- Page 1 and 2:
SMA Fee Guide (for uninsured servic
- Page 3 and 4:
INTRODUCTION / PREAMBLEAn understan
- Page 5 and 6:
INTRODUCTION / PREAMBLE8. Classific
- Page 7 and 8:
INTRODUCTION / PREAMBLERequests fro
- Page 9 and 10:
INTRODUCTION / PREAMBLEa) Keep Pati
- Page 11 and 12:
SECTION A1:UNINSURED SERVICESIICHAR
- Page 13 and 14:
SECTION A1:UNINSURED SERVICESIIIRES
- Page 15 and 16:
SECTION A1:UNINSURED SERVICESIVMEDI
- Page 17 and 18:
SECTION A2:THIRD PARTY SERVICES AT
- Page 19 and 20:
SECTION A2:THIRD PARTY SERVICES AT
- Page 21 and 22:
SECTION A2:THIRD PARTY SERVICES AT
- Page 23 and 24:
SECTION A2:THIRD PARTY SERVICES AT
- Page 25 and 26:
SECTION A2:THIRD PARTY SERVICES AT
- Page 27 and 28:
SECTION A2:THIRD PARTY SERVICES AT
- Page 29 and 30:
SECTION A2:THIRD PARTY SERVICES AT
- Page 31 and 32:
SECTION A.4:GENERAL SERVICESProcedu
- Page 33 and 34:
SECTION A.4:GENERAL SERVICESFeeSpec
- Page 35 and 36: SECTION A.4:GENERAL SERVICESFee184A
- Page 37 and 38: SECTION A.4:GENERAL SERVICESFeeDopp
- Page 39 and 40: SECTION A.4:GENERAL SERVICESIndirec
- Page 41 and 42: SECTION A.4:GENERAL SERVICESthe sur
- Page 43 and 44: SECTION A.4:GENERAL SERVICESFee626A
- Page 45 and 46: SECTION A.4:GENERAL SERVICES(g) oth
- Page 47 and 48: SECTION A.4:GENERAL SERVICESFeeRemo
- Page 49 and 50: SECTION A.4:should keep appropriate
- Page 52 and 53: SECTION B:GENERAL PRACTICEFeeHospit
- Page 54 and 55: SECTION B:GENERAL PRACTICEEmergency
- Page 56 and 57: SECTION C:PAEDIATRICSProceduresAddi
- Page 58 and 59: SECTION D:INTERNAL MEDICINEVisits F
- Page 60 and 61: SECTION D:INTERNAL MEDICINEFee141D
- Page 62 and 63: SECTION D:INTERNAL MEDICINEFeeEvoke
- Page 64 and 65: SECTION D:INTERNAL MEDICINEFee284D
- Page 66 and 67: SECTION E:PSYCHIATRYFee62E Examinat
- Page 68 and 69: SECTION E:PSYCHIATRYPsychotherapyPs
- Page 70 and 71: SECTION F:DERMATOLOGYVisitsFee5F In
- Page 72 and 73: SECTION F:DERMATOLOGYFeeIntralesion
- Page 74 and 75: SECTION G:MEDICAL GENETICS^FeeCouns
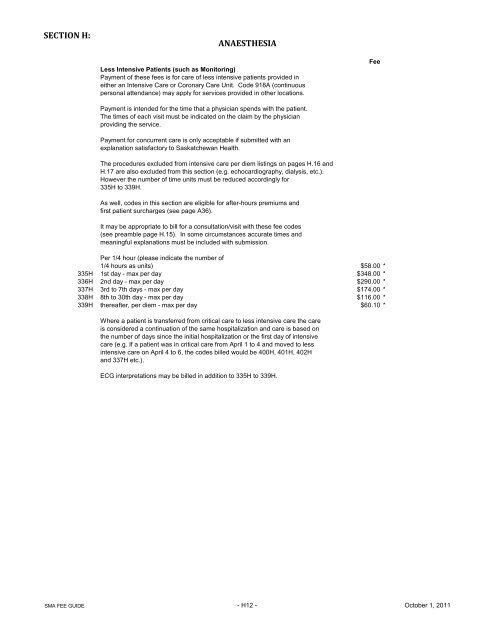
- Page 76 and 77: SECTION H:ANAESTHESIA"Standby" foll
- Page 78 and 79: SECTION H:ANAESTHESIAANAESTHESIA CA
- Page 80 and 81: SECTION H:ANAESTHESIA- Hysterosocpi
- Page 82 and 83: SECTION H:ANAESTHESIAFee132H Lumbar
- Page 84 and 85: SECTION H:ANAESTHESIA4. If Ventilat
- Page 88 and 89: SECTION I:CARDIOLOGYFee105I Full el
- Page 90 and 91: SECTION J:SURGICAL ASSISTANCEof ope
- Page 92 and 93: SECTION K:NEUROSURGERYVisits Fee An
- Page 94 and 95: SECTION K:NEUROSURGERYFeeAnaeExcisi
- Page 96 and 97: SECTION K:NEUROSURGERYFeeAnae211K T
- Page 98 and 99: SECTION K:NEUROSURGERYFeeAnaeFusion
- Page 100 and 101: SECTION K:NEUROSURGERYFeeAnae645K P
- Page 103 and 104: SECTION L:GENERAL SURGERYFeeAnaeHea
- Page 105 and 106: SECTION L:GENERAL SURGERYFeeAnae120
- Page 107 and 108: SECTION L:GENERAL SURGERYFeePeriton
- Page 109 and 110: SECTION L:GENERAL SURGERYFeeAnae215
- Page 111 and 112: SECTION L:GENERAL SURGERYFeeAnaeRup
- Page 113 and 114: SECTION L:GENERAL SURGERYFeeAnae387
- Page 115 and 116: SECTION L:GENERAL SURGERYFeeAnae860
- Page 117 and 118: SECTION L:GENERAL SURGERYFeeAnaePer
- Page 119 and 120: SECTION L:GENERAL SURGERYFeeAnae520
- Page 121 and 122: SECTION MORTHOPAEDIC SURGERYClassif
- Page 123 and 124: SECTION M:ORTHOPAEDIC SURGERYFeeAna
- Page 125 and 126: SECTION M:ORTHOPAEDIC SURGERY2. Unl
- Page 127 and 128: SECTION M:ORTHOPAEDIC SURGERYFeeAna
- Page 129 and 130: SECTION M:ORTHOPAEDIC SURGERYFeeAna
- Page 131 and 132: SECTION M:ORTHOPAEDIC SURGERYFeeAna
- Page 133 and 134: SECTION M:ORTHOPAEDIC SURGERYFeeAna
- Page 135 and 136: SECTION M:ORTHOPAEDIC SURGERYmuscul
- Page 137 and 138:
SECTION N:PLASTIC SURGERYVisits Fee
- Page 139 and 140:
SECTION N:PLASTIC SURGERY5. Abdomin
- Page 141 and 142:
SECTION N:PLASTIC SURGERYFeeAnae261
- Page 143 and 144:
SECTION N:PLASTIC SURGERYFeeAnae344
- Page 145 and 146:
SECTION N:PLASTIC SURGERYFeeAnaeEsc
- Page 147 and 148:
SECTION P:OBSTETRICS/GYNAECOLOGYVis
- Page 149 and 150:
SECTION P:OBSTETRICS/GYNAECOLOGYFee
- Page 151 and 152:
SECTION P:OBSTETRICS/GYNAECOLOGYFee
- Page 153 and 154:
SECTION P:OBSTETRICS/GYNAECOLOGYFee
- Page 155 and 156:
SECTION Q:NEUROLOGYVisitsFee3Q Comp
- Page 157 and 158:
SECTION Q:NEUROLOGYFee150Q Certific
- Page 159 and 160:
SECTION R:UROLOGICAL SURGERYProcedu
- Page 161 and 162:
SECTION R:UROLOGICAL SURGERYFeeAnae
- Page 163 and 164:
SECTION R:UROLOGICAL SURGERYFeeAnae
- Page 165 and 166:
SECTION R:UROLOGICAL SURGERYFee308R
- Page 167 and 168:
SECTION S:OPHTHALMOLOGYmuscles; con
- Page 169 and 170:
SECTION S:OPHTHALMOLOGYFee680S Infr
- Page 171 and 172:
SECTION S:OPHTHALMOLOGYFeeAnae52S D
- Page 173 and 174:
SECTION S:OPHTHALMOLOGYFeeAnaeSynec
- Page 175 and 176:
SECTION S:OPHTHALMOLOGYFeeAnae491S
- Page 177 and 178:
SECTION S:OPHTHALMOLOGYFeesAnae755S
- Page 179 and 180:
SECTION T:OTOLARYNGOLOGYFee430T Scr
- Page 181 and 182:
SECTION T:OTOLARYNGOLOGYFeeAnae292T
- Page 183 and 184:
SECTION T:OTOLARYNGOLOGYFeeAnae275T
- Page 185 and 186:
SECTION V:LABORATORY MEDICINEFee29V
- Page 187 and 188:
SECTION V:LABORATORY MEDICINESpecia
- Page 189 and 190:
SECTION V:LABORATORY MEDICINESpecia
- Page 191 and 192:
SECTION W:DIAGNOSTIC ULTRASOUNDMult
- Page 193 and 194:
SECTION X:DIAGNOSTIC RADIOLOGYFee9X
- Page 195 and 196:
SECTION X:DIAGNOSTIC RADIOLOGYTechn
- Page 197 and 198:
SECTION X:DIAGNOSTIC RADIOLOGYTechn
- Page 199 and 200:
SECTION X:DIAGNOSTIC RADIOLOGYSpeci
- Page 201 and 202:
SECTION X:DIAGNOSTIC RADIOLOGYFeeTh
- Page 203 and 204:
SECTION Z:NUCLEAR MEDICINEThis sect
- Page 205 and 206:
SECTION Z:NUCLEAR MEDICINETechnical
- Page 207 and 208:
Hand Surgery AppendixFeeAnaeCodeNer