreciativepatients and great lifestyle, farsuperior than the Northeast. I missNew Jersey, though —great pizza!”’01’02David Otterburn is an assistantprofessor of surgery in the Departmentof Surgery, division of plastic and reconstructivesurgery, at Weill Cornell<strong>Medical</strong> College.Orthopaedist Fotios Tjoumakarisjoined the Rothman Institute in EggHarbor Township.T W O T H O U S A N DO N ECarrie Burns writes: “Myhusband, Gregg Gagliardi ’01,and I are thrilled to announce thebirth of our son, Christian MichaelGagliardi, born on May 4, 2011.He was delivered at the University ofPennsylvania by Irina Burd ’03,who is a friend and was one of myanatomy lab partners!”Kathleen Greaney writes:“My husband, Michael Schmidt,and I welcomed our first child,Lauren Elizabeth Schmidt, onDecember 22, 2011. I am a boardcertifiedpediatrician and partner atMaple Avenue Pediatrics in FairLawn.”Felix Olobatuyi was appointedan assistant professor at Texas A&MUniversity <strong>School</strong> of Health Sciencesin Temple, Texas.T W O T H O U S A N DT W ODanielle Ludwin is an assistantprofessor of anesthesiology atColumbia University <strong>Medical</strong> Centerand the associate director of theregional anesthesia fellowship.Biren Saraiya was namedmedical director of <strong>The</strong> CancerInstitute of New Jersey–Hamilton.Sathya Sembugamoorthy-Bhandari reports: “We are back inthe U.S. We moved to Lansing,Michigan, for my interventional andpain and EMG fellowship atMichigan <strong>State</strong> University.”’03’04’05’06T W O T H O U S A N DT H R E EGrant Cooper and his wife, AnaBracilovic ’04, opened thePrinceton Spine and Joint Center in2008.Dianna Deignan, a primary casephysician with Harbor Family Practicein Stone Harbor, has been appointedchief medical information officer atCape Regional <strong>Medical</strong> Center.T W O T H O U S A N DF O U RLasanta Horana writes: “I wasawarded the honorary status of fellowin the American College of EmergencyPhysicians in October 2011.”T W O T H O U S A N DF I V EChristopher Gentle writes: “Mywife and I had our first child, AliciaDoligosa Gentle, born on March 1,2011. I was inducted as a fellow inthe American College of EmergencyPhysicians in October.”Nicole Eftychiou Post writes:My husband, <strong>Robert</strong> Post II ’05,and I are happy to announce thebirth of our daughter, Olivia Nicole,on June 7. Our son, Bobby (3), is sohappy to be a big brother! We arehappy to be living in the Northeastagain. Rob is the research directorfor the Virtua Family MedicineResidency in Voorhees. I am workingas a geriatric psychiatrist inPhiladelphia.”T W O T H O U S A N DS I XKalpana Narayan and GaneshShankar, MD, PhD, were married inMay 2011. Dr. Narayan is an emergencyroom physician at the Hospitalof the University of Pennsylvania,where she is also a <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> clinical scholar, focusing onresearch on the elderly and longtermcare.’08Michael Zozzaro joined <strong>The</strong>Family Center for Otolaryngology inRutherford, affiliated with HackensackUniversity <strong>Medical</strong> Center.T W O T H O U S A N DE I G H TAdrienne Collier writes: “Uponcompletion of my pediatrics residencyat RWMS at Bristol-Myers SquibbChildren’s Hospital, I will be relocatingmy family to Maryland to work as apediatrician at the People’s CommunityHealth Center in Baltimore.”Kelli Davis completed a residencyin internal medicine at Emory University.She is working as a hospitalistfor <strong>The</strong> Southeast Permanente<strong>Medical</strong> Group in Atlanta.Andrew Demidowich completedhis internal medicine residency atMount Sinai <strong>Medical</strong> Center. He isworking as a hospitalist in Denver,and will start a fellowship inendocrinology in September 2012 atthe National Institutes of Health.F O R M E RR E S I D E N T SVeronica Anderson is the founderand host of a web radio talkshow, Wellness for the Real World.Tyrone Krause is a cardio-thoracicsurgeon at Jersey City <strong>Medical</strong> Center.Sanjay Kumar specializes in vascularsurgery and treatment at Physiciansof Southern New Jersey in Vineland.I n M e m o r i a mSurekha Dwivedi, MD ’94,passed away on August 27, 2011.She was a family physician andpracticed in the Meridian system inNew Jersey. She is survived by herhusband, Jonathan Briggs, MD, andher two sons.Nancy Mao Gevirtz, MD ’86,passed away on August 25, 2011.Janet Hamilton, MD ’83,passed away on May 12, 2011.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE 71
LASTP A G EIn Memoriam:Stephen F. Lowry, MDWith great sadness, the RWJMS communitylearned of the death, in June 2011, of Stephen F.Lowry, MD, professor and chair, Department of Surgery,and senior associate dean for education.An eminent physician scientist, Dr. Lowry led internationallyrecognized research and clinical trials. He definedthe central role of cell-derived mediators as a mechanism forsystemic inflammation, septic shock, and organ dysfunctionin critically ill patients. In addition, he developed novelimmunotherapeutic approaches for the management ofthese life-threatening conditions. He recently integrated invivo and computational systems approaches to the study ofsystemic inflammation and sepsis and was developing noveltechnologies for the assessment of patient risk and responsesto therapy. He was instrumental in creating the divisionof surgical sciences, which focuses on core researchissues of inflammation, developmental biology, and healing.A superb mentor, he was the first faculty member namedto the Harvey Professorship in Innovative Teaching. He wasamong the first surgeons to earn the National Institutes ofHealth’s prestigious Research Career Development Award.In 1997, his research grant earned MERIT Award statusfrom the National Institute of General <strong>Medical</strong> Sciences. Helater received the Flance-Karl Award from the AmericanSurgical Association as well as the Philadelphia Academy ofSurgery’s prestigious Samuel D. Gross Prize in SurgicalResearch. He was made an Honorary Fellow of the RoyalCollege of Surgeons of Edinburgh and received theB Y K A T E O ’ N E I L LOutstanding <strong>Medical</strong> Research Scientist Award for ClinicalResearch from the Edward J. Ill Excellence in MedicineFoundation. He is listed as a highly cited author by theInstitute for Science Information in the field of immunology.“As remarkable as these accomplishments are, they don’tdefine Steve adequately,” says Peter S. Amenta, MD, PhD,dean. “Steve was a genuine and caring person, who showedrespect and consideration to everyone. He loved his family,and his extended family in the Department of Surgery andthe Office of Education as well as the entire <strong>Robert</strong> <strong>Wood</strong><strong>Johnson</strong> family. His warmth and sense of humor are deeplymissed.”In addition, the Honorary Alumni Award will be awardedposthumously to Dr. Lowry at the Scholarship Gala to Celebratewith Alumni and Friends on April 21, 2012. Please joinus at the Gala to celebrate Dr. Lowry’s life and career. MDr. Lowry’s family has established <strong>The</strong> Stephen F. Lowry, MD,Memorial Fund to support medical research and academiceducation. Checks may be made payable to the New JerseyHealth Foundation (NJHF)–Dr. Lowry and mailed to 120Albany Street, Tower II, Suite 850, New Brunswick, NJ 08901.Donations may also be made at www.njhealthfoundation.org.Please click on “Make a Gift”; in the first gift designationbox, write “Dr. Lowry Memorial Fund.”J O H N E M E R S O N72 <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> ■ MEDICINE
New location inPrinceton!800 Bunn DriveCall today at609-688-6859Specialties include:Cardiac SurgeryUrologyPediatric SurgeryPlastic SurgeryPulmonary DiseaseInfectious DiseaseVascular SurgeryInternationalTravel Medicine andImmunizationMain Campus:New BrunswickSatellite PracticeLocations:Hamilton ■ MontclairMonroe ■ PiscatawayPrinceton ■ Somerset<strong>The</strong> <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong><strong>Medical</strong> Group isNow in Princeton andfocused on:You.<strong>The</strong> <strong>Robert</strong><strong>Wood</strong> <strong>Johnson</strong><strong>Medical</strong> Group now has an office in Princeton.<strong>The</strong> RWJMG in Princeton is comprised ofRWJ <strong>Medical</strong> <strong>School</strong> faculty who are expertsin specialty and subspecialty care. Specialtiesoffered in this location include Urology,Pulmonary, Plastic Surgery, Cardiac Surgery,Infectious Disease, Vascular Surgery, TravelMedicine and Immunization. <strong>The</strong> RWJMGphysicians can provide you with the specialtycare found only at top academic health centers.Brilliant minds. Better medicine. All for you.Where Great Medicineis AcademicAcademic HealthCenter Partner is<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong>University Hospital1-877-4RWJDOCwww.rwjmedicalgroup.org
125 Paterson Street • Suite 1400New Brunswick, New Jersey 08903-0019Non-Profit Org.U.S. PostageP A I DPiscataway, NJPermit No. 44Susanna na thought ht her life was over.In three minutes, RWJ gave it back.LanguagegArts teacher, Susanna DeNude has a lot to say about brain cancer.For seven years,she lived with it every ery day, often wondering whether shewould ever see the last ofit. Her two previous open craniotomies, plus radiation,did not slow the growth ofa tumor in her brain. Believing she had runout ofoptions,the Riverdale resident was fortunate to getanother chance.<strong>The</strong> neurosurgical team, under the guidance ofDr.Shabbar F.Danish, director ofstereotactic and functional neurosurgery at <strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong>University Hospital and assistant professor ofsurgery at UMDNJ-<strong>Robert</strong><strong>Wood</strong> <strong>Johnson</strong> <strong>Medical</strong> <strong>School</strong>, felt that Susanna was a candidate date to undergothe nation’s first laser ablation surgery for an intracranial ependymoma, a tumor that grows fromthe cells lining the ventricles ofthe brain.<strong>The</strong> surgery has proven to be effective ective in both adult and pediatric brain tumors,and can reduce a patient’s hospital stay from a week ek to a day, withfewer side effects ects from surgery and anesthesia since the procedure is performed using only local anesthetic.And,unlike other surgeries, ifthe tumorreturns, laser ablation can be safely performed again, sparing the patient the need for more invasive treatment.<strong>Robert</strong><strong>Wood</strong> <strong>Johnson</strong> has successfullyperformed more ofthese cutting-edge surgeries than any hospital in the country.Now that Susanna is backin her classroom teaching, a lot can be learned from her experience.<strong>Robert</strong> <strong>Wood</strong> <strong>Johnson</strong> University Hospital is one of America’s best hospitals,where,what others call miracles,we simply call great medicine.<strong>The</strong> Heart of Academic MedicineeRWJUH.edu/laser1-888-MD-RWJUH