Improving JMO clinical handover at all shift changes - ARCHI
Improving JMO clinical handover at all shift changes - ARCHI
Improving JMO clinical handover at all shift changes - ARCHI
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
NSW DEPARTMENT OF HEALTH73 Miller StreetNORTH SYDNEY NSW 2060Tel. (02) 9391 9000Fax. (02) 9391 9101TTY. (02) 9391 9900www.health.nsw.gov.auProduced by:Workforce Development and Innov<strong>at</strong>ionNSW Department of HealthTel. (02) 9391 9776Fax. (02) 9391 9019Email. limbe@doh.health.nsw.gov.auThis work is copyright. It may be reproduced in whole or in part for studytraining purposes subject to the inclusion of an acknowledgement of thesource. It may not be reproduced for commercial usage or sale. Reproductionfor purposes other than those indic<strong>at</strong>ed above requires written permissionfrom the NSW Department of Health.© NSW Department of Health 2010SHPN (HSPI) 100536Further copies of this document can be downloadedfrom http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>December 2010
ForewordThe Acute Care Taskforce is working to promote safe <strong>clinical</strong><strong>handover</strong> in the NSW health system, with a special focus on<strong>clinical</strong> <strong>handover</strong> <strong>at</strong> <strong>all</strong> <strong>shift</strong> <strong>changes</strong> (weekdays and weekends)for Junior Medical Officers (<strong>JMO</strong>).Changing medical work hours has benefited the work–lifebalance of medical officers, but leads to increased transfersof p<strong>at</strong>ient care between clinicians.Dr Tim SmythDeputy Director-General, Health System Quality,Performance and Innov<strong>at</strong>ion<strong>JMO</strong>s are the least experienced members of the medicalworkforce, and frequently move between wards, facilitiesand Health Services. Inexperience and variable or absentprocesses rel<strong>at</strong>ing to <strong>clinical</strong> <strong>handover</strong> have been shownto present significant risks for p<strong>at</strong>ient care.Ensuring th<strong>at</strong> <strong>handover</strong> happens with consistency and quality,<strong>at</strong> <strong>all</strong> <strong>shift</strong> <strong>changes</strong>, will provide clarity of responsibility andaccountability for <strong>all</strong> clinicians. <strong>Improving</strong> <strong>clinical</strong> <strong>handover</strong> byproviding strong senior leadership and supervision of <strong>handover</strong>will enhance p<strong>at</strong>ient care, <strong>JMO</strong> learning, staff communic<strong>at</strong>ionand confidence.Ms Vicki ManningAcute Care TaskforceCo-ChairSafe <strong>clinical</strong> <strong>handover</strong> is essential to p<strong>at</strong>ient care.Professor Jeremy WilsonAcute Care TaskforceCo-ChairProfessor Steven BoyagesChief Executive, Clinical Educ<strong>at</strong>ion and Training InstituteDr Hamish DunnChair, Junior Medical Officer Forum (CETI)NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 1
ContentsAt a glance...........................................................................................................................................................................3Why we must change.........................................................................................................................................................5Key elements for implement<strong>at</strong>ion.....................................................................................................................................61. A communic<strong>at</strong>ion framework to facilit<strong>at</strong>e <strong>clinical</strong> <strong>handover</strong> <strong>at</strong> <strong>JMO</strong> <strong>shift</strong> change (ISBAR) .............................................62. Senior leadership: deciding who and wh<strong>at</strong> to hand over <strong>at</strong> <strong>shift</strong> change.......................................................................73. Shift to Shift <strong>handover</strong>: key principles for loc<strong>all</strong>y appropri<strong>at</strong>e implement<strong>at</strong>ion...............................................................93.1 Handover Happens...............................................................................................................................................103.2 Handover Leadership............................................................................................................................................103.3 Handover Set-up..................................................................................................................................................113.4 Handover Process.................................................................................................................................................12Appendices........................................................................................................................................................................ 13A. A clear case for change (QSA d<strong>at</strong>a, liter<strong>at</strong>ure, <strong>JMO</strong> perspectives)................................................................................13B. Wider issues th<strong>at</strong> require consider<strong>at</strong>ion (wider implement<strong>at</strong>ion for other junior doctors, rostering).............................14C. Points to consider for implement<strong>at</strong>ion across 24 hours...............................................................................................16D. Clinical inform<strong>at</strong>ion to consider when handing over a p<strong>at</strong>ient....................................................................................17E. Implement<strong>at</strong>ion framework to assist facilities with <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>...................................................................20F. Implement<strong>at</strong>ion support (templ<strong>at</strong>es, tools and links to guide implement<strong>at</strong>ion of <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> <strong>at</strong> facilities)........22G. Prevoc<strong>at</strong>ional training networks in NSW.....................................................................................................................26Useful references.............................................................................................................................................................. 27Acknowledgements..........................................................................................................................................................282 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
At a glanceBetween the Flags (PD2010_026) and Safe Clinical Handover (PD2009_060) are two important mand<strong>at</strong>es inthe NSW health system th<strong>at</strong> place a strong focus on effective and early <strong>clinical</strong> communic<strong>at</strong>ion of <strong>changes</strong> top<strong>at</strong>ient condition.This document aims to assist facilities to implement loc<strong>all</strong>y appropri<strong>at</strong>e <strong>clinical</strong> <strong>handover</strong> processes <strong>at</strong> <strong>all</strong> Junior MedicalOfficer (<strong>JMO</strong>) <strong>shift</strong> <strong>changes</strong>, improving the consistency and quality of <strong>clinical</strong> communic<strong>at</strong>ion for better p<strong>at</strong>ient outcomes.Both junior and senior medical officers, with metropolitan and rural represent<strong>at</strong>ion, have collabor<strong>at</strong>ed in the writing of thisdocument to ensure th<strong>at</strong> it meets their needs.Clinical <strong>handover</strong> definitionClinical <strong>handover</strong> has a n<strong>at</strong>ion<strong>all</strong>y and intern<strong>at</strong>ion<strong>all</strong>yrecognised definition.‘…transfer of professional responsibility andaccountability for some or <strong>all</strong> aspects of carefor a p<strong>at</strong>ient, or group of p<strong>at</strong>ients, to anotherperson or professional group on a temporaryor permanent basis.’ 1,3,10.In your facility, does <strong>JMO</strong> <strong>clinical</strong><strong>handover</strong>:• happen <strong>at</strong> <strong>all</strong> <strong>shift</strong> <strong>changes</strong>?• have a consistent process?• promote quality <strong>clinical</strong> communic<strong>at</strong>ion?• improve p<strong>at</strong>ient care outcomes?Three key elements have been definedto help improve <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>1 A communic<strong>at</strong>ion framework for <strong>JMO</strong>s (ISBAR).A communic<strong>at</strong>ion framework using a minimum d<strong>at</strong>aset to guide <strong>clinical</strong> <strong>handover</strong> can ensure consistentand complete, yet concise, <strong>handover</strong> interactions.– Detail on the ISBAR communic<strong>at</strong>ion frameworkcommences page 6.2 Senior leadership: who and wh<strong>at</strong> should behanded over?All <strong>JMO</strong>s require leadership and supervision frommore senior clinicians (eg Registrars, Consultants) todetermine which p<strong>at</strong>ients and wh<strong>at</strong> inform<strong>at</strong>ion havethe gre<strong>at</strong>est priority for <strong>handover</strong>.– Detail on senior leadership <strong>at</strong> <strong>handover</strong> commencespage 7.3 Shift to <strong>shift</strong> <strong>handover</strong>: key principles for loc<strong>all</strong>yappropri<strong>at</strong>e implement<strong>at</strong>ion.<strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> processes must be appropri<strong>at</strong>eto local needs and appropri<strong>at</strong>e to the specific <strong>shift</strong>change (day, evening or night and on weekends).All facilities have the flexibility to determine loc<strong>all</strong>yappropri<strong>at</strong>e processes, but need to ensure th<strong>at</strong> thoseprocesses (day, evening and night) meet a set of keyprinciples.– Detail on the key principles commences page 9.But wait… who is a <strong>JMO</strong>?For the purpose of this document, a <strong>JMO</strong> is defined as amedical officer who is a part of the prevoc<strong>at</strong>ional trainingprogram of the NSW Clinical Educ<strong>at</strong>ion and TrainingInstitute (CETI, formerly IMET):• Australian medical school postgradu<strong>at</strong>es,Year 1 and Year 2 and• Australian Medical Council gradu<strong>at</strong>es,Year 1 and Year 2.There is a broader intention tothe program.All facilities are encouraged to consider how the keyelements of the <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong> project can betransferred or tailored to other ‘junior’ doctors and otherscenarios of <strong>handover</strong> (eg <strong>handover</strong> between medicalteams or transfer between facilities or the community).NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 3
Key elements for implement<strong>at</strong>ion1. A communic<strong>at</strong>ion frameworkto facilit<strong>at</strong>e <strong>clinical</strong> <strong>handover</strong><strong>at</strong> <strong>JMO</strong> <strong>shift</strong> change (ISBAR)The ISBAR framework represents a standardised approachto communic<strong>at</strong>ion which can be used in any situ<strong>at</strong>ion.ISBAR is based on ‘SBAR’ a system which was developedby the US Navy for use in nuclear submarines.ISBAR stands for Introduction, Situ<strong>at</strong>ion, Background,Assessment and Recommend<strong>at</strong>ion. 7A communic<strong>at</strong>ion framework increases the consistencyin the delivery of inform<strong>at</strong>ion. As yet, there is no evidenceproving th<strong>at</strong> one mnemonic is the gold standard. ISBAR isrecommended because:Wh<strong>at</strong>, and how much, <strong>clinical</strong>inform<strong>at</strong>ion should I hand over?Appendix D has a summary to provide guidance on the<strong>clinical</strong> inform<strong>at</strong>ion th<strong>at</strong> should be considered whenhanding over specific p<strong>at</strong>ient types:• Medical• Surgical• Paedi<strong>at</strong>ric• Psychi<strong>at</strong>ry• Obstetrics and Gynaecology• Emergency Department.Sufficient <strong>clinical</strong> inform<strong>at</strong>ion must be handed over toensure transfer of responsibility and accountability forp<strong>at</strong>ient care.• It is well recognised in the current Safe ClinicalHandover implement<strong>at</strong>ion plans of a number ofHealth Services• It aligns with Between the Flags and DETECT training• It is portable, memorable and easy to use• It helps you to organise wh<strong>at</strong> you’re going to say• It is a generic communic<strong>at</strong>ion framework th<strong>at</strong> isapplicable to both <strong>clinical</strong> and non-<strong>clinical</strong> settings• Consistency of practice will benefit Junior MedicalOfficers who often move between facilities andHealth Services.P<strong>at</strong>ients who are less stable or have changingmanagement plans may require a detailed <strong>handover</strong>,while others who are rel<strong>at</strong>ively stable and with feweroutstanding tests or actions can be summarisedmore quickly.Senior clinician supervision <strong>at</strong> <strong>clinical</strong> <strong>handover</strong> isimportant to help <strong>JMO</strong>s decide which p<strong>at</strong>ients, how muchand which <strong>clinical</strong> inform<strong>at</strong>ion needs to be handed over.(See page 11 for further assistance.)See Appendix D for more detail on the <strong>clinical</strong> inform<strong>at</strong>ionyou should be considering <strong>at</strong> <strong>handover</strong>.ISBAR templ<strong>at</strong>es are available to download:http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>6 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
Hand over relevant <strong>clinical</strong> inform<strong>at</strong>ionin the ISBAR framework…IIdentific<strong>at</strong>ionIdentify yourself, the p<strong>at</strong>ient and who youare talking to.“I am (name and role), from (ward/facility) andI’m c<strong>all</strong>ing regarding (multiple p<strong>at</strong>ient identifiers,such as; name, age, gender, Ward/bed, MedicalRecord Number)”S Situ<strong>at</strong>ionSt<strong>at</strong>e the p<strong>at</strong>ient’s diagnosis/reason foradmission and the current problem.“The situ<strong>at</strong>ion is th<strong>at</strong> I have a p<strong>at</strong>ient (age/gender), who is (diagnosis/deterior<strong>at</strong>ing/stable).My concerns are (clear and succinct concerns). Thecurrent presenting symptoms are (clear, currentand relevant symptoms and observ<strong>at</strong>ions).”B BackgroundWh<strong>at</strong> is the <strong>clinical</strong> background or context?By way of background (Give pertinent inform<strong>at</strong>ionwhich may include: D<strong>at</strong>e of admission / presentingsymptoms / medic<strong>at</strong>ion / previous recent vital signs/ test results / st<strong>at</strong>us <strong>changes</strong>)A AssessmentWh<strong>at</strong> do you think the problem(s) is?(Don’t forget to have the current vital signsand a key problem list ready!)“My assessment on the basis of the above is th<strong>at</strong>the p<strong>at</strong>ient is….. they are <strong>at</strong> risk of….. andin need of….”R recommend<strong>at</strong>ionWh<strong>at</strong> are you asking the person to do?“My recommend<strong>at</strong>ion is th<strong>at</strong> this p<strong>at</strong>ient needs(wh<strong>at</strong> test/action) by (who) within (timeframe)”Repe<strong>at</strong> to confirm wh<strong>at</strong> you have heard.Eg “I understand th<strong>at</strong> I am to…. and you will…”2. Senior leadership:deciding who and wh<strong>at</strong> tohand over <strong>at</strong> <strong>shift</strong> changeAt the end of <strong>handover</strong>, the <strong>JMO</strong> receiving <strong>handover</strong>should have a clear understanding of:• sick, deterior<strong>at</strong>ing and unstable p<strong>at</strong>ients• outstanding actions, procedures, tests or resultsto be reviewed• other important factors th<strong>at</strong> will impact work onthe following <strong>shift</strong>.<strong>JMO</strong>s are <strong>at</strong> the beginning of their careers and aredeveloping their <strong>clinical</strong> experience and knowledge base.The leadership and supervision by senior clinicians isessential to help <strong>JMO</strong>s provide effective <strong>clinical</strong> <strong>handover</strong>.Senior clinicians are defined as:• Registrars• Career Medical Officers• Consultants• Staff Specialists• Visiting Medical Officers• Senior Nurses.Senior clinicians have experience th<strong>at</strong> can help <strong>JMO</strong>sdeliver the most important key messages for effectivetransfer of p<strong>at</strong>ient care in a complete yet concise manner.The leadership roles required from senior clinicians include:• oversee and implement <strong>handover</strong> processes• <strong>at</strong>tend and lead <strong>handover</strong> <strong>at</strong> <strong>JMO</strong> <strong>shift</strong> <strong>changes</strong>• understand the signs and symptoms of deterior<strong>at</strong>ion• recognise <strong>clinical</strong> risks and convey these conceptsto <strong>JMO</strong>s• prioritise which p<strong>at</strong>ients and wh<strong>at</strong> inform<strong>at</strong>ion ishanded over• Involve <strong>JMO</strong>s in clear prioritis<strong>at</strong>ion of p<strong>at</strong>ients and<strong>all</strong>oc<strong>at</strong>ion of tasks.Some examples of how senior leadership for <strong>JMO</strong><strong>handover</strong> can be demonstr<strong>at</strong>ed include:NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 7
• Senior Medical Officers involving and guiding <strong>JMO</strong>sin <strong>clinical</strong> decision-making before and during <strong>clinical</strong><strong>handover</strong>• Senior Medical Officers <strong>at</strong>tending and leading<strong>handover</strong> to manage <strong>clinical</strong> issues early and reducec<strong>all</strong> outs• Using <strong>handover</strong> as a teaching opportunity• Senior nurses facilit<strong>at</strong>ing the process of <strong>handover</strong>.It is recognised th<strong>at</strong> not <strong>all</strong> facilities haveregistrars rostered on <strong>all</strong> <strong>shift</strong>s with <strong>JMO</strong>s.In such facilities the role of the Registrar in<strong>handover</strong> could be filled by:• Career Medical Officers• Consultants• Staff Specialists• Visiting Medical Officers• Senior Nurses (for facilit<strong>at</strong>ion of the <strong>handover</strong>process, r<strong>at</strong>her than <strong>clinical</strong> supervision).It is feasible th<strong>at</strong> there may be occasions when seniorclinicians are unable to <strong>at</strong>tend and lead <strong>clinical</strong> <strong>handover</strong>.In such instances, <strong>JMO</strong>s should have access to seniorleadership in preparing their p<strong>at</strong>ient lists for <strong>shift</strong> <strong>handover</strong>.Prior to <strong>handover</strong>, senior clinician leadership can include:• <strong>JMO</strong>s consulting with senior medical staff, includingConsultants, Staff Specialists and Visiting Medical Officers• Registrars and <strong>JMO</strong>s should discuss which p<strong>at</strong>ients andwh<strong>at</strong> inform<strong>at</strong>ion to <strong>handover</strong> <strong>at</strong> <strong>shift</strong> change• <strong>JMO</strong>s undertaking a face to face or telephone paperround with registrars prior to <strong>handover</strong>.Which p<strong>at</strong>ients should be handed over?• Sick or deterior<strong>at</strong>ing p<strong>at</strong>ients (eg, PACE/MET c<strong>all</strong>s orp<strong>at</strong>ients with unstable or deterior<strong>at</strong>ing observ<strong>at</strong>ions)• P<strong>at</strong>ients with significant <strong>changes</strong> in condition ormanagement plan during the previous <strong>shift</strong>• Important outstanding actions, including:– tests or procedures th<strong>at</strong> need to be done– test results th<strong>at</strong> need review– transfer of care planning (this includes inter-wardor inter-hospital care and also discharge to GP care)• New p<strong>at</strong>ients• Any p<strong>at</strong>ients you are worried about –do not discount your <strong>clinical</strong> acumen.Do not discount your <strong>clinical</strong> acumen:Deciding who should be handed over cannot be limitedto a strict c<strong>at</strong>egoris<strong>at</strong>ion.If for any reason you are concerned by any part of ap<strong>at</strong>ient’s <strong>clinical</strong> situ<strong>at</strong>ion or their management plan, thisconcern should be handed over to the oncoming <strong>shift</strong>.Senior leadership <strong>at</strong> <strong>handover</strong> is an important part ofclarifying and managing p<strong>at</strong>ient care concerns.Do not wait for <strong>shift</strong> <strong>handover</strong>:Escal<strong>at</strong>ion of concerns for any part of a p<strong>at</strong>ient’s <strong>clinical</strong>situ<strong>at</strong>ion or management plan must not be held back until<strong>shift</strong> <strong>handover</strong> (See PD2010_026).According to the escal<strong>at</strong>ion protocols of DETECT andBetween the Flags, 6 <strong>JMO</strong>s should escal<strong>at</strong>e concerns aboutp<strong>at</strong>ients to senior clinicians immedi<strong>at</strong>ely, r<strong>at</strong>her thanwaiting for <strong>shift</strong> <strong>handover</strong>.Wh<strong>at</strong> else is important to hand over?Handover of other inform<strong>at</strong>ion about environmentalfe<strong>at</strong>ures may benefit the oncoming <strong>shift</strong> and should beled by registrars, including:• critical care bed availability• ward p<strong>at</strong>ient flow or bed pressure points• staff levels or availability• relevant contact persons if required• any specific p<strong>at</strong>ient or equipment risks th<strong>at</strong> are likelyto affect <strong>JMO</strong> or staff safety.NOTE: The ‘Concept Testing’ final report for the <strong>JMO</strong><strong>clinical</strong> <strong>handover</strong> project contains clear key messages fromboth junior and senior clinicians about the importance ofsenior leadership in <strong>clinical</strong> <strong>handover</strong> for junior clinicians.The report is available for download: http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>8 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
3. Shift to <strong>shift</strong> <strong>handover</strong>: key principles for loc<strong>all</strong>y appropri<strong>at</strong>eimplement<strong>at</strong>ion<strong>Improving</strong> the structure and senior supervision of <strong>handover</strong> (24/7) is aimed <strong>at</strong> enhancing p<strong>at</strong>ient care, <strong>JMO</strong> learning,staff communic<strong>at</strong>ion and confidence.Safe <strong>clinical</strong> <strong>handover</strong> is essential to p<strong>at</strong>ient care.Local <strong>clinical</strong> situ<strong>at</strong>ions vary depending on the facility, hour of day and day of week. For example:HandoverHandoverWeekday: day timeWeekday: evening Weekday: nightWeekend: day time Weekend: evening and nightTeam ATeam BTeam CSafety and quality of care dict<strong>at</strong>es th<strong>at</strong> the fundamentalsof <strong>handover</strong> are constant, regardless of the time, or day.However, facilities should consider variables th<strong>at</strong> impact<strong>shift</strong>s across 24 hours of the day and 7 days per week,when determining loc<strong>all</strong>y appropri<strong>at</strong>e <strong>clinical</strong> <strong>handover</strong>solutions.See Appendix C for more inform<strong>at</strong>ion on“Points to consider for implement<strong>at</strong>ion across 24 hours”OR download the ‘Concept Testing’ final report:http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>Principlec<strong>at</strong>egoryHandoverhappensHandoverleadershipHandoverset-upKey PrinciplesClinical <strong>handover</strong> occurs <strong>at</strong> <strong>all</strong> <strong>JMO</strong><strong>shift</strong> <strong>changes</strong>Senior medical leadership in <strong>JMO</strong><strong>shift</strong> <strong>handover</strong>Valuing <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong>Prepare for <strong>handover</strong> by prioritisingp<strong>at</strong>ient listsKey participant <strong>at</strong>tendance <strong>at</strong> <strong>JMO</strong><strong>shift</strong> <strong>handover</strong>Time <strong>all</strong>oc<strong>at</strong>ion for <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong>A design<strong>at</strong>ed <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong> placeKey principles to guide theimplement<strong>at</strong>ion <strong>at</strong> <strong>all</strong> <strong>JMO</strong><strong>shift</strong> <strong>changes</strong>The high-level principles th<strong>at</strong> have been developed tosupport <strong>handover</strong> <strong>at</strong> <strong>JMO</strong> <strong>shift</strong> change are mappeddirectly from the ‘Safe Clinical Handover’ – standard keyprinciples for <strong>clinical</strong> <strong>handover</strong>, developed in 2009. 10HandoverprocessThe transfer of <strong>clinical</strong> inform<strong>at</strong>ion th<strong>at</strong>is vital to continuity of p<strong>at</strong>ient careTwo-way communic<strong>at</strong>ionTools to facilit<strong>at</strong>e <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong>Implementing <strong>clinical</strong> <strong>handover</strong> <strong>at</strong> <strong>JMO</strong> <strong>shift</strong> <strong>changes</strong> mustbe appropri<strong>at</strong>e to local needs.Appendix E – High level implement<strong>at</strong>ion framework toassist local planning.Appendix F – Implement<strong>at</strong>ion support tools and templ<strong>at</strong>es.NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 9
3.1 Handover happensClinical <strong>handover</strong> occurs <strong>at</strong> <strong>all</strong><strong>JMO</strong> <strong>shift</strong> <strong>changes</strong>Clinical <strong>handover</strong> is expected and occurs <strong>at</strong> every JuniorMedical Officer <strong>shift</strong> change, regardless of specialty, in <strong>all</strong>facilities particip<strong>at</strong>ing in the Clinical Educ<strong>at</strong>ion and TrainingInstitute (CETI) prevoc<strong>at</strong>ional training networks.Essential elements for implement<strong>at</strong>ion33Shift rostering to facilit<strong>at</strong>e <strong>handover</strong>Particip<strong>at</strong>ing in <strong>shift</strong> <strong>handover</strong> is written into positiondescriptions for <strong>JMO</strong>s and RegistrarsAppropri<strong>at</strong>e supervision of <strong>JMO</strong>s is provided <strong>at</strong><strong>shift</strong> <strong>handover</strong>.HandoverHandover is essential and must occur <strong>at</strong> <strong>shift</strong> change.Electronic tools are supplementary and cannot replace processes of human interaction <strong>at</strong> <strong>handover</strong>.3.2 Handover leadershipSenior medical leadership in<strong>JMO</strong> <strong>shift</strong> <strong>handover</strong>Effective <strong>JMO</strong> <strong>handover</strong> <strong>at</strong> <strong>shift</strong> <strong>changes</strong> requiresleadership from executive and <strong>clinical</strong> leaders to:• be responsible for implement<strong>at</strong>ion of <strong>handover</strong>processes, and• ensure registrar <strong>at</strong>tendance and leadership of<strong>handover</strong> <strong>at</strong> <strong>JMO</strong> <strong>shift</strong> <strong>changes</strong>.Essential elements for implement<strong>at</strong>ion333Local executive sponsorship is essential to direct theimplement<strong>at</strong>ion of <strong>clinical</strong> <strong>handover</strong> <strong>at</strong> <strong>all</strong> <strong>JMO</strong> <strong>shift</strong><strong>changes</strong>Consultants/Staff Specialists / Visiting MedicalOfficers need to be responsible for <strong>clinical</strong> <strong>handover</strong>implement<strong>at</strong>ion across <strong>all</strong> <strong>shift</strong>sRegistrars should <strong>at</strong>tend and lead <strong>all</strong> <strong>JMO</strong> <strong>shift</strong><strong>handover</strong>.Valuing <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong>Set the expect<strong>at</strong>ion th<strong>at</strong> <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong> is a valuableand essential part of every <strong>shift</strong>.Executive and <strong>clinical</strong> leaders sponsor <strong>JMO</strong> <strong>clinical</strong><strong>handover</strong> through:• policy• monitoring and evalu<strong>at</strong>ion of processes and outcomes• training programs.Essential elements for implement<strong>at</strong>ion3333Shift rostering to facilit<strong>at</strong>e <strong>handover</strong>Particip<strong>at</strong>ing in <strong>shift</strong> <strong>handover</strong> written into positiondescriptions for <strong>JMO</strong>s and RegistrarsAppropri<strong>at</strong>e supervision of <strong>JMO</strong>s is provided <strong>at</strong><strong>shift</strong> <strong>handover</strong>All staff <strong>at</strong>tending the <strong>handover</strong> must be made awareof the local processes and the importance of <strong>handover</strong>.Not <strong>all</strong> facilities have Registrars rostered on <strong>all</strong> <strong>shift</strong>s with <strong>JMO</strong>s.Consider other options: • Career Medical Officers • Consultants • Staff Specialists• Visiting Medical Officers • Senior Nurses (eg After Hours Nurse Managers)10 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
3.3 Handover set-upPrepare for <strong>handover</strong> by prioritisingp<strong>at</strong>ient listsJunior and senior clinicians work collabor<strong>at</strong>ively (seekingand providing leadership) to prioritise p<strong>at</strong>ient lists for<strong>clinical</strong> <strong>handover</strong>.Essential elements for implement<strong>at</strong>ion3 Registrars should be present and lead <strong>clinical</strong> <strong>handover</strong>prioritis<strong>at</strong>ion <strong>at</strong> <strong>all</strong> <strong>JMO</strong> <strong>shift</strong> <strong>changes</strong>.– Involve <strong>JMO</strong>s in clear prioritis<strong>at</strong>ion of p<strong>at</strong>ients and<strong>all</strong>oc<strong>at</strong>ion of tasks3 When Registrars are unable to <strong>at</strong>tend <strong>JMO</strong> <strong>shift</strong><strong>handover</strong>, processes should be implemented tofacilit<strong>at</strong>e <strong>JMO</strong> prioritis<strong>at</strong>ion of p<strong>at</strong>ient lists, including:– face to face consult<strong>at</strong>ion between the <strong>JMO</strong> andRegistrar before <strong>shift</strong> change, and– telephone ward rounds between the <strong>JMO</strong>and Registrar.Key participant <strong>at</strong>tendance <strong>at</strong><strong>JMO</strong> <strong>shift</strong> <strong>handover</strong>Identify the key participants for <strong>handover</strong> <strong>at</strong> each <strong>JMO</strong><strong>shift</strong> change:• night to day• day to evening• evening to night• weekdays and weekends.Essential elements for implement<strong>at</strong>ion3 Wherever possible, a Consultant/Staff Specialist orVisiting Medical Officer should be included as a keyparticipant <strong>at</strong> <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong>3 Registrars should be present <strong>at</strong> every <strong>JMO</strong> <strong>shift</strong><strong>handover</strong>3 Facilities should consider local requirements whenimplementing <strong>JMO</strong> <strong>handover</strong> <strong>at</strong> <strong>all</strong> <strong>shift</strong> <strong>changes</strong>,with regard to specialty team <strong>handover</strong>, or whole ofhospital <strong>handover</strong>3 Where appropri<strong>at</strong>e, the inclusion of a senior nursingstaff member should be considered.Time <strong>all</strong>oc<strong>at</strong>ion for <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong>• Set agreed times and dur<strong>at</strong>ions for each <strong>shift</strong><strong>handover</strong> across 24 hour /7 days per week• It is highly recommended th<strong>at</strong>, where possible,str<strong>at</strong>egies are in place to reinforce punctuality.Essential elements for implement<strong>at</strong>ion3333Shift <strong>handover</strong> must start on time and finish on timeAll key participants must be informed of the time for<strong>all</strong> relevant <strong>shift</strong> <strong>handover</strong>sShift <strong>handover</strong> should be considered “pager-free”– except for emergency c<strong>all</strong>sShift rostering to facilit<strong>at</strong>e <strong>handover</strong>.A design<strong>at</strong>ed <strong>JMO</strong> <strong>shift</strong> <strong>handover</strong> place• Set a specific loc<strong>at</strong>ion for each <strong>shift</strong> <strong>handover</strong> across24 hour /7 days• Wherever possible, the <strong>handover</strong> loc<strong>at</strong>ion shouldfacilit<strong>at</strong>e face-to-face interaction.Essential elements for implement<strong>at</strong>ion3Shift <strong>handover</strong> must occur in a consistent loc<strong>at</strong>ion.The loc<strong>at</strong>ion should:– be easy for <strong>all</strong> participants to <strong>at</strong>tend– be quiet and free from distraction– promote face to face interaction– promote active and engaged interaction– have loc<strong>all</strong>y necessary IT or telecommunic<strong>at</strong>ionsfacilities to <strong>all</strong>ow engagement of <strong>all</strong> keyparticipants.NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 11
AppendicesAppendix AA clear case for changeQuality Systems Assessment D<strong>at</strong>aIn 2009 the Clinical Excellence Commission undertookits second Quality Systems Assessment (QSA) Survey ofthe NSW health system 5 . One of the 4 key topic areasinvestig<strong>at</strong>ed was <strong>clinical</strong> <strong>handover</strong>.• The results of the 2009 QSA showed th<strong>at</strong>, for medicalteams, 14% reported th<strong>at</strong> no time is spent on <strong>shift</strong><strong>handover</strong>, and a further 18% reported th<strong>at</strong> less than10 minutes is spent.Liter<strong>at</strong>ureLiter<strong>at</strong>ure cited by the Australian Commission on Safetyand Quality in HealthCare (2010) – the OSSIE Guide toClinical Handover Improvement 1 highlights the importanceof robust <strong>handover</strong> practices in the medical profession:• Handover is among the most common causes ofmalpractice claims in the USA, especi<strong>all</strong>y amongtrainees, accounting for 20% of cases(Singh et al, 2007)• A survey among trainees in the USA suggested th<strong>at</strong>15% of adverse events, errors or near misses involved<strong>handover</strong> (Jagsi et al, 2005)• Survey of junior doctors in the United Kingdomdiscovered th<strong>at</strong> 83% believed th<strong>at</strong> <strong>handover</strong> processwas poor. Written <strong>handover</strong> was rarely received,accounting for only 6% of <strong>all</strong> <strong>handover</strong>s (Roughtonand Severs, 1996)• Incorpor<strong>at</strong>ing simple document<strong>at</strong>ion processes into<strong>clinical</strong> <strong>handover</strong> ensured full maintenance of <strong>clinical</strong>d<strong>at</strong>a transferred, compared to 97.5% <strong>at</strong>trition of<strong>clinical</strong> d<strong>at</strong>a by relying solely on verbal <strong>handover</strong> andmemory (Pothier et al, 2005).A NSW Health commissioned liter<strong>at</strong>ure review by theAdvisory Board (2010) – Best Practices for PhysicianHandoffs 12 identified th<strong>at</strong> ineffective <strong>clinical</strong> <strong>handover</strong>procedures for medical officers contributed significantlyto adverse events in the USA, specific<strong>all</strong>y:• Communic<strong>at</strong>ion problems were the major source of65% of hospital sentinel events between 1995 and2004 (Runy, 2008), and th<strong>at</strong> the risk of an adverseevent increased with the number of times they weretransferred between units, physicians and teams.• One insurance company alone <strong>at</strong>tributed $173million in losses to events rel<strong>at</strong>ed to <strong>clinical</strong> <strong>handover</strong>(Hoffman, 2007), and th<strong>at</strong> over half of these eventsentailed severe injury.The same liter<strong>at</strong>ure review also identifies methods forimproving <strong>handover</strong>, including:• Increased face to face rostered time for physicians to<strong>handover</strong> in a quiet room (Buckley, 2007)• Read backs <strong>all</strong>ow for the clarific<strong>at</strong>ion of inform<strong>at</strong>ionand reduction in misconceptions following <strong>handover</strong>(Gesensway, 2006)• Formalised early educ<strong>at</strong>ion for <strong>JMO</strong>s in <strong>clinical</strong><strong>handover</strong> process and importance <strong>shift</strong>s <strong>at</strong>titudestowards clear responsibility for p<strong>at</strong>ient care(Solet et al, 2005)• Increasing two-way communic<strong>at</strong>ion in <strong>handover</strong>improves anticip<strong>at</strong>ion of next steps for p<strong>at</strong>ient care andbolsters the learning process for <strong>JMO</strong>s (Buckley, 2007).A liter<strong>at</strong>ure review commissioned by the AustralianCommission on Safety and Quality in HealthCare (2008) –A Structured Evidence-based Liter<strong>at</strong>ure Review regardingthe Effectiveness of Improvement Interventions in ClinicalHandover 14 identified risks associ<strong>at</strong>ed with <strong>clinical</strong><strong>handover</strong>, including:• inexperience of <strong>clinical</strong> staff• poor communic<strong>at</strong>ion behaviours• lack of communic<strong>at</strong>ion quality/content• lack of standardised protocols• health professional f<strong>at</strong>igue.NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 13
The <strong>clinical</strong> <strong>handover</strong> guide published by the AustralianMedical Associ<strong>at</strong>ion (2006) – Safe Handover : SafeP<strong>at</strong>ients 3 identifies a number of themes consistent withthe above liter<strong>at</strong>ure to underline the importance of <strong>clinical</strong><strong>handover</strong> processes, including:• recognition of the effects of doctor f<strong>at</strong>igue• rapidly increasing complexity of care for p<strong>at</strong>ients• safe work hours, cre<strong>at</strong>ing the requirement for <strong>shift</strong><strong>changes</strong> and hence <strong>handover</strong>• gre<strong>at</strong>er cross-over between specialty teams and themultidisciplinary team• the fact th<strong>at</strong> a doctor may have no day time contactwith a p<strong>at</strong>ient, yet be responsible and accountable forth<strong>at</strong> p<strong>at</strong>ient’s safe <strong>clinical</strong> care during rostered out-ofhoursperiods.<strong>JMO</strong> perspectiveAll work rel<strong>at</strong>ing to the <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> projecthas been developed in close consult<strong>at</strong>ion with <strong>JMO</strong>represent<strong>at</strong>ives of the CETI <strong>JMO</strong> Forum.The case for change message from the perspective ofthese Junior Medical Officers is clear:• Clinical <strong>handover</strong> <strong>at</strong> <strong>JMO</strong> <strong>shift</strong> <strong>changes</strong> needs toimprove because…“<strong>JMO</strong> <strong>handover</strong> is where lots of importantinform<strong>at</strong>ion gets missed.”“Handover from weekday to weekend andback again is a big problem. By the end of theweekend the messages about sick p<strong>at</strong>ients havebeen lost.”“Establishing continuity of care for a p<strong>at</strong>ientin a way th<strong>at</strong> will ensure th<strong>at</strong> issues or eventsth<strong>at</strong> occur outside of business hours do not justf<strong>all</strong> through the cracks and th<strong>at</strong> deterior<strong>at</strong>ingp<strong>at</strong>ients are picked up earlier r<strong>at</strong>her than l<strong>at</strong>er.”“If we don’t change we risk worse outcomesfor p<strong>at</strong>ients, including de<strong>at</strong>h, lack of ownershipof p<strong>at</strong>ient care, deskilling and constant ‘firefighting’ as opposed to care based on having the complete picture.”“It is much safer and more effective when evenminimal supervision of <strong>handover</strong> occurs.”“Morning <strong>handover</strong> meetings in our departmenthave provided some of the best learningexperiences. The consultants re<strong>all</strong>y particip<strong>at</strong>eand share their thinking processes with the junior doctors.”Appendix BWider issues th<strong>at</strong> requireconsider<strong>at</strong>ionJunior doctorsThe immedi<strong>at</strong>e scope of this project and document isfocused on the most junior doctors who are within thefirst two years of gradu<strong>at</strong>ion, but the key elements andobjectives should also be considered for implement<strong>at</strong>ion in<strong>all</strong> facilities th<strong>at</strong> employ any junior doctors during the day,evening or night.Junior doctors could refer to:• residents in their third or l<strong>at</strong>er year of work• overseas gradu<strong>at</strong>e doctors who are newly employed inthe NSW health system• newly appointed accredited or non-accreditedregistrars.According to the Dreyfus model of professionaldevelopment 4 , <strong>all</strong> doctors are continu<strong>all</strong>y developing their<strong>clinical</strong> skills and competency in <strong>clinical</strong> <strong>handover</strong>. Thecloser doctors in a facility are to the novice end of thescale, the gre<strong>at</strong>er the level of structure and supervisionth<strong>at</strong> should be put in place to support their development.14 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
The implement<strong>at</strong>ion of structured and standardised <strong>clinical</strong><strong>handover</strong> should be considered for <strong>all</strong> doctors, r<strong>at</strong>her thanlimited to the specific project scope of the most juniordoctors in their first two years of prevoc<strong>at</strong>ional training.Rostering <strong>shift</strong> overlap to facilit<strong>at</strong>e<strong>clinical</strong> <strong>handover</strong>The first objective of this project is: ‘Th<strong>at</strong> <strong>clinical</strong> <strong>handover</strong>between <strong>JMO</strong>s occurs <strong>at</strong> <strong>all</strong> <strong>shift</strong> <strong>changes</strong>’.Dreyfus Model 4Considering the Dreyfus model will help facilities plan theirlocal implement<strong>at</strong>ion of the <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> project.Th<strong>at</strong> is:The first principle to guide implement<strong>at</strong>ion is: ‘Handoverhappens: <strong>clinical</strong> <strong>handover</strong> occurs <strong>at</strong> <strong>all</strong> <strong>JMO</strong> <strong>shift</strong><strong>changes</strong>’.Rostered <strong>shift</strong> overlap is an essential element to ensureth<strong>at</strong> <strong>handover</strong> occurs <strong>at</strong> <strong>all</strong> <strong>JMO</strong> <strong>shift</strong> <strong>changes</strong>.• Facilities, specialties or times of the day wherethere are limited staffing resources to provide juniordoctors with senior leadership and supervision shouldconsider gre<strong>at</strong>er degrees of <strong>clinical</strong> <strong>handover</strong> processstandardis<strong>at</strong>ion and structure• Facilities, specialties or times of the day where thereare gre<strong>at</strong>er opportunities to access senior clinicians asleaders of <strong>clinical</strong> <strong>handover</strong> can implement processesth<strong>at</strong> are more flexible to immedi<strong>at</strong>e <strong>clinical</strong> andstaffing demands and have a gre<strong>at</strong>er focus on <strong>clinical</strong>management plans and developing junior staff.Page 7-8 provides more inform<strong>at</strong>ion on the role of seniorleadership in <strong>JMO</strong> <strong>handover</strong>.Pages 9-12 provides more inform<strong>at</strong>ion on key principlesto consider when implementing processes th<strong>at</strong> supportjunior doctors.Appendix D describes <strong>clinical</strong> inform<strong>at</strong>ion to considerwhen handing over a p<strong>at</strong>ient.The Acute Care Taskforce has explored project synergieswith the Rostering Centre of Excellence.Facilities are encouraged to maintain local implement<strong>at</strong>ionmomentum and explore innov<strong>at</strong>ive practices forappropri<strong>at</strong>e <strong>shift</strong> overlap to facilit<strong>at</strong>e <strong>handover</strong>.Some basic innov<strong>at</strong>ive rostering models should beconsidered and implemented, where appropri<strong>at</strong>e.For example:1. Change from rostered day <strong>shift</strong>s to staggered <strong>shift</strong>s toprovide <strong>shift</strong> overlap and continuity of p<strong>at</strong>ient care fromday to evening. Altern<strong>at</strong>e on weekly basis.OrthopaedicRegistrar 1OrthopaedicRegistrar 2Mon 0700 to 1530 1300 to 2100Tues 0700 to 1530 1300 to 2100Wed 0700 to 1530 1300 to 2100Thurs 0700 to 1530 1300 to 2100Fri 0700 to 1530 1300 to 2100Dreyfus ModelNoviceAdvancedbeginnerCompetent Proficient ExpertRequires significantstructure andsupervisionRequires lessstructureand supervisionProvider ofstructure andsupervisionNSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 15
2. Increase in team staffing levels to provide for <strong>shift</strong>overlap and evening cover. Altern<strong>at</strong>e on weekly basis.There is a benefit in the reduction in rosteredovertime <strong>shift</strong>s.Aged Care<strong>JMO</strong>1Aged Care<strong>JMO</strong>2Mon 0800 to 1630 1500 to 2300Tues 0700 to 1530 1500 to 2300Wed 0700 to 1530 1500 to 2300Thurs 0700 to 1530 1500 to 2300Fri 0700 to 1530 1500 to 2300Appendix CPoints to consider forimplement<strong>at</strong>ion across 24 hoursFacilities should consider a range of points whenimplementing loc<strong>all</strong>y appropri<strong>at</strong>e <strong>clinical</strong> <strong>handover</strong>processes, 24 hours per day and 7 days per week.• Are you implementing a whole of hospital or specialtyteam <strong>clinical</strong> <strong>handover</strong> meeting? The size of hospitalmay determine whether specialty team or whole ofhospital based <strong>handover</strong>s are implemented• Wh<strong>at</strong> is the local p<strong>at</strong>tern of <strong>shift</strong> times? Staggered <strong>shift</strong>times will require local consider<strong>at</strong>ion as to how theimportant inform<strong>at</strong>ion <strong>at</strong> <strong>handover</strong> is not skipped forsome staff• Wh<strong>at</strong> are the hospital and work load pressures acrossthe 24 hour clock? These may impact the purpose andstructure of the <strong>handover</strong> meeting? (eg P<strong>at</strong>ients whohave been unwell over night vs outstanding tasks ornew admissions during the day)– Day to evening <strong>handover</strong> may require gre<strong>at</strong>erprocess structure to ensure <strong>all</strong> key inform<strong>at</strong>ion iscondensed to the fewer number of oncoming staff.– Night to morning <strong>handover</strong> may have gre<strong>at</strong>eropportunity for detailed <strong>handover</strong>, casepresent<strong>at</strong>ions and teaching rel<strong>at</strong>ing to p<strong>at</strong>ient careduring the night <strong>shift</strong>.• Two-way communic<strong>at</strong>ion is a consistent requirementacross 24 hours• Wh<strong>at</strong> do local executive and <strong>clinical</strong> leaders need todo to ensure th<strong>at</strong> <strong>clinical</strong> <strong>handover</strong> is a priority <strong>at</strong> <strong>all</strong><strong>shift</strong> <strong>changes</strong>?• Can you get consultant commitment to lead <strong>handover</strong>and act on <strong>clinical</strong> management issues immedi<strong>at</strong>ely,potenti<strong>all</strong>y reducing the need for c<strong>all</strong> outs?• How can Registrars be supported (including innov<strong>at</strong>iverostering) to <strong>at</strong>tend and coordin<strong>at</strong>e <strong>clinical</strong> <strong>handover</strong>?• Who are other senior clinicians th<strong>at</strong> may be ableto facilit<strong>at</strong>e the process of <strong>clinical</strong> <strong>handover</strong>, whenRegistrars or Consultants are unavailable?• Are there clear senior contact persons to providesupport to <strong>JMO</strong>s between <strong>shift</strong>s, to reduce the risk ofissues being held over until <strong>shift</strong> change <strong>handover</strong>?• <strong>JMO</strong>s need support <strong>at</strong> <strong>all</strong> <strong>shift</strong> <strong>changes</strong>. No clinicianshould ever feel isol<strong>at</strong>ed• How can you reinforce <strong>at</strong>tendance and punctuality <strong>at</strong><strong>all</strong> <strong>shift</strong> change <strong>handover</strong>s?• Type and size of <strong>handover</strong> (specialty team vs whole ofhospital) will determine physical loc<strong>at</strong>ion requirements(room, IT and telecommunic<strong>at</strong>ions requirements)• When and how can educ<strong>at</strong>ional opportunities beincorpor<strong>at</strong>ed?• When and how can you get staff together (face toface) and facilit<strong>at</strong>e a collegial <strong>at</strong>mosphere?• Training programs in <strong>clinical</strong> <strong>handover</strong> must beaccessible to staff working on <strong>all</strong> <strong>shift</strong>s• Evalu<strong>at</strong>ion and monitoring should involve <strong>handover</strong>on <strong>all</strong> <strong>shift</strong>s• Wh<strong>at</strong> is the appropri<strong>at</strong>e communic<strong>at</strong>ion requirement toother disciplines (eg Nursing) so th<strong>at</strong> <strong>shift</strong> <strong>handover</strong> isas uninterrupted as possible?• Templ<strong>at</strong>es should be supplementary and act asmemory prompts to the <strong>shift</strong> <strong>handover</strong> process• Templ<strong>at</strong>es should not detract from the n<strong>at</strong>uraltwo-way human interaction required for effectivecommunic<strong>at</strong>ion.16 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
Appendix DClinical inform<strong>at</strong>ion to considerwhen handing over a p<strong>at</strong>ientThe right <strong>clinical</strong> inform<strong>at</strong>ion needs to be handed over toensure transfer of responsibility and accountability forp<strong>at</strong>ient care.P<strong>at</strong>ients who are less stable or have changing managementplans may require a detailed <strong>handover</strong>, while others whoare rel<strong>at</strong>ively stable and with fewer outstanding tests oractions can be summarised more quickly.Senior clinician supervision of <strong>JMO</strong>s <strong>at</strong> <strong>clinical</strong> <strong>handover</strong> isimportant to help decide which p<strong>at</strong>ients, how much andwhich <strong>clinical</strong> inform<strong>at</strong>ion needs to be handed over.(See pg 7 for further assistance)The exact structure of how you <strong>handover</strong> <strong>clinical</strong> inform<strong>at</strong>ionwill also be dependant on the scenario of <strong>handover</strong>.For example: you would pay particular <strong>at</strong>tention to theinitial introduction if you were waking a consultant inthe middle of the night, as compared to when you arehanding over <strong>at</strong> <strong>shift</strong> change to one of your peers.In total, the detailed <strong>handover</strong> example shown belowwould take no more than 2 minutes to deliver.ISBARInform<strong>at</strong>ion:Situ<strong>at</strong>ion:Background:Assessment:My name is John Smith. I am an RMO2, in Westmead, Emergency DepartmentThe situ<strong>at</strong>ion is th<strong>at</strong> I am requesting admission for Mrs Jane Jones, who is an 80 yearoldwoman with an acute exacerb<strong>at</strong>ion of chronic left ventricular failureBy way of background, she presented with gradu<strong>all</strong>y progressive SOB over 3 days,with exertional chest heaviness, and is now SOB <strong>at</strong> rest and experiencing PND.She was admitted under Dr X 2 months ago with a non-STEMI AMI, Type 2 DiabetesMellitus and hypertension.She is currently on aspirin, perindopril, diltiazem and gliclazide.She has had <strong>all</strong>ergies to penicillin, and is an ex-smoker and does not drink or usesleeping tablets.She lives alone.On assessment, she has signs of left and right heart failure with CO 2 retention:central cyanosis, asterixis, respir<strong>at</strong>ion 16, s<strong>at</strong>ur<strong>at</strong>ions 88%on room air. Her vital signs include BP 145/88, regular pulse 70 bpm and JVP slightlyelev<strong>at</strong>ed. She has moder<strong>at</strong>e peripheraloedema and medium-coarse bisbasal crackles.The CXR shows interstitial and alveolar oedema, ECG sinus rhythm with new l<strong>at</strong>eralt-wave fl<strong>at</strong>tening, TNT elev<strong>at</strong>ed <strong>at</strong> 0.4, EUCs showing mild hypon<strong>at</strong>raemia (Na 130)and renal impairment (Cr 142) but normal K (4.0). LFTs, Glc, CMP, FBC and coagsnormal.She has left ventricular failure associ<strong>at</strong>ed with a non-STEMI and has been commencedon Oxygen (6L/min), aspirin, frusemide, fluid restriction and therapeutic enoxaparinand will be monitored and have serial ECGs and TNTs. The diltiazem has beenwithheld by the team.Recommend<strong>at</strong>ion: My recommend<strong>at</strong>ion is th<strong>at</strong> this p<strong>at</strong>ient needs admission by the Cardiology team in amonitored CCU bed and will need an Echo within 24 hours.NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 17
Some basic inform<strong>at</strong>ion you should consider when handing over different p<strong>at</strong>ient types.The inform<strong>at</strong>ion in the following table shows the type of inform<strong>at</strong>ion for six broad p<strong>at</strong>ient types th<strong>at</strong> should beconsidered to ensure a concise, but comprehensive and effective <strong>handover</strong>.Medical (with multiple co-morbidities) Surgical Emergency DepartmentI– Wh<strong>at</strong> is your name?– Wh<strong>at</strong> is your surname?– Wh<strong>at</strong> is your position in the Hospital?– Which Hospital are you c<strong>all</strong>ing from?– Which part of the Hospital are you c<strong>all</strong>ing from?No changeNo changeS– Why are you c<strong>all</strong>ing me?– Wh<strong>at</strong> is the p<strong>at</strong>ient’s name(first name followed by surname)?– How old is the p<strong>at</strong>ient?– Wh<strong>at</strong> gender is the p<strong>at</strong>ient?– Wh<strong>at</strong> is/are the problem/s or diagnosis/es?No changeAdd:– Has the p<strong>at</strong>ient been admittedor accepted by a specialty team.– Is the p<strong>at</strong>ient scheduled underthe Mental Health Act, do theyneed a nurse special?B– Wh<strong>at</strong> is/are the presenting symptom/s?– How bad are these symptoms?– Wh<strong>at</strong> relevant problems has the p<strong>at</strong>ient hadpreviously?– Wh<strong>at</strong> medic<strong>at</strong>ions is the p<strong>at</strong>ient on?– Wh<strong>at</strong> <strong>all</strong>ergies does the p<strong>at</strong>ient have?– Does the p<strong>at</strong>ient smoke, drink or usebenzodiazepines?– Why does the p<strong>at</strong>ient need to be tre<strong>at</strong>ed inhospital r<strong>at</strong>her than <strong>at</strong> home or in the clinic?Remove:– “How bad are thesesymptoms”Add:– Has the p<strong>at</strong>ient hada recent surgery?If so, wh<strong>at</strong> surgeryand when?– When did the p<strong>at</strong>ientlast e<strong>at</strong> or drink?Add:– Wh<strong>at</strong> is their pre-morbidst<strong>at</strong>us and social situ<strong>at</strong>ion?– Any important linkages without of hospital care / GeneralPractice.A– Wh<strong>at</strong> are the p<strong>at</strong>ient’s vital signs (appearance,comfort, BP, pulse r<strong>at</strong>e and rhythm, JVP,respir<strong>at</strong>ory r<strong>at</strong>e, temper<strong>at</strong>ure and urine output)?– Wh<strong>at</strong> are the salient <strong>clinical</strong> signs th<strong>at</strong> supportthe diagnosis and indic<strong>at</strong>e the severity?– Wh<strong>at</strong> are the key investig<strong>at</strong>ions/ procedures –planned or results?– Wh<strong>at</strong> are the problems and tre<strong>at</strong>ments youhave begun in order of importance?– Is the p<strong>at</strong>ient/carer up to d<strong>at</strong>e with thediagnosis and tre<strong>at</strong>ment plan?Add:– Is the p<strong>at</strong>ient havingDVT prophylaxis?– Wh<strong>at</strong> intravenousfluidsare beingadministeredand <strong>at</strong> wh<strong>at</strong> r<strong>at</strong>e?– Wh<strong>at</strong> antibiotics arebeing administered?– Wh<strong>at</strong> analgesia isbeing utilised?Add:– Are they fasting, or limitedoral intake?– Can they take oral medic<strong>at</strong>ions?– Any outstanding consult<strong>at</strong>ionsor reviews– Where should the p<strong>at</strong>ientgo when they finish in ED?– Is the transfer paperworkcomplete?RYour recommend<strong>at</strong>ions for ongoing care withclear timeframes th<strong>at</strong> facilit<strong>at</strong>e the transfer ofresponsibility and accountability for p<strong>at</strong>ient care.Read back to prevent misconceptions and clarifywh<strong>at</strong> you have understood.No changeNo change18 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
Most of the fundamental inform<strong>at</strong>ion is standard, regardless of the p<strong>at</strong>ient type, but please pay <strong>at</strong>tention to the keydifferences identified against the standard medical p<strong>at</strong>ient example.Obstetrics and Gynaecology Mental Health Paedi<strong>at</strong>ricsNo change No change No changeAdd:– Is the p<strong>at</strong>ient in the ED, Ward, Community?– Is the p<strong>at</strong>ient in seclusion?– Is the p<strong>at</strong>ient under the Mental Health Act?No changeAdd:– Is the p<strong>at</strong>ient pregnant?– How many weeks gest<strong>at</strong>ion?– If in labour, wh<strong>at</strong> is the Cervixdil<strong>at</strong>ion?– Inform<strong>at</strong>ion rel<strong>at</strong>ing to theCTG traceRemove:– “How bad are these symptoms”– Why does the p<strong>at</strong>ient need to be tre<strong>at</strong>ed in hospitalr<strong>at</strong>her than <strong>at</strong> home or in the clinic?Add:– How long has this p<strong>at</strong>ient been in care?– Do they have a primary carer?– Accommod<strong>at</strong>ion?– How/why did this person get brought to hospital?– Substance abuse?Add:– Wh<strong>at</strong> is the p<strong>at</strong>ient’s current mental st<strong>at</strong>e?– Are they distressed, suicidal or wanting to harm others?– If in the ED wh<strong>at</strong> was the result of the examin<strong>at</strong>ion bythe medical officers?– Key MSE findings?– Wh<strong>at</strong> risks (to self/others) have been identified?Add:– Birth history (anten<strong>at</strong>al,perin<strong>at</strong>al etc)– Developmental &growth assessments(growth charts)– Social/family issues– Vaccin<strong>at</strong>ion st<strong>at</strong>usNo changeNo changeAdd:Specific recommend<strong>at</strong>ion rel<strong>at</strong>ing to:– Loc<strong>at</strong>ion for tre<strong>at</strong>ment– Medic<strong>at</strong>ions– Wh<strong>at</strong> other teams should be involved?No changeNSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 19
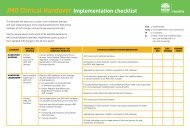
Appendix EImplement<strong>at</strong>ion framework to assist facilities with<strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>OSSIE Key Task Task Description Key leadOSSIOrganis<strong>at</strong>ionalLeadershipSimple SolutionDevelopmentStakeholderEngagementImplement<strong>at</strong>ionSponsorshipProject teamLocal authority andchampionsInvestig<strong>at</strong>e existing localpracticesDesign local <strong>clinical</strong><strong>handover</strong> processesPrepare for investig<strong>at</strong>ionof existing practiceDevelop a strongcommunic<strong>at</strong>ions planSystem communic<strong>at</strong>ionsMand<strong>at</strong>edimplement<strong>at</strong>ionSupporting tools andtempl<strong>at</strong>esIdentify executive and <strong>clinical</strong> sponsors & link with othergovernance structures.Identify relevant team members, eg Consultant, Registrar,<strong>JMO</strong>, Nursing represent<strong>at</strong>ivesEngage local Clinical Training Council and othersenior cliniciansUtilise focus groups, available d<strong>at</strong>a, observ<strong>at</strong>ions,and surveysIdentify barriers and motiv<strong>at</strong>ors. Ensure processes arespecific to the needs of day, evening, night and weekend<strong>shift</strong>s.Engage staff in necessary focus groups and developanalytical surveys of existing practicekey messages defined <strong>at</strong> <strong>all</strong> levels: Executive, Consultant,Registrar, <strong>JMO</strong>, Nursing etc.Regular effective communic<strong>at</strong>ions <strong>at</strong> <strong>all</strong> levels defined inthe communic<strong>at</strong>ion plan – Clear case for changeNecessary policy and review of position descriptions toimplement ISBAR and <strong>handover</strong> processesDevelop standard generic communic<strong>at</strong>ion templ<strong>at</strong>es andtools in ISBAR form<strong>at</strong>Facility GeneralManagerSponsorsSponsorsProject TeamProject TeamProject TeamProject TeamProject TeamSponsorsProject TeamPilot Implement<strong>at</strong>ion Implement pilot processes in day, evening and night Project TeamEEvalu<strong>at</strong>ion andMaintenanceSystem Implement<strong>at</strong>ionDevelop evalu<strong>at</strong>ion planPre-evalu<strong>at</strong>e pilot loc<strong>at</strong>ionSystem implement<strong>at</strong>ion of upd<strong>at</strong>ed <strong>clinical</strong> <strong>handover</strong>processes, following pilot evalu<strong>at</strong>ion reviewProject TeamProject TeamProject TeamPost-evalu<strong>at</strong>ion of pilot loc<strong>at</strong>ion, review and appropri<strong>at</strong>e redesign of <strong>handover</strong> processesProject TeamCyclical evalu<strong>at</strong>ion and monitoring with term <strong>changes</strong>Project Team20 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
The framework below is a framework to assist facilities plan and implement the outputs of the <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>project. This framework is not mand<strong>at</strong>ory to use, but will assist facilities to guide their implement<strong>at</strong>ion planning, utilisingthe OSSIE form<strong>at</strong> recommended by the Australian Commission on Safety and Quality in Health Care.Term 1 –10 WeeksTerm 2 –10 WeeksTerm 3 –10 WeeksTerm 4 –10 WeeksImplement<strong>at</strong>ion supportingtools & templ<strong>at</strong>es– OSSIE guide – section 3 (pg 15)– “Clinical Handover – Implementing Change”:1.0 Project Initi<strong>at</strong>ion– OSSIE guide – section 4 (pg 37)– “Clinical Handover – Implementing Change”:2.0 Diagnostics & 3.0 Solution Design– <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>:- Key principles checklist– OSSIE guide – section 5 (pg 27)– “Clinical Handover – Implementing Change”:1.0 Project Initi<strong>at</strong>ion– <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>:- Key messages from concept testing final report- How to run a focus group– OSSIE guide – section 6 (pg 41)– “Clinical Handover – Implementing Change”:4.0 Implement<strong>at</strong>ion– <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>:- ISBAR templ<strong>at</strong>es- ISBAR training- Educ<strong>at</strong>ion and Evalu<strong>at</strong>ionPilotactivitiesshouldnot ceaseduringevalu<strong>at</strong>ionreview- OSSIE guide – section 7 (pg 47)- “Clinical Handover – Implementing Change”:5.0 Evalu<strong>at</strong>ion- <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>:- key principles checklist- Educ<strong>at</strong>ion and Evalu<strong>at</strong>ionNSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 21
Appendix FImplement<strong>at</strong>ion SupportA range of templ<strong>at</strong>es, tools and links exist.Facilities are encouraged to review the tools and templ<strong>at</strong>esavailable to guide loc<strong>all</strong>y appropri<strong>at</strong>e implement<strong>at</strong>ion of<strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>.The listed guides, templ<strong>at</strong>es and tools are neithermand<strong>at</strong>ory nor exclusive.<strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>implement<strong>at</strong>ion supporting toolsand templ<strong>at</strong>es:The listed tools and templ<strong>at</strong>es have been developedspecific<strong>all</strong>y to assist implement<strong>at</strong>ion of the <strong>JMO</strong> <strong>clinical</strong><strong>handover</strong> project.These tools can be supplemented by the tools andtempl<strong>at</strong>es produced, as part of Safe Clinical Handover:standard key principles for <strong>clinical</strong> <strong>handover</strong> (2009). Alllisted tools and templ<strong>at</strong>es can be accessed on the NSWHealth Safe Clinical Handover webpage:http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>• Clinician’s Summary – a 12 page version of thisdocument designed to summarise the key elements of<strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> into a more consumable form<strong>at</strong>for clinicians• 1-pagers – single page summaries to deliver highestlevelkey messages targeted <strong>at</strong> both junior and seniorclinician’s• Key messages for local implement<strong>at</strong>ion of <strong>JMO</strong> <strong>clinical</strong><strong>handover</strong> – basic key messages th<strong>at</strong> should be aimed<strong>at</strong> multiple levels of the organis<strong>at</strong>ion to engageclinicians to review, design and implement processesfor <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong>.The final ‘Concept Testing’ report is available fordownload and contains key messages from junior andsenior clinicians about their own experiences withimplementing the <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> project.• Key principles implement<strong>at</strong>ion checklist – achecklist th<strong>at</strong> can be used as an audit tool and/or implement<strong>at</strong>ion progress tool to show how local<strong>clinical</strong> <strong>handover</strong> processes currently map to thekey principles for <strong>clinical</strong> <strong>handover</strong> <strong>at</strong> <strong>all</strong> <strong>JMO</strong> <strong>shift</strong><strong>changes</strong>.• How to run a focus group summary – a summarydeveloped by Qld Health of the steps required tosuccessfully organise and run a focus group.http://www.health.qld.gov.au/chipp/documents/32372.pdf• Educ<strong>at</strong>ion and Evalu<strong>at</strong>ion – Observed Simul<strong>at</strong>ionClinical Exam (OSCE) & Mini-CEX evalu<strong>at</strong>ion areconsidered useful when defining local training andevalu<strong>at</strong>ion programs for <strong>JMO</strong>s. The following articledescribes the implement<strong>at</strong>ion of OSCE and Mini-CEX.The article contains a number or online appendixresources.JM Farnan, JAM Paro, RM Rodriguez, ST Reddy, LHorwitz, JK Johnson, VM Arora. Hand-off Educ<strong>at</strong>ionand Evalu<strong>at</strong>ion: Piloting the Observed Simul<strong>at</strong>edHand-off Experience (OSHE). Journal of GeneralInternal Medicine, DOI 10.1007/s11606-009-1170-y.November 19, 2009.http://www.springerlink.com/content/n4m37g374355q4r2/• Basic ISBAR templ<strong>at</strong>es – ISBAR templ<strong>at</strong>es have beenadapted from the existing work of Hunter NewEngland Health Service and made available acrossNSW. Copies of these templ<strong>at</strong>es can be downloadedfrom the Safe Clinical Handover webpage, including:– Lanyard prompt card– ISBAR note pad– ISBAR A3 poster– ISBAR telephone stickers• ISBAR training – Hunter & New England HealthService has developed standard training tools forthe implement<strong>at</strong>ion of ISBAR across a health service.All tools and resources have been shared and madeavailable for download via the Safe Clinical Handoverwebpage.22 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
Existing guides:IMPLeMeNTATION TOOLKITStandard Key Principlesfor Clinical HandoverImplement<strong>at</strong>ion Toolkit –Standard Key Principlesfor Clinical Handover,(NSW Health 2009)STANDARD KEY PRINCIPLESFOR CLINICAL HANDOVERImplementing Change -Templ<strong>at</strong>esClinical Handover –Implementing Change(NSW Health 2009)The Implement<strong>at</strong>ion toolkit is a ‘how-to’ bookletaimed <strong>at</strong> those reviewing of their local <strong>clinical</strong> <strong>handover</strong>processes in line with the standard key principles for<strong>all</strong> scenarios of <strong>clinical</strong> <strong>handover</strong>.The toolkit contains further background regarding thecase for change, expanded points for the standard keyprinciples, summarised process redesign methodology,examples of existing <strong>clinical</strong> <strong>handover</strong> models, supportingtempl<strong>at</strong>es and many useful links.The implement<strong>at</strong>ion toolkit has undergone extensivesystem wide consult<strong>at</strong>ion and been endorsed by theAcute Care Taskforce.http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>Process Redesign Methodology in this document isdesigned solely as a helpful guide and is not mand<strong>at</strong>ory.The document and the templ<strong>at</strong>es referenced are availableto download from the Clinical Handover website:http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>Some templ<strong>at</strong>es of specific relevance to the <strong>JMO</strong> <strong>clinical</strong><strong>handover</strong> project are:• Templ<strong>at</strong>e 1 – Project Management Plan - Reviewingyour <strong>clinical</strong> <strong>handover</strong> process is a sm<strong>all</strong> scale project.All projects require some structure to give them thebest possible implement<strong>at</strong>ion success.• Templ<strong>at</strong>e 2 – Communic<strong>at</strong>ions Plan - Communic<strong>at</strong>ionmanagement helps you to ensure th<strong>at</strong> you communic<strong>at</strong>ewith stakeholders using the most appropri<strong>at</strong>e methods.• Templ<strong>at</strong>e 4 – Clinical Handover Staff Interview -Interview as many staff members as possible, so th<strong>at</strong>you can gain an over<strong>all</strong> understanding of how thecurrent process is working from a range of points of view.• Templ<strong>at</strong>e 6 – Tag Along / Observ<strong>at</strong>ions - Gain aninsight into the <strong>clinical</strong> <strong>handover</strong> process from anobjective point of view th<strong>at</strong> no other d<strong>at</strong>a can provide.• Templ<strong>at</strong>e 7 – Flow chart example - See an exampleof how a flow chart can help you to understand your<strong>clinical</strong> <strong>handover</strong> process.• Templ<strong>at</strong>e 8 – Handover Issues Log - Consolid<strong>at</strong>e <strong>all</strong> ofthe process issues you identify into one place.• Templ<strong>at</strong>e 9 – Issues Prioritis<strong>at</strong>ion - Be str<strong>at</strong>egic, workout which issues you should tackle first.• Templ<strong>at</strong>e 10 – Solutions Prioritis<strong>at</strong>ion - Theunfortun<strong>at</strong>e reality is th<strong>at</strong> not <strong>all</strong> of your solutions arelikely to be implemented. You have to prioritise.• Templ<strong>at</strong>e 11 – Solution Design - Detail the solutionsth<strong>at</strong> you have decided to progress with.NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 23
l OFFiceGSTON acT 2604Fax. 02 6270 5499ww.ama.com.au/raNchrTiN acT 2605Fax. 02 6273 0455aleS BraNchNardS NSW 1590Fax. 02 9438 3760riTOry BraNchSUariNa NT 0811Fax. 08 8927 7475Nd BraNchhill Qld 4059Fax. 07 3856 4727aliaN BraNchadelaide Sa 5006Fax. 08 8267 5349N BraNchOBarT TaS 7000Fax. 03 6223 6469N BraNchKVille Vic 3052Fax. 03 9280 8786raliaN BraNchlaNdS Wa 6909Fax. 08 9273 3073ical associ<strong>at</strong>ion08 426 793)gston act 2604Prepared for –OSSIE Guideto Clinical HandoverImprovementO = Organis<strong>at</strong>ional leadershipS = Simple solution developmentS = Stakeholder engagementI = Implement<strong>at</strong>ionE = Evalu<strong>at</strong>ion and maintenanceOSSIE Guide to ClinicalHandover Improvement,(Australian Commission onSafety and Quality in HealthCare 2010)A Guide forthe Safe Use ofElectronic ClinicalHandover ToolsA Guide for the Safe Useof Electronic ClinicalHandover Tools,(SA Health & the AustralianCommission on Safety andQuality in Health Care 2010)ore<strong>at</strong>iont yourFFiceThe OSSIE guide assists readers to design, implement,evalu<strong>at</strong>e and maintain <strong>clinical</strong> <strong>handover</strong> improvementprograms th<strong>at</strong> contain a standardised process andcontent d<strong>at</strong>a set.The framework presented in the OSSIE guide is basedon research conducted on medical and nursing <strong>shift</strong> to<strong>shift</strong> <strong>handover</strong> within the acute care hospital setting. Theprinciples align with those of the NSW Health standardkey principles for <strong>clinical</strong> <strong>handover</strong> and may be applicableto other <strong>handover</strong> situ<strong>at</strong>ions, including multidisciplinary,primary care and community <strong>handover</strong>s.www.safetyandquality.gov.au/internet/safety/publishing.nsf/Content/PriorityProgram-05safe <strong>handover</strong> : safe p<strong>at</strong>ientsThe guide is designed to assist <strong>all</strong> stages of the designand use of electronic <strong>handover</strong> systems. The research wasoriented around the implement<strong>at</strong>ion of an electronic toolto support different forms of <strong>clinical</strong> <strong>handover</strong> in each ofthe hospitals.It provides guidance to clinicians, medical administr<strong>at</strong>ors,quality and safety staff and health inform<strong>at</strong>ics professionals.Over<strong>all</strong>, the project found th<strong>at</strong> change management wasparticularly critical when implementing electronic systemsto assist <strong>clinical</strong> <strong>handover</strong>. It is critical th<strong>at</strong> the approach toimplement<strong>at</strong>ion emphasises th<strong>at</strong> the electronic tool shouldsupport, and not replace, processes for <strong>handover</strong>.http://www.safetyandquality.gov.au/internet/safety/publishing.nsf/Content/PriorityProgram-05_SafeTECHguidance on <strong>clinical</strong> <strong>handover</strong>for clinicians and managersSafe Handover:Safe P<strong>at</strong>ients Guide,(the Australian MedicalAssoci<strong>at</strong>ion 2006)The AMA Safe Handover: Safe P<strong>at</strong>ients guide was adaptedfrom the British Medical Associ<strong>at</strong>ion’s resource of thesame name.It was developed to assist the health sector to achievebetter p<strong>at</strong>ient outcomes through good <strong>clinical</strong> <strong>handover</strong>.The guide pays <strong>at</strong>tention to the increasing requirement foreffective <strong>clinical</strong> <strong>handover</strong> in the face of changing workp<strong>at</strong>terns and the need for clinicians and administr<strong>at</strong>ors towork together.The basic principles of this document, rel<strong>at</strong>ing to ‘Who,When, Where, How & Wh<strong>at</strong>’ align with the <strong>clinical</strong><strong>handover</strong> principles of NSW Health.www.ama.com.au/node/406424 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
CD and Video support<strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> –video vignettes and DVDHelpful video vignettes can be viewed directly via theSafe Clinical Handover webpage. Individual vignettesaddress topics such as:• Benefits for <strong>JMO</strong>s/Registrars/Consultants• Benefits for p<strong>at</strong>ients• Roles <strong>at</strong> <strong>handover</strong>• Involvement of nursingThese videos are available to be viewed <strong>at</strong> http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>A DVD of <strong>all</strong> video vignettes is also available on requestvia: HSPIB@doh.health.nsw.gov.auISBAR video vignettes(Developed by Hunter and New England Health Service)5 vignettes th<strong>at</strong> show how the ISBAR communic<strong>at</strong>ionframework can help clinicians communic<strong>at</strong>e the keymessages of <strong>clinical</strong> care effectively and quickly:http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>Safe Clinical Handover –implement<strong>at</strong>ion support CDImplement<strong>at</strong>ion support CD th<strong>at</strong> includes standardPowerPoint present<strong>at</strong>ions, video vignette resources andtoolkit resources. Copies can be requested via email <strong>at</strong>:HSPIB@doh.health.nsw.gov.aue-Learning links to assistwith <strong>clinical</strong> <strong>handover</strong>http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>GEM pl<strong>at</strong>form“Clinical Handover Implementing Change” and projectmanagement modules – will assist you with the processof reviewing and redesigning local <strong>clinical</strong> <strong>handover</strong>.All NSW Health employees can register on this websiteusing their NSW Health email address.https://gem.workstar.com.auBetween the Flags – DETECT Training(Authors: K Fraser, M Berry and A Pile, DETECT Manual1st Edition 2009)http://www.cec.health.nsw.gov.au/programs/between-the-flags.htmlhttp://nswhealth.moodle.com.auUniversity of QueenslandThe University of Queensland has developed an onlinecourse in <strong>clinical</strong> <strong>handover</strong> as part of the AustralianCommission on Safety and Quality in Health Care:N<strong>at</strong>ional Clinical Handover Initi<strong>at</strong>ive.http://www.uqhealthinsitu.com.au/products/ACSQHC8300/ACSQHC8300_brochure.cfmNSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 25
Appendix GPrevoc<strong>at</strong>ional Training Networks in New South Waleshttp://www.imet.health.nsw.gov.au/www/472/1001127/displayarticle/1005452.htmlNetwork1234567891011HospitalsBalmain HospitalDubbo Base HospitalRoyal Prince Alfred HospitalBankstown-Lidcombe HospitalsCampbelltown Camden Hospital*Broken Hill Base Hospital (PGY2 only)Canterbury HospitalConcord Rep<strong>at</strong>ri<strong>at</strong>ion GeneralHospital*Fairfield Hospital*Liverpool Public HospitalThe Tweed HospitalPort Macquarie Base HospitalRoyal North Shore HospitalRyde District HospitalHornsby Ku-ring-gai Health ServiceManly HospitalMona Vale HospitalGosford District Hospital*Wyong HospitalAlbury Base HospitalGriffith Base HospitalSt George Hospital andCommunity Health Service*Sutherland HospitalCalvary Kogarah HospitalLismore Base HospitalThe Prince of Wales Hospital*Gundagai General Practice ServicePGY2 onlySt Vincent’s HospitalWagga Wagga Base Hospital &Community H. S.Shellharbour HospitalShoalhaven District Memorial HospitalWollongong Hospital*Bulli HospitalPort Kembla HospitalColedale HospitalAccredit<strong>at</strong>ionst<strong>at</strong>usRT5T5T5T3^RT3T5T3T5T3T5T5T3T5T3^T3^T5T3T3RT5T3RT5T5GPT5T5T3RT5RRRNetworkKey12131415HospitalsArmidale Rural Referral Hospital(PGY2 only)Belmont District HospitalCalvary M<strong>at</strong>er NewcastleJames Fletcher HospitalJohn Hunter HospitalThe Maitland HospitalManning Rural Referral HospitalRoyal Newcastle CentreTamworth Rural Referral HospitalNorthwest General Practice(PGY2 only)Auburn HospitalB<strong>at</strong>hurst Base HospitalBlacktown Hospital/Mt Druitt HospitalThe Children’s Hospital <strong>at</strong> Westmead(PGY2 only)Coffs Harbour Health CampusOrange Base HospitalWestmead HospitalHawkesbury District Health ServiceNepean HospitalBega District Hospital (PGY2 only)Calvary Health Care ACTThe Canberra HospitalGoulburn Base HospitalIsabella Plains Medical CentreInterchange General PracticeAccredit<strong>at</strong>ionst<strong>at</strong>usRT3T3^RT5T3T3T3T5GPRRT3RT5T5T5T3T5RT3T5RGPGP* May contain terms <strong>at</strong> other sites not listed in the NetworksT3 3 Term Home HospitalT5 5 Term Home HospitalR Rot<strong>at</strong>ion HospitalGP PGPPP pilot, GP service^ Requesting to become 5 Term Home Hospital26 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
Useful referencesThe <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> toolkit has not sought toreinvent the wheel, but r<strong>at</strong>her channel work from existingsources into one place th<strong>at</strong> provides a <strong>JMO</strong> specificcontext to <strong>clinical</strong> <strong>handover</strong> improvement.Each of the references listed below has its own detailedlisted of references and can be accessed on demand.1. Australian Commission on Safety and Quality in HealthCare (2010). The OSSIE Guide to Clinical HandoverImprovement. Sydney, ACSQHCwww.safetyandquality.gov.au/internet/safety/publishing.nsf/Content/PriorityProgram-058. JM Farnan, JAM Paro, RM Rodriguez, ST Reddy, LHorwitz, JK Johnson, VM Arora. Hand-off Educ<strong>at</strong>ionand Evalu<strong>at</strong>ion: Piloting the Observed Simul<strong>at</strong>ed HandoffExperience (OSHE). Journal of General InternalMedicine, DOI 10.1007/s11606-009-1170-y. November19, 2009.http://www.springerlink.com/content/n4m37g374355q4r2/9. NSW Department of Health (2009). Policy Directive,Clinical Handover: Standard Key Principles(PD2009_060). Sydney, NSW DoH.www.archi.net.au/e-library/<strong>clinical</strong>/nsw-<strong>handover</strong>2. Australian Commission on Safety and Quality in HealthCare. N<strong>at</strong>ional Clinical Handover Initi<strong>at</strong>ive.www.safetyandquality.gov.au/internet/safety/publishing.nsf/Content/PriorityProgram-0510. NSW Department of Health (2009). Implement<strong>at</strong>ionToolkit: Standard Key Principles for Clinical Handover.Sydney, NSW DoH.www.archi.net.au/e-library/<strong>clinical</strong>/nsw-<strong>handover</strong>3. Australian Medical Associ<strong>at</strong>ion (2006). Safe Handover :Safe P<strong>at</strong>ients. Kingston, AMA.www.ama.com.au/node/40644. B<strong>at</strong>alden et al (2002). General Competencies andAccredit<strong>at</strong>ion in Gradu<strong>at</strong>e Medical Educ<strong>at</strong>ion. HealthAffairs, vol 21(5): pp103-11)5. Clinical Excellence Commission (2010). Quality SystemsAssessment: 2009 <strong>clinical</strong> <strong>handover</strong> d<strong>at</strong>a. Sydney, CEC.http://www.cec.health.nsw.gov.au/programs/qsa.html6. Clinical Excellence Commission (2010). Between theFlags Program.http://www.cec.health.nsw.gov.au/programs/between-the-flags.html7.Hunter and New England Area Health Service (2009).ISBAR revisited: Identifying and Solving BARriers toeffective <strong>clinical</strong> <strong>handover</strong> - Project toolkitwww.safetyandquality.gov.au/internet/safety/publishing.nsf/Content/PriorityProgram-05_ISBAR11. NSW Department of Health (2009). Standard KeyPrinciples for Clinical Handover: Implementing Change– Templ<strong>at</strong>es. Sydney, NSW DoH.www.archi.net.au/e-library/<strong>clinical</strong>/nsw-<strong>handover</strong>12. NSW Department of Health commissioned liter<strong>at</strong>urereview (2010). “Best Practices for Physician Handoffs”.The Advisory Board Company. Washington, DC.www.archi.net.au/e-library/<strong>clinical</strong>/nsw-<strong>handover</strong>13. Tomas. M.J.W., Pirone CJ, Turner P (2009). A Guidefor the Safe Use of Electronic Clinical Handover Tools,South Australian Department of Health, Adelaide, SA.www.safetyandquality.gov.au/internet/safety/publishing.nsf/Content/PriorityProgram-0514. Wong et al. “A Structured Evidence-based Liter<strong>at</strong>ureReview regarding the Effectiveness of ImprovementInterventions in Clinical Handover” – AustralianCommission on Safety and Quality in Health Care,April 2008www.safetyandquality.gov.au/internet/safety/publishing.nsf/Content/PriorityProgram-05NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 27
AcknowledgementsThe <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> project has progressed frominiti<strong>at</strong>ion to implement<strong>at</strong>ion with significant energy froma large number of clinicians and managers within thehealth system.A Core Work Group was responsible forthe intense activity required to developthe toolkit and templ<strong>at</strong>es associ<strong>at</strong>edwith the <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> project.The Acute Care Taskforce acknowledge the work ofthe Health Service Performance Improvement Branchin the program management for the <strong>JMO</strong> <strong>shift</strong> change<strong>clinical</strong> <strong>handover</strong> project and further thank those whohave directly contributed and collabor<strong>at</strong>ed on thisimportant project.The <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> projecthas benefited from alignment andcollabor<strong>at</strong>ion with existing healthstr<strong>at</strong>egies and <strong>clinical</strong> <strong>handover</strong> guides.• The Australian Commission on Safety and Quality inHealth Care – N<strong>at</strong>ional Clinical Handover Initi<strong>at</strong>ive• The Australian Commission on Safety and Qualityin Health Care – OSSIE Guide to <strong>clinical</strong> <strong>handover</strong>improvement (2010)• The Australian Medical Associ<strong>at</strong>ion – Safe Handover:Safe P<strong>at</strong>ients Guide (2006)• Hunter and New England Area Health Service – ISBARcommunic<strong>at</strong>ion framework str<strong>at</strong>egy• The Clinical Excellence Commission – Between theFlags program: recognition and management of thedeterior<strong>at</strong>ing p<strong>at</strong>ient• Clinical Educ<strong>at</strong>ion and Training Institute (formerlyIMET) – <strong>JMO</strong> Forum.Core Work Group• IMET – <strong>JMO</strong> forum represent<strong>at</strong>ives (x7)– Dr Hamish Dunn (Hornsby, Manly, Mona Vale)– Dr Penelope Aligiannis (Bankstown)– Dr Joanna Dargan (John Hunter, Maitland, Belmont,M<strong>at</strong>er, Taree, Armidale, Tamworth)– Dr Lucy Cho (Wollongong, Bulli, Port Kembla,Shoalhaven, Shellharbour, Nowra)– Dr Christine Velayuthen (St Vincents, Wagga)– Dr Pip Bunting (Wagga Wagga)– Dr K<strong>at</strong>elyn Priester (Albury, St George)• Prof Jeremy Wilson (Co-Chair Acute Care Taskforce,Professor of Medicine, Clinical Associ<strong>at</strong>e Dean, UNSWSWS Clinical School)• Ms Vicki Manning (Co-Chair Acute Care Taskforce,DON&M, St George Hospital)• Dr Annette Pantle (Acute Care Taskforce member,Clinical Excellence Commission)• Dr Kim Hill (Acute Care Taskforce member, DirectorClinical Governance, HNEAHS)• Prof Julie Johnson (Acute Care Taskforce member,Associ<strong>at</strong>e Professor and Deputy Director, Centre forClinical Governance Research, Faculty of Medicine,UNSW)• Dr Michele Harris (DMS, Sutherland Hospital)• Dr William Lancashire (Director, ICU, Port MacquarieHospital, Rural Health Priority Taskforce member)• Mr Ian Richards (<strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> project office• The Health Service Performance Improvement Branch –program management.28 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
The Acute Care Taskforce tested <strong>all</strong>outputs of the Core Work Group broadlythrough clinicians, managers andexecutive members of the NSW Healthsystem and associ<strong>at</strong>ed health agencies.The time spent and depth of critiqueprovided by diverse members ofthe health system has added to thestrength of the final <strong>JMO</strong> <strong>clinical</strong><strong>handover</strong> str<strong>at</strong>egy.Organis<strong>at</strong>ions, Committees and Groups who wereconsulted in the testing of project document<strong>at</strong>ionand str<strong>at</strong>egy.NSW Health Services• The Children’s Hospital <strong>at</strong> Westmead• Gre<strong>at</strong>er Southern Area Health Service• Gre<strong>at</strong>er Western Area Health Service• Hunter and New England Area Health Service• North Coast Area Health Service• Northern Sydney and Central Coast Area Health Service• South Eastern Sydney and Illawarra Area Health Service• Sydney South West Area Health Service• Sydney West Area Health Service.NSW Department of Health Branches• Health Service Performance Improvement Branch• Rostering Centre of Excellence• Clinical Safety, Quality and Governance Branch• Nursing and Midwifery Office• Workforce Development and Innov<strong>at</strong>ion Branch.Rel<strong>at</strong>ed Health Agencies• Australian Commission on Safety and Quality inHealth Care• Australian Medical Associ<strong>at</strong>ion, Council of Doctorsin Training.<strong>JMO</strong> Clinical Handover ConceptTesting Facilities• Campbelltown Hospital• Dubbo Base Hospital• John Hunter Hospital• Prince of Wales Hospital• Sutherland Hospital• Wagga Wagga Base Hospital.NSW Health Agencies• Agency of Clinical Innov<strong>at</strong>ion• Clinical Educ<strong>at</strong>ion and Training Institute (formerly IMET)• Clinical Excellence Commission.NSW Health Priority Taskforces• Ministerial Taskforce for Emergency Care• Surgical Services Taskforce• Rural Health Priority Taskforce• Intensive Care Taskforce.NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit 29
The Acute Care Taskforce is amulti-disciplinary taskforcereporting to the Director Generalof NSW Health.• Dr Kim Hill (Director Clinical Governance, HNEAHS)• Mr Kim Nguyen(Allied Health Manager, Gre<strong>at</strong>er Newcastle Cluster,HNEAHS)Acute Care Taskforce MembershipAcute Care Taskforce (ACT)• Prof Jeremy Wilson Co-chair(Professor of Medicine, Clinical Associ<strong>at</strong>e Dean,UNSW SWS Clinical School)• Ms Vicki Manning Co-chair(DON&M, St George Hospital)• Mr M<strong>at</strong>thew Lutze(Nurse Practitioner, Canterbury Hospital)• Mr Nicholas Marlow(Area Manager Acute/Post Acute Care (APAC) NSCCHAcute Care Taskforce)• A/Prof Paul Middleton(Director, Ambulance Research Institute Senior MedicalAdviser, Ambulance Service of NSW)• Ms Amanda Larkin(General Manager, Campbelltown and CamdenHospitals)• Mr Raj Verma(Director, Health Service Performance ImprovementBranch)• Dr Anett Wegerhoff (GP, Camden)• Mr Bill McKennariey(Consumer Represent<strong>at</strong>ive, Tweed Heads)• Ms Clare Quinn (Manager Speech P<strong>at</strong>hology,Prince Of Wales Hospital)• A/Prof Stephen Wilson(Director - Popul<strong>at</strong>ion Health ProgramSt Vincent’s Hospital)• Prof Teng Liaw(Director, General Practice Unit, Liverpool Hospital,SSWAHS)• A/Prof Debra Thoms(Chief Nursing Officer, Nursing and Midwifery Office)• Ms Helen Eccles(DON&M, Manly and Mona Vale Hospitals)• Prof Julie Johnson(Associ<strong>at</strong>e Professor and Deputy Director, Centre forClinical Governance Research, Faculty of Medicine, UNSW)• Ms Karen Lenihan (Area DON&M, GSAHS)• Ms K<strong>at</strong>harine Szitniak(DON&M, Royal Prince Alfred Hospital)Now resigned• Dr Jacqui Close(Staff Specialist, Geri<strong>at</strong>rician <strong>at</strong> Prince of Wales Hospital)• Dr Annette Pantle(Director, Clinical Improvement, Clinical ExcellenceCommission)• A/Prof Christopher Poulos(Network Clinical Director Southern Hospitals Network,SESIAHS)Thank you.30 NSW Health <strong>Improving</strong> <strong>JMO</strong> <strong>clinical</strong> <strong>handover</strong> – Implement<strong>at</strong>ion Toolkit
This document can also be downloaded <strong>at</strong>http://www.archi.net.au/e-library/safety/<strong>clinical</strong>/nsw-<strong>handover</strong>
SHPN (HSPI) 100536