2011 July - December - nuhcs
2011 July - December - nuhcs
2011 July - December - nuhcs
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
in this issue02 (Clinical Vignettes)04 Hybrid OT for EndovascularSurgeryA/Prof Tan Huay Cheem08 Work & Experience at NUHCS09 What is Optical CoherenceTomography?10 MOH Overseas Expert in VascularSurgery/Limb Preservation:It Takes a Whole Village To DoLimb Salvage12 Cardiac Family Day <strong>2011</strong>14 GP Symposium <strong>2011</strong>16 My Fellowship Days at NUHCS:17 ESC <strong>2011</strong>Objects in The Rear Mirror18 Singapore’s First AntithromboticPharmacotherapeutics Symposium20 Division of Thoraic Surgery:The New Division within NUHCS21 Happenings23 Publications26 Abstracts28 Directory, New Doctors &Congrats!EditorA/Prof Poh Kian KeongAdvisorA/Prof Tan Huay CheemContents are not to be reproducedwithout the written permission of NUHCSIt was on a wet stormy afternoon on 12 Nov <strong>2011</strong>, NationalUniversity Heart Centre, Singapore (NUHCS) hosted its inauguralpublic chinese symposium, “ 健 康 心 脏 , 健 康 生 活 ” at the newauditorium of the National University Health System (NUHS) TowerBlock. The 300 tickets catered were long sold out before the eventbut it did not stop another 80 people from braving the rain in turningup. They had to be housed in an adjacent room to the auditorium withlive audio and video feed.The audience were certainly not disappointed as they were treatedto a lively presentation of current cardiovascular topics of “Women andHeart Disease”, “Palpitation-Harbinger of Sudden Cardiac Death?”,“Coronary Stenting – Past, Present and Future” and “Coronary ArteryBypass and Valve Surgery Update”. All 4 speakers, Dr Raymond Wong,Dr Lim Toon Wei, Dr Jimmy Hon and Assoc Professor Tan Huay Cheemwere able to fully engage the audience with their fluent Mandarin andmultimedia presentation.The event was also supported by the Singapore Heart Foundationwhich conducted cardiopulmonary resuscitation (CPR) demonstrationand provided CPR training kits and educational pamphlets to theattendees.Assoc Prof Tan Huay Cheem, Director of NUHCS, also launchedhis Chinese book, “ ” or “Clinical Vignettes”, which containsall the articles that he had published in his regular column in the localChinese newspaper of LianHe ZaoBao for the last 4 years. All 300copies of his book were sold out with Assoc Prof Tan autographing formany at the end of the symposium.At the end of the afternoon, a total sum of about $5000 was raisedand donated to the NUH Patientcare Charity Fund.NUHCS PULSE | 2
(ClinicalVignettes)A total sum ofabout $5000 wasraised and donated tothe NUH PatientcareCharity Fund.NUHCS PULSE | 3
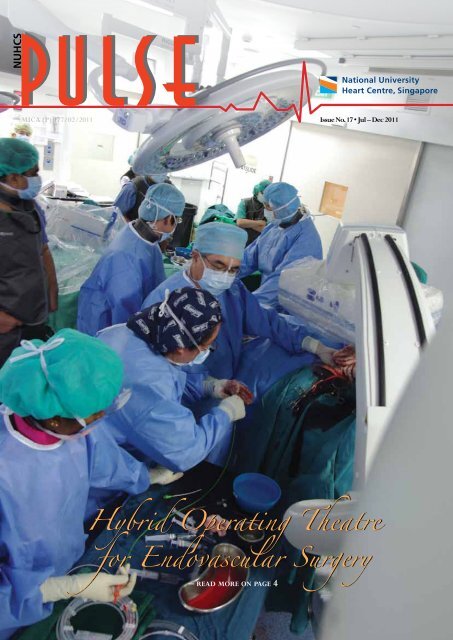
Fortunately modern and available treatments for heart andvascular disease have resulted in improved survival and quality oflife. Great leaps in open cardiovascular surgery and cardio vascularinterventions have been made in parallel over the last 50 years.These include open heart surgery with cardiopulmonary bypass,heart valve replacement, coronary stenting, drug eluting stentsand endovascular aortic aneurysm repair. Some of these areas willbe covered further in this issue.Recently there has been convergence of these interventionstowards hybrid procedures that afford a minimally invasiveapproach by a combination of surgical operations with preciseimaging and endovascular techniques. Some examples are in theevolution of hybrid coronary revascularization, trans-catheteraortic valve implantation, endovascular aortic surgery andendovascular intervention for limb salvage. Several factors drivingthis convergence are an aging patient population, improved devicetechnology and better imaging. Patients with cardiovascular diseaserequiring treatment are increasingly elderly and consequently havesignificant morbidities and therefore tolerate these less invasiveoperations much better. Moreover the proportion of emergencyand complex cases that can be treated by a hybrid approach areincreasing. Device technology and imaging continue to evolverapidly. Endovascular devices can now be customized for diseasespecific anatomy and delivered in smaller systems. The needfor precision through better imaging will be paramount. Thesepatients are now best served by aminimimally invasive procedurein a safe and sterile environmentwith full anaesthetic supportand monitoring. A “Hybrid”operating room combines all thefeatures of a standard operatingroom with state of the artimaging. It’s a glimpse into thefuture of surgery and sets a newstandard of care for patients with cardiovascular disease.Multidisciplinary teams have also evolved to perform theseprocedures in a hybrid Operating Theatre (OT) environment withexcellent angiographic imaging with digital subtraction and 3-Dimaging for planning and navigation. At NUHCS these complexprocedures are performed by multidisciplinary teams comprisingcardiac and vascular surgeons, interventional cardiologists andradiologists as well as anaesthetists. The ideal hybrid OT shouldbe configured for flexible and ample working space with a fixedimaging system, a floating radiolucent OT table, laminar airflowenvironment for sterility and full anaesthetic support with heartlung bypass capability.The newly built hybrid cardiovascular OT at NUHCS featuresa state of the art Siemens Artis Zeego angiographic system. TheSiemens Artis Zeego, is a multi-axis system based on robotictechnology that can be positioned any way the operator wants andprovides cross-sectional, large volume 3D imaging comparableto that of a traditional CT scanner. The Artis Zeego’s roboticC-arm “senses” the location of the operating table, giving surgeonsextraordinary flexibility to manoeuvre the imaging system atalmost every angle without moving the patient. As a result, internalorgans and vessels can be seen from a “fly around” perspectivein three dimensions, in great detail. This enables the surgeon toperform precise imaging in 2-D or 3-D on any part of the bodyin real time during surgery with optimal safety. The angiographicsystem is fully integrated with other imaging systems at NUHCS,so that the patients CT and MRI scans as well as live ultrasoundimaging of the heart or great vessels can be viewed on the largeHigh Definition LED operating screen. “CT like imaging” andintravascular ultrasound imaging can all be done in the sameroom while complex surgery is being performed. This improvesthe precision and safety in which these operations can be doneand allows us to combine procedures that previously had to bedone in a staged manner in two places. Without ever leaving theoperating theatre, the surgical team can use ultrasound, CT andangiography technologiesThe Hybrid OT also opens up doorsto new procedures, such as branchedendografts for thoracoabdominalaneurysms and percutaneous heart valverepair, for which imaging is crucial.during a stent graft surgeryto treat a patient’s leakingabdominal aortic aneurysm.The Hybrid OT now bringsinto the operating theatremany imaging technologiespreviously only available inimaging suites outside theOT. This will benefit manypatients who can have imaging and treatment in one setting, wheremultiple trips were required in the past. Patients who require acoronary stent and then heart valve repair, for example, previouslyneeded to have the stent inserted in the Cardiac CatheterizationLab and valve repair subsequently in the OT. Patients with diseasein the coronary arteries, heart valves, aorta as the peripheral bloodvessels may now benefit from minimally invasive procedures inthis hybrid OT suite. The Hybrid OT also opens up doors to newprocedures, such as branched endografts for thoracoabdominalaneurysms and percutaneous heart valve repair, for which imagingNUHCS PULSE | 5
The “Hybrid” operating theatre at NUHCS combinesall the features of a standard operating room with state of the art imaging.It’s a glimpse into the future of surgery and sets a new standard of carefor patients with cardiovascular disease.is crucial.HYBRID CORONARY REVASCULARIZATION ( Minimallyinvasive CABG and coronary artery stent placement)The minimally invasive CABG procedure uses robotic-assistedtechniques that allow surgery to be performed using smallincisions between the ribs rather than through a midline incisiondividing the sternum. The hybrid CABG involves a LIMA graftto LAD performed robotically by a surgeon followed by stentingof the other coronary arteries by an interventional cardiologist.Recovery from robotic assisted CABG is shorter and may beassociated with fewer complications. Most patients are able to leavethe hospital within three to four days and return to full activity,including work, in two to three weeks, rather than the two-monthrecovery generally required following traditional CABG. Whiletraditional CABG remains the first-line treatment for multiple,severe coronary blockages, the hybrid procedure is appropriatefor patients with LAD disease and one or two other blockages thatcan be treated with stents. Hybrid coronary revascularization hasbeen shown to be a durable, safe and effective option for carefullyselected patients, but more data are needed to assess long-termoutcomes and determine which patients are most appropriate forthe procedure.AORTIC DISEASEEndovascular aortic aneurysm repair (EVAR) involves theplacement of a covered stent within the enlarged aortic aneurysmsac to exclude blood flow and prevent fatal rupture. Unlike standardopen surgery, in which a large incision is made, endovascularaortic repair can be done percutaneously. Newer adaptations ofstandard EVAR are the Hybrid EVAR, fenestrated or branchedNUHCS PULSE | 6
The “Hybrid” operating theatre at NUHCS combines all the features of astandard operating room with state of the art imaging.EVAR and Chimney EVAR. A hybrid procedure aims to combineendovascular procedures with limited open surgery. The stent graftdeployment is performed in combination with an open operationto revascularise selected arteries that will be “covered” by the stentgraft i.e. deprived of arterial inflow. In this method more extensiveEVAR devices can be deployed to treat the primary lesion whilepreserving arterial flow to critical arteries.Thoraco-abdominal aneurysms (TAA) typically involvesuch vessels and deployment of the EVAR device will coverimportant arteries e.g. visceral or renal arteries, resulting inend organ ischaemia which may be critical. The open operationcomponent aims to bring a bypass graft from an artery outsidethe stent graft coverage to vital arteries within the coverageregion. This component adds to the EVAR procedure in time andrisk but is usually judged to be a lesser risk than the traditionalopen thoracoabdominal operation. Another common example isrevascularisation of the left common carotid artery and/or the leftsubclavian artery from the innominate artery or the right commoncarotid artery to allow treatment of a distal arch thoracic aneurysm.Continued design improvement in stent graft including branchedendografts will reduce but not eliminate this type of surgery.“Chimney stents” into the carotid artery with TEVAR intothe proximal aortic arch have recently been described. All suchhybrid procedures aim to reduce the morbidity and mortality oftreating aortic disease in a patient population that is increasinglyolder and less fit than when major open repairs were developedand popularised. Even then, significant risks were accepted in theunderstanding that the large open operation was the only option.Now with hybrid EVAR performed in hybrid OTs, these complexprocedures can be done with much lower risks. The trade off beingthat durability and problems such as ‘endoleaks’ require carefulsurveillance.The Hybrid OR also promises to improve care in lifethreateningemergencies such as aortic dissection or transection.TRANSCATHETER (APICAL / FEMORAL) AORTICVALVE IMPLANTATIONThe transcatheter aortic heart valve integrates balloon-expandablestent technology with a replacement tissue heart valve. NUHCSis one of the few centres in Asia to perform percutaneoustranscatheter aortic valve replacement. During the procedure, acatheter is advanced to the aortic valve, either through the femoralartery or through a small chest incision and through the leftventricle. Once the catheter is in place, a tissue valve with a metalstent scaffolding is positioned and deployed. Flouroscopic guidanceprovides real time visualization. The force of the expanding stentanchors the new valve in place, completely avoiding the needfor sutures, cardiopulmonary bypass, open surgery—and theirassociated effects.ENDOVASCULAR LIMB SALVAGERest pain, tissue loss, and gangrene are manifestations of criticallimb ischemia caused by peripheral arterial disease and define apatient subgroup at highest risk for major limb amputation. Thediagnosis of critical limb ischemia mandates prompt medical andsurgical management to achieve the best chance of limb salvage.Surgical intervention has evolved from primary amputation toopen bypass to the present era of endovascular therapy. The goals ofsurgical bypass and endovascular therapy are to improve perfusionsufficiently to permit healing. Endovascular therapy has beenshown in multiple retrospective studies to achieve limb salvagesimilar to open bypass. AT NUHCS, we are able to achieve a 75%twelve month amputation free survival using an endovascular firstapproach in patients presenting with critical limb ischaemia. Closeclinical surveillance and serial monitoring of limb perfusion bymeans of noninvasive arterial studies are needed to determine theneed for further vascular intervention. Limb salvage patients sufferfrom multiple comorbidities and benefit from a minimally invasiveand multidisciplinary, team approach to care.Combining traditional operations with angiographic imagingtechnology in the same suite promises to transform the care ofpatients, with improved safety and outcomes, while stimulatinginnovation. What previously involved two separate procedurescan now be done in one. When the best approach for a patientinvolves a combination of coronary artery bypass and stenting,by performing both at the same time, we can reduce the stress ofsurgery and improve recovery time. The imaging technology canalso be used after a standard bypass to ensure the bypass graft isproviding adequate blood flow to the heart. Published research hasshown that this approach can reduce the number of complications.All of these imaging technologies are coordinated andpresented to the surgeon through a state of the art large displayLED monitor—an 8Megapixel high definition screen that displayspatient medical information along with reference and live imagesin the OT. The system also allows for videoconferencing in thehospital and permits broadcast of live video for teaching purposes.In conclusion, the potential is for improved patient outcomesand safety is huge, its utilization synergistic and its reachmultidisciplinary. The “Hybrid” operating theatre at NUHCScombines all the features of a standard operating room with stateof the art imaging. It’s a glimpse into the future of surgery and setsa new standard of care for patients with cardiovascular disease.NUHCS PULSE | 7
Work &Experience at NUHCSDr. Eliana C. MartinezMD, PhDTime goes by very fast and in the blink ofan eye, five years have passed since I joinedthe National University of Singapore (NUS)and the National University Heart Centre,Singapore (NUHCS). A few passions of minewere combined through the opportunity tomove to Singapore: search for knowledge,exposure to multicultural environments, andpersonal development. Also, another reasonmotivated me to join the team that wouldstart-up a basic research laboratory underthe mentorship of A/Professor TheodorosKofidis at the NUHCS’ Department ofCardiothoracic and Vascular Surgery (CTVS).And this reason was my wish to take mycareer up to the next level.As a Colombian medical doctor, I hadaccomplished research post-doctoral trainings at StanfordUniversity (USA) and Hannover Medical School (Germany),moving to Singapore has been quite a fascinating and enrichingexperience. Besides, this has definitely been a good move formy scientific career as the country is a vibrant research hub inbiomedical sciences, with plenty of opportunities to acquirefunding and interact with other scientists and clinicians fromvarious disciplines and institutions. I have also been fortunate toalways count on the support from my boss, Professor Lee ChuenNeng, Head of Dept of CTVS, who has provided me with the trust,and independence I needed as a young researcher. Thanks to thissupport, I also had the exceptional opportunity to pursue a PhDdegree at NUS concomitantly to my work as a Research Fellow.Starting-up a new lab was not easy, but the learning experiencewas invaluable. A/Prof Kofidis’ Myocardial Restoration Lab wasup and running by mid-2007, and soon after, I got the chance toobtain my own funds through an NMRC/New Investigator GrantAward in 2008. This provided me a great foundation to furtherdevelop independent scientific reasoning.In the past five years, my research has been focused on thedevelopment of pre-clinical projects with translational potentialaiming at enhancing the angiogenic potential of tissue-engineeredgrafts towards improvement of cardiac performance followingmyocardial ischemia. Since <strong>July</strong> <strong>2011</strong>,I have been fortunate to have a jointappointment with the CardiovascularResearch Institute (CVRI) under thedirection of Professor Mark Richards.The NUHCS/CVRI is constituted by a multidisciplinary researchteam aimed at pursuing translational cardiovascular research,and offers me the possibility to work in an environment thatfacilitates the development of my full potential as a scientist.My future research goals within NUHCS/CTVS-CVRI involvethe development of novel therapies for heart failure throughpost-ischemic acellular regenerative strategies that will involvemodulation of paracrine signaling to promote angiogenesis andattenuate fibrosis after myocardial injury. I am interested inapproaches with realistic clinical application that can be deliveredto the patient with least morbidity and surgical complications.Furthermore, I am expanding my research scope at CVRI bygetting involved in projects aimed at a better understanding ofneuroendocrine pathways and their possible modulation throughnovel therapeutic compounds.It definitely requires dedication to perform as a young scientistabroad. Yet, my professional growth thus far would have not beenpossible without the infrastructure and opportunities provided byNUHCS, and the support from my mentors, colleagues, studentsand collaborators. I am very much looking forward to my upcomingyears in NUHCS, in the hope that all our combined efforts willproduce science with high clinical impact.NUHCS PULSE | 8
What isOptical CoherenceTomography?A/Prof Ronald LeeSince its inception 25 years ago,percutaneous coronary intervention (PCI)has gained widespread acceptance, andcoronary stent implantation has become thestandard revascularization therapy for mostpatients with obstructive coronary arterydisease. Yet, instent restenosis and stentthrombosis are two major complicationslimiting the benefits of PCI. Although the emergence of drug-elutingstents has remarkably reduced the occurrence of instent restenosis,stent thrombosis—which is associated with high incidences of fataland non-fatal myocardial infarction—remains an unsolved problem.In fact, late stent thrombosis occurs more frequently following drugelutingstent than bare metal stent implantation. Moreover, the useof drug-eluting stents in increasingly complex lesions and multivesselcoronary artery disease implies that these complications are likely topersist and effective preventive strategy is warranted.Stand-alone X-ray angiography is the traditional imaging methodguiding PCI, and is still used in majority of the procedures nowadays.Coronary angiography depicts vessel images that are relatively simpleto comprehend, making PCI procedures easy to perform. However,stand-alone angiographic guidance has some inherent inadequacies andlimitations, which, if one fails to recognize, may result in suboptimalprocedural outcomes, as well as acute and long-term complications.Among others, angiography merely produces a planar silhouette ofthe contrast-filled lumen. The severity of the lesion can vary widelywith different X-ray projection angles. In fact, visual interpretationof angiography exhibits significant inter-observer variability andcorrelates poorly with post-mortem examination. In addition, coronaryangiography is essentially a luminography, which provides no insightto the amount, tissue composition, distribution of coronary plaque, aswell as coronary remodeling pattern. After coronary stent implantation,angiography has limited ability to assess the adequacy of stent expansionand stent strut apposition. Therefore, intravascular imaging technologyhas been widely accepted as an essential tool in complex PCI.Until recently, intravascular ultrasound (IVUS) is the onlyintravascular imaging technology available. There are severalpotential utilizations of IVUS when a coronary stenosis is detectedby angiography. As a baseline evaluation tool, IVUS providesquantitative measurement on the extent of artery lumen obstruction,enabling the operator to determine if the patient would benefitfrom revascularization therapy. Once committed for PCI, IVUSalso assists in procedural strategy and device selection. In a singlecenter study, the original revascularization strategy planned waschanged after preintervention IVUSimaging of the target lesions. Followingstent implantation, IVUS plays a crucialrole in optimizing the procedural outcomes,which in turn determines the risk of futurecomplications. IVUS optimizes outcomesthrough assessment on adequacy of stentexpansion, completeness of stent strutapposition and presence of unrecognized dissection or residual stenosis.Optical Coherence Tomography (OCT) has emerged as theintravascular imaging technology. OCT is an imaging modality thatis analogous to ultrasound imaging, but uses light instead of sound.Cross-sectional images are generated by measuring the echo timedelay and intensity of light that is reflected or back-scattered frominternal structures in tissue. Preliminary experiences with OCT imagesacquisition show the technique to be safe. OCT imaging techniquehas gained considerable adoption in many centres across Europe andJapan, and various centres have presented large series of patients imagedby OCT without major complications. Compared with conventionalIVUS, OCT offers several advantages. The resolution of OCT (10 μm)is 10 times better than that of IVUS (100-150 μm). This enables thedetection of procedural complications such as stent edge dissectionwith higher accuracy. In addition, tissue coverage of the drug-elutingstent struts, which has been proposed as a parameter predicting latestent thrombosis, can be assessed reliably by OCT. Acquisition of theimages by OCT is much faster than that of IVUS (20 seconds versus2-3 minutes). Last but not least, OCT is the only technology whichcan accurately measure coronary plaque fibrous cap thickness, whichis one of the most important characteristics underlying a vulnerableplaque. With all these advancements, OCT is perceived to the overtakeIVUS as the predominant intravascular imaging technology in moderncardiac catheterization laboratory.In order for the interventional cardiology team to acquire thenecessary skills and knowledge in this new technology, we weregranted the Academic Medicine Development Award (AMDA) forshort-term training in 2 overseas centers. I have spent four weeksat the Massachusetts General Hospital, Harvard Medical Schoolunder Professor IK Jang. Mr. Anand Kalesam and Miss JY Lee(medical technologists) have each spent 2 weeks at the Thoraxcenter,The Netherlands under Dr. Everlyn Regar. Our OCT program hasstarted since 4 months ago and a few cases of OCT imaging procedureshave been performed. It is anticipated that OCT will becomethe intravascular imaging technology of choice in our catheterizationlaboratory.NUHCS PULSE | 9
MOH Overseas Expert in Vascular Surgery/Limb Preservation 29 th Aug–2nd Sept <strong>2011</strong>“It takesa whole villageto dolimb salvage”A/Prof Peter RoblessNUHCS PULSE | 10
We had the pleasure and privilege of hosting Professor BauerE Sumpio from Yale University School of Medicine as the <strong>2011</strong>MOH Overseas Expert in Vascular Surgery from the 29 th Aug to 2 ndSept <strong>2011</strong>. Professor Bauer Sumpio is a world renowned expert andkey opinion leader in this field of lower limb preservation, havingdeveloped a multidisciplinary lower limb preservation program atthe Centre for Vascular Disease and Diabetic Limb Preservation,Yale University School of Medicine. He has published widely inthis field and has numerous publications and grants on basic scienceand clinical trial research in limb preservation.Professor Sumpio is currently the Associate Director, GraduateMedical Education and previously the Program director of theGeneral Surgery Residency program at Yale University Schoolof Medicine.He holds joint appointments in Vascular surgery andRadiology and is Chief of the Section for Vascular Surgery at YaleMedical School. Prof Sumpio is a key opinion leader in the fieldof diabetic limb salvage. He has experience in starting one of thefirst multidisciplinary programs for limb salvage in an academicmedical centre. He is a regular keynote speaker at internationalmeetings on diabetic limb salvage and has numerous publicationsin this field including national guidelines for standards of care andpractice. He has an excellent track record for academic teachinghaving run a successful research laboratory and training residentsand fellows for the last 22 yearsDuring his visit to NUHS, we arranged for him to speak to ourresidents in general surgery and the University Surgical Clusteron the development of the Yale Residency training program. Healso gave a talk on the multidisciplinary limb preservation servicespecifically protocol driven clinical pathway development and keyperformance indicators to the Dept of Medicine at NUHS and atthe Hospital Grand Round at Jurong General Hospital.He has expertise in running a successful multidisciplinary teamfor limb salvage. I had the opportunity to visit his centre in Yaleduring a team HMDP funded visit to the US in 2009 for vascularmedicine. We have since adapted some of the practices at Yale intoour own program which is in its early stages at NUHCS. Duringhis visit he did a multidisciplinary ward round at NUH. His inputswere invaluable in the assessment and management of the patientwith diabetic foot disease.He also visited SGH and JGH to meet with the vascularsurgeons and interventional radiologists looking after limb salvage.An evening dinner and talk on “Aggressive MultidisciplinaryStrategies To Salvage A Functional Foot “ was open to all thehospitals and allied healthcare.The visit was rounded off by a grand round at NUH on how “Ittakes a whole village to do limb salvage”. This was well attendedand well received. The team here learnt a lot and forged newacquaintances during his memorable visit to Singapore.NUHCS PULSE | 11
<strong>2011</strong>Cardiac Family DayDr Chan Wan XianCardiac Family Day has been an annual event when everyone inthe department spends a day out for a get together. Music, games,fun and food have been the tradition during the event. It was held atthe Resorts World Sentosa on a Saturday afternoon, 10 th September<strong>2011</strong>. With the theme of “the sun, the sand and the beach”, it wasset out to be a fun and relaxing event.Our nurses and clinic staff started coming in the late morningin preparation for their dance and song rehearsals with muchenthusiasm, looking forward to putting up a good show foreveryone. Pre-event activities started around noon time as thecrowds started to form. The grown-ups were queuing up for theirshrink caricature while the children waited for their share of theballoon sculpture and to jump on the bouncer specially rented forthe afternoont. Everyone around was engaged in some activity andthe cocktails started to flow in.With the arrival of our director of the NUHCS, A/Prof TanHuay Cheem and our head of Cardiac Department, A/Prof YeoTiong Cheng, we formally started the event. We also had thehonour of having Mr Noel Cheah, the COO of the NUHS join usin our Cardiac Family Day this year. Our host was Chubby fromShowbiz Production who started the event with the familiar tuneof the Hawaii 5 O and got everyone up from their seats. Thesumptuous international buffet lunch started shortly after.As the crowd settled into desserts, we started our programmefor the afternoon with mass games. The childhood game of scissors,paper, stone which every adult was familiar with but it was thechildren who won the game in the end. We also had the game ofpassing the parcel (with a twist) and a dancing competition. Adancing competition with the dancers blindfolded, from which wediscovered talented dancing queens and kings amongst us. Afterthat, we had our talented staff from the CCU, heart clinics, ward 56and 63 who displayed their musicality with song and dance items.And of course, our registrars and residents who surprised us withtheir skit of X-men reunited and together with Prof Ronald Lee,they saved Professor X from an acute coronary event. : )Following that was the magic show by Kiki Tay, a well-knownSingaporean magician, which wowed both kids and adults. Near theend of the event was a pageant in which we found beautiful ladiesNUHCS PULSE | 12
and handsome men from among our colleagues. And then was themass dance to the tune of YMCA which really had everyone inthe crowd joined in dancing, including babies. The event came toan end with our annual Cardiac Family photo taking and a luckydraw with more than attractive prizes.On behalf of the department, I would like to thank ourdirector, A/Prof Tan Huay Cheem and our head of department,A/Prof Yeo Tiong Cheng for being really supportive throughoutthe organisation of this event. And our ladies in the organisingcommittee, Christina, Mullai, Sze Hwee and Wendy, a big thankyou for all the effort that you have put in, without which the eventwould not have been possible.It was the sincere wish of our organising committee thateveryone present would have an enjoyable and memorable daywhen we started planning the event. Hope you all had a memorableCardiac Family Day <strong>2011</strong>!NUHCS PULSE | 13
GP Symposium<strong>2011</strong>It was NUHCS’ inaugural GP Symposium for Cardiologyon the 8 th of October <strong>2011</strong>. Hosted at the NUHS Tower BlockAuditorium, the symposium brought together three of ourdistinguished cardiologists speakers.The afternoon started with a scrumptious buffet lunch cateredspecially for our GP partners. During lunch, our cardiologistsmingled and interacted with the GPs present. As 2pm drew near,the GPs proceeded to the auditorium and waited for the speakersto begin.Chaired by A/Prof Poh Kian Keong, 3 of our cardiologistsspoke about the following topics:• A/Prof James Yip – Diagnosis of Heart Disease withMultislice CT: Which patients should I send for CTcoronay angiography?• A/Prof Adrian Low – Medical Management ofChronic Ischemic Heart Disease• A/Prof Tan Huay Cheem – Acute Coronary SyndromeManagement: What a GP should know.The GPs were listening intently and taking notes throughoutthe symposium. They posed several questions during the Q&Asession, which was engaging and in-depth. Our cardiologist werevery well-received, and were given excellent feedback.It was a successful event, and we look forward to bringingmore symposiums for our GP Partners.Thank you!NUHCS PULSE | 14
Bioabsorbable Stent:A/Prof Tan Huay CheemOn 17 Feb <strong>2011</strong>, NUHCS carried out Singapore’s firstimplantation of a bioabsorbable stent as part of an internationalmulticentre study. Since then, another 2 patients have receivedsuccessful implantations of the same stent. All three patients arewell at 6 months of follow up. NUHCS has been identified as aCentre of Excellence for the launch of the bioabsorbable stent andwill be among the first centre in Asia to use it on a commercial basisfor her patients before the end of <strong>2011</strong>.What is the bioabsorbable stent and why is there a need forit? The coronary stent is now the default device in modern daypercutaneous coronary intervention. Unlike in conventional balloonangioplasty, the coronary stent provides a mechanical scaffoldingeffect to overcome early recoil and late vascular remodeling(vasoconstriction) of a treated coronary vessel. The currentstate-of-the-art drug-eluting stents (DES) are highly efficacious inreducing restenosis rates and the need for repeat intervention. Stentthrombosis, with its disastrous consequences, however, remains amajor limitation of DES. It may be somewhat controlled with dualantiplatelet therapy, which is usually given for at least a year afterthe procedure. But the presence of metallic material embedded inthe vessel wall may still cause chronic inflammation and result invery late stent thrombosis (occurring beyond a year). There is noadvantage for a stent to be permanently present in the artery afterit has served its initial function of scaffolding, while allowing forvascular healing and re-endothelialization to take place. In fact, themetallic stent prevents the artery from late favorable remodeling(lumen expansion) and vessel reactivity at the stented site.The motivation for the development of bioabsorbable stentswas driven by the need to solve the limitations of metallic stents,such as stent thrombosis, which requires prolonged antiplatelettherapy. The goal was to design a stent, which once bioabsorbedwould leave behind only the healed natural vessel, and allowingfor restoration of vasoreactivity with the potential for vesselremodeling. The concept is particularly attractive to young patientswho suffer from coronary artery disease but are now given theopportunity to have their arteries restored to their original stateafter treatment. Late stent thrombosis is unlikely since the stent isgone, and prolonged antiplatelet therapy would not be required.These stents can also be used for delivery of drugs that can preventneointimal hyperplasia. Bioabsorbable stents are compatible withMRI and MSCT imaging.The development of the bioabsorbable stent is a challengingone. The ideal polymer, degradation time and degradation rateto allow vessel support healing and prevention of acute recoiland late vessel remodeling have to be found. Many bioabsorbablestents have been developed but failed to go beyond initial firstin-manevaluation phase. The only one to make it to commercialutilization and thus far, approved by European CE regulatory bodyis the Bioresorbable Vascular Scaffold (BVS Abbott Vascular, SantaClara, California). Made of thick strut poly-L-lactide, with anotherlactide acting as a controlled release polymer coating, the stentelutes an antiproliferative drug, everolimus, to prevent smoothmuscle cell proliferation. The stent has gone into a second iteration(BVS1.1) with the improved version providing better scaffolddesign and performance. The angiographic late loss, a parameterof vascular biologic response, amounted to 0.27+/-0.32mm,which is comparable with current best DESs.The bioabsorbable stent represents another breakthrough inthe technological evolution of the coronary stent, and a potentialgame changer in the industry of stent design and materials. We areproud to provide this technology to our suitable patients.NUHCS PULSE | 15
My Fellowship Days At NUHCSObjects in the RearDr Rishi SethiView MirrorAs I pen down my experiences asan interventional fellow at NUHCS, mymind is filled with fond memories of thetime I spent here.It all started in early 2010 when I metProf Tan to discuss the possibility of myjoining the fellowship in InterventionalCardiology at NUHCS. He was kindenough to accept me as a fellow and so Ilanded in Singapore in August 2010, to start my one year fellowship.The first few days without family were difficult. I missed mydoting daughters and the dramatic silence of my hand phone- whichwas used to constant buzzing when I was in India- gave me a strangefeeling of uneasiness . But soon all my co-fellows, staff andconsultants of the cath lab made me feel comfortable and from thenon it became a very enriching journey for me.Though the days had long working hours and we had more thana few rough nights managing emergency cases, the intense traininghelped me develop and nurture my skills in interventionalcardiology. I was exposed to almost every hardware one can use inintervention cardiology including IVUS, FFR, Rotablator, OCT andvarious protection devices in SVG interventions. The unrestrictedexposure to various hardware was combined by meticulous trainingabout their clinical utility and judicious use in specific situations.The entire team at the department was extremely dedicated and Ilearned from them not only the science of angioplasty but also theart of comprehensive patient management. The nurses and thetechnical staff of the cath lab were caring and always ready to go anextra mile whenever they realized that you were stressed or overburdened by work.I had come to Singapore with a professional objective in mindtotrain myself well in interventional cardiology. But by the time Ileft, I had much more to be thankful for.I would forever remain grateful to Prof Tan for giving thisopportunity to learn at NUHCS and also for ensuring that I hadsome great time off work during my stay here. His warm and everinspiring presence infused a positive energy in all the fellows. I amalso indebted to Dr Adrian, who was my supervisor, for guiding methrough the year and ensuring that my training objectives weremore than met. Though I cannot name everyone individually but Iwish to thank all the consultants and registrars of the departmentfor extending their friendship to me during this year.As I move ahead in life I will always cherish the time I spenthere. Someone once said that if your plane is landing in a city andyour heart is filled with joy, like a child coming back home, then itmeans that you really love the place.I will probably feel the same when next time my plane touchesdown at Singapore…NUHCS PULSE | 16
ESC <strong>2011</strong>Dr YeoTee JooI recently attended my first major overseas conference – theEuropean Society of Cardiology Congress <strong>2011</strong> held in Paris,France from 27 th to 31 st August. Incidentally, this was the largestESC Congress ever, with more than 30,000 attendees. It was trulyan eye-opener to experience a world-class conference brimmingwith the latest developments from every conceivable aspect ofCardiology.Undoubtedly, the hottest topic during the Congress was thatof atrial fibrillation and the new anticoagulants, in particular theresults of the ARISTOTLE trial which showed that Apixaban wassuperior to the old warrior warfarin in stroke prevention as wellas decreased adverse effects. Not forgetting the PRODIGY trialthat demonstrated that 6 months of dual antiplatelet therapyfollowing stent implantation was actually equivalent to 2 yearswith less bleeding risk.NUHCS was certainly well represented throughout theCongress. Dr Carolyn Lam was one of the presenters for thesymposium on her pet topic, pathophysiology of heart failurewith preserved ejection fraction. Her talk on vascular remodelingand pulmonary hypertension certainly made the departmentproud! In addition, several abstracts were also accepted forthe Congress – namely from Drs Shi Hongyu (former clinicalfellow), Saket Junagade (my fellow Registrar who also attendedthe Congress), Glenn Lee (current house officer with a keeninterest in Cardiology) and Joshua Loh (Associate Consultant) –well done to all!With the multitude of symposiums running concurrently,most people were certainly left spoilt for choice when it cameto choosing the sessions to attend. Of course, selected sessionslike the launch of the new ESC <strong>2011</strong> guidelines were packed tothe brim and the organizers had to scramble to direct those whowere straining to listen in from the outside to a separate area,which promptly filled up as well. On a personal note, being anavid runner, I found myself drawn to sessions involving sports,marathon running and their effects on the heart.On a closing note, I would like to thank the Singapore CardiacSociety for allowing me to utilize my remuneration from the SCSASM <strong>2011</strong> Young Investigator Award for this trip. Additionally, I wasnominated to attend the Congress under the “ESC Cardiologistsof Tomorrow” program where those below 35 years old who arecompletely new to the ESC received a full waiver of registration.For fellow colleagues and juniors keen to make their virginvoyage to the ESC Congress, this scheme is highly desirable andis definitely encouraged!To be able to attend an international congress in one of the mostbeautiful cities in the world deserves many more superlatives thatI can ever come up with. It was an unforgettable and undeniablyinspiring time, and I await my next opportunity with greatanticipation.NUHCS PULSE | 17
24th-25th September <strong>2011</strong>Dr Mark ChanThe National Univesity Heart Centre, Singapore, togetherwith the Duke Cardiovascular Research Institute, USA, hostedSingapore’s first Antithrombotic Pharmacotherapeutics Symposiumfrom the 24th to 25th September <strong>2011</strong> at the new NationalUniversity Health System campus. International and local expertsupdated more than 250 doctors, nurses, pharmacists and industrydelegates on key clinical perspectives on the pharmacologicaltreatment of venous and arterial thrombosis.Antithrombotic therapy, comprising oral and injectableantiplatelet and anticoagulant agents, is the most widely prescribedclass of medications in clinical practice.The last 12 months have also seen a bumper crop of new drugstargetting the human platelet and coagulation system that havebegun an exciting new era of treatment options for thromboticdisorders.Drs Mark Chan and Chee Yen Lin, who co-chaired theconference, explains that there are two new revolutionary classesof antithrombotic therapy. The first belongs to the class of oralanticoagulants for prevention of stroke in atrial fibrillation, a verycommon disease of the elderly that can lead to debilitating strokesin as many as 10% of untreated patients. Warfarin, which has beenthe only useful drug for this condition for the last 5 decades,incurs a high risk of bleeding, including bleedinginto the brain, requires frequent blood tests andnecessitates strict adherence to dietary restrictions.Three new drugs, Rovaroxaban (Xarelto, Bayer),Dabigatran (Pradaxa, Boerhinger Ingelheim) andApixaban (Eliquis, Bristol Myers Squibb,) haveshown themselves to be as effective as warfarinin preventing strokes in atrial fibrillation but witha much lower risk of bleeding into the brain andwithout the need for regular monitoring blood tests.The second group of drugs belong to a class of drugs calledP2Y12 inhibitors. This class of drugs reduce the stickinessof platelets and prevent clogging of blood vessels after stentimplantation for a heart condition. For more than a decade, patientshad only one option in this drug class, clopidogrel. However, notall patients respond well to this drug and a failure to respond tothis drug can result in a rare but dreaded complication calledstent thrombosis in which a recently-implanted heart blood vesselstent clots suddenly and causes a major heart attack, frequentlyresuting in death. One reason for this poor response is the presenceof a genetic abnormality in the CYP2C19 system that convertsclopidogrel to the active form.Patients with one or more abnormal forms of this gene cannotgenerate the active compound as quickly as normal individuals.As such, their platelets remain more sticky and more prone toclogging up stents implanted in blood vessels supplying the heart.In a local study conducted on 400 patients seeking treatmentat the National University Hospital Dr Chan and colleagues showthat this abnormal gene is present in more than 40% of Indianpatients and close of 60% of Chinese and Malay patients. Thesefindings were presented at the International Society of Thrombosisand Haemostasis meeting in Kyoto, Japan this <strong>July</strong>.NUHCS PULSE | 18
The new P2Y12 – inhibiiting drugs, Ticagrelor (Brillianta,Astrat Zeneca) and Prasugrel (Effient, Eli-Lilly) reduce plateletstickiness more effectively and consistently in part because theybypass the CYP2C19 system of drug activation. Not only are thesenew drugs more expensive than clopidogrel, which is presentlygeneric, they can cause increased bleeding, so they may not besuitable for every patient.One possibility to do genetic testing to determine whichpatients may require the newer P2Y12 drugs. However, genetictesting itself can be expensive. Moreover, there are many otherdeterminants of response to clopidogrel, including age, bodyweight, renal function and diabetes. There is also the question ofwhether measuring the actual stickiness of the platelet itself, calledplatelet reactivity testing, is a better alternative.One of the symposium highlights was a hands-on plateletfunction testing workshop in which participants were trained inthe performance and interpretation of genetic tests and plateletreactivity tests.The APS meeting will be held every two years at differentlocations in South-east Asia. Through these meetings, Drs Chanand Chee hope to highlight and address some of the uncertaintiesin the use of these antithrombotic medications drugs and also equiphealthcare providers with practical yet thoughtful strategies fortreating patients with venous and arterial thrombotic disorders.NUHCS PULSE | 19
Division of Thoracic Surgery:The New DivisionDr John TamwithinNUHCSThoracic Surgery is a specialty dedicatedto the surgical management of diseases ofthe lung, pleura, mediastinum, diaphragm,and chest wall. There are a wide spectrumof diseases involving these importantstructures, including malignancies such aslung cancer and mediastinal tumors, andbenign conditions such as empyema orhemo-pneumothorax. These conditionsusually require urgent surgical attentionfor diagnosis and treatment. Patientsseeking thoracic surgical care is on the risein Singapore and internationally, driven byan aging population and increasing demandfor sophisticated medical care.The care of the thoracic surgical patientrequires a multi-disciplinary approach,integrating specialists in thoracic surgery,respiratory medicine, medical oncology,radiation oncology, critical care medicine,radiology, and pathology. This core clusterof specialists is discipline-specific and is distinctive to thoracicsurgery as compared to other specialties. We have formed a verycohesive group of specialist colleagues within the lung tumor groupto ensure our patients receive the best care.Thoracic surgery is increasingly recognized as a distinctspecialty in clinical practice, with a strong focus on thoracicsurgical oncology as well as benign diseases within the thorax.Technical and technological advances also bring the advent ofminimally invasive approaches using Video-Assisted ThoracicSurgery (VATS), which leads to further specialization in this field.VATS offers many advantages to patients including fast recoveryand less pain, and is very popular among patients who are seekingthoracic consultation. In our current practice, more than 80% ofour surgeries are performed using VATS.The Division of Thoracic Surgery is established to bring ourservices to the next peak of excellence. This development ismade possible by the strong support of Professor Lee ChuenNeng, Chief of the Department of Cardiac, Thoracic, and VascularSurgery; A/Professor Tan Huay Cheem, director of NUHCS;senior management including CMB A/Professor Aymeric Limand CEO Mr Joe Sim; and all our colleagueswithin NUH.We aim to create a center of excellencein Thoracic Surgery serving patients inSingapore and beyond. The formation ofthis Division forges a strong identity ofthoracic surgery within NUH and affirmsits status as a mature and distinct specialty.We strive to improve outcomes, createinnovations, and streamline processes. Thisallows strong integration and synergy of thetripartite mission of service, innovation,and education.I am honored and humbled to beappointed as the Head of the Divisionof Thoracic Surgery. Our division alsocomprised of Dr Agasthian Thirugnanam,who recently joined us and brings withhim extensive knowledge and experiencesin thoracic surgery; and Dr Atasha Asmat,who will soon be completing her fellowshipsin New York and Liverpool and will return with new skills andtechnologies. Prof CN Lee, Adj A/P Michael Caleb, A/P TheodorosKofidis, Dr Christie Tan, Dr Kristine Teoh, Dr Ooi Oon Cheong,Dr Jimmy Hon, and Dr Winn Maung Aye also provide thoracicsurgery service. We are assisted by many capable housestaff andsupport staff, including our case management officer Dr VijayaKumar, research assistant Mr Lim Kee Siang, and many friendlyoffice staff within the department.We have recently started a new Singapore Medical Councilapproved clinical fellowship program in Thoracic Surgery, andwill help to develop the next generation of thoracic surgeons fromaround the world. We are also organizing an international VATSworkshop in November <strong>2011</strong>, and will be hosting internationalfaculty speakers and participants to promote advanced minimallyinvasive thoracic surgery.Everyone within the Division of Thoracic Surgery is committedto deliver excellent patient care and to collectively propel thisspecialty to new heights through the process of discovery andinnovation. This is truly an exciting time for thoracic surgery inSingapore.NUHCS PULSE | 20
happeningsMO dinner 24 Oct 2012Cardiac Family Day 2012 10 Aug 2012NUHCS PULSE | 21
Echo Singapore 2012 12-14 Oct 2012National Medical Excellance Awards 5 <strong>July</strong> <strong>2011</strong>Antithrombotic Symposium 2012 24 Aug 2012NUHCS PULSE | 22
publications1. Annals of Vascular Diseases. <strong>2011</strong> Jun;4(2). Outcomesof Endovascular Intervention for Salvage of FailingHemodialysis Access. Tan TLX, May KK, Robless PA,Ho P.2. Aust N Z J Public Health. <strong>2011</strong> Jun;35(3):249-55.Kaupapa Maori approach to a community cohort studyof heart disease in New Zealand. Pitama S, Wells JE,Faatoese A, Tikao-Mason K, Robertson P, Huria T,Gillies T, Doughty R, Whalley G, Troughton R, SheerinI, Richards M, Cameron VA.3. Singapore Med J. <strong>2011</strong> Jun;52(6):400-4. Half-doseezetimibe add-on to statin therapy is effective in improvingresistant hyperlipidaemia in Asian patients with ischaemicheart disease. Chong E, Shen L, Poh KK.4. Singapore Med J. <strong>2011</strong> Jun;52(6):394-8; quiz 399.Electrocardiography Series. What is the cause of theregular wide QRS complex tachycardia? Lim SL, Teo SG,Kireyev D, Poh KK.5. Singapore Med J. <strong>2011</strong> Jul;52(7):468-73; quiz 474.Narrow QRS complex tachycardia presenting aspalpitation. Singh D, Teo SG, Kireyev D, Poh KK.6. Cardiovasc Pathol. <strong>2011</strong> Jul 14. Variable Phenotypein Murine Transverse Aortic Constriction (TAC).Mohammed SF, Storlie JR, Oehler EA, Bowen LA,Korinek J, Lam CS, Simari RD, Burnett JC Jr, RedfieldMM.7. J Biol Chem. <strong>2011</strong> Jul 7. DLK1-DIO3 genomic imprintedmicroRNA cluster at 14q32.2 defines a stem-like subtypeof hepatocellular carcinoma associated with poor survival.Luk JM, Burchard J, Zhang C, Liu AM, Wong KF, ShekFH, Lee NP, Fan ST, Poon RT, Ivanovska I, Philippar U,Cleary MA, Buser CA, Shaw PM, Lee CN, Tenen DG,Dai H, Mao M.8. Pediatr Crit Care Med. <strong>2011</strong> Jul;12(4):474-5.Pulmonary complications during cardiacextracorporeal membrane oxygenation: Isbronchoscopy worth the bother? Maclaren G.9. Circulation. 2010 Jul 20;122(3):255-64. B-type natriureticpeptide signal peptide circulates in human blood:evaluation as a potential biomarker of cardiac ischemia.Siriwardena M, Kleffmann T, Ruygrok P, Cameron VA,Yandle TG, Nicholls MG, Richards AM, Pemberton CJ.10. Can J Physiol Pharmacol. <strong>2011</strong> Aug;89(8):603-7. Tailoredtherapy for heart failure: neurohormones. Richards AM.11. Pediatr Transplant. <strong>2011</strong> Aug 11. Unusual shuntfor symptomatic portal vein thrombosis after livertransplantation – Clatworthy revisited. Mali VP, RoblessPA, Aw M, Loh DL, Quak SH, Prabhakaran K.12. J Surg Res. <strong>2011</strong> Aug 29. Surgeons’ Static Posture andMovement Repetitions in Open and Laparoscopic Surgery.Szeto GP, Cheng SW, Poon JT, Ting AC, Tsang RC, HoP.13. Am Heart J. <strong>2011</strong> Aug;162(2):291-9. Recalibration ofthe global registry of acute coronary events risk score ina multiethnic Asian population. Chan MY, Shah BR, GaoF, Sim LL, Chua T, Tan HC, Yeo TC, Ong HY, Foo D,Goh PP, Surrun SK, Pieper KS, Granger CB, Koh TH,Salim A, Tai ES.14. Eur Heart J Cardiovasc Imaging <strong>2011</strong>: In press.Left ventricular fluid dynamics in heart failure:echocardiographic measurement and utilities of vortexformation time. Poh KK, Lee LC, Shen L, Chong E, TanYL, Chai P, Yeo TC, Wood MJ.15. J Am Coll Cardiol. <strong>2011</strong>: In press. Fatal vacuolarcardiomyopathy: clinicopathological correlate. Poh KK,Chai P, Wong RC, Tan KB.16. Singapore Med <strong>2011</strong>. Electrocardiography Series. ECGsof structural heart disease (Part I). Poh KK, Teo SG, TayEL, Yip WL.17. Singapore Med <strong>2011</strong>; 52(11):772-6. ElectrocardiographySeries. Misleading ECG recordings. Yeo WT, Teo SG,Loh PY, Poh KK.18. Med of Malaysia <strong>2011</strong>; 66(3): 249-52. A cohort study ofrisk factors and clinical outcome predictors for patientspresenting with unstable angina and non ST segmentelevation myocardial infraction undergoing coronaryintervention. Chong E, Shen L, Tan HC, Poh KK.NUHCS PULSE | 23
19. Hypertension. <strong>2011</strong> Aug;58(2):140-1. TheSocioeconomics of Hyertension: How $50 000 May BuyA Drop In Blood Pressure. Lam CS.20. J Am Coll Cardiol. <strong>2011</strong> Aug 2;58(6):618-26. Influenceof Sex and Hormone Status on Circulating NatriureticPeptides. Lam CS, Cheng S, Choong K, Larson MG,Murabito JM, Newton-Cheh C, Bhasin S, McCabe EL,Miller KK, Redfield MM, Vasan RS, Coviello AD, WangTJ.21. J Am Coll Cardiol. <strong>2011</strong> Aug 30;58(10):1057-67.Midregion prohormone adrenomedullin and prognosis inpatients presenting with acute dyspnea: results from theBACH (Biomarkers in Acute Heart Failure) trial. MaiselA, Mueller C, Nowak RM, Peacock WF, PonikowskiP, Mockel M, Hogan C, Wu AH, Richards M, CloptonP, Filippatos GS, Di Somma S, Anand I, Ng LL, DanielsLB, Neath SX, Christenson R, Potocki M, McCord J,Hartmann O, Morgenthaler NG, Anker SD.22. Clin Chem. <strong>2011</strong> Aug;57(8):1154-60. Early dynamicchange in high-sensitivity cardiac troponin T in theinvestigation of acute myocardial infarction. Aldous SJ,Richards AM, Cullen L, Than MP.23. Ann Acad Med Singapore. <strong>2011</strong> Sept;40(9): 392-2. Heartfailure: a problem of our age. Richards AM, Lam C, WongRC, Ping C.24. J Hypertens. <strong>2011</strong> Sep;29(9):1829-1836. The relationshipbetween renal impairment and left ventricular structure,function, and ventricular-arterial interaction inhypertension. Shah AM, Lam CS, Cheng S, Verma A,Desai AS, Rocha RA, Hilkert R, Izzo J, Oparil S, Pitt B,Thomas JD, Zile MR, Aurigemma GP, Solomon SD.25. Ann Acad Med Singapore. <strong>2011</strong> Sep;40(9):392-3. Heartfailure: a problem of our age. Richards AM, Lam C, WongRC, Ping C.26. Pediatr Crit Care Med. <strong>2011</strong> Sep;12(5):606-7. Centralextracorporeal membrane oxygenation for refractorypediatric septic shock. Maclaren G, Butt W.27. PLoS One. <strong>2011</strong>;6(9):e25268. Epub <strong>2011</strong> Sep 23.Role of Chaperone Mediated Autophagy (CMA) in theDegradation of Misfolded N-CoR Protein in Non-SmallCell Lung Cancer (NSCLC) Cells. Ali AB, Nin DS, TamJ, Khan M.28. J Am Coll Cardiol. <strong>2011</strong> Sep 27;58(14):1507-8. Leftventricular ejection fraction in addition to N-terminalpro-B-typenatriuretic peptide for risk stratification in theambulant elderly: get the picture...or not? Richards AM.29. J Hypertens. <strong>2011</strong> Sep;29(9):1787-95. Urocortin2 sustains haemodynamic and renal function duringintroduction of beta-blockade in experimental heartfailure. Rademaker MT, Charles CJ, Nicholls G, RichardsM.30. Acad Emerg Med. <strong>2011</strong> Sep;18(9):947-58. Short termmortality risk in emergency department acute heartfailure. Peacock WF, Nowak R, Christenson R, DiSommaS, Neath SX, Hartmann O, Mueller C, Ponikowski P,Möckel M, Hogan C, Wu AH, Richards M, FilippatosGS, Anand I, Ng LL, Daniels LB, Morgenthaler N, AnkerSD, Maisel AS.31. JACC Cardiovasc Imaging. <strong>2011</strong> Sep;4(9):927-34. SerialDoppler echocardiography and tissue Doppler imagingin the detection of elevated directly measured left atrialpressure in ambulant subjects with chronic heart failure.Ritzema JL, Richards AM, Crozier IG, Frampton CF,Melton IC, Doughty RN, Stewart JT, Eigler N, WhitingJ, Abraham WT, Troughton RW.\32. Circ Heart Fail. <strong>2011</strong> Sep;4(5):613-20. Increased 90-daymortality in patients with acute heart failure with elevatedcopeptin: secondary results from the Biomarkers in AcuteHeart Failure (BACH) study. Richards M et al.33. Ann Acad Med Singapore. <strong>2011</strong> Sep;40(9):392-3. Heartfailure: a problem of our age. Richards AM, Lam C, WongRC, Ping C.34. J Cardiovasc Pharmacol. <strong>2011</strong> Oct;58(4):418-23.Urocortin 3 inhibits cardiac sympathetic nerve activityin conscious sheep. Charles CJ, Jardine DL, RademakerMT, Richards AM.35. J Tissue Eng Regen Med. <strong>2011</strong> Oct 28. doi: 10.1002/term.512. Post-ischaemic angiogenic therapy using in vivoprevascularized ascorbic acid-enriched myocardial artificialgrafts improves heart function in a rat model. MartinezEC, Wang J, Lilyanna S, Ling LH, Gan SU, Singh R, LeeCN, Kofidis T.36. Singapore Med J. <strong>2011</strong> Oct;52(10):707-14.Electrocardiography series. Managing ventricular ectopics:are ventricular ectopic beats just an annoyance? Omar AR,Lee LC, Seow SC, Teo SG, Poh KK.37. J Clin Endocrinol Metab. <strong>2011</strong> Oct;96(10):3242-9. Cardiac Natriuretic Peptides, Obesity, and InsulinResistance: Evidence from Two Community-BasedStudies. Khan AM, Cheng S, Magnusson M, Larson MG,Newton-Cheh C, McCabe EL, Coviello AD, Florez JC,Fox CS, Levy D, Robins SJ, Arora P, Bhasin S, Lam CS,Vasan RS, Melander O, Wang TJ.NUHCS PULSE | 24
38. Am J Med. <strong>2011</strong> Nov;124(11):1051-7. Epub <strong>2011</strong> Sep 22.Bedside assessment of cardiac hemodynamics: the impactof noninvasive testing and examiner experience. FromAM, Lam CS, Pitta SR, Kumar PV, Balbissi KA, BookerJD, Singh IM, Sorajja P, Reeder GS, Borlaug BA.39. Singapore Med J. <strong>2011</strong> Nov;52(11):835-9. Acutemyocardial infarction in young Asian women: acomparative study on Chinese, Malay and Indian ethnicgroups. Xie CB, Chan MY, Teo SG, Low AF, Tan HC,Lee CH.40. Int J Cardiovasc Imaging <strong>2011</strong> Nov 11. Ischemic changeson rubidium-82 positron emission tomography imagingare associated with left ventricular functional andvolumetric change independent of metabolic propertiesand echocardiographic functional variables in ischemiccardiomyopathy. Wong RC, Cerquerira MD, BrunkenRC.41. Pediatr Crit Care Med. <strong>2011</strong> Nov;12(6):e395-7.Prolonged venovenous extracorporeal membraneoxygenation in a child with leukemia and persistentbacteremia. Ong J, Ngiam N, Aye WM, Maclaren G.42. Cochrane Database Syst Rev. <strong>2011</strong> Nov 9;11:CD001272.Antiplatelet agents for intermittent claudication. WongPF, Chong LY, Mikhailidis DP, Robless P, Stansby G.43. Maturitas. <strong>2011</strong> Dec 20. Natriuretic peptides, gender andcardiovascular risk: What is the link? Santhanakrishnan R,Lam CS.44. Int J Cardiol. <strong>2011</strong> Dec 27. Immigrant status anddisparities in health care delivery in patients withmyocardial infarction. Lee CH, Choo H, Tai BC, ChanMY, Phua QH, Low TT, Richards AM, Tan HC, Ow R,Yeo TC.45. J Clin Sleep Med. <strong>2011</strong> Dec 15;7(6):616-21. Severeobstructive sleep apnea and outcomes following myocardialinfarction. Lee CH, Khoo SM, Chan MY, Wong HB, LowAF, Phua QH, Richards AM, Tan HC, Yeo TC.46. Intern Med J. <strong>2011</strong> Dec;41(12):809-14. doi:10.1111/j.1445-5994.2010.02278.x. Utilisation ofemergency medical service among Singapore patientspresenting with ST-segment elevation myocardialinfarction: prevalence and impact on ischaemic time. TanLL, Wong HB, Poh CL, Chan MY, Seow SC, Yeo TC,Teo SG, Ooi SB, Tan HC, Lee CH.47. Mediterr J Hematol Infect Dis. <strong>2011</strong>;3(1):e<strong>2011</strong>0. Epub<strong>2011</strong> Apr 1.Spontaneous Pneumothorax in an AllogeneicCell Transplant Recipient with Invasive PulmonaryAspergillosis and Antecedent RSV Pneumonitis. Koh LP,Poon ML, Tam JK, Teo L, Hsu LY.48. Crit Care Med. <strong>2011</strong> Dec;39(12):2787-8. Respiratorydialysis is not extracorporeal membrane oxygenation.Maclaren G, Combes A, Bartlett RH.49. Intensive Care Med. <strong>2011</strong> Dec 7. Contemporaryextracorporeal membrane oxygenation for adultrespiratory failure: life support in the new era. MaclarenG, Combes A, Bartlett RH.50. Pediatr Crit Care Med. <strong>2011</strong> Jul;12(4 Suppl):S76-80.Monitoring in pediatric cardiac critical care: A worldwideperspective. Spenceley N, MacLaren G, Kissoon N,Macrae DJ.51. Pediatr Crit Care Med <strong>2011</strong>; 12(4):S1-S102. The PediatricCardiac Intensive Care Society Evidence-based Review andConsensus Statement on Monitoring of Hemodynamicsand Oxygen Transport Balance. Checchia PA, BronickiRA, Allen M, Anas N, Berger JT, Bohn D, Cooper DS,Dalton HJ, Domico M, Finer NN, Gazit AZ, GhanayemNS, Hazinski MF, Hoffman GM, Kinsella JP, Kissoon N,Klugman D, Laussen P, MacLaren G, Macrae DJ, PerkinDJ, Sivarajan B, Spenceley N, Tucker D, Wernovsky G,Wong H.52. Circ Cardiovasc Genet. <strong>2011</strong> Dec 1;4(6):636-46.Genomic risk variants at 1p13.3, 1q41, and 3q22.3 areassociatedwith subsequent cardiovascular outcomes inhealthy controlsand in established coronary artery disease.Ellis KL, Frampton CM, Pilbrow AP, Troughton RW,Doughty RN, Whalley GA, Ellis CJ, Skelton L, ThomsonJ, Yandle TG, Richards AM, Cameron VA.53. Singapore Med J Oct <strong>2011</strong> 52(10):707-13. ManagingVentricular Ectopics: are ventricular ectopic beats justan annoyance? Omar AR, Lee LC, Seow SC, Teo SG,Poh KK.54. Singapore Med J Sep <strong>2011</strong>; 52(9): 647-50. Brugadapattern masking anterior myocardial infarction. Seow SC,Omar AR, Hong EC.55. Heart Asia <strong>2011</strong> 3: 35-36. Sinus arrest following stentingof the right coronary artery. Seow SC, Soo WM, TolentinoCS.NUHCS PULSE | 25
abstractsASCVTS-ATCAS <strong>2011</strong>: Joint Meeting of 19thASCVTS & 21st ATCSAPhuket, Thailand, May <strong>2011</strong>1. Is Continuation of Anti-Platelet Therapy Until CoronaryArtery Bypass Grafting a Safe Strategy? Zaw MT, Hu J,Tay CW, Ng WQ, Chia D, Lee CN, Kofidis T2. Sutureless Valve Technology Facilitates Aortic ValveReplacement Through Right Minithoracotomy.Grunenfelder J, KofidisT, Reser D, Emmert M, PlassA, Falk V.3. Post-CABG Atrial Fibrillation: Is Single/Dual AntiplateletTherapy as Safe and Effective as Anticoagulation Therapyin Preventing Major Thromboembolic Events? Ooi OC,Yang J, Luo HD, Lee CN.International Student Congress of (bio)MedicalSciencesGroningen, Netherlands, June <strong>2011</strong>1. First Prize for Best Presentation, Cardiology & PulmonaryTrack session. Ethnic differences in risk prediction forheart failure rehospitalization. Zaw MW, Wong CC,Seow SC, Chai P, Kwok B, Ng K, Ling LF, Leong G,Yeo D, Surrun SK, Sim LL, Gao F, Lam SP.The Lancet/JACC 1st Asia PacificCardiovascular SummitHong Kong, <strong>July</strong> <strong>2011</strong>1. Growth Differentiation Factor 15, ST2 and NatriureticPeptides in Heart Failure With Preserved VersusReduced Ejection Fraction. Santhanakrishnan R, ChongJ, Richards AM, Lam SP.European Society of Cardiology <strong>2011</strong>Paris, France, August <strong>2011</strong>1. Safety of deferring revascularization in lesions with FFR>0.75 but a small IVUS-derived lumen area. JunagadeS, Chan MY, Low AF, Teo SG, Richards AM, Yeo TC,Tan HC, Lee CH.2. Long-term clinical outcomes of medical therapy versuscoronary revascularisation in patients with intermediatestenoses guided by pressure wire. Shi HY, Chan MY,Low AF, Lee CH, Teo SG, Chan KH, Sethi R, RichardsAM, Tan HC.3. Wide fluctuations in capillary glucose levels during acutecoronary syndrome predicts poor prognosis. Lee GK,Yeo WT, Chan MY, Poh KK, Lau CS, Lee RC, Yeo TC.4. Novel assessment of vortex formation time of the rightventricle: comparison with left ventricular fluid dynamicsin pulmonary embolism. Reyes-Mariano M, Oinuma S,Soo WM, Loh JP, Yeo TC, Pooja J, Venkatesh SK, PohKK.5. Progression of impaired left ventricular contractility inpatients with isolated diastolic dysfunction and heartfailure with preserved ejection fraction. Zhong L, PohKK, Sia W, Lee LC, Le TT, Chua T, Tan RS.15th Annual Scientific meeting of the HeartFailure Society of AmericaBoston, United States, September <strong>2011</strong>1. Ethnic differences in risk prediction for heart failurerehospitalization. Zaw MW, Wong CC, Seow SC, ChaiP, Kwok B, Ng K, Ling LF, Leong G, Yeo D, Surrun SK,Sim LL, Gao F, Lam SP.NUHCS PULSE | 26
Western Vascular Society 26th AnnualMeetingHawaii, United States, September <strong>2011</strong>1. Characterization of Thoracic Aortic Arch Anatomy inthe Asian Elderly Population. Ho P, Chiu PX, Lee HP,Venkatesh SK.12th Asian Society for Vascular Surgery(ASVS <strong>2011</strong>)Taipei, Taiwan, September <strong>2011</strong>1. Reliability of Using Ultrasound Duplex for Screeningof Dysfunctional Hemodialysis Access2. Raju A, Kyin KM, Zaw MT, Canlas CC, Seah MH,Serrano C, Hartman M, Ho P.American Heart Association Scientific Sessions,Orlando, United States, November <strong>2011</strong>1. Sex differences in clinical characteristics and outcomesin elderly patients with heart failure and preservedejection fraction: The I-PRESERVE Trial. Lam SP,Anand IS, Carson PE, Massie BM, Rector T, KuskowskiM, McKelvie R, MZile MR, McMurray JJ, Komajda M,Kitzman DW.2. Growth Differentiation Factor 15, ST2 and NatriureticPeptides in Heart Failure with Preserved VersusReduced Ejection Fraction. Santhanakrishnan R, ChongJ, Richards AM, Lam SP.3. Comparing the Effects of Low-Flow Aortic Stenosiswith Preserved Ejection Fraction Versus Normal-FlowAortic Stenosis on Left Ventricular Diastolic Functionand Left Atrial Volumes. Soo WM, Ling LH, Chan MY,Loh J, Poh KK.Transcatheter Cardiovascular Therapeutics<strong>2011</strong>San Francisco, United States, October <strong>2011</strong>American Society of Echocardiography 22ndAnnual Scientific SessionsMontreal, June <strong>2011</strong>1. Real-World Comparison Of Clinical Outcomes OfPatients Who Received New Generation PlatinumChromium Everolimus-Eluting Stent Versus CobaltChromium Everolimus-Eluting Stent. Li RG, Low AF,Lee CH, Chan MY, Teo SG, Chan KH, Richards AM,Tan HC.1. Suboptimal left ventricular vertical formation and fluidpropagation in mitral valve stenosis. Loh JP, Yeo TC,Poh KK.NUHCS PULSE | 27
directoryNational University Heart Centre,Singapore1E Kent Ridge Road, NUHS Tower BlockLevel 9, Singapore 119228Heart Clinic @ Level & Heart Clinic @ Level 3National University HospitalMain Building, Level 1, Lift Lobby BClinic Appointment 6772 2002Emailcardiac_clinics@nuhs.edu.sgFeedbackPlease direct your feedback toThe Editor, NUHCS PULSENational University Heart Centre, Singapore1E Kent Ridge RoadNUHS Tower BlockLevel 9, Cardiac DepartmentSingapore 119228Tel 6772 6129Email<strong>nuhcs</strong>_pulse@nuhs.edu.sgAug <strong>2011</strong>–Mar 2012new doctorson boardDr Julian Wong Chi LeungSenior Consultant, Department of CTVSDr Chester DrumAssociate Consultant, Cardiac DepartmentDr Pipin KojodjojoConsultant, Cardiac DepartmentDr William KongAssociate Consultant, Cardiac DepartmentDr Tan Li LingRegistrar, Cardiac DepartmentEditorA/Prof Poh Kian Keongcongrats!AdvisorA/Prof Tan Huay CheemDr Soo Wern MiinRegistrar to Associate ConsultantA/Prof Carolyn LamPromoted to Associate Professor