Infection Prevention and Control Best Practices - College ...
Infection Prevention and Control Best Practices - College ...
Infection Prevention and Control Best Practices - College ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
INFECTION PREVENTION AND CONTROL BEST PRACTICES<br />
FOR LONG TERM CARE AND COMMUNITY CARE INCLUDING HEALTH CARE OFFICES AND AMBULATORY CLINICS<br />
Liquid waste such as urine, feces, provodine iodine, irrigating solutions, suctioned fluids, excretions <strong>and</strong><br />
secretions may be poured carefully down the client’s toilet, which is connected to a sanitary sewer or septic<br />
tank. Body fluids in small amounts such as blood in a syringe withdrawn from a CVAD before a blood<br />
sample is obtained may be discarded in a puncture proof sharps container. Provincial <strong>and</strong> territorial regulations<br />
may dictate the maximum volume of blood or body fluids that is permitted to be poured in the sanitary<br />
sewer (e.g. 300mls). If there is likely to be splashes or sprays from disposing of blood or body fluids, apply<br />
PPE.<br />
h. Healthy Workplace – Keeping your staff <strong>and</strong> clients safe<br />
All staff working in health care should have a two-step tubercline skin test at the beginning of employment<br />
unless they have documentation of a negative skin test in the past 12 months. The local Medical Officer of<br />
Health can advise on the need for routine testing depending on the prevalence of Tuberculosis in your<br />
community. Health care providers need to know their history of childhood communicable diseases.<br />
Organizations should commit to promoting vaccine preventable diseases. Documentation of immune status<br />
will be considered when assigning a health care provider to a particular case.<br />
For additional information, please review Health Canada’s Canadian Immunization Guideline at: http://<br />
www.phac-aspc.gc.ca/publicat/cig-gci/pdf/cdn_immuniz_guide-2002-6.pdf.<br />
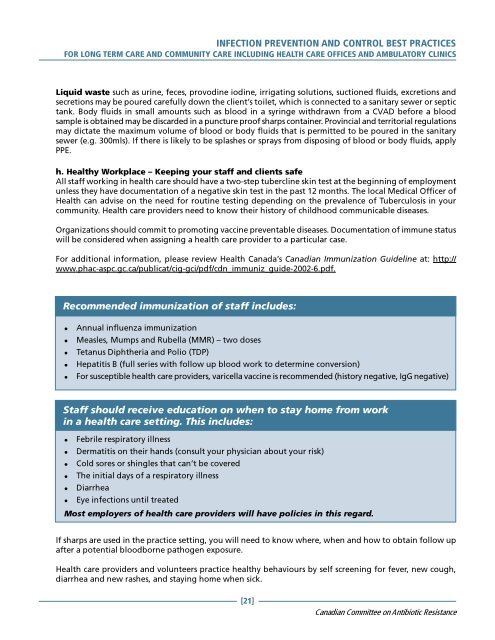
Recommended immunization of staff includes:<br />
� Annual influenza immunization<br />
� Measles, Mumps <strong>and</strong> Rubella (MMR) – two doses<br />
� Tetanus Diphtheria <strong>and</strong> Polio (TDP)<br />
� Hepatitis B (full series with follow up blood work to determine conversion)<br />
� For susceptible health care providers, varicella vaccine is recommended (history negative, IgG negative)<br />
Staff should receive education on when to stay home from work<br />
in a health care setting. This includes:<br />
� Febrile respiratory illness<br />
� Dermatitis on their h<strong>and</strong>s (consult your physician about your risk)<br />
� Cold sores or shingles that can’t be covered<br />
� The initial days of a respiratory illness<br />
� Diarrhea<br />
� Eye infections until treated<br />
Most employers of health care providers will have policies in this regard.<br />
If sharps are used in the practice setting, you will need to know where, when <strong>and</strong> how to obtain follow up<br />
after a potential bloodborne pathogen exposure.<br />
Health care providers <strong>and</strong> volunteers practice healthy behaviours by self screening for fever, new cough,<br />
diarrhea <strong>and</strong> new rashes, <strong>and</strong> staying home when sick.<br />
[21]<br />
Canadian Committee on Antibiotic Resistance