PLHIV Stigma Index in Nepal
PLHIV Stigma Index in Nepal
PLHIV Stigma Index in Nepal
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
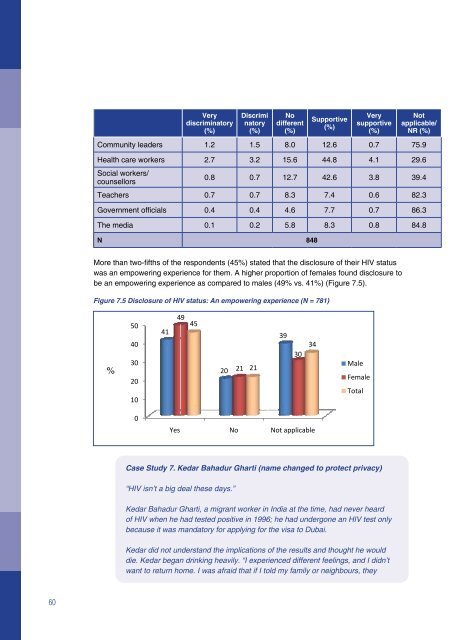
Verydiscrim<strong>in</strong>atory(%)Discrim<strong>in</strong>atory(%)Nodifferent(%)Supportive(%)Verysupportive(%)Notapplicable/NR (%)Community leaders 1.2 1.5 8.0 12.6 0.7 75.9Health care workers 2.7 3.2 15.6 44.8 4.1 29.6Social workers/counsellors0.8 0.7 12.7 42.6 3.8 39.4Teachers 0.7 0.7 8.3 7.4 0.6 82.3Government officials 0.4 0.4 4.6 7.7 0.7 86.3The media 0.1 0.2 5.8 8.3 0.8 84.8N 848More than two-fifths of the respondents (45%) stated that the disclosure of their HIV statuswas an empower<strong>in</strong>g experience for them. A higher proportion of females found disclosure tobe an empower<strong>in</strong>g experience as compared to males (49% vs. 41%) (Figure 7.5).Figure 7.5 Disclosure of HIV status: An empower<strong>in</strong>g experience (N = 781)%5040302010041Yes49 4520 21 21NoCase Study 7. Kedar Bahadur Gharti (name changed to protect privacy)“HIV isn’t a big deal these days.”Not applicableKedar Bahadur Gharti, a migrant worker <strong>in</strong> India at the time, had never heardof HIV when he had tested positive <strong>in</strong> 1996; he had undergone an HIV test onlybecause it was mandatory for apply<strong>in</strong>g for the visa to Dubai.Kedar did not understand the implications of the results and thought he woulddie. Kedar began dr<strong>in</strong>k<strong>in</strong>g heavily. “I experienced different feel<strong>in</strong>gs, and I didn’twant to return home. I was afraid that if I told my family or neighbours, they393034MaleFemaleTotalwould discrim<strong>in</strong>ate aga<strong>in</strong>st me.” Kedar lost confidence <strong>in</strong> himself and avoidedsocial engagements. “I felt uncomfortable with my friends and with myself.”After hav<strong>in</strong>g learnt his status, Kedar tried us<strong>in</strong>g condoms with his wife whenever hereturned to <strong>Nepal</strong>. However, Kedar’s wife wanted babies; therefore, he disregardedthe advice aga<strong>in</strong>st impregnat<strong>in</strong>g his wife and risked the transmission of the virus tothe child. Kedar resumed the use of condoms after the birth of his two children—ason and a daughter.In 2000, Kedar confided <strong>in</strong> his brother about his HIV-positive status. He <strong>in</strong>troducedKedar to a friend who had founded a support group for <strong>PLHIV</strong>. Kedar beganattend<strong>in</strong>g the support group meet<strong>in</strong>gs. His brother also helped Kedar disclosehis status to family members. Learn<strong>in</strong>g that Kedar was HIV-positive, his wiferesponded with resignation: “If you have HIV, I must, too. If you are go<strong>in</strong>g to die,so am I.” However, luckily, Kedar’s wife tested negative, as did his two children.Subsequently, Kedar became an outreach worker at the support group and ga<strong>in</strong>edknowledge of HIV awareness rais<strong>in</strong>g and community organiz<strong>in</strong>g.Kedar emphasizes that the key to reach<strong>in</strong>g the “hidden” population is a village-levelcampaign and persistence. Hav<strong>in</strong>g seen many village-level <strong>in</strong>terventions, membersof the “hidden” population of <strong>PLHIV</strong> have also voluntarily started com<strong>in</strong>g forward.Kedar has disclosed his status to his children and they feel comfortable question<strong>in</strong>ghim about it, for example, they ask him, “Father, if we eat together, will we getHIV?” He uses the act of answer<strong>in</strong>g such questions as opportunities to teach themabout transmission methods; the family, of course, eats meals together.7.5 Antiretroviral TreatmentAt the time of the survey, 66 per cent of the respondents (68% males, 64% females and 41%transgender people) were tak<strong>in</strong>g ART, and 48 per cent of the respondents (43% males, 53%females and 59% transgender people) were tak<strong>in</strong>g medications for prevent<strong>in</strong>g or treat<strong>in</strong>gopportunistic <strong>in</strong>fections. In addition, 67 per cent of the respondents currently not on ART wereconfident that ART would be easily and readily available to them whenever they needed it <strong>in</strong>the future (Table 7.9).Table 7.9 Access to antiretroviral treatmentCurrently tak<strong>in</strong>g antiretroviral treatmentMale(N = 424)(%)Female(N = 404)(%)TGperson(N = 27)(%)Total(N = 428)(%)Yes 70.0 63.6 40.7 65.9No 30.0 36.4 59.3 34.1Treat<strong>in</strong>g opportunistic <strong>in</strong>fectionscurrentlyMale(N = 421)(%)Female(N = 401)(%)TG person(N = 27)(%)Total(N = 822)(%)Yes 41.4 52.9 59.3 47.660 61