Neurovascular Assessments/Checks - Department of Nursing ...
Neurovascular Assessments/Checks - Department of Nursing ...
Neurovascular Assessments/Checks - Department of Nursing ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
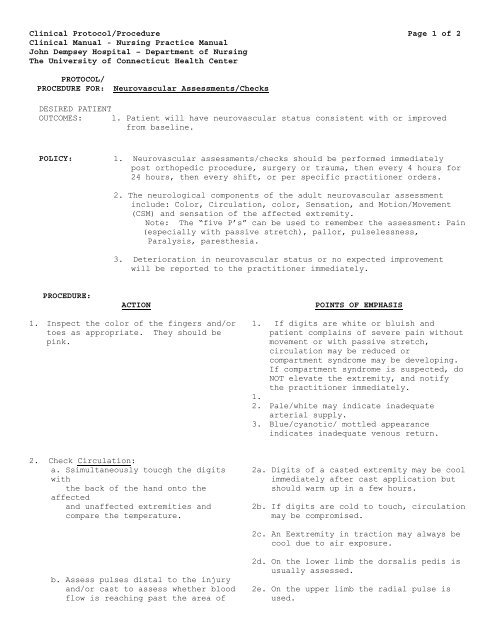
Clinical Protocol/Procedure Page 1 <strong>of</strong> 2Clinical Manual - <strong>Nursing</strong> Practice ManualJohn Dempsey Hospital – <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterPROTOCOL/PROCEDURE FOR: <strong>Neurovascular</strong> <strong>Assessments</strong>/<strong>Checks</strong>DESIRED PATIENTOUTCOMES: 1. Patient will have neurovascular status consistent with or improvedfrom baseline.POLICY:1. <strong>Neurovascular</strong> assessments/checks should be performed immediatelypost orthopedic procedure, surgery or trauma, then every 4 hours for24 hours, then every shift, or per specific practitioner orders.2. The neurological components <strong>of</strong> the adult neurovascular assessmentinclude: Color, Circulation, color, Sensation, and Motion/Movement(CSM) and sensation <strong>of</strong> the affected extremity.Note: The “five P’s” can be used to remember the assessment: Pain(especially with passive stretch), pallor, pulselessness,Paralysis, paresthesia.3. Deterioration in neurovascular status or no expected improvementwill be reported to the practitioner immediately.PROCEDURE:ACTIONPOINTS OF EMPHASIS1. Inspect the color <strong>of</strong> the fingers and/ortoes as appropriate. They should bepink.1. If digits are white or bluish andpatient complains <strong>of</strong> severe pain withoutmovement or with passive stretch,circulation may be reduced orcompartment syndrome may be developing.If compartment syndrome is suspected, doNOT elevate the extremity, and notifythe practitioner immediately.1.2. Pale/white may indicate inadequatearterial supply.3. Blue/cyanotic/ mottled appearanceindicates inadequate venous return.2. Check Circulation:a. Ssimultaneously toucgh the digitswiththe back <strong>of</strong> the hand onto theaffectedand unaffected extremities andcompare the temperature.2a. Digits <strong>of</strong> a casted extremity may be coolimmediately after cast application butshould warm up in a few hours.2b. If digits are cold to touch, circulationmay be compromised.2c. An Eextremity in traction may always becool due to air exposure.b. Assess pulses distal to the injuryand/or cast to assess whether bloodflow is reaching past the area <strong>of</strong>2d. On the lower limb the dorsalis pedis isusually assessed.2e. On the upper limb the radial pulse isused.
Clinical Protocol/Procedure Page 2 <strong>of</strong> 2Clinical Manual - <strong>Nursing</strong> Practice ManualJohn Dempsey Hospital – <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterPROTOCOL/PROCEDURE FOR: <strong>Neurovascular</strong> <strong>Assessments</strong>/<strong>Checks</strong>injury/surgery and perfusing theremaining limb effectively. Ifunable to palpate a pulse, use aDoppler (and document the use <strong>of</strong> aDoppler).c. Check capillary refill by pressingon the tips <strong>of</strong> the toe nails orfinger nails until they blanch, thenrelease pressure and note how soonnormal color returns.3. Check Sensation: Lightly touch the skinboth proximally and distally to theaffected site. Ask the patient to reportany changes in sensation to the affectedlimb. my touching the fingers and/ortoes and asking the patient how theyfeel. Note any numbness or tingling2f. An absence <strong>of</strong> pulse may indicate a lack<strong>of</strong> arterial flow.2g. Normal capillary refill is ≤3 seconds.2h. If circulation is decreased, capillaryreturn may be very sluggish.,2. Changes in sensation may result frompressure on the relevant nerve(s) and mayinclude decreased sensation,hypersensation, tingling, ‘pins andneedles’, numbness or loss <strong>of</strong> sensation.4. Check Motion/Movement: 5. To testmovement <strong>of</strong> the digits, asktell patientto fully plantar and dorsi flex andextend the toes <strong>of</strong> both limbs or volar(palm) and dorsi flex and extend thefingers <strong>of</strong> both limbs, first theunaffected and then the affected side,noting any reduced range <strong>of</strong> movement.5. Check Edema: Inspect the limb forswelling and compare with the unaffectedside.5. Although edema is not necessarilycharacteristic <strong>of</strong> neurovascular deficit,any notable increase should still bedocumented and reported.PATIENT ANDFAMILYTEACHING:Explain all procedures to patient and family and keep patient/familyinformed <strong>of</strong> plan <strong>of</strong> care.DOCUMENTATION: Documentation <strong>of</strong> color, circulation, sensation, motion/movement and use<strong>of</strong> Doppler and findings (as appropriate) should be in the nursingassessment documentation or progress note. Any other abnormal findingsmust be documented in the nursing note. Notification <strong>of</strong> the LIP for anyabnormal findings must be included in the nursing progress note.APPROVAL: <strong>Nursing</strong> Standards CommitteeEFFECTIVEDATE: 1/12